#DCCT
Explore tagged Tumblr posts
Text

#mood
#mood#down to my 99th string gavel at this point#i wish i could say i shouldn't have gotten out of bed this morning but i kind of haven't#mark mckinney#death comes to town#dcct#kith#kids in the hall#the kids in the hall
2 notes
·
View notes
Text
0 notes
Text
@thezombieprostitute does it, I also need to do it:
Work on editing Want To Be Loved By You 😔 and post it
Edit the next part of Dreams can come True... And post it
Type out the next part of Pulling against the Stream the sequel parts (short but it's still Mermay so I should do this!)
Continue writing on... Whatever wips. But mostly DCCT and my Nick fowler one.
Reading! Reading all the stories, I'm so behind! This week I have a constant zoom tone in my head and it's been hard to rest or focus, and it's taking me out, but I want to go and reblog and do this!
...I should continue working on my Lord au stories, it just takes forever.
Moodboards
15 notes
·
View notes
Text
The blood work is in: Not diabetic, not pre-diabetic, not close to anything like a risk of becoming pre-diabetic, actually incredibly low levels of anything like that, HbA1c levels like a champion.[1][2][3]
---
[1]Wikipedia: "In general, the reference range (that found in healthy young persons), is about 30–33 mmol/mol"
[2]Also Wikipedia: The International Diabetes Federation and the American College of Endocrinology recommend HbA1c values below 48 mmol/mol (6.5 DCCT %), while the American Diabetes Association recommends HbA1c be below 53 mmol/mol (7.0 DCCT %) for most patients.
[3]Me: So 29 is fine, right?
#Still big though!#Still a 260 pound middle aged dude#sitting in an office most of the day every day#BUT#CRITICALLY#Not getting diabetic from it
15 notes
·
View notes
Text
Islet Transplantation Pancreatic Islet Transplantation Advancements in the areas of beta cell replacement and islet transplantation are slow in coming and the latest long-term success rates are disappointing, as less than 14% of transplant recipients remain free of insulin therapy after two years (Mayo, p. 1). In type 1 diabetes, the body destroys its own insulin producing cells. The body's immune system attacks and destroys cells in the pancreas called beta cells. These cells are contained within small islands of endocrine cells called pancreatic islets. In 1993 the Diabetes Control and Complications Trial (DCCT) established the modern standard of care for the medical management of type 1 diabetes mellitus. The DCCT assigned 1441 patients to intensive or conventional treatment. The first step included daily determinations of blood glucose levels several times daily at home by finger stick; then daily injections of long-, intermediate-, and short-acting insulin; accompanied by dietary and psychological support (Robertson, p. 694). Diabetic complications may include hypoglycemia, diabetic hyperosmolar syndrome, diabetic ketoacidosis, neuropathy, nephropathy, retinopathy, heart and blood vessel disease, and increased risk of infection. Controlling the disease is difficult. Monitoring blood glucose, eating a healthy diet, getting daily exercise, and maintaining a healthy weight are part of maintenance. Medical therapies for managing diabetes include the use of insulin to manage type 1 and type 2 diabetes and the use of sulfonylureas, meglinitides, biguanides, alpha glucosidase inhibitors, thiazolidinediones, and drug combinations to manage type 2 diabetes (Collazo-Clavel, p. 5). For decades, researchers have searched for ways to restore blood sugar control through human islet transplantation, a procedure in which only the islets that contain insulin-producing beta cells are transplanted. In 2000, the Edmonton Protocol brought attention to a novel approach for islet transplantation. This transplantation method used a larger quantity of islets and a combination of drugs that was less toxic to suppress the immune system. Healthy islets are isolated from a donor pancreas, purified, and then infused through a small tube into the portal vein of the liver. Patients must take immunosuppressive drugs to keep their bodies from rejecting the new islets. When successful, islet transplantation can restore normal blood sugar without the need for insulin injections and can improve quality of life. Islet transplants are still experimental, so they are available only to people who participate in a clinical study and meet specific criteria (U.S., p. 1). Replacing these cells via transplantation has been the subject of research for many years. Transplantation of beta cell containing islets is less invasive than transplanting a whole pancreas, which was the established procedure before 1993. In a procedure called islet transplantation, islets are transferred into a faulty pancreas from a healthy donor pancreas. The beta cells in these islets begin to make and release insulin, once implanted. Researchers hope that islet transplantation will help people with type 1 diabetes live without daily injections of insulin. (Pancreatic, p. 1) The Islets of Langerhans The pancreas makes enzymes and insulin that help digest and use food. Spread over the pancreas are clusters of cells called the islets of Langerhans. Islets are made up of two types of cells: alpha cells, which make glucagon, a hormone that raises the level of glucose (sugar) in the blood, and beta cells, which make insulin. Insulin, a hormone, helps the body use glucose for energy. If beta cells do not make enough insulin, diabetes develops. In type 1 diabetes, an autoimmune process causes insulin shortage by the body's immune system destroying the beta cells. Having reported their findings in the June 2000 issue of the New England Journal of Medicine, researchers at the University of Alberta in Edmonton, Canada, continue to use the Edmonton protocol to transplant pancreatic islets into people with type 1 diabetes. In 2000, a multi-center clinical trial of the Edmonton protocol for islet transplantation took place, and the promising results were announced. According to the Immune Tolerance Network (ITN), in June 2003, about 50% of the patients remained insulin-free up to 1-year after receiving a transplant. A clinical trial of the Edmonton protocol also was conducted by the ITN, funded by the National Institutes of Health and the Juvenile Diabetes Research Foundation International. (Pancreatic, p. 1). This year (2006), further trials on an international scale were reported in the New England Journal of Medicine. Believing that islet transplantation offers the best potential to improve glycemic control in type 1 diabetics, an international, multicenter trial to explore the feasibility and reproducibility of islant transplantation was done with the use of a single common protocol, the Edmonton protocol. 36 subjects with type 1 diatetes mellitus underwent islent transplantation at nine international sites. Islets from the pancreases of deceased donors were transplanted within 2 hours after purification, without culture. The goal was defined to be insulin independence with adequate glycemic control after one year following the final transplantation. Of the 36 subjects, 44% met the goal, 28% had partial function and 28% had complete graft loss. The 21 subjects who attained insulin independence had good glycemic control throughout the trial. 76% of these, however, required insulin again at two years, while 31% remained insulin-free at two years (Shapiro, p. 1330). In this procedure, researchers use specialized enzymes to remove islets from the pancreas of a deceased donor. Because the islets are fragile, transplantation occurs very soon after they are removed from the deceased donor. (Pancreatic, p. 1) Ultrasound is used by the surgeon during the transplant to guide placement of a small plastic tube (catheter) through the upper abdomen into the liver. The islets are injected through the catheter into the liver. The patient may receive a local anesthetic or general anesthesia while the surgeon does the transplant through a small incision. Risks include bleeding or blood clots. It takes awhile for cells to attach to new blood vessels in the recipient patient, to begin releasing insulin. The doctor orders tests to check blood glucose levels after the transplant, and insulin may be needed until control is achieved.(Ibid.) Transplantation: Benefits, Risks, and Obstacles Islet isolation and purification, transplantation, and other new strategies toward tolerance induction have been researched in recent years. Islet cell transplantation can be performed as a percutaneous minimally invasive procedure. Islets are infused into the liver via the portal vein. This transplantation modality could circumvent the organ shortage that prevents most patients with diabetes who are eligible from pancreas transplantation from actually receiving a graft. The graft offers the possibility of maintaining a healthy pancreas without chronic immunosuppressive drugs when the induction of donor-specific tolerance or immuno-isolation emerge as clinical strategies (Sperling, pp. 529-552). The goal of islet transplantation is to infuse enough islets to control blood glucose level without insulin injection. A typical transplant requires about 1 million islets, extracted from two donor pancreases for an average-size person (70 kg). Because good control of blood glucose may slow or prevent progression of diabetic complications such as nerve or eye damage, a successful transplant may reduce the risk of these complications. But a transplant recipient still needs to take immunosuppressive drugs to stop the immune system from rejecting the transplantation. (Pancreatic, p. 1) Researchers seek new approaches to allow successful transplantation without immunosuppressive drugs, "thus eliminating the side effects that may accompany their long-term use." (Ibid.) Nine patients who became diabetic after upper-abdominal exenteration and liver transplantation were given pancreatic islet-cell grafts obtained from the liver donor (eight cases), a third-party donor (one), or both (four). Two of the diabetic patients died of infections after 48 and 109 days, and a third patient died of tumor recurrence after 178 days. The other 6 survived 101-186 days postoperatively, and five remained insulin-free or on insulin only during night-time parenteral alimentation. C-peptide increased 1.7 to 3.3 fold in response to intravenous glucose in these five patients who have had glycosylated hemoglobin in the high normal range. The kinetics of the C-peptide responses to intravenous glucose in all eight patients revealed no first-phase release and delayed peak response consistent with transplantation and/or engraftment of a suboptimal islet cell mass. "The longest survivor, who requires neither parenteral alimentation nor insulin, is the first unequivocal example of successful clinical islet-cell transplantation." (Tzakis, p. 1323) Rejection is the biggest problem with any transplant. The immune system is programmed to destroy bacteria, viruses, and tissue it recognizes as "foreign," including transplanted islets. Immunosuppressive drugs are needed to keep the transplanted islets functioning. Immunosuppressive Drugs The Edmonton protocol uses a combination of immunosuppressive drugs, also called antirejection drugs, including dacliximab (Zenapax), sirolimus (Rapamune), and tacrolimus (Prograf). Dacliximab is given intravenously right after transplantation and discontinued. Sirolimus and tacrolimus, the two main drugs that keep the immune system from destroying the transplanted islets, must be taken for life (Pancreatic, p. 1). In the 35 years since the first vascularized (using blood vessels) pancreas transplant was performed in Minneapolis, Minnesota to prevent recurrent nephropathy (kidney disease) in a concomitant renal (kidney) transplant, an estimated 12,000 procedures have been performed in this country. This number is nevertheless insignificant compared to the estimated one million patients with type 1 diabetes. However, what was once a slow journey has recently gathered momentum with the introduction of "more flexible immunosuppression protocols, the ability to individualize surgical options to patient needs, and the dramatic improvement of isolated islet transplantation results." (Allen, p. 3485) Researchers use pancreas transplant options and advanced surgical techniques, but the donor pancreas and surgical complications, as well as the type of immunosuppression affect the outcome of islet transplantation. The immunosuppressive drugs have significant side effects and long-term effects are still not known. Known side effects of immunosuppressive drugs include mouth sores and gastrointestinal problems, such as stomach upset or diarrhea. Patients also have experienced increased blood cholesterol levels, decreased white blood cell counts, decreased kidney function, and increased susceptibility to bacterial and viral infections. Taking immunosuppressive drugs increases the risk of tumors and cancer as well. Progress on whole pancreas and beta cell transplantation has been hampered by the lack of available organs and the question of immunosuppression. The Center for Islet Cell Transplantation is a project with the goal of successful transplantation of beta cells without immunosuppression. Alternative approaches to islet transplantation under investigation include mixed bone marrow chimerism and co-stimulatory blockade. Another alternative to islet transplantation pursued for many years with varying success is the approach of shielding the islets from the immune system with a physical barrier while allowing the islets to receive nutrients and the insulin generating signals they need to produce the necessary insulin, then moving them through the barrier to the bloodstream. Techniques for accomplishing this include microencapsulation and a bioartificial pancreas. Other aspects that investigators are investigating include alloreactivity and autoreactivity. Also, who might benefit most from transplantation needs to be addressed (Clark, p. 52). Insulin-secreting pancreatic beta cells derived from stem cells -- pending availability -- may be eventually transplanted into patients to help maintain blood glucose homeostasis. The relative success of the transplantation of cadaveric beta cells into patients with type 1 diabetes provides support for this approach (Stanier, p. 521) An islet cell transplant may be an option for severe type 1 diabetes that can not be effectively managed with insulin or leads to complications. Because the procedure is still considered experimental in the United States, receiving it usually means participating in a clinical trial. Available organs usually are first allocated to people waiting to receive whole pancreas transplants. If a patient is accepted into a trial, they will need to wait for a donor pancreas. If a match can not be made, an organ is then allocated to a person on the islet cell transplant list. What happens during and after the transplant? An islet cell transplant begins with technicians extracting and purifying islet cells from a donor pancreas. Often, two or more donor organs are needed to accumulate enough islet cells for a single complete transplant. An interventional radiologist performs the actual islet cell transplant. This specialist and the radiologist direct a tube through an opening made in the abdomen to the portal vein, a blood vessel leading into the liver. They then infuse the islet cells through the tube to the liver, where the cells take up residence in the organ's small blood vessels. The liver is a good site for the islet cell transplant because it is more accessible than the pancreas, and the cells produce insulin well in that environment (Mayo, p. 1). Possible risks during surgery include bleeding or blood clots. After the transplant, the new islet cells need time to start working. The transplant team closely monitors blood sugar level and give insulin as needed. If the transplant is successful, the amount of insulin needed is gradually reduced as new cells take over. Because the immune system may try to reject new cells, patients take medications that suppress the immune system. These medications may cause noticeable side effects, such as weight gain, acne, facial hair, stomach upset or diarrhea, but the effects decrease as time goes on. The post-transplant treatment is a delicate balancing act between preventing rejection and managing unwanted side effects. A doctor monitors treatment of the patient closely and adjusts medication and care as needed. Intensive care also fosters higher success rates. (Mayo, p. 1) Clinical outcomes in terms of secondary complication rates were much better in the intensively treated group than in the conventionally treated group. Therefore, intensive treatment became the norm. More recent improvements in home care have also improved outcomes (Robertson, p. 694). Intensive care includes pancreas and islet cell transplantation. In the 35 years since the first vascularized (with blood vessels) pancreas transplant was performed in Minneapolis, Minnesota to prevent recurrent nephropathy (kidney disease) in a concomitant renal (kidney) transplant, an estimated 12,000 islet transplantation procedures have been performed in the U.S. While this represents a major achievement, it is insignificant compared to the estimated one million patients with type 1 diabetes. The initially slow journey has gained momentum with the dramatic improvement of isolated islet transplantation results. With more flexible immunosuppression protocols, and the ability to individualize surgical options to patient needs, numbers have improved when intensive care is utilized (Allen, p. 3485). A major obstacle to widespread use of islet transplantation is the shortage of islet cells. The supply available from deceased donors will be enough for only a small percentage of those with type 1 diabetes. Researchers pursue avenues of alternative sources, such as creating islet cells from other types of cells. New technologies may be employed to grow islet cells in the laboratory. Limitations of Islet Transplantation Published information shows several modifications of the Edmonton Protocol have been performed in over 15 centers involving over 160 patients worldwide. Patients who respond well to islet transplantation report being free of the need for insulin for about one year, on average, with the longest case being 7 years. This is similar to the rate of insulin independence achieved following whole pancreas transplantation. Although results from clinical studies appear promising, there are significant issues that remain before the technique can be considered for widespread application: Limited islet supply remains an obstacle. Only a limited number are suitable for transplant, based on the number of pancreas donors in the United States each year. Techniques to isolate islets have not been perfected (U.S.). Denise Faustman and colleagues at Massachusetts General Hospital (MGH) have an approach that identifies and selectively eliminates only the faulty cells of the immune system that mistakenly destroy healthy insulin-producing beta cells. The research has only been conducted on mice, but the Federal Drug Administration and the MGH have approved plans for a clinical trial to correlate the mouse model findings to type 1 diabetes in humans (4). Immunosuppression toxicity: After receiving a transplant, patients receive potent immunosuppressive medications for the rest of their lives. These medications often have serious side effects, so patients also contend with a higher risk of infections resulting from a weakened immune system. Normal blood sugar levels are not achieved. Although islet transplant patients appear to have better control of their blood sugar levels compared to those who achieve it with insulin, diet, and exercise, only a small percentage of transplant patients achieve normal blood sugar levels. Long-term safety numbers are questionable. Gaining access to the portal vein of the liver to transplant islet cells involves some risks as it is a difficult procedure. Immediate risks include portal vein thrombosis and bleeding. Long-term consequences are not known, but reports of hepatic steatosis have been documented. This happens when fat globules collect within the cells of the liver and cause the tissue to deteriorate and malfunction. Duration of islet allograft function may be exhausted. In addition to rejection by a patient's immune system, the transplanted islets are susceptible to aging. It is not known how long islets function after transplantation, and whether the patient may eventually need multiple transplants. Conclusion The effect of islet transplantation on diabetic complications remains a question. Controversy remains over whether a transplant actually stops or reverses secondary complications related to diabetes. It is also not clear whether transplantation may extend a patient's long-term survival rate (U.S.) Insulin independence is difficult to sustain with islet transplantation. The Edmonton protocol can successfully restore endogenous insulin production and glycemic stability in subjects with type 1 diabetes mellitus and unstable control. But even without insulin independence, persistent islet function following the procedure provides both protection from severe hypoglycemia and improved levels of glycated hemoglobin (Shapiro, p. 1330). (ClinicalTrials.gov number, NCT00014911 .) Fortunately, there are alternative solutions to the rejection of islets by the immune system that are currently being researched. Read the full article
0 notes
Text
Seic deflagra ação contra roubo de dados do Grupo Mateus e de clientes
A Polícia Civil, por meio do Departamento de Combate a Crimes Tecnológicos (DCCT), vinculado à Superintendência Estadual de Investigações Criminais (Seic), deflagrou nesta quarta-feira, 6, uma operação com o objetivo de cumprir, em São Luís, quatro mandados de busca e apreensão, além de medidas cautelares diversas de prisão, contra suspeitos dos crimes de roubo de dados e extorsão pela…
0 notes
Text
Diploma in Critical Care Technology [DCCT] Course to Build Your Carrier
The diploma in critical care technology is a specialized course designed to train students in managing critically ill patients who require intensive medical care. This 2 year diploma in critical care technology program prepares students to assist healthcare professionals in critical care units (CCUs) and intensive care units (ICUs), focusing on patient monitoring, life-support systems, and emergency medical responses. But what is a diploma in critical care technology exactly? It equips students with the technical skills and knowledge to handle advanced medical equipment and provide patient care in high-pressure environments.

What is a Diploma in Critical Care Technology?
The diploma in critical care technology is a paramedical course that focuses on training students to support doctors in handling critically ill patients in ICUs and CCUs. The diploma in critical care technology DCCT covers a variety of medical technologies and critical care practices, making it an essential program for those who wish to specialize in the healthcare field.
Eligibility for Diploma in Critical Care Technology
To apply for the diploma in critical care technology, candidates typically need to have completed their higher secondary education (10+2) with a background in science subjects such as biology, chemistry, and physics. The diploma in critical care technology eligibility criteria may vary slightly depending on the institution, but a focus on science is generally required.
Application Form for Diploma in Critical Care Technology
Students interested in pursuing a diploma in critical care technology can obtain the application form from the colleges offering the course. The diploma in critical care technology application form is often available online, or it can be obtained directly from the college's admission office.
Short Form for Diploma in Critical Care Technology
The short form for diploma in critical care technology is DCCT. This abbreviation is widely used when referring to the course, especially in academic and professional settings.
Programme Overview
The diploma in critical care technology programme is designed to provide students with in-depth knowledge of patient care in critical situations, focusing on monitoring systems, ventilators, and other life-saving equipment. Students learn how to assist in emergencies and manage patients who are under intensive observation.
Course Details
The diploma in critical care technology course details include subjects such as anatomy, physiology, medical equipment handling, patient monitoring, and emergency care procedures. The curriculum integrates both theoretical knowledge and hands-on training, ensuring that students are well-prepared for their roles in critical care environments.
Syllabus
The diploma in critical care technology syllabus is structured to cover topics like medical terminology, critical care techniques, mechanical ventilation, patient monitoring systems, and infection control. Students will also engage in clinical internships, gaining practical experience in ICUs and critical care units.
Diploma in Critical Care Technology in West Bengal
Several institutions offer the diploma in critical care technology in West Bengal, providing students in the state with access to this important medical training. Students can explore the various diploma in critical care technology colleges in West Bengal to find the best educational facilities and faculty for their needs.
Diploma in Critical Care Technology Colleges in India
There are numerous diploma in critical care technology colleges in India offering this course, with each providing state-of-the-art facilities and clinical exposure. These colleges ensure that students receive top-quality education and training, preparing them for careers in critical care settings across the country.
In conclusion, pursuing a diploma in critical care technology is an excellent choice for those who are passionate about playing a crucial role in patient care during emergencies. The program equips students with the essential skills and knowledge required to excel in critical care environments.
#education#best courses#topcolleges#best college#top colleges#college student#students#career#higher education#learning#educación
0 notes
Text
Homem é preso, em São Luís, pelo crime de ‘sextorsão’; ele usava imagens íntimas das vítimas para extorqui-las
Segundo o Departamento de Combate a Crimes Tecnológicos (DCCT) da Superintendência Estadual de Investigações Criminais (SEIC), o investigado foi preso após várias vítimas procurarem o DCCT, relatando que haviam iniciado um relacionamento com o homem, por meio de rede social, e que, após a troca de conteúdo íntimo, ele passou a exigir mais conteúdo e dinheiro, ameaçando as mulheres de divulgar as…
0 notes
Text
LINK’s circulating supply increased courtesy of the latest token unlock. Assessing price impact and latest development which underscores long term potential growth. The LINK token’s circulating supply just increased by roughly 18.75 million tokens in the last 24 hours from non-circulating supply contracts. But could this development yield an unfavorable outcome for the coin? Token unlocks usually lead to a higher circulating supply for the underlying asset. This is currently what is happening with the LINK token. Now, there is a notable chance that LINK could experience a significant amount of sell pressure. However, this is not the first token unlock for LINK and previous such occasions did not yield a significant price change. 🚨 18.75M $LINK ($117M) was unlocked from 4 Chainlink: Noncirculating supply contracts 6hrs ago, of which: – 15.7M $LINK ($98M) was deposited to #Binance – 3.05M $LINK ($19M) remains in multisig 0xD50f Notably, 82.75M $LINK has been unlocked since Aug 2022, of which 71.8M $LINK… pic.twitter.com/lqooYQKPt9 — Spot On Chain (@spotonchain) September 16, 2023 Of course, there is the possibility that the prevailing bullish momentum observed in the last few days could end up cancelling any incoming sell pressure. Interestingly, LINK’s price action has already tanked by over 2.2% to its $2.14 press time level. Source: TradingView There is another reason why the token unlocks might not have much of an impact on LINK’s price action. The recently unlocked tokens represent just 2.82% of Chainlink’s current circulating supply. Nevertheless, the higher circulating supply may still trigger some sell pressure. Other factors may have a more pronounced impact on price. For example, Chainlink’s supply held by whales recently soared to a new weekly high, indicating that there was a large whale purchase. This may have contributed to the bullish momentum observed in the last few days. Source: Santiment On the other hand, Chainlink’s network growth and development just concluded the week at a weekly low. These findings can potentially have a negative impact on LINK’s investor sentiment. It is worth nothing that the same metrics have so far not had much of an impact on LINK’s weighted sentiment which is currently at its weekly high. Read about Chainlink’s price prediction for 2024 Chainlink’s collaboration with DCCT underscores potential growth As far as matters related to organic growth are concerned, Chainlink is reportedly on the Depository Trust & Clearing Corporation’s (DCCT) radar. The latter is the largest securities settlement system in the world. Chainlink’s involvement with DCCT is the latest development involving the protocol that underscores efforts aimed at tapping into the tokenized assets segment. The latter is a segment that is expected to be among the biggest growth segments in WEB3. .@The_DTCC settles quadrillions of dollars worth of securities transactions annually.#Chainlink CCIP unlocks interoperability for the tokenized asset market. Discover how Chainlink and DTCC are collaborating in this new blog by Stephen Prosperi: pic.twitter.com/y0uVMFsm35 — Chainlink (@chainlink) September 15, 2023 DCCT is reportedly experimenting with Chainlink in the tokenized asset market. This collaboration has the potential to bring billions of dollars into the Chainlink ecosystem and contribute to its long-term growth. Source
0 notes
Text

Researchers use genomics to identify diabetic retinopathy factors
In a search to discover the genetic factors underlying diabetic retinopathy, University of Illinois Chicago researchers also have identified a new approach that can be used as a template to study other diseases.
In the paper, “Integration of genomics and transcriptomics predicts diabetic retinopathy susceptibility genes,” published in eLife, researchers identified genes that respond differently in response to high glucose in individuals with and without diabetic retinopathy.
Dr. Michael Grassi, associate professor of ophthalmology at UIC’s College of Medicine, his collaborator, Dr. Barbara Stranger of Northwestern University, and their teams set out to identify genes that cause diabetic retinopathy, a diabetes complication caused by damage to the light-sensitive tissue at the back of the eye — the retina — resulting in vision loss.
Grassi has been interested in diabetic retinopathy since he began his clinical training as a retina specialist.
“I encountered two individuals with disparate outcomes, a 19-year-old who had well-controlled diabetes for five years and went blind, and a Vietnam veteran, who had poorly controlled diabetes for over 30 years but had no vision problems,” Grassi said.
For 10 years, Grassi has been looking at the genetic underpinnings of diabetic retinopathy. After several attempts, he finally landed on a method that resulted in identifying genes that increase the risk of developing retinopathy. Grassi and his team combined several different methods to identify the gene, known as folliculin, or FLCN, that increases the risk of developing retinopathy. They began by comparing levels of gene activity in individuals with and without retinopathy. A set of genes that was unique to those with retinopathy was identified. Next, they took the genetic markers for this set of genes and found that many were associated with the development of diabetic retinopathy. Finally, they tested whether changes in the levels of some of these genes could cause retinopathy and discovered that increased amounts of FLCN increased the retinopathy risk.
The research team examined glucose-induced changes in gene expression in cell lines from people with type 1 diabetes, both with and without retinopathy. The approach provided new insights into the disease. The identification of single nucleotide polymorphisms, or SNPs, associated with such changes — eQtls (expression quantitative trait loci) — was followed by validation in independent cohorts. The FLCN as a mediator of diabetic retinopathy using Mendelian Randomization further solidified the method. “It has been a challenge to study diabetic retinopathy because it is so heterogeneous. There are so many genetic factors that can contribute,” Grassi said.
For this study, cell lines generated from blood samples were used from the Diabetes Control and Complications Trial, or DCCT, a large clinical study of diabetic retinopathy. Because the DCCT study generated cell lines for every individual, it allowed for detailed characterization of retinopathy severity in each individual.
Understanding the genetic factors behind diabetic retinopathy can potentially lead to developing new treatment and prevention strategies for retinopathy. The current standard of care involves laser surgery to preserve the center part of vision, or injections into the eye every four weeks.
The research team also includes Ana Marija Sokovic, Poulami Borkar, Amy Lin, Maria Sverdlov, Dingcai Cao, all of UIC; Andrew Skol of the Ann and Robert H. Lurie Children’s Hospital, Chicago; Segun Jung of NeoGenomics Laboratories; Siquan Chen and Sarah Fazal of the University of Chicago; Olukayode Sosina of Johns Hopkins University; Anand Swaroop of the National Eye Institute; and the DCCT/EDIC Study Group.
1 note
·
View note
Text


KITH vs TLOG
Magic Hands
#kith#kids in the hall#the kids in the hall#mark mckinney#kevin mcdonald#kith vs tlog#the kids in the hall vs the league of gentlemen#tlog#the league of gentlemen#reece shearsmith#magic hands#massage#dcct#death comes to town
1 note
·
View note
Photo

The feeling when you beat your brother on the DCCT range and the cute bombardier points you in the direction of the enlisting office... 23 to 4... #HeWasSquatting #DCCT #Army #FamilyDay
1 note
·
View note
Text
Masterlist
I write all kinds of stories but be aware I also write mature and\or dark stuff (but not all), it's not for everyone's liking, you are free to stop reading when you don't like it💕
Minors you should know better than to interact 🤝🏻
Don't steal or put my stuff anywhere else👍🏻
You can ask me to be tagged ☺️
*coming up\ wip*
- All is well
- dreams can come true part 6
Latest updates:
Like Fate (mob!Steve Rogers)
Evermore (DCCT alpha!Lee)
Want To Be Loved By You (Lord Barnes) part 2
Tail Me Like It Is
Hallowed Water
➖➖➖➖➖➖➖➖➖➖➖➖➖➖➖➖
Sebastian Stan
Chris Evans
The Boys
Ivar the Boneless
Lord au
Original Drabbles:
*The Run (Logan (male oc) x reader)
*A Horror Story (you x writer) (fake horror)
other stuff
Snailight beginning explanation
The weird beginning of my Twilight Snail au, I'm not sure if it explains anything, but hopefully it's a start. Feel free to search for 'Snailight' or 'snail au' in my blog, and enjoy the ride
36 notes
·
View notes
Photo
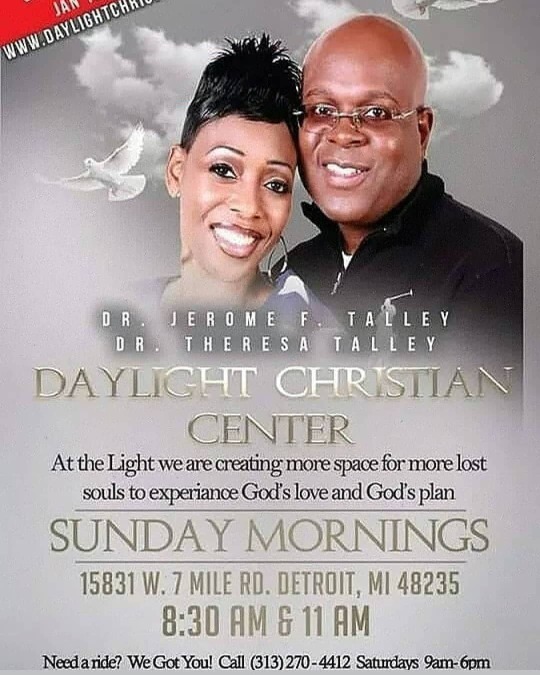
If needed don't forget to call or text our awesome transportation ministry to schedule a for a ride for Sunday 830am or 11AM service. Please do so as soon as you can or by Sat at 630pm. No delay! We're waiting on your request and excited to pick you up Sunday with your family. If you have any question regarding transportation call the number above and we will follow up with you soon. #growingministry #transportation #ride #wewillcomegetyou #detroitchurch #DCCT #daylighttransportation #Daylightchurch @daylightchristiancenter #830AM #11AM #callus #textus #thewords #salvation #churchhome #ridetochurch #DCCC #wepickup #fellowship (at Daylight Church) https://www.instagram.com/p/B48LxdaFTm2/?igshid=5rdf53e1lhid
#growingministry#transportation#ride#wewillcomegetyou#detroitchurch#dcct#daylighttransportation#daylightchurch#830am#11am#callus#textus#thewords#salvation#churchhome#ridetochurch#dccc#wepickup#fellowship
0 notes
Text
Overweight and Obesity in Youth with Type 1 Diabetes: What is Known?-Crimson Publishers

Overweight and Obesity in Youth with Type 1 Diabetes: What is Known? by Bruce King in Intervention in Obesity & Diabetes
Abstract
Obesity is a modifiable risk factor for poor health outcomes including cardiovascular disease (CVD). A trend for elevated body weight in children with type 1 diabetes (T1D) compared to the general population is clearly evident. This trend is pronounced in teenage girls with T1D and increases with age. Teenage boys with T1D more closely resemble the population norms for overweight and obesity. Given that individuals with T1D are at an increased risk of early CVD related morbidity and mortality, early weight management intervention could potentially improve CVD outcomes. Further investigation of mechanisms of weight gain in T1D is required to inform interventions.
Keywords: Type 1 diabetes; Pediatric; Obesity; Weight gain
Abbreviations:T1D: Type 1 Diabetes; CVD: Cardiovascular Disease; DCCT: Diabetes Control and Complications Trial; Diabetes Prospective Study; BMI-SDS: Body Mass Index Standard Deviation Score; MVPA: Moderate-to-Vigorous Physical Activity
Introduction
Overweight and obesity is an established risk factor for serious health outcomes including cardiovascular disease (CVD) [1] and increased mortality [2]. Individuals with type 1 diabetes (T1D) face an unequivocal risk of CVD similar to that seen in people with type 2 diabetes [3]. Atherosclerotic changes have been shown to affect individuals with T1D at younger ages, beginning in childhood. In the German/Austrian DPV registry, an alarming 69% of the 27,000 youth with T1D had one or more CVD risk factor [4]. The landmark Diabetes Control and Complications Trial (DCCT) established that in people with T1D, glycemic control was a determinant of microvascular disease highlighting the need for intensive insulin therapy to minimize long-term diabetes-related complications [5]. However, the DCCT also demonstrated significant weight gain in the intensive therapy arm compared to the conventional treatment arm [6].
Rate of Overweight and Obesity in Youth with T1D
Recent research has demonstrated an increased rate of overweight and obesity in children with T1D. The Australasian Diabetes Data Network found that 33% of children and adolescents with T1D were overweight or obese [7] compared to 25% of the pediatric population in the Australian National Health Survey [8]. Youth with T1D from the Diabetes Prospective Study (DPV) in Europe and the Type 1 Diabetes Exchange (T1DX) in America had a higher median body mass index standard deviation score (BMI-SDS) is compared to respective national reference samples [9]. The SEARCH for diabetes in youth study found significantly higher rates of overweight but not obesity in young people with T1D (3-19 years) compared to the general US population [10]. Stratification by age and gender revealed that females aged 12-19 years with T1D had significantly higher rates of combined overweight or obesity compared to the population reference (36.5% and 29.1%, respectively). Interestingly, the opposite was true in boys aged 12-19 years with T1D, where the rates in the population reference were significantly higher (28.8% and 34.6%, respectively) [10].
Research at our center demonstrated an overweight and obesity rate of 37% in children and adolescents with T1D compared to 24% for an age matched population [11]. Whilst combined overweight and obesity were significantly higher in males and females in the 5-8 year age group compared to the general population, this effect disappeared in the 9-12 year age group across sexes. Thereafter, only girls had significantly higher rates of combined overweight or obesity in the adolescent (13-16 years) and young adult groups (18-24 and 25-30 years) compared to the general population. In addition, BMI-SDS was associated with a longer duration of diabetes in girls only [11].
What are the Mechanisms of Weight Gain in Youth with Type 1 Diabetes?
Contributing factors influencing childhood obesity in youth without diabetes include insufficient physical activity, dietary factors, sleep duration [12] and socioeconomic factors [13]. An analysis of the DPV cohort showed BMI-SDS increase during the course of T1D was strongly associated with female gender in youth. Moreover, the study found specific diabetes-related factors which contributed to weight gain over time, including higher insulin dose, low BMI-SDS at diabetes onset, longer diabetes duration, intensive insulin therapy and pubertal diabetes onset (aged 10-15 years) also contributed to weight gain over time [14]. There are few studies have objectively measured moderate-to-vigorous physical activity (MVPA) levels in youth with T1D compared to healthy subjects found significantly lower rates of MVPA in youth with T1D diabetes [15]. Children with T1D may face additional barriers to those experienced by children in the general population. Fear of hypoglycemia, low fitness level and loss of control of diabetes have been identified as significant barriers to physical activity in youth over 12 years of age. Furthermore, 91% of youth also indicated that their parents discouraged physical activity [16]. Research has demonstrated that disordered eating behaviors are more common in adolescent girls with T1D compared to their peers [17]. Interestingly, disordered eating behaviors were correlated with elevated BMI-SDS in youth with T1D in the SEARCH study [18].
Management of Overweight and Obesity in Youth with T1D
Management of obesity in youth with T1D is usually done on a case-by-case basis. In the general population lifestyle interventions focusing on diet, physical activity and behavioural interventions have shown some benefit [19]. However, behavioural interventions in the general population focus on physical activity and nutrition in children but are not tailored to the unique set of circumstances encountered by children and adolescents with T1D. Factors such as glucose fluctuations caused by exercise and dietary considerations in the setting of T1D present a key challenge to work on in future interventions.
Conclusion
Both T1D and overweight and obesity carry increased and independent risk for CVD. Hence, weight management in youth with T1D is important. Recent research has highlighted that weight management should start early in adolescence and be directed towards females with T1D. However, mechanisms of weight gain and methods to address diabetes-related barriers to physical activity and weight loss are currently lacking and require further research.
References
Klein S, Burke LE, Bray GA, Blair S, Allison DB, et al. (2004) Clinical implications of obesity with specific focus on cardiovascular disease: A statement for professionals from the American Heart Association council on nutrition, physical activity, and metabolism: endorsed by the American College of Cardiology Foundation. Circulation 110(18): 2952-2967.
Adams KF, Schatzkin A, Harris TB, Kipnis V, Mouw T, et al. (2006) Overweight, obesity, and mortality in a large prospective cohort of persons 50 to 71 years old. The New England Journal of Medicine 355(8): 763-778.
Pang TT, Narendran P (2008) Addressing insulin resistance in type 1 diabetes. Diabet Med 25(9): 1015-1024.
Schwab KO, Doerfer J, Hecker W, Grulich Henn J, Wiemann D, et al. (2006) Spectrum and prevalence of atherogenic risk factors in 27,358 children, adolescents, and young adults with type 1 diabetes. Cross-sectional data from the German diabetes documentation and quality management system (DPV). Diabetes Care 29(2): 218-225.
Nathan DM, Genuth S, Lachin J, Cleary P, Crofford O, et al. (1993) The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. The New England Journal of Medicine 329(14): 977-986.
(1995) Adverse events and their association with treatment regimens in the diabetes control and complications trial. Diabetes care 18(11): 1415‐1427.
Phelan H, Clapin H, Bruns L, Cameron FJ, Cotterill AM, et al. (2017) The Australasian diabetes data network: first national audit of children and adolescents with type 1 diabetes. The Medical Journal of Australia 206(3): 121-125.
(2017-2018) Australian Bureau of Statistics. National Health Survey, Australia.
DuBose SN, Hermann JM, Tamborlane WV, Beck RW, Dost A, et al. (2015) Obesity in youth with type 1 diabetes in Germany, Austria, and the United States. The Journal of Pediatrics 167(3): 627-632.
Liu LL, Lawrence JM, Davis C, Liese AD, Pettitt DJ, et al. (2010) Prevalence of overweight and obesity in youth with diabetes in USA: The SEARCH for diabetes in youth study. Pediatric Diabetes 11(1): 4-11.
Marlow AL, Rowe CW, Anderson D, Wynne K, King BR, et al. (2019) Young children, adolescent girls and women with type 1 diabetes are more overweight and obese than reference populations, and this is associated with increased cardiovascular risk factors. Diabetic Medicine 36(11): 1487-1493.
Poorolajal J, Sahraei F, Mohamdadi Y, Doosti Irani A, Moradi L (2020) Behavioral factors influencing childhood obesity: A systematic review and meta-analysis. Obesity Research & Clinical Practice 14(2): 109-118.
Shrewsbury V, Wardle J (2008) Socioeconomic status and adiposity in childhood: A systematic review of cross-sectional studies 1990-2005. Obesity (Silver Spring) 16(2): 275-284.
Fröhlich Reiterer EE, Rosenbauer J, Bechtold Dalla Pozza S, Hofer SE, Schober E, et al. (2014) Predictors of increasing BMI during the course of diabetes in children and adolescents with type 1 diabetes: data from the German/Austrian DPV multicentre survey. Archives of Disease in Childhood 99(8): 738-743.
Trigona B, Aggoun Y, Maggio A, Martin XE, Marchand LM, et al. (2010) Preclinical noninvasive markers of atherosclerosis in children and adolescents with type 1 diabetes are influenced by physical activity. The Journal of Pediatrics 157(4): 533-539.
Jabbour G, Henderson M, Mathieu ME (2016) Barriers to active lifestyles in children with type 1 diabetes. Canadian Journal of Diabetes 40(2): 170-172.
Young V, Eiser C, Johnson B, Brierley S, Epton T, et al. (2013) Eating problems in adolescents with type 1 diabetes: A systematic review with meta-analysis. Diabet Med 30(2): 189-198.
Nip ASY, Reboussin BA, Dabelea D, Bellatorre A, Mayer Davis EJ, et al. (2019) Disordered eating behaviors in youth and young adults with type 1 or type 2 diabetes receiving insulin therapy: The SEARCH for diabetes in youth study. Diabetes Care 42(5): 859-866.
Oude Luttikhuis H, Baur L, Jansen H, Shrewsbury VA, O Malley C, et al. (2019) Interventions for treating obesity in children. Cochrane Database of Systematic Reviews.
For more about in Crimson Publishers, please click on the link: https://crimsonpublishers.com/peer-review-process.php
For more articles in Journal of Diabetes and Obesity, please click on below link: https://crimsonpublishers.com/iod/
#crimson publishers reviews#open access journals#crimsonpublishers LLC#gestational diabetes#Overweight & obesity#insulin resistance syndrome#Diet & Controlling Methods
1 note
·
View note
Text
Vì sao Nguyễn Ngọc Nam Phong phản đối phiên tòa xét xử các thành viên “Hội nhà báo độc lập”
Vì sao Nguyễn Ngọc Nam Phong phản đối phiên tòa xét xử các thành viên “Hội nhà báo độc lập”
Được biết đến là linh mục có hoạt động cực đoan, chống đối khi còn làm mục vụ tại Giáo xứ/ Cộng đoàn DCCT Thái Hà (Hà Nội) trực thuộc Tỉnh dòng chúa cứu thế Việt Nam. Khi Nguyễn Ngọc Nam Phong bị bề trên thuyên chuyển về hoạt động tại trụ sở nhà chung ở TP Hồ Chí Minh, Y vẫn “Thói nào tật nấy”, thường xuyên có hoạt động tuyên truyền chống đối trên mạng xã hội. Với các tư tưởng cực đoan, Nguyễn…
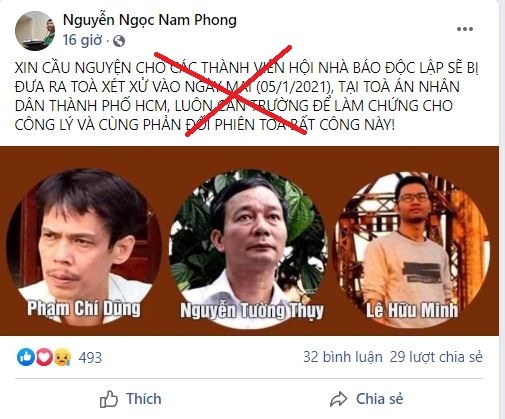
View On WordPress
#chống phá Nhà nước#cực đoan#Dòng Chúa Cứu Thế#Hà Nội#Lê Hữu Minh Tuấn#linh mục#mạng xã hội#Nguyễn Ngọc Nam Phong#Nguyễn Tường Thụy#Phạm Chí Dũng
1 note
·
View note