#ICD-10 coding for hospitals
Explore tagged Tumblr posts
Text
Common ICD-10 Codes Used in Primary Care [2025 Edition]

Primary care is the foundation of the healthcare system, covering everything from preventive services and chronic condition management to urgent care and routine screenings. Given its wide scope, primary care professionals encounter a vast variety of diagnoses on a daily basis. That’s why quick access to the most commonly used ICD-10 codes is essential. It supports accurate clinical documentation, streamlines insurance claims, enhances billing efficiency, and ensures compliance.
With stricter reimbursement policies, increased audit scrutiny, and a higher risk of denials due to coding mistakes, accuracy has never been more critical. Primary care providers often shift rapidly between tasks like wellness visits, managing diabetes, treating respiratory infections, and administering vaccines. In such a fast-paced environment, having reliable, up-to-date coding tools becomes a game-changer.
This blog highlights a 2025-ready list of the most frequently used ICD-10 codes in primary care, offering a practical reference for busy clinicians.
Most Common ICD-10 Codes in Primary Care Clinics
Primary care providers are often the first point of contact for patients, managing everything from preventive screenings to acute and chronic conditions across all age groups. Given this wide range of responsibilities, it's crucial to be familiar with the most frequently used ICD-10 codes. Below is a categorized list of top ICD-10 codes commonly used in primary care as of 2025:
1. Preventive Visits and Wellness Checks
Routine health assessments are a frequent reason for visits. Common codes include:
Z00.00 – Adult general exam with no abnormal findings
Z00.01 – Adult general exam with abnormal findings
Z00.129 – Child wellness check without abnormalities
Z00.121 – Child wellness check with abnormalities
Z13.6 – Cardiovascular screening
Z13.89 – General health screening
Z23 – Immunization encounter
2. Respiratory Conditions
Often seen during flu seasons or among patients with chronic respiratory issues:
J00 – Common cold
J02.9 – Acute pharyngitis, unspecified
J06.9 – Acute upper respiratory infection
J18.9 – Pneumonia, unspecified
J20.9 – Acute bronchitis, unspecified
J30.9 – Unspecified allergic rhinitis
J45.909 – Uncomplicated asthma, unspecified
J44.9 – Chronic obstructive pulmonary disease
J40 – Bronchitis, unspecified
3. Infections & Acute Illnesses
General infections and acute complaints use the following codes:
B34.9 – Unspecified viral infection
N39.0 – Urinary tract infection, unspecified site
4. Chronic Disease Management
Long-term condition management is a core responsibility:
Metabolic/Endocrine:
E11.9 – Type 2 diabetes, no complications
E11.65 – Type 2 diabetes with hyperglycemia
E78.0 – Pure hypercholesterolemia
E78.5 – Unspecified hyperlipidemia
E03.9 – Unspecified hypothyroidism
E66.9 – Unspecified obesity
E63.9 – Nutritional deficiency, unspecified
Cardiovascular:
I10 – Primary hypertension
I11.9 – Hypertensive heart disease, no failure
I20.9 – Unspecified angina
I25.10 – Coronary artery disease without angina
I25.110 – Coronary artery disease with unstable angina
I48.91 – Atrial fibrillation, unspecified
I50.9 – Heart failure, unspecified
5. Musculoskeletal Issues
Frequently used for joint, muscle, and back pain:
M54.5 – Lower back pain
M25.50 – Joint pain, unspecified
M19.90 – Unspecified osteoarthritis
M75.100 – Rotator cuff tear, unspecified
M17.9 – Osteoarthritis of knee, unspecified
M79.1 – Muscle pain (myalgia)
6. Mental and Behavioral Health
Mental health is often addressed in primary care:
F32.9 – Unspecified depression
F41.1 – Generalized anxiety disorder
F43.2 – Adjustment disorder
F50.9 – Eating disorder, unspecified
F90.9 – ADHD, unspecified type
7. Neurological and Sleep Disorders
G47.33 – Obstructive sleep apnea
G43.909 – Unspecified migraine
8. Gastrointestinal Conditions
K21.9 – GERD without esophagitis
K29.70 – Unspecified gastritis without bleeding
K58.9 – IBS without diarrhea
K64.4 – Unspecified anal fissure
K75.9 – Unspecified liver inflammation
9. Dermatologic Conditions
L03.90 – Unspecified cellulitis
L20.9 – Atopic dermatitis
L30.9 – Unspecified dermatitis
10. General Symptoms and Pain
R07.9 – Chest pain, unspecified
R10.9 – Abdominal pain, unspecified
R51.9 – Headache, unspecified
R53.83 – Fatigue
R63.4 – Unintended weight loss
R63.5 – Unusual weight gain
11. Social and Environmental Influences
Z20–Z29 – Exposure to infectious diseases
Z55–Z65 – Social or psychological risk factors
Z71–Z76 – Health service encounters (e.g., counseling, follow-ups)
2025 Billing Best Practices for ICD-10 in Primary Care
Be Specific: Use the most precise and current code available to avoid denials.
Annual Updates: ICD-10 codes are revised every October—always use the latest version.
Symptom Coding: Only use symptom codes (R00–R99) when a diagnosis is unclear.
Proper Code Linkage: Pair ICD-10 codes with CPT/HCPCS codes to support medical necessity.
EHR Integration: Use smart, cloud-based platforms that suggest accurate codes in real time.
How 24/7 Medical Billing Services Can Help
24/7 Medical Billing Services enhances accuracy and speed in ICD-10 coding with expert support and cutting-edge tools. Their certified coders stay current with 2025 updates, ensuring precise documentation, fewer denials, and stronger compliance. Outsourcing primary care billing and coding services to 24/7 MBS provides seamless EHR integration and boosts reimbursement efficiency—helping your primary care clinic focus on patients, not paperwork.
Content Source: [https://www.247medicalbillingservices.com/blog/common-icd-10-codes-used-in-primary-care-2025-edition]
For More Information:
Call us at +1 888-502-0537 or Sales: [email protected]
Support: [email protected]
Visit at https://www.247medicalbillingservices...
Our Office Locations:
Ohio: 28405 Osborn Road, Cleveland, OH, 44140
Texas: 2028 E Ben White Blvd, #240-1030 Austin TX, 78741
Subscribe @247medicalbillingservices
Follow us on social media channels-
Facebook: https://www.facebook.com/247MBS
Twitter: https://x.com/247MBServices
Instagram: https://www.instagram.com/247mbs/
LinkedIn: https://www.linkedin.com/company/24-7-medical-billing-services/
#ICD-10 codes#ICD-10 coding in Primary care#ICD-10 medical coding#ICD-10 billing and coding#ICD-10 coding for hospitals#Primary Care Billing Services#Primary care Coding Company#Primary health care billing#Primary health care billing agency USA#Medical Coding Services#Medical Billing Company#Medical Billing#ICD-10 codes for family physicians#ICD-10 coding#EHR coding#ICD-10 billing for outpatient care#Medical Coding Services Florida#Best Medical Coding Services USA#Medical Billing Services USA#Outsourced Medical Billing#Outsourced Medical Coding Georgia#Medical coding agency Connecticut#Top Medical coding companies#Medical coding for providers Ohio#Outsource Medical Coding Oklahoma#Outsource Medical Coding Oregon#Outsource Medical Coding Pennsylvania#Medical Coding Maine#Medical Coding Massachusetts#Medical Coding Services California
0 notes
Text
Comprensión del movimiento fetal
#decreased fetal movement#decreased fetal movement 22 weeks#decreased fetal movement 24 weeks#decreased fetal movement 38 weeks#decreased fetal movement icd 10#fetal movement#icd 10 code for decreased fetal movement#increased fetal movement#increased fetal movement 37 weeks sign of labor#increased fetal movement before labor#reasons for decreased fetal movement#reduced fetal movement#sudden increased fetal movement#what can cause decreased fetal movement in third trimester#what is considered decreased fetal movement#when do you feel fetal movement#when do you start feeling fetal movement#when to go to hospital for decreased fetal movement#when to worry about fetal movement#when to worry about increased fetal movement
0 notes
Text
Optimizing Anesthesia Billing for Maximum Reimbursement and Compliance

Anesthesia billing is one of the most complex areas of medical billing, requiring a deep understanding of Current Procedural Terminology (CPT®), ASA (American Society of Anesthesiologists) codes, ICD-10, and Medicare regulations. Accurate anesthesia billing ensures timely reimbursements and reduces the risk of denials and compliance issues. This blog explores the essential elements of anesthesia billing, common challenges, and how outsourcing to experts can improve financial performance.
Understanding Anesthesia Billing
Anesthesia billing differs from other medical billing specialties due to the use of time-based units and conversion factors. The reimbursement process involves several key components:
Base Units: Assigned by the ASA, these units reflect the complexity of the procedure.
Time Units: Billing is calculated based on the time an anesthesiologist spends with a patient.
Modifiers: Specific modifiers indicate whether the anesthesia service was personally performed, medically directed, or medically supervised.
Conversion Factor: The dollar amount assigned per unit, determined by Medicare and private payers.
Medical Direction Rules: Medicare has strict guidelines for cases where an anesthesiologist supervises multiple CRNAs.
Common Challenges in Anesthesia Billing
Incorrect Time Calculations
Miscalculating anesthesia start and stop times can lead to claim denials or underpayments.
Coding Errors
Failure to use accurate ASA codes, CPT® codes, and ICD-10 codes may result in claim rejections.
Lack of Proper Documentation
Missing information in anesthesia records can cause compliance issues and delays in reimbursement.
Medical Necessity Denials
Payers often require justification for the necessity of anesthesia services.
Failure to Use Appropriate Modifiers
Modifiers such as AA, QK, QX, QZ, and QY indicate how anesthesia services were provided and affect reimbursement rates.
Compliance with Changing Regulations
Medicare, Medicaid, and private insurers frequently update billing rules, making it essential to stay compliant.
Best Practices for Successful Anesthesia Billing
Accurate Documentation
Ensure that anesthesia start and stop times, provider details, and medical necessity are clearly documented.
Proper Use of Modifiers
Apply the correct modifiers based on medical direction and supervision levels.
Regular Audits and Quality Checks
Conduct routine audits to detect and correct errors before claim submission.
Utilizing Technology for Efficiency
Implement automated billing software and Electronic Health Records (EHRs) to reduce manual errors.
Timely Claim Submission
Submit claims within payer deadlines to avoid reimbursement delays.
Benefits of Outsourcing Anesthesia Billing Services
Outsourcing anesthesia billing to a professional medical billing company, such as Allzone Management Services, offers numerous advantages:
Increased Revenue & Faster Reimbursements
Expertise in anesthesia coding ensures correct claim submissions, reducing denials and delays.
Compliance with Industry Regulations
Professional billing teams stay updated with Medicare, Medicaid, and commercial payer guidelines.
Reduction in Administrative Burden
Physicians and anesthesiology groups can focus on patient care instead of handling billing complexities.
Improved Accuracy & Reduced Denials
Advanced billing software and trained coders help minimize claim errors.
Enhanced Financial Reporting
Regular analytics and reporting provide insights into revenue cycle performance.
Why Choose Allzone Management Services for Anesthesia Billing?
At Allzone Management Services, we provide end-to-end anesthesia billing solutions tailored to maximize your revenue and compliance. Our services include:
Accurate CPT, ICD-10, and ASA coding
Claim scrubbing and submission
Denial management and appeals
Revenue cycle management
HIPAA-compliant processes
With our technology-driven approach and experienced team, we ensure a smooth billing process for anesthesiologists, hospitals, and surgical centers.
Conclusion
Anesthesia billing requires specialized expertise to ensure accurate coding, reduce denials, and improve cash flow. By following best practices and leveraging professional billing services, anesthesia providers can optimize their revenue cycle. Partnering with Allzone Management Services allows you to focus on patient care while we handle the complexities of medical billing.
For more details, visit Allzone Management Services — Anesthesia Billing.
#Anesthesia billing#Anesthesia coding#Medical billing for anesthesia#Anesthesia revenue cycle management#ASA codes#CPT codes for anesthesia#ICD-10 anesthesia billing#Anesthesia billing services#Outsourced anesthesia billing#Anesthesia claim denials#Anesthesia reimbursement#Anesthesia billing compliance#EHR for anesthesia billing#Anesthesia billing audits#Revenue Cycle Management for Anesthesia#How to improve anesthesia billing accuracy#Best practices for anesthesia coding#Challenges in anesthesia medical billing#Benefits of outsourcing anesthesia billing services#Why choose a professional anesthesia billing company#Anesthesia billing services for surgical centers#Anesthesia billing services for hospitals#Anesthesia billing services for anesthesiologists
0 notes
Text
Start Your Career in Australian Medical Coding
Interested in an entry in the healthcare sector? Then enroll into the Australian Medical Coding course in Transorze Solutions as your entry pass.
This specific course, designed and intended to make anyone an expert on ICD-10-AM, ACHI, ACS, and Australia's regulation, is here for you to improve your ability at coding and documentation of diagnosis and procedures within Australia.
Hands on learning in action, therefore providing you an application site for what is learned; prepared to go in hospitals, clinics, and a medical coding company in Australia to the world beyond.
Be Prepared to start being a Medical coder, bill coder, coding Auditor with a good Australian Medical Coding Certification from Transorze Solutions, Take the step that will land you in that gratifying career of life.
#Australian Medical Coding#ICD-10-AM#ACHI#ACS#medical coding#healthcare careers#medical coding firms#hospitals#clinics#Transorze Solutions
0 notes
Text
Here is the child free friendly doctors list. the people on this list are compiled by other childfree people who do not want children. people submit doctors who did their sterilization regardless of age, children, or marital status.
here is a breakdown of how the ACA (affordable care act) works, and how it applies to sterilization. this is only for AFAB people however. vasectomies do not count. You cannot be charged for this surgery. No coinsurance, no deductible, nothing. my hospital originally wanted $4k from me. I told them to bill me and I'll discuss with my insurance. they might be pushy, and try to get you to pay for it ahead of time, but refuse and have them bill it.
If you are getting a bilateral salpingectomy (shortened: bisalp) (COMPLETE TUBAL REMOVAL not 'tubes tied', which is where they snip the tubes and tie them with clips [called a 'tubal ligation']) there is no possible way you can become pregnant. and it does not effect your hormones at all. im being so fr, do not let people say it effects your hormones, because theres no hormones in your tubes. those are carried in ur ovaries.
If you have a family history of reproductive cancer, a bisalp greatly reduces your risks of getting those cancers. insurance codes are CPT codes of either 58661 or 58670 and the ICD-10 code of Z30.2 you might have to plug both in and talk to insurance. if someone on the phone is an asshole to you, just hang up and try again with someone else. On the other side, I've been on plenty of birth control options. for 6 years I had a copper IUD. it does make your periods heavier, and crampier if you can stand that, but it has no hormones in it and it lasts 12 years.
3K notes
·
View notes
Text
ICD-10 code G93. 6 for Cerebral edema is a medical classification as listed by WHO under the range - Diseases of the nervous system.
For more details: 🌐 www.transorze.com ☎️ 9495833319
#medical coding#icd 10#cerebral edema#health#brain disorder#nervous system#hospitals#medical sector#transorze calicut#transorze dubai#transorzesolutions
1 note
·
View note
Text
Also preserved in our archive (Updated daily!)
Researchers report that a new AI tool enhances the diagnostic process, potentially identifying more individuals who need care. Previous diagnostic studies estimated that 7 percent of the population suffers from long COVID. However, a new study using an AI tool developed by Mass General Brigham indicates a significantly higher rate of 22.8 percent.
The AI-based tool can sift through electronic health records to help clinicians identify cases of long COVID. The often-mysterious condition can encompass a litany of enduring symptoms, including fatigue, chronic cough, and brain fog after infection from SARS-CoV-2.
The algorithm used was developed by drawing de-identified patient data from the clinical records of nearly 300,000 patients across 14 hospitals and 20 community health centers in the Mass General Brigham system. The results, published in the journal Med, could identify more people who should be receiving care for this potentially debilitating condition.
“Our AI tool could turn a foggy diagnostic process into something sharp and focused, giving clinicians the power to make sense of a challenging condition,” said senior author Hossein Estiri, head of AI Research at the Center for AI and Biomedical Informatics of the Learning Healthcare System (CAIBILS) at MGB and an associate professor of medicine at Harvard Medical School. “With this work, we may finally be able to see long COVID for what it truly is — and more importantly, how to treat it.”
For the purposes of their study, Estiri and colleagues defined long COVID as a diagnosis of exclusion that is also infection-associated. That means the diagnosis could not be explained in the patient’s unique medical record but was associated with a COVID infection. In addition, the diagnosis needed to have persisted for two months or longer in a 12-month follow-up window.
Precision Phenotyping: A Novel Approach The novel method developed by Estiri and colleagues, called “precision phenotyping,” sifts through individual records to identify symptoms and conditions linked to COVID-19 to track symptoms over time in order to differentiate them from other illnesses. For example, the algorithm can detect if shortness of breath results from pre-existing conditions like heart failure or asthma rather than long COVID. Only when every other possibility was exhausted would the tool flag the patient as having long COVID.
“Physicians are often faced with having to wade through a tangled web of symptoms and medical histories, unsure of which threads to pull, while balancing busy caseloads. Having a tool powered by AI that can methodically do it for them could be a game-changer,” said Alaleh Azhir, co-lead author and an internal medicine resident at Brigham and Women’s Hospital, a founding member of the Mass General Brigham healthcare system.
The new tool’s patient-centered diagnoses may also help alleviate biases built into current diagnostics for long COVID, said researchers, who noted diagnoses with the official ICD-10 diagnostic code for long COVID trend toward those with easier access to healthcare.
The researchers said their tool is about 3 percent more accurate than the data ICD-10 codes capture, while being less biased. Specifically, their study demonstrated that the individuals they identified as having long COVID mirror the broader demographic makeup of Massachusetts, unlike long COVID algorithms that rely on a single diagnostic code or individual clinical encounters, skewing results toward certain populations such as those with more access to care.
“This broader scope ensures that marginalized communities, often sidelined in clinical studies, are no longer invisible,” said Estiri.
Limitations and Future Directions Limitations of the study and AI tool include the fact that health record data the algorithm uses to account for long COVID symptoms may be less complete than the data physicians capture in post-visit clinical notes. Another limitation was the algorithm did not capture the possible worsening of a prior condition that may have been a long COVID symptom. For example, if a patient had COPD that worsened before they developed COVID-19, the algorithm might have removed the episodes even if they were long COVID indicators. Declines in COVID-19 testing in recent years also makes it difficult to identify when a patient may have first gotten COVID-19.
The study was limited to patients in Massachusetts.
Future studies may explore the algorithm in cohorts of patients with specific conditions, like COPD or diabetes. The researchers also plan to release this algorithm publicly on open access so physicians and healthcare systems globally can use it in their patient populations.
In addition to opening the door to better clinical care, this work may lay the foundation for future research into the genetic and biochemical factors behind long COVID’s various subtypes. “Questions about the true burden of long COVID — questions that have thus far remained elusive — now seem more within reach,” said Estiri.
Reference: “Precision phenotyping for curating research cohorts of patients with unexplained post-acute sequelae of COVID-19” by Alaleh Azhir, Jonas Hügel, Jiazi Tian, Jingya Cheng, Ingrid V. Bassett, Douglas S. Bell, Elmer V. Bernstam, Maha R. Farhat, Darren W. Henderson, Emily S. Lau, Michele Morris, Yevgeniy R. Semenov, Virginia A. Triant, Shyam Visweswaran, Zachary H. Strasser, Jeffrey G. Klann, Shawn N. Murphy and Hossein Estiri, 8 November 2024, Med. DOI: 10.1016/j.medj.2024.10.009 www.cell.com/med/fulltext/S2666-6340(24)00407-0?_returnURL=https%3A%2F%2Flinkinghub.elsevier.com%2Fretrieve%2Fpii%2FS2666634024004070%3Fshowall%3Dtrue
#long covid#covid is airborne#mask up#public health#pandemic#covid#wear a respirator#wear a mask#covid 19#coronavirus#covid is not over#covid conscious#still coviding#sars cov 2
100 notes
·
View notes
Text
Irma Aleman Mungia, 16 (USA 1975)
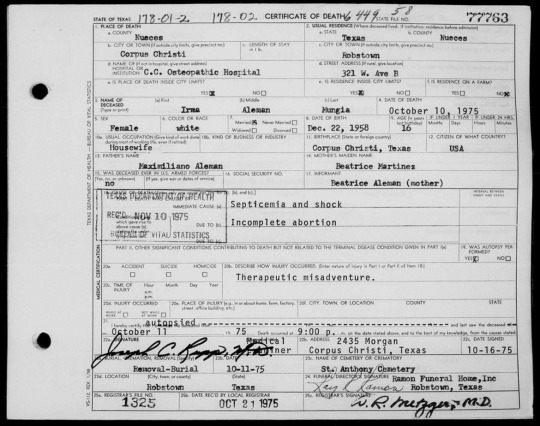
By the age of 16, Irma was already married to Jose Louis Mungia and pregnant with her third child. She had more on her shoulders than most 16-year-olds, but probably never imagined the way a “safe and legal” abortion would end her life and devastate those around her.
On October 10, 1975, Irma died at Corpus Christi Osteopathic Hospital. An autopsy performed the next day verified that she died of sepsis and shock from an incomplete abortion. She left behind her husband Jose and two surviving children. Things would never be the same for the young family.
While the ICD codes listed on her death certificate did not specify whether it was an actual abortion or a “spontaneous abortion” (meaning a miscarriage), her manner of death was not natural. The categorization of “therapeutic misadventure” indicates a legally induced abortion. If it had been an illegal abortion, the manner of death would almost certainly be listed as a homicide.
It is unknown if the abortion was done at C.C. Osteopathic Hospital, but administrators announced in 1989 that they were closing the obstetrics department due to issues with malpractice insurance. The entire hospital was sold in 1990, then stood essentially abandoned for years while it was sold repeatedly without reopening. The building was finally demolished after an elementary school student found a decomposing human corpse on site and charged his friends to come look at it.
Texas Death Certificate #77763
Corpus Christi Times, October 13, 1975 (Page 29)
#victims of roe#unsafe yet legal#tw abortion#pro life#tw ab*rtion#tw murder#abortion#abortion debate#death from legal abortion#tw human corpse
8 notes
·
View notes
Text
Medical coding courses in Ethiopia
Are you looking to build a successful career in the healthcare industry? Join top-quality medical coding courses in Ethiopia that provide the essential training and certification to launch your journey in medical billing and coding. As the healthcare sector rapidly expands, the demand for skilled medical coders is growing, creating exciting job opportunities both locally and internationally.
Medical coding involves translating medical diagnoses, procedures, and services into standardized codes used for billing and insurance purposes. By enrolling in a reputable course in Ethiopia, students gain in-depth knowledge of coding systems such as ICD-10, CPT, and HCPCS, along with a solid foundation in medical terminology, anatomy, and healthcare regulations.
These courses are ideal for high school graduates, healthcare professionals looking to specialize, or anyone interested in a rewarding remote or in-office career. Many institutes in Ethiopia now offer both in-person and online options, making it flexible and convenient for students with different schedules and commitments.
Choosing the right medical coding course in Ethiopia can open doors to employment in hospitals, clinics, insurance companies, and outsourcing firms. With proper training, you can even pursue international certification such as CPC (Certified Professional Coder), enhancing your career prospects abroad.
Start your journey toward a stable and well-paying profession by exploring the best medical coding courses in Ethiopia today. Learn from experienced instructors, gain practical skills, and become part of a growing global industry that values accuracy, detail, and professionalism.
#MedicalCodingEthiopia#HealthcareTraining#MedicalBilling#CodingCoursesEthiopia#MedicalCareers#ICD10Training#OnlineMedicalCourses#CPCTrainingEthiopia#HealthcareEducation#MedicalCodingJobs
2 notes
·
View notes
Text
Medical Billing Services in Florida: 2024 Guide to Boost Revenue
Florida’s healthcare providers encounter a perfect storm of difficulties with the hurricane season, aging patients, and the intricate rules of Medicaid. Clinics lost over $4.7 million a year due to billing mistakes in 2023 alone, which is enough to hire more than 50 nurses throughout the state. This guide explores how medical billing services in Florida mitigate these issues through expert knowledge and advanced technology to stop revenue loss and streamline profits.
What Are Medical Billing Services? (And Ohio’s Reasons For The Need)
They are the financial lifeline of a clinic. Medical billing services in Florida manage the coding of the diagnosis and the appeals for denied claims. In Florida, it is more than just a contracting firm; it is a matter of survival.
Why Florida?
Medicare Mayhem: One of the most bizarre situations in America is that 32% of people living in Florida use Medicare Advantage plans, each with its own billing rules.
Hurricane Headaches: Correctly coding claims is a difficult task. After Hurricane Ian, clinics reported using ICD-10 code Z04.1 (disaster-related care) for more than 3000 claims.
Legal Landmines: The “Balance Billing” law in Florida means that a single coding mistake could incur a loss of more than $10,000 in fines.
5 Ways Florida Medical Billing Services Boost Revenue
Slash Denial Rates
AI software, like Claim Genius, is helping Miami clinics decrease denial rates. Denials due to discrepancies such as telehealth visit Cand PT code mismatches are flagged. These tools help reduce denials by 40%.
Speed Up Payments
If correctly coded, the Staywell program of Florida Medicaid processes case management claims (HCPCS code T1015) 15 days earlier than the stipulated payment period.
Ensure Compliance
By outsourcing coding to AAPC-certified specialists, Sunset Medical Group mitigated $250,000 in anticipated AHCA fines.
Cut Costs
HealthFirst Clinic of Orlando saves $67k a year by contracting billing out to Specialized-Billing.com.
Disaster-Proof Billing
Fort Myers clinics adopted cloud-based systems for billing and were able to submit 95% of claims on time after Hurricane Ian.
How to Choose the Best Medical Billing Partner in Florida
Ask These Questions:
“What is the ‘1115 Waiver’ rule and do your coders know Florida Medicaid's version?”
“Are claims manageable during the oncoming hurricane?”
Avoid These Pitfalls:
Companies with no local client references, like Jacksonville or Tallahassee clinics,
No HIPAA-compliant data centers are located in Florida.
Case Study: Tampa Clinic Recovered $220k in 6 Months
The Problem:
A primary care clinic in Tampa encountered a 45% denial rate because the practice used incorrect Medicaid codes for chronic care management (CPT 99490).
The Solution:
Engaged Specialized-Billing.com for:
In-house coding audits.
Training workshops on Florida Medicaid’s “Episodes of Care” program.
The Result:
Denials were reduced to 20% within three months.
Revenue of $220k recovered, funding two additional exam rooms.
Future Trends in Florida Medical Billing
RevCycleAI denial prediction tools forecast Medicaid denials for submission and AI-driven denial predictions are now possible.
Telehealth Boom: New modifiers like 95 for real-time telehealth are mandated by Florida’s Senate Bill 1606.
Blockchain Security: Unity Health of Miami hospital network securely shares patient data across more than 10 hospitals using blockchain technology.
Conclusion
Nothing illustrates the ever-changing Florida billing landscape better than an unpredictable summer storm. However, the chaos can be transformed into seamless cash flow with the right medical billing partner. Specialized-Billing.com utilizes AI-driven technology with on-the-ground knowledge to ensure Florida clinics flourish, even during hurricane season.
Suffering from costly billing errors? Claim your free Florida billing audit at Specialized-Billing.com today.
2 notes
·
View notes
Text
Pag-unawa sa Fetal Movement
#decreased fetal movement#decreased fetal movement 22 weeks#decreased fetal movement 24 weeks#decreased fetal movement 38 weeks#decreased fetal movement icd 10#fetal movement#icd 10 code for decreased fetal movement#increased fetal movement#increased fetal movement 37 weeks sign of labor#increased fetal movement before labor#reasons for decreased fetal movement#reduced fetal movement#sudden increased fetal movement#what can cause decreased fetal movement in third trimester#what is considered decreased fetal movement#when do you feel fetal movement#when do you start feeling fetal movement#when to go to hospital for decreased fetal movement#when to worry about fetal movement#when to worry about increased fetal movement
0 notes
Text
With five years of experience in long-COVID, frontline doctors and mid-level providers have been searching for correctable factors to help patients get back on the right track.
Wu et al, used the TriNetX research network of COVID-19 patients between January 1 and November 30, 2022. Patients were matched using propensity score matching (PSM) and divided into VDD (< 20 ng/mL) and control (≥ 20 ng/mL) groups. The primary outcome was a composite of long-COVID, all-cause emergency department (ED) visits, hospitalization, and death during the follow-up period (90-180 days) after the diagnosis of COVID-19.
Vitamin D deficiency was not associated with the development of long-COVID identified by ICD-10 codes, however it was associated with a higher risk of all-cause ED visits (HR = 1.114; 95% CI = 1.012-1.226), all-cause hospitalization (HR = 1.230; 95% CI = 1.105-1.369), and all-cause death (HR = 1.748; 95% CI = 1.047-2.290).
In clinical practice I recommend 10,000 IU of vitamin D with 100-200 mcg of vitamin K2 to to my patients. This should eliminate any risk of vitamin D deficiency and hopefully will be part of a supplement regimen that keeps patients healthy and out of the hospital.
3 notes
·
View notes
Text
Medical Billing in India: A Comprehensive Guide to Streamlining Revenue & Ensuring Compliance
Medical Billing in India: A Comprehensive Guide to Streamlining Revenue & Ensuring Compliance
Managing medical billing efficiently is a critical aspect for healthcare providers in India. From private clinics to large hospitals, accurate billing processes not only maximize revenue but also ensure legal compliance and patient satisfaction. In this comprehensive guide, we explore everything you need to know about medical billing in India, covering best practices, benefits, challenges, and practical tips to optimize your healthcare practice’s revenue cycle management.
Introduction
as the Indian healthcare sector grows rapidly, wiht a mix of public and private entities, the importance of streamlined medical billing services cannot be overstated. Efficient billing ensures timely reimbursement, reduces revenue leakage, and maintains compliance with government regulations. This article offers a detailed overview of medical billing processes specific to India, helping healthcare providers navigate complex billing procedures with confidence and ease.
Understanding Medical Billing in India
What is medical Billing?
Medical billing is the process of translating healthcare services into billing claims to be paid by insurance companies, government agencies, or patients directly.It involves accurate coding, documentation, submission, and follow-up for reimbursement.
The Unique Landscape of Medical Billing in India
Multiple Payment Sources: Includes private insurance,government schemes (such as Ayushman Bharat),and cash payments.
Varied Regulatory Frameworks: Adherence to the Indian Medical Council, Government guidelines, and insurance policies.
Technological Adoption: Shift towards digital billing, Electronic Health Records (EHR), and telemedicine-based billing processes.
Key Components of Medical Billing in India
1. Accurate Patient billing Facts
Collect precise patient data, including insurance details, demographics, and medical history.
2. Medical Coding & Documentation
Use standardized coding systems like ICD-10 (international Classification of Diseases), CPT, or procedures codes tailored to Indian healthcare practices. Proper documentation ensures claim accuracy and reduces rejections.
3. Claim Submission
Submit claims through government portals or insurance providers’ platforms, ensuring compliance with form standards and deadlines.
4. Payment Posting & Reconciliation
Post payments accurately, reconcile discrepancies, and follow up on unpaid or rejected claims.
5. Compliance & Audit Readiness
Maintain detailed records to meet regulatory requirements and facilitate audits.
Benefits of Effective Medical Billing in India
Increased Revenue: Faster reimbursements and minimized revenue leakage.
Improved Cash Flow: Reduced billing cycle times ensure healthier financial status.
Regulatory compliance: Avoid penalties by adhering to Indian healthcare billing standards.
Patient Satisfaction: Transparent billing processes foster trust and loyalty.
Operational Efficiency: Automating billing reduces manual errors and saves time.
Practical Tips for Streamlining Medical Billing in India
Implement Robust Billing Software: Choose India-specific medical billing solutions that integrate seamlessly with EHR systems.
Train Your Staff Regularly: Ensure billing personnel are updated on latest coding standards, regulatory policies, and software usage.
Maintain Accurate and Complete Documentation: Clear medical records reduce claim denials.
Double-Check Claims Before Submission: routine audits on claim data can prevent rejections.
Leverage Automation & AI Tools: Automate repetitive tasks and use AI for fraud detection and error reduction.
Stay Updated on Regulations: Keep abreast of changes in government policies, insurance updates, and coding standards.
Challenges in Medical Billing in india
Complex Regulations: Navigating multiple payers and compliance standards.
Error-prone Processes: Manual data entry leads to increased rejection rates.
High rejection & Denial Rates: due to inaccurate coding or documentation issues.
Limited Technology Adoption: Manny clinics still rely on paper-based billing systems.
Case Study: Accomplished Implementation of Digital Medical Billing
Aspect
Before Implementation
after Implementation
Revenue Cycle Time
60-90 days
30-45 days
Claim Rejection Rate
15%
5%
Operational Efficiency
Manual, error-prone
Automated, accurate
This example highlights how adopting modern digital billing solutions in India can substantially enhance revenue flow, reduce rejection rates, and improve overall efficiency.
First-Hand Experience: Tips from a Healthcare Billing Expert in India
“In my experience, the key to successful medical billing in India lies in complete adherence to documentation standards, ongoing staff training, and leveraging the right technology. With the government launching schemes like Ayushman Bharat, understanding the specific billing requirements for such programs can unlock significant revenue streams.” – Dr. Ramesh Kumar, Healthcare Consultant
Conclusion
Medical billing in India is a vital component of healthcare management that directly impacts revenue generation and compliance. By understanding the complex Indian healthcare landscape, implementing effective billing practices, and embracing innovative technologies, healthcare providers can streamline their revenue cycles, reduce errors, and ensure regulatory adherence. Staying informed and adaptable is the key to thriving in this dynamic surroundings. Whether you own a small clinic or manage a large hospital, optimizing your medical billing process will pave the way for sustained growth and excellent patient care.
Additional Resources
India Healthcare Billing Guidelines
Top Medical Billing Software in India
Regulatory Updates on Indian Healthcare Policies
https://medicalcodingandbillingclasses.net/medical-billing-in-india-a-comprehensive-guide-to-streamlining-revenue-ensuring-compliance/
0 notes
Text
Open Your Future: How to Launch a Successful Career in Medical Billing and Coding
unlock Your Future: How to Launch a Triumphant Career in Medical Billing and Coding
Are you interested in entering the dynamic world of healthcare but not sure where to start? A career in medical billing and coding offers a promising pathway to a rewarding and stable profession. With the healthcare industry constantly growing, the need for skilled medical billing and coding specialists is on the rise.This thorough guide will walk you through essential steps, tips, and insights on how to successfully launch your career in this in-demand field.
What Is Medical Billing and Coding?
Medical billing and coding are critical components of the healthcare revenue cycle. Medical coders translate healthcare providers’ notes into standardized codes, which are then used to generate insurance claims and manage patient billing. Medical billers ensure that these claims are submitted correctly and processed efficiently, ensuring timely reimbursement for healthcare providers.
Why Choose a career in Medical Billing and Coding?
Embarking on a career in medical billing and coding offers numerous benefits, including:
High demand for qualified professionals across clinics, hospitals, and insurance companies
Flexible work options, including remote work possibilities
Competitive salaries that grow with experience
Minimal educational requirements, with certification often sufficient
Contributing to patient care by ensuring accurate medical documentation and billing
Steps to Launch a Successful Career in Medical Billing and coding
1. Understand the Role and Industry Requirements
Before diving into training, familiarize yourself with the responsibilities involved in medical billing and coding. although entry-level positions often require only a certification, some roles may prefer or require relevant experience, especially in specialized healthcare settings.
2. Enroll in Accredited Training Programs
The foundation of a successful career is proper education. Look for accredited medical billing and coding programs that offer comprehensive coursework covering topics like medical terminology, anatomy, coding systems (ICD-10, CPT, HCPCS), and healthcare compliance.
Popular options include:
Online certification courses
Community college programs
Vocational training centers
3. Obtain Relevant Certification
While certification isn’t always mandatory,earning a credential considerably enhances your job prospects and earning potential.The most recognized certifications include:
Certification
Issuing Institution
Benefits
Certificate in Medical billing and Coding
American Health Details Management Association (AHIMA)
Demonstrates professional competency
certified Professional Coder (CPC)
American Academy of Professional Coders (AAPC)
Widely recognized by employers
Certified Coding Associate (CCA)
AHIMA
ideal for beginners
4. Gain Practical Experience
Hands-on experience can be acquired through internships, volunteer opportunities, or entry-level positions. many online training programs include practical exercises to simulate real-world coding and billing tasks.
5. Build a Strong Resume and Professional Network
Create a compelling resume highlighting your training, certifications, and any relevant experience. Also, join professional associations like AAPC or AHIMA to network and discover job openings.
6. Apply for Jobs in Healthcare Facilities or Remote Positions
Start applying to clinics, hospitals, insurance companies, or consider remote medical billing and coding jobs, which are increasingly available as telehealth expands.
practical Tips for Success in Medical Billing and Coding
Stay updated on the latest coding guidelines and healthcare regulations
Develop strong attention to detail and excellent organizational skills
Enhance your computer literacy, especially with billing software and electronic health records (EHR)
Continuously seek professional development opportunities and additional certifications
Benefits of a Career in Medical Billing and Coding
Choosing this profession can led to a stable and rewarding career, especially with healthcare industry growth. Unique advantages include:
Work-life balance with flexible schedules
opportunities for advancement into management or specialized coding roles
Potential to work remotely,saving commuting time and expenses
Contributing to healthcare efficiency and patient care accuracy
Case Study: From Novice to Expert
Meet Sarah,who started as a medical billing apprentice. With her dedication to learning medical coding and earning her CPC certification,she quickly found a remote role with a healthcare provider. Over time, sarah advanced to a supervisory position, earning higher pay and gaining industry recognition.Her journey exemplifies the potential for growth in this industry-especially with a proactive approach and continuous learning.
First-Hand Experience and Testimonials
Many professionals in medical billing and coding emphasize the importance of perseverance and ongoing education. Jessica, a certified coder, mentions:
“Getting my certification opened doors I never imagined. The flexibility of remote work allowed me to balance my family life while building a thriving career.”
Conclusion
Launching a successful career in medical billing and coding is an achievable goal with the right strategy, education, and persistence. As the healthcare sector continues to grow,professionals in this field are more in demand than ever. By understanding industry requirements, obtaining proper certification, gaining practical experience, and staying updated on healthcare regulations, you can unlock a rewarding future in this vital and growing industry. Start today and take the first step toward a stable, flexible, and fulfilling career in medical billing and coding!
https://medicalbillingcertificationprograms.org/open-your-future-how-to-launch-a-successful-career-in-medical-billing-and-coding/
0 notes
Text
^follow this link^ to access an archive of over 1,000 open-access references to covid studies. Daily updates!
Abstract
BACKGROUND: COVID-19 is associated with acute risk of major adverse cardiac events (MACE), including myocardial infarction, stroke, and mortality (all-cause). However, the duration and underlying determinants of heightened risk of cardiovascular disease and MACE post–COVID-19 are not known.
METHODS: Data from the UK Biobank was used to identify COVID-19 cases (n=10 005) who were positive for polymerase chain reaction (PCR+)-based tests for SARS-CoV-2 infection (n=8062) or received hospital-based International Classification of Diseases version-10 (ICD-10) codes for COVID-19 (n=1943) between February 1, 2020 and December 31, 2020. Population controls (n=217 730) and propensity score—matched controls (n=38 860) were also drawn from the UK Biobank during the same period. Proportional hazard models were used to evaluate COVID-19 for association with long-term (>1000 days) risk of MACE and as a coronary artery disease risk equivalent. Additional analyses examined whether COVID-19 interacted with genetic determinants to affect the risk of MACE and its components.
RESULTS: The risk of MACE was elevated in COVID-19 cases at all levels of severity (HR, 2.09 [95% CI, 1.94–2.25]; P<0.0005) and to a greater extent in cases hospitalized for COVID-19 (HR, 3.85 [95% CI, 3.51–4.24]; P<0.0005). Hospitalization for COVID-19 represented a coronary artery disease risk equivalent since incident MACE risk among cases without history of cardiovascular disease was even higher than that observed in patients with cardiovascular disease without COVID-19 (HR, 1.21 [95% CI, 1.08–1.37]; P<0.005). A significant genetic interaction was observed between the ABO locus and hospitalization for COVID-19 (Pinteraction=0.01), with risk of thrombotic events being increased in subjects with non-O blood types (HR, 1.65 [95% CI, 1.29–2.09]; P=4.8×10−5) to a greater extent than subjects with blood type O (HR, 0.96 [95% CI, 0.66–1.39]; P=0.82).
CONCLUSIONS: Hospitalization for COVID-19 represents a coronary artery disease risk equivalent, with post–acute myocardial infarction and stroke risk particularly heightened in non-O blood types. These results may have important clinical implications and represent, to our knowledge, one of the first examples of a gene-pathogen exposure interaction for thrombotic events.
#mask up#covid#pandemic#covid 19#wear a mask#public health#coronavirus#sars cov 2#still coviding#wear a respirator#long covid#covid conscious#wear a fucking mask#covid is not over
32 notes
·
View notes
Text
Medical Coding Demystified: Essential Skills and Career Opportunities
In today’s rapidly growing healthcare industry, medical coding plays a pivotal role in ensuring the accuracy of medical records and the smooth processing of insurance claims. As hospitals, clinics, and insurance providers continue to digitise their processes, the demand for skilled medical coders is higher than ever. For aspiring professionals looking to break into this promising field, enrolling in Medical Coding Training in Coimbatore offers a strong foundation and career pathway in the healthcare sector.
What is Medical Coding?
Medical coding involves converting healthcare diagnoses, procedures, medical services, and equipment into standardised alphanumeric codes. These codes are drawn from standardised classification systems such as ICD (International Classification of Diseases), CPT (Current Procedural Terminology), and HCPCS (Healthcare Common Procedure Coding System). Medical coders review clinical documents and assign appropriate codes to ensure accurate billing and data analysis.
Medical coding is crucial for:
Accurate billing and reimbursement from insurance companies.
Monitoring health trends and conducting research.
Ensuring compliance with healthcare regulations.
Why Choose Medical Coding as a Career?
Choosing a career in medical coding offers numerous advantages:
High Demand: With the increasing digitisation of healthcare systems, trained coders are in constant demand.
Remote Work Opportunities: Many medical coding jobs offer the flexibility of working from home.
Job Stability: As healthcare is an essential industry, it offers strong job security.
Career Advancement: Opportunities exist to move into specialised coding, auditing, or medical billing and compliance roles.
The Importance of Medical Coding Training in Coimbatore
Coimbatore, known for its thriving educational environment and growing healthcare infrastructure, is an ideal place for aspiring coders to begin their journey. Medical Coding Training in Coimbatore offers comprehensive education and hands-on practice to equip students with the skills needed in the industry.
Key benefits of pursuing training in Coimbatore include:
Access to experienced instructors with real-world knowledge.
Exposure to up-to-date coding standards and software.
Opportunities for internships and on-the-job training.
Cost-effective education options compared to larger metro cities.
Essential Skills Acquired Through Medical Coding Training
To succeed in the field of medical coding, specific skills are vital. Training programs in Coimbatore help learners acquire and strengthen the following core competencies:
1. Understanding Medical Terminology
Medical coders must understand a wide range of medical terms related to anatomy, diseases, treatments, and procedures. Training helps students become fluent in medical language, which is critical for accurate coding.
2. Knowledge of Coding Systems
Programs typically cover various coding systems, such as:
ICD-10-CM (diagnosis coding)
CPT (procedural coding)
HCPCS Level II (services and supplies)
3. Analytical Thinking
Medical coders must evaluate medical records and determine the correct code even when documentation is complex or ambiguous. Training includes practical exercises to develop critical thinking and decision-making skills.
4. Attention to Detail
Accuracy is everything in coding. Even a small error can lead to denied claims or compliance issues. Students learn to code meticulously and review their work for accuracy.
5. Software Proficiency
Modern coding involves using Electronic Health Records (EHR) and specialised coding software. Training introduces students to these platforms to ensure they are job-ready.
Career Opportunities After Medical Coding Training in Coimbatore
Once you complete a Medical Coding Training program in Coimbatore, a wide range of career opportunities becomes accessible, including:
Medical Coder: Work in hospitals, clinics, or insurance companies, converting patient data into standardised codes.
Medical Billing Specialist: Manage the billing process, ensuring accurate reimbursement from insurers.
Coding Auditor: Review and verify coding accuracy for quality control and compliance.
Clinical Documentation Specialist: Collaborate with physicians to ensure complete and precise patient records.
Health Information Technician: Organise and manage health data, ensuring its accuracy and security.
Moreover, with the right experience and certifications (like CPC, CCS, or CCA), professionals can progress to supervisory or consulting roles.
Growing Industry and Global Opportunities
The healthcare industry is one of the fastest-growing sectors globally. Medical coders not only find employment locally but also have opportunities to work with international clients and organisations, especially in remote and outsourced roles.
Training in Coimbatore serves as a springboard for such global careers, with many programs designed to prepare students for international certifications and remote work environments.
Final Thoughts
Medical coding is no longer just a behind-the-scenes administrative task—it’s a dynamic, respected profession integral to healthcare operations. By enrolling in Medical Coding Training in Coimbatore, aspiring professionals can equip themselves with the essential skills needed to enter and excel in this promising field. With the right training, attention to detail, and continued learning, medical coding can lead to a rewarding and future-proof career.
Whether you're a recent graduate, a career switcher, or a healthcare professional seeking to expand your skillset, consider taking the next step with a structured training program in Coimbatore. It could be the beginning of a fulfilling journey into the heart of healthcare.
#Medical Billing Courses in Coimbatore#transcription certificate program in Coimbatore#Certificate Program in Medical Transcription Coimbatore#Medical Coding Academy in Coimbatore#Medical Coding Auditing training Coimbatore#Clinical Coding training Coimbatore#Dental Coding training Coimbatore#Health information Management courses Coimbatore#Saudi Coding training in Coimbatore#CPMA Training Coimbatore#AAPC institute of Medical Coding Coimbatore#Transcription Courses in Coimbatore#Medical Coding Course in Coimbatore#Australian Clinical Coding Training Coimbatore#Medical Transcription Course in Coimbatore#AM coding training in Coimbatore#Post graduate program in Health information management in Coimbatore#Medical coding Training Coimbatore#professional medical coding courses in Coimbatore#medical coding programs in Coimbatore#medical coding certification courses Coimbatore#medical coding course in India#Medical Billing Courses in India#tamilnadu#coimbatore#online learning#online courses#institution#training institute
0 notes