#HIV
Text
HIV and COVID
A major barrier to preventing the spread of HIV is accurate test results.
There is a high chance there are many people with HIV that have it and do not know. We do not know how long this undetected time period is (lentiviruses are often associated with long periods of time of virus activity that goes undetected- 5 to 10 years or more), but there is a chance many individuals with HIV go undiagnosed for many years. Individuals during this time before an HIV diagnosis complain of fatigue and many undiagnosed disabling symptoms during that time period. HIV is able to cause changes to immune cells that prevent HIV tests from finding the infection. Some people get negative HIV tests when they are HIV positive. This means you could be HIV negative, but still have HIV in your blood and can spread HIV to other individuals.
Getting a COVID vaccination (and sometimes other vaccinations like the flu vaccination) can help the body identify HIV hiding in the body. This allows earlier treatment and intervention. Once HIV has been identified, it also reduces the risk for all individuals in our population to be exposed to more severe infections.
Getting tested regularly for HIV used to be part of our federal public health recommendations.
This just further emphasizes why this information is so important to know and healthcare needs to start testing for more diseases in more people and do these tests more often.
People often assume their infection came from an unfaithful partner, but in reality HIV has been spreading unknowingly to many in the medical community and still in the public sphere no one is talking about it like the huge deal it is.
This potential means people could be raped as a child, never have sex again, never encounter drugs, and then be miserable & living with an active HIV infection into their early 20s and they would never know. Once they got a positive test result they would have no idea where the infection even came from.
Our entire understanding of these types of diseases has to change and the seriousness of this topic has to be addressed by the world. This was theorized as a mechanism of HIV spread due to how many people were getting diagnosed but had no identifiable cause of their HIV, but now it’s proven and right in front of us. This is disastrous.
To everyone that told the truth about how they didn’t know how they got these types of diseases & how they had no idea where they got it from then faced judgement from others and even the medical community- you aren’t crazy.
On behalf of everything these types of diseases did to destroy families, relationships, and your body, I’m going to apologize right now for all the individuals that I know won’t ever give you an apology for what they did and what they said.
I believe you. I always did.
Without you telling your truth , we never would have been able to figure this out about HIV.
HIV is spreading in “HIV negative” individuals to other individuals as some researchers theorized.
The mRNA vaccination technology developed is now the foundation for the next generation of HIV treatment and disease control. We must continue to push and advocate for improving the lives of all people with disease and we all just took a huge step forward.
You do not have to be sexually active to develop HIV. Your sexual trauma doesn’t have to define your life for the rest of your life- you are stronger than you know and braver than you feel.
Find a place to get tested for HIV here:
I still recommend getting a NAT or “viral load” test done as the first test to see if you have HIV.
I think considering what we know about HIV and in consideration of all the things we still don’t know that this is the safest option. Any other test for this condition available today has too high of a chance of producing a wrong result. I find it extremely uncomfortable we still use the other types of tests in the hospital and doctor office settings.
If you choose to order a test through an online service be aware some tests only tell you about either HIV-1 or HIV-2 and will not always provide you information related to type 1 and type 2.
For example, here:
This will provide you information related to ordering a test that looks for both types of HIV instead of just one strain of HIV.
Stay safe.
#hiv#virus#sick#chronically ill#chronic pain#chronic illness#chronic fatigue#pain#doctor#medicine#viral
648 notes
·
View notes
Text

Source
#politics#hiv#us politics#government#gilead#lgbt#lgbtq#progressive#current events#science#medicine#health#health care#the left#twitter post#news
34K notes
·
View notes
Text




In the midst of that amazing time in my life came the worst, and that was when my friends just started dropping dead. They were sick today and dead tomorrow. And when you would go to the hospital to look for you friend they would be out in the hallway on a gurney pushed up against a wall dying for help, dying for love, dying to be saved. And some of them with that sign on their gurney that said "do not touch". And they suffered, and people wanted to act like they weren't good people, kind people, wonderful people, somebody's son, somebody's daughter, somebody. // SHERYL LEE RALPH receiving the Human Rights Campaign's National Ally for Equality Award 2022. (x)
25K notes
·
View notes
Text

"We all deserve the right to protect and keep ourselves safe. Implementing a mask ban is not only an infringement on our human rights but also extremely ableist and inconsiderate of those disabled or immunocompromised.
. . .
About 1 in 5 adult New Yorkers have a disability. If a mask ban were to be implemented, spaces such as stores and restaurants might ban masking or set up mask-removal policy. That’s 1 in 5 adults no longer able to shop in public along with others, or participate in gatherings.
Forcing immunocompromised people to remove their face masks would likely violate the federal Americans with Disabilities Act and the New York State Human Rights Law. As a member of ACT UP NY, it’s always my goal to fight for human rights such as healthcare.
Those that are HIV+ are 8% more likely to be hospitalized due to COVlD than those that aren’t and are also at an increased risk of developing Long COVlD.
Masking SAVES LIVES. Masking is community care.”
Behind the Powecom KN95 is Serita @_seritasargent_ and her friend Bri’anna @lanoirede.jpg holding the #StopMaskBans sign.
MaskTogetherAmerica encourages everyone to speak up and write to elected officials to demand they oppose the anti-mask bills S9867/A10057 and S9194! We need to defend our right to masks.
2K notes
·
View notes
Text

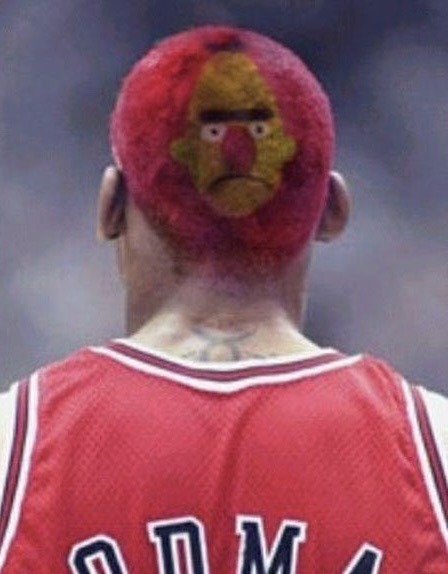
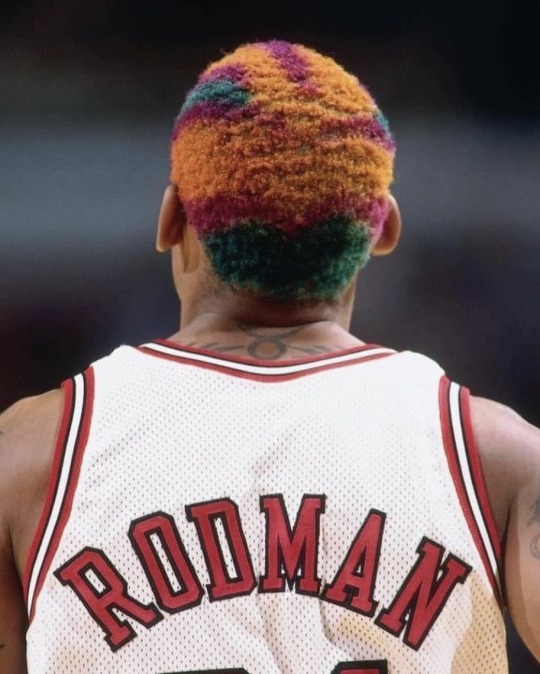

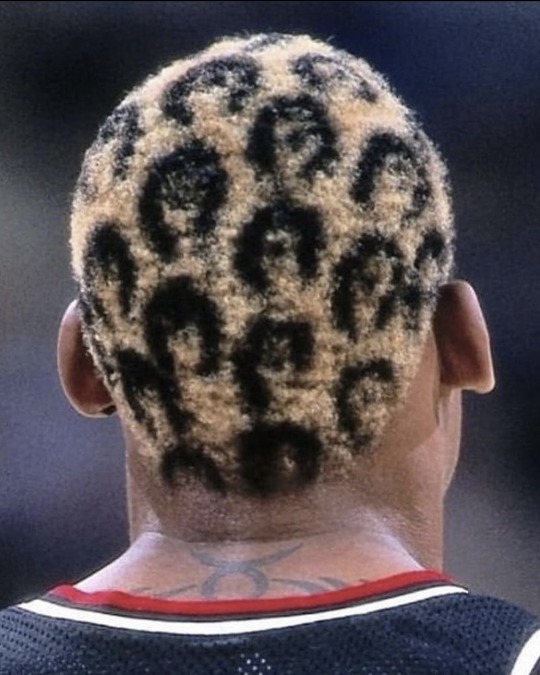
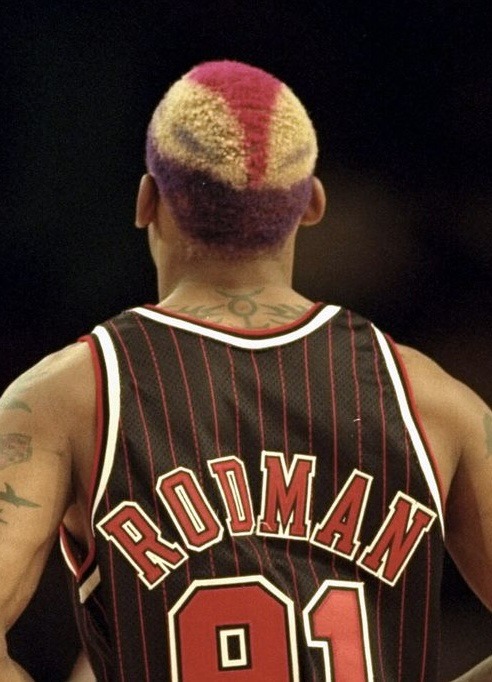
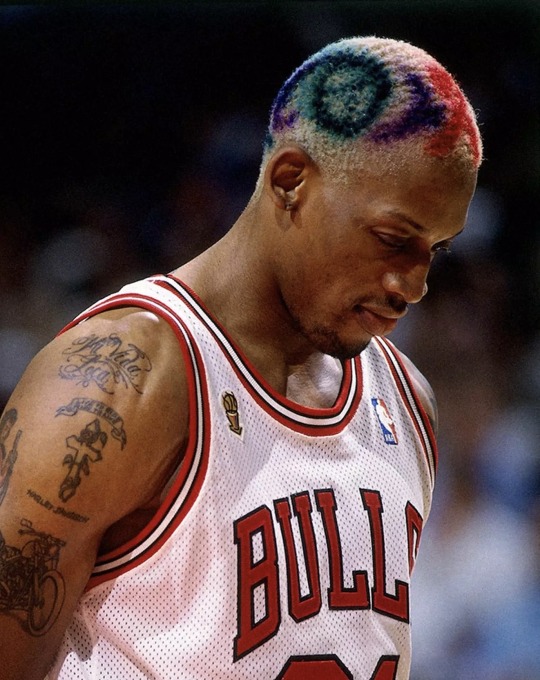

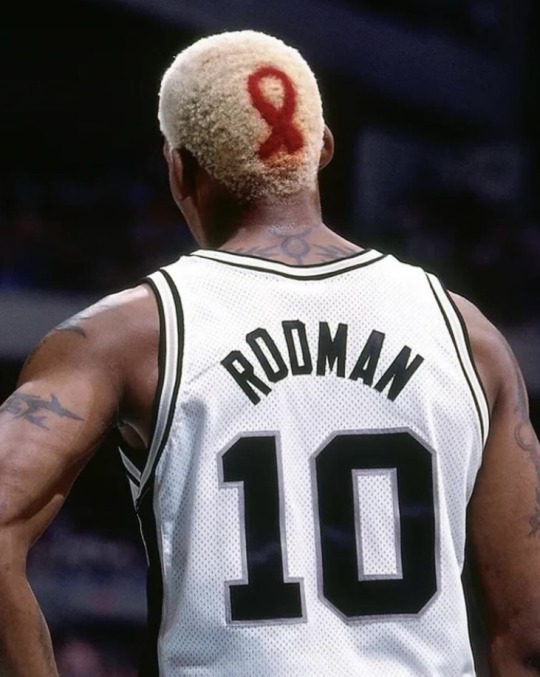
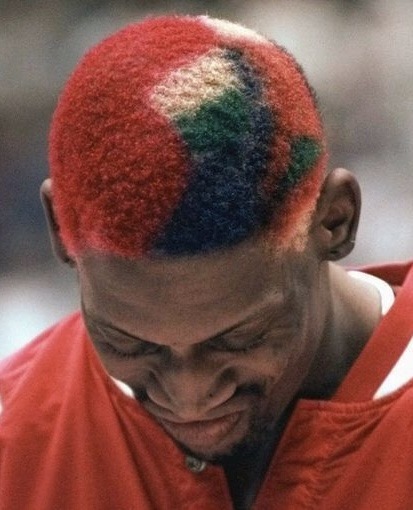
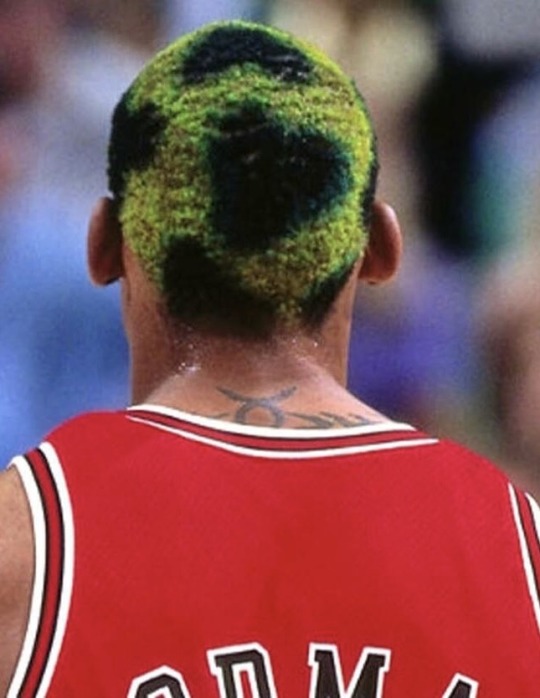
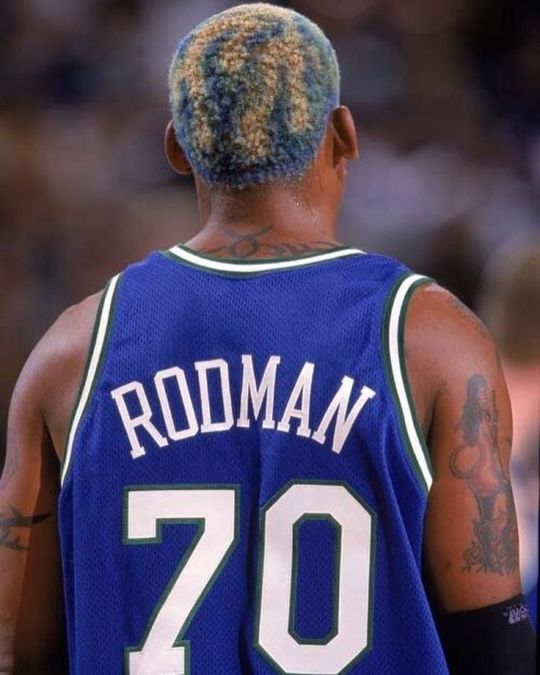

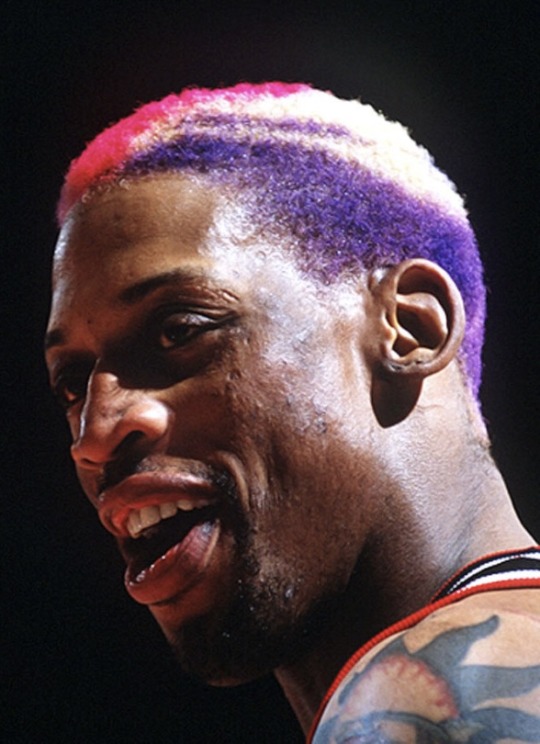



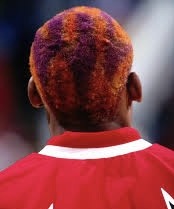
Dennis Rodman’s hairstyles
#dennis rodman#chicago bulls#sports#basketball#aesthetic#90s#nostalgia#childhood#athlete#celebs#hair#hair colour ideas#hairstyle#hair styles#aids#hiv#red ribbon#1990s#90s aesthetic#smiley face#bert#bert and ernie#sesame street#rainbowcore#people#humans
3K notes
·
View notes
Text
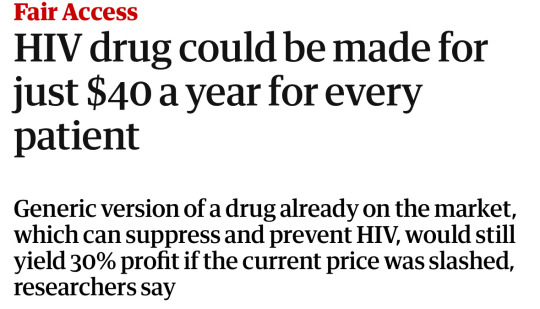
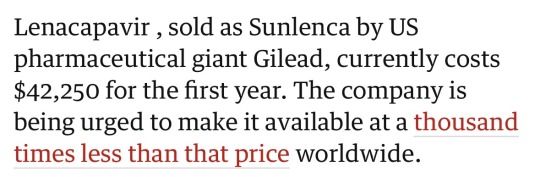
"A large clinical trial in South Africa and Uganda has shown that a twice-yearly injection of a new pre-exposure prophylaxis drug gives young women total protection from HIV infection.
The trial tested whether the six-month injection of lenacapavir would provide better protection against HIV infection than two other drugs, both daily pills. All three medications are pre-exposure prophylaxis (or PrEP) drugs.
Physician-scientist Linda-Gail Bekker, principal investigator for the South African part of the study, tells Nadine Dreyer what makes this breakthough so significant and what to expect next.
Tell us about the trial and what it set out to achieve
The Purpose 1 trial with 5,000 participants took place at three sites in Uganda and 25 sites in South Africa to test the efficacy of lenacapavir and two other drugs.
Lenacapavir (Len LA) is a fusion capside inhibitor. It interferes with the HIV capsid, a protein shell that protects HIV’s genetic material and enzymes needed for replication. It is administered just under the skin, once every six months.
The randomised controlled trial, sponsored by the drug developers Gilead Sciences, tested several things.
The first was whether a six-monthly injection of lenacapavir was safe and would provide better protection against HIV infection as PrEP for women between the ages of 16 and 25 years than Truvada F/TDF, a daily PrEP pill in wide use that has been available for more than a decade.
Secondly, the trial also tested whether Descovy F/TAF, a newer daily pill, was as effective as F/TDF...
The trial had three arms. Young women were randomly assigned to one of the arms in a 2:2:1 ratio (Len LA: F/TAF oral: F/TDF oral) in a double blinded fashion. This means neither the participants nor the researchers knew which treatment participants were receiving until the clinical trial was over.
In eastern and southern Africa, young women are the population who bear the brunt of new HIV infections. They also find a daily PrEP regimen challenging to maintain, for a number of social and structural reasons.
During the randomised phase of the trial none of the 2,134 women who received lenacapavir contracted HIV. There was 100 percent efficiency.
By comparison, 16 of the 1,068 women (or 1.5%) who took Truvada (F/TDF) and 39 of 2,136 (1.8%) who received Descovy (F/TAF) contracted the HIV virus...
What is the significance of these trials?
This breakthrough gives great hope that we have a proven, highly effective prevention tool to protect people from HIV.
There were 1.3 million new HIV infections globally in the past year. Although that’s fewer than the 2 million infections seen in 2010, it is clear that at this rate we are not going to meet the HIV new infection target that UNAIDS set for 2025 (fewer than 500,000 globally) or potentially even the goal to end Aids by 2030...
For young people, the daily decision to take a pill or use a condom or take a pill at the time of sexual intercourse can be very challenging.
HIV scientists and activists hope that young people may find that having to make this “prevention decision” only twice a year may reduce unpredictability and barriers.
For a young woman who struggles to get to an appointment at a clinic in a town or who can’t keep pills without facing stigma or violence, an injection just twice a year is the option that could keep her free of HIV.
What happens now?
The plan is that the Purpose 1 trial will go on but now in an “open label” phase. This means that study participants will be “unblinded”: they will be told whether they have been in the “injectable” or oral TDF or oral TAF groups.
They will be offered the choice of PrEP they would prefer as the trial continues.
A sister trial is also under way: Purpose 2 is being conducted in a number of regions including some sites in Africa among cisgender men, and transgender and nonbinary people who have sex with men.
It’s important to conduct trials among different groups because we have seen differences in effectiveness. Whether the sex is anal or vaginal is important and may have an impact on effectiveness.
How long until the drug is rolled out?
We have read in a Gilead Sciences press statement that within the next couple of months [from July 2024] the company will submit the dossier with all the results to a number of country regulators, particularly the Ugandan and South African regulators.
The World Health Organization will also review the data and may issue recommendations.
We hope then that this new drug will be adopted into WHO and country guidelines.
We also hope we may begin to see the drug being tested in more studies to understand better how to incorporate it into real world settings.
Price is a critical factor to ensure access and distribution in the public sector where it is badly needed.
Gilead Sciences has said it will offer licences to companies that make generic drugs, which is another critical way to get prices down.
In an ideal world, governments will be able to purchase this affordably and it will be offered to all who want it and need protection against HIV."
-via The Conversation, July 3, 2024
#HOLY FUCKING SHIT#100% EFFECTIVE AGAINST HIV INFECTION#AND JUST TWO SHOTS PER YEAR HOLY FUCKING SHIT#THIS IS UNBELIEVABLY GAME-CHANGING#hiv#hiv aids#hiv awareness#lgbtq news#medical news#drug trials#hiv prevention#prep#uganda#south africa#aids#aids crisis#good news#hope
2K notes
·
View notes
Text


Condoman
In 1987, Indigenous sexual health worker Aunty Gracelyn Smallwood and her team felt that safe sex advertising wasn’t effectively targeting people in Australia’s remote Indigenous communities. In response, they created Condoman - “The Deadly Predator of Sexual Health” - who spoke to Indigenous people in language they could relate to, and removed stigma from conversations about sexual health.
Condoman became something of a cult figure in Australia, and in 2009 he was relaunched with a suite of comics, animations, and merch, including branded condoms. He was also joined by his “deadly, slippery sister” Lubelicious, who promoted consent, the use of water based lube, and women’s health, for her sisters and sistergirls (an Indigenous term analogous to trans women).
We covered Condoman in our podcast on the AIDS epidemic in Australia.
Keep an eye on this blog throughout the week as we continue highlighting queer Aboriginal and Torres Strait Islander history and culture for NAIDOC Week.
#naidoc2024#naidoc week#aids#hiv#condoman#queer history#gay history#lgbt history#queer#gay#lgbt#lgbtq#indigenous history#aboriginal history
422 notes
·
View notes
Note
My question about the AIDS crisis, I'm mostly asking you because like I said, I don't think I was googling the right things, so even if you could just suggest some things to google that would be more likely to get me answers, that would be really helpful.
I guess it's mostly how did AIDS (and to some extent, any STD) become so widespread? I know that it spread through sexual contact and shared blood, but can you really "six degrees of separation" (god, that sounds so flippant, but i genuinely can't think how else to describe it) a chain of sexual partners and shared needles through any two people with HIV in the entire world? Maybe it's just because I'm a bit of a hermit, but while I can understand how it was so devastating once it was already widespread, I guess I'm having trouble understanding how it got such a foothold in the first place. If the first person with HIV had happened to not have a lot of sex would the AIDS crisis never have happened?
I swear I have absolutely no judgement for people that like to have a lot of sex, maybe I just have an underestimate of the amount of sex the average person has because frankly I don't have any? So I hope this doesn't sound disrespectful or anything, it's just kind of hard for me to believe those "six degrees of separation" kind of things in general when it's not like, famous people, so the realization that theoretically any two people with the same STD, on different parts of the globe, would have this string of sexual partners connecting them almost feels like there has to be something I'm missing... But when I'm googling things like "how did HIV become so widespread" and "how do STDs spread" I'm just getting things about how you should use protection and histories of *where* HIV spread rather than answering this more specific question (probably didn't help I was trying to do this research at 1am)
I mean this as kindly as possible:
What is your proposed alternate theory as to the spread of a disease which is transmitted through contact with blood, semen (and pre-seminal fluid), rectal and vaginal fluids, and breast milk? The disease does not spread through saliva or through touch which does not involve those fluids.
There are relatively rare cases of HIV spread through accidental needle sticks - according to WebMD, there are approximately 385k accidental needle sticks among health care workers per year in the US. WHO says that .7% of the global population has HIV, so for some back-of-the-napkin math, at most, you'll have about 2,700 of those needle sticks involving someone with HIV. Since (again, according to that WebMD article on accidental needle sticks), in cases of an accidental needle stick where the patient has HIV, the health care worker only has about a 1 in 300 chance of catching it (as opposed to 1 in 3 for an unvaccinated person catching hepatitis B via accidental needle stick from an infected patient). So - nationwide - you have approximately 9 people per year catching HIV from a needle stick.
And, to be clear, that fucking sucks. However, according to the Bureau of Labor Statistics, in 2022 there were approximately 14.7 million health care workers in the US. Not all of these people have equal risk for accidental needle sticks, but there's only so much research I'm gonna do for rough math to answer an ask on Tumblr.
The average US health care worker has approximately - again, based on my back-of-the-napkin math - 0.00000544% chance of contracting HIV from an accidental needle stick. It's astronomically more likely that a random health care worker will die from tripping over an extension cord or breathing in a caustic chemical than that they will catch HIV.
The chances of getting HIV via blood transfusion before we started routinely testing for it were all but assured if you got blood from someone with HIV. Testing now is so stringent that you have about a one in two million chance of getting HIV from a transfusion. The last recorded case I could find was in 2010, and before that, it was 2002, and the 2010 case happened in part because the donor lied about his risk profile and often participated in anonymous and unprotected sex with partners of multiple genders. He really shouldn't have been accepted as a donor at all. Approximately 4.5 million Americans receive blood transfusions per year, so, like, nowadays, it is excessively unlikely, but even in the 80s, it was an edge case means of infection, not a main source of pandemic spread.
A breastfeeding parent with a detectable viral load has about a 15% chance of transmitting HIV through breast milk. Likewise, HIV can be - and was - transmitted to babies during birth because of contact with vaginal fluid or blood, but, again, these relative edge cases are not the things pandemics are made of.
I want to stress that I am not in any way minimizing the absolute tragedy of the AIDS crisis, and I am not dismissing the fact that these methods of transmission are possible and did cause significant disruption to blood banks, stress for pregnant people with HIV, and so on. They just simply are not major methods of transmission, and never were.
With all of that said... what is your proposed alternate method of transmission, with these facts in hand? What do you think happened? Genuinely, this question is so baffling to me.
I think it's important to understand that before the emergence of HIV, most of the STIs we had were at that point either considered an annoyance (warts, HPV) or were extremely easy to treat and cure (syphilis, once a death sentence, became basically a non-issue for most people in the US as long as they were getting tested relatively frequently, and most other common STIs even today can be cured with a single course or even a single dose of antibiotics).
With that in mind, a lot of people, including a lot of queer people, were having a lot of unprotected sex. For people who could become pregnant, the advent of the pill and access to legal abortion meant that they didn't have to become or stay pregnant if they didn't want to, and for cis gay men, the prevalence of antibiotics meant that the vast majority of STIs were a brief inconvenience at worst.
So allo people did one of the things that allo people (and some ace people!) love to do:
They fucked. A lot. They fucked without fear of much consequence in terms of infection, and because it was much riskier to bring someone home where you could be seen, a lot of gay men cruised, fucking in parks or in literal back alleys or the bathrooms of clubs. They worried about getting arrested or getting caught and having their names in the newspaper much more than they worried about STIs. Sex workers, including trans sex workers, fucked in cars or hotels or... wherever the money was, because survival sec work is ... survival.
So... yeah. What is your proposed alternate theory, here? I am truly baffled at what you think otherwise happened, given a disease with a very narrow route of infection.
749 notes
·
View notes
Text
HIV lost an amazing advocate - since childhood she was an outspoken activist who opened a lot of people’s eyes especially in the early years of the epidemic. May she be at peace now.
402 notes
·
View notes
Text


Source
1K notes
·
View notes
Text
youtube
"AIDS is not a bad person's disease! It is not god punishing people for their sins!"
The Golden Girls is a legendary American sitcom airing from 1985, to 1992. It centered around three older women and their daily life. The show was lauded for tackling controversial issues such as lgbt+ rights, ageism, racism, ableism, and beyond.
The ensemble actresses (Bea Arthur, Betty White, Rue McClanahan and Estelle Getty) supported social justice in real life. To this day, The Golden Girls are beloved by the lgbt+ community for the mark they made on American culture.
227 notes
·
View notes
Text
For a vaccine to work, it has to raise antibodies in the immunized – antibodies that are primed to neutralize subsequent intruders. For a vaccine to be safe, it has to do so for the vast majority without major side effects or reactions.
A new vaccine candidate for HIV is facing those familiar challenges in early-stage clinical trials, succeeding in one aspect but encountering some hurdles in the other.
It's still progress though, as its developers have reformulated the vaccine to improve its safety in future studies – while their latest results show how the vaccine successfully generates broadly neutralizing antibodies in a small number of people.
Continue Reading.
205 notes
·
View notes
Text
Richard Hunt (deceased)
Gender: Male
Sexuality: Gay
DOB: 17 August 1951
RIP: 7 January 1992
Ethnicity: White - American
Occupation: Puppeteer
Note: Because he was too ill with AIDS to do so, Hunt was the only Muppet Show puppeteer who did not return for The Muppet Christmas Carol, which is dedicated to his memory as well as that of Jim Henson.
#Richard Hunt#Muppet Christmas Carol#lgbt history#gay history#lgbt#male#gay#1951#rip#historical#white#puppeteer#hiv#popular#popular post#200
392 notes
·
View notes
Text
"Since it was first identified in 1983, HIV has infected more than 85 million people and caused some 40 million deaths worldwide.
While medication known as pre-exposure prophylaxis, or PrEP, can significantly reduce the risk of getting HIV, it has to be taken every day to be effective. A vaccine to provide lasting protection has eluded researchers for decades. Now, there may finally be a viable strategy for making one.
An experimental vaccine developed at Duke University triggered an elusive type of broadly neutralizing antibody in a small group of people enrolled in a 2019 clinical trial. The findings were published today [May 17, 2024] in the scientific journal Cell.
“This is one of the most pivotal studies in the HIV vaccine field to date,” says Glenda Gray, an HIV expert and the president and CEO of the South African Medical Research Council, who was not involved in the study.
A few years ago, a team from Scripps Research and the International AIDS Vaccine Initiative (IAVI) showed that it was possible to stimulate the precursor cells needed to make these rare antibodies in people. The Duke study goes a step further to generate these antibodies, albeit at low levels.
“This is a scientific feat and gives the field great hope that one can construct an HIV vaccine regimen that directs the immune response along a path that is required for protection,” Gray says.
-via WIRED, May 17, 2024. Article continues below.
Vaccines work by training the immune system to recognize a virus or other pathogen. They introduce something that looks like the virus—a piece of it, for example, or a weakened version of it—and by doing so, spur the body’s B cells into producing protective antibodies against it. Those antibodies stick around so that when a person later encounters the real virus, the immune system remembers and is poised to attack.
While researchers were able to produce Covid-19 vaccines in a matter of months, creating a vaccine against HIV has proven much more challenging. The problem is the unique nature of the virus. HIV mutates rapidly, meaning it can quickly outmaneuver immune defenses. It also integrates into the human genome within a few days of exposure, hiding out from the immune system.
“Parts of the virus look like our own cells, and we don’t like to make antibodies against our own selves,” says Barton Haynes, director of the Duke Human Vaccine Institute and one of the authors on the paper.
The particular antibodies that researchers are interested in are known as broadly neutralizing antibodies, which can recognize and block different versions of the virus. Because of HIV’s shape-shifting nature, there are two main types of HIV and each has several strains. An effective vaccine will need to target many of them.
Some HIV-infected individuals generate broadly neutralizing antibodies, although it often takes years of living with HIV to do so, Haynes says. Even then, people don’t make enough of them to fight off the virus. These special antibodies are made by unusual B cells that are loaded with mutations they’ve acquired over time in reaction to the virus changing inside the body. “These are weird antibodies,” Haynes says. “The body doesn’t make them easily.”
Haynes and his colleagues aimed to speed up that process in healthy, HIV-negative people. Their vaccine uses synthetic molecules that mimic a part of HIV’s outer coat, or envelope, called the membrane proximal external region. This area remains stable even as the virus mutates. Antibodies against this region can block many circulating strains of HIV.
The trial enrolled 20 healthy participants who were HIV-negative. Of those, 15 people received two of four planned doses of the investigational vaccine, and five received three doses. The trial was halted when one participant experienced an allergic reaction that was not life-threatening. The team found that the reaction was likely due to an additive in the vaccine, which they plan to remove in future testing.
Still, they found that two doses of the vaccine were enough to induce low levels of broadly neutralizing antibodies within a few weeks. Notably, B cells seemed to remain in a state of development to allow them to continue acquiring mutations, so they could evolve along with the virus. Researchers tested the antibodies on HIV samples in the lab and found that they were able to neutralize between 15 and 35 percent of them.
Jeffrey Laurence, a scientific consultant at the Foundation for AIDS Research (amfAR) and a professor of medicine at Weill Cornell Medical College, says the findings represent a step forward, but that challenges remain. “It outlines a path for vaccine development, but there’s a lot of work that needs to be done,” he says.
For one, he says, a vaccine would need to generate antibody levels that are significantly higher and able to neutralize with greater efficacy. He also says a one-dose vaccine would be ideal. “If you’re ever going to have a vaccine that’s helpful to the world, you’re going to need one dose,” he says.
Targeting more regions of the virus envelope could produce a more robust response. Haynes says the next step is designing a vaccine with at least three components, all aimed at distinct regions of the virus. The goal is to guide the B cells to become much stronger neutralizers, Haynes says. “We’re going to move forward and build on what we have learned.”
-via WIRED, May 17, 2024
#hiv#aids#aids crisis#virology#immunology#viruses#vaccines#infectious diseases#vaccination#immune system#public health#medicine#healthcare#hiv aids#hiv prevention#good news#hope#medical news
912 notes
·
View notes