Dr. Chirag Gupta is an Urologist in Jaipur and has vast experience in performing all sorts of urological surgeries. He completed his MBBS from Gajra Raja Medical college, Gwalior (2003) and went on to pursue MS from Gandhi Medical College, Bhopal (2010). Aside from his clinical practice, Dr. Gupta actively engages in medical research and publications. Dr. Chirag Gupta as one of the best urologist in Jaipur is dedicated to serving exceptional healthcare services to his patients.
Don't wanna be here? Send us removal request.
Text
Expert Andrology Treatment & Surgery in Jaipur – Dr. Chirag Gupta
When it comes to sensitive male health issues like infertility, erectile dysfunction, or hormonal imbalances, you need an expert who combines compassion with clinical precision. Dr. Chirag Gupta, a leading urologist in Jaipur, offers specialized Andrology Treatment in Jaipur, helping men regain their confidence and quality of life through advanced diagnostics and personalized care.
Andrology is a specialized branch of urology focused on male reproductive health and related conditions. Dr. Gupta provides comprehensive care for conditions such as low testosterone levels, premature ejaculation, erectile dysfunction, and varicocele. With years of experience, he ensures each patient receives confidential consultation, proper guidance, and evidence-based treatment.
For cases that require surgical intervention, Dr. Gupta is also highly experienced in performing Andrology Surgery in Jaipur. He uses minimally invasive techniques that lead to faster recovery, minimal pain, and high success rates. Surgeries such as varicocelectomy, penile implants, and vasectomy reversals are performed with utmost precision and care.
If you're seeking expert, discreet, and effective andrology care, Dr. Chirag Gupta is the name you can trust in Jaipur.
📞 Book an appointment today: +91 7506943955
0 notes
Text
👨⚕️ Meet Dr. Chirag Gupta – The Best Urologist in Jaipur for Kidney Stone & Prostate Treatment
Are you searching for the Best Urologist in Jaipur for expert care in urology and andrology? Look no further than Dr. Chirag Gupta, a highly trusted name in urological treatments with a focus on compassionate, advanced, and minimally invasive care. Located conveniently in Jagatpura, Jaipur, Dr. Gupta is known for his excellence in treating kidney stones, prostate issues, male infertility, and urinary disorders.
📞 Book Your Appointment Today: +91 7506943955
🌟 Why Dr. Chirag Gupta is the Best Urologist in Jagatpura, Jaipur
Dr. Chirag Gupta is a skilled and experienced urologist in Jaipur who provides holistic care for both men and women. Patients from all over the city, especially from Jagatpura, trust his diagnosis, surgical precision, and commitment to long-term health.
With his specialized expertise, he has earned a reputation for offering the Best Urologist Treatment in Jaipur, ensuring each patient receives personalized attention and top-quality care.
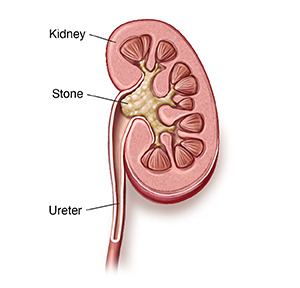
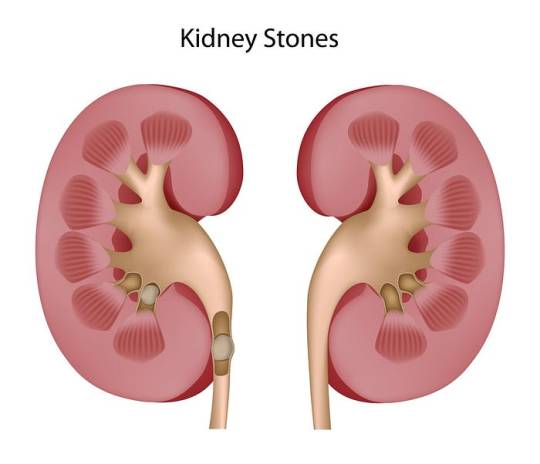
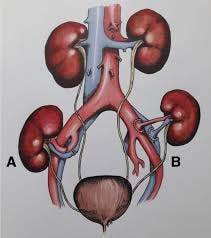
💎 Kidney Stone Treatment in Jaipur
Kidney stones are a common but painful urological issue. If you’re looking for effective kidney stone treatment in Jaipur or kidney stone treatment in Jagatpura, Dr. Chirag Gupta provides both surgical and non-surgical solutions tailored to your condition. Using advanced techniques like laser lithotripsy and ureteroscopy, he ensures fast relief and minimal recovery time.
🧔 Andrology Treatment & Surgery in Jaipur
Dr. Gupta is also widely recognized for his expertise in andrology treatment in Jaipur, helping men deal with issues such as erectile dysfunction, premature ejaculation, and male infertility. If surgery is needed, he offers safe and advanced options under his andrology surgery in Jaipur services.
🧬 Prostate Surgery in Jaipur
Enlarged prostate or BPH (Benign Prostatic Hyperplasia) can severely impact the quality of life in aging men. Dr. Chirag Gupta performs minimally invasive prostate surgery in Jaipur, helping patients manage symptoms like urinary retention, frequent urination, and weak urine flow with effective surgical outcomes.
👨⚕️ What Makes Dr. Chirag Gupta Stand Out?
✅ Patient-first approach ✅ Advanced diagnostic tools ✅ Laser-assisted surgeries ✅ High success rate ✅ Affordable care with transparent consultation
Whether you're in Jagatpura or elsewhere in the city, finding a reliable urologist in Jaipur who combines technology, skill, and empathy is crucial — and that’s exactly what you get with Dr. Chirag Gupta.
📞 Ready to Consult the Best Urologist in Jaipur? Call Now: +91 7506943955
Your health and comfort are just one call away. Don’t delay treatment — book your appointment with Dr. Chirag Gupta today and take the first step towards a healthier, pain-free life.
0 notes
Text
Kidney Stone Treatment in Jaipur – Expert Urologist Care
If you're dealing with the discomfort of kidney stones, finding specialized care is essential. For advanced and effective kidney stone treatment in Jaipur, patients can rely on the expertise of experienced urologists who provide comprehensive and minimally invasive solutions tailored to each individual’s needs.
Kidney stones are hard deposits made of minerals and salts that form inside the kidneys. They can cause severe pain, urinary issues, and potential complications if left untreated. Fortunately, Jaipur is home to several state-of-the-art clinics and hospitals equipped with the latest technology for accurate diagnosis and safe, effective treatment.
Treatment options range from medication and dietary changes to more advanced procedures like laser lithotripsy, shock wave therapy (ESWL), and ureteroscopy. These modern techniques ensure quicker recovery, less pain, and minimal hospital stay, making them ideal for those seeking fast relief with minimal disruption to daily life.
If you're searching for Urologist Treatment in Jaipur, consult a specialist with a proven track record in treating urinary tract disorders, including kidney stones. A skilled urologist will assess your condition thoroughly and recommend the most suitable course of action to prevent recurrence and promote long-term kidney health.
Prompt attention and expert care can make a significant difference. Don’t wait for the pain to escalate—get the right treatment today and regain your health and comfort.
0 notes
Text
Advanced Urology and Andrology Care in Jaipur
Urological health plays a crucial role in overall well-being, especially when it comes to issues related to male reproductive health and prostate conditions. Jaipur has emerged as a center of excellence for specialized urological care, offering modern diagnostic tools and advanced treatment options for men of all ages.
Men dealing with concerns such as infertility, erectile dysfunction, low testosterone levels, or hormonal imbalances can benefit from expert Andrology Treatment in Jaipur. With personalized treatment plans and a discreet approach, andrology care focuses on restoring function, improving quality of life, and addressing the root cause of the issue. Whether the treatment involves medication, lifestyle changes, or minimally invasive procedures, patients receive compassionate and confidential care from experienced specialists.
In addition to andrology, prostate-related issues such as benign prostatic hyperplasia (BPH), prostatitis, or even prostate cancer require timely medical attention. If symptoms like frequent urination, difficulty urinating, or pelvic discomfort are affecting your daily life, it might be time to consider Prostate Surgery in Jaipur. With the availability of cutting-edge surgical techniques including laser and laparoscopic options, patients benefit from quicker recovery, minimal pain, and reduced hospital stay.
With a growing number of dedicated professionals and technologically equipped centers, Jaipur offers reliable and effective solutions for complex male health issues, ensuring comfort, safety, and optimal outcomes.
0 notes
Text
Expert Prostate Surgery in Jaipur – Trusted Care by Top Specialists
Prostate health is a critical aspect of men’s overall well-being, and timely intervention can make a significant difference in outcomes. If you're seeking reliable and advanced prostate surgery in Jaipur, it's important to choose a healthcare provider with proven experience and a patient-focused approach. The city is home to some of the most modern urology centers, offering minimally invasive procedures, faster recovery, and excellent post-operative care.
From benign prostatic hyperplasia (BPH) to prostate cancer, urologists in Jaipur are equipped to handle a range of prostate conditions using the latest surgical technologies like TURP, laser prostatectomy, and robotic-assisted surgery. These techniques reduce hospital stays and help patients return to their normal lives quickly.
Selecting the best urologist in Jaipur ensures not only successful surgery but also compassionate pre- and post-surgical care. Top urologists here bring years of clinical expertise, a track record of successful outcomes, and a commitment to patient education. Their ability to personalize treatment plans based on individual health needs makes a real difference.
When considering prostate surgery, always ensure the hospital is well-equipped and the medical team is board-certified. A well-informed decision today can lead to a healthier, more comfortable future.
0 notes
Text
Expert Urological & Andrology Care in Jaipur
When it comes to men's health, timely diagnosis and expert surgical care are crucial for effective treatment and long-term well-being. For individuals facing concerns related to the male reproductive system or urinary tract, Andrology Surgery in Jaipur offers advanced solutions backed by experienced specialists and state-of-the-art technology.
Andrology focuses on conditions like male infertility, erectile dysfunction, varicocele, and other reproductive issues. Surgical interventions, when needed, are performed with precision to restore both function and confidence. These procedures are often minimally invasive, ensuring quicker recovery and minimal discomfort.
Finding a skilled urologist in Jaipur can make a significant difference in managing a range of conditions such as kidney stones, prostate enlargement, urinary infections, and bladder issues. Today’s urologists combine modern diagnostics with a personalized approach to deliver comprehensive care tailored to each patient.
If you're located in the southeastern part of the city, consulting the best urologist in Jagatpura ensures you don’t have to travel far for world-class treatment. From initial consultation to post-operative care, patients receive expert guidance every step of the way.
Whether you're seeking preventive advice or specialized surgical care, Jaipur's growing medical landscape offers trusted professionals dedicated to your health and comfort.
0 notes
Text
Advancements and Innovations in Penile Surgery: Recent Developments
Penile surgery has seen significant advancements in recent years, driven by technological innovations and a deeper understanding of urological and sexual health. These advancements not only enhance surgical outcomes but also improve patient satisfaction and recovery.

Here’s a look at some of the notable advancements and innovations in penile surgery:
1. Minimally Invasive Techniques
a. Laparoscopic Surgery: Laparoscopic techniques, once reserved for other areas of surgery, are increasingly being applied to penile procedures. These minimally invasive approaches use small incisions and specialized instruments, resulting in reduced postoperative pain, shorter recovery times, and less scarring compared to traditional open surgery.
b. Endoscopic Surgery: Endoscopic methods are used for a range of penile surgeries, including the treatment of penile cancer and penile implants. This approach involves inserting a camera and instruments through small incisions or natural openings, allowing for precise surgery with minimal disruption to surrounding tissues.
2. Penile Implants and Prosthetics
a. Advanced Implant Materials: Recent developments in materials science have led to the creation of more durable and flexible penile implants. Newer models are designed to mimic the natural feel and function of the penis more effectively, providing greater comfort and satisfaction for patients.
b. Inflatable Implants: Innovations in inflatable penile prostheses have improved functionality and ease of use. Modern inflatable implants offer better control over erection firmness and are often easier to operate, enhancing the overall user experience.
c. Customizable Implants: Advancements in 3D printing technology have enabled the development of customizable implants tailored to individual anatomical needs. This personalization can lead to more natural results and improved patient outcomes.
3. Tissue Engineering and Regenerative Medicine
a. Stem Cell Therapy: Stem cell research is making strides in penile tissue regeneration. Stem cells have the potential to repair or replace damaged penile tissues, improving function and aesthetics. This approach is particularly promising for patients with penile trauma or congenital anomalies.
b. Platelet-Rich Plasma (PRP) Therapy: PRP therapy, which involves injecting a concentration of platelets derived from the patient’s blood, is being explored for its ability to promote healing and tissue regeneration. In penile surgery, PRP is used to enhance recovery and improve the quality of the surgical site.
c. Tissue Engineering: Researchers are working on developing bioengineered penile tissues that can be used for reconstruction. These lab-grown tissues are designed to integrate seamlessly with the patient’s own tissues, offering new possibilities for surgical repair and enhancement.
4. Enhanced Imaging and Surgical Navigation
a. High-Resolution Imaging: Advancements in imaging technology, such as high-resolution ultrasound and MRI, have improved preoperative planning and intraoperative navigation. Detailed imaging allows surgeons to assess the anatomy more accurately, leading to more precise and effective surgeries.
b. 3D Visualization: 3D imaging and visualization tools provide surgeons with a more comprehensive view of the surgical field. This enhanced perspective can improve accuracy during complex procedures and reduce the risk of complications.
5. Robotic-Assisted Surgery
a. Precision and Control: Robotic-assisted surgical systems offer unprecedented precision and control. These systems allow surgeons to perform intricate procedures with greater accuracy, minimizing tissue damage and improving overall outcomes.
b. Reduced Recovery Time: The precision of robotic-assisted surgery often leads to less postoperative pain and faster recovery. Patients can typically return to their normal activities sooner compared to traditional surgical methods.
6. Patient-Centric Innovations
a. Improved Surgical Techniques: New techniques and protocols have been developed to enhance patient comfort and satisfaction. For example, advances in anesthesia and pain management have made postoperative recovery smoother and more comfortable.
b. Enhanced Postoperative Care: Modern surgical practices emphasize comprehensive postoperative care, including tailored rehabilitation programs and psychological support. These measures contribute to better long-term outcomes and improved quality of life for patients.
Conclusion
The field of penile surgery has evolved significantly in recent years, driven by technological advancements and a focus on improving patient outcomes. From minimally invasive techniques and innovative implants to regenerative therapies and enhanced imaging, these advancements represent a new era of precision and personalized care. As research continues and technologies develop, the future of penile surgery promises even more effective and patient-centered solutions.
0 notes
Text
Risks and Complications Associated with Kidney Transplant Surgery
Kidney transplant surgery is a life-changing procedure that offers many patients with end-stage renal disease (ESRD) a renewed chance for a healthier and more active life. However, like any major surgery, it carries certain risks and potential complications. Understanding these risks can help patients and their families make informed decisions and better prepare for the post-transplant period.
1. Surgical Risks
a. Infection: As with any major surgery, kidney transplant recipients are at risk for infections. The surgery itself can introduce bacteria, and the use of immunosuppressive medications to prevent organ rejection weakens the body’s natural defense mechanisms, making infections more likely.
b. Bleeding: Significant bleeding during or after the surgery is a potential risk. Although surgeons take extensive measures to minimize this risk, some patients may require blood transfusions or additional procedures to manage bleeding complications.
c. Anesthesia Complications: Reactions to anesthesia, although rare, can occur. Complications might include allergic reactions, breathing difficulties, or cardiovascular issues. Anesthesia risks are generally minimized by thorough pre-operative evaluations.
2. Rejection of the Transplanted Kidney
a. Acute Rejection: This is a common complication that can occur days to months after the transplant. Acute rejection happens when the recipient’s immune system recognizes the new kidney as foreign and attempts to attack it. Symptoms may include fever, pain at the transplant site, and decreased urine output.
b. Chronic Rejection: Over time, the immune system may slowly attack the transplanted kidney, leading to gradual loss of function. Chronic rejection is more difficult to manage and often results in long-term kidney function decline.
3. Graft Failure
Despite the best efforts to match donors and recipients and to manage post-transplant care, there is always a risk of graft failure. This means the transplanted kidney may not function properly or might eventually stop working altogether, necessitating further treatments or possibly another transplant.
4. Organ Dysfunction
a. Delayed Graft Function: Sometimes, the new kidney may not start working immediately after the transplant. This can result in temporary dialysis needs and requires close monitoring and management.
b. Postoperative Complications: Issues such as fluid accumulation around the kidney (hematoma or seroma) or leakage of urine from the kidney or ureter can occur. These conditions might require additional procedures or interventions.
5. Medication Side Effects
a. Immunosuppressants: To prevent rejection, transplant recipients must take immunosuppressive medications, which can have various side effects. Common issues include increased susceptibility to infections, high blood pressure, diabetes, and gastrointestinal problems.
b. Long-Term Effects: Long-term use of immunosuppressants can lead to issues such as osteoporosis, increased cancer risk, and kidney damage. Regular monitoring and adjustments to medication regimens are necessary to mitigate these risks.
6. Cardiovascular Issues
Kidney transplant patients are at a higher risk for cardiovascular diseases, including heart attacks and strokes. This increased risk is often due to underlying health conditions, medication side effects, and lifestyle changes after the transplant.
7. Psychological and Emotional Impact
Undergoing a kidney transplant and adjusting to life with a new organ can be emotionally challenging. Patients may experience anxiety, depression, or stress related to the surgery, recovery, and ongoing medical management. Psychological support and counseling can be beneficial in managing these feelings.
8. Long-Term Health Concerns
a. Cancer Risk: Immunosuppressive medications can increase the risk of certain cancers, such as skin cancer and lymphoma. Regular screenings and protective measures are important to manage this risk.
b. Diabetes and Hypertension: These conditions may develop or worsen as a result of medications and lifestyle changes post-transplant. Managing blood sugar levels and blood pressure is crucial to maintaining overall health and kidney function.
Conclusion
Kidney transplant surgery offers a vital opportunity for improved health and quality of life for many patients with severe kidney disease. However, it is important to recognize and manage the associated risks and complications. Through careful preoperative planning, postoperative care, and long-term management, many of these risks can be effectively addressed. Open communication with healthcare providers, adherence to medical recommendations, and ongoing monitoring are essential for achieving the best possible outcomes after a kidney transplant.
0 notes
Text
What are the potential complications of untreated kidney stones?
Kidney stones, or nephrolithiasis, are hard deposits of minerals and salts that form inside the kidneys. While many small stones may pass through the urinary tract without causing significant problems, untreated kidney stones can lead to serious complications.

Here’s a look at some of the potential issues that can arise if kidney stones are left untreated:
1. Pain and Discomfort
One of the most immediate complications of untreated kidney stones is severe pain. Stones can cause intense pain as they move through the urinary tract. This pain, known as renal colic, typically occurs in waves and can be accompanied by nausea, vomiting, and an overall sense of discomfort. Persistent pain can significantly impact quality of life and may require medical intervention.
2. Urinary Tract Infection (UTI)
Kidney stones can increase the risk of urinary tract infections. Stones can obstruct the flow of urine, creating a breeding ground for bacteria. An infection in the kidneys, known as pyelonephritis, can be particularly dangerous and may lead to symptoms such as fever, chills, and flank pain. Untreated infections can progress to more severe health issues.
3. Kidney Damage
When a kidney stone causes a blockage in the urinary tract, it can lead to a condition called hydronephrotic, where urine backs up into the kidney, causing it to swell. Prolonged obstruction can damage the kidney tissue and impair kidney function. In severe cases, this damage can be irreversible and lead to chronic kidney disease or kidney failure.
4. Bladder and Ureteral Damage
As stones move through the urinary tract, they can cause scratches and abrasions to the lining of the bladder and ureter. This damage can lead to bleeding and the formation of scar tissue. In some cases, scarring can cause long-term complications such as urinary obstruction or bladder dysfunction.
5. Increased Risk of Recurrent Stones
Individuals who have experienced kidney stones are at a higher risk of developing additional stones in the future. Untreated stones can serve as a nucleus for new stone formation, leading to recurrent episodes and a cycle of persistent pain and complications.
6. Electrolyte Imbalances
Large or multiple kidney stones can interfere with the kidney’s ability to regulate electrolytes and fluid balance. This can result in imbalances in essential minerals such as calcium and potassium, which are crucial for various bodily functions. Electrolyte imbalances can lead to muscle cramps, weakness, and other health issues.
7. Sepsis
In severe cases, untreated kidney stones and associated infections can lead to sepsis, a life-threatening response to infection that spreads throughout the body. Sepsis requires immediate medical treatment and can lead to organ failure and potentially be fatal if not addressed promptly.
8. Psychological Impact
The chronic pain and discomfort associated with untreated kidney stones can have a significant psychological impact. Persistent pain, frequent medical visits, and the anxiety of dealing with ongoing health issues can contribute to stress, depression, and reduced quality of life.
Prevention and Management
To avoid these complications, it’s crucial to seek medical attention if you experience symptoms of kidney stones, such as severe pain, blood in the urine, or frequent urinary tract infections. Treatment options vary based on the size and type of stone and may include medications, lifestyle changes, or surgical procedures.
Early diagnosis and management can prevent the progression of kidney stones and reduce the risk of severe complications. Maintaining adequate hydration, following a balanced diet, and managing underlying health conditions can also play a key role in preventing the formation of kidney stones.
By understanding and addressing kidney stones promptly, you can reduce the risk of serious complications and maintain better overall kidney health.
0 notes
Text
Can you explain the different types of minimally invasive surgeries available in urology?
Minimally invasive surgeries in urology are designed to reduce the physical trauma of traditional surgical methods while still effectively treating urological conditions. These techniques generally involve smaller incisions, less pain, quicker recovery times, and minimal scarring.

Here’s a look at the various types of minimally invasive surgeries commonly used in urology:
1. Laparoscopic Surgery
Laparoscopic surgery, also known as keyhole surgery, involves making small incisions (typically 0.5–1 cm) through which a camera (laparoscope) and specialized surgical instruments are inserted. The camera provides real-time images of the internal organs, allowing the surgeon to perform the procedure with precision.
Applications:
Kidney Surgery: Removal of kidney tumors or partial nephrectomy (removal of part of the kidney).
Adrenal Surgery: Removal of adrenal gland tumors.
Bladder Surgery: Treatment of bladder tumors or diverticula.
Advantages:
Less postoperative pain.
Shorter hospital stay.
Quicker recovery.
2. Robotic-Assisted Surgery
Robotic-assisted surgery is an advanced form of laparoscopic surgery where the surgeon controls robotic arms equipped with high-precision instruments. The robot provides a magnified, 3D view of the surgical field and enhances dexterity.
Applications:
Prostate Surgery: Robotic-assisted prostatectomy is often used for prostate cancer removal.
Kidney Surgery: Partial nephrectomy and radical nephrectomy.
Bladder Surgery: Complex bladder reconstructions.
Advantages:
Enhanced precision and control.
Reduced blood loss.
Faster recovery and return to normal activities.
3. Endoscopic Surgery
Endoscopic surgery involves using an endoscope — a flexible tube with a light and camera at the end — inserted through natural body openings or small incisions. The endoscope allows visualization and treatment of internal structures without large cuts.
Applications:
Cystoscopy: Examination and treatment of bladder conditions, such as tumors or stones, through the urethra.
Ureteroscopy: Evaluation and treatment of urinary tract stones or tumors by accessing the ureter through the bladder.
Nephoscopy: Inspection and treatment of kidney stones or tumors.
Advantages:
No external incisions required.
Minimal discomfort and fast recovery.
Often performed on an outpatient basis.
4. Percutaneous Surgery
Percutaneous surgery involves inserting instruments through the skin using a needle or small puncture. This technique is often used for procedures that target deep-seated organs.
Applications:
Percutaneous Nephrolithotomy (PCNL): Removal of large kidney stones through a small incision in the back.
Percutaneous Renal Biopsy: Sampling kidney tissue for diagnosis.
Advantages:
Direct access to the target area with minimal disruption of surrounding tissues.
Shorter recovery time compared to open surgery.
5. Cryoablation and Radiofrequency Ablation
These techniques involve using extreme cold or heat to destroy abnormal tissue. Cryoablation uses freezing temperatures, while radiofrequency ablation uses heat generated by electrical currents.
Applications:
Cryoablation: Treatment of small kidney tumors or prostate cancer.
Radiofrequency Ablation: Management of small renal tumors.
Advantages:
Non-invasive or minimally invasive.
Typically performed on an outpatient basis.
Reduced risk of bleeding and faster recovery.
Conclusion
Minimally invasive surgeries have revolutionized urology by offering effective treatment options with less discomfort and faster recovery. As technology continues to advance, these techniques are likely to become even more refined, offering improved outcomes and patient experiences. Whether through laparoscopy, robotics, endoscopy, or other innovative methods, the goal remains the same: to provide precise, effective care while minimizing the impact on the patient’s body and life.
0 notes
Text
What are the benefits of laser treatment for kidney stones?
Laser treatment for kidney stones is a modern, minimally invasive approach with several benefits that make it an attractive option for many patients.
Here’s a comprehensive look at the advantages of this procedure:
1. Minimally Invasive
Laser treatment, also known as Laser Lithotripsy, involves inserting a thin, flexible tube called a ureteroscope through the urethra and bladder to reach the kidney stones. The laser is then used to fragment the stones into smaller pieces. This approach requires no large incisions, which means a reduced risk of infection, less bleeding, and a quicker recovery time compared to traditional surgical methods.
2. High Precision
Lasers offer unparalleled precision in targeting and fragmenting stones. The energy from the laser can be adjusted to effectively break down different types and sizes of stones while minimizing damage to surrounding tissues. This precision helps ensure that all fragments are small enough to pass through the urinary tract without causing obstruction.
3. Shorter Recovery Time
Due to its minimally invasive nature, laser treatment typically results in a faster recovery compared to more invasive surgical procedures. Patients often experience less pain, reduced swelling, and a quicker return to their daily activities. Most individuals can resume normal activities within a few days to a week.
4. Reduced Risk of Complications
The risk of complications such as infection, bleeding, and damage to the urinary tract is lower with laser treatment than with traditional open surgery. The precision of the laser and the minimal invasiveness of the procedure contribute to a safer overall experience.
5. Effective for Various Stone Types
Laser lithotripsy is versatile and effective for treating different types of kidney stones, including those made of calcium, uric acid, struvite, and cystine. The ability to customize the laser’s energy settings allows for effective treatment across a range of stone compositions.
6. Fewer Post-Operative Symptoms
Patients undergoing laser treatment often report fewer post-operative symptoms such as pain, discomfort, and the need for medication. The minimally invasive nature of the procedure contributes to a more comfortable recovery.
7. Lower Risk of Recurrence
Laser treatment can help prevent the recurrence of kidney stones by effectively fragmenting the stones into smaller pieces that are more easily passed. By reducing the size of the stones, patients are less likely to experience the same level of obstruction or discomfort in the future.
8. Outpatient Procedure
Many laser lithotripsy procedures are performed on an outpatient basis, meaning patients can go home the same day as the procedure. This eliminates the need for a hospital stay and reduces associated costs and disruptions.
9. Reduced Hospitalization Costs
Because the procedure is less invasive and often performed on an outpatient basis, overall hospital costs can be lower. Patients benefit from reduced medical expenses and less time spent away from work or other responsibilities.
Conclusion
Laser treatment for kidney stones offers numerous advantages, including its minimally invasive nature, high precision, and quicker recovery times. It provides an effective solution for managing kidney stones while minimizing discomfort and potential complications. As with any medical treatment, it is essential for patients to consult with their healthcare provider to determine the most appropriate option based on their specific condition and needs.
0 notes
Text
How Does Physical Trauma or Injury Affect Male Fertility?
Male fertility is a complex interplay of physical, hormonal, and environmental factors. Physical trauma or injury can significantly impact fertility, often in ways that may not be immediately obvious. Understanding these effects requires a closer look at how such injuries can disrupt reproductive health.

Types of Physical Trauma and Their Impact
Testicular Injury:
Direct Trauma: Direct injury to the testicles, such as from a sports accident or fall, can lead to severe consequences. Testicular trauma can cause pain, swelling, and bruising, potentially resulting in long-term damage to the testicular tissue. This damage can disrupt sperm production, leading to lower sperm counts or compromised sperm quality.
Testicular Torsion: This is a critical condition where the testicle twists around the spermatic cord, cutting off its blood supply. If not promptly treated, it can result in permanent loss of the testicle and a significant reduction in sperm production.
2. Penile Injury:
Trauma to the Penis: Injuries to the penis, such as those from accidents or surgical procedures, can affect erectile function and ejaculatory processes. While these issues are more likely to affect sexual function than fertility directly, chronic problems can indirectly impact sperm delivery and overall reproductive health.
3. Pelvic Injuries:
Blunt Force Trauma: Injuries to the pelvic region, whether from accidents or other causes, can damage the structures involved in sperm transportation, such as the seminal vesicles, prostate, and vas deferens. This can lead to issues with semen production and ejaculation, affecting fertility.
4. Surgical Interventions:
Surgeries in the Pelvic Area: Operations such as hernia repairs, prostate surgeries, or vasectomies can have implications for fertility. While some procedures are performed with minimal disruption, others may inadvertently affect sperm transport or production.
How Trauma Affects Hormonal and Sperm Health
Hormonal Imbalance:
Physical trauma can disrupt the hormonal balance crucial for sperm production. Injuries leading to stress or systemic illness can alter levels of hormones such as testosterone, luteinizing hormone (LH), and follicle-stimulating hormone (FSH). These imbalances can impair spermatogenesis, the process by which sperm are produced in the testicles.
2. Sperm Quality and Quantity:
Trauma can impact both the quantity and quality of sperm. Testicular injuries, for instance, can lead to decreased sperm production (oligospermia) or abnormal sperm morphology and motility, which can hinder the sperm’s ability to fertilize an egg.
Long-Term Effects and Management
Chronic Pain and Discomfort:
Persistent pain or discomfort from an injury can affect overall well-being and sexual health, indirectly impacting fertility. Stress and pain can reduce libido and affect sexual performance, further complicating fertility issues.
2. Treatment and Recovery:
Addressing the effects of trauma on fertility often involves a multi-faceted approach. Medical evaluation and treatment of the initial injury are crucial. If fertility issues arise, consulting a specialist in reproductive medicine or urology can provide additional options, such as hormone therapy or assisted reproductive technologies like in vitro fertilization (IVF).
3. Preventative Measures:
Taking precautions to prevent injuries, especially in high-risk activities, is essential. For those who have experienced trauma, regular monitoring and consultations with healthcare providers can help manage and mitigate long-term effects on fertility.
Conclusion
Physical trauma and injury can have profound effects on male fertility, impacting sperm production, hormonal balance, and reproductive health. Early intervention and appropriate medical care are crucial for mitigating these effects. For men experiencing fertility issues following trauma, seeking specialized medical advice is key to addressing the problem effectively and exploring potential treatment options.
0 notes
Text
How does obesity contribute to male infertility?
Obesity is a significant health issue that impacts many aspects of well-being, including reproductive health. For men, excess body weight can contribute to infertility in several ways. Understanding these connections can help in addressing and managing fertility issues effectively.

1. Hormonal Imbalance
Obesity often leads to hormonal imbalances that can adversely affect fertility. Excess body fat, particularly abdominal fat, is linked to increased levels of estrogen, a hormone typically associated with female reproductive health. Elevated estrogen levels in men can disrupt the balance of testosterone, the primary male sex hormone responsible for sperm production. Lower testosterone levels can lead to reduced libido, diminished sperm production, and impaired sperm quality.
2. Insulin Resistance and Diabetes
Obesity is a major risk factor for developing insulin resistance and type 2 diabetes. Insulin resistance can interfere with hormonal regulation and impact sperm health. High blood sugar levels and the resultant metabolic syndrome can affect testicular function, leading to lower sperm counts and poorer sperm motility. Additionally, diabetes-related complications can further exacerbate fertility issues.
3. Heat and Sperm Production
Excess body fat, especially around the abdomen, can increase body temperature. The testes, where sperm is produced, require a temperature slightly lower than the body’s core temperature for optimal function. Increased abdominal fat can raise the temperature around the testes, leading to reduced sperm production and quality.
4. Oxidative Stress and Inflammation
Obesity is associated with higher levels of oxidative stress and inflammation in the body. Oxidative stress occurs when there’s an imbalance between free radicals and antioxidants, leading to cellular damage. Inflammation and oxidative stress can negatively impact sperm quality, causing issues like reduced sperm motility and abnormal sperm morphology.
5. Psychological Impact
Obesity can affect psychological well-being, leading to stress, depression, and anxiety. These psychological factors can further impact fertility by influencing hormone levels and sexual function. High levels of stress can reduce libido and affect the overall reproductive health of men.
6. Lifestyle Factors
Obesity often correlates with other lifestyle factors that can affect fertility, such as poor diet, lack of exercise, and smoking or alcohol use. These lifestyle choices can compound the negative effects of obesity on reproductive health. A poor diet can lead to nutritional deficiencies, while smoking and excessive alcohol consumption can directly impair sperm quality.
7. Genetic Factors
There is emerging evidence suggesting that obesity can affect genetic expression related to fertility. Certain genetic markers associated with obesity may influence reproductive health and contribute to fertility challenges.
Addressing Obesity-Related Infertility
Addressing obesity-related infertility involves a multi-faceted approach:
Weight Management: Losing weight through a balanced diet and regular exercise can help restore hormonal balance, improve insulin sensitivity, and enhance sperm quality.
Healthy Lifestyle Choices: Adopting a healthy lifestyle that includes quitting smoking, reducing alcohol intake, and managing stress can further support reproductive health.
Medical Intervention: Consulting with healthcare professionals for personalized advice and treatment plans, which may include medications or therapies to manage associated health conditions.
Conclusion
Obesity is a complex condition with wide-ranging effects on health, including male fertility. Understanding the connections between excess body weight and reproductive health can guide effective management strategies. By addressing obesity through lifestyle changes and medical interventions, men can improve their chances of maintaining optimal fertility and overall health.
0 notes
Text
What are the potential benefits of circumcision?
Circumcision, the surgical removal of the foreskin from the penis, is a practice that has been performed for various reasons across different cultures and religions. While the procedure is often controversial and debated, it’s worth exploring the potential benefits that have been identified through medical research and clinical studies. Here are some of the potential benefits of circumcision:

1. Reduced Risk of Urinary Tract Infections (UTIs)
Studies have shown that circumcision can lower the risk of urinary tract infections, particularly in infants and young children. UTIs can be painful and lead to more serious health issues if left untreated, so reducing their incidence is a significant benefit. Circumcision is believed to reduce the risk by eliminating the potential for infections that can occur in the foreskin area.
2. Decreased Risk of Sexually Transmitted Infections (STIs)
Circumcision has been associated with a lower risk of certain sexually transmitted infections, including HIV. Research has demonstrated that circumcision reduces the likelihood of acquiring and transmitting HIV, especially in high-prevalence regions. The procedure may also lower the risk of other STIs, such as herpes and human papillomavirus (HPV), contributing to better sexual health.
3. Prevention of Phimosis and Paraphimosis
Phimosis is a condition where the foreskin cannot be retracted over the glans (head) of the penis, which can cause pain and difficulty with urination. Paraphimosis occurs when the foreskin, once retracted, cannot return to its original position, potentially leading to severe complications. Circumcision prevents these conditions by removing the foreskin, thereby eliminating the risk of these issues.
4. Improved Hygiene
Circumcision can facilitate better genital hygiene. The removal of the foreskin makes it easier to clean the glans, which can help prevent the buildup of smegma (a combination of dead skin cells, oils, and other bodily fluids) that can contribute to infections and unpleasant odors. Improved hygiene is particularly beneficial for those who may have difficulty with proper cleaning due to the structure of the foreskin.
5. Potential Lower Risk of Penile Cancer
Although penile cancer is rare, circumcision may lower the risk of developing this type of cancer. The reduced risk is attributed to the removal of the foreskin, which may decrease the likelihood of chronic irritation and infection that can potentially contribute to cancerous changes.
6. Cultural and Religious Significance
For many cultures and religions, circumcision is an important rite of passage or a deeply ingrained tradition. In these contexts, the procedure has social, spiritual, and communal significance. For instance, in Judaism and Islam, circumcision is a significant religious obligation, and the practice carries substantial cultural and familial importance.
7. Potential Improvement in Sexual Function
Some studies suggest that circumcision may lead to changes in sexual function. While the evidence is mixed and subjective experiences vary, some men report increased satisfaction and decreased sensitivity in a way that may benefit their sexual experiences. However, this aspect is highly individual and may not be applicable to everyone.
Conclusion
Circumcision presents several potential benefits, including reduced risk of infections, easier hygiene, and decreased likelihood of certain medical conditions. However, it’s essential to consider that the decision to circumcise can be influenced by cultural, religious, and personal factors. Consulting with healthcare professionals and weighing the benefits against potential risks can help individuals and families make informed decisions about circumcision.
As with any medical procedure, it’s important to approach the topic with a balanced perspective, acknowledging both the potential benefits and the ethical considerations involved.
0 notes
Text
What is a kidney transplant, and who is a candidate for this procedure?
A kidney transplant is a surgical procedure that involves placing a healthy kidney from a donor into the body of a person with kidney failure. This procedure is typically recommended for individuals whose kidneys have ceased to function adequately, necessitating an alternative to dialysis for managing kidney function and overall health.
Who is a Candidate for a Kidney Transplant?
Eligibility for a kidney transplant depends on several factors, including the patient’s overall health, kidney function, and the presence of other medical conditions. The following criteria help determine if someone is a suitable candidate:
End-Stage Renal Disease (ESRD) or Kidney Failure:
Candidates typically have ESRD, where kidneys have lost about 85–90% of their function. This condition often requires dialysis, a treatment that performs the kidneys’ functions artificially.
2. Good General Health:
Patients need to be in good overall health to handle the stress of surgery and the long-term use of immunosuppressive medications. Chronic conditions like diabetes, heart disease, or severe infections might affect eligibility.
3. Adherence to Treatment:
Candidates must be able to adhere to a strict regimen of medications and follow-up care. Successful transplantation requires lifelong use of immunosuppressants to prevent rejection of the new kidney.
4. Absence of Active Cancer or Severe Infections:
Active cancer or severe infections can complicate surgery and the healing process, making these conditions a contraindication for transplantation until they are adequately treated or resolved.
5. Support System:
A strong support system of family or friends can be crucial for managing post-surgical care, medication adherence, and follow-up appointments.
6. No Significant Psychosocial Issues:
Candidates should be free of significant psychosocial issues that could affect their ability to adhere to treatment or manage post-transplant care.
Special Considerations:
Living vs. Deceased Donor:
A kidney can come from a living donor (a person who is still alive and has agreed to donate one of their kidneys) or a deceased donor. Both sources are viable, though living donor transplants often have better outcomes due to the organ’s preserved condition.
Blood Type and Tissue Matching:
Successful transplantation requires matching blood types and, ideally, tissue antigens to minimize the risk of organ rejection. Compatibility is determined through a series of tests before the transplant.
Age and Other Health Conditions:
While age alone is not a disqualifying factor, older patients or those with multiple health conditions may need thorough evaluation to ensure they can safely undergo the procedure and benefit from it.
Conclusion
A kidney transplant can offer a life-saving alternative to dialysis for individuals with severe kidney disease. The suitability of a patient for this procedure is determined through a comprehensive evaluation process that considers medical, psychological, and social factors. If you or someone you know is experiencing kidney failure, discussing the option of a kidney transplant with a nephrologist or transplant specialist can provide valuable insights into potential treatment paths and improve overall outcomes.
#Kidney Stone Treatment Specialist in Jaipur#Best Kidney Stone Treatment in Jaipur#Best Kidney Treatment in Jaipur
0 notes
Text
What types of kidney stones can be treated with laser therapy?
Laser therapy is a modern, minimally invasive technique used to treat kidney stones, especially when other methods are not suitable. Here’s a look at the types of kidney stones that can be effectively treated with laser therapy:

1. Calcium Oxalate Stones
These are the most common type of kidney stones, forming when calcium combines with oxalate in the urine. They can be hard and brittle, making them a good candidate for laser fragmentation. The laser breaks these stones into smaller pieces, which can then pass through the urinary tract more easily.
2. Calcium Phosphate Stones
These stones form when calcium combines with phosphate in the urine. They are often larger and less dense than calcium oxalate stones, but laser therapy can still be highly effective. The high-energy laser breaks them into smaller fragments, facilitating easier passage.
3. Struvite Stones
Struvite stones, also known as infection stones, form in response to a urinary tract infection. They can grow quickly and become quite large. Laser therapy is particularly useful for these stones because it can break down the stones effectively, and it helps to address the infection that contributes to their formation.
4. Cystine Stones
Cystine stones are less common and form in people with a genetic condition called cystinuria, which causes excess cystine in the urine. These stones can be quite large and difficult to treat with traditional methods. Laser therapy can effectively break down these stones into smaller pieces, making them easier to pass.
How Laser Therapy Works
Laser therapy involves the use of a laser fiber inserted through a thin tube called a ureteroscope, which is passed through the urethra and bladder to the kidney or ureter where the stones are located. Once in position, the laser targets the stones, fragmenting them into smaller pieces. These smaller fragments are then either flushed out naturally or removed through the ureteroscope.
Benefits of Laser Therapy
Minimally Invasive: Requires no major surgery, reducing recovery time and associated risks.
Effective: Can fragment stones of various compositions and sizes.
Precision: Allows for targeted treatment, minimizing damage to surrounding tissues.
Conclusion
Laser therapy is a versatile and effective treatment option for various types of kidney stones. It offers a minimally invasive alternative to more traditional surgical approaches, helping to alleviate symptoms and reduce recovery time for patients. If you have kidney stones, discussing treatment options with a urologist can help determine if laser therapy is right for you.
0 notes
Text
How do you differentiate between symptoms of a UTI and interstitial cystitis?
Differentiating between a urinary tract infection (UTI) and interstitial cystitis (IC) can be challenging, as both conditions share several similar symptoms. However, they have distinct characteristics and underlying causes that can help in making an accurate diagnosis. Here’s a breakdown to help differentiate between the two:

1. Understanding the Conditions
Urinary Tract Infection (UTI):
A UTI is an infection caused by bacteria entering the urinary tract. It can affect any part of the urinary system, including the kidneys, bladder, ureters, and urethra. UTIs are often acute and respond well to antibiotics.
Interstitial Cystitis (IC):
IC, also known as painful bladder syndrome, is a chronic condition characterized by bladder pain and discomfort without an obvious bacterial infection. The exact cause of IC is not well understood, and it is often a diagnosis of exclusion after other conditions have been ruled out.
2. Symptoms Comparison
Symptoms of a UTI:
Frequent Urination: A need to urinate more often than usual.
Urgency: A strong, persistent urge to urinate.
Pain or Burning Sensation: Pain or a burning feeling during urination.
Cloudy or Strong-Smelling Urine: Urine may appear cloudy, dark, or have a strong odor.
Hematuria: Presence of blood in the urine, which may make it appear pink or red.
Pelvic Pain: Discomfort or pain in the lower abdomen or pelvic area.
Fever and Chills: In more severe cases, systemic symptoms like fever and chills can occur, especially if the infection has spread to the kidneys (pyelonephritis).
Symptoms of Interstitial Cystitis (IC):
Chronic Pelvic Pain: Persistent pain or discomfort in the bladder or pelvic area that is not necessarily linked to urination.
Frequent Urination: Frequent need to urinate, often in small amounts.
Urgency: A sudden and strong need to urinate.
Pain During or After Urination: Pain or discomfort during or after urination, but not necessarily a burning sensation.
Bladder Pressure or Pain: Pressure or pain in the bladder that can worsen as the bladder fills.
No Evidence of Infection: No bacterial growth in urine cultures, which is a key differentiator from a UTI.
3. Diagnostic Approach
For a UTI:
Urine Analysis: A urinalysis can identify bacteria, white blood cells, and other indicators of infection.
Urine Culture: Culturing the urine can determine the specific bacteria causing the infection and the appropriate antibiotic treatment.
For Interstitial Cystitis (IC):
Exclusion of Other Conditions: Diagnosis often involves ruling out other potential causes of bladder symptoms, including UTIs and other bladder disorders.
Cystoscopy: A procedure where a thin tube with a camera is inserted into the bladder to examine its lining. It can help rule out other conditions and sometimes reveal characteristic features of IC.
Bladder Biopsy: In some cases, a biopsy may be performed during cystoscopy to assess for characteristic changes in the bladder tissue.
4. Treatment Differences
UTI Treatment:
Antibiotics: Typically treated with a course of antibiotics. Improvement is usually seen within a few days.
Interstitial Cystitis Treatment:
Lifestyle Changes: Dietary modifications, stress management, and avoiding irritants like caffeine and alcohol.
Medications: May include pain relievers, antihistamines, and medications specifically for IC.
Bladder Instillations: Solutions containing medication can be directly instilled into the bladder.
Physical Therapy: For pelvic floor issues associated with IC.
Other Therapies: Such as nerve stimulation or surgery in severe cases.
5. When to Seek Medical Advice
If you experience symptoms suggestive of a UTI or IC, it’s important to consult a healthcare provider for an accurate diagnosis and appropriate treatment. While UTIs can often be treated quickly with antibiotics, IC requires a more comprehensive approach to manage symptoms and improve quality of life.
0 notes