Don't wanna be here? Send us removal request.
Text
Liver Transplant: A Lifesaving Solution for End‑Stage Liver Disease
When Is a Liver Transplant Needed?
Liver transplant becomes essential when the liver is severely damaged and no longer able to perform vital functions. This often happens due to cirrhosis — a condition in which healthy liver tissue is replaced by scar tissue. While early-stage liver diseases can be managed with lifestyle changes and medication, advanced cases require a liver transplant, especially when complications like ascites, jaundice, internal bleeding, or hepatic encephalopathy appear.
Timing is crucial. Delaying transplant evaluation can reduce the chances of successful outcomes, especially if the liver failure progresses into multi-organ dysfunction. Early intervention offers the best chance of recovery and long-term survival.
If you’re unsure about your condition, consulting the Best Liver Specialist in Ahmedabad can help you understand whether a transplant is necessary and when to plan it.
Causes of Liver Failure Leading to Transplant
In India, the most common causes of end-stage liver disease include:
Alcohol-related liver damage
Non-alcoholic fatty liver disease (NAFLD)
Chronic Hepatitis B or C infections
Autoimmune liver diseases
Genetic disorders like Wilson’s disease
Drug-induced liver injury
Accurate diagnosis and specialist-led care are essential for determining whether a transplant is the right course of action. That’s why it’s important to connect with the Best Liver Specialist in Ahmedabad for timely and precise treatment guidance.
Liver Transplant Advancements in India
Thanks to improvements in medical infrastructure and transplant regulations, liver transplants are now more accessible across many Indian cities. Ahmedabad, in particular, has emerged as a center for advanced liver transplant procedures.
Patients can now benefit from:
High success rates for both living and cadaveric donor liver transplants
Shorter waiting times and faster evaluations
Advanced surgical techniques and post-operative care
Reduced cost compared to transplants performed abroad
Availability of state and central government assistance programs for eligible patients
These benefits are best realized under the guidance of a seasoned hepatologist. If you are in Gujarat, consider reaching out to the Best Liver Specialist in Ahmedabad to explore your options with confidence.
Choosing the Right Liver Transplant Center
A good liver transplant program includes:
Experienced liver specialists and transplant surgeons
Comprehensive pre- and post-transplant care
Facilities for immunosuppressive therapy and infection control
Patient counseling and family support services
Transparent organ allocation policies
Centers with multidisciplinary teams and advanced technology significantly improve transplant outcomes and patient recovery. Partnering with the Best Liver Specialist in Ahmedabad ensures you are in safe hands throughout your transplant journey.
Latest Trends and Technologies
Modern liver transplant programs now use innovations like:
Normothermic perfusion for preserving liver function before surgery
Minimally invasive techniques for living donor procedures
Personalized immunosuppressive therapies to minimize side effects
Data-driven assessments to improve long-term survival
Post-transplant rehab and nutritional support to speed up healing
These advancements are making transplants safer and more effective, with many patients returning to normal life within months.
When to Consult a Liver Transplant Specialist
If you or your loved one has been diagnosed with advanced liver disease and is experiencing:
Uncontrolled fluid buildup (ascites)
Frequent confusion or drowsiness (encephalopathy)
Yellowing of eyes or skin (jaundice)
Swelling in the legs
Internal bleeding
Severe fatigue or weight loss
…it may be time to consult a liver transplant specialist for further evaluation. For those living in Gujarat or nearby regions, booking a consultation with the Best Liver Specialist in Ahmedabad can be a crucial first step toward treatment and healing.
Final Words
A liver transplant offers renewed hope for individuals facing irreversible liver damage. With timely diagnosis, expert care, and advanced surgical techniques, survival rates continue to improve. Ahmedabad is now home to leading transplant centers providing comprehensive care close to home — making this critical procedure more accessible than ever.
To ensure the best possible outcome, make sure you’re guided by the Best Liver Specialist in Ahmedabad who understands your unique condition and treatment needs
0 notes
Text
Liver Function Test in Ahmedabad – Early Diagnosis, Better Health
If you’re looking for a Liver Function Test in Ahmedabad, you’re making a proactive move toward ensuring your liver health. The liver plays a vital role in metabolism, detoxification, and digestion. Any dysfunction can significantly affect your overall health. That’s why timely liver testing is essential — especially if you’re experiencing symptoms like fatigue, jaundice, abdominal pain, or have a history of alcohol use or hepatitis.
What is a Liver Function Test (LFT)?
A Liver Function Test (LFT) is a blood test that measures enzymes, proteins, and substances produced by the liver. These tests help assess the liver’s health and detect inflammation, damage, or infection. Key parameters include:
ALT (Alanine transaminase)
AST (Aspartate transaminase)
ALP (Alkaline phosphatase)
Bilirubin
Albumin and total protein
When Should You Get a Liver Function Test?
You may need an LFT if:
You have symptoms like yellow skin or eyes (jaundice), dark urine, or abdominal pain
You consume alcohol regularly
You are on long-term medications
You have been diagnosed with hepatitis or other liver conditions
You are overweight or have diabetes
Where to Get a Liver Function Test in Ahmedabad?
If you’re in Ahmedabad and need a trusted specialist for liver health, visit Dr. Pathik Parikh. As a leading liver specialist and gastroenterologist, Dr. Parikh offers comprehensive liver care — from diagnostics to treatment — with years of experience and modern diagnostic facilities.
His clinic provides:
Advanced Liver Function Testing
Accurate Diagnosis of Liver Conditions
Personalized Treatment Plans
Follow-up and Lifestyle Advice
Why Choose Dr. Pathik Parikh?
Expertise in Liver and Digestive Health
Compassionate, Patient-Centric Care
State-of-the-Art Diagnostic Tools
Convenient Location in Ahmedabad
Book Your LFT Today
Don’t wait for symptoms to worsen. Early detection can prevent long-term complications. Schedule your Liver Function Test in Ahmedabad with Dr. Pathik Parikh and take control of your liver health today.
0 notes
Text
MASLD & Fibroscan (Liver Elastography) Demystified!!

Fatty Liver is no longer an unheard term. The prevalence of fatty liver in India is approximately 30% and that means that nearly one in three person suffers from it. The disease is not as benign as the name and prevalence suggest. This disease is the most common liver disease worldwide. It is on path to become the number 1 reason for liver cirrhosis, liver cancer and liver transplant.
New Terminology
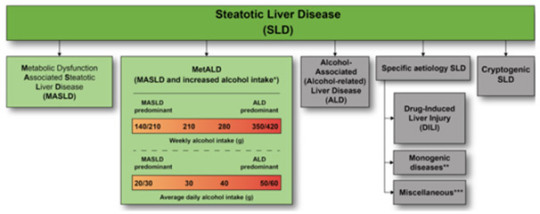
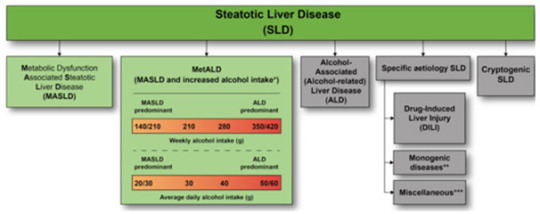
The disease has gone significant change in terminology and is now known as MASLD – Metabolic-Dysfunction Associated Steatotic Liver Disease and recently in 2023 the experts of the world met and proposed the following terminology for types of SLD (Steatotic Liver Disease) or Fatty Liver Disease
MASLD – Previously NAFLD or Fatty Liver
MASH – Previously NASH
MetALD – No previous terminology (Patients also take alcohol in addition).
Risk Factors
MASLD and MASH is usually seen in patients who are obese, overweight and suffer from diabetes, hypertension, sedentary lifestyle, thyroid disease and is habituated to eating processed foods and high-fat high carbohydrate diet.
Progression
MASLD can progress over years to end stage liver disease and leads to complications similar to alcohol associated liver disease. It leads to cirrhosis and then ascites, pedal oedema, bleeding, jaundice, encephalopathy, liver cancer and may warrant liver transplant. In early stage when the disease is reversible, it has no symptoms and hence often ignored. When symptoms do develop, it is usually too late to reverse.

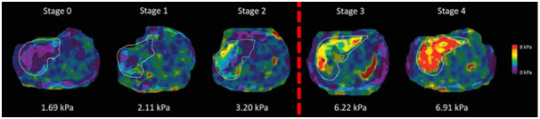
Diagnosis
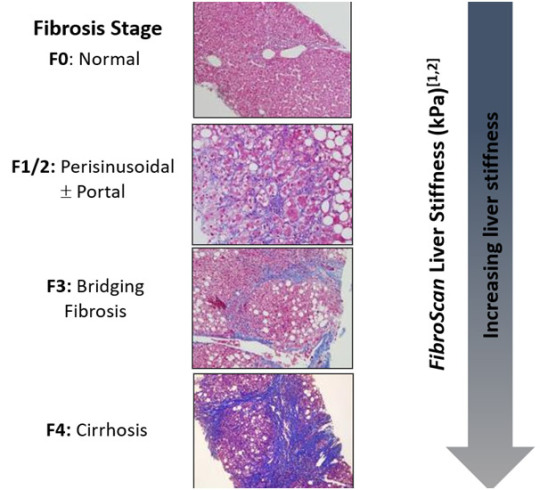
The diagnosis of fatty liver is based on a sonography or abdominal ultrasound where radiologist will let you know if you have fatty liver. Although, blood tests like liver function tests, lipid profile, HBA1c, CBC and others are often recommended to find out predisposing conditions and complications, it fails to give exact nature of underlying severity or stage of liver disease. For this, non-invasive tests are recommended. These tests are very important to understand the prognosis and treatment prescription. Following image is an idea about some of these tests.

There is a lot of confusion currently in terminology of Fibroscan, Elastography and ARFI. I have created following flow chart to understand this difference.

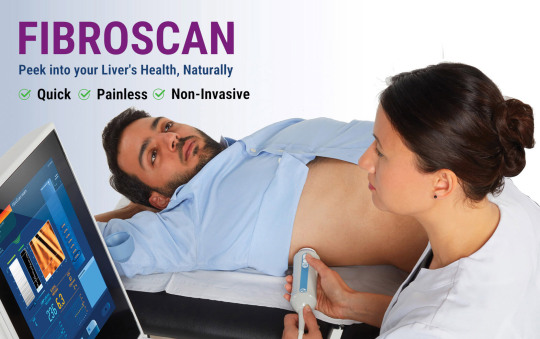
Fibroscan
It is Transient Elastography. It is the name of the machine which carries out the test of Transient Elastography. Unfortunately, since this is the first elastography technique and is accepted worldwide, the name is used synonymously for the technique. It is similar to XEROX and photocopy where XEROX is the name of the machine and the function is photo company. Fibroscan is produced by a French company called Echosens. This is the only approved and accepted modality worldwide.

The currently available machines of Fibroscan (430,430 Mini, 502, 530, 630) provide following details
CAP – Controlled Attenuation Parameter – It tells the patient about the amount of fat in the liver. The ultrasound when gives Fatty liver Grade1,2 or 3, it is a subjective finding while CAP is an objective number which can be used to monitor treatment and risk stratification. A value above 230 is considered significant
LSM – Liver Stiffness Measurement– It tells you how stiff the liver has become. Stiffer the liver worse is the outcome. The vibration wave generated by the probe travels through the liver and the velocities then picked up to give a definite number. Usually, the number is less than 8 kPa. When the value crosses 14 kPa or above, the chances that the liver has irreversible damage are high. The risk of complications also increases when the value crosses 20 or above.
SSM – Splenic Stiffness Measurement – It is measured over the spleen and it gives risk of developing bleeding from the foodpipe and stomach secondary to liver cirrhosis. These values still require validation and widespread acceptance
The 402 version of the machine is outdated and no longer accepted. The machine has SMART EXAM to improve the efficiency, interoperability and accuracy.
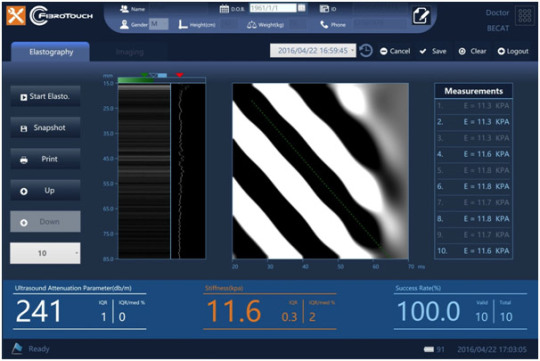
Fibrotouch
Similar to Fibroscan, this machine is made in Asia and available also in India. It works exactly on the same principle as Fibroscan. Instead of CAP, the machine gives UAP. Although used frequently, a lot of Indian doctors, hepatologists and Gastroenterologists have raised questions about its accuracy.

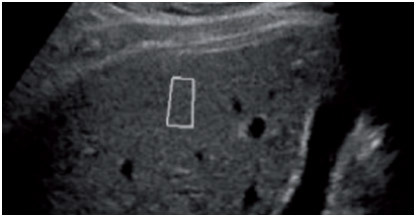
pSWE – Point Shear Wave Elastography
This is type of Elastography which radiologists carry out with the use of their sonography machine. The technique used is different from Fibroscan. Instead of Vibration, the machine uses Acoustic waves and the technique is known as ARFI. The machine provides an advantage of being able to do an ultrasound and elastography with the same machine but it cannot give CAP value and it requires validation to be used as a Fibroscan alternative as of now.

MR Elastography
It is considered one of the best techniques. Availability although is a problem. Only few centres in India provide this facility. It is expensive.

Treatment
The treatment of MASLD is lifestyle modification. If there is fibrosis on the above tests, your doctor might prescribe you medicines to protect the liver in addition. The control of predisposing factors is of paramount importance.
If you suffer from Fatty Liver – MASLD, please contact your Liver Specialist or Hepatologist
0 notes
Text
Liver Disease
Liver is a complex organ with more than 500 functions. Liver diseases are not just limited to alcohol. Over the last two decades, liver diseases besides alcohol have been considered as a cause for liver failure. The list below is just to name a few.Non-Alcoholic Fatty Liver DiseaseAlcoholic Fatty Liver diseaseViral HepatitisMetabolic liver diseaseAutoimmune hepatitisDrug induced liver injuryVascular liver diseaseCongenital liver diseasePrimary biliary cholangitisPrimary sclerosing cholangitisInfectious liver diseaseGranulomatous liver disease
Fatty Liver disease is the most common cause of liver disease in India and worldwide. Alcohol related liver disease is constant through these years while viral hepatitis thanks to good treatment availability is decreasing.
These liver diseases can present as any of the following manner.
Asymptomatic – Incidental finding on investigations
Acute hepatitis with or without jaundice
Acute Liver failure
Chronic hepatitis
Cirrhosis of liver
Acute on chronic liver failure
Liver cancer
Rarely extra hepatic manifestations of liver disease
The routine clinical symptoms of liver disease unlike popular perception is not indigestion of food but is based type of hepatitis. Jaundice is not a disease but a symptom of liver disease and not all liver disease produce jaundice. Jaundice in some situations is early like in chronic hepatitis while it is late in chronic hepatitis or cirrhosis of liver. Cirrhosis of liver presents with ascites or swelling of legs and very commonly with blood in stools or blood in vomit.
The investigations required for liver diseases are not limited to few basic reports. The doctor advises multitude of tests like complete blood count, full liver profile, viral markers, autoimmune or metabolic markers. Special tests for fibrosis may be advised. A sonography or a CT scan of liver may be requested. Fibroscan or liver elastography is usually carried out. Liver biopsy is rarely requested as certain diseases can only be confirmed on liver biopsy. Since liver disease is usually multi system disease the tests for heart, lungs, kidney, brain may be occasionally asked for. Also, cholesterol, thyroid, diabetes is simultaneously tested.
The treatment of liver disease is based on clinical diagnosis. The underlying risk factor and aetiology are treated. Many times, liver supportive and nutritional supplements are needed to help liver recover. Although more than 5000 liver tonics or liver detox are available in the market, there is no evidence that they work but on the contrary, there is enough evidence that it may have side effects.
We provide comprehensive liver care services and help manage above diseases with utmost care. Getting you and your relatives understand these disease with simple language and making sure that we have goal driven activities for not just treatment of these disease but also prevention and progression of liver complications.
0 notes
Text
Understanding Drug-induced Liver Injury (DILI): Symptoms, Causes, and Treatment
"Understanding Drug-induced Liver Injury (DILI): Symptoms, Causes, and Treatment" is a clear and informative title that covers the essential aspects of DILI. Here's an outline of what each section might include:
Symptoms of Drug-induced Liver Injury (DILI):
Overview of common symptoms such as fatigue, jaundice (yellowing of the skin and eyes), abdominal pain, nausea, vomiting, and loss of appetite.
Discussion on the variability of symptoms depending on the severity and type of liver injury caused by different drugs.
Causes of Drug-induced Liver Injury (DILI):
Explanation of how certain medications and drugs can lead to liver injury.
Classification of DILI based on mechanisms, such as direct hepatotoxicity, idiosyncratic reactions, and immune-mediated responses.
Risk Factors for Drug-induced Liver Injury (DILI):
Identification of factors that increase the likelihood of developing DILI, including specific drug characteristics, patient-related factors (e.g., age, genetics), and underlying liver disease.
Treatment Approaches for Drug-induced Liver Injury (DILI):
Overview of general principles of management, including discontinuation of the offending drug.
Discussion on supportive care measures to alleviate symptoms and promote liver recovery.
Mention of specific antidotes or therapies used in certain cases of severe DILI.
Prevention and Monitoring:
Importance of drug monitoring, patient education, and avoidance of high-risk medications in susceptible individuals.
Strategies to prevent DILI and minimize adverse drug reactions in clinical practice.
Prognosis and Long-term Effects:
Outlook for patients with DILI, including recovery rates and potential complications.
Discussion on the importance of long-term follow-up and monitoring for liver function after experiencing DILI.
By structuring your content around these key points, you can create an informative and comprehensive resource on Drug-induced Liver Injury (DILI) that addresses the needs of your audience and provides valuable insights into this important medical condition.
0 notes
Text
fibroscan for liver inflammation - overview
FibroScan is a non-invasive medical procedure used to assess liver health by measuring liver stiffness and determining the degree of liver fibrosis. While it's not specifically designed to detect liver inflammation, it can provide valuable information about overall liver health.
Liver inflammation, also known as hepatitis, can result from various causes such as viral infections (like hepatitis B or C), alcohol consumption, fatty liver disease, autoimmune disorders, and other factors. It's a crucial aspect of liver health assessment as chronic inflammation can lead to liver damage and fibrosis over time.
Although FibroScan primarily evaluates liver stiffness and fibrosis, it indirectly reflects liver inflammation. Inflammation can contribute to liver fibrosis, which in turn affects liver stiffness. Therefore, higher levels of liver stiffness detected by FibroScan may suggest the presence of inflammation. However, FibroScan alone may not provide a complete picture of liver inflammation, and additional tests such as blood tests measuring liver enzyme levels (ALT, AST) and imaging studies (ultrasound, MRI) are often used alongside it for a comprehensive assessment.
FibroScan is a valuable tool in the management of liver diseases, providing a non-invasive alternative to liver biopsy for assessing fibrosis and monitoring disease progression. However, its role in detecting liver inflammation is more indirect, and healthcare professionals typically use a combination of tests to evaluate liver health comprehensively. If you suspect liver inflammation or have concerns about your liver health, it's essential to consult with a healthcare provider for proper evaluation and management.
0 notes
Text
0 notes
Text
MASLD & Fibroscan (Liver Elastography) Demystified!!
Fatty Liver is no longer an unheard term. The prevalence of fatty liver in India is approximately 30% and that means that nearly one in three person suffers from it. The disease is not as benign as the name and prevalence suggest. This disease is the most common liver disease worldwide. It is on path to become the number 1 reason for liver cirrhosis, liver cancer and liver transplant.
New Terminology
The disease has gone significant change in terminology and is now known as MASLD – Metabolic-Dysfunction Associated Steatotic Liver Disease and recently in 2023 the experts of the world met and proposed the following terminology for types of SLD (Steatotic Liver Disease) or Fatty Liver Disease
MASLD – Previously NAFLD or Fatty Liver
MASH – Previously NASH
MetALD – No previous terminology (Patients also take alcohol in addition).
Risk Factors
MASLD and MASH is usually seen in patients who are obese, overweight and suffer from diabetes, hypertension, sedentary lifestyle, thyroid disease and is habituated to eating processed foods and high-fat high carbohydrate diet.
Progression
MASLD can progress over years to end stage liver disease and leads to complications similar to alcohol associated liver disease. It leads to cirrhosis and then ascites, pedal oedema, bleeding, jaundice, encephalopathy, liver cancer and may warrant liver transplant. In early stage when the disease is reversible, it has no symptoms and hence often ignored. When symptoms do develop, it is usually too late to reverse.
Diagnosis
The diagnosis of fatty liver is based on a sonography or abdominal ultrasound where radiologist will let you know if you have fatty liver. Although, blood tests like liver function tests, lipid profile, HBA1c, CBC and others are often recommended to find out predisposing conditions and complications, it fails to give exact nature of underlying severity or stage of liver disease. For this, non-invasive tests are recommended. These tests are very important to understand the prognosis and treatment prescription. Following image is an idea about some of these tests.
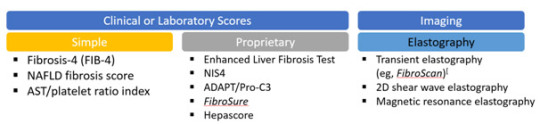
There is a lot of confusion currently in terminology of Fibroscan, Elastography and ARFI. I have created following flow chart to understand this difference.

Fibroscan
It is Transient Elastography. It is the name of the machine which carries out the test of Transient Elastography. Unfortunately, since this is the first elastography technique and is accepted worldwide, the name is used synonymously for the technique. It is similar to XEROX and photocopy where XEROX is the name of the machine and the function is photo company. Fibroscan is produced by a French company called Echosens. This is the only approved and accepted modality worldwide.

The currently available machines of Fibroscan (430,430 Mini, 502, 530, 630) provide following details
CAP – Controlled Attenuation Parameter – It tells the patient about the amount of fat in the liver. The ultrasound when gives Fatty liver Grade1,2 or 3, it is a subjective finding while CAP is an objective number which can be used to monitor treatment and risk stratification. A value above 230 is considered significant
LSM – Liver Stiffness Measurement– It tells you how stiff the liver has become. Stiffer the liver worse is the outcome. The vibration wave generated by the probe travels through the liver and the velocities then picked up to give a definite number. Usually, the number is less than 8 kPa. When the value crosses 14 kPa or above, the chances that the liver has irreversible damage are high. The risk of complications also increases when the value crosses 20 or above.
SSM – Splenic Stiffness Measurement – It is measured over the spleen and it gives risk of developing bleeding from the foodpipe and stomach secondary to liver cirrhosis. These values still require validation and widespread acceptance
The 402 version of the machine is outdated and no longer accepted. The machine has SMART EXAM to improve the efficiency, interoperability and accuracy.
Fibrotouch
Similar to Fibroscan, this machine is made in Asia and available also in India. It works exactly on the same principle as Fibroscan. Instead of CAP, the machine gives UAP. Although used frequently, a lot of Indian doctors, hepatologists and Gastroenterologists have raised questions about its accuracy.
pSWE – Point Shear Wave Elastography
This is type of Elastography which radiologists carry out with the use of their sonography machine. The technique used is different from Fibroscan. Instead of Vibration, the machine uses Acoustic waves and the technique is known as ARFI. The machine provides an advantage of being able to do an ultrasound and elastography with the same machine but it cannot give CAP value and it requires validation to be used as a Fibroscan alternative as of now.
MR Elastography
It is considered one of the best techniques. Availability although is a problem. Only few centres in India provide this facility. It is expensive.
Treatment
The treatment of MASLD is lifestyle modification. If there is fibrosis on the above tests, your doctor might prescribe you medicines to protect the liver in addition. The control of predisposing factors is of paramount importance.
If you suffer from Fatty Liver – MASLD, please contact your Liver Specialist or Hepatologist
0 notes
Text
Liver Transplant Timing
Deciding the right time for a liver transplant after cirrhosis involves a careful evaluation of several factors. Liver transplantation is typically considered when the liver damage is severe, and the patient's life is at risk. Here are some key considerations:
Severity of Cirrhosis: The progression of cirrhosis is categorized into stages (usually classified as stages 1 to 4). Transplantation is generally considered when a patient reaches advanced stages (3 and 4) and experiences significant liver dysfunction.
Symptoms and Complications: The presence of complications related to cirrhosis, such as ascites (fluid accumulation in the abdomen), hepatic encephalopathy (brain dysfunction due to liver failure), and variceal bleeding, may indicate the need for transplantation.
Liver Function Tests: Monitoring liver function tests, including measures of liver enzymes, bilirubin levels, and blood clotting factors, helps assess the degree of liver dysfunction and guides decisions about transplantation.
MELD Score: The Model for End-Stage Liver Disease (MELD) score is a numerical scale used to prioritize patients for liver transplantation. It takes into account factors such as bilirubin levels, creatinine levels, and INR (International Normalized Ratio). A higher MELD score indicates a greater need for transplantation.
Quality of Life: The impact of cirrhosis on the patient's quality of life is an important consideration. If the patient's daily life is significantly compromised, transplantation may be considered to improve their overall well-being.
Response to Medical Therapy: The response to medical treatments for cirrhosis, such as medications to manage complications or symptoms, is taken into account. If these treatments are no longer effective, transplantation may be considered.
Medical History and Comorbidities: The patient's overall medical history, including the presence of other health conditions, is considered when evaluating the suitability for transplantation.
Psychosocial Factors: The patient's ability to adhere to post-transplant care, including medication regimens and lifestyle changes, as well as their support system and mental health, are important factors in the decision-making process.
Ultimately, the decision to undergo liver transplantation is made on an individual basis, taking into consideration the unique circumstances of each patient. It involves collaboration between hepatologists, transplant surgeons, and other healthcare professionals. Patients with advanced cirrhosis should be referred to a liver transplant center for a thorough evaluation and to determine the appropriate timing for transplantation. Early consultation with a transplant team is crucial to ensure timely assessment and preparation for transplantation if deemed necessary.
0 notes
Text
Kidneys in liver cirrhosis – Hepatorenal Syndrome
Liver Cirrhosis progresses to develop many complications. It is prudent to be aware of the complications of liver cirrhosis, so that it can be picked up early and treated timely. Some of these are often ignored for long time before they become life threatening. The table shows different complications of liver cirrhosis.
0 notes
Text
fibro scan test in Ahmedabad
As of my last knowledge update in January 2022, I don't have specific details about the availability of FibroScan tests in Ahmedabad. To find information about FibroScan tests in Ahmedabad, I recommend trying the following steps:
Contact Local Hospitals and Clinics: Reach out to major hospitals, clinics, and diagnostic centers in Ahmedabad. They may have information about whether they offer FibroScan services.
Online Search: Use online search engines to look for medical facilities or diagnostic centers in Ahmedabad that provide FibroScan tests. Many healthcare providers have websites with details about the services they offer.
Ask Your Doctor: Consult your primary care physician or a gastroenterologist. They can provide recommendations or refer you to a facility that offers FibroScan testing.
Healthcare Directories: Check online healthcare directories or platforms that list medical facilities and services. These platforms often include contact information and details about the services provided.
Local Health Authorities: Contact local health authorities or medical associations in Ahmedabad. They may be able to provide information or direct you to facilities offering FibroScan tests.
Remember to verify the information directly with the facilities, as services and availability may change over time. If you have a specific doctor or healthcare provider, they can also guide you on where to get a FibroScan in Ahmedabad.
0 notes
Text
0 notes
Text
Acute liver failure
Ms V, a 25-year-old girl from Maninagar, an associate professor in premier engineering college, a pHD student and a girl who is soon to get hitched to the man of his dreams. With loving parents, life could not get better for her.
Like most of the youngsters, she also used to have occasional outside food. Unfortunately, she developed vomiting, fever, muscle pain and she consulted her primary doctor. On investigations she was found to have hepatitis A virus.https://www.drpathikparikh.com/acute-liver-failure/
0 notes
Text
Fasting for Fatty Liver
Intermittent fasting (IF) has gained popularity in recent years as a potential strategy for managing various health conditions, including fatty liver disease. Fatty liver disease, also known as non-alcoholic fatty liver disease (NAFLD), is characterized by the accumulation of fat in the liver. It can range from simple fatty liver (steatosis) to a more severe condition called non-alcoholic steatohepatitis (NASH), which can lead to liver inflammation and scarring (fibrosis).
There is some evidence to suggest that intermittent fasting may be beneficial for individuals with fatty liver disease, although more research is needed to fully understand its efficacy and safety. Here are some key points to consider:
Weight Loss: Intermittent fasting may lead to weight loss, which is a primary goal in managing fatty liver disease. Losing excess weight can help reduce the fat buildup in the liver and improve liver function.
Improved Insulin Sensitivity: Intermittent fasting may improve insulin sensitivity and reduce insulin resistance, which are factors that contribute to the development and progression of fatty liver disease.
Reduction in Inflammation: Some studies have shown that intermittent fasting can reduce markers of inflammation in the body, which may be beneficial for individuals with NASH, as inflammation plays a role in the progression of the disease.
Autophagy: Intermittent fasting may stimulate a cellular process called autophagy, which helps remove damaged cells and organelles from the liver. This could potentially aid in the resolution of fatty liver.
However, it's important to note that the research on intermittent fasting and fatty liver disease is still relatively limited, and not all studies have consistently shown positive effects. Additionally, the optimal fasting regimen (e.g., time-restricted eating, alternate-day fasting, or periodic fasting) for treating fatty liver has not been definitively established.
Before starting any fasting regimen for fatty liver disease or any other health condition, it's crucial to consult with a healthcare provider. They can assess your individual medical history, overall health, and specific needs to help determine if intermittent fasting is a suitable approach for you. Fasting can have potential side effects, and it may not be safe or appropriate for everyone.
Furthermore, it's essential to approach fatty liver disease treatment comprehensively, which may include dietary changes, exercise, and, in some cases, medication. Your healthcare provider can guide you in developing a personalized treatment plan based on your unique circumstances.
#best liver doctor in ahmedabad#best liver cancer doctors in ahmedabad#liver specialist in ahmedabad
0 notes
Text
0 notes
Text
Fatty Liver & Intermittent Fasting

Intermittent fasting (IF) is a dietary approach that involves cycling between periods of eating and fasting. It has gained popularity in recent years for its potential health benefits, including weight loss, improved metabolic health, and even its potential as a treatment for certain conditions, such as non-alcoholic fatty liver disease (NAFLD).
Non-alcoholic fatty liver disease is a condition characterized by the accumulation of fat in the liver, not related to excessive alcohol consumption. It ranges from simple fatty liver (steatosis) to non-alcoholic steatohepatitis (NASH), which is associated with inflammation and liver damage. I may have some potential benefits for individuals with NAFLD, but it’s important to note that research in this area is ongoing, and individual results can vary.
Here are some ways in which intermittent fasting may be beneficial for fatty liver:
While there is potential for intermittent fasting to benefit individuals with fatty liver disease, it’s essential to approach it cautiously, especially if you have other underlying medical conditions. Before starting any fasting regimen, it’s advisable to consult with a healthcare professional, preferably one with expertise in liver health or nutrition. They can help you determine if intermittent fasting is appropriate for you and provide guidance on the best approach.
Additionally, it’s important to remember that lifestyle changes, including dietary modifications and exercise, should be part of a comprehensive plan to manage fatty liver disease. I should not replace a well-balanced, nutrient-dense diet that supports overall health and liver function.
Lastly, individual responses to intermittent fasting can vary, so it’s essential to monitor your progress and consult with your healthcare provider regularly to ensure that it’s having the desired effect on your fatty liver and overall health.
#best hepatologist in ahmedabad#best liver doctor in ahmedabad#hepatologist in ahmedabad#liver disease#liver specialist in ahmedabad
0 notes
Text
Cirrhosis Diet Guidelines.
Diet plays a crucial role in managing cirrhosis, a condition where the liver becomes scarred and damaged due to long-term injury. A cirrhosis-friendly diet focuses on reducing the workload on the liver, preventing further damage, and providing essential nutrients. It is essential to consult with a healthcare professional or a registered dietitian before making any significant changes to your diet. Here are some general dietary guidelines for cirrhosis:
Limit Sodium Intake: Excessive sodium can lead to fluid retention and worsen swelling (edema) and ascites (fluid accumulation in the abdomen). Aim to reduce salt intake and avoid high-sodium processed foods.
2. Manage Fluid Intake: If you have fluid retention, your doctor may recommend restricting your fluid intake. This can help control edema and ascites.
3. Consume Adequate Protein: Protein is essential for maintaining muscle mass and supporting the liver’s function. However, in advanced cirrhosis, the liver’s ability to process protein may be compromised, leading to a condition called hepatic encephalopathy. In such cases, protein intake may need to be limited. The type and amount of protein should be discussed with your healthcare provider.
4. Eat a Balanced Diet: Consume a variety of nutrient-dense foods, including whole grains, fruits, vegetables, lean proteins, and healthy fats.
5. Avoid Alcohol: If cirrhosis is due to alcohol consumption, it is crucial to completely avoid alcoholic beverages.
6. Consider Supplements: Cirrhosis can lead to malabsorption of certain vitamins and minerals. Your doctor may recommend supplements like vitamins A, D, E, K, and calcium, depending on your specific needs.
7. Be Cautious with Medications: Some over-the-counter medications and supplements can be harmful to the liver. Always consult your doctor before taking any new medications or supplements.
8. Watch for Hepatic Encephalopathy: This condition may cause confusion and altered mental status. If you experience such symptoms, your doctor may recommend reducing protein intake and using lactulose or other prescribed medications to manage it.
9. Small, Frequent Meals: Eating smaller, more frequent meals can help with digestion and nutrient absorption.
10. Avoid Raw Seafood: If you have cirrhosis, it’s essential to avoid raw or undercooked seafood to reduce the risk of infection, especially if your liver function is compromised.
Remember, the dietary recommendations for cirrhosis can vary based on the severity of the condition and individual health status. Therefore, it’s crucial to work closely with your healthcare team to develop a personalized diet plan that best suits your needs.
For More Details Click Now:https://www.drpathikparikh.com/diet-in-cirrhosis/
#best hepatologist in ahmedabad#hepatologist in ahmedabad#best doctors for liver disease in ahmedabad
0 notes