This blog is an informative analysis of eating disorders as done by Omali Senaratna of UCSD's Psych 134 class.
Don't wanna be here? Send us removal request.
Photo

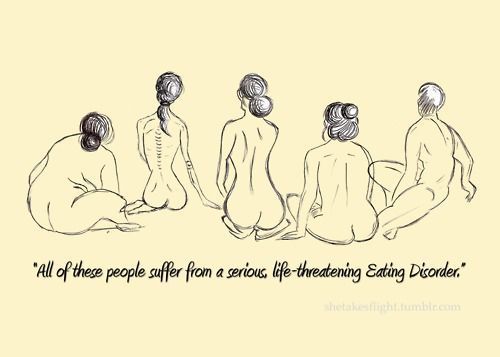
5 MYTHS OF EATING DISORDERS
1. Eating Disorders Only Affect Rich White Adolescent Girls
Eating disorders do not discriminate by age, gender, socioeconomic status or race.
2. Eating disorders are primarily about food, “Just Eat”
Eating disorders are not just about food there are nuerobioloical, sociocultural and psychological stressors that can change someone’s eating behaviors. “Just eating” will not solve an eating disorder, but therapy and support can be a start.
3. Men don’t suffer from eating disorders and those that do tend to be gay
Sexual orientation has no correlation with the development of an eating disorder. And 1 in every 3 eating disorder cases are male (roughly 4-7 million). Many don’t seek treatment because of this stigma.
4. People who are normal or overweight cannot have eating disorders
An eating disorder is not always easy to detect based on weight. Bulimics, compulsive eaters, men suffering from muscle dysmorphia don’t look necessarily thin but they are classifications of eating disorders.
5. Eating disorders are a disease by choice or for vanity
People don’t choose to have eating disorders. They slowly develop over time and have complex psychiatric and physiological symptoms. Its more than a choice, its a completely different type of thinking that needs treatment to address complex medical and underlying issues.
1 note
·
View note
Photo

Eating Disorders: A Historical Perspective
There has been historical accounts all the way back to the 4th century that cites self-starvation but anorexia nervosa wasn’t identified formally until 1873 by William Gull. In the 17th and 18th centuries, women who partook in self-starvation were dubbed “miraculous maids, and in the 18th and 19th centuries as “fasting girls”. The first male case of AN was seen as early as 870 AD, even though men weren’t recognized in any peer-reviewed journals as subjects who experienced AN until 1972.
Bulimia nervosa was first categorized by Gerald Russel in 1979 however symptoms of purging could be traced back to ancient texts as a form of “self-cleansing”. The first bulimia nervosa case study was the 1921 case of Ellen West. Bulimia was defined as “violent hunger attacks” initiated by small amounts of food. BN didn’t become a diagnosis until 1979 though because the weight and shape concern wasn’t identified until 1940.
From history we have seen how the majority of women restricting AN eventually expand into bulimic behaviors and at some point fulfill the BN diagnosis. In the Minnesota Semi-Starvation study researchers wanted to determine the physiological and psychological effects of severe and prolonged dietary restriction. Soon after there were marked psychological distress and a loss of controlled eating amongst the participants.
“Ed-like Behaviors” remained after the experiment where the men complained of still being hungry after large meals. Thereafter resulted in binge eating and associated purging. Binge eating disorder was added to DSM-5 in 2013.
From studying the historical perspective, researchers have recognized core behavioral features of eating disorders that have presented for centuries. With this we can examine the biological impact of behaviors and treatment implications.
0 notes
Photo



There are 8 feeding and eating disorders identified in the DSM-V: 1. Pica is the repetitive oral ingestion of items that aren’t edible, like ash or shampoo, for at least a month. Eating nonfood substances must be developmentally and culturally inappropriate for the individual; however, that’s why it cannot be diagnosed to children under 2 years. Additional attention may be needed if eating behaviors are within the context of another mental disorder. 2. Rumination disorder pertains to the repeated regurgitation of food, (re-chewed, re-swallowed, spit out of food) occurring over a month. Regurgitation cannot be an associated medical condition; and cannot occur with AN, BN, BED or avoidant/restrictive food disorder. Additional attention may be needed if eating behaviors are within the context of another mental disorder. 3. Avoidant-Restrictive Food Intake Disorder (ARFID) is an eating/feeding disturbance manifested by persistent failure to meet appropriate nutritional/ energy needs. There is significant weight loss, nutritional deficiency, dependence on supplements, and marked interference in psychosocial functioning. It’s common in children but can manifest in adulthood. Higher likeliness of onset if child has gastrointestinal concerns, growth delay, Mother with an eating disorder, and “prone to being perfect”. Common in males with Autism spectrum disorder. 4. Anorexia Nervosa (AN) is defined by a restriction of energy leading to a markedly low body weight, an intense fear of gaining weight, disturbance in the way one experiences their body or shape, with complete lack of recognition of one’s current low body weight. The subtypes are restricting (AN-R) and binge eating/purging (AN-BP). Onset begins in adolescence (rarely before puberty or after 40) due to life event. Mortality rate is 5% per decade. Behaviors consist of significantly reduced quantity of food eaten/variations of foods and ritualistic obsessive qualities (cutting food into tiny pieces). BMI of 17 or lower to be diagnosed. (not an official DSM-5 diagnosis) Orthorexia is wanting to attain a certain body type by focusing on health rather than food, but there is an obsession with “pure, clean” eating. These patients neglect other areas of life and their goal may not be thinness. 5. Bulimia Nervosa (BN) has recurrent episodes of bingeing (lack of control eating) and purging (self-induced vomiting, fasting, excessive exercise) at least once a week for 3 months. Unlike anorexia, person is slightly overweight/ has normal BMI. Mortality rate is 2% per decade. Behaviors include secret/rapid eating behaviors and exercise routines, prioritizing compensatory behaviors over everything. The BN emotional dysregulation is a cycle of having a trigger/stressor that heightens anxious feelings and to reduce/ stop this emotion a behavior is initiated which grants temporary relief but then the person experiences disgust and guilt 6. Binge eating disorder is the newest and also has recurrent episodes of bingeing a large about of food within a small window of time showing a lack of consumption control for at least once a week for 3 months . 7. Other Specified Feeding/ Eating disorders is seen in 50% of all diagnosed ED, with rates of death similar to AN. Atypical anorexia nervosa meets criteria for AN despite significant weight loss, individual’s weight is within/ above normal limits. Purging disorder shows recurrent purging behavior to influence weight or shape in absence of binge eating. 8. Unspecified feeding or eating disorder is basically a diagnosis that shows symptoms related to another ED but there isn’t enough to diagnose;
There are a lot of psychiatric comorbidities associated with ED, the most common being affective disorders (depression/bipolar), anxiety (PTSD, OCD), Personality disorders (BPD), substance abuse
Suicidality is very rampant in those with ED- about 20% AN and 35% BN subjects had attempted, while 4% of AN subjects committing suicide.
In asking why eating disorders exist, scientists point to run-away diets, the diet culture itself and acknowledge the sociocultural influences of media and neurochemistry. Acknowledging eating disorders is important in today’s world because there has been sharp increases over the past several years of onset, it has low recovery rates and higher mortality in comparison to other psychological disorders. There isn’t a certain look to someone who is suffering from an eating disorder because it happens to everyone regardless of culture, race, age, socioeconomic background or sexuality.
0 notes
Photo


Neurobiology of Eating Disorders
Most eating disorder treatments do not acknowledge the brain’s mechanisms regarding the syndrome. Familial studies have recently shown specific heritable genes projecting childhood (pre-morbid) traits such as perfectionism, anxiety, sensitivity, etc., suggesting an important neurological component within eating disorders. These disorders exhibit temperament and personality traits that are related to the neural circuit functioning of an individual, and are significant in it’s growth and maintenance. This neurological temperament is quantified as elevated anxiety (harm avoidance), altered reward sensitivity, altered cognitive inhibition and flexibility, and an altered interoceptive awareness. Eating disorders (ED) are not necessarily a disturbance of appetite regulation, instead it seems to be dependent on a balance between the parts of the brain that control rewards and inhibition. For example, healthy people experience a pleasurable reward when eating, on the other hand, food has the potential to incite extreme emotional dysregulation in those with ED. Anorexia nervosa (AN) has 3 temperamental biases: the difficulty to encode rewards and initiate motivation, an increase of anxiety in regards to exaggerated perceptions of risk or change and a rigid control to avoid that anxiety. Therefore eating disorders reflect a inconsistency between one’s physiological need to eat and the neural motivation to eat. Homeostatic hunger is determined by the release of either ghrelin, the hunger hormone, or leptin, the satiety hormone, as regulated by the hypothalamus, which identifies energy balance.
There are 3 primary circuits in the brain associated with AN neurobiology. Inhibitory control circuit is located in the prefrontal and frontal cortex, consists of cognitive control, behavioral inhibition, planning and judgement. The reward circuit of the nucleus accumbens, medial forebrain bundle, and ventral tegmental area acknowledges rewards, emotionally significant stimuli and generates the associated emotional response. Emotion regulation circuits contain the amydala and support the regulations of both positive and negative emotions and their conditioned effects. All three circuits react with the self-regulatory circuits; which explains the cycle in bulimia nervosa (BN) due to dysphoria and the brief euphoria associated with bingeing which manifests into a more intensified dysphoria afterwards. The salience circuit assesses interoceptive cues (taste, pain, fullness) and assimilates the cues with certain motivational and emotional processes. The insula of the salience circuit is very important as it incorporates self-awareness, the primary taste cortex and is the link between mental processes and body state. A study of taste pathways analyzes at MRIs of the brains of recovered ED patients when they tasted sucrose. Recovered AN patients had decreased activation in the reward centers of the insula, caudate and putamen- stating there is no response to rewards but rather associated anxiety. In the same study with Rec BN patients, MRIs showed greater sensitivity to the satisfying taste in the insula, explainging the propensity to binge eat in order to activate reward response. In another study analyzing potential reward processing in a game setting of winning or losing money, showed that regardless if the Rec AN patient won or loss they had an elevated reward circuitry. This suggests that AN patients may not be able to differentiate positive from negative rewards due to an underactive limbic response and an overactive executive inhibition. Rec BN patients on the other hand showed a decreased reward and cognitive response, because the reward cognition is negatively generalized it could explain why many ED patients don’t see treatment as rewarding.
Appetite regulation studies show that in the control groups and Rec BN, hunger increased brain response for rewards. In Rec AN there was little response to hunger, indicating that hunger is not a driving motivation for these patients to eat and explains their resistance to temptation. In both EDs, decreased brain reward responses to sucrose when hungry was associated with patients’ lowest lifetime BMI.
In a hunger study testing the possibility of delayed gratification between a smaller immediate reward or larger reward in the future, Rec ANs showed increased prefrontal cognitive control processing by choosing the delay regardless of hunger. The control group showed an increased response to rewards when hungry while Rec BN did not show difference in brain response to reward when hungry nor satiated. Decreased brain reward response in ED patients showed increase anxiousness, however.
Approach and avoidance refers to incentive processing and its ability to guide behavior through motivation. In an approach setting, if there is a good mismatch between anticipated and actual outcomes (prediction error) a positive experience with the outcomes would mean a greater approach in the future. It does not work with feeding ED patients; however, because their fear is still present. This could be a result of not actively learning and having a fixed mindset (expectancy).
Dopamine and its sensory rewards can mold learning in many by becoming conditioned by a stimulus to provide the positive feeling of dopamine. In spite of that, dopamine differences in binding presented in ED cases are actually associated with experiencing high anxiety and harm avoidance.
In summary, for those affected by EDs, food generates a risk signal and not eating reduces the aversive feeling of anxiety. There is little motivation to eat or acknowledge being hungry- enhancing the ability to inhibit eating.
Medical Complications of Eating Disorders
Eating disorders effect basically every system and subcell of the body. Even after patients seek treatment it is a long journey to reconstruct the person’s body, mind, and spirit.
Malnutrition is a deficiency of both macro and micronutrients. This can be defined by a greater than 10% loss of body weight or BMI less than 80%; severe malnutrition is identified as greater than 20% loss of body weight. One can be malnourished even with a normal/high BMI just depending on how much and how fast the weight got lost. The disorder’s effect on metabolism and energy are extremely effected as the body goes into survival mode to store energy.
The organ systems of the body are extremely depleted by eating disorders. In the cardiovascular system, the most obvious symptoms are bradycardia, or a low heart rate, (less than 45 bpm risks cardiac arrest) and an inefficient pump due to decreased ventricular wall mass. The combination of the two symptoms can lead to hypotension, hypothermia, orthostatic changes or tachyarrhythmia, the #1 cause of death by eating disorder. The gastrointestinal system may suffer from constipation (as a result of malnutrition or laxative us), delayed gastric emptying (bloating after meals), acid reflux, esophageal issues, increased liver enzymes or pancreatitis. The reproductive system suffers greatly as the pubertal axis is suppressed, low sex hormones in both genders meaning decreased sex drive, and the potential of having potentially irreversible pubertal delay and infertility. The musculoskeletal system may suffer from possibly irreversible height stunting, potentially irreparable decreased bone density, and hematological issues, like anemia or immune suppression. The respiratory system is very susceptible to aspiration pneumonia, inhaling stuff into your lungs like food. Head, neck and dermatologic issues may arise, as result of purging there could be dental erosion, oral abrasions, lanugo (fine baby hair) and Russell sign (deterioration of fingers).
Low fluid and electrolyte consumption, vomiting, and laxative use is related to dehydration and electrolyte abnormalities. This can start refeeding syndrome, where the body changes from starvation mode to rebuilding mode; potentially risking heart failure and death. The consequences of dehydration is low blood pressure or dehydration shock which can lead to organ failure or death. Having electrolyte abnormalities can result in cardiac arrhythmia/arrest, neurological injuries like seizures and water loading, the dilution of electrolytes-specifically the sodium action potentials (ranges from mild [lethargy]-->severe [death])
From a neuropsychiatric point of view, there can be extreme cognition problems relating to memory, learning, judgement, and concentration. Psychiatric comorbidity with anxiety, depression, psychosis and suicidality is extremely high in these patients. Suicide is incidentally the #2 cause of death in eating disorders. Mortality in these patients is the highest than with any other psychiatric illness at 10%.
Hospitalization is a must for these patients to live. They must first help any heart rate or blood pressure issues, temperature and work slowly to regain nutrition. Inpatient treatment is the best choice with goals of weight restoration, behavioral support in oral feeding and symptoms. Being able to reverse everything is doubtful; however, with the proper motivation and support, treatment is seemingly the only option for these patients for another chance at life.
0 notes
Video
youtube
dx

Psychosocial and Cultural Basis of Eating Disorders
The sociocultural theory, which states specific cultural and societal messages influence an individual’s behavior, is important in analyzing the social triggers that can influence one struggling with an eating disorder. The idea of beauty has been molded from the western, white, affluent society. Female beauty is associated with a thinness that can be quickly provided by the diet culture; while male beauty is pronounced by muscular definition through exercise. Secular trends show a significant decrease in female body size throughout the 20th and 21st centuries; correlating with a higher ratio and prevalence of eating disorders in women. The influence of western culture on eating disorders is extremely prominent in cross-cultural longitudinal studies. For example, in Fiji, the positive associations that inhabitants had with "fatness” dramatically changed with the introduction of western television, causing an atypical desire to be thin through purging and disordered eating, in the belief that wealth and success are related to thinness. To understand exactly how this can influence the individual, researchers turn to the four sociocultural models behind eating disorders. The Tripartite model identifies how the combined pressures of peers, parents, and media can lead to self-appearance comparison, which creates body dissatisfaction and eventually prompts a drop in psychological functioning of restricting, bingeing and purging. The Dual Pathway model relates the internalization and the pressure to be thin with body dissatisfaction, promoting negative affects into a bulimic pathology. Both of these models highlight the social learning theory’s pressure to conform to the group (society) and the indirect/direct influences that caused that conformity. The objectification theory comments on the psychological process of the omniscient viewpoint one has of themselves by placing greater emphasis as to how one looks to others- leading to appearance anxiety and shame. Finally, in the biopsychosocial model for males there is also combined pressures of peers, parents, and media that initiates a body-focused anxiety and unhealthy drive for muscularity followed by body dissatisfaction and a decrease in psychological functioning. Western media projects this objectification and an internalization of thinness that creates the impossible ideal, otherwise known as an unrealistic photoshopped “beauty” individuals are expected to achieve (Dove campaign). This impossible ideal can lead to cultural stress and acculturation amongst racial and ethnic minorities, who not only feel marginalized by the media; but also, along with men, face a dramatic lack of representation in eating disorders and, thus, deter from treatment.
0 notes