#medical coding outsourcing services
Text
With ever-changing Coding regulations and Specialty based updates; Quality coding can be challenging!

ecare understands these Medical Coding specifications and delivers quality claims on time. Coding can be the most challenging part in RCM unless you leverage on top expertise such as ecare for best services. To know more visit : https://www.ecareindia.com/medical-coding-services.html
0 notes
Text
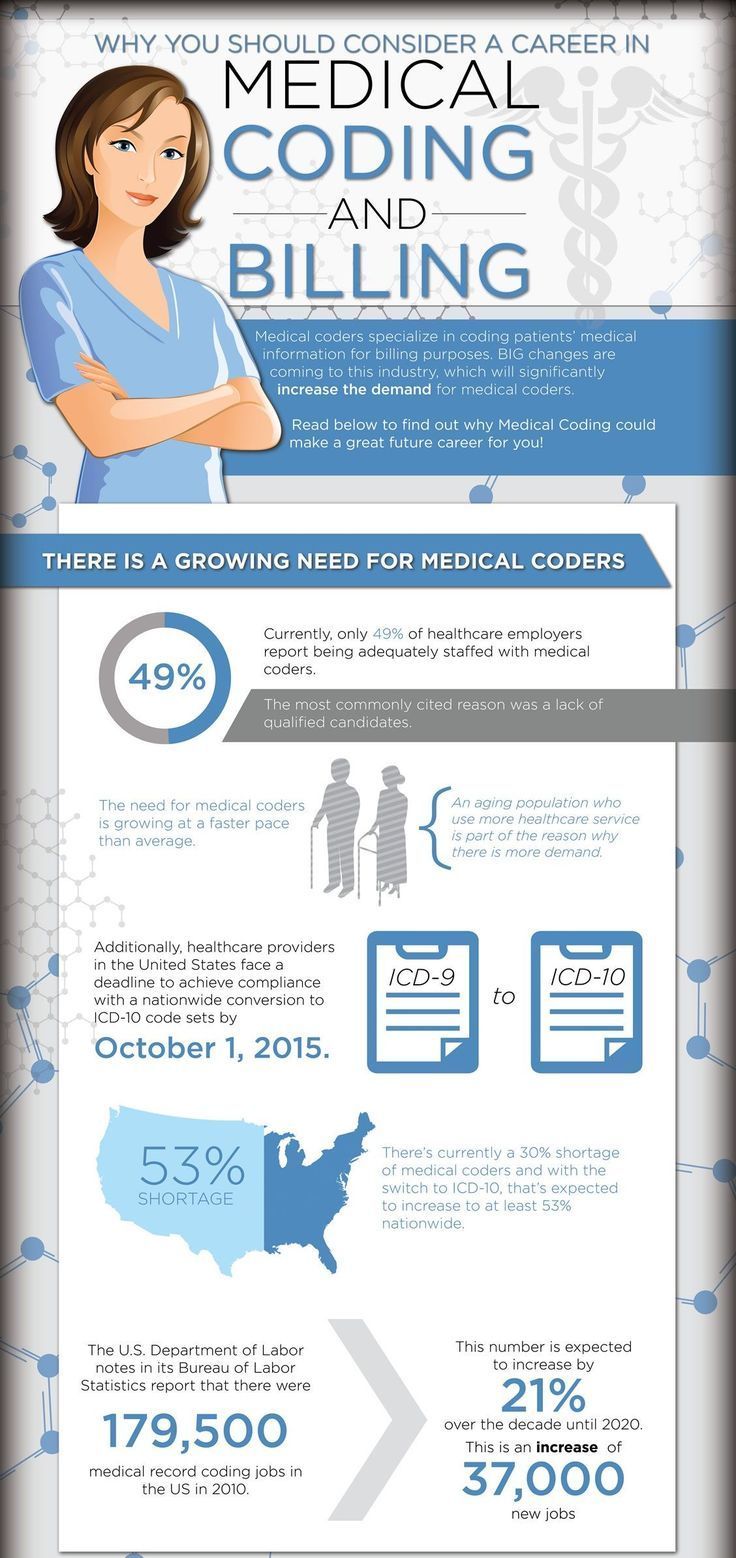
The Role of Medical Coding in Medical Research and Analysis
Source Link: https://theomnibuzz.com/the-role-of-medical-coding-in-medical-research-and-analysis/
In the intricate tapestry of the healthcare landscape, medical coding stands as the linchpin that connects disparate elements into a coherent and actionable whole. It serves as the language that harmonizes the diverse symphony of patient diagnoses, clinical procedures, and treatments, converting…

View On WordPress
#Medical coding#medical coding in medical research#medical coding outsourcing services#Medical Coding Services
0 notes
Link
Get the best medical billing and coding outsourcing services from ecare india. they provides medical billing services more than 20 years.
0 notes
Text
#offshore medical coding#temporary pacemaker cpt code#hierarchical condition category coding#clinical documentation services#anemia coding guidelines#cdi revenue cycle#international medical coding#subsequent vs sequela coding#outsource medical coding services#icd 10 solutions#medical coding outsourcing services#healthcare coding solutions#medical coding solutions#clinical documentation improvement solutions#denial claims#denials in medical billing#clinical documentation solutions#offshore medical billing services#hcc coding guidelines#clinical coding solutions#medical coding outsourcing#outsource medical coding#medical coding services#sdoh coding#offshore medical billing#revenue cycle management strategies#coding and reimbursement social determinants of health#medical coding outsourcing companies#medical billing revenue cycle#healthcare revenue cycle
0 notes
Text
CPC COACHING CENTERS IN HYDRERABAD
Thought Flows Academy, revolutionizing medical coding education since 2016, is the preferred destination in Hyderabad. As the top medical coding training institute, our 20,000 success stories and advanced CPC coaching centers make us the epitome of success in south India. Join our 6-year legacy of shaping skilled professionals and unlocking endless opportunities.
#medical billing agencies near me#medical billing outsourcing#medical billing services#medical billing service provider#medical billing company#medical coding#medical billing solutions#medical billing and coding#medical billing software#medical bill
2 notes
·
View notes
Text
Maximizing Reimbursement with CPT Codes
Reimbursement of healthcare services is an easy method of putting CPT codes on claim forms. In reality, it is a complex matter and requires a team approach to accomplish timely filing to receive accurate and fair reimbursement. CPT (Current Procedural Terminology) codes are commonly used in the medical profession to report medical services, procedures, and services of healthcare professionals. These codes play a crucial role in determining reimbursement from insurance companies. CPT (Current Procedural Terminology) codes are critical factors in maximizing reimbursement. The article will discuss some tips that help to optimize reimbursement with the CPT (Current Procedural Terminology) codes. Read More…
For further details and daily updates, Follow us on LinkedIn or Visit.
#medical billing outsourcing#medical billing service companies#healthcare#medical billing solutions#hospital#medical billing florida#physician#cardiology#cpt codes
3 notes
·
View notes
Text
Practice Management System in Medical Billing
Introduction to Practice Management Systems (PMS)
In the constantly evolving health care landscape, Practice Management System (PMS) are becoming vital tools for medical establishments of all dimensions. They are designed to facilitate administrative and clinical workflows in order to improve efficiency and enhance the quality of healthcare for patients. By integrating various functions, such as billing time, reports, and scheduling an efficient PMS, it is certain that medical practices operate effectively and profitably.
The Role of Practice Management Systems in Medical Billing
It's a complex procedure that requires attention to the smallest of things. A medical practice management system plays an integral part in this process by automating various aspects of managing revenues and billing. Here are some of the methods that practice management systems can assist in medical billing:
Automating Billing Processes:
A PMS is a tool that can automate the entire process of billing, beginning with charge capture, and finishing with the submission of claims. This reduces the risk of making mistakes and helps ensure that claims are filed in time. This system handles both electronic guidance on remittances (ERA) in addition to electronic transfer of funds (EFT) which benefit simplify the billing process.
Claims Management:
Controlling claims is one the most crucial aspects of billing for medical services. A PMS monitors claims over their entire life-cycle and provides real-time updates on their status. This transparency enables practices to recognize and fix issues quickly this reduces amount of time needed to be paid.
Revenue Cycle Management:
A complete PMS includes features to support the Revenue Cycle Management (RCM) which covers all administrative and clinical tasks which aid in the management collection and collection of revenues from services. This includes registration of patients, the verification of insurance, the capture details of the claim submission process, payment posting and follow-up following denial of claims.
Analytics and Reporting:
Effective medical billing requires access to exact reports and information. PMS provides customizable reports that give insights on the results of important indicators (KPIs) such as the rate of denials for claims, the dates of the account receivable (AR) and also overall performance. The data provided by PMS can benefit practices make informed decisions and rise the process of billing.
Benefits of Using a Practice Management System:
The utilization of the system for managing practices can bring many benefits to medical practice. Here are some of the best advantages:
Increased Efficiency: By automating repetitive tasks and providing a central system for managing different administrative tasks, the PMS dramatically improves the efficiency of medical procedures. The staff is able to concentrate on providing care for patients instead of being held back by administrative duties.
Improved Accuracy: Automation reduces the possibility of human errors in the fields of billing and coding. Both are the most common reasons for denials of claims and delays in payment. A PMS ensures that the data it enters is accurate and consistent, which results in fewer rejections of claims and quicker reimbursements.
Enhanced Patient Experience: An efficient system for managing your practice can improve the patient's experience by decreasing the time it takes to wait, making sure you are able to provide an accurate bill, and allowing them to access your medical records. This could result in greater levels of loyalty and satisfaction from patients.
Regulatory Compliance: Maintaining a steady pace with the ever-changing rules and regulations in the healthcare industry can be a challenge. A PMS can assure that practices adhere to the guidelines of HIPAA by ensuring that information is safe and transmitted. It also assists in the creation of reports to conduct compliance audits.
Key Features of an Effective Practice Management System:
When selecting the best practice management system, it is important to consider features that will meet the needs of your business. Here are some of the main elements to be considered:
Simple scheduling tools that can be utilized to improve the efficiency of appointments, decrease no-shows, and maximize the time providers spend. Options like automated reminders, online bookings, and online appointments can improve the effectiveness of scheduling.
A PMS should make registration procedures easier for patients by capturing all of the necessary details regarding the insurance plan and other demographics. The information must be accessible and editable in order to ensure its accuracy.
The capability to confirm insurance coverage in real time can significantly reduce the risk of claims being rejected because of eligibility issues. This feature allows staff to confirm the benefits and coverage prior to the patient's appointment and warrant that the entire range of services can be covered.
Integrating billing as well as coding features ensures that each service is properly documented and invoiced. This includes support for ICD-10, CPT, and HCPCS codes, in addition to automated coding suggestions based on the clinical data provided.
A PMS with claims-scrubbing features automatically checks claims for errors prior to submission. This decreases the number of claims that are rejected and speeds up the payment process.
Electronic Health Records (EHR) is a system that integrates patient documentation as well as billing and clinical information that is accessible through integrated software. This integration enhances workflow efficiency and the quality of care for patients.
A patient portal enhances communication between doctors and patients. It allows patients to gain access to the medical records of their loved ones, book appointments, and communicate securely with their health care providers.
Conclusion
Practice Management Systems is an essential instrument in contemporary medical practice. It has many advantages that boost efficiency, quality and satisfaction. By streamlining and automating of administrative and billing processes, healthcare professionals are able to focus on what's essential to providing the best patient care. The selection of the best PMS requires a thorough analysis of your practice's needs in addition to assessing whether the legitimacy of the company and ensuring that the system integrates with your current processes.
#Medical billing#practice management software#pms#medical billing outsourcing#medical billing and coding#medical billing services#medical billing company
0 notes
Text
What are the CDT Coding Changes in 2024?
The 2024 CDT Code updates are here. Submitting dental claims using the latest CDT codes is essential to prevent denials. Staying up-to-date with coding changes is easy with expert support – reach out to an experienced dental billing company to incorporate the latest CDT coding updates where appropriate, and improve billing efficiency and patient satisfaction. https://www.outsourcestrategies.com/blog/cdt-code-changes-2024/

0 notes
Text
#Neurology Billing Services#Neurology Billing Services in US#outsourced Neurology Billing Services#neurology billing company#neurology medical billing Services#Neurology Billing specialist#neurology billing codes#neurology coding and billing#neurology medical coding
0 notes
Text
Optimizing Healthcare Administration: The Vital Role of Medical Billing and Coding
In the dynamic landscape of healthcare, efficient administration is essential for ensuring quality patient care and financial stability. Medical billing and coding play a pivotal role in this context, serving as the backbone of revenue cycle management and facilitating clear communication between healthcare providers, payers, and patients.
The Fundamentals of Medical Billing and Coding
Medical billing and coding involve translating medical services provided into standardized codes that insurance companies and government programs can easily interpret. This process ensures accurate reimbursement for healthcare providers and promotes transparency and accountability within the healthcare system.
The Importance of Accuracy in Medical Coding
Medical billing software is critical for several reasons. Firstly, it protects against fraudulent billing practices and ensures compliance with regulatory guidelines. By precisely documenting every procedure, treatment, and diagnosis, healthcare providers can maintain a comprehensive record of patient care, which is vital for quality assurance and legal purposes.
Moreover, precise coding maximizes reimbursements from insurance companies and government programs. Incorrect or incomplete coding can lead to claim denials, payment delays, and financial losses for healthcare providers. In an industry where financial margins can be thin, the significance of precise coding cannot be overstated.
Technological Advancements in Medical Billing and Coding
Traditionally, medical coding services have been labor-intensive processes, requiring skilled professionals to meticulously review and interpret medical records. However, technological advancements have revolutionized this field, introducing innovative solutions that streamline and automate various aspects of the billing and coding workflow.
Electronic Health Records (EHRs): These systems have become indispensable tools for healthcare providers. EHRs facilitate the seamless integration of patient data and offer advanced coding capabilities, reducing the likelihood of errors and increasing efficiency.
Artificial Intelligence (AI) and Machine Learning:- These technologies are increasingly being employed to enhance coding accuracy and consistency. By analyzing vast datasets of medical records and coding patterns, AI can identify potential coding discrepancies and suggest appropriate codes. This reduces the workload on human coders and minimizes the risk of errors.
Choosing the Right Medical Billing and Coding Service
For healthcare providers seeking to optimize their billing and coding processes, selecting the right service provider is crucial. Medi Claim Management, for instance, offers comprehensive and innovative solutions tailored to the specific needs of healthcare practices.
Medi Claim Management - As a leading provider in the healthcare revenue cycle management space, Medi Claim Management offers a range of services designed to streamline healthcare administration. Whether you need experienced and certified medical coders to ensure accurate claim submissions or state-of-the-art billing software to automate your processes, Medi Claim Management has the expertise and tools to deliver exceptional results.
With a deep understanding of the complexities involved in medical billing and coding, Medi Claim Management is committed to maximizing reimbursements while maintaining compliance with ever-evolving regulations. By choosing Medi Claim Management as your preferred partner, you can experience the benefits of cutting-edge solutions that transform your medical billing and coding operations.
Conclusion
In the ever-evolving landscape of healthcare, the importance of efficient administration cannot be overstated. Revenue cycle management is an essential component of this efficiency, ensuring that healthcare providers receive accurate reimbursements and maintain transparent and accountable practices. With the advent of technological advancements such as EHRs and AI, the process has become more streamlined and accurate, benefiting both providers and patients.
Selecting the right medical billing and coding service, like Medi Claim Management, can further enhance the efficiency and effectiveness of healthcare administration. By leveraging innovative solutions and expert knowledge, healthcare providers can ensure they remain compliant with regulations while maximizing their financial returns.
#medical billing outsourcing#medical bias#medical billing agency#medical billing and coding#medical billing and credentialing services
0 notes
Text
The Importance of Medical Coding in the Healthcare Industry
Source Link: https://articlescad.com/the-importance-of-medical-coding-in-the-healthcare-industry-243134.html
Medical coding, a seemingly inconspicuous aspect of healthcare administration, wields a far-reaching influence on the entire healthcare industry. At its core, medical coding services serves as the bridge between the intricate world of healthcare and the structured realm of data. It…

View On WordPress
#Importance of medical coding#Medical coding#medical coding outsourcing services#Medical Coding Services
0 notes
Text
Mastering Denial Management In Medical Billing
Introduction
The intricate labyrinth of medical billing is frequently hindered by denial management challenges, a crucial facet often underestimated in its potential to undermine healthcare revenue cycles. Mastering denial management is not merely about addressing financial discrepancies; it is about ensuring a seamless flow of care delivery by mitigating interruptions in the billing process. This article delves into the sophisticated strategies and proactive measures necessary to minimize and manage denials effectively, ensuring healthcare providers can maintain a steady stream of revenue while delivering uninterrupted patient care.
Common Causes of Denials
Denials in medical billing often stem from a constellation of preventable errors and oversight. The foremost culprits include lapses in insurance verification, inaccuracies in patient data, coding anomalies, and insufficient documentation. Each of these elements plays a pivotal role in the complex tapestry of billing, where a single error can cascade into financial losses. Understanding these common pitfalls is the first step in crafting robust strategies that enhance accuracy and efficiency in billing processes, thus fortifying the financial backbone of healthcare institutions.
Strategies for Preventing Denials
Preventative strategies are indispensable in the realm of denial management. Instituting rigorous insurance verification processes at the outset ensures coverage clarity and eligibility, thereby precluding a significant fraction of potential denials. Precision in patient information gathering and the implementation of stringent coding audits further fortify the billing process against errors. Additionally, continual education and training of the billing staff act as a bulwark against evolving challenges in healthcare billing, ensuring they remain adept and proactive in their roles.
Effective Denial Resolution Techniques
When denials occur, effective resolution techniques are paramount to recoup lost revenue swiftly. Prioritization of follow-ups on denials, the employment of advanced technology for tracking and managing these denials, and the establishment of clear, open channels of communication with payers are critical. The strategic appeal of denials, backed by thorough documentation and a clear understanding of payer contracts, can significantly enhance the likelihood of overturning unjustified denials, thus safeguarding revenue integrity.
Utilizing Data Analytics in Denial Management
Data analytics offers a panoramic view of denial trends and underlying causatives, empowering healthcare providers with the insights needed to rectify systemic issues in billing processes. By harnessing data to identify patterns and root causes of denials, institutions can implement targeted improvements that not only reduce the incidence of denials but also enhance overall operational efficiency. This proactive approach, driven by analytical insights, is integral to evolving into more resilient healthcare practices.
Collaboration Between Billing and Clinical Teams
Collaboration between billing and clinical teams is critical to enhancing the accuracy of documentation and coding. By fostering robust communication and understanding between these teams, healthcare providers can ensure that clinical documentation accurately reflects the services provided, thereby minimizing denials due to discrepancies. Educational initiatives aimed at clinical staff regarding the implications of their documentation on billing processes can bridge gaps in understanding and streamline the revenue cycle.
Compliance Considerations in Denial Management
Navigating the convoluted waters of regulatory compliance is vital for effective denial management. Staying abreast of the latest regulatory requirements and ensuring that billing practices are compliant not only mitigates the risk of denials but also protects against potential legal repercussions. Regular compliance audits serve as a diagnostic tool to identify and rectify non-conformities in billing practices, thereby fortifying the institution’s adherence to industry standards and regulations.
Outsourcing Denial Management
For some healthcare entities, outsourcing denial management can be a strategic move to leverage specialized expertise and technology. Selecting the right partner—a firm that aligns with the healthcare provider’s values and expectations—can significantly enhance the efficiency of denial management processes. Outsourcing partners can offer advanced analytics, experienced staff, and refined strategies that are sometimes out of reach for in-house teams due to resource constraints.
Conclusion
Mastering denial management in medical billing is a multifaceted endeavor requiring a blend of strategic foresight, operational excellence, and continuous improvement. By understanding the common causes of denials, implementing effective prevention strategies, and utilizing data-driven insights, healthcare providers can significantly enhance their billing efficiencies. The synergy between billing and clinical teams, adherence to compliance standards, and the strategic decision to outsource are all critical components in forging a path to reduced denials and improved financial health.
#invicieq#medical billing services#rcm#revenu cycle management#medical billing outsourcing#medical coding#medical billing
0 notes
Text
#offshore medical coding#temporary pacemaker cpt code#hierarchical condition category coding#clinical documentation services#anemia coding guidelines#cdi revenue cycle#international medical coding#subsequent vs sequela coding#outsource medical coding services#icd 10 solutions#medical coding outsourcing services#healthcare coding solutions#medical coding solutions#clinical documentation improvement solutions#denial claims#denials in medical billing#clinical documentation solutions#offshore medical billing services#hcc coding guidelines#clinical coding solutions#medical coding outsourcing#outsource medical coding#medical coding services#sdoh coding#offshore medical billing#revenue cycle management strategies#coding and reimbursement social determinants of health#medical coding outsourcing companies#medical billing revenue cycle#healthcare revenue cycle
0 notes
Text
Transform Your Revenue Cycle Management: Attain Financial Stability
This Blog was originally published by Unify RCM.
https://www.unifyrcm.com/transform-your-revenue-cycle-management.php
Revenue cycle management remains to be one of the priorities for healthcare providers and practices in 2024.
The constant juggle between offering the best quality of patient care and elevating revenue can be stressful. On the other hand, losing revenue restrains healthcare practices from providing the best that they can.
Together with this, the complexities of medical billing and coding add to the administrative workload. Amidst this, medical billing services act as the crucial aspect to not just enhance revenue but also improve the workflow of operations.
A wholesome combination of professional assistance along with dedicated patient care is all a healthcare practice needs to grow financially.
This blog highlights the concept of revenue cycle management and its importance in the financial success of healthcare practices. It will also put a spotlight on the valuable contribution of medical billing services in uplifting the bottom line.

Explanation of Revenue Cycle Management
Essentially, revenue cycle management is all about implementing control and handling the different steps in medical billing. It's nothing but the management of all administrative work to get adequate cash inflow.
When a healthcare provider or practice successfully fulfills all the requirements, they can achieve financial stability. That is why every step in the process of medical billing needs to be done with precision.
RCM is a collective process where everything is kept in check including the workflow and operational functioning. Combining all aspects, it is dedicated to streamlining medical billing and coding with accuracy and efficiency.
This whole point is narrowed down to prevent errors and mistakes in billing to mitigate the potential risk of revenue leakage
Effective RCM for Financial Upgradation is the Need of the Hour
Healthcare providers and practices need a better and more productive RCM to attain financial upgradation. Whether they will be able to reach their goal is completely a matter of effective medical billing and coding.
Efficient RCM plays a vital role in handling claims, their filing, submission, and processing strategically. It works with complete optimization, progressive technologies, and a proactive approach to realize healthcare practices' full potential.
Additionally, a smooth flow of RCM strengthens the healthcare practice and prepares it to handle the ups and downs in the economy. Comprehensive attention makes the healthcare practice stronger to sustain competition and strive to maintain the quality of care to patients
Revenue Cycle Management in 2024
As the medical billing landscape is expanding, healthcare providers are looking forward to ease of handling administrative tasks. Many efforts have already been made to solve healthcare practices, and it is only the beginning
In 2024, healthcare providers and practices want to indulge in medical billing services where all their hassle is taken care of by experts.
There is a requirement for technologically advanced medical billing and coding solutions for a subsequent reduction in errors and drawbacks.
One more aspect that is gaining attention in 2024 is reporting and analytics to understand the performance of healthcare practices. All in all, healthcare providers and practices want robust strategies to meet financial stability in the dynamic medical billing environment.
Puzzle Pieces of Revenue Cycle Management
We can say that the steps in medical billing are the puzzle pieces of RCM and all of them are crucial. From the first step to the last, every bit of medical billing and coding is necessary to enhance revenue.
Patient Entry
The first step is patient registration, and this happens at the time of appointment. At this initial step itself, major information regarding patients, their insurance, and medical history is recorded. It is the foundational step, and this sets the pace for the coming steps in the process.
Claim Filing
Once the patient receives treatment, the rendered services are translated into accurate codes for claim filing. Coding errors are major mistakes in medical billing and often lead to the maximum number of claim denials
That is why it becomes important to hand over claim filing to professional coders and billers. Providentially, Medical billing services can prevent errors in coding with a persistent team of expert coders
Submission of Claims and Follow-up
After the claims are filed, it is time for claim submission to respective insurance companies for further processing. This step is done right when healthcare providers submit the claims on time and within the due date. Otherwise, the claims get denied and healthcare providers face revenue loss.
After the submission of claims, healthcare providers also need to ensure proper denial management and follow-up. This is essential in case there are denials. Healthcare providers can re-file claims after making some alterations to recover the lost revenue
The follow-up process prevents major reimbursement loss, which is why it must not be neglected or missed.
Revenue Collection
The final and ultimate step is the collection of reimbursement. If healthcare providers have reached this point that means they have successfully handled the medical billing process and revenue cycle management
The Role of Medical Billing Services in Elevating Revenue Cycle Management
Let's explore all the benefits of medical billing services
Financial Upliftment
The major advantage is financial stability, and a proper RCM allows a continuous flow of funds. When there is a reduction in revenue loss, healthcare providers and practices experience noticeable financial upliftment.
Elimination of Administrative Burden
Medical billing services reduce the overall administrative burden by taking complete responsibility for RCM. They employ a team of experts along with advanced technological tools and free healthcare providers from extensive paperwork.
Improvement in Patient Experience
As healthcare providers outsource medical billing services, they get more time to deal with the patients and provide the best quality treatments and procedures. When healthcare providers work with an untroubled mind, there is an improvement in patient experience.
Proactive Decision Making
A medical billing company helps healthcare providers in many ways and one such way is proactive decision making. The professional team fosters data reporting and defines performance so making decisions for the future becomes easy
Such insights help in maximizing revenue and improving revenue cycle management with proper planning and execution.
Compliance with Regulatory Standards
Compliance standards are an unmissable part of medical billing. This is also a factor that keeps altering. Whether it is HIPAA compliance or other coding compliance, outsourcing partners ensure the fulfillment of them all.
This protects healthcare providers from legal action and maintains their reputation among patients and other related individuals.
Expedite Processing of Claims
The direct impact of partnering with well-versed companies is the elimination of medical billing roadblocks. Reduction in errors leads to limited denial of claims which further contributes to speedy claim processing.
This is possible because professional assistance results in accuracy, timeliness, compliance, and adequate revenue
Unify Healthcare Services for Effective Revenue Cycle Management
Expertise and proficiency can improve RCM in so many ways and healthcare providers will bear the fruits. Outsourcing is a one-stop solution to coding complexities, rising claim denials, and revenue leakage
Unify Healthcare Services is a medical billing company in USA that provides complete medical billing and coding services. We have dealt with thousands of healthcare providers and helped them in their journey to achieve a robust RCM.
Our proficient coders and billers offer overall accuracy and never miss any details. Our essential services can deliver what you are looking for.
Choose Unify Healthcare Services and maintain a healthy Revenue Cycle Management!
#medical billing and coding#medical billing services#medical billing outsourcing#hospital#healthcare#dme billing services#hospital billing services
0 notes
Text
Outsourcing Success: How Medical Billing Boosts Practices
In today's fast-paced healthcare industry, efficient medical billing is paramount to the success of any practice. However, managing billing processes in-house can be overwhelming and resource-intensive. This is where medical billing outsourcing becomes a game-changer. By entrusting billing tasks to specialized providers, practices can streamline their revenue cycle management and focus on delivering exceptional patient care.
1. Introduction
The introduction sets the stage for the discussion by highlighting the importance of efficient medical billing practices in today's healthcare landscape. It emphasizes the role of medical billing outsourcing in alleviating the burden on practices and optimizing revenue generation.
2. The Basics of Medical Billing
This section provides a comprehensive overview of medical billing processes, from patient registration to claim submission and payment posting. It underscores the significance of accuracy and compliance in medical billing procedures.
3. Challenges Faced by Medical Practices
Here, we delve into the challenges that medical practices encounter when managing their medical billing in-house. These challenges may include staffing constraints, billing errors, and the need to stay abreast of regulatory changes.
4. The Benefits of Outsourcing Medical Billing
This section explores the myriad benefits of medical billing outsourcing. It highlights how outsourcing can reduce costs, improve efficiency, and enhance revenue generation for practices.
5. Choosing the Right Medical Billing Partner
Selecting the right medical billing partner is crucial for the success of medical billing outsourcing initiatives. This section outlines key considerations for practices when evaluating potential partners, such as experience, technology capabilities, and compliance measures.
6. Maximizing Revenue Through Outsourced Billing
Here, we discuss strategies for maximizing revenue through outsourced medical billing. These strategies may include optimizing coding accuracy, streamlining workflows, and implementing proactive denial management processes.
7. Case Studies: Real-Life Success Stories
Real-life case studies provide tangible examples of practices that have benefited from medical billing outsourcing. These success stories illustrate the positive impact of outsourcing on practice revenue, efficiency, and overall operations.
8. Addressing Common Concerns and Misconceptions
This section addresses common concerns and misconceptions surrounding medical billing outsourcing. It provides reassurance to practices by addressing issues such as data security, confidentiality, and loss of control.
9. The Future of Medical Billing Outsourcing
Looking ahead, this section explores emerging trends and innovations in medical billing outsourcing. It discusses how advancements in technology and changes in healthcare policy may shape the future of outsourced billing services.
10. Conclusion
In conclusion, we summarize the key points discussed in the article and reiterate the benefits of medical billing outsourcing for practices. We emphasize the importance of considering medical billing outsourcing as a strategic investment in the success and sustainability of healthcare practices.
#InvicieQ#medical billing#medical billing outsourcing#medical billing and coding#medical billing services#healthcare
0 notes
Text
Enhancing Healthcare Administration: The Importance of Billing and Coding Services
Healthcare administration is an intricate system dependent on meticulous management practices to provide optimal healthcare delivery. Coding and billing play an essential part in this complex system, providing both financial support and guaranteeing accurate patient records that satisfy regulatory compliance requirements. Here, we explore their significance.
Understanding Medical Billing and Coding:
While healthcare billing and coding may share some similarities, each plays their own special part within their specific environments.
What is Medical Coding?
Medical coding refers to the process of translating diagnoses, procedures, and equipment used by healthcare services or equipment suppliers into universal alphanumeric codes used by any healthcare service or equipment supplier. Coders review patient records carefully so as to assign the most applicable codes for every service provided by hospitals or physicians. Three primary classification systems include the ICD-10 International Classification of Diseases, CPT (current procedural terminology), and the Healthcare Common Procedure Coding System (HCPCS).
Understanding Medical Billing
Medical billing involves filing and tracking claims made to health insurance companies to secure reimbursement for services provided by medical professionals. Billers use codes generated by medical coders to create insurance claims, which they then send on to insurers so that reimbursement can occur.
Medical Billing and Coding Play an Integral Role in Healthcare Administration:
Ensuring Accurate Patient Records: Coding and medical billing play an integral role in creating accurate patient records. Accurate coding helps healthcare professionals make more informed choices regarding treatments while tracking results more closely, while an extensive patient record serves as a constant resource for treatment as well as research projects.
Simplifying Billing: Medical billing and coding have the power to streamline billing procedures and cut errors while simultaneously increasing efficiency. Codified codes enable billers to submit claims quickly without risk of error and fast reimbursement processes for healthcare providers, resulting in faster reimbursement processes with lower administrative burdens on healthcare providers.
Adherence to Regulations: Healthcare providers are subject to stringent regulations regarding documents and claims submission. Medical billing and coding experts ensure their clients comply with these regulations in order to avoid costly penalties from regulatory bodies like HIPAA (Health Insurance Portability and Accountability Law of 1996), while also helping keep patient privacy secure.
Enhancing Revenue Cycle Management: Medical billing and coding are essential to the effective administration of revenue cycles (RCM), including claims management, payments collection and revenue creation. Coding helps ensure health care providers receive prompt payments for services rendered, that helps ensure financial security of healthcare organizations.
Challenges in Medical Billing and Coding
Attracting patients through Medical Billing and Coding. Medical Coding and billing present numerous difficulties to healthcare administration, which may compromise its efficiency.
Coders face an uphill task when it comes to medical coding due to the vast array of codes as well as regular updates made to Coding systems. They must keep abreast of changes while learning constantly in order to ensure accuracy while also avoiding delays in reimbursement or claim denial due to this complexity.
Integrating medical billing systems and codes with other IT platforms for healthcare administration, such as electronic health records (EHRs), is often complex. Yet it remains essential to ensuring patient information moves freely between systems while also decreasing errors and improving efficiency in administration of care.
Healthcare regulations change frequently, which makes medical billing and coding procedures even more complicated. Staying compliant with any new laws requires continuous professional education for billing and coding specialists in order to remain compliant.
Medical billing presents many unique difficulties, with claim rejections and denials frequently happening due to mistakes in coding processes, inadequate documentation or patient data inconsistencies. Denials must be resolved through careful monitoring and ongoing communication between providers and insurers in order to effectively handle rejections and denials.
The Future of Medical Billing and Coding
Medical billing and coding will experience dramatic advancements thanks to technological innovations and ever-evolving healthcare needs.
Artificial Intelligence and Machine Learning:
AI and ML technologies hold great promise in medical billing and coding processes. AI systems can process massive volumes of data quickly with precision while automating mundane tasks while recognising patterns human coders may miss, increasing efficiency and accuracy during billing processes.
Improved Data Analytics:
Data analytics with advanced capabilities provide healthcare professionals with greater insight into codes and billing practices, helping to identify patterns or areas for improvement more easily. They could even offer predictive modeling capabilities so healthcare providers can anticipate potential revenue stream issues before they arise.
Blockchain Technology:
Blockchain is an efficient and secure method of managing transactions within healthcare, including medical bills and codes, through an uncentralized ledger that cannot be altered without prior permission from its creators. Blockchain's decentralized nature reduces fraud while also increasing data security and streamlining billing procedures.
Telehealth Integration:
Telehealth has presented billing and coding professionals with specific challenges when it comes to reimbursement and documentation of online care, reimbursement rates, and documentation accuracy. Adapting to new codes specific to telehealth will require ongoing adaptation in order to guarantee accurate documentation and reimbursement; integration will become ever more vital as more health services become accessible via telehealth.
Conclusion
Medical billing and medical coding are integral components of healthcare administration. They play an integral part in keeping patient records accurate while streamlining billing procedures, optimizing revenue cycle management strategies, meeting regulatory compliance obligations, controlling costs efficiently, and keeping costs at a manageable level. Although they face various barriers that impede their efforts to become efficient in this arena, continual training, technological developments, and efficient communication strategies can help overcome them and move this area towards greater efficiency and accuracy.
#medical billing#medical billing and coding#medical billing outsourcing#medical billing services#medical billing servise in USA#medical billing company
1 note
·
View note