#wilhelm rontgen
Explore tagged Tumblr posts
Text

Roentgenium is named after Wilhelm Röntgen, discoverer of X-rays. It is predicted to be a noble metal, since calculations indicate its atomic radius and ionization potential is similar to that of gold.
15 notes
·
View notes
Text

08.11.1895 г. – Вилхелм Рьонтген открива в университета на Залцбург Х-лъчи, по-късно известни като рентгенови лъчи. Изображение: www.britannica.com
1 note
·
View note
Text
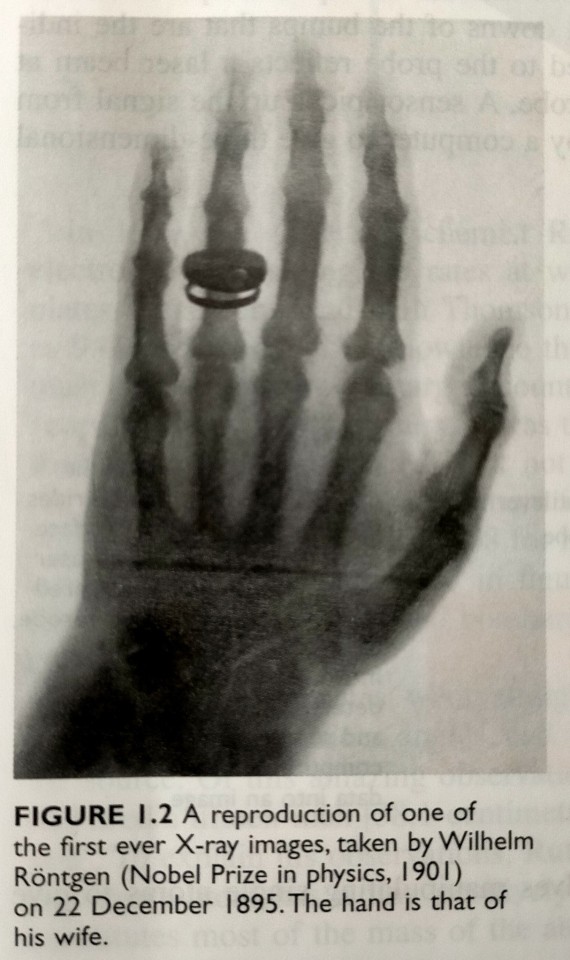
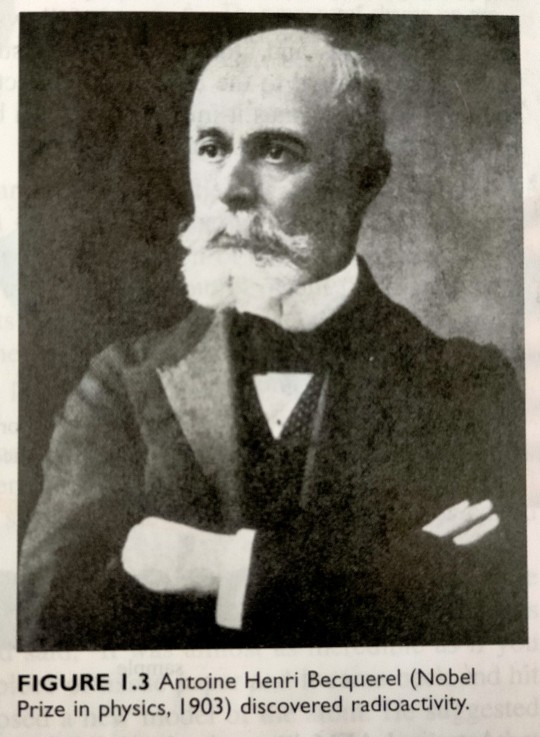
In particular, the discovery of radiation in the form of X-rays by Wilhelm Röntgen (1845-1923) in 1895 (see figure 1.2) and radioactivity by Antoine Henri Becquerel (1852-1908, pictured in figure 1.3) in 1896 led scientists to believe that the atom was composed of discrete particles, as both forms of radiation involve the release of particles from atoms, thought at that time to be indivisible.
"Chemistry" 2e - Blackman, A., Bottle, S., Schmid, S., Mocerino, M., Wille, U.
#book quotes#chemistry#nonfiction#textbook#scientific discovery#radiation#x ray#wilhelm rontgen#90s#1890s#radioactivity#antoine henri becquerel#atom#particles
1 note
·
View note
Note
very into the forensic lore :) give us more facts!! i also love radiology!
I absolutely adore forensics! I was originally going to study it in college however, another subject caught my heart.
Facts for you; Your digestive track is taller than you, if you were to spread it out. It can be up to 9 meters long/30 feet long.
The first X-ray was done on Wilhelm Rontgen’s wife’s hand! Interesting because he was the discoverer and just imagine loving so much you’d be their test rat 💞.
4 notes
·
View notes
Text

Northfleet and Swanscombe Standard (Gravesend, Kent) - Saturday 03 October 1896
Source: British Newspaper Archive
This was published just under a year after X-Rays were discovered in December 1895 by Wilhelm Rontgen. It must have been so surreal to be able to see under your skin.
4 notes
·
View notes
Text
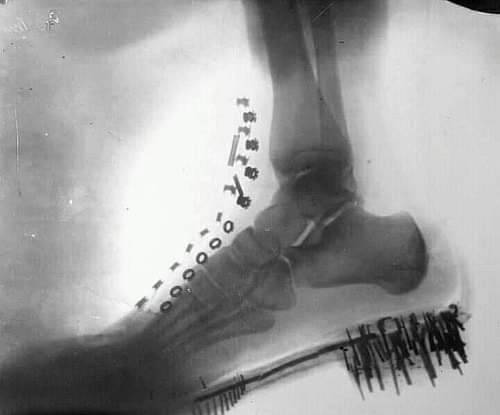
X-Ray Image Taken By Nikola Tesla (1896)
The discovery of X-rays is credited to German scientist Wilhelm Roentgen for first detecting the electromagnetic radiations by accident in his 1895 experiments where he was testing whether cathode rays could pass through glass. Not many know this, but Nikola Tesla was experimenting in the same field prior to Roentgen and published his experimental results in numerous scientific periodicals during the early 1890s. Since these rays were still unknown Tesla used the term “radiant matter" to describe these radiations. Tesla produced some of the first X-ray imaging, which he called “shadowgraphs,” but his laboratory caught fire on March 13, 1895, and Tesla would lose everything including all photos and paperwork.
He would later give all credit to Rontgen for the discovery, and throughout the next few years produced some of the best X-ray images that even Roentgen praised. Tesla would also be the first scientist to warn the scientific community about the harms of X-rays, and designed methods to use them correctly.
69 notes
·
View notes
Text
youtube
idk why i was expecting this to have the scream of wilhelm rontgen discoverer of the xray in it
26 notes
·
View notes
Text
Portable X-ray machine - The precise "viewing eye" in surgery
1. The birth of medical X-ray machine: a hundred years from laboratory to operating room
On November 8, 1895, German physicist Wilhelm Rontgen discovered a mysterious ray that could penetrate books, wood, and even human bodies while experimenting with a cathode-ray tube in his laboratory. Due to its unknown nature, Rontgen named this ray "X-rays." He used X-rays to take a photograph of his wife's hand bone, which clearly showed the outline of the bone and the ring. This photograph became a landmark in medical history.

2. The "growth history" of X-ray machines in surgical applications: from post-confirmation to real-time guidance
Early stage (early 20th century to 1980s): X-ray was only used for preoperative or postoperative radiography to assist in judging the reduction of fracture or the position of foreign bodies. It could not be involved in real time during surgery, and doctors had to rely on experience to operate, with a high error rate.
Digital transformation (1990s-2010): CR (computer radiology imaging) and DR (digital radiology imaging) technologies are popularized, X-ray machines can realize digital imaging, and images can be quickly obtained through flat panel detectors during surgery, but the equipment still needs to be fixed and installed, and the mobility is limited.
Portable Breakthrough (After 2010): As medical needs evolved towards "precision and minimally invasive" procedures, real-time intraoperative imaging guidance became essential. Portable X-ray machines emerged to meet this demand, compressing the device size to a portable level. Combined with wireless transmission technology, they allow doctors to access high-definition images at any time during surgery, completely transforming the traditional "blind operation" model.
3. Technological innovation of portable X-ray machine: Bojin is at the forefront
Miniaturized design: using integrated ball tube and detector, the weight is as low as 9 pounds (about 4.1kg), some models support handheld operation, with wheels can flexibly shuttle in the operating room, ward.
Low radiation and high clarity: Through micro-focus ball tube (0.4mm focus) and short exposure technology (minimum 0.02 seconds), the resolution of 50LP/cm can be achieved while reducing the radiation dose by more than 80%, and the fine structures at the millimeter level (such as fracture lines in children, foreign bodies in soft tissues) can be clearly displayed.
Intelligent interconnection: It supports wireless connection with computers, real-time image and video storage, and is convenient for postoperative review or remote consultation. For example, in orthopedic surgery, images can be synchronized to the cloud for real-time guidance by multidisciplinary experts.
4. Why do you need a portable X-ray machine? Three core requirements drive it
1. Timeliness in emergency situations
Traditional large X-ray machines cannot be quickly deployed to emergency sites (such as car accidents and disaster rescue), while portable devices can be carried by ambulances or medical staff to provide imaging diagnosis for trauma patients (such as suspected fractures and foreign body puncture) in the first time, so as to avoid aggravating injuries due to delay in transportation.
2. Precision upgrades in surgery
In orthopedic surgery, traditional surgery requires multiple pauses and transfer of the patient to the imaging department for film confirmation, which is time-consuming and increases the risk of infection. Portable X-ray machines can complete real-time fluoroscopy directly at the edge of the operating table, such as:
When closed reduction is performed, the alignment of the fracture ends should be observed immediately;
When intramedullary nails or external fixators are implanted, the angle and depth of the instrument should be adjusted accurately to reduce the damage to the patient caused by repeated operations.
3. Adaptability to special scenarios
Mobile health needs: Portable devices can fill the gap of imaging equipment in primary hospitals in remote areas, community health care or home visits;
Special department requirements: pediatric surgery should avoid repeated movement of children, portable X-ray machine can be completed beside the incubator; in oral implant surgery, the position of implants can be confirmed immediately to improve the success rate of surgery.
From the discovery of X-rays by Rontgen to the widespread use of portable devices, every innovation in medical imaging has centered on "making diagnoses more timely and accurate." Portable X-ray machines are not just instruments; they are key hubs for the decentralization of medical resources and the improvement of diagnostic efficiency. With their "lightweight" bodies, they are leveraging "heavy" life care.
0 notes
Text
Contrast Agent Uses in Radiology Imaging

Contrast media are chemical agents used in various radiology imaging procedures, including X-rays, computed tomography (CT), ultrasound, magnetic resonance (MRI), and fluoroscopy. Rather than taking the form of dyes, which could permanently discolor organs within the body, they undergo temporary changes when imaging tools are applied. This increases the contrast, or specificity, by which organs, tissues, and areas of inflammation are viewed.
Each modality employs its specific contrast media. Iodinated contrast agents are common in CT and angiographic studies, while agents containing the rare earth mineral gadolinium are used in MRI scans.
The first use of contrast materials came in the wake of Wilhelm Rontgen’s 1895 discovery of X-ray as a non-invasive way of visualizing the body’s internal structures. Initially used for diagnosing bone fractures and breaks, the images tended to be muddied and unclear. Radiologists found that barium sulfate, potassium bromide, and other simple salts enhanced tissue contrast, which came at a toxicity cost.
In 1906, Heinrich Albers-Schonberg developed iodopyrine, an iodine-based contrast agent that could be taken orally or injected. Iodine has an elevated atomic number, which increases X-ray absorption within tissues that contain the agent. This, in turn, improves radiographic image contrast. Unfortunately, its ionic structure often results in nausea or severe allergic reactions.
From the 1920s onward, scientists moved a series of nonionic iodine-based agents along the development pipeline, culminating in iodixanol. Introduced in the 1950s, this pioneering nonionic agent led to subsequent commercial products such as ioversol, iopamidol, and iopromide. By the 1980s, these had been refined as monomeric nonionic agents that brought risks of adverse reaction to an extremely low level. Today’s Iodinated contrast agents combine water solubility with intravenous administration.
Gadolinium (III) ions (Gd3) interact with the body’s chelating agents, creating hydrophilic, stable complexes. However, contrast agents for MRI imaging did not significantly develop until the 1980s, when gadolinium-based contrast agents (GBCAs) came onto the market.
Approved by the FDA in 1988, gadopentetate dimeglumine (Magnevist) shortens T1 water molecules’ relaxation time in tissues, which boosts MRI scan clarity and detail. When the MRI scanner is applied, water protons’ magnetic field is aligned, while a radiofrequency pulse disrupts this alignment. The T1 relaxation time indicates how long the return to equilibrium requires. Various tissues have their inherent T1 values, which boosts MRI contrast. While generally considered safe, GBCAs do carry risks of nephrogenic systemic fibrosis (NSF) among some kidney disease patients.
Microbubble contrast agents are commonly used with ultrasound imaging and allow for real-time blood flow and tissue perfusion evaluation. Manufactured as lipid-encapsulated gas microspheres, they have enough girth to reflect acoustically, boosting ultrasound signals while being small enough to travel unhindered throughout the circulatory system. This allows the accurate monitoring of cardiac function and liver lesions. Nanoparticulate systems are a current research focus for contrast agents and encapsulated therapeutic agents.
While no longer used in most X-rays, the radiopaque contrasting agent barium sulfate remains a mainstay of gastrointestinal (GI) radiography. Coating the GI tract, it contrasts mucosal details and outlines elements such as the small intestine, stomach, and esophagus. This enables the identification of reflux disease, peptic ulcer, hernias, and gastric tumors. It may also be introduced as an enema for colorectal cancer and inflammatory bowel disease.
1 note
·
View note
Text
¶ … Future of Radiology and X-Ray Technologists By tracing the historical development of radiography as a distinct field of diagnostic treatment, along with the evolving role of X-ray technologists in the delivery of quality health care within the public hospital/private practice model, it is possible to identify the attributes of this field that make it a foundational science within the practice of modern medicine. The ever-expanding ranks of X-ray technologists now serve a variety of essential functions within the health care delivery system, assisting in the cutting edge diagnostic assessment process that has improved patient acuity rates so drastically since the discovery of X-rays in the late 19th century. This paper will trace the development of radiography, radiology, and X-ray technologists within the medicinal realm, including a review of the field's past, present and future and the implications of this science for the further improvement of positive patient outcomes through preventative medicine. Introduction As the medical profession gains a greater understanding of the various approaches to healthcare delivery, the concept of segmenting the services proscribed to a patient into primary, secondary, and tertiary care has emerged as one of the most useful advancements in the field. The preventative measures advocated by proponents of primary health care (PHC) are designed to improve a patient's quality of life in such a way as to reduce or eliminate their prospects of becoming ill or injured. Among the fundamental precepts of PHC are the administration of immunizations to guard against viruses and other contagious infections, the development of a nutritious daily diet to improve the body's natural immune defenses, and the use of X-Ray technology and other radiological methods to detect abnormalities within bones, organs and blood. The increasingly prevalent use of radiology as a fundamental technique within the delivery of PHC has been documented by a number of empirical statistical studies, and on average "radiology was requested for 12% of patients seen: males 39.40% and women 60.59% & #8230; (and) the radiological findings caused 18.72% of doctors to change their therapeutic approach or diagnostic opinion, with mammographies (38.46%), barium meals (35.29%) and abdominal ecographies (31.57%) representing the most effective radiological investigations in terms of relevant findings" (Nicolas & Fernando, 1996). The evolution of radiology as a branch of medical science, and the ever-expanding role of X-ray technologists in modern hospitals and health care centers, warrant further study in order to ascertain the importance of this field during the past, present and future. Radiology's Past During the twilight of the 19th century, the German physicist Wilhelm Conrad Rontgen detected for the first time a curious form of radiation that, while passing readily through clothing and human tissue, remained unable to penetrate bone, metal and other solid matter. While Rontgen's discovery of what he termed the "X-ray" in 1895 was significant in its own right -- as evidenced by Rontgen's reception of the Nobel Prize in Physics for his pioneering research -- the work of contemporaries like the English surgeon John Hall-Edwards and professor of medicine Gilman Frost soon made it clear that the study of X-rays and the emerging field of radiography had clear implications for the improvement of health care delivery. Nurses, physicians and surgeons soon realized that the ability to scan skeletal images for the presence of fractures, or to observe subcutaneous images while detecting the presence of metallic foreign objects like bullets, presented a monumental progression in diagnostic methodology, and throughout the 20th century radiography was expanded to include crucial fields of medical inquiry such as ultrasound imaging, mammography, fluoroscopy, magnetic resonance imaging (MRI) and other techniques now considered to be routine. Radiology's Present Today, the position of X-ray technologist -- also known as radiologist -- has become a one of prominence within the medical community, and aspiring health care professionals typically gravitate towards radiography as a field of study because of the implied guarantee of job security and opportunity for career advancement. Indeed, contemporary studies on the expanding duties of X-ray technologists have revealed that "over the last two decades there have been a series of changes in medicine, technology, and national healthcare funding that have significantly changed the role that the radiologist plays in the healthcare system" (Knechtges & Carlos, 2007), and with the diversification of applications for radiology in the clinical setting, nearly all aspects of emergency care involve one form of internal imaging or another. Radiology's Future As the expansion of scientific research on the applications of radiology and X-ray technology continues its accelerated pace of progression, the future of this field is one defined by unlimited potential. There are dozens of distinct positions within the industry that are continually available to qualified candidates as the health care industry continues to integrate x-ray technology, and while "it might be expected that recent growth in radiological services would be mainly in the areas of ultrasound, computed tomography, magnetic resonance imaging, and interventional procedures & #8230; analysis of Medicare statistics shows substantial growth in the requirement for plain radiography" (Smith & Baird, 2007). This trend is especially encouraging for radiology students because the prospect of growing job market provides ample motivation for the lifelong expansion of one's specialized skill set. An extended literature review on current uses of radiographic imaging demonstrates this encouraging trend, revealing other diversified subfields such as "ultrasonography & #8230; radionuclide imaging, laser Doppler velocimetry, and particle image velocimetry" (Fouras et al., 2009), and the continual discovery of new medicinal advantages to be derived from Rontgen's century-old yet still impactful discovery of X-rays bodes well for medical students aspiring to enter the radiological technician profession. References Fouras, A., Kitchen, M.J., Dubsky, S., Lewis, R.A., Hooper, S.B., & Hourigan, K. (2009). The past, present, and future of x-ray technology for in vivo imaging of function and form. Journal of Applied Physics, 105(10), 102009-102009. https://www.paperdue.com/customer/paper/radiology-past-present-and-future-126255#:~:text=Logout-,RadiologyPastPresentandFuture,-Length3pages Knechtges, P.M., & Carlos, R.C. (2007). The evolving role of radiologists within the health care system. Journal of the American College of Radiology, 4(9), 626-635. Nicolas, D., & Fernando, P.M. (1996). Analysis of the use of radiology in primary health care. Atencion primaria/Sociedad Espanola de Medicina de Familia y Comunitaria, 17(1), 52-56. Smith, T.N., & Baird, M. (2007). Radiographers' role in radiological reporting: a model to support future demand. Medical journal of Australia, 186(12), 629. Read the full article
0 notes
Photo

Wilhelm Röntgen (27 March 1845 – 10 February 1923)
17 notes
·
View notes
Photo

On November the 8th 1895 physicist Wilhelm Rontgen (1845-1923) experimented with electro-magnetic waves and accidentally discovered x-rays. This opened up several whole new fields of medicine. Rontgen was was the winner if the first Nobel prize for physics, given in 1901.
3 notes
·
View notes
Photo
Wilhelm Röntgen was born on March 27, 1845. A German mechanical engineer and physicist who, on November 8, 1895, produced and detected electromagnetic radiation in a wavelength range known as X-rays or Röntgen rays, an achievement that earned him the inaugural Nobel Prize in Physics in 1901. In 2004 the International Union of Pure and Applied Chemistry (IUPAC) named element 111 roentgenium after him.
#wilhelm rontgen#physics#x-rays#nobel prize#nobel prize winners#first nobel prize in physics#science#today in science history#science birthdays#on this day#on this day in science history#roentgenium
1 note
·
View note
Text
I see what you did there…a (very) brief history of imaging the brain: X-rays to CT scans
A little #neuro #science #history on the development of #brain imaging# This time: #X-rays and #CT #scicomm #writing #blogging

View On WordPress
#Allan Cormack#angiography#Antonio Moniz#CT#Godfrey Hounsfield#MRI#neuroimaging#Nobel Prize#pneumoencephalography#Walter Dandy#Wilhelm Rontgen#X-Rays#Your Brain through...History#Your Brain...in Images
0 notes
Text
2021.1 - TOTAL GAMMA RADIATION IN AMERICA
2021.1 – TOTAL GAMMA RADIATION IN AMERICA
PLUS 132 previous months By Bob Nichols February 13, 2021 2021.1 – TOTAL GAMMA RADIATION IN AMERICA January 1, 2010 thru January 31, 2021, or 97,176 hours 01-01-2010 to 1/31/2021, 97,176 Hours City, State 01-01-2021 to 1/31/2021, 744 Hours 2020 8,744 Hours TGR CPM 2010-2019 TGR CPM 895,990,514 Colorado Springs, CO. 6,549,674 75,753,478 813,687,362 894,581,202 Raleigh,…

View On WordPress
#"...on the Road to Extinction"#"Two questions are: How much Gamma radiation have YOU absorbed … Today? … from 10 years ago?"#Have a wonderful radioactive weekend and remember to Dodge the Rads-it’s dangerous out there.#MILLION A WEEK CLUB#Nuclear Industry Lobby#Table of Poisoned American Cities#We Are The Media Now#Wigner Effect#Wilhelm Rontgen#YRTW.org
0 notes
Photo
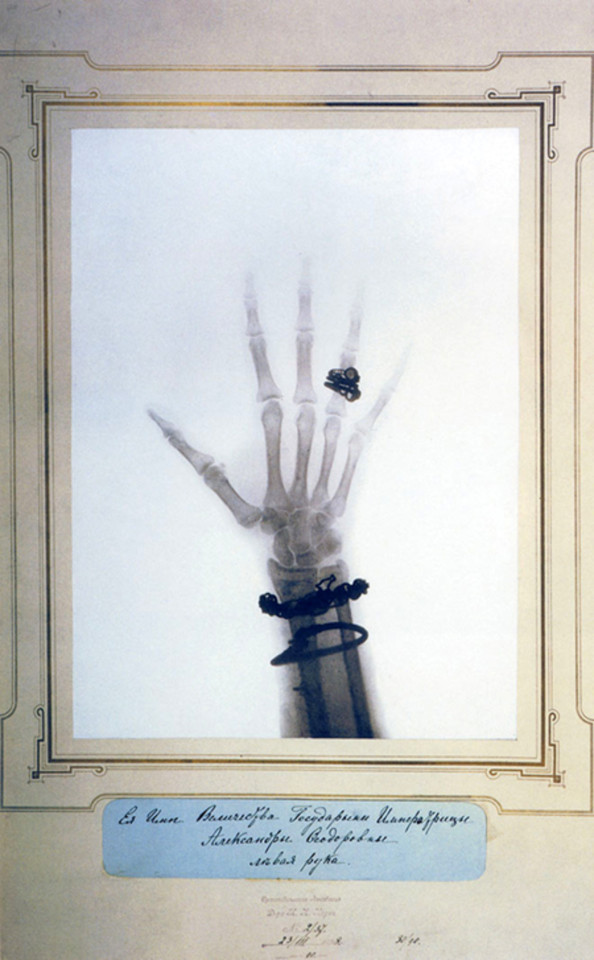
An X-ray image of a hand bearing a wedding ring was featured in the exhibition “Brought to Light: Photography and the Invisible, 1840–1900,” at San Francisco’s Museum of Modern Art.
#Brought to Light: Photography and the Invisible 1840–1900#X-ray#visible/invisible#hands#Wilhelm Conrad Röntgen#Wilhelm Roentgen#Existential Horror#Rontgen rays
58 notes
·
View notes