#Tests and Diagnosis for Diarrhea
Explore tagged Tumblr posts
Text
**EMERGENCY**
Saba, the infant daughter of a friend of mine, is critically ill in Gaza. She was born during the ongoing invasion, and has been plagued with health problems from birth. She is malnourished, and has been suffering from severe, constant diarrhea and vomiting for many weeks. My friend was able to take her to see a specialist in Gaza, who has performed special tests to be able to diagnose her. The tests are not complete yet, as testing capabilities in Gaza are minimal right now. And unfortunately, the diagnosis will probably be of limited use, as there are few to treat the condition due to the occupation’s sabotage of Gaza’s medical infrastructure.

For Saba to survive, she requires medication for her stomach problems, as well as a special diet. The cost of these things is exorbitant in Gaza due to the occupation, and Saba’s family requires direct support in order to afford the necessities that are keeping Saba alive. They have a GoFundMe to provide for their family’s needs, but it has received very little support.
Please help this baby girl survive genocide!!!
#gaza#gaza genocide#gaza strip#gaza under attack#free gaza#from the river to the sea palestine will be free#palestinian genocide#stop genocide#stop gazan genocide#stop gaza genocide#stop the genocide#save the children#save gaza#end israel's genocide#gaza under bombardment#gaza update#gaza under fire#gaza under siege#gaza under genocide#gaza relief#aid for gaza#gaza news#help gaza#relief for gaza#relief for palestine#palestine relief#gaza aid#aid for palestine#gazan families#ngu*
5K notes
·
View notes
Text
Also preserved on our archive (Daily news updates! Many can't/don't make it to Tumblr! Check it out!)
Just wanted to add a quick note: The author states that vaccination helps to prevent long covid. This is a bit of an overstatement: There is a correlation with vaccination and a small reduction in long covid diagnosis (about 30% in one study, less in others). This is a real sticking point for me, because recent studies have also shown that 1. by their own admission in surveys, doctors don't know how to diagnose long covid 2. long covid diagnosis is expensive 3. you can have long covid without a diagnosis 4. there still isn't a standard terminology or diagnostic criteria for long covid, and this has caused issue among general practitioners especially. Vaccination is best at keeping you from developing life-threatening symptoms if/when you get covid. The only way to truly prevent long covid is to not contract covid, especially if you've already been infected. Mask up. Clean the air. Avoid risky behaviors. That's real long covid prevention.
By Pandora Dewan
While nationwide COVID-19 cases have dwindled in recent weeks, wastewater detections of the virus still remain "very high" in certain states.
Newsweek have revealed this variability in a map based on data from the U.S. Centers for Disease Control and Prevention (CDC).
As of October 5, the overall viral activity level in wastewater across the country has been demoted from "moderate" to "low," although "very high" levels are still being detected in two states. A further 14 states have "high" wastewater detection levels, with seven detecting "moderate" levels and 15 classified as "low."
Eight states, including D.C., are now reporting "minimal" detection levels, the lowest classification in the CDC's system.
After a surge in COVID cases this summer, infection rates seem to be on the decline. As of October 5, positive results account for only 7.7 percent of all tests (excluding at-home testing) in the U.S., down 0.8 percent from the previous week. However, coronavirus levels do remain high in certain states, especially in the Northwest.
The map below shows which states have seen the highest detections in wastewater. (Follow the link to see the interactive map!)
Viral levels in wastewater are a helpful indicator of disease prevalence within a population.
Recent spikes in COVID cases have been largely driven by a new class of subvariants nicknamed FLiRT after the position of the mutations on the virus' spike proteins, the projections that allow them to enter our cells.
These proteins are also used as targets by immune systems and vaccinations, so changes in their structure can allow the virus to bypass the body's defenses more easily. However, existing vaccines are likely to provide at least some form of protection against more severe symptoms and long COVID.
As of October 12, the now dominant subvariant, KP.3.1.1, accounted for more than 57 percent of all U.S. COVID-19 cases over the previous two weeks, according to the CDC, with the FLiRT variants accounting for more than two thirds of cases in total.
However, while the U.S.saw a steady rise in infections over the summer, hospitalizations and deaths have remained relatively low. It appears that the new FLiRT variants, while more infectious, do not generally cause such severe symptoms.
The symptoms include the following, according to the CDC:
Fever or chills Cough Shortness of breath Fatigue Muscle or body aches Headache Loss of taste or smell Sore throat Runny nose Nausea or vomiting Diarrhea More vulnerable individuals may still be at risk of severe illness, so it is important to self-isolate if you receive a positive COVID test.

#usa news#mask up#covid#pandemic#wear a mask#public health#covid 19#wear a respirator#still coviding#coronavirus#sars cov 2
43 notes
·
View notes
Text
it's currently food allergy awareness week (may 11th-17th), and therefore, a good time to tell everyone something I wish I'd known about a decade ago, which is: if you have a lot of unexplained digestive distress, from nausea to bloating to diarrhea to anything remotely similar, it is extremely important to do food allergy testing (though I am aware that in many circumstances, this is easier said than done). many people only associate severe food allergies with either your throat closing up, a bad rash, or maybe, if they're well-informed, a dangerous drop in blood pressure — but in fact, allergies can also look like unexplained, chronic GI disease, with or without those other symptoms. lots of people also don't know that allergy onset can happen at any time, even in adulthood.
now obviously, not all mystery GI ailments are allergies (and there are non-allergenic food intolerances too, of course), and you shouldn't remove a food from your diet without evidence. but these factors lead a lot of people — including doctors! — to not suspecting allergies when they really, really should.
if a food makes your mouth itch or burn, consider looking up whether a food is "supposed" to do that. (don't be like I was until I was 16 entire years old, just wondering why people liked the "itchy flavor" of peas so much, lmao). if your GI symptoms are paired with itchiness — whether it's in your mouth, after you eat certain foods, or on your skin, around the same time you have a GI episode, that can be a strong clue (though not a guarantee) that allergies as the culprit.
and most importantly, in terms of advocating for yourself: if you're ever given a diagnosis of exclusion, like IBS — let alone waved off without a diagnosis — but your doctor hasn't even done allergy testing before arriving at that conclusion? then your doctor has failed you. any remotely competent GI specialist will test for allergies (as well as adjacent stuff, like eosinophilic esophagitis), and refer you to an allergist if necessary.
undiagnosed, unmanaged allergies can cause permanent damage to your health, to speak nothing of being potentially life-threatening — but for a supposedly "well-known" disease, a lot of doctors really don't know how to handle them. you deserve doctors who do, whether you wind up being diagnosed or just ruling something out. I frankly don't have a universally applicable experience of how to find a doctor who takes you seriously, and I'm also certainly not a medical professional — but as someone with lived experience, I can always try my best to answer questions about allergy testing, if anyone ever wants to reach out. this is, obviously, an issue very close to me, and I would like to pass on knowledge whenever I can.
15 notes
·
View notes
Text

In Baltimore City, MD: Very sweet and easy to handle stray pup found with Scabies- needs rescue ASAP - BARCS, Baltimore MD
If you can possibly find room in your home and your heart to foster this sweet boy, please email [email protected]
Mavi- 2 y/o, unaltered male, 61lbs
He might look like an older gentleman, but Mavi here is estimated to be just two years old. This sweet fella was recently found as a stray and brought to our shelter through our partnership with Animal Control. Although the shelter can be an overwhelming environment for any animal, Mavi has been friendly, easy to handle, and overall very cooperative.
Upon examination, our vets noted that Mavi has an ear infection, dermatitis, blood tinged diarrhea (Parvo SNAP test negative), and a deep skin scrape was positive for Scabies (Sarcoptic mange). He was given a dose of Bravecto, which can be used to treat Scabies, and he was also started on probiotics, dewormers, antibiotics, and an anti-inflammatory. A full medical summary can be provided upon request.
Mavi is currently on stray hold until 12/6, and due to his diagnosis and need to be isolated from other animals and people (unless PPE is worn), we are hoping to secure placement for him as soon as possible.
Please let us know if your organization can help!
Thank you,
The BARCS Rescue Team
Baltimore Animal Rescue & Care Shelter (BARCS) New Address! 2490 Giles Rd, Baltimore, MD 21225 [email protected]| (410) 396-4695
Rescue pick-up hours: Monday-Friday: 10:30 a.m.-6:30 p.m. Saturday and Sunday: 8:30 a.m.-4:30 p.m
Adoption hours: Monday-Friday: 2 p.m.-6 p.m. Saturday and Sunday: 11 a.m.-4 p.m. Baltimore Animal Rescue and Care Shelter, Inc. (BARCS) | 2490 Giles Rd | Baltimore, MD 21225 US
#dog rescue maryland#dog rescue#dog rescue baltimore maryland#doglover#cute animals#dog adoption maryland#adopt a dog#pets#fostering dogs
7 notes
·
View notes
Text
Spotting the Signs of Autoimmune Diseases Early Can Save Lives
Autoimmune diseases occur when the immune system mistakenly attacks healthy cells. These diseases can be difficult to diagnose because the symptoms often resemble other health issues. Early identification and diagnosis of these diseases can help with the management of the disease and the overall health effect on the person.
Signs You should Be Aware Of
At Hi-Tech Diagnostic Center, we try to emphasize the significance of recognizing autoimmune disease symptoms while you have the chance to catch them before they develop more serious problems. Here are some of the most common early symptoms to look out for:
1. Chronic fatigue: You felt tired even after plenty of rest.
2.Joint pain and swelling: Fingers, knees, or feet.
3.Unexplained skin rashes: Red, itchy patches or rashes, or scaly patches of skin.
4.Loss of hair: Sudden hair loss or patchy hair loss.
5.Digestive upset: Bloating, diarrhea, or stomach cramping.
6.Recurrent fevers: Low-grade fever, or low-grade fevers that persist.
7.Tingling or numbness: Often noted in hands or feet.
If you notice more than 1 or 2 of the above symptoms, you should highly consider getting medical attention.
Causational Factors That Could Trigger Autoimmune Diseases
Autoimmune diseases can affect anyone, but it is more common in women as a whole. There are a few factors that can compound your risk from very low to medium or high:
1.Genetic predisposition
2.Stress and lifestyle factors
3.Chemicals or infections that lead to exposure
4.Hormonal change, especially after giving birth
Hi-Tech Diagnostic Center provides diagnostic testing to help mitigate these triggers with early interventions.
The Importance of Early Diagnosis
Not getting a diagnosis in time can result in significant organ damage and possible complications further down the line. At Hi-Tech, we utilize the latest testing technology to provide accurate and timely diagnoses. We can deliver timely diagnosis utilizing a simple blood test to evaluate immune markers, levels of inflammation, or other indicators of autoimmune activity.
The Most Frequently Tested Autoimmune Diseases
1. Lupus (SLE) 2.Rheumatoid Arthritis (RA) 3.Type 1 Diabetes 4.Hashimoto’s Thyroiditis 5.Multiple Sclerosis (MS) 6.Psoriasis and Psoriatic Arthritis 7.Our lab professionals are knowledgeable, precise, and meticulous when handling complicated autoimmune panels.
For bookings and enquiries, please contact us at 0484 2333 888 | 944 77 123 00 or mail us at [email protected]

#health#health & fitness#health ( height and weight ) scales#health and wellness#healthy diet#healthtech#healthcare#health insurance#health tips#healthy eating
2 notes
·
View notes
Text
CNN 5/15/2025
There is a hepatitis A outbreak in LA County. Why you need to know
By Katia Hetter, CNN
Updated: 5:13 PM EDT, Thu May 15, 2025
Source: CNN
Los Angeles County is facing a community-wide outbreak of the contagious virus hepatitis A, citing a sustained increase in clinical cases and elevated virus levels detected in wastewater testing.
The county reported on May 5 that there have been 29 confirmed cases of hepatitis A this year. That number is out of a total 165 documented cases since the start of 2024, which is three times the total number of cases reported in 2023. At least seven people have died during this outbreak, according to local media.
What is hepatitis A? What symptoms does it cause? How is it diagnosed and treated? Who are the individuals most vulnerable to severe outcomes? Who should be vaccinated against the disease? And what other steps can people take to reduce their chance of contracting it?
To guide us through these questions, I spoke with CNN wellness expert Dr. Leana Wen. She is an emergency physician and clinical associate professor at the George Washington University. Wen previously served as Baltimore’s health commissioner.
CNN: What is hepatitis A?
Dr. Leana Wen: Hepatitis A is a liver disease caused by the hepatitis A virus, which is highly contagious. Most people who develop the disease will recover completely, without lasting liver damage. However, some people can become very sick — they can develop liver failure, require intensive care and die.
CNN: How is hepatitis A transmitted?
Wen: The hepatitis A virus is transmitted primarily through the fecal-oral route, meaning that someone gets it by ingesting food or water that has been contaminated with the virus from an infected person.
This type of transmission could occur with individuals living in close quarters — for instance, when an infected person prepares food for family members or when someone is caring for an infected person and doesn’t wash their hands fully before eating. Waterborne outbreaks also can happen when there is sewage contamination. Another pathway for virus transmission is through sexual contact, such as oral-anal intercourse.
CNN: What symptoms does it cause?
Wen: Symptoms of hepatitis A can include fatigue, fever, joint pain, nausea, diarrhea, dark urine or clay-colored stools and jaundice, which is yellowing of the skin or eyes. The symptoms typically resolve within two months, though some people can feel ill for as long as six months.
It’s important to note that some people with hepatitis A could be asymptomatic, which means that they could be infected without having any symptoms and pass the virus unknowingly to others. The possibility of asymptomatic transmission, along with the very long incubation period for hepatitis — people are infected for usually 14 to 28 days before they show symptoms — make controlling outbreaks challenging.
CNN: How is hepatitis A diagnosed and treated?
Wen: The diagnosis requires a blood test, which looks for the presence of a particular antibody (hepatitis A virus IGM antibody) that identifies acute infection with the hepatitis A virus. This blood test is positive two weeks before the onset of symptoms and lasts about six months after.
There is no specific treatment, antiviral or otherwise, for hepatitis A. The therapies are all supportive in nature, which means doctors will try to ease your symptoms. Individuals who are dehydrated may receive intravenous hydration. People experiencing fatigue are told to rest. The majority of cases are mild and people recovery fully. Severe cases may require hospitalization. If someone experiences the rare complication of liver failure, they may require a liver transplant.
CNN: Which people are more likely to have severe illness?
Wen: The people most likely to experience severe outcomes include older individuals and those with significant underlying medical conditions, such as chronic liver disease and immunocompromise.
CNN: Who is most likely to contract hepatitis A?
Wen: A key risk factor is visiting parts of the world where hepatitis A is common, such as Central and South Africa, eastern Europe and parts of Asia. People who may be at higher risk include those experiencing homelessness, men who have sex with men and people who use illegal drugs.
In Los Angeles County, officials have said that most of the recent cases involve individuals who do not have these specific risk factors. They don’t know what exactly is driving the outbreak; investigations are underway.
CNN: Is there a hepatitis A vaccine? Who should be vaccinated?
Wen: There are two types of hepatitis A vaccines available. One of them is a two-dose vaccine against hepatitis A. The other is a three-dose vaccine that protects against both hepatitis A and hepatitis B. The combination vaccine is only available for people 18 and older.
The US Centers for Disease Control and Prevention recommends the two-dose hepatitis A vaccine to all children ages 12 months to 23 months. The two shots are typically administered over the course of six months. The CDC recommends that children who did not receive the vaccine before 23 months still receive the two doses. No additional booster doses are recommended after initial vaccination series is completed.
Adults at increased risk of contracting hepatitis A virus as well as those at increased risk for severe disease if they were to contract the virus are also recommended to receive the vaccine. Vaccination is also recommended to people who are unvaccinated and who have been exposed to the hepatitis A virus in the preceding two weeks.
In outbreak settings, such as in Los Angeles County, unvaccinated people at higher risk for contracting the virus or for developing severe disease are recommended to receive the vaccine.
CNN: I don’t live in Los Angeles. Should I still get vaccinated?
Wen: Everyone should follow the CDC’s guidance on hepatitis A vaccinations. All children should be vaccinated as part of their routine childhood immunizations. Adults who are either at increased risk of contracting hepatitis A or at increased risk of severe disease from it should get the vaccine.
CNN: What are the side effects of the vaccine?
Wen: The hepatitis A vaccine is a safe and effective vaccine. Side effects include pain and tenderness at the site of the injection, low-grade fever, loss of appetite and nausea. They are generally mild and go away in the first two days following vaccination.
CNN: What other steps can people take to reduce their chance of contracting hepatitis A?
Wen: The best way to prevent infection is through vaccination. Individuals living in outbreak areas and others who are at high risk who have not been vaccinated should be sure to do so. Good hand hygiene can also reduce the spread of hepatitis A.
See Full Web Article
Go to the full CNN experience
© 2025 Cable News Network. A Warner Bros. Discovery Company. All Rights Reserved.
Terms of Use | Privacy Policy | Ad Choices | Do Not Sell or Share My Personal Information
2 notes
·
View notes
Text
Addison’s Disease in Pets – Causes, Symptoms, and Lifelong Care
Addison’s disease is a chronic condition that affects pets by impairing their adrenal gland function. At vets in Virginia Beach, veterinarians frequently treat dogs and cats with this hormonal disorder, which can lead to life-threatening complications if left untreated.
Recognizing the Symptoms Addison’s disease symptoms can vary but often include:
Weakness and Fatigue: Pets may seem lethargic or reluctant to play.
Digestive Issues: Vomiting, diarrhea, and reduced appetite are common.
Trembling or Shaking: In severe cases, pets may experience muscle tremors.
Causes and Risk Factors The most common cause of Addison’s disease is immune-mediated damage to the adrenal glands. Other contributing factors include:
Genetics: Certain breeds, such as Bearded Collies and Great Danes, are predisposed.
Stress Triggers: Stressful events can worsen symptoms or trigger Addisonian crises.
Diagnosis and Treatment At vets in Virginia Beach, veterinarians use blood work and ACTH stimulation tests to confirm an Addison’s diagnosis. Treatment includes:
Hormone Replacement Therapy: Pets require lifelong corticosteroid and mineralocorticoid therapy.
Emergency Care: During crises, pets may need IV fluids and electrolyte balancing.
Long-Term Management and Prevention While Addison’s disease cannot be prevented, regular veterinary checkups and consistent medication can keep symptoms under control. Pet owners should monitor for lethargy, dehydration, and changes in appetite, seeking veterinary care promptly if symptoms worsen. With ongoing management, pets with Addison’s disease can enjoy long and healthy lives.
2 notes
·
View notes
Text
The Link Between Chronic Allergies and Autoimmune Disorders in Pets
Many pet owners associate allergies with minor discomfort, but persistent allergic reactions can contribute to the onset of autoimmune diseases. At animal hospital VA Beach, veterinarians frequently diagnose pets whose prolonged allergy symptoms have triggered serious immune system complications.
How Allergies Lead to Autoimmune Issues When a pet suffers from chronic allergies, their immune system remains in a constant state of inflammation. Over time, this hyperactive response can confuse the immune system, causing it to attack healthy tissues. Autoimmune diseases linked to allergies include:
Immune-Mediated Polyarthritis (IMPA): Chronic joint inflammation due to autoimmune reactions.
Autoimmune Skin Diseases: Chronic allergies may lead to conditions like pemphigus, which causes painful skin lesions.
Inflammatory Bowel Disease (IBD): Allergic reactions to food can trigger autoimmune gastrointestinal issues.
Symptoms to Recognize Signs of autoimmune diseases include chronic diarrhea, hair loss, lameness, or unexplained fatigue. If your pet shows these symptoms, consult a veterinarian immediately.
Diagnosis and Treatment At animal hospital VA Beach, veterinarians use comprehensive testing, including allergy panels and immune function assessments, to diagnose autoimmune conditions. Treatment may involve immunosuppressive drugs, dietary modifications, and allergy management plans.
Prevention and Long-Term Care To prevent autoimmune complications, manage your pet’s allergies effectively. Use prescribed allergy medications, maintain a clean environment, and avoid common allergens. Routine veterinary checkups help detect early immune system issues, ensuring your pet receives timely care.
2 notes
·
View notes
Text
Also preserved in our archive (Daily updates!)
BY: Carmen Leitch
New studies have provided novel insights into long COVID, which continues to affect millions of people worldwide. The exact rates of the disease are hard to determine because of variations in clinical criteria, and other differences such as differing standards for who is included or excluded from a long COVID diagnosis or study. According to a July 2024 study in The Lancet, the rates of long COVID following an acute infection range from 50 to as much as 85 percent of people who were hospitalized for COVID-19 and unvaccinated; 10 to 35 percent of people who were not hospitalized and not vaccinated, and about ten percent of vaccinated people.
Scientists are still working to determine the causes of long COVID, which may vary or include several factors depending on who is affected and what their health history might be. Some research has found evidence of active infection in people with long COVID. But in that study, half of the long COVID patients did test negative for viral proteins, suggesting that there are multiple causes of the illness.
Symptoms of long COVID include but are not limited to: fatigue, fever, malaise, coughing, chest pain, headaches, sleep problrms, anxiety, diarrhea or constipation, joint pain, and rash. Long term complications may include increased risk of diabetes, blood clots, and heart problems.
A 2022 study reported in Nature Medicine determined that heart dysfunction could be one reason for the symptoms of long COVID, even after a mild infection.
A recent report published in Nature Microbiology has shown that there were abnormally high levels of inflammatory signaling molecules called cytokines in patients with long COVID.
The scientists found that these cytokines could damage heart calls called cardiomyocytes. Since these cells are responsible for the pumping action of the heart, problems with those cells may help explain long COVID symptoms like chest pain and heart palpitations. A heart condition known as POTS (postural orthostatic tachycardia syndrome) has also been associated with long COVID.
Unrelated, recent work reported in the Journal of Autoimmunity and Frontiers in Immunology, has discovered two proteins that could serve as biomarkers for long COVID, and may help explain the mechanisms underlying some cases of the disease. This work showed that people with long COVID carry abnormally high levels of proteins called galectin-9 and artemin in their blood.
These patients also had unusually high levels of certain immune cells known as neutrophils and monocytes, which may cause inflammation. There were also abnormally high levels of killer T cells that were exhausted. Long COVID patients were also deficient in immune cells that can fight infection, called lymphocytes. The researchers noted that neutrophils that are under stress often release galactin-9, which can boost inflammation.
Another recent study from this group, reported in The Lancet Microbe found no evidence of persistent infection in long COVID patients, challenging studies that have found the opposite and highlighting the complexities and sometimes confounding nature of this highly variable disorder.
Studies:
www.thelancet.com/journals/lancet/article/PIIS0140-6736(24)01136-X/fulltext www.clinicalmicrobiologyandinfection.com/article/S1198-743X(24)00432-4/abstract www.nature.com/articles/s41591-022-02000-0 www.nature.com/articles/s41564-024-01838-z pmc.ncbi.nlm.nih.gov/articles/PMC9287587/ www.sciencedirect.com/science/article/pii/S089684112400101X?via%3Dihub www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1443363/full www.thelancet.com/journals/lanmic/article/PIIS2666-5247(24)00280-5/fulltext
#mask up#covid#pandemic#public health#wear a mask#covid 19#wear a respirator#coronavirus#still coviding#sars cov 2#long covid#covid conscious#covid is airborne
26 notes
·
View notes
Text
We all hear about terrible doctors and how awful the med system is for the disabled…. And that is 100% true. So I feel the need to shout out how fucking perfect my nurse practitioner Ben is. His list of achievements:
-Getting me referred to a doctor and diagnosed with fibromyalgia in ONE appointment.
-figuring out my knee pain and the kind of specialized brace I would need with a thorough exam where he checked my full range of motion.
-Being the first medical professional to listen to WHY I think I might have hEDS instead of telling me no. Then proceeding to evaluate what I said, agree with me, and start the referral process for a specialist diagnosis. This has taken 4+ referrals because of how fucking weird the medical system is with who checks for hEDS. He is still going for it with me.
-Immediately agreeing to fill out my FMLA forms after I told him my pain doctor said I didn’t need it. While still in referral hell mind you. No hesitation. No questions. Just “Sure, I’ll do that for you.”
-Hearing that I was woefully misinformed on the definition of diarrhea for nearly 30 years and only laughing a little bit. Then setting me up with testing and treatment for IBS.
Seriously. Give this man a medal. He deserves it.
2 notes
·
View notes
Text
Think you might have Long Covid?
Symptoms:
General Symptoms:
Tiredness or fatigue
Symptoms that get worse after physical or mental effort
Fever
Neurological Symptoms:
Difficulty thinking or concentrating
Headache
Sleep problems
Lightheadedness
Pins-and-needles feelings
Change in smell or taste
Depression or anxiety
Digestive Symptoms:
Diarrhea
Stomach pain
Respiratory and Heart Symptoms:
Difficulty breathing or shortness of breath
Cough
Chest pain
Fast-beating or pounding heart.
Other Symptoms:
Joint or muscle pain
Rash
Changes in menstrual cycles
And more...
Routine blood tests, chest x-rays, and electrocardiograms may be normal in patients with Long COVID. The CDC describes the symptoms as similar to those reported by people with ME/CFS (myalgic encephalomyelitis/chronic fatigue syndrome) and other multi-system chronic complex diseases (msCCD).
These unexplained symptoms may be misunderstood by healthcare providers, which causes a delay in diagnosis and appropriate treatment. Patients with Long COVID may also present with single or multiple symptoms of varying severity.
There is no specific test to diagnose Long COVID, so doctors usually consider a diagnosis of Long COVID based on health history, current symptoms, and a health examination.
The National Academies of Sciences, Engineering, and Medicine have developed a case definition for Long COVID to facilitate diagnosis. They have defined Long COVID as an infection-associated chronic condition (IACC) that occurs after SARS-CoV-2 infection and is present for at least 3 months as a continuous, relapsing and remitting, or progressive disease state that affects one or more organ systems.
source
to learn more, or to support research into chronic illnesses like Long Covid, ME/CFS, Chronic Lyme Disease, and more, check out
Open Medicine Foundation (USA)
Open Medicine Foundation (Canada)
Open Medicine Foundation (Australia)
2 notes
·
View notes
Text
At Caesars Sidnai, Pimentel and his colleagues created a diagnostic blood test to diagnose IBS. While he said it’s not a definitive diagnosis, it can provide one with more than 90% certainty.
This is in part because of a rise in research showing a clear link between food poisoning and IBS — a less talked about cause of IBS and “gut health” on #guttok. Pimentel said it’s estimated that food poisoning triggers at least 60 percent of all IBS on the “diarrhea-mixed side.” In this kind of situation, a person may have gone on a trip and got food poisoning. If their bowel movements never return to normal, that’s IBS. Researchers have identified a toxin that’s responsible for that type of IBS, and antibodies that are created from the toxin.
. . .
For the other people who don’t get IBS from food poisoning, Pimentel said it could be that food sensitivities are the driver behind it. Mast cells, which are special cells that are part of the allergic system of the gut, tend to be higher in some IBS patients.
“And then some patients just have naturally sensitive guts,” he said. “That's called visceral hyperalgesia.”
4 notes
·
View notes
Text
14 Common Lung Diseases

Introduction
Lung diseases represent some of the most severe health threats globally. The rise of industrialization, environmental pollution, and tobacco usage significantly contribute to the prevalence of these diseases. This article, outlines the most common lung diseases, their symptoms, causes, and treatments.
1. Pneumonia

Pneumonia is an inflammation of the lung parenchyma caused by bacteria, viruses, fungi, or other pathogens. It poses a significant risk to the elderly, immunocompromised individuals, and those with chronic conditions but can also affect healthy individuals. Pneumonia can be classified based on the causative agent, such as bacterial pneumonia (e.g., Streptococcus pneumoniae), viral pneumonia (e.g., influenza virus), or fungal pneumonia (e.g., Pneumocystis jirovecii).
Symptoms
Fever
Cough with sputum
Chest pain
Shortness of breath
Fatigue
Sweating and shaking chills
Nausea, vomiting, or diarrhea (less common)
Diagnosis Diagnosis of pneumonia typically involves a combination of patient history, physical examination, chest X-rays, and sputum cultures. Blood tests may also be conducted to identify the causative agent.
Treatment Depending on the cause, treatments may include:
Antibiotics for bacterial pneumonia.
Antiviral medications for viral pneumonia.
Antifungal therapies for fungal pneumonia. Supportive care such as rest, fluids, and over-the-counter medications to reduce fever and manage pain can also alleviate symptoms. In severe cases, hospitalization may be required to provide intravenous antibiotics, oxygen therapy, or mechanical ventilation.
2. Bronchitis
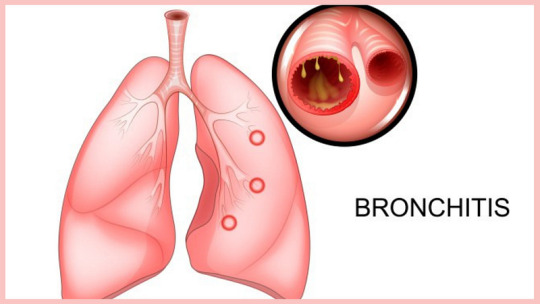
Bronchitis involves the inflammation of the bronchial tubes, which carry air to and from the lungs. It can be acute, often following colds or the flu, or chronic, usually resulting from smoking or long-term exposure to irritants like pollution or dust.
Symptoms
Persistent cough (productive or dry)
Sputum production (clear, white, yellowish-gray, or green)
Fatigue
Shortness of breath
Slight fever and chills
Chest discomfort
Diagnosis Diagnosis typically involves a physical examination, where a doctor listens to the patient’s lungs with a stethoscope. Additional tests, such as a chest X-ray, sputum tests, or pulmonary function tests, may be conducted to rule out other conditions like pneumonia or asthma.
Treatment
Acute bronchitis: Symptomatic treatment includes rest, fluids, and over-the-counter pain relievers and cough medications. Inhalers or nebulizers may be prescribed to ease breathing.
Chronic bronchitis: Management may involve bronchodilators, steroids, and pulmonary rehabilitation. Smoking cessation and avoiding lung irritants are crucial for treatment.
3. Chronic Obstructive Pulmonary Disease (COPD)
COPD is a progressive, irreversible disease characterized by chronic inflammation of the airways, primarily due to smoking, environmental pollutants, or long-term exposure to respiratory irritants. COPD includes chronic bronchitis and emphysema, conditions that often coexist and lead to airflow obstruction.
Symptoms
Chronic cough
Sputum production
Shortness of breath, especially during physical activities
Wheezing
Chest tightness
Frequent respiratory infections
Fatigue
Unintended weight loss (in advanced stages)
Diagnosis COPD is diagnosed through a combination of patient history, physical examination, and spirometry, a test that measures the amount of air a person can exhale and how quickly they can do so. Chest X-rays, CT scans, and arterial blood gas analysis may also be used.
Prevention and Treatment Preventive measures include:
Smoking cessation
Vaccinations (influenza and pneumococcal vaccines)
Reducing exposure to lung irritants
Treatments involves;
Bronchodilators to relax the muscles around the airways
Inhaled steroids to reduce airway inflammation
Pulmonary rehabilitation programs
Oxygen therapy for severe cases
Surgery (e.g., lung volume reduction surgery or lung transplant) in advanced cases
4. Lung Cancer
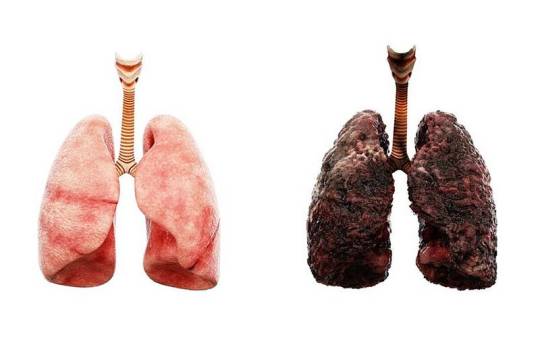
Lung cancer involves the uncontrolled growth of malignant cells in the lung tissues. Major risk factors include smoking, exposure to secondhand smoke, exposure to carcinogens (e.g., asbestos, radon), and genetic predisposition.
Types
Small cell lung cancer (SCLC): Often linked to heavy smoking, SCLC is aggressive and spreads quickly.
Non-small cell lung cancer (NSCLC): More common and includes subtypes such as adenocarcinoma, squamous cell carcinoma, and large cell carcinoma.
Symptoms
Persistent cough
Chest pain
Weight loss
Hemoptysis (coughing up blood)
Shortness of breath
Hoarseness
Bone pain (in advanced stages)
Headache (if cancer spreads to the brain)
Diagnosis Diagnosis involves imaging tests (chest X-rays, CT scans, PET scans), sputum cytology, and tissue biopsy. Molecular testing may be done to identify specific genetic mutations that can be targeted with specific treatments.
Treatment
Surgery to remove the tumor or part of the lung
Chemotherapy to kill cancer cells
Radiation therapy to destroy cancer cells or shrink tumors
Targeted drug therapies to attack specific genetic changes in cancer cells
Immunotherapy to help the immune system fight cancer
5. Pleurisy
Pleurisy, or pleuritis, is the inflammation of the pleura, the tissue lining the lungs and chest cavity. It can be caused by infections (viral, bacterial, or fungal), injuries, autoimmune diseases (e.g., lupus, rheumatoid arthritis), or other underlying conditions.
Symptoms
Sharp, stabbing chest pain that worsens with breathing, coughing, or sneezing
Shortness of breath
Cough
Fever (if infection is present)
Diagnosis Diagnosis involves a physical examination, chest X-rays, ultrasound, CT scans, and blood tests to identify the underlying cause. Thoracentesis, a procedure to remove and analyze pleural fluid, may be performed.
Treatment Treatment depends on the underlying cause and may include:
Antibiotics for bacterial infections
Antiviral medications for viral infections
Anti-inflammatory medications (e.g., NSAIDs) to reduce pain and inflammation
Pain management with medications
Thoracentesis to drain excess fluid from the pleural space
6. Pulmonary Embolism
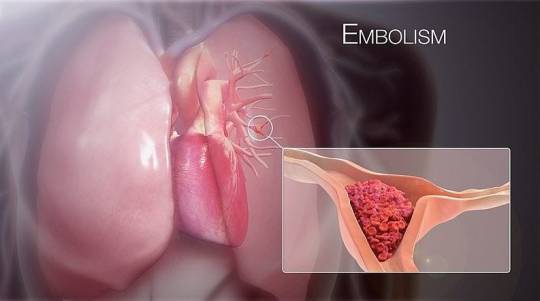
A pulmonary embolism (PE) occurs when a blood clot, usually originating in the legs (deep vein thrombosis), travels to the lungs, blocking blood flow and causing tissue damage. Risk factors include prolonged immobility, surgery, cancer, and certain genetic conditions.
Symptoms
Sudden shortness of breath
Chest pain (may be sharp and worsen with deep breathing or coughing)
Cough (sometimes with bloody sputum)
Rapid or irregular heartbeat
Lightheadedness or dizziness
Leg pain or swelling (if DVT is present)
Diagnosis: Diagnosis involves imaging tests such as chest X-rays, CT pulmonary angiography, and ventilation-perfusion (V/Q) scans. D-dimer blood tests and ultrasound of the legs may also be conducted.
Treatment Immediate treatment includes:
Anticoagulants (blood thinners) to prevent further clotting
Thrombolytics (clot-dissolving medications) for severe cases
Surgical or catheter-based procedures to remove the clot
Long-term anticoagulation therapy to prevent recurrence
7. Pulmonary Edema
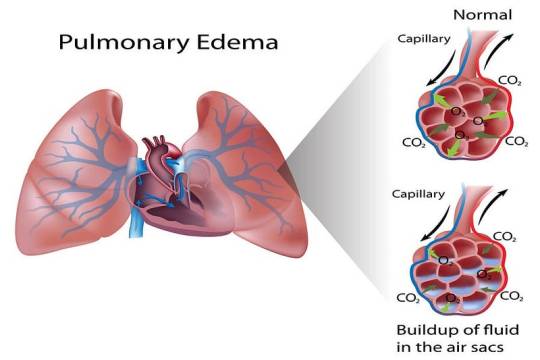
Pulmonary edema is the accumulation of fluid in the lung alveoli, making breathing difficult. It can result from heart failure (cardiogenic pulmonary edema), acute respiratory distress syndrome (ARDS), or exposure to high altitudes (non-cardiogenic pulmonary edema).
Symptoms
Difficulty breathing (dyspnea), especially when lying down
Rapid heartbeat (tachycardia)
Wheezing or gasping for breath
Coughing up frothy, pink-tinged sputum
Excessive sweating
Cyanosis (bluish skin or lips)
Diagnosis Diagnosis involves physical examination, chest X-rays, and blood tests. Echocardiography and pulmonary artery catheterization may be used to determine the underlying cause and severity.
Treatment Treatment involves addressing the underlying cause and may include:
Diuretics to remove excess fluid
Medications to improve heart function (for cardiogenic pulmonary edema)
Supplemental oxygen or mechanical ventilation
Treating underlying conditions such as infections or high altitude exposure
8. Pulmonary Fibrosis
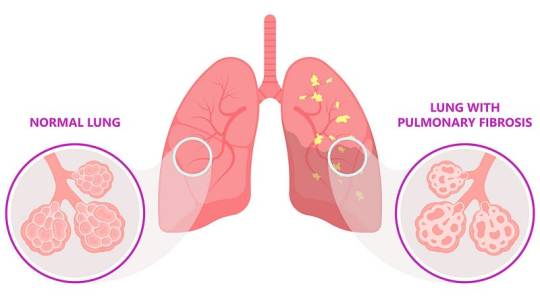
Pulmonary fibrosis is the thickening and scarring of lung tissue, leading to reduced oxygen absorption. Causes include chronic exposure to environmental pollutants, infections, genetic factors, and autoimmune diseases (e.g., scleroderma).
Symptoms
Shortness of breath (dyspnea)
Persistent dry cough
Fatigue
Unexplained weight loss
Aching muscles and joints
Clubbing (widening and rounding) of the fingertips or toes
Diagnosis Diagnosis involves a combination of patient history, physical examination, imaging tests (chest X-rays, high-resolution CT scans), pulmonary function tests, and sometimes lung biopsy. Blood tests may be used to identify underlying autoimmune diseases.
Treatment While there is no cure for pulmonary fibrosis, treatments focus on symptom management and slowing progression:
Medications such as pirfenidone and nintedanib to slow disease progression
Oxygen therapy
Pulmonary rehabilitation
Lung transplant in severe cases
9. Pneumoconiosis
Pneumoconiosis is a lung disease caused by inhaling dust particles, such as asbestos, silica, or coal dust, leading to lung scarring. It is a type of occupational lung disease commonly seen in miners, construction workers, and industrial workers.
Symptoms:
Chronic cough
Shortness of breath
Chest tightness
Progressive loss of lung function
Diagnosis: Diagnosis involves a detailed occupational history, physical examination, chest X-rays, and CT scans. Pulmonary function tests may also be conducted to assess the extent of lung damage.
Treatment Treatment includes:
Avoiding further exposure to dust
Medications to manage symptoms, such as bronchodilators and corticosteroids
Respiratory therapies
Pulmonary rehabilitation
10. Pulmonary Arterial Hypertension (PAH)
PAH is a form of high blood pressure affecting the arteries in the lungs and the right side of the heart. It can be idiopathic, familial, or associated with other conditions such as connective tissue diseases, congenital heart disease, or chronic liver disease.
Symptoms
Breathing difficulties (dyspnea), especially during physical activities
Dizziness or fainting (syncope)
Chest pain
Fatigue
Swelling in the ankles, legs, and abdomen (edema)
Cyanosis (bluish lips and skin)
Diagnosis Diagnosis involves echocardiography, right heart catheterization, chest X-rays, and CT scans. Blood tests and pulmonary function tests may also be conducted to assess lung and heart function.
Treatment Treatment strategies include:
Medications to relax blood vessels and improve blood flow, such as endothelin receptor antagonists, phosphodiesterase-5 inhibitors, and prostacyclin analogs
Diuretics to reduce fluid retention
Oxygen therapy
Anticoagulants to prevent blood clots
In severe cases, surgical procedures such as atrial septostomy or lung transplant
11. Cystic Fibrosis
Cystic fibrosis (CF) is a genetic disorder caused by mutations in the CFTR gene, leading to thick, sticky mucus buildup in the lungs and other organs. This results in frequent infections, respiratory issues, and digestive problems.
Symptoms
Persistent cough with thick mucus
Recurrent lung infections
Wheezing or shortness of breath
Poor growth and weight gain in children
Salty-tasting skin
Severe constipation
Frequent greasy, bulky stools
Diagnosis Diagnosis involves genetic testing, sweat chloride tests, and newborn screening. Pulmonary function tests, chest X-rays, and sputum cultures may also be conducted to assess lung health.
Treatment Management includes:
Medications to thin mucus, antibiotics to treat infections, and bronchodilators to open airways
Chest physiotherapy to clear mucus
Enzyme supplements and high-calorie diets to manage digestive issues
Newer therapies targeting the underlying genetic defect, such as CFTR modulators
12. Respiratory Distress Syndrome (RDS)
RDS primarily affects premature infants due to a lack of surfactant, a substance necessary to keep the lungs open and facilitate gas exchange. Risk factors include premature birth, maternal diabetes, and multiple births.
Symptoms
Rapid, shallow breathing
Grunting sounds while breathing
Nasal flaring
Chest retractions (pulling in of the chest muscles)
Cyanosis (bluish color of the skin and mucous membranes)
Diagnosis Diagnosis involves clinical assessment, chest X-rays, and blood gas analysis to measure oxygen and carbon dioxide levels. Prenatal tests can also help identify at-risk pregnancies.
Treatment Treatment includes:
Surfactant replacement therapy to improve lung function
Mechanical ventilation or continuous positive airway pressure (CPAP) to support breathing
Oxygen therapy
Supportive care such as fluids and nutrition
13. Sarcoidosis
Sarcoidosis is characterized by the growth of granulomas (small clusters of inflammatory cells) in the lungs and other organs, likely as an immune response to unknown triggers. The exact cause remains unclear, but genetic and environmental factors are believed to play a role.
Symptoms
Dry cough
Shortness of breath
Chest pain
Fatigue
Fever
Swollen lymph nodes
Skin lesions (e.g., erythema nodosum)
Diagnosis Diagnosis involves a combination of patient history, physical examination, chest X-rays, CT scans, and pulmonary function tests. Biopsy of affected tissues may be performed to confirm the presence of granulomas.
Treatment While sarcoidosis is often self-limiting and may resolve without treatment, severe cases may require:
Corticosteroids to reduce inflammation
Immunosuppressive medications (e.g., methotrexate, azathioprine)
Antimalarial drugs (e.g., hydroxychloroquine) for skin lesions
Regular monitoring and follow-up care to manage chronic cases
14. Asthma
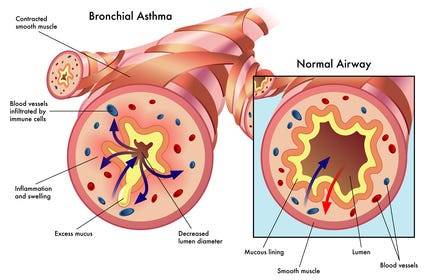
Definition and Causes: Asthma is a chronic inflammatory condition of the airways, causing episodes of wheezing, coughing, and chest tightness, often triggered by allergens, exercise, cold air, or respiratory infections. Genetic and environmental factors contribute to its development.
Symptoms
Wheezing
Shortness of breath
Chest tightness
Coughing, especially at night or early morning
Increased mucus production
Diagnosis: Diagnosis involves a detailed medical history, physical examination, and lung function tests (spirometry, peak flow measurement). Allergy testing and chest X-rays may also be conducted to identify triggers and rule out other conditions.
Treatment Management includes:
Avoiding known triggers
Inhalers (bronchodilators for quick relief, corticosteroids for long-term control)
Long-term control medications (e.g., leukotriene modifiers, long-acting beta agonists)
Immunotherapy (allergy shots) for severe allergies
Asthma action plans to manage symptoms and prevent attacks
Conclusion
Lung diseases encompass a wide range of conditions, each with distinct causes, symptoms, and treatments. Preventive measures such as avoiding smoking, reducing exposure to environmental pollutants, and timely vaccinations can significantly reduce the risk of developing many of these diseases. Early diagnosis and appropriate management are crucial in improving outcomes and quality of life for individuals affected by lung diseases. For personalized medical advice and treatment, consult with healthcare professionals.
Medical students encounter significant academic challenges during their studies, balancing coursework, clinical rotations, research, and personal commitments. Expert Academic Assignment Help offers tailored assistance to meet their needs, providing study materials, tutoring, assignment help, and exam preparation. Beyond academics, it fosters a supportive environment for mentorship and guidance. In essence, Expert Academic Assignment Help is a valuable resource for medical students, empowering them to excel academically and develop into competent healthcare professionals. Email us: [email protected] for professional guidance.
#medical students#nursing school#nursing student#assignment help#medicine#medical university#medical school#medical student#studying#studyspo#student#student life#college student#study inspiration#study blog#academic writing#writters on tumblr#online writing#do my online class
4 notes
·
View notes
Text
Wheat allergy, Celiac, and NCGS: Wait! They're not the same?

"What to expect from Wheat allergy, Celiac, and NCGS: Wait! They're not the same?" Disclaimer: None of the information provided in these posts should be taken as medical advice. Please consult with your doctor before trying recommendations or if you have concern Some posts may contain affiliate or third-party links. Okay, I said last week that I was going to cover the elimination diet this week, but I’m still researching it. Which means I’m going to cover about a topic I don’t really have to research (much) to talk about.
Meet my nemesis, Gluten
As I have mentioned before, I have several food allergies, and one of them is wheat. It happens to be one of the top nine food allergies listed in the US, but it is similar to a couple of other gluten-based issues. So this week, I’m going to talk about the differences between a wheat allergy and both celiac disease (CD) and non-celiac gluten sensitivity (NCGS or GS). Because there is a lot of confusion surrounding these gluten-based irritants, let’s take a closer look at these conditions.
Wheat allergy
A wheat allergy, like all other allergies, is an immune response. The body creates immunoglobulin (IgE) antibodies to protect the body from the usually-innocuous protein in a food. In the case of a wheat allergy, that protein is gluten, which I’ll go into more detail on in a future post. People can react differently to a wheat allergy. Some people only experience symptoms when they consume something that contains wheat. Others can react to simply breathing in wheat particles, even without eating them. Common wheat allergy symptoms include: - Anaphylaxis - Headache - Hives or skin rash - Nausea and vomiting - Runny nose, congestion or sneezing - Wheezing or asthma attack Testing for a wheat allergy follows the usual allergy testing procedures, and doctors can choose from any of the common tests to help them make a diagnosis. Our next condition, however, requires a different approach.
Celiac disease
Celiac disease is an intolerance to the wheat protein gluten as well as gluten found in barley and rye. With celiac, the body develops an auto-immune response that attacks the small intestine and damages the villi, leading to a difficulty in absorbing nutrients. It is a genetic condition often triggered by stress, trauma, and other environmental factors. Testing for CD usually involves several types of blood tests and possibly a biopsy of the small intestine. Your doctor can discuss with you what your best testing options are. Common CD symptoms include: - Bloating, gas, and constipation - Brain fog, fatigue, and headaches - Depression - Diarrhea and nausea - Joint pain - Rash (dermatitis herpetiformis) Ironically, some of these symptoms are similar to our last gluten condition, non-celiac gluten sensitivity.
Non-celiac gluten sensitivity
Symptoms in NCGS are usually more focused on digestion issue, such as bloating, constipation, diarrhea, and abdominal pain. This sensitivity is a little harder to define, largely because scientists haven’t quite figured out how it works. It isn’t an immune response (like the wheat allergy), but it also isn’t an auto-immune response (like celiac). Some scientists think it could not be related to gluten at all. One study proposes that NCGS might be a sensitivity to another protein, amylase/trypsin-inhibitors (ATIs), found in wheat, barley, and rye. Testing for it is challenging, because doctors must first rule out both a wheat allergy and celiac. If the patient tests negative for these two conditions but still reacts to gluten, the conclusion is NCGS.
Are you sure what you have isn’t celiac disease?
Short answer: maybe? The first test I had was a blood test, which isn’t as reliable as the scratch test I had two years later. The blood test checked for IgE antibodies and tissue transglutaminase IgA antibodies (tTG-IgA). All of these tests came to the same conclusion, though: I am definitely allergic to wheat. I first found out about this allergy in 2008, right before I lost a contract job and was “unemployed” and freelancing for almost two years. Talk about a bad time to have to adjust to an expensive diet. And, trust me, eating gluten free isn’t cheap, though prices are getting a little better.
Life is never simple (for me, at least)
Thankfully, my symptoms don’t include anaphylaxis, but they do include inflammation, rashes (probably from the eczema), joint pain, and digestive upset, and some of these symptoms also occur in celiac disease. Also, I react negatively digestion-wise to barley, though I can’t say for sure with rye, because all of the rye products I’ve been exposed to also include wheat (which pretty much defeats the purpose of trying to determine a potential intolerance). Since there is an allergy present, I don’t qualify for NCGS. And, though my tests don’t show it as a genetic marker, I still show some of the same symptoms as celiac. Bodies are weird, as a friend of mine says. And none seem to be more so than mine. Ah, well. That’s life. That’s all for this week. Next week I’m going to talk about what foods you can use to replace the wheat in your diet. Want to share a story about these conditions? Leave a comment below. Be safe. Eat safe. And savor life! Want to receive posts in your email? Subscribe below. Read the full article
#anaphylaxis#celiac#celiacdisease#digestion#foodallergies#foodallergy#foodintolerance#inflammation#NCGS#non-celiacglutensensitivity#swelling
2 notes
·
View notes
Text

diagnosis: freak
no but genuinely so update on little miss actual freak of nature: medical discussion of pet illness and considerations for end of life under the cut
she was doing really well up until wednesday of last week when she just tanked hard and was having diarrhea and vomiting clockwork 5 hours after every meal and stopped going for food entirely and not even the antiemetic injection was working. she started dropping all the weight she'd put on in the last two weeks.
had a quality of life discussion last night because i was straight up catastophising and was convinced that i was just keeping her alive to suffer, but when we went over the questions basically she scored a 5/10 - she's still autonomously mobile, she uses the litter box, she's still drinking on her own, etc. so the vet was like 'i wouldn't advise you to put her to sleep'. there's a specialist technician who makes the rounds of the vet clinics in the area and she was going to be in today so we planned for mo to come in, be sedated so they could do a full blood work-up and abdominal ultrasound to see the lay of the land now 8 weeks in.
so turns out her internal organs are all fine - her liver is responding really well to medication and is now all in the normal range. her kidneys are stressed, but in fairness she's been shitting and vomiting non-stop so it's probably effects of dehydration.
but her bloods? her red blood cell count is like.......so fucking low the vet was like, if she didn't know her history she would assume feline leukemia because she's like on the fucking floor. like could probably use a transfusion low. AND NO ONE KNOWS WHY. her white blood count is elevated AND WE'RE ALL JUST LIKE ????????????? WHAT IS WRONG WITH YOU?????
so they're gonna ring the lab tomorrow and pressure them for the histology results for the lymphoma test and then we'll go from there - she'll probably have to go in for sedation before the end of the week if they get a better idea of what bloods need to be done or if she needs a line put in for a transfusion but like...
the vet literally said 'i don't know she's a freak' lmaaaaooooo
AND LIKE.
YEAH.
#it's my fault i call her 'freak of nature' as a pet name and i manifested this D:#she was on my lap p much the whole time i was doing my house rewatch -- reckon she got notions#little baby mo
6 notes
·
View notes
Text
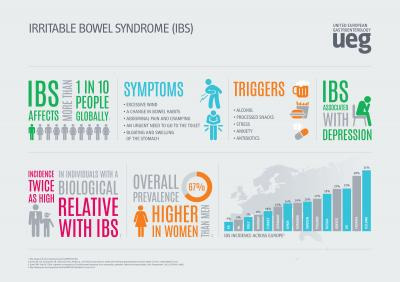
Finding Your Best IBS Treatment Plan
Irritable bowel syndrome (IBS) is a common digestive disorder estimated to affect 10-15% of the entire population. Symptoms like cramping, abdominal pain, bloating, constipation and diarrhea can range from mild to completely debilitating.
While no medical cure exists for IBS, the good news is that many effective IBS treatment options are available to significantly ease symptoms. It simply requires working with your doctor to discover the best personalized treatment plan.
Getting Properly Diagnosed
Since IBS is what’s known as a diagnosis of exclusion, the first step is to rule out the possibility of other inflammatory bowel diseases like Crohn’s or Celiac with specific testing. These may include:
Stool tests check for underlying infections or other gut issues
Blood tests look for markers of inflammation indicating disease
Colonoscopy visually examines the large intestine
Food sensitivity testing reveals if certain foods worsen symptoms
Once other conditions are ruled out, your doctor will make an official IBS diagnosis, the details of which will guide your treatment plan.
IBS Treatment Plans Depend on Type
There are four types of IBS, classified by what digestive symptoms are most prominent:
IBS with Constipation (IBS-C): Hard, infrequent stools IBS with Diarrhea (IBS-D): Frequent loose, watery stools.
IBS with Mixed Bowel Habits (IBS-M): Alternating constipation and diarrhea IBS Unspecified: Insufficient abnormality of stool consistency
Identifying your IBS type allows your doctor to select suitable therapies.
Lifestyle Treatments for IBS Relief
Certain at-home care strategies may significantly control IBS flare-ups including:
IBS Diet - Limiting intake of high FODMAP foods like dairy, beans, wheat, onions, cabbage, and artificial sweeteners can ease stool issues in 75% of IBS patients.
Stress Reduction - Stress dramatically exacerbates IBS problems, so relaxation techniques like meditation, yoga, massage are key.
More Exercise – Moderate activity at least 30 minutes daily calms the nervous system tied to digestive function.
Probiotics - These healthy gut bacteria in supplement form have been shown in studies to reduce bloating and pain.
Peppermint Oil - Shown to reduce spasms and cramping pain. Use enteric-coated capsules.
Prescription IBS Medications
If lifestyle adjustments aren’t providing enough relief, many traditional and newer medications can be very effective, including:
Antispasmodics – Helps relax intestinal muscles to reduce painful cramping and spasms
Antidiarrheals – Slows motility and stool frequency for IBS-D
Laxatives – Helps alleviate constipation with IBS-C
Low-dose Antidepressants – Alters pain signaling pathways between the brain and digestive system
Newer Agents - Prescription medications acting on neurotransmitters recently approved specifically for IBS-C and IBS-D.
Last Resort: FMT for IBS
For patients failing standard IBS treatment, research shows great promise for fecal microbiota transplantation (FMT).
This involves transplanting healthy donor stool containing balanced communities of gut bacteria into the patient’s colon via scope or enema.
Results demonstrating FMT eliminates IBS symptoms in many patients suggests disruptions to the gut microbiome play a key role in IBS development.
Finding Your Optimal Treatment Combination
Since IBS is multifactorial in cause, most experts recommend utilizing a combination approach tailored to your specific symptoms patterns.
This can mean exploring herbal supplements like peppermint capsules or artichoke leaf extract while also prioritizing daily stress-reduction practices and a modified FODMAP diet under the guidance of a registered dietician.
Your doctor may also suggest rotating various categories of medications every few months to achieve lasting relief without building tolerance.
Be patient and keep your physician informed of how you’re responding to each new IBS treatment addition or modification. It often requires tweaking strategies over several months before discovering your unique formula for success.
Hope for Life Without IBS Misery
If you feel like you’ve tried everything for your difficult-to-treat IBS with little success, don’t lose hope. The treatments options area is rapidly evolving!
Whether its emerging micobiome research showing fantastic success with FMT for stubborn IBS cases or newly approved medications targeting specific IBS symptom pathways, effective tools for relief are available.
Stay focused finding the right gastroenterologist who will personalize a therapy plan that finally quiet your symptoms for good. With a thoughtful multi-pronged approach, you can get your life back and start feeling like yourself again!
2 notes
·
View notes