#hitech billing software
Explore tagged Tumblr posts
Text

#billing software#erp#software#best gst billing software#free billing software#gst billing software#billing software for retail shop#hitech billing software#restaurant billing software
0 notes
Text
Epic Systems, a lethal health record monopolist

Epic Systems makes the dominant electronic health record (EHR) system in America; if you're a doctor, chances are you are required to use it, and for every hour a doctor spends with a patient, they have to spend two hours doing clinically useless bureaucratic data-entry on an Epic EHR.
How could a product so manifestly unfit for purpose be the absolute market leader? Simple: as Robert Kuttner describes in an excellent feature in The American Prospect, Epic may be a clinical disaster, but it's a profit-generating miracle:
https://prospect.org/health/2024-10-01-epic-dystopia/
At the core of Epic's value proposition is "upcoding," a form of billing fraud that is beloved of hospital administrators, including the "nonprofit" hospitals that generate vast fortunes that are somehow not characterized as profits. Here's a particularly egregious form of upcoding: back in 2020, the Poudre Valley Hospital in Ft Collins, CO locked all its doors except the ER entrance. Every patient entering the hospital, including those receiving absolutely routine care, was therefore processed as an "emergency."
In April 2020, Caitlin Wells Salerno – a pregnant biologist – drove to Poudre Valley with normal labor pains. She walked herself up to obstetrics, declining the offer of a wheelchair, stopping only to snap a cheeky selfie. Nevertheless, the hospital recorded her normal, uncomplicated birth as a Level 5 emergency – comparable to a major heart-attack – and whacked her with a $2755 bill for emergency care:
https://pluralistic.net/2021/10/27/crossing-a-line/#zero-fucks-given
Upcoding has its origins in the Reagan revolution, when the market-worshipping cultists he'd put in charge of health care created the "Prospective Payment System," which paid a lump sum for care. The idea was to incentivize hospitals to provide efficient care, since they could keep the difference between whatever they spent getting you better and the set PPS amount that Medicare would reimburse them. Hospitals responded by inventing upcoding: a patient with controlled, long-term coronary disease who showed up with a broken leg would get coded for the coronary condition and the cast, and the hospital would pocket both lump sums:
https://pluralistic.net/2024/06/13/a-punch-in-the-guts/#hayek-pilled
The reason hospital administrators love Epic, and pay gigantic sums for systemwide software licenses, is directly connected to the two hours that doctors spent filling in Epic forms for every hour they spend treating patients. Epic collects all that extra information in order to identify potential sources of plausible upcodes, which allows hospitals to bill patients, insurers, and Medicare through the nose for routine care. Epic can automatically recode "diabetes with no complications" from a Hierarchical Condition Category code 19 (worth $894.40) as "diabetes with kidney failure," code 18 and 136, which gooses the reimbursement to $1273.60.
Epic snitches on doctors to their bosses, giving them a dashboard to track doctors' compliance with upcoding suggestions. One of Kuttner's doctor sources says her supervisor contacts her with questions like, "That appointment was a 2. Don’t you think it might be a 3?"
Robert Kuttner is the perfect journalist to unravel the Epic scam. As a journalist who wrote for The New England Journal of Medicine, he's got an insider's knowledge of the health industry, and plenty of sources among health professionals. As he tells it, Epic is a cultlike, insular company that employs 12.500 people in its hometown of Verona, WI.
The EHR industry's origins start with a GW Bush-era law called the HITECH Act, which was later folded into Obama's Recovery Act in 2009. Obama provided $27b to hospitals that installed EHR systems. These systems had to more than track patient outcomes – they also provided the data for pay-for-performance incentives. EHRs were already trying to do something very complicated – track health outcomes – but now they were also meant to underpin a cockamamie "incentives" program that was supposed to provide a carrot to the health industry so it would stop killing people and ripping off Medicare. EHRs devolved into obscenely complex spaghetti systems that doctors and nurses loathed on sight.
But there was one group that loved EHRs: hospital administrators and the private companies offering Medicare Advantage plans (which also benefited from upcoding patients in order to soak Uncle Sucker):
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8649706/
The spread of EHRs neatly tracks with a spike in upcharging: "from 2014 through 2019, the number of hospital stays billed at the highest severity level increased almost 20 percent…the number of stays billed at each of the other severity levels decreased":
https://oig.hhs.gov/oei/reports/OEI-02-18-00380.pdf
The purpose of a system is what it does. Epic's industry-dominating EHR is great at price-gouging, but it sucks as a clinical tool – it takes 18 keystrokes just to enter a prescription:
https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2729481
Doctors need to see patients, but their bosses demand that they satisfy Epic's endless red tape. Doctors now routinely stay late after work and show up hours early, just to do paperwork. It's not enough. According to another one of Kuttner's sources, doctors routinely copy-and-paste earlier entries into the current one, a practice that generates rampant errors. Some just make up random numbers to fulfill Epic's nonsensical requirements: the same source told Kuttner that when prompted to enter a pain score for his TB patients, he just enters "zero."
Don't worry, Epic has a solution: AI. They've rolled out an "ambient listening" tool that attempts to transcribe everything the doctor and patient say during an exam and then bash it into a visit report. Not only is this prone to the customary mistakes that make AI unsuited to high-stakes, error-sensitive applications, it also represents a profound misunderstanding of the purpose of clinical notes.
The very exercise of organizing your thoughts and reflections about an event – such as a medical exam – into a coherent report makes you apply rigor and perspective to events that otherwise arrive as a series of fleeting impressions and reactions. That's why blogging is such an effective practice:
https://pluralistic.net/2021/05/09/the-memex-method/
The answer to doctors not having time to reflect and organize good notes is to give them more time – not more AI. As another doctor told Kuttner: "Ambient listening is a solution to a self-created problem of requiring too much data entry by clinicians."
EHRs are one of those especially hellish public-private partnerships. Health care doctrine from Reagan to Obama insisted that the system just needed to be exposed to market forces and incentives. EHRs are designed to allow hospitals to win as many of these incentives as possible. Epic's clinical care modules do this by bombarding doctors with low-quality diagnostic suggestions with "little to do with a patient’s actual condition and risks," leading to "alert fatigue," so doctors miss the important alerts in the storm of nonsense elbow-jostling:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5058605/
Clinicians who actually want to improve the quality of care in their facilities end up recording data manually and keying it into spreadsheets, because they can't get Epic to give them the data they need. Meanwhile, an army of high-priced consultants stand ready to give clinicians advise on getting Epic to do what they need, but can't seem to deliver.
Ironically, one of the benefits that Epic touts is its interoperability: hospitals that buy Epic systems can interconnect those with other Epic systems, and there's a large ecosystem of aftermarket add-ons that work with Epic. But Epic is a product, not a protocol, so its much-touted interop exists entirely on its terms, and at its sufferance. If Epic chooses, a doctor using its products can send files to a doctor using a rival product. But Epic can also veto that activity – and its veto extends to deciding whether a hospital can export their patient records to a competing service and get off Epic altogether.
One major selling point for Epic is its capacity to export "anonymized" data for medical research. Very large patient data-sets like Epic's are reasonably believed to contain many potential medical insights, so medical researchers are very excited at the prospect of interrogating that data.
But Epic's approach – anonymizing files containing the most sensitive information imaginable, about millions of people, and then releasing them to third parties – is a nightmare. "De-identified" data-sets are notoriously vulnerable to "re-identification" and the threat of re-identification only increases every time there's another release or breach, which can used to reveal the identities of people in anonymized records. For example, if you have a database of all the prescribing at a given hospital – a numeric identifier representing the patient, and the time and date when they saw a doctor and got a scrip. At any time in the future, a big location-data breach – say, from Uber or a transit system – can show you which people went back and forth to the hospital at the times that line up with those doctor's appointments, unmasking the person who got abortion meds, cancer meds, psychiatric meds or other sensitive prescriptions.
The fact that anonymized data can – will! – be re-identified doesn't mean we have to give up on the prospect of gleaning insight from medical records. In the UK, the eminent doctor Ben Goldacre and colleagues built an incredible effective, privacy-preserving "trusted research environment" (TRE) to operate on millions of NHS records across a decentralized system of hospitals and trusts without ever moving the data off their own servers:
https://pluralistic.net/2024/03/08/the-fire-of-orodruin/#are-we-the-baddies
The TRE is an open source, transparent server that accepts complex research questions in the form of database queries. These queries are posted to a public server for peer-review and revision, and when they're ready, the TRE sends them to each of the databases where the records are held. Those databases transmit responses to the TRE, which then publishes them. This has been unimaginably successful: the prototype of the TRE launched during the lockdown generated sixty papers in Nature in a matter of months.
Monopolies are inefficient, and Epic's outmoded and dangerous approach to research, along with the roadblocks it puts in the way of clinical excellence, epitomizes the problems with monopoly. America's health care industry is a dumpster fire from top to bottom – from Medicare Advantage to hospital cartels – and allowing Epic to dominate the EHR market has somehow, incredibly, made that system even worse.
Naturally, Kuttner finishes out his article with some antitrust analysis, sketching out how the Sherman Act could be brought to bear on Epic. Something has to be done. Epic's software is one of the many reasons that MDs are leaving the medical profession in droves.
Epic epitomizes the long-standing class war between doctors who want to take care of their patients and hospital executives who want to make a buck off of those patients.

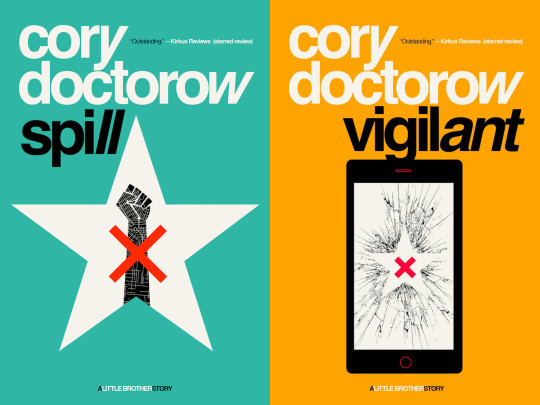
Tor Books as just published two new, free LITTLE BROTHER stories: VIGILANT, about creepy surveillance in distance education; and SPILL, about oil pipelines and indigenous landback.

If you'd like an essay-formatted version of this post to read or share, here's a link to it on pluralistic.net, my surveillance-free, ad-free, tracker-free blog:
https://pluralistic.net/2024/10/02/upcoded-to-death/#thanks-obama

Image: Flying Logos (modified) https://commons.wikimedia.org/wiki/File:Over_$1,000,000_dollars_in_USD_$100_bill_stacks.png
CC BY-SA 4.0 https://creativecommons.org/licenses/by-sa/4.0/deed.en
#pluralistic#ehrs#robert kuttner#tres#trusted research environments#ben goldacre#epic#epic systems#interoperability#privacy#reidentification#deidentification#thanks obama#upcoding#Hierarchical Condition Category#medicare#medicaid#ai#American Recovery and Reinvestment Act#HITECH act#medicare advantage#ambient listening#alert fatigue#monopoly#antitrust
829 notes
·
View notes
Text
Ensuring Compliance and Data Security in Computerized Medical Billing Systems
In the digital age, computerized medical billing systems have revolutionized healthcare administration by increasing efficiency, accuracy, and overall productivity. However, as more patient data becomes digitized, the responsibility to ensure compliance with regulatory frameworks and data security standards becomes even more critical. The combination of sensitive health information and financial data makes electronic medical billing systems a prime target for cyber threats. Thus, healthcare providers must take a proactive approach to secure these systems while staying aligned with industry regulations.
This article delves into the importance of compliance and data security in computerized medical billing, key regulations that govern healthcare data, potential risks, and actionable best practices that medical practices can adopt to maintain a secure and compliant billing environment.
Why Compliance and Security Matter in Computerized Medical Billing
The Sensitivity of Medical Billing Data
Medical billing data contains a vast amount of sensitive information, including:
Patient demographics
Insurance details
Diagnostic codes (ICD)
Treatment records
Payment history
Social Security Numbers (SSNs)
Any breach of this data can lead to devastating consequences such as identity theft, fraudulent insurance claims, or HIPAA penalties. With the integration of electronic medical billing software, ensuring that data remains secure and compliant is not just a regulatory obligation—it’s a critical component of patient trust and organizational integrity.
Rising Threats in Healthcare Cybersecurity
According to the U.S. Department of Health and Human Services (HHS), healthcare data breaches are increasing in both frequency and scale. In 2024 alone, over 100 million patient records were compromised globally, a significant number of which were due to vulnerabilities in electronic medical billing systems. These attacks exploit weak points in infrastructure, unpatched software, or lax access control, making data security a priority for healthcare providers.
Key Regulations Governing Computerized Medical Billing Compliance
Healthcare organizations that handle billing must comply with several regulatory standards designed to protect patient health information (PHI).
1. HIPAA (Health Insurance Portability and Accountability Act)
HIPAA is the cornerstone regulation for medical data protection in the United States. It mandates that any covered entity or business associate that handles PHI must:
Ensure the confidentiality, integrity, and availability of PHI.
Protect against anticipated threats or unauthorized disclosures.
Maintain workforce compliance through training and awareness.
Failure to comply with HIPAA can result in fines ranging from $100 to $50,000 per violation, depending on the severity and intent.
2. HITECH Act
The Health Information Technology for Economic and Clinical Health (HITECH) Act builds upon HIPAA by incentivizing the adoption of electronic medical billing systems and EMRs (Electronic Medical Records). It also tightens breach notification requirements and raises penalties for non-compliance.
3. PCI-DSS (Payment Card Industry Data Security Standard)
If a healthcare provider accepts payments via credit or debit cards, they must also adhere to PCI-DSS standards, which protect cardholder data during processing, transmission, and storage.
4. GDPR (General Data Protection Regulation)
For healthcare providers handling the data of EU citizens, GDPR imposes strict guidelines on data collection, consent, storage, and breach notification. It is especially relevant for multinational medical billing service providers using electronic medical billing software in international operations.
Common Security Risks in Electronic Medical Billing Systems
Despite technological advancements, several vulnerabilities continue to threaten computerized medical billing systems. These include:
1. Inadequate Access Control
Weak or improperly managed user access allows unauthorized individuals to view or manipulate sensitive data. This is often due to shared credentials, lack of multi-factor authentication, or unrevoked access rights.
2. Unencrypted Data Transmission
Sending patient or billing data over unencrypted networks exposes it to interception. Secure encryption protocols must be applied to both stored and transmitted data.
3. Software Vulnerabilities
Outdated electronic medical billing software often lacks security patches, making it an easy target for cyberattacks. Regular updates and vendor support are crucial for maintaining a secure system.
4. Insider Threats
Disgruntled or careless employees can be a significant source of data breaches. Whether intentional or accidental, human error remains one of the top causes of healthcare data exposure.
5. Lack of Audit Trails
Without a system that logs who accessed what and when, it’s difficult to detect unusual behavior or investigate potential security incidents.
Best Practices for Ensuring Compliance and Security
Now that we’ve outlined the risks and regulations, let’s look at some effective best practices that organizations should implement to safeguard their electronic medical billing systems.
1. Implement Role-Based Access Controls (RBAC)
Restrict access to patient data based on job responsibilities. For example, administrative staff should not have the same access as billing coders or healthcare providers. RBAC reduces the risk of internal breaches.
2. Use Encrypted Communication Protocols
Ensure that all data—whether stored in databases or transmitted between systems—is encrypted using strong standards such as AES-256. For communication, use HTTPS and secure VPNs.
3. Regular Security Audits and Penetration Testing
Periodic security assessments can help identify vulnerabilities before hackers exploit them. Ethical hackers can simulate attacks on your computerized medical billing system to test its defenses.
4. Maintain Updated Software and Security Patches
Outdated electronic medical billing software often lacks the latest security features. Work with vendors that offer regular updates, support, and compliance assistance.
5. Develop a Data Breach Response Plan
In the event of a data breach, a well-defined incident response plan ensures that your organization can quickly contain the damage, notify affected parties, and comply with legal obligations.
6. Employee Training and Awareness
Human error is often the weakest link in cybersecurity. Regularly train employees on phishing attacks, password policies, and HIPAA compliance to reduce the risk of accidental breaches.
7. Implement Secure Backups
Daily backups of your electronic medical billing system should be stored in secure, off-site locations. These backups should be encrypted and tested regularly to ensure reliability in the event of data loss or ransomware attacks.
Choosing Secure and Compliant Billing Software
Not all electronic medical billing software solutions are created equal. When evaluating vendors, consider the following:
Do they provide HIPAA-compliant solutions?
Do they offer end-to-end encryption?
Can they integrate with your existing EMR or EHR systems?
Do they maintain detailed audit logs and user activity tracking?
Is there support for multi-factor authentication and secure login?
Opting for a cloud-based, secure electronic medical billing system can provide built-in compliance features and reduce your infrastructure overhead while maintaining high availability and disaster recovery capabilities.
The Role of Third-Party Billing Services
Outsourcing to a third-party medical billing service can be beneficial, but it introduces additional compliance concerns. Ensure that:
The vendor signs a Business Associate Agreement (BAA) as required under HIPAA.
The vendor conducts regular internal audits.
They maintain industry certifications such as HITRUST or SOC 2.
It’s important to vet any service provider’s track record and compliance history before sharing patient data with them.
Future Trends in Billing Security and Compliance
AI and Machine Learning
Advanced electronic medical billing software is beginning to incorporate AI-driven anomaly detection, which can alert administrators of suspicious billing activities or potential fraud in real-time.
Blockchain Technology
Blockchain’s decentralized and immutable nature offers potential for secure, transparent transactions and could become integral to computerized medical billing in the future.
Zero Trust Architecture
The adoption of Zero Trust models is growing, especially in healthcare. It assumes no implicit trust in any user or system and continuously validates identity and access, ensuring tighter security controls.
Conclusion
With the increasing digitization of healthcare, ensuring compliance and robust data security in computerized medical billing systems is more vital than ever. Organizations that fail to address these concerns not only risk costly data breaches and penalties but also jeopardize patient trust.
By adhering to industry regulations like HIPAA and HITECH, deploying secure electronic medical billing software, and following best practices in cybersecurity, healthcare providers can ensure the safety of their patients’ data while optimizing billing operations.
0 notes
Text
One-stop Solution
A one-stop solution for invoicing, billing, quotations, payment collection, inventory, e-way bills and more. A one-stop solution for invoicing, billing, quotations, payment collection, inventory, e-way bills and more. Free invoice generator helps you create invoices online. Creating invoices should be simple - hitech restaurant software.
0 notes
Text
Unique Opportunity: Profitable Medical Billing Business for Sale - Invest in Healthcare Revenue Solutions Today
Exclusive Opportunity: Profitable Medical Billing Business for Sale – Invest in Healthcare revenue Solutions Today
Introduction
Are you looking for a lucrative investment opportunity within the thriving healthcare industry? The medical billing sector stands out as a highly profitable and sustainable business model, especially in today’s complex healthcare surroundings. With the increasing demand for efficient revenue cycle management and healthcare revenue solutions, acquiring a well-established medical billing business can be your key too steady income and long-term growth. In this article,we will explore the benefits of investing in a profitable medical billing business,practical tips for success,and how this opportunity can elevate your investment portfolio.
Why Invest in Medical Billing and Healthcare Revenue Solutions?
Medical billing is an essential component of the healthcare industry, ensuring healthcare providers receive timely payments for their services. The growth of this sector is driven by several factors:
Increasing healthcare expenditures: Rising medical costs create greater demand for effective revenue management.
Complex billing processes: With evolving insurance policies and coding standards, healthcare providers seek specialized billing services to avoid denials and maximize revenue.
Technological advancements: Modern medical billing software and automation improve efficiency, making outsourcing and specialized services more attractive.
Regulatory compliance: The healthcare sector requires compliance with strict laws, which specialized billing services can navigate more efficiently.
Investing in a profitable medical billing business means entering a stable, high-growth market with increasing demand for revenue cycle management services.
Benefits of Owning a Medical Billing Business
Owning a medical billing business offers numerous advantages:
Recurring Revenue: Monthly billing contracts ensure a steady income stream.
Low Overhead Costs: Digital operations minimize physical infrastructure needs.
Scalability: Easily expand by onboarding new healthcare providers or specialties.
High Profit Margins: After initial setup,profit margins are robust due to automation and efficient processes.
Impactful Service: Supporting healthcare providers to maximize their revenue ensures long-term business relationships.
These benefits make a well-established medical billing business an attractive investment for entrepreneurs and healthcare professionals alike.
Practical Tips for Investing in a Medical Billing Business
Assess the Business value and Growth Potential
Before making a purchase, evaluate the company’s financial health, client base, and operational efficiency. Look for businesses with a diverse list of healthcare providers and minimal client turnover.
Understand the Technology and Software
Ensure the business uses up-to-date, compliant billing software that can integrate with current healthcare systems like EMRs and insurance portals.
Check Legal and Regulatory Compliance
Verify the business adheres to HIPAA, HITECH, and other healthcare regulations. Non-compliance risks can jeopardize your investment.
Evaluate the Customer Base
A solid,loyal client base provides stability. Look for businesses with long-term contracts and positive client relationships.
Consider the Transition Process
Work with the seller to ensure a smooth transition, including staff training, software handover, and introduction to existing clients.
Review Financial Documentation
Parameter
details
Annual Revenue
$500,000
Profit Margin
30%
client Count
20 healthcare providers
Operational Staff
4 employees
This simple overview highlights key financial metrics you should review before purchasing.
Case Study: Success Story of a Medical Billing Business Acquisition
jane Doe,an experienced entrepreneur,acquired a medical billing company specializing in outpatient clinics. Her strategic focus on expanding the client base through targeted marketing and automation tools led to:
30% revenue growth within the first year
Enhanced operating efficiency
Extended provider relationships
Jane’s experience demonstrates how proper management and technological adoption can maximize profitability in healthcare revenue solutions.
Additional Insights: First-Hand Experience
Having personally invested in a medical billing business, I can attest to the industry’s resilience. Throughout economic fluctuations, healthcare remains a necessity, and reliable billing services are indispensable for providers. My experience underscores the importance of choosing a reputable, compliant, and scalable operation. Proper due diligence and a clear transition strategy are crucial to long-term success and maximizing your return on investment.
Conclusion
Investing in a profitable medical billing business presents a compelling opportunity to capitalize on the expanding healthcare industry. With increasing demand for healthcare revenue solutions, owning such a business can offer steady income, scalability, and long-term growth. Whether you’re an experienced entrepreneur or new to healthcare investments, this sector provides a resilient and lucrative avenue to diversify your portfolio.
Take the first step today by exploring available medical billing businesses for sale and consider how this investment aligns with your financial goals. With the right due diligence and strategic planning, you can secure a position in one of the most essential segments of the healthcare industry.
Take Action Today
Don’t miss out on this exclusive opportunity! Contact us now to learn more about profitable medical billing businesses for sale and start your journey towards healthcare revenue solutions excellence.
https://medicalbillingcodingcourses.net/unique-opportunity-profitable-medical-billing-business-for-sale-invest-in-healthcare-revenue-solutions-today/
0 notes
Text
Secure and Compliant Healthcare Data Management with MediBest Hospital Management System Software
Healthcare now tops every industry for breach costs, averaging US $4.88 million per incident in 2024—a 15 % jump in just two years. At the same time, the U.S. Office for Civil Rights has logged more than 374,000 HIPAA complaints since 2003, underscoring regulators’ growing vigilance. A recent HIMSS survey found that 59 % of providers experienced a significant cybersecurity event in the past year, and most plan to increase budgets for data protection.

Modern hospitals therefore need more than firewalls; they require a fully integrated healthcare management system software that embeds security and compliance into every workflow.
How MediBest Builds a Defense-in-Depth Architecture
MediBest—an industry-trusted hospital software company—fortifies its cloud-native platform with multiple protective layers that work together to keep patient data safe.
End-to-end encryption (TLS 1.3 in transit, AES-256 at rest)
Zero-trust access controls with MFA and role-based privileges
Continuous threat monitoring powered by AI anomaly detection
Immutable audit logs for every clinical, financial, and admin action
Automated backups and geo-redundant disaster recovery
Because all modules share a single database, these safeguards apply consistently across EHR, billing, radiology, HR, and inventory—eliminating gaps common in bolt-on tools.
Compliance by Design: Meeting HIPAA, GDPR, and NABH
MediBest’s healthcare management system ships with pre-configured compliance templates and rule engines to streamline statutory reporting:
HIPAA & HITECH: automatic PHI tagging, breach-alert workflows, and encryption keys managed in certified data centers.
GDPR: data-subject-access request (DSAR) dashboards and right-to-erasure controls.
NABH & NABL: clinical quality and infection-control reports generated in one click.
Configurable policy packs let hospitals adapt settings to local regulations without costly code changes. Google my Business :
Business Benefits of Secure, Unified Data Governance
Reduced legal and financial risk: proactive safeguards lower the likelihood of fines and lawsuits.
Operational efficiency: single-source data eliminates duplicate entry, cutting admin time by up to 30 %.
Higher patient trust: visible security measures and transparent consent management improve satisfaction scores.
Stronger brand reputation: demonstrating best-practice cybersecurity differentiates your facility in competitive markets.
Fast, Low-Friction Implementation with MediBest
Assessment & gap analysis to map current vulnerabilities.
Phased rollout starting with high-risk modules such as billing and EHR.
Staff training on secure workflows and incident-response drills.
Quarterly security audits and penetration tests included in the support plan.
This structured approach lets hospitals deploy robust protection without disrupting day-to-day care. Click Here :
Frequently Asked Questions
1. What makes hospital management system software “secure”? It combines strong encryption, least-privilege access, continuous monitoring, and compliant audit trails inside one unified platform—protecting data at every step from admission to discharge.
2. Can cloud-based healthcare management systems meet HIPAA requirements? Yes. When hosted in certified data centers with encrypted storage, MFA, and documented BAAs, cloud systems can exceed on-premise security while providing better scalability and uptime.
3. How does MediBest simplify compliance reporting? Built-in templates for HIPAA, GDPR, and NABH pull real-time data from every module, auto-populate regulatory forms, and schedule submissions—cutting report prep from days to minutes.
MEDIBEST :- CONTANT NOW :- Corporate Office 303, IT Park Center, IT Park Sinhasa Indore, Madhya Pradesh, 452013 Call Now +91 79098 11515 +91 97139 01529 +91 91713 41515 Email [email protected] [email protected]
0 notes
Text
The Evolution of Medical Records: From Paper to EMR
Medical History Records are the quiet foundation of medicine. They contain the histories of diagnoses, treatments, recoveries, and occasionally, life-or-death decisions. For centuries, those histories were recorded on paper — sometimes neatly in files, and often, poorly legible or impossible to access. In many aspects of modern life, technology has brought a kind of change in how we record, store, and retrieve patient data.

Welcome to the age of Electronic Medical Records (EMRs), where health data meets electronics. The Early Years: Paper-Based Medical Records Till the beginning of the 20th century, physicians wrote patient information in notebooks, ledgers, or in files saved for individual patients. Each patient's paper record included complete information about their interaction with the health system: symptoms, examination findings, diagnoses, medications, and follow-up. Paper documentation also had significant limitations: Storage: Hospitals had to dedicate enormous physical space to paper records. Readability: The handwriting of physicians became infamous, with sometimes fatal consequences. Inaccessibility: The sharing of patient health data across departments and hospitals was tedious and challenging. Data Loss: Disasters such as fires and floods frequently wipe out years of document storage. However, despite significant limitations as a record of patient and population health information, paper endured for 20 years as the popular standard of data record keeping, partly because it was known, easy, and did not require training or software support. The Tipping Point: Computers During the 1960s and 70s, academic medical institutions started playing around with computer health records. It wasn't to eliminate paper altogether but to enhance administrative procedures such as billing, scheduling, and coding for insurance. The breakthrough happened in the 1990s and early 2000s when technology became more accessible and the internet started to revolutionize information transfer. During this time:
Hospitals have increasingly converted a major portion of patient information to digital formats.
Tech firms, including Epic, Cerner, and Allscripts, surfaced with affordable healthcare-specific offerings.
The term Electronic Medical Records (EMR) gained popularity, indicating the electronic version of a patient's chart at one location.
EMRs vs. EHRs: Understanding the Difference Most individuals apply the terms EMR and Electronic Health Record (EHR) interchangeably, but there is a subtle difference. EMR: Electronic records within a single organization (e.g., a single hospital or clinic). It is diagnosis- and treatment-oriented. EHR: A more comprehensive, interoperable system that exchanges information among various healthcare providers and facilities. EHRs provide a wider perspective of a patient's medical history. Now, EHRs are the next step in the evolution of EMRs — more collaborative, patient-focused, and data-intensive. The Transition to EMR: Reasons in Support of the Change Shifting from paper to EMR was not simply a technological decision, it was a necessary healthcare one, and here are the reasons why: Efficiency and Speed: EMRs sharply reduced the time taken to access patient information, write prescriptions, or order tests. Reduced errors: EMRs reduce opportunities for human mistakes with templates and dropdowns, and standardization of data fields. Real-time updates: Clinicians are able to update a patient record at the point of care, increasing care coordination in real-time. Data analytics: EMRs allow better access to patient outcome data with automation, identify high-risk cases, and chronic disease. Legal and Compliance Mandates: Governments globally, most notably the U.S. (with the HITECH Act in 2009), rewarded digital adoption with incentives. Obstacles Along the Way All the benefits aside, switching to EMR wasn't without burgeoning pains: High Upfront Expenses: Integrating EMR systems involved a large initial outlay in software, hardware, and training. Learning Curve: Individual practitioners had to adapt to changed reporting style from writing in paper charts to tapping on sometimes clunky interfaces. Data Privacy and Security Concerns: The shift to digital meant the risk of data breaches, ransomware and cyber-attacks. Interoperability Issues: Most EMR systems did not "talk" to one another or share information in a seamless manner. The Role of AI and Cloud in Modern EMRs As EMRs progress, they're getting smarter and more connected. This is how innovation is molding their future: Artificial Intelligence: EMRs are increasingly utilizing AI to identify patterns, anticipate complications, and aid in diagnosis. Voice Recognition: Physicians can now use Natural Language Processing to dictate directly to EMRs. Cloud-Based EMRs: These systems are more flexible with remote access and more cost-effective than an on-premises legacy system. Patient Portals: Patients are now able to view lab results, schedule appointments, and message their physicians through secure patient portals, increasing patient engagement and transparency. Conclusion Electronic medical records improved clinical processes and allowed new avenues for preventive care, telehealth for patients, and personalized treatments. Even though there are still challenges ahead, the digital future for medical records is clear and that is dynamic, accessible, and 'smart'.
0 notes
Text
The Clinical Benefits of Electronic Health Records Systems

The adoption of Electronic Health Records (EHRs) began in the early 2000s, due to advancements in technology, and the need for better patient data management. In 2009, the Health Information Technology for Economics and Clinical Health (HITECH) Act was passed, which provided financial incentives through a Medicare and Medicaid EHR incentive program, later known as Meaningful Use. Between 2011 and 2015, a growing number of providers adopted EHRs to qualify for federal incentives and avoid penalties. Then in 2020, the COVID pandemic hit creating a sudden need for patients to be treated remotely. The Office of National Coordinator for Health Information Technology (ONC) estimated that as of 2020, approximately 88% of all U.S. physician offices used some form of electronic health records.
Electronic Health Records systems have provided significant benefits practice productivity and patient care. Providers gain access to patient data in real time. Everything from lab results to current medications is available at a glance. This reduces errors and supports more informed decision-making. Physicians can easily and effectively coordinate care with other providers, resulting in better patient outcomes and overall patient experience.
In addition to better patient care, EHR systems increase operational efficiency in your practice. Administrative tasks such as scheduling, eligibility, and billing insurance claims can be automated freeing up valuable time. Advanced features such as patient reminders can help reduce no-shows. Robust reporting tools that help you to analyze trends, track performance metrics, and identify areas for growth. By investing in an EHR, you’re investing in a system that can help your practice run more efficiently and prepare for future growth.
Unlock the EHR Software Benefits!
#ehrsoftware#electronic health records software#electronic health records solutoins#ehr solutions#emr systems#pronocis ehr software#emr solutions#electronic health record systems#healthtech#medical office software#top ehr software
0 notes
Text
💎 Jewellery Shop Billing Software: The Smart Way to Manage Your Jewellery Store
Running a jewellery store? Whether it's a small family-owned shop or a multi-branch retail outlet, managing billing, inventory, and customer records manually is a recipe for errors and stress.
That’s where Jewellery Shop Billing Software comes in. Designed specifically for jewellery retailers, this software helps you manage daily operations like invoicing, stock tracking, karigar work, and GST compliance — all from one easy dashboard.
Let’s break it down. 👇
✨ What Is Jewellery Shop Billing Software?
Unlike regular billing software, jewellery billing tools are built to handle:
Weight- and purity-based pricing
Wastage calculations
Making charges
Hallmarking support
GST-ready invoicing
It’s tailor-made for gold, silver, and diamond sellers who need more than just a printed bill.
🔧 Key Features to Look For
Here’s what makes good jewellery billing software truly shine:
💳 Smart Billing & Invoicing Generate accurate GST-compliant bills with gold/silver rates updated in real-time.
📦 Inventory Management Track jewellery by karat, weight, design, and type — no more guesswork.
📋 Karigar & Job Work Management Keep tabs on raw materials, finished items, and payments to artisans.
📈 Accounting & Reporting Automated financial reports, ledgers, and tax summaries.
📲 Mobile & Cloud Access Manage your shop from anywhere — even on your phone!
🎯 Why Your Jewellery Shop Needs It
✅ Speeds up the billing process ✅ Reduces manual errors ✅ Helps with tax filing and compliance ✅ Builds customer trust with professional invoices ✅ Gives you full control over stock and sales
🏆 Popular Jewellery Billing Software in India
Here are a few trusted names you can explore:
Marg ERP for Jewellery
Vyapar Jewellery Billing
Ornate Jewellery Software
Hitech Jewellery Billing Software
JewelX POS
Each offers different plans for small to large businesses.
0 notes
Text
What Are the Cost Considerations When Choosing Behavioral Health EHR Software?

For behavioral health practices, implementing the right Electronic Health Record (EHR) software is a crucial investment. But beyond the initial cost, there are several hidden expenses that many organizations overlook. Choosing an EHR isn’t just about finding the most affordable option—it’s about ensuring that the system aligns with your clinical needs, enhances efficiency, and remains cost-effective in the long run.
Understanding the cost considerations when selecting behavioral health EHR software is essential to making an informed decision that balances affordability and functionality.
1. Upfront Costs: Licensing and Setup Fees
When evaluating EHR solutions, the first expense you’ll encounter is the upfront cost, which typically includes:
Software licensing fees (one-time or subscription-based)
Implementation fees (system setup, customization, and integration)
Hardware costs (if you need new servers or devices)
💡 Pro Tip: Some vendors offer flexible payment models, including monthly subscriptions instead of high upfront costs. If you're a smaller practice, a cloud-based EHR can help reduce these initial expenses.
2. Ongoing Subscription and Maintenance Fees
Most EHR providers charge a recurring subscription fee, which can be monthly or annually. This fee usually covers:
System updates
Data storage and security
Routine maintenance
Customer support
💡 Pro Tip: Compare subscription models carefully—some may charge per provider, per user, or per patient record. Ensure you understand how costs will scale as your practice grows.
3. Customization and Integration Costs
Behavioral health practices have unique needs that general EHR systems may not meet. If you require:
Specialized workflows for therapy sessions and treatment plans
Custom reporting tools
Integrations with telehealth platforms or billing software
Then expect additional costs for customization and API integrations. Some EHRs come with built-in behavioral health features, saving you customization expenses.
💡 Pro Tip: Ask vendors upfront about customization fees—some may charge a flat rate, while others bill hourly for development work.
4. Training and Onboarding Costs
A sophisticated EHR system is only valuable if your team knows how to use it efficiently. Training expenses may include:
On-site or virtual training sessions
User manuals and video tutorials
Extra training for new hires
💡 Pro Tip: Look for EHR providers that offer free training resources or tiered training plans. A vendor that provides ongoing support can help reduce long-term costs.
5. Data Migration Costs
Switching from an existing system? Data migration can be a costly and time-consuming process. This includes:
Transferring patient records
Ensuring data integrity
Converting formats to meet EHR standards
💡 Pro Tip: Some vendors include basic data migration for free, while others charge based on the volume of records. Always clarify before committing.
6. Hidden Costs: Downtime and Productivity Loss
Transitioning to a new EHR system can disrupt workflow temporarily. Hidden costs can arise from:
Lost productivity as staff adapts to the new system
Temporary downtime affecting patient scheduling and billing
Errors or inefficiencies while staff learns the software
💡 Pro Tip: Opt for an EHR with an intuitive user interface and responsive customer support to minimize disruption.
7. Regulatory Compliance and Security Costs
Behavioral health data is sensitive, and your EHR must comply with:
HIPAA regulations (for patient data privacy)
HITECH Act (security and interoperability requirements)
State-specific mental health privacy laws
Some vendors charge extra for advanced security features, such as role-based access, encrypted messaging, and compliance audits.
💡 Pro Tip: Choose an EHR that is HIPAA-compliant by default rather than paying extra for security add-ons.
8. Scalability Costs: Can Your EHR Grow with You?
Your practice might start small, but as you expand, your EHR must scale with your needs. Some hidden costs of growth include:
Adding more users or locations
Increased storage for patient records
Upgrading to a higher-tier subscription
💡 Pro Tip: Choose an EHR with transparent pricing that allows you to scale affordably as your practice grows.
Conclusion: Balance Cost with Value
Choosing the right behavioral health EHR software isn’t just about picking the cheapest option—it’s about finding the right balance between cost, functionality, and long-term value. By considering all potential expenses, from licensing and training to compliance and scalability, you can make an informed decision that benefits your practice both financially and operationally.
Before committing, ask vendors for a detailed cost breakdown, request a demo, and ensure the software fits your practice’s unique behavioral health needs. The right EHR will not only save money in the long run but also enhance patient care and improve your practice’s efficiency.
0 notes
Text
Best Healthcare App Development Company: Bitlyze Technologies
In the fast-moving healthcare sector, tech solutions are at the center of reshaping patient care and hospital operations. Bitlyze Technologies, one of the best healthcare app development companies, is a master of creating innovative healthcare applications with the ability to deliver efficient care coordination, enhanced patient engagement, and operational effectiveness.
Custom Healthcare App Development ServicesBitlyze Technologies provides a variety of to meet the diverse requirements of medical facilities, healthcare institutions, and patients. Hospital management custom healthcare app development services systems, telemedicine software, and others are developed by our skilled developers as secure and effective applications for improving healthcare provision.
Key Custom Healthcare App Development Services:Telemedicine App Development: Secure and effective remote consultations.
Hospital Management System Software: Streamline hospital operations with EHR, billing, scheduling, and patient tracking.
Patient Portal Development: Improve patient satisfaction through online appointment scheduling, access to health records, and secure messaging.
Medical App Development: Tailored solutions for doctors, clinics, and hospitals.
Pharma App Development: Pharma industry digital solutions, such as inventory management and online prescription services.
HIPAA Compliance Software: Secure and compliant healthcare data management.
Hospital Management System SoftwareBitlyze Technologies' hospital management system software (HMS) is created to make the process of medical institutions' workflow simpler, so department coordination is problem-free.
Features of Our Hospital Management System:Electronic Health Records (EHR): Patient information storage and retrieval in a secure environment.
Billing & Insurance Processing: Automatic billing and insurance claims processing.
Remote Patient Monitoring: Remote monitoring of patient vital signs and medical status.
Appointment Scheduling: Patient and physician coordination in an effortless manner.
Medical Inventory Management: Monitor medical supplies, avoiding wastage.
AIBitlyze Technologies Revolutionizes Healthcare with customized AI solutions for healthcare, incorporating artificial intelligence to advance diagnostics, treatment planning, and patient monitoring.
Customized AI Solutions for Healthcare Include:
Predictive Analytics for Patient Care: AI-based insights to identify early symptoms and anticipate disease progression.
Medical Image Processing: AI-based diagnostic tools to support radiologists and pathologists.
Healthcare Chatbots: AI-powered virtual assistants for 24/7 patient management.
AI-Driven Drug Discovery: Pharma R&D sped up.
Most Popular Key Healthcare Features for Healthcare Apps1. Patient AppAppointment reminders and scheduling.
Health monitoring and symptom checker.
Secure communication with physicians and healthcare professionals.
2. Hospital & Clinic PanelReal-time patient data management.
Hospital workflow solutions built into it.
Duty management and scheduling of staff.
3. Medical Professional AppsRemote patient monitoring.
Access to prescriptions and medical history.
AI-based decision support system.
4. In-App Communication & Secure PaymentsReal-time video consultations and chat.HIPAA-compliant secure payment gateways.Why Bitlyze Technologies?1. Healthcare Apps with Compliance-FriendlinessWe strictly follow the best regulatory compliance and industry standards, including:
HIPAA (Health Insurance Portability and Accountability Act)
GDPR (General Data Protection Regulation)
HITECH (Health Information Technology for Economic and Clinical Health Act)
SaMD (Software as a Medical Device)
HL7 (Health Level Seven International)
2. Scalable and Secure SolutionsOur healthcare applications are scalable and secure, capable of processing high volumes of data with state-of-the-art security.
3. User-Centric ApproachWe provide hassle-free user experience for patients, medical professionals, and healthcare professionals.
4. Cutting-Edge TechnologyWith expertise in AI, IoT, and cloud computing, we create sophisticated solutions based on healthcare requirements.
Revitalize Your Healthcare Services with Bitlyze TechnologiesBitlyze Technologies is the top healthcare app development company and works towards transforming the healthcare industry through custom healthcare app development services and custom healthcare AI solutions. Our hospital management system software keeps running smoothly, and our healthcare app development services enable providers to deliver quality care.
Ready to revolutionize your healthcare services? Reach out to Bitlyze Technologies today for a complimentary consultation and take the leap towards digitalization!
0 notes
Text
Healthcare IT Services for Secure Data Management – WiseGTech
Healthcare IT Services for Secure Data Management – WiseGTech
Introduction
In the modern healthcare industry, secure data management is paramount. With increasing digital transformation, healthcare providers need robust IT solutions to ensure data security, streamline patient care, and comply with regulatory requirements like HIPAA and GDPR. WiseGTech specializes in providing comprehensive healthcare IT services tailored to hospitals, clinics, and healthcare organizations.
This blog explores how WiseGTech’s healthcare IT services empower medical professionals with secure, scalable, and efficient data management solutions, ensuring patient confidentiality and operational efficiency.
Why Secure Data Management is Crucial in Healthcare
The healthcare industry handles vast amounts of sensitive patient data, including Electronic Health Records (EHRs), medical histories, billing details, and insurance records. Any breach in security can lead to serious consequences, including legal penalties, financial losses, and damage to reputation. Key challenges include:
✅ Cybersecurity Threats: Healthcare is a prime target for ransomware and cyberattacks.
✅ Regulatory Compliance: Strict laws like HIPAA, HITECH, and GDPR require data protection.
✅ Data Accessibility & Interoperability: Secure and seamless access to patient records is essential.
✅ Disaster Recovery & Backup: Healthcare organizations must have fail-proof data recovery solutions.
With WiseGTech, healthcare providers get a tailored IT strategy that ensures compliance, security, and operational efficiency.
WiseGTech’s Healthcare IT Solutions
WiseGTech offers a range of advanced IT solutions specifically designed to protect patient data, streamline operations, and enhance patient care. Here are our top healthcare IT services:
1. Secure Electronic Health Records (EHR) Management
EHRs are at the core of healthcare IT. WiseGTech provides secure, cloud-based EHR solutions that ensure:
🔹 Data Encryption: Protects patient data from unauthorized access.
🔹 Interoperability: Enables seamless data exchange between healthcare systems.
🔹 Real-Time Access: Ensures doctors and nurses can retrieve records instantly.
🔹 HIPAA Compliance: Meets industry standards for patient data security.
With automated backups and disaster recovery, WiseGTech ensures zero data loss and maximum uptime.
2. Advanced Cybersecurity Solutions for Healthcare
With cyber threats on the rise, healthcare providers need multi-layered security to protect confidential patient information. WiseGTech offers:
🔹 End-to-End Data Encryption to prevent unauthorized access.
🔹 Multi-Factor Authentication (MFA) for enhanced security.
🔹 Network Security & Firewalls to safeguard against cyberattacks.
🔹 Regular Security Audits & Compliance Assessments to ensure adherence to regulations.
🔹 AI-Powered Threat Detection & Incident Response for proactive cybersecurity management.
With WiseGTech’s security framework, healthcare organizations can mitigate risks and stay ahead of cyber threats.
3. Cloud-Based Healthcare IT Infrastructure
Migrating healthcare operations to the cloud ensures scalability, security, and cost-efficiency. WiseGTech provides:
🔹 Cloud Storage & Computing for easy access to patient data.
🔹 Telemedicine Integration for remote consultations and virtual healthcare.
🔹 Automated Data Backups to prevent data loss.
🔹 Scalable Infrastructure that grows with your organization.
🔹 Disaster Recovery Solutions for quick restoration in emergencies.
With HIPAA-compliant cloud hosting, healthcare organizations can securely store and access patient data anytime, anywhere.
4. IT Support & 24/7 Monitoring for Healthcare Providers
A reliable IT infrastructure requires constant monitoring and technical support. WiseGTech provides:
🔹 24/7 IT Helpdesk Support for troubleshooting.
🔹 Network Monitoring & Performance Optimization to prevent downtime.
🔹 Software Updates & Patch Management to keep systems secure.
🔹 Remote & On-Site IT Support to address issues quickly.
With round-the-clock IT support, healthcare providers can focus on patient care without technical interruptions.
5. Healthcare IT Compliance & Regulatory Support
Healthcare organizations must comply with strict regulations. WiseGTech helps ensure:
🔹 HIPAA & GDPR Compliance for data protection.
🔹 Regular IT Security Audits & Risk Assessments.
🔹 Data Encryption & Access Control Policies to protect patient privacy.
🔹 Compliance Documentation & Reporting for audits.
By following the latest industry standards, WiseGTech ensures healthcare organizations stay compliant and avoid penalties.
6. Healthcare Data Analytics & AI Integration
Data-driven healthcare improves decision-making and patient outcomes. WiseGTech provides AI-powered analytics for:
🔹 Predictive Analytics for early disease detection.
🔹 Operational Efficiency Optimization through workflow automation.
🔹 Patient Engagement Insights to improve services.
🔹 AI-Based Diagnostics & Treatment Planning.
By leveraging Big Data & AI, healthcare providers can enhance treatment accuracy and efficiency.
Why Choose WiseGTech for Healthcare IT Services?
WiseGTech is a trusted IT partner for healthcare organizations, offering:
✅ Industry Expertise: Years of experience in healthcare IT solutions.
✅ Advanced Security Measures: Protection against cyber threats and data breaches.
✅ 24/7 IT Support: Ensuring uninterrupted system performance.
✅ Regulatory Compliance: Full adherence to HIPAA, GDPR, and other industry regulations.
✅ Custom IT Solutions: Tailored to meet your specific operational needs.
With WiseGTech, healthcare organizations get cutting-edge IT solutions that enhance security, efficiency, and patient care.
0 notes
Text
How to Develop a SaaS App for the Healthcare Industry
Developing a SaaS app for the healthcare industry involves a structured approach, focusing on compliance, functionality, and usability. Here’s a step-by-step guide to help you navigate the process:
1. Understand the Target Audience
Define Users: Identify whether your app is for hospitals, clinics, doctors, patients, or insurance providers.
Key Features: Focus on features like electronic health records (EHR), telemedicine, appointment scheduling, patient management, or billing systems.
2. Conduct Market Research
Competitor Analysis: Analyze existing healthcare SaaS apps to identify gaps.
Regulatory Landscape: Research healthcare regulations like HIPAA (US), GDPR (EU), or PIPEDA (Canada) for compliance.
Pain Points: Understand the challenges healthcare providers and patients face.
3. Choose the Right Tech Stack
Frontend: Use React, Angular, or Vue.js for a responsive and user-friendly UI.
Backend: Leverage Node.js, Python (Django/Flask), or Java Spring Boot for scalability.
Database: Opt for MySQL, PostgreSQL, or NoSQL databases for data storage.
Cloud Hosting: Use AWS, Azure, or Google Cloud for reliable hosting.
4. Ensure Compliance with Healthcare Standards
Data Security: Implement end-to-end encryption, secure APIs, and regular security audits.
Compliance Certifications: Ensure your app meets healthcare standards like HIPAA, HITECH, and SOC 2.
Privacy Policies: Clearly state how user data is collected, stored, and shared.
5. Develop Core Features
Patient Portal: Allow patients to view medical records, prescriptions, and book appointments.
Telehealth Integration: Enable video consultations and secure messaging.
EHR System: Provide tools for doctors to update and access patient records.
Analytics Dashboard: Offer insights on patient data and clinic performance.
Payment Integration: Facilitate secure online billing and insurance claims.
6. Focus on UI/UX Design
Intuitive Design: Ensure the app is easy to navigate for both healthcare providers and patients.
Mobile Responsiveness: Optimize for various devices to enhance accessibility.
Accessibility Standards: Adhere to WCAG (Web Content Accessibility Guidelines) for inclusivity.
7. Build and Test
Agile Development: Use agile methodologies for iterative development.
Testing: Conduct rigorous testing for functionality, security, and compliance.
Beta Testing: Release a beta version to gather user feedback.
8. Deploy and Scale
Cloud Deployment: Use scalable cloud infrastructure for smooth app deployment.
Monitoring Tools: Implement monitoring systems to track performance and usage.
Scaling: Be prepared to scale resources based on user demand.
9. Continuous Updates and Maintenance
Feature Updates: Regularly release updates based on user feedback and technological advancements.
Compliance Updates: Adapt to any changes in healthcare regulations.
Support: Offer 24/7 customer support for users.
10. Marketing and Sales
Targeted Marketing: Use digital marketing to reach healthcare providers and institutions.
Freemium Model: Consider offering a free trial or limited version to attract users.
Partnerships: Collaborate with hospitals and clinics to boost adoption.
Key Considerations
Trust: Build a secure and transparent platform to gain users' trust.
Scalability: Plan for growth, as healthcare data can grow exponentially.
Integration: Ensure compatibility with other healthcare software and systems.
Would you like detailed guidance on any specific part of this process?
View More: How to Develop a SaaS App for the Healthcare Industry?
0 notes
Text
Best Restaurant Management Software

Simple, clutter-free design ensures enhanced user experience so that you can focus on stuff that matters - your food & your service. With our offline mode, your restaurant POS software will always be up & running even if there is no internet. Punch-In orders, download reports or store customer data hassle-free. It can help you streamline essential inventory and supply management operations such as waste tracking, ordering from multiple suppliers, and more. Our restaurant software is a cloud-based reputation management platform that assists restaurant owners in effectively managing their online presence and enhancing customer satisfaction. By leveraging these features, restaurant owners can enhance operational efficiency, reduce costs, and focus more on delivering exceptional dining experiences. From point-of-sale functionality to inventory management, reservation. A restaurant management software is a comprehensive systematic solution designed to streamline and optimize the operations of a restaurant or food service establishment - hitech restaurant software.
This platform is designed to help restaurants efficiently schedule shifts, manage labor costs, and communicate effectively with their staff. With features like labor forecasting and team messaging, shifts aid restaurants in optimizing their workforce, resulting in improved operational efficiency and better customer service. Catering software solutions are designed to meet the unique needs of various industries, including corporate catering, event planning, and restaurant management - free restaurant billing software.
It caters to different industries, including food, retail, and automotive. It can also automate processes to ensure food safety, quality, and compliance. It can help food enterprises maximize profits by reducing waste and improving employee efficiency. This software solution allows you to analyze supplier performance, reduce risks, and improve cost efficiency. We offer restaurant owners a comprehensive platform to enhance their operations and reach a broader customer base. For restaurant owners juggling multiple responsibilities, shifts is one of the best apps for restaurant owners, simplifying one of the most time consuming tasks-scheduling. It offers real-time online booking, enabling diners to make reservations seamlessly while providing restaurants with powerful tools to efficiently handle bookings and minimize no-shows. For more information, please visit our site https://billingsoftwareindia.in/restaurant-billing-software/
0 notes
Text
Interoperability and Data Integration: The Backbone of Modern Healthcare Software Systems

In the rapidly evolving world of healthcare, the ability of software systems to communicate and share data seamlessly is more crucial than ever. Interoperability and data integration are not just technical terms; they are the foundation of efficient, patient-centered care. As healthcare facilities continue to adopt digital solutions, understanding how these elements work and why they are important can significantly impact the quality of care delivered.
What is Interoperability in Healthcare?
Interoperability in healthcare refers to the ability of different software systems, applications, and devices to connect and exchange data accurately, effectively, and consistently. This means that various healthcare management system software, hospital management system software, and other specialized hospital software can communicate without barriers, ensuring that critical information flows smoothly across different platforms.
For example, when a patient’s electronic health record (EHR) is updated in one system, that information should be instantly available across other systems used in the same hospital or even across different healthcare providers. This seamless data exchange is essential for providing timely and coordinated care.
The Importance of Data Integration in Healthcare
Data integration goes hand in hand with interoperability. It involves the process of combining data from different sources into a single, unified view. In a healthcare setting, data integration allows for the consolidation of patient information from various departments—such as laboratory results, imaging, and prescriptions—into one comprehensive record.
By leveraging data integration, healthcare providers can have a holistic view of a patient’s history, enabling them to make informed decisions quickly. Integrated data can also be analyzed to identify trends, monitor patient outcomes, and optimize hospital operations.
Benefits of Interoperability and Data Integration
1. Enhanced Patient Care
Interoperability and data integration improve the quality of care by providing healthcare providers with complete and up-to-date patient information. This minimizes the risk of errors, reduces duplicate tests, and ensures that treatment decisions are based on the most accurate data available.
2. Increased Efficiency
When healthcare systems can communicate seamlessly, administrative tasks such as scheduling, billing, and resource management become more streamlined. This leads to significant time and cost savings for healthcare facilities, allowing them to allocate resources more effectively.
3. Improved Patient Outcomes
By enabling real-time data sharing, interoperability allows healthcare providers to collaborate more effectively, leading to better-coordinated care. This is particularly important in complex cases where multiple specialists are involved. Integrated data also supports preventive care initiatives, helping providers identify and address potential health issues before they become critical.
4. Compliance with Regulatory Requirements
Interoperability and data integration are often necessary for meeting regulatory requirements, such as those mandated by the Health Information Technology for Economic and Clinical Health (HITECH) Act in the United States. By ensuring that systems can share data securely, healthcare organizations can avoid penalties and maintain compliance with healthcare standards.
Challenges of Achieving Interoperability and Data Integration
Despite the clear benefits, achieving interoperability and data integration is not without its challenges. These include:
1. Technical Barriers
Different systems may use varying data formats, communication protocols, and standards, making it difficult to ensure seamless interoperability. Overcoming these technical barriers often requires significant investment in software upgrades and system integration.
2. Data Security and Privacy
As healthcare data becomes more interconnected, the risk of data breaches and unauthorized access increases. Ensuring that all systems adhere to stringent security protocols is critical to protecting patient information.
3. Resistance to Change
Implementing new systems and workflows can be met with resistance from staff who are accustomed to existing processes. Training and change management are essential to ensure smooth adoption of interoperable systems.
The Future of Interoperability and Data Integration
As healthcare continues to evolve, so too will the technologies that support interoperability and data integration. The future holds exciting possibilities, including:
1. Advanced AI and Machine Learning
AI and machine learning can enhance data integration by analyzing vast amounts of data quickly and accurately. This will enable more personalized care and predictive analytics, helping healthcare providers anticipate patient needs and outcomes.
2. Blockchain Technology
Blockchain offers a promising solution for secure data sharing across different systems. By creating a decentralized and immutable record of transactions, blockchain can enhance data security and integrity in healthcare.
3. Greater Collaboration Across Industries
As the lines between healthcare, technology, and other industries blur, we can expect to see greater collaboration in developing interoperable solutions. This will likely lead to the creation of more comprehensive and user-friendly healthcare software systems.
Conclusion
Interoperability and data integration are not just buzzwords; they are essential components of a modern, efficient healthcare system. As healthcare organizations strive to improve patient care, reduce costs, and meet regulatory requirements, these elements will play an increasingly important role.
For healthcare facilities looking to achieve seamless interoperability and data integration, partnering with a reliable healthcare software company is key.
MediBest is a leading Healthcare-IT company focused on delivering state-of-the-art Hospital Management System software. Our solutions facilitate the complete digital transformation of client hospitals, enabling them to reach their full potential. MediBest's web-based, enterprise-grade Hospital Management System Sofware supports hundreds of concurrent users and can be deployed on-premise or in the cloud. Its robust architecture is designed with technical and functional extendibility in mind, ensuring long-term, obsolescence-proof value.
Ready to transform your healthcare facility with cutting-edge hospital software? Contact MediBest today at Tel: +91 8889904042 or visit our website at https://medibest.in/ to learn how we can help you achieve true interoperability and data integration.
0 notes
Text
The Evolution of Billing and Coding in the USA Over the Decades

Medical billing and coding are fundamental processes in the healthcare industry, ensuring that providers receive payment for their services and that patient records are accurately maintained. Over the decades, these processes have undergone significant transformations, driven by technological advancements, regulatory changes, and evolving healthcare needs. This article explores the evolution of billing and coding in USA, highlighting key developments and their impacts on the healthcare system.
Early Days: Manual Processes and Paper Records
In the early 20th century, medical billing and coding were rudimentary and manual processes. Healthcare providers relied heavily on handwritten notes and paper records to document patient visits and treatments. Billing was a straightforward, albeit labor-intensive, task, often handled by office staff or physicians themselves. The lack of standardized codes and the manual nature of record-keeping led to inconsistencies and errors, affecting reimbursement and patient care quality.
The Birth of ICD and CPT Codes
The introduction of standardized coding systems marked a significant milestone in the evolution of medical billing and coding. The International Classification of Diseases (ICD) was first implemented in the USA in the 1940s, providing a uniform way to categorize diseases and conditions. The American Medical Association (AMA) introduced the Current Procedural Terminology (CPT) codes in 1966, offering a standardized language for reporting medical procedures and services.
These coding systems revolutionized medical billing by improving accuracy and consistency. They facilitated better communication among healthcare providers, insurers, and regulatory bodies, leading to more efficient and reliable billing processes.
The Digital Revolution: Electronic Health Records (EHRs)
The advent of computers and digital technology in the late 20th century brought about a paradigm shift in medical billing and coding. The introduction of Electronic Health Records (EHRs) in the 1990s transformed how patient information was documented, stored, and accessed. EHRs replaced paper records with digital versions, enabling faster and more accurate data entry, retrieval, and sharing.
EHRs significantly enhanced the efficiency of billing and coding processes. They integrated with practice management systems and coding software, automating many tasks that were previously manual. This automation reduced errors, streamlined workflows, and improved compliance with coding standards and regulations.
The Impact of HIPAA and HITECH
The Health Insurance Portability and Accountability Act (HIPAA) of 1996 and the Health Information Technology for Economic and Clinical Health (HITECH) Act of 2009 were pivotal in shaping modern medical billing and coding. HIPAA established national standards for electronic health transactions, including billing and coding, to protect patient privacy and ensure data security.
HITECH further accelerated the adoption of EHRs by providing incentives for healthcare providers to transition from paper to electronic records. These legislative acts underscored the importance of secure, standardized, and efficient billing and coding practices, driving widespread implementation of advanced technologies and protocols.
The ICD-10 Transition
One of the most significant recent changes in medical billing and coding was the transition from ICD-9 to ICD-10 in 2015. ICD-10 introduced a much larger and more detailed set of codes, expanding from around 13,000 to over 68,000 codes. This change aimed to improve specificity in diagnosis and treatment documentation, leading to better patient care and more accurate billing.
The transition to ICD-10 posed challenges for healthcare providers, requiring extensive training, system upgrades, and process adjustments. However, it ultimately enhanced the granularity and accuracy of medical coding, supporting more precise billing and improved healthcare analytics.
The Role of Artificial Intelligence and Machine Learning
As we move further into the 21st century, artificial intelligence (AI) and machine learning (ML) are poised to revolutionize medical billing and coding. These technologies can analyze vast amounts of data quickly and accurately, identifying patterns and anomalies that might be missed by human coders. AI-powered coding systems can automate complex coding tasks, reducing the burden on healthcare professionals and minimizing errors.
Machine learning algorithms can also enhance predictive analytics, helping healthcare providers anticipate billing issues and optimize revenue cycle management. The integration of AI and ML into billing and coding processes promises to further streamline operations, improve accuracy, and support better decision-making in healthcare.
Conclusion
The evolution of billing and coding in USA over the decades reflects broader changes in healthcare, driven by technological advancements, regulatory reforms, and the growing complexity of medical practice. From manual processes and paper records to standardized coding systems, electronic health records, and AI-driven innovations, billing and coding have transformed significantly. These changes have improved accuracy, efficiency, and patient care, ensuring that healthcare providers can focus more on delivering high-quality services. As technology continues to advance, the future of medical billing and coding holds even greater potential for innovation and improvement.
For more information visit:
https://www.hrvelitercm.com/
0 notes