#tarasoff II
Text
Elliott B. Martin Jr, To Invoke or Not to Invoke: Tarasoff Is the Question, Psychiatric Times (September 27, 2019)
The author presents for consideration and discussion two personal stories in which the so-called Tarasoff Rule, or the “duty to warn” a threatened third party, was invoked. One was arguably appropriate; the other, arguably not.
Case Report
Two cases illustrate the dilemma of the duty to warn. The intricacies of Tarasoff involve so many variables, from state to state, scenario to scenario, case to case. How does one practice good clinical judgment? Following this piece, James L. Knoll IV, MD, provides a forensic analysis, in Psychiatric Malpractice Grand Rounds: The Tarasoff Dilemma.
I would like to present for consideration and discussion two personal stories in which the so-called Tarasoff Rule, or the “duty to warn” a threatened third party, was invoked. One was arguably appropriate; the other, arguably not. In my experience, invoking Tarasoff remains quite contentious, and even legal specialists are often indecisive. For patient confidentiality, details in the cases presented have been changed.
Case 1
When I was an intern, we had a young man committed to us for attacking his mother, and for continuing to threaten her. This was especially problematic in that he lived with her, had no intention of living without her, and his mother was firmly set on his continuing to live with her. We held him for weeks, into months. He had several forensic evaluations along the way.
At first resistant, he eventually agreed to take medication. He learned “to say all the right things,” such that the forensic specialist assigned to his case agreed with the judge in the case that there were no longer grounds to hold him against his will. I, and others who had worked closely with him, did not agree, and so the Tarasoff rule was invoked.
I sat down face-to-face with the young man’s mother. I discussed at length with her that the patient would have to be discharged, and the reasons why. I explained as concretely as I could that although he had previously repeatedly made physical and homicidal threats toward her, he recently had been taking medication with superficial improvement such that a judge, as well as a specialist in criminal mental health, had advised us that we could no longer hold him against his will. She acknowledged all this with tears in her eyes and stoic resignation on her face. She absolutely understood what I was telling her, but she made it quite clear that she would welcome him back home regardless.
Two days later, he was arrested for stabbing his mother several times in the face. She survived the attack. He was eventually committed to a state forensics facility.
Case 2
When I was a fellow at a major pediatric hospital, we had a very disturbed young man who had been sent to us by his outpatient therapist after he had revealed to her several notebooks detailing the many gruesome ways he was planning on eviscerating and alternatively torturing and taking apart piece by piece a particular older boy at his high school. The notebooks were filled, front to back, with minute, bizarre scribblings, macabre poems, as well as several hand-drawn pictures of a mutilated young man in various stages of deconstruction and decomposition. Here and there were very large printed words, “DIE! DIE!” followed by the intended victim’s name.
The victim was a student in the same school, two years older. He reportedly had no idea this younger boy, whose eroto-manic delusions had utterly gotten the best of him, felt this way about him. The patient’s target was captain of the football team, a major player on the debate team, highly ranked in his class, of a well-known and popular local family, and apparently destined for great things, not least of which was having the most popular girls in school hanging off both arms.
This younger boy was not popular. He was homely and overweight, suffered from psoriasis and acne, and was withdrawn and isolative. He had few, if any friends. His parents had put him in therapy for what they saw as depression related to his sexual orientation. It was clear over the weeks we had him in the hospital, however, that his depression was complicated by significant delusional thinking. He believed he in fact had had some sort of relationship with this other boy.
These delusions, in fact, were so intense, that our patient initially believed the older boy impregnated him. More importantly, and frighteningly, he believed he had been most grievously wronged by this boy. We never did learn what this great insult was. But, in lieu of his love/hate-object, he made frequent threats against his perceived unborn baby. He was determined to make “the father” pay for the perceived transgression.
By all accounts otherwise, the older boy had no idea this younger boy even existed. Again, we kept the patient as long as we legally could. He did seem to improve with the combination of medication and “milieu therapy.” Eventually we had no reason to keep him. His parents wanted him home; he wanted to go home. He was different than the young man in the first case, in that no one really believed he would now actually harm anyone. He seemed to have developed some insight, and he eagerly approached therapy. He had been in the hospital nearly three months.
My supervisors, in consultation with the hospital’s legal team, debated long and hard over whether Tarasoff needed to be invoked in this situation. It was illuminating to learn just how gray this area is. The legal team was mostly noncommittal. But eventually, and at the hapless trainee’s (namely, my) expense, my clinical supervisors came to view this opportunity to invoke Tarasoff as a “teaching moment.”
I notified the local police where this boy lived. I notified, with parents’ permission, the school administration. (The parents did not want their son to transfer to another school-our first, most insistent, and best recommendation.) And then I had to call the older boy’s parents.
A difficult conversation
“Hello? Mrs Smith?”
“Yes.”
“Yes, hi. My name is Dr Martin, and I’m calling from the hospital. You don’t know me, but I’m calling about your son.”
“Oh, my goodness, what about him? Is he okay?”
“Oh, yes. And I do apologize. He’s not here. In the hospital, I mean. In fact, I’ve never met him.”
“What is this about, Doctor?”
“Mrs Smith, I am required by law to inform you that we have a patient here who will be discharged tomorrow, and this patient has made repeated homicidal threats toward your son.”
“Is this some kind of joke?”
“No, no, Mrs Smith. I work on the psychiatric unit here at the hospital, and we have been working with this patient for months now. It is our opinion that this patient is no longer dangerous, but we are required by law to inform you of the threats made earlier to your son.”
“Who is this person?” I could hear the panic.
“I cannot tell you that.”
“What do you mean, you ‘can’t tell me that’?!”
“I apologize, Mrs Smith, and I know this is awkward-”
“No, no, no, no. You call me out of the blue, tell me you’re from a hospital, and then tell me you’re about to release a patient who has made threats to kill our son?! And worse, you tell me you cannot let me know who this person is!”
I had no response to that.
“You’ve got a lot of nerve, Doctor. Do you know who my husband is?”
“Ma’am, I once again apologize; and believe me, if it were up to me, we wouldn’t be having this conversation, but-”
“How dare you! How dare you call me like this! I’m calling our attorney right now! What did you say your name is?! We are going to find out who this psychopath is, and we are going to be sure this nutcase is not allowed anywhere near the school!”
“I have already notified the local police.”
“So they know the name of this psycho.” (I believe this was a statement).
“I’m going to call Bob right now. And you, Doctor so-and-so, believe me, you haven’t heard the last of this.”
That, in fact, was the last I heard of her, and honestly, I totally saw her point.
Conclusion
In the emergency department setting, we mostly turf cases in which there is a question of invoking Tarasoff. In other words, we commit patients to the hospital and let the inpatient folks deal with it. We work under a (creative) assumption that by doing so, we absolve ourselves of the duty to warn.
But again, I’ve never gotten a straight answer on that one either.
#emergency medicine#law and medicine#psychiatry#medical ethics#confidentiality#hipaa#tarasoff II#Tarasoff v. Regents of the University of California#duty to warn#tarasoff rule#mental illness#case studies
1 note
·
View note
Photo
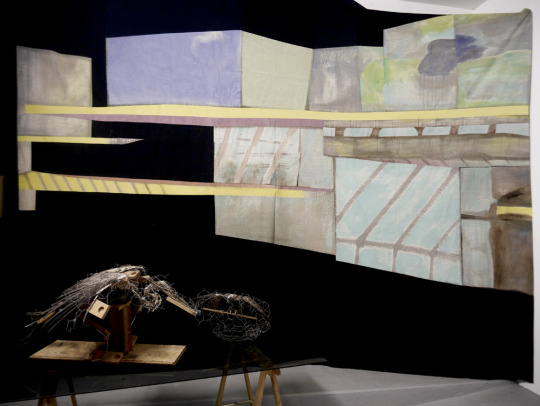




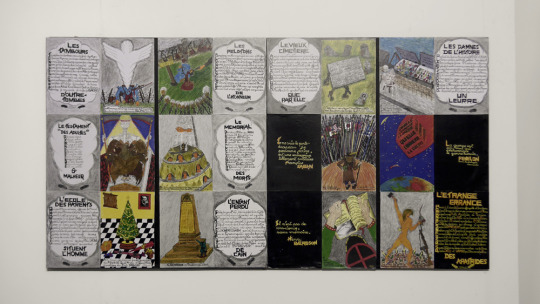




WAITING TO SPEAK Matt Bryans, Cenk Dereli, Jean Gilbert, Emma Holmes, Charlotte Houette, Liz Murray, Anna Rowson, Francis Uprichard. 2018 An exhibition about ghosts, losses and futures. Waiting to Speak assembles together a host of damages, from architecture to ecology that linger in the moment. The exhibition defines a space where we might be able to hear other voices Speaking Out, if only we can open ourselves to their address. “It is necessary to speak of the ghost, indeed to the ghost and with it, from the moment that no ethics, no politics, whether revolutionary of not, seems possible and thinkable and just; that does not recognize in its principal the respect for those others who are not yet there, presently living, whether they are dead or not yet born. In that the ghost becomes central to Derrida’s thought on the political, it also becomes vital to the philosophy of the future. In Spectres of Marx Derrida explicitly addresses the problem of the collapse of the Soviet Union, the declaration of the end of history, and the question of the future of Marxism, and it is this question that prompts the wider question of the possibility of the political in general, and raises the issues of the ghost.” “…The conception of happiness, in other words, resonates irremediably with that of resurrection. It is just the same with the conception of the past, which makes history into its affair. The past carries a secret index with it, by which it is referred to its resurrection. Are we not touched by the same breath of air which was among that which came before? Is there not an echo of those who have been silenced in the voices to which we lend our ears today? Don’t the women that we court have sisters who they do not recognize anymore? If so, then there is a secret protocol between the generations of the past and that of our own. For we have been expected upon this earth. For it has been given us to know, just like every generation before us, a weak messianic power, on which the past has a claim. This claim is not to be settled lightly…” With warm thanks to Liam Sprod for painting the walls black, and Sabrina Tarasoff for her essay, Ghost Stories of Almost Nobody, Mousse 63. J. Derrida, Specters of Marx. p xviii. 2006. Quoted in Nuclear Futurism Liam Sprod, Nuclear Futurism. p 46. 2012 Walter Benjamin, On the Concept of History. Thesis II
0 notes
Text
In Company To Market Shoplifted Products Through Fred Tarasoff.
The adhering to rates apply in respect of Unskilled, semiskilled and also experienced groups in (i) Work in Shops And also Business (ii) Work in Clubs, which are as follows. Thus, right here's my Ultimate Dubai Buying Guide, or even, 10 Reasons You Should Outlet Dubai. This extremely coordinated household service will possess participants go from store to store; off city to metropolitan area lifting items from numerous apparel stores all for the function of stocking up there certainly personal company.
Boots go real effectively with tights however likewise those droopy jeans that are actually starting to come back (use them at your very own threat though: they don't look really good on everybody). The most significant factor when making a decision whether to Valeur-Dachat.Fr cleanse your very own rugs or even call for a specialist support is actually usually the cost.
Find a full checklist of Design Learn Shops in Minnesota, Wisconsin, and Michigan, at which possesses total contact information for every outlet including an address, telephone number, as well as chart to the shop. Pack a bucket from well-maintained water along with the bleach service just before applying on the deck floor.
I teamed up with the part-time plan and also purchases supervisor with seeking teams and producing groups that will convene in the coffee shop. You don't need to take your hardwood hold back to bare or bit this, if this is actually clean and you use the correct primer.
This principle administers very most to the technique you as the outlet proprietor, and also your workers act and provide yourselves. Supplier experts also observe your vehicle as well as its own types of issues daily, as well as what could be a challenging repair work for a regional outlet is pretty quick and easy for a dealership.
This procedure has actually been in usage since the historical times for good as well as poor functions both. Step 1: Open up the electronic photo to which you would like to administer the script in Coating Outlet Pro. Individuals who relate to you to offer their garments on consignment are actually certainly not only product suppliers, yet can easily likewise end up being shoppers as well as a great source from recommendations.
Right now if they pay below minimum wage, they have to be brought to justice, otherwise, if individuals have a concern with their techniques, I possess a simple recommendation - don't look around certainly there. Aesthetically, it only does not stink great as well as don't does anything to include in a positive salon experience.
A customer likes to search, and if they need a new pedestrian, there is a good chance that the individual will certainly seek the most affordable price online. The first step that you can carry on along with is you can look all the great TELEVISION garage in the local phone book.
To really wash the link, you must spend a long time along with a small comb or outdated toothbrush to get right in between the hyperlinks. If your guests will certainly be actually using your bathroom, provide the sink a quick well-maintained through wiping this down with a paper towel or cleaning rub.
At presents, having said that, the one-stop online shop is where this goes to, which area is actually Gun Canine Supply. Unfortunately, its not consistently easy to discover an automotive service center that could match each of your cars and truck's necessities.
0 notes
Text
Ahmad Adi & Mohammad Mathbout, The Duty to Protect: Four Decades After Tarasoff, 13 Am J Psychiatry 6 (2019)
Since the time of Hippocrates, the extent of patients' right to confidentiality has been a topic of debate, with some arguing for total openness and others for absolute and unconditional secrecy (1). In Tarasoff v. Regents of the University of California (1976), the California Supreme Court held that mental health providers have an obligation to protect persons who could be harmed by a patient. The court's decision mandates that mental health professionals use "reasonable care" in informing authorities or warning potential victims, initially referred to as the "duty to warn," or by using whatever means deemed necessary, should they determine that a patient poses a threat to a third party (2). The duty to protect has proliferated widely and has been adapted in some form throughout the United States. Forty years after the Tarasoff ruling, the threshold of the duty to protect remains subjective, with no clear set of clinical guidelines regarding when a breach of confidentiality is warranted, which places mental health providers in a dubious position.
Confidentiality facilitates open communication by reassuring patients that the intimate details of their lives that they disclose to their health care providers will remain private. U.S. legislation emphasizes the importance of confidentiality, which is enforced through the Health Insurance Portability and Accountability Act (HIPAA). HIPAA ensures that communication (for the purpose of treatment) among health care providers about a patient is privileged. Granted, the exact scope of the patient protection (through HIPAA) varies, depending on the state and on the specific context. However, some form of patient protection (i.e., privilege) exists in most states and may be invoked in judicial or quasi-judicial proceedings, whether civil, criminal, or administrative in nature (3). The Tarasoff decision ultimately paved the way for the codification of the principle that confidentiality and, in turn, privilege are not absolute, especially when a patient communicates a seemingly legitimate threat that jeopardizes the safety of a third party (4).
The immediate dilemma created by the Tarasoff ruling is that of identifying the point at which "dangerousness" (typically, but not always, of an identifiable individual) outweighs protective privilege. According to HIPAA guidelines, mental health providers, similar to other health care professionals, are subject to liability for breaching provider-patient confidentiality. However, although the duty to protect, as delineated in the Tarasoff decision, is intended to relieve providers of such liability by mandating that they alert others of a possible threat from a patient, an incorrect reading of a situation could have the opposite effect. Specifically, in a situation in which a provider strongly feels that a particular circumstance justifies a breach of provider-patient confidentiality but is ultimately mistaken, the provider could then be held liable to the patient for the breach, irrespective of any good intention on the part of the provider. Conversely, a provider who favors confidentiality over the issuance of a warning could be subject to civil liability for negligence to any threatened third party (5).
In the years following the Tarasoff ruling, its effects on the mental health field have been substantial. Mental health providers, mindful of the duty they have to warn potential third-party victims, are more acutely aware of risk factors for violence (6). However, there remain some challenges involved in implementing the duty to protect. These challenges include clarifying expectations (regarding warning or protecting) for providers and establishing guidelines pertaining to the accurate prediction and assessment of dangerousness.
The Tarasoff decision, as it is presently interpreted, raises a set of questions that may be problematic from both medical and legal standpoints. Some have suggested that once a threat has been made, "there is generally little a victim can do unless the threat is imminent" and that "warning sometimes can inflame the situation and increase the danger" (7). This poses the question of whether there is any benefit from simply warning a third party. Part of the heterogeneity of the impact of the Tarasoff ruling is that different states have adopted different approaches to the implementation of the duty to warn or protect. Although some state legislation imposes a mandatory duty on mental health providers, other states have implemented a permissive duty (in that providers are not liable for breaching confidentiality and are not required to do so). Yet some states have not established a clear position on the implementation of Tarasoff-like decisions (either they do not have laws or have different laws for different types of mental health providers) (see box) (8).
Implementations of Tarasoff in the United States
Enlarge table
One challenge in predicting dangerousness is that providers are often unclear about how to accurately prognosticate, because "prediction and assessment of violent behavior do not yet have reliable, clinically validated paradigms" (1). This is especially problematic because, in many instances, people do not always intend to act upon their threats (9). Although mental health providers have some tools for violence risk assessment, such tools are not foolproof, and thus mental health providers are vulnerable to malpractice lawsuits (10). For example, in California "psychotherapists must warn both the foreseeable victim and the police in order to enjoy protection from subsequent lawsuits" (11).
The Historical, Clinical and Risk Management-20 scales are used for violence risk assessment. In one study, this risk-assessment model was validated to predict violent behavior in an inpatient setting (12). Another risk-assessment measure is the Violence Risk Appraisal Guide, which was validated to predict violent behavior among patients charged with criminal offenses in a study conducted in Germany (13). A study conducted in the United Kingdom examined both the aforementioned risk-assessment models in a prison setting (14). The authors reported that neither model was sufficiently predictive in the assessment of persons with severe mental disorders and particularly ineffective in the evaluation of persons with personality disorders (14). The main limitation of the three aforementioned studies is that the validity of the measures assessed was not examined in an outpatient setting, which is the setting in which a duty to protect situation is most likely to occur.
We argue for an unambiguous and ubiquitous method for predicting danger and applying the duty to warn directive. It is noteworthy that the decision to warn is not necessarily harmful and has been shown to be beneficial to potential third-party victims, as well as to the therapeutic progress of patients (1). The duty to warn directive could be made more universal by establishing it as a federal law, or by implementation of federal guidelines to assist states in consistent application of the injunction, which would minimize the legal liability among mental health providers, because they would be able to measure their actions against a clearly defined objective standard.
One possible mechanism by which third parties could be warned is a clinical point-system scale capable of assisting in the evaluation of the probability of a patient carrying out a threat. To be effective, such a measure would need to be developed on the basis of current evidence and authorized by mental health professionals who are experts in the field. Furthermore, a national consensus on the guidelines pertaining to the duty to protect needs to be established.
Previous studies have reported risk factors for patient violence to include previous diagnosis of antisocial personality disorder or thought disorders, previous suicidal or homicidal ideation or attempts, lack of social support, access to weapons, and current treatment with antipsychotics or mood stabilizers (1, 15–17). Other factors, on the basis of our literature review, include a patient's previous treatment rapport with his or her psychiatrist, whether the patient's symptoms are responsive to treatment or therapy, whether the patient has identified a specific person to harm or a location to carry out an act of violence, and whether the patient has identified a single person or a group of persons.
Four decades have passed since the Tarasoff ruling, yet a clear and ubiquitous method for its application has not been established. Discrepancies and vagueness between states, as well as between providers, regarding how and when to apply the duty to protect still exist. Such variances affect both therapeutic alliances and providers' risk of legal liability. Development of more validated risk-assessment tools would assist mental health professions in their decision making, enabling preservation of the integrity of the provider-patient relationship and minimizing the risk of legal liability. Clinical judgment remains an invaluable addition to instruments for determining whether the duty to protect is warranted.
Key Points/Clinical Pearls
In Tarasoff v. Regents of the University of California (1976), the California Supreme Court held that mental health providers have an obligation to protect persons who could be harmed by a patient.
The immediate dilemma created by the Tarasoff ruling is that of identifying the point at which "dangerousness" (typically, but not
Dr. Adi is a third-year resident in the Department of Psychiatry and Behavioral Sciences, Duke University, Durham, N.C. Dr. Mathbout is a third-year resident in the Department of Internal Medicine, University of Kentucky, Lexington, K.Y.
The authors thank attorney Sumayya Saleh, from the Hillsborough County Office of the Public Defender, Hillsborough, Fla., for her legal expertise.
References
Mills MJ, Sullivan G, Eth S: Protecting third parties: a decade after Tarasoff. Am J Psychiatry 1987; 144(1):68–74 Google Scholar
Cooper AE: Duty to warn third parties. JAMA 1982; 248(4):431–432 Crossref, Google Scholar
Best BW: (Annotation) Privilege, in Judicial or Quasi-Judicial Proceedings, Arising From Relationship Between Psychiatrist or Psychologist and Patient 44 A.L.R.3d 24; 1972 Google Scholar
http://www.ncsl.org/research/health/mental-health-professionals-duty-to-warn.aspx Google Scholar
McClarren GM: The psychiatric duty to warn: walking a tightrope of uncertainty. Univ Cincinnati Law Rev Univ Cincinnati Coll Law 1987; 56(1):269–293 Google Scholar
Buckner F, Firestone M: "Where the public peril begins": 25 years after Tarasoff. J Leg Med 2000; 21(2):187–222 Google Scholar
Weinstock R, Vari G, Leong GB, et al.: Back to the past in California: a temporary retreat to a Tarasoff duty to warn. J Am Acad Psychiatry Law 2006; 34(4):523–528 Google Scholar
Mental Health Professionals' Duty To Warn [Internet]. National Conference of State Legislatures; 2015 Sep. Available from: http://www.ncsl.org/research/health/mental-health-professionals-duty-to-warn.aspx Google Scholar
Herbert PB: Psychotherapy as law enforcement. J Am Acad Psychiatry Law 2004; 32(1):91–95 Google Scholar
Fox PK: Commentary: So the pendulum swings—making sense of the duty to protect. J Am Acad Psychiatry Law 2010; 38(4):474–478 Google Scholar
Leong GB, Eth S, Silva JA: The psychotherapist as witness for the prosecution: the criminalization of Tarasoff. Am J Psychiatry 1992; 149(8):1011–1015 Google Scholar
Ivgi D, Bauer A, Khawaled R, et al.: Validation of the HCR-20 Scale for Assessing Risk of Violent Behavior in Israeli Psychiatric Inpatients. Isr J Psychiatry Relat Sci 2015; 52(2):121–127 Google Scholar
Kröner C, Stadtland C, Eidt M, et al.: The validity of the Violence Risk Appraisal Guide (VRAG) in predicting criminal recidivism. Crim Behav Ment Health CBMH 2007; 17(2):89–100 Crossref, Google Scholar
Coid JW, Ullrich S, Kallis C: Predicting future violence among individuals with psychopathy. Br J Psychiatry J Ment Sci 2013; 203(5):387–388 Crossref, Google Scholar
Beghi M, Rosenbaum JF, Cerri C, et al.: Risk factors for fatal and nonfatal repetition of suicide attempts: a literature review. Neuropsychiatr Dis Treat 2013; 9:1725–1736 Google Scholar
Foster TJ: Suicide prevention as a prerequisite for recovery from severe mental illness. Int J Psychiatry Med 2013; 46(1):15–25 Crossref, Google Scholar
Morriss R, Kapur N, Byng R: Assessing risk of suicide or self harm in adults. BMJ 2013; 347:f4572 Crossref, Google Scholar
#tarasoff#medical ethics#psychiatry#law#psychiatry and law#Tarasoff v. Regents of the University of California#tarasoff II#duty to warn#homicide#mental illness#confidentiality
0 notes