Don't wanna be here? Send us removal request.
Text
Torsion of an Ovarian Endometrioma: About an Uncommon Case Report
Abstract
Endometrioma, when its size is ≥ 5 cm, can be complicated by a torsion of the ovary. In this case it is a diagnostic and therapeutic emergency with respect to the many complications of ovarian torsion including necrosis.
We report a case of endometrioma diagnosed by a torsion of the ovary. The context clinic was dominated by acute pelvic pain; the ultrasound showed a huge left cystic ovary, and the laparotomy revealed a torsion of the left adnexa. A detorsion and cystectomy was performed and the confirmation of the endometrioma was provided by the histology of the surgical specimen.
The difficulty lies in the diagnostic and therapeutic choice to preserve or not the ovary. The indications are therefore discussed on a case-by-case basis and depend on many parameters, the most important of which is the intraoperative viability of the ovary after its detorsion.
Conclusion
Adnexal torsion induced by endometrioma has rarely been reported. Due to associated pelvic adhesions. However, it constitutes the fifth gynecological emergency. It is important to be aware of the possibility of adnexal torsion in all patients of all ages presenting with acute pelvic pain, as it can have consequences for potential fertility if not treated promptly. The therapeutic choices are discussed on a case-by-case basis and depends on many parameters, the most important of which is the intraoperative viability of the ovary after its detorsion.
To Know about this article follow at: https://juniperpublishers.com/gjorm/GJORM.MS.ID.555762.php
To Know More About Open Access Journals Please click on: https://juniperpublishers.com/index.php
0 notes
Text
A Case Study on PCOS
Abstract
Polycystic ovary syndrome (PCOS)is a condition in which the ovaries produce an abnormal amount of androgens, male sex hormones that are usually present in women in small amounts. Features of PCOS in this case are oligomenorrhoea and left ovary bulky (not meeting criteria of Rottadarm,10cm size, >10 follicles, >10 mm follicles). Her symptoms aggravated leading to hospitalization with hypoglycaemia. Initial work up showed decreased gonadtrotpins and raised insulin levels with raised prolactin and with behavioural therapy and small frequent meals there is no recurrence of hypoglycaemia. Initial work up showed decreased gonadtrotpins and raised insulin levels with raised prolactin and with behavioural therapy and small frequent meals there is no recurrence of hypoglycaemia and has normalization of FSH, LH, Estradiol and prolactin with normal insulin levels. Clinical and biochemical profile is suggestive of functional Hypothalamic Amenorrhoea.
Conclusion
PCOS is extremely prevalent and probably constitutes the most frequently encountered endocrine (hormone) disorder in women of reproductive age. PCOS is one of the most common causes of female infertility, affecting 6% to 12% (as many as 5 million) of US women of reproductive age. It affects 4% - 20% of women of reproductive age worldwide.
Read More About This Article: https://juniperpublishers.com/gjorm/GJORM.MS.ID.555761.php
To know more about Global Journal of Reproductive Medicine https://juniperpublishers.com/gjorm/index.php
0 notes
Text
Homocysteine as a Predictor of Preeclampsia
Abstract
Homocysteine is an amino acid that is a product of methionine metabolism, is related to preeclampsia in 20-30%, the increase of this or hyperhomocysteinemia may result from the genetic defect of the enzyme methylenetetrahydrofolate reductase involved in the synthesis of homocysteine. Maternal mortality due to preeclampsia is up to 44% and perinatal mortality is reported at up to 27.8%. The objective of this research was to determine homocysteine levels as a predictor of preeclampsia in pregnant women 12 to 20 weeks pregnant. This was an observational, longitudinal and prospective investigation. The study population were patients attending the first antenatal care consultation between 12 to 20ava. weeks, the sample was random that included 360 patients who determined serum homocysteine Sand excluded 48 patients whodid not meet the inclusion and exclusion criteria; they found homogeneity among the patients, 270 patients (86.5%) had a normal evolutionary pregnancy, 27 patients (8.65%) had gestational hypertension, 9 (2.88%) mild preeclampsia and 6 patients (1.9%) severe preeclampsia, none developed HELLP syndrome. Increased homocysteine levels were found in 9 patients who were not related to hypertensive pregnancy disorders. In the present research, homocysteine was not shown to be a predictor of hypertensive disease in pregnancy.
0 notes
Text
Molar Twin Deliveries with Coexisting Fetus at Term: Concerning Two Uncomplicated Cases of Gestational Trophoblastic Tumor, From 2015-2021, In Conakry, Guinea
Abstract
The coexistence of a molar pregnancy with a live fetus is a rare entity of difficult diagnosis and treatment. Continuation of the pregnancy until full-term delivery is possible. We report two cases of twin molar deliveries observed empirically from 2015-2021, in the gynecology-obstetrics department of the Donka national hospital and in the maternity ward of the Jean Paul II hospital in Conakry. The discovery was made on ultrasound of the first trimester of pregnancy and macroscopic examination of the placenta. One of the neonates was alive, a healthy female and the other was polymal formed with facial dysmorphism, omphalocele and sexual ambiguity, fresh stillborn. There was no maternal complication towards a gestational trophoblastic tumor (T.T.G) in both cases. Efforts must be made in the prevention of T.T.G. by screening for twin molar pregnancies with healthy fetuses on transvaginal ultrasound in the first trimester, the dosage of HCG in the face of unexplained metrorrhagia, macroscopic observation of the placenta after each delivery and biopsy sampling of any suspicious placenta.
Introduction
Complete moles with a coexisting fetus, evolving at term with spontaneous vaginal delivery, without fetal and maternal complications, are rare. Early diagnosis of this association leads in the majority of cases to termination of pregnancy on the one hand because of the frequency of triploidy and on the other hand because of the maternal risk and the possibility of progression to persistent trophoblastic disease [1]. We report two particular cases of twin molar deliveries at term without fetal complication and without progression to maternal gestational trophoblastic disease in the gynecology-obstetrics department of the Donka national hospital, the Teaching Hospital (C.H.U) of Conakry and in the maternity ward of the Jean Paul II hospital in Conakry.
Patients and Observations
Case 1
This was Mrs. D.F.B, aged 19, primigravida and primiparous, with no particular history, admitted while in labor at the gynecology- obstetrics department of Donka National Hospital, Conakry Teaching Hospital, with two results of ultrasound performed with a transparietal probe during her pregnancy. These results did not mention any notion of hydatidiform mole or associated congenital malformation. The pregnancy would have progressed normally until its term without maternal or fetal complications. It was only after the delivery of a fresh stillborn, polymalformed (with facial dysmorphism, omphalocele and sexual ambiguity) child, that the macroscopic examination of the placenta made it possible to make the diagnosis of presumptive mole twin by the presence of a normal placenta attached to a vesicular mass characteristic of a mole. The biopsy sample allowed the histological diagnosis of a complete mole. The post molar follow- up had been organized without maternal complication 61 days before the closure of the service for renovation, on October 5, 2015.
Case 2
This was Mrs. H.C, seamstress, 30 years old, gravidity of 5 and parity of 5 including a twin birth and a laparotomy for ruptured ectopic pregnancy (GEU), who came on her own for a consultation for incoercible vomiting, physical asthenia on a menorrhea of 3 three months, June 19, 2020. The clinical examination had objectified a uterine height greater than the age of amenorrhea and dating ultrasound had made it possible to observe, intrauterine, a normal eutrophic fetus of 13 weeks – Amenorrhea (W.A) and a poorly vascularized heterogeneous multicystic mass. The beta HCG serum marker level was 16000IU/l. We had concluded a twin molar pregnancy and animated counseling on the interest of a medical termination of pregnancy to avoid the risks associated with serious maternal complications of trophoblastic tumor including choriocarcinoma. The couple, after a delay of two weeks, had opted to continue the pregnancy until its term. A pregnancy monitoring and childbirth preparation plan had been drawn up with the pregnant woman, whose morphological ultrasound at the 23rd W.A of the second trimester carried out on 03/09/2020, which had objectified a mass of 81 x 97 mm, in previa position. The pregnancy had progressed, without fetal and maternal complications, at 40 WA 2 days and ended with a vaginal delivery of a normal female child, alive and weighing 2830 grams. The woman had benefited from active management of the third stage of labor (TSLM) and digital uterine dissection to confirm the uterine cavity. Macroscopic examination of the adnexa had confirmed the presence of two separate placentas, joined together (Figure 1), one of which appeared normal and linked to the umbilical cord and had a histologically confirmed vesicular mass of “complete mole”. The planned post-molar follow-up was regular with progressive regression of the beta HCG level until negativity on the fortieth day of delivery without any clinical particularity on the closing date of January 31, 2021.
Discussion
The diagnosis of the association of a live fetus with a normal karyotype with a hydatidiform mole is often difficult, especially in the absence of revealing clinical signs [2,3]. The diagnostic modalities of molar twin pregnancy associating a complete mole with a healthy fetus were different due to the early ultrasound detection in the first trimester and the observation of the placenta. The lack of diagnosis of the coexisting mole during pregnancy despite the two ultrasound examinations in the first case would be linked to the age of the ultrasound scanners, which are often second-hand, the technique used (endovaginal in the first trimester or transparietal) and of the operator’s experience in the first observation. Early ultrasound detection made it possible to develop a follow-up plan for pregnancy, childbirth and postpartum in the second case. In the event of a twin pregnancy associating a live fetus and a molar pregnancy, the pregnancy can be continued until term if the patient wishes after having been informed of the risks and the most frequently reported complications (hemorrhages, late miscarriage, fetal death in utero and preeclampsia) [3]. Evacuation of the pregnancy is required only in cases of fetal anomalies or deterioration of the maternal condition [4]. The probability of obtaining a live birth varies between 16 and 56% [5] or 16 and 60% [4] deliveries. The continuation of the pregnancy is against payment given the risks of immediate and distant maternal complications. Close monitoring of the mother and fetus can help achieve a favorable outcome [4]. We accepted monitoring despite the maternal risks for one of our two pregnant women. The two pregnancies resulted spontaneously in the normal delivery at term of a healthy living fetus and another which would have succumbed to its multiple malformations per partum. The most feared complication is progression to gestational trophoblastic disease [1]. The diagnosis of postmolar Gestational Trophoblastic Tumor (G.G.T.) can be made according to criteria such as the persistence of h.C.G detectable more than 6 months after uterine evacuation and the histological diagnosis of choriocarcinoma [5]. According to Ikram Boubess et al., who adopted termination of two of these pregnancies, one remotely progressed to an invasive mole [6]. Regular monitoring of h.C.G levels throughout pregnancy and the postpartum period is necessary to detect GTN [7]. For Suksai M et al., a pregnancy with an initial serum h.C.G level of less than 400,000m.U.I/ml is a good candidate for the continuation of the pregnancy and the achievement of fetal viability [8]. The incidence of post-molar GTN is higher in twin pregnancies combining a complete hydatidiform mole (CHM) and a normal fetus than in single CHM [9].
Conclusion
Spontaneous evolution of the association of molar pregnancy with a live-to-term fetus, without immediate fetal and maternal complications, is possible. The most formidable complication, gestational trophoblastic tumor, choriocarcinoma, was not observed during the study period. The prevention of this complication requires the training of providers in endovaginal ultrasound, its systematic practice in the first trimester of pregnancy, ultrasound and biological monitoring of suspected cases during pregnancy, systematic macroscopic examination of the placenta with biopsy of cases suspect for histological confirmation.
0 notes
Text
Birth Injuries are Not Uncommon
Abstract
Childbirth is one of the eternal enigmas, the happiest moment in the life of most women, but also the period in which mom and baby are most sensitive. Thanks to the latest scientific knowledge and modern diagnostics, the incidence of birth injuries is decreasing, and currently amounts to approximately 0.7 percent, ie 7 out of 1000 newborns have one or more associated birth injuries. Forces acting during labor and childbirth can sometimes injure a baby. The incidence of neonatal injuries due to difficult or traumatic births is reduced due to increased cesarean section, instead of performing heavy turns, vacuum extractions, or high forceps. Traumatic childbirth is expected when the mother has small pelvic dimensions, when the child appears large for gestational age, or when the child is in a butt position or some other abnormal position, especially in a firstborn. In such circumstances, the course of labor and the condition of the fetus should be closely monitored.
Recognition
Recognition of trauma and delivery accidents is vital in order that early remedy may be initiated [9]. Review the exertions and delivery records for hazard elements, along with a extended or abrupt exertions, extraordinary or tough presentation, cephalopelvic disproportion, or mechanical forces, along with forceps or vacuum used at some stage in transport. Also overview the records for a couple of fetus deliveries, large-for-date infants, excessive prematurity, large fetal head, or newborns with congenital anomalies.
Complete a cautious bodily and neurologic evaluation of each newborn admitted to the nursery to set up whether or not accidents exist. Inspect the top for lumps, bumps, or bruises. Note if swelling or bruising crosses the suture line. Assess the eyes and face for facial paralysis, watching for asymmetry of the face with crying or look of the mouth being interested in the unaffected side. Ensure that the newborn spontaneously actions all extremities. Note any absence of or lower in deep tendon reflexes or extraordinary positioning of extremities.
Assess and report symmetry of shape and function. Be organized to help with scheduling diagnostic research to confirm trauma or accidents, if you want to be crucial in figuring out remedy modalities.
Conclusion
Childbirth injuries are not uncommon in obstetrics. They occur due to a relatively very narrow birth canal, where trauma can occur during childbirth, ie the passage of a child from the uterus to the outside world. As a rule, mechanical injuries of newborns are a consequence of difficult childbirth, and hypertrophic newborns, premature infants, and newborns with pelvic presentation are especially exposed. Further predisposing factors are cephalopelvic disproportion, labor irregularities and prolonged childbirth. The use of modern obstetric care can significantly reduce and alleviate birth injuries.
To Know More About Global Journal of Reproductive Medicine https://juniperpublishers.com/gjorm/index.php
0 notes
Text
Cylinders and Assemblage- Sertoli-Leydig Cell Tumour -Ovary
Sertoli-Leydig cell tumour is an exceptionally discerned, ovarian neoplasm composed of sex cord or Sertoli cells admixed with stromal component expounded by Leydig cells. Sertoli-Leydig cell tumour may occur in association with DICER1 syndrome or emerge as a sporadic phenomenon. Sertoli-Leydig cell tumour manifests as well differentiated, moderately differentiated or intermediate grade and poorly differentiated neoplasms. Additionally, categories such as Sertoli-Leydig cell tumour with heterologous elements or retiform variant of Sertoli-Leydig cell tumour may be expounded. Majority of paediatric Sertoli- Leydig cell tumours are moderately differentiated or poorly differentiated, concur with DICER1 syndrome and frequently display heterologous elements or retiform tumour configuration. Histological categorization of neoplasms with enhanced tumour grade appears challenging [1,2].
Well differentiated tumefaction exhibits distinctive Sertoli cell and Leydig cell components. Moderately differentiated or minimally differentiated neoplasms appear devoid of well-formed Sertoli cell tubules with scant Leydig cells [1,2].
The infrequent, paediatric, preponderantly unilateral ovarian neoplasm is commonly delineated within young females with mean age of tumour emergence at 25 years although postmenopausal women may be implicated. Retiform tumour configuration or germline DICER1 mutations occur in neoplasms occurring in younger females [1,2].
Sertoli-Leydig cell tumour is associated with DICER 1 syndrome which is an exceptional, tumour predisposition syndrome engendered by germline mutations within DICER1, a gene which encodes RNase III enzyme confined to microRNA maturation pathway.
Germline mutation expounds as a truncating mutation which may comprehensively incriminate the gene. Second hit somatic mutation occurs as focused, hotspot missense mutation implicating RNase IIIb domain of DICER [1,2].
Sertoli-Leydig Cell Tumour Exhibits Distinctive Molecular Subtypes as
• DICER1 mutant wherein moderately differentiated or poorly differentiated tumour exemplifies heterologous elements or retiform configuration and incriminates young subjects [1,2].
• FOXL2 c.402C>G (p.Cys134Trp) mutant wherein moderately differentiated or poorly differentiated tumefaction is devoid of retiform component or heterologous elements and incriminates postmenopausal women [1,2].
• DICER1 / FOXL2 wildtype wherein well differentiated neoplasm appears devoid of retiform component or heterologous elements and implicates middle aged women.
• somatic hotspot DICER1 mutations are frequently associated with germline DICER1 mutations [1,2].
• DICER1 mutations commonly appear within moderately differentiated or poorly differentiated neoplasms. In contrast, well differentiated tumours are devoid of DICER1 mutations [1,2].
• Sporadic, moderately differentiated or poorly differentiated Sertoli-Leydig cell tumours harbour somatic mutations within hotspot of DICER1 gene. FOXL2 mutation may concur with DICER1 mutations [1,2]. Clinical symptoms of hormonal or androgenic activity are discerned. However, certain representative features may concur or recede, as denominated with characteristic androgenic symptoms or tumour emergence within elderly, peri-menopausal or postmenopausal women. Clinical manifestations as pelvic pain or pelvic tumefaction may be discerned. Ascites or tumour rupture is exceptional [1,2]. Androgenic hormonal symptoms or virilisation is commonly represented as hirsutism, clitoromegaly, breast atrophy, menstrual irregularities or amenorrhea [1,2]. Oestrogenic hormonal manifestations are infrequently observed. Histological subtype and tumour grade are concordant to clinical behaviour [1,2]. Upon gross examination, predominantly unilateral tumefaction may demonstrate a cystic component, foci of heterologous elements or retiform configuration. Poorly differentiated neoplasms exhibit foci of tumour necrosis. Tumour magnitude varies from < 1 centimetre to ~ 35 centimetres with mean diameter of 12 centimetres to 14 centimetres. Characteristically, cut surface is solid and tan to yellow [1,2). Frozen section exemplifies an admixture of Sertoli cell tubules or compressed cellular cords variably intermingled with Leydig cell clusters. Intracytoplasmic Reinke crystals may be delineated [1,2].
• Well differentiated Sertoli-Leydig cell tumour expounds open or compressed Sertoli cell tubules admixed with clusters of Leydig cells accumulated within intervening stroma. Cellular and nuclear atypia or mitotic activity is absent [1,2]. Sertoli cells appear as low, columnar to cuboidal cells with spherical to elliptical nuclei, nuclear grooves and miniature nucleoli. Leydig cells demonstrate abundant, eosinophilic cytoplasm with characteristic Reinke crystals, lipofuscin pigment and spherical nuclei [1,2].
• Moderately differentiated Sertoli-Leydig cell tumour characteristically depicts diffuse or lobulated architecture with alternating hypo-cellular and hyper-cellular areas. Sertoli cells configure compressed tubules, cords or diffuse sheets wherein cells are imbued with hyperchromatic, elliptical or spindle-shaped nuclei. Mild to moderate nuclear atypia and mitotic figures ~ 5 per 10 high power fields are discerned. Exceptionally, miniature clusters of Leydig cells appear commingled with Sertoli cell component. Discernible follicular differentiation may simulate juvenile granulosa cell tumour [1,2].
• Poorly differentiated Sertoli-Leydig cell tumour is constituted of diffuse sheets of immature, sarcomatoid Sertoli cells with configuration of infrequent, indistinct cords. Nuclear atypia is moderate to marked. Mitotic activity is significant with ~ 20 mitoses per 10 high power fields. Undiscernible Leydig cells are represented by few, miniature clusters, characteristically accumulated upon periphery of tumour nodules [1,2].
• Sertoli-Leydig cell tumour with heterologous elements is constituted of epithelial or mesenchymal elements represented within moderately differentiated, poorly differentiated or retiform Sertoli-Leydig cell tumour. Benign, borderline or malignant intestinal or gastric type mucinous epithelium is a common heterologous element. Trabecular or goblet cell carcinoid tumour may arise from heterologous mucinous epithelium. Heterologous mesenchymal elements as cartilage or skeletal muscle are uncommon. Focal differentiation into hepatic parenchyma and elevated serum α-fetoprotein (AFP) levels is infrequent [1,2].
• Retiform variant of Sertoli-Leydig cell tumour demonstrates focal or diffuse retiform pattern with configuration of anastomosing, slit-like, irregular spaces or multi-cystic, sievelike or papillary architecture [1,2].
Sertoli-Leydig cell tumour is immune reactive to general sex cord proteins as inhibin, calretinin, SF1, FOXL2, CD56, WT1, CD99, vimentin, pancytokeratin, Melan A/MART1, CK20, CDX2, AFP, arginase or HepPar1 [3,4]. Sertoli-Leydig cell tumour is immune non-reactive to CK7 or EMA.
Neoplasm is devoid of histochemical staining with reticulin.
Sertoli-Leydig cell tumour requires segregation from neoplasms such as endometrioid adenocarcinoma, adult granulosa cell tumour, fibroma or tubular Krukenberg tumour emerging from metastatic signet ring cell carcinoma. Retiform variant of Sertoli- Leydig cell tumour necessitates distinction from yolk sac tumour or low grade, borderline serous carcinoma ovary. Sertoli-Leydig cell tumour with heterologous elements mandates distinction from carcinosarcoma, teratoma and primary or metastatic ovarian mucinous neoplasms [3,4].
Sertoli-Leydig cell tumour can be assessed with pertinent clinical examination of young women manifesting features such as virilisation with elevated testosterone levels. An ovarian or pelvic tumefaction can be detected upon imaging. Intraoperative frozen section is optimal for cogent tumour evaluation and adoption of relevant surgical procedures. Incriminated subjects depict elevated serum testosterone levels. Sertoli-Leydig cell tumour can be appropriately investigated with imaging of pelvic cavity with techniques as ultrasonography, computerized tomography or magnetic resonance imaging. Upon imaging, a preponderantly solid or solid and cystic adnexal tumefaction is denominated [3,4].
Genetic counselling and assessment of germline DICER1 mutation is recommended [3,4].
Optimally, Sertoli-Leydig cell tumour occurring in young women is treated with fertility sparing surgical techniques. Sertoli-Leydig cell tumour can be appropriately managed with conservative, fertility sparing surgical procedures as unilateral salpingo-oophorectomy. Cogent tumour staging along with or devoid of regional lymph node dissection can be performed in young women exemplifying stage I tumours. Incriminated elderly females, where fertility preservation is unnecessary, can classically be subjected to bilateral salpingo-oophorectomy, total abdominal hysterectomy and comprehensive surgical staging of tumefaction. Platinum based adjuvant chemotherapy is beneficial in treating moderately differentiated or poorly differentiated tumours and neoplasms with heterologous mesenchymal elements, advanced tumour stage or tumour rupture [3,4].
Biological behaviour is contingent to histological subtype and tumour grade. Well differentiated Sertoli-Leydig cell tumours are essentially benign neoplasms whereas ~ 10% of moderately differentiated and ~59% of poorly differentiated tumours demonstrate malignant biological behaviour. Occurrence of heterologous elements, retiform tumour configuration, tumour rupture, tumour dissemination beyond ovary, stage II or advanced stage neoplasms delineate an adverse prognostic outcome. Neoplasms demonstrating germline DICER1 mutations exhibit favourable prognosis, in contrast to tumours with singular somatic DICER1 mutation [3,4].
To Know More About Global Journal of Reproductive Medicine https://juniperpublishers.com/gjorm/index.php
0 notes
Text
COVID-19 Vaccination in Pregnancy
Abstract
COVID-19 pandemic has affected human lives globally. The most important measure to control this pandemic is vaccination and to follow public health measures like wearing facemasks, maintaining social distancing, and hygiene. Over the last one-year, numerous vaccines have been formulated under rigorous regulatory rules globally. During the process of vaccine development, antenatal and breastfeeding women were not included in vaccine research trials, even though they were at increased risk of developing severe COVID-19 infection in comparison to non-pregnant women. There is reassuring data that there are no safety concerns in antenatal patients who received mRNA vaccine in the third trimester and no evidence of increased miscarriage rate if taken at less than 20 weeks of pregnancy. In mRNA vaccine immunized pregnant women, antibodies were found in cord blood. The healthcare staff should provide effective counselling and promote immunization in antenatal women in all trimesters and breastfeeding mothers.
Introduction
COVID-19 pandemic has affected human lives, the healthcare system, and economies globally. The most important measure to control this pandemic is vaccination and to follow public health measures like wearing facemasks, maintaining social distancing, and strict personal hygiene. Over the last one-year, numerous vaccines have been formulated under rigorous regulatory rules globally, against the COVID-19. During the process of vaccine development, antenatal and breastfeeding women were not included in COVID-19 vaccine research trials, even though they were at increased risk of developing severe COVID-19 infection in comparison to non-pregnant women [1]. Recent literature reports that antenatal women with COVID-19 have a high chance of hospitalization, ICU care, ventilatory support, and high probability of preterm labour [2]. Studies also report that there is a 2-3% risk of transmission of COVID-19 infection to the baby and that viral RNA may be present in the breast milk of COVID-19 infected women [3]. American College of Obstetricians and Gynecologists (ACOG) and Centers for Disease Control and Prevention (CDC), recommend that all antenatal women should receive COVID-19 vaccination.
Recently, all over the world, it has been realized that there is an urgent need for including antenatal women in all research trials of the COVID-19 vaccine. According to Developmental and Reproductive Toxicity (DART) studies using Pfizer-BioNTech and Moderna vaccines, there are no direct or indirect harmful effects on antenatal or perinatal outcomes. The CDC recommends that all pregnant, lactating women and women who are planning to conceive, should take this vaccine. There is reassuring data on the safety of mRNA COVID-19 vaccine administration in antenatal women [4]. There is no evidence of an increased miscarriage rate in women who took mRNA vaccine before conception or less than 20 weeks of pregnancy [5]. Surveillance of pregnancies is underway, and CDC is following all women who took vaccination in all the three trimesters of pregnancy to analyze the effects on gestation and neonates. Recent literature found that the mRNA COVID-19 vaccine lowered the risk of infection in pregnant women. In mRNA COVID-19 vaccinated pregnant women, antibodies were found in umbilical cord blood, which may protect the neonates against COVID-19. More research is required to assess the mechanism by which these antibodies will protect the neonates [6]. Pharmaceutical companies manufacturing these vaccines are analyzing information from the various clinical trials in women who took the vaccine and became antenatal during the trial.
Effect of the vaccine in Antenatal Women
There are severe outcomes of COVID-19 infection in antenatal patients and even though vaccination is available for non-pregnant women, there is limited research assessing the effect of any COVID-19 vaccine during gestation. Vaccination in antenatal or lactating women has been approved on the basis of various reviews, cohort studies, clinical research trials, and registries,conducted by joint efforts between the World Health Organization (WHO), CDC, National Institutes of Health (NIH), to assess the vaccine:
(i) safety-no unfavorable effect on maternity outcomes or any possible health hazard to mother or the baby
(ii) efficacy-decrease the incidence of COVID-19 in the antenatal woman or the baby [7].
COVID-19 Vaccine Hesitancy
Even though there is enormous advancement in vaccine development and administration, there is inadequate acceptance for the same, therefore there is a delay in development of herd immunity. For reaching the herd immunity threshold, the immunity at the community level should reach minimum of 75% immunity to halt this pandemic. Even before this pandemic, WHO had classified hesitancy to take the vaccine as one of the top ten hazards to worldwide health [8]. Hence, it is essential to realize the various reasons for this reluctance to take vaccine and address it at the earliest. Through an online survey (Oct-Nov 2020), approximately 50 percent of antenatal women and 70 percent of non-pregnant women had the intention to receive the vaccine [8]. The most common reasons for declining the COVID-19 vaccination during pregnancy were:
i) any risk of exposure of fetus to any possible adverse effects (65 percent)
(ii) vaccine was approved because of government-related reasons (45 percent)
(iii) want to wait and see the studies on the effect of the vaccine in antenatal women
The hesitancy to take the vaccine is a multifaceted problem and variation based on area, race/ ethnicity, gestation, educational level, occupational status, interpersonal and political factors [8]. Healthcare providers need to educate patient on regular basis, to increase the vaccine acceptance rate, especially in antenatal women.
Prior to this pandemic also, immunization during gestation was recommended, which provided immunity to mother and baby from communicable diseases like influenza and pertussis. Presently, several experts recommend that mRNA and adenovirus vector COVID-19 vaccine, will not cause any risk to the fetus or breastfeeding baby [9], although there is no literature on whether there will be trans-placental transfer of intact vaccine particles or not. But the studies done in the past on other lipid nanoparticlebased vaccines suggest that they cannot cross the placenta [9].
Shimabukuro et al. reported the effects of mRNA COVID-19 vaccines, information collected from December 2020 to February 2021, using v-safe surveillance system, 14 percent resulted in pregnancy loss and 86 percent resulted in a live birth, largely immunization was received in the last trimester. They reported preterm birth in ten percent, small for gestational age in three percent, and no newborn mortalities. Proportions of unfavorable maternity and neonatal outcomes in immunized women were similar to incidences in antenatal women before the pandemic. The most common adverse outcome was spontaneous abortion [4]. Many experts have recommended the COVID-19 vaccine as vaccine-induced IgG may be secreted in breast milk and provide additive immunity to the baby against infection . Golan reported there are vaccine-stimulated IgA antibodies in breastmilk 3-4 weeks after vaccination with the mRNA vaccine [10]. They also measured IgA antibody titers in breastmilk and found them to be similar between women who got immunization and COVID-19 infection. A study by Rottenstreich et al. reported efficient placental transfer of anti-spike antibodies after immunization of antenatal women with the Pfizer vaccine [11].
Covaxin recently got WHO approval on 3rd November 2021, after evaluation under the WHO EUL protocol. WHO’s expert group recommended two doses, with gap of four weeks between both doses, in all age groups 18 and above. Covaxin vaccine has 78% efficacy against infection of any severity, two weeks after the second dose, and is appropriate for developing countries due to easy storage requirements. More than 1 lakh pregnant women have received Covaxin in India, with no short-term side effects. More studies are planned to see the effect of Covaxin in pregnant women. Various COVID-19 vaccines are still under investigation and because of non-uniformity in population, rules and regulations in all the countries, evaluation of different COVID-19 vaccines is not possible at present.
Conclusion
COVID-19 immunization is the utmost important measure to control the spread of the pandemic. It is essential to protect the antenatal and lactating women and they should be involved in vaccine clinical trials and anti-viral treatment protocols. The doctors, nursing staff and counsellors should provide evidencebased knowledge and effective counselling to the antenatal and breastfeeding women and promote immunization in antenatal women in all trimesters and breastfeeding mothers.
To Know More About Global Journal of Reproductive Medicine https://juniperpublishers.com/gjorm/index.php
0 notes
Text
Miracle Pregnancy: Management of Poor Responder in In-Vitro Fertilization
Abstract
Background:: Patient-Oriented Strategy Encompassing IndividualizeD Oocyte Number (POSEIDON) 3 and 4 subgroup is common nowadays. We hereby report a case of successful management of POSEIDON 4 patient, who underwent an individualized GnRH antagonist protocol.
Case Presentation:: A 36-year-old woman presented with primary infertility for 10 years. She had undergone multiple cycles of ovulation induction and intrauterine insemination previously. She had previous one IVF failure. Post COVID lockdown, patient was a POSEIDON 4 group patient who underwent second IVF cycle. Three grade 4 oocytes were retrieved after dual trigger. Two 8 celled grade B embryos were transferred on day 3. Patient conceived and had caesarean section at 37 weeks POG, 2.4 kg healthy male baby delivered.
Conclusion:: IVF with self-oocyte can be tried along with proper counselling to decrease the psychological and financial burden on the patient and family, therefore, ruling out oocyte donation as the only treatment option in these patients.
Keywords: POSEIDON 4; IVF; Individualised Treatment; GnRH antagoniste
Abbreviations: ESHRE: European Society of Human Reproduction and Embryology; POSEIDON: Patient-Oriented Strategies Encompassing Individualized Oocyte Number; GnRH: Gonadotrophin releasing Hormone; IVF: In Vitro Fertilization; FSH: Follicle Stimulating Hormone; HMG: Human Menopausal Gonadotrophins; rHCG: recombinant Human Chorionic Gonadotropin; E2: Estradiol; P4: Progesterone; UPT: Urine Pregnancy Test; COVID-19: CORONAVIRUS DISEASE-2019; AFC: Antral Follicle Count; DHEAS: Dehydroepiandrosterone Sulfate; ICSI: Intra-cytoplasmic Sperm Injection; AMH: Anti-Mullerian Hormone; r-hLH: Recombinant Luteinizing Hormone; POG: Period of Gestation; PGT: Preimplantation Genetic Testing
Introduction
Poor responders are often encountered by Reproductive medicine specialists around the world. A lot of research has been directed towards finding reasonable solutions for this group of patients. The lack of a universal definition has induced a considerable degree of heterogeneity to research on stimulation protocols in poor responders. Several definitions and methods have been proposed for the identification of poor responders, for individualization of their treatment, including the European Society of Human Reproduction and Embryology (ESHRE) Bologna criteria for poor responders, and the Patient-Oriented Strategies Encompassing Individualized Oocyte Number (POSEIDON) criteria [1,2]. Here we present a case of poor responder (POSEIDON 4) and her personalised/individualized successful management.
Case Presentation
Patient X, a 36-year-old woman presented with primary infertility for 10 years. She had undergone multiple cycles of ovulation induction and intrauterine insemination previously. Patient was evaluated clinically with thorough history, examination, and investigations. She underwent her first Gonadotrophin releasing Hormone (GnRH) antagonist In-Vitro Fertilization (IVF) cycle in November 2019 as mentioned in protocol (Table 1). The dose of gonadotrophins used was 2625 IU rFSH (Follicle Stimulating Hormone) and 2250 IU HMG (Human Menopausal gonadotrophins), so total 4875 IU of gonadotrophins in first IVF cycle and total 11 days of stimulation. Six oocytes were retrieved after 36 hours of rHCG (recombinant human chorionic gonadotropin) 250 microgram trigger. Serum E2(estradiol) on day of trigger was 1495 pg/ml and P4 (progesterone) 0.9 ng/ml. Conventional IVF insemination was performed with two grade 1 and four grade 2 oocytes, which resulted two 2 celled grade Bembryo, which were transferred on day 2. Urine Pregnancy test (UPT) was done after 16 days which was negative and beta hCG <1.2 IU/ml.
Patient expressed her wish for second attempt and was postponed due to COVID-19 (CORONAVIRUS DISEASE-2019) pandemic. Therefore, DHEAS (Dehydroepiandrosterone sulfate) supplements were prescribed for 6 months till her next recruitment. Post lockdown, the initial AFC (antral follicle count) at start of cycle was low (right ovary=2, left ovary=3). Antagonist Protocol followed as mentioned in table 2. The total dose of gonadotrophins used was 3800 IU rFSH and 600 IU HMG, so total 4400 IU of gonadotrophins in second IVF cycle, total 10 days of stimulation. Three grade 4 oocytes were retrieved post 35 hours of dual trigger (Inj rHCG (Ovitrelle) 250 microgram and inj leuprolide 1 mg subcutaneously). Initially, ICSI (intracytoplasmic sperm injection) was planned because of poor fertilization rate in previous IVF cycle. However, conventional IVF was performed because of poor quality of oocytes. Fortunately, two oocytes fertilized (2 out of 3) and two 8 celled grade B embryos were available for transfer on day 3, much better quality as compared to first IVF cycle. Urine pregnancy test and beta HCG was done after 16 days, which was positive. Single live intrauterine fetus was documented at 6 weeks period of gestation and luteal phase support (Vaginal micronized progesterone 400 mg twice a day and injection micronized progesterone 100 mg intramuscularly OD) was continued throughout first trimester. Patient had caesarean section at 37 weeks POG, 2.4 kg healthy male baby delivered. We are reporting this to spread the message that POSEIDON 4 patients can have successful pregnancy outcomes with individualized/ personalized treatment and that oocyte donation is not the only alternative.
Discussion
The ESHRE Bologna criteria 2011 gave the definition of poor responders [2]. According to Bologna criteria, poor responders are patients from whom we would expect to retrieve 3 oocytes after conventional COS and markers for identifying poor responders are a previous poor response (three oocytes retrieved after COS), AMH (Anti-mullerian Hormone) <0.5 ng/mL or AFC < 3 [1,3]. Though it encompasses a broad, heterogeneous group of patients but it is not considered as clinically relevant for making informed treatment decisions [4-6]. Because it does not differentiate between oocyte quality and oocyte quantity [6]. Suboptimal responders are not widely recognized as a patient subgroup and were categorized either into normal responders or poor responders [1,7]. The POSEIDON Group bridged this gap and formulated these criteria by consensus that identify different groups of low prognosis patients [1]. These were developed specifically with the aim of guiding personalized treatment protocols for second and subsequent cycles, following unexpected suboptimal or poor response. POSEIDON criteria offer the best approach to personalization for poor/suboptimal ovarian responders, to assist the clinical decision-making, patient counselling and prognostication.
The biomarkers to identify suboptimal responders are: (a) previous history of suboptimal response (>4 to 9 oocytes retrieved after COS) (b) AMH > 0.5 to <1.2 ng/mL (c) AFC > 4 to 9. These constitutes 43.3% of patients undergoing IVF treatment according to study by Polyzos et al. [8]. A recent meta-analysis, shows that suboptimal responders and potentially other patient populations are likely to benefit from r-hLH (Recombinant Luteinizing hormone) supplementation with respect to implantation, pregnancy, and live birth rates [9-12]. Age is an important prognostic marker for IVF success, and it is expected that the younger patient will have a 4 times higher chance of live birth as compared to the older patient [13]. In POSEIDON group 3 (age < 35 years, AMH <1.2 ng/ml, AFC<5) patients, recommended protocols are either long GnRH agonist down-regulation or a “primed” GnRH antagonist co-treatment followed by stimulation with a maximum dose of 300 rFSH. In selected cases with a low oocyte yield and based on the estimate made by the ART (Assisted reproductive technology) calculator, DUO-Stim should be recommended for oocyte or embryo accumulation to shorten time to pregnancy [14,15]. With the increasing prevalence of POSEIDON group 4 patients (age >35 years, AMH <1.2 ng/ml, AFC <5) due to delay in age of childbearing [16], the dual effect of poor ovarian reserve (quantity) and age-related decline of quality makes this category of patients difficult to handle [17]. Though oocyte donation is a treatment option but there is a stigma with it especially in Indian society [18]. At the same time, despite poor prognosis, we cannot deny IVF with self-oocyte. Therefore, proper counselling is required explaining the chance of cycle cancellation and risk of empty follicle syndrome.
The case in discussion received starting dose of 225 IU rFSH and 225 IU HMG in first IVF cycle, but still patient had poor outcome in terms of poor quality of oocytes, poor fertilization rate and no clinical pregnancy. Therefore, in the second cycle, even though patient fits in POSEIDON 4 classification, we took the decision to administer 450 IU rFSH from day 2 for 5 days, followed by 300 IU rFSH and 150 IU HMG from day 6 when the antagonist was added. In first and second cycle, total dose and days of gonadotrophins used was 4825 IU and 11 days, 4400 IU and 10 days respectively. This is in complement to the literature that escalating the dose of gonadotrophins and increased duration of stimulation can negatively affect the IVF outcome [19]. Another change in treatment was dual trigger compared to HCG trigger in 1st cycle because it is associated with better IVF outcome in terms of number of total embryos and grade 1 embryos in poor responders’ patients [20]. Following this change in protocol, we had better oocyte yield, fertilization rate, embryo quality, positive urine pregnancy test and ongoing pregnancy at 22 weeks POG (period of gestation). As patient was 36 years old, PGT (Preimplantation Genetic Testing) could be considered to check the ploidy status of the embryos but was avoided due to deleterious effect of embryo loss and further hampering the chance of embryo implantation/viability on biopsy of day 3 embryos [21].
Conclusion
Therefore, would conclude that individualized/personalized treatment is required in POSEIDON 3 and 4 patients, and no fixed stimulation protocol can be followed. IVF with self-oocyte can be tried along with proper counselling to decrease the psychological and financial burden on the patient and family, therefore, ruling out oocyte donation as the only treatment option in these patients.
0 notes
Text
Let’s Talk and Grow Together: A Bidirectional Communication between Granulosa- and Oocyte Derived Factors in the Ovary

Abstract
Reproduction, one of the most active and appealing area of research for endocrinologists and reproductive biologists since many a years, has several faces that remains to be unmasked in terms of its regulatory aspects. Available information on the regulation of oocyte development and maturational competence are gaping and needs elucidation to achieve utmost quality of eggs, a major area of concern. The notion of the somatic follicular cells providing an appropriate microenvironment for the development of oocyte throughout its journey has been replaced with the current perception of a complex yet regulated cross-talk between the granulosa-and oocyte-derived factors to orchestrate follicle development. Interestingly, actions of FSH and LH are mediated or modulated by these locally produced non-steroidal peptide factors from the follicular layer and the oocyte itself (insulin-like growth factors (IGFs), epidermal growth factor (EGF) family members, TGFβ super family members etc.), forming an intimate regulatory network within the ovarian follicles. Present article will provide a deeper insight into the need and underlying mechanisms of action of these growth factors in the intraovarian network to sustain a healthy oocyte.
Read More About This Article: https://juniperpublishers.com/gjorm/GJORM.MS.ID.555569.php
Read More Juniper Publishers Google Scholar Articles: https://scholar.google.com/citations?view_op=view_citation&hl=en&user=xBu_HGEAAAAJ&authuser=1&citation_for_view=xBu_HGEAAAAJ:Zph67rFs4hoC
#gjorm#overy#reproductive medicine#Juniper Publishers Indexing Sites List#Juniper Publishers PubMed Indexed Articles
0 notes
Text
Determinants of Abortion among Youth Seeking Reproductive Health Care in Selected Health Facilities, in Addis Ababa, Ethiopia

Abstract
Background: Globally an estimated 80 million unintended pregnancies, both mistimed and unwanted, occur each year. Unintended pregnancy and births have grave consequences to the mother and family and are global social and health burdens. In Ethiopia, hundreds die in health facilities each year from abortion-related complications, but many more suffer from injuries or illness related to unsafe procedures. Cognizant of these facts and with the intent to reduce maternal death due to unsafe abortion, the Ethiopian government had revised the abortion law in 2005. The national data in Ethiopia showed that about 42% of pregnancies were unintended and the annual abortion rate was 23 per 1,000 women aged 15-44 years in 2008. Thus, it is important to assess the risk factors that predisposes youths to induced abortion in order to design a sound health program for reducing unintended pregnancy and for betterment of maternal health.
Objective: To identify the main determinants of abortion in women of age 15-24 attending Sexual and Reproductive Health clinics in Addis Ababa.
Methods: Descriptive unmatched case-control study was conducted in selected health facilities in Addis Ababa. Cases were women of age 15-24 seeking an induced abortion service and controls were women of age 15-24 that seek ANC service in the clinics. A total of 330 women (110 cases and 220 controls) were studied. Chi-square test and logistic regression analysis were conducted to determine association using SPSS Version 20 after entering data using Epi Info Version 7.1
Result: This study showed that married young women are at lower risk of seeking abortion service than single young women (never married, divorced, widowed) AOR 0.04 (95%CI 0.015-0.13) P <0.001. Use of at least one method of modern contraceptive is also found to be protective factor for young women from having an induced abortion. Young women not using any method have four times higher odds of seeking induced abortion than those using at least one method (AOR 4.3 CI 1.05-17.7 p=0.043). Unintended pregnancy is a determinant that predisposes young women for seeking an abortion service (AOR 33.1 CI 12.5-87.5) p<0.001). It is concluded that young single women who are not using at least one method of contraceptives and those young women exposed to unwanted pregnancy are highly likely to resort to abortion regardless of their faith, belief and attitude towards abortion.
Read More About This Article: https://juniperpublishers.com/gjorm/GJORM.MS.ID.555560.php
Read More Juniper Publishers Google Scholar Articles: https://scholar.google.com/citations?view_op=view_citation&hl=en&user=xBu_HGEAAAAJ&authuser=1&citation_for_view=xBu_HGEAAAAJ:UebtZRa9Y70C
#Juniper publishers#Peer review journals#GJORM in juniper publishers#Reproductive medicine#Open access journals
0 notes
Text
Material Health Literacy
Authored by: Duygu Kavuncuoglu*
Introduction
In the twenty-first century; there have been many developments in medicine such as finding new diagnostic and treatment methods; demographic and epidemiological transformation; changing disease burdens and increasing the burden of non-communicable diseases; increasing the importance of gaining healthy lifestyle behaviors to individuals and preventive health services rather than therapeutic health services. In addition; advances in communication technology have increased the resources for people to obtain health information and access to information has become easier. As a result of the developments both in the field of medicine and technology; the health care providers and the areas where the service is provided have increased as well as the share of health care providers-demanders in the process of making medical decisions-in the management of diseases and in the protection and improvement of their health. As a result of the changing roles of individuals regarding their health; it has led to the necessity of providing the communication between health service providers and service providers correctly and understanding all kinds of health information provided. In addition to the negativities experienced between health service providers and beneficiaries; the low level of socioeconomic level; the lack of information related to the lack of education level; and the difficulties in accessing health services cannot be adequately conveyed to the people [1, 2].
It is possible for individuals to reach their full health potential by taking control of the factors determining their health. For this; people should assume their own health responsibility and have the equipment and skills to make healthy choices based on the determinants of their health [3]. Patients constitute the main part of the health system and the decisions taken by individuals about their diseases significantly affect the effectiveness; effectiveness and quality of health care provided with health outcomes. The decisions taken by the patients are mostly based on their health-related skills; capacities and knowledge. This is called de health literacy de in the literature. Health literacy was first coined by Scott Simonds in 1974 in an article entitled “Health Education and Social Policy “. However; its widespread use in the literature began after the 2003 National Assessment of Adult Literacy (NAAL) study in the USA. As a result of the studies carried out by health researchers and clinicians; the definition of health literacy was first developed and then the concept was expanded by adding alternative terms such as “medical literacy saclike; “patient health literacy” and “clinical health literacy [2-4]. Health literacy is associated with the concept of general literacy; and it is possible for people to develop and make decisions about health care issues throughout their lives; to protect; maintain and improve their health; to access health-related information resources to improve the quality of life; to perceive health-related information and messages accurately and understanding and desires [5, 6].
Health literacy is defined within the framework of the concept of health promotion [7]. The concept of health promotion was defined as 1986 the ability to control and improve the health of individuals geliştirme during the Ottowa International Conference on Health Promotion in 1986. The concept of ok health literacy ortaya has been introduced to include the factors that affect health (determinants of health) and the learning and perception of social; political and economic conditions [8]. However; its widespread use in the literature began after the 2003 National Assessment of Adult Literacy in the United States [9]. Health literacy enables the individual to acquire the level of knowledge; individual skills and self-confidence that will lead to behavior that will improve both individual and community health by changing the lifestyle and living conditions [10]. It supports and improves the individual’s ability to access the right information and service; and the ability to use this service in order to maintain and maintain health [10,11]. It strengthens the use of existing health services more effectively; the creation of quality conditions in health services; and the competence of the individual over his or her health and community health [12,13]. Research shows that people with inadequate health literacy find it difficult to comprehend health information. Inadequate health literacy has been associated with more hospitalization; greater use of emergency services; less preventive health care; poor use of medication; poor understanding of healthrelated messages; and a worse level of health [14,15]. Maternal health literacy can be defined as cognitive and social skills that determine the motivation and ability of women to understand and use the information they can protect; maintain and improve their own health [16]. It is known that prenatal care is important for risk assessment for a healthy maternity and to avoid complications during pregnancy and childbirth. Adequate level of women’s SOY is extremely important for the protection and promotion of both their own and their children’s health. Women with low levels of health literacy will have difficulty in making the right decisions in situations that concern the health of both themselves and their family members; as they will be inadequate in accessing; understanding and interpreting health information [17].
Kohan et al. [18] Examined the impact of maternal health literacy on prenatal care and pregnancy outcomes; found that women with adequate health literacy had significant positive differences in terms of prenatal care frequency; neonatal birth weight; maternal hematocrit; iron and folic acid consumption; weight gain during pregnancy; gestational age at birth; mode of delivery and breastfeeding [18]. Similarly; in the study of Ohnishi et al. [19]; They found that mothers with adequate health literacy had less low birth weight and premature infants; infant mortality was less; and breastfeeding rates were higher than the other group [19]. In some studies; it is reported that pregnant women with low health literacy levels are not adequate and regular in their followup; they do not have their first follow-up in time; and they do not know screening tests such as double-triple screening and glucose load test [20-22]. Increasing knowledge of the mother about pregnancy changes; care in dangerous situations and pregnancy complications are important strategies for prenatal care and better adaptation to pregnancy. It is essential to educate and provide information on the subjects needed during pregnancy; but the most important factor is the perception; understanding and ability to use information in dangerous and inevitable situations. Therefore; it is necessary to carry out basic studies to increase maternal health literacy such as assessment in pregnancy care; identification of maternal literacy issues; identification of available resources; planning for better use of educational materials; written and oral education materials.
In most countries; information that is planned and organized in the prenatal period is given to pregnant women and their spouses through pregnancy preparation classes; and practical applications are provided to improve the ability to use and understand this information. Considering that maternal health literacy affects not only maternal health but also child health; growth and death; necessary health policies and practices should be developed to improve maternal health literacy in order to improve maternal and child health.
To Know More About Please Click on: Journal of Reproductive Medicine
https://juniperpublishers.com/gjorm/index.php
To Know More About Open Access Publishers Please Click on: Juniper Publishers
#Juniper publishers#Peer review journals#GJORM in juniper publishers#Reproductive medicine#Open access journals
1 note
·
View note
Text
Maternal Mortality: Case Reviews and Lessons Learned from the Global Partnerships and the Maternal Fetal Medicine Scientific Forum on Global Health
Authored by: Zekarias Mengistu*
Introduction
The total cattle population for the rural sedentary areas of Ethiopia is estimated to be 43.12million, of which 55.41% are females. Out of the total female cattle population, only 151,344 (0.35%) and 19,263 (0.04%) heads are hybrid and exotic breeds, respectively. With an average lactation length of 6 months and an average daily milk production of 1.44 liters per cow, the total milk produced during the year 2006/07 was recorded to be 2.634 billion liters. This suggests that the total number of both exotic and hybrid female cattle produced through the crossbreeding work for many decades in the country is quite insignificant indicating unsuccessful crossbreeding work. This again suggests that Ethiopia needs to work hard on improving the work of productive and reproductive performance improvements of cattle through appropriate breeding and related activities [1].
In spite of the presence of large and diverse animal genetic resources, the productivity (i.e., meat and milk) of livestock remains low in many developing countries including Ethiopia for various reasons such as inadequate nutrition, poor genetic potential, inadequate animal health services, and other management related problems [2].Cattle breeding are mostly uncontrolled in Ethiopia making genetic improvement difficult and an appropriate bull selection criterion have not yet been established, applied and controlled [3].
Although, artificial insemination, the most commonly used and valuable biotechnology, [4]. has been in operation in Ethiopia for over 30 years, the efficiency and impact of the operation has not been well-documented [5]. Reproductive problems related to crossbreed dairy cows under farmers’ conditions are immense [6]. It is widely believed that the AI service in the country has not been successful to improve reproductive performance of dairy industry [7]. The problem is more aggravated by wrong selection and management of AI bulls along with poor motivations and skills of inseminators [8].
A successful breeding program requires an effective and sustainable method of transferring genetic materials from one population to another. This can be performed through either natural service (NS) or reproductive technologies including artificial insemination (AI), embryo transfer, invitro maturation and fertilization and cloning. However, AI is the most practical reproductive technology to be used in developing countries [1]. Therefore, the objective of this paper is to review the available literatures and provide integrated information on history of AI, advantages and disadvantages of AI, recruitment of semen producing bulls, Semen collection and assessment of ejaculates, and application of AI of cattle
Artificial Insemination of Cattle in Ethiopia
Cattle production in Ethiopia
Ethiopia has an estimated cattle population of about 41.5 million heads. Around 99.45 are indigenous breeds with very few hybrids, 0.5%, and exotic 0.1%. Cattle production together with the production of other livestock sectors has been known to be an important component of the agricultural sector. Livestock contributes much by providing meat, milk, cheese, butter, export commodities (live animals, hides and skins), draught power, manure, near-cash capital stock [9]. It is known that not enough selection and improvement for productivity has been performed on the indigenous cattle. Nevertheless, the indigenous cattle are known to have special merit of coping with the harsh environments of the country. On the other hand, the high performing exotic cattle cannot cope with the harsh environments of the country. Therefore, improvement on the indigenous cattle for productivity without losing traits, which are essential for survival, has been proposed [10].
Artificial insemination
Artificial insemination (AI) has been defined as a process by which sperm is collected from the male, processed, stored, and artificially introduced into the female reproductive tract for the purpose of conception [4]. Semen is collected from the bull, deep-frozen and stored in a container with Liquid Nitrogen at a temperature of minus 196 degrees Centigrade and made for use. Artificial insemination has become one of the most important techniques ever devised for the genetic improvement of farm animals. It has been widely used for breeding dairy cattle as the most valuable management practice available to the cattle producer and has made bulls of high genetic merit available to all [11].
In livestock rearing, the producer makes efficient use of the generous supply of sperm available from an individual male in a manner that greatly increases genetic progress, as well as improving reproductive efficiency in many situations. Today, many bulls have been reported to produce sufficient semen to provide enough sperm for 40,000 breeding units in one year. Using the long-accepted standard of 10 x 106 motile sperm at the time of insemination with an average initial motility of 60% and a 33.3% loss of sperm during freezing and thawing, the number of breeding units would entail 1 x 1012 total sperm.
By using sexual stimulation and more frequent collections, many sperm have been obtained from most bulls in a year without adversely affecting conception rate [11]. The use of AI in Ethiopia is growing but estrus detection is difficult owing to poorly expressed estrus of Zebu breeds. The short duration and low intensity of estrus signs in Ethiopian Zebu cattle caused most estrus detection failures which indicate a need for the use of current advances in AI such as estrus synchronization [12].
History of Artificial Insemination: The first successful AI was performed in Italy in 1780 and over 100 years later, in 1890, it was used for horse breeding [13]. In Russia, however, the method was first taken up seriously as a means of improving farm animals [14]. According to the history of AI is interesting in that old Arabian documents dated around 1322 A.D [4]. indicate that an Arab chieftain wanted to mate his prize mare to an outstanding stallion owned by an enemy. He introduced a wand of cotton into the mare’s reproductive tract, and then used it to sexually excite the stallion causing him to ejaculate.
The semen was introduced into the mare resulting in conception. Spallanzani has been recognized as the inventor of AI. His scientific reports of 1780 have indicated successful use of AI in dogs. In 1899, Ivanoff of Russia pioneered AI research in horses, cattle and sheep, and was apparently the first to successfully inseminate cattle artificially. Mass breeding of cows via AI was first accomplished in Russia where 19,800 cows were bred in 1931 [2]. Denmark was the first European country to establish an AI cooperative association in of New Jersey visited the AI facilities in Denmark and established the first United States AI cooperative in 1938 at the New Jersey State College of Agriculture.
The first artificial vagina (AV) was reportedly devised by G. Amantea, which was used to collect semen from the dog [15]. In the years that followed, numerous Russian researchers developed artificial vagina for the bull, stallion, and ram. The method of semen collection using artificial vagina has been reported to be closest to the natural conditions and is assumed to yield the most normal ejaculate of all methods used. An attempt has been made to simulate the normal or best temperature, pressure, lubrication, and position to obtain the optimum response of the male. The AV consists of an outer rigid or semi rigid support with an inner jacket containing controlled-temperature water and pressure and collecting funnel and container.
In Ethiopia, AI was introduced in 1938 in Asmara, then part of Ethiopia, which was interrupted due to the Second World War and restarted in 1952 [16]. It was again discontinued due to unaffordable expenses of importing semen, liquid nitrogen and other related inputs requirement. In 1967, an independent service was started in Arsi Region, Chilalo Awraja under the Swedish International Development Agency (SIDA). [17]. has described that the technology of AI for cattle has been introduced at the farm level in the country over 35 years ago as a tool for genetic improvement. The efficiency of the service in the country, however, has remained at a very low level due to infrastructure, managerial, and financial constraints and also due to poor heat detection, improper timing of insemination and embryonic death.
In Ethiopia, there is often complaint of the AI service, by service users for imbalance female and male ratios of calves born in which the latter exceeds in percentage, which is against the interests of most of the beneficiaries. Breeding using AI or natural mating affected male: female calf ratio, which gives sense and can be applicable if the system works. However, the reason why natural mating gave more female progenies than males for cows mating to AI is not clearly known.
Advantages and disadvantages of artificial insemination: The worldwide scale and importance of the artificial insemination industry in cattle breeding are beyond question [18]. Maximum use of superior sires has been considered as the greatest advantage of AI while natural service has been linked to limit the use of one bull, probably, to less than 100 mating per year [4]. The author further showed that AI usage enabled one dairy sire to provide semen for more than 60,000 services in one year has listed many advantages of AI including prevention of reproductive diseases, control of inbreeding, minimizing the cost of keeping bulls for natural service and others [19]. Besides, the availability of accurate breeding records such as breeding dates, pregnancy rates, inter-estrus intervals, and days to first service used to monitor fertility are other advantages of AI [7].
Artificial insemination, however, has disadvantages that include poor conception rates due to poor heat detection and inefficiency of AI technicians, dissemination of reproductive diseases and poor fertility rates if AI centers are not equipped with appropriate inputs & are not well managed. Other disadvantages include high cost of production (collection and processing), storage and transport of semen as well as budget and administrative problems and inefficiency of AITs
Recruitment of semen producing bulls
The selection criteria of bulls for AI service must include record-based pedigree information, individual performance as regularly recorded starting from the time of birth, which should include birth weight, subsequent weight increments. Later on, and general health status should also be parts of the selection criteria [20]. Recruitment of bull Calves for the purpose of semen production must be free from a known contagious disease. Bulls selected for AI have been shown to transmit to their offspring the genetic potential for well-above-average milk or meat production. In addition, the progeny must be of desirable conformation, be long wearing, have quiet disposition, and be free of genetic defects. Genetic improvement of cattle using AI calls for a continual replacement of the lower-production-transmitting bulls by younger, proven bulls with superior genetic merit [21].
Bull health control: Disease prevention in bulls has been considered as essential as in breeding females and new bulls need to be screened by a qualified veterinarian for infectious agents prior to entering a new herd. Bulls have been recommended to be purchased only from reputable seed stock producers with adequate herd health plans; including vaccination against infectious diseases, e.g. leptospirosis and campylobacteriosis. Bulls are also recommended to be tested annually for brucellosis, but not be vaccinated for brucellosis. In some instances, bulls need to be vaccinated for bovine viral diarrhea (BVD), infectious bovine rhinotracheitis (IBR), and trichomoniasis [22]. Unless it is made possible to make full control of the health of bulls selected for semen production, the disadvantages of artificial insemination in disseminating diseases will be much higher [20].
The frequency of tests made, and the diseases tested at NAIC are not sufficient [23]. According to the international animal health code (2001) of the Office International des Epizooties (OIE)), donor and teaser animals should be tested for the following specific diseases: Bovine Brucellosis, Bovine Tuberculosis, Bovine Viral Diarrhea, Infectious Bovine Rhinotracheitis, Campylobacter fetus/subspecies veneralis, Trichomonas fetus. Nevertheless, semen-producing bulls at NAIC are tested only for brucellosis and tuberculosis and yet not on regular basis due to many associated constraints [23].
Semen collection and assessment of ejaculates
Semen collection has been considered like harvesting any other farm crop since effective harvest of semen involves obtaining the maximum number of sperms of highest possible quality in each ejaculate to make maximum use of sires. This involves proper semen collection procedures used on males that are sexually stimulated and prepared. The initial quality of semen has been determined by the male and cannot be improved even with superior handling and processing methods. However, semen quality can be lowered by improper collection and the processing techniques [11]. Realization of the maximum benefits of AI depends upon the collection of maximal numbers of viable sperm cells at frequent intervals from genetically superior males. The success of AI depends on the collection of a relatively large numbers of potentially fertile spermatozoa from genetically superior sires [24].
Facilities needed for semen collection: The routine collection of semen for AI in dairy and beef bulls is by using artificial vagina. Several essential features have been considered in designing facilities for collecting semen, of which the safety of the handler and the collector have been found to be the most important in bulls in dairy farm. Safety fences usually constructed of 7.6 cm. steel pipe with spaces large enough for a person to step through at 2.44 meters intervals should be provided. The collection area must provide good footing to prevent slipping and injury to the male being collected. An earthen floor in the immediate collection area best provides this. Means to restrain the teaser animals to minimize lateral as well as forward movement must be provided. At the same time, easy access for semen collection must be maintained [11].
Appropriate and specialized facilities, equipment’s, and procedures have been used during collection of semen to prevent injury to the bulls and their handlers, to maximize the physiological responsiveness of the bulls in producing semen and to enhance the quantity and the quality of the semen that can be collected. The area for semen collection has been preferred clean, relatively quiet free of distractions and any other stressful procedures. There has been a report of increase in spermatozoa motility by 50% through proper sexual stimulation of the bulls [24].
Procedure for collection of semen from the bull: Standard semen collection procedures normally include sexual stimulation and sexual preparation [21].
a) Sexual stimulation: Providing a stimulus situation that elicits mounting behavior in the bull is termed “Sexual Stimulation” .The stimulation process has been best practiced by exposing the bull to a mount animal in a collection environment and allowing to move briefly around female/ teaser for a couple of minutes [21].
b) Sexual preparation: This has been found to determine the intentional prolongation of sexual stimulation. It is achieved through a series of false mounts (allowing the bull to mount but not ejaculate) and restraint and ultimately results in an increase in the quantity and quality of sperm ejaculated. In dairy bulls, one false mount plus two minutes of restraint plus two additional false mounts before each ejaculation will help obtain the maximum amount of good quality semen [25].
c) Methods of semen collection: Semen has been collected in a number of ways, and the methods of collection are governed by the intended purpose for future use. A sample for evaluation may need to be only a very small volume and not as clean a sample as one for use in artificial insemination. The following various methods have been used in collection of semen [26].
Recovery: Follows normal copulation and can be applied in different ways. A pipette such as an inseminating catheter with an attached suction bulb may be inserted into the vagina following ejaculation and the semen is, then, siphoned into it. This semen is contaminated with the fluids of the female tract but is satisfactory for evaluation. It may also be used for artificial insemination when trying to overcome some obstruction in the cervix or satisfy breeding restrictions of some pure-bred societies. This method can be applied using different mechanisms and includes spooning, using a sponge, using a cup, and blotting [26].
a) Massage: Semen has been collected from the bull, in most instances, by massage. The bull is restrained, and the gloved arm and hand are lubricated before inserting through the anus into the rectum. The area of the ampulae, vesicular glands, and prostate is located under the rectum. The fingertips then are used to exert a downward pressure milking this area caudally. This stimulates and mechanically causes the sperm to be passed through the urethra by gravity to drip from the prepuce [26].
b) Vaginal insert: Consists of a tapered insert with a flange on the end that may be placed in the vagina prior to copulation [11].
c) The electro ejaculation method of semen collection: Has been derived from observations of persons being electrocuted that ejaculated in response to the electrical stimulus. The semen collected by electro ejaculation is equal in quality to that collected by the artificial vagina, and processing, storage, and later use are comparable. The method of electro ejaculation for semen collection is preferred to the artificial vagina method under certain conditions. It has been used for dairy bulls that have become crippled, have low sexual activity due to age, or for other reasons are unable to serve the artificial vagina. However, semen should not be collected and used from males that have not demonstrated normal sexual behavior or ability to ejaculate, as the cause may be genetic and transmitted to the offspring [11].
Assessment of ejaculate: Monitoring of qualitative semen characteristics has been indicated to be an important function of the AI Laboratory. Seasonal and even daily fluctuations in a bull’s seminal characteristics are possible. Therefore, to maintain a quality AI program constant vigilance is required. An integral part of this monitoring is an accurate system for keeping records of the bull’s seminal quality. Such records document the bull’s history of seminal quality and provide information on which to base production related decisions [25].
a) Physical appearance: The gross appearance of freshly collected bull semen has been described usually to be the first measure of quality made by the semen laboratory. Neat (unaltered) semen normally appears as a thick whitish to slightly yellowish fluid whose consistency is mainly determined by the number of spermatozoa it contains. Normal bull semen has very little odor [25]. The microscopic appearance of bull’s semen varies between ejaculates, individual bulls, breed, and age. Normal bull semen is generally white or yellowish creamy in color
b) Volume: The volume of the ejaculate is readily measured by collecting the sample directly into a graduated vial [24]. Alternatively, it can be done by weighing the tubes after semen collection on top-loading balance, and later converting the reading into milliliter by using a computer program. The latter has been known to reduce error associated with visual reading of the tube specially when small volume or bubbles are found by 10% [27]. The volume has been reported to decline when young bulls are used or when there is frequent ejaculation or incomplete or failure of ejaculation and in bilateral seminal vesiculities [28].
Furthermore, those authors have described in summary that a number of factors like season of the year, method of collection, and the sexual preparation of the bull have been known to affect semen volume. The volume of bull’s semen varies between ejaculates, individual bulls, breed, and age. However, a bull with less than 2ml of semen per ejaculate is not acceptable [29]. Semen volume for Bostaurus bulls in Brazil was reported to be 6.9ml and 8.2ml in different years [30]. Crossbred bulls had higher values of semen volume while Friesian bulls had better values in the rest of the parameters and age had significant effect only on semen volume [7]. Differences between reports on semen volume could be attributed to differences in age, breed, nutritional status, geographic locations and seasons of year of study, method of semen collection and handling of bulls during collection, procedure and frequency of collection [31].
c) Spermatozoa motility: Motility of spermatozoa has been defined as the percentage of sperm cells that are motile under their own power and progressive motility of spermatozoa has been defined as those spermatozoa that are moving or progressing from one point to another in a more or less straight line [27].Spermatozoa are driven by a propulsive apparatus, the flagellum, which is equipped with contractile proteins strategically arranged in longitudinal organelles, the coarse fibers, and with associated sub filaments, and micro tubes, which provide the propulsive force necessary to overcome internal structural resistance and external viscous drag of extra cellular fluids [28].
Motility of spermatozoa at time of collection has been used commonly as a measure of the fertilizing ability of the sperm [26].However, spermatozoa have been found to lose their fertilizing capacity before they lose motility, which puts motility estimation to be not necessary indicative of fertilizing capacity of the sperm [28]. In general, however, a definite correlation has been found between concentration, morphology, and motility of spermatozoa and the proportion of the total number of actively motile normal spermatozoa in the ejaculate has been found to show levels of fertility of the bull [26].
The individual sperm motility is evaluated by taking small drops of semen onto a slide with cover slip under high magnification (200X). Sperm cells moving in a straight-line forward direction are considered in the motility measure. In order to be acceptable bull semen should have at least 70% and 40% motility respectively at the time of collection and after freezing [29].
d) Live-dead sperm evaluation (vital staining): The percentage of live sperm has been determined by means of a differential vital stain. The measure of the live-dead sperm ratio may be useful in conjunction with the motility examination for a more complete analysis. A certain percentage of dead sperm may not be apparent in initial microscopic motility examinations, since these inactive sperm might be moved about merely by action of the live motile sperm. In addition, a proportion of sperm estimated to be motile may be weak and show only slow oscillatory movements. Differential live-dead staining may help reveal these differences, thus supplementing initial motility estimations and providing more conclusive results [21].
e) Sperm morphology: The normal morphology of spermatozoa is composed of a head and a tail that is divided into a mid-piece, main-piece, and end-piece [11].Films for microscopic examination under the oil immersion lens are made immediately after the motility estimation, but the examination can be made, subsequently, in the laboratory [32]. To obviate temperature shock and the assumption of spurious morphological defects, a drop of semen is mixed with two drops of Indian ink previously raised to body temperature on a warm slide. The drops are mixed and spread like a blood film. Between 200 and 300 sperms are examined and classified according to their shape and appearance. Fertile bulls show about 90 percent of the morphologically normal sperms.
The following morphological abnormalities can be investigated. These include: tailless sperms and sperms with looped tail, the commonest sperm abnormalities which are detachment of the sperm head and bending of the middle piece and tail around and over the sperm head (looped tails), sperms with coiled tails (this abnormality is of two types: the coil involves the extremity of the tail, or the coil, which includes the whole of the tail & sometimes the middle piece) immature or unripe sperms (these are characterized by the presence of a droplet of protoplasm at the junction of the sperm head with the middle piece at the so-called neck), abnormalities of the sperm head and cytogenic disturbances, and other defective sperms [11].
f) Overall assessments: Evaluations routinely conducted by the AI laboratory that have been used to determine whether the semen that is collected and processed for use could be used for practical purpose are screening tests for quality and number of spermatozoa in order to eliminate any substandard ejaculates. This initial screening also avoids wasting expensive supplies, antibiotics, semen extenders, etc., because substandard samples are not processed [21].
Semen that passes initial screening have been further extended, cooled, packaged into straws, and frozen. After freezing, a representative sample is normally thawed and evaluated using various laboratory tests. These post-thaw evaluations not only reflect the ability of the semen to withstand the processing conditions (process quality control) but also can give some indication of the potential fertility of the semen (fertility prediction). Assessing the progressive motility of the semen sample is probably the most common evaluation made for post-thaw viability [21].
Application of artificial insemination
Estrus and estrus detection: Estrus has been defined as a period when the female shows characteristic sexual behavior in the presence of a mature male, such as immobility, raising the hind quarters or arching the back, pricking of the ears-features that are collectively termed lordosis in small laboratory animals; mounting and riding behavior between females is also common (Where AI or hand mating is being used, estrus detection is the most important limiting factor [19]. Insufficient and/or inaccurate estrus detection leads to delayed insemination. Since the fertile life of eggs in most species is relatively short and sperm may require capacitation before they are capable of fertilizing ova, insemination should precede ovulation. Ovulation is difficult to determine routinely, so inseminations are usually related to the time of onset of estrus. Estrus in the cow is characterized by the psychic manifestation of heat. The cow may bawl frequently, is usually restless, may attempt to mount other animals, and will stand to be mounted/standing heat [21].
Timing of insemination: In the cow, maximum fertility has been achieved if inseminated from mid estrus to the end of estrus. Fertilization of the ovum has been reported to occur in the oviduct at the junction of the isthmus and ampulla. The life span of the ovum is around 12 – 18 hours and its viability decrease with time. About 8 hours after service sufficient spermatozoa have reached the isthmus of the oviduct. For fertilization to take place, capacitation of the spermatozoa is required. Capacitated sperm cells show a hyper motility and have undergone the acrosome reaction. The life span of spermatozoa is limited. If insemination takes place too early, the sperm cells will die before fertilization of the ovum can occur. Conversely, when insemination is over delayed, the ovum has lost its capacity to be fertilized [33].
Factors affecting success of artificial insemination: The site of semen deposition has been an important factor in the success of AI in cattle. In addition, the deposition of semen in the uterine body resulted in a 10% higher non-return rate than did cervical deposition. An increase in the conception rate has been reported when semen was deposited in the uterine horns rather than the uterine body [34]. In contrast, no difference was found in the fertilization rate, conception rate or non-return in uterine body and uterine horn inseminations [35].
The major factors that determine AI efficiency are heat detection skills, fertility level of the herd, semen quality, and efficiency of inseminators. Similarly, a successful insemination requires the acquisition of quality semen from a bull, the detection of estrus in the female, and the ability to properly place the semen in the reproductive tract of the female [36]. Detection of estrus has been known to be one of the most difficult tasks for successful AI activities, which in turn is affected by diseases of testis, epididymis, and accessory glands in the male [37]. and diseases of the female reproductive tract [26].
The success of AI depends upon various factors such as the efficiency, capacity and commitment of AI centers in procedurally and ethically producing, processing, handling and distributing semen; the commitments and efficiencies of AITs; presence of appropriate breeding policy along with proper control of indiscriminate crossbreeding; proper heat detections by farmers and other factors [19].
Artificial insemination and fertility rates: Fertility is measured by calving rate to first service for artificially inseminated dairy cattle [38]. Conception rate at first breeding provides a useful estimate of the conception rate for a herd. However, it is a measurement that combines the effects of semen quality, fertility of the cow, timing of insemination, semen handling and insemination techniques, as well as factors such as high environmental temperature and stress [39].
In USA, conception rate of virgin heifers has been found relatively constant at approximately 65% to first service conception; whereas the first service conception rates for lactating cows has decreased approximately 33% from 60 to 40 % [40]. Number of services per conception as an indicator of reproductive efficiency has been defined as the number of services required for a successful conception [41, 42]. The number of services per conception is directly related to the conception rate in the herd. Female fertility, male fertility, environmental factors, and techniques used in AI are the four general multitude factors that determine the ultimate outcome of conception per insemination.
Female fertility refers to any factor directly related to the heifer/cow that may alter her probability of becoming pregnant, including condition of the reproductive tract, nutritional status, changes in body condition from calving to insemination, age, and breed. The mean first service conception rate for Virginia Dairy Herd Institute herds over the past 12 months in USA has been found 40 ± 13% [40]. There is a great reduction in fertility during the summer for lactating cows than for non-lactating heifers. High milk yield intensifies the effects of heat stress on conception and is related to increased metabolic rates and reduced thermoregulatory ability for cows with high milk yield.
Techniques used in AI include accuracy of heat detection, timing of insemination, semen handling, and placement in the reproductive tract. Fertility in cattle is affected by environmental, genetic, disease, and management factors. These influence the reproductive process at ovulation, fertilization, or implantation during gestation and parturition [12].
In Ethiopia, several factors have been reported to influence the number of services per conception. Breeding taking place during the dry season required more services per conception than the short and long rainy seasons [41]. Management factors such as accuracy of estrus detection, timing of insemination, insemination technique, semen quality, skill of pregnancy diagnosis have been reported to affect number of services per conception [42]. Higher number of services per conception might also result from repeat breeding due to infectious and/or noninfectious diseases [43]. In postpartum cows, the mean number of services per conception as 2.4 and 2.7 for sub clinical endometritis positive cows, fourth and eighth weeks postpartum, respectively as compared to 1.7 for sub clinical endometritis negative cows showing that sub clinical endometritis has a significant effect on number of services per conception [44].
Go to
Conclusion and Recommendations
AI service in Ethiopia has been given little or no emphasis at the federal, regional or wereda levels during the last years though it is an important and the most widely practiced animal biotechnology all over the world. Hence, it can generally be concluded that the AI service in Ethiopia is on the verge of total collapse unless urgent corrective measures are taken. The most important constraints associated with AI in Ethiopia include loss of structural linkage between AI Center and service giving units, absence of collaboration and regular communication between NAIC and stakeholders, lack of breeding policy and herd recording system, inadequate resource in terms of inputs and facilities, Based on the above conclusions the following points are recommended:
1. Selection of bulls for AI should strictly follow the standard guidelines and procedures set for the purpose and also the national livestock development policies of the country
2. Establishment of a functional breeding policy and strategy should be given at most priority and each stakeholder and professional should work hard towards its implementation;
3. Import semen of the desired quality for the immediate use in accordance with the rules and regulations for the import of genetic materials to be followed by creating reliable source of semen producing bulls through reestablishing the Milk recording Scheme of the center in a more strengthened status;
4. The AI service provision should be restructured in such a way that it responds well to the breed improvement programs of the country. It should be well organized with clearly defined duties and responsibilities of stakeholders.
To Know More About Please Click on: Journal of Reproductive Medicine
https://juniperpublishers.com/gjorm/index.php
To Know More About Open Access Publishers Please Click on: Juniper Publishers
#GJORM#peer review journals#reproductive medicine#global journal of reprodutive medicine#Juniper Publishers PubMed Indexed Articles
0 notes
Text
The Long-Term Progression Free Survival After the Combination of Radiotherapy with Concurrent Chemotherapy of Nimotuzumab And Temozolomide Followed Adjuvant Temozolomide In Recurrent Anaplastic Astrocytoma
Authored by: Xiaoqi Xie*
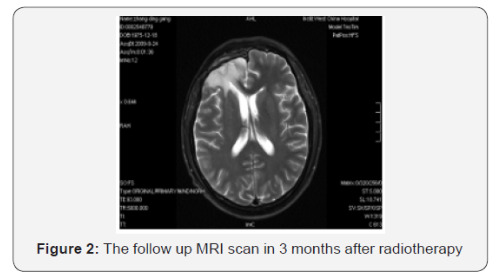
Introduction
Gliomas which originated from glial cells and made up 80% of all primary CNS tumors in the United States were classified as “low grade” (WHO grades I and II) and “high grade” (WHO grades III and IV) according to histopathologic changes [1,2]. High-grade gliomas (HGGs) are related with poor prognosis and consist of anaplastic gliomas (anaplastic astrocytoma, anaplastic oligodendroglioma and anaplastic oligoastrocytoma; WHO grade III) and glioblastomas (GBMs; WHO grade IV). The current standard therapy for newly diagnosed GBMs involves maximal safe resection followed by radiotherapy (RT) with concomitant and adjuvant temozolomide (TMZ) [3-5]. Despite optimal therapy, the median time-to-tumor progression (mTTP) for patients with newly diagnosed GBMs is approximately 6.9 months and these tumors unavoidably relapse with a median overall survival (mOS) of only 15 months [3]. However, the treatment of anaplastic gliomas is abroad controversial topics in neuro-oncology. By above therapy, anaplastic gliomas achieves a mTTP of about 1.2 to 2.6 years and a mOS of 2 to 7 years [4,6,7].
Compared with anaplastic oligodendroglioma, treatment of the anaplastic astrocytoma has been less optimistic. This tumor is more resistant to therapy and patients have a shorter mOS of only 2 to 3 years. In the United States, most oncologists treat anaplastic astrocytoma patients with maximal safe resection followed by field radiotherapy with concurrent and adjuvant chemotherapy (temozolomide), same to the regimen now deemed as the standard of care for GBMs [3]. Moreover, all HGGs nearly recur and survival following disease progression is doomed to be approximately 6 months for GBMs and 10 months for anaplastic gliomas [8,9]. Treatment options for recurrent HGGs include re-resection, chemotherapy, or re-irradiation. But, the optimal treatment strategies for recurrent HGGs are still unknown and the randomized control trials which contrast active intervention and determine standard therapy are absent. We herein report the case of a recurrent anaplastic astrocytoma patient with the long-term progression free survival (PFS) after the combination of radiation therapy with concurrent chemotherapy of nimotuzumab and temozolomide followed adjuvant temozolomide.
Case Report
We present the unique case of a 33-year-old gentleman who initially presented with a several days history of headaches behind the right brain, with associated “vomiting”. There were no complaints of numbness, weakness, or any visual changes. Physical examination of the patient revealed that he had a depressed superficial reflex in the right limbs and positive pyramidal tract signs. A MRI scan at that time revealed a large, irregularly enhancing mass in the right frontal lobe that was associated with marked edema, bleeding and mass effect. These symptoms relieved with the treatment of dehydration to reduce intracranial pressure. Following the consultation with a neurosurgeon and discussing the probability of a brain tumor and therapeutic regimen, the patient experienced a right frontal lobe Lobectomy in local hospital in October 2008. The final pathology was anaplastic astrocytoma (WHO grade III).
The patient recovered well from surgery, and his headaches were resolved. Adjuvant treatment options were explained to him and included radiotherapy plus concomitant and adjuvant Temozolomide. But the patient refused further therapy. In April 2009, a follow-up CT scan revealed local recurrence in the operative bed (Figures 1-3). And the patient was treated in West China Hospital. The pathology department in West China Hospital held a pathological consultation with tumor section in local hospital and diagnosed anaplastic astrocytoma (WHO grade III) containing a few of oligodendroglioma ingredients with histopathologic changes of partial necrosis, mitotic activity and endothelial cell proliferation (Figure 4). KRAS mutation was detected in codon 12 and codon 13 and the DNA repair enzyme O6-methylguanine- DNA methyltransferase (MGMT) promoter methylation was positive. Chromosomal 1p and 19q co-deletion was detected by FISH (Figures 5&6). Isocitrate dehydrogenase 1 mutation (codon 132) was detected by PCR and Sanger sequencing and Isocitrate dehydrogenase 2 (codon 172) was wild type (Figures 7&8).
Starting on May 22, 2009, the patient underwent whole brain radiotherapy to a dose of 4000 cGy and local lesion radiotherapy to a dose of 6000 cGy (fractionated focal irradiation in daily fractions of 2 Gy given 5 days per week for 6 weeks) with concurrent combined chemotherapy of intravenous nimotuzumab (100 mg every 1 weeks) and oral temozolomide (75 mg per square meter of body-surface area per day) for 6 weeks followed by six cycles of adjuvant temozolomide (150 mg per square meter for 5 days during each 28-day cycle). Treatment was generally well tolerated, and the adverse events were nausea, vomiting and hematologic toxicities, which all of them were classified as mild. Following his radiotherapy and chemotherapy, he was followed clinically as well as with surveillance MRI scans at regular intervals. The follow-up MRI scan in 3 months after radiotherapy were as follows (Figure 2). The latest MRI scan revealed no recurrence in May 31, 2016 (Figure 3). Until now, the patient is still alive with a long-term progression free survival lasting seven years. And the survival following the initial diagnosis is up to eight years.
Discussion
A high rate of local recurrences has been observed after multi-disciplinary therapy in high-grade gliomas (HGGs) patients.10 Important variables predicting longer survival include oligodendroglial cell line, extent of resection, and younger age (<50 years) [11]. Moreover, gliomas with the DNA repair enzyme O-6-methylguanine-DNA methyltransferase (MGMT) promoter methylation, chromosomal 1p and 19q co-deletion or isocitrate dehydrogenase 1 and 2 (IDH1/2) mutations is associated with a better prognosis [12-15]. In this patient, the chromosomal 1p and 19q co-deletion was detected by FISH; and the MGMT promoter methylation was positive and Isocitrate dehydrogenase 1 was mutation type, which was one of the reason of long-term progression free survival (PFS). PFS is associated with overall survival (OS) and has become a marker for evaluating the efficacy of treatments in recurrent HGGs patients. The 6-month PFS (PFS6) for recurrent GBM ranges from 9 to 21% [8,9,16], while PFS6 for anaplastic gliomas have ranged from 37 to 48% [17,18]. In our report, the patient still does not progress with a long-term PFS lasting seven years. Although the prognosis of recurrence HGGs patients is invariably poor, it is vital just as this case to improve the quality of life and prolong survival by multimodal therapy.
Therapy options for recurrent HGGs are limited and may include surgery, re-irradiation, chemotherapy and targeted therapies. For recurrent HGGs patients which were subjected to clinical deterioration on account of mass effect, surgery might be one of option. But, until now, no prospective researches demonstrate that re-surgery can improve the survival for recurrent HGGs patients. Moreover, due to the application of targeted therapies, a fewer proportion of recurrent HGGs patients are going through diagnostic or therapeutic re-surgery.
For HGGs patients, primary therapy most involves adjuvant radiotherapy with the maximum tolerated dose. The dose limitation of healthy brain tissue and the short duration between initial radiation therapy and recurrence confined the use of reirradiation therapy for recurrent HGGs with conventional external beam radiotherapy, which may have an influence on patient’s quality of life. However, Romanelli et al’ s research that evaluated the efficacy of stereotactic radiosurgery (SRS) in recurrent glioma have indicated median OS from 7.5 to 30 months after treatment [19]. And in Mahajan’s research [20], recurrent GBM patients treated with SRS achieved a longer median OS compared with untreated patients [20]. Hypofractionated stereotactic irradiation might be another choice for recurrent glioma. According to Fogh, et al. [21] research, the median OS after re-irradiation with a hypofractionated protocol (3.5 Gy per fraction up to a median dose of 35 Gy) over a 2-week period was 11 months. In this case, because patient did not receive any further treatment after surgery, conventional external beam radiotherapy (whole brain radiotherapy to a dose of 4000 cGy and local lesion radiotherapy to a dose of 6000 cGy) plus concomitant and adjuvant Temozolomide were recommended to him and the progression free survival after irradiation was seven years.
The efficacy of chemotherapy in recurrent HGGs was limited. And many chemotherapeutic agents, including single agents and combination chemotherapy agents, have been used to treat recurrent HGGs [22,23]. Temozolomide, PCV and bevacizumab are some of the treatment choice according to several researches [24-27]. Temozolomide was evaluated in recurrent HGGs before becoming the first line chemotherapy for glioma. The recurrent anaplastic glioma patients that were treated with single-agent TMZ showed a 35% response rate and PFS6 of 46% [28]. Bevacizumab has been authorized by FDA as the treatment of recurrent GBMs [29]. Moreover, Nimotuzumab is a humanized monoclonal antibody which binds the extracellular domain of epidermal growth factor receptor (EGFR) and blocks EGFR signal pathway activation [30]. And the efficacy of nimotuzumab in HGGs is depended on the combination of nimotuzumab with radiochemotherapy or radiotherapy. Solomon et al. [31] research has illustrated the median survival time of the combination of nimotuzumab with radiotherapy was 12.4 months or 27.0 months for patients with GBM or anaplastic astrocytoma patients. In our case, the chemotherapy agents were the concurrent combined chemotherapy of intravenous nimotuzumab and oral temozolomide for 6 weeks followed by six cycles of adjuvant temozolomide. And the efficacy was surprising. Thus, nimotuzumab might be one of the chemotherapy choice and more randomized clinical trials need to be done to clarify the efficacy of nimotuzumab.
Conclusion
This is the first reported case to our knowledge of a patient with recurrent anaplastic astrocytoma who achieved PFS lasting seven years following treatment with the combination of radiation therapy with temozolomide and nimotuzumab. The patient tolerated the therapy well and do not relapse again until now. This case highlights the unique biology of individual glioma and that the combination of radiation with chemotherapy and targeted therapy in the recurrent setting can have a significantly influence on overall survival for specific patients. We will continue doing research in this area, especially in the molecular characteristics of individual tumors. Individualized treatment according to each unique patient’s situation will improve survival as well as quality of life.
#peer review journals#Juniper Publsihers#reproductive health#open access publishers#GJORM in juniper publishers
0 notes
Text
Facility Readiness Assessment for Implementationof Adolescent and Youth Health Care Service in Central Zone, Southern Ethiopia
Authored by: Achamyelesh Gebretsadik*

Background
Adolescents and youth comprise one-third of the world’s population [1], whom 90% live in developing countries [1]. Overall the proportion of adolescent and youth expected to rise from 20% to 50% within the coming thirty years [2]. Ethiopia is a young country with 71 % of the populations are under the age of thirty and 10-24 years were 33.8 % [3,4]. Investing in young people (ages 10 to 29) now will lay the groundwork for future. Adolescent and youth is a critical age for risk taking and critical period for professional intervention [5,6]. Intervention in this time help adolescent and youth to make appropriate decision for the future live and can prevent risk behaviors which can also affect their adulthood health. Adolescent and youth need different approach than adult in service provision. Currently adolescent and youth are not getting the expected services worldwide [6,7].
Mortality rate of adolescent and youth are rising due to several health problems. Especially road traffic accident is the first contributor for mortality. Non communicable diseases and mental illness also another contributor for morbidity and mortality of adolescent and youth [7]. Globally a number of initiatives have been taken place over the last decades to provide adolescent and youth responsive health care [8,9]. However, most of the initiatives were focusing only on sexual and reproductive health issues [10-12].
Similarly, in Ethiopia though it was not in an integrated and comprehensive manner there were a lot of straggles to address adolescent and youth health since 2000 [13-16]. However, with all the efforts made the intended improvement not achieved in the health of adolescents and youth due to health system was not responsive and young people not utilized the service. Therefore, federal ministry of health revised the previous strategy and launched a new strategy that comprise comprehensive adolescent and youth health care and to make the health system responsive for that comprehensive approach [17]. Therefore, the aim of this study was to assess facility readiness for the implementation of comprehensive adolescent and youth health care.
Methods
Study settings
The Southern Nations Nationalities and Peoples’ Regional State is the third largest administrative region of Ethiopia and represents about 20% of the country’s population with close to 20 million people. The central zones of Wolita and Hadiya zones and Halaba special district contributes more than 20% of the regions population. Wolaita zone has five hospitals, 69 health centers, 372 health posts and 98 private clinics. Hadiya zone has one general hospital, 4 primary hospitals 61 health centers and 305 health posts. In Halaba there are 7 health centers and 50 health posts.
Study area and period: This readiness assessment was conducted in 14 health centers of the central zones of Southern Nation Nationalities People Region health facilities from May 14- 26, 2017.
Study design: A cross-sectional study was conducted in two central zones namely Wolaita and Hadiya and one special district (Halaba).
Sampling criteria: The zones and special district were selected purposively. Since these two zones and districts have high population density and their proximity to the head quarter of the region might be a true representative of the general health facility of the region. From Wolaita zone, six health centers were selected from five districts (namely, Offa, Damot Pulasa, Damot Gale, Bodity and Sodo). And from Hadiya zone, three districts and six health facilities and from Halaba special district one from started and one from not started were selected based on their youth friendly service delivery status among started and non-started 1:1 ratio. The health centers were selected using lottery methods (Table 1).
Study population: Health care providers (nurse and health officers), health center managers and district health office heads of the selected health facility.
Data collection and sources: Data were collected from 7-19 May 2017. Five reproductive health professional data collectors/ technical assistant were hired and trained to collect the data. Data were collected through interview and observation using questionnaires and observation check list prepared to assess national adolescent and youth health service quality by Federal Ministry of Health (FMOH). Interview were done among health providers (nurse and health officers) those working in youth friendly service room from started health centers and maternal and child health nurses from non-started health centers and health center managers and district health office heads. The collected data were entered in to Microsoft Excel 2010 software and descriptive analysis was made using percentage.
Classification criteria: Readiness of the facility was assessed based on the standard set by World Health Organization for adolescent and youth health [18]. When the facilities fulfilled>=75% of the standards we considered ready for that element i.e. staff, basic amenities etc. Support letter was also taken from RHB maternal and child health and nutrition core process office to the two zones and Halaba special district and district health office heads also communicated officially to get consent from each health centers.
Result
Staffing
During the survey, 14 health facilities, their managers, one health care provider from each and 5 district health office heads were interviewed. Of all 6 (42.8%) of health facilities have at least five health officers, 9 (64.2%) have more than ten diploma nurses, 7 (50%) have diploma midwifery at least four and 6 (42.8%) have no bachelor nurse and midwifery (Table 1). Staff numbers and their orientation to the right and confidential delivery of service is important for provision of quality adolescent and youth friendly services. In this survey 12 (86%) of the health facility managers have no training for quality improvement in adolescent and youth health care and supportive supervision. All youth friendly service started health facilities have 2-3 trained health persons. Among non YFS started health facilities only one had training. During the survey time except one health center with YFS, they were closed due to community mobilization for community based health insurance, while other units are operating their routine activities. In all YFS available health centers service for adolescent and youth were in working hours.
Basic amenities
All started health centers have clearly visible signboard that mentions operating hours of the facility. Among all 13(92.8%) have functional toilet but, only 1/14(7.1%) have functioning hand washing facilities after toilet, 3/14(21.4%) of toilets were clean, 4/14(28.5%) had disposal bin in the toilet. About 11/14(80%) of health facilities do not have adequate and comfortable seating in their waiting area. Almost all health facilities are clean and well coming however; only 2/7(28.5%) health facilities have a clean and well coming separate waiting room and 5/7(75%) were working in a room where windows and doors have no curtains. 3/7(42.8%) have no screen to separate consultation area from the examination to maintain privacy during consultation. There is pipe water in the entire health centers compound but no drinking water facilities in waiting area. Nine out of fourteen (64.2%) has permanent electric supply during working hours. All the facilities have general waste disposal system in the health center. Communication equipment (phone or shortwave radio) found in 5/14 (35.7% %) of the health facilities.
Adequacy of furniture
Seven out of fourteen (50 %) of the health centers have adequate, whereas 5/14 (36%) need repair of their furniture and 2/14 (14 %) of the health facilities do not have furniture while having separate room prepared for YSFs (Figure 1). Computer is available in7/14 (50%) of health facilities and no internet access was observed in all health facilities.
Equipment supply
Equipment/material/supplies are available in all health facilities: Blood pressure measurement machine, binaural adult stethoscope, monaural fetal stethoscope, clinical thermometer, an adult weighing scales, latex gloves, single-use standard disposable or auto-disposable syringes, pregnancy test strips and haemoglobinometer. Materials inadequately supplied /found in surveyed health facilities: Measuring tape, Light source, for example a torch, height meter, soap or alcohol-based hand rubs for hand hygiene body mass index growth charts for adolescents, test strips for urine with 10 parameters, ophthalmoscope set and otoscope set were not found in any of the health centers.
Essential medicine supplies
Condoms, oral contraceptive pills, emergency contraceptive pills, injectable contraceptives, contraceptive implants, intravenous fluids, paracetamol, amoxicillin, Ceftriaxone, ciprofloxacin, cotrimoxazole suspension, diclofenac, omeprazole, diazepam and vaccines found in all health centers uniformly. Only 8/14 (59%) of health centers have magnesium sulfate. Atenolol, Salbutamol, Glibenclamide not available in all health centers, which are important for the treatment of diabetes mellitus, hypertension and asthma respectively.
Infection prevention
All health facilities have sharps/box/container and a general waste disposal incinerator in the compound. Nine out of fourteen (64.3%) have safe storage and disposal of clinical waste and potentially infectious waste that requires special disposal i.e. disposal of equipment that may have in contact with body fluids and safe storage and disposal of sharps. However, 5 (35.7%) have adequate hand hygiene facilities that are located in or adjacent to the office/examination room.
Adolescent participation
In health facilities where services are started 4/7 (57%) health care providers involved the adolescents in the planning, monitoring, evaluation and in any aspects of health service provision for adolescents. But the vulnerable groups of adolescents are not participating.
Overall facilities readiness
All health facilities were fulfilled criterion for the essential medical supply,11 for laboratory services ,9 for infection prevention ,5 for basic equipment’s and 6 for basic amenities (Table 2).
Discussion
Readiness assessment survey was conducted for the implementation of the national adolescent and youth friendly health care strategies in SNNPR. Out of nine standards, four of them were seen in this survey, which are important for the readiness assessment, this includes: facility characteristics, data and quality improvement, adolescents’ participation and intersect oral collaboration. This study showed majorities (86%) of manager lack to get training of adolescent and youth friendly services (AYFS). According to current Ethiopia AYHS, advocate for district managers to guarantee their ownership and support for implementation the designed strategy [17]. The health workers in YFS not started health facilities were deficient in training which is one of the tools for readiness assessment. This finding is in line with study in Uganda in which all staff including the managers lack training. For the implementation of comprehensive AYH all type of health worker received the basic knowledge and skill in preservice training, but at least one person needs to have a training on AYH and can provide orientation for others to overcome the staff shortage and turnover.
Facility characteristics: this is the third standard as this is a readiness assessment study it focusses on the input aspect of the standard: among the elements of the standard availability of essential medicines were acceptable >= 75% in all surveyed facilities. This finding is in line with study conducted in Sudan [19], and higher than Northern Rwanda in which up to 73% of health facilities faced a challenge of medium to high levels of stock outs and slightly higher than study done in South west Ethiopia, which one third of the health facilities are below the standard [20,21]. This variation may be explained that the drugs were used to assess the readiness in this study may varies in types.
To provide quality and standard health care it is important to fulfill the necessary equipment and availability of basic equipment. Only 35.7% fulfilled the standard equipment needed for AYHS. Among the listed infection prevention precautions 64.9% and 78.5% of HFs fulfilled laboratory service required for AYFHS respectively [22]. This also in line with study done in 10 developing countries [23]. One of the significances of health information management system is to make evidence-based decision at all level. We could not find age and sex disaggregated data in all non-started health facilities. This might be due to the national HMIS format not captured age and sex of adolescent and youth. In the revised HIMS format the above problem might be solved. Adolescent participation in planning, monitoring and evaluation of health services and in decisions regarding their own care, as well as in certain appropriate aspects of service provision is considered as very crucial according to the current AYHS [17]. However, in this study only 4/7 health facilities delivering youth friendly service were participated adolescent and youth in planning, monitoring, evaluation and in any aspects of health services provision. This is low according to the standard and study done in Uganda. Possible explanation for this low result may be currently the program was not running very well [22,24].
On the other hand, they were not participated in decision making none of them are member of facility governing board. Possible explanation for this might be the program is not implemented properly as the standard. This may be improved when the program is implemented throughout the health facilities in the region. In assigning health workers less priority was given for AYH rooms. In addition, the working hours were not convenient for adolescents most adolescents prefer out of working hours for YFS.
Conclusion
With available resources it is possible to implement AYHS in central zones of SNNPR. Lack of training for facility managers and health care providers, Essential medicines supply were in satisfactory manner. There were shortages of essential equipment, no intersectoral collaboration and also non-governmental partners working to support this program. Less attention was given for noncommunicable disease for adolescent and youth. Job description for each profession were not including about adolescent and youth health. Therefore, training of trainers at zone level, training of managers, providers at zone and district level is very important. Health facilities should include adolescents in facility governing board. Facility-level registers and health management information systems (HMIS) need to include client information about age, sex, presenting problem, diagnosis and services provided for adolescent and youth. Communication and collaboration with the community, different governmental and non-governmental organizations are very mandatory.
Declarations
Funding
The study not supported by any funding organization.
Availability of data and materials
The datasets generated and/or analyzed during the current study available from the corresponding author on reasonable request.
Authors’ contributions
AG: Supervised the data collection, coded the data, carried out the analysis, and wrote the of the article. NM &YS: Contributed design of the study and analysis, comments throughout the entire process. All authors approved the final version of the manuscript prior to submission
Ethics approval and consent to participate
The study was approved by the Southern Nation Nationalities People Regional health bureau Ethics Committee, and verbal consent was also taken from each respondent for participation.
Disclosure of interests
I declare that we have no competing interests.
Acknowledgements
We greatly acknowledge Southern Nation Nationalities People Regional Health Bureau of Medicine and Health Sciences support letter and financial support for this research. I would like to thank study participants and data collectors as well.
0 notes
Text
Laparoscopic Reversal of Tubal Ligation – A Minimally Invasive Option for Restoring Natural Fertility
Authored by: Samantha Yeo

Case Description
We present the case of 34-year-old multiparous woman who underwent reversal of tubal ligation and subsequently delivered a livebirth from a spontaneous conception. Our patient was a 34 year-old woman who was recently remarried and trying to conceive. Her obstetric history included four term normal vaginal deliveries from her previous partner, and two early miscarriages. After her last delivery four years ago, she underwent postpartum sterilization. This was performed with tubal occlusion using non absorbable titanium and silicon rubber clips (Filschie® clips) via a minilaparotomy (Figures 1) [1].
A secondary subfertility evaluation revealed good ovarian reserve and ovulatory cycles, with satisfactory semen parameters. Counseling was directed towards the options of reversal of tubal ligation and IVF. After understanding the various success and complication rates, she requested surgical reversal of tubal ligation as she was keen on spontaneous conception (Figure 2).
She underwent laparoscopic reversal of tubal ligation and tubal re-anastomosis under general anaesthesia. Routine laparoscopic Veress entry was achieved and the status of her tubes was evaluated. Both Filschie® clips were removed with careful dissection. Methylene blue was use to identify the proximal and distal tubal lumens via hydrotubation and tubal cannulation.
Bilateral tubal reanastomosis was performed with microsurgical equipment via 3mm laparoscopic ports. Vasopressin was infiltrated into the mesosalpinx and precise electrocoagulation was used to aid haemostasis. Two Polyproprylene® sutures were placed at the muscularis layers of both ends of each tube, at the 6 and 12 o’clock positions, and apposition of the proximal and distal lumens was achieved in a tension free fashion. Tubal patency was confirmed intra-operatively via hydrotubation (Figure 3) [2].
She was discharged uneventfully on the first post-operative day and conceived spontaneously during her next menstrual cycle. Her first dating ultrasound was performed at eight weeks of gestation, and she delivered at full term via a normal vaginal delivery without antenatal complications (Figures 4).
Conclusion
Based on our experience, reversal of tubal ligation has comparable subsequent intrauterine pregnancy rates to IVF treatment. Laparoscopic microsurgery offers the advantage of faster recovery with less postoperative discomfort, less complications and a smaller surgical scar. Tubal re-anastomosis also restores natural fertility, offering an alternative to artificial reproductive technology. Appropriate patient selection and counseling, together with operator training and experience contributes to favourable outcomes. More high quality studies should be encouraged to establish the objective comparative success rates in this developing surgical field.
To Know More About Please Click on: Journal of Reproductive Medicine
https://juniperpublishers.com/gjorm/index.php
To Know More About Open Access Publishers Please Click on: Juniper Publishers
#open access journals#Juniper publishers#GJORM in juniper publishers#reproductive medicine#juniper publisher
1 note
·
View note
Text
Metformin Reduces the Extent of Varicocele-Induced Damage in Testicular Tissue
Authored by: Erkan Erdem*
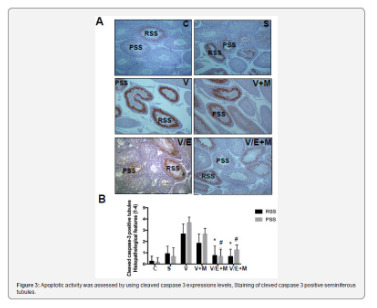
Introduction
Varicocele is an abnormal vascular dilatation of pampiniform plexus, commonly developing at puberty. Although underlying mechanisms remain poorly understood genetic background, anatomical aberrations, incompetence of venous valves, difference between the drainage of left and right testicular veins were suggested in the etiology [1]. As left spermatic vein being longer than the right vein, it is more commonly incurred to increased hydrostatic pressure and dilatation. Compression of the left renal vein between the aorta and the superior mesenteric artery may also contribute to the disturbed intravenous pressure [2].
The prevalence of varicocele varies between 15-20 % in general population and 30-40% in infertile men, and 11-19% of adolescents [3-6]. It was reported that varicocele is a progressive disease and early diagnosis and treatment in youth may enhance fertility potential [7]. Several contributing factors in the pathophysiology of varicocele have been proposed such as higher temperature of testis, the disorder of neuroendocrine system, autoimmunity, accumulation of renal and adrenal metabolites, genetic and epigenetic factors, hypoxia and oxidative stress [8-10].
Varicocele represents a chronic process within the testicle, which is linked to increased reactive oxygen species (ROS) beyond physiologic limits and, subsequently, disrupting sperm membrane fluidity, causing DNA damage and necrosis [11]. Moreover, superoxide dismutase 1, glutathione S-transferase M1 and T1 which are counteracting free superoxide radicals in cells have been reported to be decreased in men with varicocele, that may be important on disturbed sperm parameters [12]. Apoptosis of germ cells was also demonstrated in the pathogenesis of varicocele-related infertility [13]. Clinical findings suggest that surgical repair of varicocele may decrease seminal oxidative stress levels and sperm DNA fragmentation and, thus, may improve sperm quality [14]. Therefore, surgical intervention seems to be a reliable option in the treatment of varicocele-related male infertility, although some controversial reports exist.
Additionally, anti-oxidant medications such as kallikrein, L-carnitine with L-acetyl carnitine, pentoxifylline, coenzyme Q10 have been used to improve the milieu in the testis in men with varicocele [15]. Metformin is a major therapeutic agent in the treatment of type 2 diabetes mellitus as an insulin sensitizer, which decreases hepatic glucose output and increases peripheral glucose uptake. Although its action was not fully elucidated, metformin attenuated intracellular reactive oxygen species and apoptosis in aortic endothelial cells, myocardium, renal tubular cells and testicular cells [16-20].
Aim
Potential effects of metformin on varicocele-induced testicular damage have not been studied in neither humans nor in animal models. Thus, we investigated the impact of metformin on spermatogenesis, testicular integrity, and apoptotic activity in the testis of adolescent rats with experimentally-induced varicocele.
Materials and Methods
Thirty-six male adolescent Wistar rats (6-week-old) were randomly and equally divided into six experimental groups. Surgical procedures were carried out under anesthesia with intraperitoneal injection of ketamine (50 mg/kg). The experimental groups were as follows:
• (C) Control group; no surgical procedure was performed, and testis was examined after removal.
• (S) Sham group, a midline incision was performed, and testis was examined 8 weeks later.
• (V) Varicocele - only group: Experimental varicocele was induced by partial ligation of left renal vein with
Silk suture at the area medial to the insertion of the adrenal and spermatic vein into renal vein as described previously [21].
• (V+M) Varicocele + metformin group: All rats were treated with metformin (300 mg/kg per day by oral gavages) for 8 weeks following induced varicocele.
• (V/E) Varicocele + varicocelectomy group: Varicocelectomy was performed 4 weeks and the examination of the testis 8 weeks after the induction of varicocele. No medication was used.
• (V/E+M) Varicocele + varicocelectomy + metformin group: Varicocelectomy was performed 4 weeks after the induced varicocele. Metformin treatment (300 mg/kg per day by oral gavages) was initiated after the induction of varicocele and continued for 8 weeks. Left testes were examined 8 weeks after the induction of varicocele in all varicocele - induced groups. As maximum apoptotic activity initiates approximately 28 days after the induction of varicocele the procedure of varicocelectomy was performed 4 weeks after the formation of varicocele [22].
Histologic preparation and evaluation
The testicular tissue was fixed in Bouin’s solution (75% picric acid, 5% glacial acetic acid, and 25% formaldehyde) and embedded in paraffin blocks. Sections (5 μm) were formed, deparaffinized, and stained with hematoxylin and eosin. Spermatogenesis was examined in each group using Johnsen’s score (a score of 1-10 was assigned to each tubule regarding epithelial maturation) as described previously [23]. Sections were examined in a random order under a standard light microscope with 10x and 40x magnification by a blinded histologist; unaware of which group each rat belonged to. Histological grading was done by examining approximately 80 randomly selected seminiferous tubules per rat. Thus, a total of approximately 480 seminiferous tubules were scored for each group.
Histomorphometry analysis
A total of 103 randomly selected seminiferous tubules stained with hematoxylin-eosin were analyzed in each group. The presence of round spermatid stage (RSS) and primary spermatocyte stages (PSS) were assessed as described previously and compared among the groups [24].
Immunohistochemical staining for cleaved caspase-3 and ImageJ analysis
Cleaved caspase-3 was used for immunohistochemical staining. Testicular tissue samples were immediately fixed in 10% neutral-buffered formalin, embedded in paraffin, and sectioned (5 μm). Sections were deparaffinized and blocked for endogenous peroxidase activity with methanol containing 3% H2O2 for 10 m. Ultra V Block (Lab vision, Freemont, CA) for 7 m at room temperature. Cleaved Caspase-3 (#9664, Cell Signaling, U.S.) was applied at a dilution of 1: 500 and incubated overnight at +4 °C in a humidified chamber for nonspecific binding. The sections were washed in phosphate-buffered saline (PBS) and incubated with biotinylated horse anti-rabbit IgG (3 mg/mL; Vector, Burlingame, CA) at a 1: 500 dilution for 1 h at room temperature.
Antibodies were detected using a VECTASTAIN avidinbiotin complex (Vector PK 4000) for 30 m at room temperature. Antibody complexes were visualized after incubation with 3,3’-diaminobenzidine tetrahydrochloride (DAB, Bio-Genex, San Ramon, CA.) and were mounted under glass coverslips in Entellan (Merck) and then evaluated under a light microscope. Immunohistochemical staining for cleaved caspase-3 was analyzed by counting 100 seminiferous tubule cross-sections in each group and expressed as the apoptotic index. In each photomicrograph, the following parameter was measured with ImageJ software: expression levels of cleaved-caspase-3 in both groups at round spermatid stage (RSS) of testes. Each of this parameter was measured 3 times for each image and the average of the 9 measurements of each sample was used for the statistical analysis. Histopathological features examined in rats with normal testis and with sham, varicocele, varicocele+ metformin in a subjective scoring (0 - not present; 1 - low grade; 2 - moderate grade; 3 - high grade; 4 - very high grade).
Statistical analysis
Histopathological findings (Johnsen’s score) were assessed by nonparametric Kruskal-Wallis test, and the mean Johnsen’s score was used in the comparison of the groups. Multiple comparisons were made using Tukey’s procedure. p<0.05 was considered statistically significant. Analysis of variance was used for statistical analysis of the apoptotic index among the groups.
Results
Assessment of spermatogenesis
Johnsen’s score was significantly lower in V group (4.14±1.25) compared to C group (9.1±0.3) or S group (9.0 ± 0.2) groups (p<0.05). V+M group had significantly higher score (6.9±0.6) than V group (p<0.05). V/E group and V/E+M group had similar Johnsen scores (8.9 ± 1.02 and 9.2 ± 0.6). These findings suggest that the administration of metformin resulted in 40.6% of improvement in spermatogenesis in rats with varicocele. However, this favorable effect was not observed when metformin was used along with varicocelectomy.
Histological and morphological changes in seminiferous tubules
Histological and morphological changes in the testes of rats were compared via hematoxylin and eosin staining and degenerated tubules (DT) were only detected in V and V+ M groups, not in C, S, V/E and V/E+M groups (Figure 1). Visual assessment of the disorganized seminiferous tubules further supported these findings as seen in Figure 2. Seminiferous tubule degeneration scores were used for quantification of data (Figure 2b). V group had significantly higher scores of RSS and PSS compared to C and S group (2.6±0.8 and 3.7±0.4; 0.2±0.4 and 0.2±0.4; 0.9±0.6 and 0.6±0.7, respectively) (p<0.05). V/E group had significantly lower RSS (0.7±0.8) and PSS (0.8±0.7) scores than V group (p<0.05). V+M group had significantly lower RSS and PSS scores (1.8±0.7 and 2.6±0.7, p<0.05) in comparison to V group, implicating beneficial effects of metformin in rats with varicocele. When compared to V/E group, V/E+M group did not exhibit any difference in RSS (0.6±0.6) and PSS (1.4±0.5) scores, suggesting the absence of additive positive effect of metformin in varicocelectomies rats.
Apoptotic activity
Apoptotic activity was assessed by using cleaved caspase 3 expressions levels, staining of cleved caspase 3 positive seminiferous tubules were shown in Figure 3a. Cleaved caspase 3 expressions were significantly higher in V group (3.5 ± 0.5) compared to C (0) and S (0.2 ± 0.4) groups. V+M group had significantly lower cleaved caspase 3 level (3.0 ± 0.7) than V group. V/E group had lower cleaved caspase-3 expression levels (1.0 ± 0.7) compared to V group. Treatment of varicoceleectomy rats with metformin (V/E+M) did not further reduce apoptotic activity in the seminiferous tubules (1.75 ± 0.43) when compared to the varicocelectomy group (V/E) (Figure 3b).
Discussion and Conclusion
The present study demonstrates that metformin can reduce the extent of testicular damage in rats with varicocele, although having no effect in rats following varicocelectomy Spermatogenesis, seminiferous tubule integrity and the degree of apoptosis were improved using metformin in the presence of varicocele although it was not as remarkable as what was obtained through varicocelectomy. A review of the literature revealed that the impact of metformin on varicocele was not investigated in humans or animal models until now.
Although it is a commonly identified abnormality not all men with varicocele present with infertility. Some intrinsic factors may render some men to become susceptible to varicocele, thus, the best candidates who benefit from varicocelectomy yet to be clarified. Since oxidative stress was shown to be important in the pathophysiology of varicocele some agents have been used to improve the milieu in the testis [1]. A number of anti-oxidant medications have been studied to relieve detrimental effects of varicocele in the testis [25]. These agents have been used either alone or as an adjuvant therapy with surgery. However, surgery remains the treatment of choice and there exists insufficient data to recommend medical therapy in men with varicocele. Barekat et al. [26] reported that administration of an antioxidant agent N-acetyl cysytein as an adjunct therapy improved semen quality following varicocelectomy [26]. Tek et al. [21] demonstrated that vascular endothelial growth factor decreased apoptosis in varicoceleinduced rats as evidenced by diminished caspase-3 positive cells [21]. Both studies showed the benefit of these as adjunct therapy following varicocelectomy. However, in the present study metformin did not enhance the effect of varicocelectomy.
Minutoli et al. [13] demonstrated that neuronal apoptosis inhibin factor and surviving expressions were significantly reduced following varicocele induction and polydeoxyribonucleotide, an agonist of adenosine A2A receptor, administration restored testicular function [13]. Several other studies detected increased germ cell apoptosis in rats with varicocele [21,22,27]. However, in another study, apoptosis was found to be decreased in germ cells in the testes of infertile men with varicocele as compared with normal men [28]. It was speculated that the fixation of testis in formaldehyde might have played a role in the different result. In the present study, cleaved caspase 3 expression was used to assess apoptotic activity and it was found that metformin reduced apoptotic activity in rats with varicocele, whereas no additional effect was observed when metformin was administered after varicocelectomy.
Metformin is commonly used in type 2 diabetes mellitus and polycystic ovarian disease as an insulin sensitizer [29]. Also, it is present in various tissues including myocardium, liver, pancreas, thyroid, adipose tissue, hypothalamus, pituitary, and male and female gonads [19,30,31]. It has been reported that metformin is mainly transported into cells by organic cation transporters as passive diffusion is limited [32]. Although the mechanism of action is not yet fully elucidated recent studies suggested that metformin acts through AMP-activated protein kinase (AMPK) pathway, inhibits the activity of the respiratory electron transport chain in mitochondria, induces epigenetic modifications which in part may explain long term effects and decreases oxidative stress and apoptotic activity [16,19, 33-35].
Male reproductive system utilizes all these metabolic pathways and is prone to be affected by metformin administration [20,36,37]. Metformin was found to stimulate lactate production which is important in the development of germ cells and show an anti-apoptotic effect in rat Sertoli cells [38]. It was also reported that metformin reduced the apoptotic cells and caspase-3 level in rat testis [20]. The findings of the present study are consistent with previous studies that metformin reduced apoptosis in testis with varicocele. Yan et al. [37] reported that metformin improved the semen parameters related to its effects on weight loss, increased testicular weight and reduced testicular cell apoptosis [37]. On the other hand, Tartarin et al. [36] reported metformin at concentration 10 times higher than therapeutic levels decreased testosterone secretion and the number of Sertoli cells in rats when it was administered during pregnancy [36]. Faure et al. [39] reduction in testicular weight and testosterone level were observed in 6-week-old chickens treated with metformin for 3 weeks [39].
Several groups demonstrated that post-operative administration of metformin can exert protective effects in male reproductive function in rat models [40]. Bosman et al. [41] demonstrated that infertile hyperinsulinaemic men could benefit from metformin treatment in combination with an enriched antioxidant diet [41]. Besides, metformin was reported to act as a protective compound when used in the media for cryopreservation of spermatozoa [30]. In conclusion, metformin reduces detrimental effects of varicocele, although no additional benefit is expected following varicocelectomy. Further studies are required to apply metformin for this indication in humans.
#open access journals#peer review journals#Juniper Publishers PubMed Indexed Articles#reproductive medicine#GJORM in juniper publishers
1 note
·
View note
Text
Potential Estrogenic Effects of Biofield Energy Treatment Using Human Endometrial Adenocarcinoma Cell Line
Authored by: Alice Branton*
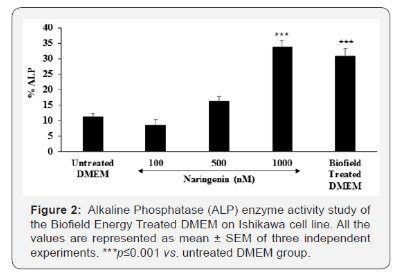
Introduction
Ishikawa cell line is a well‐differentiated human endometrial adenocarcinoma cell line, which was established to study the estrogenic potential due to the presence of estrogen and progesterone receptors (i.e., ERα and PR) [1]. Ishikawa cell line is derived from human endometrium that plays a significant role as a fertility-determining factor [2,3]. Hence, Ishikawa cell line was selected as a test system for this study. Continues basic research area in this field using this cell line like reproductive biology and molecular science, reported its vital role to compare its action using various parameters such as alkaline phosphate (ALP), a zinc-containing metalloenzymes. Human endometrial cell lines are the best characterized cell lines that are easy to cultivate for estrogenic potential. ALP is more abundant in liver, bone, and a small amount in placenta, which were denoted as ALP-1, ALP-2, and ALP-3, respectively.
Maintained the level of ALP is very important for conception as it significantly regulates the estrogen level and endometrium growth [4-6]. Various menstrual disorders take place in the presence of low level of ALP during implantation and conception. A decreased ALP level may be due to zinc deficiency, hypothyroidism, vitamin C deficiency, folic acid deficiency, excess vitamin D intake, low phosphorus levels, celiac disease, malnutrition with low protein assimilation, insufficient parathyroid gland function, pernicious anemia, vitamin B6 insufficiency, and also with the frequent use of synthetic contraceptive, which Results and Discussion in the loss of endocrine functions via estrogen receptor (ER) [7]. Thus, for identification of estrogenic potential, Ishikawa cell line was selected as a test system for this study in order to find the effect of the Biofield Energy Treated DMEM media for ALP as a biomarker.
As an alternative way of treatment, Complementary and Alternative Medicine (CAM) therapies are emerging as one of the best and safe way to treat against acute and chronic diseases [8]. Among CAM, Biofield Energy Healing Treatment (The Trivedi Effect®) one of the best approach that has provided a scientific groundwork in the past years by many renowned healers in order to understand the complex homeodynamic regulation of living systems [9]. National Institute of Health (NIH) and National Center for Complementary and Alternative Medicine (NCCAM) recommend and included various Energy Healing therapies such as natural products, deep breathing, yoga, Tai Chi, Qi Gong, chiropractic/osteopathic manipulation, meditation, massage, special diets, homeopathy, progressive relaxation, guided imagery, acupressure, acupuncture, relaxation techniques, hypnotherapy, healing touch, movement therapy, pilates, rolfing structural integration, mindfulness, Ayurvedic medicine, traditional Chinese herbs and medicines, naturopathy, essential oils, aromatherapy, Reiki, cranial sacral therapy and applied prayer under CAM category that has been accepted by the most of the U.S. population with several advantages [10].
The Trivedi Effect®- Consciousness Energy Healing Treatment contains a putative bioenergy, which is channeled by a renowned practitioner from a distance. Biofield Energy Healing as a CAM showed a significant result in biological studies [11]. The Trivedi Effect®- Consciousness Energy Healing Treatment has been reported with significant revolution in the physicochemical properties of metals, chemicals, ceramics and polymers [12-14], improved agricultural crop yield, productivity, and quality [15,16], transformed antimicrobial characteristics [17-19], biotechnology [20,21], improved bioavailability [22-24], skin health [25,26], nutraceuticals [27,28], cancer research [29,30], bone health [31- 33], human health and wellness.
In pursue with the outstanding Results and Discussion of Biofield Energy Healing Treatment outcome, authors in this study evaluates the impact of the Biofield Energy Treatment (The Trivedi Effect®) on DMEM as a test sample for estrogenic potential with respect to ALP parameter using standard in vitro assay in Ishikawa cells.
Materials & Methods
Chemicals and reagents
Naringenin was purchased from Sigma, India. Fetal bovine serum (FBS) and Dulbecco’s Modified Eagle’s Medium (DMEM) were purchased from Life Technology, USA. Antibiotics solution (penicillin-streptomycin) was procured from HiMedia, India, while 3-(4, 5-dimethyl-2-thiazolyl)-2, 5-diphenyl-2H-tetrazolium) (MTT), Direct Red 80, and ethylenediaminetetraacetic acid (EDTA) were purchased from Sigma, USA. All the other chemicals used in this experiment were analytical grade procured from India.
Cell culture
Ishikawa cell line (human endometrial adenocarcinoma) from human endometrial tissue was used as test system in the present study. Ishikawa cell line was maintained in DMEM growth medium for routine culture supplemented with 10% FBS. Growth conditions were maintained at 37 °C, 5% CO2, and 95% humidity and subcultured by trypsinisation followed by splitting the cell suspension into fresh flasks and supplementing with fresh cell growth medium. Before the start of the experiment, the growth medium of near-confluent cells was replaced with fresh phenolfree DMEM, supplemented with 10% charcoal-dextran stripped FBS (CD-FBS) and 1% penicillin-streptomycin for 3 days [34].
Experimental design
The experimental groups consisted of group 1 (G-I) the untreated DMEM. Group 2 (G-II) consisted of positive control at non-cytotoxic concentrations. Further, group 3 (G-III) included the Biofield Treated DMEM.
Consciousness energy healing treatment strategies
DMEM as the test item was divided into two parts, one part was treated with the Biofield Energy by a renowned Biofield Energy Healer (The Trivedi Effect®) and coded as the Biofield Energy Treated DMEM group, and the other part did not receive any sort of treatment and denoted as the untreated DMEM group. This Biofield Energy Healing Treatment was provided by Alice Branton remotely for ~5 minutes through the Healer’s unique Energy Transmission process to the test sample under laboratory conditions. Biofield Energy Healer was located in the USA, while the test items were located in the research laboratory of Dabur Research Foundation, New Delhi, India. Biofield Energy healer in this study never visited the laboratory in person, nor had any contact with the test item (DMEM medium). Further, the control group was treated with “sham” healer for comparative purposes. The “sham” healer did not have any knowledge about the Biofield Energy Treatment. After that, the Biofield Energy Treated and untreated samples were kept in similar sealed conditions for experimental study.
Identification of non-cytotoxic concentration
The cell viability was performed by MTT assay in human endometrial adenocarcinoma cell line (Ishikawa). The cells were counted and plated in 96-well plates at the density corresponding to 5 X 103 to 10 X 103 cells/well/180μL of cell growth medium. The above cells were incubated overnight under growth conditions and allowed the cell recovery and exponential growth, which were subjected to serum stripping or starvation. The cells were treated with the test items (DMEM) and positive control. The cells in the above plate(s) were incubated for a time point ranging from 24 to 72 hours in a CO2 incubator at 37 °C, 5% CO2, and 95% humidity. Following incubation, the plates were taken out and 20μL of 5mg/mL of MTT solution were added to all the wells followed by additional incubation for 3 hours at 37 °C. The supernatant was aspirated and 150μL of DMSO was added to each well to dissolve formazan crystals. The absorbance of each well was read at 540nm using Synergy HT microplate reader, BioTek, USA [35]. The percentage cytotoxicity at each tested concentrations of the test substance were calculated using the following equation (1):
Where,
X = Absorbance of treated cells;
R = Absorbance of untreated cells
The percentage cell viability corresponding to each treatment was obtained using the following equation (2):
The concentrations exhibiting ≥70% cell viability was considered as non-cytotoxic.
Study of alkaline phosphatase (ALP) activity
The cells were counted and plated in 96-well plates at the density corresponding to 5 X 103 cells/well/180μL phenol-free DMEM+ 10% CD-FBS. The above cells were incubated overnight under growth conditions for 48 hours in a CO2 incubator at 37°C, 5% CO2, and 95% humidity to allow the cell recovery and exponential growth. The above cells were incubated with the test samples or positive control for 6 days. Re-addition of the test sample or positive control was done on day 3. After incubation with the test samples, the ALP enzyme activity was determined by monitoring the hydrolysis of p-nitrophenyl phosphate to p-nitrophenol (pNPP). The cells were washed with 1X PBS and lysed by freeze-thaw method i.e., incubation at -80°C for 20 minutes followed by incubation at 37 °C for 10 minutes. Lysates were prepared in 0.1% triton-X. 50μL of substrate solution i.e., 10mM of pNPP in 1M diethanolamine and 0.24mM magnesium chloride (MgCl2) solution, pH 10.4 was added to all the wells containing 50μL of lysates followed by incubation for 1 hour at 37 °C. The absorbance of the above solution was recorded at 405nm using Synergy HT microplate reader. The percentage increase in ALP enzyme activity with respect to the untreated DMEM group was calculated using equation (3):
Where,
X = Absorbance of cells corresponding to positive control and test group
R = Absorbance of cells corresponding to untreated group
Statistical analysis
All the values were represented as Mean ± SEM (standard error of mean) of three independent experiments. The statistical analysis was performed using SigmaPlot statistical software (v11.0). For two groups comparison student’s t-test was used. For multiple group comparison, one-way analysis of variance (ANOVA) was used followed by post-hoc analysis by Dunnett’s test. Statistically significant values were set at the level of p≤0.05.
Results and Discussion
Cell viability study using MTT
The Biofield Energy Treated and untreated test samples were tested for cell viability using MTT assay in Ishikawa cells. The outcomes in terms of percentage cell viability are represented in Figure 1. The MTT data showed that the test samples were found to have significant cell viability after Biofield Energy Treatment by 98%, while in the naringenin (positive control) group the cell viability was 75% to 96%. Thus, the experimental MTT data suggested that the Biofield Energy Treated DMEM was found to be safe in the Ishikawa cells as compared with the untreated DMEM. Thus, DMEM was used to study the estrogenic potential (i.e., ALP activity) of The Trivedi Effect®- Biofield Energy Healing in vitro using human endometrial adenocarcinoma cell line (Ishikawa).
Alkaline phosphatase (ALP) enzyme activity
The level of ALP in terms of percentage change are presented in Figure 2. Naringenin, positive control showed a significantly increased the value of ALP by 43.75% and 200.89% (p≤0.001) at 500 and 1000nM, respectively with respect to the untreated DMEM group. The Biofield Energy Treated DMEM group showed a significant increased the ALP level by 30.8% as compared with the untreated DMEM group. Thus, the Biofield Energy Treated DMEM showed a significant increment of ALP, which play a major role in estrogen balance for conception. It might be highly significant in case of infertility and helpful against various menstrual disorders.
The scientific literature reported that decreased ALP level in placenta results in serious complications such as amyloidosis, granulation tissue, gastrointestinal inflammation such as inflammatory bowel disease, systemic infections, hypophosphatasia, postmenopausal women receiving estrogen therapy that is due to the osteoporosis, severe anemia, heart surgery, aplastic anemia, malnutrition, magnesium deficiency, hypothyroidism, chronic myelogenous leukemia, children with achondroplasia and cretinism, and pernicious anemia [35]. Thus, Biofield Energy Healing Treatment would significantly improved the estrogenic potential and worked as an index of osteoblastic differentiation as well as improved ALP enzyme activity [36]. Thus, in order to study the effect of Biofield Energy Treatment on DMEM, ALP level was significantly improved in Ishikawa cell line. It might be expected that Biofield Energy Treatment has altered the osteoblastic differentiation, which is due to an increased ALP enzyme level.
Conclusion
The Trivedi Effect®- Consciousness Energy Healing Treatment on DMEM was considered as a significant role to improve estrogenic potential with respect to increased level of ALP in Ishikawa cells. Cell viability data using MTT assay showed a significant improved cell viability after Biofield Energy Healing Treatment with 98% in the test sample group, while upto 96% in the positive control group signifies the high safety profile of the test samples. The level of ALP was significantly increased by 30.8% in the Biofield Energy Treated DMEM group as compared with the untreated DMEM group. Thus, The Trivedi Effect® on DMEM were found to have a significant impact on ALP level, which results in a better estrogenic potential and osteoblastic differentiation.
Therefore, with respect to the untreated DMEM, the Biofield Energy Treated DMEM would be highly significant in growth and viability of Ishikawa cells. Therefore, the Consciousness Energy Healing based DMEM might be a suitable alternative media for cell growth. It can be useful for the management of various estrogenic and menstrual disorders viz. Dysmenorrhea with painful cramps, Premenstrual Syndrome (PMS), Menorrhagia, Oligomenorrhea, Amenorrhea, and Missed periods. Thus, Biofield Energy Treatment would be useful to control the estrogen balance and thus control overall hormonal balance, which can be useful against stress, aging, osteoporosis, various bone diseases, cell differentiation, could improve cell-to-cell communication, normal cell growth, neurotransmission, cell cycling and proliferation, skin health, immune and cardiovascular functions. Besides, it controls various immune-related disease conditions such as Aplastic Anemia, Pernicious Anemia, Hepatitis, Sjogren Syndrome, Myasthenia Gravis, Parkinson’s Disease, Asthma, Atherosclerosis, Graves’ Disease, Dermatomyositis, Dermatitis, Diabetes, Multiple Sclerosis, Ulcerative Colitis, Alzheimer’s Disease, Irritable Bowel Syndrome, Systemic Lupus Erythematosus, stress, etc. with a safe therapeutic index to improve overall health and Quality of Life.
Acknowledgement
Authors are grateful to Dabur Research Foundation, Trivedi Global, Inc., Trivedi Science, Trivedi Testimonials, and Trivedi Master Wellness for their support throughout the work
#open access journals#Juniper Publsihers#reproductive health#peer review journals#GJORM in juniper publishers
0 notes