#oliguria
Text
Oliguria = output of < 500mL of urine
Creatinine clearance rate and glomerular filtration rate (both urine tests) decrease in kidney insufficiency, causing an increase in reuptake of BUN, so high serum BUN and creatinine result.
Azotemia results (high levels of nitrogen/urea in the blood)
0 notes
Text
Diuretics use in patients with Acute Renal Failure and Septic Shock by Dr Dale Ventour in Journal of Clinical Case Reports Medical Images and Health Sciences

ABSTRACTS
Loop diuretics should be administered in the ‘de-resuscitative’ of sepsis, this occurs after the initial resuscitative period during sepsis. The dose of diuretic should be monitored and a continuous infusion of furosemide, which is the most prescribed diuretic, should be no greater than 4mg/min.
There needs to be caution with co-administered nephrotoxic agents such as aminoglycosides, other diuretics, NSAIDS as these increase the toxicity profile. Despite the popular use of loop diuretics in critical care, loop diuretic use in sepsis has not been shown to decrease patients’ mortality.
This manuscript aims to discuss the use of diuretics in patients with septic shock exploring the evidence and consensus about the use of this therapy in critically unwell patients.
KEYWORDS: loop diuretics, septic shock, oliguria, ototoxicity, renal failure, critical care.
INTRODUCTION
Loop diuretics can be used in critical care to manipulate urine output in patients with hypoperfusion. Loop diuretics benefit the renal medulla during hypoxia by decreasing the tubular energy requirements(1, 2), which makes it a very attractive addition for patients with septic hypoperfusion. A Meta-analysis by K M Ho et al 2006 did not find in reduction in in-hospital mortality, requirement for dialysis, length of stay or number of patients remaining oliguric(3). A positive diuretic response to furosemide may indicate that the patient is in the ‘de-resuscitative’ phase of sepsis and that renal impairment is less severe. It is also appreciated that patients with non-oliguric renal failure have a lower mortality than patients with oliguric renal failure(4). The timing, duration, and dosing of diuretic therapy, plays a significant role in the morbidity associated with diuretic therapy in sepsis.
Diuretics in critical care; is used as a prophylactic measure that is, to prevent the onset of renal failure; to alleviate renal impairment in patients with established renal compromise or to convert oligo uric to non-oligo uric renal failure. There was no evidence in the meta-analysis by Ho et al 2006 that there was any benefit in the above listed uses of diuretics(3). There was great heterogeneity between groups in this analysis and most patients had existing renal impairment so that extrapolation to critical care patients with sepsis is problematic.
The goal of transitioning a septic patient from oligemic to non-oligemic renal failure is associated with a decreased mortality trend and diuretic therapy might aid patients with regard to normalizing positive fluid balances (5) but this intervention has associated risks and complications.
Diuretic therapy should be initiated not based on urine output but when the patient has transitioned from the early resuscitative phase to the “de-resuscitative” phase of septic shock. The transit point is determined clinically as the patient is no longer fluid responsive as per passive leg raises or with static/dynamic cardiac output monitoring, is less academic and inotropic support has stabilized or decreased.
Why does this matter?
There are associated side effects when initiating diuretic therapy in critically unwell patients such as ototoxicity, hypernatremia, hypotension and worsening renal function.
OTOTOXICITY
There is changes in the endolymph ionic concentration and fluid composition secondary to the inhibition of the Na-K-2Cl transporter within the stria vascularis of the inner ear(6). Aminoglycoside antibiotics potentiate furosemide ototoxicity, but noise trauma apparently does not. Methods of avoiding ototoxicity are suggested including slow continuous infusion rather than bolus injection, use of divided oral dose regimens, and the measurement of blood levels to avoid exceeding 50 mcg/ml of furosemide(6).
In heart failure patients as outlined by Salvador et al 2005(7), continuous infusions of furosemide resulted in a lower incidence of ototoxicity and fewer side effects. Continuous infusions resulted more than 30% increase in sodium excretion than bolus administration.
The ototoxicity induced by furosemide can be reversible although permanent deafness has been reported. The complication is related to both the peak serum drug concentration and the accumulated dose from continuous infusion and is aggravated with the concurrent use of aminoglycosides or Non-Steroid Anti-Inflammatory Drugs. The maximum recommended infusion dose is 4 mg/min (8).
HYPERNATREMIA
Hypernatremia as outlined by Hai-bin Ni et al 2016(9) was associated with increased mortality whether or not it was associated with diuretic use, this is a common side-effect with liberal diuretic use within the Intensive Care.
Hypernatremia as an independent predictor of mortality regardless of aetiology, speciality and across patients with different ages and co-morbidities (10-14). Risk factors include advancing age, co-existent renal impairment, associated use of nephrotoxic drugs. The phenomenon is poorly understood but correction is based on balancing renal water loss with overcorrection with isotonic solutions versus hypotonic water correction.
It necessities the use of Nasogastric water, naturetics, 5% Dextrose administration, low sodium enteral feeds and re-constituting drugs with 5% Dextrose rather than saline to correct this electrolyte imbalance. These interventions further complicates the management of the critically unwell patient, prevention is of tantamount importance.
WORSENING RENAL FUNCTION
Numerous studies have indicated that there is no benefit in the use of diuretic therapy to improve outcomes in patients with established acute renal failure in Intensive Care (15, 16). Maeder et al 2012, indicated a trend toward worsening renal function in elderly patients with chronic renal failure within a medical Intensive Care(17). His definition of chronic renal failure was >0.5 mg/dl increase in baseline creatinine over the 6 months follow up, again the findings not only supported renal failure as an independent predictor of mortality, but it was also aggravated by escalating the loop diuretic dose [17].
HOW DO WE ADMINISTER LOOP DIURETICS?
Meta-analyses support the administration of loop diuretics as continuous infusions versus boluses as there is better diuresis at a lower cumulative dose(18), this will inevitably lead to fewer side effects and more efficient fluid balance.
It has been suggested that the infusion dose be limited to 4mg/min to minimize the side effect profile as the loop diuretic has a ceiling effect around this dose [9]. It is also proposed by this author that the diuretic be administered in the ‘de-resuscitative’ phase of sepsis to manage the patient’s overall fluid balance.
The use of diuretics should be for the shortest time possible as there are considerations for electrolyte abnormalities and ototoxicity with a clear focus on serum sodium to gauge the amount of free water loss. While I am not against the administration of loop diuretics in septic patients with acute renal failure the timing of administration of the drug class with the “de-resuscitative phase of sepsis” is vitally important.
DISCUSSION
There is a paucity of evidence supporting the use of loop diuretics in septic critically unwell patients with acute renal failure leading to improved mortality(19, 20). These studies have highlighted increased risk of complications such as electrolyte disturbance without reducing the need for continuous renal replacement therapy or the duration of renal replacement.
Ototoxicity remains an underreported complication as there can be other contributing factors for altered hearing after the critical care episode. This complication will contribute to a patient’s post critical care morbidity affecting patient and patient’s family quality of life.
The is wide variation with the timing, dose, and indication for diuretic therapy in critical care. Bolus administration, low-dose continuous infusions (20) or high dose titrated to urine output or daily fluid balance are all methods used to administer diuretics. Liborio et al in his observational study of over 14,000 patients found no decreased mortality in critically ill patients with over 60% of these patient experiencing sepsis with a dose of furosemide up to 80 mg/day(21)
CONCLUSION
The indication and use of diuretics in septic patients with oliguric acute renal failure is varied and confounded by timing and effective dosage. However, there are significant complications associate with the use of diuretics in the critical care population and need serious considerations prior initiation of this therapy as there is no mortality benefit in septic patients with acute kidney injury.
Acknowledgement: No acknowledgement
For more information: https://jmedcasereportsimages.org/about-us/
For more submission : https://jmedcasereportsimages.org/
#loop diuretics#septic shock#oliguria#ototoxicity#renal failure#critical care#NSAIDS#hypoperfusion#heterogeneity#hypotonic water#Dr Dale Ventour#jcrmhs
0 notes
Video
youtube
COMMUNICATION SKILLS STATION OF CALL CONSULTANT | OLIGURIA
COMMUNICATION SKILLS STATION OF CALL CONSULTANT | OLIGURIA MRCS B OSCE - MOCK EXAM Bli medlem i kanalen för att få åtkomst till flera förmåner: https://www.youtube.com/channel/UCkkvon_blxinTHc7DGuYkpQ/join
#youtube#communication skills oliguria acutekidneyinjury medicine doctor surgery health medical healthcare mrcs mrcsbosce femalesurgeon youtube membe
0 notes
Text

physical dependence also goes under P
0 notes
Text
My Fighter
Requested Here!
Pairing: Jim Street x fem!SWAT!reader
Summary: When a serial killer you arrested breaks out of prison, you and your team are tasked with finding him. You lie to the team and meet with the killer, but Street rushes to help you and reminds you why he can't lose you.
Warnings: canon-typical violence and action (OC serial killer, depiction of murder scenes, mentions of blood and murder, threats), angst, fluff and comfort at the end. there are a few references from various episodes but no spoilers!
Word Count: 3.9k+ words
Masterlist Directory | Jim Street Masterlist | Request Info\Fandom List
“Street, hands to yourself, please. This is a workplace and I’m trying to make sure this raid goes well,” Hicks says.
Street ignores Hicks’ request, as well as Hicks’ obvious exasperation as he pinches the bridge of his nose.
“Street,” you whisper, shrugging one shoulder up.
“Fine,” he grumbles, removing his hands from your sides.
“Thank you,” Hicks sighs. “Now, you’ve got blueprints and Hondo’s breach plan is good. Deac, let’s not have another Schupatz situation, okay? Everyone stay where you’re supposed to be.”
“I’m still shocked you remembered him,” Luca comments.
“Everyone remembers big arrests,” Hondo argues. “And Deac’s just a good friend.”
“It’s true,” Deacon agrees. “First arrests are typically memorable.”
“Someone say something about memorable first arrests?” Rocker interjects from the doorway. “Mine was a drug maker. Not a seller or user, manufacturer.”
“Don’t get too cocky,” Hondo calls. “Our girl over here took down a serial killer for hers.”
“I got lucky,” you say softly.
“How so?” Rocker inquires.
“He killed one of my friends. Tried to cover his tracks, but I knew her well enough to spot every little inconsistency.”
Rocker nods before his team calls for him. As he walks away, Hicks goes over the details of your current case once more. Street’s hand returns to your back as a silent comfort after talking about one of the toughest cases you’ve ever worked on. Hicks doesn’t mention it this time but gives you an encouraging nod as you walk out of the situation room.

Hondo’s phone rings as you climb back into Black Betty after a successful raid. He furrows his brows and mumbles, “Someone’s more overbearing than usual,” before he answers the call on speaker.
“Commander,” Hondo greets.
“Back to the station. Now,” Hicks demands.
“Yes, sir. But the raid was good, so we’ve got another-“
“There was a breakout at the state prison,” Hicks interrupts. “We need 20-David on this.”
“We’re on it,” Tan agrees.
“Are you all here?” Hicks asks.
“Yes, sir,” your squad says together.
Hicks sighs, and you can picture him rubbing his jaw before he says, “Noah Oliguria broke out.”
Your eyes widen at the mention of his name, and you turn toward Hondo to make sure you heard Hicks correctly. Street moves to your side, and you know that you did. Your first arrest, the man who killed your friend, a serial killer who was supposed to be off the streets until he took his last unworthy breath, is now running free in Los Angeles.
“Where’d he go?” you ask quietly.
“He stole a van,” Hicks says, “we’ve been tracking it on traffic cams, but we need S.W.A.T. ready to roll the moment we have an opening.”
“He’s going to kill again.”
“We don’t know that.”
“I do. When I put the cuffs on him, he promised that someday he would kill again. He’s not out for tacos, Commander, he broke free to get back to what he knows.”
“It’s okay,” Street says softly.
He lays an arm over your shoulders, and you lean against him as Hicks tells Hondo more about what they know. You don’t care about how Noah broke out; you want to ensure he gets put back in. With Street beside you, your anger begins melting into fear. The last time Noah was on the streets of Los Angeles, a lot of people died, including someone you cared about deeply. That won’t happen again – it can’t, not while you can stop him.
“We’ll get him,” Hondo promises as he ends the call. “And you’re not alone this time.”

Your leg bounces with bottled anxiety as you sit outside the situation room. Dressed in your gear, you are ready to go. The rest of your team is inside with Hicks, but they decided it would be best if you didn’t have to relive the initial case against Noah. You remember it too well, anyway.
“Hey,” Street says as he lowers to sit beside you.
His hand lands on your knee, and you slow your breathing and movement at his touch.
“Hondo thinks we may have a lead. If you want to sit this one out, though, no one will blame you,” Street explains.
“I can’t sit here and do nothing, Jim.”
“I get it,” Street promises, nodding.
“You’re not helping,” you mumble as you look at him.
Street’s hand moves from your knee to the side of your thigh as you move. He furrows his brows at your comment, and you offer a small smile.
“You’re being really serious.”
“Oh, right,” Street agrees playfully. “Would you prefer a joke or just a generic sarcastic comment?”
You tap your chin as you think, but as your worry disappears (one of Street’s superpowers, you think), Hicks yells for 20 Squad to get ready to roll. Street’s hand slips into yours as you rush to Black Betty, and you can only hope to beat Noah Oliguria this time.

“Don’t,” Hondo demands as you step to his side. He extends an arm across your chest and shakes his head. “You don’t want to go in there.”
You turn away from him and press your fists harshly into your sides. Too late again. Last time you found one of Noah’s victims, it was your friend, and she had endured a bitter end until she couldn’t anymore. Despite your determination to stop him again, Hondo is right; you’ve seen enough of Noah’s work to know you don’t want to see anymore.
“He’s not going to stop, Deacon,” you say as he exits the building. “We don’t have time to go back to H.Q. and wait for a lead.”
“We don’t have to,” Street calls. “He left us one.”
You and Deacon rush toward Street, who lifts a blood-covered motel keycard. Noah’s, you assume. It’s not much, but it’s something. As you sit beside Street while Luca drives to the motel, you can feel your heart and stomach flipping with anxiety and memories you’d rather forget.
Street takes your hand and squeezes three times. Part of you wants to climb into his arms and never come out, but the other argues that you have a duty to the men and women that Noah has already killed and those he plans to. No one on your team would force you to sit this case out, but if Noah gets close to anyone you love, you won’t have a choice.
“Hondo,” you say. “Can I make entry?”
He nods slowly before agreeing. Noah has tried to taunt you from behind bars before, but if you see him face-to-face, you’ll let him know he will never get under your skin. You’re not scared of Noah Oliguria, but the idea of losing someone else to him terrifies you.
After you exit Black Betty, you run silently toward the room listed on the key. There’s an overturned housekeeping cart beside the door, and you nudge it out of the way. A blood-soaked towel falls from the laundry bin, and you don’t hesitate to kick the door open.
Street enters behind you, but your sudden stop causes him to grab your hips as he tries to stay upright. The scene on the bed holds your attention, though. Noah never seemed to have a type about who he killed. He simply liked the act, the blood between his fingers, a pulse fading under his touch as the life faded from his victim’s eyes. That’s why this scene is so wrong.
“It was too fast,” you murmur.
“Motives change,” Hondo points out. “He’s been locked up, maybe he- maybe he’s making up for lost time.”
“No, the first one was right.” You look around quickly before you decide, “He heard us coming. We just missed him.”
“That tracks,” Luca agrees. “M.E. said the first body had only been there about ten minutes. We’re not far behind him.”
“Far enough,” you snap. “We cannot let him kill again.”
Hondo looks at Street, who nods before grabbing your shoulders. He steers you out of the room with a loving but firm grip, and you let him lift you into Black Betty as you remember what Noah did on the other side of the motel wall.
“He’s going to keep killing,” you whisper.
You hold Street’s wrists as he kneels before you. He nods but doesn’t look away from you as the coroner and a detective arrive.
“You know it takes time. What he did to your friend, to you, was awful. Getting over that is impossible, but we can’t rush this,” he says.
“I know that. But… it feels like it’s my fault. I caught him once; why can’t I do it again?”
“It took you months.”
You shake your head and prepare to argue, but Street leans closer as his hands move to either side of your neck, his thumbs brushing over your jaw.
“Honey,” he murmurs. “It took you time, then, too. Be patient with yourself, okay? Those women, their blood isn’t on your hands, and you’re going to go crazy pushing yourself like this.”
“We’ll catch him eventually, right?”
“We always do.”
Street moves up to kiss your forehead before he sits beside you. The team joins you in Black Betty a moment later with another clue to chase. It feels like a breadcrumb trail, but you will always be too far behind, too slow to catch the man leaving the trail. Street keeps his hand in yours as Luca exits the motel parking lot and you gladly accept the comfort.
Your phone rings as Hondo explains the clue they found: a receipt for dry-cleaning to be picked up down the road in just under an hour. It’s an unknown number, but Hondo permits you to answer it anyway. With your helmet still on, you answer it and immediately switch it to speaker. You don’t speak before someone says your name.
“Heard you’re with S.W.A.T. now. Guess that puts a new meaning on the term ‘chasing’ me, huh?”
You recognize his voice immediately and try to end the call. Street grabs your hand gently and shakes his head, and Hondo motions for you to keep him talking.
“Noah,” you force out. “What do you want?”
“Ten years ago, you arrested me because I made some mistakes. That’s what you said at the trial. I didn’t make mistakes. Your friend was a fighter, and she wrecked her apartment. Someone leaving clues isn’t a mistake. Speaking of your friend… how’s her family?”
“What do you want?” you repeat slowly.
“To catch up. 12th and Maple, tonight at 8. Just you and me.”
“Why would I do that?”
“Because if you don’t, I’ll kill someone else. Actually, I have a better idea… for every half hour that you don’t show, I will kill another woman in L.A. How’s that for reason to come?”
“Pretty good,” you agree. “12th and Maple?”
“Right. See you tonight. Maybe wear one of those outfits that your friend liked so much.”
The line beeps as he ends the call, and you drop your phone into your lap.
“You’re not going,” Jim says.
“Yes, I am,” you argue.
“No, you’re not. We’re not letting you go off alone to meet an escaped serial killer!” Hondo adds.
“And I’m not letting him kill more women!”
“He’s going to kill anyway,” Jim says. “And he may try to kill you. Please, just trust us and don’t go meet him alone.”
“We’ll ask Hicks about setting something up,” Deacon offers. “Maybe no one else has to die.”
“Okay,” you agree. “But… I think I need some time. Can I take a little while this afternoon?”
“Of course,” Hondo answers. “As much time as you need.”
“I’ll take you home,” Street offers.
“Thank you, but I- I need to be alone right now.”
Street nods, and you lean back for the remainder of the ride to H.Q. You’re lying, but think Jim believes you. Deacon’s right, no one else is going to die at the hands of Noah Oliguria, and you’re going to make sure of that.

“East Ducasse Alley off 12th and Crocker,” you say to yourself as you drive through the garment district for your 8 o’clock meeting.
You changed the meeting place to ensure your team couldn’t arrest Noah before you got answers. They think you’re at home right now, and the meet has been called off, but as you exit your car and walk into the alley, you wish you’d told them the truth.

“Jim Street,” Street says as he answers the phone. His attention is on the screen before him until the person on the other end of the line speaks.
“So, I’ve heard. You’ve got good taste in women, picked a fighter… I guess we’ll see if she’s strong enough to fight someone like me, huh?” Noah Oliguria taunts.
The call ends immediately after Noah finishes. Street pulls his phone away from his ear and stares at the screen. He hasn’t heard from you since you let him know you got home, and either Noah thinks the meet is still happening, or you lied.
He opens his tracker app that lets him see where your phone is. Because of your job and its risks, you agreed to let your entire team see your location, though you can turn it off whenever you want. Lucky for Jim, you never remember the ghost mode capability. He sees the small dot with your initials on it at the end of an alley in the fashion district and abandons what he was working on.
“Hondo!” he yells as he exits the situation room. “She went to meet Noah! They changed the location.”
“How do you know?” Hondo inquires.
“He called me. Said we’d found out how much of a fighter she really is.”
“20 Squad!” Hondo calls. “We’re rolling!”
Tan raises his arms in question, but when Luca sees the concern on Street’s face, he yells for everyone to get to Black Betty. Time is limited, but you are family, so they’ll risk everything to get to you.

Noah slides his phone into his pocket as you near him. You stop with several yards between you and cross your arms over your chest in the dirty alley.
“I’m here,” you say. “What now?”
“You remind me a lot of her,” Noah replies. “When she opened the door of her apartment, I knew she’d be special. Even after she got me caught, she stayed special. You know why?”
“I’m not here for a trip down memory lane,” you snap.
“She was special because she led me to you. I watched you move around her place so easily, and I couldn’t help but wonder what it would have been like if you’d walked in instead of her.”
“If you just brought me here to tell me that you want to kill me, I’m calling my backup to take you back to the cell you came from.”
“What backup? Your boyfriend Street was still at the station when I called. We’re alone, and we’ve got plenty of time for that trip down memory lane. I had to finish early because of your team once today, and I won’t let it happen again.”
Noah rushes toward you, and you bend your knees slightly to catch his shoulders before impact. He flips onto the ground and pulls you with him. As you fight for the upper hand, you see a knife, a gun, and something else under his shirt. He came prepared to kill you and to make it hurt.
“You made another mistake,” you taunt as you kick him off of you. “I was never going to come alone.”

“Luca, a little faster!” Street yells.
“I’m going, Streeter,” Luca replies calmly. “We’ll get there.”
“We haven’t been ahead of him since the moment he walked out of that prison.”
“Street, you have to keep it together for her,” Deacon says. “If you go in there like this, you won’t be able to help anyone.”
“She thinks their blood is on their hands,” Street responds. “But if anything happens to her, it’s all on me. I let her go.”
“We all did,” Hondo adds. “But we’re in a position to help her before anything can happen. So, let’s keep it tight, stay liquid, and fight for our own.”
“30 seconds!” Luca alerts the team as he nears your location.
“Okay,” Street agrees. “Let’s do this.”

Noah’s knife falls from his waistband as he pulls you across the asphalt. You try to hide your yell of pain and use his own momentum to knock him over your head. Turning quickly onto your stomach, you begin to push yourself up before Noah moves the barrel of his gun into your face. You stop immediately, frozen on your hands and knees.
“I was right,” he says past a bloodied lip. “You’re putting up a better fight than her.”
“Then let’s keep going,” you reply.
“I don’t think so. Not here.”
Noah takes one hand from the gun and pulls a pair of handcuffs and a rope from his pocket. That’s what you couldn’t place earlier: the handcuffs. They look like they already have blood on them, and you wonder if it’s his or someone else’s. While he’s distracted and moving, you raise your hands and push his arms away from you. The gun falls to the ground, and you shove Noah backward and against the wall behind him.
He grunts before laughing, and you clench your jaw when you realize he closed one end of the handcuffs around your left wrist.
“I’m a fighter too,” he says lowly.
“You’re a coward with a gun,” you accuse.
“Don’t.”
“Or what?”
He kicks your shin, and your legs slide out from under you as you fall to the ground. With his knife retrieved from the ground, Noah steps back to look at you. Your gun is digging into your back, and you take the opportunity to tug against the handcuff. He’s standing on the other end, and as one hand moves beside Noah, you pull your gun from its holster.
Noah steps back to your side and poises the knife above your chest. He raises it, prepared to plunge the blade between your ribs and debilitate you before he treats your death like a toy for his enjoyment until you break, and he has to replace you with another victim.
“Remember when I said you’d never kill me?” you ask. “I meant it.”
Noah’s face hardens as he tightens his grip on the knife. He raises it a touch higher, and just as he prepares to swing down, his eyes widen as a shot echoes in the empty alley. Noah drops the knife, and you ignore it as it lands on your stomach. His hand falls to the wound in his abdomen before he falls back. You tip your head back against the road and take a deep breath. Someone yells your name, and you sit up quickly with your gun still grasped tightly between your hands. The knife clatters as it falls from your movement, and you lower your weapon when you see Street running toward you. Hondo has his hand to his ear, likely calling for backup and an ambulance for Noah, who is still conscious and groaning in pain.
Street takes your gun and knocks the knife away from your side. He raises his gloved hands to your face and tilts your head gently as he searches your skin for any sign of injury. You hook your fingers over his wrists as you lean toward him.
“Jim,” you breathe out. “You came.”
He nods and you appreciate the silent promise that he will always come. Before you can think to ask, he retrieves a key from his pocket and removes the bloody handcuff from your wrist. He flips your hand to ensure the blood isn’t yours before giving you room to stand.
You lower your hands to the concrete and push yourself up while Street hovers beside you as you stagger with each movement. An ambulance approaches the end of the alley, but you don’t look toward Noah. He screams as Deacon applies pressure to his wound, and you turn toward Street.
“Get her out of here,” Hondo calls. “Hicks said she’s good to give her statement in the morning.” He looks at you to ask, “You good?”
“Can’t complain,” you answer. “Thank you.”
“Of course. Just give us a heads-up next time, would you?”
“No, we won’t have a next time,” Street adds.
You nod as Street leads you to your car. He takes the keys from your pocket and helps you into the passenger seat before climbing behind the wheel. You each have a lot to say, but he stays quiet as he navigates through LA and drives toward your home.
Once you’re inside, changed, and comfortable in Jim’s arms, you have the space to talk and fall apart. He has a firm arm around your waist as the other holds your head against his shoulder. Your arms are wrapped over his shoulders as you breathe against him. You’re in pain, but nothing could make you separate yourself from Jim in this moment.
“I’m sorry I went without telling you. I’m sorry for going at all after you asked me not to,” you apologize against Jim's shirt.
Jim’s hand moves from your head to your back as he rubs comforting strokes against your spine. His hand slips under your shirt at the bottom, and you lean further against him with the unhindered contact.
“I’m not mad at you,” he promises. “Noah called me.”
“He told me he called you and you were at the station, so you weren’t coming. What’d he say to you?” you ask as you pull back to see Jim’s face.
“Basically, that he was going to hurt you. He said he was going to make you fight and see how good you really are. I… I don’t want to lose you.”
“I’m sorry.”
“No, listen. I don’t want to lose you, and that’s why I asked you not to go. Not because I don’t trust you or I’m scared of Noah, anything like that. But he was after you and I can’t bear the thought of losing you. I love you.”
“I know. I love you, too,” you reply softly.
“Then could you maybe try to act like it every once in a while?”
Street smiles, and your lips quirk up to match. You lean forward and kiss him, smiling against his lips as his hand travels across your back to bring you closer.
“I’ll remember that from now on,” you promise as you pull back. “And try not to do anything that could take me from you. I love you. I love you so much, Jim.”
“You know that none of this was your fault, right?” Street asks as he moves his hand from your hip to your cheek.
“Thanks to you, I do. You got me through today.”
“Kind of what I’m here for.”
“I see you chose sarcastic comments without me.”
“Well, you never answered the question.”
You shake your head lovingly and return to your previous position against Street’s shoulder. You love him, and you know he loves you; the comfort, reminders of what you mean to him, and how he treats you leave no room for doubt. Lying to him and risking your life, putting him in a place where he could lose you, wasn’t worth it.
“Can you say it again?” you ask, trailing a hand up Street’s chest and to his jaw.
“Say what?”
“You called me honey earlier.”
Street turns his face against your hand and leans into your touch as he says, “I love you, honey, and I’m going to tell you with every breath I have left.”
You smile shyly at the new pet name but take the opportunity to tease, “Hicks will love that.”
“Doesn’t matter, because I love you.”
Street pulls you into another kiss, and though you know life will never be easy, loving Jim Street is.
#hanna writes✯#jim street x fem!reader#jim street x reader#jim street fic#jim street imagine#swat x reader#swat cbs#fem!reader#requests
118 notes
·
View notes
Text

Hypothermia, starvation, lead poisoning, zinc deficiency and diseases including scurvy, along with general exposure to a hostile environment while lacking adequate clothing and nutrition, killed everyone on the expedition.
Early symptoms are malaise and lethargy. After one to three months, patients develop shortness of breath and bone pain. Myalgias may occur because of reduced carnitine production. Other symptoms include skin changes with roughness, easy bruising and petechiae, gum disease, loosening of teeth, poor wound healing, and emotional changes (which may appear before any physical changes). Dry mouth and dry eyes similar to Sjögren's syndrome may occur. In the late stages, jaundice, generalised edema, oliguria, neuropathy, fever, convulsions, and death.
3 notes
·
View notes
Text
Nephritic vs Nephrotic Syndrome
Nephritic
-- mild proteinuria
-- edema
-- hematuria
-- hypertension
-- oliguria
Nephrotic
-- proteinuria
-- edema
-- hypoalbuminemia
-- hyperitpidemia
-- lipiduria
-- hypercoagubility
#medblr#studyblr#notes#my notes#medical notes#medblr notes#med notes#anatomy#physiology#nephrotic#nephritic#pathology#pathophysiology#pathology notes#pathophysiology notes
6 notes
·
View notes
Text
SUMMARY AND RECOMMENDATIONS
●Triage – Among outpatients identified as having AKI, we refer to the emergency department those who have any of the following: Kidney Disease: Improving Global Outcomes (KDIGO) stage 2 or 3 AKI (table 1); stage 1 AKI with an unclear etiology, or one that cannot be rapidly reversed with simple interventions, or in the presence of a concomitant, uncontrolled comorbid condition; or stage 1 AKI if the initial diagnostic evaluation and management cannot be performed in the outpatient setting. (See 'Identifying patients for emergency department referral' above.)
Those who are managed as an outpatient should be referred for outpatient nephrology consultation if the cause of AKI is not immediately apparent, if initial interventions fail to improve the kidney injury, if glomerulonephritis (GN) is strongly suspected, or when AKI occurs as a complication of treatment of an unrelated condition and future treatment depends upon nephrology input. (See 'Indications for urgent nephrology referral' above.)
●Indications for emergency kidney replacement therapy (KRT) – Emergency KRT should be performed in patients with AKI who have one or more of the following (see 'Evaluate need for urgent kidney replacement therapy' above):
•Hypervolemia with pulmonary edema that does not promptly respond to diuretics (see 'Hypervolemia with pulmonary edema' above)
•Severe hyperkalemia (serum potassium >6.5 mEq/L or those with symptoms or signs of hyperkalemia) (see 'Severe hyperkalemia' above)
•Life-threatening uremic symptoms, such as seizures or severe pericardial effusion (see 'Life-threatening uremic symptoms' above)
•Exposure to certain toxins (see 'Toxin exposure' above)
●Initial management
•Eliminate potential insults – Additional management entails elimination of potential insults, including hypotension, iodinated contrast agents, or medications such as nonsteroidal antiinflammatory drugs (NSAIDs), angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), and nephrotoxins. (See 'Elimination and avoidance of potential insults' above.)
•Treat hypovolemic (if present) – Intravenous fluid therapy with 1 to 3 liters of crystalloid should be administered to patients with a clinical history consistent with fluid loss (such as vomiting and diarrhea), a physical examination consistent with hypovolemia (hypotension and tachycardia), or oliguria. However, fluid therapy should be avoided in patients with pulmonary edema or clear evidence of anuria. Additional fluid management depends upon the clinical condition and response to initial fluid therapy. (See 'Hypovolemic patients' above.)
Among patients with AKI and hypervolemia who are hemodynamically stable and not anuric, we start intravenous (IV) furosemide at 80 mg up to a single dose of 200 mg, or equivalent, to augment the urine output and relieve symptoms. Additional therapy depends upon the response to initial therapy. We typically initiate KRT for volume overload in patients who have anuria for more than 24 hours, who fail to respond to diuretics, or whose response to diuretics is insufficient to avoid worsening hypervolemia due to high obligate intake. (See 'Hypervolemic patients' above and 'Role of diuretics' above and 'Role of kidney replacement therapy' above.)
•Treat electrolyte imbalances (if present) – Electrolyte imbalances such as the following can complicate AKI and need specific management:
-Hyperkalemia (see 'Hyperkalemia' above)
-Hyperphosphatemia (see 'Hyperphosphatemia' above)
-Hypocalcemia (see 'Hypocalcemia' above)
-Hypomagnesemia and hypermagnesemia (see 'Hypomagnesemia and hypermagnesemia' above)
-Hyperuricemia (see 'Hyperuricemia' above)
•Treat metabolic acidosis (if present) – We initiate KRT in patients with oliguric or anuric AKI who are volume overloaded and have severe metabolic acidosis (a pH <7.1), unless the acidosis can be rapidly resolved by quickly correcting the underlying etiology (eg, diabetic ketoacidosis). However, in other patients who have no indications for acute KRT, bicarbonate may be administered instead of KRT to treat acidosis. Diuretics can be used in nonoliguric patients to prevent hypervolemia and to enhance excretion of acid. The goal serum bicarbonate level is 20 to 22 mEq/L and the goal pH is >7.2. Metabolic alkalosis with AKI is usually seen in volume depleted patients and responds to IV sodium chloride infusion. (See 'Managing acid-base disturbances' above.)
●Subsequent management
•Nutrition management – Patients with AKI generally benefit from dietary restrictions on potassium, phosphorous, sodium and fluid intake (1 to 1.5 L per day, except if volume depleted). Given the complexities of nutritional support in these patients and the individual needs of a given patient, we obtain a nutrition consult to best tailor therapy in hospitalized patients with severe stage 3 AKI. For patients with lesser stages of AKI, the need for consultation should be based upon an individual needs assessment. (See 'Managing nutrition' above.)
•Assess for uremia – We perform daily assessment of uremic signs and symptoms (such as anorexia, nausea, vomiting, metallic taste, altered mental status) to determine if KRT may be indicated. KRT initiation in such patients should be approached with a clear goal of monitoring whether or not putative uremic symptoms improve with therapy. Typically, several KRT sessions are required to determine if symptoms resolve with KRT. (See 'Assessing for uremia' above.)
•Assess for fluid and electrolyte imbalances – We monitor serum creatinine, electrolytes, albumin, and measures of fluid balance (weight, fluid intake, and urine output) daily in most patients, although more frequent monitoring may be warranted. (See 'Monitoring and follow-up' above.)
●Follow-up – We advise that patients hospitalized for moderate to severe AKI have an outpatient nephrology evaluation (or primary care if nephrology is unavailable) shortly after discharge. (See 'Monitoring and follow-up' above.)
2 notes
·
View notes
Text
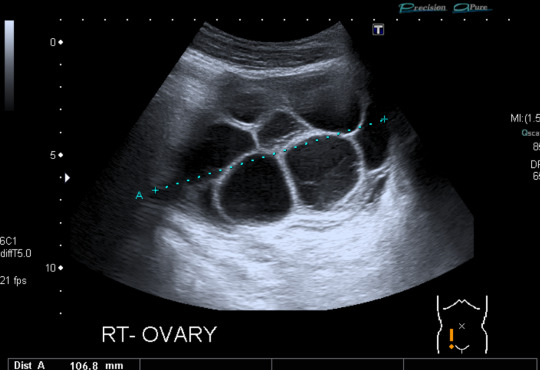

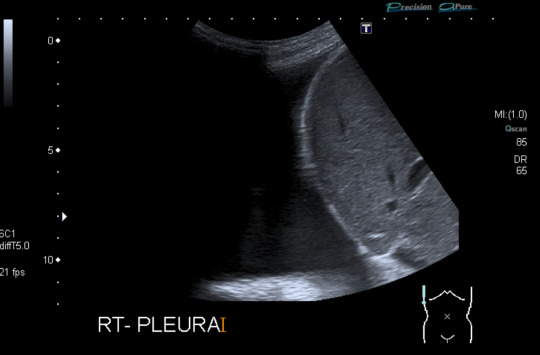
Today's case is a pelvic ultrasound of a 35-year-old woman who presented with abdominal pain and bloating 9 days after initiating controlled ovarian hyperstimulation in preparation for IVF. Ultrasound reveals enlarged ovaries with multiple large follicles, ascites, and pleural effusions. Findings are compatible with ovarian hyperstimulation syndrome (OHSS) which occurs in approximately 5% of women undergoing ovarian stimulation. Fluid shift results in hemoconcentration and oliguria. Treatment is supportive and may include paracentesis or thoracentesis to relive discomfort from accumulated fluid. Severe cases can be fatal, so patient education, prompt recognition and timely intervention are key. Risk factors include PCOS and prior OHSS. Younger age and low body weight are not good predictors of risk, as was previously posited by some papers.
Case courtesy of René Pfleger, Radiopaedia.org, rID: 29070
3 notes
·
View notes
Text
Kidney Failure Treatment Without Dialysis: Exploring Alternatives to Dialysis for Kidney Diseases

Understanding High Creatinine Levels and Kidney Health
One would be worried about one's kidney health if a high level of creatinine were detected within the bloodstream. Creatinine is a waste product produced by the metabolic processes and produced within muscles, later filtered naturally by the kidneys. When the kidneys do not function well, creatinine in the blood can increase, raising concerns with regard to kidney health and necessitating a high creatinine treatment.
The Effects of High Creatinine on the Kidneys
A high level of creatinine suggests the presence of CKD or acute kidney injury. The kidneys' role is to filter out all waste products from the blood, balance electrolytes, and regulate fluid levels. If renal function becomes impaired, the various important mechanisms within the body will be affected, resulting in the accumulation of many waste products, including creatinine, in the blood. High levels of creatinine can cause different symptoms, such as lethargy, oedema, and oliguria.
Treatment of Chronic Kidney Disease
CKD is a serious and progressive condition characterized by gradual loss of kidney function. Chronic kidney disease treatment is to slow the worsening of the disease and to manage complications:-
Blood Pressure Control: High blood pressure can further accelerate kidney injury.
Blood Sugar Management: The most common cause of CKD is diabetes; hence, management through homeopathic kidney problem medication, diet, and exercise is very crucial.
Changes in Diet: Most renal diets advocate the decrease of salt, potassium, and phosphorus consumption. For all special dietary needs regarding kidney function, a consultation with a dietitian will be essential to help make a plan accordingly and provide a cure for chronic kidney disease.
Regular Monitoring: This involves frequent visits to the doctor and blood tests that check the functioning of the kidneys for further chronic kidney disease treatment modifications.
Other Options for Dialysis and Transplant
Some treatments and approaches are available for those in search of treatment for kidney failure other than dialysis and transplantation, and these are to a limited or possibly beneficial level. These include:
Natural Kidney Treatment
Some advocate that natural kidney failure treatment without dialysis will improve kidney health. These are inclusive of:-
Herbal Supplements: Certain herbs, which are natural and carry no side effects, are administered to assist the kidneys. Consumption of these herbs should be discussed with your physician, although they are an excellent herbal remedy.
Changes in Diet and Lifestyle: Food rich in antioxidants and low consumption of processed foods, plus plenty of water intake, will help maintain general kidney health while offering a cure for chronic kidney disease.
Homeopathy
Homeopathy is a system that utilises very minute quantities of drugs in a gentle manner to stimulate the healing powers of the body. Bharat Homeopathy in Gurgaon offers a number of homeopathic remedies and kidney problem medication for renal problems. The goal of homeopathic treatment is to correct the body and improve overall well-being to support overall kidney health. Additionally, complementary high creatinine treatment approaches may be of advantage. These can include acupuncture, yoga, and other practices that are supportive of overall health and may also improve kidney function.
Natural and Homeopathic Kidney Treatments in Bharat Homeopathy, Gurgaon
Bharat Homeopathy offers a range of homeopathic treatments for kidney-related problems in Gurgaon. Homeopathy is a medical science dealing with treatments of an individual as a whole and not treating the symptoms of a disease. The doctors at Bharat Homeopathy follow a personalized approach in devising kidney failure treatment without dialysis plans as per the specific needs of each individual patient.
The salient features of the homeopathic treatment for kidneys at Bharat Homeopathy may include the following:-
Personalized Medication: Homeopathic remedies are prescribed according to the specific symptoms, past medical history, and constitution of the patient. The remedies offering treatment for kidney failure are particularly targeted at the root causes that created the kidney problem.
Holistic Medicine: It encompasses the physical, emotional, and lifestyle aspects and aspires toward maintaining balance and stimulating the body's inherent healing powers.
Consultation and Follow-up: It is very important that regular consultations take place to monitor progress, if any, and in this regard, the treatment could be readjusted. The practitioners work alongside the patients to make sure that homeopathic treatment is given parallel to other medical interventions.
Conclusion
High creatinine levels are one of the serious signs that indicate problems with the kidneys, either chronic kidney disease or acute kidney injury. The effective management would include conventional treatment for kidney failure and modifications in lifestyle, along with alternative therapies in some cases. Support through natural and homeopathic treatments offered at Bharat Homeopathy in Gurgaon might help and benefit overall kidney health in the long run.
Any therapy, however, is best undertaken under the professional supervision and guidance of health professionals. Integrating traditional and alternative approaches can offer a wide strategy in managing kidney health in view of improving general well-being.
0 notes
Text
ayurvedic treatment for kidney failure

Ayurvedic Kidney Stone Treatment
ayurvedic medicine for kidney creatinine
.
The kidneys have important tasks to perform in the human system. These are (i) regulation of the volume of the body fluids, (ii) elimination of inorganic ions both cations (e.g. Na+, K+) or anions (e.g. Cl’, phosphate, SO4) from the body, (iii) maintenance of appropriate plasma concentration of non-electrolytes such as glucose and urea, (iv) maintaining electrolyte balance by H+ and OH- ions and thus adidity or alkalinity of the blood, (v) elimination of waste products especially the nitrogen and sulphur containing substances as well as the toxic substances (e.g. drugs) which have entered the body, and (vi) retention of substances vital to body economy. These also have some more functions.
ayurvedic treatment for skin diseases
.
Major diseases or Kidney disorders are Anuria or oliguria (complete to cessation or less formation of urine), polyuria (frequent passage of small quantities of urine), abnormal constituents in urine (e.g. blood, pus etc.), Nephritis, pyelitis (inflamanation of the parenchyma & pelvis of the Kidney) uraemia (i.e. renal failure causing retention of abnormal amounts of urea in the blood), renal colic due to calculus or such other condition, Dysuria (painfull passage of urine).
Causes of kidney damage:
Basically human health miseries could be attributed to –
Abnormalities in anatomical and physiological level
Interaction or stress of biotic factors (various in fections)
Abiotic stress which includes Ahar, Vihar and Achar
Mental imbalance due to predominence of tamsik and rajsik bhavas rather than Sattvik
easy entry of microvita owing to suitability of mental and physical bodies
panchkarma in ahmedabad
.
Besides above a new dimension is added by adverse side effects of modern allopathic medicines. Most probably this is due to administering active ingredients in pure form. This certainly provides quick action but at the same time damages the system in other ways. The crude medication system of Ayurveda allows the human system to assimilate the active ingredient as well as some related compounds in a natural way and thus avoids any such bad effects on the system. One of the potent causes of increasing incidences of kidney disorders, today, is the side effects of modern medicines or wrong medication or over dosages in certain cases.
best ayurvedic doctor for psoriasis
.
Contact Us
Address: A 222, Shakti ETC ( Extol Trade Centre, Vandematram Circle, NR Vandematram Cross Rd, Gota, Ahmedabad, Gujarat 382481, India
Call: +91 99045 57565
Email: [email protected]
Website: https://advaitayutreatment.com/
0 notes
Text
Signs Of Organ Rejection Kidney
Learn about signs of organ rejection kidney
What kidney transplant rejection is and its types.
Symptoms, diagnosis, treatment, prevention, and complications of kidney transplant rejection.
What is kidney transplant rejection?
Kidney transplant rejection is a condition. The body’s immune system attacks a transplanted kidney and rejects it. It sees the kidney as foreign. This rejection can occur even if the donor kidney is a good match for the recipient. https://medlifeguide.com/signs-of-organ-rejection-kidney/
What are the types of kidney transplant rejection?
1. Hyperacute Rejection Symptoms
High fever
Oliguria (low urine output)
2. Acute Rejection Symptoms
The blood’s creatinine level has r…….Read More
Are you interested to read all about kidney disease and overall health Read More
#kidney disease#kidney stone specialist#kidney diet#kidney transplant#kidneyhealth#kidneys miserable taste#medicine#healthcare#health & fitness#healing#health and wellness#healthylifestyle#maturity
0 notes
Video
youtube
COMMUNICATION SKILLS STATION OF CALL TO CONSULTANT FOR OLIGURIA
COMMUNICATION SKILLS STATION OF CALL TO CONSULTANT FOR OLIGURIA MRCS B OSCE - MOCK EXAM Bli medlem i kanalen för att få åtkomst till flera förmåner: https://www.youtube.com/channel/UCkkvon_blxinTHc7DGuYkpQ/join
#youtube#communication communicationskills callconsultant oliguria medicine doctor surgery health medical healthcare mrcs mrcsbosce femalesurgeon you
0 notes
Text
*Aprendiendo sobre el Uso Terapéutico del Agua de Mar y plasma marino .
*_¿Cuáles son las vías de aplicación del agua de mar?_*
En diferentes fuentes bibliográficas se han descrito las siguientes:
👉🏼 *Oral:* como laxante y equilibrador osmótico, alcalina el medio interno, sana y fortalece los tejidos, desinfecta, es diurética, restaura la circulación... Ejemplos: Estreñimiento, Diarrea, Anorexia, Gastritis, Úlcera péptica, Reflujo, Hepatitis, Cirrosis, Embarazo y Lactancia, Hipertensión Arterial, Cardiopatías, Oliguria, Cálculos Renales, Artritis, Fibromialgia, Osteoporosis, Diabetes, Obesidad, Tiroides, Bocio, Dislipidemia, Hipercolesterolemia, Anemia, Fatiga, convalecencia postquirúrgica... El agua de mar se puede tomar HIPERTÓNICA (ó PURA) hasta medio litro diario ó ISOTÓNICA (ó DILUIDA) mezclada con agua corriente o jugos naturales (diluida 3 partes de esto en 1 parte de agua de mar), máximo 2 litros por día. Puede consultar cada caso en particular...
👉🏼 *Nasal:* para descongestionar: ejemplo en Sinusitis y Rinitis Alérgica... Poner agua de mar pura en la palma de la mano, tapar una fosa nasal y respirar de su palma el agua por la otra, alternando ambas fosas hasta que sienta el sabor del agua de mar en su garganta. De 3-5 veces al día hasta que mejore.
👉🏼 *Nebulizada:* para drenaje de secreciones, antibiótica y desinfectante: ejemplo en EPOC, Neumonía, Asma y Bronquitis Crónica: llenar el vasito del nebulizador con agua de mar hipertónica, colocarse la mascarilla y poner el Nebulizador en funcionamiento. En casos agudos, repetirlo 3 veces al día.
👉🏼 *Gotas óticas (en oídos):* como antibiótica y desinfectante, ejemplo en Alergias y Otitis externas. Aplicar 1 ó 2 gotas de agua de mar hipertónica de 3 a 6 veces al día.
👉🏼 *Gotas oculares (en ojos):* como colirio descongestionante y antiséptico. Ejemplo en Conjuntivitis, Glaucoma, Miopía, Astigmatismo y Cataratas. Aplicar 1 ó 2 gotas de agua de mar hipertónica de 3 a 6 veces al día, dependiendo de la afección.
👉🏼 *Gárgaras:* como antiinflamatorio, antiséptico y para la nutrición del tejido. Ejemplo en Faringitis, Amigdalitis, Laringitis... Tomar un sorbo de agua de mar hipertónica y retenerlo en la boca. Tragar una porción mínima para impregnar el órgano por dentro y esperar 2 ó 3 minutos para repetir el trago y continuar hasta agotar el sorbo. También se pueden hacer gárgaras y luego se traga el agua. Repetir 5 a 6 veces al día por lo menos por 15 días.
👉🏼 *Enjuagues Bucales:* como desinfectante, antiséptico, cicatrizante y nutriente. Ejemplos: Higiene Bucal, Gingivitis, Periodontitis, Caries dentales, Aftas bucales, Halitosis (mal aliento)... Después de cepillarse los dientes, tomar un sorbo de agua de mar hipertónica y mantenerla en la boca 2 ó 3 minutos moviéndola de un lado a otro. Expulsar o tragar el agua. Si hay infecciones o sangrados debe permitir más impregnación de la zona con el agua que sume por lo menos 1 hora al día. Hacerlo de 8 a 15 días.
👉🏼 *Aplicación tópica (en la piel):* como Emoliente no agresivo, antibiótico, fungicida, antiinflamatorio, regenerador, estimula el metabolismo dérmico y el fortalecimiento de la piel. Ejemplos: en Psoriasis (mojar un paño con agua de mar hipertónica calentada a 40°C y aplicarlo en la zona afectada, repitiendo cada vez que se enfríe el paño por 20 minutos; de 1 a 3 veces al día), en Acné, Dermatitis y Eczema (aplicar con un algodón agua de mar hipertónica calentada a 40°C en cada forúnculo o zona afectada), Micosis cutánea (pediluvios o baños de pies con agua de mar hipertónica, caliente), Alopecia y Caspa (después del baño masajear el cuero cabelludo con agua de mar hipertónica por unos minutos, dejar secar sola y peinar), Quemaduras, Úlceras, Urticaria y Alergias (aplicar agua de mar hipertónica con un spray y dejar secar al aire por lo menos 5 veces al día. Por la noche vendar la zona con una gasa empapada en agua de mar hipertónica)
Más información al respecto al 941 714 495
👉 Comparte
0 notes
Text

𝐀𝐛𝐬𝐭𝐫𝐚𝐜𝐭: The #authors et al., for this study has discovered obstructive oliguria and AKI due to #atypical #bloodclots during thoracoabdominal aortic #aneurysm #surgery, and therefore is reporting this #results.
View more here @ https://symbiosisonlinepublishing.com/anesthesiology-painmanagement/anesthesiology-painmanagement53.php
#symbiosisonlinepublishing #Anesthesiologist #anesthesiology #anesthesialife #Anesthetist #anestesia #painmanagement #painmanagementsolutions #painmanagementclinic #surgery #surgeryrecovery #research #ResearchStudy #researchers #journalwithme #journals #journal #openaccess #pubmed #peerreview #peerreviewed
0 notes
Text
Combined cervical laceration and bladder rupture: a case report of an unusual complication of precipitated labor by Dr Fatemeh Darsareh in International Journal of Clinical Images and Medical Reviews

Abstract
Cases of bladder rupture have been rarely reported following vaginal childbirth. To the best of our knowledge, however, no cases of combined cervical laceration and bladder rupture have been reported to date. We present the first case of a 31-year-old woman with gestational diabetes who suffered a combined cervical laceration and bladder rupture after childbirth. Precipitated labor caused by oxytocin induction resulted in vaginal and cervical lacerations. The bladder rupture was confirmed by cystography. A team of obstetricians and urologists performed the laparotomy. The patient was kept under observation for two weeks before being discharged with no serious complications.
Keywords: Bladder rupture; Cervical lacerations; Precipitated labor; Childbirth trauma; Case report.
Introduction
Spontaneous bladder rupture following normal vaginal delivery is a surgical postpartum emergency. Previous cesarean section, vacuum/forceps-assisted vaginal deliveries, and distended bladder compressed by engaged head in birth canal are all risk factors for bladder injuries in healthy parturient women 1. Cases of bladder rupture, accompanied by uterine rupture, have been rarely reported following vaginal birth after cesarean section 2. To the best of our knowledge, however, no cases of combined cervical laceration and bladder rupture have been reported to date. We present the first case of spontaneous bladder rupture with cervical laceration after a precipitated vaginal delivery.
Case Presentation
A 31-year-old, G2P1L0D1, woman with gestational diabetes, was admitted to our maternity ward at 38 weeks of pregnancy for elective induction of labor to terminate her pregnancy. She had a history of preterm birth and was a known case of minor thalassemia. The induction of labor began at 5:00 a.m. with oxytocin, and contractions began approximately two hours later. Table 1 depicts the progress of labor. During her labor, the patient urinated once. Finally, at 10:40 a.m., she gave birth to a baby boy weighing 3700 grams with an Apgar score of 7/9. Excessive vaginal bleeding was observed following placental expulsion. The examination revealed an extensive laceration in the vagina and cervix that was repaired by the obstetrician and midwife. The patient was catheterized and was being closely monitored. A urologist was consulted due to the oliguria and hematuria (100 cc output with gross hematuria within 5 hours of childbirth). Cystography, as recommended by the urologist, revealed the bladder rupture. The patient was prepared for a laparotomy immediately. The laparotomy was performed by a team of obstetricians and urologists. Several hematomas were discovered in the uterine body and the broad ligament that the team decided not to manipulate because it did not grow during the surgery. A bladder rupture was found at the dome of bladder that was repaired in two layers. One pack cell unit and two FFP units were transfused. A peritoneal drain was placed posterior to the bladder and the skin incision was closed in layers. The patient was observed for two weeks. The result of the ultrasound revealed the shrinking of the hematoma. The blood and renal tests were normal. The catheter was removed after 2 weeks and the patient was discharged.
Table 1: The progress of labor
Discussion
Precipitate labor is defined as the expulsion of the fetus within three hours of the start of contractions. Few studies have found that precipitated labor is harmful to both the mother and the newborn. Precipitated labor, which is most commonly associated with placental abruption and induction of labor, is a significant risk factor for maternal complications 3. Maternal morbidities reported included extensive birth canal lacerations, uterine rupture, placenta retention, the need for revision of uterine cavity, post-partum hemorrhage, and blood transfusions 3,4. The lower urinary tract's anatomic proximity to the reproductive tract predisposes it to iatrogenic injury during obstetric procedures. The bladder and lower ureter are two of the most commonly involved organs. Because the dome of the bladder is the weakest area, most bladder ruptures occur through the peritoneal cavity 5. In our case, in addition to deep vaginal tears and extensive cervical laceration, bladder rupture occurred, but the diagnosis was delayed by a few hours. Given the nonspecific clinical features of bladder rupture, the diagnosis should be approached with caution. Oliguria and gross hematuria after a traumatic childbirth increase the likelihood of bladder rupture. In such cases, a cystogram is thought to be the best method for early detection.
In our case the patient had induced labour with oxytocin. The use of oxytocin to induce labour can result in tachy-systole and thus shorter deliveries. So in our case we believe that the power of uterine contractions and quick descent of passenger (3700 grams fetus) were the main risk factors of precipitated labour and the complications accompanied with it. A distended bladder during labor, particularly in our case, where the fetus descended quickly, could also be a factor in bladder rupture. Although the patient urinated normally during labor, it was critical to ensure that the bladder was empty, especially during the active phase of labor, to avoid bladder damage.
CONCLUSIONS
Bladder and cervical rupture should be considered, after precipitated vaginal delivery. When there is gross hematuria, a urinary catheter should be inserted to monitor the hematuria and urine output. If the hematuria persists and other associated symptoms appear, cystography is a useful tool for determining the severity of the bladder injury and determining the cause.
Funding
This study received no specific funding from public, commercial, or not-for-profit funding agencies.
Conflict of Interest
Authors had no conflicts of interest to declare.
Patient consent
Obtained.
For more details: https://ijcimr.org/editorial-board/
#Bladder rupture#Cervical lacerations#Precipitated labor#Childbirth trauma#Case report#postpartum#oxytocin#vacuum#laparotomy#Cystography#hemorrhage#Dr Fatemeh Darsareh#ijcimr
0 notes