#hypoperfusion
Text
Diuretics use in patients with Acute Renal Failure and Septic Shock by Dr Dale Ventour in Journal of Clinical Case Reports Medical Images and Health Sciences

ABSTRACTS
Loop diuretics should be administered in the ‘de-resuscitative’ of sepsis, this occurs after the initial resuscitative period during sepsis. The dose of diuretic should be monitored and a continuous infusion of furosemide, which is the most prescribed diuretic, should be no greater than 4mg/min.
There needs to be caution with co-administered nephrotoxic agents such as aminoglycosides, other diuretics, NSAIDS as these increase the toxicity profile. Despite the popular use of loop diuretics in critical care, loop diuretic use in sepsis has not been shown to decrease patients’ mortality.
This manuscript aims to discuss the use of diuretics in patients with septic shock exploring the evidence and consensus about the use of this therapy in critically unwell patients.
KEYWORDS: loop diuretics, septic shock, oliguria, ototoxicity, renal failure, critical care.
INTRODUCTION
Loop diuretics can be used in critical care to manipulate urine output in patients with hypoperfusion. Loop diuretics benefit the renal medulla during hypoxia by decreasing the tubular energy requirements(1, 2), which makes it a very attractive addition for patients with septic hypoperfusion. A Meta-analysis by K M Ho et al 2006 did not find in reduction in in-hospital mortality, requirement for dialysis, length of stay or number of patients remaining oliguric(3). A positive diuretic response to furosemide may indicate that the patient is in the ‘de-resuscitative’ phase of sepsis and that renal impairment is less severe. It is also appreciated that patients with non-oliguric renal failure have a lower mortality than patients with oliguric renal failure(4). The timing, duration, and dosing of diuretic therapy, plays a significant role in the morbidity associated with diuretic therapy in sepsis.
Diuretics in critical care; is used as a prophylactic measure that is, to prevent the onset of renal failure; to alleviate renal impairment in patients with established renal compromise or to convert oligo uric to non-oligo uric renal failure. There was no evidence in the meta-analysis by Ho et al 2006 that there was any benefit in the above listed uses of diuretics(3). There was great heterogeneity between groups in this analysis and most patients had existing renal impairment so that extrapolation to critical care patients with sepsis is problematic.
The goal of transitioning a septic patient from oligemic to non-oligemic renal failure is associated with a decreased mortality trend and diuretic therapy might aid patients with regard to normalizing positive fluid balances (5) but this intervention has associated risks and complications.
Diuretic therapy should be initiated not based on urine output but when the patient has transitioned from the early resuscitative phase to the “de-resuscitative” phase of septic shock. The transit point is determined clinically as the patient is no longer fluid responsive as per passive leg raises or with static/dynamic cardiac output monitoring, is less academic and inotropic support has stabilized or decreased.
Why does this matter?
There are associated side effects when initiating diuretic therapy in critically unwell patients such as ototoxicity, hypernatremia, hypotension and worsening renal function.
OTOTOXICITY
There is changes in the endolymph ionic concentration and fluid composition secondary to the inhibition of the Na-K-2Cl transporter within the stria vascularis of the inner ear(6). Aminoglycoside antibiotics potentiate furosemide ototoxicity, but noise trauma apparently does not. Methods of avoiding ototoxicity are suggested including slow continuous infusion rather than bolus injection, use of divided oral dose regimens, and the measurement of blood levels to avoid exceeding 50 mcg/ml of furosemide(6).
In heart failure patients as outlined by Salvador et al 2005(7), continuous infusions of furosemide resulted in a lower incidence of ototoxicity and fewer side effects. Continuous infusions resulted more than 30% increase in sodium excretion than bolus administration.
The ototoxicity induced by furosemide can be reversible although permanent deafness has been reported. The complication is related to both the peak serum drug concentration and the accumulated dose from continuous infusion and is aggravated with the concurrent use of aminoglycosides or Non-Steroid Anti-Inflammatory Drugs. The maximum recommended infusion dose is 4 mg/min (8).
HYPERNATREMIA
Hypernatremia as outlined by Hai-bin Ni et al 2016(9) was associated with increased mortality whether or not it was associated with diuretic use, this is a common side-effect with liberal diuretic use within the Intensive Care.
Hypernatremia as an independent predictor of mortality regardless of aetiology, speciality and across patients with different ages and co-morbidities (10-14). Risk factors include advancing age, co-existent renal impairment, associated use of nephrotoxic drugs. The phenomenon is poorly understood but correction is based on balancing renal water loss with overcorrection with isotonic solutions versus hypotonic water correction.
It necessities the use of Nasogastric water, naturetics, 5% Dextrose administration, low sodium enteral feeds and re-constituting drugs with 5% Dextrose rather than saline to correct this electrolyte imbalance. These interventions further complicates the management of the critically unwell patient, prevention is of tantamount importance.
WORSENING RENAL FUNCTION
Numerous studies have indicated that there is no benefit in the use of diuretic therapy to improve outcomes in patients with established acute renal failure in Intensive Care (15, 16). Maeder et al 2012, indicated a trend toward worsening renal function in elderly patients with chronic renal failure within a medical Intensive Care(17). His definition of chronic renal failure was >0.5 mg/dl increase in baseline creatinine over the 6 months follow up, again the findings not only supported renal failure as an independent predictor of mortality, but it was also aggravated by escalating the loop diuretic dose [17].
HOW DO WE ADMINISTER LOOP DIURETICS?
Meta-analyses support the administration of loop diuretics as continuous infusions versus boluses as there is better diuresis at a lower cumulative dose(18), this will inevitably lead to fewer side effects and more efficient fluid balance.
It has been suggested that the infusion dose be limited to 4mg/min to minimize the side effect profile as the loop diuretic has a ceiling effect around this dose [9]. It is also proposed by this author that the diuretic be administered in the ‘de-resuscitative’ phase of sepsis to manage the patient’s overall fluid balance.
The use of diuretics should be for the shortest time possible as there are considerations for electrolyte abnormalities and ototoxicity with a clear focus on serum sodium to gauge the amount of free water loss. While I am not against the administration of loop diuretics in septic patients with acute renal failure the timing of administration of the drug class with the “de-resuscitative phase of sepsis” is vitally important.
DISCUSSION
There is a paucity of evidence supporting the use of loop diuretics in septic critically unwell patients with acute renal failure leading to improved mortality(19, 20). These studies have highlighted increased risk of complications such as electrolyte disturbance without reducing the need for continuous renal replacement therapy or the duration of renal replacement.
Ototoxicity remains an underreported complication as there can be other contributing factors for altered hearing after the critical care episode. This complication will contribute to a patient’s post critical care morbidity affecting patient and patient’s family quality of life.
The is wide variation with the timing, dose, and indication for diuretic therapy in critical care. Bolus administration, low-dose continuous infusions (20) or high dose titrated to urine output or daily fluid balance are all methods used to administer diuretics. Liborio et al in his observational study of over 14,000 patients found no decreased mortality in critically ill patients with over 60% of these patient experiencing sepsis with a dose of furosemide up to 80 mg/day(21)
CONCLUSION
The indication and use of diuretics in septic patients with oliguric acute renal failure is varied and confounded by timing and effective dosage. However, there are significant complications associate with the use of diuretics in the critical care population and need serious considerations prior initiation of this therapy as there is no mortality benefit in septic patients with acute kidney injury.
Acknowledgement: No acknowledgement
For more information: https://jmedcasereportsimages.org/about-us/
For more submission : https://jmedcasereportsimages.org/
#loop diuretics#septic shock#oliguria#ototoxicity#renal failure#critical care#NSAIDS#hypoperfusion#heterogeneity#hypotonic water#Dr Dale Ventour#jcrmhs
0 notes
Note
joey mellen wrote bore hole, hughes wrote mechanism of brainbloodvolume (i did not know there were two of these guys lol)
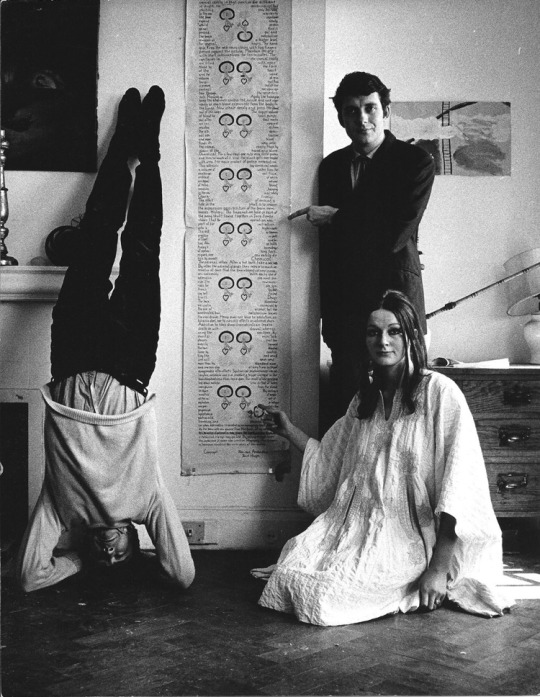
i know! those photos are alternately attributed to either of them, i still dont know who actually is in the photo because they were all white englishmen the same age.
and there were THREE. these guys were their own little trepanation cult polycule for a while in the 60s and 70s. as usual the woman, (Countess) Amanda Feilding (sic), is the one who gets forgotten, even though shes the one who made the actual gore movie of herself drilling a hole in her head for real: Heartbeat in the Brain (1970), which is considered "lost media" by that kind of person but i dont think it's actually lost, it was screened in 2011 and i think the fact that its about someone drilling a hole in their face is lending the footage more mystique than it actually possesses. looking for citations for this post is the first time ive heard it referred to as "lost", i dont think media is "lost media" just because it isnt on youtube but whatever
anyway Feilding ran for parliament several times. "Feilding ran for British Parliament twice, in 1979 and 1983, on the platform 'Trepanation for the National Health' with the intention of advocating research into its potential benefits; she advocated the provision of the procedure by the National Health Service.[3]" her parents were second cousins btw the english peerage is so fucked up it is unbelievable
she has spent her post-trepanation life advocating for drug policy reform, which is based, but unfortunately her son is also in politics and is a tory piece of shit


i have a Special Interest in trepanation and will probably eventually get it done somehow, i just have a feeling of fate about it or maybe dysmorphia. reading about idiopathic intermittent intercranial hypertension and hypoperfusion recently sounded real familiar. doctors dont like to talk about this stuff though, to them everything inside your skull is a schroedinger's cat that is assumed to be completely fine and normal until you prove to them via feats of strength that you have a Brain Problem of some kind, which heretofore is forbidden from mention
edit: trepanation doesnt actually do anything to your brain unless you have a pressure issue and the hole will just heal over anyway and reseal your brain, none of the Bore Hole claims or beliefs are anything except placebo
to people other than wumblr, who i assume has already read it: Bore Hole is an EXCELLENT book and will act as a fast and easy history lesson on how the counterculture boomers actually lived. their economy was unbelievable, americans and english used to be able to just "go to india" and hang out, things just did not cost a lot of money for a while there and this has permanently altered the part of their brain that makes cost calculations
55 notes
·
View notes
Text
i love being a cripple in the resturaunt industry, i love not being able to "just be a server for more money" because i can barely think straight half the time due to pain or fatigue or cerebral hypoperfusion which damages my ability to handle interactions with co-workers let alone do customer service on top of the autism, i love having people complain to my supervisors about how much i sit down and how it's "unfair" even though it takes my body 10x more effort to just be on my feet, i love co-workers developing resentment towards me about that kind of thing and supervisors interpreting it as laziness instead of "i am struggling to stay standing," i love busting my ass giving more attention and devotion to my shitty form of employment but that extra effort that takes more out of me than it would other people gets ignored in favor of anything they find wrong with me, i love the fact that doing this is probably making some of my conditions worse but i have no choice because applying for disability takes ages and i have no support network and i have yet to even get decent medical treatment or a solid diagnosis for any of this shit other than just POTS and a job where i can sit down job isn't a fix because of the autism and cptsd and the fact i'm also losing my tolerance for sitting due to issues with my legs and back! yipee!
#cripple punk#cpunk#physically disabled#chronic illness#postural orthostatic tachycardia syndrome#hypotonia#j#body log#i have co-workers who i know have chronic conditions/disabilities but not the same nature as mine#and surprisingly they aren't the ones complaining about me! weird!#that was sarcasm btw. i'm not surprised because they're the nicest to me#sharp pains in my fucking arms. and the side of my neck
7 notes
·
View notes
Text
Kleine–Levin syndrome (KLS) is a rare neurological disorder characterized by persistent episodic hypersomnia accompanied by cognitive and behavioral changes. These changes may include disinhibition, sometimes manifested through hypersexuality, hyperphagia or emotional lability, and other symptoms, such as derealization. Patients generally experience recurrent episodes of the condition for more than a decade, which may return at a later age. Individual episodes generally last more than a week, sometimes lasting for months. Patients commonly have about 20 episodes over about a decade. Several months may elapse between episodes.
The onset of the condition usually follows a viral infection (72% of patients); several different viruses have been observed to trigger KLS.[2] It is generally only diagnosed after similar conditions have been excluded; MRI, CT scans, lumbar puncture, and toxicology tests are used to rule out other possibilities. The syndrome's mechanism is not known, but the thalamus is thought to possibly play a role. SPECT has shown thalamic hypoperfusion in patients during episodes.
KLS is very rare, occurring at a rate of 1 in 500,000, which limits research into genetic factors.[2] The condition primarily affects teenagers (81% of reported patients), with a bias towards males (68-72% of cases), though females can also be affected, and the age of onset varies.[2] There is no known cure, and there is little evidence supporting drug treatment. Lithium has been reported to have limited effects in case reports, decreasing the length of episodes and duration between them in some patients.[3] Stimulants have been shown to promote wakefulness during episodes, but they do not counteract cognitive symptoms or decrease the duration of episodes.
Patients with Kleine–Levin syndrome (KLS) experience recurring episodes of prolonged sleep (hypersomnia).[5] In most cases, patients sleep 15 to 21 hours a day during episodes.[6] Excessive appetite (hyperphagia) and unusual cravings are present in half to two thirds of cases.[6][7][8] About half of patients, mainly male patients, experience dramatically increased sexual urges (hypersexuality).[9][7] Several other symptoms usually accompany the syndrome, including marked changes in mood and cognitive ability.[5]Derealization and severe apathy are present in at least 80 percent of cases.[10] About one third of patients experience hallucinations or delusions.[7] Depression and anxiety occur less commonly; one study found them in about 25 percent of patients.[10] Individuals usually cannot remember what happened during episodes.[6] Repetitive behaviors and headaches are commonly reported.[7] Some patients act very childlike during episodes,[11] and communication skills and coordination sometimes worsen.[6]
The first time a patient experiences KLS, it usually occurs along with symptoms that are similar to those of the flu or encephalitis. In at least 75 percent of cases, symptoms occur after an airway infection or a fever. Viruses observed before the development of the condition include Epstein–Barr virus, varicella zoster virus, herpes zoster virus, influenza A virus subtypes, and adenovirus. Several days after symptoms first occur, patients become very tired.[9] In cases that occur after an infection, KLS usually starts within three to five days for teenagers and fewer for children.[16] In other cases, alcohol consumption, head injury, or international travel precede symptoms.[9][14] Lifestyle habits, such as stress, alcohol abuse and lack of sleep and stress, have also been proposed as possible triggers.[5] First episodes of KLS are preceded by a clear event in about 90 percent of cases.[8] Recurrences generally do not have clear triggers; only about 15 percent have a precipitating event.[17]
Population-based studies of KLS have not been performed. Its prevalence is about 1 to 2 cases per million people,[8] although recent studies conducted by a French research team point to a higher number of 3 per million people.[25] It occurs most frequently among Jews in the US and Israel. First-degree relatives of people who have the syndrome are much more likely than the general population to have it, although only in about one percent of cases do family members contract it. About 68 to 72 percents of patients are male. Patients with the syndrome are more likely than the general population to have genetic disorders, and about a third of people with the syndrome encountered some form of birth difficulty.[26] In a study of 186 older patients, about ten percent had preexisting psychiatric issues.[6] One study found that about ten percent of patients had a neurological condition before KLS developed.[8] The condition does not appear to occur most frequently in one season.[11]
??? extremely strange disorder.
13 notes
·
View notes
Text
congrats to me, I have psoriatic arthritis
I've been on a prescription NSAID while we were figuring it out. I will be starting a real psoriatic arthritis med soon, but in the meantime I need more of the NSAID. And for whatever reason my rheum won't put refills on the prescription even though he always renews it when I ask, which adds at least a day to the whole process, and I cut it a little too close asking for another one this time. I spaced out my remaining pills, but I'm finally at the point where I'm just off it and oh my god, I feel horrendous. Did I feel like this all the time before I started it and I forgot what it felt like, or has it gotten worse and been masked by the meds? Or a rebound effect. I'm going with that as My preferred explanation. Regardless. My entire body feels like a sore muscle. I have a hypoperfusion headache. My joints are all angry. I have bad brain fog and compromised vision. (I think some of this is because the increased inflammation is flaring my POTS.)
I went to the pharmacy today to get the refill, only to find that for some reason they're closed today. And they're always closed sunday. So I am just going to suffer like this until monday, apparently.
12 notes
·
View notes
Text
I saw this great reference post recently about medical conditions. It has a lot of useful information about initial first aid. I wanted to add some comments about urgency because a lot of fics take place outside the hospital setting and it's helpful to know how quickly you've got to get your character to medical help before they die. I also wanted to add something about long term disability because I think fiction often doesn't address chronic illness and injuries, but it's useful to know about if your character doesn't have magic serum healing powers. (I didn't want to add directly onto that post because they had clearly spent a lot of effort on the research and I don't want to come across like I'm raining on their hard work)
Also got requested for stab wounds and falls from heights =) Going to start with a little spiel on brain injury because it will come up a lot.
Brain injury
There are different types of brain injury and they present differently depending on the areas of the brain affected. Traumatic brain injury comes from acceleration-deceleration, and typically have issues with mood control, attention/concentration and decision-making/problem-solving. This is the type that comes with amnesia of events before, around and after the injury, but particularly after. Hypoxic brain injury is when the brain didn't get enough oxygen, and is typically associated with breathing issues (drowning, suffocating, hanging, anaphylaxis). Memory may be affected, but don't have the classic course that traumatic brain injury go through. Hypoperfusion brain injury is usually due to a blood supply problem, and is typically from heart issues or low blood volume. These often affect deep territories of the brain and can have a variety of very localised and sometimes unusual symptoms, but can also present like hypoxic brain injuries. There are also a bunch of other acquired brain injury syndromes from strokes, bleeds, tumour, inflammation, etc etc and they all affect the person in different ways.
Stab wounds
- Deadly? - depends what you hit, how quickly that area bleeds, and how long it takes for them to get help. Fatal within seconds/minutes: hitting any major artery/organ that results in blood released outside the body: neck (carotids), groin/thigh (femoral), chest (aorta and heart). While veins usually bleed slower, hitting major veins (groin/abdomen/chest) can also kill quickly. Likely to be fatal within an hour or two: major organs with a lot of blood supply (e.g. liver, kidneys, spleen, lungs), the aorta - there is a buffer because they tend to bleed first into the body cavity. Depending on the cleanliness of the knife, environment and whether you perforate the gut, infection can kill them down the track (days). Stabbing into muscle and fat is not usually going to cause death by itself unless you hit a blood vessel.
- Disability? - depends on what was hit. Not enough is said about lacerated muscles and tendons. Especially around the hands and wrist (e.g. when people hold up their hands for defensive wounds), this is not easy to repair and you may not regain all your hand function (screw all the samurai movies where people catch blades one-handed, don't do it!). If an organ is hit, part or all of it might need to be removed to stop the bleeding, which causes long term problems. If the gut was perforated and infection happens in the abdomen, this usually means lots of surgeries and lots of gut problems down the track. Scarring, disfigurement, pain, body image issues (and PTSD) can all happen.
Fall from height
- Deadly? - really depends on the way a person falls and what they land on. People have died from getting punched and falling backwards onto the ground from standing height. The highest fall survived was 10km but the vast majority will not be this lucky. Statistically, the 50% survival rate is at about 4 storeys (15m) while heights above 18m (?about 6 storeys) are almost uniformly fatal. What usually kills them is either going to be massive internal bleeding or brain injury.
- Injuries - determined by which part they land on first. Common injuries are: leg fractures (usually ankles and hips), pelvic fractures, spinal fractures, rib fractures and skull fractures. Arm fractures can also happen, especially if they land heavily on one side or they try to break their fall with their hand. In general, internal injuries are correlated with where the bony injuries are. So rib fractures will usually be associated with lung bleeding or pneumothorax (air in the space between lung and the lining), or liver bleeding (the lower ribs on the right side overly the liver).
- Disability: apart from the issues with fractures and severe traumatic brain injury (discussed below), spinal fractures can (but doesn't always) cause spinal cord injury - i.e. damage to the nerves going from the brain to the rest of the body. Spinal injuries can be complete, or incomplete (and uh...it's like a massive topic by itself so I won't go into it), and comes with a huge laundry list of complications and life-changing challenges with breathing, blood pressure management, skin problems, bladder and bowel issues, and sexuality issues. Bad pelvic fractures can also come with a lot of bladder, rectal and genital issues.
Allergic reaction
- Deadly? - no, unless it is anaphylaxis. It can be very annoying or even (temporarily) disfiguring from the swelling and redness
- Disability? - most allergies recur (some get better with age some get worse), but allergic attacks alone do not usually leave permanent disability.
Traumatic Amputation
- Deadly? - depends on the level and how long you take to get to medical help. Small appendages (fingers/toes) are okay unless they get infected in the coming days. The higher the amputation on a limb, the higher the risk of severe bleeding, and you'd need to get to medical attention within hours at most. Above knee amputations with femoral artery bleeds can pour out your entire volume within minutes.
- Disability? - Yes. Even as small as fingers and toes will affect your ability, although humans are very good at adapting. Thumb amputations are a major problem because you will lose your grip. Losing the big toe will affect how your foot pushes off from the ground and can impact your walking. Lower limb prosthetics are much easier to adopt than upper limb prosthetics, and the higher the amputation, the harder it is for the prosthetic to be attached and used. Also...watch out for PTSD/psychological distress and phantom pain.
- Notes: most fics wouldn't need to describe these in detail, but traumatic amputations are...for lack of a better word, traumatic and messy. They often do not amputate completely. They are often associated with multiple fractures along that limb. In hospital, the doctors will assess whether they can reattach the amputated part, but often there is extensive damage to the blood supply and nerves around the area, and a surgical amputation has to be done higher up.
Anaphylaxis
- Deadly? - YES. Get that epinephrine/adrenaline in within minutes or they die.
- Disability? They will need to be aware of their trigger and carry the Epi-Pen with them. If the anaphylaxis is treated quickly, there's usually no lasting effects. If the anaphylaxis is treated late and they lose consciousness or even, god forbid, arrest, they can have long-term effects from hypoxic brain injury.
Asthma
- Deadly? - Potentially, depending on the severity.
- Disability? - Yes. Apart from needing to carry their puffers, the severe asthmatics sometimes have to go on long-term steroids, which causes a whole host of problems with weight, appetite, bone health, skin health etc. If it's severe enough to need ICU (rare, but possible), then they might end up with hypoxic brain injury.
- Notes: poor lungs is something that can permeate every aspect of life. Getting an attack when you go for a run in the cold, getting short of breath walking up the stairs, getting wheezy when you help move a couple of heavy furniture etc. In describing an asthma attack - a key is how much they can speak. The one holding a full conversation with you is going to be fine. Watch out for the one sitting silent on the edge of their bed, leaning forward with their arms propping them up by their sides (tripod position), their neck and chest muscles straining with every breath, who can only answer in single words.
Blood loss
- Deadly? - Potentially - the previous post had a good rundown of the volumes involved.
- Disability? - Potentially. Again, no blood for brain, brain sad. Mechanism is going to be different to anaphylaxis and asthma though, which are from low oxygen. With anaemia and shock, it can cause infarction (i.e. death of cells in area that didn't get blood supply) in deep parts of the brain.
- Notes: people can tolerate horrendously low blood (haemoglobin) levels if it's from a chronic illness (e.g. lymphoma). In acute blood loss though - the person is going to get dizzy with standing up abruptly (might even faint), they might see black spots, feel short of breath and tired, start feeling cold more easily, walking unsteadily and probably trouble concentrating. Note that blood loss can occur internally! Also note that not everyone can receive blood transfusions for biological and for cultural reasons.
Broken bones
- Deadly? - Trick question. The fracture is rarely going to kill you outright but the complications might. High impact pelvic fractures in particular can cause massive bleeding and kill (usually within hours). There are also other potentially deadly complications which I won't go into.
- Disability? - Depends on severity, yes. A fracture where the bones are well aligned usually heals fairly well; poor alignment can come with visible physical abnormalities. Hardware across joints will restrict joint movements (common for ankle and spine fractures). A really bad compound or comminuted fracture may never heal properly and be a constant source of pain. Also the complications can cause lots of disability!
- Notes: bad fractures will distort the anatomy around them, so it can affect the nerves or the muscles. Good young bones will usually take 6-12 weeks to heal enough for normal use. Old fragile bones will take much longer. In the immediate period, any force on the broken bone will hurt - so that's any attempted movement by the injured person, as well as gravity! Don't forget damn gravity! Also, in the first month it's common to get a lot of swelling and bruising in that limb.
Burns
- Deadly? - Potentially, but you've got a bit of time (hours). In the early stage it's from the inflammatory reactions and severe fluid loss discussed in the original post. NOTE FOR SMOKE INHALATION IT CAN KILL RAPIDLY if the airways swell up (which might take a few hours, barring the issue with inhalation of toxic chemicals), so these people generally have to be monitored very closely for 24 hours.
- Disability? - For the severe burns, potentially lots. Scarring across joints means a lot of movements get restricted, so anything involving hands and rest of limbs are going to be a problem. Large area burns also affects your ability to regulate temperature. Again, don't forget PTSD/psychological distress, particularly if scarring is highly visible.
Concussion/Traumatic Brain Injury
- Deadly? - Potentially. Depends on where it's bleeding from. For some people it can kill them within minutes, for others within hours or days.
- Disability? - Potentially. As the original post said in another section, head injury is divided into mild, moderate and severe. Most mild head injuries (aka concussion) recover completely within 3-6 months if not earlier. Moderate and severe traumatic brain injuries will often have long term effects on: mood, thinking skills, social skills, communication skills, seizures, headaches.
- Notes: watch out for the person with a "blown pupil" (pupil/s not contracting) they will die within the hour if they don't get medical attention. Also watch out for the "lucid interval" for a particular type of head injury bleeds - these are the ones who walk around like normal after a hard knock to their head and are found dead in their beds the next morning.
CPR - the only thing I want to add for CPR is that for someone who needs CPR in the community (i.e. not a hospital setting), chance of getting their pulse back is 1 in 3, chance of them making it to hospital alive is 1 in 5, chance of them surviving the hospital stay is 1 in 10. (source) These are not great odds!
Dehydration - symptoms are very similar to blood loss (apart from the obvious lack of blood squirting out) but usually develop over a period of hours to days. Because it's a much slower process, it's more likely to kill you from kidney failure than from poor blood flow to the brain.
Heart attack - nitpick on the original post but heart attack is not cardiac arrest. Cardiac arrest is exactly as the words say: "heart" "stops". A heart attack is usually referring to myocardial ischaemia - i.e. low blood flow to the heart muscles.
- Deadly? - a massive heart attack will cause the heart to stop so...yes. A smaller heart attack can kill within a few hours to days by causing heart failure (i.e. heart not pumping out blood properly), an even smaller one may not cause any obvious symptoms but will build up damage over time.
- Disability? - yes. Just like with lungs, a bad heart will affect all aspects of your life. Walking around the house, having a shower, running up the stairs, going for a walk up the hill, having sex. If there is any period where the heart has stopped, it can also cause brain injury.
Loss of consciousness/syncope
- Look. As much as fiction tends to depict people swooning all the time, it is not supposed to happen on the regular. Anyone who faints needs to be seen by a medical doctor. The only benign cause of loss of consciousness is a "vasovagal attack", which is where they (usually young women) drop their blood pressure because it's been a long hot day and they didn't have much to drink and they got excited and stood up too quickly.
- Loss of consciousness happens because of 3 reasons: interruption of blood flow to the brain (strokes, heart attacks, heart rhythm problems, blood loss, massive clots in lungs), electrical problems within the brain (seizures), or crappy blood getting to the brain (toxins and medications)
- The underlying cause will dictate whether it is likely to cause death or disability
Shock: This is when your entire body isn't getting good blood supply for whatever reason. This includes your brain, which means most people either become confused or lose consciousness by this stage. Will kill within the hour (depending on underlying cause) if not treated, and can still cause damage to multiple organs even if treatment started.
Stitches: erm...there are different types of stitches. The original post talked about interrupted stitches. There IS a type of suturing called continuous stitches, which is when you sew using one continuous thread and pull the wound close like you might fabric. NOT ALL WOUNDS ARE SUITABLE FOR THIS, but it is fairly common in some surgeries. Wounds can also be closed by staples.
#tw: injury#tw: amputation#medical#medical meta#writing resources#writing tips#writing references#don't know if this all made sense#happy to clarify anything
70 notes
·
View notes
Link
In the first two hypothesis papers we identified ß2 adrenergic receptor (ß2AdR) dysfunction, high sympathetic tone (stress), hypovolemia (preload failure), endothelial or vascular dysfunction, and an energetic disturbance in skeletal muscle as the main critical factors in the ME/CFS pathophysiology [43]. Meanwhile more evidence for endothelial dysfunction has accumulated. Altered endothelial dysfunction-related microRNAs were found in plasma from ME/CFS patients recently [5]. In Covid-19 infection the endothelium is severely affected and the disturbance seems to persist in post-Covid Syndrome (PCS) [12, 16, 24, 27, 38]. Particularly the finding of severe endothelial affection in Covid-19 and the persisting endothelial dysfunction corroborates our hypothesis of a role of endothelial and vascular dysfunction in the pathogenesis of PCS. Endothelial dysfunction may result in decreased CBF.
As a possible explanation for the orthostatic intolerance and the decrease in CBF we assume the presence of both a strong vasoconstrictor effect mediated by an elevated sympathetic tone and weakened vasodilator influences, that occurred in particular by dysfunction of ß2AdR and other causes of endothelial and vascular dysfunction. Covid-19 seriously affects the endothelium and there is evidence of chronic endothelial dysfunction in the post-Covid-syndrome similar to that in ME/CFS [12]. ß2AdRs have vasodilator effects in the brain, skeletal muscle and the heart, a mechanism to increase blood flow during muscular activity (a functional unit with the brain steering and coordinating muscle activity and the heart providing the blood flow for both organs). Since orthostatic stress is permanent during human activities (standing and even sitting) it is the basic stressor to which all other forms of stress are additive. It can desensitize ß2AdR and cause vasoconstrictor predominance by the α1-adrenergic effects that do not desensitize upon chronic stimulation in contrast to ß2AdR [43]. Chronic psychosocial stress itself can cause endothelial dysfunction and an increase in vasconstrictor mechanisms by functional and structural changes fixing the state of vasoconstriction (similar to the mechanisms that lead to fixed hypertension) [23, 47]. Endothelial dysfunction, which is clearly present in ME/CFS and PCS, has been found associated with cognitive impairment in different conditions, in the elderly as well as in children [17, 41]. Since the decrease in CBF already occurs after changing position from horizonal to sitting, orthostatic stress can be considered as the basic and permanent stressor during human activities in the awake state. We think that a decrease in CBF by 25% already in a sitting position, a concomitantly disturbed neurovascular coupling and endothelial dysfunction will not allow enduring cognitive efforts or mental work, with mental fatigue being the consequence.
Psychomotor slowing, ataxia and loss of coordination of movements in ME/CFS [11, 39] can also be explained by reduced perfusion, hypoperfusion of the motorcortex and other structures involved in motor function not being able to maintain coordinated neuronal activity in the motor cortex, a disturbance similar to impaired cognition. Since cognitive as well as motor function are disturbed by reduced (global) CBF there is good reason to believe that other brain functions can also be disturbed as will be explained in the following.
A reduction of global CBF is not the only cerebrovascular finding in ME/CFS. Consistent observation of sluggish fMRI signals suggests abnormal neurovascular coupling meaning that local blood flow regulation is also disturbed [32, 33, 37]. Endothelial dysfunction may play a role in the disturbance of neurovascular coupling. The question is whether the inflammatory mediators released from skeletal muscle can also affect neurovascular coupling, the local regulation of blood flow adjusting local perfusion to local neurophysiological activitiy. We think that influx of vasodilators, which otherwise also regulate local perfusion in other organs, into the cerebrovascular bed being under excessive vasoconstrictor influences via heightened sympathetic tone (stress), dysfunction of ß2AdR and endothelial dysfunction can only disturb a highly regulated fine tuning of vascular regulation and local blood distribution (neurovascular coupling).
Hypoperfusion of skeletal muscle together with mitochondrial dysfunction leads to the excessive production of various endogenous vasodilators in skeletal muscles and to their spillover into the systemic circulation, from where they can reach every organ including the brain [43]. One of these mediators, bradykinin, is the most potent opener of the blood brain barrier (BBB) [1, 31] which may be of relevance for the neurological findings and symptoms. Opening of the BBB may explain moderate IH for which we have provided the evidence above. We could not find in the literature what the symptoms of isolated opening of the BBB would be but we assume it to be rather pathological. The algesic and hyperalgesic properties of the tissue mediators released from skeletal muscles may cause headache by directly acting on cerebrovascular nociceptors, by the release of CGRP and substance P and by edematous distension. Headache could also originate from myalgia of head and neck muscles and from IH [18].
Disturbances of reflexes and autonomic function, hypervigilance and hypersensitivity to sensory stimuli such as light, noises and smells and brain fog
Disturbances of the pupillary reflex [4] upon prolonged illumination of the pupils were also reported in patients with ME/CFS: “Two unusual responses were observed that are evident on prolonged illumination of the pupils. The more frequent finding seen in three quarters of patients is a rhythmic contraction and dilatation of the pupils. The second pattern is a paradoxical dilation of the pupils after an initial contraction.“ Thus, one should consider the possibility that also other regulatory mechanisms of body and autonomic functions and reflexes, like orthostatic regulation, vascular regulation, thermoregulation and sleep are also impaired as a consequence of a reduced CBF. This could result in either sluggish responses to sudden changes or the opposite, namely large overshooting swings unable to find a new stable level of regulation after a disturbance, similar as observed with the pupillary reflex. In such a way impaired regulation of orthostatic function may contribute to orthostatic dysregulation and intolerance without necessarily being the main cause of it. Hence, dysautonomia may be enhanced by a disturbed CBF. Primary disturbances of the autonomic nervous system and dysautonomia or autonomic dysfunction arising from the brain stem may play a role in triggering ME/CFS for instance by orthostatic dysfunction causing orthostatic stress that would desensitize ß2AdR and raise α-adrenergic mediated vasoconstriction. Based on these considerations, it should be considered that ME/CFS itself could cause or at least worsen autonomic dysfunction by cerebral hypoperfusion from which another vicious circle would arise. By these mechanisms autonomic dysfunction could also be expanded to other primarily undisturbed autonomic functions.
Hypervigilance and sympathetic hyperactivity are present in ME/CFS [14]. Stress may cause hypervigilance by centrally stimulatory effects of catecholamines and PGE2 (one of the mediators released into the circulation by the skeletal muscles). The latter has awakening effects [19]. The α2-adrenergic autoreceptor, a presynaptic receptor on noradrenergic neurons modulating and inhibiting norepinephrine release [30] shows desensitization [3] similar to the ß2AdR, but unlike α1-adrenergic receptors. Thus, chronic stress could also desensitize this inhibiting autoreceptor to enhance catecholamine release in activating noradrenergic nuclei of the brain stem like the locus coeruleus thereby causing arousal and increased vigilance, and in the sympathetic nervous system leading to enhanced vasoconstrictor output while the vasodilator ß2AdR is dysfunctional and endothelial dysfunction of other causes may be present. It would finally mean that chronic stress enhances stress responses (adrenergic hyperactivity). Orthostatic stress may play a particular role since it is already present in the sitting position in ME/CFS to decrease CBF and therefore almost unavoidable. Since orthostatic stress is operative over a considerable part of the day there is not sufficient time for recovery of desensitized adrenergic receptors. Episodes of stress in human life are usually followed by episodes of rest and recovery in which re-sensitization of adrenergic receptors can take place and therefore such enhancement of stress responses can fade if sufficient time of recovery is allowed (presumeably only few days of rest needed for receptor re-sensitization). In line with these considerations, long and intense periods of psychosocial stress, in which such desensitization could take place, precede the development of ME/CFS in a subset of patients which is a potential explanation for the initiation of the disease in this subset. By the mechanisms outlined in our previous paper, ME/CFS, once fully established, is a state in which a high level of stress is maintained and fixed by a number of dysregulations and vicious circles, which the patient can hardly escape [44]. Since there is no recovery from stress in ME/CFS, α2-adrenergic autoreceptors and ß2AdR remain desensitized.
Hypervigilance caused in the way just described may lead to increased stimulus uptake in all sensory organs while stimulus processing in the corresponding brain regions may be impaired by the reduced CBF as outlined above. Increased stimulus uptake and concomitantly reduced stimulus processing may lead to stimulus overload. Stimulus overload could be the cause of hypersensitivities against sensory stimuli such as light, noises and smells.
These considerations also help to understand the simultaneous presence of signs of hypervigilance and mental fatigue in ME/CFS patients. This paradox can be explained by the discrepancy between the higher energy demand caused by neuronal overstimulation and the reduced energy supply by cerebral hypoperfusion resulting in an early energetic deficit to explain the high level of mental fatigability. The ability to perform mental work may be additionally diminished by hypervigilance (nonspecific overstimulation) reducing the ability to concentrate on a single mental task which may be part of the mechanisms causing the feeling of brain fog. Finally, brain fog may be the result of central overstimulation, cerebral hypoperfusion, IH and opening of the BBB allowing the endogenous mediators released from skeletal muscle like bradykinin and PGE2 to exert effects in the brain.
Cerebral blood flow velocity of the middle cerebral artery was reduced during head‐up tilt associated with hyperventilation. Thus the decrease in CBF can be explained only by a rise in cerebrovascular resistance by vasoconstriction.
We consider hyperventilation, an overshooting response to a respiratory stimulus, resulting from autonomic dysfunction with sympathetic overactivity. In PCS hyperventilation has recently been identified as cause of dyspnea. Hyperventilation occurred early during exercise resulting in an impaired ventilatory efficiency [2, 26]. The cause may be excessive stimulation of the respiratory center in the brain stem causing the feeling of air hunger (dyspnea). A physiological early mechanism of respiratory stimulation is via skeletal muscle afferents involving movement sensors and metabolic afferents [34]. It is obvious to incriminate a disturbed metabolic situation in skeletal muscle in this early, excessive stimulation of respiration during exercise. The latter could then be further enhanced by dysautonomia (as an overshooting response). The resulting dyspnea is not only limiting the ability to exercise but aggravates the key pathophysiological mechanisms in skeletal muscle in ME/CFS.
Difficulties to fall asleep and altered day-night rhythm may result directly from enhanced catecholamine release in activating noradrenergic nuclei of the brain stem like the locus coeruleus as a consequence of desensitized α2-autoreceptors and stress causing arousal and increased vigilance. Stimulus overload just explained above could be an indirect cause of sleep disturbances. In sleep medicine it is considered an important cause of insomnia.
Decreased CBF, disturbed local blood flow regulation and neurovascular coupling, central adrenergic hyperactivity, hypocapnia and increase in intracranial pressure seem to play a strong role in the pathophysiology of the neurological symptoms in ME/CFS (Fig. 1). They can well explain cognitive impairment, brain fog, headache, psychomotor slowing, ataxia and loss of coordination of movements, hypersensitivity, sleep disturbances and dysautonomia.
#ME/CFS#dysautonomia#long covid#science journal#hypothesis#neuroinflammation#PEM#brain fog#neuroscience#PASC
4 notes
·
View notes
Text
Still reading on heart rate variability and such for work :
"Therefore, autonomic dysfunction can lead to cerebral hypoperfusion, brain damage, and cognitive impairment."
Yeah you tell me 🥲
1 note
·
View note
Text
Management of Cerebrovascular Steno-Occlusive Disease
Patients with steno-occlusive cerebrovascular disease are at risk of ischemic symptoms from haemodynamic insufficiency in the presence of reversible hypoperfusion, exhausted autoregulation and impaired vasodilatory reserve. Multidisciplinary management approach includes blood pressure management, antithrombotic therapy, treatment of underlying brain-body interactions targeted at optimising cerebral blood flow and oxygen delivery, and revascularisation procedures.
Patients with symptomatic stenoocclusive disease have a risk of recurrent stroke of at least 10-15 per cent within 5 years. Progressive atherosclerosis of internal carotid artery (ICA) or middle cerebral artery (MCA) is the most common cause of impaired distal cerebral perfusion with cerebral misery hypoperfusion
Cerebral Hypoperfusion & Collateral Circulation
In the setting of cerebral hypoperfusion, recurrent ischaemic events occur depending on the following factors: (1) amount of collateral cerebral circulation; (2) extent of haemodynamic impairment; (3) age; (4) cardiac status; (5) presence of metabolic syndrome of hypertension, hyperlipidemia and insulin resistance; (6) factors affecting coagulation, blood oxygen carrying capacity and delivery (such as anaemia and other haematology disorders, systemic infections and sepsis, renal and hepatic disorders).
In addition to the traditional cerebral ischaemic symptomatology pertaining to the affected vascular territory (Table 2), orthostatic symptoms, syncope, transient global amnesia, episodic limb shaking and watershed infarction are possible.
In states of misery perfusion, compensatory cerebral vasodilation is not possible as the cerebral autoregulatory capacity is exhausted and, as a result, cerebral blood flow decreases proportionally with cerebral perfusion pressure (Figure 1). Possible cerebral collateral circulation routes include: (1) contralateral internal carotid artery (ICA) through anterior communicating artery; (2) posterior circulation via posterior communicating artery; (3) leptomeningeal or pial collaterals; (4) collateral circulation from external carotid artery (ECA) with retrograde flow and connections with ophthalmic artery, extracranial connections between ECA or vertebral artery (VA) branches and distal ICA; (5) collaterals through dural meningeal arteries to cortical arteries; (6) anterior cerebral artery (ACA)-posterior cerebral artery (PCA) connections via the limbic loop; and (7) anterior spinal artery collaterals with the vertebrobasilar circulation.
Medical management principles
Medical management strategies are essential to treatment of cerebral ischaemic events and prevention of recurrent strokes in face of cerebral hypoperfusion. These include: (1) cautious individualised blood pressure management (usually systolic blood pressure targets of 130-160 mmHg for those with severe bilateral carotid stenoses); (2) maintenance of fluid status to maintain appropriate plasma oncotic pressures for adequate cerebral perfusion; (3) anti-platelet and anticoagulant therapies (single anti-platelet agent and anticoagulant for those with embolic strokes or in the setting of cardiac arrthymias; dual anti-platelet therapy, with laboratory evidence of responsiveness to these agents, for those with atherosclerotic disease or perforator events), (4) statin, and (5) glycaemic control.
Treatment of underlying brainbody interactions are also essential, including attention to haemodynamic stability, cardiac status, optimising cerebral oxygen delivery with avoidance of anaemia, goal-directed therapy for sepsis, optimisation of renal perfusion and avoidance of coagulopathy and encephalopathy due to underlying multi-systemic involvement, particularly renal or hepatic impairment.
Identification of surgical candidate
For patients with symptomatic severe (> 70 per cent) carotid stenosis, carotid endarterectomy or angioplasty/stenting is considered. Thrombectomy is considered for patients with embolic strokes to large size cerebral vessels. For patients who have been medically optimised but are still at risk of ischaemic symptoms of haemodynamic insufficiency due to ICA/MCA stenosis/occlusion in the setting of hypotension or orthostasis, one can identify candidates with reversible hypoperfusion, exhausted autoregulation and impaired vasodilatory reserve. Consideration of extracranialintracranial bypass procedure can be reliably made to identify patients who have reasonable chances of augmentable flow-induced long-term cerebral blood flow re-organisation (collateral shift) while preventing future hypoperfusion events. Identification of these candidates is made after blood pressure management, antithrombotic therapy and treatment of underlying brainbody interactions targeted at optimising cerebral blood flow and oxygen delivery.
Investigational adjuncts
In addition to clinical findings on presentation and with monitoring (Table 2), other adjunctive investigations are useful in identifying such surgical candidates. CT perfusion scans demonstrate ischaemic penumbra of increased time-to-peak (TTP, time between first arrival of CT contrast intracranially and its peak concentration), increased mean transit time (MTT, average time for blood to travel through a volume of brain), with relatively preserved cerebral blood volume (CBV) due to vasodilation and recruitment of collateral flow, and decreased cerebral blood flow (CBF). As reference, an infarcted core shows increased TTP, increased MTT, decreased CBV and decreased CBF. SPECT (single photon emission computerised tomography) scan with acetazolamide (DiamoxTM) is used to identify patients with haemodynamic insufficiency who exhibit reversible hypoperfusion and decreased cerebrovascular reactivity when challenged with acetazolamide (Figure 3a-c). In those who are in the misery perfusion stage of haemodynamic insufficiency, they are already maximally vasodilated and dysautoregulated. In this regard, they cannot further vasodilate in response to increased carbon dioxide tension from diuretic acetazolamide, a carbonic anhydrase inhibitor.
Quantitative MR angiography (q-MRA)’s non-invasive optimal vessel analysis (NOVA) is also essential to quantify and measure blood flow through large vessels of the Circle of Willis (Figure 3b). Together with formal cerebral angiography, it can be used to estimate pial and collateral flow. It gives reasonable estimates of augmentable flow to ensure appropriate blood velocity ranges after bypass, and also in anticipation of longer term collateral shift, cerebral blood flow re-organisation.
Surgical procedure
Direct superficial temporal artery (STA) [donor] and middle cerebral artery (MCA) M4 cortical branch [recipient] bypass is generally preferred. Meticulous attention to blood pressure control, maintenance of intravascular volume and depth of anaesthesia are essential to avoid cerebral hypoperfusion during these cases with underlying steno-occlusive disease. Intraoperative end-to-side anastomoses are performed using 10-0 nylon sutures with indocyanine green (ICG) and intra-operative angiographic confirmation of anastomotic patency. Individualised blood pressure goals with gradual liberalisation of these parameters are done post-operatively with continuation of antithrombotic agents to maintain anastomotic patency and to avoid reperfusion-related injury.
Read More: https://www.europeanhhm.com/medical-sciences/management-of-cerebrovascular-steno-occlusive-disease
#healthcare#hospitals#health#medical care#doctors#healthy lifestyle#health and wellness#medical equipment#technologies#cerebrovascular#steno
0 notes
Text
軽症のCOVID-19から回復した患者の脳灌流
脳灌流低下は、COVID-19の重症型と軽症型の両方で報告されています。この研究の目的は、無症候性の新型コロナウイルス感染症患者の全体的および局所的な脳血流(CBF)を調査することでした。
0 notes
Text

How Heart Disease Can Lead to a Stroke: Understanding the Connection — Aditi Jagtap Pune
Certain heart conditions, including heart failure or severe coronary artery disease, can result in reduced blood flow to the brain due to low blood pressure or poor cardiac output. This hypoperfusion deprives the brain of oxygen and nutrients, says Aditi Jagtap Pune, increasing the risk of an ischemic stroke. Understanding the impact of insufficient blood flow sheds light on the connection between heart disease and stroke.
#aditi jagtap pune#dr ranjit jagtap#dr ranjit jagtap daughter#dr. ranjit jagtap news#dr. ranjit jagtap clinic
0 notes
Text
Some Benefits Of Hyperbaric Oxygen Therapy
Hyperbaric Oxygen Therapy, commonly abbreviated as HBOT is a non-invasive procedure in which patients are administered pure oxygen under higher pressure meters. While "hyper" stands for heightened, the term "baric" is related to pressure. Put together, hyperbaric simply means the inhalation of oxygen under higher atmospheric pressures.
HBOT is generally conducted in acrylic bed chambers where the patients are instructed to lie in a supine position. The pressure is gradually increased by the administration of oxygen from pipes that are attached to the compartment. Patients might experience some discomfort in their ears as long as the fluctuating pressure levels do not stabilize. To minimize such feelings of discomfiture, accessories such as cotton balls or ear plugs can also be used.
There are two kinds of HBOT therapy: mild and hard. Mild HBOT therapy is that in which the atmospheric pressure of oxygen within the chamber varies between 1.3 to 1.5 ATA. In hard HBOT therapy, the scales range between 1.5 to 2.0 ATA. According to the traditional definition of Hyperbaric Oxygen Therapy, oxygen had to be administered at a full 100% to qualify for the label. However, such demarcations have changed over the years. Currently, scientists argue that since ambient air contains 21% oxygen, any percentage that is higher than that qualifies oxygen chamber as HBOT therapy. Whatever, be the case, the therapy has been beneficial for a number of reasons as stated below.
HBOT therapy saturates body fluids and blood with oxygen, making it's content multiply by almost six times. With the increased availability of oxygen to the cells and tissues, they are activated into an actively functional mode, that is, they are no longer sedentary in their existence, thriving for the want of maintenance. Hyper-oxygenated cells function optimally, without needlessly spending too much of cellular energy.
This therapy improves oxygen supply to the cranial cavity and brain cells, thereby triggering them into an active mode. This procedure has proven to be extremely effective for the treatment of cerebral hypoperfusion and neuroinflammational tendencies in autistic children and adults. HBOT assists in cellular metabolism and the production vital glucose, which in turn, leads to the formulation and generation of neurotransmitters. These transmitters play an important role in the effective functioning of the brain.
This therapy stimulates the production of stem cells which play an important role in repairing the damaged cells and tissues.
HBOT also accelerates the growth of new blood vessels, which only result in better supply of blood and oxygen to the different parts of the body. New capillaries also ensure better circulation of drugs and medicines to the tissues and muscles, and improves the body's ability to fight the harmful effects of micro-organisms.
Hyperbaric Oxygen Therapy also helps in the production of collagen and the generation of new skin.
There are enzymatic and molecular changes, and the body's defensive capacity is improved. With regular therapy, white blood corpuscles improve in their ability to fight bacteria and other foreign bodies like fungi, waste by-products and dead cells.
Research has shown that HBOT therapy helps to increase the body's capability of producing glutathione by almost 15%.
It is also beneficial for repairing the damage undergone by cells and tissues owing to radiation therapy.
The extra supply of oxygen to the brain also helps to mitigate the poisonous effect of carbon monoxide.
It is effective for treating patients with gas gangrene, as it helps in annihilating certain types of anaerobic bacterial growths.
Hyperbaric oxygen therapy is beneficial for treating a number of conditions like autism, stroke, cerebral palsy, multiple sclerosis, Alzheimer's disease, air embolism, arthritis, gas gangrene, carbon monoxide poisoning, in short, from a number of debilitating conditions that result due to the paucity of oxygen supply. With the improved supply and circulation of oxygen, patients can enjoy better health conditions and lifestyle patterns.
0 notes
Text
The priority nursing diagnoses for the child with a fractured left femur and mild head injury are acute pain and head injury. A nurse needs to thoroughly examine this child’s whole body to identify regions of discomfort or soreness, crepitus, deformity, loss of function, and the position and quality of pulses and ascertain the neurovascular condition of the limb (Haimes & Blankstein, 2019). For a patient with a fracture, acute pain is the most appropriate nursing diagnostic. The GCS is performed after a thorough evaluation of the patient’s condition, which includes ensuring the safety of the patient’s airway, breathing, and blood circulation after a head injury. Dietary and physiotherapy nursing interventions are given priority after being transferred from ICU. Providing a healthy diet helps bone repair and keeps the patient’s weight-bearable to restrictions due to the injured limb. The patient should be helped to ensure the safe use of mobility aids and assistive gadgets. The child will require retaining his airway is clear and ensuring enough breathing while at rest ((Haimes & Blankstein, 2019). Intracranial pressure (ICP) monitoring may also be necessary in the child’s case as it may assist in preventing more secondary injuries (by recognizing and treating hypoxia, hypercapnia, or hypoperfusion). The risks of Foley catheter placement include urinary infections, bladder spasms, and urethra damage. Using a urinary catheter, such as an indwelling Foley catheter, increases the risk of infection. Urinary tract infections may result from placing a Foley catheter (Saifullah et al., 2020). Epididymitis and orchitis are both possible complications of urinary infection in men. The placement can also cause additional issues, such as bladder spasms (similar to stomach pains), obstructions, leaks, and urethra damage. Patients who are unconscious or have serious issues that prevent them from moving can have an indwelling catheter inserted to drain urine into a bag linked to a leg and emptied through a tap at the bottom. After being discharged from the Intensive Care Unit, the patient does not need an indwelling Foley catheter. The patient’s muscles will need to be strengthened and loosened up through physical therapy. It is common for patients to begin walking with the aid of a physical therapist within the first few days following an accident or operation. Hence, the child does not need an indwelling Foley catheter, and his chances of full recovery can be increased through regular activities. ORDER THIS PAPER NOW. 100% CUSTOM PAPER CategoriesNursing homework help Leave a Reply Cancel replyYour email address will not be published. Required fields are marked *Comment * Name * Email * Website Save my name, email, and website in this browser for the next time I comment. Post navigation Previous PostPrevious Students will be assigned to small groups by the end of Week 2. Group discussionNext PostNext Please review all materials on communication to receive attendance credit for th
0 notes
Text
0 notes
Text
i flirt in the fucking weirdest way possible.
i flirt by... explaining things? like i say something smart, person im flirting with say another smart thing, and we get progressively closer saying shit like "shock is a state of generalized tisular hypoperfusion" and continuing to explain it and end up kissing
damn. its hot, but damn
1 note
·
View note