Don't wanna be here? Send us removal request.
Text
Demand Ischemia
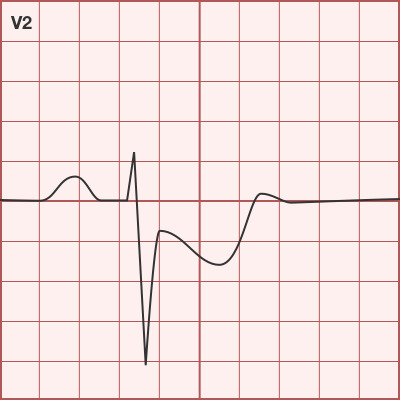
So a patient comes in with a chief complaint of chest pain and we see widespread depressions, but no elevations. The patient is pale and diaphoretic, his pulse is high, and his oxygen saturation is low. Our immediate thought is a pulmonary embolism causing heart strain. We order the Angiography scan which requires me to check the kidney function before administering contrast, and we get this unexpected result on our bedside lab machine

Never have I had a hemoglobin so low it didn’t show on the iStat. I went up to the provider and let her know. We redid it with the same result. Lab called and told me they received a suspiciously low hemoglobin and wanted to make sure I didn’t dilute the sample before informing me the hemoglobin was 3.5. They also informed me that the Troponin was positive.
Because of his clinical condition and deteriorating cardiac status, this patient received 2 units of red blood cells on a rapid infuser in the emergency department and was transferred to ICU with a diagnosis of GI bleeding.
Demand ischemia occurs when the energy demand of the heart exceeds its energy supply. Usually this is seen in patients with extremely high heart rates, but it is also possible to see the same when oxygen supply is very low from conditions such as hypoxia and anemia, as demonstrated in this case.
163 notes
·
View notes
Text
Beta-blocker Overdose
A patient came in after taking a 60 day supply of 25mg Carvedilol. He presented with a heartrate in the 50's, and a blood pressure, well, also in the 50's. 50/30 was the lowest. He was drifting in and out of consciousness, so we pushed atropine, the first line drug for bradycardia, to no effect.
You know it's gonna be fun when you call poison control, you tell them what's going on, and their first response is "ooooo that's not good." Poison control recommended Glucagon, 5-15mg IV push followed by a drip of 5-15mg every hour. This comes in 1mg vials, so we had to mix and draw up a lot of these vials. (See below)

He did respond. His pulse was now around 80, and we kept his blood pressure between 95 and 105 systollic. He was placed on a drip of 10mg/hr. I feel sorry for the pharmacist that had to mix the bag of 30mg of Glucagon. Central pharmacy also told us they only had 6 more glucagons in stock after making this bag, so if he wasn't better in 3 hours, we would have a problem.. but that was a problem for ICU to handle (I love you, ICU nurses)!
Glucagon has inotropic effects that bypass the beta blockade, this allows it to increase heartrate and blood pressure even in the presence of beta blockage. Glucagon also counteracts the negative effects of the beta blockade on a patients blood sugar.
A very interesting case with an interesting management strategy.
880 notes
·
View notes
Text
We all started somewhere
Recently I got a message from a new grad nurse who was freaking out. I also got an email from a friend of mine who’s sister is a new grad nurse. She’s freaking out too. Here is my long loooong piece of advice that I give to all of you new grads. We were all there. We all started somewhere. Even the mama or papa nurse on your unit who has been there since Flo and Clara were walking the halls. We were all new at one point or another and we didn’t know what we were doing. Me when I think back to my days on orientation:

My main preceptor was honestly one of the worst people I’ve ever had the unfortunate pleasure of working with. She was impatient, unprofessional, and a terrible teacher.

Not too far off from how she acted towards me. Perhaps it was a terrible meshing of personalities. Regardless, I cried on my first day with her yelling at me (in a patient room no less) because I didn’t know how to zero an arterial line. I didn’t cry on my second day, but that was also because she wasn’t there :) I didn’t know how to manage my time and frequently had to stay late charting. Much of my shifts with her were spent with her like this:

I had so many days where I wanted to quit. I felt like I wasn’t cut out for the job. I felt like I made a really bad decision in jumping from nursing school to the ICU, let alone the bananas environment of my ICU. I told my parents this, tearfully and with a lot of frustration. I didn’t feel comfortable on the unit, with the patients, or with anything that I was doing. I felt like a mess. I couldn’t figure out a way to manage my time well and felt like I was prioritizing things all wrong. Then I went on nights. Now I’m not saying that night shift is the saving grace of anyone’s orientation, but it was for me. I had a different preceptor for nights and it made all the difference. He was patient but firm, knew when to give me a push to get moving or when to hold back and let me find my way. He told me once after a shift, “You’re doing just fine. You know what you’re doing. It’s hard in this unit. I started on a floor unit and felt the same way. The problem with our unit (the ICU) is that our patients are that much sicker and the stakes are that much higher.”

Having him say that to me, along with repeating those thoughts to myself, helped me a lot. My manager said the same thing to me as did another nurse during day shift when my main day shift preceptor yelled at me in front of the whole nurses station. To put it in a nutshell, some people just shouldn’t be preceptors. They may be good nurses, respected nurses even throughout the unit and hospital. But when they don’t have patience or the ability to work with you as a new nurse, they shouldn’t be precepting. I like to think of it as being bilingual. I can be fluent in the language of nursing and know all of the various things, skills, idioms etc. But if I can’t figure out how to explain and teach that language to someone who only has a very basic or limited knowledge, I shouldn’t be given that responsibility. Rome wasn’t built in a day. Skills, managing your time, and getting things done perfectly and in a succinct manner takes time. Believe me, things take time. No one becomes master in a day, a week, or even a year. You’re constantly learning. I know I sure am. There are some things that you will never be good at. For some people, that’s IVs. For others, that’s getting those sheets so perfect that it looks like you ironed them and they were placed on the bed by angels. Getting the flow of charting, especially if you’re working in a system that you’re not used to (like Epic, Cerner, etc) takes time. Because lets be real, that’s unfortunately where a ridiculous portion of our life is spent.

Ask your preceptors or other nurses about how they plan their day/charting/etc. When your preceptor is telling you that you’re too slow on certain things, ask them how they do that (ex. discharging a patient) and what specific things you can change/add/adjust. I feel like a lot of people are terrified of their preceptors. Since I’ve been precepting a new grad myself these past few months, I’ve realized there’s a two way problem. I am doing things the way I have been for years now and I could do a lot of them in my sleep. I forget that my orientee doesn’t always know where to look for things on the chart or where to find certain things/do certain things. I forget that she doesn’t know how XYZ things work or who you have to call to get stuff done. What has become a second nature to me isn’t even a first to them, so I make sure to follow up with my orientee regularly and she knows that she can ask questions if there’s something that she doesn’t understand why/how to do or if something may seem contradictory or a little different than how we learned in nursing school. Even when you get off orientation, you’re probably going to be worried about how to do things. Look at your parameters or orders that are given (such as temps,HR, BP goals, etc) for guidance with that specific patient. Ask questions, speak up, and consider notifying the proper people when you don’t feel comfortable with something. We’d all rather you ask for help or information then just blindly do something and completely fuck it up. Ask your preceptor about how to best delegate certain tasks or what to do when you don’t have people (like techs) to delegate to.
Be patient with yourself. Like I said, no one is a master in a day. You’re probably not going to get all of those IV starts or blood draws on the first try and you’re probably not going to make everyone happy. Think of orientation as learning to swim. Maybe you can kind of do it and get across the pool with your floaties and your preceptor’s guidance. Some days you’re going to feel like Michael Phelps or Katie Ledecky and simply own your shift. Things will go smoothly and everything will fall into place nicely.

Other days, you’ll be lucky if you can get across without drowning. Believe me, we all still have those days from time to time. As someone once told me early on, as long as your patients are alive and you addressed/did things that you were supposed to do to the best of your abilities, you’ll be okay. Maybe you did it a little slower than people usually do or not as succinctly, but everything still turned out ok. TL;DR: being a noob nurse is rough. Really rough, especially if you’re not getting the support that you need. Be there for yourself, your fellow new grads, and keep your head up. It can get better.
359 notes
·
View notes
Photo







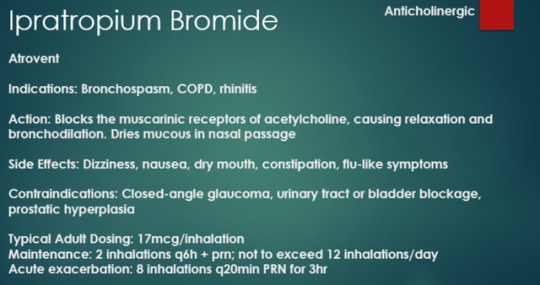


Common Drugs Part II
For all medication series click here
912 notes
·
View notes
Photo

#Repost @physiciandoodles ・・・ #EmergencyMedicine #Pharmacology #Medicine https://www.instagram.com/p/By24y8whdgD/?igshid=iuank464035p
15 notes
·
View notes
Text






A collection of really good posts on mental health.
OP by CrazyHeadComica
2K notes
·
View notes
Photo

#Repost @crazy.medicine ・・・ Anatomy of stethoscope. https://www.instagram.com/p/BykQIlFhYxU/?igshid=eqonw5kwme11
55 notes
·
View notes
Photo

#Repost @physiciandoodles ・・・ Le Fort Fractures are fractures involving the intrinsic weak lines through the mid face. Dr Rene LeFort was credited in describing these three lines and creating the classification. Type 1 (aka horizontal maxillary), Type 2 (aka pyramidal maxillary) and Type 3 (aka craniofacial dysfunction). So: Speak no evil- transverse fx line See no evil- pyramidal fx involving nasal bones, maxilla, and orbital floor Hear no evil- craniofacial dislocation with involvement of the zygomatic arches #emergencymedicine #trauma #omfs #doodle #medstudent #medicaleducation #ER #ortho https://www.instagram.com/p/BytPZwnBoyL/?igshid=1wbg3jfbfwxde
23 notes
·
View notes
Photo

#Repost @doctor.__.insta ・・・ Aorta branches. #anatomical #anatomy #medicine #oddities #s #arsanatomica #cabinetofcuriosities #anatomicalcollector #antiquemedical #antiqueanatomicalmodel #antiquescientific #wunderkammer #vintagemedical #cabinetdecuriosit #medicalstuff #medicalmodels #medicalantiques #curiosity #curiosities #ecorche #museum #anatomymodel #palazzopoggi #anatomicalwax #anatomicalmuseum #head #museianatomici #waxmodel #wax #bhfyp https://www.instagram.com/p/BynyWSNB024/?igshid=1sudx9ynu79d5
34 notes
·
View notes
Photo

#medical #medicine #doctor #health #hospital #healthcare #nurse #doctors #medstudent #surgery #medicalschool #nursing #medschool #medicalstudent #nurselife #love #surgeon #nursingschool #nurses #anatomy #medlife #nursingstudent #science #paramedicsworld #nursesofinstagram #physician #wellness https://www.instagram.com/p/BymayLznAxA/?igshid=r1arl89x5jkh
31 notes
·
View notes
Photo

#Repost @physiciandoodles ・・・ While you should not use qSOFA to diagnosis sepsis, you can use it to predict inpatient mortality in those you consider high risk. It is only helpful in patients 18yrs or older with a suspicion for infection in a non ICU setting. It can help increase awareness of a severe infectious process and prompt further testing and/or closer monitoring.
HAT is a nice mnemonic I learned while at @kingscountyem Hypotension- SBP less than or equal to 100 Alert - GCS less than 15 Tachypnea- RR greater than or equal to 22 https://www.instagram.com/p/BynySX6Boh-/?igshid=go3fgf48g6bs
11 notes
·
View notes
Photo

#Repost @doctormedicine_ ・・・ #doctor #doctors #medicine #medical #skill #girl #surgeon #anatomy #hospital #medstudent #photographic #Beginner #Photographer #nice #photo #like #and #followme #nature #anatomie #doctormedicine https://www.instagram.com/p/BxVTs-ohZYF/?utm_source=ig_tumblr_share&igshid=hpjpknbfq0j
48 notes
·
View notes
Photo

#Repost @medicalterms ・・・ #medical #medicine #doctor #nurse #md #medic #medicalschool #medschool #paramedic #finals #exams #medschoollife #doctorintraining #premed #dr #medstudent #surgeon #dentalstudent #science #surgery #anatomy #lol #humour #paschool #pastudent #medico #usmle #studentlife #unilife https://www.instagram.com/p/Bw1e-9-hMSA/?utm_source=ig_tumblr_share&igshid=qkp2n0uwhmh9
26 notes
·
View notes
Photo

#Repost @the_resuscitationist ・・・ . THE CRASHING ASTHMATIC. . But first, remember “NOT all that wheezes is asthma”. Ddx: foreign body, infection, anatomic abnorms, psychogeni, trauma (pneumothorax), chf, copd, bronchitis, cardiac/acs. . . QUESTIONS TO ASK: 1. Timelines of presenting case? 2. Med compliance and list? 3. Followed by a pulmonologist? 4. Ever been intubated? 5. Ever been admitted ICU? . . MARKERS OF BADNESS: - cant speak in full sentences - cyanosis, sweating - accessory muscle use - “shocky” vitals - quiet “silent” chest FEV1 <40% perdicted, Spo2 <92%, PaO2 <60, PaCo2 >45. . NOTE: please consider placing severe asthma in a trauma bay. Portable CXR, ABG, PeakFlow, EKG, multiple IV access. Labs as clinically indicated. Bedside US are amazing tools. . . MANAGEMENT: 1. Supplemental O2 (hypoxia main cause of death) 2. BetaAgonist (albuterol) nebs and continuous. First line therapy as bronchodilator. 3. Anticholinergic: (Atrovent) inhibit vagal cholinergic tone and bronchodilation 4. Steroids: given <1h presentation decreased rates hospital admission 5. EPI: given IM, IV, nebs (1:1000) 6. MAG: smooth muscle relaxer 2-4g/IV over 30-60min 7. Terbutiline IM/drips 8. Ketamine 0.1-0.3 mg/kg for bronchodilation and anxiolitic 9. Heliox or anaesthetic gas (hard to arrange if crashing in ER) 10. ECMO (case reports)
KEY: sever asthmatics have blown off Co2 and are volume down. Give fluids! Also NIPPV can assist and prevent ETT, especially with the pressure support. Make sure no contraindications for BiPap. . . INTUBATION: fluid bolus, have push dose pressors and acls meds ready. Consider DSI. Use Ketamine if available. .
VENT: FiO2 1 then titrate Spo2 >94% Rate 6-8bpm TV 5-6ml/kg IBW I:E >1:2 Peep <5 Target plateu pressure <20 . ***ASTHMATIC ARREST*** 1. Disconnect from vent 2. Squeeze chest (autopeeping) 3. Consider bilat chest tube 4. Fluid bolus 5. Consider hypoKalemia (Beta agnosit shift from serum to cells) . Please add if I missed anything! CHEERS TEAM! Image credit - beins apparel at zazzle.co.uk #asthma #lungs #breath #oxygen #pulmonology #puff #medic #doc #medicine #doctor #hospital #drugs #pharm #rn #nurse #paramedic #ems #emt #school #vent #ambul https://www.instagram.com/p/Bw1fQYOh-Cp/?utm_source=ig_tumblr_share&igshid=2xxh6exgjw66
14 notes
·
View notes


