Text
What are the common risk factors for developing lung cancer?
Several risk factors increase the likelihood of developing lung cancer:
Smoking: This is the leading cause of lung cancer. Cigarette, cigar, and pipe smoking all increase risk. Secondhand smoke exposure is also a significant risk factor.
Exposure to Radon: Radon is a naturally occurring radioactive gas that can accumulate in homes and buildings, especially in areas with certain types of soil or rock. Prolonged exposure to high levels of radon increases lung cancer risk.
Exposure to Asbestos and Other Carcinogens: Occupational exposure to asbestos, arsenic, chromium, nickel, and other carcinogens can significantly increase the risk of lung cancer, especially among smokers.
Family History: Individuals with a family history of lung cancer are at higher risk, indicating a potential genetic predisposition to the disease.
Air Pollution: Long-term exposure to air pollution, such as that from vehicle exhaust, industrial emissions, and other sources, can increase lung cancer risk.
Personal History of Lung Disease: People with a history of certain lung diseases, such as chronic obstructive pulmonary disease (COPD) or tuberculosis, have an increased risk of lung cancer.
Radiation Therapy to the Chest: Previous radiation therapy to the chest, typically for other types of cancer, can increase the risk of developing lung cancer later in life Best Pulmonologist in Sodala .
Dietary Factors: Some studies suggest that a diet low in fruits and vegetables but high in red and processed meats may increase the risk of lung cancer.
Certain Genetic Factors: While less common, certain genetic mutations or conditions, such as mutations in the EGFR gene, are associated with an increased risk of lung cancer.
Gender and Age: Lung cancer is more common in older adults and in males, although the gap has been narrowing in recent years.
Understanding these risk factors can help individuals take preventive measures and make informed decisions about their lifestyle choices and healthcare.

0 notes
Text
What is an asthma action plan?
An asthma action plan is a written, individualized plan developed by a healthcare provider for a person with asthma. The plan outlines how to manage asthma on a daily basis and how to handle worsening symptoms or asthma attacks. It serves as a comprehensive guide for patients, their families, and caregivers to help control asthma and respond to symptoms effectively. An asthma action plan typically includes the following components:
1. Daily Management
Medication Schedule: Detailed instructions on what medications to take daily, including controller medications (such as inhaled corticosteroids) and their dosages.
Peak Flow Meter Readings: If applicable, guidance on how to use a peak flow meter to monitor lung function and what readings indicate good control.
Avoiding Triggers: Information on known asthma triggers (such as allergens, smoke, exercise, cold air) and strategies to avoid them.
2. Recognizing and Handling Symptoms
Green Zone: Indicates good asthma control. This section includes the person's best peak flow readings and outlines the daily routine when symptoms are well-controlled.
Yellow Zone: Indicates caution. This section describes symptoms that suggest asthma is worsening (e.g., increased coughing, wheezing, or shortness of breath) and provides instructions for using rescue medications or other interventions to prevent an asthma attack.
Red Zone: Indicates a medical alert. This section details symptoms of a severe asthma attack (e.g., difficulty breathing, trouble speaking, or very low peak flow readings) and provides clear steps to take, including taking quick-relief medication and seeking emergency medical help.
3. Emergency Contacts and Information
Healthcare Provider Contact Information: Phone numbers for the primary care physician, asthma specialist, and the nearest emergency department.
Emergency Instructions: Clear steps to follow if symptoms do not improve with initial treatment, including when and how to seek emergency medical care.
4. Personal Information
Patient's Name and Contact Information: For easy identification and communication.
Emergency Contact Information: Names and phone numbers of family members or friends who should be contacted in an emergency.
Benefits of an Asthma Action Plan
Improved Asthma Control: Helps patients understand and manage their condition effectively.
Early Detection: Encourages monitoring of symptoms and peak flow readings to detect worsening asthma early.
Clear Instructions: Provides step-by-step guidance for managing daily care and responding to asthma attacks.
Empowerment: Empowers patients and caregivers with knowledge and tools to take control of asthma.
An asthma action plan should be reviewed and updated regularly with the healthcare provider to ensure it remains relevant and effective.

0 notes
Text
What are the common symptoms of asthma?
Asthma is a chronic respiratory condition characterized by inflammation and narrowing of the airways, leading to a variety of symptoms. The common symptoms of asthma, described in detail, are:
Shortness of Breath:
This is a sensation of not being able to get enough air into the lungs. It often occurs suddenly and can be particularly distressing. During an asthma attack, the airways narrow, making it difficult to breathe in and out effectively.
Wheezing:
Wheezing is a high-pitched whistling or squeaky sound that occurs when breathing, especially when exhaling. This sound is caused by the air moving through narrowed or obstructed airways. Wheezing is one of the hallmark signs of asthma.
Coughing:
Persistent coughing is common in asthma, often worse at night or early in the morning. The cough can be dry or productive (with mucus). In some cases, coughing may be the primary or only symptom of asthma, which is referred to as cough-variant asthma.
Chest Tightness:
Many people with asthma describe a feeling of tightness, pressure, or discomfort in the chest. This can feel like a heavy weight on the chest and may make it difficult to take deep breaths.
Increased Mucus Production:
Asthma can cause the airways to produce more mucus than normal, which can block the airways and make breathing more difficult. This mucus can be thick and sticky, contributing to coughing and wheezing.
Difficulty Sleeping:
Asthma symptoms often worsen at night, which can lead to difficulty falling or staying asleep. Nocturnal asthma symptoms like coughing, wheezing, and shortness of breath can disrupt sleep and lead to fatigue during the day.
These symptoms can vary widely in severity and frequency among individuals with asthma. Some people may experience symptoms only occasionally, while others may have persistent and severe symptoms that interfere with daily activities. Additionally, certain triggers such as allergens, exercise, cold air, respiratory infections, smoke, and stress can exacerbate asthma symptoms, leading to an asthma attack or flare-up.

0 notes
Text
Causes of asthma - Symptoms and prevention
Causes of Asthma
Asthma is a chronic respiratory condition characterized by inflammation and narrowing of the airways, leading to breathing difficulties. The exact cause of asthma is not fully understood, but several factors are known to contribute to its development:
Genetics: A family history of asthma or other allergic conditions increases the likelihood of developing asthma.
Environmental Factors: Exposure to allergens (such as pollen, mold, pet dander, and dust mites) and irritants (such as smoke, pollution, and strong odors) can trigger asthma symptoms.
Respiratory Infections: Viral respiratory infections during childhood can damage developing lungs and increase the risk of asthma.
Occupational Exposure: Certain jobs can expose individuals to irritants and chemicals that increase the risk of asthma.
Allergies: Many people with asthma also have allergies, and allergic reactions can trigger asthma symptoms.
Exercise: Physical exertion, especially in cold, dry air, can induce asthma symptoms, a condition known as exercise-induced bronchoconstriction (EIB).
Weather Conditions: Cold air, sudden weather changes, and high humidity can trigger asthma symptoms.
Medications: Some medications, such as beta-blockers and non-steroidal anti-inflammatory drugs (NSAIDs), can trigger asthma symptoms.
Stress and Emotions: Strong emotions and stress can lead to rapid breathing (hyperventilation) and trigger asthma symptoms.
Hormonal Changes: Hormonal fluctuations, such as those during menstruation, pregnancy, or menopause, can influence asthma symptoms in some women.
Symptoms of Asthma
Asthma symptoms can vary in frequency and severity among individuals. Common symptoms include:
Shortness of Breath: Difficulty breathing or feeling out of breath, particularly during physical activity or at night.
Wheezing: A high-pitched whistling sound when breathing, especially during exhalation.
Coughing: Persistent cough, often worse at night or early in the morning. The cough may be dry or produce mucus.
Chest Tightness: A feeling of tightness or pressure in the chest.
Trouble Sleeping: Symptoms such as coughing, wheezing, or shortness of breath can interfere with sleep.
Prevention of Asthma
While asthma cannot be completely prevented, certain strategies can help manage the condition and reduce the frequency and severity of asthma attacks:
Identify and Avoid Triggers: Recognize and avoid allergens and irritants that trigger symptoms. Common triggers include tobacco smoke, pollen, dust mites, and pet dander.
Create an Asthma Action Plan: Work with a healthcare provider to develop a personalized asthma action plan that outlines how to manage symptoms and handle asthma attacks.
Medication Management: Take prescribed medications as directed, including long-term control medications to reduce inflammation and quick-relief inhalers for acute symptoms.
Regular Monitoring: Use a peak flow meter to monitor lung function regularly and detect early signs of worsening asthma.
Maintain a Healthy Lifestyle: Eat a balanced diet, exercise regularly, and maintain a healthy weight to improve overall lung function and reduce asthma symptoms.
Vaccinations: Stay up to date with vaccinations, such as the flu shot and pneumococcal vaccine, to prevent respiratory infections that can exacerbate asthma.
Manage Allergies: If you have allergies, take steps to control them through medications, allergen avoidance, or allergy shots (immunotherapy).
Environmental Control: Use air purifiers, dehumidifiers, and allergy-proof bedding to reduce indoor allergens. Keep living areas clean and well-ventilated.
Stress Management: Practice stress-reducing techniques such as yoga, meditation, or deep-breathing exercises to help manage asthma symptoms.
Educate Yourself: Learn as much as possible about asthma and its management to make informed decisions about your health.
By understanding the causes, recognizing the symptoms, and following preventive measures, individuals with asthma can lead active and healthy lives.

0 notes
Text
Who Is Most at Risk for Developing Lung Disease?
Several factors increase the risk of developing lung disease. Understanding these risk factors can help in identifying individuals who might be more susceptible to such conditions. Here are the key risk groups:
1. Smokers and Former Smokers:
Tobacco Smoke: The primary cause of chronic obstructive pulmonary disease (COPD) and lung cancer. Smoking damages the airways and the alveoli, leading to chronic bronchitis, emphysema, and malignancies.
Secondhand Smoke: Non-smokers exposed to secondhand smoke are also at risk of developing lung diseases, including lung cancer and COPD.
2. Occupational Exposures:
Asbestos: Prolonged exposure can lead to asbestosis, lung cancer, and mesothelioma.
Silica Dust: Workers in mining, construction, and sandblasting are at risk for silicosis.
Coal Dust: Coal miners can develop coal workers' pneumoconiosis (black lung disease).
Chemical Fumes and Dust: Exposure to various industrial chemicals and dust can cause occupational asthma and other pulmonary conditions.
3. Environmental Factors:
Air Pollution: Long-term exposure to polluted air, including emissions from vehicles and industrial processes, can increase the risk of asthma, COPD, and lung cancer.
Indoor Air Pollution: Exposure to indoor pollutants like radon, mold, and certain household chemicals can also contribute to lung disease.
4. Genetic Factors:
Family History: A family history of lung diseases such as asthma, cystic fibrosis, or alpha-1 antitrypsin deficiency increases the risk.
Genetic Mutations: Certain genetic predispositions, like those affecting the CFTR gene in cystic fibrosis, can lead to lung disease.
5. Age and Gender:
Older Adults: The risk of lung diseases increases with age due to cumulative exposure to risk factors and decreased lung function.
Gender Differences: Historically, men have been at higher risk due to higher smoking rates, but rising smoking rates among women have increased their risk as well.
6. Pre-existing Health Conditions:
Chronic Health Conditions: Conditions such as HIV/AIDS, rheumatoid arthritis, and other autoimmune diseases can increase susceptibility to lung diseases.
Respiratory Infections: Frequent respiratory infections, especially in childhood, can cause chronic damage and increase the risk of developing lung diseases later in life.
7. Lifestyle and Socioeconomic Factors:
Sedentary Lifestyle: Lack of physical activity can contribute to poor respiratory health.
Poor Diet: Nutritional deficiencies can impair immune function and lung health.
Socioeconomic Status: Lower socioeconomic status is often associated with increased exposure to risk factors like smoking, air pollution, and poor access to healthcare.
8. Geographical Location:
Living in High Pollution Areas: Urban areas with high levels of industrial pollution and traffic emissions can increase the risk of lung diseases.
9. Immunocompromised Individuals:
Weakened Immune System: Individuals with weakened immune systems due to conditions like cancer treatment, organ transplants, or chronic steroid use are more susceptible to lung infections and subsequent lung disease.
Preventive Measures:
To reduce the risk of developing lung diseases, individuals can take several preventive measures:
Quit Smoking: Avoiding tobacco smoke is the most effective way to prevent lung disease.
Protective Equipment: Using masks and other protective gear in occupational settings.
Reduce Exposure to Pollutants: Minimizing exposure to both indoor and outdoor air pollutants.
Healthy Lifestyle: Maintaining a healthy diet, regular exercise, and adequate hydration.
Regular Check-ups: Regular medical check-ups, especially for those with a family history or other risk factors, to detect any early signs of lung disease.
Recognizing and mitigating these risk factors can help in the prevention and early detection of lung diseases, leading to better health outcomes.

0 notes
Text
What are the main types of pneumonia?
Pneumonia is a lung infection that can be caused by various organisms, including bacteria, viruses, fungi, and parasites. The main types of pneumonia are generally classified based on where and how the infection was acquired. Here are the primary types:
Community-Acquired Pneumonia (CAP):
This type of pneumonia is acquired outside of healthcare settings, such as hospitals or nursing homes.
It is often caused by bacteria such as Streptococcus pneumoniae, Haemophilus influenzae, and atypical bacteria like Mycoplasma pneumoniae.
Viruses, including influenza, respiratory syncytial virus (RSV), and coronaviruses, can also cause CAP.
Hospital-Acquired Pneumonia (HAP):
HAP occurs in patients during their stay in a hospital, typically 48 hours or more after admission.
It is often caused by more resistant bacteria such as Staphylococcus aureus (including MRSA) and Pseudomonas aeruginosa.
Patients with weakened immune systems or those who are on ventilators are at higher risk.
Ventilator-Associated Pneumonia (VAP):
A subtype of HAP, VAP occurs in people who are on mechanical ventilation for at least 48 hours.
The causative agents are often similar to those of HAP, with a higher likelihood of being multi-drug resistant organisms.
Healthcare-Associated Pneumonia (HCAP):
This type includes pneumonia in patients who are in regular contact with healthcare settings, such as nursing homes, dialysis centers, or outpatient clinics.
Like HAP, HCAP can be caused by antibiotic-resistant bacteria.
Aspiration Pneumonia:
Occurs when food, liquid, saliva, or vomit is inhaled into the lungs, leading to an infection.
It is more common in individuals with swallowing difficulties or those who are unconscious or have impaired gag reflexes.
Atypical Pneumonia:
Often referred to as "walking pneumonia," it is typically less severe and has a different clinical presentation.
Caused by atypical bacteria such as Mycoplasma pneumoniae, Chlamydophila pneumoniae, and Legionella pneumophila.
Symptoms are usually milder compared to typical bacterial pneumonia.
Fungal Pneumonia:
Caused by fungi, more common in people with weakened immune systems.
Examples include Histoplasmosis, Coccidioidomycosis, and Cryptococcosis.
Viral Pneumonia:
Common in children and older adults, often caused by viruses such as influenza, respiratory syncytial virus (RSV), and coronaviruses (including SARS-CoV-2).
Each type of pneumonia has different risk factors, causative organisms, and treatments, making accurate diagnosis and appropriate management crucial.

0 notes
Text
What are the main causes of COPD?
The main causes of Chronic Obstructive Pulmonary Disease (COPD) include the following:
Smoking: The primary cause of COPD, accounting for the majority of cases. This includes not only active smoking but also exposure to secondhand smoke. Tobacco smoke damages the lungs and airways, leading to inflammation, narrowing of the airways, and destruction of lung tissue.
Environmental and Occupational Exposures: Long-term exposure to various environmental and occupational irritants can lead to COPD. These include:
Air pollution
Chemical fumes
Dust
Industrial pollutants
Genetic Factors: A genetic disorder called alpha-1 antitrypsin deficiency is a significant risk factor for COPD. This deficiency leads to lower levels of the alpha-1 antitrypsin protein, which helps protect the lungs from damage. Individuals with this condition are more susceptible to lung damage, even if they have never smoked.
Respiratory Infections: Frequent and severe respiratory infections during childhood can impair lung development and increase the risk of developing COPD later in life. These infections can contribute to long-term lung damage.
Age: The risk of COPD increases with age, as lung function naturally declines over time. Most people diagnosed with COPD are at least 40 years old.
Asthma: Individuals with a history of asthma may be at increased risk of developing COPD, especially if they smoke or are exposed to other risk factors.
While these are the primary causes, it is important to note that the interaction between genetic predisposition and environmental factors plays a crucial role in the development of COPD. Preventive measures, such as avoiding smoking and reducing exposure to harmful pollutants, are essential to lower the risk of developing this chronic lung disease.

0 notes
Text
What are the most common respiratory diseases?
The most common respiratory diseases include:
Asthma: A chronic condition characterized by inflammation and narrowing of the airways, leading to episodes of wheezing, breathlessness, chest tightness, and coughing.
Chronic Obstructive Pulmonary Disease (COPD): An umbrella term for progressive lung diseases, primarily emphysema and chronic bronchitis, that cause airflow blockage and breathing-related problems.
Pneumonia: An infection that inflames the air sacs in one or both lungs, which may fill with fluid or pus, causing cough with phlegm, fever, chills, and difficulty breathing.
Bronchitis: Inflammation of the bronchial tubes, often following a cold or respiratory infection, resulting in cough and mucus production. It can be acute or chronic.
Tuberculosis (TB): A serious infectious disease that mainly affects the lungs, caused by the bacteria Mycobacterium tuberculosis, leading to symptoms like a persistent cough, chest pain, and coughing up blood.
Lung Cancer: A type of cancer that begins in the lungs, often associated with smoking, and can cause coughing, chest pain, weight loss, and other symptoms.
Influenza (Flu): A contagious respiratory illness caused by influenza viruses, leading to fever, cough, sore throat, muscle aches, and fatigue.
Pulmonary Fibrosis: A condition in which lung tissue becomes damaged and scarred, making it difficult for lungs to work properly, causing progressive shortness of breath.
Sleep Apnea: A disorder characterized by repeated interruptions in breathing during sleep, leading to poor sleep quality and other health issues.
Allergic Rhinitis (Hay Fever): An allergic response to airborne substances such as pollen, causing sneezing, runny nose, and nasal congestion, which can impact the respiratory system.
These conditions vary in severity and can significantly impact an individual's quality of life. Proper diagnosis and management by healthcare professionals are crucial for controlling symptoms and preventing complications.

0 notes
Text
What are people suffering from respiratory diseases?
People suffering from respiratory diseases experience a variety of symptoms and challenges that can significantly impact their daily lives. Respiratory diseases encompass a wide range of conditions, including asthma, chronic obstructive pulmonary disease (COPD), bronchitis, pneumonia, and lung cancer, among others. Here are some of the common experiences and symptoms associated with respiratory diseases:
Shortness of Breath: Difficulty breathing is a common symptom, especially during physical activity or even at rest in more severe cases.
Coughing: Persistent coughing, which can be dry or productive (producing mucus), is often a symptom of respiratory conditions.
Wheezing: A high-pitched whistling sound when breathing, often associated with conditions like asthma and COPD.
Chest Tightness: A feeling of tightness or pressure in the chest, which can be uncomfortable and distressing.
Fatigue: Chronic respiratory diseases can lead to persistent fatigue and weakness due to the body's reduced ability to get enough oxygen.
Frequent Respiratory Infections: People with respiratory diseases may be more prone to infections like colds, flu, or pneumonia.
Cyanosis: A bluish tint to the skin, lips, or nails, indicating low levels of oxygen in the blood.
Decreased Exercise Tolerance: Difficulty performing physical activities that were once easy, such as walking, climbing stairs, or engaging in sports.
Use of Supplemental Oxygen: In severe cases, patients may require supplemental oxygen to maintain adequate oxygen levels.
Medication Management: Daily management often includes the use of inhalers, nebulizers, or other medications to control symptoms and prevent exacerbations.
Lifestyle Adjustments: Many individuals need to make significant lifestyle changes, such as quitting smoking, avoiding pollutants, and adopting a healthier diet.
Psychological Impact: Chronic respiratory diseases can lead to anxiety, depression, and social isolation due to the limitations imposed by the disease.
Managing respiratory diseases typically involves a combination of medical treatments, lifestyle changes, and sometimes surgical interventions. Regular monitoring and follow-up with healthcare providers are essential to manage symptoms and maintain quality of life.

0 notes
Text
What treatments are available for cystic fibrosis?
Treatment for cystic fibrosis (CF) aims to manage symptoms, prevent complications, and improve quality of life. Common treatments include:
Airway Clearance Techniques: Regular methods such as chest physiotherapy and airway clearance devices help to clear mucus from the lungs, reducing the risk of infection and improving lung function.
Medications: Various medications are prescribed to manage symptoms and complications of CF, including:
Bronchodilators to open airways.
Mucolytics to thin mucus.
Antibiotics to treat lung infections.
Anti-inflammatory drugs to reduce lung inflammation.
Pancreatic enzyme supplements to aid digestion and nutrient absorption.
Nutritional Support: Individuals with CF often have difficulty absorbing nutrients due to pancreatic insufficiency. A high-calorie, high-protein diet and vitamin supplements may be recommended to maintain optimal nutrition.
Exercise: Regular physical activity helps to improve lung function, strengthen muscles, and maintain overall health.
Lung Transplant: In severe cases of CF where lung function significantly declines despite other treatments, lung transplantation may be considered.
Gene Therapy: Emerging treatments such as CFTR modulator therapies aim to address the underlying genetic cause of CF by improving the function of the defective CFTR protein.
Psychological Support: Living with CF can be challenging, so psychological support, counseling, and support groups can help individuals and families cope with the emotional aspects of the condition.
Treatment plans are personalized based on the individual's specific symptoms, disease progression, and overall health status. Regular monitoring and follow-up with healthcare providers are essential for managing CF effectively.

0 notes
Text
Who is at risk for developing bronchiolitis?
Several factors can increase the risk of developing bronchiolitis, including:
Age: Bronchiolitis most commonly affects infants and young children, particularly those under the age of 2. This is because their airways are smaller and more easily blocked by inflammation and mucus.
Premature birth: Premature infants have underdeveloped lungs and immune systems, making them more susceptible to respiratory infections like bronchiolitis.
Being born during the winter months: Bronchiolitis tends to occur more frequently during the winter season, likely due to increased exposure to respiratory viruses and closer indoor contact.
Exposure to tobacco smoke: Children who are exposed to tobacco smoke, either during pregnancy or after birth, have an increased risk of developing respiratory infections like bronchiolitis.
Crowded living conditions: Living in crowded environments, such as daycare centers or households with multiple siblings, can increase the risk of exposure to respiratory viruses that cause bronchiolitis.
Chronic lung or heart conditions: Children with underlying chronic lung or heart conditions may be more susceptible to severe cases of bronchiolitis.
Weakened immune system: Children with weakened immune systems due to conditions such as immunodeficiency disorders or chemotherapy treatment are at higher risk of developing severe bronchiolitis.
It's important to take preventive measures, such as practicing good hand hygiene, avoiding exposure to tobacco smoke, and minimizing contact with sick individuals, to reduce the risk of bronchiolitis, especially in high-risk populations.

0 notes
Text
What are the symptoms of bronchiolitis?
Bronchiolitis typically starts with symptoms similar to those of a common cold, such as a runny nose and cough. As the condition progresses, symptoms may include:
Cough: Initially, the cough might be dry, but it can become more productive with mucus as the illness progresses.
Wheezing: This is a high-pitched whistling sound that occurs when breathing out. It's caused by narrowed airways.
Difficulty breathing: Some children may develop rapid or labored breathing, which can be a sign of more severe bronchiolitis.
Fever: A low-grade fever is common in infants and young children with bronchiolitis.
Runny nose: Nasal congestion and discharge are typical early symptoms of bronchiolitis.
Fatigue or irritability: Infants and young children may appear more tired or irritable than usual due to the discomfort caused by bronchiolitis.
Decreased appetite: Difficulty breathing and discomfort can lead to a decreased appetite or difficulty feeding in infants.
It's essential to monitor infants and young children with bronchiolitis closely, especially if they show signs of respiratory distress, such as rapid or labored breathing. Severe cases may require medical attention, including hospitalization for supportive care such as oxygen therapy or intravenous fluids. Always consult a healthcare professional if you suspect your child has bronchiolitis or if their symptoms worsen.

0 notes
Text
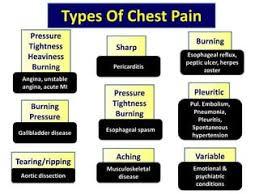
What are the common causes of chest pain?
Chest pain can arise from various conditions, some of which are serious and require immediate medical attention, while others are less severe. Here are some common causes of chest pain:
Cardiac Causes
Angina
Chest pain due to reduced blood flow to the heart muscle, often triggered by physical activity or stress.
Myocardial Infarction (Heart Attack)
Severe, crushing chest pain due to the blockage of blood flow to a part of the heart muscle.
Pericarditis
Inflammation of the pericardium (the sac surrounding the heart), causing sharp, stabbing pain.
Myocarditis
Inflammation of the heart muscle, often leading to chest pain, fatigue, and shortness of breath.
Aortic Dissection
A tear in the inner layer of the aorta, causing severe, ripping chest pain.
Gastrointestinal Causes
Gastroesophageal Reflux Disease (GERD)
Acid reflux causing a burning sensation in the chest, often after eating.
Esophageal Spasm
Sudden, intense contractions of the esophagus leading to chest pain.
Peptic Ulcer
Sores in the stomach lining causing burning pain that can be mistaken for heart pain.
Gallbladder Disease (e.g., Gallstones)
Pain from gallbladder issues can radiate to the chest.
Pulmonary Causes
Pulmonary Embolism
A blood clot in the lung causing sharp chest pain, shortness of breath, and rapid heart rate.
Pneumonia
Infection of the lungs leading to chest pain, fever, and difficulty breathing.
Pleuritis (Pleurisy)
Inflammation of the lining of the lungs, causing sharp pain, especially with breathing or coughing.
Pneumothorax (Collapsed Lung)
Sudden onset of sharp, one-sided chest pain and shortness of breath.
Musculoskeletal Causes
Costochondritis
Inflammation of the cartilage connecting ribs to the breastbone, causing sharp pain.
Muscle Strain
Overuse or injury to chest muscles can cause persistent pain.
Rib Fractures
Broken ribs from trauma can cause significant chest pain, especially when breathing deeply or coughing.
Psychological Causes
Panic Attack
Intense anxiety or panic leading to chest pain, rapid heartbeat, and shortness of breath.
Anxiety
Chronic anxiety can cause chest tightness and discomfort.
Other Causes
Herpes Zoster (Shingles)
A reactivation of the chickenpox virus causing a painful rash and chest pain if the chest area is affected.
Hiatal Hernia
Part of the stomach pushes up through the diaphragm, causing chest pain and discomfort.
Given the wide range of potential causes, chest pain should be evaluated by a healthcare professional, especially if it is severe, persistent, or associated with symptoms such as shortness of breath, sweating, nausea, or dizziness. Early diagnosis and appropriate treatment are crucial for conditions like heart attacks and pulmonary embolisms, which can be life-threatening.

0 notes
Text
What are the treatment options for different types of chest pain?
Treatment options for chest pain depend on the underlying cause. Here’s an overview of various types of chest pain and their corresponding treatment strategies:
1. Cardiac-Related Chest Pain (e.g., Angina, Heart Attack)
Medications:
Nitrates: To relax and widen blood vessels, improving blood flow to the heart.
Aspirin: To reduce blood clotting.
Beta-blockers: To lower heart rate and blood pressure, reducing heart workload.
Statins: To lower cholesterol levels.
ACE inhibitors or ARBs: To lower blood pressure and protect heart function.
Procedures:
Angioplasty and Stent Placement: To open blocked arteries.
Coronary Artery Bypass Surgery: To create a bypass around blocked arteries.
Lifestyle Changes:
Diet, exercise, quitting smoking, and managing stress are crucial for long-term management.
2. Gastroesophageal Reflux Disease (GERD)
Medications:
Antacids: For immediate relief.
H2 Blockers: To reduce acid production (e.g., ranitidine, famotidine).
Proton Pump Inhibitors (PPIs): To block acid production more effectively (e.g., omeprazole, esomeprazole).
Lifestyle Changes:
Avoiding trigger foods (e.g., spicy, fatty foods, caffeine, alcohol).
Eating smaller meals.
Not lying down immediately after eating.
Elevating the head of the bed.
Procedures:
Surgery (e.g., Nissen fundoplication): For severe cases not responding to medication.
3. Musculoskeletal Chest Pain (e.g., Costochondritis, Muscle Strain)
Medications:
NSAIDs: For pain and inflammation (e.g., ibuprofen, naproxen).
Acetaminophen: For pain relief.
Therapies:
Physical Therapy: To strengthen and stretch the muscles.
Heat/Cooling Pads: To reduce pain and inflammation.
Lifestyle Changes:
Avoiding activities that exacerbate pain.
Practicing good posture.
4. Pulmonary Conditions (e.g., Pulmonary Embolism, Pleuritis, Pneumonia)
Pulmonary Embolism:
Anticoagulants: To prevent further clotting (e.g., heparin, warfarin, DOACs like rivaroxaban).
Thrombolytics: To dissolve existing clots in severe cases.
Surgery or Catheter Procedures: In life-threatening situations.
Pleuritis:
NSAIDs: To reduce pain and inflammation.
Antibiotics: If caused by bacterial infection.
Corticosteroids: In some cases, to reduce inflammation.
Pneumonia:
Antibiotics: For bacterial infections.
Antivirals: For viral infections.
Oxygen Therapy: In severe cases to aid breathing.
5. Panic Attack or Anxiety-Related Chest Pain
Medications:
Anxiolytics: Such as benzodiazepines for immediate relief (e.g., alprazolam, lorazepam).
SSRIs or SNRIs: For long-term management of anxiety (e.g., sertraline, fluoxetine).
Therapies:
Cognitive Behavioral Therapy (CBT): To manage anxiety and panic symptoms.
Lifestyle Changes:
Stress management techniques like mindfulness, yoga, and regular exercise.
6. Pericarditis
Medications:
NSAIDs: To reduce inflammation and pain.
Colchicine: To reduce inflammation and prevent recurrences.
Corticosteroids: In severe or refractory cases.
Procedures:
Pericardiocentesis: To remove excess fluid around the heart in cases of pericardial effusion.
7. Aortic Dissection
Emergency Treatment:
Immediate Surgery: Often required to repair the tear.
Blood Pressure Control: Using IV medications to lower blood pressure and reduce stress on the aorta.
8. Other Gastrointestinal Causes (e.g., Peptic Ulcer)
Medications:
PPIs or H2 Blockers: To reduce stomach acid.
Antibiotics: If caused by H. pylori infection.
Lifestyle Changes:
Avoiding NSAIDs and other irritants.
Eating smaller, more frequent meals.
9. Herpes Zoster (Shingles)
Antiviral Medications: To reduce severity and duration (e.g., acyclovir, valacyclovir).
Pain Management:
NSAIDs, acetaminophen, or stronger pain medications.
Topical creams (e.g., capsaicin) or patches (e.g., lidocaine).
Each type of chest pain requires a specific approach to diagnosis and treatment, and it is crucial to consult with a healthcare professional to determine the exact cause and appropriate treatment plan.
0 notes
Text
What lifestyle changes can I make to reduce the risk of chest pain?
Reducing the risk of chest pain, particularly if it is related to heart issues or other serious conditions, often involves making several lifestyle changes. Here are some key changes that can help:
1. Adopt a Heart-Healthy Diet
Increase fruits and vegetables: Aim for a variety of colors and types.
Whole grains: Choose whole grains over refined grains.
Healthy fats: Opt for unsaturated fats found in nuts, seeds, avocados, and oily fish. Limit saturated fats and avoid trans fats.
Limit salt and sugar: Reducing intake of added sugars and sodium can help manage blood pressure and weight.
Lean proteins: Include sources like chicken, fish, beans, and legumes while limiting red and processed meats.
2. Maintain a Healthy Weight
Body weight: Keeping a healthy weight reduces strain on your heart. Use a balanced diet and regular exercise to maintain or achieve a healthy weight.
3. Regular Physical Activity
Exercise: Aim for at least 150 minutes of moderate aerobic exercise or 75 minutes of vigorous exercise per week, along with muscle-strengthening activities on two or more days a week.
Stay active: Incorporate physical activity into your daily routine, like taking stairs instead of the elevator, walking or biking for short trips, etc.
4. Quit Smoking
Tobacco cessation: Smoking is a major risk factor for heart disease. Seek support to quit smoking, such as counseling, medications, or nicotine replacement therapies.
5. Limit Alcohol Intake
Moderation: If you drink, do so in moderation. This means up to one drink per day for women and up to two drinks per day for men.
6. Manage Stress
Stress reduction techniques: Practice stress-reducing activities such as mindfulness, meditation, yoga, deep breathing exercises, or hobbies you enjoy.
Sleep: Ensure you get 7-9 hours of quality sleep each night to help manage stress and overall health.
7. Monitor and Manage Health Conditions
Regular check-ups: Have regular medical check-ups to monitor blood pressure, cholesterol levels, and other heart disease risk factors.
Manage chronic conditions: If you have conditions like hypertension, diabetes, or high cholesterol, work with your healthcare provider to manage them effectively.
8. Avoid Illicit Drugs
Substance use: Avoid using illicit drugs, especially stimulants like cocaine and amphetamines, which can cause serious heart problems.
9. Stay Hydrated
Adequate hydration: Drink enough water throughout the day to maintain optimal bodily functions.
10. Be Aware of Medications
Medication management: Ensure any medications you are taking do not have side effects that could contribute to chest pain. Consult your doctor about any concerns.
11. Know the Warning Signs
Early intervention: Be aware of the signs and symptoms of heart attack and seek immediate medical attention if you experience severe chest pain, especially if it is accompanied by shortness of breath, sweating, nausea, or lightheadedness.
Implementing these lifestyle changes can significantly reduce the risk of chest pain and improve overall cardiovascular health. However, it is essential to consult with a healthcare professional before making significant changes, especially if you have existing health conditions or risk factors.

0 notes
Text
Can anxiety or stress cause chest pain?
Yes, anxiety and stress can cause chest pain. This type of chest pain is often referred to as non-cardiac chest pain and can mimic the symptoms of a heart attack. Here are some key points about anxiety- and stress-related chest pain:
How Anxiety and Stress Cause Chest Pain
Muscle Tension:
Anxiety and stress can cause the muscles in the chest to tighten, leading to pain or discomfort.
Hyperventilation:
During periods of intense anxiety, you might breathe rapidly and shallowly (hyperventilation), which can lead to chest pain.
Increased Heart Rate:
Anxiety can cause your heart rate to increase (tachycardia), which can sometimes be felt as chest pain.
Adrenaline Surge:
Stress and anxiety trigger the release of adrenaline, which can cause the heart to beat faster and more forcefully, sometimes leading to pain or discomfort.
Gastrointestinal Issues:
Anxiety can exacerbate conditions like acid reflux or esophageal spasms, both of which can cause chest pain.
Symptoms of Anxiety-Related Chest Pain
The pain may be sharp, stabbing, or a persistent ache.
It can be localized or spread across the chest.
May occur at rest or during periods of high stress or anxiety.
Often accompanied by other anxiety symptoms such as sweating, dizziness, shortness of breath, or a sense of impending doom.
Differentiating Anxiety Chest Pain from Heart Pain
While anxiety-related chest pain can mimic cardiac chest pain, there are some differences:
Cardiac Chest Pain:
Often described as pressure, tightness, or a squeezing sensation.
May radiate to the arms, neck, jaw, or back.
Can be accompanied by shortness of breath, nausea, or sweating.
Usually triggered by physical exertion or stress and may last longer than a few minutes.
Anxiety Chest Pain:
May be more localized and sharp.
Often occurs during periods of rest or sudden anxiety.
Accompanied by other symptoms of anxiety such as rapid breathing, palpitations, and fear.
What to Do If You Experience Chest Pain
Don’t Ignore It:
Always take chest pain seriously. If you're unsure whether it's anxiety or something more serious, seek medical attention immediately.
Calm Yourself:
Try to relax and breathe slowly. Techniques such as deep breathing, meditation, or progressive muscle relaxation can help.
Avoid Triggers:
Identify and avoid anxiety triggers when possible.
Seek Professional Help:
If anxiety and stress are causing frequent chest pain, consider speaking to a mental health professional. Cognitive-behavioral therapy (CBT) and medication can be effective treatments for anxiety disorders.
Lifestyle Modifications:
Regular exercise, a balanced diet, adequate sleep, and stress management techniques can help reduce anxiety levels.
When to Seek Immediate Help
If the chest pain is severe, lasts more than a few minutes, or is accompanied by symptoms such as shortness of breath, sweating, nausea, or pain radiating to other parts of the body, seek emergency medical attention immediately.
Chest pain, regardless of the cause, warrants attention to rule out serious conditions and to manage symptoms effectively.

0 notes
