#medical coding consulting in usa
Explore tagged Tumblr posts
Text
MedUSA Healthcare Services offers premier coding and consulting services in the USA. Specializing in healthcare, we optimize revenue cycles and streamline operations through expert coding practices and strategic consulting, ensuring compliance and financial efficiency.
#Coding & Consulting Solutions#medical billing companies in usa#medical coding consulting in usa#coding & consulting in usa#medical coding near me#medical billing services#medical billing and coding
0 notes
Text
Enhance Your Practice with Premier Medical Billing Services in the USA
In the complex world of healthcare, managing medical billing efficiently is paramount for any practice. In the USA, the best medical billing services are crucial for reducing administrative burdens, ensuring compliance, and optimizing revenue cycles. One such standout provider is Medi Claim Management, renowned for their comprehensive and reliable services.
Medi Claim Management offers a robust suite of medical billing services designed to cater to the diverse needs of healthcare providers across the nation. As the best medical billing agency in the USA, they handle every aspect of the billing process—from claims submission to follow-up—ensuring that providers can focus on patient care rather than paperwork. Their proficiency with various EHR/EMR systems helps reduce claim denials and maximize revenue, making them a preferred choice for practices seeking efficiency and reliability.
What differentiates Medi Claim Management is their commitment to providing cost-effective, high-quality solutions tailored to each client’s unique needs. Their services not only adhere to HIPAA regulations and data security best practices but also offer 24/7 support to ensure that providers receive timely assistance whenever needed. This focus on affordability without compromising on quality has established them as a trusted partner in the medical billing industry.
Beyond traditional billing services, Medi Claim Management offers in-depth consultations to identify and address issues within existing billing systems, detailed auditing services, and staff training to enhance overall efficiency. This comprehensive approach ensures that practices not only sustain but improve their revenue cycles, resulting in better financial health and operational performance over time.
For healthcare providers across the USA, Medi Claim Management stands out as the best medical billing agency to partner with. Their dedicated team, advanced technology, and holistic service offerings ensure superior revenue cycle management, allowing providers to focus on what matters most: delivering exceptional patient care. Explore more about their services and discover how they can transform your practice by visiting here
#medical billing agency#medical billing and coding#medical billing outsourcing#medical billing company#medical billing services in usa#medical billing consultant in Boston
0 notes
Text
Top Medical Billing Companies in the USA: Everything You Need to Know Before Choosing One
Top Medical Billing Companies in the USA: Everything You Need to Know Before Choosing One
In the fast-paced world of healthcare, ensuring timely and accurate billing is crucial for the financial health of any medical practice. This is where medical billing companies in the USA come into play. These specialized service providers handle the complex process of translating medical procedures into billable claims, submitting them to insurance companies, managing reimbursements, and following up on denials.
With increasing regulations, high administrative burdens, and a growing demand for efficiency, outsourcing medical billing has become a strategic move for practices of all sizes. This comprehensive guide will help you understand the role of medical billing companies in the USA, their benefits, challenges, and how to choose the right one for your healthcare facility.
What Are Medical Billing Companies?
Medical billing companies are third-party service providers that manage the entire revenue cycle on behalf of healthcare providers. Their main job is to ensure that medical practices are paid correctly and on time by handling everything from claim creation and submission to payment posting and denial management.
These companies typically offer a suite of services including:
Insurance verification
Coding and charge entry
Claim submission
Denial management
Payment posting
Patient billing and collections
Reporting and analytics
Some companies also provide value-added services like credentialing, compliance support, and consulting.
Why Medical Practices Outsource Billing in the USA
Outsourcing medical billing is becoming increasingly popular in the United States. Here are the top reasons why:
1. Focus on Patient Care
Administrative tasks like billing can consume a significant amount of time and resources. By outsourcing, healthcare professionals can shift their focus back to patient care, improving the quality of service.
2. Reduced Errors and Rejections
Medical billing companies employ certified coders and billers who are up-to-date with the latest industry codes and payer requirements. This expertise leads to fewer billing errors, minimized claim denials, and faster reimbursements.
3. Cost-Effective Operations
Hiring and training in-house billing staff, investing in software, and staying compliant with regulatory changes can be costly. Outsourcing eliminates these expenses, often resulting in lower overhead costs.
4. Faster Payments and Better Cash Flow
Experienced billing companies streamline the claim submission and follow-up process, reducing the days in accounts receivable (A/R) and improving cash flow.
5. Scalability
Whether you’re a solo practitioner or a growing healthcare network, medical billing companies can scale their services to match your needs—without the hassle of hiring more internal staff.
Key Features to Look for in Medical Billing Companies in the USA
Not all billing companies offer the same level of service. When selecting a partner, here are the most critical features to consider:
1. Industry Experience
Look for companies with proven experience in your specific field of healthcare, whether it's primary care, surgery, radiology, or durable medical equipment (DME).
2. Certified Staff
Ensure the company employs CPC (Certified Professional Coders), CPB (Certified Professional Billers), or other relevant certified professionals.
3. Technology & Integration
Check if the company uses reliable billing software and whether it integrates with your existing EHR (Electronic Health Record) or practice management system.
4. Compliance and Security
Ensure they comply with HIPAA regulations, and inquire about their data security protocols to protect sensitive patient information.
5. Transparent Reporting
The best companies provide detailed reports on performance metrics such as claim acceptance rates, denial trends, A/R aging, and collection ratios.
6. Customizable Services
Look for a provider that offers flexible plans and services tailored to your practice's unique needs.
Top Medical Billing Companies in the USA (as of 2025)
Here are some of the leading and trusted names in the US medical billing industry:
1. Kareo
Known for its integrated platform for billing, scheduling, and EHR, Kareo supports small to mid-sized practices and offers intuitive tools to track billing progress.
2. AdvancedMD
Offers comprehensive RCM services, EHR integration, and patient engagement tools, ideal for practices that want a one-stop shop.
3. Athenahealth
Athenahealth provides end-to-end revenue cycle services with advanced analytics and payer rule engines to reduce denials.
4. PracticeSuite
Affordable and scalable, PracticeSuite is a good choice for independent practices looking for modular services and detailed reports.
5. BillingParadise
A performance-driven company that uses AI to optimize claim success rates and offers specialization in 32+ medical specialties.
6. DrChrono
With strong EHR and RCM capabilities, DrChrono caters to practices looking for mobile-based and customizable billing solutions.
Challenges of Outsourcing to Medical Billing Companies
While outsourcing offers many benefits, it also comes with certain risks:
1. Loss of Control
Some practices may feel they have less visibility or control over the billing process when outsourcing to a third party.
2. Data Security Concerns
Sharing patient information with an external provider increases the risk of data breaches if the proper security protocols aren’t in place.
3. Communication Gaps
Delays in communication between the practice and billing company can lead to errors or missed updates.
4. Variable Quality of Service
Not all billing companies offer the same level of expertise and responsiveness. It's essential to perform due diligence before making a choice.
How to Choose the Right Medical Billing Company
Here’s a step-by-step guide to help you select the best billing partner:
Define Your Needs: Do you need full-service RCM or just claim submission support? Clarify what you expect from the vendor.
Research Multiple Providers: Don’t settle for the first company you find. Compare at least 3–5 companies.
Ask for References and Case Studies: Speaking with existing clients or reviewing case studies gives insight into real-world performance.
Request a Trial or Demo: Evaluate the software, reporting dashboards, and service quality with a demo.
Negotiate Pricing Models: Billing companies may charge a percentage of collections, a flat monthly fee, or per-claim rates. Ensure the pricing aligns with your budget and practice size.
Review the SLA (Service Level Agreement): The SLA should clearly state performance expectations, turnaround times, communication protocols, and security commitments.
The Future of Medical Billing Companies in the USA
The role of medical billing companies is evolving with technological advancements and changes in healthcare regulations. Some emerging trends include:
1. AI and Robotic Process Automation (RPA)
AI-driven systems are enhancing coding accuracy, automating repetitive tasks, and predicting denial patterns to improve collection rates.
2. Telehealth Billing Expertise
With the rise of virtual healthcare, billing companies are adapting to support telehealth coding, payer rules, and regulatory changes.
3. Patient-Centric Financial Experience
Billing companies are focusing more on patient engagement by offering cost estimators, mobile payment solutions, and transparent billing practices.
4. Blockchain and Secure Data Exchange
To combat fraud and improve data integrity, some billing firms are exploring blockchain for secure transactions and audit trails.
Conclusion
Medical billing companies in the USA are essential partners for healthcare practices looking to improve revenue cycles, reduce operational costs, and remain compliant. Choosing the right company requires careful consideration of your needs, the company's expertise, technology stack, and service quality.
By outsourcing to a reputable medical billing company, providers can streamline operations, reduce claim errors, increase collections, and focus on what matters most—delivering exceptional patient care.
0 notes
Text
Cardiology Information System Market Trends and Future Outlook 2034

A Cardiology Information System (CIS), also referred to as a Cardiovascular Information System (CVIS), is a specialized software platform designed to streamline the workflows and manage the data specific to cardiology departments and practices. It acts as a centralized system for organizing and accessing cardiovascular patient information. The system offers a wide array of functions, including managing patient demographics and medical history, scheduling procedures, storing and analyzing cardiac diagnostic images and reports (such as ECGs, echocardiograms, and angiograms), tracking clinical interventions, handling billing and coding, and enabling effective communication among healthcare providers involved in a patient’s cardiac care.
According to SPER market research, ��Global Cardiology Information System Market Size- By Type, By Function, By End Use - Regional Outlook, Competitive Strategies and Segment Forecast to 2034’ state that the Global Cardiology Information System Market is predicted to reach 3.3 Billion by 2034 with a CAGR 9.58%.
Drivers:
Several key factors are driving the growth of the Cardiology Information System (CIS) market. The increasing global incidence of cardiovascular diseases has heightened the demand for precise and efficient diagnostic and treatment solutions. To enhance patient outcomes, healthcare providers are seeking systems that can streamline data handling, optimize clinical workflows, and support quicker, more informed decision-making. The adoption of CIS has been further accelerated by technological advancements such as cloud-based platforms, AI integration, and enhanced interoperability, which improve system accessibility, scalability, and overall performance. Moreover, the growing emphasis on cost reduction and operational efficiency in healthcare has led hospitals and clinics to invest in advanced cardiology information systems.
Request a Free Sample Report: https://www.sperresearch.com/report-store/cardiology-information-system-market?sample=1
Restraints:
The Cardiology Information System (CIS) market encounters several obstacles that can slow its growth and adoption. A primary challenge is the substantial upfront cost of implementation, including expenses for software, hardware, training, and ongoing maintenance, which can be prohibitive for smaller healthcare providers. Integration with existing hospital information systems and electronic health records (EHR) is often complex and time-intensive, frequently requiring tailored solutions. Concerns over data privacy and security—particularly with cloud-based platforms—also present major risks, given the sensitive nature of healthcare data and strict regulatory requirements. Additionally, the absence of standardized protocols across systems can lead to interoperability challenges, hindering smooth data exchange between platforms.
The widespread prevalence of heart disease in North America has established the region as a dominant market for cardiovascular information systems. According to the Centers for Disease Control and Prevention, heart disease remains the leading cause of death across most racial and ethnic groups in the United States. It consistently accounts for a significant portion of overall mortality, with lives lost to cardiovascular conditions occurring at frequent and alarming intervals. Some significant market players are Philips Healthcare, GE Healthcare, Cisco Systems, LUMEDX Corporation, Digisonics, Inc., and Honeywell Life Care Solutions.
For More Information, refer to below link: –
Cardiology Information System Market Growth
Related Reports:
Companion Animal Ear Infection Treatment Market Growth
Global IVD In Cardiology and Neurology Market Size
Follow Us –
LinkedIn | Instagram | Facebook | Twitter
Contact Us:
Sara Lopes, Business Consultant — USA
SPER Market Research
+1–347–460–2899
#Cardiology Information System Market#Cardiology Information System Market Share#Cardiology Information System Market Size#Cardiology Information System Market Revenue#Cardiology Information System Market Analysis#Cardiology Information System Market Segmentation#Cardiology Information System Market Future Outlook#Cardiology Information System Market Competition#Cardiology Information System Market forecast
0 notes
Text
From Concept to Code: DCom USA’s Full-Service Web Development Approach
🔹 Introduction: Why Your Business Needs a Website
Every business today needs a website. It’s how customers find you, trust you, and contact you. At DCom USA, we build professional, responsive web development that help your brand stand out online. Whether you're starting fresh or need a redesign, we’ve got the skills to bring your vision to life.
🔹 What Makes a Good Website?
A good website is more than just looks. It should:
✅ Load fast on all devices ✅ Be easy to navigate ✅ Offer clear information ✅ Match your brand style ✅ Convert visitors into customers
We focus on both design and function — so your site performs well and looks great.
🔹 Key Features We Include in Every Website
We make sure every website we build includes:
Mobile-Friendly Design
User-Friendly Navigation
Contact Forms & Calls to Action
SEO-Optimized Structure
Fast Loading Speed
SSL Security Integration
Social Media Linking
Our goal is to give you a site that’s ready to grow your business.
🔹 Our Web Development Services
🧩 Custom Website Development
No templates, no shortcuts. We design from scratch based on your goals, branding, and content.
📱 Responsive Web Design
We build websites that work perfectly on desktops, smartphones, and tablets. Your visitors get the best experience — no matter their device.
🛒 eCommerce Website Solutions
Sell products online with a secure, easy-to-use store. We integrate payment gateways, shopping carts, and order management tools.
⚙️ Content Management Systems (CMS)
Want to update your own website easily? We build with WordPress, Shopify, or custom CMS platforms so you stay in control.
🔒 Website Maintenance & Security
We offer monthly plans to keep your site safe, updated, and running fast. No stress — we handle the tech, you focus on your business.
🔹 Technologies We Work With
We use the latest and most reliable technologies in web development:
HTML5 / CSS3 / JavaScript
React / Angular / Vue.js
PHP / Laravel / Node.js
WordPress / Shopify / WooCommerce
MySQL / MongoDB / Firebase
API Integration / CRM Connections
Whatever your needs, we choose the right tools for your project.
🔹 Industries We Serve
We’ve built websites for clients in many industries, including:
🏢 Corporate & Business 🛍️ Retail & eCommerce 📚 Education & Training 🍴 Restaurants & Food Services 🏥 Healthcare & Medical 🏠 Real Estate 📱 Startups & Tech Firms
We customize the experience based on your industry’s specific needs.
🔹 Our Process: Step-by-Step
Here’s how we bring your website to life:
Consultation & Planning ��� Understand your goals, audience, and content
Design Phase – Create layout, colors, and user flow
Development – Build your site with clean, optimized code
Content Upload – Add your text, images, and branding
Testing – Check mobile, browser compatibility, and speed
Launch – Go live and make your brand shine online
Ongoing Support – We’re here for future updates and maintenance
🔹 SEO-Ready Websites
We follow best SEO practices so your site ranks well in search engines:
🔍 Fast load time 📱 Mobile responsiveness 📄 Clean code and structure 🧭 Keyword-focused content setup 🔗 Internal linking and metadata
This means more visibility, traffic, and business for you.
🔹 Why Choose DCom USA?
✔️ Experienced Team – Years of hands-on experience in modern web development ✔️ Tailored Approach – We focus on what works for your business ✔️ Affordable Packages – Quality service that fits your budget ✔️ Transparent Process – Clear communication from start to finish ✔️ Local California Expertise – We understand your market
We don’t just deliver websites — we deliver results.
🔹 FAQs – Quick Answers
Q: How long does it take to build a website? A: Typically 2–6 weeks, depending on the project size.
Q: Can I update the website myself later? A: Yes! We build CMS-based websites so you can easily make edits.
Q: Will my site work on mobile? A: Absolutely. All our sites are mobile-friendly by default.
🔹 Conclusion: Build Your Digital Future Today
A professional web development opens doors for new opportunities, clients, and sales. At DCom USA, we help you create a website that’s powerful, attractive, and ready to grow. Whether you need a basic site or a full-featured online platform — we’re here to make it happen.
0 notes
Text
Bright Well Mental Health Service Inc. (Establishing Fictitious Mental health care center) Company Background BrightWell mental health service Inc. is focused on providing health care facility to individuals of all ages. Their mental health service program is comprehensively designed to cater the needs of children, adolescent, adults and people of old age. The mental health services are not just limited to the psychological and emotional well-being of the individuals but BrightWell mental health service Inc. also provides substance abuse and chemical dependency (alcohol and drugs) services to adults. The company has been in operation since January 1990, based its head quarters in New York, USA. It has aimed to provide mental health service throughout United States and also consultancy and medical care through its medical camps in developing countries of East Africa and Asian countries like Bangladesh, Myanmar, Nepal, Afghanistan, Syria, Turkey and Tajikistan. Establishing BrightWell Mental Health Service Inc. On 501(c)(3) Clause of IRS Non-profit organizations like BrightWell mental health Service Inc., they obtain 501(c)(3) status referred to the IRS tax code that gives tax-exemption status to these organizations. The procedure adopted in forming such organization is defining the type of organization, developing the mission statement, forming board of directors team, file articles of incorporation, drafting of bylaws, developing the budget, establishing record keeping structure, designing accounting system, file for 501(c)(3) status, file for tax exemption status and finally apply for non-profit mailing permit. The Corporate governance part of this status which includes mission and vision, board of directors and governing body is discussed in the following section. Mission and Vision The corporate mission of the BrightWell Metal health Service Inc. is: "Provide wide range of metal health services and social security to the individual through comprehensive healthcare program. Also provide information and assistance necessary to ensure that each individual have bright, happy and healthy living with confidence in society." The corporate values of the health care company was based on providing benefits, high quality services, creating awareness and mental healthcare educational program in the developed and developing communities and regions. Major Challenges The major challenges confronting healthcare facility in accomplishing its mission are: a) Insurance Coverage of Health is provided to all the citizens to fulfill all the medical needs of the individual. BrightWell mental health service inc., promote broad range of mental healthcare facility through this insurance program and create awareness about the cost effectiveness of mental healthcare treatment. b) Expansion of healthcare facility through the insurance program will limit to the extent that many of the illness are not covered in the insurance coverage. This will necessitate the need for public funding for the treatment and awareness creating. This public funding is managed though trust, grants from private enterprises and individuals and public body investment. c) Develop strong research and development unit for continuous advancement and progress of the medical facility and needs of its client. The vision of the company is to fulfill the mission of the organization by taking care of the major challenges through strategically designed policies and procedures that comply with the clauses of nonprofit organization and overall objectives of the firm. BrightWell mental health service BOD and governing body Executive Committee President of the medical facility is Hart Karen. He has been associated with the National Institute of Health Association as the Vice President of Community health program. He possesses his Masters in community health program and has been associated with many residency health programs. He has profound experience the related field. Peter James, Company Secretary/Treasurer have Chartered Accountancy and have been affiliated with many accountancy firm of social and developmental sector. Hannah Hathaway, Medical Health Public Policy Market Representative. She has her Master's in Public Relations and has been accredited with many medical programs national and international levels. She also has her MBBS that give her proficiency in the medical field and enable her to run campaigns on creating public awareness on medical problems and social issues created through substance abuse and chemical addiction. Board Members at Large Dr. Angeline Lords, Managing Director, she is a PhD in Social Development. She has been active participant in assessing the performance of the medical team and healthcare facility at large. The Board of Director team comprise of 5 members associated with the marketing body, human resource body, audit committee, community health center body and public relations body. All the board members are active participants in evaluating the performance of the company in their respective areas and assessing the overall performance of the healthcare facility. Medical Health services at BrightWell Mental Health Service Inc. The medical health services offered by BrightWell Mental Health Service Inc., are: 1. Adult Psychiatric Program: BrightWell offers comprehensive inpatient psychiatric treatment for individuals of age 18 and above. These people are specifically treated for emotional disorder, anxiety, stress and abnormal behaviors. Some of the common ailments are bipolar disorder, personality disorder, depression and schizophrenia. Patients are treated with individualistic approach through specialized teams. Specialized team comprise of psychiatrists, clinical psychologists, occupational and recreational therapists, clinical social workers and counselors. The team evaluates the case make a treatment plan and conducts it as per patient needs and requirements. 2. Child and Adolescent Psychiatry: This program is structured to provide immediate, short-term inpatient care for children aged between 5 to 17 and adolescent. It provides services of crisis management, diagnostic evaluation, focused therapy, daytime treatment for behavioral diagnosis. Other such type of services includes Child and Adolescent Services. 3. Community-based programs: It includes services of in house and therapeutic day treatment. Community-based programs are designed to provide healthcare facility based on community based. Other type of such services is emergency services, In-home services and out-home services. All the services are focused on providing customized services to the client. They are designed to satisfy individual needs of the clients regardless of nationality, ethnicity or any social or demographic differences. The BrighWell Mental Health Service Inc. is making its active contribution in managing the healthcare facility of the community, nation and also the international market. The company is managing the international service in the developing countries through health camps arranged in association with the domestic Healthcare unit of that region. The health center has also taken up the responsibility of designing the mental health facility program for the war or conflict affected people globally restoring confidence, mental and psychological order of these people trying to help them recover from devastating scenario. The facility has been actively engaged nationally, regionally and globally in most of WHO's efforts in primry prevention, capacity building, injury research and trauma management. The primary focus was to carry out public health research in injuries. Around the world, injuries range from the unintentional, such as falls, road traffic disturbance and work related stress to intentional injuries like suicides and homicides in worst scenarios. The facility has identified that capacity building in these areas and professionals to prevent injury prevention and control and emergency care providers in trauma care centers. All these efforts have been designed to provide healthy living for the children, adolescent and adults through stress, anxiety and substance abuse management and rectifying the behavior of the individuals in the meaningful and rational manner that sustains for longer period. https://www.paperdue.com/customer/paper/xyz-mental-health-services-inc-117134#:~:text=Logout-,XYZMentalHealthServicesInc,-Length4pages Read the full article
0 notes
Text
Upcoding in Medical Billing: What Patients and Providers Need to Know

In the ever-evolving landscape of healthcare, medical billing plays a crucial role in ensuring that healthcare providers are reimbursed for their services. However, unethical practices like upcoding—the deliberate or accidental use of higher-level service codes in billing to secure higher reimbursements—pose a significant risk to both patients and providers. Understanding upcoding is essential for maintaining compliance, preventing fraud, and safeguarding the integrity of the healthcare system.
This comprehensive guide will shed light on what upcoding is, its consequences, and the steps that both patients and providers can take to avoid falling victim to or committing such fraudulent activity.
What is Upcoding in Medical Billing?
Upcoding occurs when healthcare providers or billing specialists use a CPT (Current Procedural Terminology) code that reflects a higher level of care or a more complex procedure than was actually provided. This could happen in outpatient, inpatient, or even telehealth settings. For instance, a simple office visit might be billed as a complex consultation, or a routine test may be coded as a more expensive diagnostic exam.
While upcoding is sometimes unintentional due to human error or miscommunication, when done deliberately, it is considered fraud under the False Claims Act (FCA) and can lead to severe penalties.
Why Does Upcoding Happen?
There are various reasons for upcoding in the medical field, including:
Financial Gain: Upcoding leads to higher reimbursements from insurance companies, Medicare, or Medicaid. This financial incentive often tempts dishonest providers to engage in this practice.
Errors in Documentation: In some cases, upcoding happens unintentionally due to inaccurate documentation or a misunderstanding of the billing codes.
Pressure from Billing Companies: In certain situations, third-party medical billing companies may pressure providers to upcode in order to increase revenue, which boosts their commissions.
Lack of Proper Training: Improper coding can also result from insufficient training for billing and coding specialists who may not fully understand the complexities of the ICD-10 or CPT coding systems.
The Impact of Upcoding on Patients
Upcoding has a far-reaching impact that extends beyond the healthcare providers. Patients can face significant repercussions, including:
Increased Healthcare Costs When upcoding occurs, the patient’s insurance company or government program is billed for services that were not actually provided or were exaggerated in complexity. This can result in higher co-pays, deductibles, and premiums for patients. Over time, these unjustified expenses can strain patients financially.
Denial of Future Coverage Upcoding can sometimes flag a patient’s medical record as having received more complex or serious care than they actually did. This can make it more difficult for patients to obtain life insurance, long-term care insurance, or even health insurance in the future, as their medical history appears more severe.
Exposure to Unnecessary Treatments Patients who are victims of upcoding might also be exposed to unnecessary follow-up tests or procedures. These can lead to more physical and emotional stress, not to mention additional financial burdens.
The Impact of Upcoding on Providers
Healthcare providers, both individual practitioners and large organizations, can face severe consequences if caught upcoding.
Deliberate upcoding is a violation of the False Claims Act. If a provider is found guilty of submitting false claims, they may be subject to substantial fines, criminal charges, and even imprisonment. Providers may also lose their license to practice and face exclusion from federal healthcare programs like Medicare.
In the competitive field of healthcare, reputation is everything. Being accused of or found guilty of upcoding can damage a provider’s credibility and trustworthiness. Patients may choose to leave the practice, and it can become harder to attract new ones, resulting in a significant loss of business.
Beyond the legal fines, providers who engage in upcoding may be required to return overpayments and compensate for any damages caused. In some cases, practices have had to close down entirely due to the financial strain caused by upcoding penalties.
How to Prevent Upcoding: Best Practices for Providers
Providers must take proactive steps to ensure that they avoid upcoding and maintain the highest levels of compliance and ethics in medical billing.
Invest in Proper Training: Ensure that all billing and coding staff are thoroughly trained in the ICD-10, CPT, and HCPCS Level II codes. Continuous education and refresher courses should be mandatory to keep staff updated on the latest coding changes and regulatory guidelines.
Conduct Regular Audits: Conducting internal audits of billing practices helps to identify potential upcoding before it escalates into a legal issue. Hiring third-party auditors can also provide an unbiased review of your billing procedures.
Improve Documentation Practices: Ensuring accurate and complete documentation of the patient encounter is crucial. Medical records should precisely reflect the care provided. Implementing Electronic Health Records (EHR) can help streamline and enhance the accuracy of medical documentation.
Use Compliance Programs: Create and enforce a strict compliance program that addresses upcoding and other potential fraudulent practices. Compliance programs should include policies, training sessions, and monitoring systems to prevent and detect upcoding.
Conclusion: The Importance of Awareness and Ethical Practices
Upcoding in medical billing is a serious issue that affects both patients and providers. By fostering a culture of transparency, accuracy, and ethical billing practices, providers can avoid the severe consequences of upcoding. At the same time, patients can take proactive steps to ensure they aren’t being overcharged for services they didn’t receive.
Awareness and prevention are key to addressing this fraudulent practice. By working together, both sides can help safeguard the integrity of the healthcare system and ensure that medical billing is fair and accurate.
Frequently Asked Questions(FAQ's)
1. What is upcoding in medical billing?
Upcoding is the practice of using a medical billing code that represents a higher level of service or more complex procedure than what was actually provided. This can lead to higher reimbursements for the provider and is considered fraudulent when done intentionally.
2. How does upcoding affect patients?
Upcoding can lead to increased healthcare costs for patients, as their insurance may be billed for more expensive services. It can also result in higher co-pays, deductibles, or even future insurance denials based on an inflated medical history.
3. What are the legal consequences of upcoding for providers?
Providers caught upcoding may face severe penalties, including fines, exclusion from Medicare or Medicaid programs, criminal charges, and even imprisonment. The practice is considered fraud under the False Claims Act.
4. How can patients protect themselves from upcoding?
Patients can protect themselves by reviewing itemized medical bills carefully, questioning any unfamiliar charges, and reporting suspicious activity to their insurance provider or Medicare/Medicaid if they suspect fraudulent billing.
5. What can healthcare providers do to avoid upcoding?
Healthcare providers can prevent upcoding by investing in proper training for their billing and coding staff, conducting regular audits, improving documentation practices, and implementing a strict compliance program to detect and prevent billing errors.
#medical billing#medical billing and coding#medical billing company#medical billing outsourcing#medical billing services#upcoding in medical billing
0 notes
Text
Discover top-notch medical billing service in Florida with MedUSA Healthcare Services. We offer tailored billing solutions to meet the unique needs of healthcare providers. Our services are designed to improve accuracy and efficiency in your billing processes.
#medical billing service in Florida#medical billing services florida#medical billing companies in florida#medical billing services in florida#coding & consulting south windsor#medical billing services#best medical billing services#billing services in florida#medical billing service#healthcare billing service#medical billing companies in usa
0 notes
Text

Top 10 business idea for USA
Top 10 business idea for USA
Here are 10 promising business ideas for the USA, reflecting current trends and opportunities:
1. E-commerce Niche Store
Focus on a specific product category, such as eco-friendly products, fitness gear, or pet accessories. With growing demand for niche products, targeted e-commerce stores can thrive.
2. Online Education Platform
With the rise of remote learning, create a platform offering specialized courses, certifications, or tutoring in high-demand areas like coding, language learning, or business skills.
3. Subscription Box Service
Offer curated monthly boxes around themes such as beauty, fitness, gourmet food, or wellness. Subscription-based businesses provide steady recurring revenue.
4. Health & Wellness Coaching
Start a business offering virtual health coaching, mental health counseling, or fitness training, catering to the growing demand for personal wellness and mental health services.
Here are 10 promising business ideas for the USA, reflecting current trends and opportunities:
1. E-commerce Niche Store
Focus on a specific product category, such as eco-friendly products, fitness gear, or pet accessories. With growing demand for niche products, targeted e-commerce stores can thrive.
2. Online Education Platform
With the rise of remote learning, create a platform offering specialized courses, certifications, or tutoring in high-demand areas like coding, language learning, or business skills.
3. Subscription Box Service
Offer curated monthly boxes around themes such as beauty, fitness, gourmet food, or wellness. Subscription-based businesses provide steady recurring revenue.
4. Health & Wellness Coaching
Start a business offering virtual health coaching, mental health counseling, or fitness training, catering to the growing demand for personal wellness and mental health services.
5. Sustainable Product Business
Focus on eco-friendly, sustainable products like reusable household items, green cleaning products, or biodegradable packaging, capitalizing on consumers' shift toward sustainability.
6. Freelance Consulting Services
Provide specialized freelance consulting in fields like marketing, IT, HR, or business strategy. As more companies turn to remote work, there's a growing demand for freelance professionals.
7. Home Improvement Services
Offer services such as home renovations, landscaping, or smart home installations. The pandemic has increased interest in home improvement projects as people spend more time at home.
8. Mobile Car Wash & Detailing
Provide a mobile car wash and detailing service that goes to customers' homes or workplaces, offering convenience and catering to busy professionals.
9. Food Truck or Ghost Kitchen
Start a food truck or a delivery-only kitchen (ghost kitchen) offering unique or healthy food options. With the rise of food delivery apps, this model requires lower upfront costs than a traditional restaurant.
10. Senior Care Services
As the population ages, there’s growing demand for non-medical in-home care services, such as companionship, meal preparation, or transportation for seniors.
Each of these business ideas leverages current consumer trends, market gaps, and future potential, especially in the post-pandemic world.
1 note
·
View note
Text
Best Medical CPA Firm in the USA: Dedicated Financial Expertise for Healthcare Professionals
When it comes to managing the finances of a healthcare practice, having a specialized CPA firm can make all the difference. If you’re searching for the best Medical CPA Firm in the USA, look no further. Our firm offers unparalleled expertise tailored to meet the unique needs of healthcare professionals.
Why Choose a Medical CPA Firm?
Expertise in Healthcare Accounting
Specialized Knowledge: Unlike general CPA firms, we understand the complexities of healthcare accounting, including billing, coding, and compliance requirements.
Regulatory Compliance: We ensure your practice adheres to all relevant regulations, helping you avoid costly penalties and focus on patient care.
Tailored Financial Solutions
Customized Services: From tax planning to financial reporting, our services are designed to address the specific challenges faced by medical professionals.
Efficient Management: We offer strategic advice to streamline your financial operations, improving both efficiency and profitability.
Comprehensive Support
Practice Management: Our team assists with budgeting, forecasting, and financial analysis to support your practice’s growth and stability.
Personalized Guidance: We provide one-on-one consultations to address your individual needs and help you make informed financial decisions.
Why We Stand Out
Proven Track Record: Our firm has a history of success with healthcare clients across the USA, providing reliable and effective financial solutions.
Dedicated Team: Our professionals are committed to delivering exceptional service and building lasting relationships with our clients.
Choosing the right CPA firm is crucial for the success of your healthcare practice. With our dedicated financial expertise and personalized approach, we ensure that your practice is well-managed and poised for growth.
Contact us today to discover how the best Medical CPA Firm in the USA can help you achieve your financial goals.
1 note
·
View note
Text
FDA 510k Clearance for Medical Device and IVDs
FDA 510k - An Overview
FDA 510k is a file containing sufficient information about a device to demonstrate that the medical device is at least as safe and effective as legally marketed devices that are not subjected to PMA. Organizations planning to launch Class I, II, and III devices in the United States intended for human use must submit a 510(k) if pre-market approval is not required.
Most class 1 devices are exempt from FDA 510k requirements. During the review of the file, if the FDA finds the device to be substantially equivalent, it will grant the FDA 510k clearance for medical devices with a ‘(k)’ number.
We offer technical and scientific assistance in identifying a suitable predicate device, regulation number, and device code, along with file drafting, e-copy conversion, and submission through the US Agent service. Few manufacturers opt for Q submission before final submission.
Role of I3CGlobal Consultants
As a prominent FDA 510k Consultants on a global scale, we have gained the trust of more than 350 plus manufacturers and specification developers. Our team consists of highly skilled subject-matter experts, assuring timely file preparation for 510(k) clearance irrespective of the manufacturer’s size or the regulatory knowledge of their internal team.
With an impressive 85% success rate, a track record of over 350+ clearances worldwide, and a history of serving more than 150+ manufacturers and specification developers since 1999, we proudly stand out from others in terms of quality and service cost.
Our dedication goes beyond mere verbal or email communication; we painstakingly assemble the complete files on behalf of our clients and take full responsibility until the 510k approval is obtained.
F
DA 510k Predicate Device
The term Predicate Device refers to a FDA 510k or PMA-cleared and legally marketed device in the USA with the same (a) intended use, (b) indications for use, and (c) similar technological characteristics as the device in question. It is crucial to note that the predicate device must be a single unit, if possible, and currently available in the USA market without any product recalls in the past years.
Substantial Equivalence Definition
It is a must to demonstrate substantial equivalence to a legally US-marketed device with similar intended use. Proving substantial equivalence to the reference device affirms that the subject device is as safe and effective as the predicate device. The key criteria for determining Substantial Equivalence include establishing similarity are the following, but are not limited to
Intended use,
Design,
Safety,
Adherence to standards,
Labelling,
Biological Compatibility,
Performance characteristics,
Materials used in the construction/ chemical composition,
Manufacturing Methods,
FDA 510k Predicate Device
The term Predicate Device refers to a FDA 510k or PMA-cleared and legally marketed device in the USA with the same (a) intended use, (b) indications for use, and (c) similar technological characteristics as the device in question. It is crucial to note that the predicate device must be a single unit, if possible, and currently available in the USA market without any product recalls in the past years.
Substantial Equivalence Definition
It is a must to demonstrate substantial equivalence to a legally US-marketed device with similar intended use. Proving substantial equivalence to the reference device affirms that the subject device is as safe and effective as the predicate device. The key criteria for determining Substantial Equivalence include establishing similarity are the following, but are not limited to
Intended use,
Design,
Safety,
Adherence to standards,
Labelling,
Biological Compatibility,
Performance characteristics,
Materials used in the construction/ chemical composition,
Manufacturing Methods,
Get more Information : https://www.i3cglobal.com/fda-510k/
0 notes
Text
Medical Billing and Coding: Streamlining Healthcare Administration
In the ever-evolving landscape of healthcare, efficient administration is paramount to ensuring quality patient care and financial sustainability. Medical billing and coding play a crucial role in this endeavor, acting as the backbone of revenue cycle management and facilitating seamless communication between healthcare providers, payers, and patients.
At its core, medical billing and coding involve the translation of medical services rendered into standardized codes that insurance companies and government programs can easily interpret. This process not only ensures accurate reimbursement for healthcare providers but also promotes transparency and accountability within the healthcare system.
The Importance of Accuracy
Accurate medical coding Services is essential for several reasons. First and foremost, it safeguards against fraudulent billing practices and ensures compliance with regulatory guidelines. By precisely documenting every procedure, treatment, and diagnosis, healthcare providers can maintain a comprehensive record of patient care, which is vital for quality assurance and legal purposes.
Moreover, accurate coding is the key to maximizing reimbursements from insurance companies and government programs. Incorrect or incomplete coding can lead to claim denials, payment delays, and financial losses for healthcare providers. In an industry where every penny counts, the significance of precise coding cannot be overstated.
Streamlining the Process
Traditionally, medical billing and coding have been labor-intensive processes, requiring skilled professionals to meticulously review and interpret medical records. However, technological advancements have revolutionized this field, introducing innovative solutions that streamline and automate various aspects of the billing and coding workflow.
Electronic Health Records (EHRs) software have become indispensable tools for healthcare providers. These systems not only facilitate the seamless integration of patient data but also offer advanced coding capabilities, reducing the likelihood of errors and increasing efficiency.
Furthermore, artificial intelligence (AI) and machine learning algorithms are being increasingly employed to enhance coding accuracy and consistency. By analyzing vast datasets of medical records and coding patterns, these cutting-edge technologies can identify potential coding discrepancies and suggest appropriate codes, thereby reducing the workload on human coders and minimizing the risk of errors.
The best Medical Billing And Coding Consultant for your business
Are you looking for the best medical billing and coding services in USA? Medi Claim Management is the answer for your question. As a leading provider in the healthcare revenue cycle management space, we offer comprehensive and innovative solutions tailored to your practice's needs. Whether you require experienced and certified medical coders to ensure accurate claim submissions or state-of-the-art billing software to automate and optimize your processes, our team is prepared to deliver exceptional services that streamline your healthcare administration. With a deep understanding of the intricacies involved in medical billing and coding, we are committed to maximizing your reimbursements while maintaining compliance with ever-evolving regulations. TrustMedi Claim Managements as your preferred partner and experience the difference our cutting-edge solutions can make in transforming your medical billing and coding operations.
#medical bias#medical billing agency#medical billing and coding#medical billing and credentialing services#medical billing call answering#medical billing outsourcing#medical billing appointment#medical billing company#medical billing providers#medical billing for dermatology
1 note
·
View note
Text
Global Top 5 Companies Accounted for 85% of total Dynamic Random Access Memory (DRAM) market (QYResearch, 2021)
Dynamic random access memory (DRAM) is a type of semiconductor memory that is typically used for the data or program code needed by a computer processor to function.
Dynamic random access memory, or DRAM, is a specific type of random access memory that allows for higher densities at a lower cost.

According to the new market research report “Global Dynamic Random Access Memory (DRAM) Market Report 2023-2029”, published by QYResearch, the global Dynamic Random Access Memory (DRAM) market size is projected to reach USD 146.64 billion by 2029, at a CAGR of 10.0% during the forecast period.
Figure. Global Dynamic Random Access Memory (DRAM) Market Size (US$ Million), 2018-2029
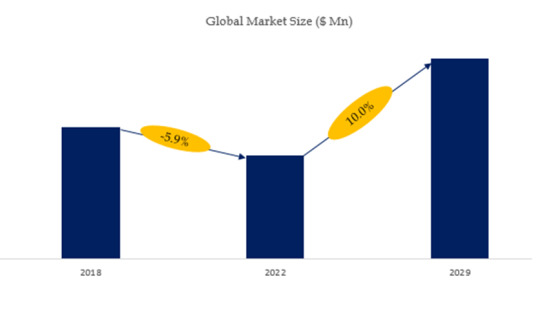
Figure. Global Dynamic Random Access Memory (DRAM) Top 5 Players Ranking and Market Share(Based on data of 2021, Continually updated)

The global key manufacturers of Dynamic Random Access Memory (DRAM) include Samsung Electronics Co. Ltd., SK Hynix Inc., Micron Technology Inc., Nanya Technology Corporation, Winbond Electronics Corporation, Company 6, Company 7, Company 8, Company 9, Company 10, etc. In 2021, the global top five players had a share approximately 85.0% in terms of revenue.
About QYResearch
QYResearch founded in California, USA in 2007.It is a leading global market research and consulting company. With over 16 years’ experience and professional research team in various cities over the world QY Research focuses on management consulting, database and seminar services, IPO consulting, industry chain research and customized research to help our clients in providing non-linear revenue model and make them successful. We are globally recognized for our expansive portfolio of services, good corporate citizenship, and our strong commitment to sustainability. Up to now, we have cooperated with more than 60,000 clients across five continents. Let’s work closely with you and build a bold and better future.
QYResearch is a world-renowned large-scale consulting company. The industry covers various high-tech industry chain market segments, spanning the semiconductor industry chain (semiconductor equipment and parts, semiconductor materials, ICs, Foundry, packaging and testing, discrete devices, sensors, optoelectronic devices), photovoltaic industry chain (equipment, cells, modules, auxiliary material brackets, inverters, power station terminals), new energy automobile industry chain (batteries and materials, auto parts, batteries, motors, electronic control, automotive semiconductors, etc.), communication industry chain (communication system equipment, terminal equipment, electronic components, RF front-end, optical modules, 4G/5G/6G, broadband, IoT, digital economy, AI), advanced materials industry Chain (metal materials, polymer materials, ceramic materials, nano materials, etc.), machinery manufacturing industry chain (CNC machine tools, construction machinery, electrical machinery, 3C automation, industrial robots, lasers, industrial control, drones), food, beverages and pharmaceuticals, medical equipment, agriculture, etc.
For more information, please contact the following e-mail address:
Email: [email protected]
Website: https://www.qyresearch.com
0 notes
Text
EHR Database and Data Management Database Management Approach The issue to address is the negative effects of drugs. Adverse reaction to drugs is "a significantly unpleasant or dangerous response caused by an intervention that is linked with using some kind of medicine, which predicts danger from future usage and assures prevention or a particular kind of treatment, a dosage regimen modification, or withdrawing from the drug" (Edwards & Aronson, 2000). Description of the patient problem ADRs (Adverse Drug Reaction) are among the top mortality and morbidity causes in medical care. On January 2000, the Medicine Institute stated that between 44,000 and 98,000 mortalities take place each year due to health care errors (Committee on Quality of Health Care in America (Institute of Medicine), 2000). ADRs caused around 7000 mortalities out of the stated total. Keep in mind that in America, job related injuries cause around 6000 annual mortalities. The next question to ask should be, how much does it cost medical care due to such negative reactions to drugs? Again, there are methodological constraints that make it difficult for estimates to be completely accurate. However, one annual cost estimate with regard to drug-caused mortality and morbidity is $136 billion, which amounts to more than USA's diabetic and cardiovascular care costs combined. Furthermore, a fifth of the annual mortalities and injuries among patients who have been hospitalized are likely to be due to negative reactions to drugs. In conclusion, there is twice the average time of stay, mortality rate and expenses among hospitalized patients afflicted with negative reactions to drugs, in comparison to those without ADRs within a control patient group. Current publications indicate that several ADRs are detectible and preventable by means of systems help. For instance, several medical systems have established new technologies for ensuring minimal patient injury caused by interactions of drugs and health care errors. Tools such as computerized prescription entry and doctor order as well as systems for bar coding have brought about significant benefits. It has been acknowledged that there is great potential for reducing medication errors through computerized health records and software for medicine-interaction screening that informs pharmacists and doctors of severe medicine interactions (FDA.gov, 2016). Management: The Electronic Health Record (EHR). The record should indicate the history of a patient's medical condition, and other medical care providers should be able to access it in order to be aware of the health problems or concerns of a patient. The records of every patient, whether or not they have been seen, need to include a significant and focused medical history, a documented evaluation and a suitable focused physical diagnosis; if it is indicated, with a provisional exam; also if indicated as well as, a management strategy (CPSO, 2012). Thus, this information includes: • Identification details of the patient (name, contact number, OHIP (?) number, address); Comment by GL: Full name • Personal information and family details (job, habits, life events, family health history); • Previous medical history (previous critical illnesses, surgeries, genetic history, accidents); • Risk aspects; • Drug reactions and allergies; • Current medical conditions (diagnoses, problems, onset date); • Health protection (yearly diagnoses, vaccinations, disease monitoring, e.g., bone density, colonoscopy, mammogram); • Names of consultants; • Long-term health care (current drugs, frequency, dosage); • Major exams; • Emergency contact. These details should be filled out the first time or second time a medical care provider meets a patient, and it should be seen clearly in the record of the patient for easy reference and access. Nonetheless, doctors should start to keep patient CPPs (?) in a practice that exists, even in places where this practice is new. Many EMRs (Electronic Medical Records) will routinely compile patient details in CPPs while it is put down on other parts of the patients' records. Comment by GL: Full name Doctors need to read through the CPP contents during every consultation and reread the details subsequently. This is similarly significant for doctors that use EMRs. Frequent rereading and review is especially significant where doctors need to forward the details to such third parties as ERs, health consultants, insurance companies as well as lawyers. In such cases, doctors need to make sure they forward up-to-date and accurate details (CPSO, 2012). Other details that are normally indicated in EHRs for hospitalized patients are; They can be recognized by those patients who might have experienced ADE (?) within 24-hour surveillance of signals by patients." These signals, which are regularly put down in health records, show the possibility that there may have been an ADE: Comment by GL: Full-form, please • Change in heart rate, hearing, breathing rate, or mental condition. • Specific lab results, low or high levels of blood of specific, wrong drug dosage for a patient's weight or age as well as chemist's medical recommendations for treating an allergic reaction. A virtual alert system installed in a regional Heath Centre known as Good Samaritan was meant for identifying and informing medical care provider of ADEs and errors in prescription. Details included in the database are the patient's lab results, radiology orders, pharmacy orders, medicine allergies, as well as demographic factors (Raschke, Collihare, & Wunderlich, 1998). EHR-Supplied Data: Structured or Unstructured The easiest data type to identify and classify within a computer database is structured data. A class of this kind of data, accounting data, entails numerals in a specified value, entered in a specific column. The use of structured type of data in medical care would involve patient demographic and lab value information, which is entered using a radio button or drop box. This kind of data is unswerving and is used in pre-defined parts of a record. Unstructured data, on the other hand, is unorganized. It may also be vague and full of errors, and usually, 'text-heavy'. Health IT, a type of this form of data, includes a paragraph on the patient's illness history. The doctors' evaluations and patients' complaints are difficult to compress into a sequence of radio buttons as well as checkboxes, while it is greatly important that patient details are evaluated without the trouble of free text management. It is important to find out pertinent details regarding a heart procedure indicated on the doctor's note. This should be regardless of whether or not the information was put down on the structured information of the list of problems. Most of the information that is given by EHR about ADR is in unstructured form. The details included are: • Patient identification details (name, contact number, OHIP number, address); This information is used in identifying a patient. Matching the patient to the intended medication is a routine every health care setting follows. Safety hazards for patients take place when the patient is matched with the wrong treatment, whether supportive, therapeutic or diagnostic care. The data is well structured within the EHR. • Medical History This data is slightly structured since it has a lot of text, which is difficult to fill out or collect from check boxes. • Risk aspects; • Medicine reactions or allergies; It is structured and easy to select. There are numerous electronic health platforms for cataloging such details. Since this data is easy to select, it can be easily put down on EHR. • Current health conditions (diagnoses, problems, onset date); This data takes both unstructured and structured form. It takes the structured form when existing problems can be selected from a record and used in determining appropriate prescription. the unstructured form appears when the future state is difficult to list and describe. • Health maintenance (yearly diagnoses, vaccinations, disease monitoring such as bone density, mammogram, colonoscopy); Most information is given numerically; making it easy to manage and determine. • Names of consultants; long-term treatment (current drugs, frequency, dosage; Major exams; Emergency contact. The name of the consultant has few characters, which makes it structured. Information on long-term treatment takes both the unstructured and structured form. Current drugs information is structured; it indicates the patient's current treatment, which is easy to determine and review in a record. The information on dosage shows the method/procedure of ingesting the prescribed drugs, as well as the frequency. This can be picked out from a record. The details entail the method, timing, and how many times to take the drug in a day. Emergency contact details have the same structure and method of handling as the consultant's name. The details on current medication are of great significance in the negative drug reaction problem since any details that are left out or wrongly put down can affect the patient greatly. This part of EHR will have many information integrity certifiers and surveillance/confirmations to make sure the information put down is right. Description of data relationships that apply to the hypothetical database Medicine exposure in EHR is identified using either administration or prescription information, through ATC (?) codes. Recommendations with similar ATC codes; and different prescription dates for different drugs are put into one drug-use episode, beginning with the preceding recommendation, and the final recommendation, last. Concomitant drug administration periods were identified as distinct episodes. The only drug exposure considered is the current one; within a month of the event in question (Hui, Vaillancourt, Bair, Wong, & King, 2016). Comment by GL: Full form The consistency and accuracy of documenting ADR within the basic documentation system of a hospital should be assessed by comparison of the type and number of ADR cases within every system. Documentation of ADR will be restored from three single medical record systems for documentation: paper charts together with an HER (?) for a hospitalized patient with only allied health and nursing documentation, the chemist system as well as EHR system for ambulances. Comment by GL: Full form References Committee on Quality of Health Care in America (Institute of Medicine). (2000). To err is human: building a safer health system. Washington, D.C.:: National Academy Press. CPSO. (2012, May). Medical Records. Retrieved from The College of Physicians and Surgeons of Onatario: http://www.cpso.on.ca/policies-publications/policy/medical-records Edwards, I., & Aronson, J. (2000). Adverse drug reactions: definitions, diagnosis, and management. Lancet, 356(9237), 1255-9. FDA.gov. (2016, March 14). Preventable Adverse Drug Reactions: A Focus on Drug Interactions. Retrieved from U.S. Food and Drug Administration: http://www.fda.gov/Drugs/Developmentapprovalprocess/Developmentresources/Druginteractionslabeling/ucm110632.htm Hui, C., Vaillancourt, R., Bair, L., Wong, E., & King, J. W. (2016). Accuracy of Adverse Drug Reaction Documentation upon Implementation of an Ambulatory Electronic Health Record System. Drugs Real World Outcomes, 3(2), 231 -- 238. Raschke, R., Collihare, B., & Wunderlich, T. (1998). A computer alert system to prevent injury from adverse drug events. JAMA, 280(15), 1317-20. Read the full article
0 notes
Text
Unparalled CX: It's Not Magic, It's SAP CX Suite
In the digital age, where customer expectations are soaring sky-high, businesses are ardently seeking solutions that not only meet but exceed these expectations, crafting a customer journey that’s seamless, personalized, and memorable. This is where Spadoom, your Swiss SAP Gold Partner, steps into the limelight, offering impeccable SAP Service Cloud Solutions that are not merely about meeting needs but about architecting customer journeys that tell a story, your story.
SAP CX Suite – A Symphony of Exceptional Customer Experiences
SAP Customer Experience (CX) Suite is not just a tool; it’s a strategy, a methodology that propels your business into the future by intelligently connecting every facet of your organization to your customers in real-time. It’s about creating experiences that resonate, that understand the customer even before they know what they want. From e-commerce solutions that enable you to launch innovative business models to customer service solutions that ensure your brand promise is always upheld, SAP CX Suite is your ticket to a world where every customer interaction is not a transaction but a meaningful connection.
Dive Deeper into the SAP CX Suite
The SAP CX Suite is a comprehensive solution that encompasses various components, each designed to enhance a specific facet of the customer experience:
SAP Commerce Cloud: This component ensures your e-commerce platforms are not just transactional but experiential, offering personalized shopping experiences that are seamless and engaging.
SAP Marketing Cloud: It empowers your marketing campaigns, ensuring that your communication is not just heard but resonates, creating a brand image that’s not just seen but remembered.
SAP Sales Cloud: This is where your sales strategy transforms, ensuring that every lead, every potential is not just identified but nurtured, ensuring that your sales teams are not just closing deals but opening relationships.
SAP Service Cloud: This ensures that your customer service is not just about resolving queries but about anticipating them, ensuring that support is not just provided but personalized.
SAP Customer Data Cloud: This component ensures that every byte of customer data is not just stored but utilized, ensuring that every interaction is not just data-driven but insight-driven.
Spadoom – Your Navigator in the SAP CX Odyssey
Spadoom, with its offices spanning across Switzerland, Germany, Italy, India, and the USA, is not just a service provider; we are your partners in this journey towards customer experience excellence. Our expertise in SAP implementation, especially in SAP CX, is not just about technology implementation but about weaving technology into the very fabric of your organizational strategy, ensuring that every byte of data, every line of code, is aligned with your vision, your promise to your customers.
Why Spadoom?
Our niche in SAP implementation, particularly SAP CX, is backed by a robust digital strategy, cloud consulting, operations excellence, Azure implementation, and custom software development solutions that cater to a myriad of industries including Automotive, Consumer Goods, Medical, Chemical, Industrial Equipment, and Retail. Our mission is to be the catalyst that accelerates your digital transformation journey, ensuring that every touchpoint, every interaction that your customers have with your brand, is not just satisfying but enchanting.
Elevate Your E-Commerce with Spadoom
In the realm of e-commerce, where the digital storefront is your first and most crucial interaction point with your customers, Spadoom ensures that your SAP Commerce Cloud is not just a platform but an experience. From migrating your SAP Commerce Cloud installations from On-Premise to the Cloud to ensuring readiness for the SAP Business Technology Platform (BTP), our services are designed to ensure that your online storefront is not just a place to buy but a place to experience, to belong.
Customer Service that Resonates
With Spadoom’s expertise in SAP Service Cloud, your customer service transcends from being a support function to being a customer success platform, ensuring that every issue is not just resolved but is an opportunity to wow your customers, to show them that they are heard, valued, and cherished.
Your Success, Our Promise
At Spadoom, your success is our success, your customers are our customers, and your promises are our promises. Let’s embark on this journey towards unparalleled customer experiences, towards crafting stories that will be told across platforms, across generations. Connect with Spadoom, and let’s create not just satisfied customers, but fans, advocates, and ambassadors for your brand.
Ready to redefine customer experiences? Connect with Spadoom and let’s create the future, today!
1 note
·
View note
Text
Top 5 Career-Defining Courses To Study In USA

Embarking on a journey toward academic excellence and career advancement often begins with choosing the right course. In the realm of possibilities, the United States stands out as a hub for diverse and career-defining education. Here, we unveil the top 5 courses that you can study in USA to shape your future and elevate your career prospects.
1. Computer Science: Mastering The Digital Frontier
In the digital age, the demand for computer science professionals has reached unprecedented heights. From artificial intelligence to cybersecurity, studying Computer Science in the USA opens doors to cutting-edge technologies and lucrative career paths. Dive into the world of coding, algorithms, and innovation to become a sought-after tech wizard.
2. Business Administration: Navigating The Corporate Landscape
For those with a flair for leadership and strategic thinking, a Business Administration course in the USA is a game-changer. Learn the ropes of management, finance, and entrepreneurship, and gain insights from industry experts. Whether you aspire to lead multinational corporations or launch your startup, this course sets the stage for success.
3. Medicine and Healthcare: Healing Minds and Bodies
Aspiring doctors and healthcare professionals find their calling in the USA's world-renowned medical education system. Immerse yourself in state-of-the-art facilities, collaborate with top medical minds, and pave the way for a rewarding career in healthcare. The USA's commitment to medical innovation ensures you stay at the forefront of advancements in the field.
4. Data Science: Unraveling Insights in a Data-Driven World
In an era dominated by data, becoming a Data Scientist is a passport to success. Study Data Science in the USA to master the art of interpreting complex data sets, deriving insights, and influencing key decisions. Equip yourself with skills in machine learning, data analytics, and statistical modeling to thrive in a data-centric professional landscape.
5. Environmental Science: Championing Sustainability
With environmental concerns taking center stage globally, a course in Environmental Science positions you as a catalyst for change. Study in the USA to explore sustainable practices, conservation efforts, and policy-making strategies. Become an advocate for the planet and contribute to a greener, more sustainable future.
Also Read: [Best Destinations to Study Abroad]
Final Words
As you embark on the exciting journey of choosing a career-defining course in the USA, don't navigate this path alone. Nationwide Overseas Education, your trusted student consultant in Ahmedabad, is here to guide you. Our expertise extends beyond borders, ensuring that your academic aspirations align seamlessly with your career goals. Let Nationwide be your compass, steering you toward educational excellence and unparalleled success. Your transformative journey starts here, with Nationwide as your dedicated companion.
0 notes