Don't wanna be here? Send us removal request.
Text
DOING, BEING AND BECOMING IN COMMUNITY BLOCK

Credit: Rachel Levett, 2025
There are several things that I have learnt thus far from the Community block. It has been a part of what Wilcock (1999) calls “doing, being and becoming”. I am engaging in the work of a student Occupational Therapist (OT) by working with clients at the clinic “doing” assessments and treatment to become a professional OT. We also do programmes where we go into the community to creches, primary and high schools looking for at-risk children and working with remediating them. Through doing this, I am “being” and discovering who I am as an OT. I am learning how to approach and interact with clients and seeing that I have much more space to grow in my handling. I am at the very early stage of “becoming” an OT. I am learning the steps through doing and being to eventually becoming a professional OT.
A stand-out point of community work is stakeholder engagement and advocacy with a purpose. Advocacy is defined as “any action that speaks in favour of, recommends, argues for a cause, supports or defends, or pleads on behalf of others” (Alliance for Justice, 2025: para 1). But advocacy can’t be done for the sake of just doing something. There should be a well-thought-out purpose for performing advocacy. This was seen with Dalton creche where an organisation called Montessori Internationale wanted to relocate the creche from its current placement in Umbilo to Davenport Park. It was unclear why, but the councillor did not agree with the creche being placed at the park. As the OT students, we were asked by Montessori Internationale to write a letter stating as to why the park would be a better environment than Umbilo, where the creche is currently located. Even though we could see that the Park would be a cleaner and healthier location, we hesitated to write the letter as we did not know all the details surrounding the move and we had not consulted our main stakeholder, the Denis Hurley Centre (DHC). The DHC told us not to get involved and direct Montessori Internationale to them. This showed me that different stakeholders have different views and agendas, and we should take into account the view of our main stakeholder, see if we agree with them or not and then proceed.
I feel that many of the projects we do are trying to improve occupational justice where the playing field is levelled through access to health services for the socio-economically disadvantaged. This is commendable, but without a permanent community occupational therapist in Cato Manor, our actions may be piecemeal.
Community block has at times been difficult and at times frustrating but it is a huge learning experience with many lessons to take into community service.
If you would like to know more about Ann Wilcock's “doing, being and becoming” see https://onlinelibrary-wiley-com.ukzn.idm.oclc.org/doi/10.1046/j.1440-1630.1999.00174.x
More information on Montessori Internationale and their practices can be found at https://montessori-ami.org/
To learn more about the Denis Hurley Centre and their projects visit https://www.denishurleycentre.org/
REFERENCES
Alliance for Justice. (2013, October 1). What is advocacy? https://afj.org/resource/what-is-advocacy/
Levett, R. (2025). What is occupational therapy? Healing and Hope for Her. Retrieved March 28, 2025, from https://www.healingandhope.com.au/what-is-occupational-therapy
Wilcock, A. A. (1999). Reflections on doing, being and becoming. Australian Occupational Therapy Journal, 46(1), 1–11. https://doi.org/10.1046/j.1440-1630.1999.00174.x
0 notes
Text
FIVE SUSTAINABLE DEVELOPMENT GOALS IN PRACTICE IN COMMUNITY FIELDWORK

Photo credit: Biobin, 2025
In 2015, the 2030 Agenda for Sustainable Development, was adopted by all United Nations Member States (UN, 2025). This agenda includes 17 goals to which each country must strive to eradicate life challenges faced by many in the world (UN, 2025).
For my Community Theory and Fieldwork block in the 4th year of Occupational Therapy (OT), I can see that we work toward the following 5 goals which are zero hunger, good health and well-being, quality education, decent work and economic growth, and reduced inequalities.
Zero Hunger involves ending hunger, achieving food security, and promoting sustainable agriculture. Good Health and Well-Being involves ensuring healthy lives and promoting well-being for all at all ages. Quality Education is to ensure inclusive and equitable quality education and promoting lifelong learning opportunities. Decent Work and Economic Growth promotes inclusive and sustainable economic growth, employment, and decent work. Reduced Inequalities involves reducing inequality within and among countries (UN, 2025).
The project that targets good health and well-being is working at the Cato Manor Clinic, seeing clients and performing health promotion talks. Also screening children at the Philamtwana Clinic and performing maternal mental health promotion talks there. These activities promote good health and well-being by treating clients and getting them to seek help if they are unwell.
Quality education is done through a programme with the Mayville Secondary grade 9s where they learn life skills, career development and coping skills. This promotes lifetime learning opportunities by showing them options to study further and how to handle the stresses of school and daily life. We also try for inclusive education by targeting students with developmental delays in the Mayville Primary School and Golden Future creche and to rectify it by planning treatment activities with them.
Decent work is done through career talks with the high school children to showcase careers that would secure them good jobs. Also, I worked one-on-one with a client to prepare her business pamphlet and advised her on where she could join a business incubator for her craft products.
For partnership, the UKZN OT department has partnered with the Denis Hurley Centre to assist with their programmes for the homeless, refugees and drug users. We currently assist at their Dalton Creche with education, fine and gross motor and social interaction skills.
Through implementing all of the above programmes we are trying to reduce inequalities by giving people and children access to better health care and opportunities for learning and growth.
Therefore, these are the ways that I see us using 5 of the SDGs to further its mission in the Community Theory and Fieldwork Block in Cato Manor and the Denis Hurley Centre.
For further details on the 17 goals on the 20230 Agenda of Sustainable Development please visit the following website https://sdgs.un.org/goals
If you would like to get involved with the Denis Hurley Centre their details can be found on the following website https://www.denishurleycentre.org/page/volunteering-in-durban
A good place to start if you would like assistance with your business is the Small Enterprise Development Agnecy (SEDA). They can found at https://www.seda.org.za/
References
Biobin South Africa. (2025). Our commitment to the Sustainable Development Goals. https://biobin.co.za/our-commitment-to-the-sustainable-development-goals/
Denis Hurley Centre. (2025). Volunteering in Durban. https://www.denishurleycentre.org/page/volunteering-in-durban
Small Enterprise Development Agency. (2025). Home. https://www.seda.org.za/
United Nations. (2025). The 17 goals. United Nations Sustainable Development Goals. https://sdgs.un.org/goals
0 notes
Text
Community Practice and Primary Health Care in the UKZN Occupational Therapy Curriculum – My Reflections

Credit: UKZN OT
The University of KwaZulu-Natal’s (UKZN) Occupational Therapy (OT) curriculum has two modules that directly teach about working in communities, namely the Community Studies module in the first year and the Community Theory and Fieldwork module in the fourth year of the degree (UKZN, 2025). Interspersed throughout the degree are lessons on Primary Health Care (PHC) and advocacy.
My first year Community Studies module was during COVID-19, and hence, we never stepped into any actual community. Instead, we experienced the community we learnt about through videos and via Zoom meetings with the community leaders and members. This did not provide us with a comprehensive interaction at a community level. The course, though, did try to provide robust conversations about communities within low socio-economic environments and the lived realities of those within them.
What has been eye-opening for me is that my initial idea was that PHC referred to just clinics and clients receiving basic medication. It was the level at which most basic healthcare services were offered. But I learnt that in South Africa, PHC is delivered through clinics, community health centres (CHCs), mobile health services, and district hospitals, with an emphasis on interdisciplinary teamwork, including nurses, doctors, occupational therapists, physiotherapists, and community health workers. The approach aims to reduce hospital admissions, manage chronic diseases, and improve public health outcomes, particularly in rural and underserved communities. PHC follows a preventative, promotive, curative, and rehabilitative approach, ensuring that people receive essential healthcare at the first point of contact before requiring specialized medical services (DoH, 2017).
During the OT degree, we have also learnt about advocacy and advocating for the vulnerable in communities in terms of improving their healthcare. These teachings are highly significant because we learnt how to put ideas into action by going through the various government and community channels to achieve our outcome. Advocacy should be taught earlier in the degree as it is the practical manner in which to assist people or communities in need.
It is during the fourth year of the Community Theory and Fieldwork block that much of the theory learnt is implemented, and the reality of marginalised communities is observed. In the third year, some time is spent within marginalised communities, but in 4th year, working in disadvantaged communities is where it all ties in together, and as students, we exponentially grow.
Thus, the pros of the OT degree are that we learn about working in local communities, advocating for our clients and the model of PHC. However, the cons are that we did not have actual exposure to disadvantaged communities from the first year, which makes our learning theory heavy, but practically, we do not know how to implement community change. More exposure to local community environments from the beginning and projects around advocacy can be included into the degree.
If you would like to learn more about Primary Health Care (PHC), the following video is informative.
Credit: Health-e News Service
If you would like to learn more about the UKZN OT curriculum, please visit the university’s website at https://ot.ukzn.ac.za/undergraduate-programmes/
References
Health-e News Service. (2015). National Health Insurance Primary Health Care - An Introduction https://youtu.be/M_u0SV9wLro?si=t8JW1FUDqixlSeYw
National Department of Health. (2017). White Paper on National Health Insurance: Towards Universal Health Coverage. Government of South Africa. Retrieved from https://www.health.gov.za/
University of KwaZulu-Natal. (2025). Discipline of Occupation Therapy Undergraduate Programmes. https://ot.ukzn.ac.za/undergraduate-programmes/
0 notes
Text
BENEFITTING SOCIETY THROUGH PRIORITISING THE HEALTH CARE OF MOTHER’S AND THEIR CHILDREN

Photo credit: Georges Gorbet/AFP/Getty Images
Maternal health refers to a mother's well-being throughout pregnancy, childbirth, and the postpartum period. Child health encompasses a child's well-being from birth to adolescence, with a primary focus on the early years, particularly from birth to five years old (Perez, 2023).
According to the World Health Organisation (WHO) good maternal and child health (MCH) has several benefits for the economy and society. The WHO found a direct correlation between investing in MCH and positive outcomes. With every $1 spent on supporting MCH, returning $7 in economic benefits through decreased healthcare costs, increased productivity and healthier generations to come (Adotey 2024). Furthermore, maternal and child health serves as a key measure of a population's overall well-being and has a direct influence on economic and social progress. Since the health of mothers and children is closely connected to the health of communities and societies, it plays a crucial role in shaping broader development outcomes (Jamaluddin, 2024).
But South Africa is a country where two opposite realities live in one space side-by-side. On the one hand, there is the advanced first-world reality experienced by a minority of the country, and on the other hand, a dystopian third-world reality suffered by the majority of the population. For instance, South Africa has a two-tier healthcare system, with the public sector utilised by 71% of the population being bankrolled by the state and under-resourced. In contrast, the private sector, used by 27% of the population, is funded by medical aid and well-resourced (Rensburg, 2021).
This disparity clearly emerged when in 2018 it was estimated that there was “one government-employed doctor for every 2,457 people not covered by medical aid” (Skosana, 2018: para 37) and “in private care, one medical aid-registered doctor sees between 429 and 571 people” (Skosana, 2018: para 37). This shows the vast doctor-to-patient ratio of care services for those in the public versus private sector.
Cato Manor, 5km west of Durban’s CBD, is a township where the residents access public health care. For 7 weeks, my prac partner and I will be placed at the Cato Manor Clinic for our 4th year Occupational Therapy Community block. In our one week there thus far, we have seen several children up to the age of seven years old with developmental delays. They are assessed and treated in a short period of time with a follow up consultation given for one month’s time. This, to me, seems like a short treatment timeline that is not intense enough to bring about a difference to the child or caregiver. Caregivers are advised on home activities to carry out with the children. How well these are implemented is unknown.
There are maternal and child health programmes run in the Cato Manor community and as students we perform health promotion around the topic. But it seems we never evaluate our projects to see if they have been of true benefit to the end-user or to what extent.
Like the lack of doctors in public hospitals, there are no permanent community occupational therapists (OT) who service the community by going into it. It is only the 4th year UKZN OT students who do so. Furthermore, there is no permanent occupational therapist employed at the clinic but only one community service OT. This hinders continuous service of care and programmes by OT’s that know the community and its health challenges.
We in South Africa, particularly in places like Cato Manor need to heed the WHO’s call for more investment into MCH. It would have more positive social and economic outcomes for all.
If you would like to read the articles I referenced, please see the reference list below:
References
Adotey, S. K. (2024, September 16). How investing in maternal and child health fuels prosperity for women, young people, and children in Africa. World Economic Forum. https://www.weforum.org/stories/2024/09/how-investing-in-maternal-and-child-health-fuels-prosperity-for-women-young-people-and-children-in-africa/
Jamaluddin SMH. (2024). Saving Lives, Building Futures: Importance of Maternal and Child Health in Achieving the Sustainable Development Goals. medtigo J Med. 2024;2(4):e14349403. doi:10.5281/zenodo.14349403
Perez, R. (2023). CMSA’s Integrated Case Management: A manual for case managers by case managers, 2nd Edition
Rensburg, R. (2021, July 6). Healthcare in South Africa: how inequity is contributing to inefficiency. The Conversation. https://theconversation.com/healthcare-in-south-africa-how-inequity-is-contributing-to-inefficiency-163753
Skosana, I. (2018, August 7). Does one SA doctor treat 4,000 patients in public care, but fewer than 300 privately? Africa Check. https://africacheck.org/fact-checks/reports/does-one-sa-doctor-treat-4000-patients-public-care-fewer-300-privately#:~:text=Using%20this%20coverage%20data%2C%20the,public%20healthcare%20sector%2C%20Day%20said.
The contact details for Cato Manor Clinic are:

0 notes
Text
THE STATE OF THE SOUTH AFRICAN MENTAL HEALTH BUDGET

Credit: Getty Images
In the annual Mental State Report of the World (2021) which ranked 34 countries, South Africa ranked as one of the lowest for its mental health (Msomi, 2022). One in three South Africans experiences a mental illness and 75% of them are unable to access treatment. Yet despite this only 5% of the national public health budget is spent on mental health (SASOP, 2020).
Interesting to note is that common and treatable mental health illnesses have overtaken physical illnesses and injuries as the main cause of medical disability claims in South Africa (Docrat et al, 2019). But not only is South Africa’s mental health budget small it is also mis-directed by being hospital-centric and reactive. It works on treating the most severe conditions which only have a prevalence of 1% instead of trying to prevent or provide early intervention and treatment for the common mental health illness like anxiety and depression before they become a worse mental illness burden (Docrat et all, 2019).
This misdirection in the focus of the budget can further be seen in that almost 20% of the mental healthcare budget is allocated to hospital re-admissions. This is known as the “revolving door syndrome” where the issue is not nipped in the bud through better care at the primary and community level (Docrat et al, 2019). Primary health care services do not include regular screening for common mental disorders, such as depression, anxiety, postnatal depression and substance abuse, even though there are simple to use tools for such screenings (Mokwena and Mokwena, 2021).
The budget for primary mental health care services is only 8% of the overall mental health budget but this is where community psychiatry can work to prevent mental illness and ensure early treatment that prevents mental health conditions becoming disabilities (SASOP, 2020).
More can be done in the primary health sector with a greater budget allocation and political will such as more screenings, active health promotion of mental health problems, the provision of treatment with well resourced teams and on-going support that follows up with clients (Mokwena and Mokwena, 2021).
The new National Mental Health Policy Framework and Strategic Plan 2023 – 2030 brings some hope to budget concerns. It states that “budget will be allocated to meet targets set for the implementation of the policy and regular discussions will be held with provinces to discuss strategies and monitor progress with implementation. At provincial level, mental health budgets will be reviewed annually to align mental health with national priorities, for each of the areas for action in 2023 and annually thereafter” (Dept of Health, 2023: 38).
How this implementation will play out, we will have to wait and see.
Further Reading
The Mental State of World report for 2021 and 2022 can be found at https://mentalstateoftheworld.report/ They provide interesting data of what is happening around the world in terms of different countries mental state.
From the same research company who does the Mental State of the World report, you can find your mental wellbeing score. Take the test here https://sapienlabs.org/mhq/
If you would like to see a review of South Africa’s budget for 2023 visit https://www.treasury.gov.za/documents/national%20budget/2023/review/FullBR.pdf
To learn about primary health as explained the World Health Organisation (WHO), please see https://www.youtube.com/watch?v=QX7Q0a8GxaA
______________________________________________________________
References
Department of Health. (2023). National Mental Health Policy Framework and Strategic Plan 2023 – 2030. Accessed from https://www.spotlightnsp.co.za/wp-content/uploads/2023/04/NMHP-FINAL-APPROVED-ON-30.04.2023.pdf
Docrat, S., Besada, D., Cleary, S., Daviaud, E. and Lund, C. (2019). Mental health system costs, resources and constraints in South Africa: a national survey. Accessed from https://academic.oup.com/heapol/article/34/9/706/5572608?login=false
Getty Images. (2023). Varied new South African Mandela banknotes with coins. Accessed from https://www.gettyimages.com/photos/south-african-currency
Mokwena, K.E and Mokwena, V.A. (2021). The Need to Strengthen Primary Health Care Services to Improve Mental Health Care Services in South Africa. Accessed from https://www.intechopen.com/chapters/78257
Msomi, N. (2022). Mental health in SA ranked among the worst in the world. Accessed from https://www.news24.com/life/archive/mental-health-in-sa-ranked-among-the-worst-in-the-world-20220315
South African Society of Psychiatrists. (2020). SA’s mental health needs better funding. Accessed from https://www.sasop.co.za/mentalhealthfunding
0 notes
Text
Silver Linings Playbook Through the Eyes of An OT Student
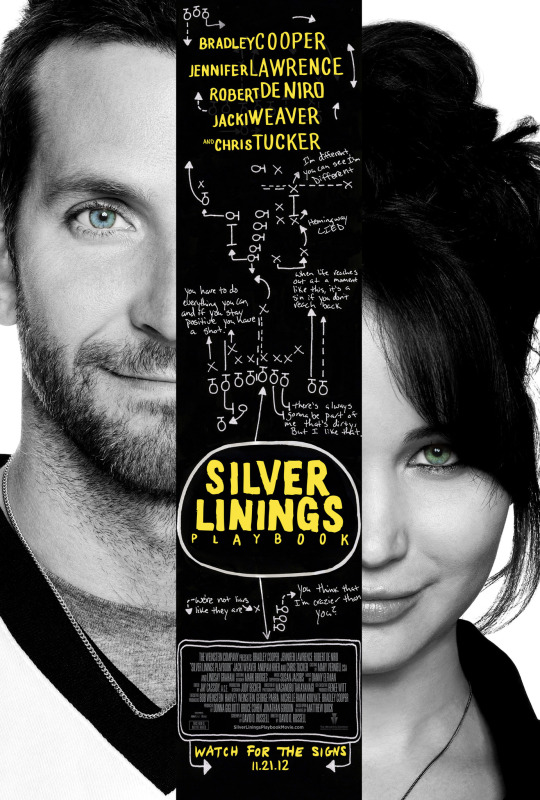
Image Credit: IMDB
Silver Linings Playbook (2012) is a film that deals with the male lead, Pat, having bi-polar disorder and the female lead, Tiffany, having depression. Pat has just come out of psychiatric hospital after 8 months. He was sent there for violently beating his ex-wife’s lover when he found them together in the shower. Having previously watched the film, I knew that the film was interesting with intense characters but watching it now with an OT lens I have a vocabulary to describe the characters and their behaviour that I did not have before.
Pat completely lacked insight as he believed he could get back together with his ex-wife that had a restraining order against him. He was initially non-compliant with taking his medication. In his manic moods he would wake his parents up in the middle of the night to tell them that a Hemmingway novel he just read had an awful ending. I got to see how difficult it was for his family to live with him. Yet they still supported him the best way they could. They made sure he went for his therapy sessions, included him in family events and reminded him to take his medication. With their support and taking his medication he found some stability at the end.
For client prognosis we talk about available support systems and how it would help the client. Pat had a very strong support system in his family and friends that proved positive for his well-being. I would thus give him a good functional prognosis. And he gained insight into his condition at the end such that he did not want to reunite with his ex-wife. Since coming out of jail, re-uniting with his ex-wife had been his sole purpose but in the end, he realised Tiffany was better for him.
Pat and Tiffany had the goal of taking part in a dance competition. Practicing for the event gave them a lot of structure to their routine and gave them discipline. It showed how a purposeful activity is beneficial for people. This reminded me of OT where activities are used for therapeutic purposes to bring about healing. Dancing was a meaningful activity for them and the competition gave them a goal.
Tiffany saw in Pat someone who experienced mental illness and took a liking to him. This reminds me of Yalom’s therapeutic factors. Even though his factors refer to groupwork, it can also be seen in this pair. The audience sees their instillation of hope as they find a shared goal, universality as Tiffany sees that there is someone like her in Pat, and imparting of information as they discuss the different medications they have taken and its affect on them.
I would recommend watching Silver Linings Playbook for anyone experiencing a mental illness, those that support them and those that treat people with mental illness. It shows the difficulties experienced but still gives a sense of hope.
Here is a link to the full movie of Silver Linings Play Book: https://www.youtube.com/watch?v=ZgPIEFgRlrU
Other films with a mental health theme that are interesting to watch are:
Rain Man (1988) https://www.youtube.com/watch?v=mlNwXuHUA8I About two brothers who meet for the first time. One is autistic and the other in debt. The autistic brother’s number counting skills allow him to win at the casino. A dream for the brother in debt.
Tim and Mary (1996) https://www.youtube.com/watch?v=WwpVLAhDxtM&t=15s (full film). Tim has an intellectual impairment and falls in love with an older woman.
A Beautiful Mind (2001) https://www.youtube.com/watch?v=EajIlG_OCvw About a mathematician who has schizophrenia.
Still Alice (2015) https://www.youtube.com/watch?v=ZrXrZ5iiR0o Alice a Professor gets early onset Alzheimer’s.
------------------------------------------------------------------------------
References
IMDB. (2012). Silver Linings Playbook. Accessed from https://www.imdb.com/title/tt1045658/
0 notes
Text
I Bring Change Into My OT Practice Through My Therapeutic Use Of Self

Credit: Hiwell
Chamberlain (2022) talks about the six modes of the therapeutic use of self, based on the Intentional Relationship Model (Taylor et al., 2009). I will look at each mode and how I have implemented them in my practical field work over the last two years.
The first is advocating which is “standing up for the patient and providing them with additional resources to enhance the therapeutic process” (Taylor et al., 2009). In the public hospital of Prince Mshiyeni, I had a client whose bandages had not been changed the entire weekend. His pressure sores were worsening. This led to me politely asking the nurses to change his bandages. They initially said they did not have bandages in their unit but after a while brought some from elsewhere. Thus, there are times when I have advocated for better treatment for my clients. His request to have his bandages changed had fallen on deaf ears with the nurses and hence I tried as best as I can to serve him.
The next mode is collaborating. This is about “including the patient in every aspect of planning and carrying out the therapeutic process” (Taylor et al., 2009). I always ask the client what their interests are and what is important for them to do in everyday life. Together we work on what will be done for the client.
Empathizing is “understanding the patient’s internal, emotional experiences during the therapeutic process” (Taylor et al., 2009). Through interviewing each of my clients, I learn a great deal of information about them and their lives. I imagine what it would be like to be them and what would be the challenges they face. This gives me an idea of how to assist them for treatment.
Encouraging is “��cheerleading’ or urging the patient to participate and progress” (Taylor et al., 2009). At times clients may not want to participate. At Kind Edward Hospital I had a client with burns on both his arms. He only wanted to sleep. But I explained to him that if he was not mobile, he would end up with contractures. Begrudgingly he performed the activities that I asked of him. I had to encourage him and speak about the benefits of doing the activities several times and then he participated.
I would say that linked to encouraging is instructing. This is where I “take on a teacher role to educate the patient” (Taylor et al., 2009). This was done with my burns client above to encourage him to participate in activities. And my client who came with pressure sores. As a paraplegic I taught him how and when to shift his body to prevent the sores. It was done through verbal instruction and a physical demonstration.
Lastly there is problem-solving. This is “working with the patient to reason through and analyze complex therapeutic situations” (Taylor et al., 2009). For example, a stroke client of mine at Prince Mshiyeni Hospital could not dress her lower body but had no trouble dressing her upper body. Together we thought through a plan of how she would dress her lower body when she is at home and then we practiced it in the hospital. She told me what furniture she had at home and we spoke about how she could reach her clothes and thereafter sit to dress.
After writing this blog I am pleasantly surprised to find that there are ways that I have been using myself therapeutically with my clients as an Occupational Therapy student. But there are times where it is easier to apply the therapeutic use of self than other times. For example, when a client does not want to cooperate it makes it more difficult for me as the therapist but all the more important for me to use therapeutic use of self to encourage them to participate and instruct them to help them understand the benefits of treatment. This highlights the importance of appropriate handling techniques. Occupational Therapy is a highly client centred profession where there is therapeutic use of self on a daily basis, therapists must ensure that they take care of themselves too and do not experience burn out. This is so that they continue being of therapeutic use to the client.
If you would like to watch videos that further explains therapeutic use of self, please see:
https://www.youtube.com/watch?v=hrS390deg5Q (therapeutic use of self: introduction)
or
https://www.youtube.com/watch?v=UFmcWq__0ig (therapeutic use of self short)
Here are a few examples of therapeutic use of self: https://www.youtube.com/watch?v=H1aqiZmvLpQ
or
youtube
______________________________________________________________
References
Chamberlain, M. (2022). How To Use Therapeutic Use Of Self In Occupational Therapy. Accessed from https://otflourish.com/therapeutic-use-of-self-occupational-therapy/
Taylor, R.R., Lee, S.W., Kielhofner, G., & Ketkar, M. (2009). Therapeutic Use of Self: A Nationwide Survey of Practitioners’ Attitudes and Experiences. American Journal of Occupational Therapy, March/April 63(2).
0 notes
Text
From Ugly Duckling to Beautiful Swan: How Mental Health Care Should Transform to Centre Stage

Credit: WHO
Two of the most common mental health conditions, depression and anxiety, cost the global economy US$ 1 trillion per annum. Despite these figures, the global median of government health spending that goes to mental health is less than 2% (WHO, 2023). Mental health is one of the most neglected areas of health globally. There are several reasons why mental health has been ignored. “The first one is an associated stigma. The second is a perception of mental health disorders as a “luxury good”, as opposed to actual illnesses. The additional top reasons include a fragmented and outdated service model. Some of these include the provision of mental health services mainly in psychiatric hospitals, severe lack of preventative mental health service; lagging policy changes and also a shortage of human resources” (Kovacevic, 2021: no page).
So, what can be done to overcome these barriers? It has been suggested that mental health care be integrated into primary health care. The benefits of integrating mental health into primary healthcare are great. Firstly, integration ensures that the population as a whole has access to the mental healthcare that they need early in the course of disorders and without disruption. Secondly, when people receive treatment in primary healthcare facilities the likelihood of better health outcomes, and even full recovery, as well as maintained social integration is increased (Funk et al, 2008).
“It is important to emphasise that mental healthcare delivered in a primary health care setting is much more likely to be effective and sustainable if complimented by a strong secondary level of care to which primary healthcare workers can turn to for referrals, as well as for support and supervision. Having in place strong informal community mental health services and support groups, run by NGOs and faith-based organisations can also compliment and strengthen the services provided through primary healthcare services” (Funk et al, 2008: no page).
In terms of the above it now makes sense for our group to have done health promotion on depression at the community level in a clinic at Mariannridge. The clinic furthermore offers the services of a counsellor one day a week. But much more could be offered at the clinic with posters on different aspects of mental health being put up and made visible. Informal support groups could be initiated with a monthly meeting to discuss mental health matters. And further mental health promotion can be done. The need for these initiatives is massive.
Good mental health needs to start taking centre stage. It not only affects the person but the economy and society at large. The numbers are staggering. Currently, almost 1 billion people live with a mental disorder and in low-income countries, more than 75% of people with the disorder do not receive treatment. Annually, close to 3 million people die due to substance abuse. Every 40 seconds, a person dies by suicide. Roughly 50% of mental health disorders start by the age of 14 (Kovacevic, 2021).
It is expected that in the next ten years, depression will put more burden on nations than any other disease. Given the chronic nature of the disease, this translates into a significant economic impact worldwide. “According to the WHO, every $1 invested in mental health yields a $4 return on investment. In Ukraine, for example, it is estimated that for the period between 2017 to 2030, the country could save $2 on restored productivity and added economic value, if it invests $1 in the treatment of common mental disorders” (Kovacevic, 2021: no page).
Thus, investing in mental health has significant benefits for the person, society and the economy. With such great benefits it is imperative that mental health care no longer be seen as the Cinderella of Health Care but as Queen Elsa (of Frozen) taking centre stage. Would you not agree?
For Further Information:
The World Health Organisation has valuable data on the burden of mental health. You can find it at https://www.who.int/health-topics/mental-health#tab=tab_2
To learn more about integrating mental health into primary health care visit https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2777555/
If you would like to start a mental health support group in your area, the South African Depression and Anxiety Group (SADAG) can assist with learning how to do it. See here https://www.sadag.org/index.php?option=com_content&view=article&id=3212:start-a-support-group&catid=96:support-groups for more information.
If you would like to raise awareness on one of the most common mental health issues namely depression, find WHO flyers on the topic here https://www.who.int/campaigns/world-mental-health-day/2021/campaign-materials
______________________________________________________________
References
Funk et al. 2008. Integrating mental health into primary healthcare. Accessed from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2777555/
Kovacevic, R. 2021. Mental health: lessons learned in 2020 for 2021 and forward. Accessed from: https://blogs.worldbank.org/health/mental-health-lessons-learned-2020-2021-and-forward
World Health Organisation. 2023. Mental Health. Accessed from:https://www.who.int/health-topics/mental-health#tab=tab_1
0 notes
Text
Standing on the Edge of Glory: Almost an Occupational Therapist by Taking it One Step at a Time

Picture: Long queues at a clinic in KwaZulu-Natal. (Photo: Rian Horn / Ritshidze)
Introduction
"Occupational Therapy has been my most difficult degree thus far but I take one step at a time to continue toward my destination of finishing my degree". This is a sentence I often hear myself repeat in my mind to motivate myself. I have previous degrees in the Humanities including a postgraduate degree but even with this advanced degree, I believe the Health Sciences has the most challenging degrees to obtain. But why is a degree in the Health Sciences so challenging to complete? I narrow it down to three aspects. The environment, the clients and the course content. In turn I will examine each below.
Environment
Coming from a Humanities background in Economic Development and moving into Occupational Therapy (OT) has been an eye opener. Working in public health facilities has given me insight into the lives of ordinary South Africans more so than when I worked in the national government department of trade and industry. There I worked with mainly policy development whereas in this degree I see the conditions in which everyday people live and the health services they obtain which can be below service standards. For example, the cleanliness of some public hospitals is questionable as cockroaches are found in spaces in close proximity to hospital service users.
As students we may also travel into low-income areas to perform our fieldwork practical and this for me shows an entirely different side of South Africa compared to where I come from. This week, we travelled to Mariannridge and in our short walk of several hundred metres from the clinic to the library, we saw a man try to hold a woman against her will and she forcefully pushed him away, a group of three teenagers conducting card gambling with R5 and R10 bets and a group of street-guys calling out to us, the OT students, trying to be over-friendly. These were somewhat disturbing sights to see and experience.
Clients
As a student therapist we see clients at sometimes their weakest point suffering from a physical or mental illness and this in turn affects us emotionally. We work with them intimately and Occupational Therapy demands that we get to know the whole person in depth. Their life story can affect us on an emotional level but we need to learn to “toughen up”. Hence, in terms of an emotional toll the journey to becoming an Occupational Therapist has its rollercoaster ups and downs and learning to deal with uncomfortable feelings is a task I am still learning to master.
Course Content
Learning to become and think like an OT clinician has been a steep learning curve. From the Humanities I am accustomed to a learning and test style of developing arguments through essays on abstract concepts. In OT I have had to learn an entirely new vocabulary relating to this field, ways of understanding and analysing clients, and coming up with treatment intervention plans. This learning process I do not believe will stop as I become a professional OT but I will become more familiar with how to think like an OT and acquire broader knowledge of how to treat clients. But in this initial learning phase it has been difficult to grasp exactly how to manoeuvre as an OT therapist (to be). I am grateful for the year of community service to come where I will have the opportunity to hone my skills further after the degree.
Way Forward
The way forward is to breath and take it step by step. It’s great to have supportive friends within my 3rd year class at UKZN to laugh with about the challenges we face together. It’s also very motivating to imagine having the degree eventually and working, though there is a worry at the back of my mind of how easy it would be to find a job. But I believe I will find one and have a fulfilling career. Hope is a great motivator.
Conclusion
Obtaining any degree is always a challenge but I am now of the belief that a degree in the Health Sciences is slightly more challenging to obtain. Having to work in under-resourced environments with clients that are vulnerable in that they are ill and for me to know the theory and implementation of OT and how to conduct myself as a professional can at times seem like a mammoth task. But is it worth it? I would say yes because I find it more fulfilling than my previous office work in that you can see if you’ve made a change in another person’s life. Thus, if you would like to pursue a degree in Occupational Therapy or the Health Science sciences, I would advise you to think deeply about whether your personality and temperament are suited to this field. If you say yes, then jump all in and “take one step at a time” to make it to the end of your degree.
______________________________________________________________
If you would like to know more about studying Occupational Therapy at the University of KwaZulu-Natal (UKZN), please visit https://ot.ukzn.ac.za/
Good mental health is important while studying and if you are experiencing problems, please speak to someone. Seek out your campus Health services. There is also the South African Depression and Anxiety Group (SADAG) who you can contact for support. Visit https://www.sadag.org/ for further information.
You can perform a fun informal career assessment at https://www.truity.com/view/tests/personality-career to see which career may suit you.
If you would like to see what kind of jobs are available in Occupational Therapy visit https://za.indeed.com/q-occupational-therapist-jobs.html?vjk=73d15426d77805f6
0 notes
Text
Reflecting on Cultural Humility

Cultural humility is about being aware of one’s own biases when treating clients (Masters et al, 2019). It is a recognition of the power imbalances between the client and therapist (Yadav, 2023). When I am a patient, I am very aware of this imbalance while interacting with doctors. I see them as having all the answers and trust them. But this trust has resulted in me undergoing an unnecessary parathyroidectomy. There was no real need to remove it and now I am left with a visible scar on my neck which I despise. Thus, in future if I ever have any surgery again, I will seek a second opinion. Referring back to my blog on the importance of the multi-disciplinary health team (MDT) collaborating, my health care providers worked in silos and did not discuss my case which resulted in an unnecessary procedure. In their defence though they were not all based at the same hospital but received each other’s referral notes.
Now that I am training to be an Occupational Therapist (OT), I need to realise that clients may implicitly trust me when I become a qualified therapist. That is a turn of the tables and places a heavy weight of responsibility upon my shoulders. I am cognisant that I may not know all the answers and may need to refer to a more experienced OT or ensure that I work within the MDT to ensure holistic treatment for the client.
On the other hand, the opposite can also occur. As I am not of the same culture as my clients or speak their language*, my assessments and treatment sessions can be taken for granted. But this may also be due to a language barrier and not understanding me. For me not being able to speak isiZulu is a shame and I feel guilt that I may not be able to treat clients as effectively as possible. Growing up in Durban (which is in the KwaZulu-Natal province of the Zulu people) I learnt pidgin isiZulu known as “fana kalo” but this can hardly be used with clients. I have bought a course on speaking isiZulu but learning the words and sentence construction takes dedication. Having been in a schooling system that taught me Afrikaans for about 10 years up to matric, I feel I could pick up speaking Afrikaans more easily. Many of the language’s words are already in my head. But Afrikaans is hardly spoken in KwaZulu-Natal. Hopefully during my community service my isiZulu speaking skills will grow.
If I am honest with myself, I may also think that if one is of a lower socio-economic status they may not have as much intellectual insight into their diagnosis as someone who is more educated. The question though is, does this affect the compliance levels of the person with the lower socio-economic status. Or do they still take their medication for instance even if they do not know the full reason for why they are taking it. For example, the doctor told them to take it, so they do (again the client trusting the health care provider implicitly). Conversely, I know people of high socio-economic status that even if they have intellectual insight into their disease like diabetes for example, they do not take the steps to lead a healthy lifestyle. Hence writing about it now, I see I am mistaken in thinking that if one is of a lower socio-economic status they may not be as compliant in healing themselves as a person of higher socio-economic status. Compliance and client behaviour is difficult to predict.
In my hopefully long journey as an OT in the coming years, I am likely to unearth more biases that I hold about my clients and see more client-therapist power dynamics play out. With introspection I will hopefully pick up on them before they cloud my judgement so that I can treat my clients effectively taking into account their wishes.
*I am South African Indian, Muslim, female, English speaker and my clients are predominantly isiZulu speaking, black, South Africans.
______________________________________________________________
I referenced from the following articles:
Masters, C., Robinson, D., Faulkner, S., Patterson, E., McIlraith, T., & Ansari, A. (2019). Addressing Biases in Patient Care with The 5Rs of Cultural Humility, a Clinician Coaching Tool. Journal of general internal medicine, 34(4), 627–630. https://doi.org/10.1007/s11606-018-4814-y https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6445906/
Yadav. S. (2023). 10 Cultural Humility Examples. https://helpfulprofessor.com/cultural-humility-examples/
Important Links
If ever you experience detrimental challenges within the health system (public or private), you can submit a complaint to the Health Ombudsman at https://healthombud.org.za/ They exist to protect and promote the health and safety of users of health services in South Africa.
The isiZulu course I purchased can be found at Taalkor Language https://www.taalkor.co.za/zulu?gclid=CjwKCAjw36GjBhAkEiwAKwIWyS_W_VNj-snB1ty73KCSVKaeJeBq0FIFbvLVdM0iLLv5VjDuG6ed7hoCg3QQAvD_BwE
0 notes
Text
My Reflections on How I have used Evidence-Based Practice to Guide My Intervention
As Occupational Therapy (OT) students several tools are used to instil in us clinical reasoning skills. These tools implicitly use evidence-based practice (EBP) to guide our intervention. In today’s blog I will look at how my learning as an OT student at the University of KwaZulu-Natal (UKZN) integrates the use of EBP.
So, what is EBP?
The EBP model was developed in 2009 by American academics Satterfield, Spring and Mullen. It is the integration of the following components.

(Asha, 2023)
It was observed that when all the above components of EBP are considered together, clinicians can make informed, evidence-based decisions and provide high-quality services reflecting the interests, values, needs, and choices of individuals with disorders (Asha, 2023).
During my OT education, I have come across two tools that include the EBP model and through using it, helps us implement the model into our intervention. These tools are the case study and session write-up.
The use of the Case Study
Taking into account EBP’s clinical expertise, evidence and perspectives model, I can clearly see that as OT students we are pushed into using this methodology to analyse our clients through the drafting of case studies on them. We gain clinical expertise from our lecturers and on-practical supervisors who teach us about client factors and occupations and how they affect each other. They furthermore teach us about how to perform intervention to combat impairments experienced by our clients. They try to instil in us clinical reasoning skills. Thereafter we gather information on the client’s diagnosis from their file and desktop research which is external evidence, and we assess the client formally and informally thus gathering internal evidence. Lastly, we speak to our clients and their families to learn about their values and lifestyle in-depth through gathering their perspectives. All together this information is written up into a case study outlining how we provided intervention to our client and how it was customised specifically for them.
The Session Write-Up to Develop EBP Clinical Reasoning
The implementation of what we have gathered on the client from the external and internal evidence and the client’s perspectives is combined with our mushrooming clinical expertise to treat the client in a 30-minute session. The details of the session are written out to display our clinical reasoning. This is reviewed by our supervisors and for me has been an incremental but steep learning curve with new information being learnt at each session.
For instance, going to back to my CVA client, the 71-year-old Gogo from my previous blogs, I learnt about CVAs in class lectures earlier in the year. We learnt about the disease, the client factors and occupations it affects and how it could possibly be treated. Thus, my clinical reasoning skills were slowly initiated. Thereafter I came to Prince Mshiyeni Hospital and met the client. I had the opportunity to assess several of her client factors and learn about her occupational performance. I read up on her illness and gauged her medical and functional prognosis. I learnt about who she is as a person through an interview and further learnt about her living environment and what occupations she performs on a daily basis. With these several streams of information I compiled a session write-up of how I would treat her in a 30-minute session. I chose to use the ADL of dressing to both improve her impaired client factors and show her how she could now dress that she has this impairment. The session was reviewed by my supervisor and my learning and clinical reasoning skills were further refined with her guidance.
Hence at this student learning stage it is a virtuous cycle about learning holistically about the client using the EBP model and developing intervention based on the findings. Thereafter implementing the intervention with the client and if not appropriate, refining the intervention with the guidance of the supervisor. The teaching and learning of OT is through the EBP model using case studies and session write-ups which in turn leads to us doing EBP intervention with our clients.
______________________________________________________________
If you would like to know more about the readings I drew on for this blog, they can be found at the following links:
Evidence-Based Practice (EBP): https://www.asha.org/research/ebp/
A Brief History of Evidence-Based Practice: https://www.eboptometry.com/content/optometry/article/brief-history-evidence-based-practice-0
If you would like to know more about my education to become an Occupational Therapist at UKZN visit: https://ot.ukzn.ac.za/undergraduate-programmes/ The programme is pretty good. Also note the entrance requirements and points needed if you would like to study OT at UKZN. The application deadline is 30 September 2023.
If you still wondering what OTs do, see this video from the UKZN OT Department:
youtube
0 notes
Text
Reflecting on Collaborative Practice in a Multidisciplinary Team and How I have been a Health Advocate

Clients have a health care team managing different aspects of their treatment. Sometimes the different role players work together and other times they do not. As a student OT therapist who is spending her second practical placement at Prince Mshiyeni Hospital this year, I have encountered various other health care practitioners from the multidisciplinary team such as nurses, doctors, physiotherapists, and UKZN students from Physiotherapy.
With a physiotherapy student I had the opportunity to observe how they assessed a client we both had in common. This taught me how to assess the client in an easier manner through a quick screening and provided information on the client. Their supervisor also included me in the Q&A she had with the physiotherapy student about the client. It got me to see how Physiotherapists and Occupational Therapists collaborate. It was a SCI client which the physiotherapy student identified had scoliosis but I was able to say (with prompting from their supervisor) that through appropriately shaped cushioning his posture could be improved while sitting in a wheelchair. Hence even from the teaching level there could be collaborative processes to bring both disciplines together to learn from each other. It would be beneficial.
I was also surprised to learn that on more than one occasion doctors have approached us to ask what more a patient requires from OT before they can discharge the patient. The doctor did not unilaterally discharge the client. These patients were not clients of the OT student but rather the OTs at the hospital. The doctors could not get through to the hospital OT department. Thus, communication channels are not as efficient as they should be between these role-players which can negatively impact the patient. For example, a delayed discharge for the patient.
Nurses are the lifeblood of providing minute-by-minute care for patients in the hospital. They are also very much in the know about the clients. They are an excellent source of information on the client and can be approached to learn about the client. On the other hand, they may not provide sufficient care to the client. For instance, I came to the hospital on a Monday morning to learn that my client’s adult incontinence product had not been changed since Friday and it was affecting his pressure sores. Once I brought this to the nurse’s attention, they took it as an ordinary occurrence as they said it was the weekend and no one changed him. Also, they did not have fresh bandaging for his pressure sores. Eventually they made the effort and obtained bandaging from another ward as my supervisor and I stood there. My minor health advocacy was informing the nurses about the plight of the client and ensuring it was in the SOAP notes that he had not been changed for two days.
My role is to ensure I provide quality service to my clients but also that other health practitioners do so too. That’s how I could be a health advocate. As behaviour is difficult to change in the long term, to do so would require systematic changes from a management level. At my level I can point out if I feel more intervention is required by an individual to the appropriate healthcare practitioner. But would they heed my call without getting offended?
This was not the case with the hospital Physiotherapist who felt as students we had over stepped our bounds by saying Physiotherapy had to assist with a certain client. Thus, it can be a fine line between being a health advocate for the client and offending others in the health care team. Collaboration amongst a multidisciplinary team takes excellent people skills and communication. I hope to develop this during my career.
______________________________________________________________
If you would like to learn more about what each health care practitioner does visit the following links from WebMD:
Occupational Therapists: https://www.webmd.com/a-to-z-guides/what-is-an-occupational-therapist
Physiotherapists: https://www.webmd.com/a-to-z-guides/what-is-a-physiotherapist
Nurses: https://www.webmd.com/a-to-z-guides/what-is-registered-nurse
Doctors: https://www.webmd.com/health-insurance/insurance-doctor-types
0 notes
Text
Reflecting on what Client-Centred Means to Me

Off the top of my head client centred would be doing what's in line with the client’s needs. Doing activities that align to the client’s interest and are meaningful to them but which I initiate and supply. A formal definition on the other hand says the following:
Client-centred occupational therapy is a kind of partnership between the client/patient and the therapist, which allows empowerment of the patient to engage in functional performance to fulfil his/her occupational roles in a variety of environments. Philosophy of client-centred therapy includes empowerment and guiding of patients to achieve a cure by means of a balance of power between the therapist and patient. In this approach, the therapist acts as an educator. Thus, sufficient information and communication skills are needed to scrutinize the treatment. Expectations and targets are achieved together with the patient. When a client-centred approach can be administered completely, the patient makes decisions alone based on his/her targets. In addition, the power is transferred from the therapist to the patient. In such a case, the therapist supports the decision-making period of the patient and accepts his/her decisions.(Tonga, Duger and Karatas, 2015)
The formal definition is in stark contrast to what I had in my head. Client-centred OT in the definition is a partnership between the client and therapist where expectations and targets are achieved together. Eventually the decision-making power is transferred to the client.
So, who really makes the decisions - therapist or client?
If my 71-year-old client with the stroke (from my last blog) had her way, she would own a wheelchair and happily wheel about. That was her request. But upon learning that she can walk, I incorporated activities involving standing and walking mobility into her intervention using a dressing activity. As my supervisor mentioned clients don’t know how far they can push themselves and the therapist should guide the way. With this in mind, I am steering the client toward the goal of learning to stand and walk again independently through the use of activity.
What I should do in the upcoming sessions is speak to my client if she thinks standing and walking are important goals to her. She has said that she is retired and spends her time sitting and watching TV mainly. Her grandchildren who live with her take care of her and the house. Hence, she may not be very motivated to stand or walk. But in intervention sessions she has shown keenness in attempting to stand and walk as if it is something she would like to achieve. Still, I need to speak to her to learn her long-term vision and show her how she can benefit with standing and walking on a day-to-day basis. I need to highlight that she could possibly use crutches instead of a wheelchair to mobilise.
The dilemma comes in for me when as suggested by the formal definition the “client-centred approach can be administered completely, (when) the patient makes decisions alone based on his/her targets” (Tonga, Duger and Karatas, 2015). Thus, the client could decide that even though she could walk with crutches, she prefers the wheelchair and would rather use that. Am I supposed to accept that? As the client is in the public sector, she will not be issued a wheelchair by the hospital and hence may be forced to use crutches. But if this client were in the private sector, she could buy her own wheelchair.
At the end of the day though, I should educate the client about what she is capable of doing, the benefits of mobility and her mobility options when performing different activities. She and I should agree on targets on how she would like to eventually be able to do her activities of daily living for instance. I believe I as the therapist should set the bar high for intervention but within reason of what the client can actually perform. So, I should set some initial goals but I need to obtain the client’s buy-in so that she will comply in the long term. As the client sees progress, she would suggest her own milestones that she would like to achieve. This would be client-centred where there is an eventual balance of power between the therapist and client with both role players setting goals.
______________________________________________________________
If you would like to read the article I quoted from, this is its reference (though it’s about rheumatoid arthritis and not stroke):
Tonga, E., Düger, T., & Karataş, M. (2015). Effectiveness of Client-Centered Occupational Therapy in Patients With Rheumatoid Arthritis: Exploratory Randomized Controlled Trial. Archives of rheumatology, 31(1), 6–13. https://doi.org/10.5606/ArchRheumatol.2016.5478
Or find it at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5827861/
If you want to know more about strokes visit:
The Heart and Stroke Foundation https://heartfoundation.co.za
More about stroke support groups:
The Stroke Survivors Foundation support groups directory https://pdss.strokesurvivors.org.za/association/
More about OT:
Occupational Therapy Association of South Africa (OTASA) to learn about and find an Occupational Therapist https://www.otasa.org.za/find-an-ot/
0 notes
Text
From theory into practice: My first week of fieldwork. How does treating make me feel?

Entrance to Prince Mshiyeni Hospital in Umlazi, Source: KZN DOH
Imagine telling your supervisor that your client can’t walk, only for your supervisor to tell you later in the day that your client walked to the bathroom while holding onto a bench for support. They saw it for themselves. Well, that’s what happened to me! Embarrassment. But lesson learnt. Never take at face value what your client tells you especially if you can easily assess it.
At Prince Mshiyeni Hospital in Umlazi where I have been placed for my third-year Occupational Therapy practical my client is a friendly and unassuming 71-year-old female that had a CVA. She is presenting with right side hemiparesis and her right leg is more affected than her right arm with a difficulty to move.
She has requested for a wheelchair several times to move about. But if in fact she can stand and even walk, I as the OT need to improve the client factors that will help her to walk better. It made me realise that clients can feign a greater degree of disability for their own benefit. In her case I’ve wondered what the benefits could be and two possibilities have come to mind. Firstly, her request for a wheelchair could be because she believes that it’s easier to mobilise with one than walk and secondly, she may prefer a wheelchair over crutches which is what she used before the CVA. This is interesting to note that there may be benefits from feigning a greater degree of disability. Thus, I as the therapist need to ensure that I am very thorough with my assessment to nip it in the bud.
Furthermore, with an incorrect assessment, the level of my treatment intervention activities were not correct. My intervention was not properly aligned to what my client can actually do. This was another lesson to me about how important performing the correct assessment is. As doing the incorrect intervention is not therapeutic for the client and wastes both mine and the client’s time when activities are not at the appropriate grade. In the next interaction with my client, I need to re-assess her lower limb capabilities and plan interventions accordingly. As my supervisor suggested (before she even saw my client walk) doing a sit to stand test is a basic assessment required.
In conclusion, I learnt several things from my two days on fieldwork practical. Firstly, it is very important to be thorough in my assessment as it has implications on intervention and treatment. In my case my treatment was not at the appropriate grade as it was too low. Secondly, I should not take the client at face value but rather verify their statements through an assessment, especially if it is easily assessed in the hospital. Thirdly, clients may benefit from exaggerating their disability. This may not be done with malice intention but it is just more convenient for them to say they can't do it (stand/walk) than doing the work to get better. Or they may exaggerate to obtain a free benefit like a wheelchair. As the OT I need to safeguard against (state) resources being used detrimentally and the client not working to get better to their full potential.
I am starting to see (and feel) the weight of my responsibilities to ensure proper assessment, treatment and care of the client and the efficient use of (state) resources.
For anyone who needs further information on CVAs (stroke), support groups in their area, access to free wheelchairs, occupational therapy in South Africa, or the Government’s disability grant, please visit the websites below.
The Heart and Stroke Foundation https://heartfoundation.co.za
The Stroke Survivors Foundation support groups directory https://pdss.strokesurvivors.org.za/association/
The Gift of the Givers for free wheelchair provision https://giftofthegivers.org/healthcare/wheelchair-and-mobility-aids/35493/
Occupational Therapy Association of South Africa (OTASA) to learn about and find an Occupational Therapist https://www.otasa.org.za/find-an-ot/
The SA Government Disability Grant criteria https://www.gov.za/services/social-benefits/disability-grant
#CVA, #stroke, #wheelchairs, #OTASA, #disabilitygrant, #princemshiyeni, #hospital, #OT, #OTstudent, #UKZN
1 note
·
View note