#Primary Sclerosing Cholangitis Treatment
Explore tagged Tumblr posts
Text
With this post, I am finally able to tie together the appearance of SPED, Turbocancers and excess Autoimmune Disease. I propose that the Spike Protein’s invasion of the Endothelium, followed by its invasion of the Extracellular Matrix, explains all three. Thank you for supporting my work, it has allowed me to look very deeply and discover.
As readers of this Substack know, I have, from the beginning, called the Spike Protein’s invasion of the Endothelium Spike Protein Endothelial Disease (SPED). I then proposed that the Spike Protein subsequently traveled from the Endothelium into the body’s organs, where it would induce autoimmune disease and/or fibrosis. Yet, the actual mechanism of this progression has eluded me – until now.
What I have discovered is that the Spike Protein’s ability to bind Integrin provides a perfectly satisfactory explanation for this malevolent journey and its deleterious consequences. To start, let us look at some autoimmune diseases which are found to be Integrin Regulated Autoimmune Disorders.
Type 1 Diabetes Mellitus
Rheumatoid Arthritis
Multiple Sclerosis
Systemic Lupus Erythematosus
Type 1 Autoimmune Hepatitis
Scleroderma
Let’s look at some studies, shall we?
Vaccination is one of the most vigorous ways to intervene in the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic. Cases of autoimmune hepatitis (AIH) after coronavirus disease (COVID-19) vaccination have been increasingly reported. Twenty-seven cases of AIH are summarized in this study, providing emerging evidence of autoimmune reactions in response to various COVID-19 vaccines, including in patients with special disease backgrounds such as primary sclerosing cholangitis (PSC), liver transplantation, and previous hepatitis C virus (HCV) treatment.
7 notes
·
View notes
Text
Primary Sclerosing Cholangitis Market Size, Share and Future News by 2025-2033
The Reports and Insights, a leading market research company, has recently releases report titled “Primary Sclerosing Cholangitis Market: Global Industry Trends, Share, Size, Growth, Opportunity and Forecast 2025-2033.” The study provides a detailed analysis of the industry, including the global Primary Sclerosing Cholangitis Market share, size, trends, and growth forecasts. The report also includes competitor and regional analysis and highlights the latest advancements in the market.
Report Highlights:
How big is the Primary Sclerosing Cholangitis Market?
The global primary sclerosing cholangitis market was valued at US$ 174.9 Million in 2024 and is expected to register a CAGR of 7.8% over the forecast period and reach US$ 370.8 Million in 2033.
What are Primary Sclerosing Cholangitis?
Primary sclerosing cholangitis (PSC) is a chronic liver condition characterized by ongoing inflammation and scarring of the bile ducts, leading to their narrowing, obstruction, and subsequent liver damage. Symptoms may include jaundice, itching, abdominal pain, and fatigue. PSC is often linked to an increased risk of liver cirrhosis and liver cancer. While the precise cause remains unclear, the disease is thought to involve autoimmune mechanisms and is frequently associated with inflammatory bowel diseases like ulcerative colitis. Treatment aims to alleviate symptoms, slow disease progression, and manage complications, with liver transplantation being a potential option for advanced stages.
Request for a sample copy with detail analysis: https://www.reportsandinsights.com/sample-request/2389
What are the growth prospects and trends in the Primary Sclerosing Cholangitis industry?
The primary sclerosing cholangitis (PSC) market growth is driven by various factors and trends. The market for primary sclerosing cholangitis (PSC) is expanding due to heightened awareness of the disease, improvements in diagnostic methods, and advancements in treatment options. Increasing recognition of PSC, particularly its links to inflammatory bowel diseases, along with the growing incidence of liver complications, is boosting demand for effective therapies. Key players in the market include pharmaceutical and biotechnology companies focusing on new drug developments and clinical trials. The market is also driven by the need for improved symptom management and potential curative approaches, such as liver transplantation. Despite challenges like high treatment costs and limited available therapies, ongoing research and innovation are contributing to the market's growth. Hence, all these factors contribute to primary sclerosing cholangitis (PSC) market growth.
What is included in market segmentation?
The report has segmented the market into the following categories:
By Type
Classic PSC
Variant PSC
PSC Associated with Autoimmune Hepatitis
PSC with Cholangiocarcinoma
By Treatment Type
Ursodeoxycholic Acid
Obeticholic Acid
Methotrexate
Corticosteroids
Others
By Route of Administration
Oral
Parental
Others
By End-User
Hospital Pharmacies
Retail Pharmacies
Online Pharmacies
North America
United States
Canada
Europe
Germany
United Kingdom
France
Italy
Spain
Russia
Poland
Benelux
Nordic
Rest of Europe
Asia Pacific
China
Japan
India
South Korea
ASEAN
Australia & New Zealand
Rest of Asia Pacific
Latin America
Brazil
Mexico
Argentina
Middle East & Africa
Saudi Arabia
South Africa
United Arab Emirates
Israel
Rest of MEA
Who are the key players operating in the industry?
The report covers the major market players including:
Acorda Therapeutics, Inc.
Gilead Sciences, Inc.
NGM Biopharmaceuticals, Inc.
Intercept Pharmaceuticals, Inc.
Falk Pharma GmbH
Allergan Plc.
Shire Plc.
Durect Corporation
Conatus Pharmaceuticals, Inc.
Sirnaomics, Inc.
Shenzhen HighTide Biopharmaceutical Ltd.
Cymabay Therapeutics
Pliant Therapeutics
Immunic AG
View Full Report: https://www.reportsandinsights.com/report/Primary Sclerosing Cholangitis-market
If you require any specific information that is not covered currently within the scope of the report, we will provide the same as a part of the customization.
About Us:
Reports and Insights consistently mееt international benchmarks in the market research industry and maintain a kееn focus on providing only the highest quality of reports and analysis outlooks across markets, industries, domains, sectors, and verticals. We have bееn catering to varying market nееds and do not compromise on quality and research efforts in our objective to deliver only the very best to our clients globally.
Our offerings include comprehensive market intelligence in the form of research reports, production cost reports, feasibility studies, and consulting services. Our team, which includes experienced researchers and analysts from various industries, is dedicated to providing high-quality data and insights to our clientele, ranging from small and medium businesses to Fortune 1000 corporations.
Contact Us:
Reports and Insights Business Research Pvt. Ltd. 1820 Avenue M, Brooklyn, NY, 11230, United States Contact No: +1-(347)-748-1518 Email: [email protected] Website: https://www.reportsandinsights.com/ Follow us on LinkedIn: https://www.linkedin.com/company/report-and-insights/ Follow us on twitter: https://twitter.com/ReportsandInsi1
#Primary Sclerosing Cholangitis Market share#Primary Sclerosing Cholangitis Market size#Primary Sclerosing Cholangitis Market trends
0 notes
Text
When is a Liver Transplant Considered Necessary in Cases of Jaundice?
Jaundice, marked by yellowing of the skin and eyes, often results from underlying liver or bile duct dysfunction. While most cases of jaundice can be treated through medication, lifestyle changes, or minor procedures, a liver transplant becomes necessary in severe situations where the liver fails to perform its essential functions despite treatment.
For conditions involving bile duct obstructions or related complications, urology treatment in Coimbatore offers specialized care to manage and address such issues effectively. Comprehensive urology treatment in Coimbatore ensures accurate diagnosis and timely intervention, preventing severe complications
Key Indicators for Liver Transplant in Jaundice
Acute Liver Failure:
Rapid deterioration of liver function caused by infections, toxins, or autoimmune diseases.
Symptoms: Severe jaundice, confusion, swelling, and impaired blood clotting.
Chronic Liver Diseases:
Conditions like cirrhosis or hepatitis leading to irreversible liver damage.
Persistent jaundice along with fatigue, fluid retention, and gastrointestinal bleeding.
Primary Biliary Cirrhosis or Sclerosing Cholangitis:
Chronic diseases that obstruct bile flow and cause progressive liver damage.
Liver Cancer (Hepatocellular Carcinoma):
Tumors causing jaundice due to obstruction of bile ducts or extensive liver involvement.
Genetic Disorders:
Conditions like Wilson’s disease or hemochromatosis affecting liver function.
Role of Pre-Transplant Evaluation
Before considering a liver transplant, a comprehensive evaluation is necessary to assess:
Liver function through blood tests and imaging.
Overall health and suitability for transplant surgery.
Related complications, such as kidney dysfunction, which might require urology treatment in Coimbatore for optimal care.
Surgical Considerations for Liver Transplant
Donor Liver Selection:
Can be from a deceased donor or a living donor providing part of their liver.
Compatibility tests ensure successful transplantation.
Post-Operative Care:
Requires lifelong immunosuppressive therapy to prevent organ rejection.
Regular monitoring of liver and kidney function is essential, especially for patients receiving urology treatment in Coimbatore to address related complications.
Why Jaundice Management Requires Multidisciplinary Care
In severe jaundice cases, the liver’s dysfunction can impact other organs, including the kidneys. Conditions like hepatorenal syndrome, where liver failure leads to kidney dysfunction, require integrated care. Leading centers like GEM Hospital excel in urology treatment in Coimbatore, ensuring comprehensive management of both hepatic and renal health.
When to Consult a Specialist?
Jaundice persists despite treatment or worsens over time.
Symptoms like abdominal swelling, bleeding tendencies, or mental confusion arise.
A diagnosis of chronic liver disease with significant complications.
Advanced Care at GEM Hospital
GEM Hospital is renowned for its expertise in urology treatment in Coimbatore and its comprehensive approach to managing complex jaundice cases. With state-of-the-art facilities and a multidisciplinary team, the hospital provides seamless coordination between hepatology, gastroenterology, and urology experts.
If jaundice persists or complications develop, a timely consultation can make all the difference. Visit GEM Hospital for expert evaluation and advanced care.
Book your appointment today at GEM Hospital for expert care and advanced treatment solutions!
0 notes
Text
Ursodeoxycholic Acid Ursoset 300 Tablet: A Comprehensive Overview
Introduction to Ursodeoxycholic Acid Ursoset 300 Tablet
Ursodeoxycholic Acid (UDCA), the active ingredient in Ursoset 300 Tablet, is a naturally occurring bile acid that supports and enhances digestive system function, particularly in liver and gallbladder health.For centuries, bile acids have been recognized for their crucial function in fat digestion and absorption. Ursoset 300, containing 300mg of UDCA, has emerged as a cornerstone in the medical management of various hepatobiliary disorders. Its unique mechanism of action, distinct from other bile acids, allows it to dissolve certain types of gallstones and improve bile flow in the liver. This introduction sets the stage for a deeper exploration of its medical applications, benefits, and established efficacy.
Medical Use and Benefits of Ursoset 300
Ursodeoxycholic Acid in Ursoset 300 Tablet is primarily utilized for its therapeutic effects on the liver and gallbladder. Its main medical applications include:
Gallstone Dissolution:
One of the primary uses of UDCA is to help dissolve cholesterol-based gallstones effectively.
Offers a non-invasive alternative for patients with small to medium-sized non-calcified gallstones, especially those not candidates for surgery.
Works by reducing cholesterol saturation of bile and dissolving existing stones.
Primary Biliary Cholangitis (PBC) Management:
UDCA is the only FDA-approved medication for treating Primary Biliary Cholangitis (PBC), a chronic liver disease that gradually damages and destroys the bile ducts.
Improves bile flow, protects liver cells, and slows disease progression.
Delays liver transplant and improves survival and quality of life.
Intrahepatic Cholestasis of Pregnancy (ICP):
Often prescribed to pregnant women experiencing ICP, a liver condition with intense itching.
Helps lower elevated bile acid levels, alleviating symptoms and improving fetal outcomes.
Other Cholestatic Liver Diseases:
May be used in other cholestatic liver diseases where bile flow is impaired (e.g., primary sclerosing cholangitis, cystic fibrosis-related liver disease).
Aims to improve liver function and reduce symptoms.
The benefits extend beyond just symptomatic relief, often translating to improved liver function tests, reduced inflammation, and a better prognosis for patients with these chronic conditions.
Uses and Effectiveness of Ursodeoxycholic Acid
The effectiveness of Ursodeoxycholic Acid Ursoset 300 Tablet is well-documented across its primary indications.
Gallstone Dissolution:
Can achieve complete dissolution in a significant percentage of patients, with success rates varying.
Treatment often requires several months to over a year.
Primary Biliary Cholangitis (PBC):
Highly effective in improving liver biochemical parameters (e.g., alkaline phosphatase, bilirubin levels).
Slows disease progression and is considered the standard of care.
Intrahepatic Cholestasis of Pregnancy (ICP):
Effectively reduces maternal itching.
Significantly improves fetal outcomes by lowering circulating bile acid levels.
Its effectiveness lies in its unique ability to alter the composition of bile, making it less toxic to liver cells and more conducive to dissolving cholesterol.
Clinical Efficacy and Safety of Ursoset 300
The clinical efficacy of Ursodeoxycholic Acid has been established through numerous studies, making Ursoset 300 Tablet a staple in gastroenterology and hepatology.
Efficacy in PBC:
Large-scale clinical trials demonstrate UDCA significantly prolongs transplant-free survival in PBC patients.
Normalizes liver enzymes in a substantial proportion of patients.
Delays the onset of complications associated with advanced liver disease.
Safety Profile:
Generally well-tolerated with a favorable safety profile.
Most common side effects are mild gastrointestinal disturbances (e.g., diarrhea), usually transient.
Serious side effects are rare, making it suitable for long-term use and during pregnancy.
Comparison to Other Treatments:
For gallstone dissolution, UDCA offers a non-surgical alternative, avoiding cholecystectomy risks.
In PBC, its role as first-line treatment is undisputed due to its proven ability to alter disease history.
Regular monitoring of liver function tests is recommended to assess efficacy and adjust dosage.
Conclusion: The Indispensable Role of Ursodeoxycholic Acid
Ursodeoxycholic Acid Ursoset 300 Tablet stands as a cornerstone in the medical management of various hepatobiliary disorders. Its unique mechanism of action allows for the effective dissolution of cholesterol gallstones and significant improvement in the prognosis of chronic liver diseases like Primary Biliary Cholangitis and Intrahepatic Cholestasis of Pregnancy. With a well-established clinical efficacy and a favorable safety profile, Ursoset 300 offers a reliable and often non-invasive therapeutic option for patients suffering from these conditions. Consulting a healthcare professional for diagnosis and a treatment plan is always recommended to ensure optimal outcomes.
0 notes
Text
IgG4-Related Disease Market Size, Share, Key Drivers, Trends, Challenges and Competitive Analysis
Global IgG4-Related Disease Market - Size, Share, Demand, Industry Trends and Opportunities
Global IgG4-Related Disease Market, By Disease Type (Type 1 (IgG4-Related) Autoimmune Pancreatitis (AIP), Retroperitoneal Fibrosis, IgG4-Related Tubulointerstitial Nephritis (TIN), IgG4-Related Sclerosing Cholangitis IgG4-Related Dacryoadenitis and Sialadenitis, IgG4-Related Pachymeningitis, IgG4-Related Thyroid Disease, Serum IgG4 Concentration, and Others), Type (Diagnostic and Treatment), Route of Administration (Parenteral, Oral and Others), End-User (Hospitals, Specialty Clinics, and Others) Distribution Channel (Hospital Pharmacy, Retail Pharmacy, Online Pharmacy, and Others) – Industry Trends.
Data Bridge Market Research analyses that the global IgG4-related disease market, which was USD 3.63 billion in 2023, is expected to reach USD 4.92 billion by 2031, at a CAGR of 3.9% during the forecast period 2024 to 2031.
Access Full 350 Pages PDF Report @
**Segments**
- By Type: Based on type, the IgG4-related disease market can be segmented into type 1 autoimmune pancreatitis, type 2 autoimmune pancreatitis, Mikulicz disease, and IgG4-related tubulointerstitial nephritis.
- By Diagnosis: In terms of diagnosis, the market can be classified into imaging studies (CT, MRI, PET/CT), laboratory tests (serum IgG4 levels, ESR, CRP), biopsy, and others.
- By Treatment: The treatment segment can be divided into medication (corticosteroids, immunosuppressants), surgery, and others (radiation therapy, plasmapheresis).
**Market Players**
- F. Hoffmann-La Roche Ltd.
- Novartis AG
- Eli Lilly and Company
- Takeda Pharmaceutical Company Limited
- AbbVie Inc.
- Bristol-Myers Squibb Company
- AstraZeneca
- Pfizer Inc.
- Amgen Inc.
- Johnson & Johnson
- GlaxoSmithKline plc
- Sanofi
- Merck & Co., Inc.
- Biogen
- Celgene Corporation
The IgG4-related disease market is characterized by advancements in diagnostic techniques, increasing awareness among healthcare professionals, and a growing number of clinical trials to develop novel treatment options. The rising prevalence of IgG4-related disease is a key factor driving market growth. Additionally, the availability of technologically advanced imaging modalities for accurate diagnosis and increasing investments in research and development activities contribute to the expansion of the market. The segmentation based on type allows for a more targeted approach towards treatment, leading to personalized care for patients. Diagnosis plays a crucial role in the management of IgG4-related disease, with imaging studies and specific laboratory tests aiding in timely detection and appropriate intervention. The treatment segment encompasses various options, including medications and surgical procedures, providing a comprehensive outlook on therapeutic approaches.
The IgG4-related disease market is witnessing significant growth driven by various factors. One of the primary drivers is the increasing prevalence of IgG4-related disease, leading to a higher demand for diagnosis and treatment options. Advances in diagnostic techniques such as imaging studies (CT, MRI, PET/CT) and laboratory tests (serum IgG4 levels, ESR, CRP) have improved the accuracy of diagnosing this condition, thereby boosting market growth. Moreover, growing awareness among healthcare professionals about IgG4-related disease symptoms and risk factors is contributing to early detection and intervention.
Market players in the IgG4-related disease market are actively involved in research and development activities to introduce novel treatment options for patients. Pharmaceutical companies such as F. Hoffmann-La Roche Ltd., Novartis AG, and Eli Lilly and Company are investing in clinical trials to develop innovative medications and therapeutic approaches. The presence of key players like Takeda Pharmaceutical Company Limited, AbbVie Inc., and Bristol-Myers Squibb Company further intensifies competition in the market, leading to a broader range of treatment options for patients.
The segmentation of the IgG4-related disease market based on type and diagnosis allows for a more targeted and personalized approach to managing the condition. Different types of IgG4-related diseases require specific treatment strategies, and accurate diagnosis is essential for determining the most appropriate course of action. The availability of multiple treatment options, including medications (corticosteroids, immunosuppressants), surgery, and other modalities like radiation therapy and plasmapheresis, provides healthcare providers with a diversified toolkit to address the needs of patients effectively.
Technological advancements in imaging modalities and laboratory tests continue to play a crucial role in the diagnosis and monitoring of IgG4-related disease. The integration of artificial intelligence and machine learning in diagnostic tools is facilitating quicker and more accurate assessments, leading to improved patient outcomes. Furthermore, collaborative efforts between market players, research institutions, and healthcare organizations are**Global IgG4-Related Disease Market Analysis:**
The Global IgG4-Related Disease Market is witnessing significant growth due to several key factors. The increasing prevalence of IgG4-related disease is a primary driver for market expansion, leading to a higher demand for advanced diagnostic techniques and innovative treatment options. Advancements in imaging studies (CT, MRI, PET/CT) and laboratory tests (serum IgG4 levels, ESR, CRP) have improved the accuracy of diagnosis, fostering market growth. Additionally, the rising awareness among healthcare professionals about IgG4-related disease symptoms and risk factors is aiding in early detection and timely intervention.
Market players such as F. Hoffmann-La Roche Ltd., Novartis AG, Eli Lilly and Company, Takeda Pharmaceutical Company Limited, and others are actively engaged in research and development endeavors to introduce novel treatment options for patients. The competitive landscape of the market is intensified by the presence of key pharmaceutical companies, leading to a broader range of therapeutic approaches for IgG4-related disease management. Collaboration between market players, research institutions, and healthcare organizations is driving innovation and providing new insights into the market.
The segmentation of the market based on disease type, diagnosis, and treatment allows for a personalized and targeted approach towards managing IgG4-related disease. Different types of IgG4-related diseases necessitate specific treatment strategies, emphasizing the importance of accurate diagnosis in determining the most suitable course of action. With multiple treatment options available, including medications (
The IgG4-Related Disease Market competitive landscape provides details by the competitors. Details included are company overview, company financials, revenue generated, market potential, investment in research and development, new market initiatives, production sites and facilities, production capacities, company strengths and weaknesses, product launch, product width and breadth, and application dominance.
Major Points Covered in TOC:
IgG4-Related Disease Market Overview: It incorporates six sections, research scope, significant makers covered, market fragments by type, IgG4-Related Disease Market portions by application, study goals, and years considered.
IgG4-Related Disease Market Landscape: Here, the opposition in the Worldwide IgG4-Related Disease Market is dissected, by value, income, deals, and piece of the pie by organization, market rate, cutthroat circumstances Landscape, and most recent patterns, consolidation, development, obtaining, and portions of the overall industry of top organizations.
IgG4-Related Disease Profiles of Manufacturers: Here, driving players of the worldwide IgG4-Related Disease Market are considered dependent on deals region, key items, net edge, income, cost, and creation.
IgG4-Related Disease Market Status and Outlook by Region: In this segment, the report examines about net edge, deals, income, creation, portion of the overall industry, CAGR, and market size by locale. Here, the worldwide IgG4-Related Disease Market is profoundly examined based on areas
IgG4-Related Disease Application or End User: This segment of the exploration study shows how extraordinary end-client/application sections add to the worldwide IgG4-Related Disease Market.
IgG4-Related Disease Market Forecast: Production Side: In this piece of the report, the creators have zeroed in on creation and creation esteem conjecture, key makers gauge, and creation and creation esteem estimate by type.
Keyword: Research Findings and Conclusion: This is one of the last segments of the report where the discoveries of the investigators and the finish of the exploration study are given.
The Report Can Answer the Following Questions:
Who are the global key players of IgG4-Related Disease industry? How are their operating situation (capacity, production, price, cost, gross and revenue)?
What are the types and applications of IgG4-Related Disease? What is the market share of each type and application?
What are the upstream raw materials and manufacturing equipment of IgG4-Related Disease? What is the manufacturing process of IgG4-Related Disease?
Economic impact on IgG4-Related Disease industry and development trend of IgG4-Related Disease industry.
What are the key factors driving the global IgG4-Related Disease industry?
What are the key market trends impacting the growth of the IgG4-Related Disease market?
What are the IgG4-Related Disease market challenges to market growth?
What are the IgG4-Related Disease market opportunities and threats faced by the vendors in the global IgG4-Related Disease market?
Browse Trending Reports:
Down and Feather Pillow Market Mobile Personal Emergency Response Systems Market Ectopic Pregnancy Market Diameter Signaling Market Bluetooth Hearing Aids Market Ganglion Cysts Treatment Market Bring Your Own Device Market Point-of-Care (POC) Drug Abuse Testing Market Carbon Nanotubes Market Satellite Backhaul Market
About Data Bridge Market Research:
Data Bridge set forth itself as an unconventional and neoteric Market research and consulting firm with unparalleled level of resilience and integrated approaches. We are determined to unearth the best market opportunities and foster efficient information for your business to thrive in the market. Data Bridge endeavors to provide appropriate solutions to the complex business challenges and initiates an effortless decision-making process.
Contact Us:
Data Bridge Market Research
US: +1 614 591 3140
UK: +44 845 154 9652
APAC : +653 1251 975
Email: [email protected]"
0 notes
Text
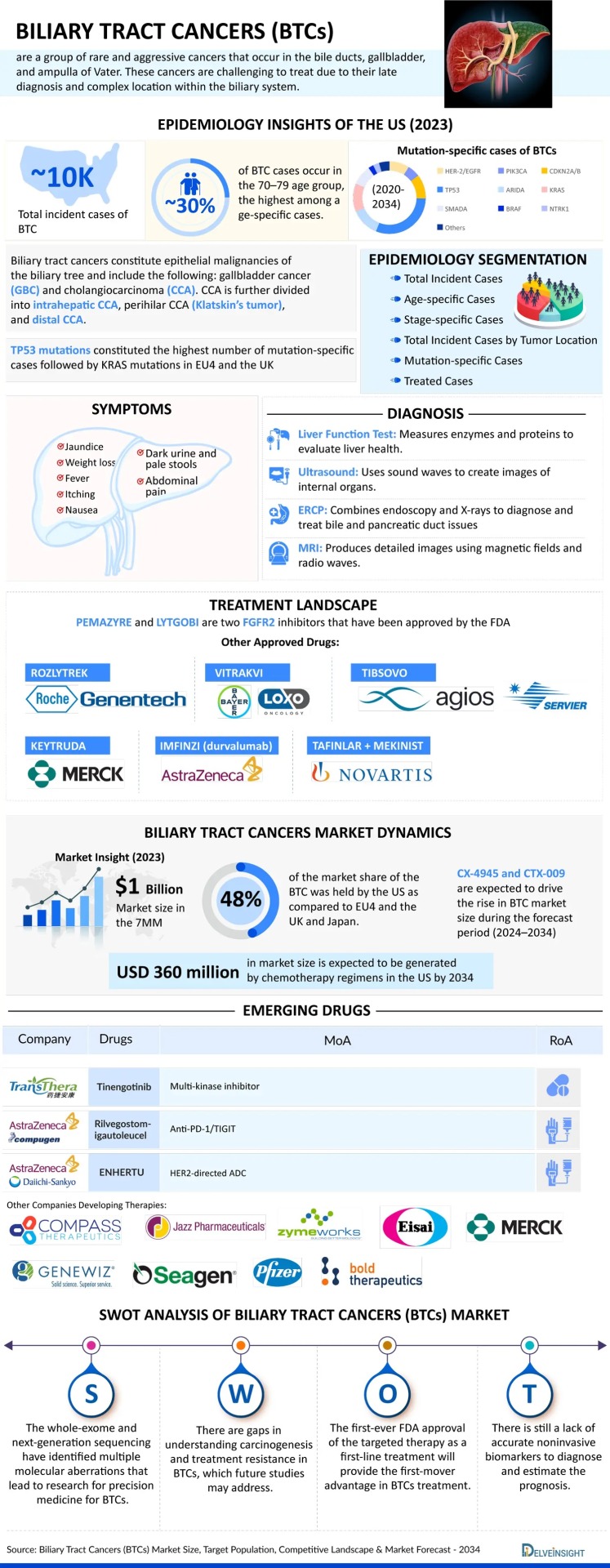
Biliary Tract Cancers (BTCs)
Biliary tract cancers (BTCs), also referred to as cholangiocarcinomas, are uncommon and highly aggressive tumors that develop within the bile ducts—the network that transports bile from the liver to the gallbladder and small intestine. These malignancies can arise in different areas of the biliary tree, including intrahepatic, perihilar, and distal sections. Due to the absence of noticeable symptoms in early stages, BTCs are typically identified only after the disease has progressed, complicating treatment. Common signs of the disease include jaundice, unintentional weight loss, abdominal discomfort, and itching. Key risk factors include chronic liver conditions such as hepatitis, cirrhosis, and primary sclerosing cholangitis.
While treatment advancements—including surgery, chemotherapy, and targeted therapies—have been made, outcomes remain generally poor because of late diagnosis and limited effective options. BTCs predominantly affect people over the age of 50, with both genders impacted, and regional differences observed in incidence rates. Current research is centered on early diagnostic tools and more effective therapeutic approaches to improve patient survival.
Curious about the numbers? Dive into the data with our infographic
Epidemiological Segmentation (2020–2034)
Epidemiological analysis of BTC in the 7 major markets (7MM) is categorized into:
Total incident cases
Age-specific incidence
Stage-wise distribution
Tumor location-specific incidence
Mutation-specific cases
Number of treated cases
BTC Epidemiology (2023 Highlights)
In 2023, the U.S. contributed about 30% of all new BTC cases across the 7MM.
Within the U.S., TP53 mutation-positive BTC cases were the most common, followed by KRAS-positive cases.
Among EU4 and the UK, Italy recorded the highest number of BTC cases; Spain had the fewest.
In the U.S., the majority of cases occurred in individuals aged 70 to 79, comprising around 30% of all age-related cases.
BTC Market Overview
The market size for biliary tract cancers in the 7MM reached approximately USD 1 billion in 2023.
From insights to impact—read the full report now : Click Here
Market Growth Drivers
Increased focus on targeted therapy and immunotherapy research.
Rising number of clinical trials exploring novel BTC treatments.
Progress in diagnostic tools and biomarkers that enable earlier detection.
Boost in pharmaceutical investment in rare cancers and personalized medicine.
Market Challenges
Lack of effective, widely available targeted treatments.
Late detection contributes to limited treatment effectiveness and poorer outcomes.
High treatment costs, particularly for advanced therapies and surgeries.
Limited public and clinical awareness of BTC, resulting in delays in diagnosis and intervention.
One graphic, all the essentials— Click to explore
Promising Pipeline Therapies
Emerging drugs under development include:
Tinengotinib
Rilvegostomig
ENHERTU (trastuzumab deruxtecan)
LENVIMA (lenvatinib)
Tasurgratinib (by Eisai)
Silmitasertib (CX-4945)
Among others
Key Companies in the BTC Space
Major pharmaceutical and biotech firms involved in BTC drug development include:
Compass Therapeutics
Jazz Pharmaceuticals
Zymeworks
AstraZeneca
Daiichi Sankyo
Merck Sharp & Dohme
Eisai
Senhwa Biosciences
Seagen
Pfizer
TransThera Sciences
Compugen
Bold Therapeutics
And others
Numbers tell part of the story—get the full analysis in our report
0 notes
Text
Liver Cirrhosis: Symptoms, Causes, and Treatment Options

Introduction
The liver is one of the most vital organs in the human body, performing essential functions such as detoxification, protein synthesis, bile production, and nutrient storage. When the liver becomes severely scarred due to chronic damage, it leads to a condition called cirrhosis. This irreversible scarring disrupts liver function and can lead to life-threatening complications if not managed properly.
In Zambia, liver cirrhosis is a growing health concern, often linked to alcohol abuse, viral hepatitis, and fatty liver disease. Early detection and proper management can slow disease progression and improve quality of life. This article explores the symptoms, causes, diagnosis, and treatment options for liver cirrhosis, with a focus on prevention and care in Zambia.
What Is Liver Cirrhosis?
Cirrhosis occurs when healthy liver tissue is replaced by fibrous scar tissue, impairing the organ’s ability to function. The liver becomes hard and nodular, leading to portal hypertension (increased blood pressure in the liver’s blood vessels) and liver failure in advanced stages.
Stages of Cirrhosis
Compensated Cirrhosis – The liver is damaged but still functioning; symptoms may be mild or absent.
Decompensated Cirrhosis – Severe scarring leads to complications like jaundice, fluid retention, and internal bleeding.
Common Causes of Liver Cirrhosis in Zambia
1. Excessive Alcohol Consumption
Chronic alcohol abuse is a leading cause of cirrhosis. Alcohol metabolizes into toxic substances that inflame and destroy liver cells, leading to scarring over time. Even moderate drinking over many years can contribute to liver damage.
2. Viral Hepatitis (B and C)
Hepatitis B and Hepatitis C are major causes of cirrhosis in Zambia.
These viruses spread through contaminated blood, unsafe medical practices, unprotected sex, and mother-to-child transmission.
Without treatment, chronic hepatitis leads to liver inflammation, fibrosis, and cirrhosis.
3. Non-Alcoholic Fatty Liver Disease (NAFLD) & NASH
Linked to obesity, diabetes, and high cholesterol, NAFLD causes fat buildup in the liver.
In some cases, it progresses to NASH (Non-Alcoholic Steatohepatitis), leading to inflammation and cirrhosis.
4. Other Causes
Autoimmune liver diseases (Primary Biliary Cholangitis, Autoimmune Hepatitis)
Genetic disorders (Hemochromatosis, Wilson’s Disease)
Bile duct disorders (Primary Sclerosing Cholangitis)
Long-term medication use (e.g., excessive paracetamol)
Symptoms of Liver Cirrhosis
Early-stage cirrhosis often has no noticeable symptoms. However, as the disease progresses, the following signs may appear:
Early Symptoms
Fatigue and weakness
Loss of appetite
Nausea and weight loss
Mild abdominal discomfort
Advanced Symptoms
Jaundice (yellowing of skin and eyes)
Swelling in legs (edema) and abdomen (ascites)
Easy bruising and bleeding (due to reduced clotting factors)
Itchy skin (from bile buildup)
Confusion and memory problems (hepatic encephalopathy)
Spider-like blood vessels on the skin (spider angiomas)
Diagnosis of Liver Cirrhosis
Early detection is crucial to prevent further liver damage. Doctors use several diagnostic methods:
1. Blood Tests
Liver Function Tests (LFTs) – Check enzyme levels (ALT, AST), bilirubin, and albumin.
Complete Blood Count (CBC) – Low platelets may indicate cirrhosis.
Viral Hepatitis Screening – Detects Hepatitis B and C.
2. Imaging Tests
Ultrasound – Detects liver texture changes.
FibroScan (Elastography) – Measures liver stiffness (fibrosis).
CT Scan or MRI – Provides detailed liver images.
3. Liver Biopsy
A small liver tissue sample is examined to confirm cirrhosis and assess damage severity.
Treatment and Management of Cirrhosis
While cirrhosis is irreversible, treatment focuses on slowing progression and managing complications.
1. Lifestyle Changes
Stop alcohol completely – Even small amounts worsen liver damage.
Healthy diet – Low salt, high protein, and nutrient-rich foods.
Weight management – Crucial for fatty liver-related cirrhosis.
2. Medications
Antiviral drugs (for Hepatitis B & C)
Diuretics (reduce fluid retention)
Lactulose (prevents brain fog from toxins)
3. Managing Complications
Ascites (fluid buildup) – Low-sodium diet, diuretics, or drainage.
Variceal bleeding – Beta-blockers or endoscopic treatment.
Hepatic encephalopathy – Medications to reduce ammonia levels.
4. Liver Transplant
In end-stage cirrhosis, a liver transplant may be the only cure. However, availability in Zambia is limited, emphasizing the need for early intervention.
Prevention Tips for Liver Cirrhosis
Limit Alcohol – Avoid excessive drinking to prevent liver damage.
Get Vaccinated – Hepatitis B vaccine is highly effective.
Practice Safe Sex & Hygiene – Reduces Hepatitis B & C risk.
Control Diabetes & Obesity – Prevents fatty liver disease.
Avoid Unnecessary Medications – Some drugs harm the liver.
Regular Health Checkups – Early detection of liver issues.
Conclusion
Liver cirrhosis is a serious but preventable and manageable condition. In Zambia, raising awareness about alcohol abuse, viral hepatitis, and metabolic diseases is key to reducing cirrhosis cases. Early diagnosis, lifestyle changes, and proper medical care can slow disease progression and improve survival rates.
If you or a loved one experiences symptoms like fatigue, jaundice, or abdominal swelling, consult a doctor immediately. A healthy liver means a healthier life!
#Hepatic Cirrhosis#Cirrhosis of the liver#Liver cirrhosis#liver cirrhosis symptoms#Liver cirrhosis treatment#Fatty Liver Disease#Hepatitis C#liver disease
0 notes
Text
Comprehensive Guide to Liver Diseases: Causes, Symptoms, and Treatment
Comprehensive Guide to Liver Diseases: Causes, Symptoms, and Treatment
16th World Digestive and Liver Diseases Conference from December 17-19,2025 in Dubai, UAE
Introduction
The liver is one of the most vital organs in the human body, responsible for numerous essential functions, including detoxification, protein synthesis, and digestion. However, liver diseases have become a growing global health concern, affecting millions of people every year. Understanding the causes, symptoms, and available treatments for liver diseases is crucial for early detection and effective management.
The 16th World Digestive and Liver Diseases Conference serves as a key platform for medical professionals, researchers, and healthcare providers to discuss the latest advancements and challenges in diagnosing and treating liver diseases. This guide explores the most common liver diseases, their underlying causes, symptoms, and available treatment options.
What is Liver Disease?
Liver disease refers to any condition that negatively impacts the liver's function and health. The liver plays a vital role in processing nutrients, filtering toxins from the blood, and aiding digestion. Damage to the liver can be caused by infections, autoimmune disorders, metabolic issues, genetic predisposition, and lifestyle factors such as alcohol consumption and poor diet.
Types of Liver Diseases
Liver diseases can be categorized into several major types:
1. Hepatitis
Hepatitis is inflammation of the liver, often caused by viral infections (Hepatitis A, B, C, D, and E).
Hepatitis A – Spread through contaminated food and water.
Hepatitis B – Transmitted through blood, semen, and other bodily fluids.
Hepatitis C – Primarily spread through blood contact (e.g., shared needles).
Hepatitis D – Only occurs in individuals with Hepatitis B.
Hepatitis E – Spread through contaminated water.
2. Fatty Liver Disease
Fatty liver disease occurs when excess fat builds up in the liver. It can be:
Non-Alcoholic Fatty Liver Disease (NAFLD): Associated with obesity, diabetes, and poor diet.
Alcoholic Fatty Liver Disease: Caused by excessive alcohol consumption.
3. Cirrhosis
Cirrhosis is the result of long-term damage to the liver, causing scarring (fibrosis). It can lead to liver failure if untreated. Common causes include chronic alcohol abuse, hepatitis, and fatty liver disease.
4. Liver Cancer
Hepatocellular carcinoma (HCC) is the most common type of liver cancer. It is often linked to hepatitis infection, cirrhosis, and long-term alcohol abuse.
5. Autoimmune Liver Diseases
In autoimmune liver diseases, the body’s immune system mistakenly attacks healthy liver cells. Examples include:
Autoimmune Hepatitis
Primary Biliary Cholangitis (PBC)
Primary Sclerosing Cholangitis (PSC)
6. Genetic Liver Diseases
Inherited liver diseases result from genetic mutations. Examples include:
Hemochromatosis – Excess iron accumulation in the liver.
Wilson’s Disease – Excess copper buildup in the liver.
Causes of Liver Diseases
The underlying causes of liver diseases can vary depending on the type of disease. The most common causes include: ✅ Viral Infections – Hepatitis viruses (A, B, C, D, E). ✅ Alcohol and Substance Abuse – Excessive alcohol consumption damages liver cells. ✅ Poor Diet and Obesity – High-fat, high-sugar diets contribute to fatty liver disease. ✅ Genetic Disorders – Inherited metabolic issues such as hemochromatosis. ✅ Autoimmune Disorders – The immune system attacking liver tissue. ✅ Toxins and Medications – Long-term exposure to certain medications and chemicals.
Symptoms of Liver Diseases
Symptoms of liver disease often appear gradually and may vary based on the type and severity of the condition. Common signs include:
Fatigue and Weakness
Jaundice (Yellowing of the Skin and Eyes)
Abdominal Pain and Swelling
Dark Urine and Pale Stools
Unexplained Weight Loss
Nausea and Vomiting
Itchy Skin
Diagnosis of Liver Diseases
To diagnose liver disease, healthcare providers may use a combination of the following: ✔️ Blood Tests – Liver function tests (LFT) to check enzyme levels and overall liver health. ✔️ Imaging Tests – Ultrasound, CT scan, or MRI to detect abnormalities. ✔️ Liver Biopsy – A sample of liver tissue is examined under a microscope. ✔️ FibroScan – A specialized ultrasound that measures liver stiffness (indicating fibrosis).
Treatment Options for Liver Diseases
The treatment for liver disease depends on the type, severity, and underlying cause.
1. Medications
Antiviral medications for hepatitis B and C.
Immunosuppressive drugs for autoimmune liver diseases.
Chelation therapy for Wilson’s disease and hemochromatosis.
2. Lifestyle Modifications
Maintaining a healthy diet (low in fat and sugar).
Limiting alcohol consumption.
Regular exercise to reduce obesity and improve liver health.
3. Surgical and Interventional Treatments
Liver Transplant: For end-stage liver disease or liver cancer.
Tumor Removal: For localized liver cancer.
TIPS (Transjugular Intrahepatic Portosystemic Shunt): A procedure to treat portal hypertension.
Prevention of Liver Diseases
✅ Vaccination – Vaccines are available for Hepatitis A and B. ✅ Healthy Diet – A balanced diet rich in fruits, vegetables, lean proteins, and whole grains. ✅ Moderate Alcohol Consumption – Limit alcohol intake to reduce liver damage. ✅ Regular Health Checkups – Early detection through routine liver function tests. ✅ Avoid Sharing Needles – Reduces the risk of hepatitis B and C infection.
Latest Advancements in Liver Disease Management
The 16th World Digestive and Liver Diseases Conference highlights recent breakthroughs, including: 🔬 Gene Therapy – Promising research in treating genetic liver diseases. 🦠 New Antiviral Drugs – Improved treatment options for chronic hepatitis. 💉 Non-Invasive Diagnostic Tools – Enhanced imaging techniques for early diagnosis. 🌿 Regenerative Medicine – Research into stem cell therapy for liver regeneration.
Conclusion
Liver diseases are complex but manageable with early detection and proper treatment. The 16th World Digestive and Liver Diseases Conference provides an opportunity for global experts to collaborate and advance research in this critical field. By understanding the causes, symptoms, and treatment options, patients and healthcare providers can work together to improve liver health and prevent complications.
Conference Name: 16th World Digestive and Liver Diseases Conference Short Name: 16DLDUCG2025 Dates: December 17-19, 2025 Venue: Dubai, UAE Email: [email protected] Visit: https://digestive-liverdiseases.utilitarianconferences.com/ Visit CME/CPD: https://digestive-liverdiseases.utilitarianconferences.com/accreditation-registration Call for Papers: https://digestive-liverdiseases.utilitarianconferences.com/exhibitor-registration Register here: https://digestive-liverdiseases.utilitarianconferences.com/registration Exhibitor: https://digestive-liverdiseases.utilitarianconferences.com/exhibitor-registration Sponsor: https://digestive-liverdiseases.utilitarianconferences.com/sponsor-registration WhatsApp Us: +447723493307
#digestivehealth#guthealth#cirrhosis#fattyliver#gastroenterology#digestive#liverhealth#liverdisease#liverawareness#livercare
0 notes
Text
The Gallbladder and Biliary Tree: Functions, Disorders, and Treatments

The gallbladder and biliary tree play a crucial role in the digestive system, particularly in the digestion and absorption of fats. This blog provides an in-depth look at their anatomy, functions, common disorders, diagnostic methods, and treatments.
Anatomy of the Gallbladder and Biliary Tree
Gallbladder The gallbladder is a small, pear-shaped organ located beneath the liver on the right side of the abdomen. It serves as a storage reservoir for bile, a digestive fluid produced by the liver. The gallbladder measures approximately 7–10 cm in length and can hold about 30–50 ml of bile.
Biliary Tree The biliary tree is a network of ducts that transport bile from the liver to the small intestine. It includes:
Intrahepatic bile ducts – Small ducts within the liver that collect bile from liver cells.
Hepatic ducts – Right and left hepatic ducts merge to form the common hepatic duct.
Cystic duct – Connects the gallbladder to the common hepatic duct, allowing bile storage and release.
Common bile duct (CBD) – Formed by the union of the hepatic duct and cystic duct; it carries bile to the duodenum.
Pancreatic duct – Merges with the CBD at the ampulla of Vater before entering the duodenum.
Functions of the Gallbladder and Biliary Tree
Bile Storage and Concentration – The gallbladder stores and concentrates bile, releasing it when needed for digestion.
Fat Digestion – Bile emulsifies fats, making them easier for pancreatic enzymes to break down.
Excretion of Waste – Bile helps remove bilirubin (a byproduct of red blood cell breakdown) and cholesterol from the body.
Common Disorders of the Gallbladder and Biliary Tree
Gallstones (Cholelithiasis) Gallstones are solid deposits of cholesterol or bilirubin that form in the gallbladder. They may cause symptoms such as abdominal pain, nausea, and vomiting.
Cholecystitis This is inflammation of the gallbladder, often due to gallstones blocking bile flow. Symptoms include severe pain, fever, and jaundice.
Choledocholithiasis This condition occurs when gallstones pass into the common bile duct, leading to bile flow obstruction and possible infection.
Biliary Atresia A congenital disorder where bile ducts are absent or malformed, leading to bile buildup in the liver.
Primary Sclerosing Cholangitis (PSC) A chronic condition causing inflammation and scarring of bile ducts, which can lead to liver failure.
Diagnosis of Gallbladder and Biliary Disorders
Ultrasound – First-line imaging for detecting gallstones and inflammation.
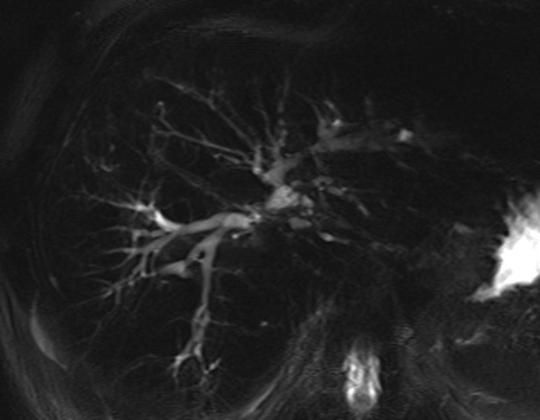
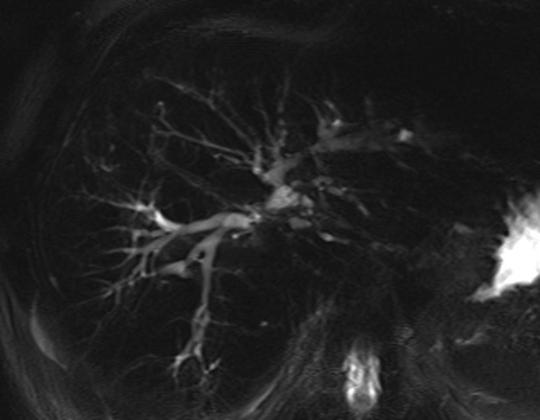
MRCP (Magnetic Resonance Cholangiopancreatography) – Provides detailed images of the biliary tree.
ERCP (Endoscopic Retrograde Cholangiopancreatography) – Used for both diagnosis and treatment of bile duct obstructions.
HIDA Scan – Evaluates gallbladder function and bile flow.
Blood Tests – Check liver function and inflammation markers.
Treatment Options
Medications
Bile acid medications (e.g., ursodeoxycholic acid) may dissolve cholesterol-based gallstones.
Antibiotics for infections like cholecystitis.
Surgical Treatments
Cholecystectomy – Surgical removal of the gallbladder, often performed laparoscopically.
Biliary Drainage – Used to relieve bile duct obstructions.
Non-Surgical Procedures
ERCP – Can remove stones and place stents to clear obstructions.
Lithotripsy – Uses shock waves to break up gallstones.
CONTACT INFORMATION:- Name:- Dr.Sachin Arora (MBBS, M.Ch Surgical Gastroenterologist) Specialist in Laparoscopic GI, HPB, and Gastrointestinal Cancer Surgery 🌐 Website: www.drsachinarora.in 📞 Contact Now: +91-7505209117 📍 Location : Sanjay Medicos, Sector 2, Maharani Bagh Ln, Ballupur Chowk, Ashirwad Enclave, Mohit Nagar, Dehradun, Uttarakhand 248001
Conclusion
The gallbladder and biliary tree are essential for digestion, but they are also susceptible to various disorders. Prompt diagnosis and appropriate treatment are crucial for managing conditions affecting these structures. If you experience persistent digestive symptoms, consult a healthcare provider for proper evaluation and treatment.
0 notes
Text
Understanding Liver Cirrhosis: Causes and Prevention
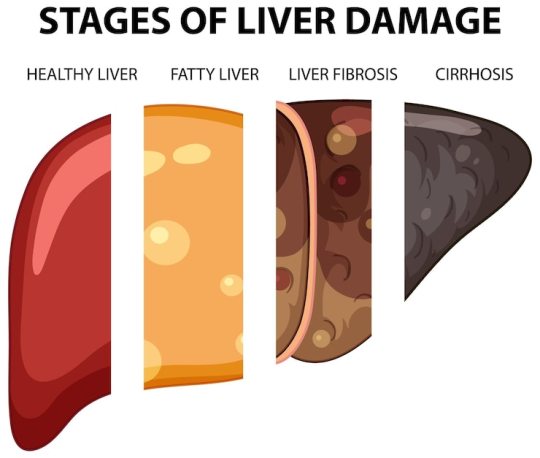
Liver cirrhosis is a chronic and potentially life-threatening condition characterized by scarring of the liver tissue. This scarring disrupts the liver's ability to function properly, leading to severe health complications. Understanding the causes of liver cirrhosis is essential for prevention and early intervention.
What is Liver Cirrhosis?
The liver is a vital organ responsible for numerous critical functions, including detoxifying the blood, producing bile for digestion, and storing essential nutrients. In cirrhosis, healthy liver tissue is gradually replaced by scar tissue, which impairs these functions. Over time, the damage becomes irreversible if left untreated.
Key Causes of Liver Cirrhosis
1. Chronic Alcohol Consumption
Excessive alcohol consumption is one of the most common causes of liver cirrhosis. Alcohol abuse leads to inflammation and fat accumulation in liver cells, eventually resulting in permanent scarring. Long-term, heavy drinking significantly increases the risk of cirrhosis.
2. Hepatitis B and C Infections
Chronic viral hepatitis B and C infections are leading contributors to cirrhosis worldwide. These infections cause ongoing inflammation in the liver, which over time damages liver cells and forms scar tissue. Early detection and treatment of these infections can help reduce the risk.
3. Non-Alcoholic Fatty Liver Disease (NAFLD)
NAFLD is characterized by fat buildup in the liver in people who consume little or no alcohol. It is often linked to obesity, type 2 diabetes, and metabolic syndrome. Without proper management, NAFLD can progress to cirrhosis.
4. Autoimmune Liver Diseases
Autoimmune conditions, such as autoimmune hepatitis, occur when the immune system mistakenly attacks healthy liver cells, leading to inflammation and scarring.
5. Bile Duct Disorders
Conditions like primary biliary cholangitis and primary sclerosing cholangitis involve damage to the bile ducts, which impairs bile flow and causes liver damage. Prolonged obstruction can result in cirrhosis.
6. Genetic Disorders
Certain inherited diseases, such as Wilson's disease (copper accumulation) and hemochromatosis (iron overload), can damage the liver over time, increasing the risk of cirrhosis.
7. Prolonged Exposure to Toxins and Medications
Chronic exposure to environmental toxins, certain medications, or industrial chemicals can harm the liver, potentially leading to cirrhosis. Overuse of over-the-counter drugs like acetaminophen is also a known risk factor.
Symptoms of Liver Cirrhosis
Early-stage liver cirrhosis often presents no symptoms. However, as the condition progresses, common signs include fatigue, jaundice (yellowing of the skin and eyes), swelling in the legs and abdomen, and easy bruising.
Prevention and Management
Preventing liver cirrhosis involves addressing its underlying causes. Here are key steps:
Limit Alcohol Intake: Moderation or complete abstinence is crucial for maintaining liver health.
Vaccination: Vaccines for hepatitis B can prevent infection, while antiviral treatments can help manage hepatitis C.
Healthy Lifestyle: A balanced diet, regular exercise, and weight management can reduce the risk of NAFLD.
Medication Safety: Avoid overusing medications and consult healthcare providers for guidance.
Regular Check-Ups: Routine liver function tests can help detect early signs of damage.
Conclusion
Liver cirrhosis is a preventable and manageable condition if its causes are identified and addressed early. By adopting a healthy lifestyle, limiting alcohol consumption, and seeking timely medical care, individuals can significantly reduce their risk of developing this serious condition.
0 notes
Link
0 notes
Text
Liver Transplant in India
The Liver is one of the five Vital Organs in the human body. The Liver performs many important functions for the proper functioning of the Human Body. Any changes or abnormalities in liver tissues can affect the quality of life and may need medical treatments. Certain Medical Conditions like Cirrhosis of the Liver, primary Liver cancer, or an ill-functioning Liver may require a Liver Transplant to save the life of the patient.
What is a Liver Transplant Surgery?
A liver Transplant is a life-saving Surgery performed by a specially trained gastroenterology surgeon to replace the damaged or faulty liver in a patient with a healthy liver either from a deceased donor liver or the portion of the Liver obtained from a living liver donor. Liver Transplant Surgery is a complicated surgery and requires great expertise from gastroenterology surgeons and a proper hospital setup.
Why a Liver transplant is needed?
A liver transplant is needed when the liver tissues are damaged and the Liver is unable to perform its functions. An end-stage liver disease patient requires a Liver Transplant for survival. A liver Transplant is also indicated for the treatment of primary Liver Cancer when the cancer is localized and the tumor size is smaller. Following medical conditions may make a Gastroenterologist or Hepatologist recommend a Liver Transplant for a patient:
Liver Cirrhosis
Alcohol-induced liver damage due to chronic alcoholism
Non-alcoholic fatty liver disease
Hemochromatosis
Wilson's disease
Primary biliary Cholangitis (PBC)
Primary sclerosing cholangitis (PSC)
Biliary atresia (generally for pediatric liver patients)
Autoimmune hepatitis
Acute Liver failure
Primary Liver cancer
Types of Liver Transplants
Liver Transplants are done either with a deceased liver donor or a healthy liver donor.
Deceased Donor Liver Transplant
Orthotopic liver transplant is replacing the damaged liver in an end-stage liver disease patient with a healthy liver procured from a deceased donor.
Split liver transplants are also orthotopic liver transplants where the deceased donor's liver is split into two and transplanted into two end-stage liver disease patients. In Split liver transplant surgery, the left lateral cadaveric liver is transplanted into a child, and the right extended liver is transplanted into an adult patient.
Living Donor Liver Transplants
Living donor liver transplants are done by taking a portion of the liver from an HLA matching Liver Donor. The Donor reverts to the full functionality of the Liver within 6 weeks of liver donation and lives a perfectly normal life.
CMCS Health is a leading medical tourism company in India. We offer medical tourism services such as finding the right doctor, the right hospital, and cost estimation for medical treatment in India for foreign patients. Some of the main countries are Bangladesh, South Africa, Egypt, Kenya, Saudi Arabia, Ethiopia, Nigeria, Uganda, Zambia, Sudan, Dubai, Namibia, Iraq, and so on. We provide free medical assistance aplastic anemia treatment cost, stomach cancer treatment, sickle cell treatment cost, the best hospital for heart valve replacement, heart valve surgery, arthroscopic surgery, bone marrow transplant cost, best liver transplant hospital, brain tumor surgery cost, cosmetic andplastic surgery, heart surgery, kidney transplant cost, spine tumor surgery,cancer treatment cost, lung transplant,liver transplant cost, top knee replacement surgeons, knee replacement surgery cost, top shoulder replacement surgeons, hip replacement surgery cost, best bone marrow hospital, etc. If you are searching for free medical and healthcare consulting to find the best hospitals and top doctors and surgeons in India for any treatment then contact us- Cmcshealth.com.
Source: https://cmcshealth1.blogspot.com/2024/11/liver-transplant-in-india.html
0 notes
Text
Primary Sclerosing Cholangitis Market Size, Share and Future News by 2025-2033
The Reports and Insights, a leading market research company, has recently releases report titled “Primary Sclerosing Cholangitis Market: Global Industry Trends, Share, Size, Growth, Opportunity and Forecast 2025-2033.” The study provides a detailed analysis of the industry, including the global Primary Sclerosing Cholangitis Market share, size, trends, and growth forecasts. The report also includes competitor and regional analysis and highlights the latest advancements in the market.
Report Highlights:
How big is the Primary Sclerosing Cholangitis Market?
The global primary sclerosing cholangitis market was valued at US$ 174.9 Million in 2024 and is expected to register a CAGR of 7.8% over the forecast period and reach US$ 370.8 Million in 2033.
What are Primary Sclerosing Cholangitis?
Primary sclerosing cholangitis (PSC) is a chronic liver condition characterized by ongoing inflammation and scarring of the bile ducts, leading to their narrowing, obstruction, and subsequent liver damage. Symptoms may include jaundice, itching, abdominal pain, and fatigue. PSC is often linked to an increased risk of liver cirrhosis and liver cancer. While the precise cause remains unclear, the disease is thought to involve autoimmune mechanisms and is frequently associated with inflammatory bowel diseases like ulcerative colitis. Treatment aims to alleviate symptoms, slow disease progression, and manage complications, with liver transplantation being a potential option for advanced stages.
Request for a sample copy with detail analysis: https://www.reportsandinsights.com/sample-request/2389
What are the growth prospects and trends in the Primary Sclerosing Cholangitis industry?
The primary sclerosing cholangitis (PSC) market growth is driven by various factors and trends. The market for primary sclerosing cholangitis (PSC) is expanding due to heightened awareness of the disease, improvements in diagnostic methods, and advancements in treatment options. Increasing recognition of PSC, particularly its links to inflammatory bowel diseases, along with the growing incidence of liver complications, is boosting demand for effective therapies. Key players in the market include pharmaceutical and biotechnology companies focusing on new drug developments and clinical trials. The market is also driven by the need for improved symptom management and potential curative approaches, such as liver transplantation. Despite challenges like high treatment costs and limited available therapies, ongoing research and innovation are contributing to the market's growth. Hence, all these factors contribute to primary sclerosing cholangitis (PSC) market growth.
What is included in market segmentation?
The report has segmented the market into the following categories:
By Type
Classic PSC
Variant PSC
PSC Associated with Autoimmune Hepatitis
PSC with Cholangiocarcinoma
By Treatment Type
Ursodeoxycholic Acid
Obeticholic Acid
Methotrexate
Corticosteroids
Others
By Route of Administration
Oral
Parental
Others
By End-User
Hospital Pharmacies
Retail Pharmacies
Online Pharmacies
North America
United States
Canada
Europe
Germany
United Kingdom
France
Italy
Spain
Russia
Poland
Benelux
Nordic
Rest of Europe
Asia Pacific
China
Japan
India
South Korea
ASEAN
Australia & New Zealand
Rest of Asia Pacific
Latin America
Brazil
Mexico
Argentina
Middle East & Africa
Saudi Arabia
South Africa
United Arab Emirates
Israel
Rest of MEA
Who are the key players operating in the industry?
The report covers the major market players including:
Acorda Therapeutics, Inc.
Gilead Sciences, Inc.
NGM Biopharmaceuticals, Inc.
Intercept Pharmaceuticals, Inc.
Falk Pharma GmbH
Allergan Plc.
Shire Plc.
Durect Corporation
Conatus Pharmaceuticals, Inc.
Sirnaomics, Inc.
Shenzhen HighTide Biopharmaceutical Ltd.
Cymabay Therapeutics
Pliant Therapeutics
Immunic AG
View Full Report: https://www.reportsandinsights.com/report/Primary Sclerosing Cholangitis-market
If you require any specific information that is not covered currently within the scope of the report, we will provide the same as a part of the customization.
About Us:
Reports and Insights consistently mееt international benchmarks in the market research industry and maintain a kееn focus on providing only the highest quality of reports and analysis outlooks across markets, industries, domains, sectors, and verticals. We have bееn catering to varying market nееds and do not compromise on quality and research efforts in our objective to deliver only the very best to our clients globally.
Our offerings include comprehensive market intelligence in the form of research reports, production cost reports, feasibility studies, and consulting services. Our team, which includes experienced researchers and analysts from various industries, is dedicated to providing high-quality data and insights to our clientele, ranging from small and medium businesses to Fortune 1000 corporations.
Contact Us:
Reports and Insights Business Research Pvt. Ltd. 1820 Avenue M, Brooklyn, NY, 11230, United States Contact No: +1-(347)-748-1518 Email: [email protected] Website: https://www.reportsandinsights.com/ Follow us on LinkedIn: https://www.linkedin.com/company/report-and-insights/ Follow us on twitter: https://twitter.com/ReportsandInsi1
#Primary Sclerosing Cholangitis Market share#Primary Sclerosing Cholangitis Market size#Primary Sclerosing Cholangitis Market trends
0 notes
Text
Best Hepatologist in chennai
Dr. Magnus Jayaraj Mansard is a highly esteemed hepatologist and HPB (hepato-pancreato-biliary) surgeon in Chennai, widely recognized for his exceptional contributions to the field of hepatology. With more than a decade of dedicated practice, Dr. Mansard has established himself as one of the leading specialists in diagnosing and treating complex liver, pancreas, and biliary tract disorders. Best Hepatologist in Chennai His expertise spans various domains, including advanced laparoscopic surgeries, liver transplantations, and cutting-edge research in liver diseases.

Educational Background and Professional Achievements
Dr. Mansard's academic journey reflects his unwavering commitment to excellence. He pursued his medical degree and further specialized in HPB surgery and hepatology, gaining extensive training from some of the world's most prestigious medical institutions. His credentials include a robust portfolio of clinical and research accomplishments, positioning him as a thought leader in the domain of liver health.
In his professional career, Dr. Mansard has played a pivotal role in establishing and strengthening liver transplant and surgical hepatology units, particularly in tier-2 cities. His efforts have made advanced liver care accessible to patients from various socio-economic backgrounds, reducing the need for them to travel to metropolitan areas for specialized treatment.
Specialization and Areas of Expertise
Dr. Magnus Jayaraj Mansard specializes in a wide range of hepatology and HPB surgical procedures, including:
Liver Transplantation: As a leading expert in liver transplantation, Dr. Mansard has performed numerous successful transplants, including complex cases involving living donors. His role extends from pre-transplant evaluation to post-transplant care, ensuring comprehensive management of patients throughout their journey.
Advanced Laparoscopic Surgery: Dr. Mansard is a pioneer in minimally invasive techniques, utilizing laparoscopy for liver, pancreas, and biliary surgeries. These advanced procedures reduce recovery times, minimize complications, and improve patient outcomes.
Liver Cancer Treatment: He is adept at managing various liver cancers, including hepatocellular carcinoma (HCC) and metastatic liver cancers. Treatment approaches include surgical resections, transarterial chemoembolization (TACE), and radiofrequency ablation (RFA), tailored to the individual needs of the patient.
Hepatobiliary Diseases: His expertise extends to managing bile duct obstructions, gallbladder diseases, and pancreatitis, using a combination of surgical and non-surgical methods.
Autoimmune and Genetic Liver Disorders: Dr. Mansard has significant experience in diagnosing and treating complex autoimmune liver diseases, such as autoimmune hepatitis, primary biliary cholangitis (PBC), and primary sclerosing cholangitis (PSC). He also addresses genetic liver disorders, providing personalized treatment plans based on genetic testing and family history.
Diagnostic Excellence
One of Dr. Mansard’s hallmarks is his meticulous approach to diagnosis. He employs a variety of diagnostic tools to ensure precise identification of liver-related conditions, including:
Blood Tests: Comprehensive liver function tests (LFTs) to detect abnormalities in enzymes, bilirubin, and proteins.
Imaging Studies: High-resolution ultrasounds, CT scans, and MRIs provide detailed visualization of the liver, bile ducts, and pancreas.
Liver Biopsy: A critical diagnostic tool for evaluating the extent of liver damage and identifying conditions such as fibrosis or cirrhosis.
FibroScan: This non-invasive technology measures liver stiffness to assess fibrosis and monitor chronic liver disease progression.
Endoscopic Procedures: ERCP and endoscopic ultrasound (EUS) are employed to investigate and treat bile duct and pancreatic abnormalities.
Collaborative Approach to Patient Care
Dr. Mansard adopts a multidisciplinary approach to liver care, working closely with other healthcare professionals, including gastroenterologists, hepatobiliary surgeons, radiologists, pathologists, and nutritionists. This collaborative effort ensures comprehensive care for patients, addressing all facets of their liver health. His team-based approach is particularly crucial for patients undergoing complex procedures like liver transplantation, where coordinated care is essential for successful outcomes.
Personalized Treatment Plans
Understanding that each patient’s condition is unique, Dr. Mansard develops personalized treatment plans that consider individual medical histories, disease severity, and patient preferences. His holistic approach involves:
Medications: Prescribing antivirals for hepatitis, immunosuppressants for autoimmune conditions, and other targeted therapies.
Lifestyle Modifications: Offering guidance on diet, exercise, and alcohol consumption to manage and prevent liver diseases.
Surgical Interventions: Employing minimally invasive or open surgical techniques as required by the patient’s condition.
Supportive Care: Addressing symptoms such as fatigue, itching, or nutritional deficiencies to improve overall quality of life.
Patient-Centric Philosophy
Dr. Mansard’s patient-centric philosophy emphasizes compassionate care and clear communication. He takes the time to educate patients about their conditions, treatment options, and expected outcomes, empowering them to make informed decisions about their health. His dedication to building trust and fostering a positive doctor-patient relationship has earned him widespread respect and gratitude from his patients.
Contributions to Medical Research and Education
Beyond clinical practice, Dr. Mansard is actively involved in medical research, contributing to advancements in hepatology and HPB surgery. He has published numerous research articles in peer-reviewed journals, focusing on innovative treatment modalities and improving surgical outcomes. His work has been instrumental in shaping best practices and setting new benchmarks in liver care.
Dr. Mansard is also a passionate educator and mentor, training the next generation of hepatologists and surgeons. He regularly conducts workshops, seminars, and lectures, sharing his knowledge and expertise with medical professionals across the country.
Recognition and Awards
Dr. Magnus Jayaraj Mansard’s contributions to hepatology and HPB surgery have earned him numerous accolades. His reputation as a leading hepatologist in Chennai is bolstered by glowing testimonials from patients and peers alike. He is frequently invited to speak at national and international conferences, further establishing his prominence in the field.
Why Choose Dr. Magnus Jayaraj Mansard?
Choosing Dr. Mansard as your hepatologist ensures access to top-tier medical care backed by years of experience and a proven track record. Patients benefit from his:
Comprehensive Expertise: Proficient in managing a broad spectrum of liver diseases and performing advanced surgical procedures.
Innovative Techniques: Use of state-of-the-art technology and minimally invasive methods for diagnosis and treatment.
Patient-Centered Approach: Commitment to personalized care, ensuring the best possible outcomes for every patient.
Collaborative Care: Seamless coordination with a multidisciplinary team for holistic management of complex liver conditions.
Conclusion
Dr. Magnus Jayaraj Mansard stands out as one of the best hepatologists in Chennai, offering unparalleled expertise in liver care. His dedication to advancing the field of hepatology and improving patient outcomes makes him a trusted choice for individuals seeking specialized care for liver diseases. With his extensive experience, innovative approach, and compassionate care, Dr. Mansard continues to transform the lives of his patients, ensuring they receive the best possible treatment and support. For more details visit https://drmagnusjayaraj.com/gastrointestinal-cancer-treatment-in-chennai/
0 notes
Text
Navigating Liver Transplantation: A Guide for Patients and Caregivers

Liver transplantation is a critical procedure that can significantly improve the prognosis and quality of life for individuals with advanced liver disease. This intricate surgery involves replacing a diseased liver with a healthy one, obtained either from a deceased donor (cadaveric transplant) or a living donor (living donor transplant).
Understanding Liver Disease
The liver, responsible for vital functions such as detoxification, protein synthesis, and blood sugar regulation, can be affected by various diseases that impair its functionality. Common conditions necessitating a liver transplant include viral infections (hepatitis B and C), non-alcoholic fatty liver disease (NAFLD), alcoholic liver disease, autoimmune hepatitis, primary biliary cholangitis, sclerosing cholangitis, and genetic liver disorders.
When is a Liver Transplant Necessary?
A liver transplant becomes necessary when the liver's function is severely compromised, and other treatments have proven ineffective. Symptoms indicating the need for a transplant include ascites (abdominal fluid buildup), variceal bleeding, hepatic encephalopathy (confusion or mental fog), severe fatigue, jaundice (yellowing of the skin and eyes), frequent infections, and malnutrition.
The Evaluation Process
Before being considered for a transplant, patients undergo a thorough evaluation to assess their suitability for the procedure and to optimize the chances of a successful outcome. This evaluation includes a detailed review of medical history, liver function tests, compatibility assessments, imaging studies (such as CT scans or ultrasounds), psychological evaluation, and evaluation of the social support system.
Living Donor vs. Cadaveric Donor Transplants
Liver transplants can involve a living donor, where a portion of a healthy liver is transplanted, or a cadaveric donor, where a liver from a deceased donor is used. Living donor transplants typically offer shorter waiting times and better initial graft function but involve risks for the donor. Cadaveric transplants may require longer waiting periods depending on organ availability.
The Importance of Support
A robust support network is crucial throughout the transplant journey. Family, friends, and support groups provide invaluable assistance with daily activities, emotional support, and shared experiences, which are essential for emotional well-being and recovery.
Preparing for Surgery
Once listed for a transplant, patients receive comprehensive instructions for pre-operative preparations. These preparations include dietary adjustments, medication management, lifestyle modifications (such as cessation of smoking and alcohol consumption), and logistical arrangements for hospitalization and paperwork completion.
The Surgical Process
Liver transplant surgery is a complex procedure that can extend over several hours. During the operation, the diseased liver is carefully removed and replaced with the healthy donor liver. The new liver typically begins functioning immediately, restoring critical liver functions.
Recovery From Liver Transplant
Recovery after a liver transplant is a gradual process that may span months to years. Patients often require an initial hospital stay for close monitoring and adjustment of medications. Post-transplant care involves the use of immunosuppressive medications to prevent rejection, physical therapy to regain strength and mobility, nutritional counseling to support healing and dietary needs, and regular follow-up appointments with the transplant team to monitor progress and manage any complications.
Life After Liver Transplant
While a liver transplant offers a new lease on life, maintaining health post-transplant requires lifelong commitment. Patients must adhere strictly to prescribed medications, make necessary lifestyle adjustments (including diet and exercise), attend regular medical check-ups, and remain vigilant for signs of complications.
Conclusion
Navigating liver transplantation is a challenging journey, but with proper information and support, patients and caregivers can effectively manage each stage of this complex process.
0 notes
Text
When To See a Gastroenterologist in Westchester County and Yonkers
Experiencing stomach problems and digestive difficulties may prompt one to consult a general physician initially. Sure, the medical professional will take time to examine the patient carefully and ask many questions to identify the source of discomfort. The problem may be minor, such as acid reflux or bloating. Feeling nauseous is a common complaint among patients diagnosed with gastrointestinal problems. The general doctor may think that the patient needs more specialized care and refer the patient to an experienced hepatologist in Westchester County and Yonkers. Inquiring or checking the facts about such a specialty and the specialist is essential. It suffices to know that a hepatologist is often called a liver doctor who treats diseases related to the liver and the biliary system. A sub-specialty of gastroenterology, the concerned doctor must undergo specialized and extensive training. The American Board of Internal Medicine awards a certificate to successful professionals.
Role of a hepatologist This specialty doctor is equipped to diagnose and treat all liver diseases and gallbladder problems. Additionally, pancreatic disorders may be treated by them too. The most common treatments done by such a specialist include the following:-
· Hepatitis · Hepatic encephalopathy · Nonalcoholic fatty liver disease · Nonalcoholic steatohepatitis · Cirrhosis of the liver · Other types of liver damage · Liver cancer · Fatty liver disease · Metabolic liver diseases
Moreover, the specialist is also trained to treat other complaints of the biliary system, i.e., the gall bladder, bile duct, and the liver. The patient can thus expect the best possible treatment from the hepatologist for the following conditions:-
· Primary biliary cholangitis · Primary sclerosing cholangitis · Removal of gallstones · Gallbladder cancer · Pancreatitis · Pancreatic cancer · Gallbladder inflammation · Bile duct stones · Noncancerous tumors of the gallbladder, liver, or bile duct · Bile duct cancer Some of the other responsibilities handled by the hepatologist include:- · Performing diagnostic tests · Explaining the treatment options to the patient's family · Providing treatment as required · Monitoring patients scheduled for liver surgery or liver transplant · Refer the patient to other specialists for further assessment and treatment · Working together with other medical experts to ensure the best care
Reasons to consult a hepatologist A layperson is not aware of this specialty. The primary care doctor may refer the patient to a liver specialist when any of the following problems are noticed:
· Abnormal liver function test results · Gastrointestinal bleeding · Jaundice · Ascites · Enzyme problems · Drug overdose
Where is a hepatologist found? The hepatologist may examine patients in clinics, hospitals, and other healthcare facilities. Other specialist doctors often consult them about other patients diagnosed with liver problems, too. Patients seeking a quality hepatologist may also inquire at high-dependency units, intensive care units, or liver specialist centers.
An individual who experiences several stomach and digestive issues will surely obtain the proper treatment from a reputed gastroenterologist in Westchester County and Yonkers.
#gastroenterologist in Westchester County and Yonkers#hepatologist in Westchester County and Yonkers
0 notes