Text
Trying to give report after a long shift
421 notes
·
View notes
Text
IF YOU’RE STUDYING CARDIOLOGY, LEARN THIS CHART
One of my study partners came up with this for our cardio exam. Since it was about 20% valvular disease, it saved my ass.
As a brief explanation, A = Aortic valve, P = Pulmonary valve, M = Mitral valve, T = tricuspid valve. It pairs up if a murmur is systolic or diastolic and associated with stenosis or regurgitation of a particular valve.
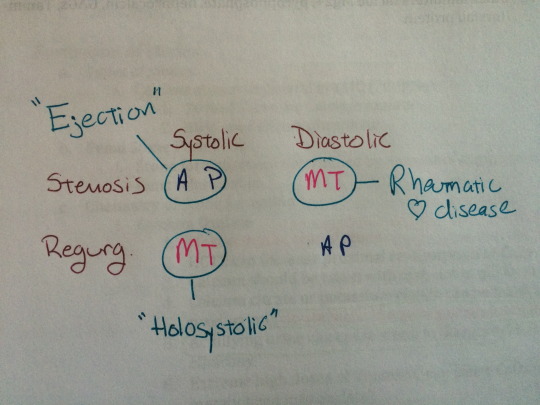
Happens to work out that Aortic & Pulmonary stenosis are both Systolic Ejection murmurs, Mitral & Tricuspid Regurgitation are both Holosystolic murmurs and both Mitral & Tricuspid Stenosis both can occur as a result of Rheumatic Fever.
There’s obviously way more to know for each of these conditions, but for someone who was mixing them up as bad as I was this turned out to be immensely helpful. Happy Studying!
3K notes
·
View notes
Photo

1. Fist: Make a fist around the epi-pen, don’t place your thumb/fingers over either end
2. Flick the blue cap off
3. Fire. Press down into the outer thigh (the big muscle in there), hold for 10 seconds before removing (the orange cap will cover the needle). Bare skin is best but the epi-pen will go through clothing. Avoid pockets and seams.
- Ring an ambulance even if everything seems to be fine!
500K notes
·
View notes
Text
When I walk in on my patient trying to get out of bed without assistance....

188 notes
·
View notes
Text
WHEN I WALK INTO A DISASTER BECAUSE I WAS STUCK IN ANOTHER ROOM FOR TOO LONG

254 notes
·
View notes
Text
How to Fake Confidence
1. Hold your head high, and look others in the eye
2. Smile
3. Stop apologizing
4. Relax and be quick to laugh at yourself (but not at others!)
5. Dress in a way that indicates you have self worth
6. Use good manners (like saying please and thank you) as this is actually a mark of self respect
7. Expect other people to believe in you, and to see and appreciate your good qualities.
589K notes
·
View notes
Text
As I walk through the valley of the shadow of death...
The call comes in, Level 1 trauma, ETA 3 minutes. We run to the trauma room, abandoning whatever it was that we were doing. Trauma takes priority over everything. Level 1 is the most critical of the alerts.
We all start to dress. For those that aren’t trauma nurses, “dressing” means throwing on an intricate ensemble of protective equipment over an already heavy load, and still being able to reach everything important. Lead gowns first to protect from the radiation exposure. I’m not so worried about my ovaries anymore, but I am however still using my thyroid. Shoe covers, because I have learned my lesson and don’t want another $125 pair of Danskos ruined from the blood pouring off the cart directly into my shoes. Impermeable gowns, goggles, masks, surgical hats and then finally, the gloves. You should always double glove. Another tried and true tactic. When your gloves get slippery from the blood, just pull off the top pair and you’re good to go. Plus, you get so sweaty in a trauma, it’s hard to get new gloves on sweaty hands.
Then, for those of us that can dress in 20 seconds flat, we take our places in the trauma room. Everyone has an assigned place… Respiratory and a doc to intubate at the head of the bed, nurse on the patients left, medic and surgical fellow or attending on the right, then there’s pharmacy, blood bank, your extra nurse, whomever is charting for the trauma, the lab, radiology, the ER attending, social work, security, pastoral care, and an OR nurse. It looks like chaos, but it’s really quite the finely tuned machine. We all have responsibilities, and we all know what we are preparing for. I get the rapid infuser ready. It can slam in 2 liters of fluid in under 2 minutes flat with a large enough IV. Pharmacy is preparing drugs, surgery is discussing how quickly they can get the patient to OR. The minutes drag on. With trauma, they are either at the back door when they call and you scramble to make it in the room before they unload the patient, or they take twice as long as they think because their adrenaline is pumping and they don’t realize how far out they are.
After several minutes, we hear the ambulance and the trauma bay comes alive. I hear screaming in the hall. The family is already here and sees the patient coming through the doors. EMS is running, a medic is doing compressions. They don’t have a line (IV line) and they are bagging the patient but he’s not intubated yet. They yell our their report. He’s been shot in the head. Point blank range. You can always tell from the gun powder residue on the skin.
They barrel into the trauma room and all at once, we take over. Within a minute we have an ET tube down. It’s a tube that we place into the trachea (hopefully!) to provide ventilation when a patient isn’t breathing. My medic and I both get large bore IVs at the same time, and I hook up the rapid infuser. There is blood pouring off the cart. I quickly note it’s coming from his head. We are all calling out our tasks and assessments for the attending surgeon and the nurse that is charting. I push some Epi, we keep up the compressions and hope to get a pulse. Nothing after 3 minutes. No pulse.
My fluid is complete on the rapid infuser. We quickly decide to change over to PRBCs, as the patient is losing more and more blood. More Epi goes in. No pulse after 3 minutes, rinse and repeat. Throw in some bicarb and calcium chloride to correct any imbalances, and then more Epi. They’re holding pressure on his head. I can see when the resident pulls her hands away that she has something white like cottage cheese on her gloves. It’s brain matter.
More Epi, and then suddenly I hear someone say they have a pulse. I hear the family outside crying. To be clear, no one is celebrating getting a pulse back. If you give enough Epi, you can get a heart rate from a flank steak. It doesn’t mean shit. We start a drip of Epi and head to CT. It’s the only way we’re going to be able to assess what the damage is.
Again, more organized chaos as we try to move a critically injured patient and 20+ trauma team members to the CT scanner. There’s blood trailing behind us down the hall. Someone steps on an IV line and pulls out one of my functioning IVs, I cuss a little too loudly, figure out it’s a resident that shouldn’t even be with us right now, and tell him he better get the hell out of my way. In another minute, I have another functioning IV in place, just as we’re putting the patient into the scanner. The nurses and a doc all stay with the patient, but I can see through the window that the attending surgeon is shaking his head. Neuro surgery has joined us in the scanner by now, and I can also see them shaking their heads, and then they leave.
Non-survivable… That’s the verdict when they come back into the room. We are loading the patient back up, preparing for transport, but it’s unclear where we are going. Is he going to OR? No… Neuro surgery declined, nothing they can do. His brain has already begun to herniate, at least what is left of it. It’s literally swelling as fast as a batch of rolls in an oven. So, we are going to the neuro ICU. But, just as we’re planning our route, the patient codes. We start compressions and call the ER, we’re coming back hot. I delegate compressions to the younger nurse, he can climb up on that cart and ride much easier than I can. We barrel down the halls back to the ER. Once we’re back in the trauma room, the surgeons ask if anyone has any suggestions. It’s last call for ideas, something more common in the last several years. No one is speaking, we know this patient met their fate the moment that bullet entered their head. The surgeons go to speak with the family while we keep up compressions. We always offer to let the family come in at the end, to be with their loved one when they pass.
Then, something odd happens. The attending surgeon comes back in and tells us to call it. The family doesn’t want to come in. We all look at each other… Who wouldn’t want to come be with their husband, son, father, or loved one when he passes? In all my years, this has never happened. I take the patients hand and hold it. I start to pray, the only prayer that comes to mind is the 23rd Psalm. I mouth the words silently. Then we stop compressions. Time of death is called. I feel like someone should cry for this man. He’s not even a man, he’s hardly out of adolescence we find out. In over his head with a gang, such a young, senseless death.
We clean the room around him, then I slowly and deliberately clean as much blood off him as I can. I bandage his wounds and secure all our tubes for the coroner. It’s obvious what killed him, but as a coroners case, he’ll need an autopsy. I leave his head and the gun shot residue. It’s all evidence.
I tag and bag him. That’s the crude way of saying I attach his identification to his toe, place him in a body bag and prepare him for the morgue. We’re busy, and I don’t have any help. Once the death is called, everyone has somewhere else they’re needed. It doesn’t take long, but my work is deliberate. I pray as I go. I talk to him, I tell him there were people that could have helped him, if only he had asked. I tell him his family is distraught, to forgive them for not coming to his side in his final moments. In my years in the ER I’ve learned that everyone grieves differently and there is no right way or wrong way. I can’t fault his family, I don’t know them, I don’t know their story. Nor do I really want to know. I feel restless, I know there is somewhere else I’m needed, but until a body goes to the morgue, it cannot be left alone. There is also a mountain of paperwork I have to complete.
I sit down at the desk and start to work. The coroner must be notified, plus the organ and tissue donation center. Finally, I’m done and I can take the patient to the morgue. We have a special bed that is supposed to “hide” the fact we have a body, but to anyone in the medical field, it’s pretty obvious. Security arrives and we head downstairs. The morgue is just where you would imagine… In the basement. It’s cold, smells of formaldehyde and it’s dark. I hate coming here. Plus, depending on the day, there are usually other bodies waiting as well. Today, there are 3 others. Mine makes 4. I pull out the table and we transfer him to the metal table. Then we log him into the morgue and close the cooler door.
On my way back to the ER, I stop in the cafeteria for a drink. The family is there, it appears they are having a family reunion in our cafeteria at 3am with children running around and everything. I just shake my head and keep walking. No one notices me, why would they… I’m just another nurse. I tried to save him, we did as much as we could, and I held his hand when the life left his body. I prayed for him, it doesn’t matter what you believe, I prayed he find peace, no matter what his religion. And here I am, walking by their table while they eat and drink. No one notices… But maybe that’s how it should be. Sometimes the most important people can be invisible. It doesn’t matter that they didn’t notice me, I don’t do this job for recognition, I do it for the patients. In his hour of need, I was there, and I didn’t let him down.
I make it back to the ER just in time to hear another squad encoding with a trauma patient. I’ve barely stopped sweating, but I dress as if it’s my first of the night. Then we wait… I hope this one will be alive, won’t be critically injured. But if they are, I’ll do it all over again.
Yea, though I walk through the valley of the shadow of death, I will fear no evil, for thou art with me…
2K notes
·
View notes
Photo

Isis chillin’ (her tummy is a little upset today) while Oliver keeps watch.
8 notes
·
View notes