#Jejunostomy
Text
Happy Disability Pride Month to people with ostomy bags, nasogastric tubes, gastrostomies and jejunostomies.
256 notes
·
View notes
Text


3 décembre/suite : Ça fait du bien de ne pas sentir de sonde traverser ‘tout mon corps’, de ne pas avoir un tube qui pendouille à mon visage, d’avoir sa peau qui peut respirer, sa narine se reposer. C’est dans ces moments que je me dis que je devrais prendre le risque d’accepter la jéjunostomie, et d’ailleurs le docteur m’a proposé de l’avoir durant cette hospitalisation mais j’ai refusée. En vu de comment mon corps est trop compliqué/ne tolère «rien», j’ai peur de n’avoir que des problèmes avec, j’ai peur d’avoir une infection et d’être dans une galère car je ne tolère pas les antibiotiques, bref je ne le sens pas de faire cette opération pour l’instant dans ces conditions…
#yamina hsaini#yamina's life#maladie#santé#médical#gastroparesie#sonde naso jejunale#jejunostomie#hopital
4 notes
·
View notes
Text
Dispelling Myths and Misconceptions About Sleeve Gastrectomy with Duodeno-Jejunostomy (DJB) with Dr. Shashank Shah-Best Bariatric Surgeon In Pune and Mumbai
Introduction: In the realm of weight loss surgery, Sleeve Gastrectomy with Duodeno-Jejunostomy (DJB) is gaining recognition as an effective procedure. However, like any medical innovation, it’s surrounded by myths and misconceptions. In this blog, we aim to debunk some of the common misunderstandings about Sleeve Gastrectomy with DJB, with insights from Dr. Shashank Shah,the best bariatric surgeon in Mumbai and Pune.
Meet Dr. Shashank Shah: Dr. Shashank Shah is a highly qualified and experienced bariatric surgeon, with a remarkable list of credentials. Holding degrees of M.B.B.S. and M.S., along with affiliations and fellowships from prestigious medical institutions, Dr. Shah is a recognized authority in bariatric and laparoscopic surgery. His dedication to advancing surgical techniques and patient care has earned him widespread acclaim in the medical community.
Director of Laparo-Obeso Centre: At the Laparo-Obeso Centre, Dr. Shashank Shah leads a team committed to providing comprehensive treatment for obesity and related metabolic diseases. Serving as a training center for laparoscopic and bariatric surgery, the Laparo-Obeso Centre is affiliated with Boston University for its bariatric training program, reflecting Dr. Shah’s commitment to excellence in surgical education and patient care.
Areas of Expertise: Dr. Shashank Shah’s expertise spans a wide range of surgical specialties, including:
Bariatric surgery for obesity
Metabolic surgery for type 2 diabetes
Hernia surgeries, both open and laparoscopic
Laparoscopic gastrointestinal surgery
Surgical emergencies
Portal hypertension
Laparoscopic oncology
Thoracoscopic thymectomy for myasthenia gravis
Dispelling Myths About Sleeve Gastrectomy with DJB: With Dr. Shashank Shah’s wealth of knowledge and experience, let’s address some common myths and misconceptions about Sleeve Gastrectomy with DJB:
Myth 1: Sleeve Gastrectomy with DJB is Riskier Than Other Bariatric Surgeries
Dr. Shah’s extensive experience and dedication to patient safety underscore the safety and efficacy of Sleeve Gastrectomy with DJB when performed by experienced surgical teams. Through meticulous pre-operative evaluations and personalized care plans, Dr. Shah ensures optimal outcomes for his patients.
Myth 2: Sleeve Gastrectomy with DJB is a Last Resort
Dr. Shashank Shah advocates for early intervention with Sleeve Gastrectomy with DJB as a proactive approach to managing obesity and improving overall health. By addressing misconceptions about the procedure’s invasiveness and promoting its effectiveness, Dr. Shah empowers patients to consider bariatric surgery earlier in their weight loss journey.
Myth 3: Sleeve Gastrectomy with DJB Leads to Severe Complications
There is a misconception that Sleeve Gastrectomy with DJB is associated with a high risk of complications, including leaks, infections, and bleeding. However, Dr. Shashank Shah’s expertise and meticulous surgical techniques minimize the risk of such complications. Through comprehensive pre-operative evaluations and adherence to best practices, Dr. Shah ensures the safety and well-being of his patients throughout the surgical process.
Myth 4: Sleeve Gastrectomy with DJB Results in Excessive Scarring and Disfigurement
Some individuals fear that undergoing Sleeve Gastrectomy with DJB will result in significant scarring and visible disfigurement. However, Dr. Shashank Shah’s expertise in minimally invasive laparoscopic techniques allows for smaller incisions and reduced scarring compared to traditional open surgery. Patients can expect minimal scarring and faster recovery times, enhancing their overall satisfaction with the procedure.
Myth 5: Sleeve Gastrectomy with DJB Is Not Suitable for Older Adults or Those with Comorbidities
There is a misconception that Sleeve Gastrectomy with DJB is only suitable for younger, healthier individuals and may not be appropriate for older adults or those with pre-existing medical conditions. However, Dr. Shashank Shah’s comprehensive approach to patient care ensures that individuals of all ages and health statuses receive personalized treatment plans tailored to their unique needs and circumstances. With careful consideration of medical history and risk factors, Sleeve Gastrectomy with DJB can be safely performed in a wide range of patients, leading to significant improvements in health and quality of life.
Conclusion: With Dr. Shashank Shah’s expertise and dedication to patient care, it’s clear that Sleeve Gastrectomy with Duodeno-Jejunostomy (DJB) offers a safe, effective, and transformative solution for individuals struggling with obesity and related metabolic diseases. By addressing common myths and misconceptions surrounding the procedure, Dr. Shah empowers patients to make informed decisions about their weight loss journey, leading to improved health outcomes and enhanced overall well-being.
0 notes
Text
February 6-10 is Feeding Tube Awareness Week!

The beginning of February was selected because of its proximity to Valentine’s Day, because we love our feeding tubes. This is my first year as a tubie and I’m looking forward to learning more about feeding tubes and the conditions that necessitate them! I do love my tube, it saved my life!
I am an adult with a feeding tube, and a lot of the awareness and attention surrounding these medical devices is child focused. A lot of children depend on tube feeding to thrive, but there are plenty of disabled adults that depend on tube feeding as well! In 2017 there were approximately 438,000 people with feeding tubes in the US, and 60% of them are adults.
I have gastroparesis, which directly translates to paralysis of the stomach. My stomach doesn’t grind food the way it’s supposed to, and my pylorus sphincter at the bottom of my stomach doesn’t open well to pass food and liquids through. While gastroparesis has a range of impact and severity, I have a very severe case, and I am no longer able to eat or drink by mouth for nutrition. I am 100% tube fed. I went into starvation ketoacidosis prior to my placement.
Tube feeding, or enteral nutrition, has several different forms. There are nasal tubes and there are surgical tubes. Nasal tubes can go into your stomach (NG), duodenum (ND), or your jejunum (NJ) and are typically for short-term use. They can be used for acute illness and malnutrition, or to trial tolerance of enteral feeding. Surgical tubes go into your stomach (gastrostomy/G) jejunum (jejunostomy/J) or both (gastrojejunostomy/GJ) and they’re for chronic conditions and/or long-term use. I have a GJ tube and it looks like this:
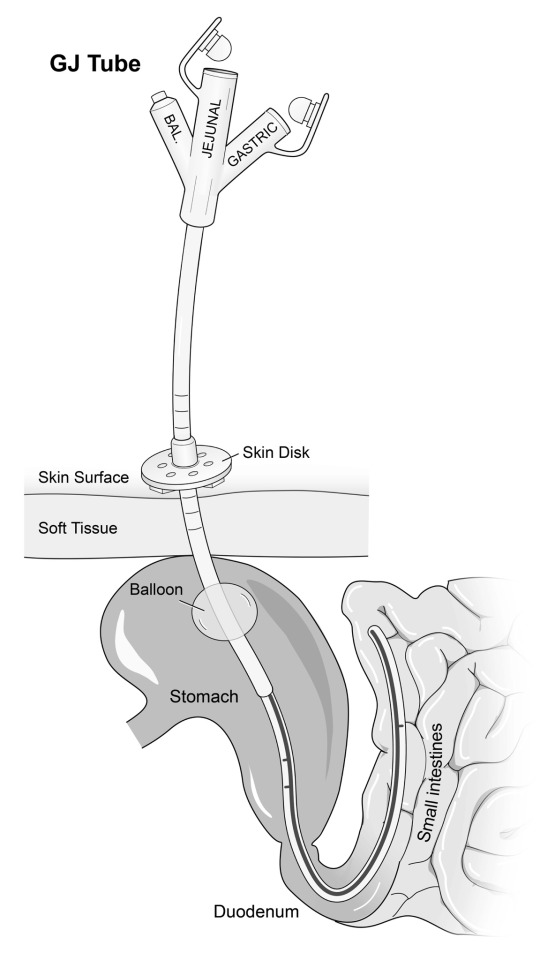
I have a GJ tube so that I can bypass my paralyzed stomach and feed directly into my intestine. I can also drain stomach contents from the gastric port, which allows me to drink liquids and drain them out before they make me sick. Different people will have different tubes depending on their diagnosis and prognosis! Some people have one form of tube, and others have separate G and J tubes.
There are over 400 conditions that can require tube feeding. Some of those include
Gastroparesis
Intestinal dysmotility
Cancer
Intestinal failure
Inflammatory Bowel Disease (Crohn’s disease and Ulcerative Colitis)
Cerebral Palsy
Congenital/chromosomal conditions
Cyclic Vomiting Syndrome
Ehlers-Danlos Syndrome
Several trisomy conditions
Prematurity
Other conditions not mentioned in the link above include
Hyperemesis gravadarium, severe nausea/vomiting during pregnancy to the point of significant weight loss and electrolyte imbalance
Acute trauma requiring bowel rest
Eating disorders
This week, I want to promote visibility for disabled adults with feeding tubes. I didn’t know anything about enteral nutrition until I got sick. Once I had a confirmed diagnosis of gastroparesis, the reality that I was facing forced me to learn and adapt quickly to a completely life changing treatment. I know there are other adults like me, as well as tubie adults that used to be a child with a tube!
4K notes
·
View notes
Note
What if people who can’t swallow end up choking on thick water? Then what?
If it is temporary you are either tube fed through your nose (nasogastric or NG tube) or your mouth (Orogastric - OG tube).
If they know it is going to be permanent they (usually a hospital) will make a surgical port in your stomach (Gastric - G tube) or small intestine (Jejunostomy - J tube) to deliver nutrition through
50 notes
·
View notes
Text



Abdomino-pelvic impalement x3 in a 17-year-old who somehow managed to not die
[Original medical journal case report]
[Credit to how this was found]
A 17-year-old female fell from second floor directly over iron rods of an under-construction building at midnight. Although three iron rods penetrated inside her body, she was conscious and oriented but cried in pain. Neighbours cut the rods from the iron pillar with drilling machine and shifted the patient from accident site to the emergency department of our hospital which took 5 hours. During this interval, she was in sitting posture and could not lie down fearing additional trauma due to the penetrating rods. On examination, she was conversant and had a pulse rate of 126/minute and pallor. Two iron rods could be seen penetrating her abdomen and pelvis while the third one went through and through her gluteal region [Figure 1].
A part of her cloth also went inside the path of the iron rods. Blood clots could be seen at the entry and exit wounds. Abdomen was not distended, and child had passed clear urine once on her way to the emergency department. There was no evidence of any injury to the chest, head, neck, spine or the extremities. At arrival, along with the primary survey, an intravenous line was secured to start fluids, antibiotics and analgesics. Tetanus toxoid and tetanus immunoglobulin were administered. Simultaneously, samples were sent for routine blood investigations and cross match. Haemoglobin was 8.9 and haematocrit was 27. Chest, abdominal and pelvic skiagrams were taken to assess the passage of the rods and any bony injury. One of the rods could be seen penetrating through the right iliac bone. Another rod went through and through the ascending colon just distal to the ileo-caecal junction and also the right iliac bone. There were no major vascular or urinary injuries. All the solid organs were spared. Resection of the jejunal segment containing the two perforations was done followed by end-to-end jejuno-jejunostomy.
Patient was shifted to the operation theatre and was put in left lateral position between the operation table and shifting trolley, so that the rods came in between the trolley and the operation table. In this position, patient had induction of anaesthesia using 100% oxygen for 3 minutes followed by Etomidate (100 mg), Fentanyl (75 mcg) and Succinylcholine (75 mg) [Rapid sequence induction], followed by intubation using cuffed oro-endotracheal tube of size 7.0. Following this, patient was maintained on Oxygen, Air and Sevoflurane, then patient was shifted to operation table in sitting posture and surgical procedure was started. Rod in the gluteal region was removed first after increasing its entry and exit wounds slightly. It was seen to pierce only the gluteal muscles. The passage was washed with hydrogen peroxide and saline and packed with betadine-soaked gauze. She was then turned supine and laparotomy was done through midline incision. One of the rods was seen to pierce the jejunum twice at approximately 30 and 40 cm from the duodeno-jejunal junction [Figure 2].
Ileo-ascending anastomosis was done after excision of the caecum along with the perforated ascending colon. No orthopaedic intervention was needed for the rod penetrating the right iliac bone. Tension suturing was done after insertion of drains in pelvis, right and left paracolic gutter. She received three units of packed cells in the peri-operative period. Patient was transferred to the Intensive Care Unit post-operatively and was there for 5 days following surgery for intensive monitoring and management. Antifungal agents were added when positive fungal blood culture was seen following fever on 3rd post-operative day. Patient passed flatus on 5th post-operative day and tolerated oral food from the next day. Drains were removed on the 5th post-operative day. Wounds over gluteal and iliac regions were conservatively managed on dressing and antibiotics. The total duration of hospitalization was 24 days and patient were discharged with advice of daily dressing of these wounds. First follow-up was after 15 days of discharge and subsequent two follow-ups were after one and three months of discharge. She has been asymptomatic on follow-ups. Figure [3] shows her scars after 3 months of discharge from hospital.
#medical gore#cw: gore#gore#impaled#impalement#medical journal#surgery#flesh#organ#wound#serious injury#personal
12 notes
·
View notes
Text
But my passion for eating came to a screeching halt this summer when I had a medical crisis that required a tracheostomy and a G-J (gastric and jejunostomy) tube rendering me unable to speak or eat. Having muscular dystrophy, a progressive disease where all muscles weaken over time, I’ve experienced difficulty swallowing in the last 10 years, adapting by shifting to soft or fatty foods that help with swallowing. While I aspirated saliva and food from time to time, there were several days in a row this summer when I kept choking every time I ate. I would swallow a bite or sip and half would not go down, requiring me to spit it in a cup so I could catch my breath. For days I tried to keep my caloric intake up by drinking lattes and letting my warm tongue melt tablespoons of peanut butter right after. Eating one small container of Trader Joe’s peach and mango yogurt would exhaust me. These were the last things I ate before going to the ER.
Food is essential to life, but it is so much more. Food is more than fuel or a calorie count. Food is cultural, political, and social — it ties people together and is a form of identity and pride. There’s nothing more wonderful than feeling satiated after a hearty meal like a bowl of spaghetti showered with grated parmesan cheese or a perfectly charred smashburger with caramelized onions and avocado dripping with special sauce. This is the sensation I miss most, as only medications and hydration go into my stomach via g-tube and liquid food through my small intestine via j-tube. Although I receive nutrition, I do not feel satisfied.
My inability to smell (because I do not inhale air through my nose) and eat has not diminished my desire for food. When I was in the ICU for four weeks I would leave the Food Network on during the times I was alert enough to pay attention, feasting on shows that I would never watch regularly: Guy’s Grocery Games and Pioneer Woman. The second episode of Iron Chef: Quest for an Iron Legend featuring Esther Choi made me want everything she made, such as her pork rib-stuffed donuts with sesame milkshake and dalgona cookie. A nurse saw me watching the episode and asked if I was torturing myself since I was temporarily on TPN (total parenteral nutrition), a form of intravenous nutrition. Was it torture? I didn’t even consider that, because it was my way of fulfilling my desire visually.
18 notes
·
View notes
Text
Managing And Caring For Enteral Feeding Tubes - Actionable Intelligence
We can train healthcare staff in the essentials of managing and caring for enteral feeding tubes
For many healthcare professionals, it is crucial to be well-informed on how they can care and maintain the safety of people with an enteral feeding tube most effectively. Enteral tube feeding is a means of supporting people who may no longer be able to consume adequate amounts of nutrition orally.
The enteral feeding tube itself is designed to provide foods and fluids in a liquid form, and a patient may require it for any of a range of reasons. For example, the patient may be suffering from swallowing problems that heighten the risk of food or fluid going down the wrong way and ending up in the lungs rather than the stomach, or they may have a medical condition that prevents the eating or digestion of food.
A person who requires enteral tube feeding may only need to have it in place for a limited time while undergoing treatment, or they may be living with it for a number of years. The situation will differ from one patient to the next.
A useful course for healthcare practitioners supporting those with a feeding tube
Healthcare practitioners will develop their theoretical and practical knowledge in the management and care of enteral feeding tubes (PEG), when they enrol on our own course on this subject. This course can be delivered in a classroom as well as remotely using Zoom video conferencing software, making it more accessible and convenient for attendees.
This course is aimed at nurses and healthcare workers who are already competent in administering medications. It covers a broad range of important aspects of the management and care of enteral feeding tubes and associated subjects, including the anatomy and physiology of the gastrointestinal tract, and the implications and complications of gastronomy and jejunostomy tubes.
Healthcare staff who may not have been exposed to feeding tubes previously or may not have a full appreciation of enteral feeding will learn the essentials on this course, including the different features of the tubes, and how they can best care for someone with a tube in place.
Attendees will also learn about the site cleaning and how to use a feeding tube to administer medication or feed their patient. Also covered in this course is the all-important matter of what to do in an emergency – what are the specific considerations and actions that should be taken involving feeding tubes in an emergency situation. Would you know how and when to use and ENPLUG?
We’ll put you in the best possible position to be more effective in your work
This course, focusing on the management and care of enteral feeding tubes, is just one of the many programmes of study that make up our highly regarded complex care courses here at Actionable Intelligence.
Our courses can be delivered either face-to-face or online depending on the circumstances and requirements of the attendees. Continued learning and professional development through courses such as ours play a crucial role in making healthcare safer and more effective for everyone and also count towards revalidation requirements for nurses.
To learn more about this or any of our courses, please reach out to us today, by calling 0330 133 4195 or sending an email [email protected]

2 notes
·
View notes
Text
Choosing the Best Feeding Tubes for Your Patient’s Needs

Choosing the right feeding tube for a patient is important. It can make a big difference in their comfort, health, and overall care. There are many types of feeding tubes, and each one is designed for different needs. In this guide, we’ll compare different feeding tubes, explain what to consider when choosing one, and help you understand the materials and designs available.
Understanding the Different Types of Feeding Tubes
Feeding tubes come in several types. Here’s a simple look at the most common ones:
Nasogastric (NG) Tubes
Nasogastric tubes are put in through the nose and go down to the stomach. They are usually used for short-term feeding, like after surgery or during a short illness. NG tubes are easy to place and remove, but they can be uncomfortable, especially if used for a long time. They can also slip out of place easily.
Gastrostomy (G-Tube)
Gastrostomy tubes, or G-tubes, are inserted directly into the stomach through the abdomen. They are meant for long-term feeding. G-tubes stay in place better than NG tubes and are more comfortable over time. However, they require surgery to be put in, which comes with some risks like infection.
Jejunostomy (J-Tube)
Jejunostomy tubes, or J-tubes, are similar to G-tubes but are inserted into the small intestine instead of the stomach. They are used for patients with severe stomach problems or those who can’t have food go into their stomach. J-tubes work well for these patients, but they are more complicated to care for.
Percutaneous Endoscopic Gastrostomy (PEG) Tubes
PEG tubes are a type of G-tube that are placed using a camera (endoscope) in a less invasive procedure. They are used for long-term feeding and are similar to G-tubes in many ways. The main benefit is that they are easier to put in, so recovery is faster. However, there is still a chance of complications like infection.
Factors to Consider When Choosing a Feeding Tubes
There are several things to think about when choosing a feeding tube. These will help you find the best option for your patient.
Patient’s Medical Condition
The patient’s health condition is the most important factor. For example, patients with trouble swallowing might do well with a G-tube or PEG tube, while those with severe stomach problems may need a J-tube. Knowing the patient’s specific needs will help you choose the right tube.
Duration of Tube Feeding
Think about how long the patient will need the tube. NG tubes are good for short-term use because they are easy to put in and take out. But for long-term feeding, a more permanent option like a G-tube, J-tube, or PEG tube is better. These tubes are more stable and comfortable over time.
Comfort and Quality of Life
Patient comfort is key. Low-profile tubes, often called “button tubes,” are small and sit close to the skin, making them more comfortable and easier to hide under clothes. They also allow patients to move around more easily. It’s important to consider how easy it is for the patient or caregiver to manage the tube, as this will affect daily life.
Ease of Use and Maintenance
Different tubes require different levels of care. For example, NG tubes are simple to insert and remove, while J-tubes need more specialized care. Consider how much support the patient has when choosing a tube, as proper care is important to avoid problems like infections or blockages.
Comparing Feeding Tube Products by Material and Design
Feeding tubes are made from different materials and come in various designs. Here’s a look at what you need to know:
Silicone vs. Polyurethane Tubes
Feeding tubes are usually made from silicone or polyurethane. Silicone tubes are flexible and comfortable, making them a good choice for long-term use. However, they might not last as long as polyurethane tubes, which are stronger and more durable. Polyurethane tubes are also thinner, which can make them easier to insert, but they may not be as comfortable.
Single vs. Double Lumen Tubes
Feeding tubes can have one channel (single lumen) or two channels (double lumen). Single lumen tubes are simple and easy to manage. Double lumen tubes offer more functions, like giving medication through one channel while feeding through the other. This can be helpful for patients with complex care needs.
Low-Profile Tubes (Button Tubes)
Low-profile tubes are designed to sit close to the skin, making them less likely to be pulled out and less noticeable under clothing. These tubes are often chosen by patients who want to be more active. While they might need to be replaced more often due to their design, the extra comfort and ease of use can be worth it.
Additional Considerations and Services
When choosing a feeding tube, there are other things to think about beyond the tube itself.
Cost and Insurance Coverage
The cost of feeding tubes can vary, depending on the type and brand. Some types of tubes may be covered by insurance, but it’s important to check what coverage is provided and what costs you may need to pay yourself.
Manufacturer Support and Warranty
Some companies offer extra support, like customer service hotlines, educational materials, and warranties on their products. Choosing a top feeding tube manufacturer that offers good support can be reassuring, especially if you have any issues with the tube.
Nutritional Services and Accessories
Patients with feeding tubes often need special nutrition formulas and tools, like syringes, extension sets, and feeding pumps. Working with a dietitian or healthcare provider can help make sure the patient gets the right nutrition and that all the accessories work well with the chosen tube.
Conclusion
Choosing the right feeding tube for your patient is an important decision. By thinking about the patient’s health, comfort, and the type of tube that will work best, you can make an informed choice. It’s also important to consider the costs, support services, and any extra needs the patient might have. Always work with healthcare providers to make sure you’re choosing the best tube for your patient’s needs, so they can have the best possible care and comfort.
Source : Choosing the Best Feeding Tubes for Your Patient’s Needs
#Feeding Tube#Right Feeding Tube#Tubes#Healthcare#Feeding Tube Selection#Medical Equipment#Feeding Tube Guide
0 notes
Text
Global enteral feeding devices market is expected to develop at a compound annual growth rate (CAGR) of 5.20%, from its estimated USD 4551.32 million in 2023 to USD 7182.55 million in 2032.The enteral feeding devices market is experiencing significant growth, driven by a combination of factors such as the increasing prevalence of chronic diseases, rising geriatric population, and advancements in medical technology. These devices, crucial for delivering nutrition directly to the gastrointestinal tract of patients who cannot consume food orally, are becoming indispensable in clinical settings.
Browse the full report at https://www.credenceresearch.com/report/enteral-feeding-devices-market
Market Dynamics
Drivers
1. Increasing Prevalence of Chronic Diseases: The growing incidence of chronic conditions like cancer, neurological disorders, and gastrointestinal diseases necessitates long-term nutritional support. Enteral feeding devices provide a lifeline for these patients, ensuring they receive the required nutrients.
2. Aging Population: The global aging population is a significant market driver. Elderly individuals often face difficulties in swallowing, necessitating enteral feeding. With the proportion of older adults rising, the demand for these devices is set to increase.
3. Technological Advancements: Innovations in enteral feeding devices, such as the development of user-friendly, portable, and highly efficient devices, are propelling market growth. Advanced features like safety alarms, anti-clogging mechanisms, and easy-to-clean designs enhance the appeal of these devices.
4. Shift Towards Home Care: There is a growing trend towards home healthcare due to its cost-effectiveness and convenience. Enteral feeding devices designed for home use are witnessing increased adoption, contributing to market expansion.
Restraints
1. Complications and Risks: The use of enteral feeding devices is associated with certain risks, including infections, tube dislodgement, and blockages. These complications can deter their use, impacting market growth.
2. High Costs: The initial costs of enteral feeding devices and the expenses associated with their maintenance can be high, which may limit their adoption, particularly in low-income regions.
Market Segmentation
The enteral feeding devices market can be segmented based on product type, age group, end-user, and geography.
By Product Type
1. Enteral Feeding Pumps: These are the most commonly used devices due to their precision in nutrient delivery and ease of use.
2. Enteral Feeding Tubes: Including nasogastric tubes, gastrostomy tubes, and jejunostomy tubes, these are essential for direct nutrient delivery to the stomach or small intestine.
3. Administration Sets: These sets are crucial for the delivery of nutrients from the feeding pump to the patient.
4. Other Accessories: Including syringes, giving sets, and connectors, these accessories support the feeding process.
By Age Group
1. Pediatrics: Children with congenital anomalies or severe illnesses often require enteral feeding.
2. Adults: Adults with chronic diseases, neurological impairments, or post-surgical conditions represent a significant user base.
3. Geriatrics: The elderly population is a primary demographic for enteral feeding due to age-related health issues.
By End-User
1. Hospitals: The largest end-user segment, where enteral feeding devices are extensively used for inpatient care.
2. Home Care Settings: Growing rapidly due to the increasing preference for home-based care.
3. Ambulatory Care Centers: These centers utilize enteral feeding devices for outpatient procedures and short-term care.
Regional Analysis
The enteral feeding devices market is geographically diverse, with significant growth observed in North America, Europe, Asia-Pacific, and the rest of the world.
1. North America: Dominates the market due to the high prevalence of chronic diseases, advanced healthcare infrastructure, and substantial healthcare expenditure.
2. Europe: Follows closely with a well-established healthcare system and increasing awareness about enteral feeding benefits.
3. Asia-Pacific: Expected to witness the fastest growth due to improving healthcare infrastructure, rising geriatric population, and increasing healthcare expenditure.
4. Rest of the World: Includes regions with emerging markets showing potential growth due to improving healthcare services.
Future Prospects
The future of the enteral feeding devices market looks promising with ongoing technological advancements and increasing awareness about the benefits of enteral nutrition. Key players in the market are focusing on developing innovative products and expanding their geographical presence through strategic collaborations and acquisitions.
Key Players
Conmed Corporation
C.R.Bard
Cook Medical
Boston Scientific Corporation
Moog Inc.
Fresenius Kabi AG
Danone Medical Nutrition
Kimberly-Clark
Abbott Nutrition
B Braun Melsungen AG
Avanos Medical, Inc.
Cardinal Health
Applied Medical Technology, Inc.
Vygon India
Fidmi Medical
ALCOR Scientific
Amsino International, Inc.
Others
Segmentation
By Product Type
Enteral Feeding Tubes
Nasogastric Tubes (NG Tubes)
Nasojejunal Tubes (NJ Tubes)
Gastrostomy Tubes (G Tubes)
Jejunostomy Tubes (J Tubes)
Percutaneous Endoscopic Gastrostomy Tubes (PEG Tubes)
Percutaneous Endoscopic Jejunostomy Tubes (PEJ Tubes)
Others
Enteral Feeding Pumps
Gravity Feeding Sets
Syringe Pumps
Electric Feeding Pumps
Ambulatory Feeding Pumps
Others
Giving Sets
Enteral Syringes
Administration Reservoirs
Accessories (Extension Sets, Connectors, Caps, etc.)
By Age Group
Pediatric
Adult
By Application
Oncology
Gastroenterology
Neurology
Critical Care
Diabetes
Geriatrics
Others
By End User
Hospitals
Ambulatory Surgical Centers
Long-term Care Centers
Home Care Settings
Others
By Region
North America
The U.S.
Canada
Mexico
Europe
Germany
France
The U.K.
Italy
Spain
Rest of Europe
Asia Pacific
China
Japan
India
South Korea
South-east Asia
Rest of Asia Pacific
Latin America
Brazil
Argentina
Rest of Latin America
Middle East & Africa
GCC Countries
South Africa
Rest of Middle East and Africa
Browse the full report at https://www.credenceresearch.com/report/enteral-feeding-devices-market
About Us:
Credence Research is committed to employee well-being and productivity. Following the COVID-19 pandemic, we have implemented a permanent work-from-home policy for all employees.
Contact:
Credence Research
Please contact us at +91 6232 49 3207
Email: [email protected]
Website: www.credenceresearch.com
0 notes
Text
Do You Need Best Home Nursing Services In Delhi?

When someone in our home is sick or has come out of the difficulties of any kind of operation or the medical condition of an elderly person in our home is not getting better, then to take care of them, you want the Best Home Nursing Services in Delhi which will be available along with the best home patient care services in Delhi. Delhi is famous for Nurse at Home services, services will be made available for every kind of work here. Whether it is normal patient care which can be done by Home Attendant Services, or the patient has a serious condition for which Nursing Care Service at Home in Delhi is always available for patient care.
Why Do Patients Actually Need In-Home Nursing Services Delhi?
One of the key advantages of Home Nursing Services in Delhi is the continuity of care they provide. Patients receive consistent, one-on-one attention from nurses at home who are familiar with their medical history, preferences, and personal circumstances. This level of personalised care can greatly enhance the healing process, improve quality of life, and reduce the risk of complications or hospital re-admissions and recover fast at home.
Personalized Care: Home Nursing Services provide to each patient specific needs which are not available in Hospitals. Nursing care at home gives individual attention to patients, helping them recover from injury very fast.
Comfort of Home: Patients recover faster and better than hospitals in familiar surroundings of their own homes. When a family is close to a patient, They feel better.
Cost Effective: Home Nursing Services In Delhi can be more affordable than hospitals without compromising the quality of care.
Convenience: When family members can stay close to the patient then the patient, elders feel better because they provide emotional support and participate in the care process.
Work of Nurse for home patient
Temperature/Pulse/Respiration/Blood pressure/Spot monitoring
Offering urinal pan, Urine bag emptying, Care of Urobag.
Enema administration, Bladder wash, Bladder irrigation, condom Bladder irrigation, condom catheterization, Foley's catheterization male, Foley's Catheterization-Female
Helping in oral feeding, RT placement RT placement, RT feeding & management, Jejunostomy care PEG tube feeding & management, TPN administration
Assist in position change, assistance walking, wheelchair mobilization, simple daily exercises, range of motion exercises, spirometry
Assistance in reading, spiritual support, engagement activities
Oxygen Therapy
Oral medicines
Medical Administration - Topical (Ointment), Eye drops installation, SC (Insulin administration), Insertion of Suppositories, IV injection, IM injection, IV Fluids administration, Assist in major wound dressing, IV cannulation, ECG taking
Conclusion
Before Choosing the right Home Nursing Service in Delhi, think very carefully because the best service can significantly impact the recovery and quality of life of your loved ones. When You search on google "Home Nursing Services Near Me" or "Best Home Nursing Services In Delhi" you will find options like Careoxy Healthcare, Portea Medical, Medfind, Apollo Homecare, and Nightingales, you can find reliable and professional care tailored to meet your specific needs in Delhi. Always ensure to do thorough research and consider all factors before making a decision to ensure the best care for your loved ones.



#home nursing services#nurses#caretaker#daycare attendant sun#Full Time Nurse At Home#Careoxy#Nursing Care At Home In Delhi#Delhi Nursing Care#Patient Caretaker At Home#Nurse For Home#Nurse At Home
0 notes
Text
Nouvelle vidéo YouTube en ligne !
youtube
#yamina hsaini#yamina's life#gastroparesie#sonde naso jejunale#gastroparésie#j tube#jejunostomie#Youtube
3 notes
·
View notes
Text
Sleeve Gastrectomy with Duodeno-Jejunostomy (DJB): A Comprehensive Treatment for Obesity and Diabetes
Introduction: Sleeve gastrectomy with duodeno-jejunal bypass (DJB) represents a cutting-edge approach to tackling both obesity and type 2 diabetes mellitus (T2DM). This combined procedure offers patients a comprehensive solution, addressing the metabolic effects of obesity while providing sustainable weight loss and glycemic control. In this blog, we’ll explore the innovative technique of sleeve gastrectomy with DJB, its mechanisms, benefits, considerations, and the transformative impact it can have on individuals struggling with obesity and diabetes, with insights from Dr. Shashank Shah, a leading expert in bariatric and metabolic surgery.
Understanding Sleeve Gastrectomy with Duodeno-Jejunostomy (DJB): Sleeve gastrectomy with duodeno-jejunal bypass combines two distinct bariatric procedures into a single intervention. The first component, sleeve gastrectomy, involves the removal of a portion of the stomach to create a smaller, banana-shaped “sleeve.” This restrictive aspect of the surgery reduces stomach capacity and limits food intake, leading to weight loss. The second component, duodeno-jejunal bypass, involves bypassing a portion of the small intestine, including the duodenum and proximal jejunum. This bypass alters the gut hormones and improves insulin sensitivity, resulting in enhanced glycemic control.
Mechanisms and Benefits of Sleeve Gastrectomy with DJB: The combined approach of sleeve gastrectomy with DJB offers several synergistic mechanisms and benefits:
Weight Loss: Sleeve gastrectomy induces weight loss by restricting food intake, while duodeno-jejunal bypass enhances weight loss through altered gut hormone signaling and reduced nutrient absorption.
Glycemic Control: The bypass of the duodenum and proximal jejunum improves insulin sensitivity and glucose metabolism, leading to significant improvements in glycemic control and potential remission of T2DM.
Metabolic Effects: Sleeve gastrectomy with DJB affects multiple metabolic pathways, including increased secretion of glucagon-like peptide-1 (GLP-1) and peptide YY (PYY), which contribute to decreased appetite, improved satiety, and enhanced glucose regulation.
Cardiometabolic Benefits: Beyond weight loss and glycemic control, sleeve gastrectomy with DJB has been associated with improvements in cardiovascular risk factors, including blood pressure, lipid profile, and markers of inflammation.
Considerations for Sleeve Gastrectomy with DJB: While sleeve gastrectomy with DJB offers significant benefits, several considerations are essential for patient selection and optimal outcomes:
Patient Selection: Candidates for sleeve gastrectomy with DJB should have a body mass index (BMI) ≥ 30 kg/m² with T2DM or a BMI ≥ 35 kg/m² with obesity-related comorbidities. Additionally, patients should have failed conservative treatments for obesity and diabetes.
Long-Term Follow-Up: Comprehensive follow-up care, including monitoring of weight loss, glycemic control, nutritional status, and potential complications, is essential for ensuring the long-term success and safety of sleeve gastrectomy with DJB.
Multidisciplinary Approach: A multidisciplinary team, including bariatric surgeons, endocrinologists, dietitians, and psychologists, should collaborate to provide comprehensive preoperative evaluation, perioperative care, and long-term support for patients undergoing sleeve gastrectomy with DJB.
The Transformative Impact of Sleeve Gastrectomy with DJB and Dr. Shashank Shah’s Expertise: Dr. Shashank Shah, a distinguished leader in bariatric and metabolic surgery and director of the Laparo-Obeso Centre, is renowned for his expertise in sleeve gastrectomy with DJB. With a patient-centered approach and dedication to excellence, Dr. Shah empowers patients to achieve significant weight loss, improved glycemic control, and enhanced overall health through personalized treatment plans and comprehensive support.
Conclusion: Sleeve gastrectomy with duodeno-jejunal bypass represents a comprehensive and innovative approach to treating both obesity and type 2 diabetes mellitus. By combining the benefits of restrictive and metabolic surgery, this procedure offers patients sustainable weight loss, improved glycemic control, and cardiometabolic benefits. Under the guidance of experts like Dr. Shashank Shah, individuals struggling with obesity and diabetes can embark on a transformative journey towards better health and a brighter future. If you’re considering sleeve gastrectomy with DJB as a treatment option, consult with Dr. Shashank Shah to explore personalized solutions tailored to your needs, and take the first step towards a healthier and more fulfilling life.
0 notes
Text
I’m going to make a simple version of this post, longer version here.
I really need help. I’ve been in the hospital after having major open surgery to place a feeding jejunostomy tube and convert my GJ tube to a gastrostomy. The J tube alone is a 6-8 week recovery.
I have no income until June when my long-term disability payments start. I have to pay $672 a month for COBRA in the meantime, and with my spouse taking care of me we haven’t been able to pay bills.
My PayPal is currently under review because people donated under goods/services, so I can only use cash.app or Venmo.
Cashapp: $forcewielder
Venmo: message me
Tube images under the cut for proof (CW: blood + surgical site)

378 notes
·
View notes
Text
Exploring New Technologies in the Enteral Feeding Devices Market
The enteral feeding devices market is set for steady growth, with a projected compound annual growth rate (CAGR) of 4.0% over the forecast period. According to recent market analysis, the market is expected to increase from USD 2.8 billion in 2023 to USD 4.1 billion by 2033, reflecting the growing demand for efficient and reliable enteral feeding solutions.
Enteral feeding devices, essential for providing nutrition to patients who cannot consume food orally, are increasingly in demand due to the rising prevalence of chronic diseases, aging populations, and advancements in medical technology. These devices play a crucial role in patient care, particularly in hospitals, long-term care facilities, and home healthcare settings.
The market’s growth is driven by the continuous innovation and improvement in enteral feeding technologies, ensuring better patient outcomes and enhanced quality of care. Key players in the industry are focusing on developing more efficient, user-friendly, and safe enteral feeding solutions to meet the evolving needs of healthcare providers and patients.
Get your PDF Sample Report:
https://www.futuremarketinsights.com/reports/sample/rep-gb-12403
The promising future of the enteral feeding device market highlights its vital function in the healthcare industry in providing for the nutritional requirements of patients unable to swallow food. With consistent expansion and ongoing innovation, the industry is poised to significantly advance patient care across the globe.
Key Takeaways:
Market Growth: The enteral feeding devices market is projected to grow at a CAGR of 4.0% from 2023 to 2033.
Current and Future Valuation: The market holds a current valuation of US$ 2.8 billion in 2023 and is expected to reach US$ 4.1 billion by 2033.
Driving Factors: Key drivers of this growth include rising incidences of chronic diseases, technological advancements in medical devices, and an aging global population necessitating increased nutritional support.
Market Dynamics: The market dynamics are influenced by healthcare providers’ increasing focus on homecare settings, enhancing patient comfort and reducing hospital stays.
Enteral Feeding Devices Market — Regional Analysis
North America and Europe are expected to cumulatively account for nearly 70% of overall market value, with the former holding 40% of the share.
The dominance of these regions is attributed to favorable medical policies and the strong presence of market players.
Asia Pacific is forecasted to register tremendous growth on the back of rising healthcare expenditure, the presence of a large patient pool, and a burgeoning number of preterm births.
Enteral Feeding Devices Market — Competitive Landscape
Major market players operating in the market include ICU Medical, Boston Scientific Corporation, Fresenius Kabi, Abbott Laboratories, Cook Medical, Cardinal Health, Inc., Becton Dickinson & Company, and Dynarex Corporation among others. Market players are focusing on developing innovative products with low weight to increase portability.
On these lines, Infinity Feeding Pumps launched the Zevex EnteraLite Infinity Feeding Pump, which weighs less than one pound.
Key Contributors:
Abbott Nutrition
ALCOR Scientific
Applied Medical Technology
B. Braun Melsungen AG
Boston Scientific
CONMED Corporation
Cook Medical
Cardinal Health, Inc.
Becton, Dickinson, and Company
Fresenius Kabi
Owens & Minor, Inc. (Halyard Health)
Medline
Moog
Nestlé Health Science
Danone SA
Vygon SA
Amsino International, Inc.
Fuji Systems Corp
Neomed
Smiths Medical (Smiths Group)
Key Segments:
By Product Type:
Enteral Feeding Pumps
Nasogastric Tubes
Nasojejunal Tubes
Percutaneous Endoscopic Gastrostomy (PEG) Kit
PEG Balloon Kit
PEG Non-Balloon Kit
Replacement G-Tubes
Replacement Balloon G-Tubes
Replacement Non-Balloon G-Tubes
Percutaneous Endoscopic Gastro-Jejunostomy (PEGJ) Tubes
Low-profile Tubes
Low-profile Balloon Tubes
Low-profile Non-Balloon Tubes
By Age Group:
Adult
Pediatric
By End User:
Hospital
Clinic
Ambulatory Surgical Center
Home Care Setting
By Region:
North America
Latin America
Europe
Asia Pacific (APAC)
The Middle East & Africa (MEA)
0 notes
Text
Feeding tubes What Cancer patients and care givers should know
Maintaining proper nutrition during cancer treatment is important. When cancer patients struggle with this, a feeding tube can be a solution. These flexible plastic tubes placed in the stomach can help provide the calories, protein, vitamins, minerals and fluids needed to help the body fight infection, heal and stay healthy – all crucial during cancer treatment.
But the idea of a feeding tube can be daunting. Even though a feeding tube may be essential for helping you maintain a healthy, active life during and after cancer treatment, it can be a big lifestyle change. In this Blog, Dr. Pratik Patil – a Cancer Specialist In Pune explains What cancer patients and caregivers should know.
When do cancer patients need a feeding tube?
According to Dr. Pratik Patil, a Best Oncologist in Pune, cancer patients may require a feeding tube if they face difficulties in swallowing, particularly due to cancer in the head or neck area.
Additionally, patients who are malnourished before or during cancer treatment, which includes surgery, chemotherapy, and radiation therapy, may also benefit from a feeding tube. In some cases, patients who have fistulas, an opening, or an abscess in the esophagus or stomach may also require a feeding tube to ensure proper nutrition during cancer treatment.
How is a feeding tube inserted?
The way a feeding tube is placed depends on the type of feeding tube you need. There are three types of feeding tubes commonly used:
Nasogastric tube (NG-tube): This flexible tube is passed through the nose, down the esophagus and into the stomach. It is placed at the patient’s bedside in the hospital and doesn’t require a surgical procedure. It is often temporary and given to patients who can’t eat for a short period following surgery.
Gastrostomy tube (G-tube): This tube is inserted through the belly and brings food directly to the stomach. It can be placed during an outpatient procedure and does not require the patient to stay overnight. This tube is often used when patients will need to rely on a feeding tube for about three to four months or longer. It’s very easy to use.
Jejunostomy tube (J-tube): A J-tube is a soft, plastic tube placed through the skin of the belly into the midsection of the small intestine. It can be placed as an inpatient or outpatient procedure. The tube delivers food and medicine until the person is healthy enough to eat by mouth. It bypasses the stomach completely and is often used when the patient cannot digest food in the stomach, like in some cases of stomach cancer. This tube is also best suited for long-term use.
Will patients feel their feeding tubes?
Again, this depends on the type of tube. Patients typically can feel an NG tube, but the good news is, it’s only used for a few days or weeks.
With longer-term tubes, like G-tubes and J-tubes, patients may experience some initial pain and discomfort, but it should fade after a day or two.
How do feeding tubes work?
Different tubes work in different ways. Some use a pump – typically formula. Others rely on gravity or a syringe to push the food. Your care team will teach you how to use your specific feeding tube.
Can patients operate feeding tubes by themselves?
Yes, all three types of the common feeding tubes mentioned above can be operated by the patients themselves. But depending on their physical and mental health, they may need help from a caregiver or health care provider. Dr Pratik Patil , we provide classes for patients and caregivers to prepare them to use feeding tubes
Are there any side effects from using a feeding tube?
Usually, there are no side effects from the tube itself. Some patients may experience some nausea, vomiting or diarrhea, but this can be addressed by adjusting how much formula is given and how much time the feeding takes. If these side effects continue, your doctor can prescribe anti-nausea medicine. It’s also important to properly clean the feeding tube and the area surrounding it as instructed by your care team. Otherwise, the patient is at risk of infection. If a patient has an infection, the skin around the feeding tube will look red and swollen. Patients with feeding tubes might feel self-conscious.
Stigma or fear of stigma surrounding feeding tubes?
According to the best oncologist in Pune, Dr. Pratik Patil, feeding tubes can easily be concealed under clothing, allowing patients to return to work without their co-workers noticing.
However, it is recommended that patients educate their close friends and family about their condition and demonstrate how the feeding tube works. It may be helpful to involve a caregiver and teach them how to use the feeding tube. An honest and straightforward approach is often the best way to handle this adjustment.
0 notes