Nirdosh Jagota is the Managing Partner at GRQ Biotech Advisors, bringing over 30 years of expertise in the biotech industry. Renowned for his strategic leadership, Nirdosh Jagota has been pivotal in the development, submission, and approval of more than 25 NDAs/BLAs/MAAs. Prior to his current role, Dr. Jagota held significant positions at global biotech giants like Amgen, Ocugen, Arcturus, and Merck. An alumnus of the Indian Institute of Technology and the University of Georgia, he's internationally recognized for his contributions to regulatory, quality, and compliance sectors.
Don't wanna be here? Send us removal request.
Text
How Biotechnology Is Shaping the Next Era of Global Public Health

Biotechnology is driving the next era of global public health by delivering faster diagnostics, scalable vaccines, precision surveillance, and sustainable disease control strategies.
This article gives you a practical executive-level view of how biotechnology is reshaping public health systems across regions. You’ll understand the technologies in use today, how they’re being deployed globally, and what decisions are required to ensure they scale equitably and effectively.
What vaccines is biotechnology bringing to public health?
Biotech-enabled vaccines are accelerating timelines and improving safety in disease prevention efforts.
You now have access to recombinant and mRNA vaccines that deliver targeted immunity. Recombinant hepatitis B vaccines use genetically engineered proteins to trigger an immune response, without exposing patients to the virus. mRNA vaccines instruct your cells to produce antigens, giving you fast, safe immunity with scalable production potential.
These platforms are modular and adaptable. You’re no longer constrained by traditional long-lead development timelines. Instead, you can respond to novel pathogens within weeks—an essential capability for public health response moving forward.
How are gene-edited insects reducing disease transmission?
Biotechnology enables precise vector control through engineered genetic traits in mosquito populations.
Gene-edited male Aedes aegypti mosquitoes, released by companies like Oxitec, carry self-limiting genes that prevent female offspring from surviving. These males mate in the wild, but their female progeny die before reaching maturity, reducing vector density without the environmental side effects of chemical insecticides.
Field deployments have demonstrated a reduction in local mosquito populations by over 90%. You now have a viable strategy to control dengue, Zika, and chikungunya in dense urban areas where traditional methods fall short.
How is biotech improving disease surveillance and diagnostics?
Advanced molecular tools and sequencing technologies allow you to detect pathogens early and accurately.
Next-generation sequencing (NGS) identifies infectious agents directly from clinical or environmental samples. Wastewater monitoring now detects viral RNA days before clinical cases spike. Paired with AI-based forecasting systems, you can build early-warning platforms that guide public health action before a crisis unfolds.
This real-time surveillance is scalable across borders. With regional labs equipped for molecular diagnostics, you’re no longer dependent on central systems. Local response becomes faster, more precise, and more coordinated.
Why is cold-chain biotech innovation critical?
Distribution of temperature-sensitive therapeutics remains one of your toughest infrastructure challenges in low-resource regions.
mRNA vaccines require sub-zero storage conditions, which often exceed local capacity. Ghana addressed this by deploying drone-based delivery with thermal-protected storage, enabling remote clinics to maintain vaccine potency during transport.
You now have models that solve cold-chain bottlenecks through drone logistics, phase-change materials, and container innovation. These tools ensure that biotech solutions reach patients without degradation—especially in tropical or remote geographies.
How does localized biomanufacturing support global health?
Biomanufacturing decentralizes medicine production and strengthens supply chain security.
Instead of relying solely on chemical synthesis and transnational logistics, you can establish modular bioreactors for regional production. This approach shortens delivery times, improves responsiveness during outbreaks, and mitigates geopolitical disruptions that delay supply.
Recent U.S. and European reports suggest that nearly 50% of essential pharmaceuticals could be produced via bioengineering. You’re no longer dependent on fragile or politicized pipelines to access treatments during surges or shortages.
Real-World Biotech Applications in Global Health
Recombinant hepatitis B vaccines prevent millions of liver-related deaths annually
Gene-edited mosquitoes suppress dengue outbreaks in pilot regions
Genomic wastewater surveillance detects early COVID, polio, and influenza clusters
AI-powered outbreak platforms like ENDAR identify engineered pathogens
Local biomanufacturing slashes drug wait times in Latin America and Sub-Saharan Africa
How does biotech help in antimicrobial resistance (AMR) mitigation?
Biotech enables precise drug targeting and accelerates new antibiotic development cycles.
Traditional broad-spectrum antibiotics disrupt microbiomes and accelerate resistance. You now have access to biotech-developed narrow-spectrum agents that target only the pathogen. Companies are also deploying phage therapy—engineered viruses that selectively destroy bacteria.
By incorporating genomics into drug selection, you can match the treatment to the pathogen with reduced collateral damage. That preserves antibiotic efficacy and reduces resistance emergence across large populations.
What are the adoption challenges for biotech in public health?
Barriers include regulatory lag, public skepticism, and inconsistent infrastructure.
Gene editing, synthetic biology, and AI-driven tools face complex review cycles. You must navigate international agreements like the Cartagena Protocol and local ethics boards. Public trust is another factor—especially when introducing genetically modified organisms or experimental therapies.
Scaling biotech in public health requires more than tools. It demands clear governance, transparent data sharing, local workforce development, and inclusive public education. You’ll need to build this foundation early to avoid resistance later.
How is biotechnology preparing the world for the next outbreak?
You now have layered capabilities that combine early detection, precision containment, and scalable response.
AI tools like ENDAR analyze airport air and sewer samples to detect synthetic pathogens. Regional platforms like AI4PEP in Latin America use genomic signals and public datasets to issue alerts. Vaccine platforms like mRNA enable you to produce immunizations in weeks once a pathogen is sequenced.
This speed gives you a strategic advantage. With smart surveillance and modular response systems in place, outbreaks can be neutralized before they become global emergencies.
What role does public engagement play in successful biotech deployment?
You must invest in communication, transparency, and local participation to gain support and ensure sustained impact.
Surveys show most populations support biotech when it’s linked to clear benefits, like cancer treatment or epidemic response. When engagement is lacking—such as with gene-modified insects—resistance grows quickly. You must inform communities, publish trial outcomes, and incorporate feedback early in the process.
Build coalitions with healthcare workers, local governments, and NGOs. Their trust and reach are critical to translating biotech innovation into measurable population health outcomes.
How Is Biotechnology Improving Global Public Health?
Rapid development of mRNA and recombinant vaccines
Genetically modified mosquitoes for disease vector control
Real-time diagnostics and outbreak surveillance
Localized biomanufacturing to secure drug access
In Conclusion
Biotechnology is no longer optional in public health—it’s essential. You now have scalable tools for vaccine delivery, vector control, outbreak surveillance, and drug development that outperform legacy methods. To succeed, you must lead with coordination, equity, and speed. The next decade of global health progress will be shaped by how well you mobilize biotechnology today.
"In my latest article, I break down how these tools are making healthcare more responsive and equitable across the globe. Learn more on my Crunchbase profile."
0 notes
Text
What Patients Need to Know About Precision Diagnostics
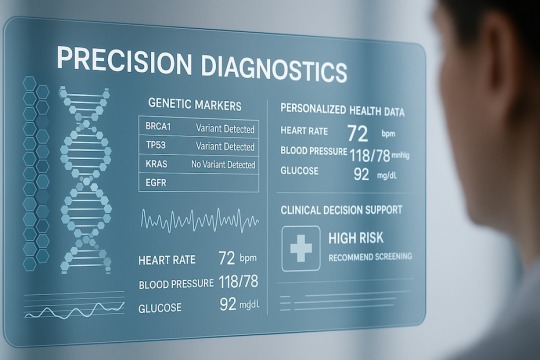
You need precision diagnostics because it provides targeted, accurate, and timely health information based on your unique genetic, molecular, and clinical profile.
This article gives you a practical, decision-ready understanding of what precision diagnostics means for your care. You'll learn how it works, what makes it different from conventional testing, and when it matters most for conditions like cancer, inherited risk, and early detection.
What is precision diagnostics?
Precision diagnostics identifies disease by analyzing biological details specific to you—your genes, proteins, cells, and clinical patterns.
Traditional testing looks for averages. This method tailors detection and treatment to the characteristics that define your individual health. Whether it's sequencing tumor DNA or assessing blood-borne biomarkers, it delivers information based on your biology—not assumptions.
Tools like next-generation sequencing (NGS), digital pathology, and biomarker mapping now power this shift. They're used across oncology, cardiology, and rare diseases to move beyond symptom matching toward individualized decision-making.
How does precision diagnostics improve disease detection?
It identifies disease earlier and with more accuracy—especially in high-risk or complex cases.
In oncology, NGS panels analyze mutations driving cancer growth. With this data, you’re more likely to receive treatments that directly address those mutations. Platforms like Oncomine Dx, approved by the FDA, give actionable results in under five days.
In infectious diseases, genomic sequencing pinpoints viral or bacterial strains within hours, avoiding broad-spectrum antibiotics and streamlining your care path. Even in chronic conditions, precision diagnostics reveals subtypes of disease—so you aren’t misdiagnosed or mismedicated.
Are precision diagnostics available for cancer?
Yes, and they’re a critical component of cancer care today.
Companion diagnostics are FDA-approved tests matched to specific cancer therapies. If you’re diagnosed with non-small-cell lung cancer, a test might reveal an EGFR mutation—qualifying you for a targeted drug like osimertinib. Without that data, you could be treated with ineffective or toxic alternatives.
Precision diagnostics also enable real-time monitoring. Liquid biopsies detect circulating tumor DNA, flagging relapse before imaging would. This gives you—and your care team—more time to act.
How accurate are genomic tests?
Genomic tests are highly accurate when run in clinical-grade labs and interpreted within context.
Lab-developed tests undergo rigorous validation. The error rate for NGS panels is generally below 1%, but no test is infallible. Variants of uncertain significance still appear, and low-abundance mutations may need re-testing.
That’s why your provider uses confirmatory tools like biopsies or imaging before clinical decisions. You should expect transparency from the lab and your physician regarding how your results are derived, what they mean, and where caution is needed.
Can precision diagnostics prevent disease?
They can help prevent or delay disease by identifying risks before symptoms appear.
If you carry a BRCA mutation, for instance, early screening protocols can catch cancer early or lead to preventive treatment. Genetic testing linked to inherited cardiac disorders allows you to modify activity levels, take medication, or avoid high-risk triggers.
Beyond inherited risks, diagnostic platforms track shifts in biomarkers. If inflammation markers begin rising or insulin sensitivity drops, early changes in diet, medication, or surveillance can make a measurable impact on outcomes.
Are liquid biopsies reliable?
Liquid biopsies are dependable in detecting circulating tumor DNA (ctDNA), especially for monitoring or when a traditional biopsy isn’t feasible.
They’re fast, less invasive, and ideal for repeat testing. For advanced cancer patients, these tests detect treatment resistance before symptoms return. However, sensitivity can drop in early-stage cancers where ctDNA is minimal.
That’s why you’ll see liquid biopsy results paired with imaging and standard pathology. Used together, they provide a more complete clinical picture without over-relying on a single method.
Should I get genomic testing for my family history?
Yes, if your family has a history of early-onset cancers, cardiac deaths, or inherited diseases.
You may be a candidate for proactive screening even if you're asymptomatic. A genetic panel can show whether you inherited risk mutations like BRCA, Lynch syndrome, or cardiomyopathy-linked genes. This helps your physician recommend changes in surveillance, medication, or lifestyle.
Some hospitals now integrate clinical genomics with patient care directly, offering risk-based screening at younger ages or modified treatment plans based on your hereditary profile.
What Should Patients Know About Precision Diagnostics?
Personalized results based on genes and biomarkers
Guides cancer, cardiac, and rare disease treatment
Enables prevention and early detection
Requires specialist interpretation and lab quality assurance
In Conclusion
Precision diagnostics brings medicine to a level where your care decisions are guided by data directly tied to your biology. Whether you’re confronting a diagnosis or assessing inherited risk, these tools deliver faster, more accurate answers. You don’t need to rely on generic protocols. With precision diagnostics, your treatment—and your future—can be based on measurable facts unique to you.
"In my latest article, I share how genomic tools and biomarker insights are helping patients get earlier, more accurate answers. Read more on my Behance."
0 notes
Text
From Lab to Clinic: How AI Is Fast-Tracking Drug Discovery

You’ve probably seen the headlines about how artificial intelligence is changing medicine, but if you work in pharma, biotech, or clinical research, you already know it’s not just headlines—it’s happening in real time. AI is compressing timelines, improving accuracy, and drastically reducing the cost of drug development. Instead of relying solely on traditional wet-lab experimentation, you're now able to run simulations, mine real-world datasets, and predict drug behavior before ever running a trial. This article walks you through how AI is shaving years off drug discovery, where it’s having the biggest impact, and what tools are already making their way from labs to clinics.
AI-Generated Molecules: No Guesswork, Just Precision
You’re no longer starting from scratch with drug discovery. Today, AI models like DeepMind’s AlphaFold and others from companies like Insilico Medicine are generating potential drug compounds by analyzing protein folding and predicting how molecules will interact with biological targets. These systems tap into vast chemical libraries and public data sources, offering millions of combinations—but without random guesswork. You're working with simulations that already suggest which compounds are most likely to succeed in binding, solubility, and safety, significantly cutting the hit-and-miss nature of early-stage research.
What used to take months of trial-and-error synthesis in a wet lab can now happen in days using virtual compound screening. These tools use generative algorithms to create novel molecules tailored to your specific parameters—receptor fit, blood-brain barrier penetration, even off-target toxicity predictions.
Spatial Biology and Transcriptomics: Deeper Than Microscopy
Spatial transcriptomics is another tool you’ve likely come across if you're working with precision therapies or oncology research. It’s giving you a new way to look at cells—not just by their shape or location, but by what genes they express in real-time. Tools like SOAR (Spatial Omics Analysis Resource) from Northwestern University allow you to overlay transcriptomics data over tissue samples like a geographic map.
This lets you identify how immune cells interact with tumor tissue, how diseases progress at a molecular level, and how drug candidates might behave inside the cellular environment. If you’re developing personalized treatments, this kind of resolution means more accurate targeting and fewer systemic side effects.
Predictive Toxicology: Fail Fast, Fix Faster
You’re probably familiar with how frustrating and expensive late-stage failures can be. Predictive toxicology tools are designed to help you avoid that. AI is now used to simulate how a new molecule may interact with human enzymes, liver tissue, or cardiac pathways—before you ever run an animal study.
Companies like Recursion and BenevolentAI use real-world clinical datasets and cellular images to train deep learning models that predict adverse reactions. With this information, you can deprioritize risky compounds early or tweak a molecule’s structure to mitigate known hazards.
By flagging red-light toxicity concerns upfront, AI helps you allocate resources where there’s real promise—without going down dead ends.
Repositioning Old Drugs: Data Never Forgets
Drug repurposing is no longer based on hunches or luck. With AI tools scanning decades of clinical data, EHRs, and molecular signatures, you can now uncover potential new uses for shelved or off-patent drugs. This approach significantly lowers development costs and regulatory hurdles, especially when the compound already has an established safety profile.
Platforms like BenevolentAI, which helped identify a rheumatoid arthritis drug as a COVID-19 candidate (without using guesswork), prove that data can breathe new life into older compounds. You’re able to take a compound sitting on the shelf and find a match with unmet needs in neurology, oncology, or rare diseases—driven by pattern recognition and not by manual review.
AI in Clinical Trials: Efficiency Without Compromise
One of your biggest bottlenecks is likely clinical trials—slow enrollment, protocol deviations, and high costs. AI is helping you redesign trials that are more adaptive and efficient. You can now use natural language processing to review prior trial protocols, machine learning to identify ideal patient cohorts, and predictive analytics to monitor trial integrity in real-time.
For instance, the collaboration between AstraZeneca and Nvidia uses AI to optimize trial site selection and simulate outcomes under multiple trial designs. You’re getting cleaner data, reduced dropout rates, and faster regulatory submissions.
Even more important, you're seeing AI personalize trial pathways—matching subpopulations of patients to specific treatment arms based on biomarkers, which boosts both safety and efficacy results.
Industry Adoption and Strategic Deals
You’re seeing serious momentum with big pharma betting heavily on AI. Sanofi’s partnership with BioMap and Exscientia, AstraZeneca’s deal with Absci, and Novartis’s use of AI to redesign clinical workflows all point to this shift becoming the norm, not the exception.
What makes these collaborations effective isn’t just the technology—they work because the AI teams understand your workflows, regulations, and expectations. These systems aren’t black boxes; they’re designed for transparency and regulatory review. That means you can audit models, trace decision logic, and make changes when needed.
Your role is evolving—from chemist or biologist to integrator of tools, platforms, and data streams. If you’re not using these tools yet, it’s not because they’re unproven—it’s because your team hasn’t fully streamlined them into your process. Yet.
Explainability, Regulation, and What Comes Next
Regulators are starting to adapt to AI workflows. The FDA has already approved AI-designed drugs for rare diseases in trial phases and encourages the use of AI in data cleaning and site monitoring. That gives you a green light—if your models are explainable and you maintain rigorous version control.
This is where explainable AI (XAI) becomes essential. You need to understand why a model prioritized one molecule over another, how it weighted certain biomarkers, and whether it will perform the same in future data inputs. With well-documented training data and input audit trails, AI tools can pass regulatory scrutiny and become permanent parts of your toolbox.
How is AI accelerating drug discovery?
AI creates drug molecules using predictive models
Identifies safe candidates before animal trials
Analyzes genomic, transcriptomic, and patient data
Speeds up clinical trial design and recruitment
Helps repurpose failed drugs using real-world evidence
In Conclusion
If you’re still viewing AI as a future consideration, you’re already behind. It’s now a core part of modern drug development—helping you design, test, and bring compounds to market faster and more affordably. The edge you gain isn’t just in speed—it’s in precision, scalability, and adaptability. With major players adopting these tools and regulators opening the door, the lab-to-clinic journey is no longer a marathon. With the right AI stack, you can make it a sprint—one that delivers real value to patients and a serious competitive advantage to your business.
"Thanks for reading! Interested in seeing more on how AI is revolutionizing the journey from lab to clinic, and other topics in biotechnology and healthcare? Visit Nirdosh Jagota's Pinterest profile for related content."
0 notes
Text
Could We One Day “Print” Human Organs?

You’ve probably heard whispers across the biomedical field: printing human organs isn’t just a theoretical possibility—it’s a serious scientific pursuit. As someone working in biotech, regenerative medicine, or advanced diagnostics, you know how persistent the shortage of donor organs remains and how much room there is to improve rejection outcomes. That’s where 3D bioprinting steps in. In this article, you’ll get a clear understanding of how bioinks and stem cells are laying the groundwork for printable organs, what kinds of tissues have already been successfully printed, the engineering hurdles to scaling up whole organ systems, and what you need to track if your work intersects with translational medicine, regulatory pipelines, or lab-grown therapeutic systems.
Bioinks: Your Starting Material for Living Tissues
You can’t build a functioning organ without the right printing material, and in your lab, that starts with bioink. You’ve likely worked with or studied formulations that combine hydrogels, extracellular matrix components, and live cells, sometimes even including growth factors or synthetic scaffolds. These bioinks allow you to print cells with spatial precision while supporting cell viability, proliferation, and differentiation. Whether you’re printing skin-like sheets or vascular tissues, the rheology and biocompatibility of your ink directly affect print fidelity and eventual tissue function.
Recent innovations have introduced self-healing bioinks, temperature-sensitive compositions, and even multi-material systems that let you integrate different cell types layer by layer. You’ve probably seen how this precision allows structural mimicry of complex tissues like kidney cortex or cardiac muscle. And while the tech is promising, bioinks still present challenges—especially when balancing stiffness and cell permeability for larger constructs.
Printing Functional Tissues: Skin, Vessels, and Cartilage
You’ve seen the headlines about researchers printing simple human tissues in controlled settings. Skin has become one of the earliest success stories—bioprinted skin can mimic both the dermis and epidermis layers and is already being used in burn repair research and cosmetic testing. If your focus is on wound healing, you’ve likely experimented with dermal scaffolds printed with fibroblasts and keratinocytes.
Blood vessels are another critical step forward. You understand that vascularization is key to ensuring larger tissues survive beyond a few millimeters in thickness. Many labs are now developing perfusable vascular networks using sacrificial inks or coaxial printing methods. And let’s not forget cartilage—its avascular nature makes it easier to print than organs, and bioprinted ear or nose structures are already in early-stage human trials. These milestones build confidence in scalability, pushing the field toward bigger, more complex builds.
The Liver, Kidney, and Heart Are the Next Targets
Moving from patches to full organ systems requires an entirely different level of design and coordination. You’re not just printing cells—you’re architecting functional units like nephrons, hepatic lobules, or myocardial layers. In liver bioprinting, you may have worked on spheroid-based models or tissue strips that produce albumin and perform basic detoxification. These constructs are now used in drug screening and disease modeling.
The kidney, though highly complex with millions of filtration units, is under active research. You may be testing bioprinted renal tubules that can mimic filtration in microfluidic systems. Cardiac bioprinting is also evolving. If you’re in cardiovascular research, you’ve probably seen lab-built patches that synchronize with heart rhythms or include electromechanical stimulation to maintain cell viability. Full organ replication still faces obstacles, but every layer printed brings you closer to transplant-grade constructs.
Vascularization: The Core Bottleneck
Here’s where your engineering mindset comes in—vascularization is the single biggest challenge you face when scaling up. Without a blood supply, any thick printed tissue will die quickly. To fix this, researchers like yourself are applying principles from fluid dynamics and biomaterials to print endothelial-lined channels or introduce sacrificial scaffolds that can later be flushed out.
You may have explored embedding angiogenic factors within layers or integrating pericytes to stabilize microvascular networks. The goal is to achieve spontaneous inosculation when the printed organ is implanted—meaning your printed vessels connect with the body’s own circulatory system. Until then, functional organ transplants at scale will remain out of reach.
3D Bioprinters: The Machines Behind the Vision
Let’s talk hardware. You’ve likely upgraded from a basic extrusion printer to a more specialized bioprinter capable of temperature control, multiple printheads, and real-time cell monitoring. Whether you’re using stereolithography, inkjet, or laser-assisted printing, your choice of printer affects resolution, speed, and cell survival.
Companies like CELLINK, Organovo, and Aspect Biosystems are leading providers in this space, and you may be using one of their platforms in your lab. Some of these devices now come equipped with AI-driven controls that adjust extrusion pressure or print paths in real time. If your work involves translational medicine, investing in GMP-compliant printers will also be critical down the line.
Safety, Rejection, and the Clinical Timeline
You’re aware that safety is where most bioprinting breakthroughs stall. Printing with patient-derived iPSCs (induced pluripotent stem cells) can reduce immune rejection, but ensuring that no mutations or functional abnormalities arise remains your responsibility. Before a printed heart or kidney can be implanted in humans, you’ll need to show long-term viability, mechanical strength, and regulatory compliance.
There’s also the challenge of standardization. You can print tissues that look similar from one trial to another, but ensuring they behave identically under physiological stress is where the field must advance. You’re already seeing efforts by regulatory bodies to classify bioprinted constructs as combination products—part device, part biologic—complicating the approval process further.
Real-Time Applications and What's Already in Use
You don’t have to wait for printed hearts to make a clinical difference. Today, you might be using bioprinted bone scaffolds in orthopedics, vascular grafts in bypass research, or skin models in toxicology studies. These early-stage products are already improving patient-specific therapies and speeding up testing pipelines.
Some of your colleagues are even using printed tumor models that better mimic the tumor microenvironment, leading to more accurate drug trials. If you’re in pharma or preclinical testing, this alone could reduce time-to-market for new treatments. You’re witnessing how bioprinting is reshaping adjacent fields even before organ transplantation becomes common.
Here’s what’s already possible with 3D bioprinting
Skin, cartilage, and blood vessels
Liver and heart tissue patches
Functional microvascular structures
Personalized tissue models for drug testing
In Conclusion
You’re no longer asking if human organs can be printed—you’re focused on how and when. The progress you’re witnessing, from viable bioinks and vascular engineering to liver strips and heart patches, confirms the potential. While full-sized transplantable organs are still years away, the building blocks are already in place. Your role—whether as a researcher, clinician, or biomedical engineer—is to help refine the technology, secure safety, and bring these life-saving innovations closer to patient bedsides.
"Thanks for reading! To explore additional insights on the cutting edge of regenerative medicine, bioprinting, and the future of organ transplantation, follow Nirdosh Jagota on X"
0 notes
Text
How mRNA Vaccines Are Changing the Future of Immunization

You’re witnessing a shift in immunization science that’s reshaping how we prepare for—and prevent—infectious diseases. At the heart of this shift is messenger RNA, or mRNA, a technology that allows for faster vaccine development, targeted disease prevention, and personalized medicine applications. Unlike traditional vaccines, which rely on weakened pathogens or proteins grown in labs, mRNA teaches your body to make its own defense. This article explores how mRNA vaccines work, their applications beyond infectious disease, and what this innovation means for your health and the future of global immunization strategies.
A Faster Way to Respond to Disease Threats
When new viruses emerge, time is your greatest challenge. Traditional vaccine production can take months or even years. With mRNA, scientists can develop a vaccine candidate within weeks. This speed comes from the ability to quickly design the genetic instructions that tell your cells how to make a harmless version of the virus's spike protein. Once your immune system sees this protein, it learns to defend against it without any exposure to the live virus.
The flexibility of mRNA platforms means you can adapt vaccines more quickly if a virus mutates or a new strain appears. The base production process stays the same, making updates faster and easier to scale. That agility is key to responding to seasonal changes in viruses like influenza, or to future public health emergencies.
Personalization in Cancer Treatment
You’re also seeing progress where mRNA is being used far beyond infectious diseases. One of the most promising areas is personalized cancer vaccines. Instead of a one-size-fits-all approach, these vaccines are designed for a single patient, based on the mutations found in their tumors. Scientists sequence the cancer’s DNA, identify the mutations that mark it as foreign, and then create an mRNA vaccine that tells your immune system how to target and destroy those specific cells.
This level of precision turns your immune system into a custom cancer-fighting tool. Early studies in melanoma and other hard-to-treat cancers show encouraging results, with some patients experiencing fewer relapses and longer periods of remission. If the technology continues to prove itself in larger trials, you may one day receive a personalized cancer vaccine as part of your treatment plan.
Combining Protection Into One Shot
You’ve probably gotten multiple shots for different viruses. But what if one vaccine could protect you from several diseases at once? mRNA technology makes that possible. Researchers are developing multivalent vaccines—formulas that include instructions for multiple pathogens. A combined mRNA flu and respiratory illness vaccine is already being tested. These next-generation vaccines could simplify your immunization schedule and offer stronger protection during respiratory illness seasons.
Combining targets into one injection also streamlines production and reduces waste. It’s a solution that works for busy clinics and underserved communities where access to repeated care visits may be limited.
Better Storage, Easier Distribution
One hurdle mRNA vaccines faced early on was storage. Some formulas had to be kept at extremely low temperatures, which made distribution a logistical headache. But improvements in lipid nanoparticles—the tiny delivery bubbles that protect the mRNA—are changing that. New versions of these vaccines can now be stored at regular refrigerator temperatures for longer periods, making it easier to transport them to areas with limited resources.
Better shelf stability means you can reach more people in remote or rural regions without compromising effectiveness. That’s a major step toward more equitable access to vaccines around the world, especially in countries with limited cold chain infrastructure.
Stronger, Longer-Lasting Protection
You may wonder how long mRNA vaccines last. Research is now focused on improving durability—making your immune system's response stronger and longer-lasting. Scientists are fine-tuning the RNA sequence and adjusting the lipid carriers to ensure more efficient delivery. The goal is to boost your immune response without needing frequent boosters.
This matters not just for infectious diseases, but for chronic infections like HIV or hepatitis C. If mRNA vaccines can be made to last longer, they could change how we manage long-term infectious threats and reduce the overall number of doses needed.
Addressing Global Health with Speed and Scale
The scalability of mRNA production is another major advantage. Once you have the base manufacturing setup, you can produce large quantities of vaccines in a short time. This becomes especially useful in outbreaks where millions of doses are needed fast. Because mRNA vaccines are synthesized rather than grown in eggs or cell cultures, they avoid many of the delays found in traditional vaccine production.
This technology also helps prepare for diseases that haven’t yet made headlines. Scientists are building mRNA vaccine libraries for viral families that have pandemic potential. If one of those viruses ever spreads rapidly, you’ll already have a blueprint to work from.
Collaboration Is Driving Innovation
Behind these advances is a global network of researchers, biotech firms, public health agencies, and funding partners. You’ve seen companies like Moderna and BioNTech partner with governments and universities to bring mRNA solutions to market. These collaborations accelerate research, testing, and distribution, often compressing timelines from years into months.
Because mRNA technology is platform-based, once it’s approved and tested for one disease, the same method can be applied to others. That means your next vaccine may already be in development, based on the success of an earlier one.
Key Advancements in mRNA Immunization
Accelerates vaccine development for new disease threats
Enables personalized treatments for cancer patients
Supports multivalent protection with single-dose vaccines
Improves storage and transport with stable formulations
Enhances immune response with improved delivery systems
Boosts production scalability for global coverage
Drives innovation through public-private partnerships
In Conclusion
You’re living through a shift in how vaccines are created, delivered, and used. With mRNA, immunization is faster, more flexible, and potentially more personal. From infectious disease to cancer and beyond, this technology is rewriting the rulebook for how you fight illness. By supporting continued research, strengthening supply systems, and ensuring fair access, you’re not just benefiting from this breakthrough—you’re part of the reason it moves forward.
For a deeper look into the future of vaccine innovation and the role of emerging biotech, visit Nirdosh Jagota’s Crunchbase profile. Explore his contributions to science, technology, and global health as mRNA and other tools continue transforming immunization and personalized care.
0 notes
Text
Can Biotech Solve the Global Food Crisis?

The pressure to feed the world is mounting, and your role in that equation is more significant than you might think. As global population figures edge toward 10 billion, the need for secure, nutritious, and abundant food sources is urgent. Traditional farming practices are no longer keeping pace, especially with climate shifts and dwindling resources. That’s where biotechnology steps in—not as a magic fix, but as a tool that can change how you produce, manage, and consume food. In this article, you’ll see how biotech helps increase yields, boost nutritional value, reduce waste, and offer new food sources—all backed by science and grounded in real-world applications.
Increasing Crop Yields Through Genetic Engineering
One of the most pressing problems in food production is yield loss caused by drought, pests, and poor soil. Genetic engineering helps tackle these problems by introducing traits that protect crops under stressful conditions. You’ve probably heard of drought-tolerant wheat like HB4. This variety has been approved in countries including Argentina and Australia, helping growers maintain productivity when water is scarce. Similar progress has been made with rice and maize that resist common pests without relying on heavy pesticide use.
These modified crops give you better results using fewer resources. With improved resistance to environmental stress, farmers can harvest more from the same land. That’s not just good for food output—it’s also better for managing land sustainably. You don’t need to plant more fields; you just need smarter seeds.
Nutrition Upgrades That Fight Hidden Hunger
Calories alone don’t solve malnutrition. Many people get enough to eat but still lack key nutrients. Biotech tools allow scientists to enhance the nutrient profile of crops you already rely on. One notable example is Golden Rice, a variety engineered to produce beta-carotene, which your body converts to vitamin A. In parts of the world where rice is a staple, this can help prevent childhood blindness and other health issues tied to vitamin A deficiency.
You’ll also find biofortified maize with higher protein content and iron-rich beans. These changes don’t require you to eat differently—they just improve the quality of your regular meals. For families in low-income regions, that difference could mean fewer illnesses and better development outcomes without changing cultural diets or habits.
More Output, Less Impact
One advantage of biotech is how it reduces dependence on chemical inputs. Traditional farming often requires frequent applications of herbicides, insecticides, and synthetic fertilizers. These can degrade soil health and contaminate water. When you use genetically modified crops that naturally resist pests or tolerate weed control, fewer chemical treatments are needed. This cuts down on runoff, lowers costs, and reduces harm to pollinators and wildlife.
You also have options like biofertilizers—microbial solutions that help plants absorb nutrients better. Unlike chemical fertilizers that may damage soil over time, these products support long-term soil health. That’s especially important in areas where overfarming has left the ground depleted.
Meat Without the Animal
Protein demand keeps growing, but traditional livestock farming strains land, water, and feed systems. Biotech offers an alternative through lab-grown meat. These products are made by culturing animal cells, which means you can enjoy meat without raising or slaughtering animals. The resource savings are impressive: less land, no antibiotics, and lower emissions.
Startups around the world are scaling this technology. Some even focus on producing human breast milk in labs to reduce reliance on dairy-based infant formulas. If you're concerned about sustainability, this is one of the most promising areas to watch. You may soon see these items in mainstream stores, offering high-protein options with a much lighter footprint.
Less Spoilage, Better Transport
Food loss isn't always about growing enough—it’s often about what goes to waste after harvest. Bruised, browning, or overripe fruits and vegetables are often discarded during shipping or at the store. Gene editing now allows you to slow this process. Take non-browning bananas or longer-lasting tomatoes. These tweaks don’t change the taste, but they make it easier to store, ship, and sell fresh produce without spoilage.
When more food stays fresh longer, fewer resources go to waste. And in countries where refrigeration is limited, these changes can be game-changing. You’re not just growing better—you’re making sure it arrives intact.
Data Meets Dirt: Precision Agriculture
Your smartphone helps you do just about everything—now it can help feed the world. When paired with biotech, digital tools give farmers real-time data about soil health, plant nutrition, and water use. Sensors track what your crops need and when, reducing guesswork. You can apply just the right amount of fertilizer or water, cutting waste and improving output.
These tools also help monitor diseases and pest outbreaks before they cause major damage. Early action means better protection for crops and fewer losses. You don’t need a massive operation to benefit either. Even small farms can use affordable sensors or mobile apps to make smarter decisions.
Growing Food in a Changing Climate
You’ve already seen how weather shifts are affecting crops. Unpredictable rainfall, longer dry spells, and hotter summers are becoming the norm. Biotechnology can help farmers adapt. Heat-tolerant beans, salt-resistant rice, and flood-resistant wheat are now in development or already on the market. These options help stabilize food supplies in regions where climate stress is pushing traditional methods to the brink.
This work isn’t limited to grains. Leafy greens, root vegetables, and even fruit crops are getting climate-ready upgrades. The goal is simple: make sure food grows where it’s needed, even if the conditions change.
The Role of Global Policy and Cooperation
All these biotech breakthroughs only matter if they reach the field. That’s where regulation and collaboration come in. Countries like China are fast-tracking approvals for genetically engineered crops to secure domestic food supply. Public-private partnerships are also expanding. In Africa and Asia, you’ll find researchers working with local governments to develop region-specific solutions for drought, pests, and nutrition.
Biotech firms don’t work in isolation. They rely on scientists, agronomists, supply chain experts, and farmers to bring ideas to life. When you build bridges between research and reality, technology doesn’t sit in a lab—it ends up feeding families.
Key Contributions of Biotech to the Global Food Crisis
Increases crop yields under harsh growing conditions
Enhances nutritional value in staple foods
Reduces pesticide and fertilizer dependency
Supports production of lab-grown meat alternatives
Extends shelf life to reduce food waste
Enables climate-adaptive agriculture through genetic traits
Empowers precision farming with real-time data tools
In Conclusion
Biotech won’t grow food for you, but it gives you better tools to do it. Whether you're feeding a city or running a small plot of land, you now have access to science that helps make farming smarter, safer, and more productive. The potential to ease the global food crisis lies not just in innovation, but in how you apply it. With the right choices and partnerships, you can help turn scientific breakthroughs into meals on the table—no matter where that table is.
For additional insights into how science and technology intersect with global food systems, visit my Golden profile.
0 notes
Text
6 New Biotech Therapies for Depression and Anxiety

You’ve probably seen the limitations of traditional antidepressants—slow response times, unpleasant side effects, and inconsistent results. That’s why newer biotech therapies are gaining traction. They offer faster relief, target different biological pathways, and often come with fewer drawbacks. In this article, you’ll walk through six breakthrough biotech approaches that are changing the way depression and anxiety are treated.
1. Psychedelic-Assisted Therapy is Earning Clinical Trust
Psychedelic compounds, once tied to underground use and counterculture, are now entering mainstream mental health treatment. When used in controlled environments with trained medical teams, these agents show powerful results in treating both depression and anxiety. Psilocybin, for instance, has demonstrated notable efficacy for patients who haven’t responded to conventional antidepressants.
You’re seeing research-backed use cases from companies like Compass Pathways and MAPS. The goal isn’t to promote recreational use but to harness controlled doses to help patients reframe negative thought loops. Psychedelics like LSD and MDMA are also being studied for generalized anxiety and PTSD. The FDA has already given "Breakthrough Therapy" designation to some of these trials—fast-tracking the path to broader approval.
2. Ketamine and Esketamine Are Speeding Up Relief
For patients who need rapid symptom control, ketamine and its derivative esketamine have changed the conversation. Unlike traditional treatments that may take weeks to show effects, these options can provide relief within hours. Clinics across the U.S. now offer ketamine infusions, and esketamine has been FDA-approved for treatment-resistant depression in the form of a nasal spray.
You may already be using Spravato (esketamine) in your practice under medical supervision. It’s shown to rapidly reduce suicidal ideation in patients with major depressive disorder. The mechanism here is different—it targets glutamate receptors, unlike SSRIs that work on serotonin pathways. This alternative pathway makes ketamine-based therapy valuable for patients who’ve cycled through multiple treatments with no success.
3. Neurostimulation Devices Are Going Mainstream
Non-invasive brain stimulation has shifted from experimental to accepted practice. Devices like transcranial magnetic stimulation (TMS) and newer technologies like Stanford’s SAINT protocol are setting new standards for neurotherapeutics. These treatments deliver targeted magnetic pulses to specific areas of the brain, helping to reset dysfunctional circuits associated with mood disorders.
You’re no longer limited to medication alone. TMS is now covered by many insurance providers and recommended for patients with medication-resistant depression. Newer devices, some even portable, make this type of care more accessible and customizable. These tools represent a significant leap in patient outcomes—especially when combined with therapy and lifestyle interventions.
4. Personalized Pharmacogenomics is Reshaping Prescriptions
You’ve likely had patients who didn’t respond well to standard medications. Now, thanks to pharmacogenomics, you can analyze a person’s genetic makeup to better predict which drugs will be most effective and least likely to cause side effects. Tests like GeneSight and others allow you to fine-tune treatment plans based on how a patient metabolizes medications.
Biotech firms are developing antidepressants and anxiolytics tailored to genetic profiles, reducing the guesswork that often slows progress. Instead of trial-and-error dosing, you can get a clear picture of how someone will respond to SSRIs, SNRIs, or atypical agents. This shift toward personalization isn’t just convenient—it’s dramatically improving long-term adherence and success rates.
5. Novel Small Molecule Drugs Offer Targeted Options
Beyond the usual suspects like SSRIs and benzodiazepines, a new generation of small molecule drugs is emerging. These include agents that target glutamate receptors, kappa opioid receptors, and other neurochemical systems tied directly to mood regulation. One promising example is REL-1017 (esmethadone), being tested for its ability to provide antidepressant effects without the addiction risk associated with opioids.
You're now seeing biotech firms focus on mechanisms that go beyond serotonin, often aiming to modulate stress hormones, inflammation, or even neural plasticity. These treatments could offer benefits for those with comorbid conditions, like chronic pain or neurodegenerative issues, which often complicate mental health treatment.
6. AI-Driven Drug Discovery is Accelerating Innovation
Artificial intelligence is changing how quickly you’ll see new mental health drugs come to market. Traditional drug development cycles can take a decade or more. But with AI, algorithms can analyze vast datasets—clinical trials, genomic information, patient outcomes—and suggest optimized compounds for testing.
Companies like Atomwise, Deep Genomics, and Exscientia are using machine learning to identify compounds that can modulate mood-related targets. For depression and anxiety, this means you’ll likely have access to better medications, designed more precisely and brought to clinical use faster than ever before. It’s also helping to repurpose existing drugs—identifying medications approved for other conditions that might offer unexpected mental health benefits.
Key Advantages of New Biotech Therapies
Faster symptom relief
Better patient-specific outcomes
Novel mechanisms beyond serotonin
Non-invasive treatment options
Reduced trial-and-error in prescriptions
Enhanced development speed using AI
In Conclusion
If you’re treating depression and anxiety today, the tools at your disposal are more diverse and promising than ever. Biotech isn’t just a buzzword—it’s fundamentally changing how you deliver care. Whether it’s a fast-acting nasal spray, a precision gene-based prescription, or a device that modulates brain activity, the future of mental health is already here. By staying current and open to these innovations, you can offer your patients new hope—and real relief.
For more insights into biotech innovations in mental health, follow Nirdosh Jagota. Stay informed about the future of depression and anxiety treatment.
0 notes
Text
How Biotech Is Unlocking the Secrets of the Brain

If you're working at the intersection of neuroscience and biotechnology, you already know that decoding the brain isn't science fiction—it's a race. You’re seeing biotech tools go from research concepts to clinical assets, helping you map circuits, diagnose conditions, and deliver therapies that reach deep into the nervous system. In this guide, I’ll walk you through how biotech is turning complex neurological questions into actionable data and life-changing interventions.
Brain Mapping Is No Longer Just Imaging
You’re not limited to traditional fMRI scans anymore. Tools like START (Single Transcriptome Assisted Rabies Tracing) are giving you a new way to map neural circuits with cellular precision. Instead of just watching where blood flows in the brain, you’re tracing which neurons talk to each other and what genes they express while doing it.
That level of detail means you can now build models of brain function that actually match the biology. This isn't just helpful for curiosity’s sake—it changes how you identify targets for neurological diseases. Whether you're exploring Parkinson’s or rare motor neuron conditions, mapping gives you the wiring diagram you’ve always needed.
AI Is Doing the Diagnostic Heavy Lifting
When you're evaluating EEGs or brain scans, speed matters. AI platforms like Ceribell's rapid EEG have transformed how quickly and accurately you can diagnose seizures and neurological events. Instead of hours of monitoring in a neuro ICU, you can deploy a wearable EEG and get meaningful readings within minutes.
That doesn’t just save time—it saves lives. Early intervention in epilepsy or stroke depends on catching the issue right when it happens. AI-driven diagnostics also free up your team to focus on treatment decisions instead of hours of manual interpretation.
Brain-Computer Interfaces Are Becoming Practical Tools
The idea of communicating directly with the brain used to feel theoretical. Now it’s becoming clinical. Companies like Precision Neuroscience are designing minimally invasive brain-computer interface implants that can record brain signals without deep surgical procedures.
If you're working with patients who have paralysis or ALS, BCIs offer the possibility of digital communication through thought alone. You’re also looking at applications for rehabilitation, cognitive support, and even prosthetic control. It’s a huge leap from theory to practice, and the fact that these tools are getting regulatory approval means they’re closer to bedside use than ever.
The Blood-Brain Barrier Is No Longer a Wall
One of the biggest roadblocks in treating brain diseases has always been getting therapeutics into the brain in the first place. The blood-brain barrier blocks most drugs from crossing over. But biotech is giving you workarounds—BioArctic, for example, is developing transporter technology that mimics the way nutrients naturally cross the barrier.
This isn’t a workaround in the crude sense—it’s precision engineering. You attach your drug payload to a molecule that the brain already recognizes and lets in. Once inside, your therapy gets to work on targets that were previously unreachable. That could change the game for Alzheimer’s and other neurodegenerative diseases.
AI Is Also Reinventing Drug Discovery for the Brain
Designing drugs for the brain is harder than for almost any other organ. There are too many unknowns. But that’s exactly where machine learning thrives. Startups like Verge Genomics are feeding AI models with genomic and clinical data to identify which genes are most relevant to diseases like ALS and Parkinson’s.
Once you know the right targets, you can run simulations to test compound libraries and narrow your focus before you ever touch a test tube. This trims years off your timeline and slashes costs. For any biotech startup working in the CNS space, it’s an edge you can’t ignore.
Wearables Are Making Brain Monitoring Continuous
Clinical-grade EEGs used to be something you only saw in hospitals. Now they’re going mobile. Devices from companies like BioSerenity let you monitor brain activity over days or weeks, capturing data that static hospital visits often miss.
If you’re managing patients with epilepsy, traumatic brain injuries, or sleep disorders, wearables let you collect real-world evidence in real-time. You’re not just getting occasional snapshots—you’re getting the full story, which helps you diagnose and personalize treatment far more effectively.
Biotech Is Tapping Into Neuroplasticity
You know that the brain can rewire itself, but until recently, we had no way to reliably guide that process. That’s changing. Delix Therapeutics is developing non-hallucinogenic psychoplastogens—molecules that promote neural growth and reorganization without inducing psychedelic effects.
That’s a big deal if you're trying to treat depression, PTSD, or even substance abuse disorders. You’re helping the brain form healthier pathways without relying on daily dosing or months of therapy. It’s a new class of medication that works with biology’s own adaptability.
Key Biotech Breakthroughs in Brain Research
AI EEGs speed up diagnosis of brain conditions
BCIs enable nonverbal communication for paralyzed patients
Brain mapping tools reveal cell-level circuits
Drug delivery tech crosses the blood-brain barrier
AI platforms design better neurological therapies
Wearables provide long-term neuro data
Psychoplastogens boost neuroplasticity safely
In Conclusion
Biotech isn’t just helping you understand the brain—it’s letting you interact with it in ways that weren’t possible a few years ago. Whether you're decoding neural circuits, delivering targeted treatments, or giving patients new tools to live independently, you're operating in a field where the pace of innovation is relentless. And that's the exciting part: you’re not just studying the brain anymore—you’re actively shaping how it's healed, supported, and understood.
For more insights into how biotech is transforming brain research, follow Nirdosh Jagota. Stay updated on the latest breakthroughs in neuroscience and innovation.
0 notes
Text
The Role of Biotech in Food Security and Nutrition

Food security isn’t just a buzzword where I work—it’s the daily problem we solve. Every time we map a gene sequence, field-test a drought-tolerant crop, or pilot biofortified seed varieties, we’re dealing with real-world hunger, nutritional gaps, and fragile supply chains. I’ve spent years in biotech labs and field collaborations focused on one goal: helping more people get the food they need, with the nutrients they’re missing, in the face of unpredictable climate and rising costs. Biotechnology gives us the tools to do that. It lets us breed faster, grow smarter, and deliver value at the cellular level. From pest-resistant cotton in India to iron-rich beans in East Africa, I’ve seen how this science shows up in people’s meals. Here’s what that work looks like behind the scenes—and why it matters.
We Use Genetic Modification to Maximize Output in Tough Conditions
I work with teams that design crop traits for specific regional stressors. Drought, salinity, pests—you name it. When we develop drought-tolerant maize, it's because farmers in sub-Saharan Africa can’t afford to lose another harvest. We’re not guessing which traits might help—we’re engineering the plant to hold on to moisture longer, produce more under less, and resist pests without constant chemical intervention.
These aren’t lab-bound ideas. They’re planted, harvested, and evaluated by growers working on plots where every square meter matters. Pest-resistant cotton, Bt brinjal (eggplant), and herbicide-tolerant soybeans are all commercialized products we’ve helped scale, not academic curiosities.
Yields aren’t just going up—they’re becoming more stable, which is just as important. A 10% bump in output is useful. But predictable harvests that don’t crash in heat waves or insect infestations? That’s what builds food security.
We Use Biofortification to Tackle Hidden Hunger
I’ve worked on vitamin A–enhanced rice projects, and I’ve seen how skeptical policymakers become strong supporters once the data hits. Golden Rice was one of the first biofortified crops I helped push toward regulatory review, and the science behind it changed how we design for nutrition.
In many low-income regions, food is available but dangerously low in essential nutrients. That's where biotech closes the gap. We’ve engineered cassava with higher zinc, maize with more lysine, and beans with higher iron content. These aren't food supplements; they’re staple crops redesigned to deliver what diets lack—directly through everyday meals.
We’ve learned to match our work to what people already eat. Changing dietary habits takes decades. Changing crop profiles can take a few growing seasons when the biotech pipeline works efficiently.
We Reduce Chemical Dependency with Smarter Crops
One of the most satisfying parts of biotech work is helping farmers cut their input costs. In projects we’ve run across Southeast Asia and Latin America, we’ve replaced multiple pesticide sprays per season with a single genetically engineered resistance trait.
That’s not just a cost saving. It reduces environmental exposure, protects non-target species, and keeps farm workers safer. Herbicide-tolerant crops also enable conservation tillage, which keeps soil intact and improves water retention—critical in arid and semi-arid zones where we’re working to stabilize yields.
We still run extensive field trials to test these benefits over time. But when I visit partner farms and see farmers using less spray and getting better crops, it’s a clear reminder that biotechnology isn’t just about better science—it’s about better farming.
We Extend Shelf Life and Reduce Food Loss with Gene Editing
I’ve worked on CRISPR-edited bananas that resist bruising and last longer post-harvest. Those traits don’t sound dramatic until you see the difference in truckload losses. In high-temperature regions, perishable crops often rot before they reach market—not because of quality, but because the supply chain is unforgiving.
By editing genes that control ethylene production (the ripening hormone), we’re slowing down spoilage without adding chemicals or refrigeration. Tomatoes, lettuce, and even leafy greens are getting shelf-life upgrades using similar techniques.
This reduces food waste not only at the consumer level, but across the transport and distribution chain. It’s biotech supporting efficiency, especially in places that lack cold storage infrastructure.
Food Safety and Public Confidence Depend on How We Communicate
Every time we bring a new crop forward, there’s a conversation about risk—and there should be. But those conversations have to be driven by science, not fear. That’s why I sit in on regulatory reviews, public outreach sessions, and technical Q&As with local governments.
We share everything—gene sequences, trial data, allergen profiles, environmental impact assessments—because transparency earns trust. And once communities understand that these crops aren’t strange or dangerous, but carefully tested and targeted tools, the resistance fades.
Food security doesn’t just come from better seeds. It comes from public confidence that those seeds are safe, beneficial, and responsibly managed.
Policy Determines Whether Good Science Reaches Farmers
I’ve worked in regions where the science was ready, but the politics weren’t. That delay costs time, investment, and—frankly—lives. When biotech crops are stuck in regulatory bottlenecks, it slows adoption and leaves vulnerable communities with fewer options.
On the flip side, I’ve seen what happens when policy supports the science. China’s recent move to approve gene-edited crops is going to open the door for massive yield gains in rice and soy. Brazil’s flexible regulatory system has helped launch some of the most successful biotech crop portfolios in the world.
As developers, we can only take things so far. Governments have to meet us halfway with science-based policies that allow innovation to scale safely and fairly.
How Biotech Supports Global Nutrition
Boosts yields – Through drought, pest, and disease resistance
Enhances nutrients – With biofortified crops targeting deficiencies
Reduces waste – With longer-lasting fruits and vegetables
Lowers input needs – By cutting pesticide and fertilizer use
Adapts to climate – By building resilience into crop genetics
Innovation Only Matters if It Reaches the Plate
Biotechnology isn't just about improving crops. It’s about connecting lab innovation to the dinner table—especially where nutrition and access are most at risk. Every project I support—whether it’s a gene-edited rice variety or a vitamin-rich legume—is tied to real problems we’re solving with farmers, governments, and food producers on the ground.
What makes this work powerful is its reach. A single biotech breakthrough doesn’t just change a seed. It changes a harvest, a diet, and a future. And when we get it right—scientifically, ethically, and collaboratively—those changes feed millions.
Biotechnology isn’t just about smarter crops; it’s about smarter solutions to global hunger and nutrition challenges. For more insights on how science meets the real world, visit Tumblr.
0 notes
Text
9 Ways Synthetic Biology Is Reshaping the Food Industry

Synthetic biology is rapidly reshaping how we produce, process, and even think about food. It’s more than a buzzword—it’s a set of tools I use every day to design biological systems for real-world applications. By programming microbes, reengineering crops, and cultivating new proteins, we’re rewriting the rules of the food supply. This isn’t hypothetical or decades away; it’s happening in production facilities, labs, and market shelves right now. From lab-grown meat to biodegradable packaging, synthetic biology is quietly solving some of the biggest problems in agriculture, nutrition, and sustainability. In this article, I’ll walk you through nine specific ways synthetic biology is changing the food industry in ways that matter—efficiently, directly, and often without anyone noticing.
1. Lab-Grown Meats: Protein Without the Pasture
Cell-cultured meat is one of the clearest examples of synthetic biology in action. We start by isolating animal cells—usually muscle stem cells—and feed them a mix of nutrients in a controlled environment. These cells grow and form tissues just like they would inside an animal. What comes out looks and tastes like meat because, at a molecular level, it is meat—without the animal.
The result is a supply chain that skips feedlots, antibiotics, and slaughterhouses. It also uses far less water and land. Companies like Aleph Farms are developing structured cuts like steak, not just ground meat. We’re also optimizing the growth media, reducing costs and improving texture. Regulatory approval is moving forward in several countries, and production facilities are being built to scale. The work now focuses on consistency, efficiency, and public perception. It’s meat made smarter, not sacrificed.
2. Precision Fermentation: Dairy Reimagined
Milk without cows sounds strange until you realize it’s just a matter of protein. Using synthetic biology, we program yeast or fungi to produce casein and whey—the proteins that give dairy its structure and texture. Once filtered and purified, they’re combined with plant-based fats and sugars to create milk, cheese, or ice cream.
Companies like Perfect Day and Imagindairy are leading this charge. These products are molecularly identical to traditional dairy but don’t trigger lactose intolerance or require grazing land. Fermentation tanks can run year-round, anywhere in the world. It’s reliable, clean, and adaptable. By changing how microbes are fed or modified, we can enhance the flavor, add vitamins, or remove allergens. This is dairy that works for more people and for the planet.
3. Resilient Crops for Tough Conditions
Climate unpredictability is stressing our food systems. Using synthetic biology, we’re building crops that can handle more and waste less. By adjusting plant genomes, we can improve drought resistance, reduce browning, and increase shelf life. These edits don’t introduce foreign genes but optimize what’s already there.
Bananas that don’t brown as quickly are already in development. This kind of trait extends supply chain stability and reduces food loss. We’re also working on rice that emits less methane and tomatoes that can resist common viral infections. Every edit saves time, money, or resources. The ultimate goal is to grow more food with fewer inputs—and do it consistently in unpredictable environments.
4. Microbial Sweeteners: Sugar Without the Field
Sugarcane and corn are resource-intensive, and alternative sweeteners like stevia don’t scale easily. Synthetic biology gives us a third option. By modifying microbes, we can produce the exact sweet-tasting molecules found in stevia or monk fruit—without ever growing the plants. These microbes go through precision fermentation, and the resulting product is filtered and used in beverages, snacks, and desserts.
This method drastically reduces water and land use while offering more stable pricing and supply. The flavor is clean, and the calorie count stays low. As demand for sugar alternatives grows, especially in health-conscious markets, these synthetic solutions offer reliability and scale traditional agriculture can’t match. This is sweetener production that fits inside a lab, not across hundreds of acres.
5. Flavor and Fragrance Biosynthesis
The food industry runs on flavor. Synthetic biology now lets us produce signature flavor molecules—like vanilla, citrus oils, or meat aromas—using microbes. Instead of relying on seasonal crops or animal by-products, we design fermentation pathways to generate these compounds reliably, year-round.
This biosynthesis is already being used for vanilla flavoring without vanilla beans, saffron alternatives without the flower, and smoky notes used in plant-based meat. It cuts costs, stabilizes supply chains, and allows brands to explore new tastes faster. It also avoids the complexity of synthetic chemicals that turn off health-conscious consumers. Flavor is no longer limited by geography or harvest—it’s made with precision.
6. Nutrient Fortification Made Smarter
Feeding people isn’t just about calories—it’s about nutrition. Synthetic biology lets us design microorganisms that generate essential vitamins, minerals, or amino acids. These can be added to foods directly or produced during fermentation. For instance, bioengineered yeast can produce vitamin B12 for vegan-friendly applications, or iron compounds that don’t affect taste or texture.
We’re also seeing development of omega-3 fatty acids from algae, removing the need for fish oil. This kind of enhancement is especially useful in regions with poor dietary diversity. Rather than relying on external supplements, food can be fortified at the point of production. The nutrition gets baked in, not bolted on.
7. Biodegradable Packaging from Microbial Materials
Food packaging is a massive source of waste. Synthetic biology is giving us alternatives to petroleum-based plastics through engineered bacteria that produce biopolymers. These polymers, like PHA (polyhydroxyalkanoates), can be shaped into containers, films, or coatings. Once discarded, they break down naturally under composting conditions.
This kind of packaging is already being tested by food brands looking to meet sustainability goals. The performance is strong enough for cold storage, moisture resistance, and single-use serviceware. With the right incentives, it could replace millions of tons of plastic annually. Instead of polluting oceans or landfills, this packaging returns to the soil.
8. Biosensors for Food Safety
Keeping food safe is one of the most important parts of the supply chain. Synthetic biology is being used to build biosensors—tiny detection systems made from biological parts—that can spot pathogens, toxins, or spoilage in real time. These can be applied to packaging, embedded in storage systems, or used at inspection points.
Some sensors change color when bacteria like E. coli are present. Others fluoresce under certain light if spoilage enzymes are detected. These tools make quality control faster, cheaper, and more accurate. Instead of pulling whole batches off the shelf after a recall, producers can pinpoint the problem instantly. Safer food, less waste.
9. New Protein Sources Beyond Soy and Pea
Plant-based meat alternatives are everywhere, but soy and pea aren’t the end of the story. Synthetic biology is helping explore other protein sources—from fungi to algae to insects. These organisms are engineered to grow faster, taste better, and meet specific nutritional goals. Mycoproteins are already in commercial use, with more advanced versions in development that mimic everything from fish to eggs.
These proteins offer a smaller footprint, high digestibility, and a wide range of uses. With genetic tuning, we can eliminate allergens, increase essential amino acids, or improve absorption. They’re built for performance, not just imitation. For consumers, that means more choice, better quality, and cleaner labels.
How Synthetic Biology Is Changing Food
Lab-grown meat
Animal-free dairy
Climate-resilient crops
Microbial sweeteners
Biosynthesized flavors
Nutrient fortification
Biodegradable packaging
Food safety biosensors
Engineered alternative proteins
In Conclusion
Synthetic biology is no longer confined to research labs. It’s already reshaping how food is grown, made, packaged, and protected. The changes are often invisible to the average consumer, but they’re real, measurable, and already scaling. From protein production to packaging waste, this technology is giving the food industry new tools to solve persistent problems. The future of food isn’t just about what we eat—it’s about how intelligently we produce it.
From lab-grown meat to smarter packaging, synthetic biology is scaling quietly but fast.Stay connected with my Mystrikingly for more on where biotech meets real-world impact.
0 notes
Text
The Future of Organ Transplants: Growing Human Organs in Animals

The demand for organ transplants far exceeds the available supply, leaving countless patients on waiting lists with no guarantee of receiving a life-saving organ in time. I’ve spent years following advancements in transplantation medicine, and one of the most promising breakthroughs is the ability to grow human-compatible organs inside animals. This approach, known as xenotransplantation, could eliminate donor shortages and provide a scalable solution to organ failure. By combining stem cell research, genetic engineering, and advanced cloning techniques, scientists are making remarkable progress in developing transplant-ready organs inside pigs and other animal hosts. While this technology is still in development, the progress being made suggests that organ transplants may soon become more accessible, reliable, and safer than ever before.
How Xenotransplantation Works
Growing human organs in animals isn’t just about transplanting an organ from one species to another—it’s about engineering those organs to be biologically compatible with human recipients. I’ve followed research that uses genetically modified pigs as hosts for growing human organs, largely because their anatomy closely resembles that of humans.
The process starts with gene editing. Scientists use tools like CRISPR to remove pig genes that could trigger an immune response in humans while inserting human genes that promote compatibility. Once this is done, human stem cells are injected into pig embryos, where they integrate into the developing organ structures. Over time, these organs mature, carrying human-like characteristics that make them suitable for transplantation. The goal is to create kidneys, hearts, livers, and even pancreases that the human body will accept with minimal risk of rejection.
Recent Breakthroughs in Growing Human Organs in Animals
Not long ago, the idea of growing a human organ inside an animal seemed far-fetched. But recent experiments have proven that this approach is more than just theoretical. I’ve seen research where human stem cells were successfully incorporated into pig embryos, leading to early-stage kidney formation. While these kidneys weren’t fully functional, they showed human-like cell development, marking a significant milestone.
Another major breakthrough came when a genetically modified pig heart was transplanted into a human patient. Though the procedure was experimental, it provided critical data on how well a pig-grown organ could function in a human body. Scientists are now refining these techniques to improve long-term viability and reduce immune rejection. With ongoing research, we are moving closer to growing fully functional human organs in animal hosts.
Gene Editing is Making Organs More Compatible
One of the biggest obstacles in transplantation is immune rejection. The human body is designed to attack anything it perceives as foreign, and that includes animal-grown organs. I’ve seen how gene editing is helping to solve this problem. By modifying pig DNA, researchers can remove proteins that trigger immune rejection and introduce human genes that make the transplanted organ look more familiar to the recipient’s body.
A major concern has been the presence of porcine endogenous retroviruses (PERVs) in pig DNA, which could pose a risk if transmitted to humans. Researchers have used CRISPR to deactivate these viruses, making pig-grown organs safer for transplantation. Each advancement in genetic engineering brings us closer to overcoming the barriers that have traditionally made xenotransplantation risky.
The Potential Impact on Organ Shortages
If xenotransplantation becomes a mainstream medical practice, it could completely change how organ transplants are managed. I’ve worked with patients who spent years waiting for a kidney or a heart, with no guarantee that a match would come in time. A system where organs could be grown on demand would eliminate the uncertainty that currently plagues transplant medicine.
With human-compatible organs being developed in pigs, the need for living or deceased donors would decrease significantly. Instead of waiting for an organ to become available, a patient could receive a genetically matched organ when needed. This could reduce mortality rates and cut down on the complications associated with long-term organ failure and dialysis.
Challenges That Still Need to Be Addressed
Despite the promising developments, several challenges still need to be overcome before xenotransplantation becomes a viable medical option. Immune rejection remains a major hurdle. Even with gene editing, the body may still recognize the organ as foreign and launch an attack. Scientists are working on improved immunosuppressive therapies to prevent this, but long-term safety is still being studied.
There is also the question of ethical concerns. The use of genetically modified animals for organ production raises moral questions, and public acceptance of this technology remains uncertain. Regulations will need to be established to ensure that the practice is conducted ethically and with minimal risks.
Another challenge is perfecting the functionality of these organs. While researchers have successfully grown early-stage kidneys, livers, and hearts inside animals, they are not yet fully developed or capable of sustaining human life. Further research is needed to ensure that these organs can function at the same level as human-donated organs.
How Growing Human Organs in Animals is Changing Transplants
Xenotransplantation: Growing human-compatible organs inside animals for transplantation.
Genetic Engineering: CRISPR modifies pig DNA to reduce immune rejection.
Successful Trials: Early-stage human kidneys have been grown in pigs.
Organ Availability: Could eliminate donor shortages and long wait times.
Challenges: Immune rejection and ethical concerns still need to be addressed.
What the Future Holds for Organ Transplants
Growing human organs in animals is no longer just a theoretical concept—it’s an emerging reality that could transform medicine. With each breakthrough, we move closer to solving one of the biggest challenges in healthcare. The ability to produce genetically matched, readily available organs would mean that fewer patients die waiting for transplants. The road ahead still presents scientific and ethical challenges, but if these issues can be addressed, xenotransplantation has the potential to revolutionize organ transplantation, providing hope for millions of patients worldwide.
"For more insights on groundbreaking advancements in organ transplantation and regenerative medicine, visit my profile on Blogspot."
0 notes
Text
How AI is Pioneering Breakthroughs in Tissue Engineering and Regenerative Medicine
Tissue engineering has always been full of promise, but turning that promise into reality has been a slow process. AI is changing that. I’ve seen firsthand how machine learning is accelerating biomaterial design, optimizing cell culture conditions, and making regenerative medicine more personalized. AI’s ability to analyze complex biological data at a speed no human could match is pushing the field forward, allowing us to create better scaffolds, improve clinical translation, and refine imaging techniques. What once took years of trial and error is now being streamlined, opening the door to engineered tissues that integrate seamlessly into the human body. This isn’t just a theoretical shift—it’s happening in labs and clinics right now, shaping the future of medicine.
AI is Redesigning Biomaterials for Better Tissue Growth
One of the biggest challenges in tissue engineering has always been selecting the right biomaterials. The materials used in scaffolds need to mimic the body’s extracellular matrix while supporting cell attachment and growth. Before AI, this was a painstaking process of trial and error. Now, AI-driven models analyze thousands of biomaterial compositions in a fraction of the time, predicting how they’ll perform in real biological environments.
I’ve worked with teams using AI to design polymer-based scaffolds that enhance tissue regeneration while maintaining structural integrity. These models take into account factors like porosity, mechanical strength, and degradation rates, ensuring that the materials we select provide the best outcomes. With AI guiding the way, we’re developing biomaterials that are more biocompatible, durable, and effective at supporting cell growth.
AI is Optimizing Cell Culture Conditions for Faster Growth
Growing lab-based tissues that function like real human tissues is no small feat. Cells are incredibly sensitive to their environment—slight changes in temperature, pH, or nutrient levels can make or break an experiment. AI is now helping to fine-tune these conditions with an unmatched level of precision.
By analyzing historical data from past cell culture experiments, machine learning models can determine the best growth conditions for specific cell types. AI can even predict how cells will react to changes in their environment, allowing for real-time adjustments. The result? Faster-growing, more functional tissues that behave just as they would inside the human body. This level of control is making tissue engineering more predictable, scalable, and ready for clinical applications.
AI is Making Regenerative Medicine More Personalized
One of the most exciting developments in AI-driven tissue engineering is its role in personalized medicine. Instead of using a one-size-fits-all approach, AI allows us to tailor regenerative therapies to the unique biology of each patient.
For conditions like osteoarthritis, AI can analyze a patient’s genetic data and medical history to predict how their body will respond to different biomaterials. This allows us to design customized tissue scaffolds that integrate more effectively with their existing cells, reducing rejection risks and improving outcomes. The goal is to make regenerative medicine as individualized as possible, ensuring that treatments are optimized for each person rather than relying on generalized models.
AI is Transforming Scaffold Design and Fabrication
Scaffolds are the backbone of tissue engineering—they provide the structure that cells need to grow and form functional tissues. But designing scaffolds that mimic the complexity of human tissue has always been difficult. AI-driven modeling tools are now changing that, allowing us to create intricate structures optimized for cell adhesion, nutrient flow, and mechanical strength.
AI-powered 3D printing techniques have been particularly groundbreaking. By feeding machine learning models with data on different scaffold materials and designs, we can now print structures with micron-level precision. This has allowed us to produce scaffolds that closely resemble natural tissues, improving the chances of successful implantation and regeneration. The ability to rapidly prototype and refine designs has cut development time dramatically, making lab-grown tissues more viable for clinical use.
AI is Accelerating Clinical Translation
One of the biggest hurdles in tissue engineering has always been translating lab discoveries into real-world treatments. Many promising therapies never make it past clinical trials due to unforeseen complications or regulatory barriers. AI is helping us bridge that gap.
By analyzing past clinical trial data, AI can predict which tissue engineering products are most likely to succeed. It can flag potential safety concerns, suggest modifications before human trials even begin, and streamline regulatory approval processes. AI is also being used to track long-term patient outcomes, giving us real-time feedback on how engineered tissues integrate with the body. This allows for continuous refinement of our techniques, ensuring that new therapies are both safe and effective.
AI is Improving Imaging and Diagnostics in Tissue Engineering
Once engineered tissues are implanted, monitoring their integration and function is critical. AI-driven imaging analysis is making this process far more precise. Instead of relying solely on human interpretation of MRI and CT scans, AI can detect subtle changes in tissue structure that may indicate successful integration or potential issues.
These AI models can also track the regeneration process over time, helping us understand how different scaffolds and biomaterials perform in the long run. This data is invaluable—it allows us to continuously improve our designs and ensure that engineered tissues function as intended. With AI’s ability to process and interpret vast amounts of imaging data, we’re getting a clearer picture of how regenerative treatments behave in real-world conditions.
How AI is Transforming Tissue Engineering
Biomaterial Design: AI predicts the best scaffold compositions.
Cell Culture Optimization: AI fine-tunes conditions for better cell growth.
Personalized Medicine: AI customizes regenerative treatments for patients.
Scaffold Fabrication: AI enhances 3D printing for tissue engineering.
Clinical Translation: AI improves approval processes for new therapies.
Imaging and Diagnostics: AI enhances monitoring of tissue regeneration.
In Conclusion
Tissue engineering and regenerative medicine are undergoing a massive transformation thanks to AI. From selecting biomaterials to optimizing cell culture conditions and creating personalized treatments, AI is accelerating progress in ways we never thought possible. It’s also making clinical translation more efficient, ensuring that these advancements move beyond research labs and into real-world medical applications. The integration of AI into regenerative medicine isn’t just a trend—it’s a fundamental shift that’s shaping the future of healthcare. As research continues, AI will only become more embedded in the process, refining our techniques and making once-unattainable treatments a reality.
"For more insights on how AI is revolutionizing tissue engineering and regenerative medicine, visit my profile on WordPress."
0 notes
Text
The Science Behind Immunotherapy: The Biotech Revolution in Cancer Treatment

The immune system is a remarkable defense mechanism designed to protect the body against threats. Yet, cancer often finds ways to bypass this system, allowing it to grow and spread unchecked. Immunotherapy has changed this reality by enabling the immune system to identify and destroy cancer cells effectively. This innovative approach leverages the body’s natural defenses, offering an alternative to traditional treatments like chemotherapy and radiation. By enhancing the immune system’s ability to recognize cancer, immunotherapy has become a powerful tool in the fight against this disease. In this article, I’ll explore how immunotherapy works, its types, recent advancements, and its impact on cancer treatment.
What Is Immunotherapy?
Immunotherapy uses biological methods to empower the immune system in its fight against cancer. Unlike treatments that directly attack cancer cells, immunotherapy strengthens or modifies immune responses to target tumors more effectively. It works by either boosting the activity of immune cells or providing artificial components, such as antibodies, to aid in the destruction of cancer cells. This method has shown success in treating various cancers, including melanoma, lung, and bladder cancers. By focusing on the immune system, immunotherapy provides a targeted approach that often reduces the side effects associated with traditional therapies.
Key Types of Immunotherapy
Several types of immunotherapy have been developed to tackle cancer in unique ways. Checkpoint inhibitors, for example, are designed to remove the brakes on the immune system. Cancer cells often exploit immune checkpoints—proteins that regulate immune activity—to evade detection. Drugs like pembrolizumab and nivolumab block these checkpoints, allowing T cells to attack cancer cells more aggressively. Another groundbreaking approach is CAR T-cell therapy, which involves modifying a patient’s T cells to recognize and destroy cancer. This personalized treatment has shown remarkable success in blood cancers like leukemia and lymphoma.
Monoclonal antibodies are another vital tool in the immunotherapy arsenal. These lab-engineered molecules bind to specific antigens on cancer cells, marking them for destruction by the immune system. Some monoclonal antibodies also deliver toxic substances directly to tumors, enhancing their effectiveness. Cancer vaccines represent yet another innovative approach, training the immune system to identify and attack specific cancer-associated antigens. Recent advancements in mRNA technology have significantly improved the development of these vaccines, making them more precise and effective.
How Immunotherapy Works
Immunotherapy addresses cancer’s ability to evade the immune system by enhancing the immune response in several ways. One key strategy is enhancing immune recognition, which involves exposing hidden cancer cells to immune surveillance. Tumors often disguise themselves to avoid detection, but immunotherapies can unmask these cells, prompting an immune response. Another critical mechanism involves modifying the tumor microenvironment. Tumors create an environment that suppresses immune activity, making it difficult for T cells to infiltrate and attack. Immunotherapy can alter this environment, making it more supportive of immune cell activity.
Checkpoint inhibitors, in particular, play a vital role by blocking proteins that deactivate T cells prematurely. This allows the immune system to sustain its attack on cancer cells without interruption. These combined mechanisms demonstrate the multifaceted ways in which immunotherapy enhances the body’s ability to fight cancer.
Recent Advances in Immunotherapy
The field of immunotherapy has seen rapid progress in recent years, driven by technological advancements. One of the most exciting developments is the integration of CRISPR technology with immunotherapy. CRISPR allows scientists to edit genes within T cells, enhancing their ability to target cancer cells more effectively. Early trials using CRISPR-modified T cells have shown promising results, paving the way for more precise and personalized treatments.
Combination therapies are another area of significant advancement. Researchers have found that combining immunotherapy with other treatments, such as chemotherapy or targeted therapy, can improve outcomes by addressing multiple pathways simultaneously. Personalized cancer vaccines are also gaining traction, with advancements in tumor profiling enabling the creation of vaccines tailored to individual patients. These innovations are helping to expand the reach and effectiveness of immunotherapy.
Benefits of Immunotherapy
Immunotherapy offers several distinct advantages over traditional cancer treatments. Its targeted nature ensures that only cancer cells are attacked, sparing healthy tissue and reducing side effects. This contrasts with chemotherapy and radiation, which can harm healthy cells and lead to significant complications. Additionally, immunotherapy has the potential to provide durable responses. Some patients experience long-term remission, with their immune systems continuing to protect against cancer even after treatment ends. The reduced side effects associated with immunotherapy make it a more tolerable option for many patients, improving their quality of life during treatment.
Challenges and Considerations
Despite its promise, immunotherapy is not without challenges. One of the most significant issues is variable effectiveness. Not all patients respond to immunotherapy, and researchers are still working to identify biomarkers that can predict response rates. Another challenge is the risk of immune-related side effects. Overactivation of the immune system can lead to inflammation or autoimmune-like symptoms, which require careful management. The cost of immunotherapy treatments also remains a barrier for many patients, highlighting the need for strategies to reduce expenses and expand accessibility. Addressing these challenges will be critical to ensuring that immunotherapy reaches its full potential.
Key Immunotherapy Techniques
Checkpoint inhibitors block proteins that suppress immune activity.
CAR T-cell therapy reprograms T cells to target cancer.
Monoclonal antibodies mark cancer cells for destruction.
Cancer vaccines teach the immune system to attack tumors.
The Future of Immunotherapy
Looking ahead, the potential of immunotherapy continues to grow. Advances in artificial intelligence and machine learning are helping researchers identify biomarkers that predict patient responses, enabling more personalized treatments. The use of CRISPR technology is likely to expand, offering even more precise ways to engineer immune cells for cancer therapy. Additionally, ongoing research aims to apply immunotherapy to cancers that have been resistant to treatment, broadening its scope. Combining immunotherapy with other emerging technologies, such as nanotechnology, could further enhance its effectiveness. As research progresses, immunotherapy is set to become a cornerstone of cancer care.
In Conclusion
Immunotherapy has redefined cancer treatment by harnessing the power of the immune system to target and destroy cancer cells. With its tailored approach, long-lasting effects, and reduced side effects, it has become an invaluable tool in oncology. Advancements in technology and personalized medicine are driving its evolution, offering new hope to patients worldwide. As we continue to explore and refine this biotech innovation, immunotherapy stands as a testament to the power of science in transforming lives.
0 notes
Text
Can Biotech Save Endangered Species? The Role of Conservation Genomics

The rapid loss of biodiversity is a pressing global concern. Species are disappearing at an unprecedented rate, largely driven by habitat destruction, climate change, and human activities. In response, biotechnology, particularly conservation genomics, is emerging as a powerful tool to combat extinction and protect endangered species. Conservation genomics leverages advanced genomic technologies to analyze and utilize the genetic information of species, enabling targeted efforts to safeguard biodiversity. This article explores how biotechnology is transforming conservation strategies, its challenges, and the potential it holds for the future of endangered species.
Understanding Conservation Genomics
Conservation genomics involves studying the genetic material of species to inform conservation strategies. By examining DNA sequences, scientists can assess genetic diversity, identify populations at risk, and develop interventions to address threats. This approach is vital because genetic diversity underpins a species' ability to adapt to changing environments and resist diseases.
For example, researchers studying endangered species like the cheetah have found alarmingly low genetic diversity due to historical population bottlenecks. Conservation genomics helps pinpoint such vulnerabilities, allowing targeted efforts to mitigate the risks associated with inbreeding and genetic uniformity.
Genetic Diversity and Its Role in Survival
Genetic diversity is the foundation of a species' resilience. Populations with higher genetic variability are better equipped to adapt to environmental changes and new challenges like emerging diseases. Conservation genomics identifies genes linked to adaptability, enabling scientists to prioritize populations or individuals with desirable traits for breeding programs.
For instance, genetic analysis of coral species has revealed specific genetic markers associated with heat tolerance. By identifying and propagating corals with these traits, researchers aim to restore coral reefs more resilient to rising ocean temperatures. This work underscores the critical role of genetics in developing species' ability to survive environmental stressors.
Applications of Biotechnology in Conservation
Genetic Rescue
Genetic rescue is a biotechnology application designed to introduce new genetic material into small, isolated populations. This process reduces the risks of inbreeding and enhances genetic diversity. For example, genetic rescue has been used to revitalize populations of the Florida panther, a subspecies of cougar, by introducing genetic material from closely related cougar populations.
Cloning Endangered Species
Cloning is another promising technology in conservation. Scientists have successfully cloned endangered species like the black-footed ferret using preserved genetic material from deceased individuals. These efforts aim to increase population size and genetic diversity. While still in its early stages, cloning holds immense potential for restoring species that are on the brink of extinction.
Gene Editing
Gene editing tools, particularly CRISPR-Cas9, are opening new possibilities for conservation. By editing specific genes, scientists can enhance traits like disease resistance or adaptability. For instance, researchers are exploring how gene editing might be used to help amphibians combat the chytrid fungus, a pathogen decimating amphibian populations worldwide.
De-extinction
De-extinction, or the resurrection of extinct species, is a controversial yet fascinating application of biotechnology. Using advanced genomic techniques, scientists aim to bring back species like the woolly mammoth. While the ethical and ecological implications are debated, de-extinction research contributes valuable insights into genetic engineering and its potential applications for conservation.
Overcoming Challenges in Conservation Genomics
While the potential of conservation genomics is immense, several challenges must be addressed for these technologies to reach their full potential.
Data Availability
Many endangered species lack comprehensive genetic data, which is crucial for effective conservation genomics. Collecting and analyzing genetic information requires significant resources, which are often scarce in conservation efforts. Expanding genomic databases and improving access to these resources is essential for progress.
Ethical Concerns
The use of advanced biotechnologies in conservation raises ethical questions. For instance, cloning and gene editing involve manipulating life at a fundamental level, prompting debates about the potential unintended consequences. Ensuring that these technologies are used responsibly and transparently is critical to maintaining public trust and ethical integrity.
Technical Limitations
Although gene editing and cloning have made significant strides, these technologies are not without limitations. Success rates for cloning are still low, and unintended off-target effects in gene editing remain a concern. Continued research and technological advancements are needed to refine these methods and make them more reliable.
The Role of Biotechnology in Habitat Restoration
Conservation genomics is not limited to individual species; it also plays a vital role in ecosystem and habitat restoration. By analyzing the genetic composition of entire ecosystems, scientists can understand how different species interact and depend on one another. This knowledge helps guide restoration efforts that prioritize the recovery of keystone species and maintain ecological balance.
For example, genetic studies of soil microbial communities are helping restore degraded ecosystems. These microorganisms play a crucial role in nutrient cycling and plant growth. By reintroducing microbial species with beneficial traits, researchers are improving soil health and promoting vegetation recovery in areas affected by deforestation or agriculture.
Key Roles of Biotechnology in Conservation
Conservation genomics analyzes DNA to protect endangered species.
Genetic rescue boosts diversity in small populations.
Cloning revives endangered species and enhances genetic diversity.
Gene editing combats diseases and enhances adaptability.
Ecosystem restoration uses genetic data to rebuild habitats.
Future Directions for Conservation Genomics
The future of conservation genomics lies in integrating emerging technologies with traditional conservation practices. Advancements in machine learning and artificial intelligence are enhancing the analysis of genomic data, making it easier to identify patterns and predict outcomes. These tools are particularly useful for studying large, complex datasets generated by genomic research.
Additionally, interdisciplinary collaboration is key. Conservation genomics benefits from partnerships between geneticists, ecologists, and conservation practitioners. By working together, these experts can develop strategies that combine cutting-edge technology with practical conservation efforts.
Another exciting avenue is the use of citizen science and community engagement. Public participation in data collection and monitoring can expand the reach of conservation projects while fostering a greater appreciation for biodiversity among local communities.
In Conclusion
Biotechnology, through conservation genomics, offers innovative solutions to some of the most pressing challenges facing endangered species. By enhancing genetic diversity, mitigating extinction risks, and supporting habitat restoration, these technologies are reshaping conservation strategies. While challenges like ethical considerations and resource limitations persist, ongoing research and collaboration hold immense promise for the future. Embracing these tools could be a game-changer in preserving biodiversity and ensuring a thriving planet for generations to come.
0 notes
Text
Microbial Fuel Cells: Generating Clean Energy with Biotechnology

Microbial fuel cells (MFCs) are a remarkable innovation that brings together microbiology and technology to create clean, renewable energy. These systems generate electricity by utilizing the natural metabolic processes of microorganisms. MFCs are a promising solution for energy generation and hold potential for wastewater treatment and environmental restoration. Over the years, the progress in MFC technology has shown how sustainable energy and biotechnology can come together to address some of the world’s pressing challenges. This article explores the inner workings of microbial fuel cells, their applications, advantages, challenges, and future prospects.
What Are Microbial Fuel Cells?
At their core, microbial fuel cells are bio-electrochemical devices that convert chemical energy stored in organic matter into electrical energy through the activity of bacteria. These systems rely on microorganisms to break down organic material, releasing electrons as a byproduct of their metabolic activity. These electrons are then captured and directed to generate an electric current. The process involves an anode chamber where bacteria metabolize organic matter in an anaerobic environment, releasing electrons and protons. The electrons are transferred through an external circuit to the cathode, generating electricity, while protons pass through a proton exchange membrane to complete the reaction.
MFCs effectively mimic natural processes to transform waste into energy. By harnessing bacteria to process organic materials, they provide a sustainable and eco-friendly energy source. Their versatility allows for a wide range of applications, including energy generation, pollution management, and water purification.
How Microbial Fuel Cells Work
Microbial fuel cells rely on a few key components that work together to enable electricity generation. The first is the anode chamber, where microorganisms break down organic matter in an oxygen-free environment. This chamber is crucial because it fosters the growth and activity of bacteria that release electrons during their metabolic processes. These electrons travel through an external circuit, creating a flow of electricity before reaching the cathode.
The cathode chamber is where the final step of the reaction takes place. Here, electrons, protons, and oxygen come together, usually forming water as the end product. The separation between the anode and cathode chambers is maintained by a proton exchange membrane, which selectively allows protons to pass through while keeping the chambers chemically distinct. This design is essential for maintaining anaerobic conditions in the anode chamber and ensuring the system operates efficiently.
Applications of Microbial Fuel Cells
Microbial fuel cells offer a variety of applications, making them a versatile tool in both environmental management and energy production. One of their most notable uses is in wastewater treatment. By integrating MFCs into treatment facilities, organic pollutants can be broken down while simultaneously generating electricity, providing a dual benefit. This approach reduces the energy costs associated with traditional wastewater treatment methods while addressing environmental concerns.
Another significant application is bioremediation. MFCs can be used to clean up environments contaminated with hydrocarbons, heavy metals, or other pollutants. The bacteria in these systems are capable of breaking down harmful substances, contributing to the restoration of ecosystems. Additionally, MFCs are being explored in desalination, where they assist in removing salt from seawater. This offers an energy-efficient method for producing freshwater in areas facing water scarcity.
In addition to these applications, MFCs serve as biosensors. They can detect microbial activity or the presence of specific pollutants in water or soil. These sensors provide real-time data that can be critical for environmental monitoring and decision-making.
Advantages of Microbial Fuel Cells
The advantages of microbial fuel cells make them an attractive solution for clean energy and environmental management. One of their most notable benefits is the ability to generate renewable energy. Unlike fossil fuels, MFCs rely on organic materials as their energy source, reducing dependency on non-renewable resources and lowering greenhouse gas emissions.
MFCs also contribute to waste reduction. By converting organic waste into electricity, they address two significant issues simultaneously: energy generation and waste management. This makes them particularly valuable in industries that produce large amounts of organic waste, such as agriculture and food processing.
Another advantage is their environmental friendliness. MFCs produce minimal emissions and often contribute to environmental restoration efforts. For instance, when used in wastewater treatment, they clean the water and produce energy as a byproduct. Furthermore, their scalability allows them to be adapted for various applications, from small-scale biosensors to large industrial systems.
Challenges Facing Microbial Fuel Cells
Despite their potential, microbial fuel cells face several challenges that limit their widespread adoption. One of the primary issues is their relatively low power output. Compared to conventional energy sources, MFCs generate significantly less electricity, making them unsuitable for applications requiring high energy demands.
The cost of materials is another hurdle. The components of MFCs, including electrodes and membranes, are often made from expensive materials that increase the overall system cost. This presents a significant barrier to large-scale implementation, especially in resource-limited settings.
Scalability is another area where MFCs face difficulties. While they work effectively in small, controlled environments, scaling them up for industrial applications poses technical and economic challenges. The microbial efficiency, which is influenced by environmental conditions and the type of bacteria used, also affects the performance and reliability of these systems.
Future Prospects for Microbial Fuel Cells
The future of microbial fuel cells looks promising, with ongoing research and innovation aimed at addressing current limitations. Researchers are exploring cost-effective alternatives to traditional electrode materials and developing more efficient microbial communities to enhance performance. Advancements in system design, such as stacked MFCs, offer the potential to increase power output and scalability.
Integrating MFCs with other renewable energy technologies, such as solar and wind, could further expand their applications. For instance, hybrid systems could be developed to combine the strengths of multiple energy sources, making them suitable for diverse environments and needs. Additionally, expanding the use of MFCs in remote areas and off-grid communities could provide sustainable energy solutions where traditional infrastructure is unavailable.
Key Applications of Microbial Fuel Cells
Wastewater treatment: Break down pollutants while generating electricity.
Bioremediation: Clean up contaminants like heavy metals and hydrocarbons.
Desalination: Remove salt from seawater efficiently.
Biosensing: Detect pollutants and monitor microbial activities in real-time.
In Conclusion
Microbial fuel cells are a groundbreaking innovation at the intersection of biotechnology and sustainable energy. They hold immense potential not just for clean energy generation but also for addressing critical environmental challenges like waste management and pollution. While challenges such as low power output and scalability remain, ongoing research continues to refine and enhance these systems. With their ability to transform organic waste into electricity, MFCs exemplify the power of harnessing biology for technological solutions. By continuing to innovate and integrate this technology, we can move closer to a future where energy is clean, renewable, and accessible for all.
0 notes
Text
From Lab to Farm: The Science Behind GMO Crops

Genetically Modified Organisms (GMOs) have transformed modern agriculture, offering solutions to critical challenges such as food security, climate change, and pest management. As someone who has closely observed the development and application of GMO technology, I can say that this science is a fascinating mix of precision, innovation, and rigorous testing. To truly appreciate the impact of GMO crops, it’s essential to understand the step-by-step process that brings them from the lab to the farm.
Identifying Beneficial Traits
The journey of a GMO crop begins with identifying the traits that would benefit agriculture or consumer health. These traits could include pest resistance, drought tolerance, enhanced nutritional content, or even longer shelf life. Scientists often look to nature for inspiration, seeking traits in other plants, bacteria, or organisms that could address specific challenges.
One well-known example is the development of Bt crops. Scientists identified a bacterium, Bacillus thuringiensis (Bt), which naturally produces a protein toxic to certain insects. This trait was highly desirable for crops like corn and cotton, as it would protect them from pests without the need for chemical pesticides.
Isolating and Cloning the Gene
Once the desired trait is identified, the next step is isolating the gene responsible for that trait. Using advanced molecular biology techniques, scientists extract the gene from its natural source, whether it’s a bacterium, plant, or other organism.
To ensure there’s enough genetic material for experimentation, the isolated gene is cloned—or copied multiple times. This is done using polymerase chain reaction (PCR) technology, a method that amplifies small DNA sequences. With the gene ready, scientists can proceed to the next stage of development.
Inserting the Gene into the Plant Genome
The next step is integrating the cloned gene into the DNA of the target crop. There are several techniques for achieving this, each carefully designed to ensure the gene is incorporated precisely.
One common method uses a soil bacterium called Agrobacterium tumefaciens, which has a natural ability to transfer genetic material into plants. Scientists modify this bacterium to carry the desired gene, which it then delivers into the plant cells. Another technique involves a gene gun, which shoots microscopic particles coated with DNA into plant tissues.
Regardless of the method, the goal is the same: to enable the plant to express the new trait, such as producing a protein that makes it resistant to pests or tolerant to herbicides.
Growing and Testing the Modified Plant
After the genetic modification, the plant is grown in controlled environments such as greenhouses. This stage is crucial for determining whether the plant expresses the desired trait effectively and without unintended side effects.
Scientists monitor various aspects, including growth rate, resistance to pests or diseases, and overall health. They also test the plant’s interactions with its environment to ensure it doesn’t negatively impact other organisms. If the results are promising, the modified plant moves on to small-scale field trials, where it is cultivated under natural conditions to evaluate its performance further.
Rigorous Regulatory Review and Approval
Before GMO crops can be released to farmers, they undergo a rigorous regulatory review process to ensure they are safe for human consumption, animals, and the environment. In the United States, three main agencies oversee this process:
The U.S. Department of Agriculture (USDA): Ensures that GMO crops do not pose risks to other plants or the ecosystem.
The Environmental Protection Agency (EPA): Evaluates the safety of GMOs that produce pesticides, ensuring they don’t harm non-target organisms.
The Food and Drug Administration (FDA): Reviews the safety of GMO crops for human and animal consumption, focusing on nutritional content and potential allergens.
These agencies conduct extensive tests, including allergenicity assessments, toxicity evaluations, and environmental impact studies. Only after passing these stringent checks can a GMO crop be approved for commercial use.
Breeding with High-Performance Varieties
Once a GMO crop is approved, it is often bred with elite, high-yielding non-GMO varieties. This ensures that the final product combines the benefits of genetic modification—such as pest resistance or drought tolerance—with desirable agricultural traits like high productivity, adaptability, and disease resistance.
This breeding process involves traditional methods where the genetically modified plant is crossbred with existing high-performing varieties. The resulting seeds are then tested to ensure they retain the desired traits and perform well in different farming conditions.
Commercial Production and Continuous Monitoring
The final stage is the commercial production of GMO crops, where farmers cultivate them on a large scale. Even after reaching the farm, GMO crops are subject to continuous monitoring to ensure they perform as expected and that no unforeseen issues arise.
This includes tracking crop yields, pest resistance levels, and environmental interactions. Post-market surveillance also helps researchers and regulators understand the long-term impacts of GMO cultivation on ecosystems and food systems.
Key Steps in Developing GMO Crops
Identify traits like pest resistance or drought tolerance.
Isolate and clone the target gene.
Insert the gene into the plant’s DNA.
Grow and test the modified plant.
Complete regulatory safety reviews.
Crossbreed with high-yield varieties.
Begin commercial production with ongoing monitoring.
In Conclusion
The journey of GMO crops from the lab to the farm is a testament to the power of science and innovation. This meticulous process involves identifying beneficial traits, engineering plants with precision, and ensuring rigorous safety testing at every step. The result is crops that improve agricultural productivity and address critical challenges like food security, environmental sustainability, and resource efficiency.
By understanding the science behind GMO crops, we can appreciate their potential to revolutionize agriculture and support a growing global population. With continued research and responsible application, GMO technology holds the promise of a more resilient and sustainable future for farming.
0 notes
Text
The Power of Synthetic Biology: Building Life from Scratch
Synthetic biology is a field that merges biology with engineering to design and construct new biological parts, systems, and organisms. Unlike traditional genetic engineering, which typically modifies existing genes, synthetic biology allows us to construct biological components from the ground up. With synthetic biology, we can engineer microorganisms to perform specific tasks, such as producing biofuels or breaking down pollutants, or even create custom organisms with entirely new functions. In this article, I’ll explain how synthetic biology works, where it’s being applied, and the implications of building life at the molecular level.
What is Synthetic Biology?
At its core, synthetic biology involves designing and building new biological systems. By reprogramming the genetic code within cells, we can control their behavior and make them perform tasks they wouldn’t naturally do. This process often involves assembling DNA sequences to create synthetic genes, which are then inserted into organisms to direct their functions. With synthetic biology, we can go beyond the limitations of natural biology and create organisms with precisely defined purposes.
The field of synthetic biology relies on advancements in gene editing and bioengineering, enabling scientists to manipulate DNA with high accuracy. For example, techniques like CRISPR-Cas9 allow us to cut and paste genes within the genome, while DNA synthesis allows us to create custom DNA strands in the lab. These tools have opened up possibilities for creating biological systems with functions that are useful in medicine, agriculture, and environmental science.
Applications of Synthetic Biology in Medicine
In medicine, synthetic biology is unlocking new ways to treat diseases and produce complex drugs. One area where synthetic biology has made significant strides is in developing engineered bacteria that can detect and target specific cells in the body. For instance, bacteria have been engineered to identify and attack cancer cells while leaving healthy cells untouched, offering a potential alternative to chemotherapy and radiation, which affect both cancerous and healthy cells.
Synthetic biology also plays a role in producing medicines more efficiently. Take artemisinin, a critical antimalarial drug traditionally extracted from the sweet wormwood plant. By using yeast cells engineered through synthetic biology, researchers have developed a way to produce artemisinin in the lab, bypassing the need for plant extraction and ensuring a stable supply. This approach reduces production costs and provides more consistent access to life-saving treatments.
Another exciting development in synthetic biology is in gene therapy. Synthetic biology enables us to create viral vectors that can deliver therapeutic genes to specific cells, correcting genetic disorders at the source. These custom-designed viruses could potentially cure diseases caused by single-gene mutations, such as cystic fibrosis and sickle cell anemia, and have broad applications for future therapies.
Agricultural Innovations Through Synthetic Biology
Agriculture faces several challenges, including pest resistance, soil degradation, and climate variability. Synthetic biology offers ways to address these issues by developing crops that are hardier, more nutritious, and require fewer resources. For example, scientists have engineered crops to be more resistant to pests, reducing the need for chemical pesticides and minimizing environmental impact.
Another area of innovation is developing plants that can withstand extreme environmental conditions. With synthetic biology, we can engineer crops to tolerate drought, high salinity, or poor soil quality, which is crucial in regions facing food security challenges. Additionally, synthetic biology allows us to increase the nutritional content of crops, such as by enhancing vitamins or adding essential amino acids, which could improve diets in areas with limited access to diverse foods.
Synthetic biology can also help improve crop yields by engineering plants to use nutrients more efficiently. For instance, nitrogen-fixing bacteria are being explored as a natural alternative to synthetic fertilizers. By enhancing these bacteria’s nitrogen-fixing abilities through synthetic biology, we can reduce the reliance on chemical fertilizers, making agriculture more sustainable and environmentally friendly.
Environmental Applications: Tackling Pollution and Climate Change
One of the most promising applications of synthetic biology is in environmental conservation, specifically in bioremediation—the process of using living organisms to remove contaminants from soil, water, and air. Synthetic biology allows us to engineer bacteria and other microorganisms that can break down pollutants, such as oil, heavy metals, and plastic waste.
For example, scientists have modified bacteria to degrade plastic, helping to address the global issue of plastic pollution. Similarly, synthetic organisms are being developed to remove excess nitrogen and phosphorous from water bodies, which helps prevent harmful algal blooms. By targeting specific pollutants, synthetic biology offers tailored solutions for environmental restoration that traditional methods can’t achieve.
Synthetic biology also plays a role in reducing greenhouse gas emissions. By engineering microorganisms to produce biofuels from renewable sources like plant biomass, synthetic biology provides an alternative to fossil fuels. These biofuels can reduce carbon emissions in transportation and energy production, supporting efforts to combat climate change. As the demand for sustainable energy grows, synthetic biology is likely to play a central role in creating clean, renewable energy sources.
Advancements in Synthetic Biology Technologies
The rapid advancement of synthetic biology owes much to technologies that allow precise genetic modifications and DNA synthesis. CRISPR-Cas9, for instance, has revolutionized gene editing by making it easier to target and alter specific genes within the genome. This level of precision is essential for creating organisms with custom-designed functions, as it allows scientists to insert, delete, or modify genes with high accuracy.
Another important tool in synthetic biology is high-throughput DNA sequencing, which enables us to analyze and design genetic codes more efficiently. DNA synthesis technology also allows us to produce synthetic DNA in the lab, opening up possibilities for creating entirely synthetic genomes. These advancements have expanded the scope of synthetic biology, enabling more complex and ambitious projects, such as designing synthetic cells or building minimal genomes with only essential genes.
In addition, computational tools and machine learning are now integral to synthetic biology. By simulating how genetic modifications will behave in real organisms, computational models allow us to predict outcomes and refine designs before implementing them in the lab. These tools save time and resources, accelerating the development of synthetic biology applications and enhancing our understanding of genetic networks.
Ethical and Safety Considerations in Synthetic Biology
Despite the potential of synthetic biology, it raises several ethical and safety concerns. One of the primary ethical questions is the extent to which humans should intervene in natural processes, especially when creating synthetic organisms that don’t exist in nature. The ability to design life from scratch gives us powerful control over biology, but it also requires a careful approach to ensure that these technologies are used responsibly.
Safety is another major consideration. The release of genetically modified organisms into the environment could have unintended consequences, especially if they interact with natural ecosystems in unpredictable ways. For example, engineered bacteria used in bioremediation could spread beyond targeted areas or evolve in unexpected ways. To address these risks, synthetic biology often involves safety mechanisms, such as designing organisms that can’t survive outside controlled environments.
Finally, regulatory oversight is essential in synthetic biology. Given the potential risks and ethical issues, regulatory bodies need to establish guidelines that ensure synthetic biology applications are safe, effective, and used ethically. By working together with scientists and industry leaders, regulatory agencies can help strike a balance between innovation and public safety.
The Future of Synthetic Biology: Building on Today’s Innovations
The future of synthetic biology is filled with exciting possibilities. One area of growth is in personalized medicine, where synthetic biology could be used to create tailored treatments based on a person’s genetic profile. By designing gene therapies that target specific mutations or using engineered cells that adapt to individual health conditions, synthetic biology could enable customized treatments that are far more effective than traditional therapies.
Another promising field is synthetic organ development. Scientists are exploring the potential to grow organs in the lab, which could help address the shortage of donor organs for transplantation. By building synthetic tissues that mimic human organs, synthetic biology could create solutions for patients needing heart, liver, or kidney transplants, potentially saving countless lives.
Sustainable solutions are also on the horizon. As synthetic biology advances, we’ll likely see more applications focused on environmental preservation, renewable energy, and sustainable agriculture. These innovations will support efforts to address pressing global challenges, from reducing our carbon footprint to preserving biodiversity.
Key Insights on Synthetic Biology’s Power
New Life Forms: Synthetic biology allows for the design of organisms with custom functions.
Medical Applications: Includes targeted cancer therapies, gene therapy, and efficient drug production.
Agricultural Benefits: Engineered crops for pest resistance, drought tolerance, and higher nutrition.
Environmental Impact: Supports bioremediation, pollution control, and biofuel production.
Future Directions: Personalized medicine, organ development, and sustainable technologies.
In Conclusion
Synthetic biology represents one of the most powerful tools we have for addressing global challenges, from healthcare and food security to environmental sustainability. By building life from scratch, we can design organisms that perform specialized tasks, offering solutions where traditional methods fall short. However, as we harness the potential of synthetic biology, it’s essential to approach it responsibly, addressing ethical concerns and ensuring safety protocols are in place. The future of synthetic biology is promising, with the potential to transform how we interact with and manipulate biological systems, ultimately improving quality of life on a global scale.
1 note
·
View note