#Empyema Surgical Treatment
Text
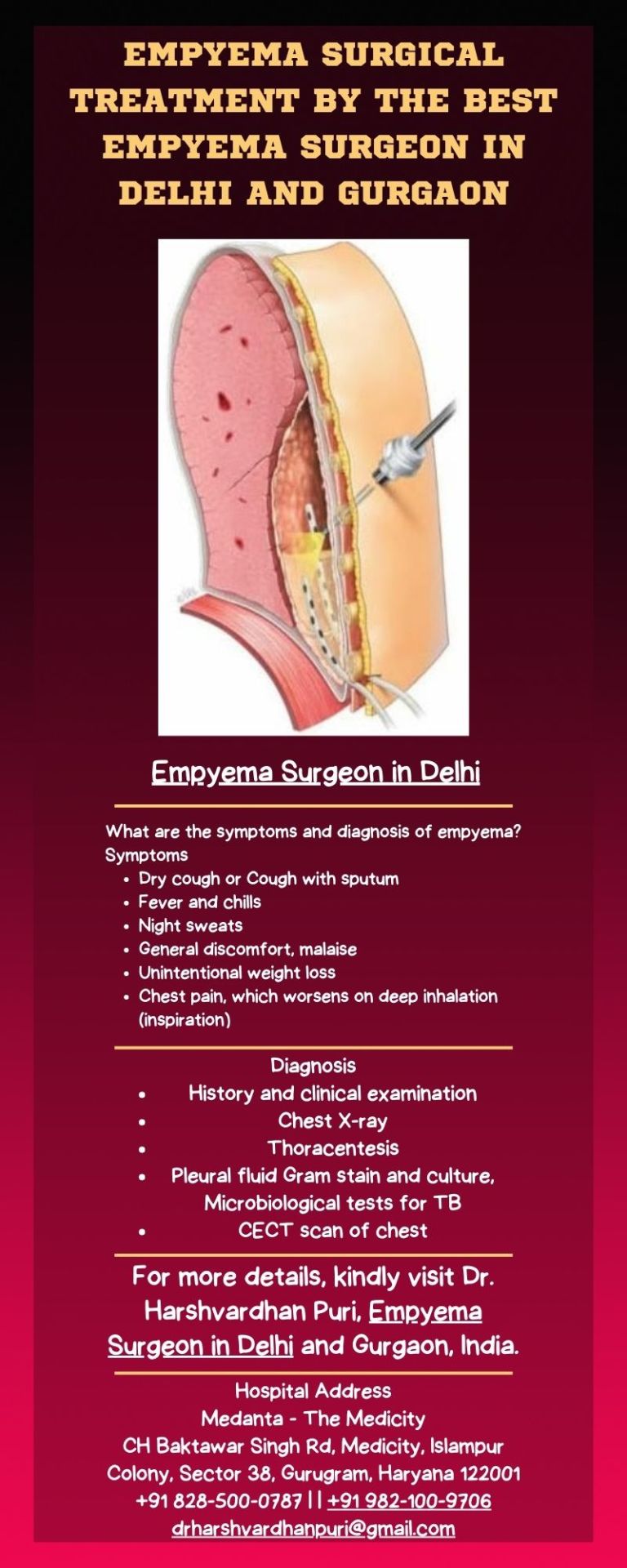
Empyema Surgeon in Delhi
Empyema is a collection of pus in between the lung and chest wall formed by two pleural layers, visceral and pariteal.
It is caused by some infective process of the lung which leads to an accumulation of pus in the pleural space. The commonest cause of empyema in our country is Tuberculosis. It however can also be a complication of pneumonias, trauma with collection of blood inside the chest that gets infected. Repeated aspiration without asepsis of pleural fluids in cases of recurrent pleural effusion can also lead to infection of the fluid leading to empyema. Also empyema can happen after lung or chest surgery also.
Empyema is a collection of pus in between the lung and chest wall formed by two pleural layers, visceral and pariteal. Consult Dr. Harsh Vardhan Puri, the best empyema surgeon in Delhi and Gurgaon, for empyema surgical treatment.
#Empyema#Empyema Surgical Treatment#Empyema Surgeon in Delhi#Empyema Surgeon in Gurgaon#Empyema Surgical Treatment in Delhi
0 notes
Text
Understanding Pleural Effusion and Its Treatment in Delhi
Pleural Effusion, commonly referred to as "water on the lungs," is a condition where excess fluid accumulates between the layers of the pleura outside the lungs. This condition can result from various underlying causes, including infections, heart failure, liver cirrhosis, kidney disease, or malignancies. In Delhi, where access to advanced healthcare facilities is readily available, effective treatment options for pleural effusion are accessible to patients.
Symptoms and Diagnosis
Patients with pleural effusion may experience symptoms such as shortness of breath, chest pain, dry cough, and a feeling of heaviness in the chest. In some cases, Pleural Effusion treatment in Delhi might be asymptomatic and detected incidentally during a routine chest X-ray. Diagnosis typically involves a combination of imaging studies such as chest X-rays, ultrasound, or CT scans, and a procedure called thoracentesis. Thoracentesis involves the removal of a small amount of fluid from the pleural space, which is then analyzed to determine the underlying cause.

Treatment Approaches
The treatment of Pleural Effusion treatment in Delhi is tailored according to the cause, severity of symptoms, and the patient's overall health. Here are some common treatment approaches:
Thoracentesis: This procedure is both diagnostic and therapeutic. It involves the insertion of a needle into the pleural space to remove fluid. In cases where a large amount of fluid is causing significant symptoms, thoracentesis can provide immediate relief by reducing the pressure on the lungs.
Pleurodesis: For patients with recurrent pleural effusions, pleurodesis may be recommended. This procedure involves the introduction of a chemical or drug into the pleural space to create inflammation and cause the pleura to stick together, preventing further fluid accumulation.
Chest Tube Insertion: In cases of large effusions, especially if the fluid is infected (empyema) or associated with malignancy, a chest tube may be inserted to continuously drain the fluid. This helps in preventing the reaccumulation of fluid and allows the underlying lung to expand.
Medication: Depending on the underlying cause, medications such as antibiotics for infections, diuretics for heart failure, or chemotherapy for malignancies may be prescribed to treat the pleural effusion.
Healthcare Facilities in Delhi
Delhi is home to numerous top-tier hospitals and clinics that offer specialized care for pleural effusion. Leading healthcare institutions such as AIIMS, Apollo Hospitals, Fortis Healthcare, and Max Super Specialty Hospitals provide comprehensive diagnostic and treatment services, including advanced imaging, thoracentesis, and surgical interventions.
Conclusion
Prompt diagnosis and treatment of Pleural Effusion treatment in Delhi are crucial to prevent complications and ensure the best possible outcomes. With access to world-class healthcare facilities and experienced specialists, patients in Delhi can expect high-quality care tailored to their specific needs. If you or a loved one is experiencing symptoms of pleural effusion, it is essential to seek medical attention promptly to receive appropriate treatment and avoid potential complications.
#Pleural Effusion treatment in Delhi#lung transplant in Delhi#lung transplant in Gurugram#Pleural Effusion treatment#Pleural Effusion treatment in Gurugram
0 notes
Text
Empyema Pleural _ Sound therapy session _ Sounds of nature

Empyema pleural is a serious condition that occurs when pus accumulates in the pleural cavity, which is the space between the lungs and the chest wall. Traditional treatments for empyema pleural typically involve antibiotics and surgical drainage, but some individuals may also benefit from alternative therapies, such as Rife-based bioresonance therapy. Rife-based bioresonance therapy is a non-invasive and drug-free treatment method that uses electromagnetic frequencies to stimulate the body's natural healing processes. The therapy is based on the principles of the Rife machine, which was developed in the early 20th century by Dr. Royal Rife. The machine emits specific frequencies that are believed to target and destroy harmful pathogens in the body. Rife-based bioresonance therapy uses similar frequencies that are tailored to the individual's needs to promote healing and stimulate tissue repair. Rife-based bioresonance therapy for empyema pleural works by targeting the root cause of the condition. The therapy uses specific frequencies that are believed to stimulate the body's natural healing mechanisms, reduce inflammation, and promote tissue repair. These frequencies are thought to be absorbed by the body's tissues and cells, which can then help to reduce inflammation, promote healing, and eliminate harmful pathogens. Benefits of Rife-based Bioresonance Therapy for Empyema Pleural One of the main benefits of Rife-based bioresonance therapy is that it is a non-invasive and drug-free treatment method. This means that it can be used in conjunction with traditional medical treatments, or as a standalone therapy for those who prefer alternative treatments. Another benefit of Rife-based bioresonance therapy is that it is personalized to the individual's needs. The specific frequencies used in the therapy are tailored to the individual's condition, which can help to optimize the treatment's effectiveness. Finally, Rife-based bioresonance therapy is believed to be a safe and gentle treatment method, with few reported side effects. This makes it an attractive option for those who are seeking alternative therapies for their medical conditions. Conclusion Rife-based bioresonance therapy is a promising alternative therapy for the treatment of empyema pleural. It is a non-invasive and drug-free treatment method that uses electromagnetic frequencies to stimulate the body's natural healing processes.
TO ACHIEVE A POSITIVE RESULT, DAILY LISTENING TO VIDEOS IS REQUIRED.
https://rumble.com/v2dciag-empyema-pleural-sound-therapy-session-sounds-of-nature.html?mref=17947j&mc=9fatg
0 notes
Text
Thoracoscopic Surgery In Children: What Is It?
Thoracoscopic Surgery In Children: What Is It?
Thoracosopic surgery is a type of minimally invasive surgery that is appropriate for children who require surgery for a variety of chest diseases. Today, a variety of straightforward and complicated surgical chest problems are regularly treated with thoracoscopy. Small incisions allow for minimally invasive surgery, which prevents damage to the muscles and nerves of the chest wall. On the other hand, huge incisions like those utilized in open surgery are uncomfortable and may eventually result in chest wall deformities.
During a thoracoscopic surgery, to see the structures inside the chest, the surgeon uses a thorascope (a small tube with an eyepiece that the surgeon sees through during surgery) and/or an endoscope (a small video camera).
The surgeon can now do procedures that would often require big thoracotomy incisions by using an endoscope to view through them. In order to undergo surgery, patients must be put under general anaesthesia in an operating room.
What are the advantages of thoracoscopic surgery in children?
On the contrary, large incisions as used in open surgery are painful and can cause chest wall deformity in the long run. Patients who have had minimally invasive surgery report the following outcomes when compared to those of regular surgery:
Reduced postoperative discomfort
Reduction in hospital stay
Faster healing and return to work
Less bleeding and a lower chance of infection are two other advantages.
How does thoracoscopic surgery in children work?
Thoracoscopic surgery is carried out by paediatric laparoscopic surgeon. During this procedure, a small incision is made to allow the surgical team to introduce a trocar into an intercostal space. Pumping carbon dioxide into the thoracic cavity creates an interior area for the surgeon to work by separating the body wall from the organs. The surgeon next inserts a thorascope and/or endoscope to view the structures of the chest. The use of tiny instruments is made possible by a number of additional incisions or tiny ports.
For whom is minimally invasive surgery appropriate?
A minimally invasive procedure can be used to perform almost all conventional thoracic procedures.
If thoracic surgery needs to be done, a minimally invasive surgical approach is the first that is considered. However, some procedures are still best carried out using the conventional “open” method. Your surgeon will thoroughly examine you to decide the safest surgical procedure to be used to treat your ailment.
Various thoracoscopic surgery procedures:
Dr. Prashant Jain, one of the finest paediatric surgeons in Delhi, has had great success in removing chest malignancies using minimally invasive surgery. He also performs a few other procedures listed below:
Mediastinal tumor removal
Mediastinal cysts removal
Lung malformations
Empyema
Lung biopsy
Spontaneous Pneumothorax
How can I get a thoracoscopic surgery evaluation?
Your physical exam and treatment choices will be discussed when you visit the laparoscopic surgeon. He will go over the advantages and possible drawbacks of the surgery that is suggested for you.
Preoperative exams typically include:
Blood test
Pulmonary function test
MRI
Electrocardiogram
Depending on the kind of treatment being performed, your surgeon will decide if any extra preoperative testing is required. A cardiologist’s visit will be arranged if a cardiac (heart) assessment is required.
You will consult with an anesthesiologist as part of your preoperative evaluation. During this time, you will talk about postoperative pain management and anesthesia.
In Delhi, Dr. Prashant Jain is a well-known paediatric laparoscopic surgeon. Call (+91) 8766 350 320 to schedule an appointment and get all your questions answered from the expert.
Tag = Thoracoscopic Surgery In Children in Delhi, Pediatric laparoscopic surgeon in Delhi, Best pediatric surgeon in delhi
#Thoracoscopic Surgery In Children in Delhi#Best pediatric surgeon in delhi#Pediatric laparoscopic surgeon in Delhi#pedsurgerydelhi
0 notes
Text

Complications Linked to Bile Duct Stones:
Cholangitis: Bile duct stones can induce an infection within the bile ducts, causing cholangitis. This condition is characterized by the inflammation and swelling of the bile ducts, leading to symptoms such as fever, abdominal pain, jaundice, and a general sense of illness. Untreated cholangitis can be life-threatening, potentially resulting in sepsis and liver abscesses.
Pancreatitis: Bile duct stones can obstruct the pancreatic duct, leading to inflammation of the pancreas, a condition known as pancreatitis. Pancreatitis is marked by severe abdominal pain, nausea, vomiting, and elevated levels of pancreatic enzymes in the bloodstream. Severe cases of pancreatitis can result in organ failure and necessitate intensive medical care.
Biliary Stricture: A bile duct stone can cause scarring and narrowing of the bile ducts, giving rise to biliary stricture. This narrowing can obstruct the flow of bile, resulting in jaundice, recurring infections, and liver damage. Biliary strictures often require additional interventions, such as endoscopic or surgical procedures, to restore proper bile flow.
Gallbladder Inflammation and Infection: Bile duct stones can lead to inflammation of the gallbladder, referred to as cholecystitis, which causes severe abdominal pain, fever, and tenderness in the upper right abdomen. In some instances, the gallbladder may become infected, resulting in a condition called empyema. Gallbladder empyema necessitates urgent medical attention and often requires surgical removal of the gallbladder.
It is important to consult a good gastroenterologist at the earliest if you have any gastric problems. Dr. Amit Maydeo is considered to be one of the best gastroenterologists in Mumbai, who can help in the early diagnosis and treatment of bike duct stones. He currently provides consultation at HN Reliance Hospital, Mumbai, which is considered to be one of the best hospitals in the country.
#gastric problems#liver disease#liver transplant#gallbladder cancer#gallbladder surgery#gallbladder removal#bile duct stones#gallstones#gastroenterologist
0 notes
Text
Best Pulmonologist in south Delhi
How Thoracoscopy procedure is performed and any risk involved?
According to Thoracoscopy Treatment Doctors in Delhi, a thoracoscopy is a minimally invasive surgical procedure that allows the doctor to access and visualize the inside of the chest cavity using a thoracoscope, a thin, lighted tube with a camera on the end. The procedure is performed through small incisions in the chest wall, rather than a large incision as in traditional open thoracic surgery. Thoracoscopy is used to diagnose and treat conditions such as lung tumors, pleural effusions, or empyema.
A thoracoscopy is a medical procedure that uses a thin, lighted tube called a thoracoscope to examine the inside of the chest. It is typically used to diagnose and treat lung diseases, such as pleural effusions, empyema, and lung cancer. Thoracoscopy can also be used to obtain a biopsy or remove fluid from the pleural cavity.
Thoracoscopy is performed by a thoracic surgeon, who is a specialist in surgical procedures related to the chest. They are trained to perform the procedure, which is usually done under general anesthesia.
In Delhi, there are several thoracoscopy doctors and treatment centers that provide specialized care to patients. Dr. Neetu is one of the thoracoscopy doctors in Delhi who specializes in thoracoscopy treatment. She is highly experienced in diagnosing and treating a range of lung diseases and conditions using thoracoscopy.
As per Best Pulmonologist in south Delhi, Thoracoscopy is a minimally invasive surgical procedure with relatively low risks compared to open thoracic surgery. However, as with any surgical procedure, there are some potential risks and complications, including:
1. Pain or discomfort in the chest area
2. Bleeding
3. Infection
4. Injury to the organs or blood vessels in the chest
5. Pneumothorax (collapsed lung)
6. Allergic reaction to anesthesia
It is important to discuss the specific risks and benefits of thoracoscopy with Thoracoscopy Treatment Doctors in Delhi and to follow their instructions for preparing for and recovering from the procedure to minimize the risk of complications.
A thoracoscopy is a minimally invasive surgical procedure that involves the insertion of a thin, lighted tube called a thoracoscope through a small incision in the chest to examine the inside of the chest cavity. During the procedure, the doctor will use the thoracoscope to view the lungs, pleura, diaphragm, and other structures in the chest cavity.
Here is what to expect during a thoracoscopy:
Preparation: Before the procedure, the doctor will explain the procedure, the potential risks and benefits, and what to expect after the procedure. You may be asked to stop eating or drinking for several hours before the procedure.
Anesthesia: A thoracoscopy is usually performed under general anesthesia, which means you will be asleep during the procedure.
Incision: The doctor will make a small incision in the chest through which the thoracoscope will be inserted.
Examining the chest cavity: The doctor will use the thoracoscope to view the inside of the chest cavity, take biopsies, and treat any conditions that are found.
Duration of the procedure: A thoracoscopy typically takes between 30 minutes to an hour.
Recovery: After the procedure, you will be taken to a recovery room to wake up from the anesthesia. You may experience some discomfort and chest pain, but these symptoms usually resolve within a few days.
Follow-up: Your doctor will schedule a follow-up appointment to discuss the results of the thoracoscopy and any additional treatment that may be necessary.
It is important to discuss the potential risks and benefits of the procedure with your doctor and ask any questions you may have before the procedure
So, if you are looking for the Thoracoscopy Treatment Doctors in Delhi, look no further than
Dr. Neetu . With her expertise and commitment to providing the best possible care, you can trust that your health is in good hands. Book an appointment with Dr. Neetu Thoracoscopy Doctors in Delhi today and take the first step towards a healthier future. Your health matters, and with Dr. Neetu on your side, you can be sure that you are in the best of hands.
0 notes
Link
If you are looking for best Empyema Surgical Treatment in Delhi then Contact to DR. Pramoj Jindal. For More Details Visit: http://www.drpramojjindal.com/empyema
0 notes
Link
Dr. Belal Bin Asaf is a Thoracic (Chest) Surgeon who specialises in the treatment of surgical diseases of the chest involving the lungs, mediastinum, Trachea (Windpipe), esophagus (food pipe) and diaphragm. He is recognised nation-wide as an expert and a leader in the field of minimally invasive thoracic surgery like Video assisted Surgery (VATS / Key-Hole surgery) and robotic thoracic surgery. Dr. Belal Bin Asaf | Thoracic Surgeon in Delhi
#Best Lung Surgeon Specialist in Delhi#best empyema treatment in delhi#Dr. Belal Bin Asaf#Lung Surgeon Specialist in Delhi
1 note
·
View note
Text
An empyema is a collection of pus within a naturally existing anatomical cavity, such as the lung pleura. It must be differentiated from an abscess, which is a collection of pus in a newly formed cavity. Usually an empyema starts with pneumonia, followed by a parapneumonic effusion. This effusion starts out sterile, then becomes infected. As the infection progresses, the thickness of the fluid increases, going from a broth-type consistency to concrete. When the fluid is still free flowing, it can be treated with a thoracentesis or a chest tube. When it thickens, it can usually be treated with thoracoscopy (Video Assisted Thoracic Surgery; VATS). Once the fluid becomes thick and loculated, a formal thoracic surgical procedure called a thoracotomy with decortication is required. This involves opening the chest, taking out the fluid, peeling the thick rind of infectious material off the lung, and then inserting chest tubes while the infection clears (usually with the help of antibiotics).
Chest tubes in the setting of empyema have a tendency to become clogged. Chest tube clogging in the setting of an empyema can lead to re-accumulation of pus and infected material, a worsening clinical picture, organ failure, and even death. Thus, managing chest tube clogging is particularly important after the treatment of an empyema.
4 notes
·
View notes
Text
What Causes Hiccups? A Neurologist Ruham Nasany Explains
Hiccups, also called singultus, is an involuntary contractions of your diaphragm. It happens suddenly by affecting a muscle involved in inhalation and exhalation.
Hiccups, also called singultus, is an involuntary contractions of your diaphragm. It happens suddenly by affecting a muscle involved in inhalation and exhalation. The muscle is between your abdomen and chest.
According to Dr. Ruham Nasany, contractions cause abrupt air inhalations with a hic sound due to the rapid closure of your vocal cords. Bear in mind that hiccups have different lengths depending on their types or classifications.
For instance, transient hiccups are the most common and last a few seconds or minutes. On the other hand, persistent hiccups last for more than 48 hours. Some people experience hiccup episodes for more than 30 days.
Although these rarely occur, consulting your health provider is crucial for immediate treatment. These are known as intractable or chronic hiccups. A growing body of research evidence shows that various factors can trigger hiccups. Today’s article will highlight the primary causes of hiccups. Read on!
Damage to the CNS
Damage or injury to your central nervous system is a common cause of hiccups. Your CNS constitutes the brain and spinal cord, and damage to these critical organs can trigger hiccups, leading to uncontrollable episodes.
Dr. Ruham Nasany says stroke, tumors, multiple sclerosis, brain injury, head trauma, encephalitis, meningitis, brain inflammation, and fluid accumulation are the most significant causes of damage to the CNS, leading to acute or chronic hiccups, depending on the intensity or severity of the problem.
Gastrointestinal and Thoracic Disorders
Research studies show that gastritis, gastric distention, pancreatic cancer, abdominal abscesses, inflammatory bowel disease, gallbladder disease, bowel obstruction, aerophagia, etc., are gastrointestinal disorders that can cause acute or chronic hiccups. Consulting your health provider is essential for proper diagnosis.
In addition to gastrointestinal disorders, thoracic-related problems can also hiccup. These conditions include inflamed lymph nodes, neoplasm, empyema, pneumonia, asthma, bronchitis, aortic aneurysm, chest trauma, mediastinal tumors, and pulmonary embolism.
Toxic-Metabolic
Heavy alcohol consumption, diabetes mellitus, hypocapnia, hypocalcemia, herpes zoster, influenza, malaria, and tuberculosis can also cause hiccups. Studies show that type-2 diabetes is a common cause of hiccups. However, these are benign and self-limiting hiccups, but some people with this endocrinal condition may experience hiccup episodes for over 48 hours.
Nerve Injuries
According to Ruham Nasany MD, injury or irritation of your phrenic nerve is the most significant cause of hiccups. The nerves control your diaphragm movements. Tumors or cysts in the esophagus, gastroesophageal reflux disease, sore throat, chest irritation, and eardrum irritation are common causes of nerve irritation.
In addition, arterial narrowing, tumors, and hormonal imbalances may also affect your nerve function and cause hiccups. The phrenic nerve plays a critical role in the inhalation and exhalation of air. It contracts and expands your diaphragm, allowing your lungs to inhale oxygen and exhale carbon dioxide.
Damage to this nerve can paralyze your diaphragm. Common signs include shortness of breath and persistent hiccups. You may also experience difficulty sleeping. Besides, an irritated phrenic nerve can also cause hiccups lasting more than 30 days.
Some studies show that tumors, cysts, and surgical procedures that involve incisions can irritate your phrenic nerve, leading to persistent hiccups. Remember, persistent hiccups are challenging to handle and cause significant discomfort, preventing you from talking, sleeping, and eating correctly.
I recommend discussing your symptoms with a qualified neurologist or health provider to overcome the issue. Health professionals usually recommend chlorpromazine to control hiccups or reduce their occurrences. However, if the problem persists for a prolonged period, your provider may recommend surgery.
Final Words
Hiccups can cause discomfort and affect your ability to talk, eat, and sleep. The primary cause of hiccups is damage to the muscle in your chest cavity or nerve irritation caused by various factors.
There are various ways to overcome hiccups naturally. These include maintaining a healthy weight via exercise and a nutrient-rich diet, stress management, meditation, yoga, proper sleep, and reducing the risk of high blood pressure, cholesterol, and diabetes.
Smoking is another cause of hiccups because nicotine slows blood circulation to your nerves. So, make sure you avoid smoking and reduce heavy alcohol consumption to reduce the risk of chronic or persistent hiccups.
Consult your health provider if your symptoms persist for more than 30 days. The purpose is to diagnose the cause and address the issue via advanced treatment options. Until Next Time!
Resource: https://www.theodysseyonline.com/what-causes-hiccups-a-neurologist-ruham-nasany-explains
0 notes
Text
Dr. Prashant Jain Provides The Treatment For Thoracoscopic Surgery In Children
Thoracoscopic Surgery For Children
Thoracosopic surgery, is a Minimally Invasive Surgery which uses multiple small incisions, and is suitable for children who need to undergo surgery for various chest conditions. Thoracoscopy is now very frequently used for various simple and complex surgical chest conditions. Since a Minimally Invasive Surgery can be done with small incisions, this avoids injury to chest wall muscles and nerves. On the contrary, large incisions as used in open surgery are painful and can cause chest wall deformity in long run. Minimally Invasive Surgery have shown great results, with lesser pain, reduced hospitalization, lesser complications and a better cosmetic result as compared to traditional thoracotomy. However, Thoracotomy will still be needed in some select cases. Dr. Prashant Jain, is one of the best paediatric surgeon in Delhi (India), who has achieved excellent results in the removal of chest tumors through minimally invasive surgery. Following are some other procedures that he performs:
Excision of mediastinal tumors: Thoracoscopy has been found to be very useful in excision of mediastinal tumors/ masses like neuroblastoma, thymoma, teratoma etc. The advantage of thoracoscopy is it gives excellent magnified vision which helps in complete excion without damaging adjacent vital structures.
Excision of Mediastinal cysts: Various mediastinal and lung cysts can be safely removed in newborns, infants and pediatric patients with excellent results. This include bronchogenic cyst, enteric duplication cyst, thymic cyst, hydatid cyst etc. Some of these cyst are diagnosed during antenatal period.
Lung Malformations: Thoracoscopy excision of lung malformation involves CCAM, CLE and lung sequestration.
Empyema: Empyema is an infection due to pus formation in the chest cavity or the pleural space. Children with empyema requires treatment with antibiotics, thoracostomy and thoracoscpic decprtication. For thoracoscopic decortication, three to four small incisions (3-5mm) are made to access the pleural space. Following which, the pleural space is cleansed off all debris and infected material, using a camera to see inside. Thus making the lung re-expand. Thoracoscopy addresses the symptoms and aids in a faster recovery, thereby reducing the patient’s stay in the hospital, especially when it is done in the initial stages of the illness.
Lung Biopsy: Lung Biopsy is carried out for children with chronic lung conditions, which may be difficult to diagnose, even after numerous tests. The Lung Biopsy is done using three small incisions, through which, the targeted area of the lung is biopsied. Diagnosis is achieved in almost 95% of the biopsies. It eliminates the requirement a large incision and its associated complications, while providing the same amount of tissue for analysis, as that of thoracotomy. Due to limited post-operative pain, and discomfort which does not compromise respiration, this procedure is well tolerated, even in children with advanced lung disease.
Spontaneous Pneumothorax: Pneumothorax is a life-threatening condition in which the lung collapses. Teenagers progressing through their adolescent growth spurt and children with underlying lung diseases, like apical cysts or cystic fibrosis are more prone to pneumothorax. The lungs need to be re-expanded to allow healing and removal of symptoms. Thoracoscopy is recommended for children with a recurring pneumothorax. The apical cysts (if present) are removed with an endoscopic stapling device. To carry out this procedure, three small incisions of 5mm – 12mm are made. To avoid air leaks in the future, the pleural cavity lining is abraided so that the lung adheres to the chest wall.
Tags - Thoracoscopic Surgery In Children, best pediatric surgeon in india, best pediatric surgeon in delhi
For more information link - www.pedsurgerydelhi.com
#best pediatric surgeon in delhi#Thoracoscopic Surgery In Children#best pediatric surgeon in india#Dr. Prashant Jain#Pedsurgerydelhi
0 notes
Text

Empyema Treatment In Delhi and Gurgaon, In India
Empyema is a collection of pus in between the lung and chest wall formed by two pleural layers, visceral and pariteal. Consult Dr. Harsh Vardhan Puri, the best empyema surgeon in Delhi and Gurgaon, for empyema surgical treatment.
#Empyema#Empyema Surgical Treatment#Empyema Surgeon in Delhi#Empyema Surgeon in Gurgaon#Empyema Surgical Treatment in Delhi
0 notes
Text
Thoracoscopic Surgery In Children, Paediatric Laparascopic Surgeon in Delhi, India - Dr. Prashant Jain
Thoracoscopic Surgery For Children
Thoracosopic surgery, is a Minimally Invasive Surgery which uses multiple small incisions, and is suitable for children who need to undergo surgery for various chest conditions. Thoracoscopy is now very frequently used for various simple and complex surgical chest conditions. Since a Minimally Invasive Surgery can be done with small incisions, this avoids injury to chest wall muscles and nerves. On the contrary, large incisions as used in open surgery are painful and can cause chest wall deformity in long run. Minimally Invasive Surgery have shown great results, with lesser pain, reduced hospitalization, lesser complications and a better cosmetic result as compared to traditional thoracotomy. However, Thoracotomy will still be needed in some select cases. Dr. Prashant Jain, is one of the best paediatric surgeon in Delhi (India), who has achieved excellent results in the removal of chest tumors through minimally invasive surgery. Following are some other procedures that he performs:
Excision of mediastinal tumors: Thoracoscopy has been found to be very useful in excision of mediastinal tumors/ masses like neuroblastoma, thymoma, teratoma etc. The advantage of thoracoscopy is it gives excellent magnified vision which helps in complete excion without damaging adjacent vital structures.
Excision of Mediastinal cysts: Various mediastinal and lung cysts can be safely removed in newborns, infants and pediatric patients with excellent results. This include bronchogenic cyst, enteric duplication cyst, thymic cyst, hydatid cyst etc. Some of these cyst are diagnosed during antenatal period.
Lung Malformations: Thoracoscopy excision of lung malformation involves CCAM, CLE and lung sequestration.
Empyema: Empyema is an infection due to pus formation in the chest cavity or the pleural space. Children with empyema requires treatment with antibiotics, thoracostomy and thoracoscpic decprtication. For thoracoscopic decortication, three to four small incisions (3-5mm) are made to access the pleural space. Following which, the pleural space is cleansed off all debris and infected material, using a camera to see inside. Thus making the lung re-expand. Thoracoscopy addresses the symptoms and aids in a faster recovery, thereby reducing the patient’s stay in the hospital, especially when it is done in the initial stages of the illness.
Lung Biopsy: Lung Biopsy is carried out for children with chronic lung conditions, which may be difficult to diagnose, even after numerous tests. The Lung Biopsy is done using three small incisions, through which, the targeted area of the lung is biopsied. Diagnosis is achieved in almost 95% of the biopsies. It eliminates the requirement a large incision and its associated complications, while providing the same amount of tissue for analysis, as that of thoracotomy. Due to limited post-operative pain, and discomfort which does not compromise respiration, this procedure is well tolerated, even in children with advanced lung disease.
Spontaneous Pneumothorax: Pneumothorax is a life-threatening condition in which the lung collapses. Teenagers progressing through their adolescent growth spurt and children with underlying lung diseases, like apical cysts or cystic fibrosis are more prone to pneumothorax. The lungs need to be re-expanded to allow healing and removal of symptoms. Thoracoscopy is recommended for children with a recurring pneumothorax. The apical cysts (if present) are removed with an endoscopic stapling device. To carry out this procedure, three small incisions of 5mm – 12mm are made. To avoid air leaks in the future, the pleural cavity lining is abraided so that the lung adheres to the chest wall.
Dr. Prashant Jain, is a renowned Paediatric Laparascopic Surgeon in Delhi, India. To book an appointment call (+91) 8766350320.
Tag = Thoracoscopic Surgery In Children, Paediatric Laparascopic Surgeon in Delhi, best pediatric surgeon in delhi
For more information = http://www.pedsurgerydelhi.com/
#Thoracoscopic Surgery In Children#Paediatric Laparascopic Surgeon in Delhi#best pediatric surgeon in delhi
0 notes
Text
WHAT CONDITIONS CAN BE TREATED WITH HYPERBARIC OXYGEN THERAPY?
Hyperbaric oxygen treatment (HBOT) entails breathing oxygen in a high-pressure chamber. It raises the amount of oxygen in the body carried by the blood to provide damaged tissues-- patients that have the HBOT sessions take a breath of around 100% oxygen while inside the chamber.
The dose of oxygen as well as recommended treatment depends on the individual's problem and also how their body reacts to the sessions. Additionally, HBOT can include dangers and also difficulties that medical professionals should inform their clients of before the treatment.
HBOT deals with several ailments ranging from infections to air bubbles in capillaries. Therapies of various clinical problems can also consist of surgical or medicinal reasons affecting an individual's body.

What Are the Hyperbaric Oxygen Treatment Signs?
Hyperbaric oxygen therapy treats many different medical conditions. The Undersea, as well as Hyperbaric Medical Society, has identified fourteen clinical disorders with successful medical trials in therapies of HBOT. Some diseases have actually been accepted by the FDA, while some are still in test.
The FDA accepts the use of HBOT treatment for some health problems such as:
Gas embolism
A gas embolism occurs when gas bubbles get in capillaries or perhaps arteries. An arterial gas embolism (AGE) usually results from submarine retreat training when someone rises after taking a breath of compressed gas at deep midst. Another condition is a venous gas embolism (VGE), which happens after pressed gas diving.
Brain abscess
Brain abscesses include analytical abscess, subdural empyema, as well as epidural empyema conditions. Relying on the medical diagnosis, the hyperbaric therapy dose is typically around 2.0 to 2.5 ambiances outright at about 60 to 90 mins per session.
Burns
Infections in burns are the leading cause of death in shed injuries. The objectives of melt treatment are to offer quick recovery, prevent scarring and pigmentation, as well as reduce financial expenses.
Carbon monoxide poisoning
Both body organ systems most likely to be injured are the cardio and also main nervous systems.
Cyanide and carbon monoxide poisoning
Cyanide and carbon monoxide gas poisoning happen in people who inhale smoke from a fire.
Injury from squashing
Injury from squashing is a trauma caused to different body parts, resulting in small or serious limb damages. The injury might entail a number of issues from the skin, muscle mass, and even the bones and also joints.
Skin grafts and flaps
Hyperbaric oxygen therapy is only essential for skin grafts or flaps impacted by direct exposure to radiation or not having enough oxygen in the tissue.
Unexpected hearing problems
An unexpected hearing problem is a hearing loss of 30 decibels that happens over three days or 3 regularities. Many clients experience sudden hearing loss, ringing in the ears, ear fullness or congestion, as well as vertigo.
Gangrene
Gangrene is an infection of the muscles. It normally exists in patients with challenging cracks that result in soft cells injuries after crashes. The favored treatment is normally HBOT therapy, surgical treatment, and anti-biotics in tandem.
Unexpected vision loss
Unexpected vision loss is a pain-free loss of vision as well as is usually permanent. It takes place in people with swelling of capillary, embolism, and also enlarging or setting of the arteries.
Necrotizing fasciitis
Necrotizing fasciitis is an infection of the soft cells caused by meat-eating germs.
Postponed radiation injury
Delayed radiation injury is one of the most examined and also reported targets of hyperbaric oxygen therapy. Nevertheless, the well-known sources of the problem are very few.
Diabetically obtained health problems
Diabetic diseases include foot abscess, retinopathy, and also nephropathy.
Decompression sickness
Decompression sickness includes gas bubbles in cells or blood. It can result in joint discomfort, skin rashes, peripheral or central nervous system dysfunction, choking, and, at some point, shock and death.
Extreme anemia
Severe anemia is the loss of red blood cells generally caused by hemorrhage, hemolysis, or aplasia that influences just how the blood lugs oxygen.
Osteomyelitis
Osteomyelitis is an infection of the bone or bone marrow.
On top of that, hyperbaric oxygen treatment might deal with different conditions that the FDA has actually not yet authorized. Various HBOT therapy facilities might allow the therapy of such problems. Conditions the FDA has not approved are known as off-label problems.
Off-label problems might benefit from hyperbaric oxygen treatment. These consist of:
-Persistent discomfort
-Lyme illness
-Migraine headache
-Fibromyalgia
-Arthritis
-Stroke
-Crohn's illness
New illnesses will certainly be included in the accepted checklist with time and also study. Nevertheless, utilizing HBOT therapy for off-label problems may not be covered by insurance coverage. Contact a medical professional who will determine whether hyperbaric oxygen treatment might be an option for you.
What Needs to Take Precautions Before HBOT?
If you are considering or have even made a decision to go after HBOT treatment, you must take some needed precautions. Before complying with the therapy treatment, make certain the doctor is licensed with experienced clinical staff.
The healthcare provider accountable for your sessions need to have the correct Undersea and Hyperbaric Medical Society training. Likewise, ask to see a certification that verifies they finished the program before you accept follow-up with the therapies.
Hyperbaric oxygen treatment is not recommended for everybody. Some people might have certain diseases or problems that HBOT can intensify or go to a higher threat of complicated problems. Those who suffer from the below problems must seek advice from a medical professional:
-Those with particular lung illness may be at greater threat for lung collapse.
-Individuals that have a cold or fever.
-Those who have actually lately undertaken ear surgery or injury.
When talking to a physician, list any problems you have that might place you in a higher-risk group. If you are not sure, ask your service provider.
Extra Read- HOW HYPERBARIC OXYGEN TREATMENT FUNCTIONS QUESTIONS FOR WOUND HEALING
What Are the Problems of HBOT?
Just like any kind of treatment, a client ought to understand the threats before continuing. However, problems take place seldom, as well as hyperbaric oxygen treatment is mostly safe.
Some problems include:
-Lung collapse: Atmospheric pressure adjustments typically trigger lung collapse.
-Seizures: Seizures might result from obtaining excessive oxygen in the main nerves.
-Middle ear injuries: Center ear injuries include eardrum rupture and also fluid leakage from changing air pressure.
-Temporary near sightedness: Eye lens adjustments might cause short-term near sightedness.
-Reduced blood glucose: Lowered blood sugar level occurs in people who utilize insulin.
-Claustrophobia: Claustrophobia is a fear of restricted places. Because HBOT treatment is done by having the person lie inside a shut chamber, those conscious limited areas should take care of.
Sometimes because of complications, clients may experience pain. Some people might likewise take time-outs to take a breath of typical air to stop oxygen poisoning if required. Do not be afraid to ask even more about other risks of hyperbaric oxygen treatment.
What Are the Negative Effects of HBOT?
Therapies of any kind will impact the body. Some can be much more extreme than others depending on the period and how each person refines the therapy.
The negative effects of hyperbaric oxygen treatment are worth keeping in mind. Some adverse effects are not as extreme, while others can take a serious toll on the body. These consist of:
-Lung damages
-Sinus damage
-Exhaustion
-Faintness
The majority of adverse effects of hyperbaric oxygen therapy are light. Nonetheless, sometimes, HBOT treatment can last for more than 2 hrs, depending upon the dosages needed for each person.
HBOT treatment sessions lasting longer than two hrs will likely cause side effects. Moreover, they will also take place if the pressure inside the hyperbaric oxygen chamber is more than three times the pressure in the ambiance.
Don't hesitate to ask your healthcare provider much more inquiries concerning the feasible negative effects. They will certainly consider any other clinical problems you have to help reduce the likelihood of experiencing side effects from the treatment.
The Hyperbaric Oxygen Therapy Procedure
Hyperbaric oxygen therapy is an outpatient treatment. There are two different sorts of chambers.
The initial chamber is made for single-person usage. In the mono system, you lie down on a table where you will be confined in a transparent chamber.
The 2nd type is an HBOT treatment room. In this chamber, multiple people are treated at the same time. Each person will certainly have an oxygen mask or a clear hood over their head. You can either sit or rest for the treatment.
While in your therapy session, the air pressure will be around two or 3 times the normal air pressure. The sensation of volume in your ears because of the enhanced atmospheric pressure will be short-lived. In addition, the health care team will certainly supervise monitoring you throughout the session.
The hyperbaric oxygen therapy treatment results will be different for every person. Some will certainly need greater than one session to be totally treated.
Treatment will be different for every client relying on the clinical condition as well as its severity degree. Some treatments will certainly also require a range of other treatments and also medicine. Ask your clinical company for the right info that ideally matches your requirements.
Rely Upon NexGen Hyperbaric to Treat Your Medical Problem
NexGen Hyperbaric is among the very best options for HOBT therapy. With the well-informed and respectful clinical team, NexGen Hyperbaric will certainly address your concerns or problems as best as possible.
Contact NexGen Hyperbaric today at 888-567-4302 to get a consultation for your problem and find out more regarding exactly how hyperbaric oxygen therapy will help you.
Extra Read- AMAZING PERKS OF HYPERBARIC OXYGEN THERAPY FOR ATHLETES
NexGen Hyperbaric, LLC
Hyperbaric Room, 2205 Cordillera Way, Edwards, CO 81632, United States
+1888-567-4302
https://goo.gl/maps/GzxgVpsrQmcEEhFG7
#hyperbaric oxygen chamber#hyperbaric oxygen therapy#wound healing#hyperbaricchamber#hyperbaric therapy
1 note
·
View note
Text
Thoracic Drainage Devices Market to Observe Strong Development by 2027
Thoracic Drainage Devices Market: Key Findings
Transparency Market Research has published a new report on the global thoracic drainage devices market. According to the report, the global thoracic drainage devices market was valued at ~US$ 615 Mn in 2018, and is projected to expand at a CAGR of ~5% from 2019 to 2027.
Chest tube thoracostomy or chest tube placement is a minimally-invasive procedure carried out to drain air, fluid, or blood from the thoracic space to prevent the lungs from collapsing. A chest tube is also called a thoracic catheter, chest drain, or intercostal drain. This thoracic catheter is inserted into the pleural space. This procedure includes the use of different devices such as thoracic drainage systems, trocar drains, unsecured needles, secured needles, pleural drainage catheters, and thoracic drainage kits. Thoracic drainage devices are used primarily for pleural effusion, pneumothorax, traumatic pneumothorax (gunshot or stab wound), and cardiac surgery procedures.
Request a PDF Sample - https://www.transparencymarketresearch.com/sample/sample.php?flag=S&rep_id=40529
Patient preference for minimally-invasive surgeries, high prevalence of cardiovascular diseases, and increase in the burden of spontaneous pneumothorax are factors driving the thoracic drainage devices market. Moreover, surge in thoracic surgeries, cardiothoracic surgeries, and cardiovascular surgeries contributes to the growth of the thoracic drainage devices market.
In terms of product, the thoracic drainage systems segment held a major share of the thoracic drainage devices market in 2018. The segment is likely to continue to dominate the market during the forecast period, owing to an increase in the adoption of thoracic drainage systems in hospitals due to a rise in the demand for surgical procedures. A thoracic drainage system also offers advanced technological benefits such as portability and new generation of smaller user-friendly digital systems and additional safety features.
Enquiry Before Buying Thoracic Drainage Devices Market Report - https://www.transparencymarketresearch.com/sample/sample.php?flag=EB&rep_id=40529
In terms of application, the thoracic surgery & pulmonology segment is anticipated to account for a major share of the global thoracic drainage devices market. The segment is expected to grow at a rapid pace during the forecast period. Thoracic and pulmonological disorders are quite common, and the prevalence of these disorders is increasing. Thoracic drainage devices are used in the treatment of pneumothorax, pleural effusions, and empyema disorders. Spontaneous pneumothorax is one of the major health problems across the globe. It is caused due to collection of air in the chest cavity, which gets resolved on its own; however, most often, it requires hospital admission and urgent medical care.
Rise in product recalls owing to improper packaging and malfunction, shortage of physicians, and challenges in maintaining chest tube patency are expected to hamper the growth of the global thoracic drainage devices market during the forecast period.
Request for Custom Research - https://www.transparencymarketresearch.com/sample/sample.php?flag=CR&rep_id=40529
Global Thoracic Drainage Devices Market: Prominent Regions
North America held a major share of the global thoracic drainage devices market in 2018. The market in the region is estimated to expand at a high CAGR during the forecast period. The thoracic drainage devices market in North America is driven by a highly structured healthcare industry and availability of well-defined reimbursement policies from private and public health insurance firms. Additionally, R&D activities being carried out to introduce new thoracic drainage devices with improved design and technology by a large number of market players in North America are driving the thoracic drainage devices market in the region.
Europe held a significant market share in 2018, after North America. Well-developed healthcare infrastructure and increase in incidence of pneumothorax, pleural effusion, and hemothorax are factors propelling the thoracic drainage devices market in the region.
Asia Pacific is a significant market for thoracic drainage devices. The region is a relatively untapped market. Hence, the region presents immense opportunities for market players. Major factors such as high prevalence of respiratory diseases, increase in number of surgeries, rise in patient population, growth of healthcare industry, and surge in awareness propel the thoracic drainage devices market in the region.
The markets in the Middle East & Africa and Latin America are projected to experience moderate growth in the near future.
Buy now Thoracic Drainage Devices Market Report - https://www.transparencymarketresearch.com/checkout.php?rep_id=40529<ype=S
Global Thoracic Drainage Devices Market: Key Players
Prominent players operating in the thoracic drainage devices market are C. R. Bard, Inc. (BD), MAQUET Holding B.V. & Co. KG (Getinge AB), Smiths Medical (Smiths Group plc), Teleflex Incorporated, Vygon SA, Medtronic, Cook Medical, Utah Medical Products, Inc., ATMOS MedizinTechnik GmbH & Co. KG, Sinapi Biomedical, Medela AG, and Rocket Medical plc.
Key players strive to strengthen their positions in the global thoracic drainage devices market. Developing economies, due to increase in government initiatives and rise in patient population, offer lucrative opportunities for these players to increase their share in the thoracic drainage devices market. Leading manufacturers engage in new product developments, collaborations, acquisitions, and distribution agreements. For instance, in 2015, Medtronic acquired Covidien plc. This has enabled the company to merge the innovative capabilities of the two companies, offer benefits of enhanced access to patients, improve clinical outcomes, and lower costs.
More Trending Reports by Transparency Market Research:
https://www.prnewswire.com/news-releases/increased-cases-of-gynecological-diseases-boost-demand-opportunities-for-players-in-gynecology-drugs-market-tmr-301155994.html
https://www.prnewswire.com/news-releases/remarkable-growth-in-working-women-population-worldwide-likely-to-fuel-breast-pumps-market-growth-tmr-301165675.html
https://www.prnewswire.co.uk/news-releases/single-use-cystoscope-market-to-reach-valuation-of-us-150-mn-by-2031-growing-acceptance-of-patient-ready-instruments-in-urology-to-bolster-demand-tmr-study-818277477.html
About Us Section:
Transparency Market Research is a global market intelligence company, providing global business information reports and services. Our exclusive blend of quantitative forecasting and trends analysis provides forward-looking insight for thousands of decision makers. Our experienced team of Analysts, Researchers, and Consultants, use proprietary data sources and various tools and techniques to gather, and analyse information. Now avail flexible Research Subscriptions, and access Research multi-format through downloadable databooks, infographics, charts, interactive playbook for data visualization and full reports through MarketNgage, the unified market intelligence engine. Sign Up for a 7 day free trial!
Contact
90 State Street, Suite 700
Albany, NY 12207
Tel: +1-518-618-1030
USA - Canada Toll Free: 866-552-3453
Website: https://www.transparencymarketresearch.com/
0 notes
Link

Global Thoracic Drainage Devices Market will expand at a stable rate owing to an increase in various incidences such as pleural effusion and pneumothorax, coupled with an acceptance of advanced thoracic drainage technological products over the forecast period.
Request for a sample copy of this report @ https://www.insightsandreports.com/request-sample/173
Thoracic Drainage Devices Market: Market Dynamics
The thoracic drainage devices can be primarily used for ailment signs of pneumothorax, pleural effusion, traumatic pneumothorax and some cardiac surgeries. Some of the key boosting factors for the growth of thoracic drainage devices market include the rise in patient’s preference of cardiovascular diseases, coupled with rising minimally invasive surgeries demand. Cardiovascular diseases are some serious health issues effecting a large number of people across the world. Some of the causes for cardiovascular problems include diabetes, hypertension, along with obesity. These factors are causing cardiovascular disorders, mainly heart strokes, atresia, regurgitation, and stenosis. Rise in open heart surgeries, caused by overweight, lack of workout, smoking and unhealthy lifestyles will further create a significant demand for thoracic drainage device, which will boost the market significantly.
Thoracic Drainage Devices Market: By Application
In terms of application, the thoracic drainage devices market has been segmented into thoracic surgery & pulmonology, general intensive care & emergency medicine, cardiac surgery, oncology & pain management, infectious disease, and military/damage control medicine. The thoracic surgery & pulmonology segment is predicted to hold the prime share of the market, owing to increasing pulmonological and thoracic disorders. Moreover, these devices are further used for treating pleural effusions, empyema, and pneumothorax disorders.
Thoracic Drainage Devices Market: By Region
North America and Europe likely to contribute the dominant share of the global thoracic drainage devices market. The market share is majorly backed by the revenue generated by the U.S. market. This is majorly augmented by the factors like high level of end-user awareness, coupled with favorable health insurance policies. Moreover, the U.S. market is mainly driven by rising adoption of new devices and affordable medical insurance plans for cardiovascular surgical treatments.
Europe held the second dominant share of the global market. It is majorly contributed by Germany. Rising consumer awareness regarding cardiovascular diseases, coupled with rising health care expenditure will drive the Europe thoracic drainage devices market.
Less healthcare facilities’ penetration, coupled with the lack of product availability of thoracic drainage devices will restrict the market growth in regions like Latin America, Middle East, and Africa.
For more information about this report @ https://www.insightsandreports.com/industry-reports/thoracic-drainage-devices-market
Thoracic Drainage Devices Market: Competitive Landscape
Some of the key contributors in the global market include Vygon S.A., Cook Medical, Maquet Holding B.V. & Co. KG, Smiths Medical, Medela, Teleflex Incorporated, Medtronic Plc., C. R. Bard, Inc., Utah Medical Products, Inc., and Atmos Medizine Technik Gmbh & Co. KG among several others.
About Us:
Insights and Reports is a research and consulting group assisting the clients with 360-degree insights with real time qualitative and quantitative information. The Insights and Reports team is valued for continuous client-oriented services. Our data scientists monitor the markets pertaining to their expertise on a daily basis with the help of 150+ analysts to back them with accurate market studies.
Contact Us:
Mr.Saby
Insights And Reports,
2201 Cooperative Way #600,
Herndon, VA 20171, USA.
Tel: +1 703 574 4447
Email:[email protected]
#Thoracic Drainage Devices Market Growth#Thoracic Drainage Devices Market#Global Thoracic Drainage Devices Market#Thoracic Drainage Devices Market Trends#Thoracic Drainage Devices Market Forecast#Thoracic Drainage Devices Market Analysis#Thoracic Drainage Devices Market Overview#Thoracic Drainage Devices Market Report#Thoracic Drainage Devices Market Size
1 note
·
View note