#Gastroesophageal reflux disorder
Text
shoutout to other physically disabled people (esp. if you're also mentally disabled/ill) who are seen as not wanting to "help ourselves" because we can't make "simple" lifestyle changes,
who can't keep up with PT/OT on their own even if the exercises "just take 10 minutes" or generally can't keep up with regular exercise,
who aren't able to cut trigger foods out of our diets even if what they trigger is actively damaging our bodies/progressing certain things,
who use assistive devices, treatments, or aids that aren't technically "good for us" but they're all we have and we just want something, anything, to make our lives less miserable and aren't able to do much else
anything else where "just making this one change" would technically be beneficial but it's difficult to keep up with, or takes too much energy/takes executive function skills that we don't have, or conflicts w/ stuff in our lives that's not seen by others as important enough or significant (like sensory issues)
we're not "lazy" and we don't "just need to try harder," we're just not capable of "just doing" many of the same "simple" things that other people are, because we're disabled
#cripple punk#cpunk#hypotonia#gastroesophageal reflux disease#hypermobility spectrum disorder#j#body log
754 notes
·
View notes
Text
undiagnosed chronic gastro illness culture is idk whats wrong w me but i think its trying to kill me
#digestive disorders#chronic illness#gastroesophageal reflux disease#food intolerance#food allergies#irritable bowel syndrome#irritable bowel disease#stomach ulcer#crohn's disease
165 notes
·
View notes
Text
Title: The Evolution in Probiotic Therapy

#gastro#vegan#“ ”gluten-free#“ ”desserts#“ ”Italian cuisine#“ or ”quick meals“ to help users find specific types of content.#Restaurant Review Platforms: Platforms like Yelp or TripAdvisor might use tags to help users find restaurants that match certain criteria#such as#sushi#“ ”burgers#“ ”healthy#“ ”family meals#“ or ”late-night.“#Cookbooks and Magazines: Tags help in organizing recipes and articles into easily searchable topics such as#“Gastro” is a shorthand that can refer to various topics related to the digestive system#food#or gastrointestinal medicine. Here are a few different contexts in which the term “gastro” might be used:#1. Gastroenterology#Gastroenterology is a branch of medicine focused on the digestive system and its disorders. Gastroenterologists diagnose and treat conditio#including:#Esophagus#Stomach#Small and large intestines#Liver#Gallbladder#Pancreas#Common conditions treated by gastroenterologists include:#Gastroesophageal reflux disease (GERD)#Irritable bowel syndrome (IBS)#Crohn's disease
0 notes
Text
#Abdominal Gastroenterology#Achalasia#Anorectal Disorders#Barret’s esophagus#Bezoars & Foreign Bodies#biliary tract disease#Case Reports in Gastroenterology#Colitis#Colon and bowel cancers#Colon polyps#Diverticular Disease#Esophageal cancers#Esophageal GI Disorders#Functional GI Disorders#Gallbladder stones and cancer#Gastric & Peptic Disorders#Gastric cancers#Gastroenterological Diseases#Gastroesophageal reflux#Hepatic Disorders#Hepatitis#Hepatology#Inflammatory Bowel Disease#Irritable Bowel Syndrome (IBS)#Malabsorption Syndrome#Neurogasteroenterology#Nutrition#Nutritional problems and malabsorption#Pancreas and Biliary Tract#Pancreatic cancers
0 notes
Text
What is Idiopathic Mast Cell Activation Syndrome?
Idiopathic Mast cell activation syndrome (MCAS) is one of several mast cell disorders. MCAS occurs when there are a normal number of mast cells in a person's body but they over-release mast cell mediators causing random allergic reactions in multiple systems of the body. MCAS is incredibly common being present in an estimated 17% of the population.
Symptoms
MCAS symptoms are incredibly varied and always occur in multiple systems of the body. Anaphylaxis is common.
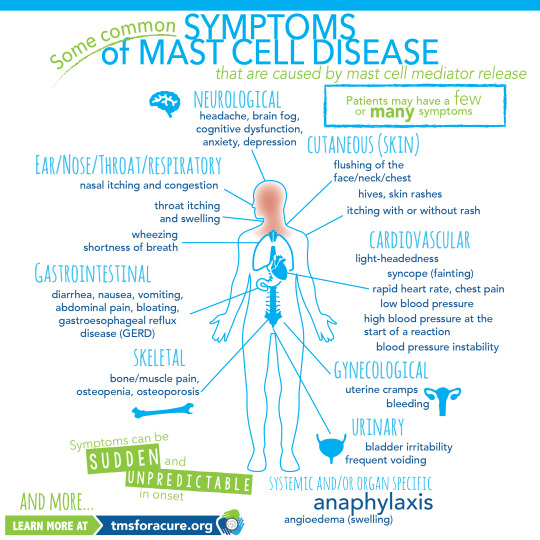
[ID: A graphic labeled "Some common symptoms of Mast Cell Disease" A graphic of a person standing in the center with multiple organs visible is shown. Around the person are lines pointing to specific areas of the body labeled with the body system and symptoms. Clockwise these read "Neurological headache, brain fog, cognitive dysfunction, anxiety, depression Cutaneous (Skin) flushing of the face/neck/chest, hives, skin rashes, itching with or without rash Cardiovascular light-heartedness, syncope (fainting), rapid heart rate, chest pain, low blood pressure, high blood pressure at the start of a reaction, blood pressure instability Gynecological uterine cramps, bleeding Urinary bladder irritability, frequent voiding Systemic and/or organ specific Anaphylaxis angioedema (swelling) Skeletal bone/muscle pain, osteopenia, osteoporosis Gastrointestinal diarrhea, nausea, vomiting, abdominal pain, bloating, gastroesophageal reflux disease (GERD) Ear/Nose/Throat/Respiratory nasal itching and congestion, throat itching and swelling, wheezing, shortness of breath and more" In the bottom left corner "Symptoms can be sudden and unpredictable in onset learn more at tmsforacure.org"]
MCAS symptoms are specifically not allergies. the reactions may look like allergies but the two are not the same and MCAS is not a condition meaning "many allergies" While MCAS can have some consistent triggers one of the defining features of the disease is that reactions are random and happen unpredictably.
Anaphylactic shock is not a requirement for diagnosis.
Diagnosis
MCAS is diagnosed by an immunologist. It is in part a diagnosis of exclusion and requires ruling out both allergies and systemic mastocytosis as well as other conditions such as certain types of tumors.
Diagnostic criteria for MCAS is debated. Some immunologists follow the symptom-based diagnosis approach in which case the diagnostic criteria are:
Recurring and severe anaphylactic-like episodes that involve more than one organ system
and
Positive response to mast cell stabilizing or mediator medications anaphylaxis-type symptoms
Others follow diagnostic criteria based on laboratory findings. In this case the diagnostic criteria are:
Episodic symptoms consistent with mast cell mediator release affecting two or more organ systems evidenced as follows:
Skin: urticaria, angioedema, flushing
Gastrointestinal: nausea, vomiting, diarrhea, abdominal cramping
Cardiovascular: hypotensive syncope or near syncope, tachycardia
Respiratory: wheezing
Naso-ocular: conjunctival injection, pruritus, nasal stuffiness
and
A decrease in the frequency or severity; or resolution of symptoms with anti-mediator therapy: H1 and H2 histamine receptor antagonists, anti-leukotriene medications (cysLT receptor blockers or 5-LO inhibitor), or mast cell stabilizers (cromolyn sodium)
and
Evidence of an elevation in a validated urinary or serum marker of mast cell activation: Documentation of elevation of the marker above the patient’s baseline during a symptomatic period on at least two occasions; or if baseline tryptase levels are persistently >15ng, documentation of elevation of the tryptase above baseline on one occasion. Total serum tryptase is recommended as the markers of choice; less specific (also from basophils) 24 hour urine histamine metabolites, or 11-beta-prostaglandin F2.
and
Primary (clonal) and secondary disorders of mast cell activation ruled out.
These are not all proposed diagnostic criteria as the subject is heavily debated. Generally, a laboratory-confirmed MCAS diagnosis is considered more legitimate.
Treatment
MCAS is a very treatable condition. Generally treatment follows a path from antihistamines -> mast cell mediators -> biologics.
Epipens are given to MCAS patients with a history of anaphylaxis.
Antihistamines are divided into 2 categories: H1 antagonists and H2 antagonists. These categories are determined based on the histamine receptor each one targets.
H1 antagonists mostly deal with systemic and cutaneous symptoms. H1 antagonists are also further divided into first and second generation antihistamines. first generation antihistamines include diphenhydramine (Benadryl) and Hydroxyzine. These tend to cause drowsiness. With second generation H1 antagonists cause fewer side effects and include drugs like loratadine (Claritin) and cetirizine (Zyrtec)
H2 antagonists primarily affect the gastrointestinal tract and include medications like famotidine (pepcid)
Typically when treating MCAS a person will be put on both a second generation H1 antagonist and an H2 antagonist.
When antihistamines do not treat symptoms well enough the next step is a mast cell mediator. The most common mast cell mediator is cromolyn sodium which is available by prescription only. (this is technically available OTC but it is at 1/50th the dose used for MCAS) Mast cell mediators work by preventing the degranulation of mast cells in the first place.
When both antihistamines and mast cell mediators are insufficient someone with MCAS might be prescribed a biologic such as Xolair to treat their remaining symptoms.
Sources:
American Academy of Allergy, Asthma, and Immunology
Mast Cell Hope
Mast Cell Activation Syndrome: Proposed Diagnostic Criteria
#mast cell activation syndrome#mcas#mast cell disease#mast cell activation disorder#mcad#chronic illness#chronically ill#physical disability#physically disabled
76 notes
·
View notes
Note
Is autism and bowel/digestive problems a popular thing? Does anyone know what causes it or what can help? I have been to doctors and hospitals so many times over the years and never get any results or help.
Hi there,
Unfortunately people with ASD have some difficulty with the gastrointestinal tract. I’ll leave some excerpts from articles below. Warning: they are very long:
Of the many medical comorbidities associated with ASD, GI distress has gained significant attention because of its reported prevalence and association with symptom severity. In fact, out of the children that Leo Kanner described in his landmark article defining “infantile autism” are described as having eating/feeding or dietary problems, supporting an early association of ASD with GI issues. Of the GI problems reported in subsets of autistic individuals, the most common are chronic constipation, diarrhea, and abdominal pain. Gastroesophageal reflux, bloody stools, vomiting, and gaseousness are also elevated in some autistic individuals, as are signs of GI inflammation, such as lymphoid nodular hyperplasia, complement activation, and elevated pro-inflammatory cytokines, and intestinal pathologies, such as enterocolitis, gastritis, and esophagitis. Increased intestinal permeability is linked to autism and hypothesized to have detrimental effects not only on intestinal barrier integrity but also on the systemic metabolome, with potential for translocation of intestinal metabolites or bacteria and consequent immune activation. Furthermore, food allergies, altered dietary nutrient intake, and metabolic disruptions have been associated with ASD.10–12 Autistic individuals with comorbid GI abnormalities exhibit altered carbohydrate digestion. Taken together, the variety of GI conditions, dietary issues, and enteric immune abnormalities reported in ASD individuals suggests that GI dysfunction can contribute to the manifestation of core symptoms of autism.
Characterized by difficulties with socializing, and often accompanied by repetitive behaviors, this neurodevelopmental disorder harbors many mysteries.
Despite its prevalence and a glut of research, the causes behind ASD are still not fully understood.
Although ASD primarily impacts the brain, over recent years, links with other systems have become clear — in particular, gastrointestinal (GI) issues seem to occur more often in individuals with ASD than in the rest of the population.
In one study, compared with typically developing (TD) children, those with ASD were six to eight times more likely to report GI symptoms such as bloating, constipation, and diarrhea.
Other studies have shown that children with ASD who experience GI problems are more likely to have more severe symptoms of ASD. Also, treating the GI symptoms can sometimes relieve the behavioral and social symptoms of ASD.
Interestingly, behavioral issues are found alongside other conditions that impact the gut. For instance, people with celiac disease are more likely to have autism-like traits and other psychological symptoms. The gut and behavior seem tied together in some way.
According to many researchers, the GI issues that come with ASD might be due to two factors: firstly, inappropriate immune activation causing inflammation of the tract; and, secondly, differences in the types of gut bacteria that are present.
However, the picture is still incredibly murky, and studies produce differing results, finding different types of inflammation and various changes in gut bacteria.
Children with autism experience more gastrointestinal symptoms
Gastrointestinal concerns are frequently reported by parents of children with autism spectrum disorder (ASD). Researchers from the UC Davis MIND Institute evaluated the presence of GI symptoms in preschool-aged children with and without autism.
The study included 255 (184 males/71 females) children with ASD between two and 3-5 years of age and 129 (75 males/54 females) typically developing children in the same age group. Pediatricians specializing in autism interviewed caregivers during the children’s medical evaluation. They asked the parents how often their children experienced GI symptoms such as difficulty swallowing, abdominal pain, bloating, diarrhea, constipation, painful stooling, vomiting, difficulty swallowing, blood in stool and blood in vomit.
The researchers grouped children in two categories: those who experienced one or more GI symptom and those who never or rarely had GI symptoms in the last three months. They compared the children in the two groups on measures of developmental, behavioral and adaptive functioning.
The study found that preschool-aged children with ASD were 2-7 times more likely to experience GI symptoms than their typically developing peers. In fact, almost 50% of children with ASD reported frequent GI symptoms - compared to 18% of children with typical development. Around 30% of the children with ASD experienced multiple GI symptoms.
I hope these sources can help. I have GI issues too and have to resort to stool softener
…
Anyway, thank you for the inbox. I hope you have a wonderful day/night. ♥️
66 notes
·
View notes
Text
𝘼-𝙕 𝙇𝙄𝙎𝙏 𝙊𝙁 𝘿𝙄𝙎𝙀𝘼𝙎𝙀𝙎/𝙄𝙇𝙇𝙉𝙀𝙎𝙎𝙀𝙎 𝙁𝙊𝙍 𝙎𝙄𝘾𝙆𝙁𝙄𝘾/𝙒𝙃𝙐𝙈𝙋
— A
Anemia.
Adenomyosis.
Asthma.
Arterial thrombosis.
Allergies.
Anxiety.
Angel toxicosis ( fictional ).
Acne.
Anorexia nervosa.
Anthrax.
Atma virus ( fictional ).
ADHD.
Agoraphobia.
Astrocytoma.
AIDS.
— B
Breast cancer.
Bunions.
Borderline personality disorder.
Botulism.
Barrett's esophagus.
Bowel polyps.
Brucellosis.
Bipolar disorder.
Bronchitis.
Bacterial vaginosis.
Binge eating disorder.
— C
Crohn's disease.
Conjunctivitis.
Coronavirus disease.
Coeliac disease.
Chronic migranes.
Coup.
Cushing syndrome.
Cystic fibrosis.
Cellulitis.
Coma.
Cooties ( fictional ).
COPD.
Chickenpox.
Cholera.
Cerebral palsy.
Chlamydia.
Constipation.
Cancer.
Common cold.
Chronic pain.
— D
Diabetes.
Dyslexia.
Dissociative identify disorder.
Dengue fever.
Delirium.
Deep vein thrombosis.
Dementia.
Dysthimia.
Diphtheria.
Diarrhoea.
Disruptive mood dysregulation disorder.
Dyspraxia.
Dehydration.
— E
Ebola.
Endometriosis.
Epilepsy.
E-coli.
Ectopic pregnancy.
Enuresis.
Erectile dysfunction.
Exzema.
— F
Fusobacterium infection.
Filariasis.
Fibromyalgia.
Fascioliasis.
Fever.
Food poisoning.
Fatal familial insomnia.
— G
Gonorrhoea.
Ganser syndrome.
Gas gangrene.
Giardiasis.
Gastroesophageal reflux disease.
Gall stones.
Glandular fever.
Greyscale ( fictional ).
Glanders.
— H
Hookworm infection.
Hand, foot and mouth disease.
Hypoglycaemia.
Herpes.
Headache.
Hanahaki disease ( fictional ).
Hyperhidrosis.
Heat stroke.
Heat exhaustion.
Heart failure.
High blood pressure.
Human papillomavirus infection.
Hypersomnia.
HIV.
Heart failure.
Hay fever.
Hepatitis.
Hemorrhoids.
— I
Influenza.
Iron deficiency anemia.
Indigestion.
Inflammatory bowel disease.
Insomnia.
Irritable bowel syndrome.
Intercranial hypertension.
Impetigo.
— K
Keratitis.
Kidney stones.
Kidney infection.
Kawasaki disease.
Kaposi's sarcoma.
— L
Lyme disease.
Lassa fever.
Low blood pressure.
Lupus.
Lactose intolerance.
Lymphatic filariasis.
Leprosy.
— M
Measles.
Mad cow disease.
Mumps.
Major depressive disorder.
Malaria.
Malnutrition.
Motor neurone disease.
Mutism.
Mouth ulcer.
Monkeypox.
Multiple sclerosis.
Meningitis.
Menopause.
Mycetoma.
— N
Norovirus.
Nipah virus infection.
Narcolepsy.
Nosebleed.
Nocardiosis.
— O
Obsessive-compulsive disorder.
Osteoporosis.
Ovarian cyst.
Overactive thyroid.
Oral thrush.
Otitis externa.
— P
Pancreatic cancer.
Pneumonia.
Pelvic inflammatory disease.
PICA.
Premenstrual dysphoric disorder.
Psoriasis.
Parkinson's disease.
Panic disorder.
Polycystic ovarian syndrome.
Plague.
Postpartum depression.
Pediculosis capitis.
Psychosis.
Post-traumatic stress disorder.
— Q
Q fever.
Quintan fever.
— R
Rubella.
Rabbit fever.
Rotavirus infection.
Ringworm.
Restless legs syndrome.
Rhinovirus infection.
Rosacea.
Relapsing fever.
Rheumatoid arthritis.
Rabies.
— S
Shingles.
Sore throat.
Stutter.
Separation anxiety disorder.
Smallpox.
Scoliosis.
Septic shock.
Shigellosis.
Sepsis.
Social anxiety disorder.
Stroke.
Scarlet fever.
Schizophrenia.
Sleep apnea.
Sun burn.
Syphilis.
Sickle cell disease.
Scabies.
Selective mutism.
Salmonella.
Sensory processing disorder.
— T
Thyroid cancer.
Tuberculosis.
Thirst.
Trichuriasis.
Tinea pedis.
Tourette's syndrome.
Trachoma.
Tetanus.
Toxic shock syndrome.
Tinnitus.
Thyroid disease.
Typhus fever.
Tonsillitis.
Thrush.
— U
Urinary tract infection.
Underactive thyroid.
— V
Valley fever.
Vertigo.
Vomiting.
— W
White piedra.
Withdrawal.
Whooping cough.
West nile fever.
— X
Xerophthalmia.
— Y
Yersiniosis.
Yellow fever.
— Z
Zygomycosis.
Zika fever.
Zeaspora.
19 notes
·
View notes
Note
bad stomach gang
reflux gang 😔
FUCK YEAH!!!!!!!!!!!!!!!!!!!!! GASTROESOPHAGEAL REFLUX DISORDER GANG!!!!!!!!!!!!!!!!!!!!!! WHERE YOU AT❗❗💥💥❗💥❗💥💥❗💥
#asks#i'm so glad i made himawari have the same issues i do#(duh she's my sona)#since literally NO ONE covers up gerd in media#i have to do it myself. himawari is the gerd leader now
13 notes
·
View notes
Text

GERD: gastroesophageal reflux disease.
* Patients on twice-daily diuretics can take their second dose in the afternoon rather than the evening.
¶ Urinating while sitting comfortably on the toilet (men included), leaning slightly forward, and then waiting for 20 to 30 seconds to urinate again.
Δ Good sleep hygiene includes sleeping in a quiet room with low lighting and appropriate temperature, avoiding nighttime use of electronic devices, and avoiding daytime naps.
◊ Patients should be referred to a physical therapist with expertise in pelvic floor rehabilitation.
------------------------
Definition and goals of management – Nocturia is a symptom, defined as any waking at night to void, most often considered clinically significant if a patient voids two or more times nightly. It is important to try to reduce the bother caused by the nocturia in addition to reducing nocturia episodes. (See 'Definition/Diagnosis' above and 'Management' above.)
●Recognition of underlying causes – Nocturia may be caused by conditions or disorders that result in low bladder volume voids, nocturnal polyuria, or sleep disturbances. Certain medical conditions may contribute to nocturia and should be treated as part of initial management. Many patients have multiple etiologies. (See 'Pathophysiology and associated conditions' above and 'Management' above.)
●Evaluation – Evaluation for nocturia should focus on patterns of fluid intake, other urinary symptoms, symptoms of possible underlying causes, and a focused physical examination. (See 'Evaluation' above.)
•A frequency-volume chart (ie, a voiding diary) will be helpful in determining the contributing causes of nocturia. Nocturnal polyuria is defined as the excretion of ≥35 percent of the 24-hour urine output during the hours of sleep (form 1). (See 'Frequency-volume chart' above.)
●Initial management – Initial measures should include adjustments in timing of fluid intake to earlier in the day, reducing salt intake if excessive, and eliminating nighttime diuretic use if present. A urinal or commode near the bed may be helpful. Fall risk at night should be considered (algorithm 1). (See 'Initial measures' above.)
●Pelvic floor muscle exercises – We suggest pelvic floor exercises for all patients (Grade 2B). Primary care providers should refer patients to physical therapists who specialize in this training. (See 'Behavioral treatment, including pelvic floor muscle exercises' above.)
●Pharmacologic treatment – Suggested initial treatment trials for nocturia include the following (algorithm 2):
•In men with nocturia related to benign prostatic hyperplasia (BPH), we suggest trials of alpha-1-adrenergic antagonists with or without 5-alpha reductase inhibitors (Grade 2B). (See 'Men with benign prostatic hyperplasia' above.)
•In patients without BPH who have low-volume voids, we suggest trials of bladder muscle relaxants (Grade 2C). (See 'Initial monotherapy: bladder relaxant therapies' above.)
•For postmenopausal women with continued nocturia despite a bladder muscle relaxant, we offer topical vaginal estrogen either alone or in combination with other therapies. (See 'Vaginal estrogen therapy (women only)' above.)
Because each of these therapies is associated with only a modest reduction in the number of nighttime voids and also has potential for side effects, many patients may choose no pharmacologic therapy.
●Refractory nocturia – For patients with refractory nocturia and who are <65 years of age, we consider treatment with desmopressin. Studies suggest that desmopressin has a small effect on nighttime voiding frequency that is of uncertain clinical significance. Baseline sodium levels must be normal, and patients must be able to recognize and report subtle fluid status changes and also be willing to undergo frequent monitoring of sodium levels in order to avoid severe hyponatremia. Desmopressin is a potentially inappropriate medication according to Beers criteria for medications for older adults. (See 'Desmopressin' above and "Drug prescribing for older adults", section on 'Beers criteria'.)
2 notes
·
View notes
Text
Choosing the Right Gastrointestinal Tract Drug – Factors to Consider
The gastrointestinal (GI) tract is a complex system responsible for digestion and absorption of nutrients. Given its critical function, disorders affecting the GI tract can significantly impact overall health and quality of life. Selecting the right medication to treat these conditions is essential for effective management and recovery. Centurion HealthCare, a leading gastrointestinal tract drugs supplier in India, offers a range of high-quality medications designed to address various GI disorders. In this article, we will explore the factors to consider when choosing the right gastrointestinal tract drug, and why Centurion HealthCare stands out in the best pharmaceutical industry in India.

Understanding Gastrointestinal Tract Disorders
GI tract disorders encompass a wide range of conditions affecting different parts of the digestive system, including the esophagus, stomach, intestines, liver, pancreas, and gallbladder. Common GI disorders include:
Gastroesophageal Reflux Disease (GERD)
Peptic Ulcer Disease
Irritable Bowel Syndrome (IBS)
Inflammatory Bowel Disease (IBD)
Hepatitis
Pancreatitis
Each condition requires specific treatment strategies and medications to manage symptoms, promote healing, and prevent complications.
Factors to Consider When Choosing a Gastrointestinal Tract Drug
Choosing the right drug for treating GI disorders involves multiple factors, including the specific condition, the patient’s medical history, and potential side effects. Here are key considerations:
1. Accurate Diagnosis
An accurate diagnosis is the first step in selecting the appropriate medication. Physicians use various diagnostic tools such as endoscopy, colonoscopy, imaging studies, and laboratory tests to identify the specific GI disorder. Understanding the underlying cause and severity of the condition is crucial for effective treatment.
2. Mechanism of Action
Different gastrointestinal tract drugs work through various mechanisms to achieve therapeutic effects. Understanding how a drug works helps in selecting the most suitable option. Common mechanisms include:
Antacids: Neutralize stomach acid, providing quick relief from heartburn and indigestion.
Proton Pump Inhibitors (PPIs): Reduce the production of stomach acid, effective in treating GERD and peptic ulcers.
H2 Receptor Antagonists: Decrease acid production by blocking histamine receptors in the stomach lining.
Prokinetics: Enhance gut motility, useful in conditions like gastroparesis.
Antispasmodics: Relieve intestinal cramps and spasms, often used in IBS treatment.
Anti-inflammatory Drugs: Reduce inflammation in the GI tract, essential for managing IBD.
3. Efficacy and Safety
The efficacy and safety profile of a drug are critical factors in the decision-making process. Clinical trials and real-world studies provide valuable information on a drug’s effectiveness and potential side effects. Physicians must weigh the benefits against the risks to ensure the chosen medication offers the best possible outcome for the patient.
4. Patient-Specific Factors
Each patient is unique, and various individual factors can influence drug selection. These include:
Age: Certain drugs may be more suitable for children, adults, or the elderly.
Medical History: Pre-existing conditions, such as kidney or liver disease, can affect drug metabolism and tolerance.
Allergies: Patients with known drug allergies must avoid medications that could trigger adverse reactions.
Concurrent Medications: Drug interactions can impact efficacy and safety, requiring careful consideration of all medications the patient is currently taking.
5. Route of Administration
The route of administration can affect the drug’s efficacy and patient compliance. Common routes for GI drugs include:
Oral: Tablets, capsules, and liquids are convenient for most patients.
Intravenous: Used in severe cases or when oral administration is not feasible.
Topical: Suppositories and enemas are used for localized treatment in the lower GI tract.
6. Cost and Availability
Cost can be a significant factor, especially for long-term treatments. Generic versions of drugs often offer the same efficacy as brand-name medications at a lower cost. Availability of the drug in the local market is also crucial to ensure uninterrupted treatment.
Centurion HealthCare: Leading the Way in GI Tract Drug Supply
Centurion HealthCare has established itself as a premier gastrointestinal tract drugs supplier in India, renowned for its commitment to quality, innovation, and patient care. Here’s why Centurion HealthCare is a trusted name in the best pharmaceutical industry in India:
1. Comprehensive Product Range
Centurion HealthCare offers a wide range of gastrointestinal tract drugs, catering to various GI disorders. Their product portfolio includes antacids, PPIs, H2 receptor antagonists, prokinetics, antispasmodics, and anti-inflammatory medications, ensuring comprehensive treatment options for healthcare providers.
2. Quality Assurance
Quality is at the heart of Centurion HealthCare’s operations. The company adheres to stringent quality control measures, from raw material sourcing to final product testing, ensuring that every medication meets international standards for safety and efficacy.
3. Research and Development
Centurion HealthCare invests heavily in research and development to stay at the forefront of pharmaceutical innovation. Their R&D team continuously works on developing new formulations and improving existing products to address emerging healthcare needs.
4. Patient-Centric Approach
Understanding that each patient is unique, Centurion HealthCare adopts a patient-centric approach in drug development and supply. Their medications are designed to provide maximum therapeutic benefit with minimal side effects, enhancing patient outcomes and quality of life.
5. Global Reach
As a leading gastrointestinal tract drugs supplier, Centurion HealthCare has a robust distribution network that ensures their products are available not only across India but also in international markets. Their commitment to excellence has earned them a reputation as a reliable partner for healthcare providers worldwide.
6. Affordability
Centurion HealthCare is dedicated to making high-quality medications accessible to all. Their cost-effective solutions, including generic versions of popular GI drugs, help reduce the financial burden on patients while maintaining high standards of care.
Conclusion
Choosing the right gastrointestinal tract drug involves careful consideration of various factors, including accurate diagnosis, mechanism of action, efficacy, safety, patient-specific factors, route of administration, and cost. Centurion HealthCare, as a leading gastrointestinal tract drugs supplier in India, excels in providing high-quality, effective medications that cater to the diverse needs of patients with GI disorders.
With a commitment to quality, innovation, and patient-centric care, Centurion HealthCare stands out in the best pharmaceutical industry in India. Their comprehensive product range, stringent quality assurance, advanced R&D, global reach, and affordability make them a trusted partner for healthcare providers seeking reliable solutions for GI tract disorders.
By choosing Centurion HealthCare, you can be confident in the quality and efficacy of the medications you are prescribing or consuming, ensuring the best possible outcomes for gastrointestinal health.
#Best Indian pharma industry 2024#Best pharmaceutical industry in India#Gastrointestinal tract drugs supplier#Gastrointestinal tract drugs supplier in India
3 notes
·
View notes
Text
What Green Tea with Turmeric goodis said to be good for.
One being strengthening the body's defense. 2 an environment in the body that supports overall immune health.But who should not drink this tea,those with gallbladder problems, bleeding disorders, diabetes, gastroesophageal reflux disease (GERD), infertility, iron deficiency, liver disease, hormone-sensitive conditions, and arrhythmia. Pregnant women and those who are going to undergo surgery should not use turmeric. Hmm I guess one of these would apply to me i'm type 2 diabetes shucks.I will ask my doctor me while since I have the tea ( had it for over a month ) I want to try it anyway for a few days or week even. hmm seems like a person with certain conditions or health issues can't consume almost anything darn it!
So many possibilities with this tea .. like it is known to Improve heart health- Curcumin being a powerful antioxidant inhibits the oxidation of LDL Cholesterol , thus preventing the deposit of cholesterol on the walls of the blood vessels of the heart. It is also known to regulate blood pressure, blood clotting, and ensure proper cardiac functioning.
3 notes
·
View notes
Text
GERD Symptoms: Causes, Treatment, and How to Manage Them
GERD, or gastroesophageal reflux disease, is a common digestive disorder that affects millions of people worldwide. It can have a significant impact on daily life, causing discomfort and disrupting daily activities. This article aims to provide valuable information on the causes, treatment, and management of GERD symptoms. By understanding the symptoms and triggers of GERD, you can take steps to manage and prevent them, leading to a better quality of life. Whether you have been recently diagnosed with GERD or are experiencing occasional heartburn, this article will provide you with the essential knowledge to take control of your symptoms. Let's dive in.

When to See a Doctor
Occasional heartburn is a common occurrence, but when it becomes a frequent and persistent issue, it may be a sign of a more serious condition – GERD. If you experience frequent heartburn or other symptoms of GERD, it is important to seek medical attention. Some warning signs that you should not ignore include difficulty swallowing and unexplained weight loss. These may indicate a more advanced stage of GERD or other complications. Seeking medical advice is crucial to properly diagnose and treat GERD. Your doctor may recommend lifestyle changes, over-the-counter or prescription medications, or other treatment options depending on the severity of your symptoms. Remember, early detection and treatment can help manage GERD and improve your quality of life. Don't hesitate to talk to your doctor if you experience symptoms of GERD.
You can consult with our dedicated team of doctors who are experts in treating various Digestive Disorders.
Read more
2 notes
·
View notes
Text
hows the tummy hurty fandom doing
#digestive disorders#chronic illness#stomach problems#irritable bowel syndrome#irritable bowel disease#gastroesophageal reflux disease#food intolerance#food allergies#stomach ulcer#crohn's disease#gastroparesis#celiac disease#dysphagia#pancreatitis#diverticulosis#delayed stomach emptying
142 notes
·
View notes
Text
Unveiling The Gastric Problems: Common Symptoms And Their Causes
Gastric problems, ranging from mild discomfort to severe pain, can significantly impact daily life. Understanding the symptoms and their underlying causes is crucial for effective management and treatment. In this article, we'll explore seven common symptoms of gastric problems and delve into their potential causes, providing valuable insights for better health and well-being.

Abdominal Pain: Abdominal pain is a hallmark symptom of various gastric issues, including gastritis, ulcers, and gastroesophageal reflux disease (GERD). The pain may vary in intensity and location, ranging from a dull ache to sharp, stabbing sensations. Gastric ulcers, caused by the erosion of the stomach lining, often result in a burning pain in the upper abdomen. GERD, characterized by the reflux of stomach acid into the esophagus, can cause a burning sensation in the chest, known as heartburn.
Bloating and Gas: Excessive gas and bloating are common complaints associated with gastric problems. Gas can accumulate in the digestive tract due to factors such as swallowing air, bacterial fermentation of undigested food, or impaired digestion. Bloating, characterized by a feeling of fullness or tightness in the abdomen, often accompanies excessive gas production. Conditions like irritable bowel syndrome (IBS) and small intestinal bacterial overgrowth (SIBO) are frequently implicated in chronic bloating and gas.
Nausea and Vomiting: Nausea and vomiting are symptoms that can occur in various gastric disorders, including gastritis, gastroparesis, and peptic ulcers. Gastritis, inflammation of the stomach lining, can trigger nausea and vomiting, particularly after meals or when the stomach is empty. Gastroparesis, a condition characterized by delayed stomach emptying, may lead to persistent nausea and vomiting, especially after consuming solid foods. Peptic ulcers, open sores in the stomach or duodenum, can cause nausea and vomiting if they irritate the stomach lining.
Indigestion (Dyspepsia): Indigestion, also known as dyspepsia, encompasses a range of symptoms, including discomfort or pain in the upper abdomen, bloating, and a feeling of fullness during or after meals. It can occur as a result of various factors, such as overeating, eating too quickly, or consuming spicy or fatty foods. Gastric disorders like GERD, gastritis, and peptic ulcers can also manifest as indigestion. Persistent or recurrent indigestion warrants medical evaluation to identify and address the underlying cause.
Acid Reflux: Acid reflux occurs when stomach acid flows back into the esophagus, causing a burning sensation in the chest (heartburn) and a sour taste in the mouth. It is a common symptom of GERD, a chronic condition characterized by frequent episodes of acid reflux. Certain dietary and lifestyle factors, such as consuming acidic or fatty foods, smoking, and obesity, can exacerbate acid reflux. In some cases, structural abnormalities like a hiatal hernia may contribute to the development of GERD.
Loss of Appetite: A decreased appetite, or anorexia, can be a symptom of various gastric disorders, including gastritis, peptic ulcers, and inflammatory bowel disease (IBD). Gastritis, characterized by inflammation of the stomach lining, can lead to a loss of appetite due to discomfort or nausea associated with eating. Peptic ulcers, particularly those located in the stomach, can cause a feeling of early satiety or discomfort after meals, leading to reduced food intake. Inflammatory bowel disease, which includes Crohn's disease and ulcerative colitis, can affect the entire digestive tract and cause appetite loss.
Changes in Bowel Habits: Changes in bowel habits, such as diarrhea, constipation, or alternating episodes of both, can indicate underlying gastric issues. Conditions like IBS, characterized by abdominal pain and altered bowel habits without any detectable structural abnormalities, often present with diarrhea, constipation, or a combination of both. Inflammatory conditions like Crohn's disease and ulcerative colitis can cause diarrhea, often accompanied by abdominal pain, rectal bleeding, and weight loss. Constipation may occur due to factors such as inadequate fiber intake, dehydration, or certain medications.
Gastric problems can manifest in various ways, ranging from abdominal pain and bloating to acid reflux and changes in bowel habits. Identifying the symptoms and understanding their underlying causes are essential steps in managing gastric disorders effectively. If you experience persistent or severe symptoms, it is important to seek medical advice for proper evaluation and treatment. With the right approach, many gastric issues can be effectively managed, allowing for improved quality of life and overall well-being.
3 notes
·
View notes
Text
Recognizing Heartburn: Causes, Symptoms, and Effective Therapy Options
""
Indigestion, additionally referred to as gastroesophageal reflux disease (GERD), is a typical digestive system disorder that affects numerous people worldwide. It takes place when the stomach acid recedes into the esophagus, creating a range of unpleasant signs. Comprehending the causes and signs of acid reflux is essential for taking care of and treating this problem effectively.One of the key
causes of indigestion is a malfunctioning reduced esophageal sphincter(LES), a muscular valve that opens to permit food and drink to go into the tummy and near avoid belly acid from flowing back up. When the LES is weak or relaxes unusually, it allows belly acid to stream right into the esophagus, bring about acid reflux. Other factors that can add to indigestion include weight problems, hiatal hernia, maternity, particular medications, smoking, and a diet high in fatty or hot foods. Recognizing the triggers that intensify your signs and symptoms can help you make way of life adjustments and avoid future episodes of acid reflux.Acid reflux can show up in a selection of symptoms, including heartburn, regurgitation, breast discomfort, problem ingesting, persistent coughing, and hoarseness. If left unattended, indigestion can cause extra severe issues such as esophagitis, abscess, strictures, and even an increased risk of developing esophageal cancer cells. Fortunately, there are various treatment alternatives readily available to manage acid reflux successfully. Lifestyle adjustments, such as preserving a healthy and balanced weight, staying clear of trigger foods, raising the head of the bed, and quitting smoking, can substantially minimize signs and symptoms. Over the counter antacids and acid reducers can give short-lived alleviation. Nevertheless, for even more consistent or extreme cases, prescription medicines or medical interventions might be necessary to control heartburn and prevent additional difficulties. It is crucial to speak with a healthcare professional for an exact diagnosis and personalized treatment strategy customized to your particular demands.
Read more here Comment Apparaître en Premier sur Google Maps
2 notes
·
View notes
Text
Understanding Indigestion: Reasons, Symptoms, and Effective Home Remedies
Indigestion, also recognized as gastroesophageal reflux condition (GERD), is a typical digestion condition that impacts countless people worldwide. It happens when tummy acid flows back into the esophagus, creating a variety of uneasy signs and symptoms. Recognizing the reasons and symptoms of indigestion is critical for effective management and prevention of this condition.There are several
elements that can add to the development of indigestion. Among the major causes is a weakened lower esophageal sphincter (LES), which is in charge of avoiding stomach acid from moving back up right into the esophagus. Particular way of living selections such as consuming fatty or spicy foods, smoking cigarettes, and excessive alcohol consumption can also enhance the threat of establishing indigestion. Furthermore, weight problems, pregnancy, and specific medical conditions like hiatal ruptures can add to the incident of acid reflux. It is vital to recognize and attend to these underlying causes to successfully handle the condition.Acid reflux can cause

a variety of symptoms, ranging from moderate to severe. One of the most typical signs and symptom is heartburn, a burning feeling in the upper body that usually takes place after eating or when existing down. Other signs might consist of regurgitation of acid right into the mouth, trouble swallowing, relentless coughing, hoarseness, and throat inflammation. These symptoms can significantly impact one's lifestyle, resulting in pain and interruption of daily activities.While medical treatment may be essential for extreme situations of acid reflux, there are numerous natural home remedy that can assist relieve milder signs. Way of living alterations such as preserving a healthy and balanced weight, avoiding trigger foods, and consuming smaller sized, much more constant meals can help in reducing the occurrence of heartburn. Elevating the head of the bed while resting and staying clear of relaxing instantly after dishes can additionally help in stopping heartburn episodes. All-natural treatments like ginger, chamomile tea, and apple cider vinegar might provide relief for some individuals.In final thought, comprehending indigestion is essential to managing and preventing this typical digestive disorder. By determining the causes and identifying the signs, individuals can take on way of life modifications and try natural home remedy to minimize the pain connected with indigestion. Nevertheless, it is essential to get in touch with a healthcare professional for appropriate medical diagnosis and advice on the most suitable therapy method.
Read more here Boost profits with affordable digital marketing strategies, Unlock growth with transparent digital marketing pricing.,Investing in effective digital marketing: Price breakdown., Get a clear picture of our digital marketing services costs., No surprises, just results: Transparent digital marketing pricing.,Talk to our experts: Personalized digital marketing pricing plan.
3 notes
·
View notes