#Vancomycin
Text
“Vancomycin is a bad antibiotic, get over it.”
#medicine#med school#medblr#antibiotics#infectious disease#vancomycin#you know since it has bad tissue distribution#takes ages to start having an effect#you have to adjust dose according to blood concentration#etc#will i prescribe it in a heartbeat if i suspect mrsa? of course#but you only use it because it’s what you have
26 notes
·
View notes
Text
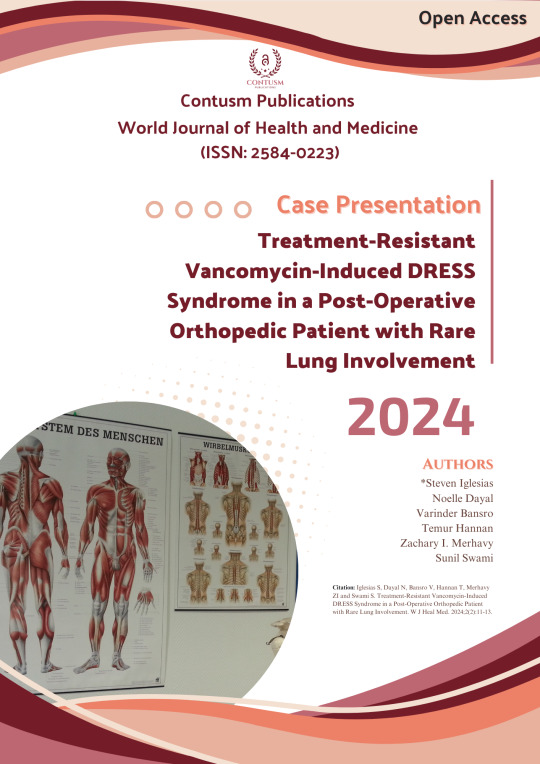
Treatment-Resistant Vancomycin-Induced DRESS Syndrome in a Post-Operative Orthopedic Patient with Rare Lung Involvement
Read Full Article Here:
https://contusmpublications.com/articles/wjhm-v2-1022.pdf
#CaseReport#MedicalCase#DRESSsyndrome#Vancomycin#DrugReaction#OrthopedicSurgery#PostOperativeCare#RareDiseases#LungInvolvement#TreatmentResistance#ClinicalResearch#MedicalScience#Healthcare#MedicalCommunity#Pharmacology#Dermatology#Immunology#PatientCare#MedicalEducation#HealthProfessionals
0 notes
Text
Antibiotics are horrible and I hate that I have to be on them right now. Damn you ear infection
#antibiotics#12 am thoughts#I’m also allergic to some antibiotics so they don’t like me either#Penicillin#and#vancomycin#want me dead#side note#don’t take antibiotics unless you absolutely have to and a doctor prescribed them#using them when unneeded is how we get antibiotic resistant diseases
0 notes
Text
Colonoscopy and Endoscopy
Hello my fellow blog readers. How are you doing? I was absent last week. I had so much going on getting ready for my colonoscopy/endoscopy on Thursday. The prep for the colonoscopy was horrible, HORRIBLE!!!! I even started 4 hours earlier than the instructions indicated. My aide changed me every hour from 12pm-6am. I was physically and mentally exhausted. Thankfully I had an early appointment.…

View On WordPress
#biopsies#c-diff#colonoscopy#colonoscopy preparation#colonoscopy results#daily life with ms#difficulties with ms#distraught#endoscopy#exhausted#gastric issues#gastroenterologist#irritable bowel syndrome#mentally#MS#ms symptoms#Multiple sclerosis#multiple sclerosis bowel issues#physically exhausted#vancomycin
0 notes
Text
look i just want to open up "el camino" and walk inside of it and take good care of jesse with all the time and medical equipment and resources i'd ever need and then take my leave once he's recovered and step out and zip up "el camino" behind me. is that so wrong??
#syd squeaks#syd's wildest fantasy: administering an antihistamine to avoid a vancomycin infusion reaction#jesse pinkman#el camino
12 notes
·
View notes
Note
You should delete that post giving incorrect information about the effects of boycotting Eurovision
my post isnt incorrect, its a different opinion.
#also i kept looking at this persons username like....do i know them. do they know me.#and then i remembered im literally allergic to vancomycin. like its my one allergy i need to tell my doctor#also im blocking this person bc in addition to sending this ask (which is wild!!) they did reblog my post w a tone so aggressive#that you might think that i myself am the owner of eurovision#which im not#clearly
0 notes
Text
"Ondansetron" sounds less like a drug name than some kind of weird dance robot. Maybe from Futurama.
Or maybe these:
youtube
#I got some to go with my doxycycline because I thought that was what screwed my stomach in the hospital#but so far all is good#maybe that epic week of nausea was just because my kidneys were trying to commit hari kari due to yet another antibiotic (vancomycin)#Youtube
0 notes
Text
141 and what their patient file looks like
┊ ⋆ ┊ . ┊ ┊┊ ⋆ ┊ . ┊ ┊┊ ⋆ ┊ . ┊ ┊┊ ⋆ ┊ . ┊ ┊┊ ⋆ ┊ . ┊ ┊┊
summary: This is what I imagine everyone's favorite pharmacist as well as medics see when they look at 141's medical file.
Based on this pharmacist and 141 interactions
pairing: Task Force 141 x pharmacist!Reader
warnings: medical/pharmacy terminology, medical inaccuracies, swearing, depiction of wounds, mention of substance use disorder and abuse
Terms
PMH - Past medical history - the total sum of a patient's health status prior to the presenting problem
FH - Family history - contributing family history, generally parents and siblings
SH - Social history - contributing social behavior and routine
a/n: not canon at all! this is just a reference for me
┊ ⋆ ┊ . ┊ ┊┊ ⋆ ┊ . ┊ ┊┊ ⋆ ┊ . ┊ ┊┊ ⋆ ┊ . ┊ ┊┊ ⋆ ┊ . ┊ ┊┊
Price
PMH
Height: 1.88 m (6' 2'')
Weight: 93 kg (205 lbs)
Blood type: O+
Extensive physical injuries
21+ stab wounds - 2 required antibiotics for recurrent infection
9x bullet wound - 5x in the extremities, 4x in the chest (no perforation of vital organs), healed without complication
5x abrasion collar - 1 near right eyebrow became infected following medical eval and stitches
3x diagnosed concussion
Aspirin-sensitivity
Previously evaluated for tinnitus and hearing loss
FH
Father - deceased at 76 from liver disease - 50 pack years, mycardial infarction (x2)
Mother - deceased at 84 due to chronic heart failure (CHF) -Glaucoma, asthma, CHF
Sister - Sports induced asthma, hypothyroidism
Negative family history of diabetes, hypertension, and cancer
SH
Smokes - 30 pack years
Drinks regularly - 4-5 hard liquor each weekend; 1 glass of whiskey occasionally
Physically active - Enjoys recreational activities such as hiking, swimming, and biking
Has 1 dog, currently under the care of pt's younger sister
History of monogynous long term relationships, currently single
Medication list + indications
Amoxicillin/Clavulanic acid 625mg - Infection
Morphine 15mg + Ketamine 3mg - IV - Pain
Paracetamol 750mg - Pain
Buproprion SR 150mg - Smoking cessation - not-taking est 2004
Allergies
Aspirin allergy - Reaction: hives and asthma - ONLY PRESCRIBE PARACETAMOL
No environmental, food, or animal allergies
Notes
Patient has denied smoking cessation options
Soap
PMH
Height: 1.88 m (6' 2'')
Weight: 91 kg (200 lbs)
Blood type: O+
7x stab wound - 6 required antibiotics for recurrent infection, 2 MRSA resistant
2x bullet wound - 2x in lower extremities, healed with no complication
6x abrasion collar
2x broken collar bone - healed, with no complication
Lactose sensitivity - Recurrent IBS if ingested
Chipped first left molar following opening a beer with teeth
FH
Father deceased at 68 due to heart failure - Type 2 Diabetes Mellitus, high cholesterol
Mother - Stage I HTN (hypertension)
Sister #1 - Postpartum depression, generalized anxiety disorder
Sister #2 - Elevated cholesterol/triglycerides
Brother - No known chronic health issues
Positive family history of diabetes and hypertension, but no cancer
SH
Drinks regularly and heavily - 8-12 beers and 2-3 glasses of hard liquor each weekend; 1 glass of scotch occasionally
Smokes socially - 5 pack years
Physically active
Close relationship with family, has 4 dogs at home under the care of pt's mothers
Avid fan of The Glasgow Football Club
Medication list + indications
Clindamycin 300mg with ciprofloxacin 400mg - Infection
Amoxicillin/Clauvanic acid 625mg - Infection
Vancomycin 18mg/kg - MRSA resistant infection
Paracetamol 500mg - Pain
Morphine 15mg IV - Pain
Doxycycline 100mg - Acne discontinued in 2004
Allergies
Insect stings - Observed anaphylaxis to childhood bee sting
Notes
Patient demonstrates medication non-adherence, counsel ESPECIALLY with antibiotics
Scored 6 on Alcohol use disorders identification test for consumption (AUDIT C)
Gaz
PMH
Height: 1.86 m (6' 1'')
Weight: 93 kg (205 lbs)
Blood type: B-
3x stab wound - healed, no complications
1x broken collar bone
2x broken femur
Diagnosed concussion - evaluated in Oct. '19
FH
Father - Type 1 Diabetes, high cholesterol
Mother - Vitiligo, Stage 3 breast cancer
Positive family history of maternal cancer and diabetes, but no hypertension
SH
Social drinker - 3-4 beers each weekend
Does not smoke
Physically active - Enjoys morning and evening runs
Enjoys spicy food and tries to introduce into diet
When on leave, enjoys attending concerts and music festivals
Medication list + indications
Piriteze 10mg - Allergic rhinitis
Fluticasone Propionate - 93 mcg/actuation - Allergic rhinitis
Paracetamol 500mg - Pain
Allergies
Seasonal - Pollen and pet dander
β-Lactam allergy - Reaction: anaphylaxis evaluated in '19
Notes
Organ donor
Ghost
PMH
Height: Weight: 1.93 m (6' 4'')
WeighT: 100 kg (220 lbs)
Blood type: AB-
Extensive cuts and scarring to entire body
4+ stab wounds - healed, no complications
Gun shot to lower abdomen - healed, no complications, evaluated in Nov. '22
13+ collar abrasion
2x broken nose
Childhood injury of broken tibia and large toe
Psych eval - History of depression and post traumatic stress disorder, childhood history indicates emotional and physical abuse
FH
Father - status unknown Diagnosed alcohol use disorder
Brother - deceased, cause of death non-contributory - Substance use disorder
Mother - deceased, cause of death non-contributory - Hypertension, thrombophilia (blood clotting disorder)
Positive family history of hypertension, but no diabetes or cancer
SH
Social drinker - 3-4 glasses of hard liquor each weekend
Smokes socially - 10 pack years
Physically active - Enjoys nightly walks
Psych eval - Other squad members act as his emotional support
Expressed interest in cats and tattoo art (FLAGGED: Further input and comments from other medical professionals would be appreciated)
Medication list + indications
Paracetamol 1000mg - Pain
Amoxicillin/Clavulanic acid 625mg - Infection
Morphine 20mg + Ketamine 4.5mg IV - Pain
Mafenide acetate 5% topical - Antimicrobial, burn wounds
Fluoxetine 20mg twice daily - Depression - not taking est 2001
Allergies
NKDA - No known drug allergies
No environmental, food, or animal allergies
Psych recommends evaluation of a pet, such as cat, for pt while on leave
┊ ⋆ ┊ . ┊ ┊┊ ⋆ ┊ . ┊ ┊┊ ⋆ ┊ . ┊ ┊┊ ⋆ ┊ . ┊ ┊┊
#task force 141 x reader#task force 141#cod x reader#call of duty modern warfare#cod mwii#modern warfare 2#simon riley x reader#simon ghost riley#call of duty#john soap mactavish#kyle gaz garrick#gaz x reader#soap x reader#price x reader#kyle garrick x reader#john price x reader#Johnny mactavish x reader#mw2 imagine#madebyizzie#mw2#izzie is writing#pharmacist! series
1K notes
·
View notes
Note
Hi! I just found your blog and noticed you have some posts where you explain how to write certain medical conditions, and I was wondering - could you perhaps do a post on blood poisoning, please? I am struggling with it a little lol.
I have a character that got stabbed, and I don't know what are the odds they could get blood poisoning and if yes, how fast and generally how it progresses.
If you don’t have time or something, don't sweat it, it's just a silly idea I got lol :D
Episode 4 of SciFiMedic Explains: How do I write sepsis?
Hi Anon!
So, your character got themselves stabbed, huh? Before we get to the nuts and bolts of how this is going to progress, we have to clear up a little choice of words here.
The term blood poisoning is not the medically correct term for an infection inside the blood- we call it sepsis. Unless you meant literal poison from the weapon (which I can do a follow-up post on, if that’s the case) I’m going to guess that we’re talking about a severe, system-wide infection of the blood.
Let’s walk through a few options:
Scenario 1:
Your character is stabbed in an area with lots of big blood vessels (highlighted red in diagram), and while everyone does all they can, the poor guy quickly dies of blood loss. There’s no time for infection to set in.
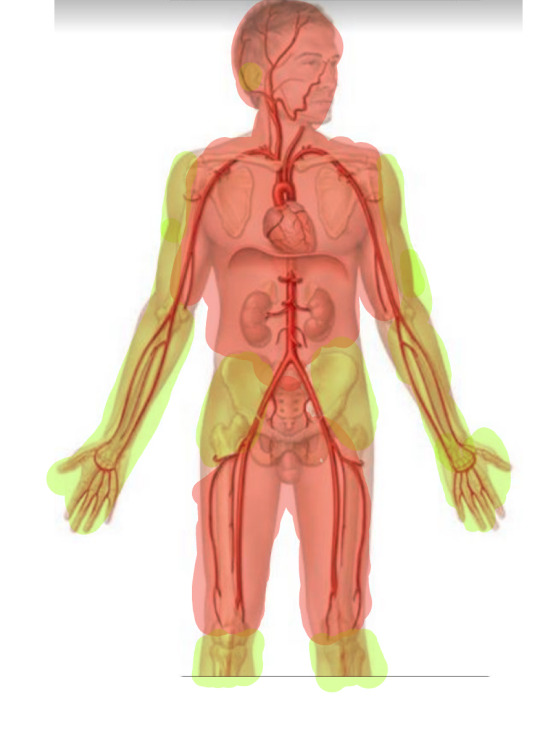
Scenario 2:
Your character is stabbed in a non-lethal area, like the arms, legs, or shallowly on the gut (highlighted green in diagram) They’re able to bandage themselves up, or maybe someone helps them out and they manage to get the bleeding stopped.
Unfortunately, 12 hours later, they notice red streaking coming from around the wound. They also:
Feel freezing cold, but have a high temperature
Are dizzy
Are shivering
Can’t quite catch their breath and feel the need to pant
Throw up
Look pale
These are all signs of the injury going septic, which is when the infection spreads away from the site of the wound and into the bloodstream. It happens fast. From the onset of these symptoms, they can be dead within only 12 hours.
Here’s what needs to happen for them to survive:
1: Hospital. No buts, no delay. If you want them to survive, they need advanced medical treatment, detailed below. (I will allow for a field hospital, or a makeshift hospital with a trained professional and plenty of supplies.)
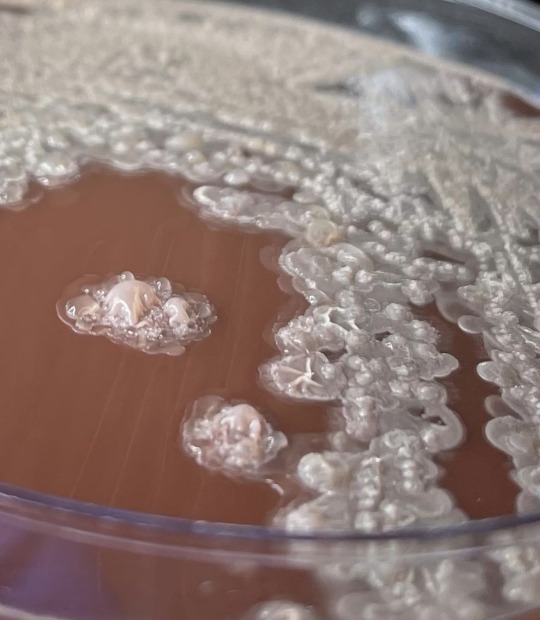
2: Blood and wound cultures. This means taking a small tube of blood from the arm, rubbing a cotton swab in the wound, and then sending both samples to the lab for study. They will smear the sample on a slide, put it in a warm, wet environment, and wait for it to grow out. Then, they’ll pop it under a microscope and run chemical tests on it to find out what the infection is. This process can take up to 4 days. The good news? The more pathogens that’s in the sample, the faster it will grow out. If you have blood that is severely infected, it could take as little as 12 hours to see results. (I know this from personal experience.)
If you’re in a field hospital, unfortunately this is a luxury you don’t have. See next step.
3: IV antibiotics immediately. Since you don’t know the bacteria causing the sepsis, you don’t know which antibiotic to give. Good news, people a lot smarter than I have created a plan for this.
3a: According to this study done by the National Library of Medicine, 67.9% of people presenting outside a hospital setting had their wounds infected with either Staphylococcus aureus or Pseudomonas aeruginosa.
3b. Thankfully, we have two very strong antibiotics- Vancomycin and Ciprofloxacin- that can each treat these pathogens. Unfortunately, each antibiotic is effective against only one of these pathogens, and nearly useless (or has developed resistance) against the other one!
3c. Good news, these antibiotics can be safely run together. Boom, you’ve just slammed (and it’s a slam- these drugs are horrible for you long term) 67.9% of patients with the right antibiotics to start treating their sepsis.
3d. What about the other 32.1% you may be asking? Good news, they’re not doomed. Just because a given antibiotic isn’t the best choice against a certain pathogen, it doesn't mean it will be completely ineffective. You may be buying them more time for the cultures to come back. You can also take your next best guess, and switch the antibiotics after a few hours if they aren’t having any effect.
4. Fluids. IV time! The biggest tell that someone has sepsis is that their blood pressure plummets to dangerous levels (which is what will eventually kill them, but we’ll get to that.) In order to prevent that drop, we need to raise the blood pressure by adding more volume to the blood through fluids. They might also need a blood transfusion, depending on how much blood they lost from the initial stab wound.
It’s important to note that it may not be possible to gain IV access, because when the blood pressure is that low, the veins tend to shrivel up and disappear (not literally.) In that case, your next best option is an IO, which is a needle drilled into the center of the upper arm bone, or lower leg bone. Yes, it hurts.
5. Vasopressors. Fancy name for medications that force the blood pressure to come up. There are four main pressors:
Norepinephrine
Epinephrine
Phenylephrine
Vasopressin
They should be added in that order, although this article admits there isn’t too much hard evidence to back this up.
It’s important to note that this is ICU level care, and unless we’re in the middle of the woods, we will have transferred there.
How do you know if it’s time to add another pressor? You’re not getting the results you need- AKA the blood pressure is continuing to stay or fall too low. In the ICU, we use a different measure of blood pressure that most people aren’t as familiar with, called a MAP score. It’s easy, I promise.
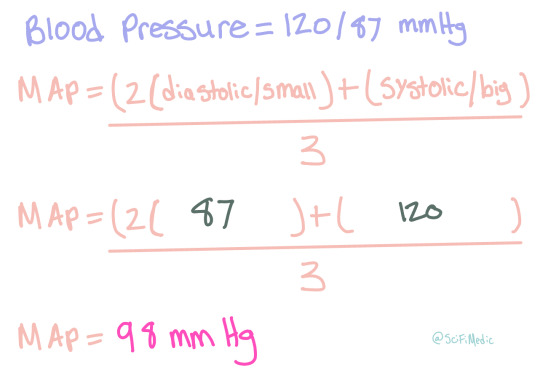
We use this method because it’s more representative of the amount of blood actually getting to the organs- though that is debated quite a bit in various circles. In America however, that’s the way most ICUs do it.
The ultimate goal for a sepsis case is to have a MAP above 65 mmHg. You can use this calculator to play around with the numbers and see if the blood pressure you’re thinking is within those parameters. If it’s not, time for another pressor.
At this point, your character is passed out most of the time. They’ve got a high fever, rapid heart beat, and are covered in sweat. They might also have a seizure from the fever and general stress on their body- at the very least they’ll be shaking from the chills. Their skin will be very, very pale, and might look kinda blue or gray in places- kinda like spots.
6. Hold your breath. No, not literally. But at this point, you’ve done all you can and you have to wait for them to either get better, or get worse.
If they get better, they’ll slowly start to maintain their own blood pressure, the fever will come down, and they’ll be able to string a coherent sentence together again. Recovery from sepsis can take a long, long time- as many as two to four months in the hospital. It totally depends on the person and how strong they are. The fittest, luckiest patient I’ve seen recover from sepsis was with us in the ICU for three weeks, then spent another month in a step down unit doing various therapies to regain strength.
However… if we’re looking at failure… well, then it’s time to move onto scenario 3.
Scenario 3:
After completing all of the above steps, they end up getting worse. Don’t worry, it’s not your fault- sepsis is fickle and kills fast. At this point, their kidneys are starting to fail from the inadequate blood pressure- you’ll need dialysis for that. They might stop breathing, or be unable to oxygenate their blood properly, then they’ll need a ventilator. At this point, they’re not stable enough to go into surgery anymore, so there’s no hope there. Eventually, the high fever will cause seizures, which will lead very quickly to brain death. As little as 12 hours after the initial dizziness and red streaks, their heart stops and they’re pronounced dead.
Summary:
The odds of your character developing sepsis from a non-fatal stab wound without immediate medical care are high- 90%
If they’re rushed to a hospital, their odds are better- 50%
If they do develop sepsis inside a hospital, they’re likley to survive- only 10.55% of people die of this kind of wound infection.
If they develop sepsis outside a hospital, then it’s almost certain they will die- 99%
Disclaimer: Although I’m in school to become a medical professional, I’m not one yet. All mistakes are mine, and I’m always open to discussion.
Anon, this was a fun prompt! If this isn’t quite what you were looking for, feel free to submit another ask with more follow up questions!
Everyone else, also feel free to send me an ask, or reblog this (or any SciFiMedicExplains Episode) with a scene you’d like me to help you write!
#whump#whump writing#medically accurate#writing help#sepsis#fever#hospital whump#infection#accurate whump#stabbing#injury#SciFiMedicExplains#medical whump
23 notes
·
View notes
Text
Friday Quiz 2.8
Changing the name of these to "Friday Quiz" and trying to do a few of them most Fridays.
All answers can be found on my blog. Or you can just give it your best guess.
18 notes
·
View notes
Text
A question that’s risen in my mind recently: can Logan ever get sick?
This came to my mind because well I’m a sucker for sickfic. A character in pain and then getting appropriate care and comfort to both heal and build stronger bonds with their loved ones? Perfect. But you can’t really write a sickfic for Logan, right? Well, maybe.
See in your stomach you have natural bacteria, the good kind. Gut flora is necessary for digestion and your health gut health overall. Logan of course has these, but they can be killed. Antibiotics. Of course they kill bacteria and can wipe out the average persons gut flora. Logan’s would likely be super strong, but if he was constantly pumped full of an incredibly potent one (i.e. Vancomycin 3.0 the strongest antibiotic there is) then it would theoretically overwhelm his body temporarily.
As seen when his adamantium skeleton was ripped out, under immense stress and damage his healing factor can be messed up, so it’s reasonable to suggest if he was captured in a form and tortured while having the steady stream of antibiotics the stress on his mind and body would fuck with his healing and wipe out his gut flora.
For the average person recovery from having their gut biome wrecked would be about one-two months, possible longer. So for Logan this would probably be about one week at most, but that still one week of sickness for a man who hasn’t really been sick since 1845, which would mess with him severely.
Basically yeah, he can get sick but of course as with everything Logan related he’d gotta suffer majorly to suffer more to recover.
I don’t think anyone cares about this or wants it but if any fic writers crave the angst of a sickfic with Logan but have believed he can’t get sick, I bring the answers. Of course you can always just say ‘fuck you he’s sick my fic my rules’, that works too.
#wolverine#x men#logan howlett#random thoughts#sickfic#fanfic#angst#fluff#I won’t do my actual science work but I’ll do this
11 notes
·
View notes
Text

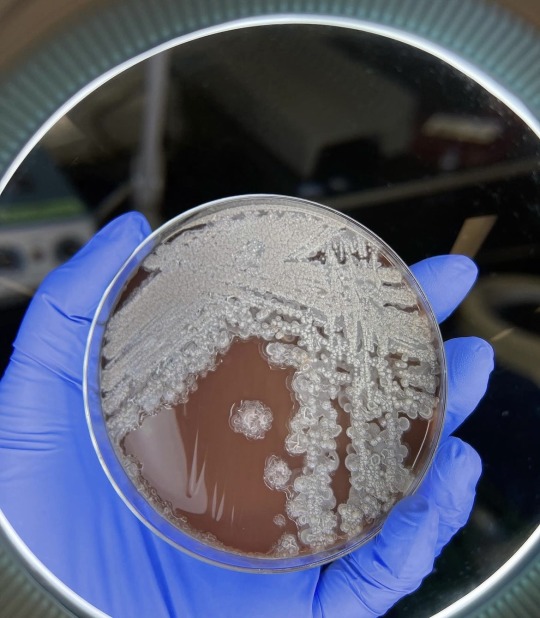

Bacillus licheniformis:
This is a gram positive bacterium commonly found in soil. It’s found on bird feathers especially chest and back plumage. It’s common in ground dwelling birds too. Is it harmful to man ? Yes it is has been found to cause infection in several cases of immunocompromised patients. It’s the causative agent of ventriculitis, ophthalmitis, bacteremia and endocarditis.
Treatment: it is sensitive to antibiotics such as cefepime, carbapenems, aminoglycosides and vancomycin.
…. Health is wealth …
22 notes
·
View notes
Note
Nurse y/n: i need to see ur arm so i can start that iv and giv u that vancomycin
Ghost: no thank ill just sleep it off
Nurse y/n: EXCUSE ME?! YOU HAVE MENINGITIS
Its all fun and games for ghost until he pisses y/n off to the point he gets re-assigned to the 5ft2 Filipino charge nurse who doest take shit from NOBODY
Charge rn: okay Riley i need to see ur arm and get this vanco drip done
Ghost: N.O.
Charge rn: N.O.? Thats not going to happen. you have 2 choices. Comply or become intubated,sedated,and restrained. So what ls gonna be.
Ghost: *low key terrified. Slowly putting his arms out*
and just then, the king felt true fear for the first time.
nah but ghost being a fussy patient because he always refuses help. and the nurses/doctors are so fucking over it. all they have to do is threaten sedation and he complies...
he could literally be on death's door and be like " 'm fine. "
#rachel speaks#not writing#simon riley#simon ghost riley#ghost mw2#mw2#call of duty#task force 141#ghost mwii#simon riley headcanons
104 notes
·
View notes
Text
Drugs!
Masterlist
Everyone loves drugs, right? And boy are there some juicy ones in surgery. There are more, especially of emergency drugs, but these are some common ones
Anaesthetic drugs
Propofol - the main sleepy juice. It looks like milk, hence the name 'milk of amnesia' (also called jackson juice because it's what killed MJ)
Ketamine - horse tranquiliser. But also used for humans! Very fast acting, and gives good pain relief too (you only need a small amount)
Isoflurane, sevoflurane - anaesthetic gases (bye desflurane, you've polluted the atmosphere for too long)
Atracurium, rocuronium - reversible muscle relaxants, they take a few minutes to fully kick in
Neostigmine, sugammadex - muscle relaxant reversal, sugammadex (nicknamed sugar) is more powerful
Suxamethonium - nonreversible muscle relaxant. It wears off after 2-6 minutes unless you have a rare genetic condition. Also works really quickly (30 seconds)
Lidocaine, bupivacaine - local anaesthetic, injected into the area you want to numb, or used in a spinal anaesthetic
Benzodiazepines (midazolam, diazepam etc.) - sedatives, not enough to fully conk you out, but will make you a bit sleepy and more relaxed
Pain relief
Paracetamol (tylenol) - mild pain relief, can be given through IV for better results
Morphine - the simplest opioid, usually IV or given orally (apparently tastes a bit like liquorice?)
Fentanyl and alfentanyl - much stronger pain relief, used rarely except during induction of anaesthesia
Antibiotics
Not always given, used more in orthopaedics or where there's a risk of infection. The type given is usually up to the anaesthetist's preference unless there's an existing infection that's been cultured
Common ones: amoxicillin, vancomycin, gentamicin, clindamycin, flucloxacillin, doxycycline
Emergency drugs
Tranexamic acid - sometimes given at the start if there's a risk of bleeding. Helps to prevent blood loss
Atropine - increases heart rate
Glycopyrronium - increases heart rate, also reduces saliva production
Ephedrine - increases blood pressure
Metaraminol - increases blood pressure
Adrenaline - increases heart rate and blood pressure, used for cardiac arrests and anaphylaxis
Intralipid - treats local anaesthetic toxicity
Dantrolene - treats malignant hyperthermia (a life threatening condition where the body temperature raises really high)
Adenosine, amiodarone - treats arrhythmias
Digoxin - slows heart rate
24 notes
·
View notes
Text
Cedars also has nice hospital rooms.
Apparently there were dual infections. I drained most of it before I came to the ER last night. I had a round of vancomycin in the ER along with a bunch of fluids. This morning they reopened the incision, cleaned it out completely, then packed it. I'm upstairs in a room because they want another 24 hours of antibiotics. I should be heading home tomorrow.
12 notes
·
View notes