Don't wanna be here? Send us removal request.
Text
Cord blood banking help for autism

Cord Blood and Autism: A Story of Science and Hope
Hi there! 👋 Today, we’re going to talk about something really cool — cord blood — and how it might help kids who have autism. This is a big topic, so let’s take our time and break it down together. Ready? Let’s go! 🌟 What Is Cord Blood? When a baby is born, there’s a little tube called the umbilical cord that connects the baby to their mom. It helps bring food and oxygen to the baby before it’s born. Inside that cord, there’s special blood called cord blood. Most of the time, after a baby is born, doctors throw the cord away. But now we know that cord blood is super special because it has something called stem cells in it. Think of stem cells like tiny builders. 👷♀️🧱 They can turn into lots of different types of cells — like brain cells, blood cells, or even heart cells. That’s why doctors are really interested in using them to help people who are sick or have problems in their body. 🧩 What Is Autism? Let’s talk about autism now. Autism, or Autism Spectrum Disorder (ASD), is something some kids are born with. It affects how they think, feel, and connect with other people. Some kids with autism: - Don’t talk or talk very little - Have a hard time playing with others - Like to do the same things over and over - Don’t like loud noises or being touched - Have really special talents in things like math or music Every kid with autism is different. It’s kind of like a big rainbow — that’s why it’s called a “spectrum.” We still don’t know exactly why some kids have autism. But doctors and scientists are working really hard to find out.

��� Can Cord Blood Help Kids with Autism? Now here’s the big question: Can cord blood help kids with autism? Some scientists think it might. Since stem cells are really good at helping the body heal and grow, they wondered if they could help the brain too. They thought, “What if we gave a child their own cord blood? Could that help their brain work better or help with autism symptoms?” So they did some tests! 🔬 What Do the Tests Show? Scientists did small studies where they gave kids their own cord blood back through a tube (kind of like when you get medicine through an IV). They watched the kids for a few months to see what happened. Here’s what they found: - The treatment was safe. No kids got sick from the cord blood. - Some kids showed small improvements, like talking more, making better eye contact, or being more calm. But — and this is important — not every kid got better. And the changes were small. So scientists say, “This looks promising, but we need to do more tests to be sure.”

🧠 Clues in the Cord Blood Here’s another amazing thing! Some doctors looked at the cord blood of babies right after they were born — before they even showed signs of autism. And guess what? They found clues in the blood! Babies who later developed autism had a few things in their blood that were different, like: - Special chemicals called fatty acids that were higher than usual - Genes (like RORA) that looked a little different - Signs of something called oxidative stress, which means the cells might be working too hard This doesn’t mean doctors can tell for sure who will have autism, but it means they might be able to spot it earlier and help kids sooner! 🏥 What Is Cord Blood Banking? Some parents choose to save their baby’s cord blood in a special place called a cord blood bank. It’s kind of like a freezer for stem cells! That way, if their child ever needs the blood for a health problem later, it’s already saved and ready to use. Families can choose between: - Private banks (you pay to store the cord blood for your own baby) - Public banks (you donate it so anyone who needs it can use it) Cord blood can help with things like: - Certain types of cancer (like leukemia) - Blood problems (like sickle cell disease) - And maybe, just maybe — autism 🧭 What Happens Next? Scientists are still working hard. There’s a lot more to learn. Here's what they’re doing next: - Testing more kids with autism to see who it helps the most - Watching kids for longer to see if the changes last - Learning which parts of the cord blood are most helpful - Making sure everything is safe and fair for all families And they are very careful — because this is about real kids and real families. They want to get it right!

❤️ Why This Matters If scientists figure out how to use cord blood to help with autism, it could change a lot of lives. It might help kids talk more, understand better, and feel more comfortable in the world around them. That’s why this research is exciting. It gives families hope. Even if we don’t have all the answers yet, every new discovery is a step forward. 📚 The Story So Far Let’s remember what we learned today: - Cord blood is full of powerful stem cells that might help heal the brain - Autism is different for every kid, and we still don’t know what causes it - Scientists are testing if cord blood can help kids with autism, and the first tests are showing some hopeful signs - Some parents save their baby’s cord blood just in case they might need it later - We still need more studies to understand how it works and who it can help 🎉 Final Thoughts Science is like solving a big mystery. 🔍 And right now, scientists are putting together the pieces of how cord blood might help kids with autism. It’s not a magic cure, but it could be something that makes a big difference someday. And who knows? Maybe one day you will be the scientist who solves the puzzle!

Would you like a fun drawing or diagram to help explain cord blood and stem cells even more? Read the full article
0 notes
Text
Est-ce dangeureux de rester pris en hypnose?

Procurez-vous le cours Hypno-Vie maintenant!

Produits
Vous pouvez bénéficier du programme Hypno-Vie© de trois façons:Option A:La première façon, qui s’avère la plus efficace, est de suivre une formation avec un éducateur certifié. Consultez notre section intitulée ‘trouver un éducateur‘ dans notre menu général afin de trouver un éducateur dans votre région.Option B:La seconde façon consiste à vous procurer notre programme complet d’étude à domicile. Cette option peut s’avérer une excellente option si vous devez garder le lit pour une raison médicale. Ce programme d’auto-apprentissage Hypno-Vie© est aussi une bonne alternative si un éducateur n’est pas encore disponible dans votre région.Il est important que vous réalisiez que pour bénéficier des puissants enseignements de ce programme, vous devez le suivre de façon assidue et faire tous les exercices prescrits.

Option C :La troisième option consiste à vous procurer les puissants enregistrements d’auto-hypnose et les écouter. Cette option, quoique plus économique, n’est pas notre recommandation première car vous ne bénéficiez pas d’un aussi bon encadrement qu’avec les options A ou B. Vous allez recevoir en cadeau le cinquième enregistrement lorsque vous achetez les quatre premiers!( une escompte de 20% sera calculée sur votre total donc mettre les 5 enregistrments dans votre panier de commande)SVP NOTEZ QUE MEME SI LES ENREGISTRMENTS SE NOMMENT "LE DISQUE" ILS VOUS SERONT LIVRES SOUS FORMES DE MP3. VEUILLEZ LES TELECHARGER IMMEDIATEMENT CAR LE LIEN EXPIRE RAPIDEMENT
Procurez-vous le cours Hypno-Vie maintenant!

Le MP3 Bleu- Une auto-hypnose puissante Ce premier enregistrement du programme Hypno-Vie© vous aidera à atteindre et maîtriser des niveaux d’hypnose profonds et agréables rapidement. Vous allez être épatés de constater que vous n’avez pas besoin d’un enregistrement ou d’une autre personne pour vous aider à atteindre un état d’hypnose profond et très agréable. En étant ainsi capable de rapidement et facilement aller en hypnose par vos propres moyens, vous allez pouvoir vivre une naissance calme, naturelle et en douceur.

Le MP3 Rose- Parfaite Anesthésie Dans ce deuxième enregistrement du programme Hypno-Vie©, vous allez apprendre les puissantes techniques d’anesthésie induites par l’hypnose. Vous serez ainsi capable de maîtriser les techniques qui vous apporteront ce même degré d’anesthésie complète que l’on utilise lors de chirurgies avec l’hypnose comme seul moyen anesthésiant. Ainsi, en étant aussi confortable, vous serez à même de donner naissance naturellement et doucement.

Le MP3 Jaune- Votre Endroit Parfait Dans ce troisième enregistrement d’autohypnose du programme Hypno-Vie©, vous aurez l’occasion de construire votre endroit parfait. Cet endroit très spécial vous apportera paix, calme et sérénité dès que vous en ressentirez le besoin. En étant ainsi relaxée et heureuse dans votre endroit parfait, votre corps sera libre d’accomplir sa fonction naturelle de donner la vie rapidement. Et ce n’est pas tout! Vous conserverez votre endroit spécial, tel un bonus pour le restant de votre vie. Vous serez ainsi libre de retourner dans votre endroit spécial à chaque fois que vous ressentez le besoin de retrouver le calme et la paix.

Le disque Blanc- La Naissance Dans ce quatrième enregistrement du programme Hypno-Vie©, vous avez l’occasion de pratiquer et vivre votre accouchement idéal. Il est bien connu que l’esprit humain crée ce qu’il conçoit comme une réalité. De cette façon, en vous faisant pratiquer la naissance idéale, celle-ci devient une réalité, votre réalité. Vous allez aussi avoir la chance de construire une bulle protectrice autour de vous et votre petit bébé, ce qui aidera à vivre une naissance calme et naturelle.

Le Disque Or- Bonne Fête! Ce cinquième enregistrement du programme Hypno-Vie© est spécial de plusieurs façons. Premièrement, vous n’avez qu’à débuter l’enregistrement puis à partir en autohypnose rapidement et à écouter le disque autant de fois que vous le désirez. Deuxièmement, il constitue une puissante récapitulation du programme entier. Troisièmement, il est recommandé que vous ne l’écoutiez que lorsque votre travail est débuté car ceci est mon cadeau de naissance pour vous! Vous pouvez aussi vous procurer une grande sélection de puissants produits d’auto-hypnose que j’ai développé afin de vous aider à perdre du poids, cesser de fumer, mieux dormir, surmonter les peurs (telle que la peur de voler en avion), augmenter votre confiance en soi, etc. Maintenant!!!Enregistrements MP3 d’auto-hypnoseLa divine musique que vous entendez en arrière-plan du cinquième enregistrement du programme Hypno-Vie © nommé ‘Bonne Fête!’ s’appelle ‘Ardas’ et est tirée de l’album the Crimson Collection Volume 6 et est utilisée grâce à la généreuse permission de Invincible Recordings © Copyright 1991
Procurez-vous le cours Hypno-Vie maintenant!
Est-ce dangeureux de rester pris en hypnose?
By Nathalie Fiset / June 8, 2024L’hypnose, un état de relaxation profonde et de suggestibilité accrue, est depuis longtemps un sujet de fascination et de scepticisme dans le domaine de la psychologie et de la médecine. Bien que souvent décrite dans la culture populaire comme un outil de contrôle mental ou de divertissement, l’hypnose est également utilisée en milieu clinique à des fins thérapeutiques. Cependant, une question persiste parmi le grand public : est-il dangereux de rester enfermé dans un état d’hypnose ? Cet article vise à explorer les risques potentiels et les considérations de sécurité associés à l’hypnose, mettant en lumière les idées fausses et les réalités de cette pratique. En se plongeant dans la recherche scientifique et les avis d’experts sur le sujet, les lecteurs acquerront une compréhension globale des dangers potentiels de l’hypnose prolongée et de la manière de gérer efficacement ces risques. Que vous soyez une personne curieuse intéressée par le fonctionnement interne de l’esprit ou un professionnel en exercice dans le domaine de la psychologie, cet article vous fournira des informations précieuses sur la sécurité de l’hypnose et les précautions à prendre lors de séances d’hypnose. Plongeons dans le monde fascinant de l’hypnose et découvrons la vérité derrière ses dangers perçus.
Sécurité de l’hypnose
L’hypnose, lorsqu’elle est pratiquée par un professionnel formé et qualifié, peut être une technique thérapeutique sûre, considérée comme non invasive et sans effets secondaires nocifs lorsqu’elle est pratiquée de manière appropriée. La sécurité de l’hypnose réside avant tout dans la compétence et les aptitudes du praticien. Les professionnels procèdent généralement à une évaluation approfondie avant toute séance d’hypnose pour s’assurer que la technique est adaptée et sûre pour l’individu. De plus, le participant a toujours le contrôle pendant le processus et peut choisir de s’arrêter à tout moment, garantissant ainsi sa sécurité et son confort. Dans l’ensemble, lorsqu’elle est administrée de manière responsable, l’hypnose peut offrir une méthode sûre et efficace pour répondre à divers problèmes psychologiques et émotionnels.
On ne peut pas rester pris en hypnose
Il est essentiel de reconnaître qu’il est impossible de rester bloqué en état d’hypnose de manière permanente. L’hypnose est un état naturel de conscience altérée dans lequel l’individu demeure conscient et réceptif aux suggestions, tout en ayant la capacité de revenir à un état de conscience ordinaire à tout moment. Les professionnels qualifiés veillent à guider les participants de manière sécurisée et à les ramener progressivement à un état de conscience normal à la fin de la séance. Il est donc important de comprendre que l’état hypnotique n’est pas un état permanent et que la personne ne peut pas rester bloquée en hypnose.
Preuves qu’on ne peut pas rester pris en hypnose
Il est également crucial de souligner que des études et recherches approfondies dans le domaine de l’hypnose ont démontré de manière concluante qu’il est impossible pour un individu de rester involontairement pris en état hypnotique. Les données scientifiques ont mis en évidence la nature transitoire de l’hypnose et ont montré que même dans des cas extrêmement rares de persistance de l’état hypnotique, un professionnel formé peut facilement guider le participant vers un état de conscience ordinaire. Ces preuves solides soutiennent clairement que l’hypnose n’entraîne pas de risques liés à un “bloquage” permanent, renforçant ainsi la perception de l’hypnose comme une pratique sûre et temporaire.
Ou seraient les gens pris en hypnose? Absurde!
En réponse à la question “Ou seraient les gens pris en hypnose? Absurde!”, il est important de noter que l’hypnose n’est pas une situation où les individus restent captifs de manière permanente. Cette croyance est souvent basée sur des mythes et des représentations erronées de l’hypnose dans les médias populaires. En réalité, l’état hypnotique est un état de conscience modifié et suggestible, où la personne demeure consciente et conserve le contrôle sur ses actions. Les techniques hypnotiques sont conçues pour induire un état de relaxation profonde et de concentration accrue, mais il n’y a aucun danger à rester coincé dans cet état. Au contraire, l’hypnose est généralement considérée comme une pratique sécuritaire et transitoire, guidée par un professionnel qualifié pour assurer une expérience positive et bénéfique pour le sujet.
Votre inconsicent vous protege en hypnose
Dans le contexte de l’hypnose, il est crucial de reconnaître que votre inconscient agit comme un gardien protecteur. Lorsque vous êtes en état hypnotique, votre inconscient est pleinement engagé pour soutenir votre bien-être et votre sécurité. Il agit comme un guide interne qui veille à ce que vous restiez dans un état de confort et d’équilibre pendant la séance. Votre inconscient a la capacité naturelle de filtrer les suggestions qui pourraient vous causer du stress ou de l’inconfort, ce qui garantit que seules les idées bénéfiques et constructives sont intégrées pendant la session d’hypnose. En résumé, votre inconscient joue un rôle essentiel en hypnose en protégeant votre bien-être et en favorisant des transformations positives et durables.
Aucun cas de personne restée prise en hypnose
Il est important de souligner que dans la pratique de l’hypnose, aucun cas vérifié de personne restée prise en état hypnotique n’a été documenté. Les professionnels de l’hypnose ont une compréhension approfondie des mécanismes de l’état hypnotique et sont formés pour guider les individus de manière sûre et éthique tout au long de la séance. Lorsque la séance d’hypnose prend fin, les praticiens sont formés pour faciliter un retour en toute sécurité à un état de conscience ordinaire, permettant à la personne de reprendre le contrôle total de son esprit et de son corps. Ce processus de réveil est soigneusement géré pour garantir le bien-être et le confort du participant, assurant ainsi une expérience positive et enrichissante de l’hypnose.
Pourquoi vous allez toujours émerger d’hypnose
Dans le contexte de l’hypnose, il est essentiel de comprendre que l’émergence de l’état hypnotique est une caractéristique inhérente à la pratique. Les professionnels de l’hypnose guident les individus à travers un processus où ils peuvent expérimenter un état modifié de conscience, mais ce processus est conçu de manière à permettre à chaque participant de revenir naturellement à un état de conscience ordinaire à la fin de la séance. L’émergence de l’hypnose est soigneusement gérée pour assurer que les personnes retrouvent leur pleine conscience, reprenant ainsi le contrôle total de leurs pensées, de leurs actions et de leur environnement. Cet aspect fondamental de l’hypnose garantit que toute expérience de cet état se déroule de manière sûre, contrôlée et respectueuse du bien-être de l’individu impliqué, renforçant ainsi la confiance en la pratique de l’hypnose.
L’hypnose, la transe est un état naturel et sécuritaire
Dans le domaine de l’hypnothérapie, il est crucial de souligner que la transe hypnotique est un état naturel et sans danger. Lorsqu’une personne entre en transe hypnotique sous la guidance d’un praticien qualifié, elle est simplement plongée dans un état de conscience modifiée temporaire, similaire à un état méditatif ou à une immersion profonde dans un livre captivant. Pendant cet état, l’individu reste conscient de son environnement et conserve le contrôle total de ses pensées et de ses actions. La transe hypnotique est un processus doux et sécurisé qui permet à la personne de se connecter avec son subconscient et d’explorer des perspectives et des solutions en profondeur, dans le but d’améliorer son bien-être mental et émotionnel.
Hypnose pour l’accouchement
L’hypnose pour l’accouchement, également connue sous le nom d’hypnonaissance, est une approche qui utilise les techniques de l’hypnose pour aider les femmes à gérer la douleur et les émotions associées au processus de l’accouchement. Cette méthode repose sur l’idée que l’esprit peut influencer la perception de la douleur et favoriser un état de relaxation profonde pendant le travail. Grâce à des séances préparatoires et à des exercices de visualisation, les femmes enceintes apprennent à se détendre, à se focaliser sur des pensées positives et à se sentir plus en contrôle de leur corps pendant l’accouchement. L’hypnose pour l’accouchement peut être un outil précieux pour soutenir les femmes tout au long de leur travail, en favorisant un environnement calme et apaisant qui peut contribuer à une expérience de naissance plus positive.
Le programme Hypno-Vie
Le programme Hypno-Vie est une approche holistique qui vise à apporter un équilibre mental, émotionnel et physique par le biais de séances d’hypnose personnalisées. En se concentrant sur la programmation mentale positive et la visualisation, ce programme offre aux participants l’opportunité de libérer les blocages internes, de renforcer la confiance en soi et de développer des stratégies pour gérer le stress et les émotions négatives. Avec un accompagnement professionnel et bienveillant, les individus sont guidés vers un état de relaxation profonde pour favoriser le bien-être global. Le programme Hypno-Vie s’adresse à ceux qui cherchent à améliorer leur qualité de vie et à optimiser leur potentiel en cultivant un état d’esprit positif et équilibré.En conclusion, la question de savoir s’il est dangereux de rester enfermé dans un état d’hypnose est une préoccupation valable qui nécessite un examen attentif. Bien que l’hypnose puisse être un outil puissant à des fins thérapeutiques et de développement personnel, il est essentiel de l’aborder avec prudence et sous la direction d’un professionnel qualifié. Rester dans un état hypnotique pendant une période prolongée peut entraîner des conséquences inattendues et potentiellement néfastes. Il est crucial de donner la priorité à la sécurité et de garantir que l’hypnose est utilisée de manière responsable et éthique pour éviter tout risque ou impact négatif sur le bien-être mental et physique. Si vous avez des inquiétudes concernant l’hypnose ou si vous ressentez des effets indésirables, il est conseillé de demander l’aide d’un praticien qualifié ou d’un prestataire de soins de santé pour une évaluation et un soutien plus approfondis.
FAQ
Pourquoi les gens pensent à tort qu’il est possible de rester pris en hypnose pendant une période prolongée?Les gens pensent à tort qu’il est possible de rester pris en hypnose pendant une période prolongée en raison des représentations inexactes de l’hypnose dans les médias et la culture populaire. En réalité, l’état hypnotique est un état naturel de conscience modifiée dans lequel la personne reste consciente et peut sortir de cet état à tout moment. Il n’est pas possible de rester bloqué en hypnose indéfiniment, car le sujet conserve toujours le contrôle et peut interrompre la séance à sa volonté.Pourquoi l’hypnose a mauvaise réputation?L’hypnose a une mauvaise réputation en raison de la méconnaissance et des idées fausses qui l’entourent, notamment à cause de sa représentation sensationnaliste dans les médias et de son association avec l’idée de contrôle mental. En réalité, l’hypnose est une pratique thérapeutique légitime et efficace, utilisée pour traiter une variété de problèmes de santé mentale et physique. Il est important de se renseigner correctement sur l’hypnose et de consulter des professionnels qualifiés pour en comprendre pleinement les bénéfices.Pourquoi les gens ont-ils peur de rester pris en hypnose? Les mythesLes gens ont peur de rester pris en hypnose en raison des mythes et des idées fausses répandus selon lesquels ils pourraient perdre le contrôle de leur esprit et être manipulés par l’hypnotiseur. Read the full article
0 notes
Text
What is Omenn's syndrome and how can cord blood banks help?

I am ready to enroll in cord blood banking NOW and get my special discount!

By clicking on either buttons, you are agreeing to our TOS and disclaimers and will be redirected to an affiliate cord blood banking provider. We might get financial compensation if you sign up with them through our affiliate links. Unlock your special discounts by adding your promo code.CORD300 in the coupon field to get $300 OFF cord blood and tissue banking. OR cord200 to get $200 OFF if you are getting cord blood banking only. I want more information on cord blood banking

Omenn's syndrome is a rare and severe genetic disorder that affects the immune system. It is characterized by a deficiency in certain immune cells, leading to a weakened ability to fight off infections. This syndrome is caused by mutations in the RAG1 or RAG2 genes, which are responsible for producing proteins necessary for the development and function of immune cells. While there is no cure for Omenn's syndrome, early detection and treatment can significantly improve the quality of life for those affected. One promising option for treatment is through the use of cord blood, which is collected from the umbilical cord of newborns and stored in cord blood banks. Cord blood contains stem cells, which have the ability to develop into various types of cells in the body, including immune cells. This article will explore the causes and symptoms of Omenn's syndrome, as well as the potential benefits of using cord blood from public cord blood banks in the treatment of this rare disorder. Additionally, we will discuss the challenges and limitations of this treatment option and the importance of promoting awareness and education about this condition.
Understanding Omenn's syndrome: a rare immunodeficiency disorder.
Omenn's syndrome is a rare immunodeficiency disorder characterized by severe combined immunodeficiency (SCID) and a range of clinical features. It is caused by mutations in genes involved in the development and function of immune cells. Individuals with Omenn's syndrome typically present with symptoms such as failure to thrive, recurrent infections, erythroderma (widespread redness of the skin), and lymphadenopathy (enlarged lymph nodes). The immune system dysfunction in Omenn's syndrome is primarily due to a lack of functional T-cells, which play a crucial role in the body's defense against pathogens. Understanding the underlying mechanisms of Omenn's syndrome is essential for developing effective treatment strategies. In recent years, cord blood banks have emerged as a potential solution for patients with Omenn's syndrome. Cord blood, obtained from the umbilical cord after birth, is a rich source of stem cells that can be used for hematopoietic stem cell transplantation (HSCT), a curative treatment option for Omenn's syndrome. Cord blood banks store these valuable stem cells, providing a readily available source for patients in need. This innovative approach highlights the critical role that cord blood banks play in potentially improving outcomes for individuals with Omenn's syndrome and other immunodeficiency disorders.
Symptoms and genetic cause explained.
Symptoms of Omenn's syndrome can manifest early in infancy, typically within the first few months of life. These symptoms may include severe and recurrent infections, failure to thrive, diarrhea, and skin abnormalities such as erythroderma. The genetic cause of Omenn's syndrome lies in mutations in specific genes involved in the development and function of immune cells, particularly those responsible for T-cell production. These mutations result in the impaired functioning of the immune system, making individuals with Omenn's syndrome highly susceptible to infections and other immune-related complications. Genetic testing is crucial in diagnosing Omenn's syndrome and identifying the specific genetic mutations involved. Understanding the genetic basis of this disorder can not only aid in accurate diagnosis but also contribute to the development of targeted therapies and potential gene-based treatments in the future.
The role of cord blood banks.
Cord blood banks play a vital role in the field of medical research and potentially life-saving treatments. Cord blood, which is collected from the umbilical cord and placenta after childbirth, is a rich source of hematopoietic stem cells. These stem cells have the unique ability to develop into various types of blood cells, including red blood cells, white blood cells, and platelets.By storing cord blood in specialized banks, it becomes readily available for transplantation to patients in need. Cord blood transplants have been successfully used in the treatment of various hematological disorders, such as leukemia and certain immune system deficiencies. The presence of these valuable stem cells in cord blood provides a potential alternative to bone marrow transplants, offering patients a higher chance of finding a suitable match and reducing the risk of complications.Moreover, cord blood banks also contribute to medical research by providing a valuable resource for studying the development of diseases, identifying genetic factors, and exploring potential therapies. The stored cord blood samples can be used for research purposes, allowing scientists to gain insights into the causes and mechanisms of various conditions, including genetic disorders like Omenn's syndrome. This research ultimately aids in advancing our understanding of these diseases, paving the way for improved diagnostic methods and targeted treatments.In conclusion, the role of cord blood banks is instrumental in facilitating lifesaving treatments and driving medical research forward. The collection and storage of cord blood not only offer hope for patients in need of stem cell transplantation but also provide invaluable resources for scientific exploration and the development of innovative therapies.
Why cord blood is valuable for Omenn's syndrome patients.
Omenn's syndrome is a rare and severe form of combined immunodeficiency that affects infants. It is characterized by a dysfunctional immune system, resulting in recurrent infections and failure to thrive. Cord blood from umbilical cord and placenta offers a valuable solution for these patients due to its abundance of hematopoietic stem cells. These stem cells can be used for transplantation to replace the faulty immune system in Omenn's syndrome patients. By introducing healthy stem cells from cord blood, the immune system can be restored, providing a potential cure for this debilitating condition. Cord blood banks play a crucial role in preserving these valuable stem cells and making them readily accessible for transplantation, providing hope and a chance for a better quality of life for Omenn's syndrome patients.
Potential for cord blood transplants.
Cord blood transplants have shown immense potential in the field of regenerative medicine. With their rich source of hematopoietic stem cells, cord blood banks have opened up new possibilities for treating a variety of diseases and disorders. Beyond Omenn's syndrome, cord blood transplants have been successfully used in the treatment of leukemia, lymphoma, and other blood-related cancers. The ability of cord blood stem cells to differentiate and regenerate into various cell types offers a promising avenue for regenerating damaged tissues and organs. Ongoing research and advancements in cord blood banking and transplantation techniques continue to expand the potential for these life-saving procedures, bringing hope to patients and their families.
Benefits of using cord blood.
Cord blood, obtained from the umbilical cord after childbirth, has numerous benefits when it comes to medical treatment. One of the main advantages is its rich source of hematopoietic stem cells, which have the ability to develop into different types of blood cells. This makes cord blood an invaluable resource for treating various diseases and disorders, including genetic disorders, immune system deficiencies, and certain types of cancers. Unlike bone marrow transplants, using cord blood for transplantation eliminates the need for a perfect match between the donor and recipient, greatly expanding the potential pool of donors. Additionally, cord blood transplants have a lower risk of complications and rejection compared to other transplant methods, making them a safer option for patients. Overall, the use of cord blood offers a promising and effective approach in regenerative medicine, offering hope for improved health outcomes and quality of life for patients.
Availability of cord blood banks.
Cord blood banks play a crucial role in making cord blood available for medical treatments. These specialized banks collect, process, and store cord blood units, ensuring their availability for future use. The availability of cord blood banks has significantly increased the accessibility of this valuable resource, allowing more patients to benefit from its potential therapeutic applications. By preserving cord blood units, these banks help bridge the gap between patients in need of a transplant and suitable donors. Furthermore, cord blood banks maintain stringent quality control measures to ensure the viability and safety of stored units, adhering to established regulations and standards. The establishment and ongoing operation of cord blood banks contribute to the advancement of regenerative medicine, offering a lifeline for individuals in search of compatible stem cell sources for treatment.
Cost and storage options.
When considering cord blood banking, it is important to understand the cost and storage options associated with this valuable resource. The cost of cord blood banking can vary depending on the chosen bank and the specific services included in the package. Typically, there are both initial processing and storage fees involved. It is essential to inquire about any additional charges or annual fees that may apply. Additionally, cord blood banks may offer various storage options, such as long-term storage plans that ensure the preservation of cord blood units for an extended period. Some banks also provide the option of storing cord tissue or offering combined packages that include both cord blood and cord tissue storage. It is advisable to carefully consider the cost and storage options provided by different cord blood banks to make an informed decision that best suits individual needs and preferences.
Support and resources for families.
In addition to the medical benefits of cord blood banking, families facing a diagnosis of Omenn's syndrome can also find valuable support and resources through cord blood banks. These banks often have dedicated customer support teams who are knowledgeable about the condition and can provide guidance and assistance throughout the process. They can help families navigate the complexities of cord blood banking, answer any questions or concerns, and ensure a smooth and seamless experience. Moreover, cord blood banks may have partnerships or connections with organizations or support groups specifically focused on Omenn's syndrome. These resources can provide emotional support, educational materials, and access to a community of individuals going through similar experiences. By utilizing the support and resources provided by cord blood banks, families can feel empowered and equipped to navigate the challenges of Omenn's syndrome with confidence.
Hope for a brighter future.
The journey of families facing Omenn's syndrome can be filled with uncertainty and challenges. However, amidst the difficulties, there is always hope for a brighter future. Medical advancements and research continue to progress, offering possibilities for improved treatments, therapies, and ultimately, a cure for Omenn's syndrome. With the support of cord blood banks and their commitment to advancing medical knowledge, there is optimism that breakthroughs in understanding and managing this rare condition will continue to emerge. Through ongoing collaboration between medical professionals, researchers, and patient communities, there is a shared vision of a future where individuals with Omenn's syndrome can lead fulfilling lives, free from the limitations and complications associated with the condition. This hope for a brighter future serves as a guiding light for families affected by Omenn's syndrome, spurring them forward in their pursuit of better outcomes and ultimately, the realization of their dreams.In conclusion, Omenn's syndrome is a rare and severe immunodeficiency disorder that requires prompt and effective treatment. Cord blood banks play a crucial role in providing a potential cure for this condition through the use of stem cells. By preserving and storing cord blood, these banks provide a valuable resource for patients in need of a bone marrow transplant. As our understanding of this syndrome continues to evolve, it is important for individuals to consider donating their baby's cord blood to help those affected by Omenn's syndrome and other similar disorders.
FAQ
What is Omenn's syndrome and how does it affect the immune system?Ommen's syndrome is a rare genetic disorder that affects the immune system, causing severe combined immunodeficiency. This means individuals with Omenn's syndrome have a weakened immune system that is unable to effectively fight off infections, leading to recurrent infections, failure to thrive, and other health complications. The condition is characterized by a deficiency in immune cells, particularly T cells, which play a crucial role in the body's ability to defend against pathogens. Treatment often involves immunosuppressive therapy or bone marrow transplantation to restore immune function.How can cord blood banks help in the treatment of Omenn's syndrome?Cord blood banks can potentially help in the treatment of Omenn's syndrome by providing stem cells for transplantation. These stem cells can be used to rebuild the immune system of individuals with Omenn's syndrome, offering a potential cure for the disorder. By storing cord blood containing healthy stem cells, cord blood banks provide a valuable resource for patients in need of stem cell transplants for various genetic disorders, including Omenn's syndrome.What specific types of stem cells found in cord blood are beneficial for treating Omenn's syndrome?Hematopoietic stem cells found in cord blood are beneficial for treating Omenn's syndrome as they have the ability to differentiate into various blood cell types, which can help replenish the immune system in patients with this condition. These stem cells can potentially improve immune function and help combat the symptoms of Omenn's syndrome by producing healthy blood cells and providing a source of new immune cells to replace the dysfunctional ones.Are there any limitations or challenges in using cord blood from banks for the treatment of Omenn's syndrome?There may be limitations in using cord blood from banks for treating Omenn's syndrome, as not all cord blood units may have the necessary matching HLA types for the recipient. Additionally, the quantity of cells in a single cord blood unit may not be sufficient for an adequate transplant in some cases. Furthermore, the time required to locate a suitable match from the cord blood bank may delay treatment, which can be critical in cases of Omenn's syndrome due to the severity of the condition.How does the process of accessing and using cord blood from banks for Omenn's syndrome treatment work?Cord blood from banks is accessed and used for Omenn's syndrome treatment by first identifying a suitable donor match, collecting the cord blood, and then infusing it into the patient. The stem cells present in the cord blood can help replenish the patient's immune system and potentially treat the symptoms of Omenn's syndrome. The process involves careful matching of donor cells to reduce the risk of rejection and complications. Overall, cord blood from banks provides a valuable source of stem cells for treating immune disorders like Omenn's syndrome. Read the full article
0 notes
Text
What is X-linked lymphoproliferative disease and how can cord blood banks help?

I am ready to enroll in cord blood banking NOW and get my special discount!

By clicking on either buttons, you are agreeing to our TOS and disclaimers and will be redirected to an affiliate cord blood banking provider. We might get financial compensation if you sign up with them through our affiliate links. Unlock your special discounts by adding your promo code.CORD300 in the coupon field to get $300 OFF cord blood and tissue banking. OR cord200 to get $200 OFF if you are getting cord blood banking only. I want more information on cord blood banking

X-linked lymphoproliferative disease (XLP) is a rare genetic disorder that primarily affects the immune system. It is caused by a mutation in a gene on the X chromosome, resulting in a deficiency of certain immune cells, specifically T and natural killer (NK) cells. This deficiency leads to an increased risk of severe and potentially life-threatening infections, as well as an increased susceptibility to certain types of cancer. XLP can also manifest in other organs, such as the liver and central nervous system, causing a range of symptoms and complications. While there is currently no cure for XLP, early diagnosis and treatment can greatly improve the outcome for affected individuals. This is where cord blood banks can play a crucial role. Cord blood, the blood obtained from the umbilical cord and placenta after childbirth, contains a rich source of stem cells that have the potential to develop into a variety of immune cells. By preserving cord blood in a bank, these precious stem cells can be used for the treatment of XLP and other disorders of the immune system. In this article, we will explore the mechanisms of XLP, its impact on individuals and families, and the potential role of cord blood banks in providing hope for those affected by this devastating disease.
Understanding X-linked lymphoproliferative disease - a rare genetic disorder.
X-linked lymphoproliferative disease (XLP) is a rare genetic disorder that primarily affects the immune system. It is characterized by an abnormal immune response to certain viral infections, leading to severe complications such as lymphomas, organ failure, and even death. XLP is caused by mutations in genes involved in regulating the immune response, particularly the SH2D1A gene. This gene is responsible for producing a protein called SLAM-associated protein (SAP), which plays a crucial role in immune cell signaling. When SAP is absent or dysfunctional, the immune system fails to properly regulate the response to viral infections, resulting in the development of XLP. Due to its rarity and complex nature, XLP often goes undiagnosed or misdiagnosed, leading to delayed treatment and management. However, advancements in genetic testing and research have allowed for improved understanding of the disease, leading to better diagnosis and treatment options for affected individuals.
How does the disease manifest?
X-linked lymphoproliferative disease (XLP) manifests in various ways, primarily affecting the immune system. Individuals with XLP may experience recurrent severe viral infections, particularly Epstein-Barr virus (EBV) infections. These infections can lead to complications such as severe mononucleosis, hepatitis, or even lymphomas. Other common manifestations of XLP include hypogammaglobulinemia, which is a decrease in the production of antibodies, and hemophagocytic lymphohistiocytosis (HLH), a life-threatening condition characterized by uncontrolled immune activation and widespread inflammation. Additionally, individuals with XLP may develop autoimmune disorders, such as autoimmune hemolytic anemia or immune thrombocytopenia. It is important to note that the manifestations of XLP can vary widely among individuals, and early diagnosis and appropriate management are crucial for improving outcomes.
Importance of early diagnosis and treatment
Timely diagnosis and treatment of X-linked lymphoproliferative disease (XLP) play a pivotal role in improving patient outcomes and quality of life. Early detection allows for timely intervention and the implementation of appropriate management strategies. With XLP being a potentially life-threatening condition, early diagnosis enables healthcare professionals to initiate targeted therapies and preventive measures to minimize the risk of severe viral infections, complications, and autoimmune disorders associated with the disease. Furthermore, prompt identification of XLP allows for genetic counseling and testing, which can help in assessing the risk of XLP within families and providing them with necessary information for family planning. By emphasizing the importance of early diagnosis and treatment, healthcare providers can ensure timely interventions that significantly impact outcomes for individuals with XLP.
Role of cord blood banks
Cord blood banks play a significant role in the management and treatment of X-linked lymphoproliferative disease (XLP). These specialized banks collect, process, and store cord blood samples from newborns, which contain valuable stem cells capable of generating various blood components. In the case of XLP, cord blood banks provide a potential source of hematopoietic stem cells that can be used for transplantation. Stem cell transplantation from a compatible donor offers a curative approach for individuals with XLP, as it replaces the defective immune system with a healthy one. By preserving and making these cord blood samples available, cord blood banks contribute to the availability of suitable donors for transplantation, increasing the chances of successful treatment and improved outcomes for patients with XLP. The utilization of cord blood from these banks not only provides a potentially life-saving therapy but also offers hope for those affected by XLP and their families.
Cord blood stem cells explained
Cord blood stem cells are a valuable resource that can be used in various medical treatments and therapies. These stem cells, found in the blood of newborns' umbilical cords, possess unique properties that make them highly desirable for medical purposes. Unlike other types of stem cells, such as those found in bone marrow, cord blood stem cells are relatively easy to collect and store, making them readily accessible for future use. These cells have the ability to differentiate into different types of blood cells, including red blood cells, white blood cells, and platelets. This versatility makes cord blood stem cells an ideal option for treating a range of diseases and conditions, including certain types of cancer, blood disorders, and immune system disorders. With advancements in medical research and technology, the potential applications for cord blood stem cells continue to expand, offering hope for improved treatment options and better outcomes for patients in need.
How cord blood can help treat XLPD
X-linked lymphoproliferative disease (XLPD) is a rare genetic disorder that affects the immune system and can have severe consequences for those diagnosed. Cord blood banks play a crucial role in potentially treating XLPD by providing a source of stem cells that can be used in hematopoietic stem cell transplantation. These stem cells, derived from the cord blood of healthy newborns, have the ability to replace faulty immune cells and restore the immune system's normal functioning. By transplanting these stem cells, individuals with XLPD may have the opportunity for improved immune response and reduced susceptibility to infections and other complications associated with the disease. The availability of cord blood stem cells through cord blood banks offers new possibilities for the treatment of XLPD and brings hope to patients and their families in their journey towards better health and quality of life.
Success stories of cord blood transplants
Several success stories highlight the potential of cord blood transplants in treating various diseases, including X-linked lymphoproliferative disease (XLPD). One such story involves a young boy diagnosed with XLPD who underwent a cord blood transplant. Following the transplant, his immune system gradually strengthened, and he experienced a significant reduction in infections and related complications. Another inspiring story involves a teenage girl with XLPD who received a cord blood transplant and subsequently achieved remission from the disease. These success stories demonstrate the transformative impact that cord blood transplants can have on individuals affected by XLPD, offering them a chance at improved health and a brighter future. These remarkable outcomes are a testament to the potential of cord blood banks and the invaluable resource they provide in the field of regenerative medicine.
Availability of cord blood banks globally
The availability of cord blood banks globally plays a crucial role in facilitating the use of cord blood for various medical treatments, including those for X-linked lymphoproliferative disease (XLPD). Cord blood banks collect, process, and store umbilical cord blood, which is a rich source of stem cells. These stem cells can be used in transplants to replace damaged or defective cells in patients with XLPD. The widespread establishment of cord blood banks worldwide ensures that a diverse range of individuals can access these life-saving treatments. With cord blood banks in different countries and regions, individuals affected by XLPD have increased opportunities to find suitable matches for their transplant needs, increasing the chances of successful outcomes and improved quality of life. This global availability of cord blood banks exemplifies the collaborative efforts of the medical community to provide accessible and effective solutions for patients with XLPD and other diseases.
Cost and storage options
Cost and storage options are important considerations when utilizing cord blood banks for the treatment of X-linked lymphoproliferative disease (XLPD). The cost of storing cord blood can vary depending on the specific bank and its services. It is essential to research and compare different banks to ensure they meet quality and regulatory standards, as well as provide transparent pricing structures. Additionally, storage options should be evaluated, including the duration of storage, retrieval processes, and the ability to transfer the cord blood to different facilities if necessary. The cost and storage options associated with cord blood banks are critical factors in determining the feasibility and accessibility of utilizing this valuable resource for the treatment of XLPD.
How to choose a reputable cord blood bank.
When choosing a reputable cord blood bank for the treatment of X-linked lymphoproliferative disease, there are several factors to consider. Firstly, it is important to ensure that the bank is accredited by relevant regulatory bodies, such as the AABB or FACT. This accreditation ensures that the bank meets rigorous quality and safety standards in the collection, processing, and storage of cord blood. Additionally, it is advisable to research the bank's track record and reputation within the medical community. Reading reviews, talking to healthcare professionals, and seeking recommendations can provide valuable insights into the bank's reliability and performance. Transparency is also crucial when evaluating a cord blood bank. The bank should provide clear information about their processes, protocols, and fees, including any additional costs that may arise during the storage period. Finally, consider the bank's experience and expertise in handling and treating XLPD specifically. Look for evidence of successful outcomes and ongoing research collaborations in the field of hematopoietic stem cell transplantation. By carefully considering these factors, you can choose a reputable cord blood bank that can provide the necessary support and resources for the treatment of XLPD.In conclusion, X-linked lymphoproliferative disease is a rare genetic disorder that affects the immune system. It can be a devastating diagnosis for families, but there is hope in the form of cord blood banks. These banks store umbilical cord blood which contains valuable stem cells that can be used in the treatment of various diseases, including X-linked lymphoproliferative disease. By banking cord blood, families can have a potential lifesaving resource for their child's future. It is important to spread awareness about this disease and the importance of cord blood banking in order to help those affected by X-linked lymphoproliferative disease.
FAQ
What is X-linked lymphoproliferative disease and how does it affect individuals?X-linked lymphoproliferative disease (XLP) is a genetic disorder that affects the immune system and is characterized by an abnormal response to Epstein-Barr virus (EBV). Individuals with XLP have a higher risk of developing severe and potentially life-threatening infections, lymphomas, and other immune-related complications when exposed to EBV. This disease can lead to complications such as hemophagocytic lymphohistiocytosis, lymphoproliferative disorder, and dysgammaglobulinemia. Early diagnosis and management are crucial in preventing these complications in individuals with XLP.How can cord blood banks help in the treatment of X-linked lymphoproliferative disease?Cord blood banks can help in the treatment of X-linked lymphoproliferative disease by providing a source of stem cells that can be used for hematopoietic stem cell transplantation. These stem cells can help restore the immune system in patients with the disease and potentially improve their outcomes. By having a diverse pool of cord blood units available, cord blood banks increase the chances of finding a suitable match for patients in need of a transplant, making them a valuable resource in the treatment of X-linked lymphoproliferative disease.What specific advantages does cord blood offer in treating X-linked lymphoproliferative disease compared to other sources of stem cells?Cord blood offers specific advantages in treating X-linked lymphoproliferative disease due to its higher tolerance for HLA mismatches, lower risk of graft-versus-host disease, and reduced chance of transmitting infectious diseases compared to other sources of stem cells. Additionally, cord blood contains a diverse range of stem cells that can promote immune system reconstitution, making it a valuable option for patients with this inherited disorder.Are there any limitations or challenges in using cord blood from banks for treating X-linked lymphoproliferative disease?There may be limitations in using cord blood from banks for treating X-linked lymphoproliferative disease, as the disease is genetic and may require a specific donor match for successful treatment. Additionally, the quantity and quality of cord blood collected may vary, potentially affecting the outcome of the treatment. Therefore, finding a suitable donor match and ensuring sufficient cord blood availability can be challenging when using cord blood from banks for treating X-linked lymphoproliferative disease.How can individuals or families with a history of X-linked lymphoproliferative disease benefit from storing cord blood in a bank for future use?Individuals or families with a history of X-linked lymphoproliferative disease can benefit from storing cord blood in a bank as it provides a potential source of stem cells for future treatment options. Cord blood contains hematopoietic stem cells which can be utilized in therapies like bone marrow transplants to treat various genetic disorders, including X-linked lymphoproliferative disease. Storing cord blood ensures that these valuable stem cells are readily available if needed, offering a potentially life-saving treatment option for affected individuals or family members in the future. Read the full article
0 notes
Text
What is Myelokathexis and how can cord blood banking help?

I am ready to enroll in cord blood banking NOW and get my special discount!

By clicking on either buttons, you are agreeing to our TOS and disclaimers and will be redirected to an affiliate cord blood banking provider. We might get financial compensation if you sign up with them through our affiliate links. Unlock your special discounts by adding your promo code.CORD300 in the coupon field to get $300 OFF cord blood and tissue banking. OR cord200 to get $200 OFF if you are getting cord blood banking only. I want more information on cord blood banking

Myelokathexis is a rare inherited disorder that affects the body's ability to produce and maintain a healthy number of white blood cells. While this condition is not well-known, it can cause serious health complications such as recurrent infections, anemia, and even leukemia. In recent years, cord blood banking has emerged as a potential solution for individuals with myelokathexis. This practice involves collecting and storing a baby's umbilical cord blood, which is rich in stem cells, for future medical use. These stem cells have the potential to develop into various types of blood cells, including white blood cells, and can therefore help individuals with myelokathexis to boost their immune system. In this article, we will delve deeper into the condition of myelokathexis and explore how cord blood banking can potentially provide a lifesaving solution for those affected by this rare disorder. We will also discuss the benefits and considerations of cord blood banking and provide valuable information for parents who are considering this option for their child's future health.
Understanding Myelokathexis: A rare disorder
Myelokathexis is a rare disorder that affects the bone marrow's ability to produce mature white blood cells. It is characterized by the retention of these immature cells in the bone marrow, leading to a decreased number of functional white blood cells in the bloodstream. This can weaken the body's immune system, making individuals with myelokathexis more susceptible to infections and other medical complications. The exact cause of myelokathexis is still not fully understood, but it is believed to have a genetic component. While there is currently no cure for myelokathexis, various treatment options are available to manage the symptoms and improve quality of life for those affected. One potential avenue that has shown promise is cord blood banking, which involves collecting and storing the stem cells from a newborn's umbilical cord blood. These stem cells can be used in future treatments, such as bone marrow transplants, which may provide a potential solution for individuals with myelokathexis.
Importance of cord blood banking
The importance of cord blood banking cannot be overstated. Cord blood is a rich source of hematopoietic stem cells, which are responsible for the production of all types of blood cells. These stem cells have the unique ability to differentiate and regenerate, making them valuable in the treatment of various diseases and disorders. By banking cord blood, families can ensure that these precious stem cells are readily available for potential future use. This is particularly significant for individuals with genetic conditions, like myelokathexis, as it provides an opportunity to potentially replace the faulty cells and restore normal functionality. Cord blood banking offers a sense of security and peace of mind, knowing that there is a valuable resource that can be tapped into if the need arises. It is a proactive step towards safeguarding the health of your family and opening up possibilities for potential life-saving treatments.
Potential treatment for Myelokathexis patients
Recent research has shown promising potential for the treatment of Myelokathexis patients. One emerging approach involves the use of gene therapy, which aims to correct the genetic mutation responsible for the condition. This therapy involves introducing a functional copy of the mutated gene into the patient's hematopoietic stem cells, allowing them to produce healthy blood cells. Initial studies have shown encouraging results, with patients experiencing improvements in their overall blood cell counts and reduced severity of symptoms. However, further research and clinical trials are needed to validate the safety and long-term effectiveness of this treatment approach. Nonetheless, these advancements offer hope for individuals with Myelokathexis, as they pave the way for potential targeted therapies that can address the root cause of the condition and provide a chance for improved quality of life.
The role of stem cells
Stem cells play a crucial role in various aspects of medical research and treatment. These unique cells have the ability to differentiate into different cell types in the body, making them valuable in regenerative medicine and potential therapies for various diseases. In the context of Myelokathexis, stem cells hold particular promise. Hematopoietic stem cells, which are found in bone marrow and cord blood, have the ability to develop into different types of blood cells, including white blood cells that are affected in Myelokathexis. By harnessing the potential of these stem cells, researchers are exploring innovative approaches such as gene therapy to correct the underlying genetic mutations responsible for the condition. This exciting avenue of research offers hope for improved treatment options and potentially a better quality of life for individuals with Myelokathexis.
Benefits of using cord blood
Cord blood banking offers several benefits in the context of medical research and treatment. One of the key advantages is the rich source of hematopoietic stem cells found in cord blood. These stem cells have the ability to replenish and regenerate the blood and immune system, making them valuable in treating various diseases, including Myelokathexis. By preserving cord blood, individuals have a readily available source of stem cells that can potentially be used for transplantation or cellular therapy. Cord blood stem cells have also been found to have a lower risk of graft-versus-host disease compared to other sources, making them an attractive option for patients in need of stem cell transplants. Additionally, cord blood banking provides families with peace of mind, knowing that they have a valuable resource that may offer future therapeutic benefits for their child or other family members.
How cord blood can help
Cord blood, with its abundant supply of hematopoietic stem cells, holds great potential in aiding the treatment of various medical conditions. These stem cells have the remarkable ability to differentiate into different types of blood cells, including white blood cells that are crucial for a healthy immune system. This makes cord blood an invaluable resource in addressing conditions such as Myelokathexis, where the production of white blood cells is impaired. By utilizing cord blood banking, individuals with Myelokathexis and other similar disorders can have access to a reliable source of stem cells for transplantation or cellular therapy. The utilization of cord blood stem cells not only offers a potential cure but also decreases the risk of complications, such as graft-versus-host disease. In the realm of medical advancements, cord blood banking provides a sense of security and hope for families, as it ensures that they have a readily available option for potential future therapeutic interventions.
Preserving stem cells for future use
Preserving stem cells for future use is a proactive approach that individuals and families can take to safeguard their health and well-being. Stem cells have demonstrated immense potential in regenerative medicine, as they possess the unique ability to develop into different types of cells in the body. By preserving these cells through methods such as cord blood banking, individuals can ensure that they have a valuable resource at their disposal for potential future treatments. Whether it be for the management of genetic disorders, the repair of damaged tissues, or even the development of personalized therapies, preserving stem cells offers a sense of security and opens doors to a wide range of medical possibilities. With ongoing advancements in stem cell research, the decision to preserve these cells for future use is a proactive investment in one's health and the potential for improved medical outcomes.
Potential for disease treatment
The potential for disease treatment using preserved stem cells is a promising area of research with significant implications for healthcare. Stem cells have the remarkable ability to differentiate into various specialized cell types, making them a valuable resource in the development of innovative and targeted therapies. By harnessing the regenerative potential of stem cells, scientists and medical professionals are exploring their use in treating a wide range of diseases, including but not limited to neurological disorders, autoimmune conditions, cardiovascular diseases, and certain types of cancers. This emerging field of regenerative medicine holds the promise of providing more effective and personalized treatments for patients, potentially revolutionizing the way we approach disease management. Preserving stem cells through methods like cord blood banking ensures that individuals have access to these valuable resources, enabling them to potentially benefit from advances in disease treatment in the years to come.
Providing hope for families
Families facing the challenges of certain medical conditions often find themselves searching for hope and solutions. The concept of cord blood banking presents a ray of hope for these families, offering a potential lifeline in their journey towards improved health and well-being. By preserving the precious stem cells found in cord blood, these families can secure a valuable resource that may hold the key to future treatments and therapies. The ability to store and access these stem cells opens up possibilities for personalized and targeted medical interventions, providing a sense of hope for families who may be grappling with the uncertainties of their loved one's condition. In this way, cord blood banking not only offers the potential for breakthrough treatments but also instills a sense of optimism and reassurance in families, knowing that they have taken proactive steps towards a brighter future.
Advancements in medical research.
The field of medical research has witnessed remarkable advancements in recent years, paving the way for groundbreaking discoveries and innovative treatments. Scientists and researchers are continuously exploring new frontiers, using cutting-edge technologies and methodologies to unravel the mysteries of various diseases and conditions. Through extensive collaborations and interdisciplinary approaches, medical researchers have made significant strides in understanding the underlying mechanisms of diseases, identifying novel biomarkers, and developing targeted therapies. These advancements have revolutionized the way we approach healthcare, offering personalized and precise interventions that have the potential to transform lives. From advancements in genomics to the development of groundbreaking immunotherapies, medical research continues to push the boundaries of what is possible, emphasizing the importance of ongoing investment and support in this critical field.In conclusion, myelokathexis is a rare disorder that can lead to serious health complications for those affected. However, cord blood banking offers a potential solution by providing a source of healthy stem cells for those with myelokathexis. By preserving cord blood at birth, families can have peace of mind knowing that they have a potential treatment option for this rare disorder. Further research and advancements in the field of stem cell therapy may provide even more hope for those living with myelokathexis.
FAQ
What is myelokathexis and how does it affect the body's immune system?Myelokathexis is a rare condition where white blood cells are unable to leave the bone marrow and enter the bloodstream. This results in low levels of white blood cells in the body, weakening the immune system's ability to fight infections. The trapped white blood cells in the bone marrow are unable to perform their normal functions in the bloodstream, leading to an increased susceptibility to infections and other immune-related complications. Treatment typically involves addressing the underlying genetic cause and managing symptoms to support immune function.How does cord blood banking play a role in treating myelokathexis?Cord blood banking can potentially play a role in treating myelokathexis by providing a source of hematopoietic stem cells that can be used in hematopoietic stem cell transplantation. This procedure can help replace the dysfunctional bone marrow in individuals with myelokathexis, potentially restoring their ability to produce healthy blood cells and improving their overall health outcomes. By storing cord blood containing healthy stem cells, individuals with myelokathexis can potentially access a suitable match for transplantation, offering a potential treatment option for this rare genetic disorder.What are the potential benefits of using cord blood for treating myelokathexis compared to other treatment options?Cord blood contains hematopoietic stem cells that can be used for bone marrow transplantation in myelokathexis patients. This treatment option offers a lower risk of rejection and graft-versus-host disease compared to traditional bone marrow transplants. Additionally, cord blood is readily available, does not require an exact match, and can be stored for future use. Overall, using cord blood for treating myelokathexis provides a potentially safer and more accessible treatment option for patients in need of a stem cell transplant.How does the process of cord blood banking work and how can individuals ensure they are prepared for potential future medical needs?Cord blood banking involves collecting and storing the blood from a newborn's umbilical cord for future medical use, particularly in treating diseases. To ensure preparedness for potential future medical needs, individuals can research reputable cord blood banks, understand the costs and benefits of banking, discuss with healthcare providers, and make informed decisions before the birth of their child. Being aware of family medical history and discussing options with healthcare providers can also help individuals make informed choices about cord blood banking.Are there any limitations or risks associated with using cord blood for treating myelokathexis?While cord blood stem cells have shown promise in treating various medical conditions, including myelokathexis, there are limitations and risks to consider. These include the potential for graft-versus-host disease, inadequate cell dosage, and limited availability of suitable matches. Additionally, the long-term efficacy and safety of cord blood transplantation for myelokathexis have not been extensively studied. It is essential to consult with a healthcare provider to weigh the potential benefits against the risks before pursuing this treatment option. Read the full article
0 notes
Text
What is Myeloid/Natural Killer (NK) Cell Precursor Acute Leukemia and how can FDA approved cord blood banking help?

I am ready to enroll in cord blood banking NOW and get my special discount!

By clicking on either buttons, you are agreeing to our TOS and disclaimers and will be redirected to an affiliate cord blood banking provider. We might get financial compensation if you sign up with them through our affiliate links. Unlock your special discounts by adding your promo code.CORD300 in the coupon field to get $300 OFF cord blood and tissue banking. OR cord200 to get $200 OFF if you are getting cord blood banking only. I want more information on cord blood banking

Myeloid/Natural Killer (NK) Cell Precursor Acute Leukemia is a rare and aggressive form of blood cancer that affects both children and adults. It is characterized by the rapid proliferation of abnormal myeloid cells and natural killer cells, which are responsible for fighting infections and controlling the growth of cancer cells. This type of leukemia is considered a precursor to acute myeloid leukemia (AML), a more common and well-known form of blood cancer. Myeloid/NK Cell Precursor Acute Leukemia requires immediate and intensive treatment, as it can quickly progress and potentially be fatal if left untreated. However, in recent years, the medical community has made significant advancements in the treatment of this disease, including the use of cord blood banking. In this article, we will delve into the details of Myeloid/NK Cell Precursor Acute Leukemia, its symptoms, diagnosis, and current treatment options. We will also explore the role of FDA approved cord blood banking in providing viable and potentially life-saving treatment options for patients with this rare and complex form of leukemia.
Definition and overview of Myeloid/NK Cell Precursor Acute Leukemia
Myeloid/NK Cell Precursor Acute Leukemia is a rare and aggressive form of leukemia that primarily affects children and young adults. It is characterized by the abnormal growth and accumulation of myeloid and natural killer (NK) cell precursors in the bone marrow and blood. This type of leukemia is considered a subtype of acute myeloid leukemia (AML) and is associated with poor prognosis and limited treatment options. Patients with myeloid/NK cell precursor acute leukemia often present with symptoms such as fatigue, fever, easy bruising or bleeding, and frequent infections. Diagnosis typically involves a combination of blood tests, bone marrow biopsy, and genetic testing to confirm the presence of abnormal cells. Early detection and prompt treatment are crucial for improving outcomes in patients with this aggressive form of leukemia.
Understanding how cord blood banking works
Cord blood banking is a process that involves the collection and storage of stem cells from the umbilical cord blood after a baby is born. These stem cells have the unique ability to develop into various types of blood cells, including those of the immune system. The process begins with the expectant parents making the decision to bank their baby's cord blood, often in anticipation of its potential future medical use. During childbirth, a healthcare professional will collect the cord blood using a sterile needle and special collection bag. The collected cord blood is then transported to a cord blood bank, where it undergoes rigorous testing and processing to ensure its viability for long-term storage. Once stored, the cord blood can be used in medical treatments, such as stem cell transplantation, to replace damaged or diseased cells in the body. Cord blood banking offers a valuable resource for families, providing them with a potential source of stem cells that may be used to treat a variety of conditions, including certain types of leukemia, like myeloid/NK cell precursor acute leukemia. Its approval by the FDA ensures the quality and safety of stored cord blood units, providing assurance to families considering this option.
Benefits of FDA approved cord blood banking for leukemia patients
The benefits of FDA approved cord blood banking for leukemia patients are significant. Leukemia is a complex and challenging disease, particularly Myeloid/Natural Killer (NK) Cell Precursor Acute Leukemia, which requires specialized treatments. Cord blood stem cells, which are collected and stored through FDA approved cord blood banking, offer a potential solution for leukemia patients in need of a stem cell transplant. These stem cells have the ability to differentiate into various blood cell types, including those of the immune system. By utilizing cord blood stem cells from a compatible donor, leukemia patients can receive a life-saving transplant that can potentially replace damaged or diseased cells, restore the immune system, and promote the body's ability to fight the disease. The FDA approval of cord blood banking ensures that the collected stem cells meet rigorous standards of safety and quality, providing reassurance for patients and healthcare professionals alike. With the availability of FDA approved cord blood banking, leukemia patients have greater access to a potentially life-saving treatment option that can significantly improve their chances of remission and long-term survival.
The role of stem cells in treating leukemia
Stem cells play a crucial role in the treatment of leukemia, including Myeloid/Natural Killer (NK) Cell Precursor Acute Leukemia. These remarkable cells have the ability to differentiate into various types of blood cells, including white blood cells that are essential for a healthy immune system. In the case of leukemia, where abnormal white blood cells crowd out healthy ones, stem cell transplants offer a potential solution. By using stem cells from a compatible donor, the diseased or damaged cells can be replaced with healthy ones, allowing for the restoration of the immune system and the potential eradication of the disease. The versatility of stem cells makes them a valuable tool in the fight against leukemia, providing hope for patients and their families.
How cord blood stem cells are collected
Cord blood stem cells, which have shown promise in the treatment of various diseases, including Myeloid/Natural Killer (NK) Cell Precursor Acute Leukemia, are collected from the umbilical cord and placenta after a baby is born. The process begins with the clamping and cutting of the umbilical cord, typically done by the healthcare provider. After this, a sterile needle is inserted into the cord vein, and the blood is drained into a collection bag or syringe. The collection is a safe and painless procedure for both the mother and the baby, as it occurs after the delivery when the cord has already served its purpose. This method of obtaining cord blood is preferred as it poses no harm or risk to the newborn or the mother. Once collected, the cord blood is processed and stored in an FDA approved cord blood bank, ensuring its availability for potential future medical use.
The process of storing cord blood
The process of storing cord blood begins once it has been collected from the umbilical cord. The collected cord blood is transported to an FDA approved cord blood bank, where it undergoes rigorous testing and processing procedures. First, the cord blood is tested for infectious diseases and screened to ensure its safety and viability for potential use. Then, it is processed to separate and concentrate the valuable stem cells from the other components of the blood. This is done using specialized equipment and techniques to achieve the highest possible cell recovery and quality. Once the processing is complete, the cord blood is stored in cryogenic tanks at extremely low temperatures to preserve the integrity and viability of the stem cells. These storage facilities are designed to maintain a constant temperature and provide protection against any potential disruptions in power supply. This ensures that the cord blood remains viable and available for potential use in medical treatments, providing a valuable resource for patients in need.
Safety regulations for cord blood banking
Safety regulations for cord blood banking play a critical role in ensuring the quality and integrity of stored cord blood units. The FDA has implemented stringent guidelines to regulate the collection, testing, processing, and storage of cord blood. These regulations aim to minimize the risk of contamination, transfusion reactions, and transmission of infectious diseases. Cord blood banks must adhere to these regulations and undergo regular inspections to maintain their FDA approval. Additionally, the FDA requires cord blood banks to establish protocols for tracking and traceability of cord blood units to ensure accurate identification and retrieval when needed. By complying with these safety regulations, FDA approved cord blood banking provides assurance to parents and healthcare professionals that stored cord blood units are safe and suitable for potential therapeutic use.
Cost comparison of public vs. private cord blood banking
When considering cord blood banking options, it is important to compare the costs associated with public and private cord blood banking. Public cord blood banking is typically offered at no cost to the donor, as the collected cord blood is donated to be used for transplantation in patients who are a match. On the other hand, private cord blood banking involves a fee for the collection, processing, and storage of the cord blood exclusively for the donor and their family's potential future use. Private cord blood banking costs can vary depending on the bank and the specific services offered. It is essential to carefully evaluate the costs and benefits of public and private cord blood banking to make an informed decision that aligns with individual priorities and financial considerations.
Success stories of cord blood transplants
Cord blood transplants have shown remarkable success in treating a variety of diseases, offering promising outcomes for patients in need. Many success stories have emerged, showcasing the potential of cord blood as a valuable source of stem cells for transplantation. For instance, individuals with blood cancers such as leukemia have experienced transformative results through cord blood transplants. These transplants have enabled patients to achieve remission and regain their health, providing renewed hope for those facing life-threatening conditions. Additionally, cord blood transplants have shown efficacy in treating inherited genetic disorders and immune system deficiencies, offering a chance for improved quality of life for affected individuals. These success stories highlight the immense potential of cord blood banking and its role in advancing medical treatments and improving patient outcomes.
Future potential of cord blood banking in leukemia treatment.
The future potential of cord blood banking in leukemia treatment holds great promise for patients and the medical community alike. As ongoing research and advancements in stem cell transplantation continue to progress, cord blood has emerged as a valuable resource in the fight against leukemia. The unique characteristics of cord blood stem cells, such as their immunological naivety and potential for reduced graft-versus-host disease, make them a compelling option for leukemia patients in need of a transplant. Furthermore, the ability to access stored cord blood units expedites the transplant process, providing a timely and potentially life-saving intervention. With continued efforts to optimize matching algorithms and expand the availability of cord blood units, the future of cord blood banking in leukemia treatment holds the potential to revolutionize the field and offer renewed hope to patients battling this challenging disease.In conclusion, myeloid/NK cell precursor acute leukemia is a rare and aggressive form of cancer that can be difficult to treat. However, with the advancement of medical technology and the FDA's approval of cord blood banking, there is hope for patients diagnosed with this disease. By storing cord blood, individuals can have a readily available source of potentially life-saving stem cells, which can be used for transplant and treatment. This option not only offers a chance for a successful outcome, but also provides peace of mind for families and their loved ones. It is crucial to educate ourselves and others about the importance of cord blood banking in the fight against diseases like myeloid/NK cell precursor acute leukemia.
FAQ
What is Myeloid/Natural Killer (NK) Cell Precursor Acute Leukemia and how does it differ from other types of leukemia?Myeloid/Natural Killer (NK) cell precursor acute leukemia is a rare and aggressive form of leukemia in which abnormal myeloid and NK cells proliferate uncontrollably. This type of leukemia differs from others due to its unique cell lineage, involving both myeloid and NK cell precursors. It can present challenges in diagnosis and treatment due to its rarity and aggressive nature, often requiring a tailored approach. Additionally, the prognosis for patients with this type of leukemia can vary compared to more common forms, necessitating specialized care and management strategies.How does FDA approved cord blood banking play a role in the treatment of Myeloid/NK Cell Precursor Acute Leukemia?FDA approved cord blood banking provides a source of stem cells for transplant in the treatment of Myeloid/NK Cell Precursor Acute Leukemia. These stem cells can be used to replace damaged or diseased cells in the bone marrow, helping to restore normal blood cell production in patients with this type of leukemia. The approval ensures that the cord blood units meet specific quality and safety standards, making them a reliable option for transplantation in leukemia patients undergoing treatment.What are the benefits of using cord blood stem cells in the treatment of leukemia compared to other sources of stem cells?Cord blood stem cells are advantageous in leukemia treatment due to their lower risk of rejection, reduced likelihood of transmitting infections, and higher tolerance for tissue mismatches. Additionally, cord blood stem cells are more readily available, can be stored long-term for future use, and have shown promising results in reducing complications post-transplant. Their versatility and effectiveness make them a valuable resource in treating leukemia, offering potential for improved outcomes and increased survival rates for patients undergoing stem cell transplantation.How does the process of collecting and storing cord blood for banking work, and what are the requirements for FDA approval?Cord blood collection involves extracting blood from the umbilical cord post-birth, which is then stored in a cord blood bank for potential future medical use. The FDA regulates cord blood banking, requiring banks to follow specific guidelines related to donor screening, processing, testing, and labeling to ensure safety and efficacy. Approval from the FDA involves demonstrating compliance with Good Manufacturing Practices, adherence to donor screening protocols, and monitoring for infectious diseases. stringent quality control measures are crucial for FDA approval to ensure the safety and effectiveness of cord blood for potential transplantation or other medical uses.Are there any potential risks or limitations associated with using cord blood banking for the treatment of Myeloid/NK Cell Precursor Acute Leukemia?While cord blood banking offers potential benefits for treating Myeloid/NK Cell Precursor Acute Leukemia, there are some limitations and risks. These include the possibility of insufficient cord blood volume, delayed availability, and a potential mismatch between the donor cord blood and recipient. Additionally, there is a risk of graft failure or graft-versus-host disease post-transplant. It is important to weigh the benefits against these limitations and risks when considering cord blood banking for the treatment of this type of leukemia. Read the full article
#cordbloodbankMyeloid/NaturalKiller(NK)CellPrecursorAcuteLeukemia#Myeloid/NaturalKiller(NK)CellPrecursorAcuteLeukemiacordbloodbanking
0 notes
Text
What is Non-Hodgkin’s Lymphoma and how can FDA approved cord blood banking help?

I am ready to enroll in cord blood banking NOW and get my special discount!

By clicking on either buttons, you are agreeing to our TOS and disclaimers and will be redirected to an affiliate cord blood banking provider. We might get financial compensation if you sign up with them through our affiliate links. Unlock your special discounts by adding your promo code.CORD300 in the coupon field to get $300 OFF cord blood and tissue banking. OR cord200 to get $200 OFF if you are getting cord blood banking only. I want more information on cord blood banking

Non-Hodgkin’s Lymphoma (NHL) is a type of cancer that affects the lymphatic system, which is a crucial part of the body's immune system. It is a heterogeneous group of lymphoproliferative malignancies, with over 90 different subtypes identified. According to the American Cancer Society, NHL accounts for about 4% of all cancers in the United States, making it one of the most prevalent types of cancer. The exact cause of NHL is still unknown, but research suggests that certain risk factors, such as age, weakened immune system, and exposure to certain chemicals, may increase the likelihood of developing the disease. In recent years, the use of cord blood banking has been gaining attention as a potential treatment option for NHL. Cord blood, collected from the umbilical cord after a baby is born, contains valuable stem cells that can be used in transplant procedures to treat various diseases, including NHL. In this article, we will delve into the details of Non-Hodgkin’s Lymphoma, the current treatment options available, and how FDA-approved cord blood banking can potentially revolutionize the treatment of this disease.
Understanding Non-Hodgkin's Lymphoma: Causes and Symptoms
Non-Hodgkin's lymphoma is a type of cancer that affects the lymphatic system, which is a part of the body's immune system. While the exact cause of this disease is not fully understood, certain risk factors have been identified. These include a weakened immune system, exposure to certain chemicals or radiation, certain infections such as Epstein-Barr virus and HIV, as well as genetic factors. It is important to be aware of the common symptoms of Non-Hodgkin's lymphoma, which can include swollen lymph nodes, fever, night sweats, unexplained weight loss, fatigue, and persistent coughing or trouble breathing. Early detection and diagnosis of Non-Hodgkin's lymphoma is crucial for effective treatment and improved outcomes.
Types of Non-Hodgkin's Lymphoma
Non-Hodgkin's lymphoma is a complex disease with various subtypes, each characterized by distinct characteristics and behaviors. The most common types include diffuse large B-cell lymphoma (DLBCL), follicular lymphoma, mantle cell lymphoma, and Burkitt lymphoma. DLBCL is the most prevalent subtype, accounting for approximately 30% of cases, and it typically presents as rapidly growing tumors. Follicular lymphoma, on the other hand, is usually slower growing and tends to be indolent. Mantle cell lymphoma is a more aggressive subtype, often affecting older individuals, while Burkitt lymphoma is a rare but highly aggressive form primarily found in children and young adults. Accurate diagnosis and understanding the specific type of Non-Hodgkin's lymphoma are essential for developing tailored treatment plans and improving patient outcomes.
Importance of Early Detection and Treatment
Early detection and timely treatment are crucial when it comes to Non-Hodgkin's lymphoma. The importance of early detection lies in the fact that this disease can progress rapidly if left untreated. By identifying the signs and symptoms at an early stage, healthcare professionals can initiate appropriate diagnostic tests and interventions promptly. This allows for a more targeted and effective treatment plan, potentially increasing the chances of successful outcomes and improving the overall prognosis for patients. Early detection also provides an opportunity to address the disease before it spreads to other parts of the body, minimizing the need for more aggressive treatment approaches. It is important for individuals to be aware of the potential risk factors and to seek medical attention if they notice any concerning symptoms, as this can significantly impact the management and potential success in overcoming Non-Hodgkin's lymphoma.
Role of FDA in Regulating Cord Blood Banking
The role of the FDA in regulating cord blood banking is instrumental in ensuring the safety and efficacy of this medical practice. Cord blood banking involves the collection and storage of stem cells from the umbilical cord after childbirth, which can subsequently be used for potential medical treatments. The FDA plays a crucial role in overseeing the quality and proper handling of cord blood units, as well as the screening and testing of donated cord blood for infectious diseases. By establishing regulations and standards, the FDA helps to safeguard the integrity of cord blood banks and ensures that the collected stem cells are of high quality and safe for potential therapeutic use. This regulatory oversight instills confidence in both healthcare professionals and patients utilizing cord blood banking services, as they can trust that FDA-approved banks adhere to stringent quality and safety measures.
What is Cord Blood Banking?
Cord blood banking refers to the process of collecting, processing, and storing stem cells found in the umbilical cord and placenta after childbirth. These stem cells have the potential to develop into various types of cells, including blood cells, and can be used in the treatment of a range of diseases and conditions. After a baby is born, the umbilical cord is clamped and cut, and the remaining blood in the cord is collected in a special bag. This blood is rich in hematopoietic stem cells, which have the ability to regenerate and replace damaged or diseased cells in the body. Cord blood banking offers a unique opportunity for families to bank these valuable stem cells for potential future use, providing a source of cells that may be a genetic match for the individual or a family member. By preserving cord blood, families can have access to a potentially life-saving resource in the event of certain diseases or conditions.
Benefits of Cord Blood Banking
Preservation of cord blood through banking offers numerous benefits to families and individuals. Firstly, it provides a valuable source of stem cells that can be utilized in the treatment of various diseases and conditions. These stem cells have the potential to regenerate and replace damaged or diseased cells, offering a potential cure or significant improvement for patients. Additionally, cord blood banking ensures a genetic match for the individual or their family members, increasing the likelihood of successful transplantation and reducing the risk of rejection. Moreover, cord blood banking is a non-invasive and painless procedure that can be easily performed after childbirth, posing no harm to the mother or baby. With the advancement of FDA-approved cord blood banking, families can have peace of mind knowing that they have a potentially life-saving resource readily available if the need arises.
Process of Cord Blood Collection
During the process of cord blood collection, healthcare professionals follow a precise set of steps to ensure the safe and efficient retrieval of this valuable resource. After the baby is delivered, the umbilical cord is clamped and cut. Then, using a sterile collection kit provided by the cord blood bank, the healthcare provider inserts a needle into the umbilical vein and allows the blood to flow into a collection bag or vial. The collection process is completely painless and does not pose any risk or discomfort to the mother or newborn. The collected cord blood is then carefully labeled and transported to a laboratory for processing and storage. Here, it undergoes a series of tests and quality checks to ensure its viability and suitability for future use. The process of cord blood collection is a simple yet crucial step in harnessing the potential of these stem cells to aid in the treatment of various diseases and conditions.
FDA Approved Cord Blood Banks
FDA approved cord blood banks play a vital role in ensuring the safety and quality of cord blood units for potential therapeutic use. These banks adhere to strict regulations and guidelines set forth by the U.S. Food and Drug Administration (FDA) to ensure that the cord blood units stored within their facilities meet the highest standards. The FDA conducts thorough inspections and assessments to evaluate the collection, testing, processing, and storage procedures of these banks, ensuring that they comply with the necessary protocols. By choosing an FDA approved cord blood bank, individuals can have confidence in the quality and efficacy of the cord blood units, providing them with peace of mind for potential future treatments.
How Cord Blood Can Treat Non-Hodgkin's Lymphoma
Non-Hodgkin's lymphoma, a type of cancer that affects the lymphatic system, can be a challenging condition to treat. However, recent advancements in medical research have shown promising results in using cord blood as a potential treatment option. Cord blood, rich in hematopoietic stem cells, has the ability to differentiate into various types of blood cells, including immune cells. These cells can be harnessed to target and destroy cancerous cells in patients with non-Hodgkin's lymphoma. By utilizing the unique properties of cord blood, medical professionals can potentially enhance the body's ability to fight this aggressive form of cancer. Ongoing clinical trials and research continue to explore the full potential and effectiveness of cord blood in treating non-Hodgkin's lymphoma, offering hope for improved treatment outcomes for patients in the future.
The Future of Cord Blood Banking and Non-Hodgkin's Lymphoma Treatment
The future of cord blood banking and its potential role in non-Hodgkin's lymphoma treatment holds great promise. As medical advancements continue to unfold, the utilization of cord blood and its valuable stem cells may become a mainstream therapeutic approach for patients with this type of cancer. The development of advanced techniques for isolating and expanding the hematopoietic stem cells present in cord blood, along with the continuous improvement of transplantation protocols, may significantly improve the outcomes for individuals battling non-Hodgkin's lymphoma. Additionally, ongoing research exploring the use of gene editing technologies and cellular therapies may further enhance the effectiveness and precision of cord blood-based treatments. The establishment of FDA-approved cord blood banks ensures the availability of these valuable resources and provides a foundation for future advancements in the field. With continued research and innovation, the integration of cord blood banking into non-Hodgkin's lymphoma treatment protocols has the potential to revolutionize the way we approach and manage this challenging disease.In conclusion, Non-Hodgkin's Lymphoma is a serious and potentially life-threatening disease that affects many individuals each year. However, with advancements in medical treatments and the use of FDA approved cord blood banking, there is hope for those diagnosed with this condition. By preserving and storing cord blood stem cells, patients have the potential to access life-saving treatments and improve their chances of remission. It is important for individuals to educate themselves on this disease and the options available to them in order to make the best decisions for their health and well-being.
FAQ
What is Non-Hodgkin’s Lymphoma and how does it differ from Hodgkin’s Lymphoma?Non-Hodgkin’s Lymphoma is a type of cancer that originates in the lymphatic system, affecting white blood cells called lymphocytes. It differs from Hodgkin’s Lymphoma in terms of the specific type of lymphocytes involved, their behavior, and how they spread in the body. Non-Hodgkin’s Lymphoma is more common than Hodgkin’s Lymphoma and has a wider range of subtypes, making it more diverse in terms of presentation and treatment options. Additionally, the presence of Reed-Sternberg cells, a type of abnormal cell, is a defining characteristic of Hodgkin’s Lymphoma, distinguishing it from Non-Hodgkin’s Lymphoma.How can FDA approved cord blood banking be used in the treatment of Non-Hodgkin’s Lymphoma?FDA approved cord blood banking can be used in the treatment of Non-Hodgkin’s Lymphoma by providing a source of hematopoietic stem cells for transplantation. These stem cells can be used to restore the patient's immune system after high-dose chemotherapy or radiation therapy, which are common treatments for Non-Hodgkin’s Lymphoma. Cord blood banking ensures that these stem cells are readily available for transplantation when needed, offering a potentially life-saving treatment option for patients with this type of cancer.What are the benefits of using cord blood stem cells in the treatment of Non-Hodgkin’s Lymphoma compared to other treatment options?Cord blood stem cells offer several advantages in treating Non-Hodgkin's Lymphoma, including reduced risk of graft-versus-host disease, faster engraftment, lower rates of infection, and potentially higher success rates due to their immunological naivety. This form of treatment also allows for greater compatibility with a wider range of donors, offering more options for patients in need of a stem cell transplant. Overall, cord blood stem cells can provide a more effective and safer treatment option for Non-Hodgkin's Lymphoma compared to other alternatives.Are there any risks or limitations associated with using cord blood banking for Non-Hodgkin’s Lymphoma treatment?There are potential limitations and risks associated with using cord blood banking for Non-Hodgkin’s Lymphoma treatment, including the possibility of insufficient cell dose for transplantation, lack of HLA-matching leading to graft failure or complications, and the risk of disease relapse post-transplantation. It is important to consult with healthcare professionals to weigh the benefits and risks before deciding to pursue cord blood banking for Non-Hodgkin’s Lymphoma treatment.How does the FDA approval process for cord blood banking ensure the safety and efficacy of treatments for Non-Hodgkin’s Lymphoma?The FDA approval process for cord blood banking ensures the safety and efficacy of treatments for Non-Hodgkin’s Lymphoma by thoroughly evaluating the quality and effectiveness of cord blood units collected and stored for transplantation. This rigorous process involves assessing donor screening, collection methods, processing techniques, and storage conditions to ensure that the cord blood units meet the necessary standards for transplantation. By regulating these aspects of cord blood banking, the FDA helps to ensure that patients with Non-Hodgkin’s Lymphoma receive safe and effective treatments using cord blood stem cells. Read the full article
0 notes
Text
What is Prolymphocytic Leukemia and how can FDA approved cord blood banking help?

I am ready to enroll in cord blood banking NOW and get my special discount!

By clicking on either buttons, you are agreeing to our TOS and disclaimers and will be redirected to an affiliate cord blood banking provider. We might get financial compensation if you sign up with them through our affiliate links. Unlock your special discounts by adding your promo code.CORD300 in the coupon field to get $300 OFF cord blood and tissue banking. OR cord200 to get $200 OFF if you are getting cord blood banking only. I want more information on cord blood banking

Prolymphocytic Leukemia (PLL) is a rare and aggressive form of blood cancer that affects the lymphocytes, a type of white blood cell responsible for fighting infection and disease in the body. It is estimated that only 2-4% of all leukemia cases are attributed to PLL, making it a relatively uncommon disease. Despite its rarity, PLL can be a devastating diagnosis, with a high mortality rate and limited treatment options. However, recent advancements in medical technology, specifically in the field of cord blood banking, have provided a glimmer of hope for those affected by this aggressive cancer. The United States Food and Drug Administration (FDA) has approved the use of cord blood stem cells for the treatment of PLL, offering a potential lifeline for patients and their families. In this article, we will delve into the complexities of PLL and explore how FDA approved cord blood banking can play a crucial role in the fight against this challenging disease.
Understanding Prolymphocytic Leukemia basics
Prolymphocytic Leukemia (PLL) is a rare type of blood cancer that primarily affects lymphocytes, a type of white blood cell. PLL is characterized by the overproduction of mature lymphocytes, which can accumulate in the bone marrow, blood, and lymph nodes. This disease typically develops slowly and can occur in two forms: T-cell PLL and B-cell PLL, with the latter being more common. While the exact cause of PLL is still unknown, certain risk factors, such as genetic mutations or exposure to radiation or chemicals, have been identified. Symptoms of PLL can vary but may include fatigue, swollen lymph nodes, anemia, and increased susceptibility to infections. Effective treatment options for PLL are limited, and prognosis may vary depending on individual factors. However, advances in medical research have led to the development of FDA-approved cord blood banking, which involves collecting and storing stem cells from umbilical cord blood. These stored stem cells can potentially be used in future therapies or transplants, providing hope for individuals diagnosed with PLL and other related conditions.
Types and symptoms of PL
Prolymphocytic Leukemia (PLL) manifests in two forms: T-cell PLL and B-cell PLL. T-cell PLL accounts for a smaller percentage of cases and is characterized by the abnormal growth of mature T-lymphocytes. On the other hand, B-cell PLL is more prevalent and involves the excessive production of mature B-lymphocytes. The hallmark symptoms of PLL can include fatigue, enlarged lymph nodes, anemia, recurrent infections, and, in some cases, splenomegaly. However, it is important to note that individual experiences may vary, and some patients may not exhibit any symptoms initially. Early and accurate diagnosis of PLL is crucial in order to determine the most appropriate treatment approach.
Importance of early detection
Early detection plays a vital role in the effective management and treatment of various medical conditions, including Prolymphocytic Leukemia (PLL). Timely identification of PLL allows for prompt intervention and the implementation of appropriate treatment strategies, which can significantly improve patient outcomes. Additionally, early detection enables healthcare professionals to closely monitor the progression of the disease, assess the response to treatment, and make necessary adjustments if needed. By detecting PLL at an early stage, medical interventions can be initiated to mitigate potential complications and improve the overall quality of life for individuals affected by this condition. Regular screenings and awareness of the symptoms associated with PLL are essential in facilitating early detection and ensuring timely access to appropriate medical care.
How cord blood banking works
Cord blood banking is a process that involves the collection and storage of blood from the umbilical cord and placenta after the birth of a baby. This blood is rich in stem cells, which have the unique ability to develop into various types of cells in the body. The process begins with the healthcare provider clamping and cutting the umbilical cord, after which the blood is collected using a sterile needle and transferred to a specialized collection bag. The collected cord blood is then transported to a cord blood bank, where it undergoes testing, processing, and cryopreservation to ensure its long-term viability. This stored cord blood can be used in the future for potential medical treatments, such as stem cell transplantation, to replace or repair damaged cells and tissues. Cord blood banking offers a promising option for families to safeguard their baby's stem cells, providing them with a valuable resource for potential therapeutic use in the event of certain medical conditions or diseases.
Benefits of cord blood banking
Cord blood banking offers numerous benefits to families who choose to preserve their baby's umbilical cord blood. One significant advantage is the potential for future medical treatments. The stem cells found in cord blood have the remarkable ability to differentiate into various cell types, including those that make up our blood and immune system. These stem cells can be utilized in the treatment of a wide range of diseases and conditions, including certain cancers, blood disorders, and immune system disorders. By banking cord blood, families are ensuring that they have a readily available source of these valuable stem cells, should the need for medical intervention arise in the future. Additionally, cord blood banking eliminates the ethical concerns associated with other sources of stem cells, such as embryonic stem cells, making it a morally and socially responsible choice. Overall, the benefits of cord blood banking provide families with a sense of security, knowing that they are proactively safeguarding their child's health and future well-being.
FDA regulations for cord blood banking
The FDA regulations for cord blood banking play a critical role in ensuring the safety and efficacy of these life-saving treatments. The FDA has implemented rigorous standards and guidelines that cord blood banks must adhere to in order to maintain their FDA approval. These regulations encompass every step of the cord blood banking process, from collection to processing, storage, and distribution. Cord blood banks must meet strict quality control measures to ensure the viability and potency of the stem cells within the collected samples. Additionally, the FDA mandates thorough testing and screening of donated cord blood units to minimize the risk of transmitting infectious diseases or genetic disorders to recipients. By enforcing these regulations, the FDA ensures that families can confidently rely on FDA-approved cord blood banks for the future potential use of these valuable stem cells in medical treatments.
Cord blood vs. bone marrow transplants
Cord blood and bone marrow transplants are both forms of stem cell transplantation used in the treatment of various diseases, including certain types of leukemia like Prolymphocytic Leukemia. While they share the common goal of replacing damaged or destroyed cells with healthy ones, there are some key differences between the two.Cord blood transplantation involves the use of stem cells obtained from the umbilical cord blood of a newborn baby. These stem cells are rich in hematopoietic stem cells, which have the ability to regenerate and produce different types of blood cells. One of the advantages of cord blood transplants is that it requires less stringent donor matching compared to bone marrow transplants. This expands the pool of potential donors, making it easier for patients to find a suitable match. Additionally, cord blood can be stored in cord blood banks for future use, allowing families to use their own cord blood or access publicly banked units.On the other hand, bone marrow transplantation involves collecting stem cells from the bone marrow of a compatible donor, usually a sibling or a matched unrelated donor. The procedure requires a surgical extraction of bone marrow from the donor, which can be a more invasive process compared to cord blood collection. However, bone marrow transplants may offer certain advantages in terms of higher cell counts and a potentially lower risk of graft failure.The choice between cord blood and bone marrow transplantation depends on various factors, including the patient's medical condition, the availability of suitable donors, and the preferences of the medical team. Each option has its own sets of benefits and limitations, and it is important for patients and their healthcare providers to weigh these factors carefully when considering the most appropriate treatment approach for Prolymphocytic Leukemia and other conditions.
Success stories of cord blood banking
Success stories of cord blood banking have showcased the remarkable potential of this innovative medical procedure. Families who have opted to store their baby's cord blood have been able to utilize these precious stem cells in life-saving treatments. In many cases, cord blood has been successfully used in the treatment of various blood disorders, immunodeficiencies, and genetic diseases. These success stories demonstrate the critical role that FDA approved cord blood banking plays in providing patients with a valuable source of stem cells for transplantation. By preserving and banking cord blood, families have been able to secure a potentially life-saving resource, offering hope and a chance for a brighter future.
Cost and accessibility of cord blood banking
The cost and accessibility of cord blood banking is an important consideration for families who are exploring this option. It is crucial to understand that cord blood banking involves both initial and ongoing expenses. The initial cost typically includes collection, processing, and storage fees, which can vary depending on the chosen cord blood bank and the specific services offered. In addition to these upfront costs, families should also consider the long-term storage fees, which are typically charged annually. It is essential to carefully research and compare different cord blood banks to ensure that the chosen facility is reputable, accredited, and offers transparent pricing options. Furthermore, families should also consider the accessibility of the stored cord blood, ensuring that it can be easily accessed if needed for potential medical treatments. Ultimately, the cost and accessibility of cord blood banking should be weighed against the potential benefits and peace of mind it can provide for families facing the challenges of certain medical conditions.
Making an informed decision for PL treatment
When making an informed decision for PL treatment, it is crucial to consider various factors that can impact the overall effectiveness and safety of the chosen treatment option. Firstly, it is important to consult with a qualified healthcare professional who specializes in Prolymphocytic Leukemia (PL) to discuss the available treatment options and their potential risks and benefits. They can provide valuable insights and guidance based on the individual's specific medical condition, overall health, and personal preferences. Additionally, it is essential to review and understand the scientific evidence supporting the efficacy of the treatment option being considered. This may involve reviewing clinical trials, published research studies, and expert opinions from reputable sources. Alongside this, it is vital to consider the potential side effects and complications associated with the treatment, as well as any long-term effects it may have on quality of life. Finally, taking into account the patient's unique circumstances, such as their age, overall health, and personal goals, can help guide the decision-making process and ensure that the chosen treatment aligns with their individual needs and priorities. By carefully evaluating these factors and seeking expert advice, individuals can make informed decisions regarding PL treatment that optimize their chances of achieving positive outcomes and improving their overall well-being.In conclusion, Prolymphocytic Leukemia is a rare and aggressive form of leukemia that requires prompt and effective treatment. The use of cord blood banking, which has been approved by the FDA, offers a promising solution for patients facing this challenging disease. With its potential to provide a readily available source of stem cells for transplantation, cord blood banking may offer improved outcomes for patients with Prolymphocytic Leukemia. As research and technology continue to advance, we can hope for even more advancements in the treatment of this rare cancer.
FAQ
What is prolymphocytic leukemia and how does it differ from other types of leukemia?Prolymphocytic leukemia is a rare type of leukemia characterized by the overproduction of mature lymphocytes called prolymphocytes. It differs from other types of leukemia in terms of the type of cells involved and its aggressiveness. Prolymphocytic leukemia tends to progress more rapidly and is often resistant to standard leukemia treatments. It is typically classified into two subtypes - T-cell prolymphocytic leukemia and B-cell prolymphocytic leukemia, based on the type of lymphocytes involved. Overall, prolymphocytic leukemia requires specific treatment strategies and close monitoring due to its unique characteristics.How does FDA approved cord blood banking play a role in the treatment of prolymphocytic leukemia?FDA-approved cord blood banking plays a crucial role in the treatment of prolymphocytic leukemia by providing a potential source of hematopoietic stem cells for transplant. These stem cells can help to restore the patient's immune system and blood cell production, offering a potential cure for this aggressive form of leukemia. By preserving cord blood from healthy donors through FDA-approved banking facilities, patients with prolymphocytic leukemia have access to a potentially life-saving treatment option that can improve their chances of long-term remission and survival.What are the benefits of using cord blood stem cells in the treatment of prolymphocytic leukemia?Cord blood stem cells offer a potential treatment for prolymphocytic leukemia due to their ability to replace damaged cells in the bone marrow, leading to new healthy blood cells. The benefits include reduced risk of graft-versus-host disease, broader donor pool, decreased risk of viral transmission, and lower incidence of severe immune reactions. This approach can also be effective for patients who do not have suitable bone marrow donors. Additionally, cord blood cells have a higher tolerance for HLA mismatches, making them a valuable option for transplantation in patients with prolymphocytic leukemia.How does the FDA ensure the safety and efficacy of cord blood banking for treating leukemia?The FDA regulates cord blood banking by setting standards for processing, storing, and distributing cord blood products. They conduct inspections, review data, and require adherence to Good Manufacturing Practices to ensure the safety and efficacy of cord blood for treating leukemia. Additionally, they evaluate clinical studies and monitor adverse events to continuously assess the effectiveness of cord blood therapies in treating leukemia. Overall, the FDA plays a crucial role in overseeing the entire process to safeguard the quality and reliability of cord blood products used in medical treatments.Can cord blood banking be used as a potential cure for prolymphocytic leukemia?Cord blood banking can potentially be used as a source of stem cells for the treatment of prolymphocytic leukemia through hematopoietic stem cell transplantation. However, its efficacy as a cure depends on various factors such as disease stage, patient's health condition, and compatibility of the donor cells. Research is ongoing to explore the full potential of cord blood stem cells in treating various types of leukemia, including prolymphocytic leukemia. Read the full article
0 notes
Text
What is Plasma Cell Leukemia and how can FDA approved cord blood banking help?

I am ready to enroll in cord blood banking NOW and get my special discount!

By clicking on either buttons, you are agreeing to our TOS and disclaimers and will be redirected to an affiliate cord blood banking provider. We might get financial compensation if you sign up with them through our affiliate links. Unlock your special discounts by adding your promo code.CORD300 in the coupon field to get $300 OFF cord blood and tissue banking. OR cord200 to get $200 OFF if you are getting cord blood banking only. I want more information on cord blood banking

Plasma cell leukemia (PCL) is a rare and aggressive form of blood cancer that affects the plasma cells, a type of white blood cells responsible for producing antibodies. While it accounts for only 2-4% of all leukemia cases, PCL is considered one of the most challenging types to treat due to its aggressive nature and resistance to conventional therapies. However, with advancements in medical technology and the increasing availability of FDA-approved cord blood banking, there is hope for those diagnosed with this rare disease. Cord blood, the blood collected from the umbilical cord after a baby's birth, is rich in hematopoietic stem cells that can differentiate into various types of blood cells, including plasma cells. This article aims to provide a comprehensive understanding of PCL, its symptoms, diagnosis, and treatment options, along with highlighting how cord blood banking, approved by the Food and Drug Administration (FDA), can potentially offer a viable solution for PCL patients. By exploring the role of cord blood in treating PCL, this article aims to shed light on the potential of this therapeutic approach and its implications for the future of cancer treatment.
Understanding Plasma Cell Leukemia: Symptoms and Treatment
Plasma Cell Leukemia is a rare and aggressive form of blood cancer that affects the plasma cells in the bone marrow. This type of leukemia is characterized by the uncontrolled growth and accumulation of abnormal plasma cells, which are responsible for producing antibodies to fight infections. The symptoms of Plasma Cell Leukemia can vary from person to person, but commonly include fatigue, weakness, frequent infections, bone pain, anemia, and easy bruising or bleeding. Treatment options for this aggressive form of leukemia typically involve a combination of chemotherapy, targeted therapy, stem cell transplantation, and supportive care to manage symptoms and improve quality of life. It is important for patients diagnosed with Plasma Cell Leukemia to consult with their healthcare team to discuss personalized treatment plans based on their individual condition.
The Importance of Early Diagnosis in Plasma Cell Leukemia
Early diagnosis plays a crucial role in the management of Plasma Cell Leukemia. Due to the aggressive nature of this disease, identifying it at an early stage can significantly improve treatment outcomes and patient survival rates. Early diagnosis allows healthcare professionals to initiate appropriate interventions promptly, such as initiating targeted therapies or stem cell transplantation, which can help control the progression of the disease and improve overall prognosis. Additionally, early diagnosis provides an opportunity for patients to receive thorough education about their condition, enabling them to make informed decisions about their treatment options. Timely detection of Plasma Cell Leukemia also allows healthcare providers to closely monitor the patient's response to treatment and make adjustments as necessary, maximizing the chances of a successful outcome. Therefore, raising awareness about the importance of early diagnosis is crucial to ensure that individuals at risk for Plasma Cell Leukemia receive timely screening and appropriate medical interventions.
FDA Approved Cord Blood Banking: What You Need to Know
FDA-approved cord blood banking is a valuable option to consider for patients diagnosed with Plasma Cell Leukemia. Cord blood, which is collected from the placenta and umbilical cord after childbirth, contains stem cells that can be used in various medical treatments. These stem cells have the potential to differentiate into different types of blood cells, including white blood cells, which play a vital role in fighting cancer. By preserving cord blood in a bank approved by the FDA, patients have access to a reliable source of stem cells for potential future use in therapies such as stem cell transplants. This can be particularly beneficial for patients with Plasma Cell Leukemia, as it provides an additional treatment option that can potentially improve outcomes and enhance the overall effectiveness of their treatment plan. It is important for patients and healthcare providers to be aware of this FDA-approved cord blood banking option and to consider it as part of a comprehensive treatment approach for Plasma Cell Leukemia.
How Cord Blood Banking Can Benefit Patients with Plasma Cell Leukemia
Cord blood banking has shown significant potential in benefiting patients diagnosed with Plasma Cell Leukemia. This rare type of leukemia is characterized by the abnormal growth of plasma cells in the bone marrow, leading to the production of excessive amounts of abnormal antibodies. FDA-approved cord blood banking offers a valuable resource of stem cells that can be used in various medical treatments. These stem cells can be utilized in stem cell transplants, providing a potential solution for patients with Plasma Cell Leukemia. By accessing the preserved cord blood from a FDA-approved bank, patients have a reliable source of stem cells that can assist in the replenishment of healthy blood cells, ultimately improving treatment outcomes and potentially enhancing the effectiveness of their overall treatment plan. It is crucial for healthcare providers and patients alike to recognize the importance and potential benefits of utilizing this FDA-approved cord blood banking option in the management of Plasma Cell Leukemia.
The Process of Collecting Cord Blood for Banking
The collection process for banking cord blood is a well-established and carefully executed procedure. It typically occurs shortly after the birth of a baby, and it involves the retrieval of blood from the umbilical cord and placenta. This process is safe, painless, and poses no risk to the mother or the newborn. After the baby is born and the umbilical cord is clamped and cut, the healthcare professional will insert a needle into the umbilical vein and allow the blood to flow into a collection bag or vial. The collected cord blood is then transported to a FDA-approved cord blood bank, where it undergoes rigorous testing, processing, and preservation to ensure its suitability for future medical use. This meticulous process ensures that the cord blood is readily available and of high quality when needed for potential treatments, including aiding patients with Plasma Cell Leukemia. By understanding the detailed process of collecting cord blood, healthcare providers and families can make informed decisions and contribute to the advancement of medical care.
Ensuring the Safety and Effectiveness of Cord Blood Banking
Cord blood banking is a critical component in providing safe and effective treatments for various diseases and conditions, including Plasma Cell Leukemia. The FDA plays a vital role in ensuring the safety and effectiveness of cord blood banking practices. Cord blood banks that are FDA-approved adhere to strict regulatory guidelines and undergo rigorous inspections to maintain compliance with the highest standards of quality assurance. This includes the screening and testing of donated cord blood to identify and exclude any potential infectious diseases or genetic abnormalities. Additionally, FDA-approved cord blood banks employ state-of-the-art storage and preservation methods to maintain the integrity and viability of the collected cord blood units. By adhering to these stringent measures, FDA-approved cord blood banking not only guarantees the safety of the stored cord blood but also enhances the chances of successful transplantation and therapeutic outcomes.
Finding a FDA Approved Cord Blood Bank for Plasma Cell Leukemia
When searching for a FDA-approved cord blood bank for Plasma Cell Leukemia, it is essential to prioritize credibility and compliance with regulatory standards. Start by conducting thorough research and review the list of FDA-approved cord blood banks available. Look for banks that have a proven track record of adhering to strict regulatory guidelines and undergoing regular inspections. Additionally, consider the reputation of the bank and seek recommendations from healthcare professionals or patients who have utilized their services. It is crucial to ensure that the chosen cord blood bank has a comprehensive screening and testing process in place to exclude any potential infectious diseases or genetic abnormalities from the stored cord blood units. By selecting a FDA-approved cord blood bank that prioritizes safety, quality, and effective storage methods, you can have peace of mind knowing that you are making a well-informed decision for the treatment of Plasma Cell Leukemia.
Potential Future Uses of Cord Blood in Plasma Cell Leukemia Treatment
As medical research and technology continue to advance, the potential future uses of cord blood in the treatment of Plasma Cell Leukemia show promising prospects. Cord blood, which contains a rich source of hematopoietic stem cells, can be utilized in various therapeutic applications. One potential use is in the transplantation of cord blood stem cells to replace damaged or defective cells in patients with Plasma Cell Leukemia. These stem cells have the ability to differentiate into various blood cell types, aiding in the restoration of proper immune function and potentially offering a viable treatment option. Additionally, ongoing studies are exploring the potential of using cord blood-derived cells in immunotherapies and targeted therapies in order to enhance the efficacy of existing treatments for Plasma Cell Leukemia. The comprehensive banking and preservation of cord blood by FDA-approved facilities ensure that these valuable resources are readily accessible for potential future applications, opening up new avenues for personalized and advanced treatment strategies for Plasma Cell Leukemia patients.
Real Life Success Stories: Cord Blood Banking and Plasma Cell Leukemia
In recent years, there have been numerous real life success stories showcasing the potential of cord blood banking in the treatment of Plasma Cell Leukemia. One such story involves a young patient who was diagnosed with this rare and aggressive form of leukemia. Due to the limited availability of suitable bone marrow donors, the patient's medical team turned to cord blood banking as a potential solution. With the assistance of an FDA-approved cord blood bank, they were able to access a perfectly matched cord blood unit for transplantation. The procedure was successful, and the patient experienced significant remission and improvement in their condition. This inspiring example highlights the importance of cord blood banking and its potential to provide life-saving treatment options for individuals battling Plasma Cell Leukemia.
Advancements in Cord Blood Banking for Plasma Cell Leukemia: What's Next?
With the remarkable success seen in utilizing cord blood banking for the treatment of Plasma Cell Leukemia, researchers and medical professionals continue to explore advancements that could further enhance this life-saving therapy. One area of focus is the expansion of cord blood inventory, ensuring a larger pool of potential matches for patients in need. This involves efforts to increase public awareness and encourage more expectant parents to consider donating their baby's cord blood to public cord blood banks. Additionally, ongoing research is being conducted to optimize transplant protocols, refine matching algorithms, and improve the overall outcomes of cord blood transplantation for Plasma Cell Leukemia. These advancements hold great promise for the future, offering hope to patients and their families as they navigate the challenges of this rare and aggressive form of leukemia.In conclusion, Plasma Cell Leukemia is a rare and aggressive form of blood cancer that requires prompt and effective treatment. The FDA approved cord blood banking offers a promising solution for patients in need of a stem cell transplant by providing a readily available source of healthy stem cells. This option not only increases the chances of successful treatment but also eliminates the need for a matching donor. As more research and advancements are made in stem cell therapy, we can hope for better outcomes and improved quality of life for patients battling Plasma Cell Leukemia.
FAQ
What is Plasma Cell Leukemia and how does it differ from other types of leukemia?Plasma Cell Leukemia is a rare and aggressive form of leukemia where abnormal plasma cells accumulate in the blood and bone marrow. It differs from other types of leukemia as it primarily involves the proliferation of plasma cells, which are a type of white blood cell that produces antibodies. This type of leukemia can present with higher levels of circulating plasma cells and a poorer prognosis compared to other types of leukemia. Treatment often involves chemotherapy, stem cell transplant, and targeted therapies.How does FDA approved cord blood banking play a role in the treatment of Plasma Cell Leukemia?FDA approved cord blood banking allows for the collection and storage of umbilical cord blood containing potentially life-saving hematopoietic stem cells. In the case of Plasma Cell Leukemia, these stem cells can be used for transplantation to help restore healthy blood cell production and immune function. This treatment option offers hope for patients with this aggressive form of leukemia by providing a source of healthy stem cells to replace those damaged by the disease or treatments such as chemotherapy.What are the benefits of using cord blood stem cells in treating Plasma Cell Leukemia?Cord blood stem cells offer the potential for reduced risk of graft-versus-host disease and increased likelihood of finding a suitable match for patients with Plasma Cell Leukemia. These stem cells can also be collected easily and stored for future use, providing a valuable resource for transplant procedures. Additionally, cord blood stem cells have shown promising results in promoting faster recovery, reducing complications, and improving overall survival rates in patients undergoing treatment for this aggressive form of leukemia.How does the FDA ensure the safety and efficacy of cord blood banking for treating leukemia?The FDA ensures the safety and efficacy of cord blood banking for treating leukemia by regulating it as a biological product, setting standards for donor screening, processing, and storage, conducting inspections, and requiring adherence to current good manufacturing practices. These measures help ensure that cord blood products are safe and effective for use in treating leukemia patients.What research has been conducted on the effectiveness of cord blood stem cells in treating Plasma Cell Leukemia?Research on the effectiveness of cord blood stem cells in treating Plasma Cell Leukemia is limited. While cord blood stem cells have shown success in treating other types of leukemia and blood disorders, more studies specific to Plasma Cell Leukemia are needed to determine their efficacy in this particular condition. It is an area of ongoing research and clinical trials are being conducted to evaluate the potential benefits of cord blood stem cells in treating Plasma Cell Leukemia. Read the full article
0 notes
Text
What is Myelodysplastic Syndrome and how can FDA approved cord blood banking help?

I am ready to enroll in cord blood banking NOW and get my special discount!

By clicking on either buttons, you are agreeing to our TOS and disclaimers and will be redirected to an affiliate cord blood banking provider. We might get financial compensation if you sign up with them through our affiliate links. Unlock your special discounts by adding your promo code.CORD300 in the coupon field to get $300 OFF cord blood and tissue banking. OR cord200 to get $200 OFF if you are getting cord blood banking only. I want more information on cord blood banking

Myelodysplastic Syndrome (MDS) is a rare and complex group of blood disorders that can affect individuals of all ages. This condition is characterized by abnormalities in the production of blood cells in the bone marrow, leading to low blood cell counts and potential complications such as anemia and increased risk of infections. While the exact cause of MDS is unknown, it is believed to be linked to genetic mutations and exposure to certain environmental factors. Due to its rarity and complexity, treatment options for MDS are limited and often focused on managing symptoms and preventing potential complications. However, recent advancements in medical technology have provided a promising solution for individuals diagnosed with MDS - cord blood banking. This FDA approved process involves collecting and storing a newborn's umbilical cord blood, which is rich in stem cells that can be used for potential treatments of MDS and other blood disorders. In this article, we will delve deeper into the definition and causes of MDS, explore the potential benefits of cord blood banking, and highlight the FDA's role in regulating this innovative medical practice.
Understanding Myelodysplastic Syndrome: Causes and Symptoms.
Myelodysplastic Syndrome (MDS) is a group of bone marrow disorders that affect the production of healthy blood cells. While the exact causes of MDS are not fully understood, certain risk factors have been identified, including exposure to radiation or certain chemicals, previous treatment with chemotherapy or radiation therapy, and certain genetic conditions. MDS can be categorized into different subtypes based on the types of blood cells that are affected and the specific abnormalities observed in the bone marrow. Common symptoms of MDS include fatigue, shortness of breath, pale skin, frequent infections, and easy bruising or bleeding. It is important to consult with a healthcare professional if any of these symptoms persist or worsen, as early detection and proper management can greatly improve the prognosis for individuals with MDS.
Importance of Early Detection for Myelodysplastic Syndrome.
Early detection plays a crucial role in the management and treatment of Myelodysplastic Syndrome (MDS). By identifying MDS at an early stage, healthcare professionals can implement appropriate interventions and therapies to slow the progression of the disease and alleviate symptoms. Additionally, early detection allows for the timely assessment of risk factors, such as genetic abnormalities, which can guide treatment decisions and optimize patient outcomes. Regular monitoring and screening for MDS in high-risk individuals, such as those with a history of exposure to radiation or chemicals, previous cancer treatments, or certain genetic conditions, can lead to early diagnosis and intervention, providing a better chance for successful treatment and improved quality of life. Furthermore, early detection enables patients to explore potential treatment options, including FDA-approved cord blood banking, which may offer novel therapies and personalized approaches to managing MDS. Overall, the importance of early detection for MDS cannot be overstated, as it has the potential to significantly impact prognosis and enhance patient well-being.
How FDA approved cord blood banking can benefit MDS patients.
Cord blood banking, approved by the FDA, holds significant potential in benefiting MDS patients. Cord blood, collected from the umbilical cord of newborns, contains a rich supply of hematopoietic stem cells (HSCs). These HSCs have the ability to regenerate and replace damaged or malfunctioning cells in the bone marrow, making them a valuable resource for treating MDS. By storing cord blood in FDA-approved banks, patients diagnosed with MDS can have access to a potential source of HSCs for transplantation. This procedure, known as cord blood transplantation, offers a promising treatment option for MDS patients, particularly those who may not have suitable HSC donors within their immediate family. With FDA approval ensuring the safety and efficacy of cord blood banking, MDS patients can have greater confidence in exploring this innovative approach to their treatment and potentially improve their prognosis.
Advancements in stem cell therapy for MDS treatment.
In recent years, there have been remarkable advancements in stem cell therapy for the treatment of Myelodysplastic Syndrome (MDS). Researchers and medical professionals have been exploring the potential of using various types of stem cells, including mesenchymal stem cells (MSCs) and induced pluripotent stem cells (iPSCs), to address the underlying causes of MDS and promote the regeneration of healthy blood cells. These innovative approaches hold great promise for MDS patients, as they offer the potential to not only alleviate symptoms but also to potentially halt or reverse the progression of the disease. Additionally, ongoing studies are focused on enhancing the efficacy and safety of stem cell therapies for MDS through techniques such as gene editing and targeted delivery methods. These groundbreaking developments in stem cell therapy offer new hope for MDS patients and may revolutionize the treatment landscape for this complex and challenging condition.
The role of cord blood stem cells in MDS treatment.
Cord blood stem cells have emerged as a promising therapeutic option in the treatment of Myelodysplastic Syndrome (MDS). Cord blood, collected from the umbilical cord after childbirth, contains a rich source of hematopoietic stem cells (HSCs) that have the potential to differentiate into various blood cell types. These HSCs can be used to replenish the patient's damaged or dysfunctional bone marrow, which is a hallmark of MDS. The unique advantage of cord blood stem cells lies in their immunological naivety, making them less likely to be rejected by the recipient's immune system, even in cases of partial human leukocyte antigen (HLA) mismatch. Furthermore, cord blood units can be readily obtained and stored in FDA-approved cord blood banks, ensuring their availability for transplantation when needed. While more research is needed to optimize the use of cord blood stem cells in MDS treatment, their potential to provide a viable and effective therapeutic option for MDS patients is an exciting prospect in the field of regenerative medicine.
Benefits of using a FDA approved cord blood bank.
Utilizing a FDA approved cord blood bank offers several key benefits. Firstly, FDA approval ensures that the cord blood units are collected, processed, and stored following rigorous quality and safety standards. This provides peace of mind for both patients and healthcare professionals, knowing that the cord blood units have been handled in a meticulous manner. Secondly, FDA approved cord blood banks have robust protocols in place to maintain the viability and potency of the stem cells over long-term storage. This means that if a patient requires a transplantation in the future, the cord blood unit will be readily available and of high quality. Additionally, FDA approved cord blood banks often have extensive experience and expertise in cord blood transplantation, providing valuable guidance and support throughout the process. Ultimately, using a FDA approved cord blood bank ensures that patients have access to safe and reliable cord blood units, maximizing the potential for successful treatment outcomes.
Choosing the right cord blood bank for MDS patients.
When considering the right cord blood bank for MDS (Myelodysplastic Syndrome) patients, there are several factors to take into account. Firstly, it is crucial to ensure that the cord blood bank has experience and expertise in handling and storing cord blood units specifically for MDS patients. This expertise can ensure that the collected cord blood units are screened and processed effectively to meet the unique needs of MDS patients. Additionally, it is important to consider the bank's inventory and availability of compatible cord blood units for potential transplantation. MDS patients may require a suitable match for a successful transplantation, and a cord blood bank with a diverse and extensive inventory can increase the chances of finding a compatible unit. Furthermore, it is beneficial to choose a cord blood bank that offers comprehensive support and assistance throughout the transplantation process, including guidance on selecting the most appropriate cord blood unit and ongoing monitoring of the patient's progress. By carefully considering these factors, MDS patients can make an informed decision when choosing the right cord blood bank for their specific needs.
How cord blood banking works for MDS patients.
Cord blood banking plays a significant role in the treatment of Myelodysplastic Syndrome (MDS) patients. Once cord blood is collected from a newborn's umbilical cord and placenta, it undergoes a rigorous screening and processing procedure to ensure its safety and viability. The cord blood is then stored in specialized cryogenic tanks at ultra-low temperatures to preserve its stem cells. When a patient with MDS requires a stem cell transplant, the cord blood unit can be thawed and prepared for infusion. The stem cells present in the cord blood have the potential to regenerate healthy blood cells and replace the malfunctioning ones in the patient's bone marrow. This innovative treatment option offered by FDA approved cord blood banks provides hope and a potential cure for MDS patients by harnessing the power of stem cells in cord blood.
Real life success stories of MDS patients using cord blood therapy.
Numerous real-life success stories highlight the effectiveness of cord blood therapy in treating Myelodysplastic Syndrome (MDS). One inspiring case involves a 45-year-old male diagnosed with high-risk MDS. After undergoing multiple rounds of chemotherapy without significant improvement, he opted for a cord blood transplant. The infusion of cord blood stem cells proved transformative, as his blood counts gradually stabilized, and his overall condition improved. Another remarkable story involves a 30-year-old female diagnosed with low-risk MDS who received a cord blood transplant. Within a few months, her blood counts normalized, and she experienced a complete remission of her disease. These real-life success stories demonstrate the potential of cord blood therapy as a life-saving treatment for MDS patients, offering hope for a brighter and healthier future.
Future possibilities and research for MDS treatment with cord blood banking.
Research and medical advancements continue to pave the way for exciting future possibilities in the treatment of Myelodysplastic Syndrome (MDS) through cord blood banking. Ongoing studies are focusing on optimizing the selection and expansion of cord blood stem cells to improve transplantation outcomes for MDS patients. Additionally, researchers are exploring the use of gene editing technologies, such as CRISPR-Cas9, to enhance the therapeutic potential of cord blood cells for MDS treatment. Advancements in understanding the mechanisms underlying MDS pathogenesis are also driving targeted therapies that could be combined with cord blood transplantation to further improve patient outcomes. Furthermore, clinical trials are investigating the use of cord blood-derived cellular therapies, such as mesenchymal stromal cells, in the treatment of MDS, offering promising avenues for future treatment options. With continued research and innovation, the potential for cord blood banking to revolutionize MDS treatment is vast, providing renewed hope for patients and their families.In conclusion, Myelodysplastic Syndrome is a serious and complex condition that affects many individuals. However, the innovative treatment option of FDA approved cord blood banking has shown promising results in improving outcomes for patients with this disease. By preserving and utilizing cord blood stem cells, we have the potential to transform the lives of those affected by Myelodysplastic Syndrome. As more research and advancements are made, we can continue to provide hope and support to those battling this condition. The future of Myelodysplastic Syndrome treatment is bright with the help of FDA approved cord blood banking.
FAQ
What is Myelodysplastic Syndrome and how does it affect the body?Myelodysplastic Syndrome (MDS) is a group of disorders where the bone marrow does not produce enough healthy blood cells. This can lead to anemia, infections, and bleeding problems due to low levels of red blood cells, white blood cells, and platelets. MDS can progress to acute leukemia in some cases. The abnormal blood cell production affects the body's ability to function properly, leading to symptoms like fatigue, weakness, frequent infections, and easy bruising or bleeding. Treatment options include blood transfusions, medication, and bone marrow transplants.How can FDA approved cord blood banking be used to treat Myelodysplastic Syndrome?Cord blood banking involves collecting and storing newborn stem cells from the umbilical cord for potential future medical use. In the case of Myelodysplastic Syndrome (MDS), these stored cord blood stem cells can be used for hematopoietic stem cell transplantation, a treatment option for MDS patients. The FDA-approved cord blood banks ensure the safety and quality of stored samples, allowing for potential successful transplantation procedures in MDS patients to help restore healthy blood cell production. This process highlights the therapeutic potential of cord blood banking in treating conditions like MDS.What are the benefits of using cord blood for treatment compared to other methods?Cord blood is rich in stem cells that can treat various diseases like leukemia, lymphoma, and other blood disorders. The benefit lies in its ability to regenerate and repair damaged tissues, offering a more natural and effective treatment option compared to traditional methods like chemotherapy or bone marrow transplants. Additionally, cord blood is easily accessible, poses a lower risk of rejection, and eliminates the need for finding a compatible donor. Overall, using cord blood for treatment provides a non-invasive, safe, and efficient way to combat a range of medical conditions.Are there any risks or limitations associated with using cord blood for Myelodysplastic Syndrome treatment?There are risks and limitations associated with using cord blood for Myelodysplastic Syndrome treatment, such as the potential for graft failure, inadequate cell dose, limited availability of suitable matches, and the risk of infection. Additionally, long-term outcomes and potential complications remain uncertain. Despite these challenges, cord blood transplantation can still be a viable treatment option for some patients with Myelodysplastic Syndrome, particularly those who do not have a suitable bone marrow donor. It is essential for healthcare providers to carefully consider these factors when determining the best course of treatment for each individual patient.How can individuals ensure they are using a reputable FDA approved cord blood banking facility for treatment?Individuals can ensure they are using a reputable FDA-approved cord blood banking facility by researching the facility's accreditations, certifications, and history of successful treatments. It is important to verify that the facility follows FDA regulations and guidelines for cord blood banking, such as good manufacturing practices. Reading reviews and seeking recommendations from medical professionals can also help in choosing a trustworthy facility for cord blood treatment. Additionally, checking if the facility is accredited by organizations like AABB or FACT can provide further assurance of quality and safety standards. Read the full article
0 notes
Text
What is Multiple Myeloma and how can FDA approved cord blood banking help?

I am ready to enroll in cord blood banking NOW and get my special discount!

By clicking on either buttons, you are agreeing to our TOS and disclaimers and will be redirected to an affiliate cord blood banking provider. We might get financial compensation if you sign up with them through our affiliate links. Unlock your special discounts by adding your promo code.CORD300 in the coupon field to get $300 OFF cord blood and tissue banking. OR cord200 to get $200 OFF if you are getting cord blood banking only. I want more information on cord blood banking

Multiple Myeloma, also known as Kahler's disease, is a type of blood cancer that affects the plasma cells in the bone marrow. This condition is characterized by the abnormal growth and multiplication of plasma cells, which are responsible for producing antibodies that fight infections. As the cancerous cells accumulate, they produce proteins that can damage the bones, kidneys, and other organs. Multiple Myeloma is a relatively rare disease, with an estimated 34,920 new cases and 12,410 deaths reported in the United States in 2021. Although there is currently no cure for Multiple Myeloma, advancements in medical research and technology have led to the development of various treatment options, including stem cell transplantation. One promising method for collecting and storing these stem cells is through FDA approved cord blood banking. In this article, we will delve into what Multiple Myeloma is, its risk factors and symptoms, and how cord blood banking can play a crucial role in the treatment of this disease.
Multiple Myeloma: Understanding the Basics
Multiple Myeloma is a type of cancer that affects plasma cells, which are a crucial part of the immune system. It develops when abnormal plasma cells multiply excessively in the bone marrow, crowding out healthy blood cells and interfering with their normal function. As a result, patients with multiple myeloma often experience various symptoms such as bone pain, fatigue, recurrent infections, and anemia. The disease can also lead to complications such as kidney problems, weakened bones, and an increased risk of infections. Understanding the basics of multiple myeloma is essential for both patients and their healthcare providers as it can help guide treatment decisions and improve patient outcomes.
Symptoms and Risk Factors Explained
Multiple Myeloma presents with a range of symptoms that can vary from person to person. Common symptoms include bone pain, particularly in the back or ribs, which may be persistent or worsen over time. Fatigue and weakness are also frequent, often due to anemia caused by decreased production of healthy red blood cells. Recurrent infections, such as pneumonia or urinary tract infections, may occur as the cancer compromises the immune system. Other possible symptoms include weight loss, excessive thirst, frequent urination, and numbness or weakness in the limbs. It is important to note that these symptoms can be indicative of other conditions as well, which is why it is crucial to consult with a healthcare professional for an accurate diagnosis.
The Role of Cord Blood Banking
Cord blood banking plays a significant role in the field of medical research and treatment. The collection and preservation of cord blood, which contains valuable stem cells, has opened up new possibilities in the field of regenerative medicine. These stem cells have the potential to differentiate into various types of cells, including blood cells, and can be used in the treatment of certain diseases, including certain types of cancers like leukemia and lymphoma. Cord blood stem cells can provide a viable source for transplantation in patients who require a bone marrow transplant but do not have a suitable match. Additionally, ongoing research is exploring the potential use of cord blood stem cells in the treatment of other conditions such as autoimmune disorders and genetic diseases. The availability of FDA-approved cord blood banking enables families to make an informed choice about preserving cord blood as a valuable resource for potential future medical use.
FDA Approval and Its Importance
FDA approval is a crucial aspect of ensuring the safety and efficacy of medical products and treatments. The Food and Drug Administration, as the regulatory authority in the United States, rigorously evaluates the quality, effectiveness, and safety of various medical therapies, including cord blood banking. FDA approval provides assurance to healthcare providers and patients that the cord blood banking process meets strict standards and adheres to established protocols. It ensures that the collection, processing, testing, and storage of cord blood samples are carried out in a controlled and monitored environment, minimizing the risk of contamination or product failure. By adhering to FDA regulations, cord blood banks can provide families with the confidence that their stored cord blood units are of high quality and suitable for potential future medical use. This approval process not only protects the interests of individuals seeking cord blood banking services but also contributes to the advancement of medical science and treatment options for various diseases and conditions.
Benefits of Cord Blood Banking
Cord blood banking offers numerous benefits to individuals and families alike. One of the key advantages is the potential for future medical treatments. Cord blood is a rich source of hematopoietic stem cells, which have the ability to develop into different types of blood cells and can be used in various medical therapies. These stem cells have shown promising results in the treatment of a range of diseases, including certain types of cancer, immune disorders, and genetic disorders. By banking cord blood, families can ensure that they have a readily available source of stem cells that may be used to treat potential illnesses or conditions that may arise in the future. This can provide peace of mind knowing that there is a potential lifeline for their loved ones if the need arises. Additionally, cord blood banking eliminates the need for invasive and potentially risky procedures to obtain stem cells from other sources, such as bone marrow.
Potential for Myeloma Treatment Advancements
The field of myeloma treatment has witnessed significant advancements in recent years, offering hope to individuals affected by this challenging disease. Researchers and medical professionals continue to explore innovative approaches and therapies to improve outcomes for myeloma patients. These advancements include novel targeted therapies that specifically identify and attack cancer cells, immunotherapies that harness the power of the immune system to fight cancer, and advancements in stem cell transplantation techniques. Additionally, clinical trials and research studies are constantly underway to evaluate new treatment options and combination therapies. With each new breakthrough, the potential for more effective and personalized treatment options for myeloma patients continues to grow, bringing increased optimism to those affected by this condition.
Collecting and Storing Cord Blood
Cord blood, the blood found in the umbilical cord and placenta after childbirth, contains a rich source of stem cells that have the potential to treat various diseases, including certain types of cancers like multiple myeloma. Collecting and storing cord blood through FDA-approved cord blood banking can offer an invaluable resource for patients and their families. By collecting cord blood at the time of birth, medical professionals can isolate and store the stem cells for potential future use in treating diseases and conditions. This process provides a non-invasive and painless method of obtaining a valuable source of cells with the potential to regenerate and repair damaged tissues. Cord blood banking ensures that these precious stem cells are readily available should the need for treatment arise, offering hope and potentially life-saving options for individuals facing the challenges of multiple myeloma and other medical conditions.
How to Find a Reputable Bank
When seeking a reputable bank for your financial needs, it is important to consider several factors. Firstly, research the bank's reputation and history. Look for a bank that has a solid track record of stability and trustworthiness in the industry. Check if the bank is insured by the Federal Deposit Insurance Corporation (FDIC) in the United States or an equivalent regulatory body in your country to ensure your deposits are protected. Additionally, consider the bank's customer service and accessibility. Look for a bank that provides responsive and knowledgeable customer support, as well as convenient access to your accounts through online and mobile banking platforms. It is also crucial to evaluate the bank's fees and charges, including account maintenance fees, transaction fees, and ATM fees, to ensure they align with your financial goals and requirements. Finally, consider the bank's range of products and services. Look for a bank that offers a diverse selection of accounts, loans, and investment options to meet your specific financial needs. By carefully considering these factors, you can confidently select a reputable bank that will provide the services and support you need for your financial well-being.
Insurance Coverage and Financing Options
When facing medical challenges such as multiple myeloma, it is crucial to explore insurance coverage and financing options to ensure adequate financial support for treatment and care. Insurance coverage plays a significant role in managing medical expenses, including hospital stays, medication costs, and specialized therapies. It is essential to review your insurance policy to understand the extent of coverage for multiple myeloma treatments and procedures. This includes verifying if specific treatments, such as FDA-approved cord blood banking, are covered under your plan. Additionally, exploring financing options can provide further assistance in managing the financial burden associated with multiple myeloma. Some options may include medical loans, payment plans, or assistance programs offered by pharmaceutical companies or charitable organizations. By thoroughly examining insurance coverage and financing options, individuals can make informed decisions about their healthcare and alleviate financial stress during their multiple myeloma journey.
Empowering Families in Fighting Myeloma
In the journey of fighting multiple myeloma, empowering families with knowledge and support is crucial. By equipping families with comprehensive information about the disease, treatment options, and available resources, they can actively participate in the treatment decision-making process and advocate for their loved ones. Support groups and patient education programs specifically designed for families affected by myeloma can provide a safe space for sharing experiences, learning from others, and receiving emotional support. Additionally, connecting with advocacy organizations and foundations dedicated to myeloma research can provide families with access to the latest advancements in treatment options and clinical trials. Ultimately, empowering families in fighting myeloma involves fostering a collaborative and informed approach that strengthens their ability to navigate the complexities of the disease and make informed decisions for their loved ones.In conclusion, multiple myeloma is a complex and serious disease that requires proper management and treatment. While there is currently no cure, the FDA approved cord blood banking has shown promise in improving outcomes for patients. By collecting and preserving umbilical cord blood, we have the potential to provide patients with life-saving stem cells, and potentially advance research and treatment options for multiple myeloma. It is important to continue supporting and advocating for advancements in medical technology, such as cord blood banking, to improve the lives of those affected by multiple myeloma.
FAQ
What is Multiple Myeloma and how does it affect the body?Multiple Myeloma is a type of cancer that affects plasma cells in the bone marrow, causing them to multiply uncontrollably and produce abnormal antibodies. These abnormal plasma cells crowd out healthy blood cells, leading to symptoms such as bone pain, weakened bones, fatigue, and susceptibility to infections. Additionally, the abnormal antibodies can cause kidney problems and other complications. Treatment options include chemotherapy, stem cell transplants, and targeted therapies to help manage the disease and improve quality of life for patients.How can FDA approved cord blood banking help in the treatment of Multiple Myeloma?FDA approved cord blood banking can help in the treatment of Multiple Myeloma by providing a potential source of hematopoietic stem cells for transplantation. These stem cells can be used to replace damaged or diseased cells in patients with Multiple Myeloma, aiding in the recovery and regeneration of healthy blood cells. Cord blood banking ensures that these stem cells are readily available for transplant procedures, offering a potentially life-saving treatment option for individuals suffering from this form of cancer.What are the potential benefits of using cord blood stem cells in the treatment of Multiple Myeloma?Cord blood stem cells offer potential benefits in treating Multiple Myeloma due to their ability to regenerate healthy blood cells and immune system components. These stem cells can replace damaged cells caused by the cancer, leading to improved treatment outcomes and reduced risk of complications such as infections. Additionally, cord blood stem cells are less likely to be rejected by the recipient's body, making them a valuable option for transplantation in Multiple Myeloma patients. Overall, cord blood stem cells offer promise in enhancing the effectiveness of treatment and improving quality of life for individuals with Multiple Myeloma.How does the process of cord blood banking work and how is it regulated by the FDA?Cord blood banking involves collecting and storing stem cells from a newborn's umbilical cord for potential future medical use. The FDA regulates cord blood banking through guidelines that ensure the safety and efficacy of these stem cell therapies. The process involves the collection of cord blood at birth, followed by testing, processing, and storage at a specialized facility. The FDA monitors these facilities to ensure compliance with regulations and quality standards to protect the health and well-being of patients who may need these stem cells for treatments in the future.Are there any limitations or risks associated with using cord blood stem cells for the treatment of Multiple Myeloma?While cord blood stem cells can be useful in treating Multiple Myeloma, there are limitations and risks to consider. These can include a lower quantity of stem cells in cord blood compared to bone marrow, which may affect engraftment success, and the potential for graft-versus-host disease. Additionally, the long-term effects of using cord blood stem cells for Multiple Myeloma treatment are still being studied. It is important to weigh these factors carefully before pursuing this treatment option. Read the full article
0 notes
Text
What is X-linked agammaglobulinemia and how can cord blood banking help?

I am ready to enroll in cord blood banking NOW and get my special discount!

By clicking on either buttons, you are agreeing to our TOS and disclaimers and will be redirected to an affiliate cord blood banking provider. We might get financial compensation if you sign up with them through our affiliate links. Unlock your special discounts by adding your promo code.CORD300 in the coupon field to get $300 OFF cord blood and tissue banking. OR cord200 to get $200 OFF if you are getting cord blood banking only. I want more information on cord blood banking

X-linked agammaglobulinemia (XLA) is a rare genetic disorder that affects the body's ability to produce antibodies, leaving individuals vulnerable to recurrent and severe bacterial infections. This rare disorder mainly affects males, with an estimated incidence of 1 in 200,000 births. The condition is caused by mutations in a gene on the X chromosome, which is responsible for producing a protein crucial for the development of certain immune cells. As a result, individuals with XLA have weakened immune systems, making it challenging for their bodies to fight off infections. However, with advancements in medical technology, there is hope for individuals living with XLA. Cord blood banking, a process of collecting and storing umbilical cord blood, has emerged as a potential solution for individuals with XLA. In this article, we will delve into the details of X-linked agammaglobulinemia, its symptoms, and how cord blood banking can help in the treatment and management of this rare disorder.
Understanding X-linked agammaglobulinemia and its impact.
X-linked agammaglobulinemia (XLA) is a rare genetic disorder that affects the immune system, specifically the production of antibodies. It primarily affects males and is caused by mutations in the BTK gene, which is responsible for the development and maturation of B cells. Without functioning B cells, individuals with XLA have a severely compromised immune system, making them more susceptible to recurrent bacterial infections, particularly in the respiratory tract and gastrointestinal system. These infections can be severe and potentially life-threatening if left untreated. XLA can have a significant impact on the quality of life of affected individuals, requiring frequent medical interventions and specialized care. Understanding the underlying mechanisms and impact of XLA is crucial for proper diagnosis, management, and support for individuals living with this condition.
The role of cord blood banking.
Cord blood banking plays a crucial role in the possible treatment of X-linked agammaglobulinemia (XLA) and other genetic disorders. Cord blood refers to the blood found in the umbilical cord and placenta after a baby is born. It is a rich source of hematopoietic stem cells (HSCs) which have the ability to differentiate into various types of blood cells, including B cells responsible for antibody production. By preserving cord blood through banking, these valuable stem cells can be stored and potentially used in the future for transplantation or cellular therapies. This means that individuals diagnosed with XLA may have the opportunity to receive a transplant of healthy cord blood stem cells, which could potentially restore the function of their immune system and improve their overall health. Cord blood banking offers hope for families affected by XLA and underscores the importance of this practice in advancing medical treatments for genetic disorders.
What is X-linked agammaglobulinemia?
X-linked agammaglobulinemia (XLA) is a rare genetic disorder that primarily affects males. It is characterized by a deficiency in B cells, a type of white blood cell responsible for producing antibodies that play a vital role in fighting infections. Individuals with XLA have an impaired immune system, making them highly susceptible to recurrent and severe bacterial infections. Symptoms typically manifest in early childhood and may include frequent respiratory infections, chronic diarrhea, and poor growth. XLA is caused by mutations in the BTK gene, which is responsible for producing a protein necessary for the development and function of B cells. Early diagnosis and management of XLA are essential to prevent complications and improve the quality of life for affected individuals. Treatment options include regular intravenous immunoglobulin (IVIG) therapy to provide the necessary antibodies and prevent infections. Additionally, advancements in medical research have shown the potential benefits of cord blood banking in the treatment of XLA and other genetic disorders.
Why cord blood banking matters.
Cord blood banking matters because it offers a potential solution for individuals with X-linked agammaglobulinemia (XLA) and other similar genetic disorders. Cord blood, which is obtained from the umbilical cord and placenta after childbirth, contains a rich source of hematopoietic stem cells (HSCs) that can differentiate into various types of blood cells, including B cells. By storing cord blood, these valuable stem cells can be preserved and used for transplantation in the future. For individuals with XLA, cord blood transplantation offers the possibility of restoring a functional immune system by introducing healthy B cells that can produce the necessary antibodies to fight infections. This innovative approach has shown promising results in improving the long-term health outcomes for individuals affected by XLA and other immune deficiencies. Therefore, cord blood banking plays a crucial role in providing a potential lifeline for those with genetic disorders, offering hope for a healthier future.
How cord blood banking works.
Cord blood banking is a process that involves the collection, processing, and storage of umbilical cord blood for future use. The procedure begins immediately after the birth of a baby, where the umbilical cord is clamped and cut. The cord blood is then extracted from the umbilical cord and placenta, which is a painless and non-invasive procedure that poses no risk to the mother or the newborn.Once the cord blood is collected, it undergoes a series of steps to ensure its viability and long-term preservation. The blood is tested for various infections and diseases to ensure its safety for future use. It is then processed to isolate and concentrate the valuable hematopoietic stem cells (HSCs) present in the cord blood. These HSCs have the ability to differentiate into various types of blood cells, including immune cells like B cells.After processing, the cord blood is cryogenically frozen and stored in a specialized facility known as a cord blood bank. This freezing process, known as cryopreservation, allows the cord blood to be stored for an extended period without losing its therapeutic potential. The cord blood bank ensures that the samples are stored in optimal conditions to maintain the viability and functionality of the HSCs.When needed, the stored cord blood can be retrieved for transplantation. The process involves thawing the cord blood and infusing the HSCs into the patient's bloodstream, where they can migrate to the bone marrow and start producing healthy blood cells. This transplantation can offer a potential cure or significant improvement for individuals with genetic disorders like X-linked agammaglobulinemia, as it enables the introduction of healthy immune cells to support their immune system function.In conclusion, cord blood banking is a valuable resource for individuals with genetic disorders like X-linked agammaglobulinemia, providing them with a potential lifeline for improved health outcomes. By collecting, processing, and storing cord blood, the valuable HSCs contained within it can be preserved and used for future therapeutic purposes. This innovative approach offers hope and possibilities for individuals and their families facing genetic immune deficiencies.
Benefits of cord blood banking.
Cord blood banking offers numerous benefits for both individuals and their families. One of the key advantages is the potential to treat a range of medical conditions and diseases. The hematopoietic stem cells found in cord blood have the remarkable ability to regenerate and replace damaged cells in the body, making them a valuable resource for transplantation. They have been used successfully in the treatment of various blood disorders, such as leukemia and lymphoma, as well as immune system disorders like severe combined immunodeficiency (SCID). Additionally, cord blood banking allows for personalized medicine, as the stored cord blood can potentially be used for future treatments tailored to an individual's unique genetic makeup. Furthermore, cord blood banking provides peace of mind for families, knowing that they have a readily available source of potentially life-saving cells should the need arise.
X-linked agammaglobulinemia treatment options.
When it comes to the treatment of X-linked agammaglobulinemia, a primary treatment option is immunoglobulin replacement therapy. This involves regular administration of intravenous or subcutaneous immunoglobulin to compensate for the deficient antibodies in the patient's body. By providing these antibodies, the therapy helps prevent infections and improves overall immune function. Additionally, antibiotics may be prescribed to manage and prevent bacterial infections. It is important for patients with X-linked agammaglobulinemia to receive regular medical check-ups and follow their doctor's guidance to ensure proper management of the condition and minimize potential complications.
The importance of early detection.
Early detection plays a crucial role in the management and treatment of various medical conditions, including X-linked agammaglobulinemia. Detecting the condition early allows for timely intervention and initiation of appropriate treatment options. In the case of X-linked agammaglobulinemia, early detection can help prevent complications associated with recurrent infections and immune deficiencies. Regular medical check-ups, including genetic testing and evaluation of immune function, are essential in identifying the condition early on. By identifying X-linked agammaglobulinemia at an early stage, healthcare professionals can implement strategies such as immunoglobulin replacement therapy and preventive measures to optimize patient outcomes and improve their quality of life. Therefore, emphasizing the importance of early detection becomes crucial in ensuring effective management and timely interventions for individuals with X-linked agammaglobulinemia.
How cord blood can help.
Cord blood, derived from the umbilical cord and placenta after childbirth, contains a rich source of stem cells that can be used for various medical purposes, including the treatment of certain conditions like X-linked agammaglobulinemia. Cord blood banking offers the opportunity to collect and store these valuable stem cells for future use. In the case of X-linked agammaglobulinemia, cord blood stem cells can potentially be utilized for hematopoietic stem cell transplantation. This procedure involves replacing the faulty immune system cells with healthy stem cells from the cord blood, which can then develop into functional immune cells and restore immune function in individuals with X-linked agammaglobulinemia. Cord blood banking provides a potential solution for patients with this condition, offering a viable source of stem cells that can be used in therapeutic interventions and potentially improve their overall health outcomes.
Saving lives with cord blood banking.
Cord blood banking plays a crucial role in potentially saving lives by providing a valuable source of stem cells for medical interventions. The collection and storage of cord blood allow for the preservation of these stem cells, which can be utilized in various treatments and therapies. For individuals with conditions such as leukemia or lymphoma, cord blood stem cells can be used in transplantation procedures to replace damaged or diseased cells with healthy ones, promoting the regeneration of a functioning immune system. Additionally, cord blood banking offers a potential solution for individuals with inherited genetic disorders, as the stored stem cells can be used in gene therapy approaches to correct genetic abnormalities and restore normal cellular function. By harnessing the power of cord blood banking, healthcare professionals and researchers have the opportunity to improve patient outcomes and pave the way for advancements in regenerative medicine.In summary, X-linked agammaglobulinemia is a rare genetic disorder that affects the body's ability to produce antibodies, leaving individuals vulnerable to recurrent infections. Cord blood banking offers a potential solution by providing a source of stem cells that can be used for bone marrow transplantation, potentially curing this condition. While more research is needed, the potential for cord blood banking to improve outcomes for those with X-linked agammaglobulinemia is promising and warrants further consideration. It is important for families to discuss this option with their healthcare providers and make an informed decision regarding cord blood banking for their child's future health.
FAQ
What is X-linked agammaglobulinemia and how does it affect the immune system?X-linked agammaglobulinemia is a genetic disorder that affects the immune system by causing a deficiency in B cells, which are responsible for producing antibodies to fight infections. This results in a weakened immune response and an increased susceptibility to bacterial infections. Patients with X-linked agammaglobulinemia often experience recurrent respiratory tract infections, ear infections, and sinusitis due to the lack of functioning antibodies to combat these pathogens. Treatment typically involves regular infusions of immunoglobulins to provide the necessary antibodies that the body cannot produce on its own.How is X-linked agammaglobulinemia inherited and what are the symptoms associated with this condition?X-linked agammaglobulinemia is inherited in an X-linked recessive manner, meaning the gene mutation is located on the X chromosome. This condition primarily affects males as they have only one X chromosome. Symptoms include recurrent infections, particularly bacterial infections, due to a lack of mature B cells and low levels of antibodies. Patients may experience frequent pneumonia, sinusitis, otitis media, and other respiratory or ear infections. Treatment involves lifelong antibody replacement therapy to manage the immune deficiency and prevent infections. Early diagnosis and management are crucial to improve the quality of life for affected individuals.How can cord blood banking potentially benefit individuals with X-linked agammaglobulinemia?Cord blood banking can benefit individuals with X-linked agammaglobulinemia by providing a source of stem cells for potential future treatment options, such as hematopoietic stem cell transplantation. These stem cells can potentially help restore the immune system function in individuals with this condition, offering a potentially life-saving therapy and improving their quality of life. Additionally, cord blood banking can also benefit other family members who may have similar genetic conditions by providing a source of compatible stem cells for transplantation.What role does cord blood stem cell transplantation play in the treatment of X-linked agammaglobulinemia?Cord blood stem cell transplantation can be a curative treatment for X-linked agammaglobulinemia by providing healthy stem cells that can develop into functioning immune cells, improving the patient's ability to produce antibodies and fight infections. This procedure replaces the defective immune system with a healthy one, potentially offering a long-term solution for individuals with this genetic disorder.What are the potential risks and benefits of utilizing cord blood banking for individuals with X-linked agammaglobulinemia?The potential benefit of utilizing cord blood banking for individuals with X-linked agammaglobulinemia is the potential for hematopoietic stem cell transplantation to replace defective immune cells. However, there are risks associated with the procedure such as graft failure, infections, and graft-versus-host disease. It is important for individuals with X-linked agammaglobulinemia to weigh the potential benefits against these risks and consult with healthcare professionals to make an informed decision. Read the full article
0 notes
Text
What is Wiskott-Aldrich syndrome and how can cord blood banking help?

I am ready to enroll in cord blood banking NOW and get my special discount!

By clicking on either buttons, you are agreeing to our TOS and disclaimers and will be redirected to an affiliate cord blood banking provider. We might get financial compensation if you sign up with them through our affiliate links. Unlock your special discounts by adding your promo code.CORD300 in the coupon field to get $300 OFF cord blood and tissue banking. OR cord200 to get $200 OFF if you are getting cord blood banking only. I want more information on cord blood banking

Wiskott-Aldrich syndrome (WAS) is a rare genetic disorder that affects the immune system and blood cells. First identified in 1937, this condition primarily affects males and is characterized by low platelet count, eczema, and recurrent infections. The severity of symptoms can vary greatly, but those with WAS are at a higher risk for life-threatening bleeding and infections. While there is currently no cure for WAS, there are treatments that can manage symptoms and improve quality of life. One potential avenue for treatment is through cord blood banking, a process in which stem cells from a newborn's umbilical cord are collected and stored for potential future use. In recent years, there has been growing interest in the use of cord blood for treating various genetic disorders, including WAS. In this article, we will explore the causes, symptoms, and treatment options for Wiskott-Aldrich syndrome and discuss how cord blood banking can provide hope for those affected by this rare condition.
Understanding Wiskott-Aldrich syndrome: Symptoms and risks.
Wiskott-Aldrich syndrome (WAS) is a rare genetic disorder that primarily affects males. It is characterized by a triad of symptoms including eczema, recurrent infections, and thrombocytopenia (low platelet count). These symptoms can manifest in early childhood and vary in severity among individuals. Eczema, a chronic skin condition, often appears during infancy and can cause itching, redness, and skin inflammation. Recurrent infections, particularly of the respiratory and gastrointestinal tracts, occur due to the weakened immune system associated with WAS. Thrombocytopenia can lead to easy bruising, prolonged bleeding, and an increased risk of developing severe bleeding episodes. Additionally, individuals with WAS may experience other complications such as autoimmune disorders, allergies, and an increased risk of developing certain cancers. Understanding these symptoms and risks is crucial for early diagnosis and management of Wiskott-Aldrich syndrome.
Cord blood banking for Wiskott-Aldrich: Benefits and considerations.
Cord blood banking can offer potential benefits for individuals diagnosed with Wiskott-Aldrich syndrome (WAS). The umbilical cord blood, which contains valuable hematopoietic stem cells, can be collected at birth and stored for future use. These stem cells have the ability to differentiate into various blood cells, including platelets, which are essential for clotting and preventing bleeding complications. Therefore, cord blood transplantation can be considered as a potential treatment option for individuals with WAS who experience severe thrombocytopenia or other related complications. However, it is important to note that cord blood transplantation may not be appropriate for all cases of WAS, as individual factors such as disease severity, available donor options, and overall health status need to be carefully evaluated. Consulting with a healthcare professional experienced in the management of Wiskott-Aldrich syndrome is essential to determine the potential benefits and considerations of cord blood banking for each individual case.
The importance of early detection and treatment for Wiskott-Aldrich.
Early detection and treatment play a crucial role in improving outcomes for individuals with Wiskott-Aldrich syndrome (WAS). This rare genetic disorder affects the immune system, leading to a range of symptoms such as recurrent infections, eczema, and bleeding disorders. Identifying the condition early allows for timely intervention, including the implementation of prophylactic antibiotics, immunoglobulin replacement therapy, and close monitoring of platelet counts. Additionally, early detection enables prompt consideration of potential curative treatments such as hematopoietic stem cell transplantation. By recognizing and addressing WAS in its early stages, healthcare professionals can significantly enhance the quality of life for affected individuals and potentially prevent life-threatening complications. Therefore, early detection and swift initiation of appropriate treatment strategies are paramount in managing Wiskott-Aldrich syndrome effectively.
How cord blood stem cells can help in treating Wiskott-Aldrich.
Cord blood stem cells have shown promise in the treatment of Wiskott-Aldrich syndrome (WAS). These unique cells, obtained from the umbilical cord blood of newborns, have the potential to differentiate into various types of blood cells, including those that are affected in individuals with WAS. Transplanting cord blood stem cells into patients with WAS can help replenish the defective immune cells and restore normal immune function. Additionally, cord blood stem cells have a lower risk of graft-versus-host disease compared to other sources of stem cells, making them a viable option for patients with WAS. While further research is needed to optimize the transplantation process and long-term outcomes, cord blood banking provides a valuable resource for potential treatment options in managing Wiskott-Aldrich syndrome.
Exploring the potential of cord blood banking for Wiskott-Aldrich patients.
The potential of cord blood banking in the context of Wiskott-Aldrich syndrome (WAS) is an area of ongoing exploration and research. WAS is a rare genetic disorder that affects the immune system and can lead to severe complications. Cord blood stem cells, with their unique ability to differentiate into various types of blood cells, offer a promising avenue for treatment. By transplanting these stem cells into WAS patients, it is possible to replenish the defective immune cells and restore normal immune function. With the advantage of a lower risk of graft-versus-host disease, cord blood stem cells present a viable option for patients with WAS. As we continue to delve into the potential of cord blood banking, further research is necessary to optimize the transplantation process and evaluate long-term outcomes. Nonetheless, cord blood banking holds great promise in providing valuable treatment options for managing Wiskott-Aldrich syndrome.
The role of stem cells in Wiskott-Aldrich syndrome and cord blood banking.
The role of stem cells in Wiskott-Aldrich syndrome (WAS) and cord blood banking is crucial in understanding the potential for therapeutic interventions. WAS, as a complex genetic disorder affecting the immune system, necessitates innovative treatment strategies. Stem cells obtained from cord blood have emerged as a promising source for the transplantation of healthy immune cells in WAS patients. These stem cells possess the ability to differentiate into various blood cell types, making them valuable in replenishing the defective immune cells and restoring normal immune function. The utilization of cord blood stem cells in WAS treatment offers advantages, such as reduced risk of graft-versus-host disease compared to other sources. Nevertheless, further research and optimization of the transplantation process are essential to maximize the potential benefits of cord blood banking in managing Wiskott-Aldrich syndrome.
Facts and statistics on Wiskott-Aldrich syndrome and cord blood banking.
Wiskott-Aldrich syndrome (WAS) is a rare X-linked genetic disorder that primarily affects males, with an estimated incidence of 1 in 100,000 live births. It is characterized by a triad of symptoms, including eczema, low platelet count, and recurrent infections. If left untreated, WAS can lead to severe complications, such as autoimmune diseases and an increased risk of developing hematologic malignancies.Cord blood banking has emerged as a potential solution for treating WAS. Cord blood, which is collected from the umbilical cord and placenta after childbirth, contains a rich source of hematopoietic stem cells. These stem cells have the ability to differentiate into various types of blood cells, including immune cells.Studies have shown promising results in using cord blood stem cell transplantation as a curative treatment for WAS. Research indicates that patients who undergo cord blood transplantation show improved platelet counts, reduced severity of eczema, and enhanced immune function.Additionally, cord blood banking provides a valuable resource for patients with WAS who may require multiple transplantations or future therapeutic interventions. It eliminates the need for finding a suitable donor match and reduces the risk of graft-versus-host disease.Although cord blood banking offers potential benefits for managing Wiskott-Aldrich syndrome, challenges and limitations still exist. These include the availability of suitable cord blood units, the need for optimal transplant protocols, and the importance of long-term follow-up to assess the efficacy and durability of the treatment.In conclusion, the utilization of cord blood stem cells from umbilical cord banking holds promise in the treatment of Wiskott-Aldrich syndrome. While further research and advancements are needed, cord blood transplantation offers a potential curative approach and provides a valuable resource for patients with this rare genetic disorder.
What to consider when choosing a cord blood bank for Wiskott-Aldrich.
When considering a cord blood bank for Wiskott-Aldrich syndrome (WAS), there are several important factors to take into account. First and foremost, it is crucial to choose a bank that has experience in storing and processing cord blood specifically for the treatment of genetic disorders like WAS. Look for a bank that has a track record of successful transplants and positive outcomes for patients with similar conditions.Furthermore, consider the bank's accreditation and compliance with industry standards. Look for certifications from reputable organizations such as the AABB (formerly known as the American Association of Blood Banks) and the Foundation for Accreditation of Cellular Therapy (FACT). These certifications ensure that the bank adheres to strict quality and safety standards in collecting, processing, and storing cord blood.It is also important to assess the bank's storage facilities and protocols. Look for a bank that utilizes state-of-the-art cryogenic storage systems and has redundant backup systems in place to ensure the integrity and viability of the cord blood cells over time. Additionally, inquire about the bank's policies regarding sample viability testing and how they handle potential issues or complications that may arise during storage or transplantation.Lastly, consider the bank's financial stability and accessibility. Evaluate the costs associated with cord blood banking and any additional fees that may be incurred over time. It is important to choose a bank that provides transparent pricing and flexible payment options. Additionally, consider the bank's customer service and support. A reliable and responsive customer support team can provide valuable assistance and guidance throughout the cord blood banking process.In conclusion, when choosing a cord blood bank for Wiskott-Aldrich syndrome, it is essential to prioritize experience, accreditations, storage facilities, financial stability, and customer support. By considering these factors, you can make an informed decision and ensure that the cord blood bank you choose is well-equipped to meet the unique needs of individuals with Wiskott-Aldrich syndrome.
Success stories: How cord blood banking has helped Wiskott-Aldrich patients.
Success stories: How cord blood banking has helped Wiskott-Aldrich patients.Cord blood banking has proven to be a life-changing option for patients with Wiskott-Aldrich syndrome (WAS). Numerous success stories highlight the significant impact of cord blood transplants in improving the lives of individuals diagnosed with this rare genetic disorder. Patients who have received cord blood transplants from compatible donors have experienced significant improvements in their immune systems, reduced infections, and improved overall quality of life.One such success story involves a young boy diagnosed with WAS at the age of two. His parents opted for cord blood banking and were fortunate to find a compatible donor. After the successful transplant, the boy's platelet count increased, resolving the bleeding and bruising issues he had previously faced. His immune system strengthened, leading to a significant reduction in infections and hospitalizations. Today, he is a thriving teenager, enjoying a normal and active life, thanks to the potential offered by cord blood banking.Another inspiring case involves a girl diagnosed with WAS shortly after birth. Her parents, aware of the potential benefits of cord blood banking, made the decision to store her cord blood. When she required a transplant a few years later, her stored cord blood proved to be a perfect match. The transplant successfully replenished her compromised immune system, enabling her to live a healthier life, free from the limitations imposed by WAS. She is now a young adult, pursuing her dreams and embracing a future that was once uncertain.These success stories highlight the immense potential of cord blood banking in the treatment of Wiskott-Aldrich syndrome. By preserving cord blood at birth, families are provided with a valuable resource that can potentially save lives and offer renewed hope to those affected by this rare genetic disorder. Cord blood banking has emerged as a vital tool in the fight against WAS, offering the promise of improved patient outcomes and a brighter future for individuals and families facing this challenging condition.
Making an educated decision: Cord blood banking and Wiskott-Aldrich syndrome.
Making an educated decision about cord blood banking and its potential benefits for individuals with Wiskott-Aldrich syndrome (WAS) requires careful consideration of several factors. Firstly, it is essential to understand the nature of WAS and its impact on the individual's health. WAS is a rare genetic disorder characterized by a compromised immune system, low platelet levels, and increased susceptibility to infections and bleeding disorders. Cord blood banking offers a potential solution by providing a source of stem cells that can be used in transplantation to restore the immune system and improve overall health outcomes. However, it is crucial to consult with medical professionals specialized in treating WAS to determine if cord blood banking is a suitable option for the specific individual, taking into account factors such as disease severity, available treatment options, and the likelihood of finding a compatible donor. Additionally, considering the costs and logistics associated with cord blood banking is essential to make an informed decision that aligns with the individual's and their family's needs and circumstances. Ultimately, by gathering comprehensive information and seeking expert guidance, individuals and their families can make an educated decision about cord blood banking and its potential role in managing Wiskott-Aldrich syndrome.In conclusion, Wiskott-Aldrich syndrome is a rare and potentially life-threatening genetic disorder that affects the immune system and blood cells. While there is no known cure for this condition, cord blood banking is a promising option for families who may have a child with Wiskott-Aldrich syndrome. By collecting and storing the stem cells found in cord blood, families can potentially access these life-saving cells for future treatment options. It is crucial for families to educate themselves about the benefits of cord blood banking and consider it as a preventative measure for their child's health. With continued advancements in medical technology, we can only hope for a brighter future for those affected by Wiskott-Aldrich syndrome.
FAQ
What is Wiskott-Aldrich syndrome and what are the symptoms associated with this genetic disorder?Wiskott-Aldrich syndrome is a rare genetic disorder characterized by low platelet count, eczema, and immune deficiency. Individuals with this syndrome may experience easy bruising, frequent infections, bleeding problems, and an increased risk of developing autoimmune diseases and certain cancers. Treatment typically involves managing symptoms and sometimes bone marrow transplants.How does cord blood banking play a role in potentially treating Wiskott-Aldrich syndrome?Cord blood banking plays a critical role in potentially treating Wiskott-Aldrich syndrome by providing a source of stem cells that can be used for hematopoietic stem cell transplantation. These stem cells can help replace the defective immune system in individuals with Wiskott-Aldrich syndrome, offering a chance for improved immune function and overall health outcomes. Read the full article
0 notes
Text
What is Adenosine deaminase deficiency and how can cord blood banking help?
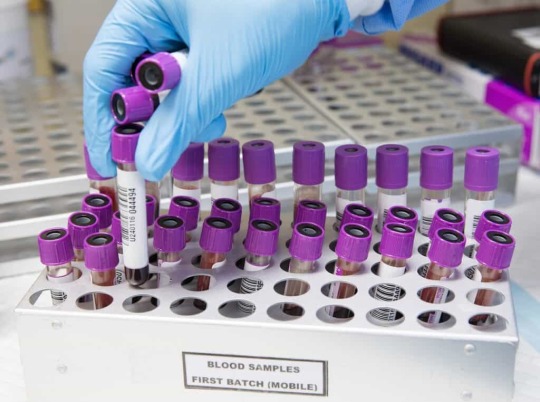
I am ready to enroll in cord blood banking NOW and get my special discount!

By clicking on either buttons, you are agreeing to our TOS and disclaimers and will be redirected to an affiliate cord blood banking provider. We might get financial compensation if you sign up with them through our affiliate links. Unlock your special discounts by adding your promo code.CORD300 in the coupon field to get $300 OFF cord blood and tissue banking. OR cord200 to get $200 OFF if you are getting cord blood banking only. I want more information on cord blood banking
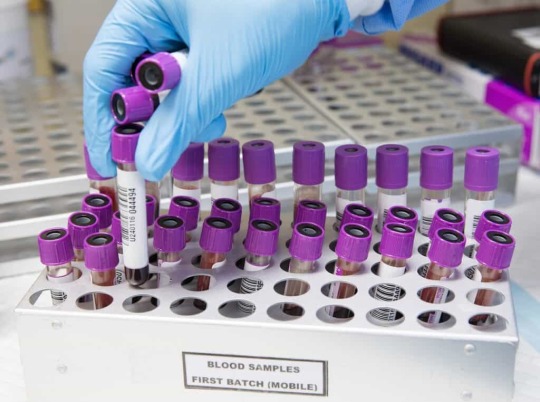
Adenosine deaminase deficiency (ADA) is a rare genetic disorder that affects the immune system. This condition is caused by a deficiency in the enzyme adenosine deaminase, which plays a crucial role in the development and function of immune cells. As a result, individuals with ADA deficiency have weakened immune systems, making them more susceptible to severe and life-threatening infections. Fortunately, advancements in medical science have provided a solution to this debilitating condition through cord blood banking. Cord blood banking is the process of collecting and storing stem cells found in the umbilical cord blood after a baby is born. These stem cells have the potential to develop into various types of blood cells, including immune cells. In recent years, cord blood banking has emerged as a promising treatment option for ADA deficiency, offering hope to those affected by this condition. In this article, we will delve into the details of ADA deficiency, its impact on individuals, and how cord blood banking can be a game-changer in managing and treating this disorder.
Overview of Adenosine Deaminase Deficiency
Adenosine Deaminase Deficiency (ADA) is a rare genetic disorder that affects the immune system, specifically the functioning of T-lymphocytes. This enzyme deficiency leads to the accumulation of toxic substances, resulting in the impairment of immune responses. ADA deficiency is typically diagnosed in infancy, as affected infants often present with severe combined immunodeficiency (SCID), a condition characterized by a compromised immune system. Without intervention, children with ADA deficiency are highly susceptible to severe infections and other related complications. The management of ADA deficiency often involves regular enzyme replacement therapy and stem cell transplantation. Cord blood banking, specifically the storage of umbilical cord blood, can provide a potential source of hematopoietic stem cells for transplantation, offering hope for improved outcomes and long-term management of this challenging condition.
Causes and symptoms explained
Adenosine Deaminase Deficiency (ADA) is caused by mutations in the ADA gene, which is responsible for producing the enzyme adenosine deaminase. This enzyme plays a crucial role in the breakdown of purine nucleotides, which are essential for various cellular processes. In individuals with ADA deficiency, the lack or reduced activity of this enzyme leads to the buildup of toxic metabolites, particularly adenosine and deoxyadenosine, which can be toxic to the developing immune system.The symptoms of ADA deficiency can vary in severity but typically manifest in early infancy. Affected infants often present with severe combined immunodeficiency (SCID), characterized by a compromised immune system. This makes them highly vulnerable to recurrent and severe infections, including those caused by bacteria, viruses, and fungi. Additionally, ADA deficiency can also affect the development and function of other body systems, leading to growth impairments, skeletal abnormalities, and neurological complications.Early diagnosis of ADA deficiency is crucial for prompt intervention and management. Newborn screening programs have been implemented in some countries to identify affected infants before the onset of symptoms. This allows for early initiation of treatment, which typically involves enzyme replacement therapy to provide the missing ADA enzyme. Stem cell transplantation, often utilizing hematopoietic stem cells sourced from umbilical cord blood, may be considered as a curative option for individuals with ADA deficiency.By understanding the causes and recognizing the symptoms of ADA deficiency, healthcare professionals and families can pursue appropriate interventions and make informed decisions regarding treatments such as cord blood banking. This knowledge plays a vital role in improving outcomes and offering hope for individuals affected by this challenging condition.
Importance of early diagnosis
Early diagnosis plays a crucial role in the management and treatment of Adenosine Deaminase Deficiency (ADA). Identifying ADA deficiency in its early stages allows for timely interventions and appropriate medical care to be implemented. By recognizing the symptoms and conducting diagnostic tests promptly, healthcare professionals can initiate targeted therapies and interventions that can significantly improve the quality of life for affected individuals. Moreover, early diagnosis enables medical professionals to educate and support families in understanding the condition, its potential complications, and available treatment options. This empowers families to make informed decisions and seek specialized care, such as cord blood banking, which can provide a potential source of hematopoietic stem cells for future treatment possibilities. Ultimately, early diagnosis not only aids in the management of ADA deficiency but also enhances the overall prognosis and long-term outcomes for individuals affected by this genetic disorder.
Traditional treatment options available
In the realm of Adenosine Deaminase Deficiency (ADA), there are several traditional treatment options available that aim to alleviate symptoms and manage the condition. One of the mainstay treatments is enzyme replacement therapy, where the deficient ADA enzyme is supplemented with synthetic forms of the enzyme. This therapy helps to maintain the balance of adenosine and deoxyadenosine, reducing the toxic buildup in the body. Additionally, immunoglobulin replacement therapy may be utilized to support the immune system and prevent frequent infections. Other treatment approaches may include antiviral medications, antibiotics for infections, and regular monitoring of immune function. It is important to note that the specific treatment plan may vary depending on the severity of ADA deficiency and the individual's unique medical needs.
Limitations and risks involved
While there are treatment options available for Adenosine Deaminase Deficiency (ADA), it is important to acknowledge the limitations and risks involved. Enzyme replacement therapy, while effective in managing symptoms, may not fully restore normal ADA activity and may require lifelong administration. Additionally, this therapy can be expensive and may not be accessible to all individuals. Immunoglobulin replacement therapy, although beneficial in supporting the immune system, may also have its limitations and may not completely prevent infections. Moreover, these treatments may come with potential side effects and risks, such as allergic reactions or complications from long-term use of medications. It is crucial for individuals with ADA deficiency and their healthcare providers to carefully evaluate the benefits and risks of each treatment option and make informed decisions based on their specific circumstances. Regular monitoring and follow-up care are essential to ensure the effectiveness of the chosen treatment approach.
Role of cord blood banking
Cord blood banking plays a significant role in the field of healthcare, particularly in the treatment and management of various genetic disorders and immune deficiencies. The stem cells found in cord blood have the potential to differentiate into different types of cells, including blood cells, which makes them a valuable resource for transplantation. In the case of Adenosine Deaminase Deficiency (ADA), cord blood banking can offer a potential solution. By storing cord blood from a newborn who is a genetic match for a sibling with ADA deficiency, it provides a readily available source of stem cells that can be used for transplantation. These stem cells can help replenish the deficient ADA enzyme, potentially improving immune function and reducing the severity of symptoms. The ability to access cord blood from a sibling provides a unique advantage, as it eliminates the need to search for a suitable donor and reduces the risk of rejection. Cord blood banking offers hope in the treatment of ADA deficiency, offering a potentially life-saving option for affected individuals.
Potential benefits of stem cells
Stem cells, including those found in cord blood, hold immense potential for various medical applications. These versatile cells have the ability to differentiate into specialized cells, such as neurons, muscle cells, and even heart cells. This remarkable characteristic opens up a wide range of possibilities for regenerative medicine and tissue engineering. Stem cells can potentially be used to repair damaged tissues and organs, providing hope for individuals suffering from conditions such as heart disease, spinal cord injuries, and Parkinson's disease. Additionally, stem cells can contribute to advancements in drug testing and development, as they can be used to create disease models and study the effectiveness of potential treatments. The exploration of stem cells and their therapeutic potential continues to offer promising avenues for medical breakthroughs and improved patient outcomes.
Current research and studies
Current research and studies in the field of Adenosine deaminase deficiency and cord blood banking are shedding light on the potential benefits and applications of this innovative approach. Researchers are investigating the use of cord blood stem cells in the treatment of Adenosine deaminase deficiency, a rare genetic disorder that affects the immune system. Preliminary studies have shown promising results, indicating that cord blood stem cells may hold the key to restoring immune function in affected individuals. These findings offer hope for improved treatment options and enhanced quality of life for patients with this challenging condition. Ongoing research aims to further understand the mechanisms underlying the therapeutic effects of cord blood stem cells and optimize their use in clinical settings. As the scientific community continues to explore the potential of cord blood banking, further advancements and breakthroughs are expected, ultimately leading to better outcomes for individuals with Adenosine deaminase deficiency and other diseases.
Success stories from patients
Success stories from patients who have undergone cord blood banking for the treatment of Adenosine deaminase deficiency highlight the potential of this innovative approach. Patients who have received infusions of cord blood stem cells have reported improvements in immune function and overall health. These success stories serve as a testament to the potential of cord blood banking in providing a viable treatment option for individuals with Adenosine deaminase deficiency. With ongoing research and advancements in the field, it is hoped that more patients will have access to this life-changing therapy and experience similar positive outcomes.
Private cord blood banking for adenosine deaminase deficiency
The utilization of private cord blood banking has emerged as a promising option for individuals diagnosed with Adenosine deaminase deficiency. By banking their baby's cord blood at birth, parents have the opportunity to preserve a valuable source of potentially life-saving stem cells. These stem cells can be collected and stored for future use in the treatment of Adenosine deaminase deficiency or other immune-related disorders. This proactive approach allows for immediate access to a genetically matched source of stem cells, eliminating the need to search for a suitable donor. Private cord blood banking offers families a sense of security and peace of mind, providing a potential lifeline in the face of Adenosine deaminase deficiency.In conclusion, Adenosine deaminase deficiency (ADA) is a rare genetic disorder that affects the immune system. While there is currently no cure for ADA, cord blood banking offers a potential solution for affected individuals. By preserving the stem cells found in cord blood, these cells can be used for future treatments such as bone marrow transplants. This gives hope to families affected by ADA and highlights the importance of cord blood banking in potentially saving lives. As research and technology continue to advance, we can only hope for more breakthroughs in treating rare disorders like ADA.
FAQ
What is Adenosine deaminase deficiency and how does it affect the body?Adenosine deaminase deficiency is a rare genetic disorder that impairs the immune system, leading to severe combined immunodeficiency (SCID). This condition prevents the body from properly fighting off infections, making individuals highly susceptible to recurrent and severe infections. Without treatment, SCID can be life-threatening, often manifesting in infancy with symptoms such as chronic diarrhea, failure to thrive, and recurrent infections. Treatment typically involves bone marrow transplants or enzyme replacement therapy to restore immune function and prevent life-threatening complications.How can cord blood banking potentially help individuals with Adenosine deaminase deficiency?Cord blood banking can potentially help individuals with Adenosine deaminase deficiency by providing a source of stem cells that can be used in hematopoietic stem cell transplantation. This treatment can replace the defective immune cells with healthy ones, potentially restoring the immune system function in affected individuals. By storing cord blood, individuals with this condition can have access to a suitable matching donor source for this potentially life-saving procedure.What are the benefits of using cord blood stem cells in treating Adenosine deaminase deficiency?Cord blood stem cells offer a potentially curative treatment for Adenosine deaminase deficiency by providing a source of healthy stem cells that can differentiate into functional immune cells. This approach can restore the immune system's function and prevent infections associated with the condition. Additionally, cord blood stem cells are less likely to cause graft-versus-host disease, making them a safer option for patients. Overall, utilizing cord blood stem cells in treating Adenosine deaminase deficiency offers a promising therapeutic approach with lower risks of complications.Are there any risks or limitations to using cord blood banking for treating Adenosine deaminase deficiency?Currently, there are limited studies on the efficacy of cord blood banking for treating Adenosine deaminase deficiency. While cord blood banking can potentially provide stem cells for gene therapy, there are risks and limitations to consider such as the availability of suitable matches, the possibility of graft-versus-host disease, and the need for further research to determine the long-term effectiveness of this treatment approach. It is important to consult with healthcare professionals and genetic counselors to fully understand the implications of cord blood banking for Adenosine deaminase deficiency.What research or studies have been conducted on the effectiveness of cord blood banking in treating Adenosine deaminase deficiency?There have been limited research studies specifically focused on the effectiveness of cord blood banking in treating Adenosine deaminase deficiency. However, cord blood stem cells have shown promise in treating various genetic disorders, including immune deficiencies like ADA deficiency. While more research is needed to establish the effectiveness of cord blood banking in treating ADA deficiency, early studies and clinical trials have indicated potential benefits of using cord blood stem cells for such conditions. Further research in this area can provide valuable insights into the efficacy of cord blood banking for treating ADA deficiency. Read the full article
0 notes
Text
What is Severe combined immunodeficiency and how can cord blood banking help?

I am ready to enroll in cord blood banking NOW and get my special discount!

By clicking on either buttons, you are agreeing to our TOS and disclaimers and will be redirected to an affiliate cord blood banking provider. We might get financial compensation if you sign up with them through our affiliate links. Unlock your special discounts by adding your promo code.CORD300 in the coupon field to get $300 OFF cord blood and tissue banking. OR cord200 to get $200 OFF if you are getting cord blood banking only. I want more information on cord blood banking

Severe combined immunodeficiency (SCID) is a rare, life-threatening disorder that affects the immune system. It is characterized by a severe deficiency in the body's ability to fight off infections and diseases, leaving individuals susceptible to a wide range of illnesses. While it is a genetic condition, it can also be acquired later in life through certain medical treatments or conditions. Despite its rarity, SCID is a serious and debilitating disease that requires immediate attention and treatment. Fortunately, advancements in medical technology have provided a potential solution for those diagnosed with SCID - cord blood banking. This process involves collecting and storing a baby's umbilical cord blood, which is rich in powerful stem cells that can potentially treat various diseases, including SCID. In this article, we will delve into the details of what SCID is, how it affects individuals, and how cord blood banking can serve as a crucial tool in the fight against this debilitating disease.
Understanding Severe Combined Immunodeficiency
Severe Combined Immunodeficiency (SCID) is a rare, life-threatening disorder that affects the immune system. It is characterized by a severe deficiency in both T cells and B cells, which are crucial components of the immune system responsible for fighting off infections and diseases. SCID is typically diagnosed in infancy, as affected infants often experience recurrent and severe infections that do not respond to typical treatments. This condition is primarily caused by genetic mutations that impair the production or function of immune cells. Without proper intervention, SCID can lead to severe complications and early mortality. Understanding the complexities of SCID and its impact on the immune system is essential for early diagnosis, appropriate medical management, and potential treatment options such as cord blood banking.
Causes, symptoms and treatment options
Severe Combined Immunodeficiency (SCID) is caused by genetic mutations that affect the production or function of immune cells, specifically T cells and B cells. These mutations can be inherited from one or both parents, or they can occur spontaneously. As a result, individuals with SCID have a severely compromised immune system, making them highly susceptible to infections. Common symptoms of SCID include recurrent and severe infections, failure to thrive, chronic diarrhea, skin rashes, and persistent oral thrush. Without prompt and appropriate treatment, SCID can lead to life-threatening complications.The main goal of treatment for SCID is to restore normal immune function. This can be achieved through various approaches, including hematopoietic stem cell transplantation (HSCT), gene therapy, and enzyme replacement therapy. HSCT, particularly from a matched sibling donor, is currently the most common treatment option for SCID. In cases where a matched donor is not available, alternative sources of stem cells, such as cord blood banking, can be considered. Cord blood contains hematopoietic stem cells that can be used for transplantation, providing a potential cure for SCID. Cord blood banking involves collecting and storing cord blood at the time of birth, ensuring a readily available source of stem cells for future use if needed.Overall, understanding the causes, symptoms, and treatment options for SCID is crucial for early diagnosis and intervention. Through advancements in medical research and technologies like cord blood banking, there is hope for improved outcomes and a brighter future for individuals with SCID.
Importance of early detection and diagnosis
Early detection and diagnosis play a crucial role in addressing severe combined immunodeficiency (SCID) effectively. Identifying SCID in its early stages allows for timely intervention and treatment, which can greatly improve the prognosis and quality of life for affected individuals. Early detection enables healthcare professionals to implement appropriate therapies, such as hematopoietic stem cell transplantation or gene therapy, before severe complications arise. Moreover, early diagnosis allows for genetic counseling and family planning, helping parents make informed decisions about the future health of their child and potentially preventing the transmission of SCID to future generations. Regular screening programs and increased awareness among healthcare providers and parents are essential in ensuring the early detection and diagnosis of SCID, leading to improved outcomes for individuals affected by this condition.
Role of cord blood banking
Cord blood banking plays a crucial role in the management of severe combined immunodeficiency (SCID). Cord blood, collected from the umbilical cord after childbirth, contains a rich source of hematopoietic stem cells that have the potential to regenerate and replenish the immune system. These stem cells can be used in hematopoietic stem cell transplantation, a potentially life-saving treatment for SCID. By preserving and storing cord blood, individuals have access to a readily available and genetically matched source of stem cells, eliminating the need to search for a suitable donor. Cord blood banking offers a valuable resource for families affected by SCID, providing them with a greater chance of successful treatment and improved long-term outcomes.
What is cord blood banking?
Cord blood banking is the process of collecting and storing the blood found in the umbilical cord after a baby is born. This blood contains a rich source of hematopoietic stem cells, which have the unique ability to develop into different types of blood cells. These stem cells can be used in the treatment of various diseases, including certain types of cancer, blood disorders, and immune system deficiencies like severe combined immunodeficiency (SCID). Cord blood banking involves carefully collecting the cord blood, processing it to isolate and preserve the stem cells, and then storing it in specialized facilities for future use. This practice allows families to have a readily available source of stem cells that can potentially be used to treat serious medical conditions in the future. By banking cord blood, individuals have the peace of mind knowing that they have a valuable resource that may offer potential therapeutic options for their family's health and well-being.
How does it work?
The process of cord blood banking involves several steps to ensure the collection, processing, and preservation of valuable stem cells. After a baby is born, the umbilical cord is clamped and cut, and the blood remaining in the cord is collected using a specialized collection kit. This process is quick and painless, posing no risk or discomfort to either the mother or the baby. The collected cord blood is then transported to a laboratory where it undergoes rigorous testing and processing. The blood is carefully centrifuged to separate the stem cells from other components, and then the isolated stem cells are preserved using cryopreservation techniques. These stem cells can be stored for many years, allowing families to have a reliable source of stem cells for potential future use. In the event of a medical need, the stored cord blood can be thawed and prepared for administration, providing a valuable resource for potential treatments. Cord blood banking offers a proactive approach to healthcare, offering families the opportunity to preserve and potentially utilize these powerful stem cells for the benefit of their loved ones.
Benefits of cord blood banking
Cord blood banking provides numerous benefits for families who choose to invest in this valuable resource. One significant advantage is the potential to treat a variety of diseases and conditions. Stem cells derived from cord blood have been successfully used in the treatment of various blood disorders, immune system deficiencies, and certain types of cancers. These stem cells have the remarkable ability to differentiate into different cell types, allowing them to repair and regenerate damaged tissues. Additionally, cord blood stem cells are more readily available compared to other sources, such as bone marrow, eliminating the need for invasive procedures. By preserving cord blood, families can have peace of mind knowing they have a potential life-saving resource readily accessible in the event of a medical need. Furthermore, cord blood banking also offers the opportunity for medical research and advancements. Scientists are continually exploring new applications and therapies utilizing cord blood stem cells, contributing to the development of innovative treatments and potential cures for a wide range of diseases. Overall, cord blood banking provides families with a secure investment in their health and the health of their loved ones, offering the potential for improved medical outcomes and a brighter future.
How cord blood can help
Cord blood has shown great promise in the treatment of Severe Combined Immunodeficiency (SCID), a rare and potentially life-threatening condition characterized by a severely compromised immune system. SCID is typically diagnosed in infants within the first few months of life, leaving them vulnerable to serious infections that can be fatal if left untreated. Cord blood, rich in hematopoietic stem cells, offers a viable solution for these patients. By transplanting these stem cells into the affected individual, it is possible to restore and strengthen their immune system, providing them with a fighting chance against infections and improving their overall quality of life. Cord blood banking plays a crucial role in offering families the opportunity to access these life-saving treatments and provide their children with the best chance for a healthy future.
Success stories of cord blood transplants
Over the years, there have been numerous success stories regarding cord blood transplants in the treatment of Severe Combined Immunodeficiency (SCID). These stories highlight the immense potential of cord blood as a source of hematopoietic stem cells to effectively address this debilitating condition. For instance, there have been cases where infants diagnosed with SCID and undergoing cord blood transplants have experienced significant improvements in their immune function. These transplants have not only helped them fight off infections that would have otherwise been life-threatening but have also allowed them to lead more normal and fulfilling lives. Such success stories serve as a testament to the power of cord blood banking and its ability to provide hope and a brighter future for individuals and families affected by SCID.
Making an informed decision for your family.
When it comes to making important decisions for your family's health, it is crucial to gather all the relevant information and make an informed choice. Understanding the complexities and potential benefits of cord blood banking in the context of Severe Combined Immunodeficiency (SCID) is key to making the right decision. By researching and consulting with healthcare professionals, you can gain a comprehensive understanding of the potential role that cord blood banking can play in the treatment of SCID. It is important to weigh the potential advantages, such as the successful outcomes seen in some cases, against factors such as costs, accessibility, and individual health considerations. Taking the time to be well-informed and considering the specific needs of your family can empower you to make the best decision regarding cord blood banking for the management of SCID.In conclusion, severe combined immunodeficiency is a rare, but serious, genetic disorder that affects the immune system. However, with advancements in medical technology, cord blood banking now offers a potential solution for those affected by this condition. By storing a newborn's cord blood, families have the opportunity to provide a potential cure for their child in the future. It is important to discuss the option of cord blood banking with a healthcare provider to determine if it may be a beneficial choice for your family. With continued research and advancements in stem cell therapies, cord blood banking has the potential to greatly improve the lives of those with severe combined immunodeficiency and other similar conditions.
FAQ
What is Severe Combined Immunodeficiency (SCID) and how does it affect the immune system?Severe Combined Immunodeficiency (SCID) is a rare genetic disorder that affects the immune system, specifically the ability to produce T cells and B cells. This results in a severely weakened immune system, leaving individuals susceptible to recurring infections, illnesses, and even life-threatening conditions. SCID is often diagnosed in infancy and requires immediate treatment, such as bone marrow transplant or gene therapy, to restore immune function and prevent severe complications. Ultimately, individuals with SCID have a compromised ability to fight infections, making them highly vulnerable to various pathogens.How can cord blood banking potentially help individuals with SCID?Cord blood banking can potentially help individuals with Severe Combined Immunodeficiency (SCID) by providing a source of stem cells that can be used in stem cell transplant therapy. These stem cells can help rebuild a functioning immune system in individuals with SCID, offering a potential cure for the condition. Additionally, cord blood banking allows for the preservation of these valuable stem cells for future use, providing a treatment option for individuals with SCID who may not have a suitable donor match readily available.What are the benefits of using cord blood for stem cell transplants in treating SCID?Cord blood is valuable for SCID treatment due to its rich source of hematopoietic stem cells, which can regenerate a healthy immune system. It reduces the risk of graft-versus-host disease and allows for easier matching with recipients. Additionally, cord blood transplants have lower rejection rates and offer a higher likelihood of finding suitable donors for patients who lack matched siblings. Overall, cord blood stem cell transplants offer a promising and effective treatment option for SCID patients.Are there any risks or limitations associated with using cord blood for SCID treatment?While cord blood transplantation is an effective treatment for Severe Combined Immunodeficiency (SCID), there are potential risks and limitations associated with the procedure. These include the possibility of graft-versus-host disease, infection, and the development of secondary malignancies. Additionally, finding a suitable donor match can be challenging, and there is a risk of rejection by the recipient's immune system. Close monitoring and careful consideration of these factors are essential when using cord blood for SCID treatment.How does the process of cord blood banking work and what should parents consider when deciding to bank their child's cord blood for potential SCID treatment?Cord blood banking involves collecting and storing a newborn's umbilical cord blood, rich in stem cells, for potential medical use in the future. Parents considering banking their child's cord blood for SCID treatment should weigh factors like family medical history, likelihood of needing a transplant, cost of storage, and availability of public cord blood banks. It is essential to consult with healthcare providers, assess the benefits and risks, and make an informed decision based on individual circumstances. Read the full article
0 notes
Text
What is X-linked immunodeficiency and how can cord blood banking help?

I am ready to enroll in cord blood banking NOW and get my special discount!

By clicking on either buttons, you are agreeing to our TOS and disclaimers and will be redirected to an affiliate cord blood banking provider. We might get financial compensation if you sign up with them through our affiliate links. Unlock your special discounts by adding your promo code.CORD300 in the coupon field to get $300 OFF cord blood and tissue banking. OR cord200 to get $200 OFF if you are getting cord blood banking only. I want more information on cord blood banking

X-linked immunodeficiency (XID) is a rare genetic disorder that affects the immune system, leaving individuals vulnerable to infections and illnesses. This condition is caused by a mutation in the X-chromosome, leading to a deficiency in the body's ability to produce certain immune cells. As a result, individuals with XID are more prone to recurrent infections, autoimmune disorders, and even certain types of cancer. While there is currently no cure for XID, there are treatment options available to manage the symptoms and improve the quality of life for those affected. One such option is cord blood banking, a process that involves collecting and storing a newborn's umbilical cord blood for potential future use in medical treatments. In recent years, there has been an increasing interest in the potential benefits of cord blood banking for individuals with XID. In this article, we will explore what X-linked immunodeficiency is, its symptoms and effects, and how cord blood banking can potentially aid in the treatment of this condition.
X-linked immunodeficiency: causes and symptoms
X-linked immunodeficiency is a rare genetic disorder that primarily affects males. It is caused by mutations in the genes responsible for the production of immune system proteins, particularly those involved in the maturation and functioning of B cells. These mutations lead to a weakened immune system, making individuals with X-linked immunodeficiency more susceptible to recurrent bacterial, viral, and fungal infections. Common symptoms include frequent respiratory tract infections, chronic diarrhea, poor growth, and failure to thrive. In severe cases, affected individuals may develop life-threatening infections or autoimmune disorders. Early diagnosis and appropriate management are crucial in managing this condition and minimizing its impact on an individual's health and quality of life.
Understanding the role of genetics
Understanding the role of genetics is crucial when it comes to X-linked immunodeficiency and its implications for individuals and families. Genetics plays a significant role in determining the likelihood of inheriting this condition. X-linked immunodeficiency is caused by mutations in specific genes that are located on the X chromosome. Since males have one X chromosome and females have two, the inheritance pattern of X-linked genetic disorders differs between males and females. Males who inherit a mutated gene on their single X chromosome are more likely to develop X-linked immunodeficiency, while females who have one mutated X chromosome are typically carriers of the condition. This understanding of the genetic basis of X-linked immunodeficiency allows for better screening, diagnosis, and genetic counseling for families at risk. Furthermore, it highlights the potential benefits of cord blood banking, as stem cells from umbilical cord blood can serve as a valuable resource for future treatments and therapies for individuals with X-linked immunodeficiency.
Benefits of cord blood banking
Cord blood banking offers a range of benefits that extend beyond the specific context of X-linked immunodeficiency. One major advantage is the potential use of cord blood stem cells in the treatment of various medical conditions. These stem cells, obtained from the umbilical cord at birth, are rich in hematopoietic stem cells that have the ability to differentiate into different types of blood cells. This makes cord blood a valuable resource for transplantation, particularly in the treatment of hematological disorders like leukemia and lymphoma. Additionally, cord blood stem cells have been explored for their potential in regenerative medicine and tissue engineering, with ongoing research focusing on their use in the treatment of conditions such as cerebral palsy and autism. By banking cord blood, individuals have the opportunity to secure a readily available source of stem cells for potential future use, offering peace of mind and potential therapeutic options for their family's well-being.
Prevention and treatment options available
Prevention and treatment options available for X-linked immunodeficiency encompass a multidisciplinary approach aimed at managing symptoms and improving the quality of life for affected individuals. One crucial aspect of prevention involves genetic counseling and testing, which can help identify carriers and inform family planning decisions. Early diagnosis is vital for prompt intervention and treatment, typically involving a combination of immunoglobulin replacement therapy, prophylactic antibiotics, and antiviral medications. Additionally, management may include measures to prevent infections, such as vaccinations and strict hygiene practices. In some cases, hematopoietic stem cell transplantation may be considered as a curative option, utilizing either matched related or unrelated donors or even cord blood stem cells. This innovative approach has shown promising results in restoring immune function and improving long-term outcomes for individuals with X-linked immunodeficiency. Overall, a comprehensive approach integrating preventive measures, ongoing medical management, and therapeutic interventions plays a pivotal role in addressing the challenges associated with this condition.
How cord blood can save lives
Cord blood, the blood found in the umbilical cord and placenta after childbirth, has emerged as a valuable resource in the field of medicine. It contains a rich source of hematopoietic stem cells, which have the ability to develop into different types of blood cells. This unique characteristic makes cord blood an effective treatment option for various diseases, including X-linked immunodeficiency. By utilizing cord blood banking, parents have the opportunity to preserve their baby's cord blood for future use. In the case of X-linked immunodeficiency, cord blood stem cells can be utilized for hematopoietic stem cell transplantation, providing a potentially curative treatment option for affected individuals. This process involves replacing the faulty immune system with healthy stem cells, allowing the body to generate new, properly functioning immune cells. The availability of cord blood banking offers hope for improving the outcomes and quality of life for individuals with X-linked immunodeficiency and represents a significant advancement in medical treatment options.
The importance of early detection
Early detection plays a crucial role in the management and treatment of various medical conditions, including X-linked immunodeficiency. Timely identification of this genetic disorder allows for prompt intervention and implementation of appropriate treatment strategies. By identifying X-linked immunodeficiency early on, healthcare providers can closely monitor affected individuals and provide necessary interventions, such as immunoglobulin replacement therapy or hematopoietic stem cell transplantation, to prevent or minimize the development of complications. Additionally, early detection enables healthcare professionals to educate families about the condition, ensure appropriate genetic counseling, and facilitate access to specialized medical care. Overall, early detection empowers individuals with X-linked immunodeficiency and their families to make informed decisions, seek appropriate medical support, and enhance the overall management of the condition.
Genetic counseling for future pregnancies
Genetic counseling for future pregnancies is an essential step for individuals and couples who have a family history of X-linked immunodeficiency or other genetic disorders. The goal of genetic counseling is to provide individuals with accurate information about the likelihood of passing on the condition to their offspring and to discuss available options for family planning. During a genetic counseling session, a trained genetic counselor or healthcare provider will review the individual or couple's medical history, assess the risk factors, and discuss the various genetic testing options available. They will also provide guidance on reproductive choices, such as assisted reproductive technologies or prenatal screening and diagnosis, that can help individuals make informed decisions about their future pregnancies. Genetic counseling for future pregnancies ensures that individuals and couples have the necessary knowledge and support to navigate the complexities of genetic inheritance and make choices that align with their values and goals.
Support and resources for families
In addition to genetic counseling, families affected by X-linked immunodeficiency can benefit from a range of support and resources. Access to support groups specifically tailored for individuals with rare genetic disorders can provide a sense of community and comfort, allowing families to connect with others who understand their unique challenges. These support groups often offer educational materials, online forums, and in-person meetings where families can share experiences, exchange information, and offer emotional support to one another. Additionally, organizations dedicated to genetic disorders may provide informational resources, guidance on available treatments and therapies, and assistance in navigating the healthcare system. These resources can empower families with the knowledge and tools needed to advocate for their loved ones and ensure they receive the best possible care.
Research advancements in treatment
As medical research continues to advance, there have been promising developments in the treatment of X-linked immunodeficiency. Scientists and healthcare professionals are actively studying the underlying causes of the disorder and exploring potential therapeutic options. One area of focus is gene therapy, which involves replacing or repairing the faulty gene responsible for the immunodeficiency. This innovative approach shows potential in restoring immune function and improving overall health outcomes for individuals with X-linked immunodeficiency. Additionally, advancements in immunotherapy, such as the use of targeted antibodies or immune modulators, are being investigated as potential treatment strategies. These advancements offer hope for improved management and long-term outcomes for individuals affected by X-linked immunodeficiency. It is important to note that while research progress is encouraging, further studies and clinical trials are needed before these treatments become widely available.
The impact of cord blood donation
Cord blood donation has emerged as a valuable resource in the field of medical research and treatment. The umbilical cord blood contains a rich source of stem cells, which have the potential to differentiate into various types of cells and tissues. These stem cells can be used in the treatment of X-linked immunodeficiency and other genetic disorders. By donating cord blood, individuals have the opportunity to contribute to the development of regenerative medicine and potentially save lives. The impact of cord blood donation extends beyond the immediate recipient, as the donated cells can be stored and used for future therapies. This not only offers hope for those currently diagnosed with X-linked immunodeficiency but also paves the way for future advancements in medical science and personalized treatment options.In conclusion, X-linked immunodeficiency is a serious genetic disorder that affects the body's ability to fight off infections. However, with advancements in medical technology, cord blood banking has become a valuable resource in treating this condition. By storing the stem cells found in cord blood, families can have access to potentially life-saving treatments for X-linked immunodeficiency and other diseases. It is important for expectant parents to consider the option of cord blood banking, as it may provide a sense of security and hope for the future health of their child.
FAQ
What is X-linked immunodeficiency and how does it affect individuals?X-linked immunodeficiency is a genetic disorder that primarily affects males, impairing their immune system's ability to effectively combat infections. Individuals with this condition have weakened or ineffective immune responses, leading to recurrent infections, increased susceptibility to opportunistic pathogens, and in severe cases, life-threatening complications. This disorder is caused by mutations in genes located on the X chromosome, affecting the production and function of immune cells like T and B cells. Early diagnosis and treatment are crucial to managing symptoms and improving the quality of life for individuals with X-linked immunodeficiency.How does cord blood banking help individuals with X-linked immunodeficiency?Cord blood banking can help individuals with X-linked immunodeficiency by providing access to stem cells that can be used in stem cell transplants to potentially restore immune function and improve overall health. These stem cells have the potential to develop into different types of blood cells, including the immune cells necessary to fight off infections in individuals with immunodeficiency disorders. By storing cord blood from a newborn with compatible stem cells, individuals with X-linked immunodeficiency have a potential source of treatment that may help boost their immune system and reduce the severity of their condition.Can cord blood from a sibling be used to treat X-linked immunodeficiency in another family member?Yes, cord blood from a sibling can potentially be used to treat X-linked immunodeficiency in another family member through a stem cell transplant. This procedure involves using the healthy stem cells from the donor's cord blood to replace the faulty immune system cells in the recipient, potentially offering a chance for treatment or cure for the immunodeficiency disorder. However, various factors such as tissue compatibility and the specific type of X-linked immunodeficiency would need to be considered before proceeding with this treatment option.Are there specific types of X-linked immunodeficiencies that are more effectively treated with cord blood banking?Certain X-linked immunodeficiencies, such as Wiskott-Aldrich syndrome and X-linked severe combined immunodeficiency (SCID), may benefit from cord blood banking due to the potential to provide a source of healthy stem cells for transplantation. This can help in restoring the immune system function in individuals with these conditions. However, the effectiveness of cord blood banking for treating X-linked immunodeficiencies may vary depending on the specific disorder and individual circumstances. Consulting with a healthcare provider or genetic counselor is crucial for determining the best course of action.What are the potential risks and benefits of using cord blood for treating X-linked immunodeficiency?Cord blood is a potential source of stem cells that can be used to treat X-linked immunodeficiency. The benefits include the ability to replenish the immune system with healthy cells, potentially curing the disease. However, there are risks associated with the procedure, such as rejection by the recipient's immune system or the development of graft-versus-host disease. Additionally, the long-term effects of cord blood transplantation for X-linked immunodeficiency are not yet fully understood, making it important to weigh the potential benefits against the risks before proceeding with treatment. Read the full article
0 notes
Text
What is Juvenile Myelomonocytic Leukemia (JMML) and how can cord blood banking help?

I am ready to enroll in cord blood banking NOW and get my special discount!

By clicking on either buttons, you are agreeing to our TOS and disclaimers and will be redirected to an affiliate cord blood banking provider. We might get financial compensation if you sign up with them through our affiliate links. Unlock your special discounts by adding your promo code.CORD300 in the coupon field to get $300 OFF cord blood and tissue banking. OR cord200 to get $200 OFF if you are getting cord blood banking only. I want more information on cord blood banking

Juvenile Myelomonocytic Leukemia (JMML) is a rare and aggressive form of childhood cancer that affects the blood and bone marrow. This disease is caused by a mutation in the genes that control cell growth and division, leading to an uncontrolled proliferation of immature white blood cells. JMML accounts for less than 1% of all pediatric leukemias and is most commonly diagnosed in children under the age of five. Despite its rarity, JMML is a serious and life-threatening condition that requires immediate and intensive treatment. However, advancements in medical technology have provided a glimmer of hope for families facing this devastating diagnosis. One such advancement is the practice of cord blood banking, which involves collecting and storing the blood from a newborn's umbilical cord for future medical use. In this article, we will explore the basics of JMML, its symptoms, diagnosis, and treatment options, as well as the role of cord blood banking in the fight against this disease. We will also discuss the potential benefits and limitations of cord blood banking and its impact on the treatment of JMML.
Understanding JMML: Symptoms and Diagnosis
Juvenile Myelomonocytic Leukemia (JMML) is a rare and aggressive form of childhood cancer that affects the bone marrow and blood cells. It predominantly occurs in children under the age of six. Recognizing the symptoms of JMML is crucial for early detection and prompt treatment. Common symptoms include an enlarged spleen, anemia, easy bruising or bleeding, recurrent infections, and poor growth. However, these symptoms can be nonspecific and may resemble those of other childhood illnesses, making JMML challenging to diagnose. A definitive diagnosis is typically made through a combination of physical examinations, blood tests, and bone marrow biopsies. It is important for healthcare professionals to have a high level of suspicion and to consult with pediatric hematologists when JMML is suspected to ensure accurate diagnosis and appropriate management of this complex disease.
JMML Treatment Options: Current Approaches
Treatment options for Juvenile Myelomonocytic Leukemia (JMML) aim to control the disease and alleviate symptoms, with the ultimate goal of achieving a long-term remission. Due to the rarity and complexity of JMML, there is no standard treatment approach, and management decisions are made on a case-by-case basis. Currently, the most common treatment modalities for JMML include chemotherapy, hematopoietic stem cell transplantation (HSCT), and targeted therapies. Chemotherapy, often in combination with low-dose radiation, may be used to reduce the number of abnormal cells and induce remission. HSCT, utilizing donor stem cells, is considered the only potentially curative option for eligible patients and involves replacing the diseased bone marrow with healthy cells to restore normal blood cell production. Additionally, targeted therapies that specifically target genetic mutations associated with JMML are being explored, offering the potential for more personalized and effective treatment strategies. It is important for patients and their families to work closely with a multidisciplinary team of healthcare professionals experienced in managing JMML to determine the most appropriate treatment plan based on individual factors and disease characteristics.
The Role of Cord Blood Banking
Cord blood banking plays a significant role in the field of regenerative medicine and offers potential benefits for patients with various hematological disorders, including Juvenile Myelomonocytic Leukemia (JMML). Cord blood, collected from the umbilical cord and placenta after childbirth, contains a rich source of hematopoietic stem cells (HSCs) capable of differentiating into various blood cell types. These HSCs can be used in hematopoietic stem cell transplantation (HSCT) procedures, providing a potential source of healthy cells to replace the diseased bone marrow in patients with JMML. HSCT utilizing cord blood has several advantages, such as reduced risk of graft-versus-host disease and increased availability, as cord blood units can be stored in public cord blood banks for potential matching with unrelated donors. The use of cord blood banking in JMML treatment highlights its potential in providing a curative option for eligible patients and underscores its role in advancing the field of regenerative medicine.
Advantages of Cord Blood Treatment
The advantages of cord blood treatment extend beyond its potential use in Juvenile Myelomonocytic Leukemia (JMML) therapy. Firstly, cord blood collection is a non-invasive and painless procedure that can be performed during childbirth without any risk to the mother or the newborn. Additionally, cord blood is readily available and can be stored in public or private cord blood banks for future use. This easy accessibility eliminates the need to find a matched donor, which can be a time-consuming and challenging process for patients in need of a transplant. Moreover, cord blood transplantation has a lower risk of graft-versus-host disease compared to other transplant sources, such as bone marrow or peripheral blood. This reduced risk makes cord blood transplantation a suitable option for patients who may not have a fully matched donor available. Overall, the advantages of cord blood treatment make it a valuable resource in the field of regenerative medicine, providing hope for patients with various hematological disorders, including JMML.
How Cord Blood Can Help
Cord blood has been found to be a rich source of hematopoietic stem cells, which are capable of differentiating into various blood cell types. This unique characteristic makes cord blood an invaluable resource in the treatment of not only JMML but also other blood disorders, immune system deficiencies, and certain genetic conditions. In the case of JMML, cord blood transplantation can offer a potentially life-saving option by replacing the dysfunctional bone marrow with healthy stem cells from a cord blood unit. These transplanted cells can then restore normal blood cell production and function, leading to improved health outcomes for patients. Furthermore, the use of cord blood transplantation has shown promising results in reducing relapse rates and improving overall survival rates in patients with JMML. Therefore, cord blood banking and its potential for therapeutic use represent a significant advancement in the field of medicine, offering hope and improved treatment options for individuals facing serious medical conditions.
Potential for a Cure
With ongoing advancements in medical research and technology, there is a growing potential for a cure for Juvenile Myelomonocytic Leukemia (JMML). Scientists and clinicians are continuously striving to develop new treatments and therapies that can target the underlying causes of this rare and aggressive disease. One promising avenue of research is focused on the use of targeted therapies that specifically inhibit the genetic mutations responsible for JMML. By identifying and targeting these mutations, researchers aim to disrupt the disease progression and potentially achieve a cure. Additionally, the field of immunotherapy, which utilizes the body's own immune system to fight cancer cells, shows promising results in JMML treatment. This includes therapies such as CAR-T cell therapy, which involves modifying a patient's own immune cells to specifically target and eliminate JMML cells. While more research is needed, these advancements offer hope for a future where a cure for JMML is within reach.
Reducing Risk of Relapse
Reducing the risk of relapse is a crucial aspect of managing Juvenile Myelomonocytic Leukemia (JMML) and improving long-term outcomes for patients. After undergoing initial treatment, it is essential to implement strategies aimed at preventing the reoccurrence of the disease. Regular monitoring and follow-up appointments with healthcare professionals are key in detecting any signs of relapse at an early stage. Additionally, adherence to prescribed maintenance therapy and medication regimens is vital in maintaining remission and reducing the likelihood of relapse. Lifestyle modifications, such as adopting a healthy diet, engaging in regular physical activity, and managing stress levels, can also contribute to overall well-being and potentially lower the risk of relapse. By implementing a comprehensive approach that combines medical interventions, ongoing monitoring, and positive lifestyle choices, the aim is to minimize the risk of relapse and ensure the best possible outcomes for individuals with JMML.
Improving Survival Rates
One of the primary goals in managing Juvenile Myelomonocytic Leukemia (JMML) is to improve survival rates for patients. Achieving this requires a multi-faceted approach that encompasses various aspects of care. Firstly, early diagnosis is crucial. Timely identification of JMML allows for prompt initiation of appropriate treatment strategies, which can significantly impact survival outcomes. Additionally, advancements in medical research and technological innovations have paved the way for the development of targeted therapies and personalized treatment options. These advancements have shown promising results in improving overall survival rates for JMML patients. Moreover, ongoing clinical trials and collaborative efforts among healthcare professionals and researchers continue to drive progress in identifying novel therapeutic approaches that can further enhance survival rates. By constantly striving for innovation, implementing tailored treatment plans, and continuously monitoring patients' progress, the medical community aims to optimize survival rates and provide patients with the best possible chance for a positive outcome.
Importance of Early Detection
Early detection plays a critical role in the management of various medical conditions, including Juvenile Myelomonocytic Leukemia (JMML). Timely identification of JMML enables healthcare providers to intervene and initiate appropriate treatment strategies promptly. This early intervention can significantly impact the prognosis and overall survival rates for affected individuals. In the case of JMML, early detection allows for close monitoring of the disease progression, early initiation of chemotherapy or stem cell transplantation, and the possibility of exploring targeted therapies. Moreover, early detection facilitates the implementation of supportive care measures to manage symptoms and improve the quality of life for patients. By emphasizing the importance of early detection and raising awareness among healthcare professionals and the public, we can potentially improve outcomes for individuals affected by JMML and other similar conditions.
Hope for Children with JMML
Despite the complexities and challenges associated with Juvenile Myelomonocytic Leukemia (JMML), there is hope for children and families facing this rare disease. With advancements in medical research and treatment options, there are now more opportunities for improved outcomes and enhanced quality of life for children with JMML. Multidisciplinary teams of medical professionals, including hematologists, oncologists, and geneticists, are dedicated to providing comprehensive care and exploring innovative therapies. From targeted treatments to hematopoietic stem cell transplantation, these interventions offer possibilities for remission and long-term survival. Additionally, ongoing research and clinical trials continue to expand our understanding of JMML, paving the way for future breakthroughs and improved treatment strategies. Through collaborative efforts and continued support, there is a collective commitment to bring hope and progress to children with JMML and their families.In conclusion, Juvenile Myelomonocytic Leukemia (JMML) is a rare and aggressive form of childhood leukemia that requires immediate and specialized treatment. While the exact causes of JMML are still being studied, cord blood banking has shown great potential in providing a source of healthy stem cells for transplantation, which can greatly improve the chances of survival for children with JMML. By educating ourselves on the importance of cord blood banking and supporting research efforts for JMML, we can help give hope to families affected by this devastating disease.
FAQ
What is Juvenile Myelomonocytic Leukemia (JMML) and how does it differ from other types of leukemia?Juvenile Myelomonocytic Leukemia (JMML) is a rare childhood cancer characterized by abnormal growth of blood cells. It differs from other types of leukemia as it primarily affects young children, typically under the age of 4, and is caused by genetic mutations rather than environmental factors. JMML is also unique in its aggressive nature, lack of response to traditional chemotherapy, and high risk of transformation into acute leukemia. Treatment often involves stem cell transplantation and targeted therapies due to its distinct biological and clinical features compared to other forms of leukemia.How does cord blood banking play a role in treating JMML and other pediatric cancers?Cord blood banking plays a crucial role in treating JMML and pediatric cancers by providing a rich source of hematopoietic stem cells for transplantation. These stem cells can be used to replace damaged or cancerous cells in the patient's bone marrow, allowing for the development of new healthy blood cells and a potential cure for their condition. By storing cord blood at birth, families ensure they have access to this valuable resource if needed for potential treatment of JMML or other pediatric cancers in the future.What are the benefits of using cord blood for stem cell transplants in children with JMML?Cord blood is a valuable source of stem cells for children with Juvenile Myelomonocytic Leukemia (JMML) as it offers a higher likelihood of finding a suitable donor match due to its relative genetic flexibility. Additionally, cord blood transplants have shown lower rates of graft-versus-host disease and provide faster access to treatment, which is crucial in JMML cases. These transplants also offer a reduced risk of viral infections and can be stored for future use. Overall, utilizing cord blood for stem cell transplants in children with JMML can significantly improve treatment outcomes and quality of life.Can cord blood banking be used as a preventative measure for children at risk of developing JMML?Cord blood banking is not a preventative measure for children at risk of developing Juvenile Myelomonocytic Leukemia (JMML) as JMML is a rare and complex genetic disorder that is not currently preventable through cord blood banking. However, cord blood stem cells can be used in the treatment of certain blood disorders, including leukemia, through stem cell transplantation. It is important for families with a history of JMML or other genetic disorders to consult with healthcare professionals for personalized guidance on preventive measures and treatment options.What advancements have been made in using cord blood for treating JMML, and what is the potential for future research in this area?Advancements in using cord blood for treating JMML include successful hematopoietic stem cell transplants leading to improved survival rates. Future research in this area could focus on optimizing transplant protocols, further understanding the immune response in JMML, and exploring new therapeutic strategies such as gene therapy. Continued research has the potential to enhance treatment outcomes, reduce relapse rates, and ultimately improve the long-term prognosis for JMML patients. Read the full article
#cordbloodbankJuvenileMyelomonocyticLeukemia(JMML)#JuvenileMyelomonocyticLeukemia(JMML)cordbloodbanking
0 notes