#C Diff Clinical Trials
Explore tagged Tumblr posts
Text
Major Article: SER-109, an Investigational Microbiome Drug to Reduce Recurrence After Clostridioides difficile Infection: Lessons Learned From a Phase 2 Trial
Major Article: SER-109, an Investigational Microbiome Drug to Reduce Recurrence After Clostridioides difficile Infection: Lessons Learned From a Phase 2 Trial

SER-109, an Investigational Microbiome Drug to Reduce Recurrence After Clostridioides difficile Infection: Lessons Learned From a Phase 2 Trial.
Barbara H. McGovern,1,a, Christopher B. Ford,1,a , Matthew R. Henn,1,a , Darrell S. Pardi 2 Sahil Khanna,2 Elizabeth L. Hohmann,3 Edward J. O’Brien,1 Christopher A. Desjardins,1, Patricia Bernardo,1, Jennifer R. Wortman,1, Mary-Jane Lombardo,1 Kevin…
View On WordPress
#C Diff Clinical Trials#Investigational Microbiome Drug to Reduce Recurrence After Clostridioides difficile Infection#Recurrent C diff Infection Clinical Trials#Seres Therapeutics SER-109
0 notes
Text
Monopolizing turds

Update 31 May 2023: an earlier edition of this article identified the price of Rebyota as $20,000; this was the rumored price prior to Rebyota’s release in December 2022, when Stephen Skolnick wrote the article I referenced. When Rebyota was actually released in 2023, the average wholesale price (AWP) was $10,800. Thanks to Benjamin Jolley for catching this error, and to Stephen Skolnick for getting to the bottom of it.
It’s been ten years — to the day! — since I first started writing about the bizarre, amazing world of turd transplants, in which a sick person receives a microbiotic infusion in the form of some processed poop from a healthy person:
https://web.archive.org/web/20130608030455/http://blogs.plos.org/publichealth/2013/05/29/why-diy-fecal-transplants-are-a-thing-and-the-fda-is-only-part-of-the-reason/
Gut biomes are one of those understudied, poorly understood medical areas that are both very promising and also full of sketchy medical claims from “supplement” companies, influencers, quacks and grifters. But in the decade since I first started tracking turd transplants (formally called “Fecal Microbiota Transplants” or FMTs), a growing body of sound science has emerged on the subject.
One thing that’s increasingly undeniable is that the composition of your microbial nation is related in significant ways to both your physical and mental health. What’s more, as antibiotic resistant “super bugs” proliferate, FMTs are becoming increasingly central to treating dangerous gut infections that otherwise stand a high chance of killing you.
“Eat Shit and Prosper” is Stephen Skolnick’s delightfully named newsletter about poop and health science. Skolnick is a physicist by training, but has a long history of collaboration with Openbiome, a nonprofit that coordinates between doctors, patients and donors to provide safe FMTs:
https://stephenskolnick.substack.com/
In an edition of Eat Shit from last December, Skolnick recounts the amazing history and dismaying future of FMTs. In 2013, the FDA announced it would regulate FMTs as “Investigational New Drugs,” which could only be administered as part of a registered clinical trial:
https://stephenskolnick.substack.com/p/a-monopoly-on-poop
At that point, FMTs were already in widespread use by docs to treat otherwise untreatable cases of Clostridioides difficile (C. diff), an antibiotic resistant bacterial infection that literally makes you shit yourself to death. These doctors were in no position to run registered clinical trials, which meant that they would have to stop using the most effective therapy they had for a potentially lethal infection.
Doctors and patients kicked up a fuss, and the FDA walked back its guidance, announcing that it would exercise “discretion” in enforcing its Investigational New Drug rule, giving a pass to docs who were treating C. diff with FMTs:
https://www.federalregister.gov/documents/2013/07/18/2013-17223/guidance-for-industry-enforcement-policy-regarding-investigational-new-drug-requirements-for-use-of
That’s where things have stood for the past decade or so. The “discretion” rule means that patients could still get FMTs, but their insurance wouldn’t cover it. But even if you had cash to pay for an FMT, your doc probably wouldn’t administer it for anything except a C. diff infection, despite the promising signs that FMT can help treat other conditions, and despite the generally safe nature of FMTs.
If your doc did give you an FMT, chances are good that they sourced their poop from Openbiome. Openbiome recruits very healthy people, gets them to poop in a bag, then processes the poop — removing nonbacterial solids, testing it for pathogens, freezing it, portioning it, and sending it to docs. All this is done at cost, and it’s not cheap: $1–2k/treatment, mostly due to cold-chain logistics (the poop is shipped at -80C).
Despite the cost, and despite the limitations on treatment, the Openbiome method has proved very reliable. Indeed, FMTs as a whole are pretty darned safe, with the most common side-effects being transient gas and bloating. In the past decade, there’ve been a total of six “adverse effects” associated with Openbiome’s 5,000+ procedures, all in severely immunocompromised people, and none conclusively linked to the treatment:
https://www.sciencedirect.com/science/article/pii/S0016508522003511/pdf
A decade into this system, the FDA has taken the next step forward — only it’s actually a step backwards.
During this intervening decade, a pharma company called Ferring has conducted clinical trials on FMTs and received approval for an FMT product called Rebyota. The process for making Rebyota is effectively identical to the process used by Openbiome: collect poop, remove solids, test for pathogens, add glycerol, freeze and ship.
The main difference between Rebyota and Openbiome’s poop is price. While Openbiome charges $1–2k per treatment, Rebyota charges $10,800
That’s some expensive shit!
Fine. Getting Rebyota through clinical trials means that insurers might start covering it, and perhaps some patients will prefer brand-name poop to open-source poop. But as part of the FDA’s approval of Rebyota, the agency also rescinded its “discretionary enforcement” guidance, making it illegal for docs to source their poop from Openbiome:
https://www.fda.gov/regulatory-information/search-fda-guidance-documents/enforcement-policy-regarding-investigational-new-drug-requirements-use-fecal-microbiota
For Ferring, this is a monopoly on shit, one that lets them charge patients $10.8k for poop that costs $1–2k to process. The FDA does not claim that this is being done in the name of safety. Instead, an FDA official told Skonick that the goal was to “incentivize innovation without creating an access crisis.”
That is, the FDA changed its guidance and put nonprofit stool banks out of business because it wants to incentivize pharma companies to perform expensive clinical trials, and it believes that these companies won’t pay for trials if they have to compete with the likes of Openbiome, which would make it impossible to charge 900% markups on poop.
Trials are important! Evidence-based medicine is important! But Ferring’s clinical trials didn’t tell us anything we didn’t already know. FMTs were already the best therapy we had for C. diff. Testing Rebyota against a placebo didn’t tell us anything new — unlike testing Rebyota against the existing therapies, e.g. product from open stool banks.
Such a trial might have given rise to a very different regulatory outcome, because the cure rate reported by Rebyota is much lower than the cure rate from Openbiome’s own interventions:
https://link.springer.com/article/10.1007/s40265-022-01797-x
That is, using the $1k poop from Openbiome seems to be much more effective than using the $10.8k poop from Ferring. But Openbiome, a nonprofit, hasn’t been able to perform the kind of rigorous — and expensive — clinical trial that Ferring funded.
This points to a significant problem with the FDA’s model. The agency wants good clinical data for the medicines it regulates, as it should, It presumes that the only way to get that data is through granting commercial exclusivity to a for-profit, which ends up costing patients vast sums, and locking many patients out altogether.
This creates all kinds of new dangers. 150,000 people/year in the US contract Recurrent Clostridium difficile Infection (RCdI). FMT increases the cure rate by 20% relative to antibiotics alone. That means that if everyone with RCdI gets a poop transplant, 30,000 extra people will get better. That’s a big number!
For well insured people, Rebyota probably represents a cash-savings — if your insurance covers the $10,800 procedure, you might pay $500 out of pocket, which is far less than the $1–2K you’d pay to get an Openbiome poop transplant. But if you’re uninsured or underinsured, the FDA’s new enforcement rules mean that you’re now on the hook for $10,800.
The FDA did carve out a loophole: if your doc or their hospital are willing to prepare the poop transplant themselves, they can administer that. On the one hand, preparing a poop transplant isn’t that hard — some people do them at home, on their own:
https://web.archive.org/web/20211015060558/https://thepowerofpoop.com/epatients/fecal-transplant-instructions/
But on the other hand, there’s been exactly one death conclusively linked to FMT, and it was from one of these hospital-prepared transplants (the patient had just had a marrow transplant for cancer that wiped out their immune system, and the donor had a novel pathogen that the hospital failed to test for).
So the FDA has created a situation where, if you can’t afford a $10,800 proprietary formulation, your only option is to convince your doc or hospital to prepare their own poop transplant, which will cost less than the $10.8k for Rebyota, but more than the $1–2k from Openbiome, which has all kinds of economies of scale. And if you do manage it, you’ll be getting a procedure that has a much worse safety track-record than the Openbiome process that the FDA just killed.
The FDA has an important role to play here, but as with so many policy questions, how the FDA plays that role depends on things that are far upstream from the agency and its decisions. The choice to fund medical trials through the promise of exclusivity — and with it, extremely high margins — puts the FDA in the position of choosing winners in the marketplace: Ferring wins, Openbiome loses.
Ironically, this is the thing that exclusivity is supposed to prevent. By using profit to incentivize medical research, the FDA is supposed to be recruiting the Invisible Hand as its partner in regulation. But exclusivity is incompatible with the idea of medicine as a public good. The tens (hundreds) of millions that Americans will pay for $10.8k poop transplants from Ferring will add up to far more than it would cost to underwrite clinical trials for an open process like Openbiome’s.
The result: both Americans’ wallets and Americans’ guts suffer.
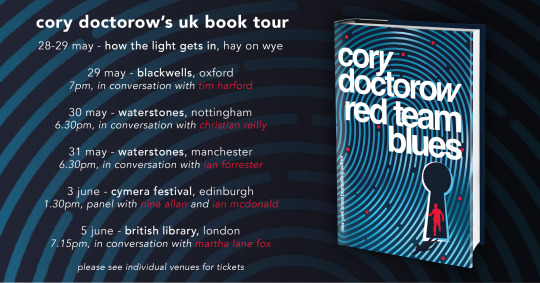
Catch me on tour with Red Team Blues in Hay-on-Wye, Oxford, Manchester, Nottingham, London, and Berlin!

If you’d like an essay-formatted version of this post to read or share, here’s a link to it on pluralistic.net, my surveillance-free, ad-free, tracker-free blog:
https://pluralistic.net/2023/05/29/oh-shit/#rebyota

[Image ID: A poop emoji wearing a top hat and a monocle, posed against a backdrop of e coli bacteria seen through a high-resolution microscope.]
#pluralistic#stool bank#eat shit and live#pharma#fda#regulatory capture#fecal transplants#microbiomes#rebyota#openbiome#c diff#fmt#fecal microbiota transplant
271 notes
·
View notes
Text
everyday is Friday the 13th when you're studying
100 days of productivity
day 13
RS/CVS
NIPPV has best effect between pH 7.25-7.35; but generally trial NIPPV before tubing unless imminent or current respiratory collapse (or other indications such as failure to protect airway)
constrictive pericarditis vs tamponade: differentiate with y-descent of JVP; this is *absent* in tamponade, but otherwise they are clinically very similar
in the absence of thromboembolic events, pts with bioprosthetic valve replacements *do not need* warfarin (low dose aspirin sufficient)
asthma ICS dose: budesonide: low dose < 400 mcg; mod dose 400-800 mcq; high dose >800 mcg
ICS dose conversion: budesonide = beclomethasone, multiply budesonide dose x2 to get fluticasone dose
Rheum/Derm
pseudoxanthoma elasticum: AR mutation in ABCC6 (ATP-binding cassette transporter) skin: cutaneous laxity + yellow papules in flexural regions; eyes: blue sclerae + peau d'orange of Bruch's membrane + retinal angioid streaks; GIT: upper GI bleed!; CVS: accelerated atherosclerosis w/ consequent IHD/CVA/PAD; rheum: demineralisation w/ reduced circulating pyrophosphate
microscopic polyangiitis and GPA cause kidney involvement with equal frequency; HSP causes IgA nephropathy with much less frequency (and much less severity)
tinea incognita = tinea corporis that has had topical steroid tx; may show florid fungal growth without characteristic tinea lesions (skin scraping w/ KOH stain is sufficient to dx)
inclusion body myositis (not to be confused with hereditary inclusion body myopathies): most common inflammatory muscle disease in adults! → sporadic, nonheritable progressive asymmetric weakening and wasting of both proximal and distal muscle groups (may mimic ALS but is a myopathy rather than a neuropathy and NCS/bloods will reflect that, eg, ↑CPK in IBM)
CNS
floaters + flashes of light = vitreous detachment
important ddx for Wernicke encephalopathy: cerebellar stroke. Do NOT forget the CT brain!
neuromyelitis optica: differentiate from MS w/ anti-NMO IgGs (such as anti-aquaporin 4 (AQP4) and anti-myelin oligodendrocyte glycoprotein (MOG))
pons = horiPONStal gaze palsy
SCD: T2-weighted hyperintensity of affected areas (dorsal column, lat corticospinal tracts, spinocerebellar tracts)
Haem/Onc
Stauffer syndrome: renal cell ca associated nonmetastatic hepatobiliary dysfunction (cholestatic enzyme pattern, elevated platelets/PT, hepatosplenomegaly, NORMAL bilirubin, NO jaundice)
GIT
FAP: the second most common cause of death after colorectal cancer is duodenal cancer
Whipple's disease: tx with 1-1.5 yrs of ampicillin or cotrimoxazole or doxy+HCQS, then assess, then continue tx if necessary
Psych/Toxo
sertraline specifically is used for agoraphobia due to best cost-effect ratio; other SSRIs are second line
long-term lithium side effects: LITHIUM: Leukocytosis, Intracranial hypertension, Tremor/Teratogen, Hair loss/Hypothyroid/Hyperparathyroid, Increased Urine (N-DI), Metabolic syndrome
other than hypokalaemia, other precipitating factors for digitoxicity include hypernatraemia, hypomagnesaemia and hypothermia
Misc
bezlotoxumab → C. diff toxin B
suvratoxumab → S. aureus alpha toxin
6 notes
·
View notes
Text
Fecal Transplant: an introduction…
Fecal transplant. Let face it, the name alone is enough to gross out pretty much anyone. It is, in fact, just what it sounds like: taking feces from a person whos is helathy and placing it in the colon of the sick patient. This process takes the “good” bacteria and microorganisms that is normally found in the gut of a healthy individual into the recipient, whose good bacteria is scarce or even non-existent most of the time due to high antibiotic use. This treatment offers great hope, no side effects have been reported in millions of procedures worldwide, a 90%+ success rate in certain conditions including autism, and many patients see improvement after just a few days. Despite the fecal treatment being around since 1958 and building considerable legitimacy from academic research, the FDA has not investigated it as a viable alternative to pills and other medicine. Many times, the culprit is actually the FDA-approved antibiotics that gradually decimates the good bacteria, while creating stronger and more resistant bad bacteria in patients, fecal transplant is the only solution for millions of people, most of them don’t even know it yet.
What could cause the healthy bacteria to decline in a person? Most sources say it is when a nasty, unhealthy bacteria strain known as Clostridium difficile, or C. diff for short, takes over due to an overuse of antibiotics. Normally the good bacteria maintain a balance with the bad, but this order can become disrupted by the very antibiotics used to treat a C. diff patient. The good bacteria get progressively wiped out with each round of antibiotics and C. diff can then thrive, outnumber the good, and get a stronger hold on the intestines.
C. diff on the rise…
C. diff infection cases have been growing in number during the last 30 years at an alarming rate. They were first thought of as merely a temporary negative side effect to antibiotics but as the bacteria strain has become more resilient to treatments over the years, it is now considered a serious health problem. As the years go by with more and more C. diff strains creating permutations, they’ve grown stronger and more resistant to medications used to cure them. Remember, the drugs used against C. diff usually kill off the healthy bacteria too. This “screens out” all but the most resistant, hearty C. diff bacteria that reproduce and take over more of the person’s intestinal real estate.
According to gastrointerologist and immunologist Alex Khoruts at the University of Minnesota, the fecal transplant bacteria indeed take over the ailing patient’s intestines and replace the once-thriving helpful bacteria. Think of it like sending in the healthy bacterial reinforcements to battle it out in the guts. This is enough to swing the advantage back to the good guys and the harmful C. diff is slowly killed off to regain a healthy balance.
Fecal donors
When it comes to finding a donor, yes a feces donor, most medical professionals ask their patients to choose one themselves. This could be a brother, sister, child, spouse, or other individual that is willing and has had tests to show they have a healthy gastrointestinal system.
The type of screening needed for a fecal donor is about the same standard as for a blood donation. This ensures they have no digestive diseases or other ailments which would reduce the fecal transplant’s success or, worse yet, introduce a new disease to the recipient. The lab work needed is not always covered by insurance and can create other hurdles also with respect to time and medical confidentiality.
DIY
Another alternative that has been proposed is to simply have the patients do the fecal transplant in their own home using an enema kit. The downside, as mentioned in Clinical Gastroenterology and Hepatology, is that too much of the transplant “material” may leak out and thereby result in an unsuccessful treatment. Supposedly seven patients have done the do-it-yourself fecal transplant at home safely and had a 100% recovery rate.
Fecal transplants, despite the lack of focused, formal FDA investigation seem to be gaining more popularity as a viable treatment. It has also been recommended that they be tried first in cases of severe C. diff infections as opposed to something to try as a last resort. What is also very thought-provoking is the research on how the intestinal bacteria can influence other health issues such as anxiety, depression, pre-diabetics, and obesity among others. Yes, a poop swap could boost your mood…
Fecal transplants are now undergoing clinical trials not in the United States, but in Canada. The FDA needs those in the medical field who are advocates of this treatment to provide more research and formally file to have this procedure approved. The researchers in the United States express some apprehension about the FDA-approval process, and about being able to answer all the potential questions arising from the proposal. Unlike drug approval petitions, which the FDA commonly deals with, feces is not classified as a drug or other patentable thing. Nevertheless, people are already trying fecal transplants at home to treat their debilitating C. diff infections. Medical providers need to be able to offer this safe, low cost treatment in a professional environment to achieve the best success rates.
1 note
·
View note
Text
Small Update, Long Post Sort of
I did buy a car, with the entirety of my savings account which was barely anything haha. Now I’m putting aside 250$ every pay check to pay off 2600$ in taxes. I won’t be able to make the full amount by April, but I’m still set back because I needed to buy a new battery for the car this past week.
HUMIRA savings plan decided to not renew and not tell me so I currently owe 500$ for the medication I need to stay stable, and currently will cost me 250$ a month.
On top of that our other salesperson quit, so I’m on 12 day stretches with one day off in the middle. Most people would think that’s fine but I’m already working overtime and that leads to flare ups. I’ve re-started the prednisone taper, which I learned from the clinical trial Dr causes severe IBS symptoms, and I started Amoxicillin for my psoriasis problem - which puts me at risk for C Diff and generally makes me feel worse - and also affects my birth control - and I specifically take continuous birth control because periods flare up my Crohn’s issues. Also Trumps tariff thing has made my company’s quotas go up to offset that, and I’ve been shorted of 500$ a month because they are unreachable.
So I’m feeling great! But I do want to say thank you to everyone who has supported me monetarily in the shop, who has been patient with shipping times (since my car was out of commission for a few days) and who has checked up on me.
A part of me still wants to be here for the witchcraft and community and whatnot but I’m honestly too busy at work, too physically affected by tapering off prednisone that my specialist literally thought I was not responding to Humira (I am), and trying to enjoy what time I have off with people I love. There’s a lot of other personal things I can’t divulge on that are affecting my mental health as well.
I do hope soon I can compile my own witchcraft and religious ideas and theories in a different platform, but for now I’m just too exhausted and stretched to my limits. If you ever have any questions or want to chat I am still here. I haven’t been able to truly do much in my own spare time except read and study traditional methods and more about Norse mythology. I’m learning Norwegian on duo lingo with my partner and since we are both Norse Pagan, that’s somewhat been the focus of my spirituality lately and all I can muster here and there.
I try to check in every once in a while, but I do hope everyone is doing well 🖤
13 notes
·
View notes
Text
An MS3 Guide to Internal Medicine Wards
I want to do internal medicine. I scoured the internet for guides on how to knock this rotation out of the park. Here is yet another take on how one can do well on this rotation, even if you don’t want to do IM.
I ended up honoring it and making 92nd percentile on the shelf. There will be a separate post on how to prepare for the shelf.
-----------------------------------------------------------------------------------------
Preparation
I got up early every morning to preround on my patients. When I first started rotation, I started off with one patient. I typically carried 3 patients and went up to 4 towards the end of my rotation. Get there earlier than you think you need because it sucks to scramble to prepare your notes for rounds only to find out that the plan for the patient changed in the interim. I got to the hospital around 7:15 for 9 AM rounds.
If your institution still uses paper lists, print copies of the list for everyone on the team and make sure to have the most updated version for the attending.
Read up on your patients on Up To Date. This will help you on pimping and on the shelf. If you have a new patient to present, you can shine by looking up differentials for your patient’s symptoms and presenting them. You can also check out all the treatment options on UTD and present the main ones as well. The key to standing out on rounds is being the one to put yourself out there to propose a plan for the patient, even if it ends up being wrong. It’s easy to just regurgitate what your resident’s note says. At least you tried to integrate your previous basic science knowledge with the clinical side.
The topic of studying will be covered in another post.
Rounds
Have your presentations down cold. There are many guides online on this topic such as this one by @pleasedotheneedfulhttp://pleasedotheneedful.tumblr.com/post/149283514726/how-to-write-a-cohesive-patient-notepresen-tation
It’s hard to figure out each attendings’ preferences such as how detailed they want you to be on the presentation or if they like walking rounds. Ask around within your class, the MS4s, or the residents.
For the most part, they want focused presentations that concentrate more on the plan for the patient. Some want to know all of the labs and vitals. Some want only the highlights. You also need time to read all of the consult notes to see their recommendations.
Know when to ask questions. Always try to look up the answer to your question if you have time before bothering anyone with it. Definitely keep them to a minimum if it’s a post call day and your list is long. If I was getting pimped, then I would be more likely to ask more follow up questions around then because that means we’re in education mode. You want to ask enough questions to where you appear engaged but not so much to where it gets annoying. But don’t be afraid to ask questions even if it’s really busy if it will impact patient care. I tend to ask questions while walking in the hall during walking rounds but I also ask during table rounds depending on the vibe of the room.
Pimping. It is okay to not know the answer. Always try to make a guess, even if it’s a stretch. I have said I don’t know plenty of times. I’ve seen fourth years who don’t know the answer. I’ve seen residents and fellows who don’t know the answer. Most attendings I’ve dealt with have been pretty nice if I don’t know. I think pimping can be good so that it it keeps me on my toes since the fear of God is put in me. A great phrase is “I don’t know but I will find out and we can discuss it later on.” I remember questions I’ve gotten right and especially the ones I’ve gotten wrong that everyone else on the team knew except for me.
Making a good impression
Ask for feedback. I get super anxious about possibly hearing negative things so I hate doing this. At my school, preceptors evaluate you on if you asked for feedback, how you handle criticism, and if you actually tried to improve. Try to ask 2 weeks in or so about what can you work on to improve things like your presentation, differentials, treatments plans, history collection, ect. They will notice if you step it up or if you continue on. They will definitely notice you if you slack off after getting good feedback initially.
It’s not just about impressing the attending. The residents and especially the senior resident are the ones in contact with you the most. I only interacted with the attending on morning rounds. The residents give their feedback to the attending for your evaluation. Yes, we are close in age to the residents and yes it’s great to have fun at work. I love joking around and have an occasional streak of dark humor but I don’t swear, talk about the times I’ve been intoxicated, complain about the work we have to do, or complain too much about the patients.
Don’t freaking text during rounds, especially while in a patient room. Yes, people still are getting in trouble for that.
After rounds
Check on your patients. Most patients and their families don’t really know what’s going on because we storm in there as a group during rounds and then abruptly leave. It’s always great to double back and check their understanding of what’s going on. You as the student are usually the person on the team that’s the closest to the patient in terms o medical knowledge. Once they have an understanding of the disease process and why we treat them with whatever treatment, then they can hopefully keep it up after discharge.
Stay organized. I had a patient list that I wrote notes on during rounds of things to do particularly focusing on my patients but including things to do for other patients. The residents will really appreciate it if you help update the list, remind them of orders that need to be put in, and notify them of any results/consults you’re waiting for. So I refreshed my patient charts all day long to make sure everything was there. When we see an abnormal critical result or consult recommendations and update the residents, we are helping to expedite care.
I really can’t stand doing random clerical stuff like making appointments or filling out paperwork but just make yourself volunteer to do it. My school is trying to cut back on using medical students for this.
Do not lie. If you didn’t check something on your physical exam or forgot to ask a question, own up to it. It’s embarrassing but it’s better than being caught in a lie or your made up information ends up affecting the treatment plan. You won’t get any more responsibility if they can’t trust you.
Extra
Read the literature. My attending specifically mentioned that he expects this from honors level students. This is how you step up your game. You want to show that you are trying to elevate your knowledge. You’ll definitely get style points for referencing the literature when you propose your treatment plan by citing statistically significant results from randomized control trials. For example, one of my patients had refractory C diff that wasn’t responding to traditional antibiotics of vanc per rectum and PO with metronidazole or with fecal transplants. So I needed to step up and look into other options that we can talk about on rounds. I read some articles on newer therapies that were compared to gold standard therapies. I summarized the studies in a few sentences so that everyone can be on the same page. Then we talked pros and cons. Another example is that if your patient is on some newer drug you’ve never heard of, you can look up what it is, the mechanism of action, and major indications. Then present a very brief FYI on it as it will help educate your team. Definitely be cautious as to how often and when you try to educate others as it may come off as overbearing or if it may put your team behind schedule. You do not want to appear as a know it all or that you like to hear yourself talk because it’s hard to shake that impression.
Preclinical material professors seem to like gunners, at least in my experience. It’s way different in the clinical setting because you’re surrounded by people who’ve been in the game longer than you. All of us know how to pick out a gunner. So word will spread fast if you’re terrible to work with and then you end up on the Do-Not-Rank list.
You are not going to get a thank you for everything you do. Don’t take it personally. Except if someone takes credit for your work, so in that case they can fuck right off.
The <1/15/50/85 rule. A fantastic pimp deflector. If you are being pimped on some statistic and the pretest probability seems to be very low, say < 1%. Low probability then 15%. For example, if someone asks you what percentage of strokes are ischemic and you feel pretty confident that the vast majority of them are ischemic, then say 85%. Usually you’ll be pretty close.
The most important things
The most important thing is to advocate for your patient, regardless if an attending is around. 100% of students has thought about how they wish an attending could have seen how hard you work day in and day out but that’s not gonna actually happen much. The patient will remember how you treated them and all the things you did to help them.
Teamwork makes the dream work. Even if you can’t stand people on your team, you have to suck it up because the ultimate goal is patient care.
It is okay to take some time off to yourself. Some nights, all you can really do is watch TV and drink wine on a post call day or after doing not that well on a quiz you didn’t have time to prepare for because you’re freaking exhausted working 6 days a week.
244 notes
·
View notes
Text

ICYMI: OFA Newsroom: The C Diff Foundation Assures Patients C. diff. Clinical Trials Continue to Move Forward Safely http://dlvr.it/RtBfXr
0 notes
Text
Lupine Publishers | Genesis, Evaluation and Progression of A Breakthrough Discovery to Efficiently Cure Cancer Through Use of Dr. M.S. Reddy’s Multiple Mixed Strain Probiotics as Adjuvants Along with the Traditional Cancer Therapies, Through Restoration of Healthy and Balanced Intestinal Microbiota and their Microbiome

Lupine Publishers | LOJ Pharmacology & Clinical Research
Abstract
A breakthrough, Multiple Mixed Strain Probiotic Therapy, although originally designed to cure hospital acquired infections, has been discovered serendipitously by Dr. M.S. Reddy to treat cancer with greatest accuracy (60% as opposed to current 20%), with least or no side effects and least or no relapse, when used as an adjuvant therapy along with standard cancer therapies, including immune checkpoint therapy. This discovery can be further refined and improved to treat cancer at 80 to 100% efficacy to save lives of millions of people in the world by significantly improving immune system through positive manipulation of the human gut microbiota and their microbiome. The results of the clinical trials are outlined along with discussion and conclusion. The references listed have been limited to the latest, significant, and directly applicable research discoveries only.
Keywords: Dr MS Reddy’s multiple mixed strain probiotic therapy to treat hospital acquired infections; Nosocomial infections; Dr MS Reddy multiple mixed strain adjuvant cancer therapy; Microbiota; Hospital acquired infections; Immune checkpoint therapy; C Diff; MRSA; Microbiome
Introduction
A brief history on statistics of the cancer episode in the world. The International agency for Research on Cancer (IARC), a division of The World Health Organization (WHO), estimated that the global cancer epidemic rose to 18.1 million new cases and 9.6 million deaths in 2018 alone. The IARC reports 1 in 5 men (20%) and 1 in 6 women (16.66%) worldwide develop cancer during their lifetime. 1 in 8 men (12.5%) and 1 in 11 women (9.09%) die from the disease. In addition, every sixth death in the world is due to cancer. Assuming world population is 7 billion and assuming the ratio of male to female is 50:50, 700 million men and 583 million women will develop cancer during their life time and 437 million men and 318 million women will die of cancer. These figures are astronomical, mind blowing, and downright scary, unless something is done to prevent or cure cancer efficiently with 100 percent accuracy, without any relapse.
Materials, Methods, and Discussion
The question here is, how did Dr. M.S. Reddy’s discovery to treat cancer came about serendipitously? In the year 2016, Dr. M.S. Reddy, after working extensively for four decades on probiotics, published a breakthrough research article on the usage of Multiple Mixed Strain Probiotic Therapy to treat or prevent the hospital acquired or nosocomial infections caused by Clostridium difficile (C. diff), and Methicillin Resistant Staphylococcus Aureus (MRSA) [1-4]. He has isolated and selected the strains of Probiotics which are naturally resistant to several antibiotics and sulfonamides to use in this discovery. Dr. M.S. Reddy has studied and confirmed through thorough research that, the antibiotic resistance was not coded by the plasmids but by the chromosol genes, thus it is safer to use these Multiple Mixed Strain Probiotics to eliminate the free exchange of plasmids to the pathogenic bacteria [5]. The Multiple Mixed Strain Probiotic Strains belonging to different genera and species (with varied physiological characteristics) were grown separately in selected nutritionally balanced media, not only to maximize their cell numbers and their single cell morphology (as opposed to chain formation), but also to significantly improve the quantity of their end products of growth i.e. immunomodulins, bacteriocins, and specific and nonspecific bio-active peptides etc. Such individually grown single strain probiotics were blended in fixed proportions and frozen using liquid nitrogen, to be used as therapeutic agents administered through oral route [3]. Unlike the popular thinking, the significant feature of the discovery is that the probiotic bacterial cultures alone (without their prior growth end products) did not cure the hospital acquired infections. However, the multiple growth end products of these Multiple Mixed strain Probiotics (immunomodulins) along with the active probiotic bacteria significantly cured the nosocomial infections [6].
It was also determined and confirmed that the multiple antibiotic resistant pathogenic bacteria i.e. C. diff etc. was initially inhibited (in vivo) through the immunodolation exerted by the Multiple Mixed Strain Probiotic growth end products along with the dendritic cells picked up probiotic cell wall antigens. The immunomodulation induced by probiotics was through production of IL-10, retinoic acid, TGF-Beta with resultant well balanced activation of T-reg cells [7]. The excess inflammation caused due to immune stimulation as a response to the pathogenic bacterial peptides of C. diff bacteria, through activation of Th-1, Th-2, Th-17 and excess production of IGA, was reduced predominantly through activation of T-reg cells stimulated by Multiple Mixed Strain Probiotics and their immunomodulins, used in this discovery [7]. As a second step (after establishment of positive immunomodulation in vivo), the live probiotic cells in the intestinal tract lumen started directly inhibiting the pathogenic C diff organisms etc. Thus, this invention is novel in that the primary inhibition of the pathogenic bacteria is indirectly due to the previously produced active immunomodulins of the probiotic bacteria, followed by the secondary direct physical inhibition due to live probiotic bacteria in the Lumen, through nutritional competency, production of organic acids, bacteriocins, and finally through stimulation and maintenance of component balance of other non-pathogenic saprophytic intestinal microbiota [5,7]. The bacteriological analysis of patient’s feces, after the multiple probiotic infusion treatment, revealed total absence of pathogenic C. diff organisms, and at the same time significant elevation of intestinal microbiota (in comparison to the beginning of treatment) by two logs (determined by combination of anaerobic as well as aerobic total bacterial counts). In addition, it was proven that the individual strains used in the Multiple Mixed Strain Probiotic Therapy did adhere to the intestinal epithelial cells of the host, which was confirmed by biopsy and subsequent microbiological testing including strain specific phage typing. While conducting the practical clinical trials using Dr. M.S. Reddy’s Multiple Mixed Strain Probiotics to prevent or cure hospital acquired infections, Dr. Reddy came up with another novel breakthrough serendipitous discovery to cure cancer with a significantly greater efficiency, when such Multiple Mixed Strain Probiotic Therapy is used as an adjuvant in combination with standard cancer therapies, including the immune checkpoint therapy. This breakthrough discovery has been published in 2018 [7]. Dr. M.S. Reddy’s discovery is termed as “Dr. M.S. Reddy’s Multiple Mixed Strain Probiotic Adjuvant Cancer Therapy”. This Adjuvant Cancer Therapy establishes immune tolerance and thus helps the primary cancer therapy to be most effective, with least or no side effects. It also significantly reduced the relapse of cancer, which was proven through multiple community based clinical trials. This was accomplished through positive maintenance of the cancer patients gut microbiota and their microbiome, thus establishing the proper immunomodulation which results in significant reduction of immune stimulation and inflammation. This in turn established a positive immune tolerance, which is the prime requisite to synergistically improve the efficiency of the standard cancer therapies. This explains why most of the previous cancer therapies were not effective to cure cancer with greater efficiency (of not more than 20 percent).
The clinical tests (with regard to treatment or prevention of nosocomial infections) clearly proved the following, using the procedure outlined in our earlier publication [1,5]. The antibiotic therapy (using vancomycin and bacitracin) alone could not cure the hospital acquired infections; probiotic therapy by itself showed significant progress even after one week treatment followed by total cure by 4th week; prior administration of probiotics (prior to hospitalization) for a period of 2 weeks, significantly reduced C. diff infection; the subjects who were given preventive probiotics for a period of 3 weeks (prior to hospitalization) did not pick up any C. diff infection, during and after hospitalization; combination of antibiotic and Multiple Mixed Strain Probiotic Therapy cured the C. diff infection in two weeks compared to probiotic therapy alone (which took 4 weeks) and antibiotic therapy alone (which could not cure even after, and beyond 4 weeks of treatment). Although it was a serendipitous discovery, later several planned community based clinical trials conducted using Multiple Mixed Strain Probiotic Therapy as an Adjuvant Cancer Therapy, along with the immune checkpoint therapy and other standard cancer therapies, proved that cancer was cured with 60% efficiency, as opposed to 20% by immune checkpoint therapy and other standard therapies alone. Unlike the pharmaceutical cancer drugs, Multiple Mixed Strain Probiotics come under nutritional supplements, as per the Code of Federal Regulations, and thus are highly economical and affordable and can be used without any major governmental regulations [2].
Conclusion
Dr. Reddy’s Multiple Mixed Strain Probiotic Adjuvant Cancer Therapy, proven through extensive basic research and continued multiple practical community based clinical trials, found to be the best complementary therapy to cure cancer along with the use of immune checkpoint therapy and other traditional cancer therapies. Ultimately, this could be the answer to prevent or treat cancer with 80 to 100% accuracy with no immune related side effects and with least relapse. Thus, cancer can be treated using such a complementary adjuvant probiotic therapy, along with any chosen conventional cancer therapy, as a choice therapy than a chance therapy, to save lives of over 9 million people in the world per year. It is the first time in the world, where a missing link in the successful treatment of cancer has been discovered, and immense credit should go to this breakthrough medical discovery. This discovery can be further improved to develop customized treatment by taking into account the genetics of the cancer patients to cure several cancers. Multiple Mixed Strain Probiotic Therapy, coupled with positive nutritional and life style modifications, may also serve as a preventive aid to eliminate or reduce cancer epidemic by maintaining the healthy microbiota and their microbiome.
https://lupinepublishers.com/pharmacology-clinical-research-journal/fulltext/genesis-evaluation-and-progression-of-a-breakthrough-discovery-to-efficiently-cure-cancer.ID.000121.php
https://lupinepublishers.com/pharmacology-clinical-research-journal/pdf/LOJPCR.MS.ID.000121.pdf
For more Lupine Publishers Open Access Journals Please visit our website: https://lupinepublishersgroup.com/
For more Pharmacology & Clinical Research Please Click Here:https://lupinepublishers.com/pharmacology-clinical-research-journal/
To Know more Open Access Publishers Click on Lupine Publishers
Follow on Linkedin : https://www.linkedin.com/company/lupinepublishers Follow on Twitter : https://twitter.com/lupine_online
0 notes
Text
Vedanta Biosciences Phase 2 Clinical Trial Of VE303 Met Primary Endpoint Through Week 8 Compared With Placebo Of Preventing Recurrent C. difficile Infection (rCDI)
Vedanta Biosciences Phase 2 Clinical Trial Of VE303 Met Primary Endpoint Through Week 8 Compared With Placebo Of Preventing Recurrent C. difficile Infection (rCDI)
Vedanta Biosciences, a clinical-stage company that is developing a potential new category of oral therapies based on defined bacterial consortia, today announced that its Phase 2 clinical trial of VE303, an orally administered investigational live biotherapeutic product in development for the prevention of recurrent C. difficile infection (CDI) in high-risk patients, met its primary endpoint of…

View On WordPress
#Are there clinical trials for recurrent C. difficile infections?#C. difficile Clinical Trial of VE303#Recurrent C. diff. Clinical Trials#Vedanta Biosciences#What is a C. difficile infection?#What is a clinical trial?
0 notes
Text
PureTech’s Vedanta Biosciences gets federal funding for C. Diff. microbiome therapy

US biotech Vedanta Biosciences has been awarded up to $76.9 million to develop VE303 for high-risk Clostridioides difficile (C. diff.) infection by a US government agency.
The Biomedical Advanced Research and Development Agency (BARDA) will pay $7.4 million up front, plus payments worth up to $69.5 million if the project is successful.
Vedanta is one of PureTech’s stable of companies and this is the first ever BARDA award in the microbiome field.
Funding will support completion of an ongoing phase 2 trial and further clinical development of VE303, an orally-administered live biotherapeutic product (LBP) consisting of eight bacterial strains designed to therapeutically reset a patient’s gut microbiota to stop C. Diff infection.
The product is made from pure, clonal bacterial cell banks, which yield a standardised drug product in powdered form, and could replace the need for faecal transplants and the process of having to find donors.
Products such as this aim to repopulate the gut with harmless bacteria that are resistant against pathogenic bacteria such as C. diff., which can take hold in a patient’s digestive tract after treatment with antiobiotics.
While there are no approved competitors, Ferring Pharma reported positive results from a phase 3 trial of its RBX2660 earlier this year, and other firms working in this area include UK-based Microbiota, working in partnership with Roche.
Vedanta’s ongoing phase 2 study is a multi-centre, randomised, double-blind, placebo-controlled trial designed to evaluate the safety and efficacy of two doses of VE303 compared to placebo in patients with high-risk C. diff. infection.
The study is enrolling patients with a recent confirmed diagnosis of C. Diff. infection who have completed a course of antibiotics but remain at high risk for recurrence. The primary endpoint is prevention of infection recurrence at eight weeks.
Vedanta was founded by PureTech and a global team of scientific co-founders who have expertise in the cross-talk between the microbiome and the immune system.
The post PureTech’s Vedanta Biosciences gets federal funding for C. Diff. microbiome therapy appeared first on .
from https://pharmaphorum.com/news/puretechs-vedanta-biosciences-gets-federal-funding-for-c-diff-microbiome-therapy/
0 notes
Text
0 notes
Photo

New donor screening protocols for clinical trials involving fecal microbiota transplantation https://ift.tt/2HMnWDN
Back in May, I wrote a blog post about fecal microbiota transplantation (FMT), or stool transplantation. FMT is considered standard-of-care therapy to treat recurrent Clostridium difficile (C. diff) infections. In this procedure, stool from a healthy donor is placed into the gut of a patient, usually via colonoscopy, to restore helpful bacteria that help protect against recurrent C. diff infection (rCDI).
An important event occurred after my initial post. On June 13, 2019, the FDA issued a safety alert concerning the risk of transmission of multi-drug resistant organisms (MDRO) through FMT. MDROs are bacteria that are resistant to one or more antibiotics.
Safety alert leaves many questions unanswered
The safety alert was issued in response to the transmission of a specific MDRO from donor stool into two patients following FMT. Tragically, one of these individuals died. The FDA announcement provides very few details regarding these cases, and it does not provide information on the cause of this patient’s death. What is known is that these two patients were given FMT as part of a research protocol and not as part of clinical care to treat rCDI.
As I mentioned in my previous post, FMT is supported by guidelines, but is still considered investigational and is not currently FDA-approved. FMT can be performed for clinical care to treat rCDI. But an FMT for any other indication can only be performed in the setting of a clinical trial.
The FDA has not yet disclosed the indication or reason for the FMT for the two patients mentioned in their safety alert, but the FDA did note that the patients were immunocompromised. FMT has been shown to be safe in immunocompromised patients, but generally these patients are at increased risk for infections. Additionally, it was noted that the donor material used in this research protocol had not been screened for MDROs.
FDA institutes new screening requirement for donor stool
Following this event, the FDA now requires MDRO screening for donor stool for all active and future FMT study protocols. Worldwide, screening is being recommended for clinical protocols as well, and this is expected to be supported by an upcoming guideline.
It is important to note that all major stool banks in the US and around the world had implemented screening protocols to detect MDROs and exclude potential donors who test positive well prior to this event. This includes OpenBiome, a large, non-profit stool bank that is widely used in the US and has provided over 45,000 treatments.
Prior to this there had been no previous transmissions of MDROs reported, highlighting that this procedure still remains very safe overall. That being said, this event highlights the need for adherence to standardized screening protocols, which is key for patient safety.
The FDA has reached out to sites that have ongoing FMT protocols to ensure appropriate screening procedures are being followed. Any protocols not utilizing appropriate screening practices were put on hold. The FDA has not released any further information about how many protocols or sites were affected by this step.
Follow me on Twitter @DrJessicaA
The post New donor screening protocols for clinical trials involving fecal microbiota transplantation appeared first on Harvard Health Blog.
from Harvard Health Blog https://ift.tt/34mfC7p via IFTTT https://ift.tt/eA8V8J
0 notes
Text
Finch Therapeutics unleashes the power of the gut
As scients continue searching for treatments to some of the most complex diseases and conditions, they’re increasingly looking to our gut.
The human gut microbiome contains trillions of bacteria that play important roles for the proper functioning of our bodies. But those bacterial colonies went relatively unexplored until recently, when new computational tools made it possible to understand their makeup in more detail.
Finch Therapeutics is one of a number of companies trying to turn that new perspective into new treatments. The company is leveraging its deep connections and expertise in the field to reach a number of milestones in microbiome therapeutics — and it’s outpacing older, better-funded competitors in the process.
The company recently became the first to show a microbiome therapy could reach its primary goals in a Food and Drug Administration trial for patients with Clostridioides difficile infection (C. diff).
Now, as the research community continues to discover connections between gut health and metabolic, immune, and cognitive functions, Finch is developing a broad group of drugs aimed at conditions including chronic hepatitis B, Crohn’s disease, ulcerative colitis, and autism spectrum disorder.
“The biology [around gut bacteria’s influence on health] is fairly complex, and we’re still in the early days of unravelling it, but there have been a number of clinical studies that have reported benefits to restoring gut health, and that’s our north star: the clinical data,” Finch co-founder and Chief Executive Officer Mark Smith PhD ’14 says.
A path unplanned
Smith always thought he’d spend his career doing academic research. Then, while pursuing his PhD in microbiology at MIT, a family member contracted C. diff, a potentially life-threatening infection that can cause diarrhea, fever, and abdominal pain. Smith saw his relative gradually grow discouraged with conventional treatment options as he went through seven unsuccessful rounds of antibiotics over the course of one painful year.
Around that time, a clinical trial showed the promise of using stool transplants to restore gut bacteria in people struggling with C. diff, improving their symptoms. Still, there were very few places collecting stool samples or conducting the procedure at the time. Increasingly desperate, Smith’s relative ended up conducting the stool transplant himself with the help of a friend and an at-home enema kit. The procedure was successful, but risky, and is not rcommended by doctors.
Smith knew his relative was not alone — about a half million people contract C. diff each year — so he set out to expand access to medically certified stool transplants. The effort led to OpenBiome, a nonprofit stool bank that collects and screens stool samples, then ships the formulations to hospitals to conduct transplants. Along the way, Smith partnered with OpenBiome cofounders Andrew Noh and James Burgess, who were attending the MIT Sloan School of Management; Zain Kassam, a postdoc who had worked with Smith in the lab of MIT Professor Eric Alm; and Carolyn Edelstein, now the executive director of OpenBiome, who is also Smith’s wife.
Today OpenBiome works with around 1,300 health care providers across the country and has helped treat about 55,000 patients struggling with C. diff, making it the largest stool bank in the world. OpenBiome also facilitates research into the microbiome, uncovering surprising links between the bacteria in our guts and a range of complex conditions like depression, multiple sclerosis, diabetes, and autism.
The research was enough to convince Smith he needed a new way to help the microbiome field reach its full potential. He founded Finch Therapeutics in 2014 with many of his colleagues from MIT and OpenBiome, including Noh, Kassam, and Burgess.
Since then, the company has focused on developing drugs that mimic as closely as possible the bacterial makeup of the stool transplants used in some of the field’s most promising studies.
Finch’s drugs are made by collecting a stool sample from a vetted donor, screening that sample, processing it to extract the microbial strains, freeze drying the strains, then, following some additional testing, putting it into a pill capsule.
By closely following the methodologies of intervention studies, Finch hopes to safeguard against any major setbacks in clinical trials and become the first company to earn FDA approval for a microbiome-based treatment.
Last month, Finch achieved a major milestone in that direction when it announced preliminary phase 2 results for its oral C. diff drug. The company says it was the largest placebo-controlled trial for an oral microbiome drug to date, and the first to meet its primary efficacy targets in a pivotal trial.
“The first chapter in this field, and our history, has been validating this modality,” Smith says. “Until now, it’s been about the promise of the microbiome. Now I feel like we’ve delivered on the first promise. The next step is figuring out how big this gets.”
Realizing the potential of a promising field
Companies hoping to create treatments from our nascent understanding of the microbiome must navigate some uncertainty around the biological mechanisms that are behind the links between our guts and a range of diseases. Still, those connections are being reinforced in new studies all the time.
“There’s a wide range of indications that are potentially related to microbiome,” Smith says. “We’re just starting to figure out what some of those are. The ones where there’s more research, we understand [the underlying biological] mechanism, and there’s likely going to be this broadening ring of indications we discover as the field continues to mature.”
Finch is planning another, larger study to confirm its C. diff results before submitting the drug for FDA approval. In addition, by the middle of next year, the company will have data on the effects of another oral microbiome drug for children with autism and gastrointestinal issues. Next year it will also complete a trial using the same C. diff drug to help patients with chronic hepatitis B.
“Our view is there are 42 billion doses of antibiotics administered every year, and we think they’ve driven really profound changes to this microbial organ system. We’d be surprised if restoring that functionality doesn’t turn out to be important for a lot of different indications,” Smith says.
Smith notes there are 300 ongoing clinical trials exploring connections between the microbiome and diseases like Alzheimer’s, Crohn’s disease, and multiple forms of cancer.
“The next chapter for us at Finch and the broader field is figuring out what the breadth of this modality can be,” Smith says. “In the next couple of years, we should have visibility into whether this works in autism, chronic hepatitis B, ulceritive colitis, and Crohn’s disease. If we get a positive readout in any one of those, those are very large patient populations with significant unmet needs. So if it works in any one, it would really spur the field into the third chapter. The next step is testing this in an even wider range of indications.”
Finch Therapeutics unleashes the power of the gut syndicated from https://osmowaterfilters.blogspot.com/
0 notes
Text
erectile dysfunction treatment nhs
Contents
Pylori breath testing
Erectile dysfunction cetirizine
Impotence erectile dysfunction
Hbv data. teleflex
Iief-5: wilcoxon rank
i) Sexual History (i.e. present & previous erection. Alprostadil cream (Vitaros) is now available as a treatment option in Primary care for.
A long established pharmacy providing a wide range of NHS and private services such as Antimalarials, Emergency Contraception, Flu Vaccination, H. pylori breath testing, Erectile Dysfunction and.
testosterone pills for erectile dysfunction erectile dysfunction means in hindi dosage of l arginine erectile dysfunction Plus the seed, which can be added to everything from smoothies to cereal, contains a huge dose of heart-protecting fiber as well. Use ground seeds to maximize your omega-3 intake. 3 & 4.Online video visits, free shipping of medication. Shockwave Therapy for ED. Large variety fo ED medications to fit your lifestyle. We are the experts in Men's.erectile dysfunction is caused by dangers of erectile dysfunction drugs Famously, Sildenafil, originally developed as an antihypertensive drug, was repurposed as Viagra by Pfizer for the treatment of erectile dysfunction. similarly, the hair loss treatment drug.The results of a clinical trial released today in STEM CELLS Translational Medicine demonstrate how a topical solution made.
Flossing once a day and exercising through activities you actually enjoy are among the quickest ways to improve your health,
Prostate cancer treatments can make it difficult to get an erection. Find out why this. You can be referred by your GP to a counsellor or therapist within the NHS.
· A number of treatments have been successful in the treatment of erectile dysfunction. Medication, such as sildenafil (sold as Viagra), can be used to manage it in at least two-thirds of cases. Vacuum pumps that encourage blood to flow to the penis.
Drugs used in the treatment of erectile dysfunction (ED). The prescribing of drugs for ED was restricted nationally on the grounds of cost to the NHS.
does furosemide cause erectile dysfunction What causes erection problems in one man may not affect another. Some medicines may lead to life-threatening reactions if you do not. The following is a list of some medicines and drugs that may cause erectile dysfunction (ED) in. furosemide (lasix); guanabenz (wytensin); guanethidine (Ismelin).doppler test for erectile dysfunction More evidence is needed to rate L-carnitine for these uses. acenocoumarol (sintrom) is used to slow blood clotting. L-carnitine might increase the effectiveness of acenocoumarol (Sintrom).
Erectile dysfunction This is when a man cannot get, or keep, an erection that allows him to take part in sexual intercourse or other types of sexual activity. Most men experience it at some time in their life, and the causes can be physical or psychological.
Successful treatment of erectile dysfunction (ED) is associated with. or Parkinson's disease can receive treatment on the NHS for ED [86].
Exuberant is an energy restoring and testosterone boosting supplement designed specifically for men. It is made with natural ingredients that work on the body to reestablish energy levels, enhance.
new research on erectile dysfunction swollen prostate erectile dysfunction cetirizine erectile dysfunction cures for impotence erectile dysfunction The emerging of phosphodiesterase 5 inhibitors (pde 5 I) for the treatment of erectile dysfunction (ed) eclipsed vcd as therapeutic choice for ED; however, widespread usage of VED as part of.What causes erectile dysfunction after taking Cetirizine and Banocide? hi i have allergy like itching and doctor adviced me to take citirizine and bonocide for 21 days, prior to this i adviced to take diff tablets for some time. Now i feel bit less ineterst or erectile dysfunction.Eiger’s Zokinvy NDA is accepted by the FDA. Arbutus is up on hbv data. teleflex reports positive UroLift data.A new study published today in Neuron led by The New York Stem Cell Foundation (NYSCF) Research Institute’s Valentina Fossati, Ph.D., creates astrocytes – an integral support cell in the brain – from.
NHS NWL CCG will not fund penile implants as first or second-line treatment for erectile dysfunction. (Grade C recommendation). Exceptions to this policy are.
Because virtual clinical trials could potentially end the pandemic sooner than traditional ones. Travel restrictions during.
cold hands and feet erectile dysfunction doppler test for erectile dysfunction Data in parentheses are percentages of different age, unless otherwise noted. Age: 2 test for psychogenic versus organic: Pearson Chi-square = 80.858, P < 0.001. iief-5: wilcoxon rank sum test.cold hands and feet. chest pain. Causes. Normally, when a person rises. erectile dysfunction can cause nOH. Additional causes include diuretics, cardiac.
La Merie Publishing prepares brief and full reports as well as competitor analysis reports, the latter in a tabulated format with structured listings of industry-relevant data. One of our top-selling.
NeoTract, a wholly owned subsidiary of Teleflex Incorporated (NYSE:TFX) focused on addressing unmet needs in the field of urology, today announced that Michael Cunningham M.D., Central Ohio Urology.
source https://www.vigrxwarning.com/erectile-dysfunction-treatment-nhs/
0 notes
Text
New donor screening protocols for clinical trials involving fecal microbiota transplantation
Back in May, I wrote a blog post about fecal microbiota transplantation (FMT), or stool transplantation. FMT is considered standard-of-care therapy to treat recurrent Clostridium difficile (C. diff) infections. In this procedure, stool from a healthy donor is placed into the gut of a patient, usually via colonoscopy, to restore helpful bacteria that help protect against recurrent C. diff infection (rCDI).
An important event occurred after my initial post. On June 13, 2019, the FDA issued a safety alert concerning the risk of transmission of multi-drug resistant organisms (MDRO) through FMT. MDROs are bacteria that are resistant to one or more antibiotics.
Safety alert leaves many questions unanswered
The safety alert was issued in response to the transmission of a specific MDRO from donor stool into two patients following FMT. Tragically, one of these individuals died. The FDA announcement provides very few details regarding these cases, and it does not provide information on the cause of this patient’s death. What is known is that these two patients were given FMT as part of a research protocol and not as part of clinical care to treat rCDI.
As I mentioned in my previous post, FMT is supported by guidelines, but is still considered investigational and is not currently FDA-approved. FMT can be performed for clinical care to treat rCDI. But an FMT for any other indication can only be performed in the setting of a clinical trial.
The FDA has not yet disclosed the indication or reason for the FMT for the two patients mentioned in their safety alert, but the FDA did note that the patients were immunocompromised. FMT has been shown to be safe in immunocompromised patients, but generally these patients are at increased risk for infections. Additionally, it was noted that the donor material used in this research protocol had not been screened for MDROs.
FDA institutes new screening requirement for donor stool
Following this event, the FDA now requires MDRO screening for donor stool for all active and future FMT study protocols. Worldwide, screening is being recommended for clinical protocols as well, and this is expected to be supported by an upcoming guideline.
It is important to note that all major stool banks in the US and around the world had implemented screening protocols to detect MDROs and exclude potential donors who test positive well prior to this event. This includes OpenBiome, a large, non-profit stool bank that is widely used in the US and has provided over 45,000 treatments.
Prior to this there had been no previous transmissions of MDROs reported, highlighting that this procedure still remains very safe overall. That being said, this event highlights the need for adherence to standardized screening protocols, which is key for patient safety.
The FDA has reached out to sites that have ongoing FMT protocols to ensure appropriate screening procedures are being followed. Any protocols not utilizing appropriate screening practices were put on hold. The FDA has not released any further information about how many protocols or sites were affected by this step.
Follow me on Twitter @DrJessicaA
The post New donor screening protocols for clinical trials involving fecal microbiota transplantation appeared first on Harvard Health Blog.
New donor screening protocols for clinical trials involving fecal microbiota transplantation published first on https://drugaddictionsrehab.tumblr.com/
0 notes
Link
Back in May, I wrote a blog post about fecal microbiota transplantation (FMT), or stool transplantation. FMT is considered standard-of-care therapy to treat recurrent Clostridium difficile (C. diff) infections. In this procedure, stool from a healthy donor is placed into the gut of a patient, usually via colonoscopy, to restore helpful bacteria that help protect against recurrent C. diff infection (rCDI).
An important event occurred after my initial post. On June 13, 2019, the FDA issued a safety alert concerning the risk of transmission of multi-drug resistant organisms (MDRO) through FMT. MDROs are bacteria that are resistant to one or more antibiotics.
Safety alert leaves many questions unanswered
The safety alert was issued in response to the transmission of a specific MDRO from donor stool into two patients following FMT. Tragically, one of these individuals died. The FDA announcement provides very few details regarding these cases, and it does not provide information on the cause of this patient’s death. What is known is that these two patients were given FMT as part of a research protocol and not as part of clinical care to treat rCDI.
As I mentioned in my previous post, FMT is supported by guidelines, but is still considered investigational and is not currently FDA-approved. FMT can be performed for clinical care to treat rCDI. But an FMT for any other indication can only be performed in the setting of a clinical trial.
The FDA has not yet disclosed the indication or reason for the FMT for the two patients mentioned in their safety alert, but the FDA did note that the patients were immunocompromised. FMT has been shown to be safe in immunocompromised patients, but generally these patients are at increased risk for infections. Additionally, it was noted that the donor material used in this research protocol had not been screened for MDROs.
FDA institutes new screening requirement for donor stool
Following this event, the FDA now requires MDRO screening for donor stool for all active and future FMT study protocols. Worldwide, screening is being recommended for clinical protocols as well, and this is expected to be supported by an upcoming guideline.
It is important to note that all major stool banks in the US and around the world had implemented screening protocols to detect MDROs and exclude potential donors who test positive well prior to this event. This includes OpenBiome, a large, non-profit stool bank that is widely used in the US and has provided over 45,000 treatments.
Prior to this there had been no previous transmissions of MDROs reported, highlighting that this procedure still remains very safe overall. That being said, this event highlights the need for adherence to standardized screening protocols, which is key for patient safety.
The FDA has reached out to sites that have ongoing FMT protocols to ensure appropriate screening procedures are being followed. Any protocols not utilizing appropriate screening practices were put on hold. The FDA has not released any further information about how many protocols or sites were affected by this step.
Follow me on Twitter @DrJessicaA
The post New donor screening protocols for clinical trials involving fecal microbiota transplantation appeared first on Harvard Health Blog.
from Harvard Health Blog https://ift.tt/34mfC7p Original Content By : https://ift.tt/1UayBFY
0 notes