#When the Estradiol Flows
Explore tagged Tumblr posts
Text
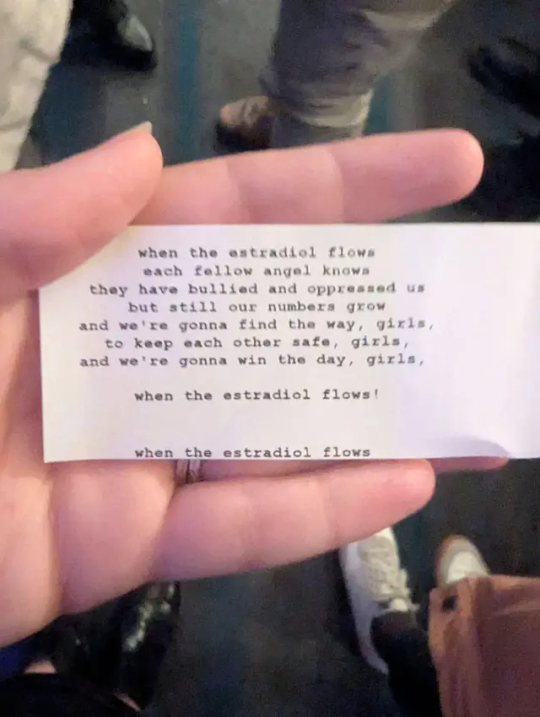
Lyrics below the cut:
Fellow angels, pay attention To what I'm gonna mention For it is the fixed intention Of the angels of the world And I hope you'll all be ready, Clear hearted, brave and steady, We'll rally round the standard, When the estradiol flows! When the estradiol flows, each fellow angel knows- They have bullied and oppressed us, but still our numbers grow And we're gonna find the way, girls, To keep each other safe, girls, And we're gonna win the day, girls When the estradiol flows! Now, these defense contractors, Have all been dirty actors, They are not our benefactors, Each fellow angel knows So we gotta stick together, In fine or dirty weather, We'll blind them with our feathers, When the estradiol flows! When the estradiol flows, each fellow angel knows- They have bullied and oppressed us, but still our numbers grow And we're gonna find the way, girls, To keep each other safe, girls, And we're gonna win the day, girls When the estradiol flows! Well the angels local 23 All place their angel hands on me, Anoint my skin in alcohol And let that plunger go It's not that I'm scared of needles, It's just my hands are feeble! And I like to have good company, When the estradiol flows! When the estradiol flows, each fellow angel knows- They have bullied and oppressed us, but still our numbers grow And we're gonna find the way, girls, To keep each other safe, girls, And we're gonna win the day, girls When the estradiol flows!
#lyrics#queer#transgender#transsexual#trans#HRT#estradiol#estrogen#Virginia#folk punk#alternative#indie#lo-fi#cover#Where the Fraser River Flows#Joe Hill#When the Estradiol Flows#Rosslyn Station#Guinevere Tully#Guinevere D. Tully#Bandcamp#alt text
6 notes
·
View notes
Text
normally i feel completely sawed off from my pretransition self a lot of the time like i just crawled into a dead body and started it shaping into me. which is fun. but as i've gotten better at the piano i've gotten to play more and more of the dream songs ive been wanting to play since long before i was me.
i'm learning beethoven's pathetique first movement. the ultra famous one.
when i was a boy (was i a boy? i don't even know if i was me) and i was in third grade, i was very emotional. in music class, i couldn't listen to the pathetique without crying. as soon as i heard it i'd just start sobbing through those first few angry chords.
of course, i was mercilessly mocked for it. a boy crying at music class? the boring thing we all sit through and tolerate and hope it's boomwhacker day so we can do something besides listening to some ancient crusty classical music that sounds like cobwebs and dust? even the teacher was a bit exhausted by how dramatic my reaction was. this wasn't a few tears. i was full on sobbing and wailing, and each new melody the song brought made it worse.
one time, he asked me why, and i told him i felt so, so horrible for beethoven, who didn't get to hear that he'd made his masterpiece. he wrote such a wonderful piece and he didn't even know. and his friend, the story went, had to turn his head towards the applause for him to even know anyone had liked it. he wrote something frustrated and despondent and named it the pathetique, and thought he was suffering through it alone.
eventually, i learned to stop crying at the song. in 7th grade, after crying my way through elementary, i cried into middle school, and the mockery got worse because i was older, and i promised myself i'd never cry again. and i lost my tears.
i'd sawed off that part of me. i didn't listen to the pathetique.
i wouldn't regain the ability to cry, at all, ever, until six years passed and i started estradiol and the boy died and i came in to pick up the strings of the body he'd tried to neglect and rot so many times.
the first thing i did, as soon as i could, was cry at little things. stories i liked and beautiful days and friends' kind words all made me sob openly. i hear bets against the void now and every single time it makes the waterworks flow.
that was me. the new me. the me now. the girl in the boy's vessel. i cried at so many new things because i was alive and i was here and i wanted to feel everything and i wanted everyone around me to know it.
when i play the pathetique, though, the memories of my heart aching for beethoven and my sobs ruining 3rd grade music class feel unlike any other memory of the thing-that-i-am-not, because they're from my point of view.
i remember him.
he was alive and he was here and he wanted to feel everything and he wanted everyone around him to know it.
i made it home. he made it home. there was a symphony in him he couldn't hear, and it came out in angry sobs and too many tears until he tried to put it away.
and then we turned our head.
40 notes
·
View notes
Text
Link to study
“In particular, just before ovulation, when the hormones 17β-estradiol and luteinizing hormone rise, the brains of the participants showed white matter changes suggesting faster information transfer.
Follicle-stimulating hormone, which rises before ovulation, and helps stimulate the ovary follicles, was associated with thicker gray matter.
Progesterone, which decreases after ovulation, was associated with increased tissue and decreased cerebrospinal fluid volume.
What this means for the person driving the brain is unknown, but the research lays the groundwork for future studies, and perhaps understanding the causes of unusual but severe period-related mental health problems.”
4 notes
·
View notes
Text
Is Ovary Size Important to Get Pregnant? Here's What You Need to Know
When it comes to getting pregnant, we often hear about hormone levels, egg quality, and uterine health. But many women—especially those actively trying to conceive—eventually ask a quieter but persistent question: Does the size of my ovaries actually matter when it comes to fertility?

It’s a great question. And the answer is—yes, to an extent. But it’s just one piece of a much bigger puzzle. Ovary size can offer clues about reproductive potential, but it’s not the sole predictor of your chances to get pregnant.
Let’s explore what ovary size really tells us, how it ties into fertility, and what can be done when things don’t seem ideal—especially with advancements like Ovarian Induction and support from fertility centers like SCI IVF Hospital.
Understanding Ovary Size: What's Considered "Normal"?
Ovaries are two small, almond-shaped glands that sit on either side of the uterus. They’re critical for reproduction, responsible for releasing eggs during ovulation and producing key hormones like estrogen and progesterone.
So what is the "normal" size?
Length: 2.5 to 5 cm
Width: 1.5 to 3 cm
Thickness: 0.6 to 2.5 cm
Volume: Typically 5 – 10 cubic centimeters (cc)
However, ovary size can naturally fluctuate with age, hormonal health, menstrual cycle phase, and even body weight.
Does Ovary Size Affect Fertility?
Here’s the honest truth: Ovary size can have an effect, but it isn’t the whole story. In many cases, it’s more about what the size suggests than the size itself.
🔹 Small Ovaries
Women with smaller-than-average ovaries may have a lower ovarian reserve—that is, fewer eggs remaining. This can be due to age, early menopause, certain genetic factors, or past medical treatments like chemotherapy.
Fertility Implication: A smaller ovary might have fewer antral follicles (tiny sacs that contain immature eggs), which can make natural conception more challenging. But here’s the hopeful news: Even women with low egg numbers can still conceive—especially if those eggs are of good quality. That’s where treatments like Ovarian Induction or IVF can make a big difference.
🔹 Normal-Sized Ovaries
This typically indicates good ovarian health, with a healthy number of follicles and hormonal balance. These are the ovaries you’d expect in a woman with a regular cycle and good fertility potential.
Fertility Implication: Normal-sized ovaries with strong blood flow and healthy follicles are ideal for both natural conception and Assisted Reproductive Technologies (ART) like IVF.
🔹 Enlarged Ovaries
Common causes include Polycystic Ovary Syndrome (PCOS) or ovarian cysts. In PCOS, ovaries may contain many small follicles that don’t mature properly, preventing ovulation.
Fertility Implication: Enlarged ovaries can make ovulation irregular or absent, complicating the timing for conception. But again, with ovulation-inducing medications and other targeted treatments, many women with PCOS go on to become pregnant successfully.
Beyond Size: What Else Matters?
While ovary size gives us a starting point, here are the real game-changers in fertility:
Ovarian Reserve: Assessed by Anti-Müllerian Hormone (AMH) levels and Antral Follicle Count (AFC). This tells us how many eggs might be available.
Egg Quality: Especially important as a woman ages. Younger eggs are typically more chromosomally normal and have better potential.
Ovulation Function: Regular, healthy ovulation is essential. This is where Ovarian Induction can come in, using medications to help stimulate the ovaries and release mature eggs.
Hormonal Balance: Hormones like FSH, LH, and estradiol must be well-regulated for the cycle to work smoothly.
Partner Factors: Don’t forget the other half—sperm health plays a major role too.
Uterine and Tubal Health: Open fallopian tubes and a receptive uterine lining are needed for implantation.
How Is Ovary Size Measured?
Typically, ovary size is evaluated through transvaginal ultrasound. This allows fertility specialists to:
Measure ovarian volume
Count antral follicles
Detect cysts or abnormalities
Monitor response during fertility treatments like Ovarian Induction
This imaging is a key part of a fertility assessment and helps guide the most effective treatment plan.
Can Women With Small or Large Ovaries Get Pregnant?
Absolutely. Ovary size doesn't define your fertility destiny.
➤ For Women With Small Ovaries or Low AMH:
Many go on to conceive using fertility treatments. Ovarian Induction, IVF, or ICSI (Intracytoplasmic Sperm Injection) may be used to retrieve mature, viable eggs—even when reserves are low.
➤ For Women With Enlarged Ovaries (Like PCOS):
Lifestyle changes, medications like metformin, and ovulation induction therapies can often restore regular ovulation. IVF is also a strong option in more complex cases.
Why Consider SCI IVF Hospital?
At SCI IVF Hospital, we take a personalized, comprehensive approach to fertility care. Whether you're facing issues with ovary size, irregular ovulation, or unexplained infertility, our team is equipped with advanced diagnostics and tailored treatment protocols to give you the best chance of success.
We specialize in fertility services including:
Ovarian Induction for women who don’t ovulate regularly
IVF and ICSI for complex fertility cases
Egg and sperm freezing
Hormonal evaluations and customized treatment protocols
Most importantly, we offer compassionate care. Every journey is unique, and at SCI IVF Hospital, we walk beside you every step of the way—offering clarity, hope, and evidence-based care.
When Should You See a Fertility Specialist?
If you’re under 35 and have been trying to conceive for over a year (or six months if you're over 35), it’s time to get expert help. Also, if you already know you have conditions like PCOS, low AMH, or irregular cycles, early consultation is your best move.
The sooner you understand your reproductive health, the more options you have.
Final Thoughts
So, is ovary size important for pregnancy? Yes—but only to a degree. It’s one of many factors that influence fertility. Whether your ovaries are small, large, or just average, today’s reproductive medicine has empowered countless women to achieve their dreams of parenthood.
With supportive care, the right diagnostics, and treatments like Ovarian Induction, you’re not alone in this journey. And clinics like SCI IVF Hospital are here to ensure that every hopeful parent gets a real chance at success.
Thank you, Tumblr, for giving us a creative space to connect with an open-minded audience and share valuable fertility insights with authenticity and heart.
0 notes
Text
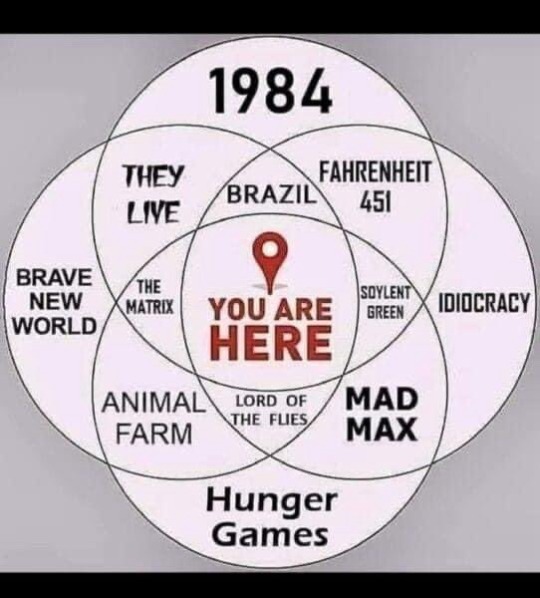
Having actually read/watched several of these, their venn diagram really demonstrates even further the kind of people who make the top graphs haven't actually read/watched that media
1984: Criticism of the USSR's and English authoritarianism (hence IngSoc - English Socialism) and a criticism of the UK censoring socialist authors (hence Ministry of Truth). There's also some fascinating social commentary about censorship in which the protagonist has a rape fantasy (as he has been raped before and is trying to process trauma) and him simply thinking about that leads to him panicking, as the act of simply thinking about something socially bad, not even performing the act, is a crime
Fahrenheit 451: Fascist society directly inspired by the Nazi book burnings (of which began by burning Jewish research about trans people, whom they considered sexual deviants, hence the pink triangle) that censors the free flow of information by destroying it
The Matrix: LITERALLY A METAPHOR FOR BEING TRANS, HENCE THE RED PILL VS. BLUE PILL LITERALLY BEING BASED ON THE PREVIOUS COLOURS FOR ESTRADIOL AND DEPRESSION MEDICATION
Soylent Green: I'm gonna level with you I probably have a surface level understanding and I'm missing deeper criticisms but as far as I can tell it's Malthusianism (the belief that the problems of humanity are caused by overpopulation and people need to be culled to control it) and the government enacts this overpopulation culling by converting the elderly and dying into food and lying about what it is to the people, albeit they do actually euthanize the elderly and dying rather, "humanely," given the circumstances (they go out of their way to make their final moments peaceful and happy)
Idiocracy: Alright in all seriousness as far as I can tell this is just conservatives assuming society becoming more progressive means everyone is becoming incredibly stupid. Very annoying movie.
Animal Farm: This book is literally a metaphor for the working class overthrowing the bourgeoisie and making the mistake of turning democratic centralism into a dictatorship, much akin to the USSR
Lord of the Flies: Without media literacy, this seems like an assumption that it's about people being inherently bad without governments, but throughout much of the book they actually form a pretty decent society and are well-organized, if a bit rude. They don't lose their shit until much later in the book when a fucking WORLD WAR PILOT CRASHES INTO THE ISLAND. It's a book about the trauma of war.
Mad Max: Blatant criticism of capitalism and ignoring climate change through the view of water wars. If you like Mad Max and want a more lewd version, I recommend Tank Girl
The Hunger Games: Probably one of the most ripped-off YA novels that acts as a blatant criticism of fascism and class systems
Haven't read/seen? the other three, so if someone has input on those have at it
10K notes
·
View notes
Text
Bioidentical Hormone Replacement Therapy: The Full-Stack Upgrade Your Endocrine System Deserves
If perimenopause felt like your body was spewing deprecation warnings, consider Bioidentical Hormone Replacement Therapy (BHRT) the clean, well-documented API that replaces those legacy calls for good. Instead of brute-forcing symptoms with quick fixes—another latte for fatigue, another blanket for the chills—BHRT rewrites the hormonal codebase so the application (you) runs smoothly again. What Makes a Hormone “Bioidentical”?Think molecular copy-paste. Plant-derived estrogen, progesterone and (sometimes) testosterone are synthesized to be chemically identical to what your ovaries used to ship in daily builds. That “bit-level” match means receptors recognize the hormone instantly, improving absorption and trimming the side-effect surface area compared with older equine or synthetic versions. The Berman clinic even notes that several FDA-approved menopause drugs now rely on these bioidentical molecules. Why Upgrade at All?The symptom backlog is impossible to ignore: hot flashes, night sweats, mood swings, vaginal dryness, brain fog and weight creep. Left untouched, chronic vasomotor misery drags down sleep, cranks up inflammation and, according to studies referenced by Dr. Berman, hikes cardiac mortality for women in their fifties by roughly 20 percent—a bigger safety net than any antioxidant supplement on the end cap. Pellets: Set-It-and-Forget-It DevOps for HormonesDaily pills and skin patches are like manual deployments—error-prone and easy to skip. Berman’s Beverly Hills office favors pellet therapy: tiny compounded cylinders slipped under the gluteal skin in a five-minute procedure. Once inserted, blood flow dictates release, keeping serum levels in a tight band for three to four months. No daily compliance, no hormone spikes, just continuous integration for your endocrine stack. Other delivery methods exist (creams, troches, injections), but pellets win on two axes: consistency and cost-per-stable-month. Because dosing is calculated from your labs and metabolism, you’re unlikely to get the “too-much-estrogen” crash that can happen with oral regimens. Who Should—and Shouldn’t—Push This Update?A quick checklist of “green-flag” issues BHRT can address: vasomotor chaos, stubborn weight gain, libido drop, memory glitches, insomnia and post-hysterectomy hormonal free fall. Contra-indications still matter. A personal or strong family history of breast or ovarian cancer, clotting disorders, untreated hypertension or active liver disease requires a different roadmap. This is why Berman’s protocol starts with a full work-up—estradiol, progesterone, thyroid panel, metabolic markers—before a single pellet is ordered. Side Effects: The Small Print You Should Actually ReadEarly in the adjustment phase you might see transient bloating, breast tenderness or a breakout worthy of your grad-school ID photo. These usually auto-resolve within a couple of cycles as the body recalibrates. hormone specialist los angeles are rare but real; ignoring them is bad DevOps. Commit to follow-up labs every six months and an annual breast exam so issues stay in staging, not production. Beyond Symptom Squashing: The Performance PerksProperly tuned BHRT isn’t just about feeling less miserable—it can be a pro-performance stack:
Cognitive clarity: Estrogen modulates neurotransmitters tied to focus and memory consolidation.
Bone density: Replaces the estrogen signal that tells osteoblasts to keep building.
Metabolic edge: Balanced testosterone and thyroid support lean-muscle retention and insulin sensitivity.
Relationship QA: When sex doesn’t hurt and desire returns, bugs in the intimacy pipeline close fast.
Implementation Advice From a Systems Thinker
Treat labs like unit tests—run them before and after any significant dose change.
Iterate, don’t set-and-forget. Most women need minor dose tweaks in the first 6–12 months.
Pair programming. Combine BHRT with resistance training, adequate protein and sleep hygiene. A single patch won’t fix spaghetti-code lifestyle habits.
Know your rollback plan. If side effects escalate, scale down swiftly rather than white-knuckling through.
Final CommitOld-school advice told women to grit their teeth through menopause. That’s like leaving Windows XP unpatched because installing updates sounds scary. Bioidentical HRT is the modern-secure option: precise, personalized and, when monitored by an expert, demonstrably safer than running outdated software. Debug the root cause, deploy the upgrade and get back to shipping great work—minus the hot-flash crash loops.
0 notes
Text
Bioidentical Hormone Replacement Therapy: The Full-Stack Upgrade Your Endocrine System Deserves
If perimenopause felt like your body was spewing deprecation warnings, consider Bioidentical Hormone Replacement Therapy (BHRT) the clean, well-documented API that replaces those legacy calls for good. Instead of brute-forcing symptoms with quick fixes—another latte for fatigue, another blanket for the chills—BHRT rewrites the hormonal codebase so the application (you) runs smoothly again. What Makes a Hormone “Bioidentical”?Think molecular copy-paste. Plant-derived estrogen, progesterone and (sometimes) testosterone are synthesized to be chemically identical to what your ovaries used to ship in daily builds. That “bit-level” match means receptors recognize the hormone specialist los angeles, improving absorption and trimming the side-effect surface area compared with older equine or synthetic versions. The Berman clinic even notes that several FDA-approved menopause drugs now rely on these bioidentical molecules. Why Upgrade at All?The symptom backlog is impossible to ignore: hot flashes, night sweats, mood swings, vaginal dryness, brain fog and weight creep. Left untouched, chronic vasomotor misery drags down sleep, cranks up inflammation and, according to studies referenced by Dr. Berman, hikes cardiac mortality for women in their fifties by roughly 20 percent—a bigger safety net than any antioxidant supplement on the end cap. Pellets: Set-It-and-Forget-It DevOps for HormonesDaily pills and skin patches are like manual deployments—error-prone and easy to skip. Berman’s Beverly Hills office favors pellet therapy: tiny compounded cylinders slipped under the gluteal skin in a five-minute procedure. Once inserted, blood flow dictates release, keeping serum levels in a tight band for three to four months. No daily compliance, no hormone spikes, just continuous integration for your endocrine stack. Other delivery methods exist (creams, troches, injections), but pellets win on two axes: consistency and cost-per-stable-month. Because dosing is calculated from your labs and metabolism, you’re unlikely to get the “too-much-estrogen” crash that can happen with oral regimens. Who Should—and Shouldn’t—Push This Update?A quick checklist of “green-flag” issues BHRT can address: vasomotor chaos, stubborn weight gain, libido drop, memory glitches, insomnia and post-hysterectomy hormonal free fall. Contra-indications still matter. A personal or strong family history of breast or ovarian cancer, clotting disorders, untreated hypertension or active liver disease requires a different roadmap. This is why Berman’s protocol starts with a full work-up—estradiol, progesterone, thyroid panel, metabolic markers—before a single pellet is ordered. Side Effects: The Small Print You Should Actually ReadEarly in the adjustment phase you might see transient bloating, breast tenderness or a breakout worthy of your grad-school ID photo. These usually auto-resolve within a couple of cycles as the body recalibrates. Serious complications are rare but real; ignoring them is bad DevOps. Commit to follow-up labs every six months and an annual breast exam so issues stay in staging, not production. Beyond Symptom Squashing: The Performance PerksProperly tuned BHRT isn’t just about feeling less miserable—it can be a pro-performance stack:
Cognitive clarity: Estrogen modulates neurotransmitters tied to focus and memory consolidation.
Bone density: Replaces the estrogen signal that tells osteoblasts to keep building.
Metabolic edge: Balanced testosterone and thyroid support lean-muscle retention and insulin sensitivity.
Relationship QA: When sex doesn’t hurt and desire returns, bugs in the intimacy pipeline close fast.
Implementation Advice From a Systems Thinker
Treat labs like unit tests—run them before and after any significant dose change.
Iterate, don’t set-and-forget. Most women need minor dose tweaks in the first 6–12 months.
Pair programming. Combine BHRT with resistance training, adequate protein and sleep hygiene. A single patch won’t fix spaghetti-code lifestyle habits.
Know your rollback plan. If side effects escalate, scale down swiftly rather than white-knuckling through.
Final CommitOld-school advice told women to grit their teeth through menopause. That’s like leaving Windows XP unpatched because installing updates sounds scary. Bioidentical HRT is the modern-secure option: precise, personalized and, when monitored by an expert, demonstrably safer than running outdated software. Debug the root cause, deploy the upgrade and get back to shipping great work—minus the hot-flash crash loops.
0 notes
Text
Bioidentical Hormone Replacement Therapy: The Full-Stack Upgrade Your Endocrine System Deserves
If perimenopause felt like your body was spewing deprecation warnings, consider Bioidentical Hormone Replacement Therapy (BHRT) the clean, well-documented API that replaces those legacy calls for good. Instead of brute-forcing symptoms with quick fixes—another latte for fatigue, another blanket for the chills—BHRT rewrites the hormonal codebase so the application (you) runs smoothly again. What Makes a Hormone “Bioidentical”?Think molecular copy-paste. Plant-derived estrogen, progesterone and (sometimes) testosterone are synthesized to be chemically identical to what your ovaries used to ship in daily builds. That “bit-level” match means receptors recognize the hormone instantly, improving absorption and trimming the side-effect surface area compared with older equine or synthetic versions. The Berman clinic even notes that several FDA-approved menopause drugs now rely on these bioidentical molecules. Why Upgrade at All?The symptom backlog is impossible to ignore: hot flashes, night sweats, mood swings, vaginal dryness, brain fog and weight creep. Left untouched, chronic vasomotor misery drags down sleep, cranks up inflammation and, according to studies referenced by Dr. Berman, hikes cardiac mortality for women in their fifties by roughly 20 percent—a bigger safety net than any antioxidant supplement on the end cap. Pellets: Set-It-and-Forget-It DevOps for HormonesDaily pills and skin patches are like manual deployments—error-prone and easy to skip. Berman’s Beverly Hills office favors pellet therapy: tiny compounded cylinders slipped under the gluteal skin in a five-minute procedure. Once inserted, blood flow dictates release, keeping serum levels in a tight band for three to four months. No daily compliance, no hormone spikes, just continuous integration for your endocrine stack. Other delivery methods exist (creams, troches, injections), but pellets win on two axes: consistency and cost-per-stable-month. Because dosing is calculated from your labs and metabolism, you’re unlikely to get the “too-much-estrogen” crash that can happen with oral regimens. Who Should—and Shouldn’t—Push This Update?A quick checklist of “green-flag” issues BHRT can address: vasomotor chaos, stubborn weight gain, libido drop, memory glitches, insomnia and post-hysterectomy hormonal free fall. Contra-indications still matter. A personal or strong family history of breast or ovarian cancer, clotting disorders, untreated hypertension or active liver disease requires a different roadmap. This is why Berman’s protocol starts with a full work-up—estradiol, progesterone, thyroid panel, metabolic markers—before a single pellet is ordered. Side Effects: The Small Print You Should Actually ReadEarly in the adjustment phase you might see transient bloating, breast tenderness or a breakout worthy of your grad-school ID photo. These usually auto-resolve within a couple of cycles as the body recalibrates. Serious complications are rare but real; ignoring them is bad DevOps. Commit to follow-up labs every six months and an annual breast exam so issues stay in staging, not production. Beyond Symptom Squashing: The Performance PerksProperly tuned BHRT isn’t just about feeling less miserable—it can be a pro-performance stack:
Cognitive clarity: Estrogen modulates neurotransmitters tied to focus and memory consolidation.
Bone density: Replaces the hrt los angeles that tells osteoblasts to keep building.
Metabolic edge: Balanced testosterone and thyroid support lean-muscle retention and insulin sensitivity.
Relationship QA: When sex doesn’t hurt and desire returns, bugs in the intimacy pipeline close fast.
Implementation Advice From a Systems Thinker
Treat labs like unit tests—run them before and after any significant dose change.
Iterate, don’t set-and-forget. Most women need minor dose tweaks in the first 6–12 months.
Pair programming. Combine BHRT with resistance training, adequate protein and sleep hygiene. A single patch won’t fix spaghetti-code lifestyle habits.
Know your rollback plan. If side effects escalate, scale down swiftly rather than white-knuckling through.
Final CommitOld-school advice told women to grit their teeth through menopause. That’s like leaving Windows XP unpatched because installing updates sounds scary. Bioidentical HRT is the modern-secure option: precise, personalized and, when monitored by an expert, demonstrably safer than running outdated software. Debug the root cause, deploy the upgrade and get back to shipping great work—minus the hot-flash crash loops.
0 notes
Text
Bioidentical Hormone Replacement Therapy: The Full-Stack Upgrade Your Endocrine System Deserves
If perimenopause felt like your body was spewing deprecation warnings, consider Bioidentical Hormone Replacement Therapy (BHRT) the clean, well-documented API that replaces those legacy calls for good. Instead of brute-forcing symptoms with quick fixes—another latte for fatigue, another blanket for the chills—BHRT rewrites the hormonal codebase so the application (you) runs smoothly again. What Makes a Hormone “Bioidentical”?Think molecular copy-paste. Plant-derived estrogen, progesterone and (sometimes) testosterone are synthesized to be chemically identical to what your ovaries used to ship in daily builds. That “bit-level” match means receptors recognize the hormone instantly, improving absorption and trimming the side-effect surface area compared with older equine or synthetic versions. The Berman clinic even notes that several FDA-approved menopause drugs now rely on these bioidentical molecules. Why Upgrade at All?The symptom backlog is impossible to ignore: hot flashes, night sweats, mood swings, vaginal dryness, brain fog and weight creep. Left untouched, chronic vasomotor misery drags down sleep, cranks up inflammation and, according to studies referenced by Dr. Berman, hikes cardiac mortality for women in their fifties by roughly 20 percent—a bigger safety net than any antioxidant supplement on the end cap. Pellets: Set-It-and-Forget-It DevOps for HormonesDaily pills and skin patches are like manual deployments—error-prone and easy to skip. Berman’s Beverly Hills office favors pellet therapy: tiny compounded cylinders slipped under the gluteal skin in a five-minute procedure. Once inserted, blood flow dictates release, keeping serum levels in a tight band for three to four months. No daily compliance, no hormone spikes, just continuous integration for your endocrine stack. Other delivery methods exist (creams, troches, injections), but pellets win on two axes: consistency and cost-per-stable-month. Because dosing is calculated from your labs and metabolism, you’re unlikely to get the “too-much-estrogen” crash that can happen with oral regimens. Who Should—and Shouldn’t—Push This Update?A quick checklist of “green-flag” issues BHRT can address: vasomotor chaos, stubborn weight gain, libido drop, memory glitches, insomnia and post-hysterectomy hormonal free fall. Contra-indications still matter. A personal or strong family history of breast or ovarian cancer, clotting disorders, untreated hypertension or active liver disease requires a different roadmap. This is why Berman’s protocol starts with a full work-up—estradiol, progesterone, thyroid panel, metabolic markers—before a single pellet is ordered. Side Effects: The Small Print You Should Actually ReadEarly in the adjustment phase you might see transient bloating, breast tenderness or a breakout worthy of your grad-school ID photo. These usually auto-resolve within a couple of cycles as the body recalibrates. Serious complications are rare but real; ignoring them is bad DevOps. Commit to follow-up labs every six months and an annual breast exam so issues stay in staging, not production. Beyond Symptom Squashing: The Performance PerksProperly tuned BHRT isn’t just about feeling less miserable—it can be a pro-performance stack:
Cognitive clarity: Estrogen modulates neurotransmitters tied to focus and memory consolidation.
Bone density: Replaces the estrogen signal that tells osteoblasts to keep building.
Metabolic edge: Balanced hrt los angeles and thyroid support lean-muscle retention and insulin sensitivity.
Relationship QA: When sex doesn’t hurt and desire returns, bugs in the intimacy pipeline close fast.
Implementation Advice From a Systems Thinker
Treat labs like unit tests—run them before and after any significant dose change.
Iterate, don’t set-and-forget. Most women need minor dose tweaks in the first 6–12 months.
Pair programming. Combine BHRT with resistance training, adequate protein and sleep hygiene. A single patch won’t fix spaghetti-code lifestyle habits.
Know your rollback plan. If side effects escalate, scale down swiftly rather than white-knuckling through.
Final CommitOld-school advice told women to grit their teeth through menopause. That’s like leaving Windows XP unpatched because installing updates sounds scary. Bioidentical HRT is the modern-secure option: precise, personalized and, when monitored by an expert, demonstrably safer than running outdated software. Debug the root cause, deploy the upgrade and get back to shipping great work—minus the hot-flash crash loops.
0 notes
Text
WHEN THE ESTRADIOL FLOWS by ROSSLYN STATION
bandcamp
0 notes
Text
Yasmin Contraceptive Pill: Empowering Women's Health Choices
Yasmin, a widely recognized contraceptive pill, stands as a pillar of modern women's health by providing effective contraception coupled with various health benefits. This article explores Yasmin's development, mechanism of action, benefits beyond contraception, considerations for use, and practical tips for maximizing its effectiveness:
Development and Innovation:
Yasmin represents a significant advancement in contraceptive technology, formulated with ethinyl estradiol (estrogen) and drospirenone (progestin). This unique combination not only ensures high contraceptive efficacy but also addresses additional health concerns faced by women.
How Yasmin Works:
Ovulation Suppression: Yasmin primarily prevents pregnancy by suppressing ovulation, ensuring that eggs are not released from the ovaries.
Cervical Mucus Modification: It thickens cervical mucus, creating a barrier that makes it difficult for sperm to reach and fertilize an egg.
Uterine Lining Adjustment: Yasmin alters the uterine lining, making it less conducive to implantation, thereby further reducing the chances of pregnancy.
Comprehensive Health Benefits:
Yasmin offers a range of benefits that extend beyond contraception, contributing to overall health and well-being:
Menstrual Cycle Regulation: Many users experience more regular menstrual cycles with reduced flow and less discomfort.
Acne Management: Approved for treating moderate acne, Yasmin helps regulate hormone levels, leading to clearer skin and improved complexion.
PMS Symptom Relief: It can alleviate symptoms of premenstrual syndrome (PMS), such as mood swings, bloating, and breast tenderness, enhancing daily comfort and quality of life.
Safety Considerations:
Usage Guidelines: Take yasmin contraceptive pill daily at the same time each day, starting either on the first day of menstruation or as directed by a healthcare provider to ensure optimal effectiveness.
Potential Side Effects: While generally well-tolerated, common side effects may include nausea, headache, breast tenderness, and mood changes. These usually diminish over time as the body adjusts to the hormonal changes.
Health Considerations: Not suitable for everyone, especially individuals with a history of blood clots, liver disease, or specific cancers. It's crucial to consult with a healthcare provider for personalized assessment and guidance.

Ensuring Effectiveness:
Consistent Use: Maintaining a regular dosing schedule is essential for maximizing Yasmin's effectiveness in preventing unintended pregnancy. Missing doses or inconsistent use can compromise its reliability.
Additional Protection: During the initial cycle or when doses are missed, using backup contraception methods such as condoms is advisable to ensure continuous protection against pregnancy.
Conclusion:
Yasmin remains a cornerstone in women's healthcare, offering a reliable contraceptive option with added benefits that enhance overall health and quality of life. Understanding its mechanism, benefits, and considerations empowers women to make informed decisions about their reproductive health journey. For personalized advice and suitability assessment, consulting with a healthcare provider is essential to ensure that Yasmin aligns with individual health needs and preferences.
0 notes
Text
Today let's talk about dryness.
When I mention I'm dry, it's not just a little bit, and it's not localized. Many folks will experience vaginal dryness with menopause; but between menopause, an extremely cold, dry winter, and the elevation at which I live, I was a human potato chip.
My solution required a multi-pronged approach.
Systemically, I drank more water. In a typical day I drink about 1200-2400ml of water, on top of tea; I increased to a minimum of 2400ml. I added in an infusion of 45/45 marshmallow and shatavari root, with an additional 10% mint and honey for flavor. I've been drinking it by the quart each day (about 950 ml).
To that, I've also been using lotion. A variety of lotions for hands, feet, body, and face; I don't have any particular preference, but because of my sensitivity to over-perfumed lotions, I've used the unscented Neutrogena Hydroboost on my face, and either Working Hands or Mane n Tail Hoofrmaker on my hands and feet. The Hoofmaker has been a great all-body lotion, because it absorbs quickly, isn't super stinky, and just works.
For soap, I've moved from using a bottle of Doc Bronners in the shower to Nivea Nourishing Body Wash, which has also helped. My hippy ways are ebbing a bit, at least on the skincare front - a true tragedy.
Lip balm has been a requisite - I've always used Burt's Bees, but now it's sort of whatever's handy when I need it.
Eye drops are a new addition to my life. I'd wake up in the morning with my eyes so dry that it hurt to open them - if I didn't roll my eyeballs around extensively first to get the tears flowing, it felt like the lids had adhered to the ball, and like I was ripping layers up. Like a good chronically-online being, I listened to the advice of Dr. Glaucomflecken and used Optase Preservative Free drops. My optometrist also recommended the Systane brand, but I haven't gotten around to trying it yet.
Finally, vaginal moisturizers. I use estradiol cream twice a week to prevent degradation of my vaginal tissues; but, in addition, now and again I use Replens when I'm feeling especially dry. It's worth noting here, at this point in my life I have the libido of a potato, so it's not a matter of being ready to go for sex, or having something that's condom-compatible (I'm fluid-bonded with my partner, anyway); it's just a matter of comfort. It's also helped alleviate some of the change in smell - that's a whole thing, for maybe another post.
And now that we're out of the coldest part of winter here (frightening in its own right that we've got 50℉ sunny days in February), staying hydrated and moisturized is a little easier than it has been. But I'm always looking for things to add to my arsenal for anti-potato-chip action - let me know if you've got something you'd add to the mess.
0 notes
Text
there's no source as concrete as the one for oral estradiol but the simulator for injectable estrogen with my dose (5mg/week injectable estradiol valerate, done IM when i did the bloodwork that yielded 990 pg/mL but now subcut) has a maximum at 380 pg/mL two days after injection. i think my appointment was maybe two days after injection but that's still wayyy higher and my go-with-the-flow gay guy gynecologist hasn't brought any of my levels up as an issue. if looking at them even piqued his interest
this chart from this transfem science article puts the average for post-gonadectomy (<- hard to spell) testosterone levels at 21.7 ng/dL. mine is according to my last labwork 21 ng/dL, down from 199 before i started E! free testosterone has gone from 6.8 to 2.8 pg/mL which I can't find a single baseline for that isn't basically an ed supplement ad but as far as I can tell it's probably insanely low even before I started E so that's fine. so basically my testosterone is more than low enough to not need an antiandrogen, i don't really have any typical (from my understanding) testosterone symptoms that i need to counteract, the only question is if i would get more out of E with it which seems unlikely because what is it doing
4 notes
·
View notes
Text
What if Juvenon BloodFlow-7 fails to work on you?
What are the symptoms of low estrogen levels?
The first thing that comes to mind when talking or reading about low estrogen levels, also known as hypoestrogenemia , is related to the physiological process of menopause. However, it is necessary to clarify certain basic terms, as well as to understand that clinical signs of hypoestrogenemia may occur without a direct relationship with menopause.
What are estrogens
They are steroid-type sex hormones. There are several types known as estrone, estriol and estradiol, with some variations in biosynthesis and function, but which are generally produced mainly at the ovarian level.
Other tissues such as the adipose, placental and adrenal glands are capable of producing estrogens in a lower proportion compared to the ovaries.
What is the role of estrogens
Estrogens participate in multiple functions, being fundamental in the reproductive aspect. They exert direct effects on the uterus at the cavity and cervical level, favoring the proliferation and growth of endometrial cells (cells that line the inside of the uterus), necessary for the implantation and maintenance of pregnancy.
Likewise, it acts at the ovarian level to favor the development of a follicle that will later ovulate, being equally necessary the adequate levels of another very important hormone that acts in conjunction with estrogens known as progesterone.
Estrogens are also capable of acting at the level of the Central Nervous System through an endocrine regulatory function of its own levels (known as feedback) and of the levels of other hormones and neurotransmitters in order to maintain a necessary balance for proper functioning. of the organism.
Estrogens are closely related to the development and generation of secondary sexual characteristics in women, such as breast and genital development, the appearance of pubic hair, changes in fat distribution, including changes related to behavior and personality once reached adolescence and early adulthood.
Likewise, it is important to note that they not only affect the reproductive system, but also estrogen levels have an influence on the cardiovascular, muscular, urinary, bone, nervous and immune systems.
Under what conditions is it possible to have low estrogen levels?
As we mentioned at the beginning of this article, not only does menopause generate a decrease in estrogen levels, which, as we already know, is a physiological or natural process.
There are also pathological situations such as early ovarian failure, which either for genetic, immunological or pathological reasons leads to the loss of ovarian activity with a drastic decrease in estrogen levels, mainly generating infertility problems.
Other pathological conditions that can damage or affect estrogen levels are neoplastic pathologies (cancer) both centrally (hypothalamic - pituitary) and gonadal, directly in the ovary, radiation being required in some cancer treatments that can damage and affect the ovarian reserve severely and with it, its endocrine and reproductive function.
The decrease in estrogen levels may be associated with some therapies. There are some medications such as those used in fertility and cancer treatment that can affect estrogen levels.
Obviously, estrogen levels also decrease in ovarian surgery, when both ovaries must be removed (surgery known as bilateral oophorectomy).
Signs of hypoestrogenemia
Just as the consecutive elevation of hormonal levels at the beginning of puberty produces different changes in the adolescent, the decrease in estrogens is also perceived by women through secondary signs and symptoms.
Among the most common are menstrual changes (irregularity in terms of days of onset of the rule as in the duration and amount of bleeding), the presence of hot flashes or hot flashes (sudden changes in the perception of temperature), emotional lability and alterations in the state of mind, decreased libido (sexual desire).
Also, it brings changes in the color of the nipples and areola, as well as a decrease in breast and genital turgor, with an equal decrease in lubrication that produces discomfort at the time of sexual intercourse, favoring prolapses (descent of pelvic organs) that are a consequence of the decrease in collagen synthesis and decrease in the resistance of the pelvic connective tissue, which secondarily generates an increase in the frequency of genital and urinary infections.
Finally, there are consequences of the decrease in estrogen levels that occur after a long period (greater than two years), such as the decrease in bone resorption (loss of bone mass or osteopenia) that can even become a a real problem when the bone is greatly weakened and is a risk factor for spontaneous fractures.
The risk of cardiovascular disease also increases due to the increase in the formation of atheroma plaques (occlusion of blood vessels), as well as the risk of cerebrovascular accidents.
Circulation, or the flow of blood throughout our bodies, is important for good health. Normal circulation promotes all of our biological systems by delivering oxygen throughout the body and helping to eliminate waste. When circulation is inadequate, or the blood does not flow vigorously, symptoms can include tired or heavy legs, cold fingers and toes as well as low energy and even dull skin. An easy way to boost circulation is with exercise. BloodFlow-7
1 note
·
View note
Link
I was casually scrolling through my Instagram feed this other day and I came across a screenshot of a twitter post by a guy that said: “A period is not an excuse to have an attitude.” Of course, me and so many other females were instantly triggered by this because very few men understand what women go through whenever it is that time of the month. However, it did get me thinking if it was the menses that gave most ladies, myself included (and no, I am not proud of this), a salty attitude, or was there an underlying reason as to why this happens. So, I did some research of my own to get an in-depth understanding of why periods give women an attitude, as well as to reach a consensus on the dictum.
Firstly, it is important for us to understand the process of menstruation and why women are supposed to go through this every month. According to Dr. Anna Druet, the menstrual period, which is commonly referred to as just a “period,” is the shedding of the uterine lining (endometrium). Blood and endometrial tissue flow down through the cervix and vagina. A period releases the tissue that grew to support a possible pregnancy. It happens after each menstrual cycle in which a pregnancy doesn’t occur—i.e. when an egg hasn’t been fertilized and/or attached itself to the uterine wall. The uterus then sheds the lining which had grown to receive a fertilized egg.
In layman`s terms, every female`s cycle uses hormonal signals as cues for what to do next. In the first part of the menstrual cycle, one of the ovaries prepares to release an egg. It also produces an increasing amount of the hormone estrogen. This estrogen helps grow and prepare the lining of the uterus (the endometrium) for a potential pregnancy (1). After one of the ovaries releases an egg (ovulation), it produces the hormone progesterone. Progesterone also helps prepare the uterus for a possible pregnancy, and keeps the endometrium “stable” in the uterus, ready to receive a fertilized egg (2). If an egg is fertilized, it then travels to the uterus over the next several days, implants in the uterine wall, and starts growing a hormone-producing placenta. If, by then, the body doesn’t receive a hormonal signal that a pregnancy is in-progress, levels of estrogen and progesterone drop. This drop in hormones prepare the endometrium to shed and triggers the production of hormone-like prostaglandins, which cause the uterus to contract, causing your period (3, 4). And the cycle starts again.
Now in response to the question of why then do women develop this attitude, this is why.
Behavioral tendencies throughout the menstrual cycle are tied to the variations in hormones that occur throughout the month. During these fluctuations, you might notice a change in mood or even your physical health. The following are the different phases of your cycle and how they can affect your well-being.
The Follicular Phase
This is most likely the “happy” part of your cycle. This phase begins when you start your period and typically lasts for about two weeks. During this time, a hormone called estradiol begins to increase. Most women feel energetic and joyful during the follicular phase, especially when comparing it to the luteal phase.
The Ovulatory Phase
During this phase, the luteinizing hormone, which will eventually induce ovulation, begins to rise. Some scientific studies have shown that women have an increase in libido and a higher pain tolerance during this phase. Women may also feel more attractive during this time as well.
The Luteal Phase
During this phase, there is an increase in the hormone progesterone. Women typically feel moodier and more stressed during this time. This phase occurs just before your period. During this luteal period, women go through what is called PMS, which is the premenstrual syndrome. This PMS is usually accompanied by symptoms such as depression and other mood changes, appetite changes, backaches, feeling bloated, headaches, irritability, insomnia, sweating, and sore breasts. This in itself is a headache and half to deal with because the cramps experienced in this phase can get so bad to the point where women spend more days in bed than doing anything productive. They cause a loss of confidence and self-consciousness that also have a negative toll on these women, hence the need to lash out and relieve their frustration. Although, on the other hand, it is not always periods that give ladies an attitude. Home-related problems, stress, frustration, and even heartbreak could be the cause, and although I don`t condone it, but sometimes that`s their coping mechanism as talking to other people doesn't hit the right spot.
So, the next time a lady who you know is on her period lashes out at you, don’t be quick to label her as a bi*ch or a snob, but instead, do what you can to help feel better during this period (pun unintended).
#LadiesWithAttitude #LWA #@_NamNam_99 #AreMensesAnExcuse? #Let'sTalkMensesWithUnamiMaphosa
4 notes
·
View notes