#premenopausal symptoms
Text
How CBD Can Help with Sleep Disruption During Menopause and Perimenopause | @UnderstandingCBD
Hello everyone, Welcome back to our channel! Today, we have Linda, Chief of Myth Busting who will share her thoughts on Menopause and Perimenopause. So, let's start! Menopause and perimenopause bring about hormonal changes that can bring disturbance to sleep patterns. During these stages of life, many women experience various symptoms, including disturbed sleep due to hormonal changes, hot flashes, and more. Make sure to watch the video until the end, so you don't miss out on this important discussion about the potential benefits of CBD in managing anxiety during menopause and perimenopause.
Don't forget to like this video and subscribe to my channel to know more about the latest informative content on cannabinoids and CBD.
0 notes
Text
#premenopause#perimenopause#menopause treatment mckinney#menopause management#menopause symptoms#menopause
0 notes
Text
On Power, and on Powering Through, and Why They’re Really Not the Same
I don’t pay much attention to personal attacks in reviews. It comes as the flipside of success; an attempt by the critic to puncture what they see as too much success. But I still remember one review, just after the film of Chocolat, when two of my novels happened to be in the Top 5 at the same time, in which a (male) newspaper critic referred to me dismissively as a premenopausal woman writer. I was a little taken aback. Clearly, it was meant to disparage, but I was only 35, ten years away from the perimenopause. What exactly did he mean? It wasn’t a comment about the book (which I doubt he had even read). The obvious misogyny aside, it seemed to express resentment, not of my books, but of me, myself, my right to take up space in his world. That word – premenopausal – was at the same time a comment on my age, my looks, my value, and a strong suggestion that someone like me shouldn’t be this successful, shouldn’t be writing bestsellers, shouldn’t be so – visible.
I don’t recall the name of the man, or the paper for which he was writing. He was far from being the only journalist who felt I didn’t deserve success. I shrugged off the unpleasant comment, but he’d meant it to hurt, and it did. I still wonder why he – and his editor - thought that was appropriate. I also wonder why, 20 years on, women are still dealing with this kind of thing. It’s still not enough for a woman to be successful in her chosen field. Whatever her achievements, you can be pretty sure that at some point, some man in his 50s or 60s – maybe an Oxbridge graduate, author of an unpublished novel or two - will offer his opinion on her desirability, either in the national Press, or most likely nowadays, by means of social media. The subtext is clear: women who don’t conform to societal values of what a woman should be are asking for this kind of treatment; especially those who dare to achieve more than their detractors.
10 years after that nasty review, I finally began the journey into perimenopause. No-one told me it was happening. No-one in the media was talking about it at the time. Even my doctor never thought to mention that my symptoms – the insomnia, headaches, mood swings, anxiety, depression, sleep paralysis, hair loss, brown patches on my skin – might have a single origin. I began to feel I was losing my mind: as if I were starting to disappear. I started to doubt my own senses. I blamed it all on the stress from my job. My mother had powered through menopause – or so she led me to believe – and made no secret of her contempt for modern women who complained, or treated the symptoms as anything more than a minor inconvenience.
And so I did the same. I powered through; and when at last I began to experience the classic symptoms of menopause - irregular bleeding, hot flushes, exhaustion, night sweats so bad that I would awake in sheets that were wringing wet – it did not occur to me to seek help. After over a year of this, I finally went to my doctor, who took a few tests, cheerfully announced I was menopausal, and when I inquired after HRT, advised me to power through – that phrase again - and let Mother Nature take her course. The internet was slightly more helpful. I took up running, lost weight, cut down on alcohol, downed supplements and sleeping pills and vitamin D, and felt a little better. Then, breast cancer came to call, and by the time my treatment was done, the symptoms had more or less disappeared, or at least had been superseded by the symptoms of chemo. I congratulated myself at having powered through cancer as well as surviving menopause.
But two years later, I feel old. I look that way, too. I’ve aged ten years. Some of that’s the cancer, of course. I was quite open about my treatment when I was powering through it – partly in order to pre-empt any questions about my hair loss or any of the all-too visible effects of three courses of chemo. Not that it stopped the comments, though. Even at my lowest ebb, a sector of social media made it clear that my only concern should be to look young and feminine to anonymous men on Twitter.
Right now, I don’t feel either. My hair has gone grey and very thin. My skin, too, seems thinner; both physically and mentally. At a recent publishing event, several acquaintances failed to recognize me; others just looked through me as if I had become invisible. Invisibility would be a relief; I find myself dressing for camouflage. I tend to wear baggy black outfits. I got my OBE last week. Photographs in the Press show me talking to Prince William. I’m wearing a boxy black trouser suit, flat shoes and a red fedora. I think I look nice. Not glamorous, but comfortable; quirky; unpretentious.
On a thread of largely supportive messages, one Twitter user pops up to say: Jesus, who’d accept an honour looking like that middle-aged disaster? @Joannechocolat thought she’d make an impact? She needs a stylist. If you look in the dictionary for the definition of “dowdy”, it features this photo.
It’s not the same man who belittled me over 20 years ago. But the sentiment hasn’t changed. Regardless of your achievements, as a woman, you’ll always be judged on your age and fuckability. I ought to be used to this by now. But somehow, that comment got to me. Going through menopause isn’t just a series of physical symptoms. It’s how other people make you feel; old, unattractive, and strangely ashamed.
I think of the Glass Delusion, a mental disorder common between the 14th and 17th centuries, characterized by the belief that the sufferer was made of glass. King Charles VI of France famously suffered from this delusion, and so did Princess Alexandra Amélie, daughter of Ludwig 1st of Bavaria. The condition affected mostly high-profile individuals; writers, royals, intellectuals. The physician to Philip II of Spain writes of an unnamed royal who believed he was a glass vase, which made him terribly fragile, and able to disappear at will. It seems to have been a reaction to feelings of social anxiety, fear of change and the unknown, a feeling both of vulnerability and invisibility.
I can relate. Since the menopause, I’ve felt increasingly broken. I don’t believe I’m a glass vase, and yet I know what it feels like to want to be wrapped in a protective duvet all day. I’ve started buying cushions. I feel both transparent, and under the lens, as if the light might consume me. On social media, I’ve learnt to block the people who make mean comments. To make myself invisible. To hide myself in plain sight. I power through, but sometimes I think: why do women power through? And who told them that powering through meant suffering in silence?
Fortunately, some things have changed since I went through the menopause. Over the past few years, we’ve seen more people talking about their experiences. Menopause is likely to affect half the population. We should be talking about it. If men experienced half these symptoms, you bet they’d be discussing it. Because power isn’t silence. You’d think that, as writer, I would have worked that out sooner. Words are power. Sharing is strength. Communication breaks down barriers. And sometimes, power means speaking up for those less able to speak for themselves.
I look at myself in the mirror. I see my mother’s mouth; my father’s eyes. I see the woman I used to be; the woman I will one day become. I see the woman my husband loves, a woman he still finds attractive. A woman with a grown-up child who makes her proud every single day. A menopausal woman. A cancer survivor. A woman who writes books that make other people sit up and think. A woman who doesn’t need the approval of some man she’s never met to be happy. She can be happy now. I can. And finally, I understand. Powering through isn’t about learning to be invisible. It isn’t about acceptance, or shame, or letting Nature take its course, or lying about feeling broken. It’s looking beyond your reflection. It’s seeing yourself, not through the lens of other people’s expectations, but as yourself. The sum of everything you’ve been; of everyone who loves you. Of claiming your right to be more than glass, or your reflection in it. The right to be valued. The right to shine, regardless of age or reproductive status. Men seldom question their own right to these things. But women have to fight for them. That’s why it’s so exhausting.
This morning, instead of putting on my usual baggy black sweatshirt, I chose a bright yellow pullover. I looked at myself in the mirror. It’s not a great colour on me now, but it feels like dressing in sunshine. My husband came into the bathroom. You look –
My husband rarely gives compliments. I can’t remember the last time he commented on how I was dressed. I wondered what he was going to say. Dowdy, perhaps? Inappropriate? Like a menopausal woman in dire need of a stylist?
At last, he said: When you smile like that, you look like a friendly assassin.
A friendly assassin. I’ll take that.
Shining like the sun. That’s me.
2K notes
·
View notes
Note
Is it possible for lc disability after a covid infection 4 months ago to cause your period to never show again? It has been over 60 days since my last and I ain't pregnant cause I don't even fuck anyone w a penis /g
Yup, it sure is. Here's four articles/studies on it!! A bit of a warning for heavily gendered language :\
#asks#long covid#disability#disabled#chronic illness#chronically ill#invisible disability#actually disabled#disability awareness#covid 19#covid#menstrual health#menstruation
8 notes
·
View notes
Text
The Menopause Breakthrough Women Over 40 Have Been Waiting For..
MenoPhix is an all-natural and effective menopause breakthrough for women over 40 who have been waiting for it.
It helps you naturally soothe symptoms of menopause with the combination of six incredible all-natural ingredients. The added ingredients in this formula are purely sourced from nature’s extract, which won’t cause any side effects.

MenoPhix: Natural Formula Supports Manopause
What is MenoPhix?
Menophix is a dietary supplement available without a prescription. It is a supplement intended for women who are going through menopause or who may be premenopausal. Menophix addresses the key factor that causes menopause symptoms: hormone imbalances.
Menophix is designed by doctors to tackle a key factor that worsens menopausal symptoms: high cortisol levels.
It works by regulating cortisol, promoting a balance in estrogen and progesterone. The goal is to lessen symptoms like mood swings, hot flashes, low libido, digestive problems, insomnia, and more.
Real MenoPhix Users Click Here:
How Does MenoPhix Work?
MenoPhix operates through a unique blend of six natural ingredients meticulously crafted to tackle the multifaceted symptoms of menopause. By integrating just one capsule of MenoPhix into your daily routine, these natural compounds collaborate to address menopausal challenges through diverse mechanisms.
Primarily, specific ingredients within MenoPhix work to naturally enhance estrogen levels in the body, thereby fostering the hormonal equilibrium crucial for mitigating menopausal discomforts. By providing essential nutrients essential for hormone synthesis, MenoPhix facilitates the production of vital female sex hormones like estrogen, aiding in symptom relief.
The Science Behind The Ingredients
1. Ashwagandha
2. Mucuna Pruriens
3. Sarsaparilla
4. Horny Goat Weed
5. Zingiber
#Menophix#Menophix supplement#MenoPhix Manopause#Manopause#Menophix dietary supplement#health & fitness#menopause symptoms#Solution for Menopause Relief
2 notes
·
View notes
Photo
At my age, I know a lot of women that are either suffering from bad periods every month or menopausal symptoms. I’ve used OVA-M for a month and a half and I’m finally starting to feel myself and those premenopausal symptoms are under control. I had no idea how bad those symptoms would get. Women don’t talk about this enough. I found through this journey that it is important to share so we know what to expect. I also never had really bad periods until I started perimenopause but after talking to a lot of my girlfriends, I found that many women suffer from tons of different types of period issues every month. Some are debilitating. I have a couple of friends who have been taking OVA for bad periods and are having an easier period. It is so important for me to feel myself and before taking these healthy, nontoxic supplements, I felt like someone had taken over my body. Mood swings, fatigue, joint pain, horrible periods, and just not recognizing myself. All those symptoms were to the extreme. Take control of the things that seem so uncontrollable. Leave a ❤️ below if you want to take control. #ova #ovam #perimenopausehealth #perimenopause #period #endometriosis #fibroids #menstruation #health #healthandwellness #nontoxic #nohormones #supplements #menopausesupplements #booksta #itlnbrt #love #family #modere (at Fullerton, California) https://www.instagram.com/p/CprIHFaL0V-/?igshid=NGJjMDIxMWI=
#ova#ovam#perimenopausehealth#perimenopause#period#endometriosis#fibroids#menstruation#health#healthandwellness#nontoxic#nohormones#supplements#menopausesupplements#booksta#itlnbrt#love#family#modere
8 notes
·
View notes
Text
How common are ovarian cysts and their symptoms?

Ovarian cysts are common. Most women are unaware that they have a cyst since they generally produce no symptoms and disappear on their own. One in every ten women will need ovarian cyst surgery at some time in their life.
Most ovarian cysts in premenopausal women are asymptomatic and go away without the woman even noticing it. The most frequent symptom of a cyst is discomfort in the lower abdomen or pelvis. Other is
Period pains or a shift in your menstrual cycle
Pain in your intestines/pressure on your bowels,
Intercourse discomfort (dyspareunia)
Urination has become more frequent and urgent.
A change in appetite, a sensation of fullness, or bloating
An abdomen that is distended or bulging
Endometriosis may cause difficulty conceiving (getting pregnant).
If you are looking for treatment, Consult Dr. Arohi Tasgaonkar one of the best Gynecologist in Thane.
5 notes
·
View notes
Text
Does Occipital Neuralgia Improve with Lifestyle Adjustments?
Occipital neuralgia is a condition that causes sharp pain in the head's rear side, affecting the area near the eyes and scalp. This discomfort significantly impacts daily life, making tasks difficult. Many patients use medications or injectable treatments to alleviate symptoms. However, it is unclear if lifestyle adjustments can alleviate occipital neuralgia. Explore effective treatments for premenopausal hormone issues. Do Lifestyle Adjustments Improve Occipital Neuralgia? Explore the full article!
0 notes
Text
Best Solutions for Premenopausal Hormonal Issues
Menopause, the phase before menstruation pauses, is a natural physiological process that affects mental and physical well-being, leading to changes in periods and loss of interest in sex. Hormone treatment may be used for perimenopause symptoms, but self-care activities and high-quality supplements and hormonal medications can also be beneficial. Explore the best solutions for premenopausal hormonal issues. Our comprehensive guide offers expert advice to help you navigate this transitional phase with confidence.
0 notes
Link
0 notes
Text
It would probably be a good idea to take some biofilm dissolvers (Kirkman or Interphase) before doing the test, so you can "break out" as much bacteria as possible so it will show up on the test. It is possible to have a negative result if your bacteria are still embedded in a biofilm.
_____________________________
My understanding is that cirrus actually test your urine against antibiotics. Microgen look for DNA which should tell what you are resistant to. Pathnostics go one step further and rate antibiotics on what should work best. Use them only as a guide, I’ve had both say R and actually I’m S.
I like cirrus bc they test with abx. Microgen goes by the Sanford guide mostly with picking up some resistance - But due to individual resistance I have found it to only e helpful in terms of identifying bugs but not necessarily treating. Plus my insurance covers cirrus abd I love their support.
—————
Dr Ryan heer - Ruth kritz testing. Recommended on uti website for curing via biofilm disruptors.
_________
The study, by researchers at Washington University School of Medicine in St. Louis and the Broad Institute of MIT and Harvard, showed that a round of antibiotics eliminates disease-causing bacteria from the bladder but not from the intestines. Surviving bacteria in the gut can multiply and spread to the bladder again, causing another UTI.
At the same time, repeated cycles of antibiotics wreak havoc on the community of helpful bacteria that normally live in the intestines, the so-called gut microbiome.
Notably, the microbiomes of women with recurrent UTIs were particularly scarce in bacteria that produce butyrate, a short-chain fatty acid with anti-inflammatory effects.
__________
Can be prescribed pyridium for pain
__________________
My understanding is that cirrus actually test your urine against antibiotics. Microgen look for DNA which should tell what you are resistant to. Pathnostics go one step further and rate antibiotics on what should work best. Use them only as a guide, I’ve had both say R and actually I’m S.
_______
Urinary tract infections (UTIs) typically begin to show symptoms within 2-3 days after the initial bacteria enters the urinary tract. However, the exact timeline can vary:
* Symptoms like a burning sensation during urination, increased urination frequency, and pelvic discomfort often manifest within 1-2 days after the infection starts.
* More severe symptoms like pain, fever, back/abdominal pain, and bloody or cloudy urine may take 2-3 days to develop, as the infection progresses.
* Some individuals may be asymptomatic initially, with the infection only causing noticeable symptoms after a few days.
Frequent or recent sexual activity is the most important risk factor for UTIs in young women. Nearly 80% of all UTIs in premenopausal women occur within 24 hours of intercourse or up to 2 days
_____________________
a frequent and strong urge to urinate even after you empty your bladder, which is called frequency and urgency. a painful or burning sensation when urinating, which is called dysuria.
_____________________
Acute cystitis is an infection of your bladder. “Acute” means that the infection develops suddenly and rises sharply
_____________________
Tumeric:
Curcumin can significantly improve the symptoms of chronic urinary tract infections, protect renal tubular function, and also decline inflammatory responses by influencing the expressions of TLR2 mRNA and TLR4 mRNA so as to exert its curative effect on chronic urinary tract infections
____________
believe Methylene Blue (MB) is safe (and as effective from what I’ve read). And it works for me. I’m not comfortable considering taking Methenamine (Hiprex) because it turns to formaldehyde in the body. Methylene Blue can be gotten on line without an Rx, something I am very grateful for. My urologist dismissed MB when I brought up the idea of taking it to her. She shrugged her shoulders and said “nah, it’s just like pyridium.” Well that simply isn’t true so she lost credibility with me. MB is a treatment that docs apparently don’t want to offer up. Hmm. I wonder why? It’s not because it’s not effective and not safe.
______________________________
https://pharmaceutical-journal.com/article/feature/stuck-in-the-1950s-why-uti-diagnosis-badly-needs-an-update?fbclid=IwZXh0bgNhZW0CMTEAAR1GFwL9LGBBrcSMu3DdXzlj4rQTp3mvj8P2zOGVwCFmpcUh9rJgdQKGEqs_aem_ZUCzdoo6Qa4C7ujVHqWfSQ
Urine culture testing is based on work carried out in 1957 by the scientist Edward Kass, who gathered urine samples from a small group of pregnant women who had pyelonephritis, meaning his work was not representative of patients with acute cystitis.
The subsequent microbiological threshold that was developed based on Kass’ work, and that is still used to diagnose UTIs, looks for the presence of at least 100,000 colony-forming units of bacteria per millilitre of urine (CFU/ml) of a single species of a known pathogen to confirm an infection[4].
Further work in patients with classic symptoms of acute cystitis has demonstrated that a 100,000 CFU/ml threshold missed nearly 50% of genuine infections[5],[6]. In such patients, a threshold of 100 CFU/ml of a known urinary pathogen was proposed as more appropriate.
If your testing is inaccurate then you’ll unintentionally misdiagnose. It’s no surprise that if someone presents with symptoms that sound like a UTI on several occasions, but each time the urine result is negative, they get led down the IC path.”
___________
You will find reading professor Malone-Lee's book very informative. The sex isn't necessarily giving you the uti. If you have embedded infection and sex aggravates my shaking loose the infection therefore causing a rise in your symptoms, that is normally interrupted incorrectly as a new infection. Some may be, but not likely if you consistently get uti symptoms. It's more likely you have Chronic UTI (embedded) and the activity is stirring up and releasing the infection into your urine causing the symptoms. In a few cases sex can be the issue if your partner is carrying infection, obviously tests need to be done to prove this.
———-
Oil of oregano - Any brand is good if it has carvacrol level of 60% or greater.
____________
* Keep the urine's pH at or slightly below 7 during the course of your D-Mannose regimen. Bacteria thrive in an acidic environment doubling in numbers every 20 - 40 minutes. Conversely, bacterial growth is inhibited in a more alkaline environment.
_______________
https://liveutifree.com/uro-vaxom/amp/
Research team at Duke - Dr. Soman Abraham - creating a new treatment:
The immune system’s response is to shed the bladder lining entirely, taking bacteria with it. However, there is a problem with this. The underlying tissue is now exposed to urine and the ammonia, salts, etc, therein, which can cause a great deal of pain.
Continuing on heroically, the immune system then sends in two types of T-cells to kill off any remaining bacteria (TH1 T-cells) and repair the bladder lining (TH2 T-cells). But in order to save the body from further pain, the repair bit tends to occur faster than the bacteria-killing bit. This can mean that some residual bacteria are left to hide, safe and snug, within the urinary tissues. Multiplying within these tissues, the result is often recurrent UTIs.
0 notes
Text
How to Relieve Vaginal Dryness Naturally: 10 Remedies
Vaginal dryness is common, especially during menopause, due to reduced estrogen levels. Symptoms include discomfort and pain during intercourse. Natural remedies like proper hydration, phytoestrogens, natural oils, herbal treatments, and probiotics can help. Rosebud Woman's products, such as Honor Everyday Balm and Arouse Stimulating Serum, offer targeted relief. Regular exercise, stress management, and using natural personal care products can also support vaginal health.
0 notes
Text
#health center#mckinney#mckinney texas#Premenopause#Perimenopause#fatigue#menopause#menopause symptoms#menopause relief#menopause specialist nyc#menopause management#menopause treatment mckinney
0 notes
Text
Challenges and Solutions in Neonatal and Paediatric Bronchoscopy
Challenges and Solutions in Neonatal and Paediatric Bronchoscopy
Welcome to our blog where we delve into the intriguing topic of normal endometrial thickness. Whether you’re a curious individual seeking knowledge or someone navigating medical terms, we’ve got you covered. Let’s explore what normal endometrial thickness entails and why it matters.
What is Endometrial Thickness?
The endometrium is the lining of the uterus that thickens and sheds during the menstrual cycle in response to hormones like estrogen and progesterone. This thickness is crucial for various reproductive processes, including menstruation, embryo implantation, and pregnancy maintenance.
Normal Range Across Menstrual Cycle Phases
Postmenopausal Women: After menopause, hormonal levels decline, leading to a thinner endometrium. Typically, it measures ≤ 4 mm.
Premenopausal Women: Throughout the menstrual cycle, the endometrial thickness fluctuates:
Early Proliferative Phase: 2–4 mm
Late Proliferative Phase: 5–7 mm
Secretory Phase: 7–14 mm
Mid-Cycle (around ovulation): 8–15 mm
Pregnancy: During pregnancy, the endometrium thickens significantly to support embryo implantation and development. It can reach 15–20 mm or more under the influence of pregnancy hormones.
Factors Influencing Endometrial Thickness
Several factors can affect endometrial thickness:
Hormonal Imbalance: Conditions like polycystic ovary syndrome (PCOS) or thyroid disorders can disrupt hormonal levels and impact endometrial thickness.
Medications: Certain medications, such as hormone therapy or fertility drugs, can alter endometrial thickness.
Medical Conditions: Conditions like endometrial hyperplasia or endometrial cancer can lead to abnormal thickening of the endometrium.
Clinical Assessment
Endometrial thickness is typically assessed via transvaginal ultrasound. This non-invasive procedure allows healthcare providers to measure the thickness accurately and detect any abnormalities that may warrant further investigation.
When to Seek Medical Advice
While normal endometrial thickness varies, significant deviations from the expected range may indicate underlying issues. It’s essential to consult a healthcare provider if you experience abnormal menstrual bleeding, infertility concerns, or other symptoms suggestive of a hormonal imbalance or reproductive health issue.
0 notes
Text
From Fibroids to Ovarian Cysts: A Guide to Benign Gynecological Tumors
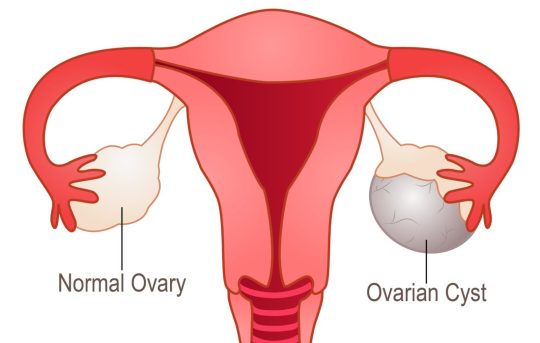
As women, we are no strangers to dealing with various health issues, including those related to our reproductive system. One common problem that many women face is benign gynecological tumors, such as fibroids and ovarian cysts. These conditions can cause discomfort and even impact fertility, making it important to understand and seek proper treatment. As a gynecologist in Indore, I have encountered many patients with these tumors and understand the need for awareness and education around them.
Firstly, let's understand what exactly are fibroids and ovarian cysts. Fibroids are non-cancerous growths that develop in the uterus, while ovarian cysts are fluid-filled sacs that form on the ovaries. Both of these conditions are quite common, with fibroids affecting about 20-80% of women and ovarian cysts being found in almost all premenopausal women at some point in their lives.
The symptoms of fibroids and ovarian cysts can vary from person to person. Fibroids can cause heavy and prolonged menstrual bleeding, pelvic pain, and pressure on the bladder or rectum. On the other hand, ovarian cysts can cause pain in the lower abdomen, bloating, and changes in menstrual cycles. In some cases, these tumors may not cause any symptoms and are only discovered during routine gynecological exams.
Also Read: Best Gynaecologist in Indore
While the exact cause of these tumors is still unknown, certain factors can increase the risk of developing them. These include hormonal imbalances, family history, and obesity. It is essential to note that these tumors are not cancerous and do not increase the risk of developing ovarian or uterine cancer.
Now, let's talk about the diagnosis and treatment of fibroids and ovarian cysts. Gynecologists in Indore use various methods to diagnose these tumors, including pelvic exams, ultrasounds, and blood tests. In some cases, a biopsy may be required to rule out any cancerous growth. The treatment options for these tumors depend on the size, location, and severity of symptoms.
For fibroids, the treatment options include medication to regulate hormones and reduce symptoms, minimally invasive procedures to remove the fibroids, or surgery to remove the entire uterus (hysterectomy) in severe cases. Ovarian cysts, on the other hand, may resolve on their own, or medication may be prescribed to shrink them. In some cases, surgery may be required to remove the cysts or the entire ovary.
0 notes
Text
Cancer treatments, such as chemotherapy, radiation therapy, and hormone therapy, can cause hormonal changes in the body. These changes can vary depending on the type of cancer, the treatment regimen, and individual factors.
Here are some common hormonal changes associated with cancer treatment:
Menopause: Chemotherapy and hormone therapy can induce menopause or exacerbate menopausal symptoms in premenopausal women. This may include hot flashes, night sweats, vaginal dryness, and mood swings.
Changes in Fertility: Cancer treatments can affect fertility in both men and women. Chemotherapy and radiation therapy can damage reproductive organs and decrease fertility. In some cases, fertility preservation methods may be considered before starting cancer treatment.
Thyroid Function: Radiation therapy, especially if directed towards the head and neck area, can affect thyroid function, leading to hypothyroidism or hyperthyroidism.
Adrenal Function: Some cancer treatments may affect adrenal gland function, which can lead to adrenal insufficiency.
Sex Hormones: Hormone therapy, commonly used in breast and prostate cancer treatment, aims to block or suppress the production or action of certain hormones that fuel cancer growth. This can lead to hormonal imbalances and associated side effects.
Bone Health: Cancer treatments, particularly hormonal therapies used in breast and prostate cancer, can increase the risk of osteoporosis and bone fractures due to decreased estrogen or testosterone levels.
Weight Changes: Hormonal changes during cancer treatment can affect metabolism and lead to weight gain or loss.
Cancer patients must discuss potential hormonal changes and their management with their healthcare team.
Hormonal changes can have significant effects on quality of life and may require additional supportive care or interventions.
Cancer patients of reproductive age must discuss fertility preservation options with their healthcare team before starting treatment. Fertility preservation decisions should be made promptly to maximize the chances of success.
Get the best treatment for cancer, and full body health checkup at the best hospitals in India.
0 notes