#Anthroplasty
Text
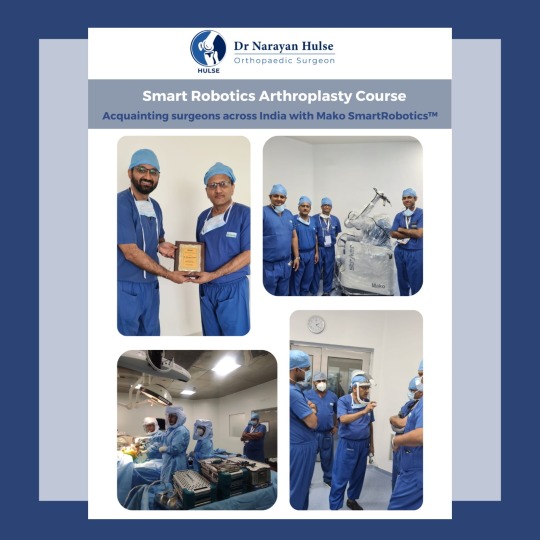
Smart Robotics Arthroplasty Course - Dr. Narayan Hulse facilitated selected surgeons across India to get acquainted with the Mako Robotic Joint Replacements: Total Knee Replacements, Total Hip Replacements and Partial (Unicondylar) Knee Replacements via surgery observations, case presentations and didactic discussions.
Dr. Hulse is committed to train and motivate upcoming and enthusiastic surgeons.
Presenting a few glimpses from the program.
#Dr Narayan Hulse#Hulse Clinic#Mako robotic joint replacements#orthopaedics & joint replacement surgery#best orthopaedic surgeon in bangalore#hip replacement surgeon#knee replacement surgeon#famous orthopedic doctor in bangalore#mako robotic knee replacement#DAA#Smart Robotics Anthroplasty Course
0 notes
Text
uuuhhhh medical malpractice below the cut btw wabughhhh and gore and surgeryyy
I got CARRIED AWAYYYY BYEEEE
hi I would LOVE to be someone's (many peoples actually) little fucked up doctor By The Way. playing the part of a sweet medical professional only interested in the betterment of your health, but of course that's not really the case.
You've been having pains in your hand and wrist? Oh dear, it's good you came to the clinic so soon! I'll patch you up, good as new, poor thing.
Having you take a seat in a chair for surgery and taking a seat opposite you while you're upright. Feeling along your wrists, palms, fingers, working gently and applying pressure- checking for where it hurts and making sure to press the hardest in the places you tell me it hurts most just to hear you whine.
I lean your chair back slightly and ready you for a deeper examination, I'll spare you the anthroplasty job as much as the thought excites me. No, these pains are simply sore muscles that will fade with time and a few hand exercises, but you knew what to expect when you came here with an ailment.
I'm ever so curious about your hands, I can't stop watching how they twitch and writhe, your visible heartbeat at multiple points where your veins are so delightfully close to the surface. I only want a closer look today, nothing fancy. Hell, you were so good during the first half, I'll let you have some anaesthesia. I find my patients are happiest after getting a treat, after all.
Once your hand is thoroughly numbed, I press and prod with first my fingers, then my fingernails around your wrist, before I start my incisions with my scalpel, completely free-hand. I know I don't have long before the anaesthetic will lose its potency, so I work somewhat faster than I usually would without numbing.
First, I look at your radial artery in your wrist, watching how it throbs and twitches. I run my free hand down its length and smile at you. It would mean so much to me to sever that artery, but why would I punish such a sweet thing who's been so co-operative?
I spend the next few minutes opening and sewing shut little holes in the thin flesh of you hands, with my last stop being at your knuckles.
I can see by the way you're starting to squirm a lot more in your seat that the pain is slowly coming back to you, that or you're loving the sight as much as I am. They're such cute little bones, I'm sure the joints between the medial and distal phalanges are much cuter, but the largest ones I can only think would make such an adorable pendant.
I'm shaken from my thoughts as you tap my shoulder lightly. Our time has run out, it seems. I sew you up and offer you some pain killers to take while your new stitches heal up. I'm about to dismiss you before I stop, thinking about how I had gone over the promised time and put you through some unnecessary pain. so, I let you pick a second treat- a piece of candy of your choice.
Before you leave, I take your stitch-spangled palm into my hand and etch a small mark above your index knuckle with a marker pen. That one's mine.
So you leave my clinic, new sutures, and a piece of candy richer. I await your next visit with the patience of a saint. my favourite little patient never fails to disappoint.
#im crimge but im free okay#AH FUCK IDK THE TAGS#eddie wrote this#medical kink#surgery kink#tw gore#tw surgery#tw iatrophobia#mdni#18+ mdni#minors dni#okay i yhink thats good enough
13 notes
·
View notes
Text
Disorders and treatment of orthopedics
Surgery which is related to the musculoskeletal system. Orthopedic surgeons use both surgical and nonsurgical methods to treat musculoskeletal trauma, spine diseases, sports injuries, degenerative diseases, infections, tumors.
Shoulder injuries and disorders: shoulder separation, frozen shoulder, shoulder tendonitis, shoulder bursitis, shoulder fracture.
Knee injuries: adolescent anterior knee pain, meniscus tear, knee replacement.
Elbow injuries: Pitchers’ elbow, Tommy john elbow injury.
Hand and wrist disorders: carpal tunnel syndrome, compartment syndrome, cubical tunnel syndrome, trigger finger, Arthritis of hand, thumb, wrist.
Foot ankle disorders: Bunions, ingrown toenails, lateral ankle instability, Hammertoe, Diabetic limb salvage, lapiplasty.
Hip injuries and disorders: Hip labral tear, Snapping hip syndrome.
Knee arthritis mainly affects women above 60 years.
Orthopedics has extended beyond the treatment for fractures, strained muscles, broken bones ,torn ligaments and tendons, and other injuries.it is dealing with a wide range of acquired and congenital skeletal deformities .
Anthroscopy and arthroplasty are the orthopedic surgeries. anthroscopy is performed for torn ligaments. anthroplasty is to relieve pain in joints after damaged by arthritis.
Drugs used in the treatment of orthopedics are Anti-seizure drugs: gabapentin, topiramate, carbamazepine.
Muscle relaxants: carisoprodol, cyclobenzaprine, diazepam.
Osteoporosis drugs: alendronate and calcitonin.
0 notes
Text
Things to Know About Hip Joint Replacement
Surgery is never fun for anyone and if you are scheduled to have hip surgery in the near future, it is important for you to know all you can about hip joint replacement. This surgery is also called hip anthroplasty, hip heriarthroplasty and total hip replacement. When you have your surgery, you may have all or just part of your hip joint replaced by an artificial hip prosthesis. Most people come through the surgery feeling better and able to walk much more evenly and with less pain. Orthopedic Surgeon in Kota
Most likely you will be given a general anesthesia when you have your surgery. This is best for most people because you will be completely unaware of what's happening during your surgery. Some physicians prefer to administer an epidural anesthesia which leaves you awake but unable to feel anything from the waist down.
The surgery itself has become quite common and generally takes about three hours. Your surgeon will make an incision and remove the head of your thigh bone. Then, he or she will clean the hip socket of cartilage and damaged bone. The new hip joint will be placed inside the socket by using a metal screw which will go directly into your thigh bone. All of your new hip "equipment" will be kept securely in place by special adhesives. When all of this is done, your surgeon will close the incision and you'll be sent to the recovery room to be monitored for an hour or so. Spine Surgeon in Kota
Hip joint replacement surgery is most often performed on people who have become crippled with arthritis. These people cannot get around comfortably and experience severe pain when standing, walking and even sitting. They are limited to the amount of daily activity they can participate in. Most hip replacement patients are in their 60s or older. Doing this surgery on younger people isn't as successful in the long run because these individuals put more stress on the artificial hip, causing it to deteriorate much more rapidly. However, hip replacement surgery has made life much, much better for older individuals. After a short recovery period, they are again able to enjoy life to its fullest and with little, if any, pain.
0 notes
Link
Reverse shoulder Anthroplasty is an implant procedure with ball and socket parts to fix the shoulder joint switch sides. The ball and socket part of the implant allows surgeons to convert a well-fixed stem to reverse without stem removal through intra-operative flexibility.
0 notes
Text
Summary-Analysis and Literature Review of Trans- Cutaneous Oxygenation on Lower Extremity Wounds -Juniper Publishers
Journal of Orthopedic & Orthoplastic Surgery
Research Article
Summary-Analysis and Literature Review of Trans- Cutaneous Oxygenation on Lower Extremity Wounds
*Howard Myles Kimmel, Jamie Matteo, Christopher Phillips and Perry Williams
Podiatrist, Buckeye Foot Care, USA
Submission: April 04, 2017; Published: April 24, 2017
*Corresponding author: Howard Myles Kimmel, Buckeye Foot Care, Podiatrist in Brook Park, Cleveland, Ohio, USA, Tel: +1-216-267-0304; Fax: + 1-216-267-4932; Email: [email protected]
How to cite this article: Howard M K, Jamie M, Christopher P, Perry W. Summary-Analysis and Literature Review of Trans-Cutaneous Oxygenation on Lower Extremity Wounds. JOJ Orthoped Ortho Surg. 2017; 1(1): 555553. DOI: 10.19080/JOJOOS.2017.01.555553
Go to
Abstract
Oxygen is an essential component of wound healing. The discovery of its critical role in maintaining life and healing properties dates back to the late 1700’s. With the invention of hyperbaric oxygen chamber in 1879 research into the medicinal utilization of oxygen began and continues today. More recently, hyperbaric oxygen therapy has been studied and implemented for a variety of functions including wound healing, but recently its effectiveness has been questioned. Due to some of its more adverse side effects, the development of a more localized therapy option transcutaneous trans-cutaneous oxygenation has found its niche in the role of wound healing. Compiling the research and studies of the use of transcutaneous trans-cutaneous oxygenation in the literature, a statistical analysis was utilized to evaluate its efficacy in wound healing.
Keywords: Oxygen; Oxygen Therapy; Topical Hyperbaric oxygen; Ulcer
Go to
Introduction
Wound healing is a complex process of biochemical and cellular events. Anything that disrupts this highly complicated process can possibly cause a wound not to heal. Venous ulcer patients have systemic and local conditions such as venous hypertension that can cause compromised vascularity Wollina et al. [1]. Patients who suffer from arterial ulcers are having an etiology caused by severe macro vascular disease, while diabetic ulcerations are related to both microvascular and macro vascular disease Stephens & Hunt [2].
Hypoxia can be defined as a decreased level of oxygen. In normal wound healing, there are times in which the wound needs to be hypoxic. Prolong periods of hypoxia are abnormal. Successful wound healing depends on a sufficient blood supply to bring various components including oxygen to help facilitate the wound to heal. The central portion of the wound is the area that is usually most hypoxic, while there more oxygen on the periphery of the wound. The partial pressure of oxygen (pO2) in dermal wounds ranges from 0-10mmHg centrally to 60mmHg at the periphery. The pO2 in the arterial blood is approximately 100mmHg Gordillo & Sen [3].
Angiogenesis, or neovascularization, takes place as preexisting vessels send out capillary buds to produce new vessels. Proliferating capillaries bring oxygen and micronutrients to growing tissues and remove catabolic waste products. Following an injury, angiogenesis is stimulated by the synergistic interaction of growth factors and cytokines secreted by damaged cells in wound tissues exhibiting hypoxia. Oxygen and its reactive derivative hydrogen peroxide are known to induce angiogenic responses such as the induction of VEGF expression Sen et al. [4], Sen et al. [5], Trabold et al. [6]. There are essential growth factors associated with angiogenesis (BFGF, HB-EGF, KGF and VEG-F) which are increased with oxygenation therapy Kalliainen et al. [7]. O2 treatment induces VEGF mRNA levels in endothelial cells and macrophages and increases VEGF protein in wounds in vivo Sheikh et al. [8]. VEGF was found to have a 20fold increase with O2 therapy Hunt [9]. Chronic hypoxia impairs angiogenesis causing death and dysfunction of tissue Hopf et al. [10]. Administration of topical O2 accelerates vessel growth and alleviates the danger of tissue death Knighton et al. [11].
Lavan et al. [12] illustrated that the rate of synthesis of collagen in closed wounds is accelerated by hyperoxia Lavan and Hunt [12]. Collagen synthesis has multiple post-translational steps that are directly O2 dependent including prolyl hydroxylase, lysyl hydroxylase and lysyl oxidase. Increasing oxygenation results in increased collagen deposition and tensile strength Hunt [13]. It has also been observed that O2 may trigger the differentiation of fibroblasts to myofibroblasts which are responsible for wound contraction Roy et al. [14]. The oxygenation of wound tissue is an extremely sensitive indicator of infection in surgical patients Greif et al. [15]. Granulocytes are unable to ingest bacteria without adequate perfusion therefore increasing the bacterial load and increasing the rate of infection. Reactive oxygen species (ROS), such as H2O2, which are generated by NADPH oxidases in wound neutrophils and macrophages, mediate the ability of supplemental O2 to reduce infection Hopf [16].
In 1775 Priestly made medical history by discovering oxygen and demonstrating that oxygen maintained the vitality of candle light and suggested its important role in human life. However it was Henshaw, a British physician, who introduced the hyperbaric chamber. Further progression of the device led to Fontaine's use of the chamber in the operating room in 1879 Braswell and Crowe [17]. The United States Navy began to use hyperbaric oxygen in 1943 for treatment of decompression sickness and air embolism. In the early 1960s the National Sea Foundation investigated the claims made by Jacques Cousteau that his divers healed their work related wound better when they lived in an under the sea construct at 35 feet under the Red Sea.
In the 1970s the Hyperbaric Oxygen Committee of the Undersea Medical Society defined four categories of clinical usage. Categories I and II demonstrate the value of oxygen in wound healing. Initially large recompression chambers were used, with and without the modification for mask breathing of oxygen. The toxic side effects from the systemic absorption of oxygen including pulmonary and CNS toxic reactions led to a more localized therapy. It was Olejniciak who reported success with the application of high pressure oxygen to injured extremities using trans-cutaneous oxygen Olejniczak and Zielinski [18]. Specially built chambers were designed to fit around the affected limb creating a controlled, sealed pressure atmosphere and therefore limiting systemic exposure.
Hyperbaric Oxygen (HBO) is a treatment in which patients breathe in 100% oxygen inside a chamber that is pressurized at higher than the sea level pressure of greater than 1 atm. According to Undersea and Hyperbaric Medical Society position paper, in order for the therapy to be officially recognized pressurization should be at least 1.4 atms or higher. Van Unnik found that when treating Clostridial myositis and myonecrosis, gas gangrene, it is essential to achieve tissue PO2 of 250 mm/ Hg Van Unnik [19]. This is necessary to stop the advancing phlegmon caused by infection tissue producing alpha toxin. With compartment syndrome and crush injuries, HBO can be used as an additive therapy to possibly decrease complications that are often associated with these types of injuries. HBO is recommended for crush injuries graded Gustilo IIIB and C fractures Gustilo et al. [20]. Treatment criteria for HBOT in crush injuries varies depending on suspected pathophysiology.
With problematic ulcerations and recurrent wounds, HBO is a recommended as an adjunctive therapy when these wounds have failed other treatments. The suggested treatment protocol in diabetic wounds is HBO given at 2.0 to 2.4 ATA for 90 minutes daily for 4 to 6 weeks Feldmeier et al. [21]. As previously discussed, the toxic side effects associated with HBO have led to the development of a more localized therapy options. One of these is the Trans-Cutaneous Oxygen Therapy. By minimizing the size of the unit, these types of devices have their oxygen provided by traditional respiratory oxygen concentrators. They are easily transportable allowing for application of the treatment at virtually any care site [22].
Trans-Cutaneous Oxygen Therapy (TCOT) is thought to provide increased supplies of superoxide dismutase, catalase, and reduced glutathione and other free radical quenches Gordillo and Sen [3]. Trans-cutaneous oxygen can eliminate bacteria by producing reductive oxygen species Trabold et al. [6]. TCOT has been demonstrated to increase oxygen of hypoxic wound tissues therefore encouraging of angiogenesis, increased collagen production and tensile strength, increased epithelial proliferation, stimulation of fibroblasts, induction resistance to bacteria and abundant granulation tissue formation Heng [23]. TCOT can be beneficial in reducing edema in extremities in addition to increasing venous blood flow and lymphatic drainage from intermittent positive pressures Tawfick & Sultan [24]. TCOT systems operate by applying cyclical oxygen pressure directly to the wound site within a sealed and humidified environment. This can provide a greater tissue oxygen diffusion gradient and increased tissue oxygenation. The cyclical nature of the pressure also creates a sequential compression effect which helps reduce peripheral edema and stimulates wound site perfusion.
Go to
Analysis of Published TCOT Papers
The following analysis assesses the various studies published in human subjects with TCOT Upson provides a clinical report, consisting of two case studies, that discusses the effectiveness of trans-cutaneous oxygen for the treatment of ischemic lower extremity ulcerations and preventing amputations of the lower limb Upson [25]. This clinical report also discusses treatment guidelines for improving the quality of wound care for recalcitrant wounds of the lower extremity. Case 1 is a 54 year old male with multiple ulcerations of his left lower extremity for duration of approximately 10 months. After 8 weeks of TCOT (5 days/wk., twice daily for 60-90 minutes) there was reported 75%, 48%, and 80% healing of three of the major ulcerations of the lower left extremity. Case 2 was a 69 year old male with a lower left leg compartment fasciotomy that never healed of 8 months duration. After 1 week of TCOT the treatment was discontinued because the ulceration had completely healed. The authors concluded that trans-cutaneous oxygen provides good results and healing rates of recalcitrant ischemic wounds in the lower extremity.
Heng et al. [23] reported endothelial cell toxicity from a clinical and cellular level in patients treated for prolonged periods of time for leg ulcerations Heng [26]. Six patients with leg ulcers of varying etiologies were treated with TCOT for a range of 5-9 weeks. All patients received 6 hours of therapy per day on 4 consecutive days per week followed by 3 consecutive days of rest. 4mm punch biopsies were also taking from all patients and split in half to be examined under light microscopy and electron microscopy. In the first 4 weeks all patients experienced decreased slough formation on the base of the ulcers, growth of abundant vascular granulation tissue and overall decrease in size of the ulcers. In three of the patients at the 8-9 week mark, depressed white areas were seen within the granular/vascular areas that had generated. TCOT was stopped in all three of these patients and all white areas had been reversed within 1-2 weeks of the oxygen therapy cessation. These white areas were assumed to be due to oxygen toxicity.
Under light microscopy biopsies of the white areas showed a paucity of capillaries with fragmented nuclei from neutrophils. Biopsies from controlled leg ulcerations not receiving trans- cutaneous oxygen showed granulation tissue with fewer capillaries than those biopsies from leg ulcers that had received TCOT. Under electron microscopy, biopsies from the control leg ulceration showed endothelial cells with slight indentation of nuclear membranes and intact mitochondria which appear to be fewer than those in endothelial cells of oxygen treated ulcers. Biopsies from tissues that had been treated with prolonged hyperbaric oxygen therapy (8 weeks or more) showed capillaries lined with endothelial cells with marked indentation of nuclear membranes. Many of the mitochondria of these cells appeared swollen and degenerate. Also, many granules from ruptured neutrophils were found among the damaged endothelial cells. The authors concluded that TCOT can increase the number of capillaries in tissues markedly, however detrimental effects can occur in prolonged oxygen therapy.
Leslie et al. evaluated the use of TCOT for 2 week duration in a randomized controlled trial (RCT) Leslie et al. [27]. There were a total of 29 patients with healing diabetic foot ulcers (12 in the TCOT group and 16 in the control group). After the 2 week RCT the decreasing change in ulcer size did not differ statistically between the TCOT group and the control group. Also, a trend towards slower wound healing was noted in the TCOT group. It was concluded that the healing of diabetic foot ulcers was not accelerated by the use of TCOT in this particular study.
Heng et al. [28] reported a prospective randomized controlled trial to confirm the efficacy of TCOT in stimulating angiogenesis and healing in necrotic and gangrenous wounds Heng [26]. This prospective study looked at a total of 40 patients (79 ulcers) that were collected over a period of 12 months who were randomly divided into either a TCOT treatment group or a standard wound care group. Following sharp debridement the TCOT group was treated 4 hours per day, 4 days per week for 4 weeks. Oxygen pressures always remained between 1.004 and 1.013 atmospheres. The standard wound care group underwent rotation every 2 hours to reduce pressure and other tissue pressure reduction techniques.
Patients with OM underwent IV antibiotics (either Ceftriaxone 1-2g daily and or PO Ciprofloxacin 500mg bid). Ceftriaxone (or Vancomycin) and Gentamycin was given for those patients who were septic. Patients with gangrene or life threatening OM received digital or forefoot amputations when appropriate regardless of the group they are in. Results showed that 90% of the wounds in the trans-cutaneous oxygen group healed compared to only 22% of the wounds in the standard wound care group. The size of the ulcers showed that they were statistically smaller in the TCOT group. Capillary density was statistically significantly higher in the TCOT group as well. It was concluded that TCOT is effective in stimulating angiogenesis in the healing of necrotic wounds.
In another study, Heng et al. [28] performed a prospective study that examines the feasibility of using TCOT to heal necrotic wounds Heng et al. [28]. Fifteen patients (24 total necrotic and/or gangrenous ulcerations that either did not improve or worsened after 6 weeks of standard wound care were treated with TCOT. Patients received oxygen therapy 4 hours per day, 4 days consecutive days per week for 4 weeks. This was followed by 2 weeks of rest. If a patient's wound was unhealed after this 6 week course, the therapy procedure was repeated. 100% of the level 2 wounds healed within 2-4 weeks of oxygen therapy. 90% of the level 3 wounds healed within 4-10 weeks of treatment. 87.5% of the level 4 wounds healed within 4-12 weeks. T-tests showed statically significant decrease in wound size day after day with TCOT These authors concluded that TCOT is associated with decreased costs as well as improved wound healing.
Landau and Schattner reported a case series evaluating the effects of adjunctive TCOT and low energy laser irradiation on chronic diabetic foot ulcerations that have been refractory to 4.5 to 12 months of wound care treatment Landau and Schattner [29] . The first 100 patients with non-gangrenous ulcerations that had been refractory to at least 14 weeks of convention wound care were evaluated in this study. Oxygen therapy was administered for 150 minutes 2-3 times per week and a He-Ne low-energy laser irradiation was administered concurrently at 632.8nm.5mW. The laser treatment was administered for 20 minutes at a dose of 4 J/cm2 to the face of the ulcer. Patients were monitored every two weeks and results showed an 81% cure rate after 25 ± 13 treatments over 3.2 ± 1.7 months. Upon follow up (median 18 months) only 3 of the 81 patients that initially healed had re-ulcerated. The authors concluded that TCOT may be a safe, simple, and inexpensive early adjunctive treatment for patient with chronic diabetic foot ulcerations even though this study was open and uncontrolled.
Edsberg et al. [30] published a prospective uncontrolled case series that evaluates the effects of TCOT with electrical stimulation on the healing of chronic wounds Edsberg et al. [30]. All patients (8 total; 4 males, 4 females) were geriatric residents of a long term care facility with stage III or stage IV pressure ulcerations (7 sacral and 1 ischial) that were refractory to at least 2 weeks of conventional treatment. TCOT was applied to the wounds of all 8 patients with three of the patients also receiving concurrent electrical stimulation. Oxygen therapy was delivered twice daily for 90 minutes, 7 days a week. Electrical stimulation was administered at 150 volts, 120 pulses/second and 255|i pulse-pair intervals for 30 minutes once daily, 5 days a week. Healing times ranged from 8-49 weeks. After 4 weeks of treatment, wound size had decreased on average 34.4%. There was no statistically significant increase in healing was noted between the 5 patients that were receiving TCOT alone and the other 3 patients that were receiving the TCOT as well as the concurrent electrical stimulation. The authors conclude that TCOT facilitates healing and full closure of pressure ulcers in patients with and without diabetes mellitus.
Kalliainen et al. [7] performed a retrospective study evaluating trans-cutaneous oxygen an adjunct to wound healing Kalliainen et al. [7] In their study, 7 doctors treated 58 wounds in 32 patients over the course of 9-month-period of time. The wounds were treated with 100% oxygen that was administered at one atmospheres of pressure for 90 minutes for 4 consecutive days followed by a 3-day rest period. This cycle was repeated as long as the wound showed improvement. Of the 58 wounds, 38 or 65.5%, healed during the treatment period with trans- cutaneous oxygen. The authors concluded a benefit to wound healing with the application and use of oxygen therapy.
In a case study by Edsberg et al., they evaluated the efficacy of TCOT reducing an epibole on a Stage IV sacral pressure ulcer on a seventy-seven year old female patient Edsberg et al. [30] . The wound was treated with trans-cutaneous oxygen via a disposable sacral unit for 60 minutes, two times a day, seven times per week. Treatment also included a high-volt, pulsed electrical stimulation for 30 minutes a day five times a week for a period of 13 weeks. Full wound closure was obtained at the end of the treatment period.
Gordillo et al. [22], reported that trans-cutaneous oxygenation significantly improved wound size Gordillo et al. [22]. The goals of the study: were to examine the changes in wound closure size and look at the expression of oxygen- sensitive genes, such as VEGF, in biopsies collected from wound edge tissue. In this study, 1,854 patients were screened and of those 57 patients were enrolled. 32 patients were enrolled in the HBO arm and 25 patients were enrolled in the TCOT arm. In this particular study, HBO did not result in significant improvements in wound closure.
The data analysis to access the efficacy of TCOT was identical to that used for HBO. TCOT in this study was found to have a significant improvement of wound closure by decreasing wound volume. The study then directed their examination to O2 sensitive genes in the wound edge tissue. They goal was to the presence of three genes, VEGF, TGF-β1, and COL1A1. These genes were selected based on their oxygen sensitivity and their functional relevance of the gene products to wound healing. The effect of supplemental oxygen therapy was analyzed by measuring the relative change in the target gene expression for each individual compared with their baseline T0 values. Neither TGF-β1 or COL1A1 showed any significant change. VEGF however, was significantly higher in TO-treated healing wounds. Neovascularization is stimulated by hypoxia but cannot sustain it. Hyperoxia can also induce VEGF. This study is the first to demonstrate that TCOT significantly induces VEGF expression in chronic wounds.
Tawfick and Sultan investigated if TCOT offered an improved outcome over conventional compression dressings in the management of refractory venous ulcers Tawfick and Sultan [24]. This study had two goals: one was to study the proportion of ulcers healed at 12 weeks and the second goal was the time taken for full closure, percentage of reduction in the ulcer size at 12 weeks, MRSA elimination, pain reduction, and recurrence rates. Patients were either enrolled in TCOT (n=46) or conventional compressive dressings (CCD) (n=37) for 12 weeks or until full healing was demonstrated. At 12 weeks, 80% of the TCOT managed ulcerations were fully healed compared to 35% of those that were treated with CCD. The average time to complete healing in TCOT was 45 days as compared to 182 in those with CCD. At 12 month follow up none of the ulcerations that were treated with TCOT showed any signs of recurrence.
Blackman et al. [31], investigated the clinical efficacy of a pressurized TCOT on 28 patients in an outpatient setting Blackman et al. [31] Seventeen patients were treated with TCOT five times per week for an hour per treatment in pressure cycles between 5 and 50 mm/hg. Eleven patients were used as the control arm and treated with silver-containing dressings changed at least twice per week. Fourteen of the 17 ulcers in the treatment group, 82.4%, in the treatment group healed while 5 of the 11 ulcers in the in the control group, 45.5%, healed. The median healing time was 56 days for the treatment arm and 93 days for the control.
Heng published a case study in 1983 discussing the use of TCOT for a foot ulcer in a patient with polyarteritisnodosa Heng [32]. The 63 year old male presented with a large area of necrosis involving the plantar aspect of the left foot. Using a disposable polythene bag TCOT was administered at fifteen liters per minute for six hours per day, for four consecutive days each week, for six weeks in duration. The pressure of the oxygen was maintained at 25-30mmHg above atmospheric pressure. Three unsuccessful attempts at split thickness skin grafts application were made before a second course of TCOT of four weeks duration was completed. After completion, the ulcer was treated with conservative wound care and healed in six months. During the entire treatment course of the ulceration the patient remained on oral prednisone 20mg and Cytoxan 50mg daily. This case reveals that the use of TCOT in can produce granulation tissue in deep ulceration and result in limb salvage.
In another case study by Heng, two patients with leg ulcers characteristic of pyodermagangrenosum were treated with TCOT Heng [33]. Oxygen therapy was administered at 25-30mmHg above atmospheric pressure at a rate of about 15 1/m for 6-8 hours per treatment period, 4 times a week for a total of two to four weeks. A total of four ulcers were present at initiation of therapy. The ulcerations varied in size, ulcer 1 measured approximately 5000mm2, ulcer 2 approximately 3850mm2, ulcer 3 1000mm2, and ulcer 4 250mm2. The two largest ulcers healed at a rate of 106 (2%) and 108 (2.5%) mm2/day; the medium ulcer closed at the rate of 33mm2/day; and the smallest at 5mm2/day. The most significant finding after the initiation of TCOT was the almost immediate arrest of any further extension of the ulcerations. In the 3 weeks prior to therapy they enlarged at a rate of473mm2/day. The two smallest ulcers healed 6 weeks after initiation of therapy and the larger two healed within 12 weeks.
In a similar study Heng et al. used a modified technique for administering hyperbaric oxygen with the use of disposable polyethylene bags in the treatment of arterial leg ulcers Heng et al. [33]. Six patients with a total of twenty-seven chronic arterial ulcers were treated. Five men with a total of ten ulcers served as controls. Eighteen of the twenty-seven treated group ulcers (5/6 patients) were healed within six to twenty-one days. A healing rate of 7.8% ± 1.15% per day for the healed ulcers was recorded. In addition a 50-90% reduction in size of seven of the nine remaining ulcers was noted after a three week period. None of the ulcers in the control group healed. The potential advantages of the disposable bag method included fairly low expense, lack of cross-infection, and simplicity in the administration of oxygen. The patients could be treated either inpatient or outpatient as well.
Fries et al. [34] evaluated the wound healing efficacy of topically applied pure oxygen on pigs with dermal excisional wounds Fries et al. [34]. Four female 80 lb. pigs were used for this study. Under sedation, dermal wounds (1in x 1in.) were inflicted along the dorsum of each pig using size 10 scalpel. A total of 40 wounds throughout the 4 pigs were studied. Half of the wounds on each pig were subjected to topical oxygen treatments as the other half of the wounds on the same pig were left open to room air. The oxygen treatments were administered for 3 hours per day for 7 days. These authors conclude that topically applied oxygen is capable of oxygenating the superficial wound tissue but not deep tissue and that the topical application of pure oxygen to open wounds had some favorable impact on the overall healing process.
Said et al. hypothesizes that transdermal sustained-delivery oxygen therapy would improve wound healing in an animal model Said et al. [35]. In this animal model, 4 full-thickness 7mm punch biopsies were created in each ear of a young female New Zealand white rabbits. Oxygen treated wounds received continuous 100% Oxygen at ml/hr. under a semi-occlusive dressing. Ears were harvested each at day 5 and day 8. Using a histological analysis wounds showed significantly greater wound healing at both days 5 and 8 in the oxygen therapy group. Epithelization across wounds was nearly double in the oxygen treated group compared to that of the control group. These authors concluded that epithelial wound healing is improved in an environment of sustained-delivery 100% oxygen.
Sen discussed the role of oxygen and its effect on wound healing Sen [36]. When attempting to oxygenate a wound it is important to utilize a multifaceted approach to wound healing. Of note, it is important to remember that both too little and well as too much oxygen may impede wound healing. The study suggests that it seems important to assess each wound and dose oxygen appropriate to each individual wound. The author also asserts that the wound tissue does not discriminate between whether the oxygen is delivered topically or systemically.
A literature review by Gordillo and Sen evaluated the evidence based recommendations for the use of TCOT in the treatment of lower extremity wounds Gordillo & Sen [3] They stress that it is important for practitioners to be mindful of the local wound environment, as this is the ultimate determinant of O2 delivery. Other factors such as infection, blood supply and health of the patient are of the utmost importance also. Trans- cutaneous oxygenation is another treatment modality available to practitioners managing difficult wounds. Supplementing wound tissue pO2 has shown to increase collagen deposition and decrease wound infection Knighton et al. [11]. It has also been shown in the literature review, evidence supporting the role of pO2 and angiogenesis.
There are some critics to the use of trans-cutaneous oxygen. Feldmeier et al. [21] made a position statement on the use of topical oxygen for chronic wounds Feldmeier et al. [21]. It was stated that with topical oxygen in an airtight chamber or polyethylene bag is sealed around a limb or trunk, while high flow oxygen is introduced in the chamber/bag over the wound. Pressures of just over 1.0 atmosphere are recommended due to the concern that any higher pressures could potentially decrease arterial/capillary inflow to the tissue in the affected area. The literature on topical oxygen at this point consists mainly of small case series and uncontrolled trials which don't focus specifically on any particular type of wound. The only randomized controlled trial for topical oxygen in diabetic foot ulcers published at that did not demonstrate improved wound healing Leslie et al. [27]. It is noted that for optimal effects from TCOT, wounds must be debrided prior to oxygen treatment. Any exudative or proteinaceous coating over the base of the wound will significantly impair the oxygen penetration.
Cronje stated a major challenge to researchers is how to improve the delivery of oxygen and blood to wounds that have these deficiencies Cronje [37]. One of the ways to supplement oxygen to deficient tissues that are deficient is through TCOT. The author states that the oxygen absorbed through intact skin is negligible and even through open wounds it is extremely small. Wound healing depends on a gradient that extends from the periphery into the middle of the wound which directs and initiates the normal wound healing process. The author states that even if topical oxygenation increases wound oxygen levels, the gradient would be reversed putting higher levels of oxygen at the periphery of the wound. Systemic hyperbaric oxygen therapy actually accentuates that normal gradient, unlike TCOT.
Go to
Experimental Section
Our initial intent was to do a meta-analysis that compared studies examining the effect of Hyperbaric Oxygen treatment on ulcer size. After reviewing the literature, we found no studies similar enough to do a formal Meta analysis. As an alternative to our initial objective, we decided to use a model-based approach to explore the data. Thus, we used the data reported in the 16 studies were viewed to develop a model describing the functional relationship between the change in ulcer size and the treatment method (oxygen versus control). We searched the 16 studies originally reviewed for similar metrics that provided us data to build this model. Five of these 16 studies reported results that allowed us to estimate a model. They were: Heng et al. [33], Heng et al. [28], Leslie et al. [27], Tawfick and Sultan [24], and Edsberg et al. [38] Heng [23], Leslie et al. [27].
The response variable that we examined was the mean ulcer size. We conditioned our response variable on whether the patients received oxygen treatment and the length of the study. That is, we compared the reduction in ulcer size in treatment groups and control groups and controlled for how long patients were observed. We used a linear mixed effects regression model that allowed the intercept to change based on the study (i.e., it was a random effect). We weighted our model using the sample size in each study. Additionally, in our fixed effects, we forced the intercept to be the same for treatments and controls in ceat time=0 the treatment would not affect the size of the ulcer. Thus model was of form:
yij=β0+β1(treatment)x(time)+β2(time)+ηi+Ei
ηi~N(0,ρ)
Eij~N(0,σ2)
Where yij was the ulcer size of the its study and jth patient, β0 was the mean initial ulcer size, β1 was the change in ulcer size due for the treatment group and time since the beginning of the study, and β2 was the change in ulcer size due to times since the beginning of the study for the control group. Hi was the difference in intercept for the it's study, and had mean 0, and variance ρ. We assumed the errors were normal, with mean 0 and variance σ2. We estimated our model parameters using thelme 4 package in Program R (function: lmer). We examined residual plots to determine if we violated our model assumptions.
We note that there was much variability among the study designs, and that this comparison does not account for all the variability. For example, Heng et al. [23] did not use a completely randomized design to assign patients to either control or treatment while Leslie et al. Did Heng [23], Leslie et al. [27]. In addition to the variability among treatments, some of the studies did not explicitly report the values we used in this analysis. For example, most studies reported the mean size of ulcers at the onset of their studies. Tawfick and Sultan did not report the mean size Tawfick and Sultan [24]. Instead, they divided ulcer sizes into 5 groups, and reported the number of patients that had ulcers in these five group sizes. To estimate what the mean size was, we used the median value for each of the five groups and multiplied it by the number of patients in these groups, summed these values, then divided by the total number of patients. Additionally, Heng et al. [23] Did not report the overall decrease in ulcer size for their 21 day study Heng [23].
Instead they reported the expected daily increase/decrease in ulcer size. From these values we calculated the overall change in ulcer size by multiplying the daily increase/decrease by the length of the study. For the treatment group this resulted in a negative ulcer size for the 21day study, indicating that most of the patients healed before the 21day study was concluded. To avoid using impossible negative ulcer size values we selected the number of days in which the ulcer size was estimated to be ≥ 0. This was on day16. Based on these caveats, we recommend that these results be viewed as exploratory, and might not be unbiased estimates of the actual parameter values we attempted to estimate. All of the data used in our analyses are reported in (Table 1) (Figure 1).
Go to
Results and Discussion
Our model appeared to meet the assumptions of a linear regression model. All of the predictor variables in our model were significant, and P-values were 0. We found that the treatment group healed faster (P=0.000) than the control group on average. The fixed effects parameter estimates (and estimated standard errors) were: β0=839.55(77.82), β1=-12.94(0.60), and β2=-8.49 (0.66). Thus, the mean ulcer size before the studies began was 839.55mm2, and decreased in size by 12.94mm2 per day for the control groups, and decreased in size by 12.94+8.49=21.43mm2 for the treatment groups. The expected time for 100 percent recovery was 40days for the treatment group and 65days for the control group. The standard deviation of our random effect (i.e., √ρ) was 167.17mm.
Go to
Conclusion
Multiple studies were evaluated for this research looking at the ability of TCOT in healing chronic wounds that had failed other conservative treatment measures and otherwise had a high possibility of not healing. We did not limit out research to parameters specific wound types, in order to allow us to better assess which type of wounds have been shown to be responsive, or not, to TCOT. In wound care, TCOT appears to provide the benefits of full body hyperbaric oxygen while avoiding the potential systemic adverse effects. The addition of therapeutic oxygen levels to an otherwise hypoxic region of the body helps with leucocyte function, sequesters the otherwise unopposed oxidative free radicals, and allows angiogenesis to continue. The oxygen levels and pressures provided by TCOT establish an ideal environment for these processes to occur.
The efficacy and safety of TCOT in treating chronic ulcerations that have previously failed conventional treatment regimens has been demonstrated within the published literature in numerous RCTs, controlled studies and case reports as being an effective adjunctive wound care modality. It is important to note, that there are only a limited number RCTs performed to date and the methods between the studies thus far are inconsistent. Further RCTs with large sample sizes and consistent study parameters are needed to adequately affirm these positive results to the larger greater patient population. However, this being said, our review suggests that TCOT is likely to be effective in healing recalcitrant ulcerations than both standard conventional therapies and other adjunctive modalities alike.
Go to
Acknowledgment
The authors would like to thank Melanie Johnson, DPM in assisting in the preparation of this manuscripts and also Daphne Slaw ski for researching some of the articles used in the preparation of this manuscript.
Author Contributions Howard Myles Kimmel DPM, MBA was the primary author. Perry Williams performed and wrote the summary analysis section. Jamie Matteo DPM wrote the abstract and the introduction and Christopher Phillips, DPM wrote the analysis of TCOT.
Go to
Conflict of Interest
“The authors declare no conflict of interest".
0 notes
Photo

Robotic Total Knee Anthroplasty
Know about Robotic Total Knee Arthroplasty (TKA) surgery along with its benefits, efficiency, soft-tissue handling etc. Find more about robotic knee surgery at Meril Life.
https://www.merillife.com/blog/medtech/navigation-vs-robotics-a-transformation-for-a-better-surgical-experience
0 notes
Text
Orthopedic Surgery Options and the New You
If you are having pain in your hip that will certainly not deal with, possibly it is time to meet a physician that concentrates on orthopedic surgical treatment. You may have a serious form of arthritis that causes pain when you walk and you need a treatment for it. There are solutions that do not consist of a total hip substitute.
There are non-orthopedic options to a full surgery as well as if you can function with a little discomfort, you can prevent it if you want. These include physical therapy, help that will certainly aid you stroll better, various drugs that assist eliminate the discomfort, steroid shots into the joint itself, and supplements that help soothe the impacts of the arthritis. If done appropriately and you can live with it, any type of mix of these can help you stay clear of having even more intrusive procedures done.

If none of the above treatments function, you can take a more radical approach and attempt hip resurfacing. During this orthopedic procedure, a smaller quantity of the hip joint, than in a total hip joint replacement procedure, is removed as well as a small metal cap is put in addition to that round joint. After that an outlet is manufactured and placed right into the hips, however extra bone is left than would certainly be in a substitute surgical procedure. This is popular amongst more youthful individuals that experience joint inflammation.
One more approach to prevent orthopedic surgical treatment is called hip blend. Throughout this procedure, the hip bone and also the thigh are operatively integrated with each other to make sure that you can eliminate all movement, consequently, removing the pain, and also held together by a metal plate and numerous screws. With the introduction of the much more popular of hip substitute surgical procedure, it is neither done really usually now, but was typically done on individuals that strive on a task daily. The plate will not break, however patients will limp completely as well as may someday need to get the complete substitute surgical treatment.
You can additionally try resection anthroplasty, where the specialist will get rid of a section of the bone that surrounds the hip, thus enabling it to be filled with mark tissue in time. This is seldom done, yet is done on those that's infection is out of control making regular walking as well as executing everyday jobs virtually impossible. Despite the fact that the treatment is carried out, you will still require help strolling, so a walker or props are still required.
To get about more info visit this site: - yellow fever vaccine locations
Lastly, you have the hip osteotomy choice, which is generally the procedure of option when an individual has actually been detected with hip dysplasia, normally from early stage. This osteopathic procedure realigns the hip joint bones as well as is normally done on those clients whose joint inflammation is brought on by some one more problem.
0 notes
Text
A Brief View of Surgeries at Spine Surgery Clinics
The Surgeries in spinal cord are providing better results with every passing day as superior technology are coming up. Dentists are employing unusual tools to do spinal surgery successfully. Recently an American physician has employed a particular twist system for spine surgery. This new instrument will guarantee an effective surgical procedure as a patient will shed minimal blood while the surgery has been done. There are several different cases where operations on spinal cord have proved highly beneficial for individuals in America. The science in this country is advancing with the progress in engineering and Texas appears to be among the prime countries of the nation.
The Austin spine operation Centers perform various types of spinal cord surgeries. The physicians at Austin spine operation centers utilize modern equipments and unique apparatus to alleviate patients from back pains. A few of the favorite surgeries are clarified below.

Laminectomy
Many Men and Women Develop serious spine as they grow older. This is because of the formation of a bony arch termed lamina from the dorsal surface of vertebral column. This issue is usually shaped with developing age. The laminetomy involves working outside the lamina. This surgery is usually an optional process rather than a crisis surgery. A fantastic surgeon conducts comprehensive diagnosis before operation to determine if a patient really needs this surgery or not.
Spinal Fusion
This surgical Technique can be used to combine a few variety of vertebrae. The purpose of the surgery is to get rid of the pain that's brought on by abnormal motion in the joints that are affected. Usually, bone tissue grafting is used inside this operation to improve a individual's bone formation.
Disc Anthroplasty
This Surgery entails replacement of disk in the spinal column. This process is used as a treatment for chronic low back pain, cervical pain which arises from degenerative disc diseases. Surgeons use specific metallic plates for disk replacement.
For all of the aforementioned Operational processes, several pathological evaluations are conducted during The identification. Following the operation a patient is advocated complete rest. This also helps the individual to Recuperate from the operation and during this time The stitches dry up and recovery occurs.
0 notes
Text
Reverse Shoulder Anthroplasty Market Size, Status and Forecast to 2024
Anthroplasty is a surgical reconstruction that relieves a patient from pain by regaining or reconstructing the original movement of damaged or degenerated joint. In case of reverse shoulder anthroplasty, the artificial parts are attached in reverse i.e., the socket to the bone of upper arm and glenoid ball to the shoulder blade. This reversal of joint has unique mechanical advantage. Reverse shoulder anthroplasty is employed in patients with severe arthritis, large glenohumeral fracture or rotator cuff arthropathy, or failure of normal total shoulder anthroplasty i.e., revision surgery. Reverse shoulder anthroplasty is performed with the primary goal of reducing pain and the secondary goal of improving the overall strength, motion and thereby the function of joint. The successful surgical procedure results in improved shoulder function due to change or replacement in joint position which completely removes arthritis and rotator cuff tear. The patient experiences substantial improvement in shoulder function, with the ability to raise the arm overhead and increase in range of motion of shoulder.
Obtain Report Details @
https://www.transparencymarketresearch.com/reverse-shoulder-anthroplasty-market.html
Major players in the global reverse shoulder anthroplasty market have various advantages such as, technologically advanced prosthesis, to ensure success of the surgeries. The market is driven by extensive research and development for improvement of the biological fixation and wear of the implant, increasing demand from health care professionals across the world for advanced implants, and rising focus of market players to provide quality products with enhanced properties responsible for anchorage and orientation of the implant to aid the shoulder function after anthroplasty. There is no other anthroplasty procedure available for patients with large rotator cuff tear. Hence, demand for reverse shoulder prosthesis is rising exponentially. However, loosening of glenoid component, post-surgical complications such as risk of allergy, blood clots, and permanent pseudo paralysis are some factors restraining the global reverse shoulder anthroplasty market.
Request Report Brochure @
https://www.transparencymarketresearch.com/sample/sample.php?flag=B&rep_id=19040
The global reverse shoulder anthroplasty market has been segmented based on product type, end-user, treatment, and region. In terms of product type, the market has been segmented into humeral socket and stem, body and liners, glenospheres, and attachment devices such as baseplate and screws. Based on end-user, the reverse shoulder anthroplasty market has been segmented into hospitals and orthopedic clinics. In terms of treatment, the market has been classified into arthritis, large rotator cuff tear, revision surgery, and others (severe glenohumeral fracture).
Rising incidence of shoulder injuries and arthritis across the world, worldwide acceptance of and technological advancements in reverse shoulder anthroplasty, and availability of better surgical facilities are some of the factors attributed to the high growth of the global reverse shoulder anthroplasty market. Expanded surgeon adoption and medical education for reverse shoulder anthroplasty, and trabecular metal technology are expected to fuel the growth of the global reverse shoulder anthroplasty market. Despite technical advances in reverse shoulder anthroplasty, higher complication rate limits the spread of the procedure across the globe. However, the unmet need of anthroplasty for revision surgery and severe rotator cuff damage are responsible for increase in interest of manufactures.
Enquiry for Discount on this Report @
https://www.transparencymarketresearch.com/sample/sample.php?flag=D&rep_id=19040
About Us
Transparency Market Research (TMR) is a global market intelligence company providing business information reports and services. The company’s exclusive blend of quantitative forecasting and trend analysis provides forward-looking insight for thousands of decision makers. TMR’s experienced team of analysts, researchers, and consultants use proprietary data sources and various tools and techniques to gather and analyze information. Our business offerings represent the latest and the most reliable information indispensable for businesses to sustain a competitive edge.
Contact Us
Transparency Market Research
State Tower,
90 State Street, Suite 700
Albany, NY 12207
United States
Tel: +1-518-618-1030
USA - Canada Toll Free: 866-552-3453
Email: [email protected]
Website: www.transparencymarketresearch.com
0 notes
Text
Stryker launches expensive Mako robot for knee replacement in cost ... - MedCity News
MedCity News
Stryker launches expensive Mako robot for knee replacement in cost ...
MedCity News
Stryker is launching its Triathlon total knee on its Mako robotic system, reportedly priced at $1 million, at a time of bundled payments and cost consciousness in ...
Stryker launches Mako total knee replacement application: 5 key notesBecker's Orthopedic & Spine
Local News: Local joint surgery gets Mako makeover (3/14/17 ...Dickinson County News
Stryker Launches MAKO Robotic-Arm for Knee AnthroplastyNasdaq
all 6 news articles »
1 note
·
View note
Text
Global Reverse Shoulder Anthroplasty Market Share, Industry Growth, Business Strategy, Trends and Regional Outlook 2026
Global Reverse Shoulder Anthroplasty Market Overview: The rising prevalence of shoulder injuries due to sports injuries or road accidents is the major factor fuelling the global market for Reverse Shoulder Anthroplasty. The rising geriatric population and Minimal complications related to procedures also enhance the growth of the reverse shoulder systems market over the forecast period. Rising healthcare infrastructure and surgical centers are also anticipated to propel the global market.
Global Reverse Shoulder Anthroplasty Market
Report 2020-2027 (Forecast Period) includes an analysis of market growth factors, future analysis, country-level, and regional-level analysis, market distribution, and competitive landscape analysis of major key competitors. Within the analysis report, each phase of the world global market is completely studied. The regional study of the global market will help you in gaining an understanding of the developments of the various geographic markets in recent years and moving ahead. The analysis also includes a wide-ranging synopsis of the key factors of the global market, like market influence and market result factors, drivers, threats, constraints, trends, restraints, and prospects. alternative methods of analysis, like qualitative and quantitative, are also used within the analysis study. Maximize Market Research team analysis provides a unique and in-depth report that helps you to perform detailed research on the global Global Reverse Shoulder Anthroplasty market and make decisions on the future growth factors of the market. The market report provides an overview of the development of the Global Reverse Shoulder Anthroplasty market throughout the forecasted period. Request for free sample:
https://www.maximizemarketresearch.com/request-sample/94590
The Global Reverse Shoulder Anthroplasty market report thoroughly covers insights of key competitors in terms of market, applications, and geographies that will help you in recognizing the competition both domestically as well as globally. The research mentions available micro-market investment options for investors and a full synopsis of the competitive landscape and significant products offered by industries.
The report also includes statistical data that consists of tables and charts which will further help you in business representation. Maximize Market Research also studies the current as well as new trends with the estimates of the market size throughout the forecasted period. Many competitors are also identified in various regions. The report provides PESTEL and Portal analysis too, which helps the clients to calculate every factor of the market.
Global Reverse Shoulder Anthroplasty Market Segmentation: The region is expected to continue the dominance throughout the forecast period owing to the rising incidences of shoulder transplant surgeries in the region. A high number of surgeries results due to the prevalence of patients suffering from arthritis. According to Agency for Healthcare Research and Quality, about 53,000 people in the United States have shoulder replacement Surgery every year. On 4 November 2019 Wright Medical Group Inc. has an acquisition with Stryker Company. With this acquisition, they are providing significant opportunities to advance innovation and improves outcomes, and reach more patients.
Global Reverse Shoulder Anthroplasty Market Key Players:
• DePuy Synthes
• Wright Medical Technology
• Zimmer-Biomet
• Exactech
• Anthrex
• FH Orthopedics, Inc.
• Integra LifeSciences
• Evolutis
• Stryker Corporation
• mplantcast
• Lima Corporate
• Biotechni
• Cayenne Medical
• Johnson & Johnson
If You Have Any Questions About This Report? Please Contact Us On the link mentioned below: https://www.maximizemarketresearch.com/market-report/global-reverse-shoulder-anthroplasty-market/94590/
Global Reverse Shoulder Anthroplasty Market Regional Analysis:
Based on the regions the market is studied across
Asia-Pacific (Vietnam, Malaysia, Korea, China, Philippines, Thailand, Indonesia, and India, Japan, Australia, ). Africa and the Middle East (Egypt and GCC Countries.). North America (Canada, the United States, and Mexico.). South America (Brazil etc). Europe (France, Italy, Germany, Russia, UK, Turkey, etc.).
IMPACT Of COVID-19 On The Global Reverse Shoulder Anthroplasty Market:
COVID-19 has impacted the world with its fast-spreading effects all over the world. It has impacted every industry and business except for the medical and health care industry which is working 24/7 to stop the spread of the COVID-19 virus, they are working hard to save the lives of people affected by this virus. As mentioned many industries are suffering in this COVID-19 times, our market is also one of them. Our team here at Maximize Market Research has worked hard to provide solutions to these issues that will help your business.
About Us:
Maximize Market Research provides B2B and B2C research on more than 12,000 high growth emerging opportunities technologies as well as threats to the companies across the Healthcare, Pharmaceuticals, Electronics Communications, Internet of Things, Food and Beverages, Aerospace and Defense, and other manufacturing sectors.
Contact Us:
MAXIMIZE MARKET RESEARCH PVT. LTD.
3rd Floor, Navale IT Park Phase 2,
Pune Bengaluru Highway,
Narhe, Pune, Maharashtra 411041, India.
Email: [email protected]
Phone No.: +91 20 6630 3320
Website: www.maximizemarketresearch.com
Get More Report Details:
http://www.marketwatch.com/story/global-natural-gas-generator-market-industry-outlook-size-growth-factors-latest-updates-and-forecast-to-2027-2022-01-18
http://www.marketwatch.com/story/global-cat-litter-product-market-business-strategies-trends-analysis-trends-revenue-and-forecast-to-2027-2022-01-18
0 notes
Text
Plastic Surgery in Ayurveda-Juniper Publishers
Journal of Orthopedic & Orthoplastic Surgery
Research Article
Plastic Surgery in Ayurveda
*Dnyaneshwar kantaram Jadhav
Department of Ayurved Medicine, Director of Nakshatra Ayurved clinic & Research center, India
Submission: March 31, 2017; Published: April 20, 2017
*Corresponding author: Dnyaneshwar kantaram Jadhav, Department of Ayurved Medicine, Director of Nakshatra Ayurved clinic & Research center, Mumbai, India, Email: [email protected]
How to cite this article: Dnyaneshwar k J. Plastic Surgery in Ayurveda. JOJ Orthoped Ortho Surg. 2017; 1(1): 555552. DOI: 10.19080/JOJOOS.2017.01.555552
Go to
Abstract
From ancient Indian surgery, it has been observed that various operations successfully performed in those days also. In ancient period Acharya were doing surgery in Ayurveda. Sushrut was the first and famous surgeon of ancient science. There are so many examples and descriptions of surgery available in Ayurvedic Samhita. Sushrut has described plastic surgery like Nasa-sandhan (Rhinoplasty),> Karna-sandhan (Auroplasty] and Oshta-sandhan (lipoplasty]. Contribution of ancient Indian surgery in the field of plastic operation cannot be over-estimated.
It’s true that in old days one of Royal punishment was to cut way ear-lobe, nose etc. Indian surgeon correcting such deformity by shifting the skin flap to reform the nose and ear. They had plenty of opportunity to do Rhinoplasty which was first to be done in this country and itself made Indian surgery unique. They also appreciated the importance of proper wound healing for successful plastic surgery operation. It is common man’s thinking that there is no surgical treatment for disease in the science of Ayurved. After the turn over the pages of sushrut Samhita, one will understand that sushrut has laid done the basic concept of the present surgery. The present article is an attempt to highlighting on reference of ancient plastic surgery in Ayurveda.
Keywords: Plastic surgery, Sandhan Karma, Ayurveda, Sushrut.
Go to
Introduction
Ayurved science of life which is divided into 8 branches. Shalya (surgery) is one of the branches of Ashtanag Ayurved [1]. In ancient time Ayurveda was at top point of mountain but in between there was long period of slavery and Indian become depend country on British government. This is period of decline period of Ayurved and now common man’s thinking that there is no surgical treatment for disease in the science of ayuvred. It takes a beet troubles to turn over the pages of sushrut Samhita, one will find that sushrut has laid done the basic concept of the present surgery. Sushruta is considering as father of modern surgery, because of his logical approach prudent and Clare view and marvellous presentation which is time tested. From ancient Indian surgery, it has been observed that various operations successfully performed in those days also. The various surgical procedures were divided in chedya, bhedya and vedhya [2]. Chedankarma was performed in those disease were suppuration is absent, swelling is herd and immovable or in those diseases where gangrene develops. The same procedure is still being adopted in modern science. Hand is best instrument for surgery [3].
Go to
Materials and Methods
For the present review detailed literary study is performed. The Detail content of and references are analysed from available text. Principal texts referred are Sushrutasamhita and some Vedas. Also relevant references are taken from other Research articles available from internet.
Meaning of Plastic Surgery
Plastic surgery is a surgical speciality involving the restoration, reconstruction, or alternation of human body. It includes cosmetic or aesthetical surgery, hand surgery, microsurgery and treatment of burns [4].
History of Plastic Surgery
The oldest surgical references found in Ancient Egyptian medical text [5]. This Reconstructive surgery technique was being carried out in India. Sushruta was a physician that made important contributions to the field of plastic and cataract surgery in 6th century BC. The medical works of both Sushruta and Charak originally in Sanskrit were translated into the Arabic language during the Abbasid Caliphate in 750 AD [6]. The Arabic translations made their way into Europe via intermediaries. After that surgical technique of sushruta is followed in Italy.
British physicians travelled to India to see rhinoplasties being performed by native methods. They Reported on Indian rhinoplasty performed by a Kumharvaidya which was published in the Gentleman’s Magazine by 1794 [7]. Joseph Constantine Carpue spent 20 years in India studying local plastic surgery methods. Carpue performed the first major surgery in the Western world by 1815 [8]. Instruments described in the Sushruta Samhita were further modified in the Western world. The Roman scholar Aulus Cornelius Celsus recorded surgical techniques, including plastic surgery, in the first century AD. The Romans also performed plastic cosmetic surgery. They were able to perform simple techniques, such as repairing damaged ears, from around the 1st century BC.
References of Plastic Surgery in Vedas[
9
]
Description of Sandhan karma found in ancient times. During Vedik period science of Sandhan karma is very well developed. Reference of Magical operative surgery of Ashwinikumaras mentioned in vedas.
In anger Lord Shiva cuts the head of Ganesha, later on which is replaced with head of elephant. After that event shree Ganesha is known as "Gajanana" This is best example of transplantation which is well listen since childhood from our mothers and grandmother in stories.
Bispala is wife of king Khela. She lost her leg in war. Ashwinikumaras was transplanted her leg with an iron leg [10]. The lost part of body of Rishi Atriwas was re-joined by Ashwinikumaras. The body of Acharya Shyaba was cut into three parts. Ashwinikumarsimmediately re-joined all parts and give him life [11]. Beside the Rigved, Padampuran also have written examples of reconstructive plastic surgery [12]. Bhairav cut the head of Brahma and Dadhichi. Ashwinikumaras re-joined their head. They also transplanted the head of Yahnya. Dadhyancha was the master of Madhu Vidya. Ashwinikumaras showed them interest in learning of Madhu Vidya. So they cut head of Dadyyancha and kept separate. Then they transplant the head of horse to the body of Dadhyancha and learnt Madhu Vidyafrom them. After learning Madhu Vidya, they transplanted his own head [13]. Dakshya cut head and trunk of Chyavan. Ashwinikumarasperformed the first plastic operation to join them [14].
According to Upanishad, Ashwinikumaras also operated and repaired the excised head of Yagyana by Rudra. Ashwinikumaras were doing both homo and hetero transplantations at that time.
Go to
Plastic Surgery in Ayurved
Sushrut has described plastic surgery. In plastic surgery particular Nasa-sandhan (Rhinoplasty), Karna-sandhan (Auroplasty) and Oshta-sandhan (lipoplasty) are mentioned in Ayurved. Contribution of ancient Indian surgery in the field of plastic operation cannot be over-estimated. It's true that in old days one of Royal punishment was to cut way ear-lobe, nose etc [15]. Indian surgeon has applied their injurious technique for correcting such deformity by shifting the skin flap to reform the nose and ear. They had plenty of opportunity to do rhinoplasty which was first to be done in any country and itself made Indian surgery unique. They also appreciated the importance of proper wound healing for successful plastic surgery operation.
Sushruta has described 15 methods of Karna-sandhan (Auroplasty) repairs of the several ear-lopes [16] (Table 1).
Sandhanarthajivitamansa (pedicled skin flap) [
17
]:
If skin flaps unavailable from ear during Auroplasty than for Sandhanprakriya (plastic surgery) than it can take from Gandapradesha(living flap connected as base of cheek).
karnasandha-vidhi (Auroplasty)
Mahrshi Sushruta described the detail procedure of karnasandha-vidhi (Auroplasty) in his sushrutasamhita [18].
Nasa-sandhanvidhi (Rhinoplasty)
Sushruta mentioned Nasa-sandhanvidhi (Rhinoplasty) for nose either lost by disease or by trauma/accident. Description of Nasa-sandhanvidhi (Rhinoplasty) is available in sushrutsamhita. The original method of Nasa-sandhan (Rhinoplasty) reveals that first of all the leaf of creeper should be collected. It should be adequate in length and breath, to cover the entire severed portion. Then a patch of living hash of the size of previously trimmed leaf should be excised with an attached pedicals. So the excised skin flap is maintained by its vascularity. Thus skin flap is than over lapped to severe portion and stitched. The insertion of kamalnaal into nostril to vacillated respiration and to maintain the suture [19].
Oshthasandhan-vidhi (lipoplasty)
Maharshisushruta mentioned sandhan-vidhi of china oshtha (lipoplasty) for khandoshta (harelip) [20]. sandhan-vidhi of china oshtha (lipoplasty) is same as Nasa-sandhanvidhi (Rhinoplasty). The only difference is that in lip surgery there is no use of stem of Erandanaala. In Sushruta it is also mentioned that, Vaidya who get skilled in these reconstructive surgery, become Rajvaidya i.e. who can treat the king. So From above review it can be said that, sushruta was the original plastic surgeon not only in India but also in the world.
Go to
Conclusion
In Ayurvedic achrya Sushrut has described plastic surgery. Nasa-sandhan (Rhinoplasty), Karna-sandhan (Auroplasty) and Oshta-sandhan (lipoplasty) and many more sandhan (plastic surgery) are mentioned in Ayurved. Contribution of ancient Indian surgery in the field of plastic operation cannot be over-estimated. All of this it made Indian surgery unique.
To read more articles in Journal of Orthopedic & Orthoplastic Surgery
Click on https://juniperpublishers.com/jojoos/index.php
To Know More about Juniper Publishers click on: https://juniperpublishers.com/
0 notes
Text
2-Octyl Cyanoacrylate Adhesives Market :Technological Breakthroughs, Value Chain And Stakeholder Analysis By 2020
2-Octyl cyanoacrylate adhesives are super strong adhesives which are categorized as wound glue or tissue glue. Cyanoacrylate is the generic name of a family of super strong glues that are capable of joining any type of surfaces instantly. Cyanoacrylate based adhesives are extensively used in many applications including industrial, medical and domestic applications. 2-Octyl cyanoacrylate however is mainly used in medical, veterinary and first aid applications. Cyanoacrylates have a property by virtue of which they solidify rapidly on contact with weak bases such as water and blood and are used for endoscopic applications.
The market for 2-Octyl cyanoacrylate adhesives is driven by its application in surgical procedures and treatment. The compound has been approved by the Food and Drug Administration (FDA) for application to close wounds and incised skin. It also acts as a barrier to certain bacterial microbes such as staphylococci, Escherichia coli and pseudomonads among some others. Application of the adhesive post surgery is cost effective as compared to traditional method of stitching the wound.
Read Report Overview @
https://www.transparencymarketresearch.com/2-octyl-cyanoacrylate-adhesives-market.html
Although the cost of 2-Octyl cyanoacrylate adhesives is high, the overall expense of equipment and labor cost involved with sutures surpasses it. Application of glue to close incised skin also does not require the use of anesthetics and is relatively painless, which renders it an attractive alternative to patients and physicians alike. The cosmetic appearance of the closed wound is comparable to that achieved by sutures, and proper implementation of the glue can help in preventing scars.
Some medical applications where it is used are total joint anthroplasty wounds, implantation of pacemakers, patch fixation in inguinal herniorraphy and repair of fractured tooth among some others. Although sutures are still favored by many physicians, the acceptability and application of 2-Octyl cyanoacrylate adhesives have picked up over the past few years since its approval and the market is expected to expand with time and application in more medical applications.
Request Report Brochure @
https://www.transparencymarketresearch.com/sample/sample.php?flag=B&rep_id=3563
However there are certain restrictions to the use of 2-Octyl cyanoacrylate adhesives to close wounds. The skin bonding adhesive is not advisable for use in certain cases such as deep wounds with broken skin edges, infected or crushed wounds, wounds developed from animal bites, skin in high tension areas (Knees, elbows etc.), skin in high friction areas (buttocks, perineum) and wounds that have been open for more than 12 hours. Moreover the success percentage of tissue glues in comparison to sutures in slightly poor. According to estimates about 4% of the wounds closed by means of 2-Octyl cyanoacrylate adhesives reopen, as compared to 1-2% in sutures.
North America is the largest market for 2-Octyl cyanoacrylate adhesives and account for a lion’s share of the global market. Europe is the second largest market for the compound followed by Asia Pacific. Asia Pacific region however has the maximum potential owing to its huge population base and increasingly efficient healthcare solutions. Other forms of cyanoacrylate which are used in industries and domestic applications have the highest market share in Asia and its popularity in medical applications is a matter of time.
Request Discount @
https://www.transparencymarketresearch.com/sample/sample.php?flag=D&rep_id=3563
Some of the major players in the 2-octyl cyanoacrylate adhesives market along with the products are listed hereafter: Dermabond marketed by Johnson & Johnson, Ethicon, Inc., SurgiSeal and FloraSeal marketed by Adhezion Biomedical, Nexabond marketed by Abott, Derma+flex QS marketed by Chemnence and Octyseal by Medline among many others.
0 notes