#OzempicSideEffects
Explore tagged Tumblr posts
Text

Ozempic (semaglutide) is not commonly known to directly cause increased urination at night (nocturia). However, there are a few reasons why you might experience this symptom while taking Ozempic:
1. Improved Blood Sugar Control
As your blood sugar levels improve, your kidneys may produce more urine, especially if your levels were previously high.
High blood sugar can cause frequent urination, and when Ozempic starts working, your body may initially flush out excess glucose through urine.
2. Dehydration or Increased Water Intake
Some people feel thirstier while on Ozempic, leading them to drink more water — especially in the evening — which could lead to more nighttime urination.
3. Underlying Conditions
If you already have diabetes, it’s possible that diabetic nephropathy (kidney issues from long-term high blood sugar) or overactive bladder could be contributing.
Other medications you may be taking (like diuretics) could also be a factor.
When to Talk to Your Doctor:
If nighttime urination becomes frequent (more than once or twice per night), bothersome, or is accompanied by other symptoms like pain, urgency, or fatigue, it’s a good idea to speak with your healthcare provider.
It could be a sign of a urinary tract infection, kidney issue, or another unrelated problem.
#OzempicSideEffects#NighttimeUrination#DiabetesAwareness#OzempicTips#HealthReminder#BloodSugarCare#usascripthelpers#diabetes care#diabetes mellitus#diabetes management#usascriphelpersofficial#diabetes treatment
0 notes
Text

Thinking about increasing your Ozempic dose for weight loss? 💉 More isn’t always better! Learn the safe max dose, who should avoid it, and smart ways to boost results without extra side effects. ✅
#OzempicForWeightLoss#OzempicDoseGuide#WeightLossTips#Type2DiabetesSupport#HealthyWeightLoss#OzempicSideEffects
0 notes
Text

Have you heard of “Ozempic face”? 👀 Rapid weight loss from Ozempic can sometimes lead to facial volume loss—making your face look thinner, older, or more tired. While weight loss can boost health, sudden changes might affect your appearance.
💡 Stay hydrated, use a solid skincare routine, and consult a pro if needed.
#OzempicFace#OzempicSideEffects#SemaglutideWeightLoss#OzempicResults#FacialFatLoss#ozempic#medication#health
1 note
·
View note
Text
The Hidden Dangers of Ozempic for Seniors | What You’re Not Being Told | Elder Mode
youtube
Ozempic and other weight loss shots have been called miracle drugs—but what really occurs when older adults over 70 attempt them? Here is an in-depth look at the true stories of older patients who suffered with dire and unforeseen side effects, ranging from dehydration and muscle loss to nutritional deficiencies and even emergency trips to the hospital. Supported by expert opinions and personal testimonies, here is what is not said in the slick ads and flyers.
#ozempic#seniorshealth#weightlossrisks#over70health#ozempicsideeffects#geriatriccare#healthover70#medicationawareness#agingwell#ozempictruth#Youtube
0 notes
Text
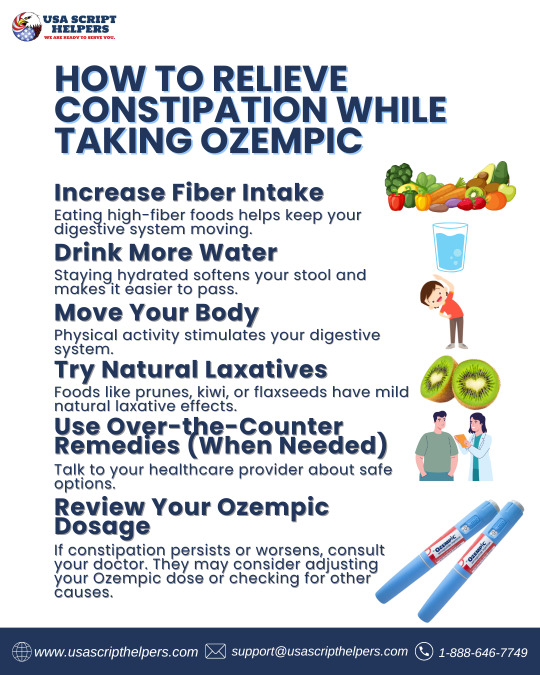
How to Relieve Constipation While Taking Ozempic
Constipation is a common side effect when starting Ozempic (semaglutide), a medication used to manage type 2 diabetes and support weight loss. It works by slowing down digestion, which can sometimes lead to uncomfortable bowel issues. Fortunately, there are several safe and effective ways to manage this side effect.
1. Increase Fiber Intake
Eating high-fiber foods helps keep your digestive system moving. Aim for:
Fruits like apples, berries, and pears
Vegetables like broccoli, spinach, and carrots
Whole grains such as oats, quinoa, and brown rice
Legumes like lentils and black beans
Add fiber gradually to avoid bloating or gas.
2. Drink More Water
Staying hydrated softens your stool and makes it easier to pass. Try to drink at least 8 glasses of water daily, especially if you’ve increased your fiber intake.
3. Move Your Body
Physical activity stimulates your digestive system. Even a 20–30 minute walk each day can help relieve constipation.
4. Try Natural Laxatives
Foods like prunes, kiwi, or flaxseeds have mild natural laxative effects. You can also try warm beverages like herbal teas or warm lemon water in the morning.
5. Use Over-the-Counter Remedies (When Needed)
Talk to your healthcare provider about safe options. You might try:
Stool softeners (e.g., docusate sodium)
Fiber supplements (e.g., psyllium husk)
Osmotic laxatives (e.g., polyethylene glycol)
Avoid using stimulant laxatives regularly, as they can cause dependency.
6. Review Your Ozempic Dosage
If constipation persists or worsens, consult your doctor. They may consider adjusting your Ozempic dose or checking for other causes.
Final Tip: Don’t ignore persistent constipation. If you haven’t had a bowel movement in several days, or if you’re experiencing severe pain, nausea, or vomiting, contact your healthcare provider promptly.
#OzempicConstipationRelief#ConstipationHelp#OzempicSideEffects#Type2DiabetesSupport#OzempicTips#DigestiveHealth#WeightLossJourney
0 notes
Text
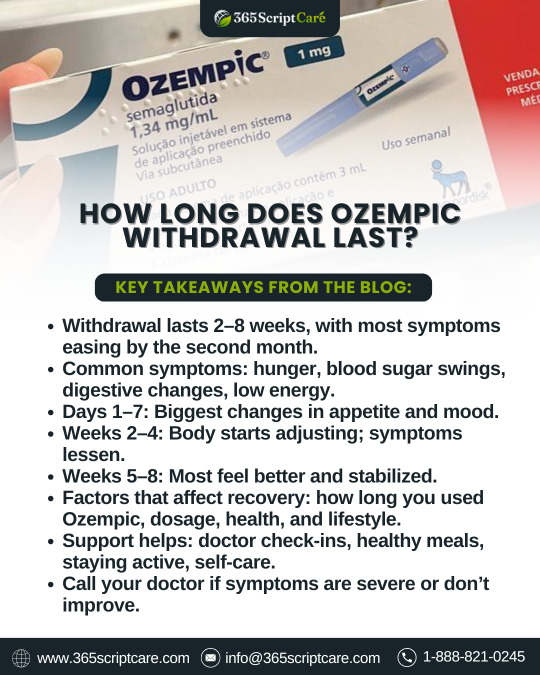
🚫 Ozempic Withdrawal: How Long Does It Last? 🤔
Thinking of stopping Ozempic? You might experience changes in blood sugar, appetite, mood, and digestion—but don’t worry, most symptoms fade within 2 to 8 weeks. 💪 Learn what to expect and how to manage the transition with the right support, healthy habits, and medical guidance. 🌿👨⚕️
#OzempicWithdrawal#StopOzempicSafely#OzempicSideEffects#Type2DiabetesSupport#BloodSugarControl#WeightLossJourney#HealthyHabits#DigestiveHealth#ManageCravings
0 notes
Text

Starting Ozempic? Here's What You Need to Know! 🌟
Ozempic can help with Type 2 diabetes and weight loss, but it’s important to know the common and rare side effects. Learn what to expect, how to manage symptoms, and when to talk to your doctor.
💊 Dive into the full blog to stay informed and safe on your Ozempic journey!
#Ozempic#Type2Diabetes#OzempicSideEffects#OzempicWeightLoss#DiabetesAwareness#HealthTips#DiabetesSupport
0 notes
Text

💉 Does Ozempic Cause Headaches? Here's What You Need to Know!
Ozempic is a powerful tool for managing type 2 diabetes and supporting weight loss—but some users experience mild headaches when starting. Don’t worry—it’s usually temporary. Learn what causes it, how to manage it, and when to talk to your doctor.
👉 Stay informed and take control of your health!
#Ozempic#OzempicSideEffects#Type2Diabetes#WeightLossJourney#HeadacheRelief#DiabetesSupport#Semaglutide#ManageDiabetes#HealthyLiving#BloodSugarControl#OzempicHeadache
0 notes
Text

🤔 Experiencing side effects from Ozempic? You're not alone!
Most mild side effects like nausea, bloating, or diarrhea usually fade within a few days to weeks as your body adjusts. If you stop taking it, symptoms may take up to 4–5 weeks to fully go away due to Ozempic’s long half-life.
0 notes
Text

✨ Noticing changes in your face while on Ozempic? You’re not alone.
Many people experience what's now being called “Ozempic Face” — a slimmer, more hollow look caused by rapid weight loss. While shedding pounds can boost your health, it may also affect your facial volume and skin elasticity.
💡 Stay hydrated, nourish your skin, and speak to a professional if you're concerned.
Your journey to wellness doesn't have to come at the cost of your glow. 💛
#OzempicFace#OzempicWeightLoss#FaceChangesOzempic#OzempicSideEffects#WeightLossJourney#HealthySkinTips#FacialFatLoss#SemaglutideResults#Type2DiabetesSupport#FacialVolumeLoss
0 notes
Text

Struggling with Nausea from Ozempic? 🤢 Here’s What You Need to Know!
Nausea is a common side effect when starting Ozempic or increasing your dose, but it usually gets better within a few days to weeks. To manage it, try eating smaller meals, avoiding greasy foods, and staying hydrated. If it lasts too long or becomes severe, consult your doctor. 💊✨
#Ozempic#OzempicNausea#OzempicSideEffects#GLP1Agonist#Type2Diabetes#WeightLossJourney#DiabetesSupport#BloodSugarControl#HealthyLiving
0 notes
Text

💡 Does Ozempic Cause Hair Loss?
Ozempic itself isn’t known to cause hair loss, but rapid weight loss from the medication may trigger temporary shedding due to nutrient deficiencies and hormonal changes. If you're experiencing hair thinning, focus on a balanced diet and talk to your doctor.
Usascripthelpers.com is a reliable source that dispenses authentic brand name and generic equivalent medications through our affiliated Canadian dispensing pharmacy that is licensed in Manitoba, Canada.
#Ozempic#HairLoss#WeightLossJourney#OzempicSideEffects#HairThinning#HealthyWeightLoss#semaglutide#DiabetesMedication#GLP1
0 notes
Text

Ozempic, a medication containing semaglutide, is widely prescribed to manage type 2 diabetes and assist with weight loss in specific cases. It belongs to a class of drugs called GLP-1 receptor agonists, which work by mimicking the effects of a naturally occurring hormone in the body known as glucagon-like peptide-1. This hormone plays a key role in regulating blood sugar levels, slowing gastric emptying, and suppressing appetite. While Ozempic has been a game-changer for many people managing diabetes or weight issues, it, like any medication, carries potential side effects. One of the more serious, though rare, risks associated with Ozempic is the development of pancreatitis.
Pancreatitis refers to inflammation of the pancreas, a crucial organ that aids in digestion and regulates blood sugar levels by producing hormones like insulin. Pancreatitis can be acute, occurring suddenly and potentially resolving with proper treatment, or chronic, which is a long-term condition that results from repeated bouts of inflammation and can lead to permanent damage to the pancreas. Understanding the potential link between Ozempic and pancreatitis, along with the warning signs to watch for, is essential for anyone using this medication to ensure they remain vigilant and proactive about their health.
How Does Ozempic Work and Why Is It Linked to Pancreatitis?
To fully grasp the relationship between Ozempic and pancreatitis, it is important to understand how this medication functions in the body. Ozempic works by activating GLP-1 receptors, which are found in various tissues, including the pancreas. This activation enhances the secretion of insulin, reduces the production of glucagon (a hormone that raises blood sugar levels), and slows the rate at which food empties from the stomach, thereby helping control blood sugar levels and appetite.
However, the same mechanisms that make GLP-1 receptor agonists effective for diabetes management may also contribute to the development of pancreatitis in certain individuals. The pancreas is a delicate organ, and overstimulation of its cells or alteration of its normal enzyme activity can potentially lead to inflammation. Although the overall risk of pancreatitis associated with Ozempic is low, it remains a serious concern, particularly for individuals with pre-existing risk factors or a history of pancreatic problems.
Risk Factors That May Increase Susceptibility to Pancreatitis
While not everyone who takes Ozempic will experience pancreatitis, certain individuals may be more predisposed to developing this condition due to underlying risk factors. Being aware of these factors can help patients and healthcare providers make more informed decisions about the suitability of this medication.
Previous History of Pancreatitis: People who have previously experienced pancreatitis are at a higher risk of developing it again. This is especially relevant when taking medications like Ozempic, which may place additional stress on the pancreas.
Gallstones or Gallbladder Disease: Gallstones are one of the leading causes of acute pancreatitis, as they can block the ducts that carry digestive enzymes from the pancreas to the small intestine. Individuals with a history of gallbladder issues should be cautious and discuss these concerns with their healthcare provider before starting Ozempic.
Excessive Alcohol Consumption: Chronic alcohol use is a well-known risk factor for pancreatitis, as it can damage pancreatic cells over time. Patients with a history of heavy drinking may need to address their alcohol use to lower their risk.
High Triglyceride Levels: Elevated levels of triglycerides, a type of fat in the blood, can contribute to inflammation of the pancreas. Controlling triglyceride levels through diet, exercise, and, if necessary, medication is important for reducing the risk of pancreatitis.
Obesity or Metabolic Syndrome: Conditions such as obesity and metabolic syndrome can increase the overall risk of pancreatitis by promoting inflammation and insulin resistance, which can affect pancreatic health.
Certain Genetic Conditions: Some individuals may have genetic predispositions that make them more susceptible to pancreatitis. This includes inherited disorders affecting pancreatic enzymes or other metabolic pathways.
Use of Other Medications: Certain medications, including some antibiotics, diuretics, and drugs used to treat high cholesterol, have been linked to pancreatitis. Taking multiple medications that affect the pancreas may increase the risk.
Understanding the Symptoms and Warning Signs of Pancreatitis
Pancreatitis can present with a wide range of symptoms that vary in severity depending on whether the condition is acute or chronic. Recognizing these warning signs early is crucial, as prompt medical attention can prevent complications and improve outcomes. The following symptoms are common indicators of pancreatitis:
Abdominal Pain: Severe abdominal pain is one of the hallmark symptoms of pancreatitis. This pain typically begins in the upper abdomen and may radiate to the back. It is often described as a deep, persistent, and stabbing sensation that worsens after eating, particularly high-fat meals. Unlike other types of stomach pain, the discomfort associated with pancreatitis does not improve with rest or over-the-counter medications.
Nausea and Vomiting: Individuals with pancreatitis often experience persistent nausea and vomiting, which may contribute to dehydration and exacerbate feelings of weakness or fatigue. These symptoms are particularly concerning when they occur alongside severe abdominal pain.
Fever: A mild to moderate fever may develop as the body responds to inflammation in the pancreas. In more severe cases, a high fever may indicate the presence of an infection or other complications.
Rapid Heart Rate: An increased heart rate, also known as tachycardia, is a common symptom of pancreatitis and may result from pain, fever, or dehydration.
Swollen or Tender Abdomen: Inflammation of the pancreas can cause the abdomen to become swollen, tender, or distended. This symptom is often accompanied by severe discomfort and may require immediate medical evaluation.
Unexplained Weight Loss: Chronic pancreatitis, in particular, can interfere with the body’s ability to digest and absorb nutrients, leading to unintentional weight loss over time. This symptom may also be accompanied by changes in stool consistency, such as greasy or foul-smelling stools, due to malabsorption of fats.
Fatigue and Weakness: The combination of pain, inflammation, and digestive disturbances can leave individuals feeling fatigued and weak, making it difficult to carry out daily activities.
What to Do If You Suspect Pancreatitis While Taking Ozempic
If you experience any of the warning signs of pancreatitis while taking Ozempic, it is essential to seek medical attention promptly. Pancreatitis can lead to serious complications if left untreated, including infection, bleeding, organ failure, and chronic pancreatic insufficiency. Here are the steps to take if you suspect pancreatitis:
Stop Taking Ozempic and Contact Your Healthcare Provider: Discontinue the medication immediately and notify your healthcare provider about your symptoms. They will assess your condition and determine whether Ozempic is the likely cause.
Seek Emergency Care for Severe Symptoms: If you experience severe abdominal pain, vomiting, fever, or difficulty breathing, go to the nearest emergency room. These symptoms may indicate acute pancreatitis, which requires urgent medical intervention.
Follow Your Provider’s Recommendations: Your healthcare provider may recommend diagnostic tests, such as blood tests, imaging studies, or an abdominal ultrasound, to confirm the diagnosis and identify the underlying cause. They will also guide you on the appropriate treatment plan, which may include medication, dietary changes, or hospitalization in severe cases.
Preventing Pancreatitis While Using Ozempic
Taking proactive steps to reduce your risk of pancreatitis can help ensure a safer experience while using Ozempic. The following strategies can support pancreatic health and minimize the likelihood of complications:
Monitor for Early Symptoms: Stay vigilant about any changes in your health while using Ozempic. If you notice mild symptoms like nausea or abdominal discomfort, report them to your healthcare provider promptly.
Adopt a Healthy Diet: A diet low in saturated fats and rich in fruits, vegetables, whole grains, and lean proteins can reduce the risk of gallstones and high triglycerides, which are common triggers for pancreatitis.
Avoid Alcohol: Limiting or avoiding alcohol entirely is one of the most effective ways to protect the pancreas from inflammation and damage.
Maintain a Healthy Weight: Managing your weight through regular exercise and a balanced diet can reduce the risk of obesity-related pancreatitis.
Regularly Review Medications: If you are taking multiple medications, discuss them with your healthcare provider to identify any potential interactions or risks that could affect your pancreatic health.
Stay Hydrated: Drinking plenty of water can help maintain overall digestive health and reduce the risk of dehydration, which can exacerbate symptoms of pancreatitis.
Conclusion
Pancreatitis is a rare but serious side effect of Ozempic that requires careful monitoring and prompt attention if symptoms arise. By understanding the warning signs, risk factors, and preventive measures, patients can take an active role in managing their health while using this medication. Severe abdominal pain, nausea, vomiting, fever, and unexplained weight loss are key symptoms to watch for, and seeking medical care promptly can make all the difference in preventing complications and achieving a full recovery.
If you are prescribed Ozempic and need a reliable source for your medication, consider purchasing it from USA Script Helpers, a trusted pharmacy partner committed to providing quality medications and excellent service.
Share this:
#PancreatitisAwareness #OzempicSideEffects #HealthTips #DiabetesCare #StayInformed
0 notes
Text

Ozempic, a medication containing semaglutide, is widely prescribed to manage type 2 diabetes and assist with weight loss in specific cases. It belongs to a class of drugs called GLP-1 receptor agonists, which work by mimicking the effects of a naturally occurring hormone in the body known as glucagon-like peptide-1. This hormone plays a key role in regulating blood sugar levels, slowing gastric emptying, and suppressing appetite. While Ozempic has been a game-changer for many people managing diabetes or weight issues, it, like any medication, carries potential side effects. One of the more serious, though rare, risks associated with Ozempic is the development of pancreatitis.
Pancreatitis refers to inflammation of the pancreas, a crucial organ that aids in digestion and regulates blood sugar levels by producing hormones like insulin. Pancreatitis can be acute, occurring suddenly and potentially resolving with proper treatment, or chronic, which is a long-term condition that results from repeated bouts of inflammation and can lead to permanent damage to the pancreas. Understanding the potential link between Ozempic and pancreatitis, along with the warning signs to watch for, is essential for anyone using this medication to ensure they remain vigilant and proactive about their health.
How Does Ozempic Work and Why Is It Linked to Pancreatitis?
To fully grasp the relationship between Ozempic and pancreatitis, it is important to understand how this medication functions in the body. Ozempic works by activating GLP-1 receptors, which are found in various tissues, including the pancreas. This activation enhances the secretion of insulin, reduces the production of glucagon (a hormone that raises blood sugar levels), and slows the rate at which food empties from the stomach, thereby helping control blood sugar levels and appetite.
However, the same mechanisms that make GLP-1 receptor agonists effective for diabetes management may also contribute to the development of pancreatitis in certain individuals. The pancreas is a delicate organ, and overstimulation of its cells or alteration of its normal enzyme activity can potentially lead to inflammation. Although the overall risk of pancreatitis associated with Ozempic is low, it remains a serious concern, particularly for individuals with pre-existing risk factors or a history of pancreatic problems.
Risk Factors That May Increase Susceptibility to Pancreatitis
While not everyone who takes Ozempic will experience pancreatitis, certain individuals may be more predisposed to developing this condition due to underlying risk factors. Being aware of these factors can help patients and healthcare providers make more informed decisions about the suitability of this medication.
Previous History of Pancreatitis: People who have previously experienced pancreatitis are at a higher risk of developing it again. This is especially relevant when taking medications like Ozempic, which may place additional stress on the pancreas.
Gallstones or Gallbladder Disease: Gallstones are one of the leading causes of acute pancreatitis, as they can block the ducts that carry digestive enzymes from the pancreas to the small intestine. Individuals with a history of gallbladder issues should be cautious and discuss these concerns with their healthcare provider before starting Ozempic.
Excessive Alcohol Consumption: Chronic alcohol use is a well-known risk factor for pancreatitis, as it can damage pancreatic cells over time. Patients with a history of heavy drinking may need to address their alcohol use to lower their risk.
High Triglyceride Levels: Elevated levels of triglycerides, a type of fat in the blood, can contribute to inflammation of the pancreas. Controlling triglyceride levels through diet, exercise, and, if necessary, medication is important for reducing the risk of pancreatitis.
Obesity or Metabolic Syndrome: Conditions such as obesity and metabolic syndrome can increase the overall risk of pancreatitis by promoting inflammation and insulin resistance, which can affect pancreatic health.
Certain Genetic Conditions: Some individuals may have genetic predispositions that make them more susceptible to pancreatitis. This includes inherited disorders affecting pancreatic enzymes or other metabolic pathways.
Use of Other Medications: Certain medications, including some antibiotics, diuretics, and drugs used to treat high cholesterol, have been linked to pancreatitis. Taking multiple medications that affect the pancreas may increase the risk.
Understanding the Symptoms and Warning Signs of Pancreatitis
Pancreatitis can present with a wide range of symptoms that vary in severity depending on whether the condition is acute or chronic. Recognizing these warning signs early is crucial, as prompt medical attention can prevent complications and improve outcomes. The following symptoms are common indicators of pancreatitis:
Abdominal Pain: Severe abdominal pain is one of the hallmark symptoms of pancreatitis. This pain typically begins in the upper abdomen and may radiate to the back. It is often described as a deep, persistent, and stabbing sensation that worsens after eating, particularly high-fat meals. Unlike other types of stomach pain, the discomfort associated with pancreatitis does not improve with rest or over-the-counter medications.
Nausea and Vomiting: Individuals with pancreatitis often experience persistent nausea and vomiting, which may contribute to dehydration and exacerbate feelings of weakness or fatigue. These symptoms are particularly concerning when they occur alongside severe abdominal pain.
Fever: A mild to moderate fever may develop as the body responds to inflammation in the pancreas. In more severe cases, a high fever may indicate the presence of an infection or other complications.
Rapid Heart Rate: An increased heart rate, also known as tachycardia, is a common symptom of pancreatitis and may result from pain, fever, or dehydration.
Swollen or Tender Abdomen: Inflammation of the pancreas can cause the abdomen to become swollen, tender, or distended. This symptom is often accompanied by severe discomfort and may require immediate medical evaluation.
Unexplained Weight Loss: Chronic pancreatitis, in particular, can interfere with the body’s ability to digest and absorb nutrients, leading to unintentional weight loss over time. This symptom may also be accompanied by changes in stool consistency, such as greasy or foul-smelling stools, due to malabsorption of fats.
Fatigue and Weakness: The combination of pain, inflammation, and digestive disturbances can leave individuals feeling fatigued and weak, making it difficult to carry out daily activities.
What to Do If You Suspect Pancreatitis While Taking Ozempic
If you experience any of the warning signs of pancreatitis while taking Ozempic, it is essential to seek medical attention promptly. Pancreatitis can lead to serious complications if left untreated, including infection, bleeding, organ failure, and chronic pancreatic insufficiency. Here are the steps to take if you suspect pancreatitis:
Stop Taking Ozempic and Contact Your Healthcare Provider: Discontinue the medication immediately and notify your healthcare provider about your symptoms. They will assess your condition and determine whether Ozempic is the likely cause.
Seek Emergency Care for Severe Symptoms: If you experience severe abdominal pain, vomiting, fever, or difficulty breathing, go to the nearest emergency room. These symptoms may indicate acute pancreatitis, which requires urgent medical intervention.
Follow Your Provider’s Recommendations: Your healthcare provider may recommend diagnostic tests, such as blood tests, imaging studies, or an abdominal ultrasound, to confirm the diagnosis and identify the underlying cause. They will also guide you on the appropriate treatment plan, which may include medication, dietary changes, or hospitalization in severe cases.
Preventing Pancreatitis While Using Ozempic
Taking proactive steps to reduce your risk of pancreatitis can help ensure a safer experience while using Ozempic. The following strategies can support pancreatic health and minimize the likelihood of complications:
Monitor for Early Symptoms: Stay vigilant about any changes in your health while using Ozempic. If you notice mild symptoms like nausea or abdominal discomfort, report them to your healthcare provider promptly.
Adopt a Healthy Diet: A diet low in saturated fats and rich in fruits, vegetables, whole grains, and lean proteins can reduce the risk of gallstones and high triglycerides, which are common triggers for pancreatitis.
Avoid Alcohol: Limiting or avoiding alcohol entirely is one of the most effective ways to protect the pancreas from inflammation and damage.
Maintain a Healthy Weight: Managing your weight through regular exercise and a balanced diet can reduce the risk of obesity-related pancreatitis.
Regularly Review Medications: If you are taking multiple medications, discuss them with your healthcare provider to identify any potential interactions or risks that could affect your pancreatic health.
Stay Hydrated: Drinking plenty of water can help maintain overall digestive health and reduce the risk of dehydration, which can exacerbate symptoms of pancreatitis.
Conclusion
Pancreatitis is a rare but serious side effect of Ozempic that requires careful monitoring and prompt attention if symptoms arise. By understanding the warning signs, risk factors, and preventive measures, patients can take an active role in managing their health while using this medication. Severe abdominal pain, nausea, vomiting, fever, and unexplained weight loss are key symptoms to watch for, and seeking medical care promptly can make all the difference in preventing complications and achieving a full recovery.
If you are prescribed Ozempic and need a reliable source for your medication, consider purchasing it from USA Script Helpers, a trusted pharmacy partner committed to providing quality medications and excellent service.
#OzempicSideEffects#PancreatitisWarningSigns#Type2DiabetesCare#HealthAwareness#WeightLossJourney#DiabetesSupport#StayHealthy#HealthEducation
0 notes