#medical coding icd 10
Explore tagged Tumblr posts
Text
#ICD10 coding services#ICD10 coding services in medical billing#ICD10 coding services in US#medical coding icd 10#Outsource ICD coding services#best ICD10 coding services#ICD coding service providers in the US
0 notes
Text

My medical coding book has a whole section for heelies accidents.
2 notes
·
View notes
Text
I need everyone to be aware of this right now
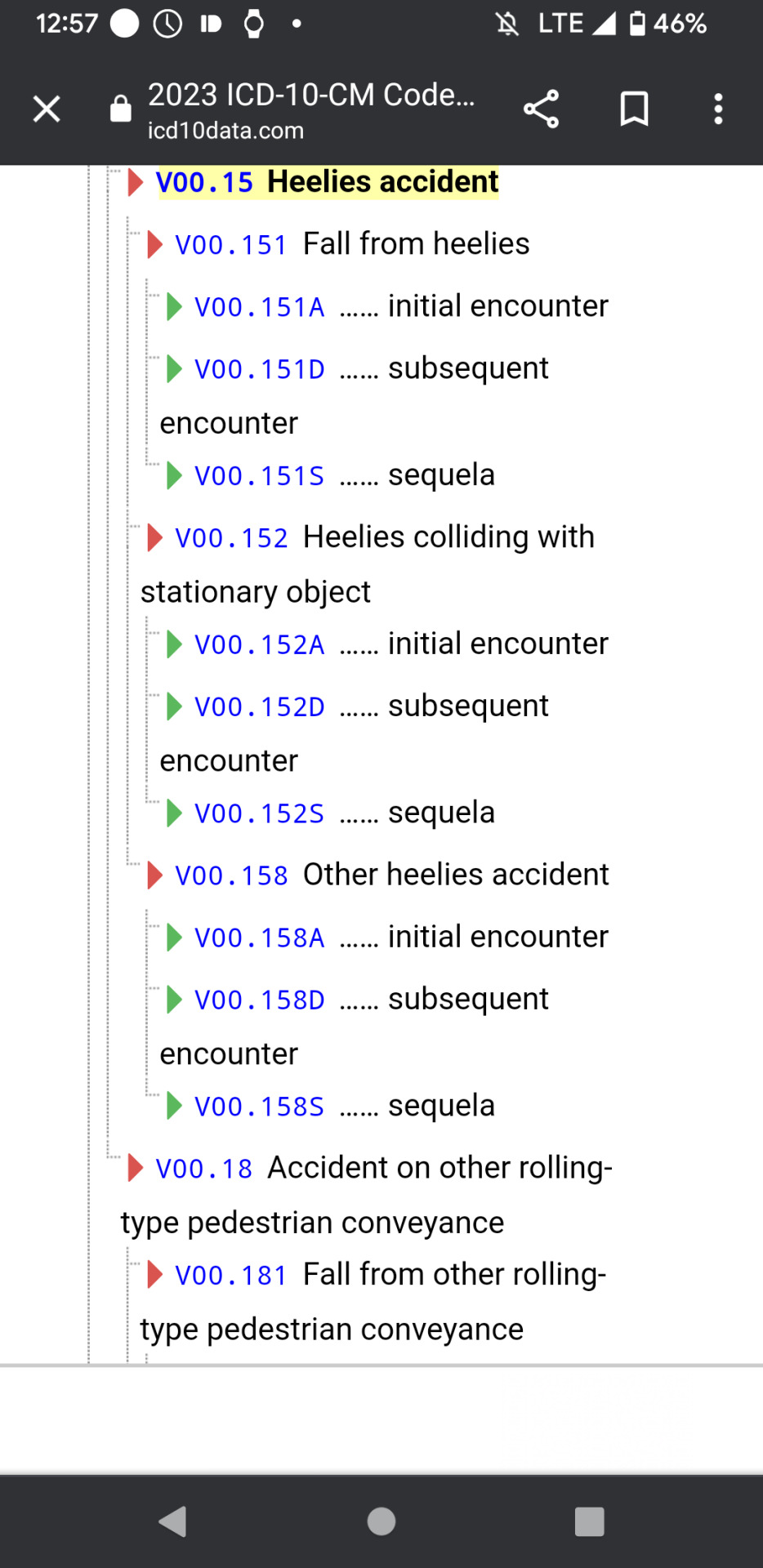
This is a real ICD-10 diagnostic code.
12 notes
·
View notes
Text
Common ICD-10 Codes Used in Primary Care [2025 Edition]

Primary care is the foundation of the healthcare system, covering everything from preventive services and chronic condition management to urgent care and routine screenings. Given its wide scope, primary care professionals encounter a vast variety of diagnoses on a daily basis. That’s why quick access to the most commonly used ICD-10 codes is essential. It supports accurate clinical documentation, streamlines insurance claims, enhances billing efficiency, and ensures compliance.
With stricter reimbursement policies, increased audit scrutiny, and a higher risk of denials due to coding mistakes, accuracy has never been more critical. Primary care providers often shift rapidly between tasks like wellness visits, managing diabetes, treating respiratory infections, and administering vaccines. In such a fast-paced environment, having reliable, up-to-date coding tools becomes a game-changer.
This blog highlights a 2025-ready list of the most frequently used ICD-10 codes in primary care, offering a practical reference for busy clinicians.
Most Common ICD-10 Codes in Primary Care Clinics
Primary care providers are often the first point of contact for patients, managing everything from preventive screenings to acute and chronic conditions across all age groups. Given this wide range of responsibilities, it's crucial to be familiar with the most frequently used ICD-10 codes. Below is a categorized list of top ICD-10 codes commonly used in primary care as of 2025:
1. Preventive Visits and Wellness Checks
Routine health assessments are a frequent reason for visits. Common codes include:
Z00.00 – Adult general exam with no abnormal findings
Z00.01 – Adult general exam with abnormal findings
Z00.129 – Child wellness check without abnormalities
Z00.121 – Child wellness check with abnormalities
Z13.6 – Cardiovascular screening
Z13.89 – General health screening
Z23 – Immunization encounter
2. Respiratory Conditions
Often seen during flu seasons or among patients with chronic respiratory issues:
J00 – Common cold
J02.9 – Acute pharyngitis, unspecified
J06.9 – Acute upper respiratory infection
J18.9 – Pneumonia, unspecified
J20.9 – Acute bronchitis, unspecified
J30.9 – Unspecified allergic rhinitis
J45.909 – Uncomplicated asthma, unspecified
J44.9 – Chronic obstructive pulmonary disease
J40 – Bronchitis, unspecified
3. Infections & Acute Illnesses
General infections and acute complaints use the following codes:
B34.9 – Unspecified viral infection
N39.0 – Urinary tract infection, unspecified site
4. Chronic Disease Management
Long-term condition management is a core responsibility:
Metabolic/Endocrine:
E11.9 – Type 2 diabetes, no complications
E11.65 – Type 2 diabetes with hyperglycemia
E78.0 – Pure hypercholesterolemia
E78.5 – Unspecified hyperlipidemia
E03.9 – Unspecified hypothyroidism
E66.9 – Unspecified obesity
E63.9 – Nutritional deficiency, unspecified
Cardiovascular:
I10 – Primary hypertension
I11.9 – Hypertensive heart disease, no failure
I20.9 – Unspecified angina
I25.10 – Coronary artery disease without angina
I25.110 – Coronary artery disease with unstable angina
I48.91 – Atrial fibrillation, unspecified
I50.9 – Heart failure, unspecified
5. Musculoskeletal Issues
Frequently used for joint, muscle, and back pain:
M54.5 – Lower back pain
M25.50 – Joint pain, unspecified
M19.90 – Unspecified osteoarthritis
M75.100 – Rotator cuff tear, unspecified
M17.9 – Osteoarthritis of knee, unspecified
M79.1 ��� Muscle pain (myalgia)
6. Mental and Behavioral Health
Mental health is often addressed in primary care:
F32.9 – Unspecified depression
F41.1 – Generalized anxiety disorder
F43.2 – Adjustment disorder
F50.9 – Eating disorder, unspecified
F90.9 – ADHD, unspecified type
7. Neurological and Sleep Disorders
G47.33 – Obstructive sleep apnea
G43.909 – Unspecified migraine
8. Gastrointestinal Conditions
K21.9 – GERD without esophagitis
K29.70 – Unspecified gastritis without bleeding
K58.9 – IBS without diarrhea
K64.4 – Unspecified anal fissure
K75.9 – Unspecified liver inflammation
9. Dermatologic Conditions
L03.90 – Unspecified cellulitis
L20.9 – Atopic dermatitis
L30.9 – Unspecified dermatitis
10. General Symptoms and Pain
R07.9 – Chest pain, unspecified
R10.9 – Abdominal pain, unspecified
R51.9 – Headache, unspecified
R53.83 – Fatigue
R63.4 – Unintended weight loss
R63.5 – Unusual weight gain
11. Social and Environmental Influences
Z20–Z29 – Exposure to infectious diseases
Z55–Z65 – Social or psychological risk factors
Z71–Z76 – Health service encounters (e.g., counseling, follow-ups)
2025 Billing Best Practices for ICD-10 in Primary Care
Be Specific: Use the most precise and current code available to avoid denials.
Annual Updates: ICD-10 codes are revised every October—always use the latest version.
Symptom Coding: Only use symptom codes (R00–R99) when a diagnosis is unclear.
Proper Code Linkage: Pair ICD-10 codes with CPT/HCPCS codes to support medical necessity.
EHR Integration: Use smart, cloud-based platforms that suggest accurate codes in real time.
How 24/7 Medical Billing Services Can Help
24/7 Medical Billing Services enhances accuracy and speed in ICD-10 coding with expert support and cutting-edge tools. Their certified coders stay current with 2025 updates, ensuring precise documentation, fewer denials, and stronger compliance. Outsourcing primary care billing and coding services to 24/7 MBS provides seamless EHR integration and boosts reimbursement efficiency—helping your primary care clinic focus on patients, not paperwork.
Content Source: [https://www.247medicalbillingservices.com/blog/common-icd-10-codes-used-in-primary-care-2025-edition]
For More Information:
Call us at +1 888-502-0537 or Sales: [email protected]
Support: [email protected]
Visit at https://www.247medicalbillingservices...
Our Office Locations:
Ohio: 28405 Osborn Road, Cleveland, OH, 44140
Texas: 2028 E Ben White Blvd, #240-1030 Austin TX, 78741
Subscribe @247medicalbillingservices
Follow us on social media channels-
Facebook: https://www.facebook.com/247MBS
Twitter: https://x.com/247MBServices
Instagram: https://www.instagram.com/247mbs/
LinkedIn: https://www.linkedin.com/company/24-7-medical-billing-services/
#ICD-10 codes#ICD-10 coding in Primary care#ICD-10 medical coding#ICD-10 billing and coding#ICD-10 coding for hospitals#Primary Care Billing Services#Primary care Coding Company#Primary health care billing#Primary health care billing agency USA#Medical Coding Services#Medical Billing Company#Medical Billing#ICD-10 codes for family physicians#ICD-10 coding#EHR coding#ICD-10 billing for outpatient care#Medical Coding Services Florida#Best Medical Coding Services USA#Medical Billing Services USA#Outsourced Medical Billing#Outsourced Medical Coding Georgia#Medical coding agency Connecticut#Top Medical coding companies#Medical coding for providers Ohio#Outsource Medical Coding Oklahoma#Outsource Medical Coding Oregon#Outsource Medical Coding Pennsylvania#Medical Coding Maine#Medical Coding Massachusetts#Medical Coding Services California
0 notes
Text
Top 10 Medical Coding Errors in 2025 and How to Prevent Them

The world of medical billing and coding is evolving rapidly. In 2025, new technologies, shifting payer guidelines, and the ongoing transition to value-based care have brought both major advancements and new challenges. Amid these changes, one issue continues to plague healthcare providers: medical coding errors.
From claim rejections and payment delays to compliance risks and revenue leakage, coding errors can have costly consequences. This guide—created by experts in medical coding services—dives into the Top 10 Medical Coding Errors in 2025, and offers clear, actionable strategies to eliminate them.
If you're a healthcare administrator, coding professional, or part of a medical coding company, this guide will help you improve accuracy, minimize denials, and enhance compliance across the revenue cycle.
1. Upcoding and Downcoding: Misrepresentation of Services
The Problem: Assigning codes that inaccurately reflect the level of care provided—either too high (upcoding) or too low (downcoding).
Causes:
Misreading documentation
Revenue pressure or audit fear
Lack of education
Impact:
Denials, audits, legal risks
Solutions:
Documentation training for providers
Quarterly internal audits
NLP tools to assist in code selection
2. Incomplete or Missing Documentation
The Problem: Insufficient clinical detail leads to coding inaccuracies.
Causes:
Clinician time constraints
Inadequate EHR templates
Communication gaps between coders and providers
Impact:
Increased denial rates
Delayed payments
Compliance issues
Solutions:
Tailored EHR prompts
Team-based query culture
Monthly documentation workshops
3. Incorrect Use of Modifiers
The Problem: Misused or omitted modifiers can change the meaning of procedures, affecting reimbursements.
Solutions:
Quick-reference modifier charts
Quarterly training by specialty
Software alerts for incorrect modifier use
4. Using Outdated Codes
The Problem: Failing to update CPT, ICD-10-CM, or HCPCS codes annually results in claim rejections.
Solutions:
Subscribe to CMS, AMA updates
Annual training for coders
Software audits to catch obsolete codes
5. Lack of Specificity in Diagnosis Coding
The Problem: Using unspecified codes when a specific diagnosis is available hurts both revenue and care quality tracking.
Solutions:
Coders should issue clinical queries
Dashboards to track provider specificity
AI-based code suggestion tools
6. Unbundling Services That Should Be Billed Together
The Problem: Reporting bundled procedures separately to increase reimbursement leads to compliance issues.
Solutions:
Integrate NCCI edit checks
Create specialty-specific bundling guides
Peer reviews within coding teams
7. Errors in Telehealth Coding
The Problem: Constantly changing payer rules make telehealth coding prone to error.
Solutions:
Maintain a payer-specific telehealth resource
Conduct regular telehealth compliance training
Use checklists before claim submission
8. Incorrect Principal Diagnosis Assignment
The Problem: Incorrect sequencing in inpatient claims leads to DRG misclassification and underpayment.
Solutions:
Conduct random audits
Train on UHDDS guidelines
Improve physician documentation clarity
9. Duplicate Billing
The Problem: Submitting the same claim more than once—either by accident or system error.
Solutions:
Automated claim scrubbers
Verify status before re-submitting
Reconciliation tools for encounter-to-charge matching
10. Not Adhering to Payer-Specific Rules
The Problem: Each payer has unique coding, billing, and documentation rules.
Solutions:
Maintain a live payer policy manual
Weekly email updates on payer changes
Analyze denial trends for targeted education
Bonus Tips for 2025 Coding Excellence
✅ Invest in Smart Technology
Medical coding companies that use AI, computer-assisted coding (CAC), and predictive analytics can significantly boost accuracy and efficiency—when combined with expert oversight.
✅ Commit to Ongoing Education
Top medical coding services invest in continuous learning. Stay updated with AAPC, AHIMA, CMS, and payer alerts. Regular team huddles can reduce costly errors.
✅ Encourage Clinical Understanding
Coders must go beyond guidelines to understand clinical intent. Host cross-training with providers to close the gap between documentation and accurate coding.
✅ Track and Improve KPIs
Use coding performance metrics such as:
Coding accuracy rate
Coding-related denial rate
Query turnaround time
DRG mismatch trends
These metrics help identify gaps and training needs—enabling your medical coding company or internal team to continuously improve.
Final Thoughts:
Whether you're a hospital, private practice, or part of a growing medical coding company, reducing errors in 2025 requires a proactive, tech-enabled, and education-driven approach. By implementing these strategies and partnering with the right medical coding services, healthcare organizations can achieve accurate coding, faster reimbursements, and stronger compliance.
For more information: https://www.allzonems.com/top-10-medical-coding-errors/
#Medical coding errors#medical coding services#medical coding company#coding-related claim denials#ICD-10 coding errors#CPT coding accuracy#healthcare coding compliance#medical billing and coding#medical billing services#medical billing solutions#cpt coding services#cpt coding solution#denial management services#denial management company
0 notes
Text
Bakit Mas Maraming Mga Teenager ang Nagkakaroon ng Prediabetes?
#7-day meal plan for prediabetes#can prediabetes be reversed#diet for prediabetes#how to reverse prediabetes#how to reverse prediabetes in 3 months#icd 10 code for prediabetes#icd 10 prediabetes#prediabetes#prediabetes a1c#prediabetes a1c range#prediabetes diet#prediabetes icd 10#prediabetes medication#prediabetes range#prediabetes symptoms#prediabetes treatments#signs of prediabetes#symptoms of prediabetes#symptoms of prediabetes in females#what is prediabetes
0 notes
Text
ICD 10 Codes For Mental Health: A Quick Reference Guide

Mental health professionals and medical billing specialists need accurate ICD 10 codes to ensure proper documentation and reimbursement. This guide covers the essential codes for common mental health conditions, billing requirements, and best practices for 2025 compliance standards.
Mental health services have become increasingly vital in healthcare delivery. Proper coding ensures providers receive appropriate compensation while maintaining compliance with insurance requirements.
Essential ICD 10 Codes For Mental Health Conditions
Mental health diagnosis coding requires precision and attention to detail. The International Classification of Diseases, 10th Revision (ICD-10) provides standardized codes that healthcare providers must use for accurate documentation.
Major depressive disorder remains one of the most frequently coded conditions. The primary code F32.9 covers unspecified major depressive disorder, while F33.1 addresses recurrent major depressive disorder, moderate severity.
Anxiety disorders follow closely behind in frequency. Generalized anxiety disorder uses code F41.1, while panic disorder without agoraphobia is coded as F41.0. These distinctions matter significantly for treatment planning and reimbursement.
Common Mental Health Diagnostic Categories
Mood disorders encompass a broad range of conditions that affect emotional regulation. Bipolar disorder type I uses code F31.10 for manic episodes without psychotic features, while F31.30 covers depressive episodes.
Trauma-related conditions require specific coding attention. Post-traumatic stress disorder (PTSD) is coded as F43.10, while acute stress reaction uses F43.0. These codes help track treatment outcomes and resource allocation.
Substance use disorders present unique coding challenges. Alcohol use disorder severity levels range from mild (F10.10) to severe (F10.20), with specific codes for withdrawal and intoxication states.
Best Practices for Mental Health Coding
Accurate documentation supports proper code selection and reduces claim denials. Clinical notes should clearly indicate symptom severity, duration, and functional impact on the patient's daily life.
Regular training updates keep coding staff current with annual ICD-10 revisions. Mental health codes often receive updates that affect reimbursement rates and documentation requirements.
Quality assurance reviews help identify coding patterns that may trigger audits. Consistent application of coding guidelines protects practices from compliance issues while optimizing revenue streams.
Technology Solutions for Mental Health Billing
Electronic health records (EHR) systems increasingly incorporate coding assistance features. These tools help reduce errors while improving documentation quality and billing accuracy.
Automated coding suggestions can streamline workflow efficiency. However, human oversight remains essential for complex cases that require clinical judgment and interpretation.
Integration between clinical documentation and billing systems reduces transcription errors. This connection ensures that diagnostic information flows seamlessly from patient encounters to claims processing.
Modern practices benefit from specialized support services that handle Medical Claims Billing complexities. Professional billing companies understand the nuances of mental health coding and can help optimize revenue cycles.
Compliance and Regulatory Considerations
Medicare and Medicaid programs maintain specific requirements for mental health service documentation. Providers must demonstrate medical necessity through detailed clinical notes that support chosen diagnostic codes.
Privacy regulations add complexity to mental health billing processes. HIPAA compliance requires careful handling of sensitive psychiatric information throughout the billing cycle.
Regular audits help identify potential compliance gaps before they become problematic. Proactive reviews of coding practices can prevent costly penalties and claim denials.
Frequently Asked Questions
What happens if I use the wrong ICD-10 code for a mental health diagnosis? Incorrect codes can lead to claim denials, delays in payment, and potential audit triggers. Always verify codes match the documented clinical presentation and severity level.
How often do ICD-10 mental health codes change? The ICD-10 system receives annual updates each October. Mental health codes may be added, deleted, or modified based on clinical research and healthcare industry feedback.
Can I use unspecified codes for mental health conditions? Unspecified codes should be used sparingly and only when clinical documentation lacks sufficient detail for a more specific code. Detailed documentation supports better coding choices.
What documentation is required to support mental health ICD-10 codes? Clinical notes must include symptom presentation, severity assessment, functional impact, and treatment response. This documentation justifies the selected diagnostic code and treatment plan.
How do I stay current with mental health coding changes? Subscribe to official ICD-10 updates, attend continuing education programs, and consider working with professional billing services that specialize in mental health coding requirements.
Final Note
Accurate ICD 10 Codes For Mental Health services require ongoing attention to detail and regulatory compliance. Healthcare providers who invest in proper coding practices protect their revenue while ensuring patients receive appropriate care documentation. Consider partnering with experienced billing professionals at MCB Collects to optimize your mental health coding processes and improve your practice's financial performance through their specialized revenue cycle management services.
#ICD 10 codes#mental health billing#medical coding#healthcare documentation#psychiatric diagnosis codes#mental health claims#mental health services
0 notes
Text
https://trilogyqualityassurance.com/blog/the-ultimate-guide-to-home-health-coding-icd10-services-in-2025/
#home health coding 2025#ICD-10 updates#medical coding services#home care billing#ICD-10 for home health#coding compliance#CMS coding changes
0 notes
Text
Medical Coding Services in California | Error-Free Coding

At Bristol Healthcare, we offer a comprehensive suite of medical coding services designed to support healthcare providers in every aspect of their revenue cycle management process. Our team of certified coders possesses extensive expertise across 40+ medical specialties, ensuring that our medical coding services are both precise and compliant with industry standards.
#medical coding services#icd-10 coding#cpt-4 coding#hcpcs coding#hcc coding#clinical documentation#medicare rac audits and appeals
0 notes
Text

Causes of Medical Claim Denials & How to Prevent Them?
Medical claim denials impact revenue and delay reimbursements. Common causes include coding errors, missing documentation, eligibility issues, and lack of medical necessity. Prevent denials with accurate coding, thorough documentation, eligibility verification, and proactive audits. Strengthen denial management to optimize revenue cycle efficiency and reduce financial losses. https://alpineprohealth.com/blog/causes-of-medical-claim-denials-how-to-prevent-them/
0 notes
Text
ICD-10 codes play a vital role in revenue cycle management, ensuring accurate billing, fewer denials, and higher reimbursements. With its vast range of detailed diagnosis and procedure classifications, ICD-10 enhances coding precision but also introduces challenges like compliance and ongoing training. Is your practice making the most of ICD-10 to improve financial performance?
Read detailed blog @ https://bit.ly/4hafhsF To maximize the benefits of ICD-10, healthcare providers should:
Invest in continuous coder training
Leverage AI-driven coding technology
Conduct regular internal audits
Stay updated on payer policies and regulations
By implementing these best practices, your practice can reduce claim denials, enhance compliance, and optimize revenue cycles. The future of medical billing is evolving—make sure your RCM strategy is built for success.
Contact Info Hub Consultancy Services for expert medical billing and coding solutions. Visit: www.infohubconsultancy.com Email: [email protected]
#ICD-10 codes play a vital role in revenue cycle management#ensuring accurate billing#fewer denials#and higher reimbursements. With its vast range of detailed diagnosis and procedure classifications#ICD-10 enhances coding precision but also introduces challenges like compliance and ongoing training. Is your practice making the most of I#Read detailed blog @ https://bit.ly/4hafhsF#To maximize the benefits of ICD-10#healthcare providers should:#•#Invest in continuous coder training#Leverage AI-driven coding technology#Conduct regular internal audits#Stay updated on payer policies and regulations#By implementing these best practices#your practice can reduce claim denials#enhance compliance#and optimize revenue cycles. The future of medical billing is evolving—make sure your RCM strategy is built for success.#Contact Info Hub Consultancy Services for expert medical billing and coding solutions.#Visit: www.infohubconsultancy.com#Email: [email protected]
0 notes
Text

this has happened enough times that there is a diagnostic code for it.
The code is V01.131D if you're curious.
1 note
·
View note
Text
The need for correct coding for urinary tract infections (UTIs) is paramount for accurate diagnosis and payment. Dominantly focusing on UTI ICD-10 codes, this guide enables healthcare entities to smooth the billing process, reduce claim denial, and uphold coding guideline compliance.
0 notes
Text
CPT Code 80053 Billing Guide: Accurate CMP Panel Reimbursement with CPT Coding Services

One of the most frequently used codes in laboratory testing is CPT Code 80053, which represents the Comprehensive Metabolic Panel (CMP). This panel provides essential information about a patient’s metabolic state and organ function, helping physicians diagnose and manage chronic diseases effectively. For healthcare providers and billing professionals, understanding how to accurately bill for this panel is vital to avoid claim denials and ensure proper revenue cycle management.
In this guide, we’ll break down CPT Code 80053, its components, billing requirements, and how a trusted medical coding company offering CPT coding services can help streamline the process for healthcare providers. This ultimately serves as a complete CPT coding solution for your practice.
What is CPT Code 80053?
CPT 80053 refers to the Comprehensive Metabolic Panel, a routine blood test that measures 14 different substances in the blood. These measurements help assess a patient’s kidney and liver function, electrolyte and acid/base balance, and blood glucose levels.
Components of the 80053 CMP Panel Include:
Glucose
Calcium
Sodium
Potassium
Chloride
Carbon Dioxide (Bicarbonate)
Blood Urea Nitrogen (BUN)
Creatinine
Albumin
Total Protein
ALP (Alkaline Phosphatase)
ALT (Alanine Aminotransferase)
AST (Aspartate Aminotransferase)
Bilirubin, Total
Each of these individual tests can be billed separately, but when ordered together and medically necessary, they are billed under a single panel using 80053, simplifying the billing process and reflecting appropriate bundling as per CPT guidelines.
Billing Guidelines for CPT 80053
Correct billing of CPT 80053 requires that all 14 component tests be performed on the same date and ordered together. Failing to meet this requirement can result in a denied claim or reduced reimbursement.
Key Billing Considerations:
Medical Necessity: Documentation must support the medical necessity of all the panel components.
Bundled Services: The test is reimbursed as a single unit. Individual billing of panel components without justification may lead to duplicate billing flags.
Frequency Limitations: Many insurance carriers have frequency guidelines for how often a CMP panel can be reimbursed. Check payer policies to avoid denials.
Modifiers: If not all components of the panel are performed, modifiers may be needed to unbundle and bill separately (if permitted by the payer).
Diagnosis Coding: Ensure correct ICD-10-CM diagnosis codes that justify the medical necessity for the test.
A reputable medical billing services provider will be well-versed in these rules and help ensure accurate claim submission.
Common Denial Reasons for CPT Code 80053
Despite being a routine panel, CPT 80053 can be subject to billing errors, resulting in denied claims. Understanding these pitfalls is crucial for compliance and timely reimbursement.
Top Reasons for Denials:
Incomplete Panel Components: If all 14 components are not performed, billing 80053 is not appropriate.
Lack of Medical Necessity: Missing or inadequate documentation can result in denial due to insufficient justification.
Frequency Issues: Billing for CMP more frequently than allowed by the payer.
Incorrect Diagnosis Code Linkage: Diagnosis codes that don’t support medical necessity for each test.
Bundling Errors: Attempting to bill panel components separately without appropriate justification or modifiers.
Partnering with an experienced medical coding company can help mitigate these issues by ensuring every claim is coded accurately and compliantly. This forms a critical part of a robust CPT coding solution.
The Role of a Medical Coding Company in CMP Billing
Medical coding is more than just assigning codes; it’s about accuracy, compliance, and maximizing reimbursement. A professional medical coding company plays a pivotal role in improving coding accuracy for CPT 80053 and other panels by offering comprehensive CPT coding services:
Ensuring Proper Code Selection: Coders are trained to follow CPT and payer guidelines to code tests appropriately.
ICD-10 Mapping: Coders match appropriate diagnosis codes to lab tests to support medical necessity.
Documentation Review: Coders review physician orders and lab results to ensure all components are performed and documented.
Compliance Audits: Regular internal audits help reduce the risk of overcoding, undercoding, and payer scrutiny.
Whether you’re a small clinic or a large hospital system, CPT coding outsourcing to a medical coding company helps reduce administrative burdens and enhance revenue integrity.
Benefits of Outsourcing CMP Panel Billing
Accurate billing of panels like 80053 requires attention to detail, ongoing training, and familiarity with payer-specific guidelines. Many providers choose to outsource their medical billing services for increased accuracy and efficiency. Opting for CPT coding outsourcing provides numerous advantages:
Advantages Include:
Faster Reimbursements
Reduced Denials and Rework
Regulatory Compliance
Better Resource Allocation
Revenue Cycle Optimization
CPT coding outsourcing also gives providers access to technology-driven platforms, coding automation, and skilled professionals who stay current with CMS updates and CPT changes.
Stay Updated on CPT Changes
Every year, CPT codes and payer guidelines are subject to revisions. Inaccurate billing due to outdated knowledge can severely impact reimbursements.
To stay compliant:
Review annual CPT and HCPCS code updates
Subscribe to CMS and payer newsletters
Conduct quarterly coding audits
Partner with a reliable medical billing services company that monitors these changes for you. This is an essential aspect of a complete CPT coding solution.
Conclusion
The 80053 CPT Code for the Comprehensive Metabolic Panel (CMP) is a crucial part of routine lab testing, but it comes with specific coding and billing requirements. Missteps in documentation, code selection, or frequency guidelines can result in revenue loss and compliance risks.
One of the most frequently used codes in laboratory testing is CPT Code 80053, which represents the Comprehensive Metabolic Panel (CMP). This panel provides essential information about a patient’s metabolic state and organ function, helping physicians diagnose and manage chronic diseases effectively. For healthcare providers and billing professionals, understanding how to accurately bill for this panel is vital to avoid claim denials and ensure proper revenue cycle management.
In this guide, we’ll break down CPT Code 80053, its components, billing requirements, and how a trusted medical coding company offering CPT coding services can help streamline the process for healthcare providers. This ultimately serves as a complete CPT coding solution for your practice.
What is CPT Code 80053?
CPT 80053 refers to the Comprehensive Metabolic Panel, a routine blood test that measures 14 different substances in the blood. These measurements help assess a patient’s kidney and liver function, electrolyte and acid/base balance, and blood glucose levels.
Components of the 80053 CMP Panel Include:
Glucose
Calcium
Sodium
Potassium
Chloride
Carbon Dioxide (Bicarbonate)
Blood Urea Nitrogen (BUN)
Creatinine
Albumin
Total Protein
ALP (Alkaline Phosphatase)
ALT (Alanine Aminotransferase)
AST (Aspartate Aminotransferase)
Bilirubin, Total
Each of these individual tests can be billed separately, but when ordered together and medically necessary, they are billed under a single panel using 80053, simplifying the billing process and reflecting appropriate bundling as per CPT guidelines.
Billing Guidelines for CPT 80053
Correct billing of CPT 80053 requires that all 14 component tests be performed on the same date and ordered together. Failing to meet this requirement can result in a denied claim or reduced reimbursement.
Key Billing Considerations:
Medical Necessity: Documentation must support the medical necessity of all the panel components.
Bundled Services: The test is reimbursed as a single unit. Individual billing of panel components without justification may lead to duplicate billing flags.
Frequency Limitations: Many insurance carriers have frequency guidelines for how often a CMP panel can be reimbursed. Check payer policies to avoid denials.
Modifiers: If not all components of the panel are performed, modifiers may be needed to unbundle and bill separately (if permitted by the payer).
Diagnosis Coding: Ensure correct ICD-10-CM diagnosis codes that justify the medical necessity for the test.
A reputable medical billing services provider will be well-versed in these rules and help ensure accurate claim submission.
Common Denial Reasons for CPT Code 80053
Despite being a routine panel, CPT 80053 can be subject to billing errors, resulting in denied claims. Understanding these pitfalls is crucial for compliance and timely reimbursement.
Top Reasons for Denials:
Incomplete Panel Components: If all 14 components are not performed, billing 80053 is not appropriate.
Lack of Medical Necessity: Missing or inadequate documentation can result in denial due to insufficient justification.
Frequency Issues: Billing for CMP more frequently than allowed by the payer.
Incorrect Diagnosis Code Linkage: Diagnosis codes that don’t support medical necessity for each test.
Bundling Errors: Attempting to bill panel components separately without appropriate justification or modifiers.
Partnering with an experienced medical coding company can help mitigate these issues by ensuring every claim is coded accurately and compliantly. This forms a critical part of a robust CPT coding solution.
The Role of a Medical Coding Company in CMP Billing
Medical coding is more than just assigning codes; it’s about accuracy, compliance, and maximizing reimbursement. A professional medical coding company plays a pivotal role in improving coding accuracy for CPT 80053 and other panels by offering comprehensive CPT coding services:
Ensuring Proper Code Selection: Coders are trained to follow CPT and payer guidelines to code tests appropriately.
ICD-10 Mapping: Coders match appropriate diagnosis codes to lab tests to support medical necessity.
Documentation Review: Coders review physician orders and lab results to ensure all components are performed and documented.
Compliance Audits: Regular internal audits help reduce the risk of overcoding, undercoding, and payer scrutiny.
Whether you’re a small clinic or a large hospital system, CPT coding outsourcing to a medical coding company helps reduce administrative burdens and enhance revenue integrity.
Benefits of Outsourcing CMP Panel Billing
Accurate billing of panels like 80053 requires attention to detail, ongoing training, and familiarity with payer-specific guidelines. Many providers choose to outsource their medical billing services for increased accuracy and efficiency. Opting for CPT coding outsourcing provides numerous advantages:
Advantages Include:
Faster Reimbursements
Reduced Denials and Rework
Regulatory Compliance
Better Resource Allocation
Revenue Cycle Optimization
CPT coding outsourcing also gives providers access to technology-driven platforms, coding automation, and skilled professionals who stay current with CMS updates and CPT changes.
Stay Updated on CPT Changes
Every year, CPT codes and payer guidelines are subject to revisions. Inaccurate billing due to outdated knowledge can severely impact reimbursements.
To stay compliant:
Review annual CPT and HCPCS code updates
Subscribe to CMS and payer newsletters
Conduct quarterly coding audits
Partner with a reliable medical billing services company that monitors these changes for you. This is an essential aspect of a complete CPT coding solution.
Conclusion
The 80053 CPT Code for the Comprehensive Metabolic Panel (CMP) is a crucial part of routine lab testing, but it comes with specific coding and billing requirements. Missteps in documentation, code selection, or frequency guidelines can result in revenue loss and compliance risks.
Collaborating with a professional medical coding company ensures that your CMP billing is accurate, compliant, and optimized for maximum reimbursement. By leveraging the expertise of specialized CPT coding services through CPT coding outsourcing, healthcare providers can focus on delivering quality care while safeguarding their financial health.
Read more: https://www.allzonems.com/80053-cpt-code-cmp-panel-billing-guide/
Need Expert Help with CMP Billing?
Allzone Management Services is a trusted medical coding company offering end-to-end medical billing services tailored to your specialty. From lab coding to revenue cycle optimization, we ensure clean claims, fewer denials, and faster payments. We offer a comprehensive CPT coding solution to meet your needs.
📞 Call us today: 8668542714 📧 Email: [email protected] 🌐 Visit: www.allzonems.com
Let us take care of your coding and billing, so you can focus on patient care.
#medical billing outsourcing companies#healthcare medical billing management solutions#revenue cycle management services#outsource medical billing services#healthcare rcm companies#medical billing solutions#80053 CPT Code#claim denials CMP#CMP billing errors#CMP panel coding#compliance in lab billing#CPT 80053 documentation#ICD-10 coding for CMP#lab panel billing guidelines#Medical Billing Services#Medical coding company#Metabolic Panel billing#Outsourcing Medical Billing#panel component verification#Revenue Cycle Optimization
0 notes
Text
Why Are More Teenagers Getting Prediabetes?
The Silent Epidemic: Understanding the Rising Rates of Prediabetes in American Teenagers Continue reading Why Are More Teenagers Getting Prediabetes?
#7-day meal plan for prediabetes#can prediabetes be reversed#diet for prediabetes#how to reverse prediabetes#how to reverse prediabetes in 3 months#icd 10 code for prediabetes#icd 10 prediabetes#prediabetes#prediabetes a1c#prediabetes a1c range#prediabetes diet#prediabetes icd 10#prediabetes medication#prediabetes range#prediabetes symptoms#prediabetes treatments#signs of prediabetes#symptoms of prediabetes#symptoms of prediabetes in females#what is prediabetes
0 notes
Text
Enroll in IGMPI’s Medical Coding Certification Course to gain industry-recognized training. Learn ICD-10, CPT, HCPCS coding, and compliance for a rewarding healthcare career.

#Medical Coding Course#Medical Coding Certification#ICD-10 Training#CPT Coding#HCPCS Training#Medical Billing and Coding#IGMPI Medical Coding#Healthcare Coding Course
0 notes