#tocilizumab injection price
Explore tagged Tumblr posts
Text
Actemra Drug Market is driven by Increasing RA Prevalence

The Actemra Drug Market encompasses the development, commercialization, and distribution of tocilizumab-based therapies, primarily targeting rheumatoid arthritis (RA) and other inflammatory disorders. As a biologic immunotherapy, Actemra offers targeted inhibition of the interleukin-6 receptor, delivering rapid symptomatic relief and slowing joint degradation. The product advantages include high specificity, improved patient outcomes, and a favorable safety profile compared to conventional disease-modifying antirheumatic drugs, driving strong adoption among healthcare providers and patients. The growing incidence of autoimmune diseases, coupled with advancements in monoclonal antibody engineering and supportive reimbursement frameworks, underscores the escalating need for effective biologics in treatment regimens.
Ongoing clinical trials exploring Actemra Drug Market efficacy in conditions such as juvenile idiopathic arthritis, giant cell arteritis, and cytokine release syndrome are creating new market segments and revenue streams. The market scope includes both intravenous infusion and subcutaneous injection formulations, catering to diverse patient preferences and inpatient or outpatient settings. Comprehensive market analysis and market research provide critical market insights into prevailing market trends, emerging market opportunities in developing regions, and potential market challenges, including biosimilar competition and pricing pressures. With strategic collaborations among market players, robust R&D investments, and growing awareness of personalized medicine, the market’s future market growth potential remains strong.
The Actemra drug market is estimated to be valued at USD 4.13 Bn in 2025 and is expected to reach USD 7.41 Bn by 2032, growing at a compound annual growth rate (CAGR) of 8.7% from 2025 to 2032. Key Takeaways
Key players operating in the Actemra Drug Market are:
-Hoffmann-La Roche
-Genentech
-Novartis
-Biogen
-Sanofi
These market players hold significant market share due to their strong product portfolios, extensive distribution networks, and robust research capabilities. Hoffmann-La Roche and Genentech lead the market with pioneering clinical trials and high market revenue contributions, while Novartis and Biogen focus on innovative formulations and lifecycle management strategies to maintain market dynamics. Sanofi leverages strategic acquisitions and partnerships to expand its biologics footprint. These market companies continuously invest in clinical research, aiming to enhance efficacy and safety profiles to address unmet clinical needs. Market growth strategies such as targeted marketing, patient support programs, and pricing negotiations have allowed these companies to navigate market restraints and capitalize on evolving market segments. Combined, these key players shape the competitive landscape through product innovation, aggressive market penetration, and strategic collaborations, reinforcing their industry share and driving industry trends across regions. The Actemra Drug Market has witnessed growing demand driven by the rising global incidence of rheumatoid arthritis and other chronic inflammatory conditions, as revealed by recent market research. Increased disease awareness among patients and healthcare professionals has boosted prescription rates, particularly in developed markets where early diagnosis and aggressive treatment approaches are standard practice. Favorable reimbursement policies and the establishment of comprehensive patient assistance programs have reduced cost-related barriers, thereby widening market access. Additionally, the shift toward biologic therapies over traditional small-molecule drugs, supported by positive long-term efficacy and safety data, is contributing to sustained market growth. Emerging market segments such as pediatric rheumatology and off-label indications are also offering new market opportunities, while ongoing educational initiatives are addressing market challenges related to treatment adherence and physician familiarity. These factors collectively underpin the robust expansion in demand across both established and emerging healthcare systems.
‣ Get More Insights On: Actemra Drug Market
‣ Get this Report in Japanese Language: アクテムラ医薬品市場
‣ Get this Report in Korean Language: 악템라의약품시장
0 notes
Text
Rheumatology Revolution: Sarilumab’s $1.1218 B Surge on the Horizon
Sarilumab—the monoclonal antibody that once played second fiddle—is stepping into the limelight, with the global Sarilumab market projected to hit $1.1218 billion by 2035. As physicians demand targeted, high‑efficacy solutions for rheumatoid arthritis and other autoimmune disorders, Sarilumab’s IL‑6 receptor blockade is carving out a premium niche in an increasingly crowded biologics arena.
Breaking New Ground in Autoimmunity
Originally approved for moderate‑to‑severe rheumatoid arthritis, Sarilumab’s next act is expansion into giant cell arteritis, juvenile idiopathic arthritis, and even off‑label trials for cytokine storm syndromes. Its once‑monthly subcutaneous dosing contrasts with bi‑weekly regimens of legacy TNF‑inhibitors, delivering patient‑centric convenience without sacrificing disease control. Real‑world data is stacking up: patients switched from tocilizumab report similar ACR50 response rates but cite fewer injection‑site reactions and improved quality‑of‑life scores.
Market Dynamics & Competitive Edge
Premium Positioning: Despite biosimilar pressure on other biologics, Sarilumab’s patent protection through 2032 buys R&D teams breathing room to refine delivery devices—think auto‑injectors with real‑time dosage feedback.
Payer Partnerships: Value‑based contracting pilots in Europe and the U.S. tie reimbursement to sustained remission rates, aligning payer priorities with patient outcomes and locking in formulary access.
Emerging Regions: Latin America and Asia‑Pacific are growth catalysts. Brazil’s Ministry of Health added Sarilumab to its rheumatoid arthritis protocol in 2029, and China’s National Medical Products Administration granted accelerated review for pediatric indications this year.
Innovation Pipeline & Formulation Advances
Biotech labs aren’t resting on their laurels. Next‑gen Sarilumab variants with half‑life extensions and dual‑mechanism fusions (combining IL‑6R blockade with T‑cell modulation) are in preclinical stages. Lyophilized, room‑temperature stable syringes are slated for launch in 2028, slashing cold‑chain costs and boosting accessibility in resource‑limited settings. Meanwhile, inhalable microsphere formulations—still a moonshot—promise direct lung delivery for COVID‑19–related cytokine storms.
Challenges on the Horizon
No blockbuster sails unchallenged.
Biosimilar Encroachment: As patents begin to expire in certain markets by the early 2030s, Sarilumab must lean into device patents and proprietary auto‑injector designs to maintain premium pricing.
Safety & Long‑Term Data: IL‑6 blockade carries infection and lipid‑profile risks. Ongoing pharmacovigilance studies and real‑world registries will determine whether Sarilumab’s safety profile holds over decades of use.
Market Saturation: With multiple IL‑6 inhibitors and JAK‑inhibitors vying for share, Sarilumab’s brand must stay on point—think high‑touch patient support, digital disease‑management apps, and HCP educational symposia.
The Road Ahead
By 2035, success won’t just be hitting $1.1218 billion—it’ll be about securing Sarilumab’s place as the go‑to IL‑6 agent across indications. Companies that pair clinical innovation with patient‑first delivery systems, data‑driven payer value propositions, and razor‑sharp market access strategies will own rheumatoid arthritis treatment—and beyond.
Source: DataStringConsulting
0 notes
Text
COVID-19 Impact on Dexamethasone on Healthcare Industry | Data Bridge Market Research

COVID-19 Impact on Dexamethasone on Healthcare Industry
OVERVIEW
A novel coronavirus, SARS-CoV-2, appeared in December 2019 in Wuhan, China, spreading much faster than its predecessors and has already infected millions of patients worldwide as of April 19, 2020. As the scope of the current COVID-19 outbreak has reached the proportion of pandemics, major international efforts in public health are underway to control the outbreak. Although the favorable vaccine was discovered to save the patient life, not everyone gets the dose, so there is considerable interest in repeating existing corticosteroid-based drugs against COVID-19. Several many clinical interpretations of the Randomized Evaluation of COVID-19 Therapy were performed to evaluate useful tool whether dexamethasone is useful for the severe hospitalized patients.
Dexamethasone is a corticosteroid widely used or known for its anti-inflammatory and immunosuppressant activity. Dexamethasone exerts its action in decreasing inflammation by suppressing the migration of cells known as polymorph nuclear leukocytes of PMN and reducing capillary permeability. Through this phenomenon, it stabilizes the cell and lysosomal membrane. In premature infants, dexamethasone also stimulates increased surfactant production in the lungs. It also can inhibit pro-inflammatory cytokines and prostaglandin synthesis. Moreover, dexamethasone also suppresses the proliferation of lymphocytes through direct cytolysis and can inhibit mitosis process of cell division.
IMPACT ON PRICE
Various market players face many challenges due to the coming of the novel Coronavirus and different strains. One such issue is the uncertainty surrounding the impact of COVID-19 on dexamethasone demands. Due to the increased demand for life-saving drugs such as Tocilizumab, Remdesivir, Favipiravir, Dexamethasone, and several more for coronavirus treatment and stiff competition between the market players.
According to the reports, countries such as India, the U.K., Spain, and many more face second and third waves of Coronavirus due to a sudden surge in demand, and India already grant the use of dexamethasone for severe patients. It looks like as the severity of the COVID infection increases, the dexamethasone usage is also increasing.
According to the reports, the drug cost in U.K. only costs 5 pounds which are needed for ten days, and for the U.S. the cost of this drug is USD 50. Moreover, according to the Health-e News, the regulated price for the injection in South Africa is between R149. 03, and R176.44.
The impact of COVID-19 does not create any major impact on the price of dexamethasone, although some small or developing countries are facing the issue of pricing.
IMPACT ON DEMAND
The Coronavirus zone is the result of various markets around the world. This is the cause of the widespread closures and isolation that are affecting world economic activity. As the cases increase in April, the sudden surge in demand has seen, and the drug went out of stock.
Patient’s families are in a panic situation due to the limited stock of the injection and the higher price of the drug. The injection being sold at a higher price in the black market. In that particular situation, the government takes over the allocation and supply of injection in the different states of India.
Moreover, as the cases increase, the WHO chief pointed out the need for equitable supplies of dexamethasone for possible use in critical patients worldwide as the demand is rising to save the patients. As the India and U.K. regulatory grant, the emergency use of dexamethasone for severe patients the demand is continuously rising after the second wave of Coronavirus hits different countries. WHO also stated that to meet the rising demand for dexamethasone the production facility or capacity must be increased to meet the global demand.
In June 2020, as the University of Oxford releases the clinical results, they demand dexamethasone increases and the orders for dexamethasone surpassed 2.8 million compared to the 397,500 in the month of May 2020. According to Vizient Inc. one of the largest groups for drug purchasing organizations in U.S. hospitals said that as the Oxford clinical studies results on dexamethasone releases, the demand rose by 167%. Vizient Inc. spoke person also said that after the rising demand drug’s makers have been able to fill only about half of hospital orders on time.
The impact of COVID -19 has created an opportunity for the number of clinical research to cure the diseases or related symptoms. The impact of COVID-19 created a positive impact on the dexamethasone market because a number of regulatory bodies approved the emergency use of the drug, and the strong clinical evidence also supports the usage.
IMPACT ON SUPPLY
As the pandemic intensifies, supply chains can be at significant risk due to over-located locations that can potentially be disrupted. The supply chain of drugs has been disrupted. The spread of COVID-19 makes it difficult for governments to use these drugs; the availability of these systems faces constant challenges due to their components of use and limited initial needs.
Due to the sudden surge in cases and rise in demand for the drug, the supply is also increasing. After the U.K. report on dexamethasone usage in COVID-19 patients, a massive surge in demand due to this drug supply also increases. As the WHO stated, the drug is inexpensive, and there are many dexamethasone manufacturers worldwide, who we are confident can accelerate production, so there is no supply chain disruption. One more reason is dexamethasone is only used for critically ill patients or in severe patients. The usage is limited for the patients.
The trade restrictions have chosen nothing more than to produce the necessary medicines domestically during the pandemic, when the increase, counterfeiting, and price increases of imported goods increase. This signifies that even during the COVID-19 pandemic, the market players are able to maintain the supply chain.
The impact of COVID-19 on dexamethasone supply chain was positively affected because it creates an opportunity for researchers and drug manufacturers.
STRATEGIC DECISIONS OF GOVERNMENT AND MANUFACTURERS
As the Coronavirus continues to spread to various countries, concerns are growing about drug production and distribution disruptions. Collaborations, agreements, initiatives of market participants such as Fresenius Kabi expand their business to overcome the growing demand for dexamethasone, especially in Indian, U.S., U.K., and highly affected countries. This will help increase the demand for the product among the consumers and thus increase the company's future sales.
· U.K.-based Oxford University started a clinical trial (Recovery Trial), which is funded by U.K. government showed beneficial results. The results showed that dexamethasone reduces the risk of death by approximately one-third in patients on ventilators and one-fifth in patients receiving oxygen. Moreover, U.K. government also ensures that the lifesaving drugs will be available in NHS healthcare settings with immediate effect
· World Health Organization (WHO) also closely monitored the supply and demand of dexamethasone across the globe. Moreover, WHO advises the scale-up production of dexamethasone for the continuous supply of drugs
· German drug manufacturer “Fresenius Kabi” spoke person also stated that we are confident to meet customers’ needs with COVID-related medicines such as dexamethasone. Moreover, the company also stated that they have a good inventory on hand of the steroid and is ramping up production in three of its U.S. factories to meet the surging demand
· In Boston, Massachusetts General Hospital, infectious disease specialist “Arthur Kim”, stated that we revised our treatment protocol for the recommendation of dexamethasone for patients with severe COVID-19 who require supplemental oxygen
The increasing demand and increasing sale of dexamethasone drugs are fueling the growth of dexamethasone drug market in the near future.
Market participants are involved in the production of dexamethasone drugs, expanding their business through various programs, including collaboration, contracts, pipeline development, collaboration, and market expansion. It is expected that the strategic decisions of these companies will provide significant opportunities for market participants operating in the dexamethasone market.
CONCLUSION
The available clinical evidence suggests that dexamethasone is relatively safe with minimum side effects. Moreover, studies showed that when dexamethasone is administered, it reduces one-third of the risk for patients on ventilators and one-fifth risk for patients on oxygen supply and reduces 35% mortality benefit in certain patients with COVID-19 who are severely ill. However, the FDA still does not approve dexamethasone's use on severe patients, but doctors recommend the usage to save the patient life.
Moreover, ongoing trials are evaluating the use of dexamethasone for the treatment of COVID-19. Government and pharmaceutical market players have also taken strategic initiatives to overcome the pandemic.
#Dexamethasone Market#Dexamethasone Market Analysis#Dexamethasone Market by Application#Dexamethasone Market by Type#Dexamethasone Market Development#Dexamethasone Market Forcast#Dexamethasone Market Future Innovation
0 notes
Text
Coronavirus: which treatments work and which don’t?
PongMoji/Shutterstock
Donald Trump’s transient keep in hospital in early October raised consciousness – as soon as once more – of the number of remedies being investigated for COVID-19.
Some therapies the president obtained have been on the radar for a very long time, others are new to the listing of potential remedies. Notably, medication corresponding to hydroxychloroquine that had been as soon as broadly touted as a remedy weren’t used, having been proven to be ineffective.
Because of the Restoration trial, based mostly at Oxford College, we’re discovering out extra on a regular basis about which therapies are helpful. So, whereas the beneath gained’t be the definitive reply on the best way to deal with COVID-19, 9 months into the pandemic, that is what we all know to date about what works.
Corticosteroids
As early as June 2020, there was proof that dexamethasone, an inexpensive steroid, might scale back the danger of demise in severely unwell sufferers with COVID-19 by as much as a 3rd.
Later research confirmed the same discount in demise with one other widespread steroid, hydrocortisone. It might be that these medication are efficient as a result of they suppress extreme irritation within the lungs.
Interferon beta
We’ve identified for a while that sufferers who don’t produce sufficient interferon beta are inclined to extreme lung injury attributable to viral infections, because it performs a key function in immunity to viruses.
In a small medical trial, inhaled interferon beta diminished hospitalised COVID-19 sufferers’ danger of growing extreme respiratory illness by 79%. Sufferers handled with interferon beta had been additionally twice as more likely to get better absolutely over the 16-day remedy interval.
Whereas promising, these outcomes must be confirmed in bigger research evaluating the drug with different remedies. Interferon beta can also be being investigated together with different therapies, together with remdesivir.
A latest giant trial of a number of therapies confirmed no advantage of injected interferon beta in hospitalised COVID-19 sufferers.
Remdesivir
This antiviral drug, which stops sure viruses – together with coronaviruses – from reproducing their genetic materials, is already briefly licensed in roughly 50 nations for treating COVID-19 sufferers with pneumonia who want supplemental oxygen.
The drug initially underwent trials to be used towards COVID-19 in China, however as a result of the outbreak there was quickly introduced beneath management, not sufficient sufferers had been enrolled to supply statistically important outcomes. Subsequent trials within the US had been extra optimistic, exhibiting that it might shorten the restoration time of hospitalised COVID-19 sufferers with decrease respiratory tract infections.
Different research haven’t added a lot: COVID-19 sufferers with average pneumonia placed on a five-day course of remdesivir fared higher than these receiving normal care, however these placed on a ten-day course didn’t. This led the authors of the examine to query the importance of the outcomes. Disappointingly, a latest WHO examine additionally confirmed no enchancment in demise charges or restoration time for hospitalised sufferers.
Nonetheless, remdesivir is the one antiviral drug proven to be efficient towards COVID-19. It’s now a part of most nations’ normal remedy packages, regardless of the pretty weak proof behind it.

Remdesivir has momentary approvals to be used however nonetheless lacks sound proof of effectiveness. felipe caparros/Shutterstock
Tocilizumab
Monoclonal antibodies – antibodies which have been artificially generated to focus on sure molecules – are already used to deal with inflammatory ailments corresponding to rheumatoid arthritis. One in every of these is tocilizumab, which blocks the actions of an inflammatory protein known as interleukin 6.
Within the US, tocilizumab is licensed for treating cytokine launch syndrome – a extreme side-effect of some most cancers remedies that’s much like the intense inflammatory results of COVID-19. Research of tocilizumab’s impression on COVID-19 have supplied blended outcomes. Some have instructed that it reduces the chance of hospitalised sufferers needing mechanical air flow, and it reduces the demise price of sufferers who do require air flow. Others have proven that the drug has no impact on affected person outcomes.
Nevertheless, these research had been too small to permit for particular conclusions. One giant observational examine discovered optimistic results, however different elements (corresponding to variations in age, underlying well being circumstances and different remedies) might have influenced the outcomes.
Bigger, extra sturdy research are wanted. Tocilizumab is now being investigated in Restoration and in one other giant randomised managed trial within the US.
Convalescent plasma
One other antibody-based strategy is to present sufferers blood plasma from individuals who have recovered from COVID-19. This plasma will include pure antibodies produced by the donor throughout an infection.
Convalescent plasma was authorised within the US for emergency use in COVID-19 sufferers in August, regardless of very restricted proof of profit. Now that it has been authorised, docs within the US aren’t obliged to report on its results, which has made it tough to assemble good information on its effectiveness. Giant randomised managed trials are wanted.
REGN-COV2
REGN-COV2 is a combination of two monoclonal antibodies directed towards particular areas of the coronavirus’s spike protein, which is the important thing construction that it makes use of to enter our cells.
Animal research have proven promising outcomes, however they will’t reliably predict REGN-COV2’s results in people. Its maker has requested emergency use authorisation within the US which, as with convalescent plasma, might make accumulating dependable information tougher. Nevertheless, REGN-COV2 can also be beneath investigation within the Restoration trial.
A rival product – LY-CoV555/LYCoV016 – is beneath related consideration for emergency use. There’s very restricted information on its advantages, but it surely too is being examined in a big medical trial.
Different potential remedies
The one different remedy included within the Restoration trial is the antibiotic azithromycin. Given to deal with quite a lot of infections, it has anti-inflammatory and antibiotic properties, and may have antiviral actions. Trials to date present that there’s no profit when it’s given to sufferers already admitted to hospital, however the Restoration trial is testing its impact throughout earlier phases of COVID-19.
Regardless of early issues that sure blood strain medication would possibly improve the danger of COVID-19, giant research have proven that they’re secure. Research at the moment are investigating whether or not they may need some protecting impact.
Lastly, a number of research have proven that the antimalarial drug hydroxychloroquine and the antiviral mixture lopinavir/ritonavir are ineffective towards COVID-19. Derivatives of one other (plant-derived) antimalarial drug, artemisinin, have antiviral exercise and grow to be concentrated within the lungs. In idea, they might have medical advantages, however there’s no information but to point out this.

Gordon Dent doesn’t work for, seek the advice of, personal shares in or obtain funding from any firm or organisation that may profit from this text, and has disclosed no related affiliations past their tutorial appointment.
from Growth News https://growthnews.in/coronavirus-which-treatments-work-and-which-dont/ via https://growthnews.in
0 notes
Text
Coronavirus: Govt to take action against plasma selling

The Ministry of National Health Services has decided to take strict action against all the people who have been selling plasma in the country.
The health authorities have issued guidelines about plasma therapy treatment for COVID-19, urging people not to pay donors as the treatment was still “an experimental therapy”.
The illegal trade of plasma started after the government allowed it to be used for the treatment of CIVID-19 patients.
It was disclosed that mafia in Punjab doing business with the blood plasma of recovered patients of COVID-19, minting millions of rupees from the immoral business.
Dr. Shamsi had disclosed that the blood plasma being sold at the price of upto one lac rupees for each donation.
Moreover, the federal government has also warned that strict action would be taken against elements involved in over-charging or black marketing of life-saving drugs used by coronavirus patients.
In a statement, Special Assistant on National Health Services, Dr Zafar Mirza said the Drugs Regulatory Authority (DRAP) has been directed to ensure availability of medicines used for management of COVID-19 patients.
He said Tocilizumab (Actemra) and Remedesivir injections used for COVID-19 patients will be distributed to critically ill patients through a robust mechanism to meet the needs of various hospitals.
Read More
0 notes
Text
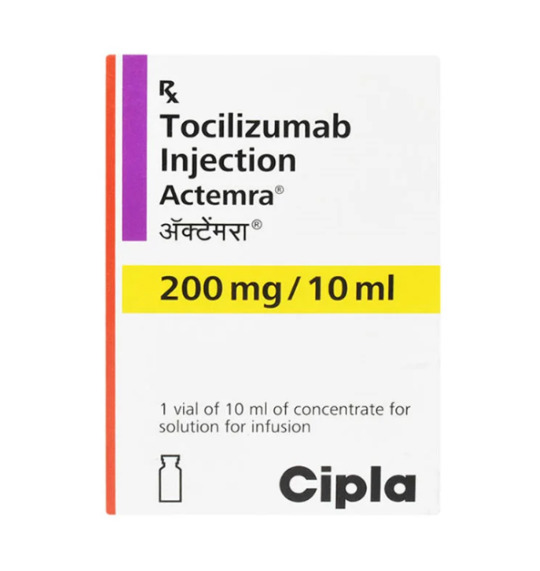
Buy Tocilizumab Injection at the Best Price – Medlama Offers
Tocilizumab is a vital medication used to treat autoimmune conditions like rheumatoid arthritis and cytokine release syndrome. It is widely prescribed by healthcare professionals to manage inflammatory diseases effectively. However, finding the best Tocilizumab injection price can be challenging, given the varying costs and availability across different suppliers and pharmacies. Medlama stands out as a trusted platform, offering the best prices, genuine products, and reliable service.
Understanding Tocilizumab Injection
Tocilizumab, sold under brand names like Actemra, is a monoclonal antibody that works by inhibiting interleukin-6 (IL-6), a cytokine responsible for inflammation. It is primarily used for treating conditions such as:
Rheumatoid Arthritis (RA)
Systemic Juvenile Idiopathic Arthritis (SJIA)
Polyarticular Juvenile Idiopathic Arthritis (PJIA)
Giant Cell Arteritis (GCA)
Cytokine Release Syndrome (CRS)
COVID-19 related severe inflammation (as per emergency use authorization)
Given its importance in managing these conditions, ensuring accessibility at a reasonable Tocilizumab injection price is crucial for patients.
Why Choose Medlama for Tocilizumab Injection?
Medlama has emerged as a leading platform in the pharmaceutical sector, providing high-quality medications at competitive prices. Here’s why Medlama is the best choice compared to other brands and suppliers:
1. Affordable and Competitive Pricing
Medlama ensures that patients get the most affordable Tocilizumab injection price without compromising on quality. By collaborating with certified manufacturers and suppliers, Medlama negotiates better prices, passing the savings on to customers.
2. Authentic and Certified Medications
One major concern when purchasing medications online is authenticity. Medlama sources only genuine, FDA-approved Tocilizumab injections, ensuring safety and efficacy. Every product comes with a proper certification, so customers can trust that they are receiving authentic medicine.
3. Reliable and Timely Delivery
Medlama offers a seamless ordering experience with prompt delivery services. Patients can get their required medication at their doorstep without long waiting times or supply issues, ensuring uninterrupted treatment.
4. 24/7 Customer Support
Understanding the urgency of medical needs, Medlama provides 24/7 customer support to assist customers with their orders, inquiries, and concerns. Their dedicated team ensures a hassle-free purchasing experience.
5. Bulk Purchase and Discount Offers
For hospitals, clinics, and bulk buyers, Medlama offers attractive discounts on large orders. This is particularly beneficial for healthcare providers looking to stock up on Tocilizumab injections at the best possible price.
6. Easy Prescription Upload & Hassle-Free Ordering
Purchasing medication through Medlama is simple. Customers can upload their prescriptions online, and Medlama’s team will verify them before processing the order. This ensures compliance with medical regulations while maintaining convenience for the buyers.
7. Global Shipping & Availability
Medlama not only serves customers in India but also offers international shipping, making it a preferred choice for buyers looking for a reasonable Tocilizumab injection price worldwide.
How to Buy Tocilizumab Injection from Medlama?
Ordering Tocilizumab injection from Medlama is simple and can be done in a few easy steps:
Visit the Medlama Website – Browse the available medications and find Tocilizumab injection.
Check the Pricing – Compare the Tocilizumab injection price with other suppliers to see the best deal Medlama offers.
Upload Prescription – Submit your valid prescription for verification.
Confirm Your Order – Add the required quantity to your cart and proceed to checkout.
Make Payment – Choose a convenient payment method and complete the transaction securely.
Receive Your Order – Medlama ensures quick and safe delivery to your doorstep.
Factors Affecting Tocilizumab Injection Price
While Medlama strives to offer the best prices, several factors can influence the cost of Tocilizumab injections:
Brand & Manufacturer: Prices may vary depending on the brand, with generic versions typically being more affordable.
Dosage & Strength: Different strengths (80mg, 200mg, 400mg) have varying prices.
Geographical Location: Availability and demand in different regions affect the cost.
Regulatory Guidelines: Import/export duties and government regulations can impact pricing.
Supply & Demand: During peak demand periods (e.g., COVID-19 crisis), prices may fluctuate.
Customer Testimonials – Why Patients Trust Medlama
Many satisfied customers have shared their experiences with Medlama, highlighting its affordability, reliability, and excellent service. Here’s what some of them have to say:
“Medlama offered the best Tocilizumab injection price compared to local pharmacies. The ordering process was smooth, and I received my medication on time.” – Rahul S.
“Authenticity and pricing were my biggest concerns when purchasing online. Medlama ensured I got genuine Tocilizumab at a fair price.” – Priya M.
“Their customer support team was very helpful. I highly recommend Medlama for anyone looking for reliable medication suppliers.” – Dr. Anil K.
Final Thoughts
Finding the best Tocilizumab injection price is no longer a challenge with Medlama. As a trusted and customer-friendly pharmaceutical platform, Medlama ensures that patients receive authentic medication at competitive rates with timely delivery and excellent support. Whether you are an individual looking for personal use or a healthcare provider needing bulk supplies, Medlama offers the best deals, making it the ultimate choice for Tocilizumab injections.
Don’t compromise on quality and affordability – Choose Medlama today and get the best Tocilizumab injection price!
0 notes
Text
Nearly two months after Delhi govt caps COVID-19 treatment prices, patients complain of overcharging by private hospitals
On 20 June, the Delhi government issued an order capping prices for COVID-19 treatments in private hospitals “with the proviso that all COVID-19 beds would be at rates given by the committee (formed under NITI Aayog member Dr VK Paul) subject to upper limit of 60 percent of the beds of total hospital bed capacity".
According to the order, the prices for all National Accreditation Board for Hospitals & Healthcare Providers-accredited hospitals were to be capped at Rs 10,000, Rs 15,000, and Rs 18,000 for isolation beds, ICU beds without ventilators, and with ventilators support, respectively.
Similarly, for all non-NABH accredited hospitals, the prices were Rs 8,000, Rs 13,000, and Rs 15,000, respectively.
The order clarified further: "The rates for private hospitals beds would be all inclusive as a package. This will include, but not limited to: bed, food and other amenities, monitoring, nursing care, doctors' visits/ consults, investigations including imaging, treatment as per the national protocol for COVID-19 care and standard care for co-morbidities, oxygen, blood transfusion, etc.”
Despite the order, private hospitals have continued to not only violate the norms, as the following case studies show, they have often been kept in dark about the scheme.
The authorities, for their part seem reluctant to fix the flaws in the government order or take the violators to task as issues remain despite repeated interventions from civil society organisations.
Caught between insurance provider, hospital
On 20 June, 60-year-old Tarun Lata was admitted to Shri Moolchand Kharaiti Ram Hospital and Ayurvedic Research Institute, a NABH-accredited facility for COVID-19 with left side pneumonia and pleural effusion. After being kept in an isolation ward for 10 days, Lata was billed Rs 2,59,348.
The hospital bill included an average cost of PPE kits at Rs 4,477 per day and oxygen charges for nine days at the rate of Rs 1,400 per day even though she was not even administered oxygen.
When Lata's son Nitin Gulati objected to the bill and asked the hospital to charge as per the rates fixed by the Delhi government, the hospital claimed the order was passed a day after Lata was admitted to the hospital.
His father and brother also tested COVID-19 positive and were under home isolation.
“It was a very traumatic situation for me, running between my mother in hospital and two other family members at home, and then there was this fiasco with the hospital,” said Gulati.
On 8 August, when I spoke to people in the cash counter and the admission department, and the billing department, they said that Lata’s case was to be charged under insurance and not the Delhi government price capping.
The front desk executive then called back to give me email addresses to write to.
“Please send us your queries again. Our senior team will have to discuss and revert accordingly,” the executive said.
In the meantime, the hospital had already sent a response on the case on 7 August denying these charges.
Dr Madhu Handa, medical administrator, wrote that the billing was done as per the agreement between the hospital and the insurance company.
The Delhi government order, however, lays down no special exceptions for insurance cases.
Gulati explained that he sought help from the corporate insurance cover provided by his employer.
He says that there was a tussle between the hospital and the insurance company over the bill. At first, the insurance company had said that they would pay as per the Delhi government price capping only, and refused to adhere to the full billing, informed Gulati.
The hospital, however, refused to budge. As a result, the insurance covered only Rs 1.02 lakh of the bill. After Gulati's employer approached the insurance company, an additional Rs 80,000 was added to the amount covered.
“That still meant an out of pocket expenditure of Rs 80,000. But, the larger issue is that the hospital never bothered to inform us properly about the Delhi government price capping, let alone implement it,” said Gulati.
Lata's is not the only case involving overcharging by Delhi hospitals, though.
Representational image. AP
Selective redressal
Nitin Kumar, 22, had to take up against three different hospitals: Max Super Speciality Hospital Saket (East Block), Goyal Hospital and Urology Centre, and Max Smart Super Speciality in Saket over rampant overcharging.
He and his mother Binney Rani tested COVID-19 positive while the rest of their family was in isolation.
"It was difficult to continue challenging the hospitals in that situation,” he said.
Kumar noted that he was administered FabiFlu at Max Super Speciality Hospital without his informed consent.
“Even though I consumed FabiFlu for only two days (26 tablets in total), I have been charged for two boxes of the medicine (34 tablets each). I was not given any of the medicine to take home when I was discharged,” he said, adding that he had been charged Rs 6,998.
“This was all via Whatsapp!” he added and recalled that he repeatedly refused to give consent to these practices of the hospitals.
Additionally, he had also been charged for medicines and investigations that are a part of the standard care for COVID-19 patients at Rs 2,185.50 and Rs 8,850, respectively.
Kumar’s grievances with Max Super Speciality Hospital were drafted and sent as a complaint letter to the hospital authorities as well as members of the state and central health departments.
In fact, on 1 August, Arti Ahuja, additional secretary (MoHFW) forwarded Nitin’s petition against Max Super Speciality Hospital to Vikram Dev Dutt, principal secretary (Delhi HFW) urging him to "enquire into the matter and take appropriate action".
Thereafter, the hospital took cognisance of this and refunded the overbilled amount. The hospital asked him to sign a non-disclosure agreement, which he had reservations against doing and thus only gave only a written acknowledgement instead.
The complaints regarding Kumar's mother’s treatment charges at Max Smart Super Speciality Hospital, Saket (East Block) and Goyal Hospital and Urology Center, however, have still not been acknowledged.
She was overbilled Rs 75,947 at Max Smart, and Rs 28,000 on a COVID-19 package along with an arbitrary pricing of Rs 4,000 for ambulance transfer at Goyal Hospital.
On 30 July, when this author spoke to Shaleen Mitra, the OSD to Delhi health minister Satyendar Jain, he was not aware of these complaints sent to his department and requested that these be forwarded to him again.
On 4 August, Mitra replied that “Nitin's payment was returned by the hospital”. However, he gave no acknowledgement of the complaints about overcharging in Nitin's mother's medical bills.
Tanushree Roy Chowdhury, the deputy general manager, corporate communications and public relations of Max Healthcare, initially said the complaint was resolved.
Then on 1 August, Chowdhury replied again saying she would look into the matter after the 'long weekend'. There has been no response.
Pay or take the patient out
Mayanka Sanghotra’s mother Narender Kaur breathed her last on 17 July in Shanti Mukand Hospital. Kaur was admitted there since 24 June after being diagnosed as COVID-19 positive. This hospital too didn't inform Mayanka of the government orders, and asked her to pay for a COVID-19 package of Rs 4 lakh instead.
Later, she was asked to procure three injections costing Rs 40,000 each and six vials of remdesiver which is really not easy to find.
“When I went to search for remdesiver outside, there was so much blackmarketing happening! The prices ranged from Rs 30,000 to Rs 80,000. And, the doctors had asked for six vials of the medicine,” she said.
Malini Aisola from All India Drugs Action Network (AIDAN) said, "The (20 June) order does mention an exclusion from the rate caps for experimental therapies such as remdesivir and tocilizumab which can be charged separately. Similarly, the IL-6 test and COVID-19 diagnostic test are also excluded from the package rates. However, in spite of the order, hospitals have been tacking on charges for both medicines routinely used in COVID-19 treatment and for investigations and baseline tests that should have been included in the package. We have observed these violations repeatedly and in numerous private hospitals.”
When Mayanka was informed that the bills had exceeded Rs 7.5 lakh by 5 July, she was worried. She looked around for help and managed to contact Amresh Kumar, the Aam Aadmi Party, as well as Malini.
When conversations did not seem to yield results, she wrote a complaint letter on 11 July. On 14 July, when she went to speak to the authorities about the complaint, Malini accompanied her.
Dr Tejender Pal, a physiotherapist, and Dr Samrul Hoda, from the billing department, said that that these escalations would make no difference.
Mayanka claims that on On 17 July, Dr Hoda told her on a phone call to “either arrange the payment" or she could "take the patient out of this hospital".
Later that day, Mayanka received another call from the billing department saying that the hospital has finally agreed to revise her bills according to the government capping. The issues in her mother's medical bills were settled, but two hours later, the hospital informed Mayanka that her mother's condition was unstable. Kaur was declared dead by 9.30 pm that night.
On 26 July, the hospital directed this reporter to Dr Hoda for a statement about the overbilling in this case, however, he said that he couldn't discuss the details.
He further added that he does not particularly remember this case, and did not have access to the records as it was a weekend. He promised to get in touch with further details later.
On 7 August, he informed that he was not authorised to talk about these things, but still explained: "The patient had agreed to pay the hospital rates and was not admitted as a government category. It might have happened that they ran out of money later, and hence started saying that they want the government prices.”
He also informed that though a certain undertaking exists, access to that document is restricted to me as well as the patient’s family.
“It is a hospital document, after all. We can only hand it to authorised persons,” he said.
Representational image. AP
Month after order, issues remain
On 23 June, several CSOs including AIDAN, Jan Swasthya Abhiyan (JSA), and twenty five others wrote to authorities welcoming the order capping prices for COVID-19 treatments and suggested immediate action points.
The capping restriction to only 60 percent of the beds seemed “arbitrary and incomprehensible” to them, and they suggested that this provision be extended to “all persons accessing treatment through private hospitals, and who are not covered under any laws or schemes that guarantee free treatment."
They also said that the order must apply to all COVID-19 patients including those who currently admitted and undergoing treatment in private hospitals.
In a press conference on 25 July, Inayat Singh Kakar of People's Health Movement noted that there has been no transparency or political will to implement the order.
On 25 July, these CSOs also organised a virtual press conference highlighting the continued violations of the order by private hospitals. They released another letter that highlighted problems in implementation and suggested remedial measures to the authorities.
The above mentioned testimonies are just the tip of the iceberg. More than a month after the order was passed and subsequent interventions from the CSOs, issues remain.
Crumbling infrastructure
According to the National Health Accounts estimates, released in March 2019, patients in India bear about 61 percent of the total health expenditure. The government’s health expenditure stands at an abysmally low 30.6 percent.
The Economic Survey 2020 shows that the government expenditure on healthcare was 1.6 percent in FY20 budget, a minuscule change from 1.5 percent in FY19. The National Health Policy, 2017, has recommended that health expenditure by the government should be 2.5 percent of GDP by 2025.
A 2018 study which analysed the financial burden of households’ out-of-pocket payments on medicine in India over a period of 2o years between 1994 and 2014 found that 3.8 crore Indians fell below the poverty line due to spending on medicines alone.
Jashodhara Dasgupta, from Sahayog, a non-profit voluntary organisation, explained how the term "out of pocket expenditure" concealed quite a few crucial facts about medical costs in India.
“Our public healthcare is immensely under-resourced and almost dysfunctional. In contrast, the private hospitals do have substantially more resources — both in terms of infrastructure as well as number of doctors. In times of a crisis like the pandemic, the people will be compelled to go to private hospitals,” she says.
Dasgupta informs that private hospitals function primarily with the support of private insurance and State-funded insurance companies, which allows them to hike prices astronomically.
She lays out two scenarios: “You see, when a minister gets admitted in a private hospital, the government covers the costs of that treatment, right? We, the taxpayers, pay for the treatment in private hospitals. The second situation is when corporate employees or PSU employees go to private hospitals, there’s the safety net of employer paid insurance. Concurrently, in both the cases, private hospitals use this to their advantage and their prices are hiked up astronomically.”
While the Delhi government did put together an order to contain some of the issues plaguing the private healthcare sector, the political will to implement it seems to be lacking.
When Amresh was approached about Mayanka’s case on 6 August, he said that he has followed the usual process of putting the patient in touch with the DMS of the hospital.
While that is an essential step, it still leaves the patient trying to fight for his or her rights against the hospital.
via Blogger https://ift.tt/3gJTlGn
0 notes
Text

0 notes
Text
Tocilizumab Injection Price and Detailed Information on Actemra at MedLama
Tocilizumab, sold under the brand name Actemra, is a biologic medication used to treat various autoimmune diseases, including rheumatoid arthritis, juvenile idiopathic arthritis, and cytokine release syndrome associated with certain cancer treatments. This medication has helped countless individuals manage their conditions, reduce inflammation, and improve their quality of life. However, as with many biologic drugs, the cost is an important factor to consider when seeking treatment.
In this blog, we will explore the tocilizumab injection price, provide an overview of Actemra’s uses and benefits, and show you how MedLama can help you access up-to-date information on this medication and its cost.
What is Tocilizumab (Actemra)?
Tocilizumab is a monoclonal antibody that targets and inhibits the interleukin-6 receptor (IL-6R), a key driver in the inflammation process in many autoimmune diseases. By blocking IL-6R, tocilizumab helps reduce inflammation and suppress the immune system's abnormal response, which is essential for managing conditions like rheumatoid arthritis, systemic juvenile idiopathic arthritis, and cytokine release syndrome.
The drug is administered via an intravenous infusion or subcutaneous injection, depending on the prescribed regimen. The intravenous infusion typically requires a visit to a healthcare facility, whereas the subcutaneous injection can be self-administered at home after receiving the necessary training from a healthcare professional.
Conditions Treated by Tocilizumab (Actemra)
Actemra is approved to treat a variety of autoimmune conditions, including:
Rheumatoid Arthritis (RA): Tocilizumab is commonly prescribed for patients with moderate to severe RA who have not responded well to other treatments. It helps reduce joint inflammation, pain, and damage.
Systemic Juvenile Idiopathic Arthritis (SJIA): A type of arthritis affecting children, SJIA can cause fever, rash, and joint pain. Actemra is used to treat this rare condition, helping reduce inflammation and manage symptoms.
Cytokine Release Syndrome (CRS): This condition can occur after certain cancer treatments, such as CAR T-cell therapy. Tocilizumab is used to manage severe cases of CRS by reducing the excessive immune response.
Giant Cell Arteritis (GCA): An inflammation of the blood vessels, often affecting the arteries in the head. Actemra can help reduce the symptoms and prevent complications associated with GCA.
COVID-19 (in certain cases): Tocilizumab has been used in hospitalized patients with severe COVID-19 to manage cytokine release syndrome, a life-threatening inflammation reaction.
Understanding the Tocilizumab Injection Price
The tocilizumab injection price is an essential consideration for individuals seeking treatment with Actemra. Biologic drugs like tocilizumab tend to be more expensive than traditional medications due to their complex manufacturing processes, targeted mechanisms, and the research and development costs involved in bringing them to market.
The price of Actemra can vary based on a number of factors, including:
Dosage: Tocilizumab is available in different doses, and the cost will vary depending on the strength and frequency of the injections required.
Healthcare Provider and Administration Fees: If you're receiving the intravenous infusion form of Actemra, you may incur additional costs for healthcare provider visits, infusion center fees, and medical supervision.
Location: The cost of medications like Actemra can vary depending on the region in which you live. Prices may differ between countries or even within different healthcare systems in the same country.
Insurance Coverage: One of the most significant factors affecting out-of-pocket costs is whether your health insurance covers the medication. Some insurance plans may cover the full cost, while others may require co-pays or high deductibles.
Pharmacy or Supplier: Prices can also vary depending on the pharmacy or supplier you use. Some online platforms or pharmacies may offer discounts, patient assistance programs, or lower prices for medications like Actemra.
As you can imagine, the tocilizumab injection price can fluctuate based on these factors, so it’s essential to explore different options and gather as much information as possible before making a decision.
How MedLama Helps You with the Tocilizumab Injection Price
MedLama is an online platform designed to provide reliable, accurate, and up-to-date information on medications, including pricing. When it comes to tocilizumab injection price, MedLama offers comprehensive data to help you make informed decisions about your treatment.
By visiting MedLama’s dedicated page for Actemra, you will gain access to the following:
Current Pricing Information: MedLama provides up-to-date pricing for Actemra injections, ensuring that you have accurate information before purchasing. This helps you budget accordingly and avoid unexpected costs.
Product Information: MedLama's product pages offer detailed descriptions of the drug, including its approved uses, dosage recommendations, administration methods, side effects, and potential interactions. This allows you to fully understand what you’re investing in.
Comparisons with Other Treatment Options: If you're unsure about whether Actemra is the right treatment for you, MedLama offers comparisons with other biologic therapies. This helps you weigh the costs, benefits, and potential side effects of various options.
Patient Assistance Programs: MedLama also provides information on patient assistance programs that may help reduce the financial burden of Actemra. Some pharmaceutical companies offer discounts or financial support to eligible patients, making it easier to access the medication.
Pharmacy Discounts and Offers: MedLama frequently partners with pharmacies to offer discounts, special deals, or payment plans. This can help lower the overall cost of treatment for patients who are concerned about affordability.
You can visit the Actemra product page at MedLama to explore all of this helpful information and ensure you get the best deal on your tocilizumab injection price.
Additional Factors to Consider
While the tocilizumab injection price is a key consideration, it’s also important to factor in the long-term benefits of the treatment. Actemra has been shown to significantly reduce symptoms of autoimmune diseases, prevent disease progression, and improve the quality of life for patients. By reducing inflammation and the need for additional treatments, Actemra may result in fewer doctor visits, fewer hospitalizations, and a better overall prognosis.
Moreover, many healthcare providers offer financial counseling or support to help navigate the cost of biologic drugs. It's worth discussing financial assistance options with your healthcare provider or pharmacist to reduce the burden of the treatment cost.
Conclusion
The tocilizumab injection price is an important factor when considering treatment with Actemra, but it’s not the only consideration. MedLama offers a comprehensive resource to help you understand the full picture, from pricing to administration, and can direct you to patient assistance programs that may make this life-changing treatment more affordable.
Visit MedLama’s Actemra page for up-to-date pricing, detailed product information, and resources to help you navigate your healthcare journey. With the right information, you can make an informed decision about whether Actemra is the right choice for managing your condition.
0 notes
Text
0 notes
Text
0 notes
Text
Tocilizumab: An Essential Medication for Managing Autoimmune Disorders

Tocilizumab, also known by its brand name ACTEMRA INJECTION, has become an essential treatment for various inflammatory conditions, including rheumatoid arthritis (RA), juvenile idiopathic arthritis, and cytokine release syndrome (CRS). More recently, it has played a critical role in managing severe cases of COVID-19. But what exactly is Tocilizumab, how does it work, and what should patients know about its uses and price? In this post, we’ll walk you through the key aspects of Tocilizumab, its significance in healthcare, and what to expect if you’re prescribed this medication.
Tocilizumab: An Overview
Tocilizumab is a monoclonal antibody that targets the IL-6 receptor, which is involved in the body’s immune response. IL-6 is a protein that can cause inflammation, particularly in autoimmune diseases where the immune system mistakenly attacks healthy cells. By inhibiting the IL-6 receptor, Tocilizumab helps reduce inflammation and prevent damage to tissues and organs.
Initially developed for autoimmune disorders like RA, Tocilizumab’s scope has broadened, especially during the COVID-19 pandemic. It is typically administered as an intravenous (IV) infusion or subcutaneous injection, depending on the condition being treated.
Tocilizumab – Uses & Introduction
Tocilizumab is a versatile drug with multiple applications. It is commonly prescribed for autoimmune diseases like rheumatoid arthritis and juvenile idiopathic arthritis, providing relief from debilitating joint pain, swelling, and other symptoms caused by chronic inflammation.
In addition, Tocilizumab is approved for treating cytokine release syndrome (CRS), a severe side effect of cancer therapies like CAR T-cell therapy, where the immune system releases excessive cytokines, leading to dangerous inflammation. In such cases, Tocilizumab helps control this immune overreaction and prevents life-threatening complications.
More recently, Tocilizumab has gained recognition for its effectiveness in treating severe COVID-19 cases, particularly in patients experiencing acute respiratory distress. By reducing the immune system’s overreaction to the virus, Tocilizumab offers critically ill patients a better chance of recovery.
How Does Tocilizumab Work?
Tocilizumab works by targeting and blocking the IL-6 receptor, a protein that plays a critical role in immune regulation. While IL-6 is necessary for normal immune function, excessive IL-6 levels can trigger harmful inflammation, especially in autoimmune diseases and severe infections like COVID-19.
When administered, Tocilizumab binds to the IL-6 receptor and prevents it from signaling the immune system to produce more inflammation. This reduces symptoms such as pain, swelling, and fever, bringing balance to the immune response while still allowing the body to fight infections or other threats.
The drug’s impact varies depending on the condition being treated, but many patients experience significant relief, particularly those with RA and CRS. In the context of COVID-19, Tocilizumab has been shown to lower the need for mechanical ventilation and improve survival rates in severely ill patients.
ACTEMRA INJECTION: A Key Brand
ACTEMRA INJECTION, the branded version of Tocilizumab, is available in two forms: intravenous infusion and subcutaneous injection. The choice between these options depends on the patient’s condition and the severity of their symptoms.
For instance, rheumatoid arthritis patients may prefer the subcutaneous injection for its convenience, as it can be administered at home. Conversely, patients with severe COVID-19 or CRS may require IV infusions, which are given in hospital settings.
Although ACTEMRA INJECTION is generally well-tolerated, potential side effects include headaches, high blood pressure, respiratory infections, and injection site reactions. More serious but rare side effects, such as liver damage and gastrointestinal perforations, make it necessary for patients to be closely monitored throughout treatment.
Tocilizumab Injection Price: What to Expect
The Tocilizumab Injection price can vary based on factors such as dosage, form (IV or subcutaneous), and location. Like many biologic drugs, Tocilizumab is not inexpensive, with costs ranging from several hundred to a few thousand dollars per dose, depending on the treatment plan.
Many health insurance plans cover Tocilizumab, especially when prescribed for FDA-approved uses like rheumatoid arthritis or CRS. However, if you’re concerned about out-of-pocket expenses, it’s essential to explore options regarding the Tocilizumab Injection price. Medlama can help you explore financial assistance programs that may reduce the cost of treatment. Talking to a healthcare or pharmacy counselor can help you secure the best possible offer, ensuring access to this vital medication without significant financial strain.
Side Effects and Monitoring During Treatment
While Tocilizumab is effective and generally safe, patients should be aware of potential side effects. Common side effects include:
Upper respiratory infections like colds and sinus infections
Headaches and dizziness
Injection site reactions such as redness, swelling, or pain
Elevated liver enzymes, which may signal liver stress
More serious but rare side effects include gastrointestinal perforations and severe allergic reactions. Tocilizumab can also weaken the immune system, increasing the risk of infections. Therefore, it’s essential for patients to be closely monitored, particularly those on long-term treatment for conditions like RA.
Patients will undergo regular blood tests to ensure proper liver function and monitor for any potential complications. Despite the risks, the overall benefits of Tocilizumab make it a powerful option for patients who haven’t responded to other treatments.
Conclusion: A Vital Drug for Multiple Conditions
Tocilizumab, marketed as ACTEMRA INJECTION, plays a crucial role in managing autoimmune diseases such as rheumatoid arthritis, as well as life-threatening conditions like severe COVID-19 and cytokine release syndrome. By targeting the IL-6 receptor, it reduces inflammation and provides relief for patients suffering from chronic immune conditions.
While the Tocilizumab Injection price can be high, many patients find the benefits outweigh the cost, especially when financial assistance programs are available. If you or a loved one has been prescribed Tocilizumab, it’s essential to understand the medical and financial aspects of this treatment. For personalized support and assistance in navigating treatment costs, talk to your healthcare provider or pharmacy counselor at Medlama, who can help explore the best options for managing your care.
1 note
·
View note
Text
Significant COVID-19 Impact on Tocilizumab | Healthcare Industry | Data Bridge Market Research

COVID-19 Impact on Tocilizumab in Healthcare Industry
A novel coronavirus SARS-CoV-2 appeared in December 2019 in Wuhan, China spreading much faster than its predecessors and has already diseased millions of patients worldwide as of April 19th, 2020. As the scope of the current COVID-19 eruption has reached section of pandemics, major international efforts in public health are ongoing to control the eruption. Although, the favorable vaccine discovered to save the patient life but not everyone get the dose so there is considerable interest in repeating existing antiviral drugs for use against COVID-19.
Tocilizumab (TCZ) is a monoclonal antibody against interleukin-6 (IL-6). It may ameliorate the inflammation associated with the severe coronavirus disease and hence improve the symptoms. The monoclonal antibody targets the host immune system to infection which potentially diminishes the inflammation.
IMPACT ON PRICE
A large number of challenges are being confronted by various market players due to the impending of the unusual coronavirus and different strains, one such issue is the uncertainty surrounding the impact of COVID-19 on tocilizumab demands. Due to the increased demand of life saving drugs such as tocilizumab, remdesivir and favipiravir for coronavirus treatment and stiff rivalry between the market players.
According to the reports in the month of April, as the India face second wave of coronavirus due to a sudden surge in its demand and fresh limited stocks have been imported in India. It looks as the product is present in black market and patients’ families are imposed to buy the products on higher rates to save their loved ones life.
For instance,
· Tocilizumab is taken in two doses as manufactured by F. Hoffmann-La Roche AG (Originator: Actemra) and distributed by Cipla Inc. in India. According to the company, the single dose of injection is about Rs 40,545 but due to the surge in the demand and rising cases, the shortages have led to a thriving black market where the drug was quoting more than Rs 1.00 lakh for a single injection.
The impact of COVID-19 has created huge price impact on the government as well as on patient families that they have to buy the drugs on higher rate as compared to the normal rate.
IMPACT ON DEMAND
Patient’s families are in panic situation due to the limited stock of the injection and higher price of the drug. The injection being sold on higher price in the black market. In that particular situation, government take over the allocation and supply of injection in the different states of India.
For instance,
· According to the reports in consultation with the company, among the states, the interim allocation of the drug has been finalized by Ministry of Health and Family Welfare and Department of Pharmaceuticals. Maharashtra got 800 vials followed by Delhi that received 500 vials. Gujarat, Madhya Pradesh, Punjab, Tamil Nadu and Central Institutions got 200 each. Telangana and Haryana got 160 and Uttar Pradesh got 150. Karnataka and Rajasthan have got 100 each.
The impact of COVID-19 has created an prospect for the number of drugs being clinically tested to cure the diseases or related symptoms.
IMPACT ON SUPPLY
As the endemic intensifies, supply chains can be at substantial risk due to over-located locations that can possibly be disrupted. The supply chain of drugs has been interrupted. The spread of COVID-19 makes it tough for governments to use the drugs, the obtainability of these systems faces constant trials due to their components of use as well as limited initial needs.
Due to the unexpected surge in cases and rising demand of the injection, the supply is disrupted. The Swiss drug maker F. Hoffmann-La Roche AG has responded to the short-supply of its drug Tocilizumab used to treat COVID-19 patients. Moreover F. Hoffmann-La Roche AG pointed out that given the rising number of infection in India, minimizing hospitalizations and easing pressure on healthcare systems was particularly important.
The trade limitations have chosen nothing more than to produce the necessary medications domestically. During the pandemic, when the disease increases, forging and price upsurges for the imported goods. This signifies that even during the COVID-19 pandemic, the market players are able to preserve supply chain.
FIGURE 1. EFFECT OF TOCILIZUMAB FOR THE TREATMENT OF SEVERE COVID-19 INFECTION

STRATEGIC DECISIONS OF GOVERNMENT AND MANUFACTURERS
As the coronavirus remains to spread to various nations, anxieties are growing about disturbances in drug production and distribution. Agreements, collaborations and initiatives of market participants such as F. Hoffmann-La Roche AG and Cipla Inc. expand their business to overcome the growing demand of Tocilizumab especially in Indian and highly affected countries. This will in turn will help to increase the growth for the products among the consumers and thus upsurge the future sales of the company.
· The U.K. NHS started clinical trial (REMAP-CAP) which is funded by the U.K. government showed beneficial results. The results showed that the tocilizumab reduces the risk of death by approximately 24%, when administrated within 24 hours of patient entering in intensive or critical care. Moreover, the U.K. government also ensures that the lifesaving drugs will be available in NHS healthcare settings with immediate effect.
· In Indian, Ministry of Health and Family Welfare and Department of Pharmaceuticals closely monitored the situation of critical ill-patients and also taken charge for the smooth supply of Tocilizumab across the country.
· F. Hoffmann-La Roche AG was also working with regional local players to accelerate the emergency use authorization of other antibody cocktail. An emergency use authorization in India would enable the import of globally manufactured product batches to India as soon as possible.
· National Institutes of Health (NIH) also regulated or stated guidelines for the emergency use of Tocilizumab in combination with dexamethasone for the hospitalized patients who are exhibiting rapid respiratory decompensation due to COVID-19. Moreover, the authority also stated the dose of the drugs, type patients and other consideration for the use of injection.
With the increasing demand and cumulative sale of Tocilizumab drugs are fueling the growth of tocilizumab medications market in the near future.
As such, market participants are tangled in the manufacture of tocilizumab drugs increasing their business through a variety of programs including contracts, collaboration and pipeline development and market expansion. It is expected that the strategic decisions of these companies will provide significant opportunities for market participants operating in the tocilizumab market.
CONCLUSION
The available clinical evidence suggests that tocilizumab is relatively safe with minimum side effects. Moreover, studies showed that when tocilizumab administered in combination of corticosteroids offers the modest mortality benefit in certain patients with COVID-19 who are severely ill. However, some adverse effects have been found related to the use of tocilizumab in patients with COVID-19 such as elevated liver enzyme levels and neutropenia or thrombocytopenia which are uncommon. Clinical studies also showed that the effect of tocilizumab in COVID-19 patients, may be prolonged and earlier outcomes have more relevance in view of the acuteness of presentation and rapid progression in the absence of immunomodulation in patients with hyper inflammation and ARDS.
Moreover, ongoing trials are evaluating the use of tocilizumab for the treatment of COVID-19. Government and pharmaceutical market players have also taken strategic initiatives to overcome the pandemic.
#Tocilizumab#Tocilizumab Market#Tocilizumab Market Analysis#Tocilizumab Market Analysis in Developed Countries#Tocilizumab Market by Application#Tocilizumab Market by Type#Tocilizumab Market Development#Tocilizumab Market Forecast#Tocilizumab Future Innovation
0 notes
Text
Govt swings into action after dwindling supplies of tocilizumab, remedesivir reported

The health ministry swung into action on Saturday after reports emerged that two drugs currently being used for the management of COVID-19 patients were in short supply in the country.
Chairing a meeting regarding the coronavirus situation in the federal capital, Special Assistant to the Prime Minister on Health Dr Zafar Mirza said tocilizumab and remedesivir injections used for the COVID-19 patients will be made available by the government.
The premier's aide said these medicines will be distributed to critically ill patients through a robust mechanism to meet the needs of various hospitals.
Dr Mirza said that taking cognizance of reports of short supply of these two injections immediate action was taken. After extensive efforts, there is an improvement in the availability status of the tocilizumab injection, he said.
Tocilizumab is a humanized monoclonal antibody that ordinarily used as an immune suppressant agent in rheumatoid arthritis.
The authorities have included it in the National Clinical Management Guidelines for use in the treatment of critically ill patients of COVID-19 who have Cytokine Release Storm.
The SAPM said directions have been issued to National Task Force on Eradication of Spurious and Sub-standard drugs to apprehend the black marketeers.
"The public is encouraged to inform the Drug Regulatory Authority of Pakistan (DRAP) on its toll-free number 0800-03727 in case they have been over-charged for the Actemra Injection."
"Strict action will be taken against elements found involved in over-charging or black marketing of life-saving drugs in accordance with DRAP Act 2012," he said.
Approved Maximum Retail Price (MRP) for Actemra 80mg injection is Rs11,952 per vial, Rs29,882 for 200mg and Rs59,764 for 400mg vial.
Meanwhile, in a meeting of DRAP's Drug Pricing Committee, the price of remedesivir was also finalised.
In the Drug Registration Board meeting held on 8th – 11th June 2020, two importers and 12 local manufacturers of remedesivir have been approved for market authorisation. The approvals would allow larger quantities to be made available.
Actemra import from US approved Later in the day, Punjab Health Minister Yasmin Rashid said that the government has allowed the import of Actemra from the US. The manufacturer (Roche) had earlier informed the authorities that due to certain restrictions, the drug can only be imported from Japan.
Addressing a media briefing, the health minister said the provincial government had requested the drug regulatory authority (DRAP) to grant the permission to import it from other destinations.
“Roche, the manufacturer of Actemra, informed us that the drug is not produced in a large quantity in Japan to meet the local requirements so we asked the federal government to allow import from the US,” Rashid said.
She, however, warned the people to not use it on their own and follow the protocols issued by the health officials.
“It could be dangerous for the patient if it is used without doctor’s advice. We are using it on a trial basis and we will be only able to decide after it is tried on 1,000 patients.”
She cautioned that the government will take action against those hoarding the drug to sell it at higher rates.
Through advertisements in today’s newspaper, the Swiss manufacturer also informed health practitioners to contact their authorised distributor for its availability on government-approved rates.
Read More
0 notes
Quote
On 20 June, the Delhi government issued an order capping prices for COVID-19 treatments in private hospitals “with the proviso that all COVID-19 beds would be at rates given by the committee (formed under NITI Aayog member Dr VK Paul) subject to upper limit of 60 percent of the beds of total hospital bed capacity". According to the order, the prices for all National Accreditation Board for Hospitals & Healthcare Providers-accredited hospitals were to be capped at Rs 10,000, Rs 15,000, and Rs 18,000 for isolation beds, ICU beds without ventilators, and with ventilators support, respectively. Similarly, for all non-NABH accredited hospitals, the prices were Rs 8,000, Rs 13,000, and Rs 15,000, respectively. The order clarified further: "The rates for private hospitals beds would be all inclusive as a package. This will include, but not limited to: bed, food and other amenities, monitoring, nursing care, doctors' visits/ consults, investigations including imaging, treatment as per the national protocol for COVID-19 care and standard care for co-morbidities, oxygen, blood transfusion, etc.” Despite the order, private hospitals have continued to not only violate the norms, as the following case studies show, they have often been kept in dark about the scheme. The authorities, for their part seem reluctant to fix the flaws in the government order or take the violators to task as issues remain despite repeated interventions from civil society organisations. Caught between insurance provider, hospital On 20 June, 60-year-old Tarun Lata was admitted to Shri Moolchand Kharaiti Ram Hospital and Ayurvedic Research Institute, a NABH-accredited facility for COVID-19 with left side pneumonia and pleural effusion. After being kept in an isolation ward for 10 days, Lata was billed Rs 2,59,348. The hospital bill included an average cost of PPE kits at Rs 4,477 per day and oxygen charges for nine days at the rate of Rs 1,400 per day even though she was not even administered oxygen. When Lata's son Nitin Gulati objected to the bill and asked the hospital to charge as per the rates fixed by the Delhi government, the hospital claimed the order was passed a day after Lata was admitted to the hospital. His father and brother also tested COVID-19 positive and were under home isolation. “It was a very traumatic situation for me, running between my mother in hospital and two other family members at home, and then there was this fiasco with the hospital,” said Gulati. On 8 August, when I spoke to people in the cash counter and the admission department, and the billing department, they said that Lata’s case was to be charged under insurance and not the Delhi government price capping. The front desk executive then called back to give me email addresses to write to. “Please send us your queries again. Our senior team will have to discuss and revert accordingly,” the executive said. In the meantime, the hospital had already sent a response on the case on 7 August denying these charges. Dr Madhu Handa, medical administrator, wrote that the billing was done as per the agreement between the hospital and the insurance company. The Delhi government order, however, lays down no special exceptions for insurance cases. Gulati explained that he sought help from the corporate insurance cover provided by his employer. He says that there was a tussle between the hospital and the insurance company over the bill. At first, the insurance company had said that they would pay as per the Delhi government price capping only, and refused to adhere to the full billing, informed Gulati. The hospital, however, refused to budge. As a result, the insurance covered only Rs 1.02 lakh of the bill. After Gulati's employer approached the insurance company, an additional Rs 80,000 was added to the amount covered. “That still meant an out of pocket expenditure of Rs 80,000. But, the larger issue is that the hospital never bothered to inform us properly about the Delhi government price capping, let alone implement it,” said Gulati. Lata's is not the only case involving overcharging by Delhi hospitals, though. Representational image. AP Selective redressal Nitin Kumar, 22, had to take up against three different hospitals: Max Super Speciality Hospital Saket (East Block), Goyal Hospital and Urology Centre, and Max Smart Super Speciality in Saket over rampant overcharging. He and his mother Binney Rani tested COVID-19 positive while the rest of their family was in isolation. "It was difficult to continue challenging the hospitals in that situation,” he said. Kumar noted that he was administered FabiFlu at Max Super Speciality Hospital without his informed consent. “Even though I consumed FabiFlu for only two days (26 tablets in total), I have been charged for two boxes of the medicine (34 tablets each). I was not given any of the medicine to take home when I was discharged,” he said, adding that he had been charged Rs 6,998. “This was all via Whatsapp!” he added and recalled that he repeatedly refused to give consent to these practices of the hospitals. Additionally, he had also been charged for medicines and investigations that are a part of the standard care for COVID-19 patients at Rs 2,185.50 and Rs 8,850, respectively. Kumar’s grievances with Max Super Speciality Hospital were drafted and sent as a complaint letter to the hospital authorities as well as members of the state and central health departments. In fact, on 1 August, Arti Ahuja, additional secretary (MoHFW) forwarded Nitin’s petition against Max Super Speciality Hospital to Vikram Dev Dutt, principal secretary (Delhi HFW) urging him to "enquire into the matter and take appropriate action". Thereafter, the hospital took cognisance of this and refunded the overbilled amount. The hospital asked him to sign a non-disclosure agreement, which he had reservations against doing and thus only gave only a written acknowledgement instead. The complaints regarding Kumar's mother’s treatment charges at Max Smart Super Speciality Hospital, Saket (East Block) and Goyal Hospital and Urology Center, however, have still not been acknowledged. She was overbilled Rs 75,947 at Max Smart, and Rs 28,000 on a COVID-19 package along with an arbitrary pricing of Rs 4,000 for ambulance transfer at Goyal Hospital. On 30 July, when this author spoke to Shaleen Mitra, the OSD to Delhi health minister Satyendar Jain, he was not aware of these complaints sent to his department and requested that these be forwarded to him again. On 4 August, Mitra replied that “Nitin's payment was returned by the hospital”. However, he gave no acknowledgement of the complaints about overcharging in Nitin's mother's medical bills. Tanushree Roy Chowdhury, the deputy general manager, corporate communications and public relations of Max Healthcare, initially said the complaint was resolved. Then on 1 August, Chowdhury replied again saying she would look into the matter after the 'long weekend'. There has been no response. Pay or take the patient out Mayanka Sanghotra’s mother Narender Kaur breathed her last on 17 July in Shanti Mukand Hospital. Kaur was admitted there since 24 June after being diagnosed as COVID-19 positive. This hospital too didn't inform Mayanka of the government orders, and asked her to pay for a COVID-19 package of Rs 4 lakh instead. Later, she was asked to procure three injections costing Rs 40,000 each and six vials of remdesiver which is really not easy to find. “When I went to search for remdesiver outside, there was so much blackmarketing happening! The prices ranged from Rs 30,000 to Rs 80,000. And, the doctors had asked for six vials of the medicine,” she said. Malini Aisola from All India Drugs Action Network (AIDAN) said, "The (20 June) order does mention an exclusion from the rate caps for experimental therapies such as remdesivir and tocilizumab which can be charged separately. Similarly, the IL-6 test and COVID-19 diagnostic test are also excluded from the package rates. However, in spite of the order, hospitals have been tacking on charges for both medicines routinely used in COVID-19 treatment and for investigations and baseline tests that should have been included in the package. We have observed these violations repeatedly and in numerous private hospitals.” When Mayanka was informed that the bills had exceeded Rs 7.5 lakh by 5 July, she was worried. She looked around for help and managed to contact Amresh Kumar, the Aam Aadmi Party, as well as Malini. When conversations did not seem to yield results, she wrote a complaint letter on 11 July. On 14 July, when she went to speak to the authorities about the complaint, Malini accompanied her. Dr Tejender Pal, a physiotherapist, and Dr Samrul Hoda, from the billing department, said that that these escalations would make no difference. Mayanka claims that on On 17 July, Dr Hoda told her on a phone call to “either arrange the payment" or she could "take the patient out of this hospital". Later that day, Mayanka received another call from the billing department saying that the hospital has finally agreed to revise her bills according to the government capping. The issues in her mother's medical bills were settled, but two hours later, the hospital informed Mayanka that her mother's condition was unstable. Kaur was declared dead by 9.30 pm that night. On 26 July, the hospital directed this reporter to Dr Hoda for a statement about the overbilling in this case, however, he said that he couldn't discuss the details. He further added that he does not particularly remember this case, and did not have access to the records as it was a weekend. He promised to get in touch with further details later. On 7 August, he informed that he was not authorised to talk about these things, but still explained: "The patient had agreed to pay the hospital rates and was not admitted as a government category. It might have happened that they ran out of money later, and hence started saying that they want the government prices.” He also informed that though a certain undertaking exists, access to that document is restricted to me as well as the patient’s family. “It is a hospital document, after all. We can only hand it to authorised persons,” he said. Representational image. AP Month after order, issues remain On 23 June, several CSOs including AIDAN, Jan Swasthya Abhiyan (JSA), and twenty five others wrote to authorities welcoming the order capping prices for COVID-19 treatments and suggested immediate action points. The capping restriction to only 60 percent of the beds seemed “arbitrary and incomprehensible” to them, and they suggested that this provision be extended to “all persons accessing treatment through private hospitals, and who are not covered under any laws or schemes that guarantee free treatment." They also said that the order must apply to all COVID-19 patients including those who currently admitted and undergoing treatment in private hospitals. In a press conference on 25 July, Inayat Singh Kakar of People's Health Movement noted that there has been no transparency or political will to implement the order. On 25 July, these CSOs also organised a virtual press conference highlighting the continued violations of the order by private hospitals. They released another letter that highlighted problems in implementation and suggested remedial measures to the authorities. The above mentioned testimonies are just the tip of the iceberg. More than a month after the order was passed and subsequent interventions from the CSOs, issues remain. Crumbling infrastructure According to the National Health Accounts estimates, released in March 2019, patients in India bear about 61 percent of the total health expenditure. The government’s health expenditure stands at an abysmally low 30.6 percent. The Economic Survey 2020 shows that the government expenditure on healthcare was 1.6 percent in FY20 budget, a minuscule change from 1.5 percent in FY19. The National Health Policy, 2017, has recommended that health expenditure by the government should be 2.5 percent of GDP by 2025. A 2018 study which analysed the financial burden of households’ out-of-pocket payments on medicine in India over a period of 2o years between 1994 and 2014 found that 3.8 crore Indians fell below the poverty line due to spending on medicines alone. Jashodhara Dasgupta, from Sahayog, a non-profit voluntary organisation, explained how the term "out of pocket expenditure" concealed quite a few crucial facts about medical costs in India. “Our public healthcare is immensely under-resourced and almost dysfunctional. In contrast, the private hospitals do have substantially more resources — both in terms of infrastructure as well as number of doctors. In times of a crisis like the pandemic, the people will be compelled to go to private hospitals,” she says. Dasgupta informs that private hospitals function primarily with the support of private insurance and State-funded insurance companies, which allows them to hike prices astronomically. She lays out two scenarios: “You see, when a minister gets admitted in a private hospital, the government covers the costs of that treatment, right? We, the taxpayers, pay for the treatment in private hospitals. The second situation is when corporate employees or PSU employees go to private hospitals, there’s the safety net of employer paid insurance. Concurrently, in both the cases, private hospitals use this to their advantage and their prices are hiked up astronomically.” While the Delhi government did put together an order to contain some of the issues plaguing the private healthcare sector, the political will to implement it seems to be lacking. When Amresh was approached about Mayanka’s case on 6 August, he said that he has followed the usual process of putting the patient in touch with the DMS of the hospital. While that is an essential step, it still leaves the patient trying to fight for his or her rights against the hospital.
http://sansaartimes.blogspot.com/2020/08/nearly-two-months-after-delhi-govt-caps.html
0 notes