#Minimally invasive procedure
Explore tagged Tumblr posts
Text
Robotic Knee Replacement Surgery in Aurangabad — Dhoot Hospitals
Looking for advanced knee replacement surgery in Aurangabad? Dhoot Hospitals now offers cutting-edge robotic knee replacement surgery — ensuring higher precision, faster recovery, and better results for patients suffering from severe knee pain or arthritis.

Why Choose Robotic Knee Replacement at Dhoot Hospitals?
Minimally invasive procedure
Reduced pain and blood loss
Faster rehabilitation
Personalized surgical plans
Trusted by thousands of patients in Aurangabad
Dhoot Hospitals is known for combining expert medical care with the latest in robotic surgical technology — making it a top choice for knee replacement in Aurangabad.
#Looking for advanced knee replacement surgery in Aurangabad? Dhoot Hospitals now offers cutting-edge robotic knee replacement surgery — ensu#faster recovery#and better results for patients suffering from severe knee pain or arthritis.#With the help of advanced robotics and expert orthopedic surgeons#Dhoot Hospitals brings the future of joint care to Aurangabad. Whether you’re struggling with knee stiffness#pain while walking#or have been advised to consider knee surgery#robotic technology helps improve the accuracy of implant positioning and reduces complications.#Robotic Knee Replacement Surgery in Aurangabad — Dhoot Hospitals#Robotic Knee Replacement Surgery in Aurangabad — Dhoot Hospitals#Why Choose Robotic Knee Replacement at Dhoot Hospitals?#Minimally invasive procedure#Reduced pain and blood loss#Faster rehabilitation#Personalized surgical plans#Trusted by thousands of patients in Aurangabad
0 notes
Text
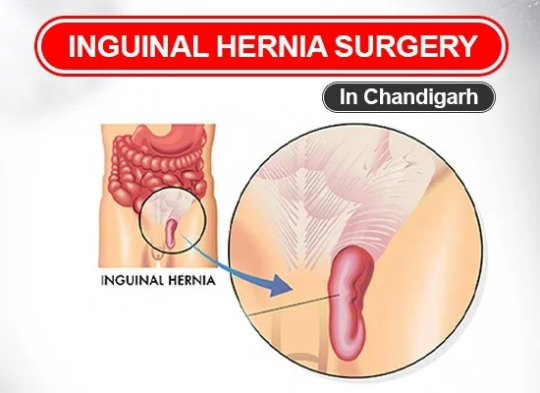
Get expert hernia surgery in Chandigarh at Mukat Hospital. Our skilled surgeons offer advanced, minimally invasive procedures for quick recovery. Book your consultation today!
1 note
·
View note
Text
Introduction:
In the realm of modern medicine, certain techniques stand as pillars of innovation, revolutionizing the way procedures are performed and patient outcomes are improved. One such technique is the Seldinger Technique. Developed by Dr. Sven-Ivar Seldinger in 1953, this method has become a cornerstone in various medical procedures, from inserting central venous catheters to performing angiography and even certain types of biopsies.
In this comprehensive guide, we delve into the intricacies of the Seldinger Technique, its applications, and its significance in contemporary healthcare.
#CARDIAC CATHETERIZATION#CENTRAL VENOUS ACCESS#EMERGENCY MEDICINE#HEALTHCARE ADVANCEMENTS#INTERVENTIONAL RADIOLOGY#MEDICAL INNOVATION#MEDICAL PROCEDURES#MINIMALLY INVASIVE PROCEDURE#SPATIENT SAFETY#SELDINGER TECHNIQUE
0 notes
Text

Exploring Diverse Applications of Stereotactic Radiosurgery:
The versatility of stereotactic radiosurgery spans various neurological conditions, providing personalized solutions for patients with different medical challenges. Notable applications include:
1. Brain Tumors: Stereotactic radiosurgery plays a vital role in treating both malignant and benign brain tumors. Whether addressing high-grade gliomas, meningiomas, or pituitary adenomas, SRS offers a non-invasive approach to reducing or eliminating tumors while preserving neurological function and quality of life.
2. Arteriovenous Malformations (AVMs): AVMs are abnormal clusters of blood vessels in the brain that increase the risk of hemorrhagic strokes. Stereotactic radiosurgery presents a compelling alternative to traditional surgical removal, allowing clinicians to destroy AVMs with targeted radiation while minimizing procedural risks.
3. Trigeminal Neuralgia: This condition causes severe facial pain and presents challenges in pain management. Stereotactic radiosurgery offers relief for patients who do not respond to medical therapy by selectively targeting the trigeminal nerve and disrupting abnormal pain signals.
4. Movement Disorders: Essential tremor and Parkinson's disease can significantly affect quality of life. Stereotactic radiosurgery allows clinicians to modulate neural circuits involved in these disorders, reducing symptoms and restoring functional independence for patients who have exhausted conventional treatments.
Unveiling the Benefits of Stereotactic Radiosurgery:
Adopting stereotactic radiosurgery brings several advantages to neurological care:
1. Minimally Invasive: Stereotactic radiosurgery eliminates the need for traditional surgery, reducing surgical risks, recovery time, and postoperative complications. This approach enhances patient comfort, promotes quicker recovery, and allows patients to resume normal activities sooner.
2. Precision: Utilizing advanced imaging and targeting technologies, stereotactic radiosurgery delivers radiation with exceptional precision, sparing healthy tissues while effectively treating lesions. This precision lowers the risk of treatment-related complications and improves therapeutic outcomes.
3. Expedited Treatment: Unlike conventional radiation therapy, which may require prolonged treatment over weeks or months, stereotactic radiosurgery typically involves only one to a few treatment sessions. This shorter treatment timeline improves patient convenience, compliance, and minimizes disruptions to daily life.
4. Versatility: Stereotactic radiosurgery can address a wide range of neurological conditions, offering tailored treatments for each patient's specific needs. This versatility highlights SRS as an adaptable therapeutic approach capable of meeting diverse patient requirements across the neurological spectrum.
There are many good hospitals in Mumbai that offer stereotactic radiosurgery followed by regular health checkups to check the success of treatment and also detect and manage any complications due to the procedure, such as a full body health checkup at Jaslok Hospital Mumbai.
#stereotactic radiosurgery#radiosurgery#cancer treatment#brain tumors#full body health checkup#regular health checkups#trigeminal neuralgia#parkinson disease#minimally invasive procedure
0 notes
Text
0 notes
Text

I got my fallopian tubes removed today! The surgery was fast and easy AND THEY’RE LETTING ME KEEP THEM!
& my husband and mom got me this cutie from the gift shop.
We named him Jimmy Fallopian (get it lmfao)
#nonsims#tw surgery#surgery tw#salem rambles#I’m so glad it’s over and went well#I knew it was minimally invasive#but anesthesia scares the shit out of me#but I’m SO GLAD I get to keep my tubes#🤣🤣🤣#my doctor seemed so tickled by me asking for them#and she took a bunch of pictures during the procedure too#I’m convinced she’s a nerd like me lmao#& maybe collects wacky things#I think I’m going to make Christmas ornaments out of them 🤣🤣🤣🤣🤣🤣#since I got them removed on Christmas Eve#💀💀💀💀
26 notes
·
View notes
Text
Going to attempt drafts right now and lurky around to see if I can't get the ol' writing hamster goin on it's wheel 🙃
#ooc#for such a minimally invasive heart procedure you'd think my dad survived death with the way he's acting rn
2 notes
·
View notes
Text
It's insane how many people are so opposed to getting vasectomies. Oh we have a solution to this big ole problem. If you want to start a family the old fashioned way just go get it reversed. We'll even give you anesthesia! How is this not the most popular thing to do. A call to all the penis'd, get a vasectomy. Sincerely, the uterus'd
#i know why if anyone explains sexism to me one more time im making pvp real on this site and pain haptics mandatory#yes yes of course i believe everyone should do what they want with their body#and for the sake of childfree t4t sex we need everyone to be infertile this is my america#and im even sensitibe to the fact that people.dont like surgeries#but the amount of brutality present in birth control from a uterus'd perspective vs a simple vasectomy#a minimally invasive#low pain#and REVERSABLE procedure vs ripping and clamping and piercing your organs to avoid pregancy that inherently effects one person more#like you want to smash? snip it bitch this is kentucky
4 notes
·
View notes
Text
The Case for Uterine Fibroid Embolization: A Game-Changer in Best Treatment for Fibroid

Fibroids are a common yet often misunderstood condition that affect many women. While surgery has long been the go-to solution for fibroid removal, there's a revolutionary, non-surgical alternative that’s changing the way we approach fibroid treatment: Uterine Fibroid Embolization (UFE). As experts in fibroid care, we believe UFE stands out as the best treatment for fibroids, offering numerous benefits over traditional surgical methods.
What Are Uterine Fibroids?
Before diving into why UFE is a game-changer, it’s essential to understand what uterine fibroids are. These are benign (non-cancerous) tumors that grow in the uterus. Although they vary in size, location, and symptoms, fibroids can lead to significant health problems, including heavy menstrual bleeding, pelvic pain, and fertility challenges.
The Traditional Approach: Surgery
For years, women suffering from fibroids had limited options for treatment, with surgery being the most common approach. Surgical procedures, such as myomectomy or hysterectomy, involve removing the fibroids or even the entire uterus. While these surgeries can offer relief, they come with significant risks, including extended recovery times, scarring, and potential complications.
Uterine Fibroid Embolization: A Non-Surgical Solution
Uterine Fibroid Embolization (UFE) offers a groundbreaking alternative to surgery. UFE is a minimally invasive procedure where small particles are injected into the blood vessels that supply blood to the fibroids. This causes the fibroids to shrink and eventually die off due to the lack of blood supply. Unlike traditional surgery, UFE doesn’t require large incisions, and recovery time is much shorter.
Why UFE is a Game-Changer
Non-Surgical and Minimally Invasive
UFE is performed through a small catheter inserted into the femoral artery in the groin. This means no large incisions, no stitches, and a much quicker recovery time compared to traditional surgery. Most women can return to their normal activities within a week, whereas recovery from surgery can take weeks or even months.
Preservation of the Uterus
One of the most significant advantages of UFE is that it allows women to keep their uterus. For many women, especially those who wish to have children in the future, this is a critical factor in choosing UFE over more invasive surgical options.
Reduced Risk and Complications
Since UFE is a minimally invasive procedure, the risk of complications is significantly lower than with traditional surgeries. There’s no risk of scarring on the uterus or the reproductive organs, and the chances of major complications are rare.
Effective Symptom Relief
UFE is proven to be highly effective in reducing or completely eliminating symptoms caused by fibroids. This includes heavy bleeding, pelvic pain, frequent urination, and bloating. Many women report significant improvement in their quality of life shortly after the procedure.
Faster Recovery and Less Downtime
Unlike traditional surgeries that may require weeks of recovery and hospital stays, UFE typically allows women to return to their daily routine within just 7 to 10 days. This makes it a highly appealing option for those who cannot afford long periods away from work or family.
Why Choose UFE Over Traditional Surgery?
At USA Fibroid Centers, we believe that UFE is the future of fibroid treatment. It combines the effectiveness of surgery with the minimal invasiveness of modern medical procedures. For women who want to avoid the pain, long recovery time, and risks associated with surgery, UFE offers an ideal solution. Plus, with high success rates and patient satisfaction, it has become the gold standard for fibroid treatment.
Conclusion
Fibroids don’t have to control your life, and neither should the treatments used to address them. Uterine Fibroid Embolization offers a safe, effective, and minimally invasive way to tackle fibroids while preserving your uterus and avoiding the risks of traditional surgery. If you’re considering treatment options for fibroids, UFE should be at the top of your list.
Schedule Your Free Consultation Today
If you're ready to explore UFE or want to learn more about the procedure, we’re here to help. Click here to learn more about our advanced, non-surgical treatments or call us to book your consultation.
#fibroid treatment#uterine fibroids#non-surgical fibroid treatment#uterine fibroid embolization#fibroid removal#best treatment for fibroids#UFE procedure#fibroid relief#fibroid symptoms#minimally invasive fibroid treatment#uterus preservation
1 note
·
View note
Text
The Rise of Interventional Oncology: A $7.5 Billion Market Opportunity

Introduction
The global interventional oncology market is undergoing rapid expansion, fueled by the increasing prevalence of cancer, advancements in image-guided therapies, and the growing adoption of minimally invasive oncology treatments. By 2025, the market is projected to reach USD 3.9 billion, growing at a CAGR of 7.2%. With continual technological progress in tumor ablation, embolization, and targeted radiation therapies, interventional oncology is reshaping modern cancer treatment paradigms. Moreover, next-generation ablation devices, AI-driven imaging solutions, and precision-based oncological interventions are revolutionizing this domain, making treatments more effective and accessible.
With projections estimating the interventional oncology market to surpass USD 7.5 billion by 2032, lucrative opportunities exist for medical device manufacturers, biotech firms, and healthcare providers. Strategic collaborations, regulatory advancements, and sustained investments in oncology innovation are poised to further accelerate growth in this transformative field.
Request Sample Report PDF (including TOC, Graphs & Tables): https://www.statsandresearch.com/request-sample/40647-global-interventional-oncology-market
Interventional Oncology Market Dynamics:
Interventional Oncology Market Growth Drivers
Increasing Cancer Incidence: The rising burden of cancer worldwide necessitates advanced interventional oncology solutions, particularly for liver, lung, kidney, and bone malignancies.
Minimally Invasive Procedures: The shift toward non-surgical cancer treatments is driven by reduced recovery time, lower procedural risks, and improved patient outcomes.
Technological Innovations: Developments in radiofrequency ablation (RFA), microwave ablation (MWA), cryoablation, transarterial chemoembolization (TACE), and radioembolization (Y-90 therapy) are boosting market adoption.
Favorable Reimbursement Policies: Governments and private insurers are expanding coverage for interventional oncology procedures, increasing patient accessibility.
Integration of AI and Robotics: AI-assisted imaging and robotic intervention systems are enhancing precision, efficiency, and treatment outcomes.
Get up to 30%-40% Discount: https://www.statsandresearch.com/check-discount/40647-global-interventional-oncology-market
Interventional Oncology Market Challenges
Regulatory Compliance: Stringent approvals from FDA, EMA, and CE Mark create barriers for new entrants and prolong the commercialization process.
High Procedural Costs: The expense associated with interventional oncology devices and treatments may limit adoption, particularly in low-income regions.
Limited Awareness: In developing markets, lack of knowledge among both patients and physicians regarding advanced oncology interventions hampers growth.
Skilled Workforce Requirement: The execution of these procedures necessitates highly trained interventional radiologists, restricting adoption in areas with limited specialists.
Emerging Trends in Interventional Oncology
1. AI and Machine Learning in Imaging
The incorporation of AI-driven imaging solutions facilitates real-time tumor detection, automated lesion segmentation, and enhanced decision-making, leading to improved precision in interventional procedures.
2. Nanotechnology in Drug Delivery
Advanced nanoparticle-based drug delivery systems are enhancing the efficacy of chemoembolization and localized tumor treatment while minimizing systemic side effects.
3. Biodegradable Embolic Agents
Biodegradable materials for embolization, such as drug-eluting beads (DEB) and radiopharmaceutical embolic agents, are gaining traction due to their effectiveness in localized cancer treatment.
4. Expansion of Ambulatory Surgical Centers (ASCs)
The increasing shift of oncology procedures to ASCs is reducing hospital stays, lowering treatment costs, and enhancing patient convenience.
Interventional Oncology Market Segmentation Analysis
By Product Type
Ablation Devices: Leading segment, holding over 45.7% of the interventional oncology market in 2024 due to advancements in RFA, MWA, and cryoablation.
Embolization Devices: Expected to grow at a CAGR of 8.2% through 2032, driven by the adoption of TACE, Y-90 radioembolization, and DEBs.
Support Devices: Includes catheters, guidewires, balloons, and navigation technologies enhancing precision in interventional procedures.
By Procedure Type
Ablation Procedures: Dominant category, representing 48.3% of the market, with increasing demand for thermal and non-thermal ablation techniques.
Embolization Procedures: Witnessing significant growth, particularly for liver, kidney, and lung cancer treatment.
Radionuclide Therapy: Expected to grow at 7.8% CAGR, driven by Y-90 and Lu-177-based targeted radionuclide treatments.
By Cancer Type
Liver Cancer: Largest segment (37.6% interventional oncology market share) due to widespread adoption of TACE, radioembolization, and ablation techniques.
Lung Cancer: Fastest-growing segment (7.9% CAGR), driven by increasing cases of NSCLC and bronchoscopic interventional treatments.
Prostate & Breast Cancer: Gaining traction with innovations in focal ablation therapies and minimally invasive interventions.
By End-User
Hospitals: Largest market share (60.4%), as oncology centers and tertiary care hospitals dominate procedural volumes.
Ambulatory Surgical Centers (ASCs): Expected to grow at 7.6% CAGR, owing to the rise in cost-effective, outpatient interventional oncology treatments.
Specialty Clinics & Research Institutions: Playing a critical role in clinical trials, novel therapeutic research, and oncology device development.
By Region
North America: Dominant market (42.3% share), driven by high healthcare expenditure, strong regulatory frameworks, and cancer research initiatives.
Asia-Pacific: Fastest-growing region (8.5% CAGR), with increasing medical investments and rising cancer prevalence in China, India, and Japan.
Europe: Witnessing sustained growth due to regulatory standardization, advanced oncology infrastructure, and rising adoption of minimally invasive procedures.
Competitive Landscape
The interventional oncology market is highly competitive, with key players focusing on mergers, acquisitions, and technological advancements to enhance their market position. Major companies include:
Medtronic plc
Boston Scientific Corporation
Johnson & Johnson (Ethicon)
Baxter International Inc.
Cook Medical
C.R. Bard Inc.
Stryker Corporation
B. Braun Melsungen AG
Terumo Corporation
Sirtex Medical
Siemens Healthineers
GE Healthcare
Recent Developments
March 2024: Boston Scientific acquired a leading ablation technology firm, strengthening its MWA and RFA portfolio.
April 2024: Sirtex Medical launched an advanced Y-90 radioembolization platform to enhance liver cancer treatment precision.
June 2024: Terumo Corporation introduced a next-generation drug-eluting embolic microsphere for optimized TACE procedures.
Purchase Exclusive Report: https://www.statsandresearch.com/enquire-before/40647-global-interventional-oncology-market
Future Outlook
The interventional oncology market is poised for transformative growth, with advancements in radiofrequency ablation, transarterial chemoembolization, and AI-assisted oncology interventions leading the way. As global healthcare investment in oncology rises, new opportunities emerge in nanotechnology-driven drug delivery, AI-enhanced procedural planning, and bioabsorbable embolic agents.
With the demand for minimally invasive, image-guided cancer treatments increasing, the industry is set to revolutionize oncological care, making precision medicine the future of cancer treatment.
Our Services:
On-Demand Reports: https://www.statsandresearch.com/on-demand-reports
Subscription Plans: https://www.statsandresearch.com/subscription-plans
Consulting Services: https://www.statsandresearch.com/consulting-services
ESG Solutions: https://www.statsandresearch.com/esg-solutions
Contact Us:
Stats and Research
Email: [email protected]
Phone: +91 8530698844Website: https://www.statsandresearch.com
#Interventional Oncology Market#Oncology Treatment#Cancer Therapy#Minimally Invasive Procedures#Image-Guided Therapy#Tumor Ablation#Radioembolization#Chemoembolization#Cryoablation#Microwave Ablation#Cancer Care Innovation#Medical Imaging#Oncology Devices#Targeted Cancer Treatment#Interventional Radiology#Healthcare Technology#Cancer Diagnostics#Radiation Therapy#Precision Medicine#Global Healthcare Market#Medical Device Industry#Oncology Research#Cancer Treatment Trends#Healthcare Investment#Emerging Medical Technologies#Market Growth Analysis
1 note
·
View note
Text
Bariatric Surgery Devices: Revolutionizing Long-Term Weight Loss Outcomes
The Progression of Bariatric Surgery
Over time, bariatric surgery has evolved into a crucial intervention in the global fight against obesity. With obesity rates climbing across the world, the field has transitioned from traditional open surgeries to modern, minimally invasive bariatric surgery devices. This advancement has accelerated recovery times, minimized complications, and spurred widespread adoption of advanced tools that enhance procedural safety and patient outcomes.
Leading Bariatric Surgery Procedures in Use
Among the most widely performed procedures are sleeve gastrectomy, gastric bypass, biliopancreatic diversion, and adjustable gastric banding. Of these, the sleeve gastrectomy device market has shown particularly robust growth, largely due to its balance of effectiveness and procedural simplicity. Each method utilizes precise bariatric surgical instruments tailored for minimally invasive interventions, supporting more accurate and efficient operations.
👉 Explore more about the latest sleeve gastrectomy devices here: https://www.delveinsight.com/blog/bariatric-surgery-devices-for-obesity?utm_source=blog&utm_medium=promotion&utm_campaign=akpr
How Bariatric Surgery Devices Improve Outcomes
The integration of next-generation bariatric devices has played a pivotal role in enhancing surgical outcomes. These innovations contribute to shorter operative times, safer procedures, and improved long-term weight-loss success rates. Additionally, they allow for reduced hospital stays and quicker recoveries. However, potential complications—such as device erosion, infection, or band slippage—highlight the importance of continued device innovation and skilled surgical technique.
Bariatric Surgery Devices Market Trends
The global market for bariatric surgery devices is on a strong upward trajectory, fueled by the growing obesity epidemic and increased demand for minimally invasive solutions. Technological breakthroughs and stronger healthcare systems are driving market growth in key regions such as North America, Europe, and Asia-Pacific. Particularly, the South Korea bariatric surgery market is emerging as a key player, supported by advanced healthcare technology and a thriving medical tourism industry.
👉 Discover key market trends in the South Korea bariatric surgery segment: https://www.delveinsight.com/blog/bariatric-surgery-devices-for-obesity?utm_source=blog&utm_medium=promotion&utm_campaign=akpr
Key Industry Players in Bariatric Devices
Major companies in the bariatric surgery devices space include Medtronic, Johnson & Johnson (Ethicon), Apollo Endosurgery, Olympus Corporation, and Intuitive Surgical. These industry leaders are actively developing innovative tools aimed at enhancing surgical safety, procedural precision, and overall patient care.
Future Outlook for the Bariatric Surgery Devices Sector
With obesity-linked health risks gaining more visibility, the outlook for the bariatric surgery devices market is highly optimistic. Continued advancements, improved surgical training, and broader access to care are expected to accelerate adoption, empowering more individuals to achieve long-term weight loss through cutting-edge surgical solutions.
Latest Reports Offered By DelveInsight:
crd medical abbreviation, ulcerative colitis drugs, best iol lens, iclepertin, tecelra cost, tecnis odyssey iol, bone pipeline, clostridium difficile tests market, solrikitug, prurigo nodularis marketed and pipeline drugs, bronchiectasis market, hidradenitis suppurativa medication, oncology consulting, nontuberculous mycobacteria market, acute ischemic stroke diagnosis market, how to treat gastroparesis, myocardial infarction market, colitis and symptoms, mobile apps in healthcare industry, multiple system atrophy treatment, apthera iol, iol lens brands, fauci igg4, what is achondroplasia, pritelivir availability 2024
Other Reports Offered By DelveInsight:
https://www.delveinsight.com/sample-request/sarcoidosis-global-api-manufacturers-marketed-and-phase-iii-drugs-landscapehttps://www.delveinsight.com/sample-request/sbp-101-emerging-drug-insight-and-market-forecast
#minimally invasive bariatric devices#device related complications in bariatric procedures#bariatric surgery devices market#bariatric surgery devices#bariatric devices#south korea bariatric surgery market#obesity surgery devices market#bariatric surgical instruments#sleeve gastrectomy device market
0 notes
Text
Are you looking for the best in knee surgery? 🦵🇮🇳 Dr. Ashok Rajagopal, one of the most renowned orthopedic surgeons in India, is a pioneer in knee replacement and has thousands of successful surgeries to his name. He is trusted by patients across the world for his expertise, precision and innovation.

#“Advance Knee Procedures in India”#“Top Minimally Invasive Knee Surgeon in India”#“Minimally Invasive Knee Replacement in India”#“Best Surgeon for Advanced Knee Surgery in India”#“Dr. Rajgopal Minimally Invasive Knee Surgeon in Delhi”#“Dr. Ashok Rajgopal Top Robotic Knee Surgeon in India”
0 notes
Text

Thymectomy is like a carefully choreographed dance in surgery, with different moves. The classic open thymectomy is the main act, involving a big cut in the chest for surgeons to carefully take out the thymus. While it works well, it also means a longer recovery time and more discomfort afterward. On the other hand, modern methods like video-assisted thoracic surgery (VATS) and robotic-assisted surgery bring a fresh approach. They use smaller cuts and special tools, making thymectomy less painful, with shorter hospital stays and quicker recovery.
1. Open Thymectomy: In the open thymectomy routine, the surgical team makes a big opening to access the thymus. It's like a big performance, allowing thorough exploration and removal. However, this grand show comes with a downside – a longer recovery time and more discomfort afterward, things to think about when choosing the surgery.
2. Minimally Invasive Techniques: New techniques like VATS and robotic-assisted surgery are changing the game. VATS uses a camera and special tools for precise work with less invasion. Robotic-assisted surgery, with its robotic arms, adds a level of precision. These methods give the thymectomy a fresh feel, making it less painful and speeding up recovery.
Postoperative Recovery:
After thymectomy, the recovery is a process marked by initial pain and discomfort that gradually lessens. Managing pain is crucial in this recovery process, often involving carefully prescribed medications. How fast you recover, like a musical piece, depends on the surgery method and individual factors. While most people can get back to normal activities in a few weeks, full recovery may take months. This recovery phase shows how the chosen surgery method impacts the experience, with less invasive methods often making the return to normal life quicker.
Efficacy and Risks:
The success of thymectomy for myasthenia gravis is like a dynamic performance with varied outcomes. Some see a big improvement, but it's not the same for everyone. Responses, like different harmonies, are nuanced, making it a complex situation. Risks in this surgical performance include bleeding, infection, and possible reactions to anesthesia. Dealing with these risks needs a careful preparation before surgery, with open communication between patients and healthcare providers being crucial.
It is advisable to undergo a full body health checkup following a thymectomy to check the success of treatment and evaluate the overall health of the patient after the procedure.
#thymectomy#open thymectomy#minimally invasive procedure#VATS#robotic surgery#regular health checkups#full body health checkup
0 notes
Text
Is Robotic Whipple the New Gold Standard for Pancreatic Cancer?
Is the Robotic Whipple Procedure the New Gold Standard for Pancreatic Cancer?” by Dr. Srivatsan Gurumurthy explores the transformative impact of robotic-assisted surgery on pancreatic cancer treatment. Dr Gurumurthy, a leading pancreatic cancer surgeon at GEM Hospital in Chennai, explains how the robotic Whipple procedure—also known as robotic pancreaticoduodenectomy—redefines surgical standards for carefully selected patients.
Understanding the Robotic Whipple Procedure
The Whipple procedure involves the removal of the pancreas's head, duodenum, gallbladder, and part of the bile duct. Traditionally performed through open surgery, this complex operation has evolved with robotic assistance. Surgeons now utilize robotic arms controlled from a console, offering enhanced precision and 3D visualization. This advancement is particularly beneficial in delicate areas like the pancreas, where millimeter-level accuracy is crucial.
Advantages for Patients
Dr. Gurumurthy highlights several patient-centric benefits of the robotic approach:
Faster Recovery: Minimally invasive techniques lead to quicker healing and shorter hospital stays.
Reduced Pain: Smaller incisions result in less postoperative discomfort.
Lower Infection Risk: Minimized wound exposure decreases the chance of complications.
Enhanced Surgical Precision: Robotic systems provide superior control, especially in complex cases.
These benefits contribute to improved patient outcomes, positioning the robotic Whipple as a promising advancement in pancreatic cancer surgery.
Patient Eligibility
Not all patients are suitable candidates for the robotic Whipple procedure. Ideal candidates are those with localized tumours not involving major blood vessels. Factors such as overall health, tumour size, and proximity to vital structures are considered. A comprehensive evaluation by an experienced robotic surgeon, like Dr. Gurumurthy, is essential to determine the most appropriate surgical approach.
Pre- and Postoperative Care
Patients undergo thorough preoperative assessments, including blood tests, imaging, and dietary counselling. Post-surgery, they may spend a brief period in the ICU, gradually resume eating and walking within days, and attend follow-up visits to monitor recovery and long-term outcomes.
The Future of Pancreatic Surgery
While robotic Whipple surgery is not yet the standard everywhere, it is gaining traction in high-volume centres with skilled surgeons and advanced infrastructure. Dr. Gurumurthy emphasizes that robotic surgery is not replacing traditional methods but enhancing safety and accuracy. In facilities like GEM Hospital, the robotic Whipple procedure is emerging as a preferred option for suitable patients, signalling a shift towards more precise and patient-friendly surgical interventions.
For individuals diagnosed with pancreatic cancer, consulting with a specialized surgeon experienced in both traditional and robotic techniques is crucial. Dr. Srivatsan Gurumurthy and his team offer comprehensive evaluations and personalized treatment plans, guiding patients through every step from diagnosis to recovery. Learn more.
#Robotic Whipple procedure#pancreatic cancer surgery#minimally invasive surgery#Whipple surgery#robotic-assisted surgery#pancreatic cancer treatment#surgical innovations#robotic surgery benefits#pancreatic tumor removal#Dr. Srivatsan
0 notes
Text
Glaucoma Drainage Implant Surgery: A Step-by-Step Guide
Glaucoma is a progressive eye disease that can lead to permanent vision loss if not managed effectively. For patients looking for advanced treatment options, Clairevision Eye Care in Wakad, Pune, under the expert care of Dr. Archana Singh, offers specialized solutions like glaucoma drainage implant surgery. This blog offers a comprehensive guide to help you understand the procedure, its benefits, and what to expect.
At times, eye drops and laser treatments are not enough to control intraocular pressure (IOP). That’s when a glaucoma drainage implant procedure becomes necessary. This surgery involves placing a small device inside the eye to drain excess fluid, reducing IOP and preserving vision. It is highly beneficial for patients with advanced or complex glaucoma conditions.
There are several types of implants used, including the Ahmed glaucoma valve surgery, Baerveldt implant for glaucoma, and the more recent PAUL glaucoma implant. These devices are tailored to the patient’s condition and designed to provide long-term pressure control. Each comes with its benefits and is selected based on the severity of glaucoma. During the surgery, the implant is placed under the conjunctiva, and a tube is inserted into the front chamber of the eye to help fluid drain. The procedure usually takes about an hour and is done under local anesthesia.
Glaucoma implant surgery recovery involves regular follow-ups to monitor healing and eye pressure levels. Mild discomfort, temporary blurred vision, and redness are common but manageable with medication and care. The post-operative care for glaucoma implant includes using prescribed eye drops, avoiding strenuous activities, and attending all follow-up appointments.
The blog also compares trabeculectomy vs. glaucoma drainage implants, discussing how implants are often preferred for complex or previously failed cases. While all surgeries carry some risks, including infection or implant failure, the risks of glaucoma drainage devices are minimal when handled by experienced surgeons. With high success rates of glaucoma implant surgeries, Clairevision Eye Care in Punawale has earned a reputation as one of the most trusted clinics for glaucoma treatment in Punawale, Pune. Patients searching for glaucoma specialists in Wakad, Pune, minimally invasive glaucoma surgery (MIGS), or glaucoma tube shunt surgery, often turn to Dr. Archana Singh for her expertise, compassionate care, and exceptional surgical outcomes for AMD.
#glaucoma specialists in Wakad#Pune#glaucoma treatment in Punawale#glaucoma drainage implant procedure#glaucoma implant surgery recovery#Ahmed glaucoma valve surgery#Baerveldt implant for glaucoma#glaucoma tube shunt surgery#minimally invasive glaucoma surgery (MIGS)#trabeculectomy vs. glaucoma drainage implants#post-operative care for glaucoma implant#risks of glaucoma drainage devices#success rates of glaucoma implant surgeries
0 notes
Text
pin hole procedure performed by interventional radiologists to treat fibroid related issues like heavy periods, painful periods or urinary urgency. its a minimally invasive procedure which treats fibroids without surgery or anaesthesia. Through a tiny hole in the blood vessel in the groin or wrist a small catheter is introduced and advanced in to the blood vessels supplying the uterus and the blood supply to the fibroids is cut off using small particles. the fibroids die and shrink permanently. patient can recover very fast within a few days of the procedure and have complete relief from their symptoms. so its a very effective treatment for fibroids. patients can have pregnancy after this treatment,
#pin hole procedure#interventional radiologists#pin hole procedure performed by interventional radiologists to treat fibroid related issues like heavy periods#painful periods or urinary urgency. its a minimally invasive procedure which treats fibroids without surgery or anaesthesia. Through a tiny
0 notes