Catalouging the expansive field of clinical and laboratory pathology through the eyes of a Transfusion Medicine Technologist. Boston, MA
Don't wanna be here? Send us removal request.
Text
Subarachnoid hemorrhage
Greetings all! I haven't done an informative post for awhile and since I'm in a neuro/surgical ICU, I figured I discuss subarachnoid hemorrhage (SAH), particularly in a critical care context.

A SAH is a type of hemorrhage stroke. Bleeding occurs spontaneously or from a traumatic source within the subarachnoid space. As a quick reminder, the brain has tissue layers creating separate intracranial spaces where blood or CSF can collect. We name these bleeds often based on WHERE they occur.
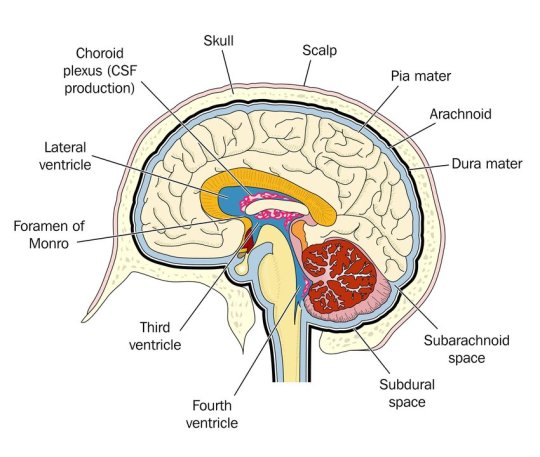
Therefore, a SUBarachnoid hemorrhage occurs beneath the arachnoid mater but above the pia mater.
Background
Most SAH are spontaneous from a ruptured aneurysm, though around 20% of SAH do not have a defined cause. Less commonly people experience traumatic SAH (tSAH) from a fall or MVC. The management of a spontaneous SAH and tSAH are different.
Most common in patients >40 y/o, with dominance in woman. Most common cause is rupture of an aneurysm, 80% of which are berry aneurysms. Risk factors for aneurysm rupture are hypertension, smoking, hyperlipidemia, atherosclerosis, advanced age, and extreme emotional stress.
Diagnosis and ED Care
Symptoms: classically the "thunderclap" headache or "worst headache of my life" which progresses rapidly over several minutes. This is usually a constant headache that pain meds really can't touch. Patients can also have nausea or vomiting - beware if you see this as it is a sign of increasing intracranial pressures. Can also have photophobia, delirium. They do NOT have a focal neuro deficit.
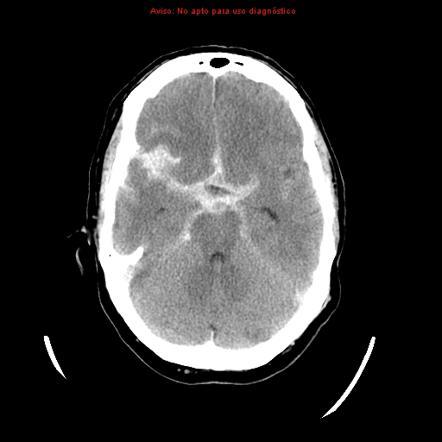
Have a LOW threshold to scan this patient's head. Diagnosis is obtained from head imaging. Get a non-contrast head CT to identify the presence of intracranial blood. Of note, xanthochromia on LP is also diagnostic; however, this isn't helpful for surgical planning. On a non-contrast CT, blood will appear white.
Surgical & Critical Care Management
Emergency Surgery: At minimum people receive a ventriculostomy to drain the head of blood. Some people with significant swelling require a hemicraniectomy. Below is a general illustration of ventric placement (also called EVD - external ventricular drain).

After immediate drainage (or sometimes before), patients receive a CTA of the head to locate the aneurysm and if surgically repairable, the aneurysm will be coiled the next day in the neuro IR suite. These patients will also receive CT perfusion (at least once, sometimes twice) to check for vasospasm.
SAH precautions: apply to all patients at all times
HOB >30
Strict bedrest
Arterial line for precise BP measurement (you'll find disagreement among critical care providers about this since arterial lines have not been shown to improve patient mortality. However, that study was NOT in a neuro critical care population)
Continued ICP monitoring (via the ventric)
Antibiotics while the drain is in place (usually ancef)
Daily stool softeners to avoid straining with bowel movements
Low lights, quiet environment (no phone, little tv, etc)
Stat head CT for any acute neuro decline
Maintenance of euvolemia (SUPER important as hypovolemia can trigger vasospasm)
Seizure prophylaxis x 7 days (usually keppra 500 mg BID)
Vasospasm prophylaxis x 21 days (nimodipine 60 mg q4h)
No antiplatelets or blood thinners.
No dvt prophylaxis until bleeding has significantly decreased (usually after coiling- surgeon dependent)
Avoid hypercapnia, hyperglycemia, hyperthermia
Aggressive blood pressure control (usually SBP <140)
Sodium goals (patient dependent, higher goal if significant swelling present)
Worth noting that tSAH patients have SOME of these precautions but not all. Nimodipine is not indicated for vasospasm prevention in these patients. I've seen it used in special situations but most commonly not. Depending on size of tSAH, they may not need a ventric or seizure prophylaxis.
Prognosis
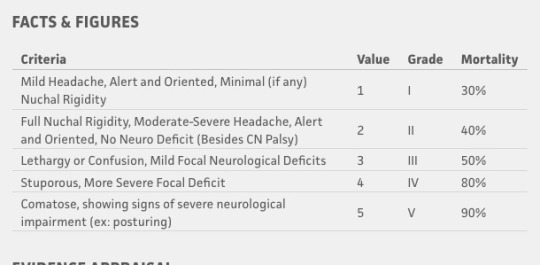
Prognosis has improved over the past 2 decades. Outcomes are multifactorial on age, size of bleed, overall health, and presence of rebleed or complication (vasospasm, ischemic stroke) etc. Roughly 1/3 of patients have a good outcome, meaning return to baseline functionality. 1/3 of patients will have a focal neuro deficit, usually due to vasospasm which caused an ischemic infarct. The remaining 1/3 of patients die from SAH.
At presentation you can use the Hunt and Hess Scale to help guide education for families about prognosis. Generally, the poorer the neuro exam at presentation, the worse the prognosis. There has been some criticism that it is observer dependent and distinguishing between Grade I and Grade II is moot. The important thing about this scale is that is does NOT include the CT imaging. I personally have seen HUGE bleeds that one would think would kill the patient but with prompt intervention they have a normal exam and good outcomes.
The most common complication is rebleeding of the aneurysm even if it has been repaired. This is usually due to poor blood pressure control, vasospasm, or head trauma after SAH recovery. Rebleeding is usually bad for most patients.
These patients stay in the ICU for at least 7 days for ICP and neuro monitoring. Some stay more if vasospasm is present. I do not get to interact with patients on neuro step down and don't have the privilege to see them in outpatient clinic. But if comorbidities that contributed to the stroke are well managed and the patient receives the necessary PT/OT and other support services, outcomes are good. It's still a horrible diagnosis to get but it's not as devastating as it used to be.
If you work in neurology/neurosurgery and see these patients in clinic, please reblog and comment. I think a lot of ICU providers (myself included) get jaded with the horrible stuff we see and don't have a good grasp of longer term recovery.
44 notes
·
View notes
Photo
537 notes
·
View notes
Photo










The Taming of the Shrub
- Art by Nunzio Paci
3K notes
·
View notes
Text
How Long Covid Exhausts the Body
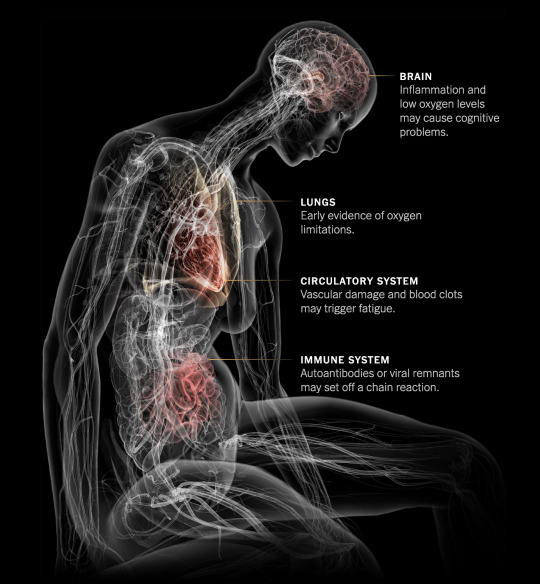
Millions of people continue to suffer from exhaustion, cognitive problems and other long-lasting symptoms after a coronavirus infection. The exact causes of the illness, known as long Covid, are not known. But new research offers clues, describing the toll the illness takes on the body and why it can be so debilitating.
Diagnosing Long Covid
Patients with severe Covid may wind up in hospitals or on ventilators until their symptoms resolve. Damage to the body from severe Covid — pneumonia, low oxygen, inflammation — typically shows up on traditional diagnostic tests.
Long Covid is different: A chronic illness with a wide variety of symptoms, many of which are not explainable using conventional lab tests. Difficulties in detecting the illness have led some doctors to dismiss patients, or to misdiagnose their symptoms as psychosomatic. But researchers looking more deeply at long Covid patients have found visible dysfunction throughout the body.
Studies estimate that perhaps 10 to 30 percent of people infected with the coronavirus may develop long-term symptoms. It’s unclear why some people develop long Covid and others don’t, but four factors appear to increase the risk: high levels of viral RNA early during an infection, the presence of certain autoantibodies, the reactivation of Epstein-Barr virus and having Type 2 diabetes.
The Immune System
“Dang, why am I always so sick?”— Messiah Rodriguez, 17
Long Covid patients appear to have disrupted immune systems compared to post-Covid patients who fully recover. Many researchers believe chronic immune dysfunction after a coronavirus infection may set off a chain of symptoms throughout the body.
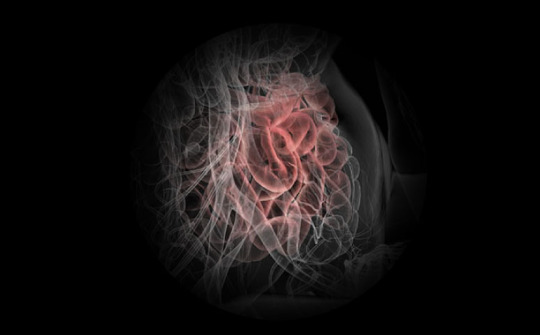
One possibility is that the body is still fighting remnants of the coronavirus. Researchers found that the virus spreads widely during an initial infection, and that viral genetic material can remain embedded in tissues — in the intestines, lymph nodes and elsewhere — for many months.
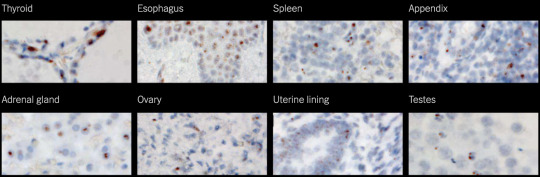
Figure: Coronavirus RNA is visible in different body tissues at 500x magnification. Daniel Chertow et al., preprint via Research Square
Ongoing studies are trying to determine if these viral reservoirs cause inflammation in surrounding tissues, which could lead to brain fog, gastrointestinal problems and other symptoms.
Figure: Coronavirus components persist in one patient’s small intestine, 92 days after the start of their Covid symptoms. Christian Gaebler et al., Nature
Researchers have also found evidence that Covid may trigger a lasting and damaging autoimmune response. Studies have found surprisingly high levels of autoantibodies, which mistakenly attack a patient’s own tissues, many months after an initial infection.
A third possibility is that the initial viral infection triggers chronic inflammation, possibly by reactivating other viruses in the patient’s body that are normally dormant. The reactivation of Epstein-Barr virus, which infects most people when they are young, might help predict whether a person will develop long Covid, one study found.
Inside the intricate world of the immune system, these explanations may coexist. And just as different long Covid patients may have different symptoms, they may also have different immune problems, too. Identifying the problems that are central to each patient’s illness will be critical for guiding treatment, said Dr. Akiko Iwasaki, an immunologist at Yale.
For instance, a patient with autoantibodies might benefit from immunosuppressive medication, while a patient with remnants of the Covid virus should receive antivirals, Dr. Iwasaki said. “Depending on what each person has, the treatment would be quite different.”
The Circulatory System
“Something as simple as climbing on a ladder all of a sudden became a mountain.”— Eddie Palacios, 50
Many long Covid patients struggle with physical activity long after their initial infection, and experience a relapse of symptoms if they exercise. Initial studies suggest that dysfunction in the circulatory system might impair the flow of oxygen to muscles and other tissues, limiting aerobic capacity and causing severe fatigue.
In one study, patients with long-lasting Covid symptoms had unexpected responses to riding a bike. Despite having apparently normal hearts and lungs, their muscles were only able to extract a portion of the normal amount of oxygen from small blood vessels as they pedaled, markedly reducing their exercise capacity.
One possible culprit: Chronic inflammation may damage nerve fibers that help control circulation, a condition called small fiber neuropathy. The damaged fibers, seen in skin biopsies, are associated with dysautonomia, a malfunction of automatic functions like heart rate, breathing and digestion that is very common in long Covid patients.

Figure: Chronic inflammation in long Covid patients may damage small nerve fibers. Peter Novak et al., Annals of Neurology
These findings demonstrate that people with long Covid are suffering systemic physical problems, rather than just being anxious or out of shape, said Dr. David M. Systrom, an exercise physiologist at Brigham and Women’s Hospital who helped conduct the bike study.
“You can’t make up small fiber neuropathy by skin biopsy. That isn’t in somebody’s head,” Dr. Systrom said. “You can’t make up poor oxygen extraction to this degree. All of these are objective measures of disease.”
South African researchers found another circulation problem: Microscopic blood clots. Tiny clots that form during an initial Covid infection will typically break down naturally, but might persist in long Covid patients. These clots could block the tiny capillaries that carry oxygen to tissues throughout the body.
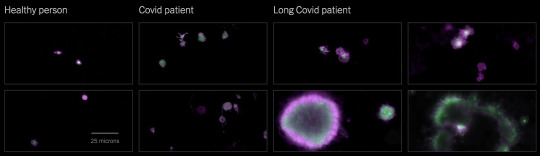
Figure: Platelets in the blood can become hyperactivated in Covid and long Covid patients, contributing to microclots. Etheresia Pretorius et al., Cardiovascular Diabetology
Inflammatory substances called cytokines, which are often elevated in long Covid patients, may injure the mitochondria that power the body’s cells, making them less able to use oxygen. Walls of blood vessels may also become inflamed, limiting the uptake of oxygen.
Whatever the cause, low oxygen levels may contribute to long Covid’s most common symptom, severe fatigue. Some long Covid patients meet the criteria for ME/CFS (also known as chronic fatigue syndrome), which often starts after a viral infection. Researchers have found that ME/CFS patients also suffer from a lack of oxygen triggered by circulatory problems. That puts enormous strain on the body’s metabolism and makes simple activities feel like strenuous exercise.
The Brain

“I approach a red light, my brain knows that it’s red, but it’s not reacting to the rest of my body to put my foot on the brake. Do you understand how terrifying that is?”— Samantha Lewis, 34
Even people with mild cases of Covid can experience sustained cognitive impairments, including reduced attention, memory and word-finding. Possible long-term neurological problems from Covid constitute “a major public health crisis,” according to Dr. Avindra Nath, the clinical director of the National Institute of Neurological Disorders and Stroke.
Researchers found a wide range of dysfunction in the brains of long Covid patients. Although it is unclear how often the virus directly penetrates the brain, even mild infections appear to cause significant brain inflammation, according to the researchers, who included Dr. Nath, Dr. Iwasaki and Dr. Michelle Monje, a neurologist at Stanford.
Infections may trigger the over-activation of immune cells called microglia in a way that appears similar to the process that can contribute to cognitive problems in aging and some neurodegenerative diseases.
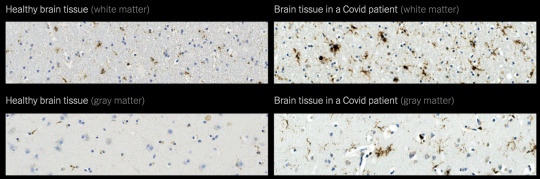
Figure: Microglia are activated in the brain of a Covid patient, contributing to brain inflammation. Anthony Fernández-Castañeda et al., preprint via bioRxiv. Photos: Myoung-Hwa Lee
Another research group found that long Covid may significantly reduce the amount of blood that reaches the brain, a finding that has was also seen in patients with a related chronic condition, ME/CFS, before the pandemic.
The Lungs

“I couldn’t breathe. It literally felt like someone was sitting on my chest.”— Angelica Baez, 23
Shortness of breath is a frequent symptom of long Covid. But common lung tests — including chest X-rays, CT scans and functional tests — often come back normal.
Using specialized M.R.I. scans, a team of British researchers found preliminary evidence of lung damage in a small group of long Covid patients who had never been hospitalized. Detailed scans of their lung function indicated that most of the patients took up oxygen less efficiently than healthy people did, even if the structure of their lungs appeared to be normal.
The researchers cautioned that a larger group of patients will be needed to confirm the findings. If the results hold up, possible explanations for the observed shortness of breath include microclots in lung tissues or a thickening of the blood-air barrier that regulates the uptake of oxygen in the lungs.
Living With Long Covid
“It’s really not something you can push through.”— Dr. Abigail Bosk
Many hospitals now offer post-Covid clinics or recovery programs, which bring together doctors with experience treating long Covid patients. Given the number of patients, some doctors and programs have long waits for appointments. It can help to plan ahead and try multiple options.
— Survivor Corps keeps a directory of post-Covid clinics.
— Dysautonomia International offers a list of doctors with experience treating autonomic disorders commonly seen in long Covid.
— Body Politic hosts a Covid support group where thousands of long haulers share information and advice on Slack.
— The Long Covid Support Group hosts a community on Facebook.
— The Royal College of Occupational Therapists offers advice for managing post-Covid fatigue.
— An essay from Maria Farrell offers advice on how to get well, and the importance of making time to rest.
— ME Action, a group supporting people with ME/CFS, offers advice to long Covid patients on how to manage symptoms.
— Americans with long Covid may qualify for disability benefits, although without conclusive medical results, many people face roadblocks.
— Three leading researchers into long Covid often share information about the latest findings on Twitter: Dr. Amy Proal, a microbiologist at PolyBio Research Institute; Dr. David Putrino, the director of rehabilitation innovation for the Mount Sinai Health System; and Dr. Iwasaki, the Yale immunologist.
— Health Rising covers the latest research into long Covid, ME/CFS and other chronic illnesses in detail.
— Gez Medinger, a video producer, interviews some prominent researchers into long Covid on YouTube.
— A video interview with Dr. Svetlana Blitshteyn, a neurologist and the director of the Dysautonomia Clinic, offers advice for treatment and an overview of current research into autonomic disorders.
— A detailed guide to understanding, treating and living with orthostatic intolerance is available from the Johns Hopkins Children’s Center.
Source: by Josh Keller (The New York Times). Illustration by Violet Frances for Bryan Christie Design. Produced by Jonathan Corum. Additional reporting by Pam Belluck and Amanda Morris.
1K notes
·
View notes
Photo






Anatomical studies and drawings by Leonardo da Vinci
Leonardo da Vinci (1452-1519), known as one of the pivotal figures in the development of Western art, was also one of the most original and perceptive anatomists of his or any other era. Although he spent over 25 years investigating the workings of the human body, only a few friends and associates had any intimation of the extent of his medical research. He never taught the subject and never published any of his findings.
Source: Leonardo Da Vinci: The Mechanics of Man (by Martin Clayton and Ronald Philo); Royal Collection Trust
11K notes
·
View notes
Text
I prep for sickle cell exchanges all the time in the Blood Bank. They often require specific antigen negative units (often Rh family antigens) or even washing of the unit on top of testing for Hgb S. Some exchanges even exceed 14 units for one transfusion sitting.
14 Things You May Not Know About Sickle Cell
The problem with Sickle Cell is that it’s a bit too complicated and most people don’t understand how it works. So here are a few basic facts from you might want to know.
[We’re not doctors or medical professionals. We recommend you seek professional medical advice if you think you may be affected by Sickle Cell. If you have any more suggestions to add to this list please let us know]
1. You can't “catch” Sickle Cell
Sickle Cell Disease (also known as Sickle Cell Disorder or Anaemia) is not contagious. Repeat, you can not catch it. It's passed down to a child from its parents genetically.
2. Sickle Cell is NOT a terminal disease
Sickle Cell is very painful and serious disease which can cause a range of health issues and in some cases short life expectancy. In Nigeria 98% of children born with Sickle Cell Disease die before they’re 5 years old. However, when diagnosed early and with support, it's also a manageable condition. There’s no practical cure yet, but people with the disorder can live into their 50s, 60s and beyond when they manage their condition carefully. The point is, people with Sickle Cell should be hopeful and their families and friends shouldn’t consign them to an early death.
3. People with Sickle Cell trait are usually perfectly healthy carriers
People who have the genetic trait also known as "AS", “AC” or one of the Thalassemia variant statuses, do not normally suffer any symptoms. There are some exceptions to this but it’s generally not a health issue if you carry the trait. People who have “full” Sickle Cell Disease, also referred to as SS or SC, will likely have significant health difficulties however.
4. The Sickle Cell "trait" is extremely common in Ghana and other African countries.
Some statistics say that between 20-25% of all Ghanaians and Nigerians have either the Sickle Cell trait AS or AC. Most of us don’t know we have it because it’s normally harmless, so you’d never be able to guess without a proper test. Some of those tests don’t look for AC, so people should specifically ask for AS, AC and Thalassemia screening.
5. If two parents who have the Sickle Cell “Trait” have a baby, it might be born with full Sickle Cell Disease
If a mother and father have one of the Sickle Cell traits, the future child is at significant risk of being born with "full" Sickle Cell Disease. There's a 1 in 4 chance this will happen. If you choose to take that risk, you should be prepared and speak to a doctor about treatment and testing of the child. Before having children, we recommend you ask a doctor or clinic to check your status and for them to provide genetic counselling if you carry the trait.
6. Getting tested for Sickle Cell trait will NOT ruin your life.
If you have it, the trait doesn’t normally cause any health problems. Then you and your future partner can make informed decisions when it comes to making babies. Remember that if both parents are carriers, there is a 1 in 4 chance the baby will have full Sickle Cell Disease. There are other situations like when one parent has full ‘SS’ sickle cell and the other has ‘AS’. In those cases it’s always wise to talk to an informed, up to date doctor before having children.
7. People with Sickle Cell are not sick all the time!
People with Sickle Cell Disease feel okay most of the time. When they have a ‘crisis’, that’s when the mis-shaped blood cells prevent enough oxygen getting around the body and the pain starts. At this stage, they often need to be admitted to hospital for treatment with pain killers, hydration and other treatments.
8. People with Sickle Cell can live full, productive lives.
Many successful Ghanaians in business, entertainment and government have Sickle Cell Disease. Yes, even though Sickle Cell Disease is a serious health problem, when it’s managed well, sufferers can live productive lives, have children and work. They deserve consideration from others when they’re sick, but they shouldn’t be discriminated against.
9. Don't wait, don't leave it too late, find out if you have the trait!
Relax, having the trait is NOT like finding out you have a disease because there are is no suffering and it's not contagious. You will be simply be able to make informed decisions about having kids with your future or current partner. Go to your doctor, clinic or ask someone you trust to suggest a testing facility near to home.
10. Sickle Cell children can ONLY be born to parents who BOTH carry the trait
That's right, if a kid has Sickle Cell Disease, the kid’s parents both have the trait, or have Sickle Cell. There are no known exceptions, despite what some men might like to believe.
11. There is no available cure for Sickle Cell Disease
There are medical treatments like Hydroxyurea but no practically available cure. Even though this is a such huge health, social and economic problem in Africa, the research and funding levels are astonishingly low. Maybe that’s because most of the people who have the condition can’t afford to pay for expensive treatments.
12. Sickle Cell Stigma is wrong.
People with Sickle Cell Disease have a tough time, they deserve admiration and support. They didn’t catch it, it happened to them before they were born. We all have friends and family with Sickle Cell Disease, let’s treat them with the respect they deserve.
13. Sickle Cell is not a “curse”
It's a genetic disorder not a curse. It’s serious, but people who manage their Sickle Cell Disease can live long happy lives. If anyone tries to tell you something different, they don’t know what they’re talking about.
14. People with Sickle Cell are not immune to Malaria
People with the “AS” trait have more immunity than those without, but people with full Sickle Cell Disease have no immunity and are actually at greater risk.
15. Not only black people can have Sickle Cell
Sickle Cell is very common in Africa and amongst people of African descent. However, it's also prevalent in the Middle East, Asia, North and Latin America.

For a medical explanation of Sickle Cell, please check out this page from the UK’s NHS.
If you have Sickle Cell and want advice on managing your condition, this page has some good advice.
If you want to help us spread the word in Ghana, please come and join our Facebook Page.
Thanks!
[email protected] | giftyfoundation.org
74 notes
·
View notes
Text
Gallstones (Cholelith)
Very common incidence –> up to half a million surgeries per year
Predisposing factors:
Gender: 3x higher incidence in women than men
Race/ethnicity: Native Americans and Caucasians have a higher incidence
Age: 20% seen in patients older than 65
Diet: high fat diet and obesity can drive stones from high cholesterol
Pregnancy
Hemolytic disorders: causes increased bilirubin
Cholesterol Stones: >75%

Usually solitary but can come in multiple
Forms in bile with supersaturated cholesterol or from decreased bile acids
Seen in the 4 Fs: Female, Fertile (pregnancy, hormone therapy), in the Forties, Fat (obesity)
Pigmented Stones:

Black stones:
Usually multiple
Formed from calcium bilirubinate
Seen in hemolytic anemia, sickle cell disease, cirrhosis
Brown stones:
Formed from alternating layers of calcium bilirubinate and cholesterol
Seen in biliary infections, liver flukes
Clinical Features:
Mostly asymptomatic or minor symptoms
Chronic cholecystitis
Obstruction of the gallbladder cystic duct: colic pain, fever
Obstruction of the common bile duct: jaundice, ascending infection, gangrene
30-50% seen on routine x-ray films
Complications:
Impaired lipid digestion
Acute and chronic cholecystitis, gangrene
Biliary colic
Ascending infection
Acute pancreatitis
Treatment:
Surgery
Lithotripsy: crushing of gallstones with outside energy
Dissolution drugs
148 notes
·
View notes
Text
Part 1: Metal Splints - Can You X-ray Through Them?
Splinting is an important part of the trauma resuscitation process. No patient should leave your trauma resuscitation room without splinting of all major fractures. It reduces pain, bleeding, and soft tissue injury, and can keep a closed fracture from becoming an open one.
But what about imaging? Can’t the splint degrade x-rays and hamper interpretation of the fracture images? Especially those pre-formed aluminum ones with the holes in them? It’s metal, after all.

Some of my orthopedic colleagues insist that the splint be removed in the x-ray department before obtaining images. And who ends up doing it? The poor radiographic tech, who has no training in fracture immobilization and can’t provide additional pain control on their own.
But does it really make a difference? Judge for yourself. Here are some knee images with one of these splints on:


Amazingly, this thin aluminum shows up only faintly. There is minimal impact on interpretation of the tibial plateau. And on the lateral view, the splint is well posterior to bones.


On the tib-fib above, the holes are a little distracting on the AP view, but still allow for good images to be obtained.
Bottom line: In general, splints should not be removed during the imaging process for acute trauma. For most fractures, the images obtained are more than adequate to define the injury and formulate a treatment plan. If the fracture pattern is complex, it may be helpful to temporarily remove it, but this should only be done by a physician who can ensure the fracture site is handled properly. In some cases, CT scan may be more helpful and does not require splint removal. And in all cases, the splint should also be replaced immediately at the end of the study.
In my next post, I’ll look at the use of CT scans when this type of splint is in use.
Source: http://thetraumapro.com/?p=3633
70 notes
·
View notes
Photo
Now that smallpox has some news attention...

Comparing the Sizes of Microorganisms Up to 1mm
246 notes
·
View notes
Photo
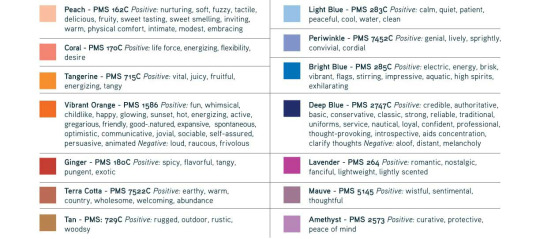
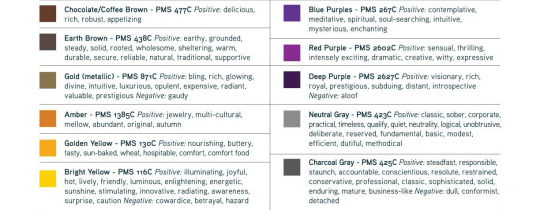
Think about how we perceive certain shades across marketing, social media, businesses, etc.! We are influenced far more subliminally than we realize.



379K notes
·
View notes
Text
In the first year of the pandemic I remember epidemiologists linking COVID to cardiovascular behaviors. In my facility, a lot of COVID patients in 2020 were going on ECMO.
Cautionary
A while back I had a COVID patient transferred to us from an OSH because they developed an interesting and complex complication from their COVID infection.
This person ended up developing retroperitoneal hematomas from lumbar arterial hemorrhages, presumably from endothelial damage and apoptosis from COVID. It should be known that this person was unvaccinated but had no other comorbidities associated with "bad" COVID infection. Also no other reason to explain the hemorrhaged (trauma, clotting factor problem, etc).
I admitted this person and they were a hot mess when they came in: on 3 pressors (while I was adding a 4th), hemorrhaging in the belly after one failed IR attempt to stop the bleeding, and gradually developing abdominal compartment syndrome from the massive about of blood in their belly. I spent the first 7 hours of my shift with this patient only because they were too unstable to go to imaging or IR without a provider present in case they coded. Literally followed them around with the box of blood product and just handing the nurse more blood. It was ridiculous.
They ended up going for an ex/lap and are doing better now. Long road ahead for recovery but they are alive.
I'm sharing this because I'm wondering if other people caring for COVID patients have seen hemorrhaging? We are all accustomed to the risk of clotting with COVID patients, but this was my first who was bleeding out. What were your experiences? How often do you see this?
154 notes
·
View notes
Photo

1. Fist: Make a fist around the epi-pen, don’t place your thumb/fingers over either end
2. Flick the blue cap off
3. Fire. Press down into the outer thigh (the big muscle in there), hold for 10 seconds before removing (the orange cap will cover the needle). Bare skin is best but the epi-pen will go through clothing. Avoid pockets and seams.
- Ring an ambulance even if everything seems to be fine!
500K notes
·
View notes
Text
Tips on Phlebotomy
I was assigned to report about Phlebotomy in our hospital tomorrow and I just want to share some of the contents of what I will be reporting. These tips may be helpful for you! :)
The secret to being a good phlebotomist is not to look for the vein, but to feel for it and you fill find it.
If you are having trouble getting blood, then please suck up your pride and ask someone else. It is okay to have an off day.
Smile and talk to your patient. If you act confident and calm, you will help your patient feel at ease.
If you can’t find a suitable vein in the bend of the arm, it’s okay to draw from an alternate site. But remember not to draw from anyone’s foot if they are diabetic.
One of the preconditions for dealing successfully with difficult patients is an initial analysis of the possible reasons for their behaviour.
Rotating the patient’s wrist gently in either direction while palpating can move the vein away from a close by tendon or bone, reducing the risk of hitting something other than the intended vein.
If the patient feels dizzy or faint in the middle of the venipuncture procedure, special precautions should be taken immediately. The procedure should be discontinued at once and the patient should be asked to place the head between the knees. After a brief resting period, the patient should be asked to lie down on the examination table. Chances are, the patient recovers after a period of monitoring and agrees that the procedure will be continued.
To put an apprehensive patient at ease, tell them that you’re going to count to 3 and that they should take a deep breath at that time. Wait for them to start to take the breath and stick them at the same time. Their mind will be at taking the breath that they won’t be thinking about the stick. Make sure not to hesitate when sticking. The slower you are at inserting the needle, the more it will hurt the patient. Be swift!
No fist pumping! Having the patient making a fist and holding it for better vein fill as opposed to pumping the fist. Pumping can increase the potassium level.
Direct pressure is best in reducing formation of a hematoma. Keep your finger on the phlebotomy site after the draw instead of letting the patient do it. Your finger was there first! Tape the cotton ball down tight for added pressure. And don’t let them bend their arm up either.
Most injections or draws are all in your mind. If you know you can get it, chances are you will! You must do it in your head first. Start by visualizing.
When drawing on a patient with “rolling veins”, ask them to lay their arm down, but instead of palm up, have them twist their wrist palm down. Great for elderly patients!
853 notes
·
View notes
Photo










A gift for your self still counts as a gift…right?
2K notes
·
View notes
Text
The Psychology of Stabbing

The way someone murders another person says a lot. In the instance of a knife, it can help gauge the height of a murderer. It can help determine their strength level and build. It can even tell you which hand they used.
But what about psychologically? Does it tell you anything about that? Absolutely.
Stabbings are often personal.
In order to stab someone to death, you have to be in a very close proximity to them. It’s not generally a weapon used in self defense or in professional killings. That’s because stabbing someone requires manually killing the person, it’s a lot more intense than pulling a trigger.
It usually involves a lot of anger.
Stabbings require a lot more strength than you would assume. The number of stab wounds also tells a lot about the killer. And if there is postmortem stabbing as well, it can signify that the killer was close to the victim and had a great amount of rage.
It’s often a crime of passion.
Of course this isn’t always true. But stabbing isn’t the most effective method of murder. If you don’t know where to stab, if you can’t stab deeply enough, and if it’s not the right kind of knife, the victim has a good chance of survival. Of course stabbings are serious and very lethal, but compared to some other methods it’s not as practical and effective. Especially in relatives or spousal murder, it just happens to be the weapon they have laying around.
516 notes
·
View notes
Photo


Nephrolithiasis is the formation of kidney stones, which form when solutes precipitate out into crystals in the urine. The most common type of stones are calcium oxalate stones, though other types include uric acid stones and struvite stones.
Nephrolithiasis 是指肾结石的形成,即当溶质在尿液中沉淀成晶体时形成。草酸钙结石是最常见的类型,其他类型的结石有尿酸结石和感染性结石。
Meducal! Joint us at Osmosis
106 notes
·
View notes
Photo
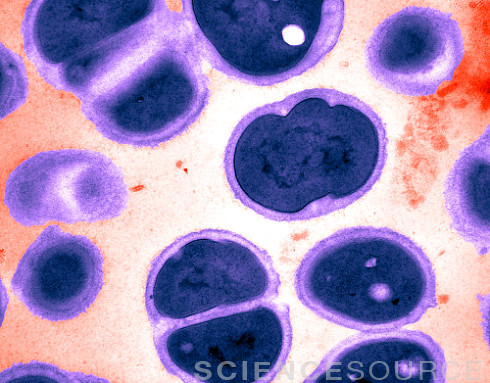
Gonorrhea (AKA The Clap) Is Excellent At Resisting Antibiotics
by Rina Shaikh-Lesko / NPR
People like to make jokes about gonorrhea.
Maybe it’s because this sexually transmitted disease is known as “the clap” (perhaps a reference to the French term “clapier,” meaning brothel, or to an early treatment – clapping a heavy object on the man’s sexual organ to get discharge to come out).
See More Images Of Neisseria Gonorrhea
As the old (and not very funny) joke goes, “if you spread it around, is it called applause?”
But a new study illustrates why this sexually transmitted disease is no laughing matter. Neisseria gonorrhoeae, the bacterium that causes gonorrhea, is developing resistance to the antibiotics that have successfully treated it for decades.
A global group of experts on sexually transmitted diseases published an article in the scientific journal, PLOS Medicine, outlining the challenges of drug-resistant gonorrhea. They surveyed 77 countries that participate in a global gonorrhea tracking program and found that more than 90 percent report some kind of antibiotic-resistant gonorrhea.
That’s bad news for patients. Because while gonorrhea doesn’t have the death toll that untreated HIV does — annual deaths from gonorrhea are about 2,300 — it still causes incalculable suffering. About 78 million adults contracted the disease in 2012, according to the World Health Organization. Symptoms include painful urination, itching and a pus-like discharge from the penis, vagina or anus, or a sore throat (in throat infections).
Read the entire article
119 notes
·
View notes