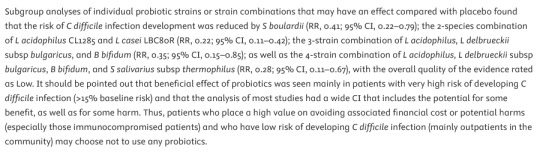
#What is a C. diff. infection?
Explore tagged Tumblr posts
Note
That level of confidence on rejecting anything beyond what a MD will tell you (and not even a DO apparently?) has reached peak stupid I see. Probiotics work. Saccharomyces boulardii straight up saves lives. Come the fuck on.
I haven't criticized DOs, DOs are fully qualified physicians. For those not aware: In the US a Doctor of Osteopathic Medicine (DO) has the same qualifications as an MD; if you want a doctor who does more holistic care but is a real-ass doctor, look for a DO.
DC, doctor of chiropractic, is the degree that you get from the ITT Tech of medical schools to lie to people and call yourself a doctor.
Saccharomyces boulardii is one of the probiotics included in the recommendations of the AGA as conditionally recommended in spite of low quality of evidence.
Saying "probiotics are largely woo" and including a link to A) guidelines that recommend evidence-based use of probiotics and B) a commentary on those guidelines lamenting that the lax regulation of the supplement industry has made it excessively difficult to study potentially helpful interventions is not the same thing as saying "probiotics don't work."
I know it can be hard to see but on tumblr when there's a little line under some words that means the words are a link; you can place your cursor over that link and single-click to go to a different page of the internet that might include more words you can read are a much longer and more comprehensive explanation of the words that you initially clicked on.
There's no conclusive evidence that regular supplementation of probiotics improves digestive issues in healthy people and taking probiotics regularly if you are not at risk for c. diff likely means that you're just shitting money down the drain.
Aspirin saves lives too, but that doesn't mean that literally everyone should take it daily for its life-saving benefits.
I became *absolutely ironclad* in my support for evidence based medicine over medical woo after my chronic illness diagnosis and while trying to figure out how to not feel sick all the time. Getting diagnosed with celiac in 2012 meant getting inundated with books like Wheat Belly and links to Joseph Mercola and advice to take probiotics and to stop eating the yoga mat chemical. Navigating a chronic illness and *massive dietary changes* on an internet awash with medical woo was a nightmare, and you're making the exact same kind of argument that I stumbled across on a ton of forums where parents were trying to treat their kids' symptoms, or where people were searching for help with their own pain and struggles and were getting *bad fucking answers* about probiotics and essential aminos and diatomaceous earth.
Probiotics "work" to help some people in extremely specific situations, but, like most supplementation, they are absolutely unnecessary for the vast majority of people and unless you know that you have a specific condition that will be improved by taking them, you're mostly spending a lot of money to swallow a lot of things and shit them out. If you have a gut disorder, probiotics will not make your gut disorder better. If you have diarrhea as a result of food borne illness, probiotics will not get your poop back to normal. If you are constipated, probiotics will not soften your stools or make you more regular. If you are at risk of c. diff from a course of antibiotics and you are NOT immune compromised, probiotics may potentially reduce your risk of c. diff infection and you should talk to a doctor who is treating you for that specific situation about whether or not probiotics might be helpful in the short term while your gut microbiome recovers from the antibiotics.
233 notes
·
View notes
Text
My body will use its last little bit of strength to menstruate like nothing in the world will stop it except extreme prolonged mental stress. Two years ago I was having the worst ulcerative colitis flareup of my life and battling relapsing c. Diff due to my suppressed immune system and tattered colon, anemic from blood loss and extremely dehydrated and my body used what remaining blood I had to give me the worst period of my life. Those priorities are so wild. Make blood? No. Digest food? No. Fight serious infection? No. Shed uterine lining? Yes.
105 notes
·
View notes
Text
i plan on rewatching the show now that the second season is fully out but i keep thinking ab it so im gonna say some thoughts. warning this is long and rambly—mostly personal opinions and criticisms (not hate)
season one was a fantastic adaptation of the game. the main thing they did right with it was using the most important moments from the game and focusing on that—AND the changes that were made served a purpose to the story or to the world building in general and/or the message the audience is supposed to take away. since it’s a show the gaming aspect of constant enemies and killing doesn’t work the same, it needs to be tactful.
in a s1 interview or episode recap (i can’t recall which) the show creators talked about how they wanted to display violence carefully as to not desensitize viewers. the reason they did this is because in the apocalypse humanity is the last thing we as people have. in a game it’s fun to shoot and find new weapons and whatnot, but in a show your main goal is for viewers to be able to empathize with characters and their actions.
that being said, i think that’s what went wrong in season 2.
first of all, i feel like they did not focus enough on the distinct aspects of the game in the second season. as a show, it felt like the episodes blurred together and nothing really stood out, major moments became minor and they changed some things without there being a clear reason as to why that choice needed made. ex. jesse saving ellie and dina last minute—it would have been more compelling to have ellie showcase her abilities against most of the infected and maybe jesse shows up to kill one suprise stalker. this would show a) ellie’s skills b) how she fights alone (dina being in a safe spot makes sense to me because) c) dina seeing a different side to ellie, more rage, more power (show her feeling both scared and maybe even more attracted to her).
ellie’s game time in the first season has plenty of material that I think could have made a compelling narrative. ep. 1 and 2, generally, were very good with minor complaints. seattle days 1,2,3 are lost on me because it doesn’t feel like very much happened. the joel/ellie flashback episode was super well done imo and i obviously think it’s important to the story—but i do wonder if it’s place is right. i know there were mixed opinions about the porch scene being changed and being so early in the show and i don’t have a solid take on that but i am interested in that decision to move it.
secondly, the violence in s2 did not need to match that of s1 because the circumstances are different. they can still evoke an emotional response from viewers with ellie killing people. i made a post a few years back talking about the music choice when joel kills all the fireflies (x) and i feel like they could have made similar choices. the same way joel killing everyone in that hospital is pivitol to the plot, truthfully ellie is a very similar story.
i don’t think it would be like the game because there’s A Lot of killing enemies in the game, in the show they could’ve built up to it. from a few soldiers to a few more to a group and then she gets to nora. they could imply that ellie is so far removed from killing people in so many ways, and then after what happens with nora—the real violence and rage finally bursts through—the scene with dina cleaning her up would hit so much more, because at this point she has killed so many people and the cognitive dissonance didn’t hit until she finally hurt one of them, someone important, someone who deserved it (or did they?) (side note i did not like dina’s lack of comfort to ellie in the show but diff rant perhaps)
violence doesn’t need to be gory and there’s so many storytelling elements that can be utilized to evoke the emotion you want from viewers. i dont think they made the right choices because while the important scenes (joel’s death, nora, ellie’s bday, abby/ellie confrontation at the end) were done very well, too much of the in between got changed and it’s hard to understand why.
a few random things, ellie and dina should have been trapped together w all the weed, i had hope for whoever slow burn vision they had but again it just felt unclear why they wanted to slow burn it, dina’s character wasn’t given that much more agency or detail than in the game which is the only reason i can think of, but they didn’t do it. the pregnancy reveal into hook up is a bit strange when i think about it—if they wanted to change ellie’s reaction to the news i think that could still work, i think they should have maybe had their relationship established already and could have ellie be shocked and scared and curious and then excited (since pregnancy is a motif almost, kinda life/death kind of thing, also another rant). i personally liked ellie’s “im gonna be a dad” i don’t think it would’ve been as corny if they had don’t everything surrounding it differently.
bc i think it shows ellie is still the silly and loving girl we met in s1, she has someone she cares about again, and something she can look forward to. she never would have expected to responsibility over a child but if it’s with this girl she’s been obsessed with for years then yeah, i think she’d be excited. after she was a bitch to dina in the game she still came around yk? anyway
final part of my rant is the change to jesse where suddenly he’s super mean and doesn’t side with ellie is weird considering we know how his story ends. it’s not a good move to take a character who is important to the plot (friends w ellie and dina, father of dina’s child, works with on the counsel, close with tommy, cares enough to go to seattle for ellie/tommy) be mean and unlikable to audiences. in the game the reason his death hurts is because he is kind, of all people he did not deserve that. just because in the show jesse makes “the right choices” does not make him kind, it makes him arrogant and annoying.
the last episode should have been spent binding ellie and jesse together rather than pushing them apart. then it’s more impactful that ellie chooses to find abby instead of joel, and it emphasizes ellie’s actions directly resulting in the death of someone she cares so much for that had no horse in this race. it feels like bad storytelling to spend an episode of jesse pissing us off and then half making up just to kill him a second later, that is an example of needless violence—exactly what the writers previously said they wanted to avoid.
anyway, i don’t think everything they did was bad, but it is disappointing from the perspective of a tv show. i didn’t want it to be exactly like the game, but i don’t think how they chose to share the second part of this story narratively fit and im disappointed in it myself. i wish a lot of things were done differently. again, i want to watch it again to see if i feel the same so when i do that ill put these biases aside and maybe ill stand by this, maybe i wont. ig we’ll see
#bonk thoughts#to each their own- this is my opinion on s2#i’m trying to judge their story telling not the use of source material because i think that’s not a valid form of criticism#‘bUt in tHe GaMe’ that was the game. this is a show. things are different.#so i care more ab the story being coherent and choices they make that change the narrative and why and all that#if anyone has any other perspectives or thoughts feel free to share#please don’t just shit on the show tho i’m tired of just hearing ‘yeah it was shit’#cause i dont think thats fair#the last of us#tlou#tlou hbo#tlou2#the last of us hbo#ellie williams#joel miller#dina tlou#ellie x dina#jesse tlou
16 notes
·
View notes
Text
Well it's been a rollercoaster of post surgical hospital stay. I came in for surgery on November 25th and am still here! I really, really hope I can go home tomorrow (December 9th) but a lot of that will depend on a scan I have today.
Surgery itself went okay. Although in the surgical prep area my husband and I overheard a bunch of doctors talking about how complicated my surgery was....which wasn't helpful. Especially as the prior surgery was a kidney transplant.
More felt for my husband and sister (my parents were home with my kids) that day as I went to the operating theatre about 7:30am and they didn't get to see me till 11:30pm! What a long, long day for them!
Next couple of days I don't remember much. I did become delirious from pain meds at one point which was again scary for my family.
Next I developed a C. diff infection which was awful. Like terrible, no good, bad in every way. Such such pain.
Pain management throughout has been awful. I am restricted from many types of meds due to my condition so finding a combination that works took forever.
After the infection started to clear up I was still experiencing a lot of focal pain so got sent for a CT. The CT didn't show any specific cause of pain (likely just deep bruising) but did have an incidental finding of an 'ugly' blood clot at my graft site. This was scary as I've actually become temporarily paralyzed from a blood clot before and of course the risk of stroke. So I am glad it was found but also so sad it's delayed my stay. There was lots of talk about whether there should be a surgical removal or treatment with blood thinners. They decided to start with blood thinners so I've been on them for awhile now. I guess my scan today will determine whether I can go home tomorrow (with self injecting blood thinners) or have to stay and possibly have a second surgery.
I really, really want to go home. I miss my kids so much. I miss my bodily autonomy and privacy. I miss my husband (who I sent home this week asvtye kids needed him more) and bed and Christmas tree and real life.
I'm still in pain but I know I'll feel so much better in my own space.
Friends and neighbours have been amazing to my family. There is a meal train and today they've been invited to make gingerbread houses at a neighbours home. The kind of neighbour that does everything from scratch. I hope my kids have felt surrounded by love.
Anyway, please send good wishes that I get to go home tomorrow. It's my husband's birthday (happy birthday to him, 😂).
22 notes
·
View notes
Text
Parasites take an enormous toll on human and veterinary health. But researchers may have found a way for patients with brain disorders and a common brain parasite to become frenemies.
A new study published in Nature Microbiology has pioneered the use of a single-cell parasite, Toxoplasma gondii, to inject therapeutic proteins into brain cells. The brain is very picky about what it lets in, including many drugs, which limits treatment options for neurological conditions.
As a professor of microbiology, I’ve dedicated my career to finding ways to kill dangerous parasites such as Toxoplasma. I’m fascinated by the prospect that we may be able to use their weaponry to instead treat other maladies.
Microbes as Medicine
Ever since scientists realized that microscopic organisms can cause illness—what’s called the 19th-century germ theory of disease—humanity has been on a quest to keep infectious agents out of our bodies. Many people’s understandable aversion to germs may make the idea of adapting these microbial adversaries for therapeutic purposes seem counterintuitive.
But preventing and treating disease by co-opting the very microbes that threaten us has a history that long predates germ theory. As early as the 1500s, people in the Middle East and Asia noted that those lucky enough to survive smallpox never got infected again. These observations led to the practice of purposefully exposing an uninfected person to the material from an infected person’s pus-filled sores—which unbeknownst to them contained weakened smallpox virus—to protect them from severe disease.
This concept of inoculation has yielded a plethora of vaccines that have saved countless lives.
Viruses, bacteria, and parasites have also evolved many tricks to penetrate organs such as the brain and could be retooled to deliver drugs into the body. Such uses could include viruses for gene therapy and intestinal bacteria to treat a gut infection known as C. diff.
Why Can’t We Just Take a Pill for Brain Diseases?
Pills offer a convenient and effective way to get medicine into the body. Chemical drugs such as aspirin or penicillin are small and easily absorbed from the gut into the bloodstream.
Biologic drugs such as insulin or semaglutide, on the other hand, are large and complex molecules that are vulnerable to breaking down in the stomach before they can be absorbed. They are also too big to pass through the intestinal wall into the bloodstream.
All drugs, especially biologics, have great difficulty penetrating the brain due to the blood-brain barrier. The blood-brain barrier is a layer of cells lining the brain’s blood vessels that acts like a gatekeeper to block germs and other unwanted substances from gaining access to neurons.
Toxoplasma Offers Delivery Service to Brain Cells
Toxoplasma parasites infect all animals, including humans. Infection can occur in multiple ways, including ingesting spores released in the stool of infected cats or consuming contaminated meat or water. Toxoplasmosis in otherwise healthy people produces only mild symptoms but can be serious in immunocompromised people and to gestating fetuses.
Unlike most pathogens, Toxoplasma can cross the blood-brain barrier and invade brain cells. Once inside neurons, the parasite releases a suite of proteins that alter gene expression in its host, which may be a factor in the behavioral changes it causes in infected animals and people.
In a new study, a global team of researchers hijacked the system Toxoplasma uses to secrete proteins into its host cell. The team genetically engineered Toxoplasma to make a hybrid protein, fusing one of its secreted proteins to a protein called MECP2, which regulates gene activity in the brain—in effect, giving the MECP2 a piggyback ride into neurons. Researchers found that the parasites secreted the MECP2 protein hybrid into neurons grown in a petri dish as well as in the brains of infected mice.
A genetic deficiency in MECP2 causes a rare brain development disorder called Rett syndrome. Gene therapy trials using viruses to deliver the MECP2 protein to treat Rett syndrome are underway. If Toxoplasma can deliver a form of MECP2 protein into brain cells, it may provide another option to treat this currently incurable condition. It also may offer another treatment option for other neurological problems that arise from errant proteins, such as Alzheimer’s and Parkinson’s disease.
The Long Road Ahead
The road from laboratory bench to bedside is long and filled with obstacles, so don’t expect to see engineered Toxoplasma in the clinic anytime soon.
The obvious complication in using Toxoplasma for medical purposes is that it can produce a serious, lifelong infection that is currently incurable. Infecting someone with Toxoplasma can damage critical organ systems, including the brain, eyes, and heart.
However, up to one-third of people worldwide currently carry Toxoplasma in their brain, apparently without incident. Emerging studies have correlated infection with increased risk of schizophrenia, rage disorder, and recklessness, hinting that this quiet infection may be predisposing some people to serious neurological problems.
The widespread prevalence of Toxoplasma infections may also be another complication, as it disqualifies many people from using it for treatment. Since the billions of people who already carry the parasite have developed immunity against future infection, therapeutic forms of Toxoplasma would be rapidly destroyed by their immune systems once injected.
In some cases, the benefits of using Toxoplasma as a drug delivery system may outweigh the risks. Engineering benign forms of this parasite could produce the proteins patients need without harming the organ—the brain—that defines who we are.
17 notes
·
View notes
Text
Q. What are the more serious potential adverse effects of short-term use of proton-pump inhibitors (PPIs)?

A. Be aware of the rare but serious potential for acute interstitial nephritis or Clostridioides difficile infection. Since PPIs are often started in the ICU for stress, we'll include aspiration pneumonia, instead of aspiration pneumonitis, since higher gastric pH allows more bacteria to live in the stomach and potentially wash into the lungs.
Pro-tip: The risk for C. diff increases significantly after 2 weeks on a PPI.
Image: J.S. Choi, MD
6 notes
·
View notes
Note
i might have already asked, but, opinions on nixos if you've tried it?
i haven't actually tried it but i think it's based and i want to try it really bad. the general premise is that you can fix all of your dependency management and reproducibility problems and replace them with new, more exciting problems that have to do with the nix language
i would very much like to trade to have those problems, because my builds would be so much faster than docker builds. docker builds are also a nightmare because they require a bunch of privileges to even run the docker daemon
so like, a brief list of things you get with nix
verifiable, reproducible builds: you could rerun your build pipeline from scratch and get the same SHA for the final artifact. all of your dependencies are also built with this property. so you basically have transitively pinned dependencies for everything managed by nix. that's huge for security and assurance
great build caching: a side effect of the above, this means you can cache intermediate build results instead of starting the whole build over. and you can be very confident that your cache isn't bringing in stale/incorrect gunk. compare to docker, where caching happens at the layer level, has a bunch of confusing caching rules, and can't account for side effects that make cached layers undesirable. plus the layers build on top of one another, so you can't really pick and choose which layers to cache; if you invalidate a lower layer, everything above it has to be rebuilt, even if the diff would be the same
hermiticity: since you know up front the full list of dependency files you need for your build, you can download those ahead of time and then do the build without talking to the internet! this is another huge win for security, because the internet is where all the fucked up and evil shit comes from, so you want to avoid it wherever possible. reduces your attack surface. this is especially important because infecting the build chain is an increasingly popular attack (supply chain attacks) and extremely effective at owning a ton of computers at once--that package you're building will be trusted by the rest of your machines, so it better be built in a secure environment
avoid a large swath of dependency issues that happen with other package managers: nix lets you have multiple versions of the same package, which removes a lot of pain that happens with other package managers. say you have package A, and package B requires A>=1.3 but package C requires A<=1.0. what do you do? well... you suffer. you also can't install A==5.0 for fun because you live on the bleeding edge. not so with nix
there's probably more goodies im forgetting but yeah. nix is based and solves a lot of cool problems in dependency management, build correctness and speed, and supply chain security. the flip side is that you have to learn a new configuration language just for this one thing, and in addition to being a functional language (which most programmers aren't used to), it has its own quirks and sharp edges because it's somewhat niche. also you have to hope the packages you want are already supported, otherwise you'll have to figure out how to build them yourself.
9 notes
·
View notes
Text
No! Wrong! @transcyberism you are spreading misinformation.
Don't use soap on your genitals at all and don't douche! Plain water on the outside of your ano-genital area is all you need and BE GENTLE!! Moisturise with food oil or petroleum jelly only!!
Anal sex should always be done with gloves and condoms even if you're just using toys, and you should only use glass, metals, and platinum silicone that can be sterilised between sessions. You should, also, just get used to the idea that if you're gonna do anal you're gonna have to get okay with a little bit of poop. That's why you wear gloves and use condoms. Poop is just dirt.
Your body cleans itself pretty well. Your gut flora is very important. The only time you should be doing enemas is if enemas is the actual kink you have, and even then you should be very careful because decimating your gut flora is no joke and western medicine currently does not acknowledge there being a way to fix that unless you have really bad infections of c. diff! NOBODY OTHER THAN PEOPLE WITH REALLY BAD C. DIFF GETS APPROVAL FOR FECAL TRANSPLANTS!! And especially if you have IBS of any kind, you need what little gut flora you still have so don't fuck it up!!
40K notes
·
View notes
Text
Is it really possible to transfer healthy gut bacteria from one person to another to improve health?
Yes, it is absolutely possible and it is already helping many people! This process is called Gut Microbiome Transplants, and it is one of the most exciting developments in digestive health today.
Think of your gut as a busy city filled with tiny helpful workers (bacteria) who keep things running smoothly. But when the balance gets disturbed due to illness, infection, or even too many antibiotics, your gut struggles. That’s where a gut microbiome transplant comes in.
What is a Gut Microbiome Transplant?
It is a medical procedure where healthy gut bacteria from a donor (usually someone very healthy) is transferred to someone who has gut problems. This helps bring back balance and improve digestion.
Benefits of Gut Microbiome Transplants:
Helps treat serious gut infections
Especially effective for Clostridium difficile (C. diff), a harmful bacterial infection.
Improves digestion
Many people report smoother digestion and less bloating after the transplant.
Boosts immunity
A balanced gut supports a stronger immune system.
Reduces inflammation
It may help in reducing inflammation linked to diseases like colitis or Crohn’s.
Restores natural balance
It brings back the ‘good bugs’ that keep your gut healthy.
Key Features:
Done under medical supervision
Involves strict screening of the donor
Usually done through capsules, colonoscopy, or enema
Safe and quick when handled by experts
Gut Microbiome Transplants are showing a lot of promise. They are not just about fixing stomach issues - they can help improve overall health too.
1 note
·
View note
Text
Antibiotics have transformed modern medicine. They save millions of lives by effectively fighting bacterial infections. However, while they eliminate harmful bacteria, they do not distinguish between good and bad bacteria, which can disrupt gut health. This has led to increasing discussions on when to take probiotics when taking antibiotics to minimize digestive side effects and restore microbial balance. Many experts now recommend taking probiotics alongside antibiotics to replenish beneficial gut bacteria. But what is the best time to take probiotics with antibiotics? Can probiotics improve antibiotic effectiveness, and how long should you continue them after finishing a course of antibiotics? This article clears the confusion and provides evidence-based insights into why and when to take probiotics while on antibiotics, their role in gut health, and how to maximize their benefits. Antibiotics and Gut Health: Understanding the Impact Antibiotics are designed to eliminate bacterial infections, but they lack selectivity. It means they kill both harmful and beneficial bacteria in the gut. This unintended side effect can cause digestive imbalances, immune dysfunction, and an increased risk of infections. How Do Antibiotics Work? Antibiotics function by either killing bacteria (bactericidal) or inhibiting bacterial growth (bacteriostatic). They target bacterial cell walls, proteins, or DNA replication, depending on the type of antibiotic used. However, because our gut contains over 100 trillion beneficial bacteria, antibiotics often wipe out both the good and the bad. That leads to gut dysbiosis, which is a condition where microbial balance is disturbed. The Consequences of Antibiotics on Gut Health When antibiotics disrupt the gut microbiome, several issues can arise: Antibiotic-Associated Diarrhea (AAD): One of the most common side effects, AAD occurs in 5% to 35% of antibiotic users, depending on the drug type and dosage. Increased Risk of Clostridium difficile (C. diff) Infection: C. diff is a harmful bacterium that can overgrow when beneficial gut bacteria are depleted. It can lead to severe diarrhea and colitis. Weakened Immune Function: The gut microbiome plays a crucial role in immunity. Hence, disrupting it can lead to higher susceptibility to infections. Digestive Discomfort: Bloating, indigestion, nausea, and loss of appetite are common symptoms of gut microbial imbalance. Yeast Infections: Antibiotics can promote the overgrowth of Candida. It can lead to vaginal thrush and fungal infections. While antibiotics are essential in treating infections, their disruptive impact on gut bacteria has sparked interest in probiotics as a protective measure. Why Take Probiotics for Taking Antibiotics? Probiotics are live microorganisms that help restore balance in the gut microbiome by replenishing beneficial bacteria. These “good bacteria” aid in digestion, immune defense, and overall gut function. Probiotics work by: Competing with harmful bacteria for nutrients and space in the gut. Strengthening the gut lining to prevent infections. Producing antimicrobial compounds that inhibit pathogen growth. Enhancing digestion and nutrient absorption. The Benefits of Taking Probiotics with Antibiotics Research suggests that taking probiotics alongside antibiotics can reduce side effects, restore gut health, and improve treatment outcomes. Reduces Antibiotic-Associated Diarrhea (AAD) A meta-analysis of 34 studies found that probiotic supplementation reduces AAD by 52%. The most effective probiotic strains for preventing AAD are Lactobacillus rhamnosus GG and Saccharomyces boulardii. Prevents C. difficile Overgrowth Probiotics can suppress the growth of C. difficile. It lowers the risk of colitis and chronic gut infections caused by antibiotic use. Enhances Antibiotic Effectiveness Probiotics help increase antibiotic efficacy by reducing bacterial resistance and improving gut absorption of the medication.
Reduces Yeast Infections Women taking antibiotics often experience vaginal yeast infections due to microbial imbalance. Probiotics, especially Lactobacillus strains, can help restore vaginal flora. Boosts Immune Function Since 70% of immune function is tied to gut health, probiotics play a role in immune regulation and reducing post-antibiotic infections. Best Probiotics to Take with Antibiotics Not all probiotics work effectively when taken alongside antibiotics. The right probiotic strain plays a crucial role in reducing antibiotic side effects and restoring gut health. Research suggests that certain strains are more effective than others in replenishing beneficial bacteria. That prevents antibiotic-associated diarrhea (AAD) and improves overall gut function. When looking for the best probiotic for antibiotics, consider the following. Choosing the Right Probiotic Strains When selecting a probiotic to take with antibiotics, consider the following scientifically supported strains: Lactobacillus rhamnosus GG (LGG): One of the most studied probiotic strains for preventing antibiotic-associated diarrhea and gut dysbiosis. LGG can survive stomach acid and colonize the gut. As a result, it reduces antibiotic side effects. Saccharomyces boulardii: This yeast-based probiotic is resistant to antibiotics. That means it does not get destroyed like bacterial probiotics. It helps restore microbial balance and reduce C. difficile infections. Bifidobacterium lactis: It supports immune function and improves digestion. Hence, it helps enhance the gut lining and prevents the overgrowth of harmful bacteria. Lactobacillus acidophilus: Helps maintain gut health and prevents fungal overgrowth. It is particularly helpful in reducing yeast infections caused by antibiotics. Streptococcus thermophilus: Aids lactose digestion and promotes a balanced gut microbiome post-antibiotic treatment. How to Take Probiotics with Antibiotics Start probiotics on the same day as antibiotics, but take them at least two hours apart to avoid direct interaction. Continue taking probiotics for at least one to two weeks after finishing antibiotics to restore gut microbiome diversity fully. Opt for high-quality probiotic supplements with at least 10-20 billion CFUs per dose for maximum efficacy. Consider fermented foods like yogurt, kefir, and sauerkraut to replenish probiotics naturally. When to Take Probiotics While on Antibiotics Timing is crucial when taking probiotics with antibiotics. If taken incorrectly, antibiotics may destroy the beneficial bacteria in probiotics. That will reduce their effectiveness. Let us find out when to take probiotics on antibiotics. Should I Take Probiotics Before or After Antibiotics? To maximize probiotic survival, follow this timing strategy: Take your antibiotic dose first, as prescribed. Wait at least 2-3 hours before taking your probiotic supplement. Repeat this process for every antibiotic dose throughout the day. By spacing out probiotics from antibiotics, you allow probiotics to colonize the gut before being exposed to antibiotic disruption. How Long Should I Take Probiotics After Taking Antibiotics? The gut microbiome takes time to recover after antibiotic use. Experts recommend: At least 1-2 weeks of probiotic supplementation post-antibiotics. 4-6 weeks for individuals with gut sensitivity or previous digestive issues. Long-term probiotic use for those on chronic antibiotic therapy or with weakened immunity. Should You Take Prebiotics with Antibiotics? Prebiotics are non-digestible fibers that feed beneficial gut bacteria and help them thrive. When combined with probiotics, they enhance gut restoration during and after antibiotic treatment. Best Prebiotic Foods to Eat with Antibiotics Including prebiotic-rich foods in your diet can support probiotic function and gut health. Examples include: Leafy greens – Spinach, kale, and dandelion greens.
Root vegetables – Chicory root, Jerusalem artichoke, and jicama. Legumes – Lentils, chickpeas, and black beans. Whole grains – Oats, barley, and flaxseeds. Fruits – Bananas, apples, and berries. By combining probiotics and prebiotics, you support gut flora recovery and enhance digestion post-antibiotic therapy. Do Antibiotics Kill Probiotics? A common concern is whether antibiotics destroy probiotics and make them ineffective. The answer depends on the probiotic strain and timing of administration. Bacterial probiotics (e.g., Lactobacillus, Bifidobacterium) – Can be destroyed by antibiotics if taken at the same time. Yeast-based probiotics (e.g., Saccharomyces boulardii) – Resistant to antibiotics, making them ideal for co-administration. How to Protect Probiotics from Antibiotics To ensure probiotics remain effective, follow these steps: Take probiotics two hours apart from antibiotics. Choose antibiotic-resistant strains, like Saccharomyces boulardii. Consume probiotic-rich foods to reinforce gut bacteria naturally. Can You Take Probiotics While on Doxycycline? Doxycycline is a broad-spectrum antibiotic that treats infections ranging from respiratory conditions to skin infections. It is known for causing digestive side effects and makes probiotics beneficial. Best Probiotics to Take with Doxycycline Lactobacillus rhamnosus GG – Prevents diarrhea and bloating. Bifidobacterium lactis – Supports gut balance. Saccharomyces boulardii – Protects against C. difficile overgrowth. Now, the common question is: when to take probiotics with doxycycline? Since doxycycline affects gut bacteria, one should take probiotics at least 2-3 hours after each dose to minimize disruption. Should You Take Probiotics After a Course of Antibiotics? The gut microbiome does not immediately recover after antibiotics. That makes continued probiotic supplementation essential. How Soon After Antibiotics Can You Take Probiotics? Immediately after finishing antibiotics – To restore beneficial bacteria. For at least two weeks – To stabilize gut health. For up to six weeks – If experiencing digestive issues or weakened immunity. What to Eat While on Antibiotics to Support Gut Health A gut-friendly diet can help counteract the adverse effects of antibiotics and promote faster recovery. Best Foods to Eat with Antibiotics Probiotic-rich foods – Yogurt, kefir, sauerkraut, kimchi, miso, and tempeh. Prebiotic foods – Leafy greens, onions, garlic, and bananas. High-fiber foods – Whole grains, beans, and legumes. Foods to Avoid During Antibiotic Therapy Refined sugars – Promote harmful bacterial overgrowth. Processed foods – Disrupt gut bacteria. Excess alcohol – Weakens gut lining and digestion. By eating probiotic and prebiotic foods, you support gut healing and prevent antibiotic-related digestive issues. how2fit Note Your body is a delicate balance of systems working together, and gut health is a cornerstone of overall well-being. While antibiotics are essential for fighting bacterial infections, they disrupt the gut microbiome. They often lead to digestive discomfort. That is where probiotics step in as reinforcements. They help restore the good bacteria that antibiotics deplete. But gut health is not just about taking supplements; it is about mindful eating, regular physical activity, and a lifestyle that nurtures your body’s natural defenses. A well-balanced diet, rich in prebiotic and probiotic foods, plays a significant role in supporting your digestive system. Also, consulting a healthcare expert can help determine the best probiotic when taking antibiotics and ensure optimal gut health. Remember, good health is a consistent effort to take care of your body. Make mindful choices, and your gut will thank you. The Final Word People often overlook gut health until discomfort arises, but it is one of the most vital aspects of overall well-being.
Antibiotics are a necessity in modern medicine, yet they can disrupt the gut microbiome. They can lead to digestive issues, weakened immunity, and discomfort. Probiotics provide a natural, science-backed way to counteract these effects. They restore microbial balance and enhance gut resilience. The key lies in timing and consistency. Take probiotics at the right time and continue them after antibiotics to ensure complete gut recovery. When choosing a good probiotic after antibiotics, selecting the right strains is essential. Lactobacillus rhamnosus GG, Saccharomyces boulardii, and Bifidobacterium lactis have shown significant benefits in clinical research. Additionally, incorporating prebiotic-rich foods, avoiding excess sugar, and maintaining a balanced diet can help your gut microbiome flourish. By taking a proactive approach to gut health, you not only recover from antibiotic-related side effects but also strengthen your immune system, digestion, and overall well-being. If you are looking for a reliable, high-quality probiotic, the Healthify Pre & Probiotic Capsules offer 30 billion CFU of probiotics combined with 100 mg of prebiotics. It supports digestion, immunity, and gut balance. A healthy gut is the foundation of a healthy body, and how2fit’s trusted probiotic formula can help you maintain that balance. Make gut health a priority, and let your body thrive. Frequently Asked Questions (FAQs) Q: Can you take probiotics when taking antibiotics? A: Yes, you can take probiotics while on antibiotics, but timing matters. Since antibiotics can kill both good and bad bacteria, it is best to take probiotics at least two hours apart from antibiotics. It ensures that the probiotics remain effective and can help restore gut balance without being destroyed. Q: How long should I take probiotics after taking antibiotics? A: The gut microbiome takes time to recover after antibiotic use. Experts recommend taking probiotics for at least two weeks after finishing a course of antibiotics. However, for those with digestive sensitivities, weakened immunity, or gut-related issues, continuing probiotics for 4-6 weeks may be beneficial. Q: When is it best to take probiotics while on antibiotics? A: The best time to take probiotics when taking antibiotics is two to three hours after your antibiotic dose. It helps minimize interference and ensures that the probiotic bacteria can survive and colonize the gut effectively. Maintaining consistency in timing is key to maximizing the benefits. Q: How long after antibiotics can I take probiotics? A: You can start taking probiotics immediately after finishing antibiotics to help restore gut flora. Some studies suggest that the microbiome may take weeks or even months to recover fully, so continuing probiotic supplementation for several weeks can be beneficial. Q: What is a good probiotic after antibiotic treatment? A: A good probiotic after antibiotic treatment contains clinically studied strains like Lactobacillus rhamnosus GG, Saccharomyces boulardii, and Bifidobacterium lactis. These strains help restore gut health, prevent digestive issues, and improve immune function. The Healthify Pre & Probiotic Capsules are formulated to support optimal gut recovery post-antibiotics. Q: How soon after antibiotics can you take probiotics? A: You can start taking probiotics while on antibiotics, but ensure you take them a few hours apart. If you are taking probiotics after finishing antibiotics, start them immediately and continue for at least two weeks for proper gut restoration. Q: How long should I wait to take vitamins after antibiotics? A: Most vitamins and minerals do not interact with antibiotics, but some (like calcium, magnesium, and iron) can reduce antibiotic absorption. It is best to wait at least two hours after taking antibiotics before consuming vitamins to avoid any interference. Research Sources 1. Impact of antibiotics on the human microbiome and consequences for host health
2. Probiotics for the prevention of pediatric antibiotic-associated diarrhea 3. Post-antibiotic Gut Mucosal Microbiome Reconstitution Is Impaired by Probiotics and Improved by Autologous FMT 4. Helicobacter pylori treatment: antibiotics or probiotics 5. Probiotics for the Prevention of Antibiotic-Associated Diarrhea in Outpatients—A Systematic Review and Meta-Analysis: 6. How to get more probiotics: 7. Using Probiotics as Supplementation for Helicobacter pylori Antibiotic Therapy. 8. Post-Antibiotic Gut Mucosal Microbiome Reconstitution Is Impaired by Probiotics and Improved by Autologous FMT 9. Achievements in Public Health 10. Probiotics – NHS 11. Antibiotics – Side Effects 12. The Use of Probiotics, Prebiotics, and Synbiotics as an Alternative to Antibiotics 13. Differential responses of the gut microbiome and resistome to antibiotic exposures in infants and adults
0 notes
Text

Heartburn and acid reflux can be uncomfortable and disruptive, preventing people from enjoying their meals and sleeping well. A lot of people seek relief from Dexilant, a commonly utilized medicine. Although Dexilant works well, the cost may be a concern for people suffering from chronic problems. Fortunately, there are inexpensive choices that provide good heartburn relief. This article will define acid reflux and heartburn, explain how Dexilant works, and discuss cost-effective symptom control options.
Understanding Acid Reflux and Heartburn
What Are Acid Reflux and Heartburn?
Acid reflux occurs when stomach acid flows back up into the esophagus, the tube that connects the throat and stomach. This reverse movement can cause discomfort, resulting in a burning sensation in the chest, which is commonly referred to as heartburn.
Causes of Acid Reflux
Acid reflux occurs when the lower esophageal sphincter (LES) fails to properly close. Some of the most common triggers include:
Eating large meals or lying down right after eating
Consuming acidic, spicy, or fatty foods
Drinking beverages like coffee, soda, or alcohol
Smoking
Stress or anxiety
Risk Factors
Obesity, pregnancy, and certain medical problems, such as hiatal hernia, can all increase the risk of developing acid reflux.
Emerging Insights on Acid Reflux
According to recent study, various hereditary variables, such as LES muscle tone and esophageal sensitivity, may increase the likelihood of acid reflux. Gut microbiota has also been shown to play an important role in acid reflux. Disruptions in the gut microbiome can cause increased inflammation and acid production, resulting in the development of symptoms. This research could lead to novel treatments for gut health, such as probiotics and individualized dietary adjustments to maintain a healthy microbiome.
Impact on Long-Term Health
Untreated persistent acid reflux can lead to esophagitis, Barrett’s esophagus, and even esophageal cancer. Recent research emphasizes the need of quick intervention in minimizing these risks. Avoiding long-term harm requires regular monitoring, lifestyle adjustments, and the use of appropriate drugs. This emphasizes the growing necessity of discovering cost-effective and easily accessible medicines for general health and well-being.
Dexilant: A Closer Look
Dexilant (dexlansoprazole) is a proton pump inhibitor (PPI) that reduces acid production in the stomach. Dexilant lowers acid levels, protecting the esophagus and relieving heartburn symptoms.
Benefits of Dexilant
Dual delayed-release technology gives longer relief, which can last up to 24 hours.
Effective for treating GERD (gastroesophageal reflux disease) and repairing esophageal damage.
Potential Side Effects
Dexilant is effective, however it may cause headaches, nausea, diarrhea, or constipation. Prolonged use may lead to issues such as low magnesium levels or brittle bones.
The Cost Factor
Dexilant’s high cost is justified by its efficacy. Those without insurance or limited coverage may find the monthly expense prohibitively expensive. This is when budget-friendly options become critical.
New Research on PPIs Like Dexilant
Recent study has looked into the long-term health repercussions of using PPIs, including suspected links to kidney difficulties and an increased risk of certain infections such Clostridioides difficile (C. diff). These findings have generated discussions about being more cautious with the use of PPIs and ensuring they are only administered when necessary. This emphasizes the importance of considering cost-effective alternatives to avoid becoming overly reliant on a single medicine.
Emerging Benefits of Dexilant’s Mechanism
Beyond symptom relief, research suggests that Dexilant’s dual delayed-release mechanism may offer other benefits. Its ability to regulate stomach acid levels over lengthy periods of time may be especially advantageous for people who suffer from severe nocturnal reflux or require esophageal repair. However, cheaper comparable medications with the same functionalities are already appearing, offering patients with cost-effective options for managing their money.
Affordable Alternatives to Dexilant
Over-the-Counter Medications
Antacids
Antacids neutralize stomach acid, offering immediate, temporary relief.
How They Work:These medications act by neutralizing stomach acid, reducing esophageal irritation.
Popular Brands:Tums, Rolaids, and Maalox can be purchased for between $5 and $10 per bottle.
Limitations:Antacids are most effective when used sparingly and do not address the underlying causes of acid reflux. Excessive use might have negative consequences like constipation or diarrhea.
H2-Receptor Blockers
H2-receptor blockers lower stomach acid production.
How They Work:These medications suppress histamine, a chemical that causes the stomach to produce acid.
Popular Brands:Famotidine products like Pepcid and Zantac 360 are popular, with prices ranging from $10 to $15 for a modest container.
Effectiveness and Side Effects:They have a delayed onset than antacids but provide longer-lasting comfort. Possible adverse effects include dizziness or fatigue.
Prescription Medications
Proton Pump Inhibitors (PPIs)
PPIs are one of the most effective therapy options for heartburn and acid reflux.
How They Work:They inhibit the acid pumps in the stomach, causing a significant decrease in acid output.
Popular Brands: Nexium (esomeprazole), Prilosec (omeprazole), and Prevacid (lansoprazole) are well-known and cost between $30 and $50 a month.
Generic Options: Non-branded proton pump inhibitors (PPIs), such as omeprazole, cost $10-$15 a month and provide the same level of efficacy as their branded counterparts.
Side Effects: As with Dexilant, prolonged use may result in nutritional shortages or bone issues.
Other Prescription Options
Other drugs that may help those who do not respond well to PPIs include:
Sucralfate:Creates a protective layer on the stomach lining to defend against acid, with a monthly cost of around $20-$30.
Baclofen: Reduces relaxation of the lower esophageal sphincter, which prevents acid reflux. Monthly costs range from $15 to $40.
New Non-PPI Options
Emerging alternatives to standard PPIs, such as potassium-competitive acid blockers (PCABs), offer potential. Medications like vonoprazan act faster and may have fewer long-term negative effects than PPIs. Though not yet widely available, preliminary research suggests they could provide effective relief for chronic heartburn at a cost comparable to present treatments.
Combination Therapies
Recent research suggests that combining drugs, such as sucralfate and a PPI, can improve the efficacy of treatment for severe reflux. These mixes protect the esophagus by reducing acid production, providing total comfort. They also underline the importance of consulting with a healthcare professional to tailor medicines to individual needs, hence improving efficacy and cost-effectiveness.
Lifestyle Modifications for Heartburn Relief
Aside from medicine, lifestyle changes can considerably reduce heartburn symptoms.
Dietary Changes
Certain foods and drinks can trigger acid reflux.
Foods to Avoid: Avoid eating citrus fruits, tomatoes, chocolate, coffee, and spicy or fatty foods.
Better Choices: Choose bananas, oats, lean meats, and non-citrus veggies.
Tip: Eating smaller, more frequent meals may help reduce symptoms.
Recent studies also show that limiting late-night eating and finishing meals at least three hours before bedtime can significantly reduce nocturnal heartburn. Choosing herbal teas like chamomile or ginger tea over caffeine-containing beverages might help relax the digestive tract and prevent reflux symptoms.
Weight Management
Carrying extra pounds can put stress on your stomach, leading to an exacerbation of acid reflux.
Why It Matters: Losing 5-10% of your body weight can help improve your symptoms.
How to Start: To achieve long-term weight loss, combine consistent physical exercise with a well-balanced diet.
According to new research, prioritizing core-strengthening activities such as yoga or Pilates not only helps with weight management but also improves digestive health by improving posture and relieving stomach pressure. Including these workouts in your weekly routine may also help reduce episodes of reflux.
Lifestyle Habits
Stress Management: Practice relaxation techniques like deep breathing or meditation.
Sleeping Posture: Prop your head up with a wedge cushion and avoid eating within 2-3 hours of going to bed.
Avoid Tight Clothing: Loose clothing can help relieve abdominal pressure.
Choosing the Right Alternative
Personalized Approach
Everybody has various symptoms and needs. Take into account Remember:
Severity of your symptoms
Medical history
Budget and insurance coverage
Recent advances in pharmacogenomics suggest that genetic testing may soon be used to assist choose the best medicine for treating acid reflux. These tests may be able to predict how well your body will process particular medications, resulting in more targeted and effective therapies. Despite being in development, this strategy has the potential to reduce the guesswork associated in medicine selection.
Consult a Healthcare Provider
A physician can recommend the most appropriate treatment plan based on your specific needs. Other solutions or alternative therapies may be equally effective as Dexilant but significantly less expensive.
Pharmacists can also help you identify more affordable solutions. Numerous pharmacies now provide consultation services to assist patients in understanding pharmaceutical options and potential savings schemes. These services may also include offering discount cards or access to manufacturer coupons, which can help make treatment more inexpensive.
Why Choose Our Online Pharmacy Referral Service?
If you require low-cost heartburn medicine, our online pharmacy referral service can help. Here’s the reason:
Affordable Options: We connect you with pharmacies that offer the most affordable prices for both prescription and non-prescription medications.
Convenience: Make purchases from the comfort of your own home and have medications delivered to your door.
Quality Assurance: Working with accredited pharmacies ensures the availability of safe and effective pharmaceuticals.
Support: Our team can assist you in finding the best treatment that fits your budget and matches your needs.
Conclusion
Heartburn can be properly treated without the high cost of Dexilant. Over-the-counter drugs including antacids and H2-receptor blockers, as well as prescription PPIs and generic versions, give cost-effective treatment. Adding lifestyle changes to these therapy can lead to better results.
Before commencing any drug, consult with a healthcare expert to determine the best option for your specific needs. If you’re looking for low-cost heartburn relief drugs, check out our online pharmacy referral service. Say goodbye to acid reflux without breaking the wallet.
365scriptcare.com is an established pharmacy referral service. Order brand name and generic equivalent drugs online from a trusted Canadian drug source. Log onto http://www.365scriptcare.com to see how you can buy discounted drug prices shipped to the USA from Canada.
0 notes
Text
Hard Roads
I stand - ready, willing, and able to reap what I sow and sow what I reap - so be ready to get bloody & smell death! 💀
Everybody claims, "Oh my life is so hard! My hair won't set or my food is cold. Or politics is...blah blah..I need my Versace purse! College is sooo hard, I failed underwater basket weaving! I was abused! I drink two bottles of vodka every night..." Whatever!
Who cares about petty problems? Get over them! It doesn't take a genius. I liked alcohol too much and so I stopped drinking it. No AA or therapy, just stopped. Ppl can stop, they just don't want to. They're weak. Both my grandma & my mom both stopped drinking without anyone but their doctor knowing. Same here. Counselors ask me how?? I said, "Don't buy alcohol & don't drink any."
My grandparents on both sides were galvanized. They were born in 1921, at least my maternal side was. I think my dad's dad, grandpa Ben, was born in 1918, and grandma Jane was born in 1921. Grandpa Ben, I'd love to try my necromancy with. He sounded cool. A machinist! I never heard anything about him or his life, temperament, likes, dislikes, etc. But I have a feeling he had the Thorp family power. My dad passed it to me & my brother got none!!
Story goes: August 22nd, last year. I heard three, very intentional knocks - evenly dispersed and firm. Thought to myself: "Three knocks usually means someone is gonna die." I put the thought away. August 23rd - I text my brother asking how dad & the family is. I get his text later saying the nursing home had him rushed to the hospital.
My brother offers to drive 2 hours South to pick me up. We go to the hospital and find out dad looks terrible and cannot talk due to his dementia and he has C. Diff infection! Awful! He's on aggressive antibiotics & is in so much pain, I can see it on his face. Imagine looking at your father, in agony, & you cannot exchange words! How hard is life now, puny political protester?! Lol! Fucking weak willed children!
So yeah..my brother & I (moreso ME) talk to palliative care the next day - the 24th. We (I, again) decide to take dad off of antibiotics because we know he's not going to make it, he's miserable & we want him comfortable. He got the morphine, thank god!! The next day, he is dead, and the nurses didn't have the decency to fucking close his eyes. They could have before rigor mortis set in. Fuck! So Jerry, my brother, the *atheist* couldn't believe how I basically knew there was something wrong with dad!
Of course I knew! There is the Thorp family power. Dad had it strong & for years I didn't know or believe him! He was always so intuitive compared to my brass knuckled mom. She loved psychic shit but had no measurable gifts of her own. She may have, but was so uptight that she couldn't access them.
And now, I have little family left. My son, my brother & nephew. A few aunts, a couple blood related uncles, some cousins & little known relatives (like 3rd cousins) in Germany. None of these relatives are near me, except my brother & nephew. How little my family is!
But alas! I have my husband. We are all each other needs. Sounds lonely but we're not at all. 😘 Ppl think that you need to be social. Well, being around others is very draining & tiring. I pick up all the energies if my guard is down. Putting on a show for others is exhausting & pointless. I'm not putting on airs or being egotistical. I tell the truth. And the Thorp family power lets me see the real person you are & I'm rarely wrong.
Mmmkay. Ready & done with this post!
M.M. 💖💀💖
0 notes
Text
A Global Stroll In the Park To Raise C. diff. Awareness On September 25th
A Global Stroll In the Park To Raise C. diff. Awareness On September 25th
Join Us For a Stroll In the Park on September 25th In-Person, and On-Line To Raise C. diff. Awareness Around the Globe! September 25th is right around the corner and we are so excited to have this opportunity to walk together either in-person at the following park locations: Sims Park, New Port Richey, FL Milton A. Votee Park, Teaneck, NJ Brown Street Park Complex, Spring City,…

View On WordPress
#Are there ways to tell others about C. diff?#C Diff Awareness#C. diff. Community Events#C. difficile Awareness#Global C. diff. Awareness Walk#How Antibiotics trigger C. diff. Infections#How can I get involved in a clincial trial?#How can I learn more about C-diff#What is a C. diff. infection?#What is C. difficile?
0 notes
Text
got that end of project buzz andnothing to do with it. i don’t even have money to buy cider or something until i get paid next week for the projects!
#also in the middle of what is hopefully a c diff scare and not an actual re-infection so. i should not be doing anything anyway#but what do i do with all of this energy.....laundry?
4 notes
·
View notes
Text
Different types of Infected (All Infected have an expiration date, some shorter then others.)
Walkers/Shamblers: Standard zombie entities. Shoot them in the chest with widespread weapons, or rip out their lungs somehow. Destroy the Infection to end them.
Crawlers: Legless Walkers. Crawl extremely fast due to overuse of upper body. Destroy the head first, or throw them off buildings.
Headers: Headless Infected. Lost souls without heads, they wander aimlessly. The least dangerous entities aside from Infected animals. Let them die out on their own.
Shriekers: Mutated Infected. Elongated limbs and necks, their jaws extending all the way down to their clavicles. Take them out before they unhinge said jaw, or you're in for a world of hurt. Summon Tanks, Prowlers and Spewers with an earsplitting shriek that echos out pretty far. Pretty fragile though, go for the legs and then the lungs/heart.
Tanks: Mutated Infected. Infection goo covers their upper bodies, contorting it into a very large and muscular shape. Not much can destroy them, fire, explosives, and corrosives are powerful here. Destroy their arms first.
Spewers: Mutated Infected. Extremely swollen bodies, full of corrosive bile that they spit up on prey. The smell, which can only be described as "decaying, rotten flesh mixed with horse shit and c-diff" attracts Walkers, who converge on the prey and devour it whole. Explosive rounds or weapons are essential. Blow up their stomachs to throw acid everywhere.
Witches: Mutated Infected. Usually small girls. Don't appear infected, untill you get close. Eyeless, mouthless creatures with acute hearing and the same earsplitting scream as Shriekers. Extremely large claws and spines down their backs. Kill them before they hear you. Use long range weapons.
Prowlers: Mutated Infected. Avoid large piles of skinned bodies. Prowlers gather in packs with Walkers and Shriekers. Extremely agile, yet small. Extremely powerful legs and super sharp claws. They jump on you, claw your clothes off whilst laughing like hyenas, and then eat your skin. Always just the skin. Rather easy to avoid, however, if you get past the Shriekers they pair with.
Animalia: aInfected animals. Usually die out within a few weeks to months. Larger animals take longer. Will sometimes mutate. Not dangerous to humans. (See Fenne.)
The Grey One: The Source. The nest of the horde in Burrow City. Avoid at all costs without Furis in the group, otherwise you'll never return alive. Essentially a massive pulsating heart that spits out mutations and Infected at random, surrounded by the walls of the facility and backed by S.S.P.A.R.K and the hordes of loyal Infected. Can only be destroyed by what made it. (Hint hint)
You know what, fuck it
Heres my notecard of all the stuff for the Zombie AU. Some of this is spoilers, but I know somebody ( @lex165 ) will mind his business and not look-!
Your characters are new stragglers heading into the city. Upon crossing the bridge, you're met with Furis, who guides you into Nazareth, an 8 block square centered around an old church on the riverside that has been converted into a demonology worship hub. He provided food and shelter for as long as you wish to stay there, but there are secrets in the walls and out in the city beyond. Infected trail the streets, strange mutated ones haunt the nights. Will you all make it out alive?
Infection Information: The Infection started as a cure for cancer. Scientists accidentally over-mutated it, and it caused the patient's cancer cells to be destroyed, but also shot the regeneration of cell to shit, so the body couldn't keep up and fell apart. The first outbreak was contained within the facility, so only a few were infected and all those ones died. They tried again, with less mutations, and it seemed to work for a little bit, no skin sloughing off or chunks disintegrating. But the Infection formed in the lungs, slowly growing and changing and mutating into something almost sentient. This is where Furis comes in. Hehehehehehehehehehehehehe.The sentient Infection (refered to as The Source) grew and grew in his lungs until it violently exploded out of him, killing him at 13. His body was kept stable and safe whilst the second outbreak happened, infecting the entire US and forcing the UN to close down its borders. He awakens 5 years later, and stumbles out into the world, very much gross and infected, but still conscious. Cue stumbling into Nazareth, where a bunch of kids promptly jump him with wooden planks. After smacking him around a bit, he explains who he is, what happened, and that he can help them. They get him dressed and patched up and now he lives with them, keeping them safe and helping the adults fight the Infected.
1 note
·
View note
Text
Monopolizing turds

Update 31 May 2023: an earlier edition of this article identified the price of Rebyota as $20,000; this was the rumored price prior to Rebyota’s release in December 2022, when Stephen Skolnick wrote the article I referenced. When Rebyota was actually released in 2023, the average wholesale price (AWP) was $10,800. Thanks to Benjamin Jolley for catching this error, and to Stephen Skolnick for getting to the bottom of it.
It’s been ten years — to the day! — since I first started writing about the bizarre, amazing world of turd transplants, in which a sick person receives a microbiotic infusion in the form of some processed poop from a healthy person:
https://web.archive.org/web/20130608030455/http://blogs.plos.org/publichealth/2013/05/29/why-diy-fecal-transplants-are-a-thing-and-the-fda-is-only-part-of-the-reason/
Gut biomes are one of those understudied, poorly understood medical areas that are both very promising and also full of sketchy medical claims from “supplement” companies, influencers, quacks and grifters. But in the decade since I first started tracking turd transplants (formally called “Fecal Microbiota Transplants” or FMTs), a growing body of sound science has emerged on the subject.
One thing that’s increasingly undeniable is that the composition of your microbial nation is related in significant ways to both your physical and mental health. What’s more, as antibiotic resistant “super bugs” proliferate, FMTs are becoming increasingly central to treating dangerous gut infections that otherwise stand a high chance of killing you.
“Eat Shit and Prosper” is Stephen Skolnick’s delightfully named newsletter about poop and health science. Skolnick is a physicist by training, but has a long history of collaboration with Openbiome, a nonprofit that coordinates between doctors, patients and donors to provide safe FMTs:
https://stephenskolnick.substack.com/
In an edition of Eat Shit from last December, Skolnick recounts the amazing history and dismaying future of FMTs. In 2013, the FDA announced it would regulate FMTs as “Investigational New Drugs,” which could only be administered as part of a registered clinical trial:
https://stephenskolnick.substack.com/p/a-monopoly-on-poop
At that point, FMTs were already in widespread use by docs to treat otherwise untreatable cases of Clostridioides difficile (C. diff), an antibiotic resistant bacterial infection that literally makes you shit yourself to death. These doctors were in no position to run registered clinical trials, which meant that they would have to stop using the most effective therapy they had for a potentially lethal infection.
Doctors and patients kicked up a fuss, and the FDA walked back its guidance, announcing that it would exercise “discretion” in enforcing its Investigational New Drug rule, giving a pass to docs who were treating C. diff with FMTs:
https://www.federalregister.gov/documents/2013/07/18/2013-17223/guidance-for-industry-enforcement-policy-regarding-investigational-new-drug-requirements-for-use-of
That’s where things have stood for the past decade or so. The “discretion” rule means that patients could still get FMTs, but their insurance wouldn’t cover it. But even if you had cash to pay for an FMT, your doc probably wouldn’t administer it for anything except a C. diff infection, despite the promising signs that FMT can help treat other conditions, and despite the generally safe nature of FMTs.
If your doc did give you an FMT, chances are good that they sourced their poop from Openbiome. Openbiome recruits very healthy people, gets them to poop in a bag, then processes the poop — removing nonbacterial solids, testing it for pathogens, freezing it, portioning it, and sending it to docs. All this is done at cost, and it’s not cheap: $1–2k/treatment, mostly due to cold-chain logistics (the poop is shipped at -80C).
Despite the cost, and despite the limitations on treatment, the Openbiome method has proved very reliable. Indeed, FMTs as a whole are pretty darned safe, with the most common side-effects being transient gas and bloating. In the past decade, there’ve been a total of six “adverse effects” associated with Openbiome’s 5,000+ procedures, all in severely immunocompromised people, and none conclusively linked to the treatment:
https://www.sciencedirect.com/science/article/pii/S0016508522003511/pdf
A decade into this system, the FDA has taken the next step forward — only it’s actually a step backwards.
During this intervening decade, a pharma company called Ferring has conducted clinical trials on FMTs and received approval for an FMT product called Rebyota. The process for making Rebyota is effectively identical to the process used by Openbiome: collect poop, remove solids, test for pathogens, add glycerol, freeze and ship.
The main difference between Rebyota and Openbiome’s poop is price. While Openbiome charges $1–2k per treatment, Rebyota charges $10,800
That’s some expensive shit!
Fine. Getting Rebyota through clinical trials means that insurers might start covering it, and perhaps some patients will prefer brand-name poop to open-source poop. But as part of the FDA’s approval of Rebyota, the agency also rescinded its “discretionary enforcement” guidance, making it illegal for docs to source their poop from Openbiome:
https://www.fda.gov/regulatory-information/search-fda-guidance-documents/enforcement-policy-regarding-investigational-new-drug-requirements-use-fecal-microbiota
For Ferring, this is a monopoly on shit, one that lets them charge patients $10.8k for poop that costs $1–2k to process. The FDA does not claim that this is being done in the name of safety. Instead, an FDA official told Skonick that the goal was to “incentivize innovation without creating an access crisis.”
That is, the FDA changed its guidance and put nonprofit stool banks out of business because it wants to incentivize pharma companies to perform expensive clinical trials, and it believes that these companies won’t pay for trials if they have to compete with the likes of Openbiome, which would make it impossible to charge 900% markups on poop.
Trials are important! Evidence-based medicine is important! But Ferring’s clinical trials didn’t tell us anything we didn’t already know. FMTs were already the best therapy we had for C. diff. Testing Rebyota against a placebo didn’t tell us anything new — unlike testing Rebyota against the existing therapies, e.g. product from open stool banks.
Such a trial might have given rise to a very different regulatory outcome, because the cure rate reported by Rebyota is much lower than the cure rate from Openbiome’s own interventions:
https://link.springer.com/article/10.1007/s40265-022-01797-x
That is, using the $1k poop from Openbiome seems to be much more effective than using the $10.8k poop from Ferring. But Openbiome, a nonprofit, hasn’t been able to perform the kind of rigorous — and expensive — clinical trial that Ferring funded.
This points to a significant problem with the FDA’s model. The agency wants good clinical data for the medicines it regulates, as it should, It presumes that the only way to get that data is through granting commercial exclusivity to a for-profit, which ends up costing patients vast sums, and locking many patients out altogether.
This creates all kinds of new dangers. 150,000 people/year in the US contract Recurrent Clostridium difficile Infection (RCdI). FMT increases the cure rate by 20% relative to antibiotics alone. That means that if everyone with RCdI gets a poop transplant, 30,000 extra people will get better. That’s a big number!
For well insured people, Rebyota probably represents a cash-savings — if your insurance covers the $10,800 procedure, you might pay $500 out of pocket, which is far less than the $1–2K you’d pay to get an Openbiome poop transplant. But if you’re uninsured or underinsured, the FDA’s new enforcement rules mean that you’re now on the hook for $10,800.
The FDA did carve out a loophole: if your doc or their hospital are willing to prepare the poop transplant themselves, they can administer that. On the one hand, preparing a poop transplant isn’t that hard — some people do them at home, on their own:
https://web.archive.org/web/20211015060558/https://thepowerofpoop.com/epatients/fecal-transplant-instructions/
But on the other hand, there’s been exactly one death conclusively linked to FMT, and it was from one of these hospital-prepared transplants (the patient had just had a marrow transplant for cancer that wiped out their immune system, and the donor had a novel pathogen that the hospital failed to test for).
So the FDA has created a situation where, if you can’t afford a $10,800 proprietary formulation, your only option is to convince your doc or hospital to prepare their own poop transplant, which will cost less than the $10.8k for Rebyota, but more than the $1–2k from Openbiome, which has all kinds of economies of scale. And if you do manage it, you’ll be getting a procedure that has a much worse safety track-record than the Openbiome process that the FDA just killed.
The FDA has an important role to play here, but as with so many policy questions, how the FDA plays that role depends on things that are far upstream from the agency and its decisions. The choice to fund medical trials through the promise of exclusivity — and with it, extremely high margins — puts the FDA in the position of choosing winners in the marketplace: Ferring wins, Openbiome loses.
Ironically, this is the thing that exclusivity is supposed to prevent. By using profit to incentivize medical research, the FDA is supposed to be recruiting the Invisible Hand as its partner in regulation. But exclusivity is incompatible with the idea of medicine as a public good. The tens (hundreds) of millions that Americans will pay for $10.8k poop transplants from Ferring will add up to far more than it would cost to underwrite clinical trials for an open process like Openbiome’s.
The result: both Americans’ wallets and Americans’ guts suffer.
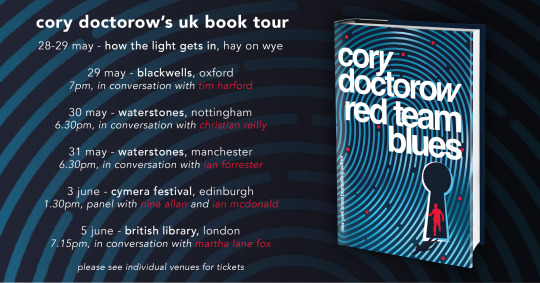
Catch me on tour with Red Team Blues in Hay-on-Wye, Oxford, Manchester, Nottingham, London, and Berlin!

If you’d like an essay-formatted version of this post to read or share, here’s a link to it on pluralistic.net, my surveillance-free, ad-free, tracker-free blog:
https://pluralistic.net/2023/05/29/oh-shit/#rebyota

[Image ID: A poop emoji wearing a top hat and a monocle, posed against a backdrop of e coli bacteria seen through a high-resolution microscope.]
#pluralistic#stool bank#eat shit and live#pharma#fda#regulatory capture#fecal transplants#microbiomes#rebyota#openbiome#c diff#fmt#fecal microbiota transplant
271 notes
·
View notes