#Primary Sclerosing Cholangitis (PSC)
Explore tagged Tumblr posts
Text
youtube
New song coming soon!
Lyrics:
[verse 1]
Born sick with extra fees
In debt to save the body
Christ would save you for free
They won’t do that in America baby
They’re makin’ dimes off your desperation
And you’ll keep your life as consolation
Paying everything you got to stay alive,
Cause you’re not worth enough for savin’
[chrous]
Well I’ve been
Livin’ on
borrowed time
And I got no patience left
Corrupted politicians
Are out of line
They’ll leave us all for dead
Their pockets lined
With these warning signs
Buyin’ votes with pretty lies
You know God won’t save the wicked
And He damn sure won’t save the rich
#Youtube#spoonie problems#spoonie stuff#spoonie#musicians on tumblr#flyawayrage#independent artist#lesbiansontumblr#new music#chronically ill#ibd#crohns disease#crohns#ibd problems#ehlers danlos syndrome#potsie#pots#primary sclerosing cholangitis#PSC#chronic illness#chronic migraine#just chronic illness things
9 notes
·
View notes
Text
With this post, I am finally able to tie together the appearance of SPED, Turbocancers and excess Autoimmune Disease. I propose that the Spike Protein’s invasion of the Endothelium, followed by its invasion of the Extracellular Matrix, explains all three. Thank you for supporting my work, it has allowed me to look very deeply and discover.
As readers of this Substack know, I have, from the beginning, called the Spike Protein’s invasion of the Endothelium Spike Protein Endothelial Disease (SPED). I then proposed that the Spike Protein subsequently traveled from the Endothelium into the body’s organs, where it would induce autoimmune disease and/or fibrosis. Yet, the actual mechanism of this progression has eluded me – until now.
What I have discovered is that the Spike Protein’s ability to bind Integrin provides a perfectly satisfactory explanation for this malevolent journey and its deleterious consequences. To start, let us look at some autoimmune diseases which are found to be Integrin Regulated Autoimmune Disorders.
Type 1 Diabetes Mellitus
Rheumatoid Arthritis
Multiple Sclerosis
Systemic Lupus Erythematosus
Type 1 Autoimmune Hepatitis
Scleroderma
Let’s look at some studies, shall we?
Vaccination is one of the most vigorous ways to intervene in the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic. Cases of autoimmune hepatitis (AIH) after coronavirus disease (COVID-19) vaccination have been increasingly reported. Twenty-seven cases of AIH are summarized in this study, providing emerging evidence of autoimmune reactions in response to various COVID-19 vaccines, including in patients with special disease backgrounds such as primary sclerosing cholangitis (PSC), liver transplantation, and previous hepatitis C virus (HCV) treatment.
7 notes
·
View notes
Text
What is Ulcerative Colitis: A Comprehensive Summary
Ulcerative colitis (UC) is a chronic, inflammatory bowel disease (IBD) characterised by continuous inflammation of the colonic lining, beginning in the rectum and potentially extending proximally throughout the entire colon. UC is limited to the colon and involves only the superficial layers.
UC is a relapsing-remitting condition, meaning it alternates between periods of active disease (flares) and times of little or no symptoms (remission). Its onset can be gradual or sudden, and the severity can range from mild discomfort to life-threatening complications.
When your gut doesn’t feel good, nothing else feels right. Pain, bloating, and unpredictable bowel movements can make you feel helpless. It’s not just physical; it impacts your confidence, routines, and relationships. Many people live with chronic digestive discomfort without knowing that a condition like ulcerative colitis could be the cause, and that it’s treatable.
What are the symptoms of UC? How do I know if I have UC?
The clinical presentation of ulcerative colitis depends on the extent and severity of the disease. Symptoms may develop gradually or suddenly and may vary from person to person.
Intestinal Symptoms
Bloody diarrhoea: This is the hallmark symptom, often with mucus.
Abdominal pain: Commonly crampy and located in the lower left quadrant.
Urgency and pain during defecation: Sudden urge to defecate and a feeling of incomplete evacuation.
Increased frequency of bowel movements: Often more than six times per day during flares.
Passage of stools in sleep causes extreme discomfort and may disrupt sleep.
2. Generalised Symptoms
Fever
Fatigue
Weight loss
Anaemia: Due to chronic blood loss and inflammation.
3. Problems outside of the intestine:
UC is associated with systemic inflammation that can affect other organs:
Arthritis: Especially peripheral joints.
Uveitis and episcleritis: Eye inflammation.
Erythema nodosum and pyoderma gangrenosum: Skin manifestations.
Primary sclerosing cholangitis (PSC): A liver disease that can occur in association with UC.
Why did I get UC? What are the Causes and Risk Factors?
The exact cause of ulcerative colitis remains unknown. It is believed to be the result of a complex interplay of genetic, environmental, immune-related, and microbial factors.
Here are some key contributors:
Genetic Factors
Family history increases the risk significantly. First-degree relatives of individuals with UC are at a higher risk.
2. Immune System Dysfunction
UC is thought to be an autoimmune condition, where the immune system inappropriately attacks the lining of the colon.
3. Environmental Factors
Geography: More common in industrialised countries, particularly in North America and Northern Europe.
Diet: High-fat and high-sugar diets, low intake of fruits and vegetables, and excessive red meat consumption may increase risk.
Smoking: Interestingly, UC is less common in smokers. Some studies suggest that smoking may have a protective effect against UC.
Hygiene hypothesis: Overly sterile environments may lead to immune system dysregulation.
4. Gut bacteria
Alterations in the diversity and composition of intestinal bacteria (dysbiosis) have been noted in UC.
A reduction in beneficial bacteria and an increase in harmful species may contribute to inflammation.
How is Ulcerative Colitis Diagnosed?
The diagnosis of UC is based on a combination of clinical evaluation, laboratory tests, imaging, and endoscopic examination with biopsy.
Laboratory Tests
Complete blood count (CBC): May show anaemia or elevated white blood cell count.
C-reactive protein (CRP) and ESR: Markers of inflammation.
Fecal calprotectin: Elevated in intestinal inflammation.
2. Endoscopy
Colonoscopy with biopsy: The gold standard. Shows continuous inflammation beginning in the rectum. Biopsies confirm mucosal inflammation and rule out infections or dysplasia.
3. Imaging
Abdominal X-rays or CT scans: To assess complications like toxic megacolon or perforation.
Types of Ulcerative Colitis
UC is classified by the extent of colonic involvement:
Ulcerative proctitis: Inflammation limited to the rectum.
Left-sided colitis: Extends from the rectum to the splenic flexure.
Pancolitis: Involves the entire colon.
Do I need treatment for UC? Will I need surgery?
The goal of treatment is to induce and maintain remission, reduce symptoms, and improve quality of life. Therapy depends on disease severity and extent.
The main objective is to suppress inflammation, assist in healing, and sustain remission for as long as possible.
Conclusion
Ulcerative colitis can be a chronic condition, but it doesn’t have to dominate your life. With early diagnosis, an appropriate treatment regimen, and frequent medical check-ups, most individuals can successfully control their symptoms and lead a good quality of life.
Knowing your body, monitoring symptoms, and steering clear of personal triggers can help minimise flare-ups. From medication to diet to surgery, regular contact with your doctor is necessary to get appropriate care at any point.
If you have symptoms of ulcerative colitis or suspect you might, consult a Ulcerative Colitis Specialist at Chirag Hospitals to begin appropriate care.
Continue reading here to know more about: Ulcerative Colitis
0 notes
Text
Primary Sclerosing Cholangitis Market Size, Share and Future News by 2025-2033
The Reports and Insights, a leading market research company, has recently releases report titled “Primary Sclerosing Cholangitis Market: Global Industry Trends, Share, Size, Growth, Opportunity and Forecast 2025-2033.” The study provides a detailed analysis of the industry, including the global Primary Sclerosing Cholangitis Market share, size, trends, and growth forecasts. The report also includes competitor and regional analysis and highlights the latest advancements in the market.
Report Highlights:
How big is the Primary Sclerosing Cholangitis Market?
The global primary sclerosing cholangitis market was valued at US$ 174.9 Million in 2024 and is expected to register a CAGR of 7.8% over the forecast period and reach US$ 370.8 Million in 2033.
What are Primary Sclerosing Cholangitis?
Primary sclerosing cholangitis (PSC) is a chronic liver condition characterized by ongoing inflammation and scarring of the bile ducts, leading to their narrowing, obstruction, and subsequent liver damage. Symptoms may include jaundice, itching, abdominal pain, and fatigue. PSC is often linked to an increased risk of liver cirrhosis and liver cancer. While the precise cause remains unclear, the disease is thought to involve autoimmune mechanisms and is frequently associated with inflammatory bowel diseases like ulcerative colitis. Treatment aims to alleviate symptoms, slow disease progression, and manage complications, with liver transplantation being a potential option for advanced stages.
Request for a sample copy with detail analysis: https://www.reportsandinsights.com/sample-request/2389
What are the growth prospects and trends in the Primary Sclerosing Cholangitis industry?
The primary sclerosing cholangitis (PSC) market growth is driven by various factors and trends. The market for primary sclerosing cholangitis (PSC) is expanding due to heightened awareness of the disease, improvements in diagnostic methods, and advancements in treatment options. Increasing recognition of PSC, particularly its links to inflammatory bowel diseases, along with the growing incidence of liver complications, is boosting demand for effective therapies. Key players in the market include pharmaceutical and biotechnology companies focusing on new drug developments and clinical trials. The market is also driven by the need for improved symptom management and potential curative approaches, such as liver transplantation. Despite challenges like high treatment costs and limited available therapies, ongoing research and innovation are contributing to the market's growth. Hence, all these factors contribute to primary sclerosing cholangitis (PSC) market growth.
What is included in market segmentation?
The report has segmented the market into the following categories:
By Type
Classic PSC
Variant PSC
PSC Associated with Autoimmune Hepatitis
PSC with Cholangiocarcinoma
By Treatment Type
Ursodeoxycholic Acid
Obeticholic Acid
Methotrexate
Corticosteroids
Others
By Route of Administration
Oral
Parental
Others
By End-User
Hospital Pharmacies
Retail Pharmacies
Online Pharmacies
North America
United States
Canada
Europe
Germany
United Kingdom
France
Italy
Spain
Russia
Poland
Benelux
Nordic
Rest of Europe
Asia Pacific
China
Japan
India
South Korea
ASEAN
Australia & New Zealand
Rest of Asia Pacific
Latin America
Brazil
Mexico
Argentina
Middle East & Africa
Saudi Arabia
South Africa
United Arab Emirates
Israel
Rest of MEA
Who are the key players operating in the industry?
The report covers the major market players including:
Acorda Therapeutics, Inc.
Gilead Sciences, Inc.
NGM Biopharmaceuticals, Inc.
Intercept Pharmaceuticals, Inc.
Falk Pharma GmbH
Allergan Plc.
Shire Plc.
Durect Corporation
Conatus Pharmaceuticals, Inc.
Sirnaomics, Inc.
Shenzhen HighTide Biopharmaceutical Ltd.
Cymabay Therapeutics
Pliant Therapeutics
Immunic AG
View Full Report: https://www.reportsandinsights.com/report/Primary Sclerosing Cholangitis-market
If you require any specific information that is not covered currently within the scope of the report, we will provide the same as a part of the customization.
About Us:
Reports and Insights consistently mееt international benchmarks in the market research industry and maintain a kееn focus on providing only the highest quality of reports and analysis outlooks across markets, industries, domains, sectors, and verticals. We have bееn catering to varying market nееds and do not compromise on quality and research efforts in our objective to deliver only the very best to our clients globally.
Our offerings include comprehensive market intelligence in the form of research reports, production cost reports, feasibility studies, and consulting services. Our team, which includes experienced researchers and analysts from various industries, is dedicated to providing high-quality data and insights to our clientele, ranging from small and medium businesses to Fortune 1000 corporations.
Contact Us:
Reports and Insights Business Research Pvt. Ltd. 1820 Avenue M, Brooklyn, NY, 11230, United States Contact No: +1-(347)-748-1518 Email: [email protected] Website: https://www.reportsandinsights.com/ Follow us on LinkedIn: https://www.linkedin.com/company/report-and-insights/ Follow us on twitter: https://twitter.com/ReportsandInsi1
#Primary Sclerosing Cholangitis Market share#Primary Sclerosing Cholangitis Market size#Primary Sclerosing Cholangitis Market trends
0 notes
Text

THE ABBY AND REID GRAY BROADCAST IS TONIGHT AT 7PMCST/8PMEST
Tune in Friday, May 2d at 7pmCST for a live broadcast with James Myers & ABBY AND REID GRAY, Reid is a Ulcerative Colitis and Primary Sclerosing Cholangitis (PSC), Liver Patient, No Cure, Infertility and Heartbreaking Pregnancy Losses, Directed Liver Donor Transplant, Birthday of Miracle Twins, Abby as Biographical Author, Organ Donation Advocates, Abby Gray Writes.Com. Join us and hang out with Uncle Jim!
https://www.youtube.com/live/vDYIg0QQGN8?si=a-VDrnWIOk6R9Th
FACEBOOK LINK:
https://fb.me/1YKAfyqoU7RO7SP
YOU TUBE LINK :
https://www.youtube.com/live/vDYIg0QQGN8?si=RgSbpmxAZL6vaG-3
0 notes
Text
Comprehensive Guide to Liver Diseases: Causes, Symptoms, and Treatment
Comprehensive Guide to Liver Diseases: Causes, Symptoms, and Treatment
16th World Digestive and Liver Diseases Conference from December 17-19,2025 in Dubai, UAE
Introduction
The liver is one of the most vital organs in the human body, responsible for numerous essential functions, including detoxification, protein synthesis, and digestion. However, liver diseases have become a growing global health concern, affecting millions of people every year. Understanding the causes, symptoms, and available treatments for liver diseases is crucial for early detection and effective management.
The 16th World Digestive and Liver Diseases Conference serves as a key platform for medical professionals, researchers, and healthcare providers to discuss the latest advancements and challenges in diagnosing and treating liver diseases. This guide explores the most common liver diseases, their underlying causes, symptoms, and available treatment options.
What is Liver Disease?
Liver disease refers to any condition that negatively impacts the liver's function and health. The liver plays a vital role in processing nutrients, filtering toxins from the blood, and aiding digestion. Damage to the liver can be caused by infections, autoimmune disorders, metabolic issues, genetic predisposition, and lifestyle factors such as alcohol consumption and poor diet.
Types of Liver Diseases
Liver diseases can be categorized into several major types:
1. Hepatitis
Hepatitis is inflammation of the liver, often caused by viral infections (Hepatitis A, B, C, D, and E).
Hepatitis A – Spread through contaminated food and water.
Hepatitis B – Transmitted through blood, semen, and other bodily fluids.
Hepatitis C – Primarily spread through blood contact (e.g., shared needles).
Hepatitis D – Only occurs in individuals with Hepatitis B.
Hepatitis E – Spread through contaminated water.
2. Fatty Liver Disease
Fatty liver disease occurs when excess fat builds up in the liver. It can be:
Non-Alcoholic Fatty Liver Disease (NAFLD): Associated with obesity, diabetes, and poor diet.
Alcoholic Fatty Liver Disease: Caused by excessive alcohol consumption.
3. Cirrhosis
Cirrhosis is the result of long-term damage to the liver, causing scarring (fibrosis). It can lead to liver failure if untreated. Common causes include chronic alcohol abuse, hepatitis, and fatty liver disease.
4. Liver Cancer
Hepatocellular carcinoma (HCC) is the most common type of liver cancer. It is often linked to hepatitis infection, cirrhosis, and long-term alcohol abuse.
5. Autoimmune Liver Diseases
In autoimmune liver diseases, the body’s immune system mistakenly attacks healthy liver cells. Examples include:
Autoimmune Hepatitis
Primary Biliary Cholangitis (PBC)
Primary Sclerosing Cholangitis (PSC)
6. Genetic Liver Diseases
Inherited liver diseases result from genetic mutations. Examples include:
Hemochromatosis – Excess iron accumulation in the liver.
Wilson’s Disease – Excess copper buildup in the liver.
Causes of Liver Diseases
The underlying causes of liver diseases can vary depending on the type of disease. The most common causes include: ✅ Viral Infections – Hepatitis viruses (A, B, C, D, E). ✅ Alcohol and Substance Abuse – Excessive alcohol consumption damages liver cells. ✅ Poor Diet and Obesity – High-fat, high-sugar diets contribute to fatty liver disease. ✅ Genetic Disorders – Inherited metabolic issues such as hemochromatosis. ✅ Autoimmune Disorders – The immune system attacking liver tissue. ✅ Toxins and Medications – Long-term exposure to certain medications and chemicals.
Symptoms of Liver Diseases
Symptoms of liver disease often appear gradually and may vary based on the type and severity of the condition. Common signs include:
Fatigue and Weakness
Jaundice (Yellowing of the Skin and Eyes)
Abdominal Pain and Swelling
Dark Urine and Pale Stools
Unexplained Weight Loss
Nausea and Vomiting
Itchy Skin
Diagnosis of Liver Diseases
To diagnose liver disease, healthcare providers may use a combination of the following: ✔️ Blood Tests – Liver function tests (LFT) to check enzyme levels and overall liver health. ✔️ Imaging Tests – Ultrasound, CT scan, or MRI to detect abnormalities. ✔️ Liver Biopsy – A sample of liver tissue is examined under a microscope. ✔️ FibroScan – A specialized ultrasound that measures liver stiffness (indicating fibrosis).
Treatment Options for Liver Diseases
The treatment for liver disease depends on the type, severity, and underlying cause.
1. Medications
Antiviral medications for hepatitis B and C.
Immunosuppressive drugs for autoimmune liver diseases.
Chelation therapy for Wilson’s disease and hemochromatosis.
2. Lifestyle Modifications
Maintaining a healthy diet (low in fat and sugar).
Limiting alcohol consumption.
Regular exercise to reduce obesity and improve liver health.
3. Surgical and Interventional Treatments
Liver Transplant: For end-stage liver disease or liver cancer.
Tumor Removal: For localized liver cancer.
TIPS (Transjugular Intrahepatic Portosystemic Shunt): A procedure to treat portal hypertension.
Prevention of Liver Diseases
✅ Vaccination – Vaccines are available for Hepatitis A and B. ✅ Healthy Diet – A balanced diet rich in fruits, vegetables, lean proteins, and whole grains. ✅ Moderate Alcohol Consumption – Limit alcohol intake to reduce liver damage. ✅ Regular Health Checkups – Early detection through routine liver function tests. ✅ Avoid Sharing Needles – Reduces the risk of hepatitis B and C infection.
Latest Advancements in Liver Disease Management
The 16th World Digestive and Liver Diseases Conference highlights recent breakthroughs, including: 🔬 Gene Therapy – Promising research in treating genetic liver diseases. 🦠 New Antiviral Drugs – Improved treatment options for chronic hepatitis. 💉 Non-Invasive Diagnostic Tools – Enhanced imaging techniques for early diagnosis. 🌿 Regenerative Medicine – Research into stem cell therapy for liver regeneration.
Conclusion
Liver diseases are complex but manageable with early detection and proper treatment. The 16th World Digestive and Liver Diseases Conference provides an opportunity for global experts to collaborate and advance research in this critical field. By understanding the causes, symptoms, and treatment options, patients and healthcare providers can work together to improve liver health and prevent complications.
Conference Name: 16th World Digestive and Liver Diseases Conference Short Name: 16DLDUCG2025 Dates: December 17-19, 2025 Venue: Dubai, UAE Email: [email protected] Visit: https://digestive-liverdiseases.utilitarianconferences.com/ Visit CME/CPD: https://digestive-liverdiseases.utilitarianconferences.com/accreditation-registration Call for Papers: https://digestive-liverdiseases.utilitarianconferences.com/exhibitor-registration Register here: https://digestive-liverdiseases.utilitarianconferences.com/registration Exhibitor: https://digestive-liverdiseases.utilitarianconferences.com/exhibitor-registration Sponsor: https://digestive-liverdiseases.utilitarianconferences.com/sponsor-registration WhatsApp Us: +447723493307
#digestivehealth#guthealth#cirrhosis#fattyliver#gastroenterology#digestive#liverhealth#liverdisease#liverawareness#livercare
0 notes
Text
The Gallbladder and Biliary Tree: Functions, Disorders, and Treatments

The gallbladder and biliary tree play a crucial role in the digestive system, particularly in the digestion and absorption of fats. This blog provides an in-depth look at their anatomy, functions, common disorders, diagnostic methods, and treatments.
Anatomy of the Gallbladder and Biliary Tree
Gallbladder The gallbladder is a small, pear-shaped organ located beneath the liver on the right side of the abdomen. It serves as a storage reservoir for bile, a digestive fluid produced by the liver. The gallbladder measures approximately 7–10 cm in length and can hold about 30–50 ml of bile.
Biliary Tree The biliary tree is a network of ducts that transport bile from the liver to the small intestine. It includes:
Intrahepatic bile ducts – Small ducts within the liver that collect bile from liver cells.
Hepatic ducts – Right and left hepatic ducts merge to form the common hepatic duct.
Cystic duct – Connects the gallbladder to the common hepatic duct, allowing bile storage and release.
Common bile duct (CBD) – Formed by the union of the hepatic duct and cystic duct; it carries bile to the duodenum.
Pancreatic duct – Merges with the CBD at the ampulla of Vater before entering the duodenum.
Functions of the Gallbladder and Biliary Tree
Bile Storage and Concentration – The gallbladder stores and concentrates bile, releasing it when needed for digestion.
Fat Digestion – Bile emulsifies fats, making them easier for pancreatic enzymes to break down.
Excretion of Waste – Bile helps remove bilirubin (a byproduct of red blood cell breakdown) and cholesterol from the body.
Common Disorders of the Gallbladder and Biliary Tree
Gallstones (Cholelithiasis) Gallstones are solid deposits of cholesterol or bilirubin that form in the gallbladder. They may cause symptoms such as abdominal pain, nausea, and vomiting.
Cholecystitis This is inflammation of the gallbladder, often due to gallstones blocking bile flow. Symptoms include severe pain, fever, and jaundice.
Choledocholithiasis This condition occurs when gallstones pass into the common bile duct, leading to bile flow obstruction and possible infection.
Biliary Atresia A congenital disorder where bile ducts are absent or malformed, leading to bile buildup in the liver.
Primary Sclerosing Cholangitis (PSC) A chronic condition causing inflammation and scarring of bile ducts, which can lead to liver failure.
Diagnosis of Gallbladder and Biliary Disorders
Ultrasound – First-line imaging for detecting gallstones and inflammation.
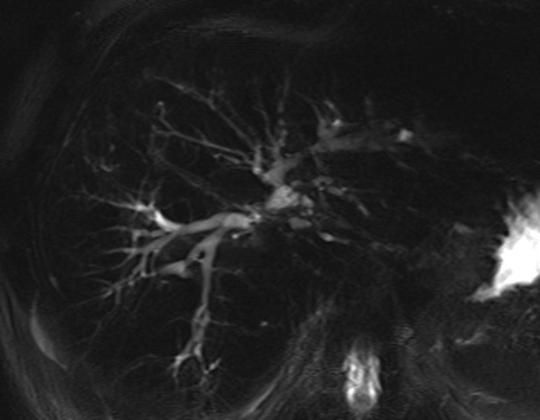
MRCP (Magnetic Resonance Cholangiopancreatography) – Provides detailed images of the biliary tree.
ERCP (Endoscopic Retrograde Cholangiopancreatography) – Used for both diagnosis and treatment of bile duct obstructions.
HIDA Scan – Evaluates gallbladder function and bile flow.
Blood Tests – Check liver function and inflammation markers.
Treatment Options
Medications
Bile acid medications (e.g., ursodeoxycholic acid) may dissolve cholesterol-based gallstones.
Antibiotics for infections like cholecystitis.
Surgical Treatments
Cholecystectomy – Surgical removal of the gallbladder, often performed laparoscopically.
Biliary Drainage – Used to relieve bile duct obstructions.
Non-Surgical Procedures
ERCP – Can remove stones and place stents to clear obstructions.
Lithotripsy – Uses shock waves to break up gallstones.
CONTACT INFORMATION:- Name:- Dr.Sachin Arora (MBBS, M.Ch Surgical Gastroenterologist) Specialist in Laparoscopic GI, HPB, and Gastrointestinal Cancer Surgery 🌐 Website: www.drsachinarora.in 📞 Contact Now: +91-7505209117 📍 Location : Sanjay Medicos, Sector 2, Maharani Bagh Ln, Ballupur Chowk, Ashirwad Enclave, Mohit Nagar, Dehradun, Uttarakhand 248001
Conclusion
The gallbladder and biliary tree are essential for digestion, but they are also susceptible to various disorders. Prompt diagnosis and appropriate treatment are crucial for managing conditions affecting these structures. If you experience persistent digestive symptoms, consult a healthcare provider for proper evaluation and treatment.
0 notes
Text
OBIT: Richard Allan Zeien
OBIT: Richard Allan Zeien
Richard Allan Zeien age 62 of New Hampton passed away surrounded by his family on Sunday, January 26, 2025 from complications of PSC (Primary Sclerosing Cholangitis) Liver Disease from ulcerative colitis. Funeral service will be held 10:30 a.m. Friday, January 31, 2025 at Hugeback-Johnson Funeral Home & Crematory in New Hampton with Rev. James Goerend presiding. Interment will follow at Calvary…
0 notes
Text
0 notes
Link
0 notes
Text
New song coming soon - I think the lyrics speak for themselves.
“Desperate Dimes”
[verse 1]
Born sick with extra fees
In debt to save the body
Christ would save you for free
They won’t do that in America baby
They’re makin dimes off your desperation
And you’ll keep your life as consolation
Paying everything you got to stay alive,
Cause you’re not worth enough for savin’
[chrous]
Well I’ve been
Livin on
borrowed time
And I got no patience left
Corrupted politicians
Are out of line
They’ll leave us all for dead
Their pockets lined
With these warning signs
Buyin votes with pretty lies
You know God won’t save the wicked
And He damn sure won’t save the rich
[verse 2]
Stay quiet, don’t dare to cry
Pay your dues to survive
I’m tired of forsaken lies
“Do everything right and you’ll be fine”
Right and wrong ain’t black and white
God they really aren’t too bright
They all got planks in their eyes
While they focus on the speck in mine
[chrous]
Well I’ve been
Livin on
borrowed time
And I got no patience left
These crooked
Politicians
Are out of their minds
They’re gonna leave us all for dead
Their pockets lined
With these warning signs
Bought your votes with pretty lies
You know God won’t save the wicked
And he damn sure won’t save the rich
[bridge]
Thoughts and prayers won’t buy my cure
Well wishes won’t heal the sick
They call this a nation of the Lord
But won’t do the least of what He did
[Chorus]
And I’m still
Livin on
borrowed time
Not a shred of patience left
Too many
Politicians
Don’t give a damn
About their citizens
Their pockets lined
With all their lies
They let the sick march to their death
You know God won’t save the wicked
And he damn sure won’t save the rich
#chronic illness#spoonie#new music#ibd#primary sclerosing cholangitis#psc#pots#potsie#spoonie problems#crohns
2 notes
·
View notes
Text
Liver Transplant in India
The Liver is one of the five Vital Organs in the human body. The Liver performs many important functions for the proper functioning of the Human Body. Any changes or abnormalities in liver tissues can affect the quality of life and may need medical treatments. Certain Medical Conditions like Cirrhosis of the Liver, primary Liver cancer, or an ill-functioning Liver may require a Liver Transplant to save the life of the patient.
What is a Liver Transplant Surgery?
A liver Transplant is a life-saving Surgery performed by a specially trained gastroenterology surgeon to replace the damaged or faulty liver in a patient with a healthy liver either from a deceased donor liver or the portion of the Liver obtained from a living liver donor. Liver Transplant Surgery is a complicated surgery and requires great expertise from gastroenterology surgeons and a proper hospital setup.
Why a Liver transplant is needed?
A liver transplant is needed when the liver tissues are damaged and the Liver is unable to perform its functions. An end-stage liver disease patient requires a Liver Transplant for survival. A liver Transplant is also indicated for the treatment of primary Liver Cancer when the cancer is localized and the tumor size is smaller. Following medical conditions may make a Gastroenterologist or Hepatologist recommend a Liver Transplant for a patient:
Liver Cirrhosis
Alcohol-induced liver damage due to chronic alcoholism
Non-alcoholic fatty liver disease
Hemochromatosis
Wilson's disease
Primary biliary Cholangitis (PBC)
Primary sclerosing cholangitis (PSC)
Biliary atresia (generally for pediatric liver patients)
Autoimmune hepatitis
Acute Liver failure
Primary Liver cancer
Types of Liver Transplants
Liver Transplants are done either with a deceased liver donor or a healthy liver donor.
Deceased Donor Liver Transplant
Orthotopic liver transplant is replacing the damaged liver in an end-stage liver disease patient with a healthy liver procured from a deceased donor.
Split liver transplants are also orthotopic liver transplants where the deceased donor's liver is split into two and transplanted into two end-stage liver disease patients. In Split liver transplant surgery, the left lateral cadaveric liver is transplanted into a child, and the right extended liver is transplanted into an adult patient.
Living Donor Liver Transplants
Living donor liver transplants are done by taking a portion of the liver from an HLA matching Liver Donor. The Donor reverts to the full functionality of the Liver within 6 weeks of liver donation and lives a perfectly normal life.
CMCS Health is a leading medical tourism company in India. We offer medical tourism services such as finding the right doctor, the right hospital, and cost estimation for medical treatment in India for foreign patients. Some of the main countries are Bangladesh, South Africa, Egypt, Kenya, Saudi Arabia, Ethiopia, Nigeria, Uganda, Zambia, Sudan, Dubai, Namibia, Iraq, and so on. We provide free medical assistance aplastic anemia treatment cost, stomach cancer treatment, sickle cell treatment cost, the best hospital for heart valve replacement, heart valve surgery, arthroscopic surgery, bone marrow transplant cost, best liver transplant hospital, brain tumor surgery cost, cosmetic andplastic surgery, heart surgery, kidney transplant cost, spine tumor surgery,cancer treatment cost, lung transplant,liver transplant cost, top knee replacement surgeons, knee replacement surgery cost, top shoulder replacement surgeons, hip replacement surgery cost, best bone marrow hospital, etc. If you are searching for free medical and healthcare consulting to find the best hospitals and top doctors and surgeons in India for any treatment then contact us- Cmcshealth.com.
Source: https://cmcshealth1.blogspot.com/2024/11/liver-transplant-in-india.html
0 notes
Text
Best Hepatologist in chennai
Dr. Magnus Jayaraj Mansard is a highly esteemed hepatologist and HPB (hepato-pancreato-biliary) surgeon in Chennai, widely recognized for his exceptional contributions to the field of hepatology. With more than a decade of dedicated practice, Dr. Mansard has established himself as one of the leading specialists in diagnosing and treating complex liver, pancreas, and biliary tract disorders. Best Hepatologist in Chennai His expertise spans various domains, including advanced laparoscopic surgeries, liver transplantations, and cutting-edge research in liver diseases.

Educational Background and Professional Achievements
Dr. Mansard's academic journey reflects his unwavering commitment to excellence. He pursued his medical degree and further specialized in HPB surgery and hepatology, gaining extensive training from some of the world's most prestigious medical institutions. His credentials include a robust portfolio of clinical and research accomplishments, positioning him as a thought leader in the domain of liver health.
In his professional career, Dr. Mansard has played a pivotal role in establishing and strengthening liver transplant and surgical hepatology units, particularly in tier-2 cities. His efforts have made advanced liver care accessible to patients from various socio-economic backgrounds, reducing the need for them to travel to metropolitan areas for specialized treatment.
Specialization and Areas of Expertise
Dr. Magnus Jayaraj Mansard specializes in a wide range of hepatology and HPB surgical procedures, including:
Liver Transplantation: As a leading expert in liver transplantation, Dr. Mansard has performed numerous successful transplants, including complex cases involving living donors. His role extends from pre-transplant evaluation to post-transplant care, ensuring comprehensive management of patients throughout their journey.
Advanced Laparoscopic Surgery: Dr. Mansard is a pioneer in minimally invasive techniques, utilizing laparoscopy for liver, pancreas, and biliary surgeries. These advanced procedures reduce recovery times, minimize complications, and improve patient outcomes.
Liver Cancer Treatment: He is adept at managing various liver cancers, including hepatocellular carcinoma (HCC) and metastatic liver cancers. Treatment approaches include surgical resections, transarterial chemoembolization (TACE), and radiofrequency ablation (RFA), tailored to the individual needs of the patient.
Hepatobiliary Diseases: His expertise extends to managing bile duct obstructions, gallbladder diseases, and pancreatitis, using a combination of surgical and non-surgical methods.
Autoimmune and Genetic Liver Disorders: Dr. Mansard has significant experience in diagnosing and treating complex autoimmune liver diseases, such as autoimmune hepatitis, primary biliary cholangitis (PBC), and primary sclerosing cholangitis (PSC). He also addresses genetic liver disorders, providing personalized treatment plans based on genetic testing and family history.
Diagnostic Excellence
One of Dr. Mansard’s hallmarks is his meticulous approach to diagnosis. He employs a variety of diagnostic tools to ensure precise identification of liver-related conditions, including:
Blood Tests: Comprehensive liver function tests (LFTs) to detect abnormalities in enzymes, bilirubin, and proteins.
Imaging Studies: High-resolution ultrasounds, CT scans, and MRIs provide detailed visualization of the liver, bile ducts, and pancreas.
Liver Biopsy: A critical diagnostic tool for evaluating the extent of liver damage and identifying conditions such as fibrosis or cirrhosis.
FibroScan: This non-invasive technology measures liver stiffness to assess fibrosis and monitor chronic liver disease progression.
Endoscopic Procedures: ERCP and endoscopic ultrasound (EUS) are employed to investigate and treat bile duct and pancreatic abnormalities.
Collaborative Approach to Patient Care
Dr. Mansard adopts a multidisciplinary approach to liver care, working closely with other healthcare professionals, including gastroenterologists, hepatobiliary surgeons, radiologists, pathologists, and nutritionists. This collaborative effort ensures comprehensive care for patients, addressing all facets of their liver health. His team-based approach is particularly crucial for patients undergoing complex procedures like liver transplantation, where coordinated care is essential for successful outcomes.
Personalized Treatment Plans
Understanding that each patient’s condition is unique, Dr. Mansard develops personalized treatment plans that consider individual medical histories, disease severity, and patient preferences. His holistic approach involves:
Medications: Prescribing antivirals for hepatitis, immunosuppressants for autoimmune conditions, and other targeted therapies.
Lifestyle Modifications: Offering guidance on diet, exercise, and alcohol consumption to manage and prevent liver diseases.
Surgical Interventions: Employing minimally invasive or open surgical techniques as required by the patient’s condition.
Supportive Care: Addressing symptoms such as fatigue, itching, or nutritional deficiencies to improve overall quality of life.
Patient-Centric Philosophy
Dr. Mansard’s patient-centric philosophy emphasizes compassionate care and clear communication. He takes the time to educate patients about their conditions, treatment options, and expected outcomes, empowering them to make informed decisions about their health. His dedication to building trust and fostering a positive doctor-patient relationship has earned him widespread respect and gratitude from his patients.
Contributions to Medical Research and Education
Beyond clinical practice, Dr. Mansard is actively involved in medical research, contributing to advancements in hepatology and HPB surgery. He has published numerous research articles in peer-reviewed journals, focusing on innovative treatment modalities and improving surgical outcomes. His work has been instrumental in shaping best practices and setting new benchmarks in liver care.
Dr. Mansard is also a passionate educator and mentor, training the next generation of hepatologists and surgeons. He regularly conducts workshops, seminars, and lectures, sharing his knowledge and expertise with medical professionals across the country.
Recognition and Awards
Dr. Magnus Jayaraj Mansard’s contributions to hepatology and HPB surgery have earned him numerous accolades. His reputation as a leading hepatologist in Chennai is bolstered by glowing testimonials from patients and peers alike. He is frequently invited to speak at national and international conferences, further establishing his prominence in the field.
Why Choose Dr. Magnus Jayaraj Mansard?
Choosing Dr. Mansard as your hepatologist ensures access to top-tier medical care backed by years of experience and a proven track record. Patients benefit from his:
Comprehensive Expertise: Proficient in managing a broad spectrum of liver diseases and performing advanced surgical procedures.
Innovative Techniques: Use of state-of-the-art technology and minimally invasive methods for diagnosis and treatment.
Patient-Centered Approach: Commitment to personalized care, ensuring the best possible outcomes for every patient.
Collaborative Care: Seamless coordination with a multidisciplinary team for holistic management of complex liver conditions.
Conclusion
Dr. Magnus Jayaraj Mansard stands out as one of the best hepatologists in Chennai, offering unparalleled expertise in liver care. His dedication to advancing the field of hepatology and improving patient outcomes makes him a trusted choice for individuals seeking specialized care for liver diseases. With his extensive experience, innovative approach, and compassionate care, Dr. Mansard continues to transform the lives of his patients, ensuring they receive the best possible treatment and support. For more details visit https://drmagnusjayaraj.com/gastrointestinal-cancer-treatment-in-chennai/
0 notes
Text
The Hidden Dangers of Bile Duct Diseases and Cirrhosis: Protecting Your Liver Health

Our liver, a resilient and vital organ, often works tirelessly in the background, performing numerous essential functions. However, certain conditions can severely impact its health and functionality. Among these are bile duct diseases and cirrhosis, both of which can lead to significant complications if not properly managed. This blog aims to shed light on these conditions, their symptoms, and their treatments.
What Are Bile Duct Diseases?
The bile ducts are a network of tubes that carry bile from the liver to the gallbladder and the small intestine. Bile is crucial for the digestion of fats. When these ducts are compromised, it can lead to serious health issues. Here are some common bile duct diseases:
Primary Biliary Cholangitis (PBC):
What It Is: PBC is an autoimmune condition where the body's immune system attacks the bile ducts within the liver.
Symptoms: Patients often experience fatigue, itching, and jaundice (yellowing of the skin and eyes).
Diagnosis and Treatment: Diagnosed through blood tests for specific antibodies, liver function tests, and imaging studies. Treatment includes medications like ursodeoxycholic acid (UDCA) and obeticholic acid. In severe cases, a liver transplant may be necessary.
Primary Sclerosing Cholangitis (PSC):
What It Is: PSC involves chronic inflammation and scarring of the bile ducts, causing them to narrow.
Symptoms: This condition leads to fatigue, itching, jaundice, and abdominal pain.
Diagnosis and Treatment: Diagnosed through MRCP (magnetic resonance cholangiopancreatography) and ERCP (endoscopic retrograde cholangiopancreatography). Treatment focuses on symptom management, endoscopic procedures to open blocked ducts, and potentially liver transplant.
Biliary Atresia:
What It Is: A congenital condition where the bile ducts are absent or blocked.
Symptoms: Jaundice in newborns, dark urine, pale stools, and poor growth are common signs.
Diagnosis and Treatment: Blood tests, liver biopsy, and imaging studies are used for diagnosis. Surgery (Kasai procedure) is the primary treatment, with liver transplant being necessary in some cases.
Cholangitis:
What It Is: Infection of the bile ducts, often due to gallstone obstruction.
Symptoms: This includes fever, jaundice, and abdominal pain, known collectively as Charcot’s triad.
Diagnosis and Treatment: Diagnosed through blood tests, imaging, and ERCP. Treatment involves antibiotics and procedures to relieve the obstruction.
What is Cirrhosis?
Cirrhosis is the end result of long-term, continuous damage to the liver, leading to permanent scarring (fibrosis). It can result from various liver diseases, including bile duct diseases.

Causes of Cirrhosis
Chronic Alcohol Abuse: Prolonged alcohol consumption can severely damage liver cells, leading to cirrhosis.
Chronic Viral Hepatitis: Hepatitis B and C infections are major contributors.
Non-Alcoholic Steatohepatitis (NASH): Fat accumulation in the liver that causes inflammation and scarring.
Bile Duct Diseases: Conditions like PBC and PSC, which chronically obstruct bile flow, can also lead to cirrhosis.
Symptoms of Cirrhosis
Fatigue and weakness
Jaundice (yellowing of the skin and eyes)
Easy bruising and bleeding
Ascites (fluid accumulation in the abdomen)
Swelling in the legs
Itching
Hepatic encephalopathy (confusion and cognitive impairment)
Diagnosis of Cirrhosis
Physical Examination: Signs of liver disease include jaundice, spider angiomas, and ascites.
Blood Tests: Liver function tests, complete blood count, and clotting profile.
Imaging Studies: Ultrasound, CT scan, or MRI to assess liver size, structure, and complications.
Liver Biopsy: A definitive method to diagnose cirrhosis and assess its severity.
Treatment of Cirrhosis
Medications: To manage symptoms and complications, such as diuretics for ascites and lactulose for hepatic encephalopathy.
Lifestyle Changes: Avoidance of alcohol, a healthy diet, and regular monitoring.
Management of Complications: Endoscopic procedures for varices, paracentesis for ascites, and antibiotics for infections.
Liver Transplant: Considered in advanced cases where the liver is severely damaged.
The Connection Between Bile Duct Diseases and Cirrhosis
Bile duct diseases like PBC and PSC can lead to cirrhosis by causing chronic inflammation and bile flow obstruction. Over time, this chronic damage results in liver scarring, ultimately leading to cirrhosis. Effective management of bile duct diseases is crucial to prevent or delay the onset of cirrhosis.
Conclusion
Bile duct diseases and cirrhosis are complex conditions that require careful medical management. Early diagnosis and treatment are essential to prevent progression and complications. Regular monitoring and a multidisciplinary approach involving hepatologists, gastroenterologists, and other healthcare professionals are key to optimal patient care.
Understanding these conditions and their implications can empower individuals to seek timely medical attention and make informed decisions about their health. Stay proactive about liver health, and consult healthcare providers if you notice any concerning symptoms.
Important Information:
Conference Name: 14th World Gastroenterology, IBD & Hepatology Conference Short Name: 14GHUCG2024 Dates: December 17-19, 2024 Venue: Dubai, UAE Email: [email protected] Visit: https://gastroenterology.universeconferences.com/ Call for Papers: https://gastroenterology.universeconferences.com/submit-abstract/ Register here: https://gastroenterology.universeconferences.com/registration/ Exhibitor/Sponsor: https://gastroenterology.universeconferences.com/exhibit-sponsor-opportunities/ Call Us: +12073070027 WhatsApp Us: +442033222718
0 notes
Text

TRIGGERS BEHIND CBD STRICTURE 💡 1. Autoimmune Disorders (e.g., IgG4 Disease) 🛡️ 2. Postoperative Complications (following Gall Bladder Removal) 🏥 3. Infectious Causes 🦠 4. Malignancies (such as Gall Bladder, Bile Duct, or Pancreatic Cancer) 🩺 5. Tuberculosis Infection 🦠 6. Chronic Pancreatitis 🫁 7. HIV Infection 🌐 8. Effects Post-Liver Transplantation 🩺 9. Primary Sclerosing Cholangitis (PSC) 🔍
Meet Dr. Hitendra K. Garg DM (GASTROENTEROLOGY), MD(MEDICINE) Senior Consultant - Hepatology, Gastroenterology & Liver Transplant At Indraprastha Apollo Hospitals, Delhi Mathura Road, Sarita Vihar, Delhi, India, Delhi
Schedule a consultation at Indraprastha Apollo Hospitals Delhi Mathura Road, Sarita Vihar, Delhi, India, DelhiVisit www.drhitendrakgarg.com Email: [email protected]
#CBDStricture#Health#Autoimmune#GallBladder#Infections#Malignancy#Tuberculosis#Pancreatitis#HIV#LiverTransplant"#gastroenterologist#drhitendragarg#cbdstones
0 notes