Don't wanna be here? Send us removal request.
Text
Plutus Health Helps a Medical Lab Collect $1,282 Per Claim
DALLAS, TX – September, 2022 – Plutus Health is proud to have helped a medical laboratory boost its average collection per claim from $808 to $1,282 and reduce its outstanding accounts receivable (AR) by $1.1M.
“Our client—an out-of-network specialty lab based in Phoenix, Arizona—was beset by coding errors and inaccuracies that resulted in unprocessed denials and rejections,” shares Thomas John, the CEO of Plutus Health. “Those challenges ultimately caused delays in claims posting and payments,” he added.
To address these challenges, Plutus Health conducted a free revenue health analysis. It transformed the lab’s overall revenue cycle strategies, prioritizing the creation and application of coding standards and modifiers during implementation. The company also conducted eligibility checks to boost the medical lab’s clean claims percentages.
Aside from optimizing the coding and eligibility process, Plutus Health created a more efficient procedure for managing appeals and collecting direct-to-patient payments. This helped increase collections per claim by 58%.
Plutus Health is an established provider of revenue cycle management (RCM) and billing services for healthcare organizations. It offers HIPAA-compliant end-to-end business solutions and revenue cycle management outsourcing to US healthcare providers and RCM companies.
“Our mission is to provide services that decrease administrative burdens and maximize revenues so our clients can focus on caring for their patients and delivering timely care,” says John. Plutus Health incorporates automation into its optimized processes to enhance the client’s current processes and cash flow. It works closely with every client, synthesizing data, optimizing revenue management, and tracking revenue cycle management goals. Its HIPAA-compliant RCM solutions exceed the most stringent standards in the industry, while its robust redundancy systems and data security protect against data loss. Clients are assured of custom strategies tailored to their laboratory or practice.
MEDIA CONTACT
Thomas John
Plutus Health Inc.
Tel: (469) 242-6053
Address: 4835 LBJ Freeway, Suite 300, Dallas, Texas, USA
Website: https://www.plutushealthinc.com/
0 notes
Text
What Are Mental Health Billing Services? The Process and Benefits
When you’re busy attending to patients, it’s easy to make errors in billing and coding and miss deadlines, resulting in claim denials and loss of revenue. To get around these problems, successful practices frequently outsource mental health billing services. Making this move can also help your billing team deal with changes in insurer policies, coding requirements, and governmental restrictions with less uncertainty. Mental health billing face challenges that differ from other medical billing.
How does it work?
In mental health billing, insurers and patients are primarily billed for psychological testing services, therapy, and medical management. Insurers have rules for the length of sessions they are willing to pay for, how many they will pay per week or day, and the maximum number of treatments they can cover. However, there are situations when a patient's mental health requirements go beyond an insurer's coverage, making it challenging for mental health professionals to balance an effective treatment plan with sufficient reimbursement.
Mental health billing services can help your practice prevent revenue shortfalls and payment delays. Custom solutions can free up time, boost revenues, and reduce costs in your practice. They also ensure compliance while enhancing transparency regarding your billing operations.
Leave it to the experts.
Insurance companies have different timelines for each therapy, and because they don't match the amount of time it actually takes to deliver or finish a treatment, there are inconsistencies in the way the services are billed. Practitioners must be aware of the issues that result in denials and delayed reimbursements, such as prior authorization, documentation errors, policy violations, and coding accuracy.
You don’t have to worry about when you outsource your mental health billing to dependable service providers specializing in the area. They have a dedicated team of trained mental health billing and coding specialists that can provide data-driven solutions to enhance your practice’s revenue cycle.
Additional reasons to outsource
Customized mental health billing services offer the following benefits to your practice:
· Scalable and affordable – Access the human resources and systems to handle every bill more cost-effectively than when you do it in-house. A pay-as-you-go service charges only for the work done while taking only a small percentage of the collection, so you pay less when you file a few claims.
· Fast payouts – Reputable mental health billing professionals use technology to immediately manage claims, bills, and re-bills fast and accurately. Rejections and errors are fixed right away.
· Enhance your patient care – Outsourcing mental health billing frees up your schedule, allowing you more time for your patients. Additionally, it relieves your support team's workload so they can concentrate on helping your patients.
Outsource mental health billing to Plutus Health. We offer customized solutions to reduce costs, save time, and boost your ROI. Our mental health billing systems use automation, artificial intelligence, and other technologies to automate chores like payment reminders, ensuring on-time bill payment. Contact us for an assessment.
0 notes
Text
Understanding Why ASC Billing Services Are Important Tools for the Healthcare Industry
Like many healthcare facilities, Ambulatory Surgical Centers (ASC) tend to experience challenges and difficulties in medical billing and coding. Some issues are particular to its unique environment and operations. In-house ASC billing can be time-consuming, labor-intensive, and difficult due to distinct specialty-based needs, other specifications, and issues with areas like claims processing with insurance companies.. These must be considered when outsourcing ASC billing services.
Ambulatory surgical centers provide outpatient surgical services as independent facilities or an aspect of a larger medical group or hospital. CMS mandated only specific surgical procedures in ASCs. ASCs differ from other specialty clinics due to these characteristics and distinctions with Medicare rules, which leads to challenging ASC coding and medical billing procedures. The good news is that by outsourcing ASC billing and coding to a specialized provider, ASCs can get around these challenges.
How does outsourcing help?
ASCs must maintain financial viability in order to continue providing high-quality, affordable same-day pain treatment and surgery. Tailored ASC medical billing systems ensure viable services and operations daily. Here’s a closer look at the importance of ASC billing services to the healthcare industry:
Revenue cycle management
Ambulatory Surgical Centers lose revenue due to late and denied payments, which can be caused by improper ASC coding. ASC billing specialists can provide complete RCM services to help collect lost revenue, identify issues in the payment process, and improve revenue generation.
Accurate and detailed clinical documentation
ASC billing and coding service providers can collect relevant documents and meticulously verify patient information and eligibility to reduce the risk of denials. To go even farther and maximize the chance of quicker approvals, they adhere to all rules and compliance when coding.
Accounts receivables and denial management
A dedicated team handles critical areas in ASC medical billing, such as accounts receivables (AR), to reduce the rate of denials. It can manage payer contracts, find issues on local coverage determinations, review denials and file appeals, and deliver analytics and business intelligence reports.
Is it time to outsource ASC billing services?
Plutus Health offers dependable and high-quality ASC billing and coding services with its revenue cycle management solutions for ASCs. You may rest easy knowing that its ASC billing solutions abide by all local, state, and federal laws. Your ARs will also be worked on by an internal team to reduce denials.
Contact Plutus Health for a free revenue analysis to get started.
0 notes
Text
Plutus Health Inc. Helped Freestanding Emergency Room Facility Increase its Collection by 150%
DALLAS, TX – August 25, 2022 – A premier 24-hour freestanding emergency room facility increased its collections by 150%, thanks to Plutus Health Inc. The facility faced multiple challenges that negatively impacted its financial viability, including piled-up accounts receivables, inefficient billing processes, and significant delays in payment posting. It also experienced multiple loopholes in its insurance verification process. “We implemented a step-by-step solution to improve the client’s billing accuracy gradually,” explains Thomas John, CEO of Plutus Health Inc. “We tailored a plan and set timelines for each method process improvement to keep their process on track while measuring progress.” Plutus Health Inc. also implemented a charge reconciliation process for the client to make the billing gradual, easy to measure, and accurate.
In only three years, these solutions drove the client’s overall collection from $4 million to $10 million each month. The client’s first pass collections also increased from 60% to 85%, and its gross collection ratio went from 15% to 40%. Plutus Health is a trusted and experienced provider of HIPAA-compliant revenue cycle management (RCM) and end-to-end business solutions to US healthcare providers. It is best known for combining robotic process automation and machine learning to address its clients' most challenging RCM and billing issues. “Our goal is to eliminate the obstacles that prevent our clients from earning and realizing their income,” explains John. “Our solutions boost revenue and claims percentage while decreasing overhead costs.” Plutus Health Inc.’s process can improve a healthcare organization’s performance in three steps: synthesizing all data from the practice, optimizing revenue management, and empowering the client to set and track its RCM goals. The company guarantees an error-free and high-quality output that meets the most stringent industry standards with robust redundancy systems and data security to protect against data loss.
MEDIA CONTACT Thomas John Plutus Health Inc. Tel: (469) 242-6053 Email: [email protected] 4835 LBJ Freeway, Suite 300, Dallas, TX 75244
0 notes
Text
What are the 3 Phases in Revenue Cycle Management?
Is your healthcare practice collecting promptly and sufficiently from insurance companies? If you’re having payment issues and your revenue cycle management isn’t as cost-effective as you hope, you might need to step back and analyze your current system. It’s also important to take time to understand the three phases in RCM for healthcare so you can identify opportunities and avoid mistakes that cost money. Finally, consider using automation in revenue cycle management to ease your staff’s workload, improve their productivity, allow them to focus on critical tasks, and deliver better customer service.
The revenue cycle in the medical setting starts when the patient sets an appointment and concludes with the final payment resolution. There are plenty of opportunities to improve collections throughout the process, and simple mistakes that may occur along the way could be costly. Breaking down the RCM for healthcare, examining each phase, and tracking, improving, and measuring the metrics can encourage improvements.
Here are the three phases of RCM with some best practices to improve each.
Phase 1: Appointment setting and obtaining patient demos
At this phase, your objective is to avoid errors at your front desk. Revenue cycle management automation must efficiently collect and organize patient demographics and insurance information. You should also have a system for tracking and balancing appointments, electronically checking insurance eligibility, and template-driven scheduling.
Phase 2: Capture charges and submit claims
Your goal should be to reduce incidents of denials on the first submission and enable daily electronic filing. You need a system that lets you accurately track the amount billed against collections when the claim is submitted. It’s also important to keep up with changes in payer policies and rules to effectively cut the percentage of denials.
Phase 3: Data analysis, remittance posting, and collection
Manage denied claims and no-response claims as quickly as possible. Phase 3 is where you and your team should promptly track write-offs, adjustments, underpayments, and down coding. Ensure data transparency and easy access so you can quickly analyze information and make solid decisions from anywhere at any time.
How is your RCM process?
Optimize your RCM with Plutus Health, a medical billing company that provides custom solutions, including revenue cycle management automation. Get custom strategies that can solve your RCM challenges so you can save money and improve your ROI.
About the Author:
Thomas John leads a global team of 500 employees in 3 locations as the President & CEO of Plutus Health providing, RPA powered revenue cycle management services to healthcare organizations across 22 states. Plutus Health Inc. is a 15-year-old full-cycle RCM firm specializing in medical coding & billing, denial management, credentialing, prior authorizations, AR follow-up for both medical and behavioral health specialties. As the industry experts in revenue cycle management solutions, they've created a unique process that combines machine learning and robotic process automation to address the clients' most frustrating problems.
0 notes
Text
Medical Coding: A Critical Role in Healthcare Today
Medical coding and billing are important for healthcare providers to get paid for the services they render. They are also crucial for tracking medical data and providing accurate information to patients. Any inaccuracies can lead to overcharging or undercharging, denial of insurance claims, and even fraud.
Medical coding translates medical procedures and diagnoses by healthcare providers into alphanumeric codes known as ICD or CPT. Medical coders need to accurately classifying clinical statements and assign the right codes create accurate patient records that facilitate efficient medical billing. In this sense, medical coding and billing go hand in hand; billing is made more efficient with correct medical coding.
A complex process
Coding is critical in every medical specialty, including ambulatory surgery centers (ASCs) and anesthesia and DME services. Each specialty needs to follow complicated and ever-changing guidelines that make medical coding and billing even more challenging. If your in-house team is finding it hard to stay up-to-date with the latest regulations, it may be time to outsource medical coding to third-party experts.
One of the biggest benefits of outsourcing is that it can save you money. You're essentially hiring a company to handle all of the administrative tasks associated with billing and collections. This can free up a significant amount of time and money that you would otherwise have to spend on these tasks.
Additionally, outsourcing can help improve your practice's cash flow. You'll have access to a team of experts who can help you maximize reimbursement and collect payments quickly. This can increase the amount of money that comes in each month and boost your bottom line.
Outsourcing medical billing can also help improve the quality of care that you're able to provide. You'll have access to a team of experts who can help you streamline your billing process and improve the way that you interact with patients. This can lead to better patient satisfaction and improved care overall.
For a healthy practice
Accurate coding and billing practices build a financially healthy healthcare practice that is ready and able to deliver optimum care. Precise preparation and submission of billing claims enables prompt and proper reimbursement in the expected amount for the services provided to the patients. It is essential for ensuring correct and timely reimbursements from healthcare programs like Medicaid, Medicare, and private insurance providers. It also prevents delays and denials that may affect the financial viability of a practice.
Get help from specialists
Outsource your medical coding and billing to Plutus Health. With AAPC and remote processing automation, Plutus Health ensures compliant medical coding that encourages the most reimbursements based on governing guidelines and the services provided.
About the Author:
Thomas John leads a global team of 500 employees in 3 locations as the President & CEO of Plutus Health providing, RPA powered revenue cycle management services to healthcare organizations across 22 states. Plutus Health Inc. is a 15-year-old full-cycle RCM firm specializing in medical coding & billing, denial management, credentialing, prior authorizations, AR follow-up for both medical and behavioral health specialties. As the industry experts in revenue cycle management solutions, they've created a unique process that combines machine learning and robotic process automation to address the clients' most frustrating problems.
0 notes
Text
Plutus Health Inc. Has Helped an ABA Practice Reduce Its 90+ AR in Just 90 Days
DALLAS, TX – July 25, 2022 – Plutus Health Inc., the best medical billing company in US, helped an applied behavioral therapy (ABA) practice decrease its A/R days to less than 5% in three months. The client is a large mental health service organization with several locations across the US.
The term ‘accounts receivable days’ or A/R days refers to the number of days it takes for a medical organization to collect outstanding amounts from insurance carriers for services provided to their patients. It is a vital benchmark that reflects the financial health of medical practice. Rising A/R days often cause cash flow problems and underlying medical billing issues.
“Our client was dealing with a massive backlog of around $8M in payment posting,” explained Thomas John, CEO of Plutus Health Inc. To solve this issue, Plutus Health Inc. conducted an AR audit to analyze the client’s RCM strategy and understand their workflow. Along the way, the team identified critical issues, such as gaps in patient medical records, the absence of a solid patient eligibility verification process, and plenty of non-posted payments.
“We then designed and implemented a robust process that checks a patient’s benefits and eligibility three to five days before appointments. This optimized the eligibility verification procedure and reduced gaps in the medical records,” said Thomas.
The team also utilized best-in-class ABA billing software to consolidate all backlog payments, post all legacy payments, and resolve legacy claims. They also customized an appropriate denial management process.
A leader in medical RCM, Plutus Health Inc. uses unique processes that combine robotic process automation, machine learning, and human expertise to assist healthcare companies realize more earnings and stay financially viable. Learn more about the company’s ABA therapy billing services at www.plutushealthinc.com.
MEDIA CONTACT
Thomas John
Plutus Health Inc.
Tel: (469) 242-6053
4835 LBJ Freeway, Suite 300,
Dallas, TX 75244
0 notes
Text
Plutus Health Inc. Participates in CASP 2022
DALLAS, TX - June 24, 2022 – Plutus Health, a provider of revenue cycle management (RCM) solutions for the healthcare segment, took part in the Council of Autism Service Providers (CASP) annual conference on May 2 at the Hilton Hotel in Portland. The CASP is a non-profit organization that provides specialized assistance and organizes peer-directed gatherings for senior and mid-level staff who serve individuals with autism-related disorders.
The conference is for healthcare providers seeking support to enhance billing services and patient engagement. Attendees at the conference were top service providers in the US and specialists with in-depth knowledge of the current challenges in the autism industry and the whole applied behavioral therapy (ABA) sector.
“Our participation in CASP 2022 allowed us to introduce our HIPAA-compliant revenue cycle management outsourcing and end-to-end business solutions to more healthcare providers in the autism segment,” explains Thomas John, CEO of Plutus Health Inc. “We were able to share our unique technology of combining robotic process automation and machine learning to address the most frustrating problems in ABA billing,” he adds.
Plutus Health also discussed different strategies for keeping medical practices financially viable.
“Our robust RCM services can eliminate the interruptions preventing healthcare practitioners from realizing income. We can help them boost their percentage of clean claims and their overall revenue while reducing their overhead costs,” explains John.
Plutus Health has 14 years of experience as a full-cycle technology-driven RCM firm specializing in medical billing, coding, denial management, payment posting, AR follow-up, prior authorizations, out-of-network negotiations, and credentialing. It is SOC2 Certified for data security and compliance. Healthcare organizations interested in learning more about its solutions can find more information on www.plutushealthinc.com.
MEDIA CONTACT
Thomas John
Plutus Health Inc.
Tel: (469) 242-6053
4835 LBJ Freeway, Suite 300,
Dallas, TX 75244
0 notes
Text
Plutus Health Inc. Participates in AIS 2022
Dallas, TX – May 19, 2022 – Plutus Health Inc. successfully participated in the Autism Investors Summit (AIS) held in the SLS Hotel Beverly Hills in Los Angeles, California.
Often described as one of the most prominent healthcare summits in the US, the AIS is a yearly event attended by experts in applied behavioral therapy (ABA), investors, and key stakeholders in autism services. This year’s summit ran from April 18 to 20.
In an event highlight, Plutus Health Inc. CEO Thomas John spoke about the essentials of revenue cycle management (RCM) for ABA practices. He also presented solutions to help providers deal with complex ABA billing protocols and ever-changing guidelines.
“A healthy and successful ABA RCM process ensures steady collections, timely revenue, and continued financial viability, allowing providers to focus on giving their patients the highest quality of care,” said John. “Our complete RCM and billing solutions help ABA therapy providers reduce denials and increase cash flow by boosting collections while ensuring compliance,” he adds.
Plutus Health Inc. is a leading provider of HIPAA-compliant RCM solutions for US healthcare organizations.
It is known for using efficient and cost-effective RCM processes that combine artificial intelligence, robotic process automation, and machine learning to address billing and collection problems commonly faced by healthcare providers. Its mission is to help hospitals, clinics, therapy centers, and private practices boost their clean claims percentage, maximize revenue, decrease overhead costs, and achieve financial stability to grow and serve more patients.
Plutus Health Inc.’s behavioral health billing services are delivered by teams of highly-trained professionals, that produce data-driven and actionable solutions for ABA providers. Certified by the American Academy of Professional Coders, they are proficient in HCPCS, ICD-9/10, and CPT coding.
The company’s behavioral health billing solutions are customizable to the client’s requirements. They can include verification of benefits, utilization reviews, billing, and collections, claim audits, reimbursement negotiations, appeals, and patient responsibility collections.
More information is available on the Plutus Health Inc. website.
MEDIA CONTACT
Thomas John
Plutus Health Inc.
Tel: (469) 242-6053
Email: [email protected]
4835 LBJ Freeway, Suite 300,
Dallas, TX 7524
0 notes
Text
Plutus Health is Joining ASCA Summit 2022
DALLAS, TX – March 11, 2022 – Plutus Health Inc., a proud leader in healthcare innovation, is joining the Ambulatory Surgery Center Association (ASCA) Summit 2022.
The event will run from April 27 to 30 in Dallas, Texas. Plutus Health Inc. will be in Booth 303.
“We are proud to take part in this year’s summit,” says Thomas John, CEO of Plutus Health, Inc. “Joining this conference; underscores our commitment to helping ASCs improve patient engagement and deliver medical billing solutions to boost their revenue cycle management.”
Plutus Health Inc. focuses on healthcare innovation by providing revenue cycle management services. Many ASC providers rely on its solutions to increase cash flow and collections and minimize the rate of denials while ensuring compliance.
“ASC medical billing is notoriously complex, but our solutions make it easier for ASC providers. We help them grow and sustain their practices by empowering patient engagement,” John adds.
The ASCA 2022 Conference & Expo lets participants gather top-quality clinical, competitive, financial, regulatory, and business information from some of the most renowned professionals in the ASC community. The conference also provides opportunities to earn CEs, including AEU credits for the CASC credential, IPCHs for the CAIP credential, and nursing contact hours.
Aside from this, ASCA 2022 highlights a wide array of solutions that can boost the financial viability of ASC practices, including medical billing and revenue cycle management solutions from Plutus Health Inc. The conference likewise offers networking opportunities, allowing participants to connect with contemporaries, talk to industry leaders and peers, and meet other ASC professionals.
MEDIA CONTACT
Thomas John
Plutus Health Inc.
Tel: (469) 242-6053
Email: [email protected]
4835 LBJ Freeway, Suite 300,
Dallas, TX 75244
0 notes
Photo

Key Benefits of RPA In Medical Billing and How It Is Changing the Healthcare World
RPA in medical billing is promising, as it benefits your practice in all aspects where manual work is tedious and consists of repetitive tasks. One of the significant advantages of RPA is that it can enhance the medical billing and overall revenue cycle management process so that you can promptly get paid for the medical care you provide to the patients. Revenue in the healthcare system predominantly comes from medical billing, so it’s essential to take care of this aspect of running a practice.
0 notes
Photo
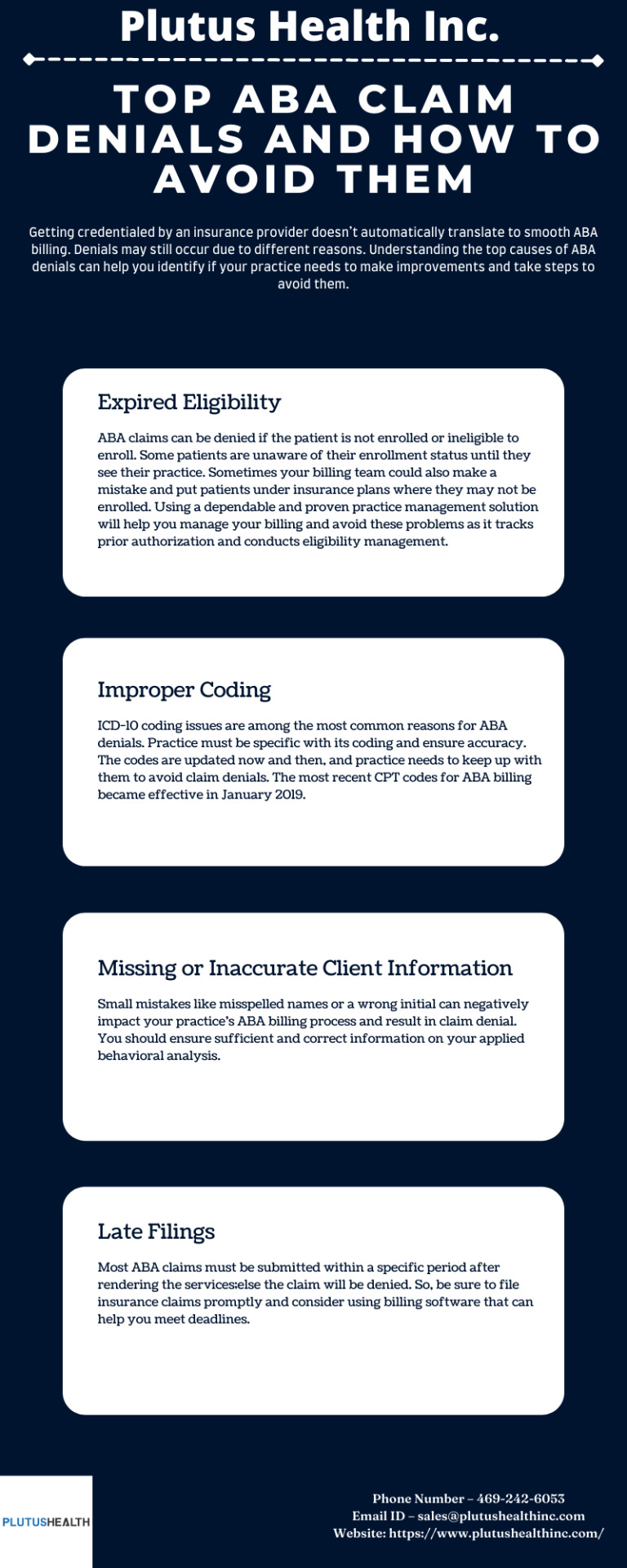
Top ABA Claim Denials and How to Avoid Them
Getting credentialed by an insurance provider doesn’t automatically translate to smooth ABA billing. Denials may still occur due to different reasons. Understanding the top causes of ABA denials can help you identify if your practice needs to make improvements and take steps to avoid them. Here’s a quick list:
0 notes
Text
How Using Good ABA Software Can Improve Your Practice
Applied behavior analysis or ABA is a growing field of therapy as more patients seek treatment for developmental and behavioral disorders. A robust ABA software solution that supports ABA billing can help practices thrive financially; so that you can keep doing what you do best: provide the finest care for your patients.
Qualities of good software for ABA
Not every software solution will suit your practice. You need to consider your unique needs and challenges and use those as the basis when choosing ABA software.
Search for software witha range of capabilities, such as ABA billing, note-taking, automation, scheduling, collaboration functionality, and progress reports. The developer should be able to configure each feature to simplify your day-to-day functions, particularly when it comes to repetitive and time-consuming tasks.
ABA software should help patients or their guardians, caregivers, and clinical staff, oversee progress on milestones and targets that may include many different client criteria. It should keep everyone up to date. Therapists should also rely on the software to streamline ABA billing and improve the way they work as it automates labor-intensive administrative tasks.
Simplifying workflows
ABA software systems come with workflows such as basic communication, progress reports, and therapy notes. They make it easier to input information like BIRP or SOAP notes and apply a coding system like ICD-10. ABA billing, scheduling, and timesheets are also considered workflows that therapists use in the administrative side of their practice. These are useful for managing and processing health insurance reporting. Automated billing lets you focus on your clients while reducing the chances of ending sessions prematurely.
Newer and more flexible solutions are usually cloud-based, accessible from any web-connected device through a dedicated app or a web browser. Reputable providers of these solutions offer a free trial or a demo to help you decide if their product’s features and functions can meet your requirements.
If looking for a good ABA software solution, Plutus Health is what you need. As a leading ABA billing services company, it provides end-to-end revenue cycle management solutions for ABA providers and centers. It helps to decrease the rate of rejections and denials, improve cash flow, reduce coding errors, and enhance the eligibility and pre-authorization processes.
About the Author:
Thomas John leads a global team of 500 employees in 3 locations as the President & CEO of Plutus Health providing, RPA powered revenue cycle management services to healthcare organizations across 22 states. Plutus Health Inc. is a 15-year-old full-cycle RCM firm specializing in medical coding & billing, denial management, credentialing, prior authorizations, AR follow-up for both medical and behavioral health specialties. As the industry experts in revenue cycle management solutions, they've created a unique process that combines machine learning and robotic process automation to address the clients' most frustrating problems.
0 notes
Text
Plutus Health Inc. is Proud to Sponsor the Autism Investor Summit 2022
DALLAS, TX – February 7, 2022 – Plutus Health Inc. is sponsoring the Autism Investor Summit, held from April 18 to 20, 2022, at the SLS Hotel Beverly Hills in Los Angeles, California.
The event provides autism service providers, key stakeholders, and investors a chance to discuss investment opportunities, expand their professional network, and learn about the latest innovations and best practices in all areas of autism therapy services.
"Plutus Health Inc. is proud to sponsor and exhibit at the Autism Investor Summit," says Thomas John, the company's CEO. He further states, "This underscores our commitment to supporting applied behavioral analysis (ABA) providers with technologies that empower them to deliver the best client care."
Plutus Health Inc. provides ABA-focused revenue cycle management services to help ABA therapy providers increase collections, reduce denials, and increase cash flow, with a strong emphasis on compliance.
"ABA billing is notoriously complicated because of the ever-changing protocols, POS and Modifier variations, different portals, and new Telehealth guidelines," explains John. "Our billing and revenue solutions take this stress off the shoulders of ABA providers, helping them sustain and grow their practices so that they can serve more clients."
The Autism Investor Summit aims to bring together ABA stakeholders from all segments, including advocates, service providers, consumers, payers, researchers, and investors.
Among the chief topics for discussion are the service models with the most promising outlook and how outcomes can impact autism services down the line. Investors will explain what they are looking for when exploring acquisitions, and non-investor attendees can learn what questions to ask when doing due diligence on companies, what to look for in investors, and how to identify funding opportunities.
The conference also allows participants to explore new technologies in ABA practice management, including therapy billing and insurance services from Plutus Health Inc.
MEDIA CONTACT
Thomas John
Plutus Health Inc.
Tel: (469) 242-6053
Email: [email protected]
4835 LBJ Freeway, Suite 300,
Dallas, TX 75244
0 notes
Photo

Common Reimbursement Issues Costing ASCs The Most
If you run an Ambulatory Surgery Center (ASC), you may already be familiar with the challenges and issues around coding and billing in your sector. ASC billing can be complicated, but your facility can avoid the most common reimbursement issues that can cost your practice when you use the correct process. It also helps to know the most common problems that can affect ASCs the most, so you can immediately identify them when they happen and take the necessary action to correct them.
0 notes
Photo

Primary Factors to Consider While Implementing Surgery Billing Solutions
Plutus Health make it easier for Surgery Centers to manage their RCM. If you struggle with billing, collection, and overall RCM Management, our expert team will get the fastest reimbursement possible and increase your practice's performance.
0 notes
Text
Outsource Mental Health Medical Billing Services to Plutus Health Inc. – A Leader in RCM Services Healthcare
DALLAS, TX – Plutus Health offers behavior and mental health billing services in its range of revenue cycle management (RCM) solutions for the healthcare sector.
This service further strengthens the company’s long-standing reputation as a full cycle technology-driven RCM firm specializing in medical billing, medical Coding, and denial management.
“Our behavioral health billers and medical coders are trained to address the unique challenges of mental health billing,” explains Thomas John, the company’s CEO.
“We offer automation-based services and analytics to reduce denials, increase revenue, and improve insurance accounts receivables. Our client base extends to more than ten states and covers a vast range of mental health providers,” he adds.
“The pandemic and resultant restrictions and uncertainties have caused mental stress to many people and an increase in mental health issues amongst the population. Mental Health organizations and providers find it increasingly challenging to handle billing & collections for their ever-increasing patient base.
Plutus Health, with its strong team of mental health billing experts and technologies, is the ideal choice for such organizations to focus on their patients and leave the administrative tasks to a professional team.” Adds Balaji Ramani, VP Business Development
Based on CMS and AMA guidelines, Plutus Health coders are certified by the American Academy of Professional Coders (AAPC) / AHIMA and proficient in ICD-10, CPT, and HCPCS coding.
The firm’s mental health billing solutions support the services offered by a wide range of practitioners, including psychiatrists, counselors, psychologists, clinicians, social workers, therapists, primary care physicians, Behavior therapists. These solutions also support behavioral health billing for psychotherapy, psychiatric therapy, and psychologist billing. The Plutus Health team has vast knowledge in the billing range of codes, including 90785, 90791, 90792, 90832 to 90837, 90846, 90847, 90853, 96127, 96130, 96131, 96136, 96137, 99051, and 99404.
Addressing challenges in mental health billing
A major problem in mental health billing is that claims are processed and paid according to provider type, with fee schedules varying for each type of provider. Plutus Health can verify the provider type right away during eligibility verification and add exact provider information.
Another challenge is that most patients only have health cover, without mental health benefits. Plutus Health prevents issues by efficiently verifying eligibility. If the payer will not cover the service for the appointment date, the client is informed right away.
Learn more about Plutus Health’s mental health billing services by visiting plutushealthinc.com and filling out and submitting the ‘Get Started’ form.
About Plutus Health Inc.
Plutus Health Inc. is a leading Healthcare Revenue Cycle Management organization with a global footprint in Dallas, TX. Plutus Health provides Coding, pre-billing Audits, Billing & Insurance AR collections using advanced technologies such as Machine Learning and Robotic Process Automation.
MEDIA CONTACT
Lisa Williams
Plutus Health Inc.
(469) 242-6053
0 notes