#Coders and compliance staff
Explore tagged Tumblr posts
Text
All about Humalife Healthcare
Optimizing Healthcare Operations Through Excellence in RCM: The Humalife Healthcare Approach
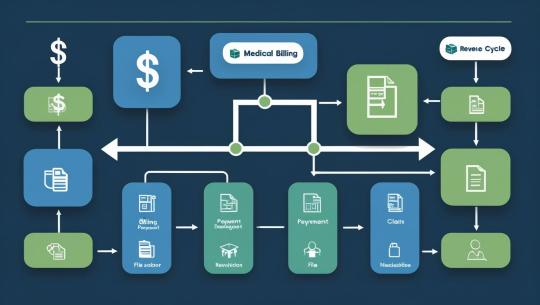
As healthcare systems across the globe continue to evolve, the need for reliable, efficient, and accurate Revenue Cycle Management (RCM) has never been greater. Providers are under increasing pressure to maintain compliance, reduce administrative burden, and ensure timely reimbursement — all while delivering exceptional patient care.
Humalife Healthcare serves as a trusted RCM partner for healthcare organizations in the United States, United Kingdom, and India, delivering high-quality back-end support that enhances operational efficiency and accuracy across the revenue cycle.
A Partner in Operational Clarity and Compliance
Humalife Healthcare offers specialized RCM services that help healthcare providers manage complex workflows with confidence. Our team of trained professionals works as an extension of your internal staff — handling the technical and administrative processes that keep your revenue cycle functioning smoothly.
We understand the regulatory and operational differences across regions and tailor our services to fit each market, ensuring compliance with standards like HIPAA, NHS, and local payer requirements.
Our Core RCM Services
Medical Coding Our certified coders ensure documentation accuracy and compliance with ICD, CPT, and HCPCS standards. We help providers maintain coding integrity, reduce rejections, and stay audit-ready.
Medical Billing Accurate charge entry, timely claim submission, and attention to payer-specific requirements are at the heart of our billing process. We help providers maintain clean claims and reduce delays in reimbursement.
Eligibility and Benefits Verification We verify patient insurance details before service delivery, minimizing the risk of coverage issues and improving patient communication.
Accounts Receivable (AR) Follow-up We manage and track pending claims, follow up with payers, and resolve delays — helping providers reduce days in AR and improve collection timelines.
Denial Management Our team identifies denial trends, appeals rejected claims, and recommends corrective action to minimize recurrence.
Regulatory Compliance and Quality Control Our operations align with healthcare regulations across all served regions. Routine internal audits and strict quality control ensure accuracy, security, and compliance.
What Sets Humalife Healthcare Apart
Industry Specialization We focus exclusively on healthcare RCM. Our domain expertise ensures a deep understanding of provider workflows, payer expectations, and compliance standards.
Global Operational Presence With teams across India, the US, and the UK, we offer time zone-aligned support, operational flexibility, and regional knowledge that enhances collaboration and service delivery.
Process-Driven Execution Our standardized workflows, quality benchmarks, and automation tools help streamline back-end operations, minimize errors, and improve claim cycle performance.
Client-Centric Model We believe in long-term partnerships. Every engagement is structured around your unique needs, with performance metrics, service-level commitments, and continuous process improvements.
Building Healthcare Efficiency Through RCM Excellence
RCM is more than a back-office function — it’s a critical enabler of healthcare performance. By outsourcing your RCM to a trusted partner like Humalife Healthcare, you gain operational support that improves accuracy, reduces administrative burden, and frees up internal resources to focus on patient care.
#HumalifeHealthcare#RCMservices#healthcarebilling#medicalbilling#revenuecyclemanagement#healthcarefinance#medicalrevenue#claimsmanagement#billingaccuracy#healthtech
3 notes
·
View notes
Text
Vanator RPO – Leading Offshore Recruiters USA for Smart Hiring Solutions
In a fast-evolving business environment, companies must adapt quickly to hire the right talent at the right time. This is where offshore recruiters USA play a vital role. Vanator RPO has emerged as one of the top offshore recruitment firms in the United States, offering scalable and specialized Recruitment Process Outsourcing (RPO) solutions. With a strong commitment to quality, speed, and innovation, Vanator is helping businesses of all sizes find the best talent while reducing costs and time-to-hire.
Why Offshore Recruiters USA Are Gaining Popularity
The global workforce is becoming increasingly borderless. Offshore recruiters USA, like Vanator RPO, help bridge the talent gap by leveraging a vast international talent pool. They offer the flexibility, expertise, and tools needed to manage recruitment at scale—whether it’s for IT professionals, healthcare workers, engineers, or finance experts. This model enables companies to focus on their core operations while outsourcing the time-consuming aspects of recruitment to a dedicated team.
End-to-End RPO Solutions
Vanator RPO provides end-to-end recruitment support, making it a one-stop destination for businesses seeking high-quality candidates. Its services include:
24/7 Sourcing Support: Ensures a continuous pipeline of qualified candidates for open roles across industries.
AI-Driven Screening: Uses advanced algorithms to match resumes with job requirements, improving hiring accuracy.
Recruitment Support: Manages full-cycle recruitment, from candidate engagement to final onboarding.
VMS Recruiting: Handles vendor management systems for companies that need volume hiring with strict compliance.
Training Academy: Regularly upskills its recruiters and staff to align with market trends and client expectations.
Virtual Assistance: Offers administrative, technical, and non-technical assistance through remote professionals.
Industry Specialization
One of Vanator’s key strengths lies in its industry-specific approach. The team understands that hiring needs vary by domain, and they customize their strategies accordingly. The major industries served include:
Information Technology: Filling roles from developers to system architects.
Engineering: Recruiting civil, mechanical, electrical, and software engineers.
Medical & Healthcare: Supplying certified coders, nurses, and clinical support staff.
Finance & Accounting: Placing experienced accountants, auditors, and analysts.
Sales & Marketing: Sourcing dynamic sales leaders and digital marketing experts.
Global Presence, Local Expertise
Headquartered in the United States with a major operations hub in India, Vanator RPO serves clients across North America, Europe, and Asia. This global presence allows them to provide localized solutions with the efficiency of offshore recruiters. They are available round-the-clock, helping businesses keep up with hiring demands regardless of time zone or location.
Client-Centric Model
Vanator’s success is built on a deep understanding of client needs. Their recruiters work as an extension of the internal HR teams, aligning with company culture and long-term hiring goals. By doing so, they help reduce hiring costs by up to 30% and significantly cut down the average time-to-fill. Whether it's high-volume recruitment or niche role fulfillment, Vanator RPO adapts seamlessly.
Innovation at the Core
Incorporating AI in recruitment is not just a trend—it's a necessity. Vanator RPO uses AI-powered tools to automate resume screening, enhance candidate engagement, and predict hiring outcomes. This technology-first approach helps them stay ahead in a competitive recruiting market.
Conclusion
Vanator RPO is a trusted name among offshore recruiters USA, offering unmatched expertise in recruitment process outsourcing. With a strategic mix of technology, global reach, and personalized service, they empower organizations to build world-class teams. If your business is looking to optimize its hiring strategy, Vanator is the ideal partner for intelligent, cost-effective, and scalable recruitment solutions.
Visit us at: www.govanator.com
1 note
·
View note
Text
Open Your Healthcare Career: Top Benefits of Internships in Medical Billing and Coding
Unlock Your Healthcare Career: top Benefits of Internships in Medical Billing and Coding
Starting a career in healthcare can be both exciting and rewarding. Among the many entry points into this dynamic industry, internships in medical billing and coding stand out as a fantastic way to gain real-world experience, develop valuable skills, and build a professional network. Whether you’re a newbie exploring healthcare or a recent graduate aiming to specialize, interning in medical billing and coding can set you on a successful career path.
Why Are internships in medical Billing and Coding Critically important?
Internships serve as a bridge between education and professional employment. In the realm of medical billing and coding, they provide an invaluable prospect to apply classroom knowledge in real clinical settings, understand industry standards, and discover the nuances of healthcare management.
Key Benefits of Internships in Medical billing and coding
1. Practical skills Growth
Hands-on experience wiht Electronic Health Records (EHR) systems
Proficiency in coding languages such as ICD-10, CPT, and HCPCS
Understanding insurance claim processing and reimbursement procedures
Mastering accurate data entry and management skills
2. Enhanced Job Prospects
Internships often lead directly to full-time positions. Employers value prior internship experience as it demonstrates your commitment and familiarity with industry tools and standards, giving you a competitive edge in the job market.
3. Networking Opportunities
Internships connect you with healthcare professionals, including billing specialists, medical coders, and administrative managers. Building professional relationships can lead to mentorship opportunities and recommendations that boost your career.
4. Industry Insights and Career Clarity
By working in real healthcare environments, interns gain clarity about their career interests, whether they want to focus more on coding, billing, or healthcare administration. This insight helps in choosing specialized certifications or further education.
5. Confidence Building
Practical experience helps build confidence in your abilities, making you more comfortable navigating healthcare systems and communicating with medical staff and insurance companies.
Practical Tips for Making the Most of Your Medical Billing and Coding Internship
Research the association: Understand its services and systems beforehand.
Ask questions: Never hesitate to clarify processes or protocols.
Stay organized: Keep detailed notes and logs of your tasks and learnings.
Seek feedback: Regularly ask supervisors for constructive feedback to improve your skills.
Leverage online resources: complement your internship with online courses or certification programs in medical coding and billing.
Real-Life Case Study: Sarah’s Journey to success
Aspect
Details
Internship Organization
WellMed Healthcare Facility
Duration
6 months
Learnings
Mastered Epic EHR system,ICD-10 coding,and insurance claim submissions
Outcome
Received a full-time medical coder position immediately after internship
Sarah’s story exemplifies how internships can be transformative,leading from learner to professional,and providing a clear pathway into the healthcare industry.
Additional Insights: certifications and Continuous Learning
While internships provide foundational experience, obtaining industry-recognized certifications can further enhance your employability. Popular options include:
Certified Professional Coder (CPC)
Certified Coding Associate (CCA)
Certified Healthcare reimbursement Specialist (CHRS)
Continuing education and specialization keep your skills current and can open doors to advanced roles in healthcare administration, compliance, or specialty coding.
Conclusion: Unlock Your Healthcare Career Today
Internships in medical billing and coding are more than just temporary positions-they are gateways to a promising healthcare career. They equip you with essential skills, industry insight, and professional connections needed to succeed. Whether you’re just starting out or looking to specialize, embracing an internship can accelerate your journey into the healthcare field and elevate your professional profile.
Take the first step today-search for reputable internship programs, prepare your application, and commit to gaining practical experience in this evolving industry. Your healthcare career awaits!
https://medicalcodingandbillingclasses.net/open-your-healthcare-career-top-benefits-of-internships-in-medical-billing-and-coding/
0 notes
Text
Discover Top Medical Billing & Coding Jobs in Rhode Island - Your Guide to Lucrative Healthcare Careers
Discover Top medical Billing & Coding jobs in Rhode Island - Your Guide to Lucrative Healthcare Careers
Are you looking to start a rewarding career in healthcare that offers stability, growth potential, and an excellent work environment? Medical billing and coding are among the most promising healthcare careers today, especially in Rhode Island, a state known for its vibrant healthcare sector. In this thorough guide, we’ll explore the top medical billing and coding jobs available in Rhode Island, provide tips on how to land your dream position, and highlight why this field is an excellent choice for your professional future.
Why choose Medical Billing & Coding as a Healthcare Career?
Medical billing and coding professionals play a vital role in the healthcare system. They ensure that healthcare providers are accurately reimbursed for their services by translating medical procedures into universally recognized codes. these roles combine healthcare knowledge with administrative skills and often allow for flexible work environments, including remote opportunities.
Key benefits of pursuing a career in medical billing and coding include:
high demand: The evolving healthcare landscape constantly requires skilled billing and coding specialists.
Lucrative salaries: Competitive pay rates with growth potential.
Flexible working options: Many roles support remote or hybrid work setups.
Career advancement: Opportunities for certification and specialization.
Low entry barriers: Short-term training programs and certification requirements.
Overview of the medical Billing & Coding Job Market in Rhode Island
Rhode Island boasts a robust healthcare industry, with prominent hospitals, clinics, and health systems such as Rhode Island Hospital, Lifespan, and Care New England Health System. These institutions generate a consistent demand for certified medical billing and coding specialists.
According to recent employment data, Rhode Island’s healthcare sector is experiencing steady growth, fueling demand for qualified professionals in medical billing and coding. The state’s strategic focus on expanding healthcare services makes it an ideal location for aspiring healthcare workers.
Top Medical Billing & Coding Jobs in Rhode Island
1. Medical Biller
Medical billers are responsible for submitting claims to insurance companies, following up on unpaid claims, and ensuring accurate billing practices. They must be detail-oriented and familiar with insurance policies and coding standards.
2. Medical coder
Medical coders translate clinical diagnoses, procedures, and services into standardized codes (ICD, CPT, HCPCS). Their accuracy directly impacts the reimbursement process and healthcare compliance.
3. Healthcare Office Manager
This role involves overseeing daily office operations,including billing and coding departments,ensuring compliance,and managing staff.
4. Insurance Claims Specialist
Specialists handle claim submissions, resolve denials, and communicate with insurance providers to facilitate timely payments.
Essential Skills and Qualifications for Rhode Island Medical Billing & Coding Jobs
Certification: Certifications such as Certified Professional Coder (CPC), Certified Coding Associate (CCA), or Certified Medical reimbursement Specialist (CMRS) enhance employability.
Technical Skills: Familiarity with Electronic Health Records (EHR) systems, billing software, and coding tools.
attention to Detail: Accuracy in coding to prevent claim denials.
Knowledge of Healthcare Regulations: Understanding of HIPAA, CMS guidelines, and insurance policies.
Communication Skills: Ability to liaise effectively with healthcare providers and insurance companies.
Getting Started: Education & Certification programs in Rhode Island
Several institutions in Rhode Island offer comprehensive training programs in medical billing and coding, both online and in-person. Key options include:
Rhode Island medical Billing & Coding School – Offers diploma programs designed to prepare students for certification.
Community College of Rhode Island (CCRI) – Provides certificate courses in medical coding and billing as part of healthcare administration programs.
Online Certification options – Accredited programs from AAPC,AHIMA,and Penn Foster allow flexible learning from anywhere.
Salary Expectations and Job Outlook in Rhode Island
Medical billing and coding salaries in Rhode Island are competitive and vary depending on experience, certification, and work environment. Here’s a quick overview:
Position
Average Salary in Rhode Island
Experience Level
Medical Biller
$40,000 - $55,000
Entry to Mid-Level
Medical Coder
$45,000 - $60,000
Mid-Level to Senior
Healthcare Office Manager
$65,000 – $85,000
senior Experience
With the increase in healthcare services, job opportunities in Rhode Island are expected to grow by around 10% over the next decade, according to the Bureau of Labor Statistics.
practical Tips for Landing Your Dream Healthcare Job in Rhode Island
Gain Relevant Certification: Enroll in reputable certification programs to increase marketability.
Build Experience: Seek internships or volunteer opportunities in healthcare settings to gain practical knowledge.
Network: Join professional organizations like AAPC Rhode Island Chapter or AHIMA Rhode Island for networking and job leads.
Optimize Your Resume: Highlight certifications, software skills, and relevant healthcare experience.
Stay Updated: Keep up with changes in coding standards and healthcare regulations.
Case Study: A Success Story from Rhode Island
Jessica, a native of Providence, Rhode Island, started her career as a medical biller after completing a certification program at CCRI. Within two years, she obtained her CPC certification and transitioned into a medical coding role at a local hospital. Jessica’s dedication, combined with networking and continuous learning, enabled her to advance quickly and now earns a competitive salary while working remotely part-time.
Conclusion
Rhode Island offers a fertile ground for aspiring medical billing and coding professionals. With a strong healthcare infrastructure, ample job opportunities, and competitive salaries, there’s no better time to start or advance your healthcare career in this vibrant state. Whether you’re just beginning and exploring training programs or a seasoned professional seeking new opportunities, the medical billing and coding field provides a secure, lucrative, and rewarding career path. Embrace the opportunities in Rhode Island and take your first step toward a thriving healthcare career today!
https://medicalbillingcertificationprograms.org/discover-top-medical-billing-coding-jobs-in-rhode-island-your-guide-to-lucrative-healthcare-careers/
0 notes
Text
Why Pulmonary Medical Billing Services Matter More Than Ever in 2025

In the ever-evolving healthcare landscape, pulmonary care providers face mounting challenges in managing their revenue cycle while delivering optimal care to patients. From complex coding requirements to rapidly changing payer policies, managing billing in-house is often overwhelming. That’s where Pulmonary Medical Billing Services comes into play—offering a specialised and efficient solution tailored to the unique needs of pulmonology practices.
At Atlantic RCM, we understand the intricacies of pulmonary billing and provide dedicated, expert-level Pulmonary Medical Billing Services to ensure accuracy, compliance, and faster reimbursements. Explore how outsourcing to a professional billing partner can transform the financial health of your pulmonology practice.
The Complexity of Pulmonary Billing
Pulmonologists treat a wide range of respiratory conditions, including asthma, COPD, sleep apnea, interstitial lung disease, and more. This breadth of care brings with it a complex matrix of:
CPT and ICD-10 codes
Modifiers
Pre-authorizations
Diagnostic testing and procedure documentation
Payer-specific policies
Mistakes in any of these areas can result in claim denials, delayed payments, and compliance risks.
Moreover, billing for services like spirometry, bronchoscopy, pulmonary function tests, and sleep studies often requires deep knowledge of how these procedures are interpreted by Medicare and private insurers. A general billing approach simply won’t do.
That’s why specialised pulmonary medical billing services are essential. They ensure not only billing precision but also maximise reimbursements and maintain cash flow stability.
Why Choose Atlantic RCM’s Pulmonary Medical Billing Services?
1. Specialised Expertise in Pulmonology
Unlike generic billing companies, Atlantic RCM has a team that’s specifically trained in pulmonary coding, billing regulations, and documentation standards. Our specialists stay updated with the latest in payer guidelines, CPT updates, and industry best practices.
2. Accurate Coding & Charge Entry
Accurate CPT and ICD-10 coding is the backbone of successful billing. Atlantic RCM ensures that all patient encounters are translated into the correct codes with no errors or omissions. We use automated tools and manual checks to minimize denials and ensure compliant billing.
3. Faster Reimbursements
Our streamlined workflow—from charge capture to claim submission and AR follow-up—reduces billing cycle time. On average, practices see a 25–30% increase in cash flow after switching to our services.
4. End-to-End Revenue Cycle Management
We offer complete support, including:
Insurance eligibility verification
Coding audits
Claims submission
Denial management
Patient billing & statements
Monthly financial reports
This holistic approach ensures that no revenue is left on the table.
5. Transparent Reporting and Analytics
Atlantic RCM provides clients with regular performance reports, so you can track KPIs like:
Collection rates
Average days in AR
Denial rate
Clean claim rate
This transparency gives you full control over your financial performance while we manage the heavy lifting.
Benefits of Outsourcing Pulmonary Billing
Improved Compliance
Healthcare regulations are constantly evolving. Our billing team stays on top of HIPAA, OIG guidelines, and Medicare compliance so you don’t have to.
Reduced Administrative Burden
Free up your front-office staff to focus on patient care, not paperwork. With Atlantic RCM managing your billing, your team can breathe easy.
Higher Collection Rates
With a sharp focus on proper coding, timely filing, and AR follow-up, we help pulmonologists increase collections and reduce write-offs.
Access to Certified Billing Experts
Our team includes Certified Professional Coders (CPCs) and Certified Medical Reimbursement Specialists (CMRS) who specialise in pulmonary billing.
Who Can Benefit from Our Pulmonary Billing Services?
Atlantic RCM works with:
Independent pulmonology clinics
Sleep centers
Hospital-affiliated pulmonary departments
Multi-specialty practices with pulmonary units
Critical care physicians
No matter your practice size, we tailor our pulmonary medical billing services to meet your workflow, EHR system, and billing goals.
Seamless Integration with EHR/EMR Systems
We work with all major EHRs, including:
Epic
Cerner
Athenahealth
Kareo
eClinicalWorks
AdvancedMD
Whether you need full-service RCM or support for specific functions, our tech-enabled solutions integrate smoothly with your existing systems to minimise disruptions.
Why 2025 Is the Right Time to Upgrade Your Billing Partner
With tightening reimbursement policies, rising patient responsibilities, and inflationary pressures on practice costs, revenue integrity is more critical than ever.
Here’s why more pulmonologists are turning to Atlantic RCM in 2025:
Payer policies are more aggressive in denying claims
In-house billing teams are increasingly overworked or understaffed
Errors in sleep study and pulmonary function test billing are on the rise
Prior authorization requirements are more complex
Outsourcing is more cost-effective than maintaining a billing department
Partner with Atlantic RCM – A Leader in Pulmonary Medical Billing
At Atlantic RCM, we believe in precision, partnership, and performance. Our mission is to help pulmonologists focus on breathing life into their patients—not chasing claims or battling denials.
With decades of experience and a track record of success, our Pulmonary Medical Billing Services are designed to support your practice’s growth and sustainability.
Ready to optimise your billing?
Explore our pulmonology billing services:
https://atlanticrcm.com/pulmonary-medical-billing-services.php
Or get in touch today for a free revenue cycle analysis and see how we can elevate your practice's financial performance.
Final Thoughts
Pulmonary billing is complex—but it doesn’t have to be a headache. By partnering with experts who understand the nuances of respiratory care billing, you can unlock faster payments, reduce denials, and gain peace of mind.
Atlantic RCM is here to provide specialised, efficient, and transparent pulmonary medical billing services—so you can focus on what you do best: helping patients breathe easier.
1 note
·
View note
Text
youtube
FTE Model Explained: Offshore RCM with Onshore Quality
The Real Cost of In-House Billing Staff turnover | Training costs | High payroll | Cash flow delays
What Is an FTE? Your coder or biller — dedicated, integrated, only $8.5/hour
Save Big Without Sacrificing Quality Up to 70% savings | Just $8.5/hour | 100% billing precision
Monitored Performance. Measurable Results. Claim turnaround | Clean claims | Denial rate reduction
HIPAA-Secure, U.S.-Grade Compliance Encrypted access | Role-based security | Full audit controls
Instant Scalability On-demand growth | Trained talent | Zero ramp-up time
Why ICS? 200+ experts | 100+ specialties | 40+ EMRs | U.S. RCM impact
Start with ICS at $8.5/hour
Thanks for watching!
For More Details Visit- @infohubconsultancy
#FTEemployeeinmedicalbillingservices#FTEequivalentoutsourcemedicalbillingservices#FTEinmedicalbilling#fulltimeequivalent(FTE)employeesforoutsourcemedicalbilling#FullTimeequivalent(FTE)Modelforoutsorcemedicalbillingandcoding#Youtube
0 notes
Text
Why Accurate Physician Billing is the Backbone of Private Practices in 2025

In today’s rapidly evolving healthcare landscape, accurate physician medical billing services are no longer just an operational necessity—they’re the backbone of private practices. As we move through 2025, private practices are facing unprecedented challenges: rising administrative burdens, frequent regulation updates, and increasing patient expectations. Amid these pressures, ensuring precise billing is what keeps practices solvent, scalable, and sustainable.
The High Stakes of Inaccurate Billing
Billing errors cost private practices billions of dollars annually. A simple coding mistake, missed modifier, or delayed submission can trigger claim denials, lost revenue, and compliance risks. In 2025, with even tighter payer scrutiny and updated CMS regulations, the margin for error has become even thinner.
Inaccurate billing not only affects revenue flow but also damages patient trust. Incorrect charges or unexpected bills frustrate patients and tarnish a practice’s reputation—something no private clinic can afford in a review-driven digital era.
Why Accuracy is More Critical Than Ever in 2025
1. Increased Regulatory Demands
With the implementation of new compliance frameworks and payer policies in 2025, such as AI-driven claim audits and real-time data validation, practices are under the microscope. Accurate physician billing services ensure compliance, help avoid audits, and reduce the risk of hefty fines.
2. Shift to Value-Based Care
Reimbursement is no longer just about volume; it’s about outcomes and documentation. Practices must report the right codes and modifiers to reflect quality and outcomes accurately. Faulty billing here doesn’t just mean delayed payment—it can cost a practice its value-based incentives.
3. Rising Patient Consumerism
Today’s patients are savvier, more informed, and demand transparent billing. They want digital access to estimates, easy-to-understand statements, and fewer billing surprises. Practices that get billing right from the start build stronger patient loyalty.
4. Technology Integration & Automation
While EHRs and billing software are becoming more advanced, they still require accurate human input and oversight. In 2025, successful practices are those that strike the right balance between automation and expert oversight to catch coding errors and ensure clean claims.
The Backbone of Financial Health
Accurate physician medical billing services are the foundation for:
Timely and full reimbursements
Reduced denial rates
Faster revenue cycles
Better cash flow
Stronger patient relationships
It also enables practices to reinvest in growth, technology, staffing, and patient care initiatives.
How to Ensure Accuracy in Physician Billing
To keep up in 2025, private practices must:
Outsource to professional physician billing services that stay current with payer policies and coding changes.
Invest in staff training for in-house billers and coders.
Conduct regular audits to catch and correct errors before submission.
Leverage advanced billing software with AI-based error detection and reporting tools.
Track KPIs like denial rates, days in A/R, and clean claim rates for continuous improvement.
Partner with 360 Medical Billing Solutions
At 360 Medical Billing Solutions, we specialize in accurate, efficient, and compliant physician medical billing services designed to meet the demands of 2025 and beyond. Our experienced team ensures faster reimbursements, fewer denials, and complete peace of mind for private practices.
✅ Stay compliant ✅ Maximize revenue ✅ Free up your staff for patient care
📞 Contact 360 Medical Billing Solutions today to schedule a free consultation and see how we can transform your billing process into a growth engine for your practice.
👉 Visit 360medicalbillingservices.com or Call Now to get started!
0 notes
Text
The Rise of Contract Staffing in Malaysia’s Evolving Job Market
Malaysia’s workforce is changing and fast. As digitalisation reshapes industries and businesses strive to stay agile, one hiring model is quietly gaining momentum: contract staffing.
From startups in Cyberjaya to manufacturers in Penang, companies are rethinking how they hire. Full-time roles used to dominate, but that’s shifting. Today, more organisations are choosing contract staff to manage workload spikes, bring in specialised skills, and respond to change faster.

📈 Why More Malaysian Businesses Are Embracing Contract Staffing
So, what’s driving this shift? The reasons are practical and powerful.
1. Quicker hiring, faster results When deadlines are tight, waiting weeks to fill a role just isn’t an option. Contract staffing lets businesses bring in the right people quickly sometimes in just days.
2. Lower long-term costs Hiring full-time staff comes with permanent commitments EPF, SOCSO, insurance, training. Contract roles offer a more flexible cost model, helping businesses manage budgets better.
3. Access to niche skills Need a cybersecurity consultant? A software developer for a 3-month project? Or a warehouse coordinator during the holiday rush? Contract staffing makes it easy to bring in talent with specific expertise when and where you need it.
4. Flexibility to scale Whether it’s seasonal demand, a sudden project, or business expansion, contract staffing helps teams scale up (or down) without a long-term commitment.
🏭 Which Industries Are Leading the Way?
Contract staffing isn’t just for one sector. Across Malaysia, several industries are turning to this model:
Tech & IT The rise of fintech, AI, and cloud platforms has made contract IT roles more common especially in KL and Cyberjaya.
Manufacturing In places like Selangor and Penang, factories are hiring contract engineers and production staff to handle new product lines or meet export demand.
Healthcare With growing demand in public and private healthcare, hospitals are hiring contract nurses, lab staff, and coders to ease the load.
Shared Services & BPOs Malaysia’s growing BPO sector relies heavily on temporary and contract talent to fill roles in finance, HR, and customer support.
👥 What Do Malaysian Job Seekers Think?
Contract work isn’t just good for companies it’s also appealing to many workers.
Young professionals, especially Gen Z and millennials, are increasingly open to short-term contracts. Why? They want exposure to different industries, flexibility to explore their options, and the chance to build skills fast.
Plus, in competitive fields like tech or design, contract gigs often pay well and offer valuable experience that opens doors down the road.
🛠 How Net2Source Helps Malaysian Businesses Thrive
At Net2Source Malaysia, we understand the local talent market and how fast things move.
With a presence in Kuala Lumpur, we support companies across Penang, Johor Bahru, Selangor, and beyond with:
Fast access to pre-vetted contract professionals
End-to-end workforce support from sourcing to onboarding
Full compliance with Malaysian labour laws
Tailored hiring strategies that fit your industry and goals
Whether you need a developer for a 6-month system upgrade, a logistics team for peak season, or a team of engineers for a new plant, we’ve got you covered.
💡 Final Thought
Contract staffing in Malaysia isn’t just a workaround it’s becoming a core part of how smart businesses grow. It's about staying lean, moving fast, and hiring smarter. If you're looking to build a resilient and flexible team in Malaysia, contract staffing might be exactly what your business needs.
#HiringInMalaysia#MalaysiaWorkforceTrends#ContractJobsMalaysia#SmartHiringSolutions#KLBusinessUpdates#FlexibleHiringMY#TalentSolutionsMalaysia#Net2SourceMY#PenangHiringSupport#GrowWithContractStaffing
0 notes
Text
Optimize Your Revenue: Expert Tips for Efficient Medical Claims Billing and Avoiding Denials
Maximize Your Revenue: Expert Tips for Efficient Medical Claims Billing and Avoiding Denials
Effective medical claims billing is a cornerstone of a prosperous healthcare practice. Proper billing practices not only ensure timely reimbursements but also help avoid costly claim denials that can delay revenue and frustrate both providers and patients. In this comprehensive guide, we’ll explore proven strategies and expert tips to enhance your medical claims process, maximize revenue, and substantially reduce claim denials.
Understanding the Importance of Efficient Medical Claims Billing
Medical billing is a complex task that requires precision, legal compliance, and a thorough understanding of insurance workflows. Errors, omissions, or delays can lead to claim denials, delayed payments, and decreased revenue flow. Thus, adopting best practices for billing can definitely help your practice improve cash flow, reduce administrative costs, and strengthen your bottom line.
Key Benefits of Optimized Medical Claims Billing
Increased Revenue: Faster, more accurate claims mean quicker reimbursements.
Reduced Claim Denials: Minimize errors that cause rejections or delays.
Enhanced patient Satisfaction: Obvious billing processes improve trust and compliance.
Lower Administrative Costs: Efficient workflows reduce the need for resubmissions and follow-ups.
Practical Tips for Efficient Medical Claims Billing
1. Keep Accurate and Up-to-Date Patient Records
Accurate patient data is fundamental to successful medical claims billing.Confirm details such as:
Full legal name
Date of birth
Insurance policy number
Primary and secondary insurance details
Correct billing address
Regularly update and verify this information to prevent claim rejections due to mismatched or outdated data.
2. Implement Robust Coding Standards
Proper use of medical codes, including ICD-10, CPT, and HCPCS, is crucial for accurate billing. Consider investing in coding training or partnering with certified medical coders to ensure:
Codes accurately reflect procedures and diagnoses
Prevent coding mismatches that can trigger denials
Comply with insurance and government regulations
3. Use Advanced Billing Software and Technology
Modern billing software automates many steps of the claims process, reduces errors, and tracks submission status. Features to look for include:
EDI (Electronic Data Interchange) capabilities
Real-time claims tracking
Automated reminders for follow-ups
Built-in code validation tools
Investing in reliable billing technology streamlines your workflow and boosts efficiency.
4. Submit Clean and Complete Claims
Claims free of errors are approved faster. To ensure this, double-check for:
Correct patient and insurance details
Accurate coding and modifiers
Legible or electronically legible documentation
Proper signatures and authorizations
Utilize software with validation features that flag common errors before submission.
5. Establish Clear Follow-Up Procedures
Timely follow-up on unpaid or rejected claims prevents revenue leakage. Keep track of claim statuses and implement workflows for:
Resubmitting denied claims with corrections
Communicating with insurance companies
Keeping detailed records of all interactions
Strategies to Avoid Common Medical Claims Denials
1. Understand Payer Policies and Requirements
Each insurance provider has specific rules. Review payer manuals regularly to stay compliant and adapt billing practices accordingly.
2. Prioritize Documentation Accuracy
Supporting documentation should justify diagnoses and procedures.Missing or incomplete records often cause claims to be denied.
3. Educate Staff Regularly
Continuous training for your billing team on coding updates, payer policies, and billing best practices is vital.
4. Check for Authorization and Pre-Certification
Many payers require prior approvals. Ensure necessary pre-authorizations are obtained and documented to avoid denials due to authorization issues.
5. Use Denial Management Tools
Tools and analytics enable your practice to identify frequent denial reasons, allowing targeted improvements to your billing process.
Case study: How a Small Clinic increased Revenue by 30%
Challenge
Solution
Result
High rate of claim denials due to coding errors
Invested in coding training and upgraded billing software with validation tools
30% increase in successful claims and faster reimbursements
Delayed follow-up on unpaid claims
Established automated tracking workflows
Reduced outstanding claims by 20%
First-Hand Experience: My Journey to Optimized Medical Billing
As a healthcare administrator, I faced persistent billing issues that hindered revenue flow. Implementing targeted staff training, upgrading our billing platform, and establishing clear follow-up protocols transformed our financial performance. Regular audits and staying current with insurance policies proved essential in avoiding denials and improving cash flow.
Conclusion
Maximizing revenue through efficient medical claims billing is achievable with the right strategies, technology, and ongoing education. By focusing on accurate data entry, proper coding, leveraging automation, and proactively managing denied claims, healthcare practices can significantly improve their reimbursement rates and reduce financial stress. Remember,continuous improvement and staying informed about industry changes are key to long-term success in medical billing. Start implementing these expert tips today to see tangible results and enhance your practice’s financial health.
https://medicalbillingcodingcourses.net/optimize-your-revenue-expert-tips-for-efficient-medical-claims-billing-and-avoiding-denials/
0 notes
Text
The Benefits of Outsourcing Home Health Coding ICD10 Services

Let’s not sugarcoat it—ICD-10 coding in home health isn’t for the faint of heart. It’s detail-heavy, ever-changing, and honestly, a little intimidating if you’re not knee-deep in it every day. And if you’re running a home health agency in 2025? You’ve got enough on your plate without having to memorize the difference between I10 and E11.9 (those are real codes, by the way).
That’s where outsourcing Home Health Coding ICD10 Services can be a total game changer. I know, I know. Outsourcing anything can feel like a big leap. But let’s break it down, human to human.
1. Accuracy Without the Guesswork
ICD-10 codes aren’t just random numbers—they impact your agency’s reimbursement and compliance. Miss a detail or code something out of sequence, and boom: denied claim. Or worse, flagged audit. That’s not exactly the kind of surprise anyone enjoys.
By outsourcing to specialists (like the team over at Trilogy Quality Assurance), you’re tapping into a group of certified coders who eat, sleep, and breathe these codes. They know what’s changed, what documentation supports what code, and how to stay on the right side of CMS guidelines.
Frankly, that kind of expertise is hard to find in-house unless you’ve got a really large operation—and even then, turnover and training are a whole other headache.
2. Time Back for Your Team (And Yourself)
Let’s face it: clinicians didn’t get into healthcare to argue with codes. They want to take care of patients. But when they’re bogged down in documentation or coding decisions, it pulls their focus—and morale takes a hit too.
Outsourcing coding frees up your nurses and admin staff to do what they do best. No more burning time trying to figure out the fifth character in an ICD-10 code when they could be wrapping up visits or planning care.
And you? You get time back to actually run your agency instead of playing catch-up with compliance.
3. Reduced Costs (No, Really)
Here’s where it gets interesting: outsourcing often costs less than hiring and training an in-house coder. Especially when you factor in benefits, turnover, continuing education, and the software they’ll need. Plus, if coding errors are causing claim denials or delays, that’s lost revenue stacking up quietly in the background.
Companies like Trilogy offer scalable services, so you’re only paying for what you need. High volume? They’ve got you. Just getting started? They’ll grow with you. It’s like having a coding department without the HR responsibilities.
4. Built-In Compliance & Peace of Mind
This one might not show up on your balance sheet, but it matters—especially in today’s climate. Staying compliant with ever-shifting Medicare rules is stressful. One wrong code, one poorly worded note, and suddenly you’re fielding an audit.
Outsourced coding partners monitor regulatory updates and adjust your coding in real-time. It’s one less thing to worry about. And honestly? That peace of mind is priceless.
Final Thought?
Outsourcing Home Health Coding ICD10 Services isn’t just about saving time or money (though it does both). It’s about running a more efficient, less stressed, and more compliant agency. If you’re ready to take that step, Trilogy Quality Assurance might just be your secret weapon.
Because let’s be honest—life’s too short to code alone.
0 notes
Text
Maximizing AR Collections: A Strategic Guide to RCM Best Practices

In today’s competitive healthcare landscape, Maximizing AR Collections is more than just a financial goal — it’s a strategic necessity. With tight margins and increasing administrative complexities, healthcare providers must streamline their revenue cycle to ensure financial sustainability. One of the most crucial elements of this process is Accounts Receivable Follow-Up. When done correctly, it accelerates reimbursements, minimizes denials, and ensures continuous cash flow.
This guide explores the best practices and modern strategies, including AR Follow-Up Services and AR Recovery Services, that help optimize revenue cycle management (RCM) and drive growth.
Understanding the AR Challenge in Healthcare
Effective Account Receivable Follow-Up Services are essential for managing common revenue cycle hurdles:
Payer Complexity: Varying payer rules and timelines require expertise and adaptability.
Coding Errors: Inaccurate coding can lead to rejections and delays.
Patient Payment Confusion: Unclear financial responsibility contributes to slower self-pay collections.
Manual Processes: Outdated workflows hinder staff productivity and timely follow-up.
Lack of Analytics: Without real-time data, it’s difficult to identify bottlenecks and root causes of denials.
These issues can snowball without a robust AR Follow-Up system in place — making automation, training, and specialized support essential.
Front-End Excellence: Setting the Stage for AR Success
The foundation of efficient Accounts Receivable Follow-Up begins before the first claim is even submitted.
1. Accurate Patient Registration and Eligibility Verification
Ensure demographic accuracy to avoid claim mismatches.
Use automated tools for insurance eligibility verification to avoid ineligible claims.
Provide patient financial counseling to improve collections from the start.
2. Clinical Documentation and Coding Precision
Invest in quality documentation that supports medical necessity.
Train coders on current ICD-10 and CPT codes and payer-specific guidelines.
Regularly audit documentation and coding to minimize errors and ensure compliance.
Mid-Cycle Optimization: Denial Prevention and Claim Submission
1. Automated Claims Submission
Leverage EDI and clearinghouses to speed up submissions and track issues.
Use claim scrubbers to detect and fix issues before claims reach the payer.
2. Denial Management and Appeals
Categorize denials to identify systemic issues.
Create standardized workflows for timely appeals.
Train your staff to understand and respond to common denial codes effectively.
These steps ensure fewer denials and support faster processing, reducing the burden on AR Follow-Up Services teams.
Back-End Focus: Driving Results Through AR Recovery Services
The post-adjudication phase is where specialized AR Recovery Services and Outsourced A/R Follow-Up make a significant impact.
1. Targeted Follow-Up on Outstanding Claims
Use technology to flag aging claims and ensure timely action.
Assign dedicated specialists to handle high-value or complex payer claims.
Prioritize based on aging buckets, value, and payer performance.
2. Enhancing Patient Self-Pay Collections
Offer online payments, mobile pay, and flexible plans to improve collections.
Send clear, concise statements outlining balances and insurance coverage.
Train collection teams to communicate professionally and empathetically with patients.
Leveraging Technology for Smarter AR Management
Today’s healthcare RCM teams can no longer rely on manual processes alone. Embracing innovation is key to Maximizing AR Collections.
AI and Machine Learning: Predict denials, identify underpayments, and automate eligibility verification.
Robotic Process Automation (RPA): Automate repetitive tasks like status checks and payment posting.
Integrated RCM Software: Centralize all AR activities for visibility across teams.
Advanced Analytics: Use dashboards and reporting to measure KPIs such as days in AR, denial rates, and recovery timelines.
These tools amplify the efficiency of Account Receivable Follow-Up Services and free your team to focus on high-priority accounts.
Continuous Improvement: The Core of Long-Term AR Success
Maximizing AR collections is not a one-and-done project — it’s a continuous cycle of performance enhancement.
Monitor KPIs: Track metrics such as AR aging, first-pass resolution rate, and clean claim rate.
Enhance Communication: Foster collaboration across registration, coding, billing, and AR teams.
Ongoing Training: Keep teams up to date on payer changes, billing guidelines, and software updates.
Benchmarking: Compare internal performance to industry standards to identify gaps.
Why Outsourced A/R Follow-Up Is the Smart Move
Healthcare organizations increasingly turn to Outsourced A/R Follow-Up providers to alleviate internal workload and drive better outcomes. Here’s why:
Expertise: Trained AR specialists know payer rules and timelines.
Scalability: Easily manage high claim volumes without overwhelming internal staff.
Faster Recovery: Dedicated teams focus solely on AR recovery, improving turnaround time.
Cost Efficiency: Save on staffing, training, and technology investments.
Choosing a trusted partner for AR Follow-Up Services ensures consistent revenue, reduced aging, and stronger overall RCM performance.
Conclusion
In an industry where cash flow determines care quality and growth potential, Maximizing AR Collections is a non-negotiable priority. From proactive front-end processes to advanced back-end AR Recovery Services, every step in the RCM cycle matters. Leveraging the right blend of people, processes, and technology — and considering Outsourced A/R Follow-Up for added support — can transform your organization’s financial outlook.
Take control of your revenue cycle with specialized Account Receivable Follow-Up Services that deliver results.
Read more: https://www.allzonems.com/maximizing-ar-collections/
🚀 Ready to Improve AR Performance?
Partner with Allzone Management Services — a trusted leader in AR Follow-Up Services and RCM optimization. Our expert team ensures maximum recovery, faster collections, and clean claims — all with full transparency and compliance.
📞 Call us today at +1 866–854–2714 🌐 Visit us at www.allzonems.com 📧 Email: [email protected]
Let us handle your AR, so you can focus on patient care.
#AR Follow-Up Services#Accounts Receivable Follow-Up#Account Receivable Follow-Up Services#Outsourced A/R Follow-Up#AR Recovery Services#allzone#outsourcing revenue cycle management#healthcare medical billing management solutions#medical billing solutions#rcm services#healthcare rcm companies#medical billing outsourcing#medical billing outsourcing companies#outsource medical billing services#medical coding services
0 notes
Text
Blog For APC Codes and Dental Coding
Understanding APC Codes: A Guide to Ambulatory Payment Classification Codes
In the world of outpatient healthcare billing, APC Codes (Ambulatory Payment Classification Codes) play a crucial role in determining how providers are reimbursed for services. These codes are used to categorize outpatient procedures and services for payment under the outpatient prospective payment system.
Ambulatory Payment Classification Codes are assigned based on the type and complexity of the service provided. For example, a routine clinic visit and an outpatient surgery would fall under different APC Codes because of their varying resources and costs. This classification ensures consistency in billing and simplifies the reimbursement process for outpatient services.
One of the key advantages of using Ambulatory Payment Classification Codes is that they promote transparency and efficiency in hospital billing. Each code corresponds to a fixed reimbursement rate, which helps healthcare providers estimate payments in advance. This system also reduces administrative burdens and minimizes errors in claim processing.
For medical coders and billing professionals, understanding APC Codes is essential for accurate documentation and timely reimbursement. Misclassification or use of outdated codes can lead to claim denials or payment delays. Staying updated with changes in Ambulatory Payment Classification Codes ensures compliance with healthcare regulations and maintains smooth revenue flow.
In summary, APC Codes are an integral part of the healthcare reimbursement system, especially in outpatient settings. They standardize the way procedures are billed and paid for, helping healthcare providers deliver care more efficiently while ensuring fair compensation. Whether you're a healthcare administrator, coder, or provider, a solid understanding of Ambulatory Payment Classification Codes is key to navigating the complex world of outpatient billing.
Understanding Dental Coding: A Key to Accurate Insurance Claims
Dental coding plays a vital role in streamlining the communication between dental practices and insurance companies. Accurate dental coding ensures that the services provided are correctly represented, leading to timely and proper reimbursement.
One of the most important elements in dental coding is the use of CDT Codes in Dental Coding. These Current Dental Terminology (CDT) codes are maintained by the American Dental Association and provide a standardized way to report dental procedures and services. Using the correct CDT Codes in Dental Coding helps avoid confusion, claim rejections, and delays in payment.
When submitting dental coding for insurance claims, precision is essential. Each code must match the treatment actually performed, along with the appropriate documentation. Inaccurate coding not only impacts reimbursement but can also lead to compliance issues or audits. That's why staying updated on the latest CDT Codes in Dental Coding is critical for both dental staff and billing professionals.
Moreover, effective dental coding for insurance claims goes beyond just assigning the right code. It involves understanding payer requirements, attaching relevant diagnostic information, and verifying patient coverage. A small mistake in dental coding can result in denied claims or financial loss for the practice.
In conclusion, mastering dental coding is crucial for dental practices aiming to maintain financial health and ensure a smooth revenue cycle. By properly using CDT Codes in Dental Coding and following best practices in dental coding for insurance claims, dental professionals can minimize errors and enhance claim approval rates. Whether you're a billing specialist or a dental provider, investing time in learning and applying correct dental coding techniques is a smart move toward operational success.
0 notes
Text
Medical Billing vs. Medical Coding: Key Differences Every Healthcare Professional Must Know
Medical billing vs.Medical Coding: Key Differences Every Healthcare Professional Must Know
Introduction
In the complex world of healthcare governance, understanding the roles of medical billing and medical coding is vital for ensuring smooth operations and maximized revenue. These two functions, although closely intertwined, serve distinct purposes within the healthcare revenue cycle. For healthcare professionals, administrative staff, and students entering the healthcare industry, distinguishing between medical billing and medical coding can streamline workflows, improve communication, and prevent costly errors.
This comprehensive guide will explore the differences between medical billing and medical coding, their roles in healthcare, benefits, and practical tips to master these key aspects of healthcare administration.
Understanding Medical Coding
What Is Medical Coding?
Medical coding is the process of translating healthcare diagnoses, procedures, medical services, and equipment into standardized codes. These codes facilitate accurate documentation, billing, and data analysis within the healthcare system.
The Role of Medical Coders
Review medical records to identify diagnoses and procedures
Assign appropriate coding systems like ICD-10-CM, CPT, and HCPCS Level II
Ensure compliance with healthcare regulations and standards
Maintain accurate and detailed documentation for insurance claims and legal purposes
Key Coding Systems
System
Purpose
Examples
ICD-10-CM
diagnoses classification
F32.1 - Major depressive disorder, single episode
CPT
Procedures and Services
99213 – Office or other outpatient visit
HCPCS Level II
Supplies, equipment, and services
J1885 – Injection, Ketorolac, per 15 mg
Why Medical Coding Matters
Accurate medical coding ensures:
Proper reimbursement from insurance companies
Compliance with healthcare regulations
Reliable health data for research and policy-making
Improved patient record keeping
Understanding Medical Billing
What Is Medical Billing?
Medical billing involves generating and submitting claims to insurance companies or patients for payment.It focuses on the financial aspect of healthcare delivery, ensuring providers are compensated for their services.
The Role of Medical Billers
Create accurate insurance claims based on coded data
Submit claims electronically or via paper to payers
Follow up with insurance companies for claim status
Manage patient billing,payments,and collections
Handle denials and resubmit claims as necessary
Key Billing Processes
Verification of patient insurance eligibility
Calculation of patient balances and out-of-pocket expenses
payment posting and reconciliation
Patient invoicing and communication
Why Medical Billing Is Critical
Effective medical billing directly impacts:
Healthcare practise revenue and cash flow
Patient satisfaction and financial openness
compliance with billing regulations and legal standards
Minimization of billing errors and claim rejections
Key Differences Between Medical Billing and medical Coding
Feature
Medical Coding
Medical Billing
Primary Focus
translating healthcare services into codes
Submitting claims and managing payments
process Stage
Preliminary; occurs before billing
Final step; after coding
Core Tasks
Assigning ICD,CPT,HCPCS codes
Claim submission,follow-up,and collections
Skills Needed
Attention to detail,knowledge of coding systems,regulatory compliance
Communication,negotiation,knowledge of insurance processes
output
Accurate medical codes and documentation
Paid claims or denials for reimbursement
Impact
Ensures proper billing and compliance
Maintains revenue flow and cash reserves
Interdependence of medical Coding and billing
While they serve different functions,medical coding and billing are interconnected. Accurate coding is essential for prosperous billing, as incorrect codes can lead to claim denials, delays, or underpayment.Conversely, skilled billers understand coding intricacies to optimize reimbursement.
Benefits of Mastering Both Skills
Enhanced revenue cycle management: Proper coding and billing streamline cash flow.
Reduced claim rejections: Accurate data minimizes errors and appeals.
Compliance assurance: Following coding and billing regulations prevents legal issues.
Career advancement: Skills in both areas make healthcare professionals more versatile and valuable.
Practical Tips for Healthcare Professionals
Invest in continuous education: Stay updated with coding updates like ICD-10 changes and billing regulations.
Use reliable software tools: Implement certified EHR and billing software to reduce errors.
Double-check documentation: Ensure medical records are accurate and complete before coding and billing.
Communicate effectively: Maintain open lines between coders, billers, and clinicians to clarify procedures and diagnoses.
Regularly review denial reports: Analyze claim rejections to identify and correct patterns.
Case Study: Streamlining Medical Billing and Coding
ABC Medical Clinic faced a 15% claim rejection rate, impacting its revenue.upon assessing their process,they invested in comprehensive coding training and integrated a modern billing software system. As a result, they saw:
Reduction of claim rejections by 40%
Faster reimbursement cycles
Improved patient satisfaction due to clear billing
This case exemplifies how understanding and properly implementing medical billing and coding can considerably enhance a healthcare provider’s financial health.
First-Hand Experiance: The Healthcare Professional’s Perspective
“being proficient in both medical coding and billing has transformed how I manage patient records and revenue. It’s rewarding to see fewer claim rejections and quicker payments, which allows us to focus more on patient care instead of administrative hassles.” – Jane D., Medical Billing Specialist
Conclusion
Understanding the key differences between medical billing and medical coding is essential for healthcare professionals aiming to optimize their practice’s revenue cycle management.While coding focuses on translating healthcare services into standardized codes, billing ensures those codes are accurately submitted for reimbursement. Mastering both functions not onyl enhances financial stability but also improves compliance, efficiency, and patient satisfaction.
If you’re involved in healthcare administration, investing in training and tools to develop expertise in both areas can provide long-term benefits. By staying informed and proactive,you can help your practice thrive in today’s dynamic healthcare environment.
For more insights on healthcare administration, coding, and billing best practices, subscribe to our newsletter or contact our training experts today!
https://medicalcodingandbillingclasses.net/medical-billing-vs-medical-coding-key-differences-every-healthcare-professional-must-know/
0 notes
Text
Secure and Compliant Billing Across Massachusetts and New Jersey
In today's healthcare landscape, accurate and compliant billing is not optional—it’s essential. Clinics, hospitals, and healthcare providers in Massachusetts and New Jersey must navigate a maze of insurance guidelines, federal regulations, and payer-specific requirements, all while delivering exceptional patient care. One misstep in billing can lead to denied claims, revenue loss, audits, or even legal trouble.
That’s why secure and compliant billing has become the cornerstone of successful medical practices across these states. Whether you're managing a small specialty clinic in Boston or a multi-location healthcare group in Newark, choosing the right billing partner or optimizing your in-house systems is critical to achieving long-term financial success and regulatory peace of mind.
This comprehensive guide explores everything providers need to know about maintaining security and compliance in medical billing across Massachusetts and New Jersey.
The Importance of Secure and Compliant Medical Billing
1. Protecting Patient Information
Security in medical billing starts with protecting protected health information (PHI) under the Health Insurance Portability and Accountability Act (HIPAA). Any billing operation—whether in-house or outsourced—must follow strict guidelines for:
Data encryption
Secure transmission of EHR/EMR data
Staff training on privacy policies
Risk assessments and data breach protocols
In both New Jersey and Massachusetts, non-compliance can lead to:
Civil monetary penalties
License suspensions
Reputational damage
2. Ensuring Regulatory Compliance
Beyond HIPAA, billing teams must also follow regulations such as:
CMS billing and coding guidelines
State Medicaid program policies
Private payer contracts
The False Claims Act (FCA)
OIG Compliance Program Guidance
Failure to comply can lead to audits, clawbacks, and lost reimbursement. Clinics that invest in compliant billing practices have higher success rates in claims processing and lower chances of financial penalties.
Challenges Unique to Massachusetts and New Jersey
Massachusetts: Progressive and Complex
Massachusetts, known for its universal health coverage policies and advanced healthcare systems, brings both opportunities and challenges for billers.
MassHealth Requirements: The state’s Medicaid program includes specialized billing rules for behavioral health, long-term services, and pediatric care.
Academic Affiliations: Many clinics are tied to teaching hospitals, which require accurate split billing between institutional and professional services.
Frequent Audits: With robust healthcare oversight, providers are often audited to ensure compliance with billing protocols.
New Jersey: Diverse and Dynamic
New Jersey clinics deal with a diverse patient population, payer mix, and service offerings. Key challenges include:
New Jersey Medicaid (NJ FamilyCare): Each MCO (Managed Care Organization) has unique claim filing requirements.
High Volume Practices: Urgent care, family medicine, and multi-specialty practices often experience fast-paced, high-volume operations.
Urban vs. Suburban Dynamics: Urban clinics need multilanguage billing support; suburban areas see a higher proportion of commercial payers and employer-sponsored plans.
What Secure and Compliant Billing Looks Like in Practice
Let’s break down the foundational components of a secure and compliant billing strategy.
1. HIPAA-Compliant Infrastructure
Every billing system must comply with HIPAA Security Rule standards, including:
Secure servers with encryption for all PHI
Role-based access controls for staff
Automatic logout and session timeouts
Regular system audits and penetration testing
Whether you use third-party billing software or in-house systems, data integrity and protection must be prioritized.
2. Certified Medical Coders and Billers
Hiring or partnering with certified professionals (CPC, CPB, or CCS-P) ensures accurate code assignments and familiarity with:
ICD-10 for diagnoses
CPT/HCPCS for procedures
Modifers (25, 59, 95, etc.)
E&M coding updates
Incorrect coding can lead to upcoding, undercoding, or bundling issues, all of which can trigger audits and repayment demands.
3. Audit-Ready Documentation
In New Jersey and Massachusetts, state Medicaid and private payers frequently perform post-payment audits. A compliant billing operation includes:
Proper clinical documentation
Signed patient consent and insurance forms
Time-based notes for therapy/behavioral health
Easy-to-retrieve audit logs
4. Compliance Policies and Training
Every billing department or partner should have written policies for:
Coding compliance
Claim submission timelines
Data security protocols
Staff responsibilities and reporting procedures
Regular training ensures that staff remain updated with CMS rules, state Medicaid policies, and annual coding updates.
Common Billing Risks and How to Avoid Them
1. Fraudulent Claims
Billing for services not rendered, unbundling procedures, or altering diagnosis codes are considered fraud under the False Claims Act. Avoid this by:
Implementing strict claim review processes
Maintaining clinical documentation that supports each claim
Using coding audits to catch patterns or anomalies
2. Data Breaches
A HIPAA violation involving exposed PHI can lead to thousands of dollars in fines. Prevent breaches by:
Using secure cloud billing systems
Enforcing multi-factor authentication
Restricting access to authorized users only
3. Duplicate Billing
This error often occurs due to poor system integration or manual oversight. It can result in claim denials or payer blacklisting. Solutions include:
Integrated EHR and billing systems
Automated alerts for duplicate claims
Weekly reconciliation reports
4. Underpayments and Lost Revenue
Missing modifiers, incorrect place of service (POS), or failing to verify insurance can lead to lower reimbursements. Stay compliant and profitable by:
Running pre-bill audits
Conducting regular payment posting reviews
Appealing underpaid or denied claims promptly
The Role of Technology in Secure Billing
Modern billing relies heavily on advanced technologies for compliance and security. Key tools include:
1. Electronic Health Records (EHR)
EHR systems like Epic, Athenahealth, and eClinicalWorks offer built-in compliance checks, audit trails, and HIPAA-compliant interfaces that protect patient data and improve coding accuracy.
2. Claims Scrubbing Software
Scrubbers check claims for coding or data errors before submission. This reduces denials, improves first-pass rates, and ensures payer compliance.
3. Secure Patient Portals
Allowing patients to pay bills or verify insurance through encrypted portals enhances data security and supports billing transparency.
4. AI and Predictive Analytics
Artificial intelligence tools can:
Predict claim outcomes
Highlight documentation gaps
Detect fraud patterns
Suggest the correct codes based on chart notes
These tools significantly reduce compliance risks and support proactive billing strategies.
Best Practices for Massachusetts and New Jersey Clinics
1. Implement a Compliance Plan
The Office of Inspector General (OIG) recommends every healthcare provider have a formal compliance program. Your plan should include:
Compliance officer or designated staff
Written policies and procedures
Monitoring and internal audits
Corrective action plans
2. Schedule Regular Internal Audits
Internal audits identify potential compliance gaps. Focus on:
High-volume CPT codes
Time-based billing (for therapy and counseling)
Use of modifiers
Patient eligibility logs
3. Stay Updated on Regulatory Changes
Both states frequently update Medicaid policies. CMS also releases quarterly and annual changes to CPT/HCPCS/ICD-10 codes. Assign a staff member or partner with a medical billing services in Massachusetts and New Jersey that tracks these changes in real-time.
4. Train Staff Continuously
Front desk staff, coders, and billers must undergo regular training on:
Insurance verification
Coding updates
Data security protocols
Documentation standards
Benefits of Outsourcing to Secure and Compliant Billing Services
Partnering with a trusted billing company in NJ or MA offers several advantages:BenefitDescriptionLower Compliance RiskProfessional billing services stay current with all HIPAA and CMS updatesImproved Cash FlowFaster, cleaner claims result in more predictable revenueCredentialing SupportMany billing companies also handle insurance credentialing and contract negotiationsScalabilityEasy to manage billing as your practice growsAdvanced ReportingTrack compliance KPIs like denial rate, clean claim rate, and days in A/R
What to Look for in a Billing Partner
When choosing Medical billing services in New Jersey or Massachusetts, ensure they offer:
State-specific expertise
HIPAA-certified staff and software
On-shore processing (no overseas data exposure)
Real-time reporting
Secure data backup and disaster recovery protocols
Ask about their compliance training programs, audit support services, and how they handle changes in state or federal billing regulations.
Real-World Impact: Success Stories
Massachusetts Mental Health Group
A behavioral health group in Worcester faced regular Medicaid denials due to incorrect use of modifiers and incomplete documentation. After switching to a compliant billing service:
Denials dropped by 68%
Reimbursement increased by 22% within 6 months
They passed a MassHealth audit with no findings
Multispecialty Clinic in New Jersey
A large clinic in Jersey City experienced a data breach due to outdated billing software. By outsourcing to a secure billing provider:
All PHI was encrypted and backed up in secure cloud servers
Staff received cybersecurity and HIPAA training
The clinic improved patient trust and avoided future fines
Looking Ahead: The Future of Secure Billing
Healthcare billing in New Jersey and Massachusetts will continue to evolve. Clinics should prepare for:
Increased payer scrutiny and audits
Value-based payment models
Integrated RCM and EHR systems
Blockchain-based health record security
Stricter state-specific compliance laws
Providers who invest in secure, forward-thinking billing systems will be well-positioned to meet future demands.
Conclusion
Secure and compliant billing is more than just accurate coding and claim submission—it’s about building a sustainable, audit-ready, and trusted healthcare practice. For clinics across Massachusetts and New Jersey, this means investing in the right technology, training, and professional support.
Whether you manage a behavioral health clinic in Boston or a family medicine group in Trenton, your revenue and reputation depend on maintaining the highest standards in billing. By aligning with secure and compliant billing practices—or partnering with a professional service—you safeguard your patients, your practice, and your future.
0 notes
Text

Struggling with staff turnover, high billing costs, and inconsistent collections? ICS’s FTE model offers certified, full-time medical billing professionals — starting at just $7.5/hour. You get a dedicated coder or biller who works exclusively with your practice, just like an in-house team member. Our FTEs are trained in over 100 specialties and familiar with 40+ EMR/PM platforms like eClinicalWorks, NextGen, Kareo, and more. With 24/7 availability, HIPAA-compliant operations, and KPI-driven performance tracking, our FTE model delivers quality, transparency, and cost control. Clients using ICS’s FTE services have seen: ✔️ 30% increase in revenue ✔️ 25% fewer denials ✔️ 35% savings compared to U.S.-based billing hires Whether you're a solo provider or large group practice, our FTE model scales as you grow — without sacrificing compliance or quality.
To know how ICS’s FTE model can transform your medical billing operations at https://infohubconsultancy.com/full-time-equivalent-model/
Want a full-time billing team at just $7.5/hour? Visit www.infohubconsultancy.com, or email [email protected] to request an FTE quote.
#FTEEmployeeinMedicalBillingServices#FTEEquivalentOutsourceMedicalBillingServices#FTEinMedicalBilling#FullTimeEquivalent(FTE)ModelForOutsorceMedicalBillingandCoding
0 notes
Text
Cloud-Based Revenue Cycle Management Solutions: Pros, Cons & Future Trends
In today’s dynamic healthcare landscape, financial operations are as critical as patient care. Managing the flow of revenue—from appointment scheduling and insurance verification to billing and payment collection—requires a robust system known as revenue cycle management in medical billing. As healthcare providers face increasing complexities, many are turning to cloud-based revenue cycle management solutions. But what exactly do these systems offer? What are their drawbacks, and what does the future hold?
This blog delves deep into the pros, cons, and emerging trends shaping cloud-based revenue cycle management, providing insights for any healthcare practice or revenue cycle management company seeking to stay ahead.
Understanding Revenue Cycle Management in Healthcare
Before diving into cloud-based solutions, let’s briefly revisit what revenue cycle management in medical billing entails. At its core, it refers to the financial process healthcare facilities use to track patient care episodes from registration and appointment scheduling to the final payment of a balance.
Effective revenue cycle management ensures:
Accurate patient information and insurance verification
Proper coding of services for insurance claims
Timely billing and follow-ups
Denial management and appeals
Transparent patient payment processes
Traditionally, many hospitals and clinics relied on on-premises software managed by internal IT teams or outsourced to a revenue cycle management company. However, with the digital revolution, cloud-based systems are rapidly gaining traction.
What Are Cloud-Based Revenue Cycle Management Solutions?
Cloud-based revenue cycle management (RCM) solutions are software applications hosted on secure, remote servers. Instead of managing infrastructure on-site, healthcare organizations access these systems over the internet.
This model offers several advantages over traditional on-premises setups:
Reduced IT infrastructure costs (no need for costly servers or constant hardware upgrades)
Automatic software updates
Scalability to match growing patient volumes or new service lines
Remote accessibility, enabling staff and billing partners to work from anywhere
Given these benefits, it’s no surprise that a revenue cycle management company often integrates cloud-based systems into its offerings for clients.
The Pros of Cloud-Based Revenue Cycle Management Solutions
1. Cost Efficiency
One of the standout benefits is cost savings. Cloud-based systems operate on a subscription model, eliminating hefty upfront costs associated with hardware purchases and on-premises software licenses. This is especially beneficial for small to mid-sized practices that might not have deep capital reserves.
A revenue cycle management company leveraging the cloud can also pass these savings on to clients, offering more competitive pricing.
2. Enhanced Data Security and Compliance
Many healthcare organizations initially feared that storing sensitive patient data offsite could expose them to breaches. However, most reputable cloud vendors invest heavily in security—often more than individual hospitals could afford. Encryption, intrusion detection, and 24/7 monitoring are standard. They also ensure compliance with HIPAA and other regulations governing revenue cycle management in medical billing.
3. Better Scalability and Flexibility
As practices grow, add locations, or integrate telehealth services, their RCM needs evolve. Cloud-based systems easily scale to accommodate new workflows, user accounts, and patient volumes without major infrastructure overhauls.
4. Improved Accessibility and Collaboration
Since data is hosted online, billing staff, coders, and even a revenue cycle management company can access records from anywhere. This is critical in today’s hybrid work environment. Whether it’s remote medical coders or offsite patient support teams, cloud platforms ensure seamless collaboration.
5. Real-Time Analytics and Reporting
Modern cloud-based RCM platforms provide powerful dashboards and analytics. This empowers providers and their partners to monitor KPIs like denial rates, days in A/R (accounts receivable), and collections—helping identify bottlenecks in revenue cycle management in medical billing early.
The Cons of Cloud-Based Revenue Cycle Management Solutions
Despite the numerous advantages, cloud-based RCM solutions are not without challenges.
1. Dependence on Internet Connectivity
Since these systems are accessed online, any disruption in internet connectivity can hamper operations. Practices in rural areas or regions with unreliable internet may face occasional access issues.
2. Data Migration Complexities
Switching from legacy systems to a cloud-based platform requires careful data migration. Errors during this process can lead to missing or corrupted patient records, which directly impacts revenue cycle management in medical billing.
3. Vendor Reliability Concerns
Entrusting critical financial data to an external provider means practices must thoroughly vet vendors. Not all offer the same level of uptime guarantees or customer support. A subpar vendor could result in costly downtime.
4. Recurring Costs Over Time
While the subscription model minimizes upfront costs, over many years, continuous monthly or annual fees could add up. It’s essential for healthcare practices or a revenue cycle management company to conduct a total cost of ownership (TCO) analysis before switching.
Why Revenue Cycle Management Companies Prefer Cloud Solutions
Many modern revenue cycle management companies champion cloud-based solutions for their clients because it simplifies operations across multiple practices and specialties.
These companies often:
Deploy standardized cloud platforms that integrate with various EHR/EMR systems.
Offer consolidated reporting dashboards across multiple providers.
Use cloud-based AI tools for denial prediction or to flag coding inconsistencies.
Provide flexible remote billing services, made possible through secure cloud access.
The scalability and interoperability of cloud systems allow a revenue cycle management company to onboard new clients quickly, reduce IT complexities, and deliver consistent quality.
Future Trends in Cloud-Based Revenue Cycle Management
Looking ahead, several exciting trends are shaping the future of cloud-based revenue cycle management in medical billing.
1. AI and Machine Learning Integration
Expect deeper integration of AI to:
Predict claims likely to be denied and suggest corrections before submission.
Automate charge capture and coding from physician notes.
Identify patterns of underpayments.
This proactive approach could significantly boost collections.
2. Patient-Centric Billing Experiences
As high-deductible health plans become common, patient collections form a growing slice of revenue. Cloud platforms are evolving to offer self-service portals, transparent cost estimations, and digital payment options. A revenue cycle management company leveraging such tools can greatly enhance patient satisfaction.
3. Interoperability with Emerging Health Tech
Cloud-based systems are increasingly designed to integrate seamlessly with wearable devices, telehealth platforms, and even home health monitoring tools. This ensures that billing and coding accurately reflect modern care delivery models.
4. Blockchain for Audit Trails
Some innovators are exploring blockchain to maintain immutable records of billing activities. This could streamline audits, reduce fraud, and instill more trust in the revenue cycle management in medical billing process.
5. Predictive Financial Modeling
Advanced cloud analytics are helping CFOs and practice managers forecast cash flows based on patient demographics, payer mix, and historical data. This empowers smarter strategic decisions.
How to Choose the Right Cloud-Based RCM Solution
Whether you’re a hospital evaluating internal systems or a revenue cycle management company selecting software for clients, keep these factors in mind:
✅ Compliance and Security: Does the vendor offer HIPAA-compliant data centers? What about SOC 2 certifications? ✅ Integration Capabilities: Can it easily connect with your existing EHR, practice management, or laboratory systems? ✅ Custom Reporting: Are dashboards configurable to track your unique KPIs? ✅ User Training & Support: Does the vendor provide robust onboarding and 24/7 support? ✅ Scalability: Will the platform grow with your organization without frequent costly upgrades? ✅ Transparent Pricing: Understand the full pricing structure—monthly fees, transaction costs, data storage, and any hidden charges.
The Bottom Line
Cloud-based revenue cycle management solutions represent a powerful evolution in healthcare financial operations. They offer compelling benefits—cost efficiency, scalability, and advanced analytics—that directly enhance revenue cycle management in medical billing. For healthcare organizations and every revenue cycle management company, adopting cloud platforms is often a strategic move to stay competitive.
However, it’s essential to weigh these benefits against potential challenges, such as vendor reliability and long-term subscription costs. By choosing the right partner and leveraging future-focused features like AI and patient-centric billing tools, providers can transform their revenue cycles into engines of growth and stability.
Final Thoughts
As the healthcare industry continues its digital transformation, the question is no longer if you should adopt cloud-based RCM solutions, but how quickly. Those who move thoughtfully—selecting secure, interoperable, and analytics-driven platforms—will be best positioned to navigate the evolving landscape of revenue cycle management in medical billing.
For clinics, hospitals, and any revenue cycle management company, staying ahead of these trends is crucial. The future of RCM is undoubtedly in the cloud—bringing greater efficiency, smarter insights, and a more patient-friendly financial experience.
0 notes