Newly graduated veterinarian here to talk to you beautiful people about the wonderful world of veterinary medicine.
Don't wanna be here? Send us removal request.
Text
Can eyes “pop out”?
In short, the answer is yes.
In emergency practice you may see traumatic proptosis, seen on the schedule as “dogs eye popped out, on the way immediately”.
Experiencing this diagnosis for the first time can be quite shocking, and even nerve wracking. How do I fix this? What do I do? Will the eye be okay?
Proptosis is caused by a traumatic event, often blunt force trauma, and is especially likely in brachycephalic breeds (the ones with the short faces and buggy eyes).

The eyelids become trapped behind the globe (eyeball) and prevent the globe from returning to its normal position. Swelling of the surrounding tissues further prevents the ability of the globe to return.
What to discuss with the owners.
Prognosis ~25% of dogs will regain vision, this number is much less in cats. If PLR is intact, prognosis for return to vision is improved. The globe may remain comfortable with or without vision though the following factors worsen prognosis: skull fracture, tearing of multiple extraocular muscles, and globe rupture. Clinical Pearl - without globe rupture or obvious severe trauma, the only way to know if comfort or vision will be maintained is time. Advise clients that despite treatment, the eye may need to be removed later.
Brachycephalic Being brachycephalic may improve the prognosis for the eye as less force is needed to displace the eye, as opposed to severe force that is likely to cause additional damage in a non-bracycephalic breed. However, this animal is more prone to recurrence of proptosis, including the other eye, due to conformation. Discuss possible referral options to help prevent recurrence - medial canthotomy can be performed to tighten the eyelids around the healthy eye.
Treatment
There are two treatment options, depending upon severity of presentation.
Tarsorrhaphy If the globe appears to possibly be salvageable, this option may save the eye, and in a small percentage also save the vision. When stable, the patient is anesthetized for the procedure. Copious amounts of lubricant is applied and the globe is returned to position. Once in position, multiple horizontal mattress sutures with stenting material (sterile IV tubing, buttons) are placed. Sometimes a lateral canthotomy is performed to further open the eyelids and assist closure. Multiple medications are to be sent home including oral antibiotics, pain medication, topical antibiotics and topical atropine. Sutures remain for 2-3 weeks (with an e-collar) - at which time, they are removed and the fate of the globe is determined.
Possible complications include corneal ulceration, retinal degeneration, cataract formation, strabismus, keratoconjunctivitis sica, etc.
If the eye has any significant complications at suture removal, enucleation may be pursued.
Enucleation If there are negative prognostic indicators as discussed above, enucleation may be elected at the time of presentation. Otherwise, enucleation may be elected after tarsorrhaphy with unideal final results. For example, a globe with severe strabismus and cataract formation preventing vision.
Summary
This is an EMERGENCY and requires prompt attention with clear communication with the owner. They should be informed of prognosis and complicating factors to help guide their decision for tarsorrhaphy vs enucleation.
When electing tarsorrhaphy the owner must be adequately informed of possible complications, the low chance of return to vision, and the possibility of requiring enucleation after 2-3 weeks.
30 notes
·
View notes
Text
Leaving isn’t easy but sometimes it’s amazing.
Hello vetlings, long time no talk. Since last posting I have gone through a lot of change and development. I decided that my previous job was no longer providing me with what I needed, and was not the type of environment that I wanted to be in.
I fairly spontaneously found a new job, in a new city, and just went for it. I have been here for about 6 months now and have learned so much that I want to share with you all.
So, how do you know it’s time to move on, specifically from a veterinary job?
Here’s what I learned.
1. No job is forever. There is nothing wrong with admitting your job is not the right one for you. Whether it be for career reasons, interpersonal reasons, or something else. Leaving a job is not a failure.
2. No, you are not guaranteed to bring your problems with you. I stayed in my previous job way too long as I was constantly told that I was the problem and it would follow me. I believed that and tried so hard to change things that I didn’t even believe were happening. I do not experience any of these issues in my new clinic.
3. Not every clinic is full of toxic gossip - don’t talk about your coworkers behind their back every day. Don’t normalize this behaviour.
4. You can outgrow a clinic. A big reason I decided to leave was my learning had stagnated. I was no longer learning new procedures or treatments and I often had to refer cases that I wanted to manage due to lack of equipment or training. I decided it was time for more.
5. You can outgrow a clientele - quite frankly, I got sick of people refusing to spend any money on their pets. I work somewhere with an entirely different mindset and clientele.
6. Sometimes people need help - it’s amazing how good having flexibility in billing is for our mental health. Working at a clinic that is willing to work with people, while also valuing their staff, is wonderful.
7. How they pay their staff matters. Underpaid support staff are not often fully satisfied with their job, it shows.
8. When you discuss issues with management, you should see change.
9. If you get to a point where you dread going into work every day, please evaluate why this is and leave. Don’t stay somewhere you’re not happy because you feel like you have to.
10. Finally, pay attention to how employees are/were treated during a pandemic. It shows you a lot about a companies priorities.
I can’t wait to share the amazing things that I’ve been learning with you all now that I’ve found my new home <3
30 notes
·
View notes
Text
Physical Examination of the Eye in Veterinary Medicine
A thorough ocular examination is an important diagnostic procedure in veterinary medicine. Primary and secondary ocular disease may occur. The changes seen in the eye may be related to another disease process, directing you to further diagnostics.
Before being able to perform a proper ocular examination, you must understand the anatomy of the species that you are examining. This post will largely focus on mammalian eyes.
Basic ocular anatomy includes: The cornea - clear tissue covering the front of the eye. The uvea (ciliary body, choroid, and iris) - vascular tissue of the eye. The iris is the coloured section surrounding the pupil. The lens - clear disc within the eye that is used to focus light. The retina - photoreceptors are present here. Light is converted into a signal for the brain to interpret as a visual. The sclera - the white connective tissue surrounding the globe. The optic nerve - carries nervous information to the brain.
Related structures include: The third eyelid (nictitating membrane). The eyelids and conjunctiva. The lacrimal glands - produce the watery portion of tears. The meibomian glands - produce the oily portion of tears.
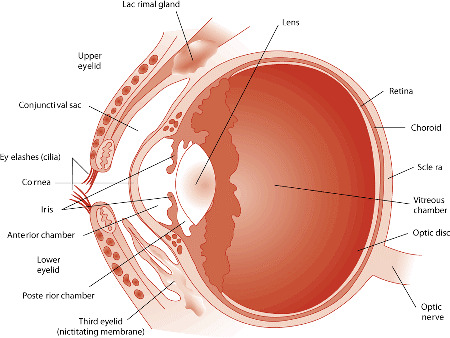
Image source: https://www.merckvetmanual.com/dog-owners/eye-disorders-of-dogs/eye-structure-and-function-in-dogs
Vision
The patient should be observed as they move around the examination room. Signs that the patient may be experiencing difficulty in seeing include reluctance to move, running into things, and high stepping.
Menace response: This test is performed by performing a threatening hand gesture heading towards the eye. The contralateral eye should be covered when performing this test. It is important to avoid pushing air/creating a breeze toward the patient as air stimulus alone may cause the patient to blink. You must avoid contact with the whiskers. A positive menace response is achieved when the patient blinks. The menace response is a learned response and is not present consistently in cats and dogs under the age of 3-4 months. Tests: peripheral and central visual pathways, visual cortex, CN7.
Pupillary light reflex: This test does NOT test vision as it is a subcortical reflex. This may be normal in a cortically blind animal. This test is performed by shining a light into the eye and observing the response of pupil size. This should be done with a bright light in a dimly lit room. Both direct (the eye in which light is being shined) and indirect (the contralateral eye) PLRs are observed. Both direct and indirect should be present when light is shined into either eye. Birds and reptiles do not have a PLR. They are able to control the constriction and dilation of their pupils independent of light.
Dazzle: This test does NOT test vision as it is a subcortical reflex. This test is performed by intensely illuminating the eye. A positive dazzle response is achieved when the patient reacts to the light. This reaction can be a blink, third eyelid protrusion, head movement, or globe retraction. Tests: retina, CN2, CN7.
Periocular
Evaluate the orbits (bone surrounding the globe) for symmetry, deformity, or enlargement. Breed variations are important to understand during this portion of the examination. The orbital rim should be palpated to ensure no irregularities are missed.
The position and general movement of the eyes should be observed: Strabismus - abnormal alignment of the eyes. Nystagmus - rapid involuntary movement of the eyes.
Eyelids
Blink (palpebral) reflex: This test is performed by touching the skin near both corners of the eye. This should produce a blink response. The finger should be gently dragged across the closed eye to ensure that the patient is capable of holding their eye closed. Tests: CV7, orbicularis oculi muscle, CN2, CN5.
The eyelids should be observed for any abnormalities. Abnormalities may include: Masses or cysts. Entropion - rolling in of the eyelid. Ectropion - rolling out of the eyelid. Ectopic cilia - eyelashes in abnormal locations.
Conjunctiva
The upper and lower eyelids should be manually everted. This allows for evaluation of the tissue. Abnormalities may include: Increased vascularity. Lacerations or foreign bodies. Growths. Chemosis - edema.
Third eyelid
The third eyelid can often be extruded by placing gentle pressure on the tissues near the inner corner of the eye. Abnormalities may include: Prolapse of the gland - cherry eye. Conjunctivitis. Enlarged glands or lymphoid tissue.
Sclera
The sclera should be observed for changes in vasculature, colour, masses, or lacerations.
Cornea
The cornea should be avascular and unpigmented. It should be smooth. The cornea should be examined for change in transparency/opacity, vascularization, pigmentation, laceration/ulceration, masses, and foreign bodies.
Fluorescein stain: This stain is used to confirm the absence or presence of superficial ulcers. No corneal examination is complete without this test. The dye does not stick to the outer layer of the cornea as it is lipid selective. The corneal stroma, when exposed, allows rapid diffusion of the dye. An area of fluorescein retention is indicative of an epithelial defect such as an ulcer or erosion.
Anterior Chamber
A focal light source should be shined through the anterior chamber of the eye to examine the aqueous humor. When increased protein is present, the beam of light should appear to be passing through smoke. This is called aqueous flare and is indicative of uveitis.
Lens
The lens should be transparent and avascular. The lens should be observed with an ophthalmoscope for opacities, position, and size.
Cataracts: Focal - localized within various parts of the lens. Nuclear cataracts are usually stationary. Equatorial cataracts are usually progressive. Immature cataract - involves more of the lens and causes blurred vision. Mature cataract - entire lens affected, vision loss.
Lenticular sclerosis: Begins to develop in dogs around 6 years of age. This is seen as a blue zone in the nucleus of the lens that does not impair visualization of the fundus.
Fundus
An ophthalmoscope is required for examination of the fundus. An examination can be performed without drug induced mydriasis (dilation of the iris) though it assists in complete examination.
Abnormalities may include: Vascular patterns. Retinal detachment. Congestion or hemorrhage. Changes in pigmentation.
Tear Production
Tear film is essential in maintaining normal corneal health. When the cornea is not appropriately moisturized, ulcers and other pathology can result.
The schirmer tear test is used to quantify the amount of aqueous tear portion present in each eye. This test does not evaluate the quality or make-up of the tears. The test strip is placed in the lacrimal lake at the junction of the lateral and middle thirds of the lower eyelid. It is held in place for 60 seconds while the animal typically holds their eye closed. The test is not linear and therefore you cannot measure for 30 seconds and simply multiply by two. Normal values are > 15mm for cats and dogs. Other species may have species-specific values published.
Intraocular Pressure
This is measured with tonometry. Applanation tonometers, such as the tonopen, are very accurate. Normal IOP is 16.8 ± 4.0 mm Hg in dogs; 20.2 ± 5.5 in cats. Low IOP indicates uveitis while high IOP indicates glaucoma.
#veterinarian#veterinary medicine#veterinary#vet med#vet school#vet student#ophthalmology#vet ophthalmology#vetblr
55 notes
·
View notes
Text
WHY you shouldn’t feed these 10 foods to your dog
Dogs might think they’re human, but their physiology is not like ours. Humans might eat a wide variety of foods with little concern, but there are some very common human foods which you should not feed to your canine companion. You’ve probably seen the foods on this list before, but this is WHY these foods should not be fed to dogs.

Chocolate, Theobromine and Caffeine:
Everybody’s heard that chocolate is bad for dogs, and it’s true. Chocolate contains a compound called Theobromine. Theobromine is a type of compound called a methylxanthine, and another methylxanthine you might be more familiar with is caffeine. We know quite a lot about these compounds, as humans use them both medicinally and recreationally. The long version is that they all inhibit phosphodiesterase and antagonise adenosine receptors. The short version is that they increase muscle activity, including the heart, and stimulate the central nervous system.
This presents as dogs that have fast and irregular heart rates, high body temperatures and increased muscle activity that can progress to seizures.
It takes a reasonable amount of chocolate to poison a dog. One M&M isn’t going to do it. For a 35kg dog it’s going to take at least 3500mg of theobromine, which is about 5kg of typical milk chocolate. But only 1.2kg of dark chocolate or 600g of cooking chocolate, which is possible.
A 10kg dog needs much less. 1.5kg of milk chocolate would do it, which is only about 3 large Easter Bunnies, or 300g of dark chocolate, which is one packet from the cooking isle.
Chocolate is super tasty, dogs will absolutely gorge themselves on all chocolate available, so it’s not too difficult to poison smaller dogs with it.
And even if you get the dog through the toxicity, the high fat content of chocolate can go on to cause other gastrointestinal problems.

Onions & Garlic:
Yes, I said onions AND garlic. All allium species contain the same potentially toxic compounds, whether raw or cooked. That goes for spring onions too, it’s just really difficult to convince a dog to eat enough of them to be poisoned. These plants cause a Heinz body anaemia by inducing oxidative damage to the surface of the red blood cells, and for some reason breeds of Japanese origin like the Akita and Shiba Inu seem particularly prone to this toxicity.
It usually takes 10 to 15g per kg of body weight to poison a dog, but those breeds can be affected by as little as 5g per kilo. So for a big, 35kg dog, that’s about three medium sized onions.
Poisoning can happen all in one go, or it can happen by eating small amounts over a longer period of time, which is why it’s infuriating to see garlic being suggested as a natural remedy for things.
Bad cases will have to be treated with a blood transfusion as there is no direct antidote. And for interest, there are other things that can cause Heinz body anaemia too, like zinc.
Keep reading
2K notes
·
View notes
Text
Clients have huge impact
As many of you know, the suicide rate in veterinary medicine is unfortunately high. Imposter syndrome, compassion fatigue, verbal abuse from clients, etc... That’s not taking into consideration what the veterinarians are dealing with at home - anxiety, depression, family, friends, etc... It is a hard job. A job that I love.
I have been going through a rough time emotionally over the past few weeks. I am okay, I am not depressed or suicidal. Do not worry about me.
I just wanted to let each and every one of you know how much impact you can have in your veterinarian's life (or vet tech, vet assistant, receptionist etc).
“You’re good at what you do” “I’m glad we have found you” “Thank you for everything you have done” Positive reviews online - especially those that mention people by name. Bringing in cards, treats, etc for the team.
I hold simple comments and actions such as these very close to my heart. To be appreciated by clients is an amazing feeling. Something that can help pull me out of a funk, put on a smile, believe in myself. Never doubt the importance of your words.
I’m not going to list examples of negative comments I’ve heard, I’m sure you can imagine some. I value constructive criticism and want to know if there are things we could do better. I do not want to be bullied. Harsh and abusive comments can impact your veterinary team in ways you may not have intended. We are all people too.
I will not let the negative keep me down because I have so many clients that I cherish dearly.
Love your vet, be kind to your vet, TELL THEM. You never know how much you can change their day, their week, their year.
116 notes
·
View notes
Text
Tips for Dog Owners
There are lot’s of things to know about owning a dog and the internet can be an overwhelming source of information. You may find multiple different sources that all disagree with each other; so how do you know what to believe?
The best source for information is your veterinary clinic. Your pets annual physical exam is a great time to talk to your veterinarian about lifestyle topics such as diet and exercise. If you ever have a question about if certain foods or activities are safe for your dog, please reach out to the clinic.
Below I have compiled some broad tips for dog owners, including how to choose the right diet and toxins to avoid.
Diet
Choosing the right food is something that every pet owner is faced with. The internet is certainly full of misinformation and strong beliefs when it comes to the best food for cats and dogs. Who’s right? How do you choose?
The best source of nutritional information is your veterinarian. They are able to combine their knowledge of nutrition with their knowledge of your pets needs to help decide the best options for you.
Listed below are some things to think about when deciding on a food:
AAFCO Statement Food should include an AAFCO (Association of American Feed Control Officials) statement on the back of the bag. This is a nutritional adequacy statement that reads: “[Name] is formulated to meet the nutritional levels established by the AAFCO Dog (or Cat) Food Nutrient Profiles for [life stage(s)]". A statement such as above means the food formulation is determined via laboratory analysis versus being determined by feeding to animals. If the statement mentions “feeding trials” then it has been fed to animals to ensure an adequate nutrient profile.
Research The reason that veterinary clinics carry the food that they do (ie Hills, Royal Canin, Purina Veterinary Diets) is that many of the diets have research backing them. We do not receive any “kickbacks” or benefits from carrying and selling specific foods. We carry them simply because we believe in them. Many of these diets have undergone various types of testing and research. As well as safety and palatability, effectiveness for certain goals (dental, urinary etc) are also tested.
Life stage The AAFCO statement includes what life stage the food is formulated for. “All life stages” - this is the descriptor for puppy/kitten, pregnant or lactating animals. To be “all life stages” a food must meet the requirements for the most demanding life stage (ie growing babies). This leads to higher levels of certain nutrients than adult or mature pets require. Foods marketed to be appropriate for all life stages are unfortunately not. “Adult maintenance” - this is the descriptor for adult food. This is the descriptor you should look for when feeding an adult who is not pregnant or lactating.
Specific Goals There are many foods available that help addresses specific goals. Determining what goals you have for your pet may be helpful in choosing the right food. Examples include: Dental diets - veterinary dental diets are formulated to help keep the teeth clean and prolong the amount of time between dental cleanings. Urinary diets - veterinary urinary diets help promote a healthy urinary environment and may be recommended for patients that are predisposed to urinary issues.
Medical condition If your pet has a medical condition which requires certain food for adequate management your veterinarian will discuss this with you.
Exercise
The amount and type of exercise that your dog needs ranges widely depending on breed. High energy breeds such as border collies require much more exercise than a bulldog. Daily exercise is important for all dogs. Please talk to your veterinarian about the appropriate amount and type of exercise for your pet as it ranges widely depending on breed and medical condition.
Toxins
There are many toxins that dogs have the potential of being exposed to. Some toxins that you should prevent your dog from accessing:
Chocolate
Xylitol (artificial sweetener)
Grapes/Raisins
Garlic
Onion
Human medications (ie ibuprofen, naproxen)
Other
Bones - it is recommended that you avoid feeding bones to your dog. Possible dangers associated with bones include broken teeth, intestinal obstruction, and intestinal rupture.
Tooth brushing - the best way to help prevent dental disease is by brushing their teeth. It is recommended to do this once daily. It is best to begin exposing your dog to tooth brushing when they are a puppy.
Weight - it important to maintain an appropriate weight for your pet. Weight is much harder to lose than it is to prevent weight gain. You should be measuring out the appropriate amount of food for your pet and not meal feeding.
53 notes
·
View notes
Text
“If you bring a dog in with a fractured toe, a traditional vet might amputate the entire limb,” said Campana. “But even though people say ‘my dog does pretty well on three legs,’ when you hop on one leg, the rest of your body can break down so quickly. We have proven that we can tack on at least two years to a dog’s life by adding a prosthetic.”
No veterinarian is going to amputate a limb to treat a broken toe, that is a ridiculous comment.
And four legged animals do extremely well with just three legs. We aren’t shortening lives or causing a “break down” by amputating a limb.
Prosthetics for pets make really good media stories but most stories aren’t completely truthful and I think pet owners get the wrong idea.
You cannot just slap a prosthetic limb on a pet and move on with life. These are not meant to stay on permanently, most are put on for exercise but taken off when the animal is at home. Prosthetics can cause pressure sores and skin infections and often need to be refitted. Many prosthetics also fail but we don’t see those stories.
If your pet needs a limb amputation they don’t need a prosthetic limb they will do very well without. For pets that can use a prosthetic it’s important to completely understand the pros and cons and be prepared for constant maintenance and costs.
224 notes
·
View notes
Text
What does it mean if my pet has a heart murmur?
A routine part of physical examination of your pet includes listening to the heart and lungs. When listening to the heart your veterinarian will count the rate, listen to the rhythm, and listen to the quality and type of sounds.
What is a heart murmur?
Typically, when listening to a heart you would hear a “lub-dub lub-dub” as the heart beats. These noises are created by the valves in the heart closing.
When an animal has a heart murmur, the typical “lub-dub lub-dub” will not be heard. Instead your veterinarian will hear a “whoosh”. This noise is created by turbulent blood flow in the heart, blood swirling or flowing in abnormal directions.
Possible causes include:
Birth defect in the heart
Leaky heart valves (malformed or degeneration)
Hypertrophic cardiomyopathy (thickening of heart muscle)
Dilated cardiomyopathy (thinning and ballooning of heart muscle)
Non-heart disease such as anemia or hyperthyroidism
Can my vet tell what caused the murmur by listening to the heart?
Your veterinarian will be able to characterize the heart murmur based on volume and location, but unfortunately listening alone cannot lead to a diagnosis of the cause.
What should I do next?
Depending upon the species, grade, and signs (caught on routine exam or presenting with illness) your veterinarian will advise you on the appropriate next steps.
Possible recommendations may include:
Chest radiographs (x-rays)
Allows evaluation of heart size and shape
Allows evaluation of lungs (signs of heart failure may be seen in the lungs)
Allows your veterinarian to determine if preventative medications are indicated (there is a drug that has recently been proven to extend the amount of time before heart failure in dogs diagnosed with hearts of a certain size)
These will not allow for a definitive diagnosis of cause
Blood work
Allows for evaluation of non-heart related disease (ie thyroid levels)
Echocardiogram (heart ultrasound)
This is the only way to determine the cause of the heart murmur
This is performed by a veterinary cardiologist
The valves and other structures in the heart can be evaluated
Function of the heart muscle can be observed
Many measurements may be performed
Allows for medication planning if indicated
Allows for close monitoring of disease
What do I need to watch for?
Though it is great if your pet is active and energetic, it does not necessarily mean that they do not have significant changes in their heart. Any animal with heart disease may develop heart failure.
Signs to monitor for include:
Slowing down during usual activity
Sleeping more
Coughing
Retching
Rapid or laboured breathing
Collapse
Blue or pale gums
If you are concerned that your pet may be in heart failure, please bring them in to a veterinarian immediately. Your veterinarian will discuss appropriate diagnostics and treatment depending upon the presentation of your pet.
The changes in the heart that lead to heart failure cannot be repaired, though symptoms may be able to be managed. Response to treatment of heart failure varies greatly depending upon the individual - many animals may be able to return to a good quality of life, though some do not respond well to treatment. Treatment must be closely monitored and follow up examinations, x-rays, and blood work may be indicated to ensure appropriate control of disease. Heart failure, unfortunately, may occur again at any time.
74 notes
·
View notes
Text
This past week, as many before it, I had many tough cases and many euthansias. One of my favourite clients lost their pet despite all of my medical and surgical intervention. One of my favourite clients had to schedule expensive surgery for their animal this upcoming week, months away from expecting their first child. I am heartbroken for many, but uplifted by them all.
After euthanizing an old sick pet, the client returned later in the day to thank me. To tell me he knows it can’t be easy for me and that he appreciates all that we do. After losing his best friend, the client gave me the biggest bear hug ever and thanked me for everything we did for him and his pet. Asked me to thank every member of our team that helped him along the way. While making the decision to move ahead with surgery, the clients told me how happy they were to have found me to care for their pets. How they would travel to bring their animals to me if I moved, though they hope that I never do.
I am so thankful for clients like these. They keep me moving through the difficult days. I am so honoured to be involved in the care of their animals <3
28 notes
·
View notes
Text
Veterinarian vs Veterinary Technician
So you’ve decided that you want to work in the veterinary field but you’re not quite sure if you want to become a veterinarian or a veterinary technician. This post is for you.
Both veterinarians and veterinary technicians are integral parts of the veterinary team. They work very closely together, and are both involved in patient care and client communication. How do they differ?
Education
Veterinary Technician - most veterinary technicians attend a two-year college program. This program does not require any prior post-secondary schooling.
Veterinarian - veterinarians must attend veterinary school, this is often four years. This program requires prior post-secondary education in North-America. Refer to my previous post for details on veterinary schooling.
Responsibilities
Veterinary Technician Throughout certain jurisdictions, technicians are referred to as veterinary nurses. While it is certainly not as simple as nurse vs doctor, that can be broad way of looking at the positions. Veterinary technicians perform a much wider range of duties than a human nurse as they are involved in every aspect of human care. Duties include: - positioning for and taking radiographs - drawing and running blood - performing laboratory tests such as urinalysis and fecal examination - medication administration - prepping patients for surgery - recovering patients form surgery - monitoring anesthesia - dental cleaning - client communication Duties do NOT include: - diagnosing - creating treatment plans - surgery
Veterinarian As the doctor, the responsibility of diagnosing and treating falls upon you. All diagnostic interpretation and treatment plans must come form the veterinarian. Veterinarians may create diagnostic or treatment plans for their technicians to then perform. Duties include: - all duties previously mentioned under technician (depending on the clinic, these duties may be shared or placed solely under technicians) - interpreting laboratory tests (bloodwork, urinalysis, fecal examination etc) - interpreting radiographs - diagnosing patients - creating treatment plans - performing surgery - removing teeth during dentistry There are no duties that veterinarians cannot perform.
Pay
Pay will depend largely upon the area of the world that you work in. Veterinary technicians often do not make more than minimum wage, though raises and contract negotiations are possibilities. Veterinary salary ranges drastically depending upon a number of factors though median salary is approximated at $70-90,000 yearly.
Whether or not you know for sure which path to follow or you're not quite decided, spend some time in a veterinary clinic. Work with all members of the veterinary team. Ask them questions - what are their days like? do they like their job? pros and cons? Experience the running of a clinic and observe the different positions. Questions? Feel free to reply to this post or message me, I’m always here to help.
44 notes
·
View notes
Text
So you want to be a veterinarian...
Ask a handful of children what they want to be when they grow up and there’s a good chance that someone will say veterinarian. It has long been a dream career of many animal lovers, but is it right for you?
I fall into the “it’s all I’ve ever wanted to be” category. For as long as I can remember I was telling my parents that I was going to be a veterinarian. Human medicine? No, thank you. While I thought I had a pretty good understanding of veterinary medicine before I started veterinary school, I soon realized I didn’t know it all. That being said, veterinary medicine is definitely the right career for me. This post will go over the process of becoming a veterinarian, and the pros and cons of the job.
How do I become a Veterinarian?
To become a veterinarian, you must attend veterinary school. In North America, these programs are typically four years long.
Pre-Veterinary School Depending on where you live, there are prerequisites you must complete before applying to veterinary school. Many programs require completion of a four year undergraduate degree, taking some specific required courses. Some schools only require 20 prerequisite undergraduate courses (two years) in order to apply. The admissions process is competitive so keeping competitive grades is advantageous, though a 4.0 is not necessary. Good, but not great, grades do not mean you’re immediately cast aside. There are other components to your application. Many applications include veterinary/animal experience and extra circulars. During high school and undergraduate you should participate in a variety of clubs and volunteer activities. This makes you a more well rounded applicant, and also can be quite enjoyable. Some examples: - volunteer at a veterinary clinic: I personally believe everyone should spend time in a veterinary clinic before applying to veterinary school, regardless of importance for application. This will allow you to see what the job actually involves. - volunteer at farms, wildlife clinics, SPCAs etc. - 4-H or similar. - Student government (leadership, communication). - Pre-vet society/club. - Any other club/society on campus, ie. biology society, GSA, yearbook etc. Some schools, especially in the USA, require letters of recommendation. The school may specify who they are looking for letters from (i.e. vet, professor, etc). Make sure you make positive connections with the people you work with in order to allow for a positive recommendation. Finally, standardized testing is required by most veterinary schools, specifically the GRE (Graduate Record Examination). More information about this can be found online.
As a Canadian student, you may only apply to your regional Canadian school, unless you would like to apply internationally. As an American student, you can apply to a large number of schools within your county. Research each school as many have specific areas of interest, different cost, different living style etc. After applying to veterinary school, many schools will then invite candidates for an interview. The type of interview varies depending on the school so make sure you look into the specifics of each school you will be interviewed at. Veterinary School I will give you specifics of my education as an example, though all veterinary schools differ. In general, be prepared for a lot of work. You will be taking many classes at once. For example, I was often taking 10 courses per semester. Many of these courses included a laboratory component. A large number of classes equates to a large amount of home preparation and studying. Midterm season at my school was typically weeks long. The work load is certainly manageable, don’t let that alone scare you off, though it does take a lot of dedication and planning. The most important piece of advice I have in regards to course load is to make sure you still find time for yourself. Without taking care of yourself and constantly studying, you will burnout. My school had three years of course work, followed by one year of clinical practice. During the three pre-clinical years, we did have exposure to animals throughout labs and shifts in the clinic. We first perform surgery in third year under supervision of the course doctors. For the most part, the pre-clinical years followed a pretty general schedule (other than surgery duties). Starting class at 8 and being done by 4. There are opportunities outside of courses to get involved with clinical/medical activities. Veterinary school have a large variety of clubs that may offer these extra opportunities - ie. pathology club necropsies, exotic animal club medical producers, internal medicine club cadaver labs... There may be opportunity with a local stray spay/neuter program through your school to get extra experience with surgery as well. Clinical year is a whole new ball game. At my school the year was broken into three week segments. Each segment you are placed somewhere new - i.e.. three weeks in the surgery department, three weeks in radiology, three weeks at an external clinic of your choosing... This year takes you away form the classroom and puts you into “doctor” mode. Keep in mind that each veterinary school operates on a different schedule (some introducing clinical earlier in the program) and that this is my personal experience. What your duties are will depend on the school as well. During my clinical year, student are involved in client communication, history taking, diagnostic planning, treatment administration, clinical skills, participation in surgery, etc. All under direct supervision. The hours for this portion of schooling are not predictable and definitely do not run 8-4. Many placements include after hours care of the patients, on-call work, lengthly paperwork, etc. All while studying for the dreaded NAVLE. Even though it was often dreadful, clinical year was my favourite year of veterinary school. Everything started to come together and honestly, it was a lot of fun.
NAVLE In North America, in order to practice veterinary medicine, you must past the licensing examination, the NAVLE. This is a 360 question multiple choice test that encompasses everything you have studied throughout veterinary school. Your school will help you apply and register when the time comes. You will technically be preparing for the NAVLE all of veterinary school but will specifically study for it in your final year. There are preparatory courses that you may purchase and your school may host review classes. The test is written in December and April.
So those are the cliff-notes of how to become a veterinarian. Feel free to reach out to me if you have any questions, would like clarification or would like me to go further into detail.
So after all of that, what are the pros and cons?
Lets not beat around the bush, starts with the cons:
Debt - veterinary school is NOT cheap and the income does not match the level of debt obtained. The majority of students will graduate with $100,000-$200,000+ in debt. This is not unmanageable, though it can be daunting.
Extensive training - veterinary school is not easy, and it is not for everyone. You will need to be knowledgeable about many species and many subjects.
Working with owners - “I want to be a vet because I don’t like people”, just no. This is a customer service career. You will speak to people every day. You will have to convince people to spend hundreds or thousands of dollars on their pets. You will get yelled at, told you’re in it for the money, probably threatened at some point.
Working within a budget - unlike human doctors, we really need to think about the cost of each and every thing we do. You will often have owners come in with $100 dollars to their name and a very sick animal, you need to figure out what the options are in each instance.
Euthanasia - many people find this one of the more difficult parts of the job. I personally believe it’s how you look at it. Euthanasia can be a wonderful gift. I do not euthanize healthy animals.
Work-place hazards - our patients can be aggressive and difficult to handle. This is often due to stress or being scared, but it is a danger to veterinary staff. You need to understand how to read signals and prevent dangerous situations from happening. Veterinarians are also exposed to chemicals, radiation, heavy lifting etc.
Hours - depending on where you work, the hours can be gruelling. Not everyone has the luxury of a 40 hour work week. We often stay late (for no extra pay) finishing cases, tending to patients, calling clients, doing paperwork, etc. Many veterinarians must perform on-call duties. This may lead to 2 hours of sleep between shifts.
Responsibility - every decision we make is life or death. The type of drug, the dose, surgery, etc. The job carries a huge amount of responsibility that can be very stressful for certain people.
Ok, so despite all of that, I’m still a veterinarian. I still love my job. Why?
Debt - yes, I have a huge amount of debt. Is it manageable, yes. There are many people in the world who have more debt than me. I hate that its becoming normal for people to have debt, but it is.
Extensive training - vet school sucked, but it was also awesome. I know so much about so many things. I’m proud of the level of knowledge I gained while in vet school. I’m proud of the person I have become through my extensive training.
Working with owners - the vast majority of my clients are absolutely wonderful. There are owners that light up my day, that I look forward to talking to, that remind me how much I love my job. We have many lovely reviews written about us, cards sent in, treats brought in for staff etc. For every person that gets mad at me for cost, there are many more that are understanding and work with me to find a solution within their budget
Working within a budget - this is a con no matter what way you look at it, though I can say that when you’re willing to work with owners and help them within their means, they are often very thankful. There are many cases you can help within a tight budget.
Euthanasia - I tell every owner that euthanasia is a gift. We get to take away pain and suffering. This makes it much easier for me to deal with this on a daily basis.
Work-place hazards - proper training and education can help minimize hazards. Low stress handling, proper restraint etc.
Hours - not every job has horrible hours. I work, on average 40 hours a week. Some days I stay a little late to finish up, but it usually doesn't bother me. Yes, I do on-call but it is not very often. I have a great work life balance. You need to take this into consideration when looking for a job.
Responsibility - you get to call the shots, you get to save lives, help pets, help owners. You do not have to do it alone. There are so many resources out there to help. It’s definitely scary and daunting the first few years out, but its also very satisfying. Confidence grows day by day.
You get to live you dream job.
You get to be a part of an amazing team that shares the same goals as you.
You get to impact the lives of so many people and their pets.
You get to be an ambassador of the animals.
You get to go to work and learn something new every single day.
So, still think veterinary medicine is for you? Reach for the stars <3
#veterinary medicine#veterinarian#vet#vetmed#vetblr#vet student#vet school#veterinary#veterinary school
54 notes
·
View notes
Text
Hello there followers!
What types of posts do you want to see more of? Any specific topics that youd like to see (medical, advice, etc)?
5 notes
·
View notes
Text
How to find a good External Rotation
Clinical year in Vet School is a very exciting time. There are many great opportunities to learn and expand upon your clinical skills. Many schools offer the opportunity to partake in external rotations, placements at clinics outside of your schools teaching hospital.
How do you find external rotations that are right for you?
1) Determine what your schools requirements are:
- do they require a certain number of doctors in the practice?
- how many weeks are allotted for externals?
- are there limitations to how many weeks can be spent at certain types of practices (general practice vs speciality)?
- what is required of the clinic that you do your placement at (paperwork, grading, etc)?
2) Determine what you're looking for:
- general practice vs speciality
- academic vs private practice
- referral and/or emergency
- types of species seen
- medicine and/or surgery
- level of involvement
3) See what's out there:
- determine if your school has a list of rotations that previous students have been on.
- talk to other veterinary students.
- look online for rotation/externship advertisements (various veterinary organizations may list opportunities).
- look at the internship matching program (many places that offer internships will host externs - this also allows you to see if you would be interested in their internship).
- search for clinics that offer what you're looking for (ie exotic speciality practice) and contact them to see if they host students.
4) Find out if your chosen clinic fits your plan (ie ask questions):
- contact the clinic, if they are willing to host students they will put you in touch with the appropriate contact person.
- do they meet all requirements set by your school?
- are they willing to grade you according to your schools requirements?
- ask questions pertaining to what you're looking for (type of clinic, type of animals, case load, emergency, referral etc)
- what level of involvement are they offering (participation in surgery, development of technical skills such as blood drawing, history taking, diagnostic planning, diagnostic interpretation, treatment planning)? Do you want to shadow, or do you want to be involved in clinical practice and decision making?
- what do they require of you as a student?
5) Make the most out of your time there:
- ask questions
- get involved
- offer to help
- even if the rotation isnt what you imagined it to be, do what you can to learn the most while you're there!
Feel free to ask any questions about choosing rotations and what to expect during your clinical year!
Good luck 😊
#veterinarian#veterinary#veterinary medicine#vetmed#vetblr#vet student#vet school#vetstudent#vetschool#veterinary school
21 notes
·
View notes
Text
Urolithiasis
Stones can be located anywhere along the urinary tract - nephrolith, ureterolith, urocystolith, urethrolith.
Signs of urolithiasis may include: - Abdominal pain - Abnormalities of urination (difficulty, frequency, blood) - Straining with the absence of urine (this is an emergency - obstruction) - Anorexia - Vomiting - Depression - Palpation of stone in empty bladder or urethra per rectum
Diagnostics:
Bloodwork If blockage may see post renal azotemia - increased K, P, BUN, creatinine.
Urinalysis Urinary tract inflammation - hematuria, pyuria, may see bacteriuria. Urine pH - struvite crystals precipitate in alkaline urine. Crystals - presence does not mean there are stones, absence does not mean there are not stones. Can be observed in normal individuals.
What is the relationship between stones and UTIs? Stones may lead to infection - mucosal damage, incomplete voiding, bacterial entrapment in stones. UTIs may lead to stones - urease producing bacteria can alkalinize urine.
Radiographs Stones only visible if >1mm in diameter. Generally radiopaque (visible on radiograph) - struvite and calcium oxalate. Asses bladder size - evidence of obstruction? Ultrasound is superior for detection as it detects all types of stones (urate, cystine, and calcium phosphate may not show up on radiograph).
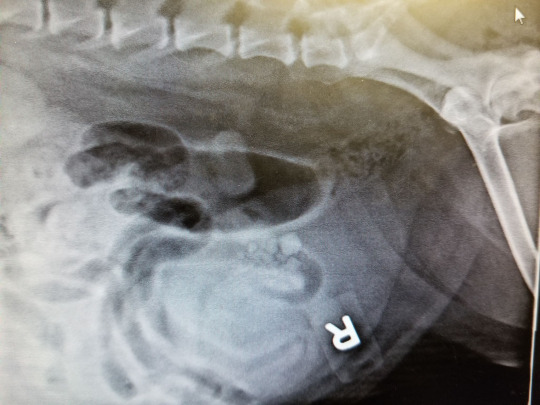
Above is a lateral view demonstrating stones within the bladder. A V/D was also obtained. Always take at least two views. This patient presented for increased frequency of small amounts of urine.
Types of stones:
Struvite Accounts for 50% of canine stones and 30% of feline stones. UTI may predispose to the formation through acidification of the urine.
Calcium Oxalate Accounts for 35% of canine stones and 50-70% of feline stones.
Urate Seen in dogs with portosystemic shunts - high excretion of ammonium biurate crystals. Seen in dalmations - defective hepatic transport of uric acid. My not show on radiographs - show up on ultrasound.
Cystine Inherited disorder - excessive elimination of cystine in the urine. Most commonly seen in male Dachshunds between age 3-6. Stones may show faintly on radiographs - show up on ultrasound.
Silicate Linked to consumption of large amounts of corn gluten and soybean hulls (high in silicates).
Treatment:
Treatment largely depends on the presentation of the patient. Medical management is not suitable for many patients (obstruction occurring or imminent, stone type not known, very large stones, sharp stones etc). If obstructed, emergency intervention is required.
Medical Management Calcium oxalate, urate, cystine, and silicate stones CAN NOT be dissolved and require surgical removal. Struvite stones can occasionally be dissolved with a special diet.
Surgical Treatment Stones may be removed surgically. Surgery varies depending upon the location of the stone. Bladder stones are removed via cystotomy which is often performed in general practice. Stones should be sent away for analysis to determine the appropriate steps moving forward (ie diet).

Above is an exposed bladder at the start of a cystotomy procedure. The patient was only passing small amounts of urine. Over 300ml of urine was removed from the bladder before an incision was able to be made.

Above is the same bladder after emptying the urine via cystocentesis, before incision.
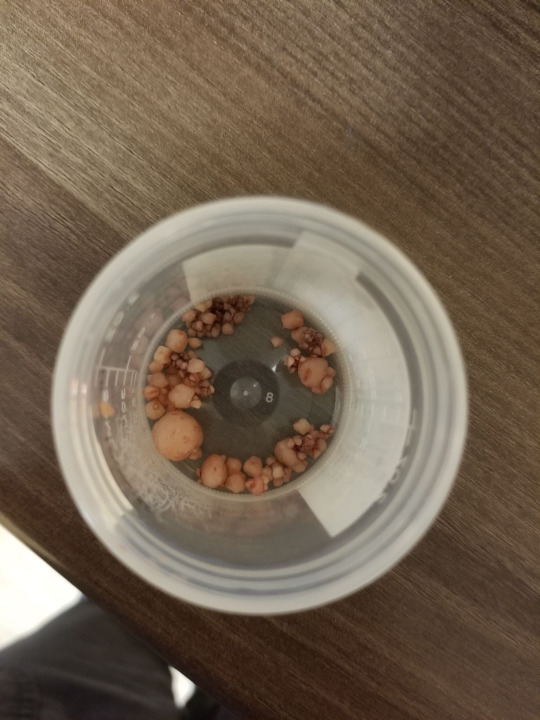
Above are the stones that were removed from the bladder and urethra. The largest stone pictured was located within the urethra, causing a partial obstruction. The stones were sent away for analysis.
Aftercare Many of these stones have a high occurrence rate. Prevention with the appropriate prescription diet is essential. Treatment of concurrent urinary tract infection is essential. Appropriate monitoring is helpful in guiding recommendations moving forward - ie follow up urinalysis.
16 notes
·
View notes
Text
Antibiotics - Metronidazole
Antibiotics are something used very frequently in veterinary medicine. Making the appropriate choice for the disease that you are treating is not only important for the patient, but also for anti-microbial stewardship. It is important to make responsible, educated choices when using antibiotics.
This series of posts will briefly review the families of antibiotics and some commonly used drugs within each family.
Metronidazole
Metabolized by anaerobic bacteria to produce a cytotoxic compound.
Spectrum: anaerobes and protozoa.
Wide distribution including bone, abscess, and central nervous system.
Adverse effects may include: neurotoxicity.
Prohibited by the FDA for use in food animals.
37 notes
·
View notes
Text
Antibiotics - Rifampin
Antibiotics are something used very frequently in veterinary medicine. Making the appropriate choice for the disease that you are treating is not only important for the patient, but also for anti-microbial stewardship. It is important to make responsible, educated choices when using antibiotics.
This series of posts will briefly review the families of antibiotics and some commonly used drugs within each family.
Rifampin
Functions by inhibiting DNA dependent RNA polymerase.
Spectrum: gram positives, some mycobacteria, some gram negatives, some anaerobes, and chlamydiae. Some antiviral and antifungal activity at higher concentrations.
Most commonly used in the treatment of Rhodococcus equi in horses.
Resistance develops rapidly.
Adverse effects may include: red/orange staining of secretions, hepatotoxicity in dogs.
17 notes
·
View notes
Text
Antibiotics - Macrolides and Lincosamides
Antibiotics are something used very frequently in veterinary medicine. Making the appropriate choice for the disease that you are treating is not only important for the patient, but also for anti-microbial stewardship. It is important to make responsible, educated choices when using antibiotics.
This series of posts will briefly review the families of antibiotics and some commonly used drugs within each family.
Macrolides and Lincosamides
Function by binding to the 50S ribosomal subunit. These drugs are bacteriostatic.
Macrolides - erythromycin, tylosin, tilmicosin.
Lincosamides - clindamycin. Spectrum - mainly gram positive, some gram negative (Pasteurella, mycoplasma). Clindamycin is also effective against toxoplasma, mycoplasma, anaerobes, and staph.
Adverse effects may include: potentially fatal diarrhea in horses/ruminants/rabbits, any injection of tilmicosin can be fatal in swine/horses/humans.
15 notes
·
View notes