#Exercise with an ostomy
Explore tagged Tumblr posts
Note
I was wondering: I noticed that in art I almost always see limb stumps that are, for the lack of a better word, thick and with a rounded end. But observing amputees around me, what I noticed is that their stumps are more tapered, they also are often uneven instead of perfectly round, and the rest of the limb is often thinner as a result of less muscle mass.
Is this coincidental, or do you think stumps are represented in a way that is assumed to be more aesthetically pleasing to abled folk? How common is the "perfect round muscular stump" thing, if at all??
Hello!
As an artist that seeks out art of disabled characters, it's 100% trying to make the character look "less disabled and more pretty". It's usually not a conscious decision, most people just have pretty=good and disabled=ugly ingrained into them and don't think about it ever. Positive depictions of disabled people will do everything to portray them as conventionally attractive as possible, and there is no disability that is exempt from this.
This applies to everything. Most art showing disabled people will try to keep the disability to the absolute minimum - it's not coincidence that positive disabled characters have to be white, thin, young, if they use a prosthetic it has to be really cool and/or unrealistic, if they use a wheelchair it has to be a manual that has to be really cool and/or unrealistic, and they have to look as abled as possible; an abled model who just happened to be holding a cane is preferable since gait disorders are ugly. Good luck trying to find a drawing of a character using an ostomy bag, with congenital skeletal conditions, with severe spasticity, in one of these big powerchairs, I won't mention facial differences and how non-existent realistic representation of them is. Hell, it can be hard to find art of blind characters who aren't wearing blindfolds and eyepatches (since disabled body part ugly), let alone using an aid like a cane or a brailler (since that's Disability, and not just a quirky character trait).
With stumps, it's the same thing. Most often you don't see them, since they are Clearly Disabled. Usually they're behind a cool prosthetic that's called something else (cyborg bionic automail whatever...) that sounds less disabled. If they aren't, they're probably bandaged, since they are Surely Scary. If they aren't that, they will be perfectly round, scarless (or with that big "starburst" type scar for some reason), symmetrical to other limb, and essentially look like you just erased the rest of a model's leg or arm.
Again, I don't think this is done on purpose, I think artists just don't think enough about how they choose to portray minorities. No one is researching anything, everything is a game of telephone from how someone else draws it, who cares that that person didn't bother to check anything either.
[Disclaimer that we don't have amputee mods]
How common is the "perfect round muscular stump" thing?
Not very common, but someone with a disarticulation (much more rare than through-bone) will have their muscles still attached to something and thus may not have the kind of tissue atrophy like someone with an above the knee amputation will. Even weightlifters with an above/below amputation will have some degree of atrophy (you can look at guys like Max Okun, etc.) so it's not like you can just "exercise it out".
A residual limb can be fairly round, but it mostly depends on where it actually is. A lot of people will have excess skin from skin flaps + tissue atrophy which gives it a different shape, BE amputees can have the actual bone shapes visible on the stump, etc. And of course there is scar tissue (unless it's congenital) which can affect how the limb looks like beyond just the sew line being visible; it can leave the stump with an indent around it, etc.
But all of that is of course Disability and Different, so it gets omitted in art. It'd be cool if this wasn't the case, but what can you do.
mod Sasza
258 notes
·
View notes
Text
Recovery and exercise
Once upon a time, I could bike 7 miles per day, walk like nobody's business. I hiked. I loved it. Yes, I was heavy and carrying an autoimmune disorder diagnosis, but able to do things outdoors that I enjoyed. At home, I had resistance bands and dumbbells. I used a foldaway rowing machine. I was marshmallow-coated steel.
Cancer, as it does, changed all that.
Two years later, exercising at all has been difficult. My neighborhood is no longer safe to walk.
I need to exercise, so I started looking for alternatives.
Local gyms are less than welcoming to silver-haired Gen-X ladies, and even with 'no commitment' contracts, it is important to note that some come with built-in 'account management' and termination fees. You may not be able to use all of the gym's amenities unless you have a higher tier two to three year contract or are willing to pay 'use fees' for access. They may even limit the hours you can use the gym, blocking out 'prime time' hours and even weekends.
Fuck that.
My limitations include a right shoulder with surgical scars, titanium rods, plates, and screws. I have extensive surgical scars on my torso and adhesions under the large ileostomy scar. My treatment with platinum drugs left me with chemo induced neuropathy. Radiation damaged my lower spine and has impaired my thyroid. Galdolinium interacting with oxalic acid may have caused some soft tissue damage. I have overdone exercise to the point where the ostomy scar was in so much pain that I thought I was passing a gallstone.
Weights and bands are limited to the very lightest ones. My old pedal machine has been repurposed to arms. Wall Pilates and chair yoga help. But it has not been enough.
I calculated the minimum I would incur in gym fees just to use a treadmill and take some classes.
So, I bought this on sale. It came out to $400 after promotion, with free shipping. A big investment, but not as much as a gym membership + the time and money spent going back and forth.

First, it's 60lbs. Your Fedex/UPS driver will hate you if you have stairs. Once you get it out of the box, it's good to go in five minutes. Plug it in and hop on. The lowest speed is .50 MPH going up in .25 MPH increments from there. It has a remote, and if you need balance help, don't buy the overpriced handrail, just get an oversized walking frame.
I can do 1000 steps in 20 minutes, starting with the .50 MPH setting, then progressing up to .75, then to 1.0 MPH before coming back down. Right now, I am at 6,000 steps per day, working my way up to 10,000. It's very comfortable to walk in bare feet, slippers, or sneakers. It can go under a standing desk. When done, it goes under my bed. If you have problems finding time to exercise, or if you have mobility issues, I recommend this.
5 notes
·
View notes
Text

The Global Ileostomy Market will grow at highest pace owing to increasing prevalence of inflammatory bowel diseases.
The ileostomy market involves surgical procedures that divert the small intestine or ileum to the abdominal wall by creating an opening called a stoma. It may involve temporary or permanent diversion of the small intestine. The procedure is generally carried out to treat severe cases of ulcerative colitis, Crohn's disease or other medical conditions. Ileostomies help manage symptoms of these conditions by diverting the flow of digested foodcontents and stool out of the body. Products such as ostomy pouches, belts and accessories are used post-surgery to collect and dispose of waste safely. The global ileostomy market is primarily driven by rising prevalence of inflammatory bowel diseases including Crohn's disease and ulcerative colitis. According to estimates, over 1.6 million Americans suffer from IBD resulting in higher number of ileostomy procedures. Additionally, favorable reimbursement and reimbursement policies along with increasing awareness regarding ostomy care are favoring market growth. The Global Ileostomy Market is estimated to be valued at US$ 1.90 Bn in 2024 and is expected to exhibit a CAGR of 7.4% over the forecast period 2024 to 2031. Key Takeaways Global Ileostomy Market Companies are Coloplast Corp, ConvaTec Inc., Hollister Incorporated, Marlen Manufacturing & Development Company, Perma-Type Company, Inc., Nu-Hope Laboratories, Inc., Perfect Choice Medical Technologies, Fortis Medical Products, Safe n' Simple, AdvaCare Pharma, Schena Ostomy Technologies, Inc., Cymed, TG Eakin Limited, Alcare Diagnostic Research Center Pvt. Ltd., Welland Medical Limited. Growing prevalence of Crohn's disease and ulcerative colitis in developed nations as well as emerging economies is fueling the demand for ileostomy products. Technological advancements include development of new ostomy pouches with advanced adhesives that help prevent leaks and offer discreet wear. Market Trends There is an increased demand for one-piece ostomy pouches owing to their ease of use and discretion. Manufacturers are focusing on development of skin friendly hydrocolloid polymers and adhesives to prevent irritation and extend wear time. Another key trend is growing preference for closed pouches that collect stool and eliminate odor without needing to be frequently emptied. This offers better comfort and discretion to patients. Market Opportunities Emerging markets in Asia Pacific and Middle East regions offer lucrative growth opportunities owing to growing aging population, rise in lifestyle diseases and improving access to healthcare infrastructures. Manufacturers can invest in development of specialized accessories, belt and protective wraps tailored for outdoor activities and physical exercises to address needs of active ostomates.
Get more insights on Global Ileostomy Market
About Author:
Ravina Pandya, Content Writer, has a strong foothold in the market research industry. She specializes in writing well-researched articles from different industries, including food and beverages, information and technology, healthcare, chemical and materials, etc. (https://www.linkedin.com/in/ravina-pandya-1a3984191)
2 notes
·
View notes
Text
I was denied SSDI due to my family (just my Dad, a 73 year-old who is retired and living on SSDI himself) having too many resources, that medical marijuana was proving beneficial to me (what job can you do while high, your honor? I wish I asked..) and it might “make me better, my nerve damage affecting “only” one limb primarily and arthritis from multiple orthopedic surgeries being localized to the bones purposefully broken by surgeons for the purpose of osteotomies and/malformed due to my birth defect. The birth defect that required 30+ surgeries from the day I was born including multiple orthopedic procedures was referred to by the judge as just “bladder issues”. My PTSD, MDD, and ASD were considered managed because I’ve never been involuntarily committed. I’m still working with DVS but being unable to do manual labor, restaurant work, or retail, all physically demanding jobs. I was only able to work as long as I did due to my first job being accommodating to my health issues. I feel utterly despondent but most of all I am afraid and don’t know where do from here.
I’m so numb I have no idea where to go from here. DVS and the job search is a constant exercise in humiliation. No wonder the highest employment rate ever logged by the DoL for those with severe disabilities is 29%… in 1979.
I worked for 6 years and those SSA work credits are now expired, naturally. I could apply for SSI as I have nothing to my name but being on Medicaid with an ostomy requiring medical supplies to not die a slow and painful death makes the prospect dire. I’ve helped and been privy to enough of my fellow BE folks needing to pool resources to get supplies because Medicaid refuses an adequate supply.
I wish just one thing wasn’t such a damn struggle.
6 notes
·
View notes
Text
Reasons For Physical Therapy in Baltimore and Arlington, MD
Being gravely ill necessitates admission to a hospital to undergo treatment for the underlying cause of pain and discomfort. Complete recovery is not always possible when hospitalized. Instead, most specialists and general doctors recommend physical therapy in Baltimore and Arlington, MD, after being discharged. This requires the assistance of a trained therapist equipped to guide and help with the condition and enable the patient to recover steadily while regaining the lost strength in the musculoskeletal system. Often referred to as PT, Physical therapy is a rehabilitation technique in which trained therapists use several pieces of equipment and formulate exercise regimens for their patients. Weakened areas of the body and abnormal physical conditions are effectively treated, allowing the patient to overcome the associated pain, restore muscle strength, and restore lost body functions. PT may be used both before and after conventional treatment and may also be a form of alternative therapy when the musculoskeletal system has been affected by illness or injury.
True, medical professionals such as doctors often recommend PT for full recovery after treatment, but the patient may also go for therapy when the following signs and symptoms become apparent:
Pain Management—Constant pain can affect one's morale and physical well-being. Thankfully, a physical therapist can help by identifying the real cause of the pain and addressing it properly. Pain management often involves following a customized exercise plan that treats the cause to alleviate the pain by restoring blood flow to the affected part of the body.
Movement- Severe injury and/or ailment can rob the muscles and bones of strength. Most patients fail to move the affected limb or body part. The therapist can advise relief and exercises to increase the range of movement by removing the related pain and joint stiffness as needed.
Recurring Injuries—A weakened musculoskeletal system invites frequent injuries. Many individuals experience sprains, strains, and other muscle injuries repeatedly. The physical therapist will address the root cause by alleviating the pain and helping the patient increase the range of movement slowly but surely, thus reducing the frequency of repeated injuries.
Recovery after Surgery—Patients who undergo surgery are often unable to return to normal life due to problems with posture, movement, and balance. Undergoing PT can help restore the fitness of such patients. Following the therapist's advice, the body's strength and flexibility return slowly. The possible complications associated with the surgery, like muscle stiffness and lack of body coordination, are also addressed effectively.
A patient recuperating at home may be able to do it effectively with the help of a medical professional adept at providing skilled nursing in Washington, D.C., and Baltimore, MD. Apart from conventional patient care, such a nurse will also provide specialized care with tube feeding, wound care, or ostomy care as needed. A trained and experienced nurse also manages central lines and ports.
0 notes
Text
9 Best Exercises You Can Do With an Ostomy Bag

9 Best Exercises You Can Do With an Ostomy Bag
0 notes
Text
Inflammatory Bowel Disease: Symptoms, & Treatment -Discuss at the 13th World Gastroenterology, IBD & Hepatology Conference 2023.

Inflammatory Bowel Disease (IBD) is a group of chronic inflammatory conditions that affect the digestive tract. The two primary types of IBD are Crohn's disease and ulcerative colitis. These conditions have similar symptoms, but they affect different parts of the digestive system and have some differences in their treatment approaches. Here's an overview of IBD, including its symptoms, types, and treatments:
Types of Inflammatory Bowel Disease:
Crohn's Disease: Crohn's disease can affect any part of the digestive tract from the mouth to the anus, but it most commonly involves the small intestine and the colon. It causes inflammation that extends deep into the intestinal wall and can lead to complications such as strictures (narrowing of the intestine), fistulas (abnormal connections between different parts of the digestive tract), and abscesses.
Ulcerative Colitis: Ulcerative colitis primarily affects the colon (large intestine) and the rectum. Unlike Crohn's disease, which can affect any part of the digestive tract, ulcerative colitis is limited to the colon's inner lining (mucosa). It causes continuous areas of inflammation and ulcers, often starting from the rectum and extending upward into the colon.
Common Symptoms of Inflammatory Bowel Disease (Crohn's Disease and Ulcerative Colitis):
Diarrhea: Frequent, loose, and bloody stools.
Abdominal Pain and Cramping: Often in the lower abdomen.
Fatigue: Due to chronic inflammation and malabsorption of nutrients.
Weight Loss: Typically from reduced appetite and malnutrition.
Fever: Occurs during flare-ups.
Rectal Bleeding: Common in ulcerative colitis.
Loss of Appetite: Reduced food intake due to discomfort.
Joint Pain: Arthritis-like symptoms in some cases.
Skin Problems: Rashes, sores, and other skin conditions.
Eye Inflammation: Redness, pain, and irritation in the eyes.
Mouth Sores: Ulcers in the mouth.
Delayed Growth (in children): Due to poor nutrient absorption.
Treatment of Inflammatory Bowel Disease:
Treatment for IBD aims to control inflammation, alleviate symptoms, and maintain remission. The choice of treatment depends on the severity of the disease, its location, and individual patient factors. Treatment options include:
Medications:
Anti-Inflammatory Drugs: Such as aminosalicylates (e.g., mesalamine), which are often used in mild to moderate cases.
Corticosteroids: For short-term relief of severe symptoms.
Immunosuppressants: Drugs like azathioprine, 6-mercaptopurine, or methotrexate to suppress the immune system's response.
Biologics: Monoclonal antibodies like infliximab and adalimumab that target specific immune system proteins.
Dietary Modifications:
Some individuals may benefit from dietary changes, such as a low-residue diet or an exclusion diet, to reduce symptoms.
In severe cases, patients may require exclusive enteral nutrition (EEN), which involves consuming a specialized liquid formula instead of solid food.
Lifestyle Modifications:
Stress management and regular exercise can help reduce symptoms and improve overall well-being.
Smoking cessation is essential, as smoking worsens Crohn's disease but may have a protective effect in some cases of ulcerative colitis.
Surgery:
In cases of severe complications or when medications are ineffective, surgery may be necessary. This can involve removing damaged sections of the intestine or creating an ostomy.
It's crucial for individuals with IBD to work closely with healthcare professionals to develop a personalized treatment plan that effectively manages their condition and improves their quality of life. Regular monitoring and follow-up visits are essential to track disease progression and adjust treatments as needed.
Connect with us:
More info: https://gastroenterology.universeconferences.com/
Email: [email protected]
WhatsApp No: +442033222718
#IBD #Exploredubai #Medical #EmiratesCongress #GHUCG2023 #hepatologyconference2023 #DigestiveDisorders #gastroforum #gastroenterologia #Hepatologist
0 notes
Text
What are the potential long-term effects of colorectal surgery?

The potential long-term effects of colorectal surgery can vary based on the type of surgery, the underlying condition being treated, your individual health, and how well you follow post-operative care instructions. Here are some common long-term considerations after colorectal surgery:
1. Changes in Bowel Habits:Depending on the extent of surgery, you might experience changes in bowel habits. These could include alterations in stool consistency, frequency, or urgency. Your digestive system may need time to adjust to any modifications made during surgery.
2. Digestive Changes: Some individuals might experience changes in digestion, absorption of nutrients, or sensitivity to certain foods after colorectal surgery. Your surgeon or a dietitian can provide guidance on managing your diet to ensure proper nutrition.
3. Bowel Control:Surgical procedures that involve the rectum or anus can impact bowel control. Temporary or permanent changes in bowel control, including gas, liquid stool, or solid stool leakage, could occur. This is especially relevant if you've had surgery for conditions like anal fistulas or rectal cancer.
4. Sexual Function:As mentioned earlier, surgeries in the pelvic region can potentially affect sexual function due to their proximity to nerves and structures involved in sexual response. Changes in sensation or function might occur.
5. Ostomy Management: If you've undergone a procedure that involves creating an ostomy (colostomy or ileostomy), you'll need to learn how to manage it, which involves caring for the stoma and using an ostomy pouch for waste collection.
6. Scar Tissue Formation: Scar tissue can form at the surgical site, which might lead to discomfort or adhesions. Adhesions are bands of scar tissue that can cause organs or tissues to stick together, potentially causing pain or bowel obstruction.
7. Recurrence of Conditions:Some conditions, such as inflammatory bowel disease or certain types of cancer, have a risk of recurrence even after surgical treatment. Regular follow-up with your medical team is important to monitor your health and catch any potential issues early.
8. Emotional and Psychological Impact:Surgery and adjustments to bodily changes can have emotional and psychological effects. Support from loved ones, counseling, and joining support groups can be helpful in coping with these aspects.
9. Functional Limitations: In certain cases, depending on the type of surgery and its impact on your body, there might be limitations in terms of physical activities, exercise, or heavy lifting.
It's essential to have open and ongoing communication with your colorectal surgeon and medical team about any concerns you have related to potential long-term effects. They can provide you with personalized information based on your specific surgery, help you manage any changes, and offer guidance on maintaining the best possible quality of life post-surgery.
For more information, Consult Dr. Chintamani Godbole one of the best Colorectal Surgeon in Mumbai.
0 notes
Text
D is for Diagnosis
Hello, I hope you are all well. Thank you for sticking with me despite my lack of consistent posts. I’m trying to keep with the alphabet theme because it’s more interesting, I think. It also gives my posts a bit more structure, rather than me just rambling.
Anyway, today I want to talk about diagnosis. Specifically, a new diagnosis.
As you should know (if you’ve been following me for a while but don’t worry if not), I have Inflammatory Bowel Disease and Primary Sclerosing Cholangitis, as well as a few other less impressive-sounding conditions. The IBD and PSC I mention specifically because there are thought to be links between them, mainly that patients with Ulcerative Colitis (the form of IBD I have) are more likely to develop PSC than those without UC. This is known as an extraintestinal manifestation which means that other conditions may develop because I have IBD.
Other extraintestinal manifestations include condition such as arthritis, skin conditions, inflammation of the eye, anaemia, problems with the kidneys, and osteoporosis. That last one is what I want to focus on today.
Just to clarify, I do not have osteoporosis. I do, however, have thinning in the base of my spine which they found recently in a bone density scan. This, I believe this is called osteopenia, but I’m not 100% sure as my GP didn’t put a name to it. Anyway, the thinning isn’t too serious, by the sounds of things, but they do want to start a form of treatment to stop it from developing into osteoporosis. My GP is consulting my GI as she doesn’t want to start anything that may aggravate my IBD. In the meantime, I am doing daily exercises that are designed for those with sciatica. This may or may not help but seeing as how I do get mild sciatic symptoms from time to time, I don’t think this will do any harm.
Speaking of exercises, I am still doing my knee exercises, as it doesn get stiff if I've not moved around for a while, and I’ve also added abdominal core exercises to my routine to strengthen my core. My goal is to do them all at least once daily so that I am as strong as I can be to return to work in two weeks. I am also trying to stick to a routine of getting up and going to bed at the same time each day (even the weekends) to regulate my sleep and get my fatigue under control.
Thank you for reading and I hope you are keeping safe and well. Until next time!
#ulcerative colitis#colitis#ibd#Inflammatory Bowel Disease#chronic illness#invisible illness#osteoporosis#osteopenia#ostomate#ostomy bag#Exercise with an ostomy#exercise#diagnosis#extraintestinal manifestation
37 notes
·
View notes
Text
Bodyboostbros.com is a Professional Fitness Platform. Here we will provide you only interesting content, which you will like very much. We’re dedicated to providing you the best of Fitness, with a focus on dependability and Fitness. We hope you enjoy our Fitness as much as we enjoy offering them to you.
In Bodyboostbros.com we discuss about:
Cardio Training & Fitness Technology, Cardio Training, Exercise Bikes, Rowers, Step Machines, Treadmills, Vibration Platform Machines, Exercise Machine Parts & Accessories, Exercise Machine Attachments, Treadmill Lubricants, Treadmill Replacement Parts, Fitness Technology, Activity & Fitness Trackers, App-Enabled Fitness Trackers, Heart Rate Monitors, Pedometers, Stopwatches, Clothing and Footwear, Clothing, Boys’ Activewear, Girls’ Activewear, Men’s Activewear, Women’s Activewear
Footwear, Men's Cross-Training Shoes, Women's Cross Training Shoes, Endurance & Energy, Candy & Mints, Chews & Gels, Herbals, Powders, Shots, Supplements, Sports Nutrition, Amino Acids, CLA, Electrolyte Replacements, Fat Burners, Healthy Snacks & Beverages, L-Carnitine, Post-Workout & Recovery, Pre-Workout, Protein, Testosterone Boosters, Weight Gainers, Weight Loss & Keto Diet Systems, Appetite Control & Suppressants, Weight Loss Supplements, 7-Keto Nutritional Supplements, Keto Diet Book, Diet Kits & Systems, Nutrition Bars & Drinks, Nutrition Bars, Ready to Drink Shakes, Exercise & Fitness Accessories, Aquatic Fitness Equipment, Battle Ropes, Exercise Gloves, Fitness Planners, Fitness Trampolines, Jump Ropes, Sauna Suits, Waist Trimmers
Pilates, Chairs, Fitness Circles, Flexbands, Floor Mats, Reformers, Spine Supporters, Straps, Balance Trainers, Balance Boards, Exercise Balls, Foam Rollers, Speed & Agility Training, Agility Ladders, Reaction Balls, Speed Hurdles, Running Clothing, Boys’ Running Clothing, Girls’ Running Clothing, Men’s Running Clothing, Women’s Running Clothing, Running GPS Units, Waist Packs.
Running Accessories, Armbands, Headlamps, Hydration Belts, Hydration Packs, Reflective Gear, Weights & Accessories, Bars, Bicep Supports, Collars, Dumbbells, Kettlebells, Medicine Balls, Plates, Thigh Weights, Weight Belts, Weight Vests, Wrist & Ankle Weights, Strength Training Equipment Attachments, Chest Expanders, Thigh & Hip Strengtheners Grip Strengtheners, Strength Training Sets, Suspension Trainer, Twist Boards, Core Slider, Dip Stands, Exercise Wheels Home Gym Systems, Inversion Equipment, Pull-Up Bars, Pushup Stands, Resistance Bands.
Weight Storage Racks & Benches, Power Cages, Dumbbell Racks, Free-Weight Racks, Plate Storage Racks, Plate Trees, Adjustable Benches, Olympic Weight Benches, Roman Chairs, Standard Weight Benches, Weight Machines, Leg Machines, Upper Body Machines, Smith Machines, Health Care, Alternative Medicine, Diabetes Care, Ear Care, Eye Health, Feminine Care, First Aid, Foot Health, Incontinence & Ostomy, More Health Care, Insect & Pest Repellents, OTC Medications & Treatments, Respiratory Aids & Accessories, Sleep & Snoring, Smoking Cessation, Women’s Health, Book Health, Fitness & Dieting.
Vitamins, Minerals & Supplements, Antioxidants, Blended Vitamin & Mineral Supplements, Chondroitin & Glucosamine Collagen, Digestive Supplements, Enzymes, Essential Fatty Acids, Glandular Extracts, More Vitamins, Minerals & Supplements, Herbal Supplements, Hyaluronic Acid, Lipid, MCT Oil, Minerals, MSM, Royal Jelly, Sleep Supplements Vitamins, Yoga Clothing, Boys’ Yoga Clothing, Girls’ Yoga Clothing, Men’s Yoga Clothing.
Yoga Equipment, Women’s Yoga Clothing, Yoga Blocks, Yoga Foam Wedges, Yoga Mat Bags, Yoga Mat Straps, Yoga Mats, Yoga Meditation Benches, More Yoga Equipment, Yoga Sandbags, Yoga Silk Eye Bags, Yoga Starter Sets, Yoga Straps, Yoga Towels.
2 notes
·
View notes
Text
I don’t have something like Crohn’s or IBD myself, but my sister-in-law is very open about her experience with an ostomy bag and I hope that sharing a little bit of her story might help someone in a similar situation feel better.
My sister-in-law has Crohn’s disease. It’s been really bad since she was pretty young. She had her colon removed when she was a teenager.
In 2014 she gave birth to my nephew, her first child. It was an incredibly difficult process, and she knew that she couldn’t possibly have another child without some kind of big medical intervention.
In 2016 she decided to get an ileostomy at age 35. This means that there’s a small hole in her abdomen where the end of her small intestine pokes out (a stoma) into a plastic pouch which is only removed for her to clean her stoma. She can exercise, sleep, bathe, and do pretty much any activity she wants with the ileostomy bag. She named her stoma Donny.
She raves about how her ileostomy changed her life. She was able to give birth to a daughter in 2019, which she could not have done otherwise. Her Crohn’s symptoms are much more manageable now. She doesn’t have to decline or cancel on plans and activities nearly as much as anymore.
A lot of chronically ill people are discouraged from utilizing tools because they would have to “rely on them” for the rest of their life. It’s not inherently a bad thing to rely on medical intervention! My sister-in-law will have her ileostomy for the rest of her life, and it’s a good thing; she’s going to be able to live her life with fewer restrictions than ever before.
This story is particularly about an ileostomy, but this point can apply to a lot of different symptom management options. Getting a permanent ostomy might be the right choice. Taking pills might be the right choice. Using a mobility aid might be the right choice. Needing help isn’t a bad thing, even if you’ll need it for the rest of your life.
#ostomy#ileostomy#spoonie#chronic illness#surgery#surgery mention#i don't know if she named donny after trump but it's could be a joke about how he's an asshole? idk#i remember a while ago she posted on fb about going ziplining and said 'if i could shit my pants i would have' lol#og text
15 notes
·
View notes
Text
jotting down something related to cancer and myself. something ive taken from a website somewhere, that may or may not be valid, but hits a lot of marks from what ive dealt with recently. here we go.
((With your treatment completed, you'll likely see your cancer care team less often. Though you, your friends and your family are all eager to return to a more normal life, it can be scary to leave the protective cocoon of doctors and nurses who supported you through treatment.
Everything you're feeling right now is normal for cancer survivors. Recovering from cancer treatment isn't just about your body — it's also about healing your mind.
Take time to acknowledge the fear, grief and loneliness you're feeling right now. Then take steps to understand why you feel these emotions and what you can do about them. -- taken from Mayo Clinic.))
My last chemotherapy session was around May 2018, so I’ll hit that third year mark very soon, which means I’m halfway through recovering. In a sense, I’m not a survivor yet, unless I hit that five year mark, but between now and then, I’m trying to adjust to a certain sense of normality that I’ve never felt before. In short, I’m a little uncertain, and very scared, of what could happen in the future to me.
((Stress in cancer survivors
When you were diagnosed with cancer, you might have focused completely on your treatment and getting healthy. Now that you've completed treatment, all those projects around the house and the things on your to-do list are competing for your attention. This can make you feel stressed and overwhelmed.
Don't feel you need to do everything at once. Take time for yourself as you establish a new daily routine. Try exercising, talking with other cancer survivors and taking time for activities you enjoy.
Depression and anxiety in cancer survivors
Lingering feelings of sadness and anger can interfere with your daily life. For many people these feelings will dissipate. But for others, these feelings can develop into depression.
Tell your doctor about your feelings. If needed, you can be referred to someone who can help you through talk therapy, medication or both. Early diagnosis and prompt treatment are keys to successfully overcoming depression.
Self-consciousness in cancer survivors
If surgery or other treatment changed your appearance, you might feel self-conscious about your body.
Changes in skin color, weight gain or loss, the loss of a limb, or the placement of an ostomy might make you feel like you'd rather stay home, away from other people. You might withdraw from friends and family. And self-consciousness can strain your relationship with your partner if you don't feel worthy of love or affection.
Take time to grieve. But also learn to focus on the ways cancer has made you a stronger person and realize that you're more than the scars that cancer has left behind. When you're more confident about your appearance, others will feel more comfortable around you.
Loneliness in cancer survivors
You might feel as if others can't understand what you've been through, which makes it hard to relate to other people and can lead to loneliness. Friends and family might be unsure of how to help you, and some people may even be afraid of you because you've had cancer.
Don't deal with loneliness on your own. Consider joining a support group with other cancer survivors who are having the same emotions you are. Contact your local chapter of the American Cancer Society for more information. Or try an online message board for cancer survivors, such as the American Cancer Society's Cancer Survivors Network.))
A lot of these hit the mark pretty close to me, which makes things difficult to manage, but I know I’m not alone.
But sometimes, I can’t help but feel that way.
All in all, I think taking my time to come to terms with what happened to me is the only thing I can do, while managing everything else in between, from finally getting support on finding a job to figuring myself out over time. I mean, the tumor was basically in my uterus, which is what killed it, so that definitely affected my identity and thoughts on my own gender. But, regardless, I’m still me, yknow? Nothing can change that.
Well, not entirely. I think, in a way, I see myself non-binary, but still prefer to use she/her pronouns, because I don’t want to erase something I’ve been embracing for a good portion of my life, which is my womanhood. I don’t have a uterus, but that doesn’t mean I’m any less than a woman, but the traumatic event really shook me up enough to have second thoughts, yknow? At the end of the day, I can only figure that out for myself.
Anyway, I’m getting off point. I just want to say, while I’m sure I’ll get better, the trauma is still difficult to deal with. And while I’m still scared of things, like a relapse or perhaps the disease spreading, given it’s sarcoma related, I pray, and want to work hard, on getting better more ways than one.
Thinking back on it, I remember what a doctor of mine told me, who was a Czech Republican, that if I continue thinking negative thoughts, I’ll only feel worse, and won’t recover well, which is what gave me the strength to power through those negative thoughts. He also mention that fear is a natural reaction, and it can help the body fight as well, but it’s also important to think positive and work on that, because I’ll heal better that way. I got to say, it was definitely helpful, and I don’t want to forget him and the others that worked on my case.
God, I’ve been through a lot, but I’m trying to sort out my feelings somehow, as I’m slowly but surely adjusting to the changes around me. It’s hard, but it’s not impossible.(But my depression will slow me down. Ugh.)
#blah blah blabbity blah#long post#health stuff#cancer warning#cancer mention warning#cancer tw#now i just need to rest.#or do something absolutely silly that may or may not get me banned from a game.#:}
5 notes
·
View notes
Text
Retraining my body: Shit that should not be hard.
Sitting up at a desk should not be hard, but after my shoulder surgery, followed a month later by an 8-incision massive abdominal surgery round robin, followed by an ostomy closure and healing...
I have not been able to sit up since mid-October of 2022.
It's as hard as any of my PT exercises. It hurts after a few hours.
It makes me sad, because like so much that I used to do without a second thought, I can't do it any longer. I have to relearn so much.
10 notes
·
View notes
Text
A Few Tips for Ostomates for Flying
Many of us like traveling and holidays are ringing the bells. Thus, you must have some plans for trips. For ostomates, it seems hard to travel with ostomy supplies. However, you can make it easy by following a few tips. Apart from holiday traveling, some people need to travel a lot for work purposes. Thus, you can make it lighter and cozy by the below guidelines.
The following are the tips for ostomates for flying to ease their travel and reduce the anxiety.

Pack some Extra Ostomy Tools in your Luggage
While packing up your luggage, you should keep your ostomy supplies in the bag according to the days you want to spend there. Here, I suggest you bring two to three extra tools with you. However, you can bring as many supplies as you typically use per day. It will make your luggage heavy, but you have to keep it fully equipped for traveling and living out of the station for a few days or weeks.
Moreover, you should bring some coy wearables like a supportive belt, hernia prevention strap, cleaning kit, and exercising tool. So, whenever you are out for vacation or on a professional trip, you should bring two to three extra ostomy kits.
Your Emergency Ostomy Kit Should be Accessible
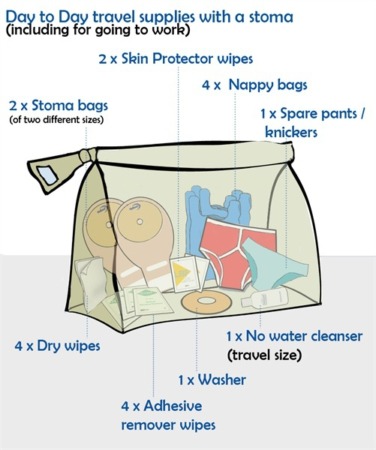
While traveling, your emergency tool kit should be in front of your hand carry, or suitcase. Make sure that you are keeping the ostomy supplies accessible. In the need of an emergency, you can find them and use, before encountering ostomy related trouble.
Moreover, you should pack your ostomy tools in multiple bags. You should keep one kit in the hand carry, one in the suitcase, and another in your other bag (if you are carrying any extra bag). Merely, you should have one ostomy kit in every suitcase and handbags.
After packing your luggage, you need to keep in mind as few essential precautionary measures that are important at the airport.
Bring Emergency Ostomy Supplies through Security
In some countries like the USA, allowed to bring a few ostomy tools like scissors. You can pack this too in your hand carry, and the security will pass. Therefore, you can bring such emergency supplies at the airport. However, a few security checks do not allow you to bring cutters; therefore, before traveling check out the guidelines of packing and luggage. But, you can take medications along with you.

Ask TSA Officer at Airport
Before going into the security check process, you should inform the TSA officer regarding your medical health, medications, accessories, and emergency supplies. You should ask the officer about separating your other belongings from the liquid medicines and ostomy supplies for the screening process.
The Rule for Liquid Medicines at Airport
You can bring your liquid medicines and other necessary medications along with you at the airport. However, there is a rule for that you can take 3.4 ounces or 100 milliliters in your hand carry. Before screening at the airport, you should separate your medicines and supplies from your other luggage in the carry-on bag. Both will have to go through separate checking steps. Apart from the liquids, you can bring ice packs, freezer packs, gel packs, scissors, and some other essentials of ostomy tools.
After airport screening, you are now on the plane and the tips to follow there are:
Be Careful while Using Overhead Compartment
We all usually use overhead compartments on planes. However, for ostomates, it would be tough to lift the luggage from the ground to up above the head. It needs a lot of strength. You should not use your muscles in the initial stage of ostomy for lifting the carry-on bag. Thus, be careful, you can ask for help.
Use Lavatory in the Airplane
You can use lavatory to change your ostomy bag, clean yourself, and drain the stoma pouch.
youtube
4 notes
·
View notes
Text
How To Manage Dehydration When You Have IBD
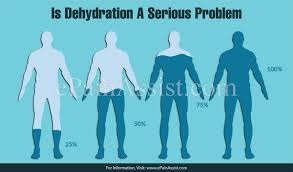
Do you find that you have trouble staying hydrated because of the signs and symptoms of inflammatory bowel disease (IBD)? Diarrhea can lead to dehydration even in healthy adults and can be a special problem when IBD causes chronic diarrhea. People with Crohn's disease and ulcerative colitis sometimes also have surgery to treat their disease, which can include the removal of some or all of the large intestine. The large intestine is where most water is absorbed, and when part or all of it is missing, less water might be absorbed by the body. This is why hydration is a special area of concern for people who have an ileostomy or have had j-pouch surgery (ileal pouch-anal anastomosis or IPAA). Dehydration is a major cause of readmission to the hospital after ileostomy surgery.
The Origin Of Sports And Energy Drinks
Many people turn to sports drinks as a source of hydration. There are a few different groups that developed drinks that were meant to provide hydration and energy before, during, and after exercise. The most famous of them was originally developed for use by athletes who may lose a lot of water by sweating, especially during hot weather. Dr. Robert Cade of the University of Florida, at the request of the university's assistant football coach, led a team that originally developed a drink containing electrolytes and carbohydrates. The football team went on to have a successful season while using the drink, and other colleges started asking for it. This, of course, was the start of the sports drink Gatorade. In time, manufacturers began adding other ingredients to their drinks, including stimulants like caffeine, to create energy drinks. Most energy and sports drinks also contain artificial colors and sweeteners.
Sports Drinks May Not Be the Answer to Dehydration
There are a few things about sports and energy drinks that make them a less than perfect choice for people with IBD who need to replenish fluids and electrolytes. The first is that they don't actually offer the right mix of nutrients: most don't contain enough electrolytes. The second is that some brands contain things that aren't needed that make them taste better (sugar or artificial sweeteners), look colorful (artificial colors), and provide a burst of energy (caffeine). The World Health Organization has developed an oral rehydration salts (ORS) solution that is used across the world, especially in areas where severe dehydration is a cause of illness and death.2 Using a special combination of salts and water to rehydrate is called oral rehydration therapy (ORT), and it saves lives in areas of the world where diarrheal disease is a leading cause of death in children. ORS is available in Western countries at pharmacies, hospital supply stores, and sometimes in sporting goods stores with the first aid kits. There are also recipes for ORS that can be made at home. ORS is usually fairly inexpensive but checks with a doctor before resorting to buying it or making it at home for rehydration.
How Can People With IBD Get Hydrated?
Short of keeping a supply of ORS on hand (although it's not a bad idea to keep some with your emergency supplies), how can people with a j-pouch, an ileostomy, or IBD, rehydrate at home? According to the University of Michigan IBD Team, rehydration is probably best done with a mix of a few things most people with IBD probably already have at home. The experts at U of M recommend that the sports drink is just a start.4 To bring hydration up, they suggest eating and drinking the items in this "recipe" designed to mimic ORT: 1 liter of sports drink1/2 cup of chicken soupOne of the following:1.6 bananas1.6 sweet potatoes1.6 medium avocados1.5 cups of yogurt1 cup of spinach3 1/2 tablets of 650 mg of sodium bicarbonate (or 7 325 mg tablets) The United Ostomy Association of America also has recipes available for replacing electrolytes and fluids. This is the suggested homemade electrolyte drink:5 1 teaspoon salt1 teaspoon baking soda1 teaspoon white Karo syrup1 6-ounce can freeze orange juiceAdd water to make one quart, mix well
What To Do If You're Dehydrated
Mild cases of dehydration can usually be dealt with at home. Severe cases of dehydration may need to be treated by a physician or in a hospital. For severe dehydration, with symptoms of confusion, dizziness, or fainting, call 911. If you have more questions about how to avoid becoming dehydrated, or what you should eat or drink if you are dehydrated, ask your physician. click here to read more Read the full article
1 note
·
View note
Text
Global Urinary Incontinence Market size share Covid-19 Impact and Forecast2028
The global urinary incontinence market is expected to continue its growth trajectory over the next few years, with a CAGR of 8.12% from 2023 to 2028. By 2028, the market is projected to reach USD 21100.62 Million, driven by several factors including the growing aging population, increasing prevalence of chronic diseases such as diabetes and obesity, and rising awareness about urinary incontinence.
The market can be segmented by product type, treatment type, and end-user. Products used for the treatment of urinary incontinence include adult diapers, catheters, and absorbent pads, among others. The catheter segment is expected to be the fastest-growing product segment during the forecast period, owing to the increasing adoption of intermittent catheters as a safe and effective treatment option for urinary incontinence.
Treatment types include behavioral therapy, pharmacological therapy, and surgical therapy. The behavioral therapy segment is expected to continue its dominance in the market, driven by the increasing adoption of non-invasive and non-pharmacological treatment options such as pelvic floor exercises, bladder training, and lifestyle modifications.
In terms of end-user, the market can be segmented into hospitals, clinics, and home care settings. The hospital segment is expected to dominate the market, owing to the increasing number of patients seeking medical care for urinary incontinence and the availability of advanced diagnostic and treatment options in hospital settings.
Geographically, the global urinary incontinence market can be segmented into North America, Europe, Asia Pacific, Latin America, and Middle East & Africa. North America is expected to continue its dominance in the market, driven by the high prevalence of urinary incontinence in the region and the presence of advanced healthcare infrastructure.
In conclusion, the global urinary incontinence market is expected to witness significant growth over the next few years, driven by several factors including the growing aging population and rising awareness about urinary incontinence. The market is highly competitive, with several key players operating in the space, including Boston Scientific Corporation, C.R. Bard Inc., and Coroplast A/S, among others.
Technological advancements in the field of urinary incontinence treatment are also expected to fuel the growth of the market. For instance, several companies are investing in the development of new products and technologies, such as neuromodulation devices and biodegradable bladder implants, which are expected to revolutionize the treatment of urinary incontinence.
Moreover, the growing trend of home healthcare is expected to drive the demand for home-based treatment options for urinary incontinence. This has led to the development of innovative products, such as portable catheters and adult diapers, which are designed to provide patients with greater comfort and convenience.
However, the high cost of urinary incontinence treatment and the lack of reimbursement policies in certain regions may hinder market growth. Additionally, the social stigma associated with urinary incontinence may discourage patients from seeking medical help, which could limit the adoption of treatment options.
In terms of the competitive landscape, the global urinary incontinence market is highly fragmented, with several players operating in the space. These companies are focusing on product innovation, strategic collaborations, and mergers and acquisitions to gain a competitive edge in the market. For instance, in February 2021, Coloplast A/S announced the acquisition of Nine Continents Medical, a Chinese manufacturer of urology and ostomy products, to expand its presence in the Asia Pacific region.
In conclusion, the global urinary incontinence market is expected to witness significant growth over the next few years, driven by several factors including technological advancements, increasing adoption of home-based treatment options, and the growing prevalence of urinary incontinence. However, challenges such as high treatment costs and social stigma may hinder market growth, and companies are focusing on product innovation and strategic partnerships to stay ahead of the competition.
0 notes