Text
11/11/19 Weekly Update
A lot of my time this weekend was spent trying to understand how best we could integrate the user workflows of our proposed app with the existing EHR workflows.
As I went through some of our interview recordings with our mentor, and notes from Shiv and Tereze’s meeting with the nurses, the scope of our app was very clear: our app’s primary purpose is to sync with EPIC in accessing accurate doctor and nurse data, while using this information to provide a consolidated view of the care team and helping them communicate with each other.
Essentially, our app leverages EPIC as a verification resource so that we have accurate data on the care team, while helping set up user profiles, and establish communication channels.
My next steps involve fleshing out these symbiotic workflows between EPIC and our own app and designing these workflows in the context of a specific use case: like a gunshot victim being admitted into the ICU.
0 notes
Text
11/10 ICU & Trauma: Progress Update
Problem Statement:
Breakdowns in communication between patients, care providers, and families tend to disrupt the continuity of care, and be a cause of anxiety to patients’ families. This problem can be tackled from two major points: upstream communication between nurses and doctors and downstream communication between providers and patients’ families. How might we design a streamlined system of communication between nurses, surgeons, and other providers that is able to be integrated with pre-existing infrastructure, such that downstream patient flow is optimized?
General design concept:
We are generating a prototype of a mobile and desktop application that might serve as an extension of Epic, the pre-existing electronic health record database used in Rhode Island Hospital, via utilization of FHIR. The Fast Healthcare Interoperability Resource (FHIR) has the potential to increase interoperability and health information exchange by using secure standard URLs to transfer information across systems and platforms. Given our recent pivot from patient-provider communication to nurse-physician communication, the transfer of secure information might not be as prominent as an issue given our app’s integration with Epic’s patient database.
Key features we would like to implement for our prototype include:
Syncing seamlessly from existing EHR for accurate doctor and nurse information
Providing a consolidated, unified and real-time view of patient’s care team
Allows personal physicians to add new consulting doctors to the care team
Documents, at every stage, treatment decisions, results, and medication administered
Allows creation of new user profiles (doctors, nurses, consultants, verified by EHR)
Allows creation of new patient profiles & access to patient history in case of old patient
Enables doctor-nurse communication using secure text messaging and voice calls
Onboarding tutorial for the user
Patient calendar (i.e. scheduled operations, when and where)
Medication/Procedure updates
Timeline record for each patient since being admitted
A way for nurses/physicians to confirm, rescind, or reject updates for reapproval
Delivery times for medications
Knowing when things are being canceled
Being easily updated on patient flow
User personas:
The key people we are focusing on are trauma surgeons, nurses, and their patients.
Surgeon:
Pains
Surgeons often do not know the details about every patient. They only want to know the key points about each patient.
The ED/OR is an incredibly hectic space, with many key providers aside from the surgeon (anesthetists, PAs, etc.)
Gains
They only want to know the key points about each patient.
Prefer face-to-face communication for important decisions. How can our application streamline key information to make in-person communication more effective?
Nurses:
Pains
Feel that physician-nurse communication is an extremely prevalent and overlooked issue.
Feel conflicted and stressed when physicians give different/conflicting instructions (i.e. two tests/scans scheduled at overlapping times).
Gains
Would like a way to receive timely patient care updates and clarify those updates if there is a conflict or issue.
Patients:
Pains
Lack of communication between providers causes confusion, i.e. among family members, on what medications are necessary, what scans/tests are needed, and generally what is going on with treatment plan
Gains
Streamlined communication between providers would allow for more efficient, transparent care.
Decreased stress among nurses would lead to a better quality of care.
More efficient care has the potential to decrease medical costs (fewer days in hospital)
Plan for Prototyping:
The prototyping stage will begin with narrowing in the main problem we want to tackle aka communication between staff members and other departments.
Asking questions such as:
How are users solving this problem currently? Can your target market think of another product that does something similar?
Do users understand what this product or service does?
How do users feel about the product or service?
Who is your competition?
1. They are currently using a program called Epic. Its promises predictive analytics and embedded decision support tools support clinical practice to yield better outcomes. There is also an extension to the program they are using called lifespan and they provide updates every couple of months which causes unnecessary issues. Lifespan is a health care system primarily used in rhode island. It provides resources for patients but also for doctors and nurses who need to give information to patients.
2. They understand everything about they just can't deal with the never-ending updates, slow computer systems and the inability to tend to the patients the way that they want to. The problems stem from the fact that they strictly only use desktop computers, and they can’t tend to patients as much as they want to. The computer systems are old and since they are constantly updated it wipes out all of the system setups specifically tailored for the nurses using those computers.
3. After discussing our ideas with the nurses they seem to be very interested in the idea of implementing work tablets that are specific for each staff member. They stated in our interviews that the hospital is very gadget friendly and would be willing to try out a new system. They would mainly use it to log patients symptoms, updates etc. The only thing is keeping in mind patient security. The plus about creating an application would be the fact that it can be an extension of the system that they are currently using. They can also personalize it to fit the way that they do their rounds, calendar logging, a prompt messaging system that is fast and efficient, knowing when there are cancelations, increasing patient flow, pharmacies, numbers of other units etc.
4. Our competition are brands that are stand-alone apps. We would most likely make an app that is an extension of the current system.
Prototyping Strategy:
Before delving into the workflows and sketching possible concepts, we began by assessing what we considered the biggest challenges to our app’s success, chief among which was integration into existing hospital infrastructure.
We wanted to fit our app seamlessly into existing clinical workflows and infrastructural specifications. Hence, we decided that our app must leverage what EPIC, the existing EHR system can offer, while offering its own unique value—improving communication between caregivers, thereby simplifying clinical workflows and not complicating them.
Below are two diagrams that illustrate the functionalities of our app:
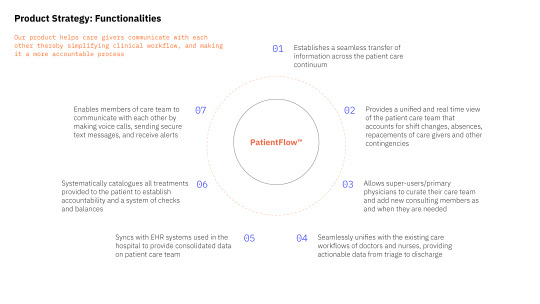

The diagrams can also be found here
Next Steps for prototyping:
Identify Specific Use Case: We will begin charting detailed user-specific workflows given a common scenario which is patients suffering from gunshot wounds.
Charting User Workflows and Engagement with App: With an understanding of the current treatment continuum (from patient arrival to discharge), we will clearly outline what our app would provide at each stage, and describe the user’s interaction with the app at every step.
Visual Prototyping: Once we have enough information on the user workflows, we will transfer that information into visual screens and sketches for testing.
0 notes
Text
Update 11/10 Shivam
I’ve been thinking a lot about what kinds of issues the stakeholders in the ICU face in terms of being out of the loop on the status of the patient. I want to spend more time at the hospital talking to nurses to get more information. Mukul and I have also been meeting up to talk about the design of the product. We’re thinking of tailoring the product to the specific use case of providing better care to a gunshot wound victim.
0 notes
Text
Weekly Update 11/10
This week, I worked on developing a first pass for the patient journey map. We decided to focus on one specific type of patient: patients who enter the trauma ICU for gunshot wounds are very common.

Since patients receive different scans and tests, we want to make sure we can target the major “branch points” for communication.

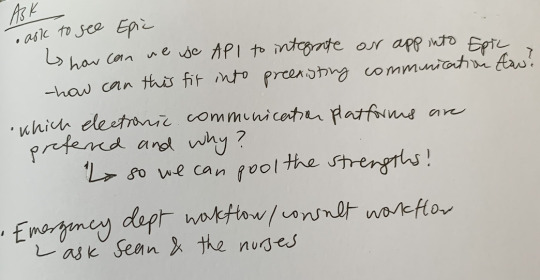
I definitely want to confirm that these diagrams are accurate and receive input from doctors and nurses themselves on which points are most high-stakes or hectic for communication. We were planning on meeting with Sean this past Friday but we unfortunately all got sick, so we will be rescheduling for this week. Some questions we need to ask:
0 notes
Text
Excel-Teréz
Over the weekend I created an excel sheet that helped disperse the work load based on all of the teams strengths.

0 notes
Text
11/4 Weekly Update
This week, I looked at inspiration from preexisting mobile apps (not limited to the healthcare space) and thought about which aesthetic criteria would be crucial to our user groups.
Color scheme: Using a muted, minimal color scheme like the one below.

Something like this may be too overwhelming:

Since a lot of our users are going to be older, we have to design for those with low visual acuity. - use high contrasting colors - larger text - clearly distinguish interactive from non-interactive elements
Other ideas: - “gameifying” the educational aspects, i.e. low-stress quizzes to reinforce information
Challenges: - infrastructure is limited: the desktop computers are not very up-to-date in that you can’t run much at the same time - nurses don’t use phones regularly - nurses want more communication between themselves and doctors, not necessarily with patients
To-do: Develop specific use cases and map out the patient journey. Since gunshot wounds were cited to be particularly common at the RI trauma center, I will focus on developing this use case.
Resources: Trauma flow sheet
0 notes
Text
Weekly Update 02
We met with Dr. Monaghan on Wednesday the 23rd to get some initial feedback on our idea of addressing the communication challenges that exist between doctors and patients’ families. Here were some of his thoughts and suggestions: 1. He supported our choice of problem space and agreed that a better system of communication between doctor and family needed to be established.
2. Dr. Monaghan mentioned that currently, all communication to patients’ families is done ad hoc, and it is the nurse who is the primary point of contact.
3. Citing overworked schedules and possible lapses in info transfer from doctor to nurse, Dr. Monaghan suggested that we gear our app towards doctors and families and not nurses and families.
4. Since a patient’s treatment could include interventions from several doctors and consultants, options to add new consultants to the treatment plan should be considered.
5. However, a consequence of having a team of caregivers is that there could be too much information being conveyed to the families. Hence, a clear chain of communication must be established in the workflow, where all info from the several doctors are parsed, and is communicated succinctly by one primary point of contact.
6. In order to convey just the right kind, and amount of information to families, Dr. Monaghan suggested a scale of 5 format for doctors to check off in regard to the patient’s progress and treatment.
7. An offboarding workflow/use-case must also be accounted for, as patients are transferred from the ICU to the floor.
In general, we’re happy to report that Dr. Monaghan attested to our choice of problem space and saw great value in our intervention so far.
0 notes
Text
Weekly Update
10/28/19
I looked more into FHIR and how that can play with with the integration of our mobile/desktop app prototype into the healthcare workflow. “The Fast Healthcare Interoperability Resource, commonly known as FHIR, has quickly become one of the most popular protocols for joining disparate systems together, and holds great promise for the development of an application-based approach to interoperability and health information exchange... By creating an accessible and standard URL for these information bundles instead of just passing individual documents back and forth between systems, a number of different applications can point to the same version of the same data each and every time.” Source
An analogy that has been made is FHIR is like the internet but for healthcare records. Its greatest advantage over other interoperability standards is its sheer speed, plus it’s safe and secure.
Example of data exchange using FHIR: patient browser,
demo
“Resources represent healthcare data in the FHIR realm. Resources are used to build an instance-level picture of the data to exchange. Resources may aid in exchanging the data or provide a means to store the data like a web page does for the internet. In order to keep this process and the structure of resources consistent, resources must include the following things:
A URL to identify the resource
Metadata to aid in searches and for cataloging
An XHTML summary so people can read it
Definitions for data elements
An extensibility framework specific to healthcare”
Source
More sources:
https://www.intersystems.com/fhir/#understanding-hl7-fhir
https://www.hl7.org/fhir/usecases.html
0 notes
Text
Team Update - Prototype Insights
This week, we met with Dr. Monaghan again to discuss our prototype idea to gain insight into the below questions and assumptions.
Key Features
Onboarding
Diagnosis and its implications
Calendar
Medication/Procedure updates
Education: steps for planning end of life care
Offboarding process: next steps to take, where to go
Possible: providers don’t have to input anything. Integrate with EHR, patient has opportunity to input information
Key Terms
Personal health records
FHIR
Improve interoperability between health care systems
Risky Assumptions
What assumptions are you making while designing the app?
If these assumptions are false, everything would break
Questions for Nurses
Run idea by them
What are some immediate barriers as they see them?
Competing products? Why are they/are they not using them?
Ask Sean about electronic health record
Chief Information officer can be a key source on EHR
Insights for Prototypes
What is that interaction between the EHR and the app like?
What does that workflow look like? (Who’s using it? What does their usage look like?)
What do you want your prototype to achieve?
10/28/19
0 notes
Text
Team Update
Refining Our Parameters
Patient privacy/HIPAA Laws
EASE is a mobile application that is very similar to our concept. They are HIPAA compliant and provide photograph updates of surgical operations and send them through the app to the family members.
What we could do better: the EASE application is marketed as “Snapchat” but in the healthcare realm. As a team, we feel that this marketing is not appropriate for the type of product we’d like to provide. We’d focus more on increasing comprehension of care among patients and their families rather than constantly being connected.
How much information is necessary to share?
Our goal is not to overwhelm family members with every minutiae of the patient’s care. The level of depth of information we provide through the application/product is incredibly important to consider. For instance, we would not want to stream live updates of the patient’s vitals, as that could stir more distress among family members.
Would patients’ families want to see updates of every scan/medication change as explained by the doctor? Would doctors even be okay with spending more time doing that? (Refer to video by EASE in which a doctor is explaining the angiogram)
Integrating with existing modes of communication + Integrating with existing workflows of nurses and doctors to increase chances of adoption
An idea we could borrow is scanning the patient’s wristband to integrate with the application. Is there another way to integrate with pre-existing patient databases?
Would this primarily be used by nurses and family members, and/or would physicians be incentivized to use the app to receive patient updates?
Design Principles
Addressing parameter #2: Users are able to customize the types of updates and information they receive.
The user learns how to use the application through an onboarding process (module for mandatory video tutorial).
Hospital can give out steps to take for the future when discharged from the hospital
The application has a feature for receiving feedback (optional).
10/21/19
0 notes
Text
Weekly Update #4
This week, I focused on researching the market and preexisting competitors in the digital app space aiming to solve the issue of spotty family communication when a patient is admitted for a procedure.
A mobile application named EASE seems to be the biggest competitor.
EASE is a HIPAA compliant mobile application. Slide 18 shows the flow of information; blue boxes represent when information is communicated via EASE. The pilot study was done with families of patients undergoing CT surgery.
Key Takeaways (SOURCE LINKED BELOW):
The use of a mobile application to communicate in real-time from the operating room enhances the family experience and improves satisfaction.
Physicians and nurses report that this method of updating the family is more efficient, reliable, valuable, and enjoyable than the traditional phone call.
Communication is a vital component of the health care experience, and the surgical operating room has often lagged behind other areas in keeping families informed.
The utilization of real-time text and visual updates with mobile technology is an efficient and effective tool that has been embraced by physicians, nurses, patients, and their families.
Successful adoption and implementation of electronic communication requires a cultural change within an organization. Buy-in from executive administration, the legal office, the compliance office, and medical leadership is necessary.
Adoption and implementation of innovations in health care can follow a phased process that identifies innovators to test the process and then allows expansion to occur organically.
Providing enhanced communication has been shown to improve the patient experience and increase satisfaction scores and other valuable metrics.
More details on EASE: here, here.
For our team, we might not even decide to take a digital app approach. Our future steps are to hammer out idea(s) of non-application-based technology that might serve the same purpose of improving physician-family communication. We may even narrow our painpoint to improving family understanding of the decision making process nearing the transition to end of life care, or increasing comprehension of the patient’s procedures and medications in general, rather than focusing on the efficiency of real-time updates and photos (which requires greater degree of attention to legal compliance).
10/20/19
0 notes
Text
Team Update
This week we discussed the problems we would encounter while developing an interface that would be useful for all parties in the hospital space. Together we researched, discussed, brainstormed ideas and possible outcomes for our final project. Along with that we created a presentation for the midterm critique.

0 notes
Text
Weekly Update #3 - May
This past week, I did a lot more secondary research on the prevalence of anxiety among family members of patients in the SICU. The rest of the time was spent on putting together the Midterm Crit presentation.
Excerpt:
“Families desire more frequent communication with nurses and physicians, and access to and comprehension of information often is lacking. Failure to comprehend a diagnosis, prognosis, or treatment occurs in 35–50% of family members.”
Citation: Jacobowski NL, Girard TD, Mulder JA, Ely EW. Communication in critical care: family rounds in the intensive care unit. Am J Crit Care. 2010;19(5):421–430. doi:10.4037/ajcc2010656
https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2729390
Additionally, there is a high need to improve preparation of surrogate decision-makers for difficult conversations in end of life (EOL) care. A majority of family-clinician conferences about prognosis neglect discussion of values and patient vs. family preferences. This topic is particularly difficult to navigate because in the state of Rhode Island, family preferences for care override the patient’s own directives.
Citation: Scheunemann LP, Ernecoff NC, Buddadhumaruk P, et al. Clinician-Family Communication About Patients’ Values and Preferences in Intensive Care Units. JAMA Intern Med. Published online April 01, 2019179(5):676–684. doi:10.1001/jamainternmed.2019.0027
0 notes
Text
Update 2 - Shiv
This week we talked to Dr. Monaghan in our in depth interview and asked him more specific questions about the experience in the ICU. We’ve decided to narrow down our focus to improving communication between the doctors and nurses with the family members of the patient in the ICU.
On my end, I visited Sean and helped with the IDI. I also spent a bit of extra time after the initial IDI asking him more questions about the healthcare industry in general. On Sunday we met up and did some secondary research. I found a few journal articles where doctors talk about how they want family members by the bedside of the patient. There were also articles detailing the difficulty nurses may have with family members.
0 notes
Text
Team Update Week 2: Post-IDI
The team reconvened on Sunday the 29th of Sep to debrief after our IDI session with Dr. Sean Monaghan.
There was clear consensus on the problem space after our meeting with Dr. Monaghan, and that was the relationship between patients and their family/friends during treatment in the ICU.
Today, the only point of contact for families/friends wanting to know how a patient is doing is the nurse. That can be a cause of anxiety for families who have other commitments to meet and cannot be by the patient’s bedside during the day.
With Dr. Monaghan clearly stating the advantages of having one’s family by their side during treatment, the design challenge then becomes a question of establishing sufficient levels of transparency about a patients’ progress/treatment with their families.
An important part of our intervention would be adhering to regulatory requirements and not disrupting any existing workflows followed by nurses, doctors and other stakeholders in order to get their buy-ins.
Things to do:
1. Stakeholder Analysis
2. Personas
3. Journey Maps for Patient, a Famly member, Nurses, and Doctors.
0 notes
Text
Team Update Week 2 - IDI
We conducted an IDI with Dr. Monaghan to get a better sense of pain points and areas of opportunity. The document linked below includes our questions and insights from the interview.
https://docs.google.com/document/d/17hKqUbp2aerTJaM_4rdnyQfpHnCu25veyKIDtSLbgl4/edit?usp=sharing
Additionally, we met as a team on 9/29 to discuss future steps to take. Pictured below are our insights and areas of opportunity stickies from class.




0 notes



