#neurology billing and coding services
Explore tagged Tumblr posts
Text
Demystifying the Maze: A Guide to Neurology Billing and Coding Services
The intricate world of neurology, with its specialized procedures, complex diagnoses, and evolving coding landscape, can leave billing and coding feeling like a tangled web. But fear not, fellow neurologists! This guide illuminates the path to accurate and efficient neura-billing, empowering you to navigate the maze with confidence.
Understanding the Nuances of Neurology Billing:
Neurology billing differs from general US medical billing in several key ways:
Highly specialized procedures: Electromyography (EMG), electroencephalography (EEG), and nerve blocks require specific codes and modifiers.
Dynamic coding changes: CPT and HCPCS updates necessitate continuous vigilance to avoid compliance issues.
Interpretation and reporting challenges: Translating complex neurological diagnoses into accurate codes requires expertise.
Medicare Part B complexities: Understanding Medicare Part B coverage and billing requirements is crucial for neurology practices.
Essential Resources for Neuro-Billing Success:
Equipping yourself with the right resources is key to mastering this intricate domain:
1. Professional Organizations:
American Academy of Neurology (AAN): Provides access to coding manuals, webinars, and conferences specifically tailored for neurology billing.
American Academy of Professional Coders (AAPC): Offers industry-leading coding education, certifications, and online coding forums, invaluable for staying up-to-date.
Medical Group Management Association (MGMA): Delivers practice management resources, including neurology-specific billing guides and compliance checklists.
2. Technology Solutions:
Neurology-specific billing software: Invest in software designed for neurology practices, featuring pre-populated codes, automated claim scrubbing, and compliance alerts.
Electronic health records (EHRs): EHRs with integrated neurology modules can streamline coding, documentation, and reporting, minimizing errors and denials.
Revenue cycle management (RCM) services: Consider partnering with an RCM provider specializing in neurology billing. They handle the entire billing process, freeing you to focus on patient care.
3. Educational Resources:
Neurology coding manuals and references: Invest in updated coding manuals and online resources specifically designed for neurology, like the AAN Coding Primer and the AMA CPT Assistant.
Coding webinars and conferences: Attend online or in-person coding workshops and conferences tailored to neurology to gain practical knowledge and network with other neuro-billing professionals.
Online coding communities and forums: Join online forums and communities dedicated to neurology coding to ask questions, share experiences, and stay updated on the latest coding trends.
Building a Strong Foundation for Neuro-Billing:
Beyond resources, building a robust neuro-billing foundation requires several key steps:
Invest in staff training: Train your billing team on neurology-specific coding, documentation, and compliance requirements.
Develop clear internal policies and procedures: Establish standardized processes for coding, claim submission, and error resolution.
Implement regular audits and compliance checks: Proactively identify and address any billing errors or compliance issues.
Maintain open communication with payers: Communicate clearly and promptly with insurance companies to resolve billing discrepancies and prevent denials.
Remember, mastering neurology billing is an ongoing journey. By actively seeking resources, investing in staff development, and implementing robust internal processes, you can transform this complex challenge into a well-oiled revenue engine for your practice.
Bonus Tips:
Utilize modifier expertise: Understand and apply appropriate modifiers to accurately reflect the complexity of neurological procedures.
Master medical necessity documentation: Clearly document medical necessity to justify procedures and maximize reimbursement.
Stay informed about payer policies: Regularly review insurance company policies and billing guidelines specific to neurology billing services.
Final Thoughts:
While navigating neurology billing can be complex, with the right resources, dedicated effort, and a focus on compliance, you can conquer this challenge and ensure your practice thrives. Remember, accurate billing translates to optimal reimbursement, satisfied patients, and a secure future for your neurology practice. So, arm yourself with knowledge, leverage technology, and build a strong foundation to navigate the labyrinth of neuro-billing with confidence.
0 notes
Text
Struggling with the complexities of Neurology Medical Billing? Info Hub Consultancy Services is your trusted offshore partner for accurate, efficient, and compliant billing solutions. From coding to claims submission—we handle it all, so you can focus on patient care. Maximize reimbursements and reduce denials with our expert team. 📞 Call us at 1-888-694-8634 or +91 82974 56441 to discuss your needs! Info Hub – Your One-Stop RCM Solution.
#Neurology Medical Billing Services India#Offshore Medical Billing Company#Offshore Neurology Medical Billing Services India#Outsource Medical Billing Services#Medical Billing Services Agency#Best Medical Billing Agency#Offshore Medical Billing and coding#Offshore Medical Billing Services India#Offshore Medical Billing Agency India#Best Offshore Medical Billing Company India#Offshore Medical Billing Company In India#Outsource Medical Billing Services Agency India#1 Outsource Medical Billing Services Company India#Best Medical Billing Services Agency India#Top Medical Billing Services Agency India#Offshore Medical Billing and Coding#Offshore Medical Billing and Coding Services#Offshore Medical Billing and Coding Agency
0 notes
Text
The Role of Modifiers in Pain Management Coding

Accurate medical coding is crucial for ensuring correct reimbursement, minimizing denials, and maintaining compliance in healthcare billing. Pain management, in particular, involves a wide range of procedures, from injections and nerve blocks to radiofrequency ablations and implantable pain devices. Modifiers help distinguish between unilateral and bilateral procedures, indicate repeat or staged interventions, and specify provider roles, ultimately ensuring that services are reported accurately. Without proper modifier application, claims can be denied, payments delayed, or reimbursements reduced, leading to financial and operational challenges for healthcare providers. This blog explores the importance of modifiers in pain management coding, their impact on claims processing, and best practices to enhance billing efficiency.
What Are Modifiers in Medical Coding?
Modifiers are two-character alphanumeric or numeric codes appended to CPT (Current Procedural Terminology) and HCPCS (Healthcare Common Procedure Coding System) codes. They provide additional information about a procedure or service, such as location, provider involvement, or special circumstances, without altering the core meaning of the code. Modifiers serve as an essential tool to ensure proper claim adjudication by payers and help in accurately describing complex medical services.
Why Are Modifiers Important in Pain Management?
Modifiers are essential in pain management billing company because they provide critical details that ensure accurate claim processing, appropriate reimbursement, and compliance with payer guidelines. Pain management at 5 Star Billing Services procedures often involve a variety of services that require precise differentiation, such as whether a treatment was performed on one side of the body or both (unilateral vs. bilateral), if a procedure was staged or repeated, or if multiple procedures were performed during the same session. Without the correct modifiers, claims may be denied, underpaid, or misinterpreted, leading to financial losses and administrative burdens for healthcare providers.
Best Practices for Using Modifiers in Pain Management
To effectively utilize modifiers in pain management coding, follow these best practices:
Ensure Medical Necessity: Proper documentation should support the use of modifiers. Each claim must include clear and complete medical records justifying the procedure and its necessity.
Stay Updated on Payer-Specific Guidelines: Different insurance carriers may have unique modifier policies. Regularly reviewing payer requirements can prevent claim denials and ensure correct oncology billing services.
Use Modifiers Correctly to Avoid Claim Denials: Improper usage can result in rejections or audits. Understanding the distinction between modifiers (e.g., when to use Modifier 59 versus Modifier 51) is crucial for coding accuracy. Visit 5 Star Billing Services today.
Avoid Overuse or Misuse: Ensure that modifiers are applied only when truly necessary to describe a distinct circumstance. Misuse of modifiers can trigger audits, delay payments, and result in penalties.
Final Thoughts
Modifiers in pain management coding help clarify medical services, ensure proper reimbursement, and minimize claim denials. Understanding how to apply these modifiers correctly can enhance billing efficiency and compliance. Pain management providers and billing professionals should stay informed about evolving coding practices to optimize their revenue cycle and maintain regulatory compliance. As coding regulations evolve, keeping up with the latest guidelines will help pain management practices streamline their neurology billing services and maximize reimbursements.
#pain management coding#pain management billing company#oncology billing services#neurology billing services
0 notes
Text

Neurology Billing Services – Boost Revenue, Reduce Hassles
Enhance your neurology practice with expert billing solutions. We manage claims, denials, and reimbursements, ensuring faster payments and compliance. Focus on patient care while we handle your revenue cycle.
0 notes
Text
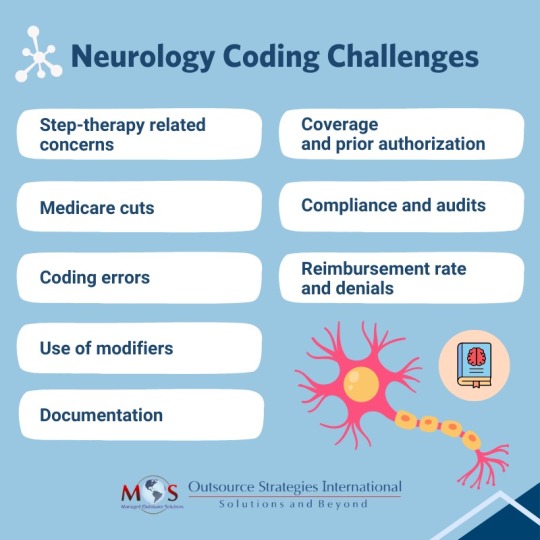
Neurology Coding Challenges
Providers in neurology often encounter obstacles like claim denials, payment delays, insurance coverage disputes, and regulatory compliance issues. To navigate these challenges effectively, leveraging specialized neurology medical coding services is essential.
0 notes
Text
Struggling with complex billing and collections? Let Instapay Healthcare Services take the headache out of your neurology billing! 💼 We specialize in maximizing revenue and streamlining your billing process, so you can focus on what truly matters—caring for your patients.
✅ Expert Neurology Billing Solutions
✅ Reduced Claim Denials
✅ End-to-End Revenue Cycle Management
Partner with us today and see the difference! Your practice’s profitability is just a click away. 💡
Fax:- 9179607960
📞: +1(646) 851-2115
#Neurology Billing Services#Neurology Billing Services in US#outsourced Neurology Billing Services#neurology billing company#neurology medical billing Services#Neurology Billing specialist#neurology billing codes#neurology coding and billing#neurology medical coding
0 notes
Text
#Neurology Billing Services#Neurology Billing Services in US#outsourced Neurology Billing Services#neurology billing company#neurology medical billing Services#Neurology Billing specialist#neurology billing codes#neurology coding and billing#neurology medical coding
0 notes
Text

Seeking professional and reliable medical billing services tailored specifically for neurology practices? Look no further! Our experienced team specializes in accurately managing neurology billing tasks, ensuring timely submissions, maximizing reimbursements, and minimizing claim denials.
With a deep understanding of neurology coding and regulations, we streamline your billing processes, allowing you to focus on providing exceptional patient care.
Contact us today to optimize your revenue cycle and enhance practice efficiency: https://shorturl.at/bjBI6
#medical billing services#medical coding services#rcm#revenue cycle management#medical billing company#rcm services#neurology medical billing
0 notes
Text
-$500 in the bank and suddenly att thinks repeatedly shutting off my internet this month for "non payment" is ok. Doesn't matter I have a confirmation code for my payment. Doesn't matter that my bill isn't due until the 7th. Doesn't matter that it's clearly an error. Thry won't turn it back on until I find $65. To pay them.
The 3rd their guy in billing said I should just pull from the savings I don't have. Or borrow money! That they can refund me later! That's normal!
He literally said turning it back on would be unfair. Refunding the service disconnection charge would be UNFAIR. Even though I have all the proof that this is an error on their part.
I'm so tired.
I can't even afford the gas to go to my neurology appointment next week. Let alone this shit.
And I have been calling them non stop for two weeks due to the billing issues!! But apparently that wasn't good enough! Paying them on the 1st isn't good enough!
I'm so tired. This is just too much as everything else goes to shit around me
5 notes
·
View notes
Text

Neurology Billing and Coding: A Step-by-Step Guide
Navigate neurology billing and coding effortlessly with our step-by-step guide. Ensure accuracy and compliance in your practice's financial processes.
#neurology billing and coding services#us medical billing#medical billing services#medical billing services florida#medical billing services usa#medical coding company florida#medical coding company usa
0 notes
Text
Medical Service Provider: A Complete Overview
In today’s fast-evolving healthcare industry, the term medical service provider has gained immense importance. These providers form the backbone of the healthcare system by delivering essential medical services — from clinical care and diagnostics to administrative support and medical billing.
What is a Medical Service Provider?
A medical service provider refers to any individual or organization that offers medical-related services to patients or healthcare institutions. These services can be clinical (like treatment or diagnosis) or non-clinical (like billing, coding, or telemedicine support).
Common examples include:
Hospitals & clinics
Physicians & specialists
Diagnostic labs & imaging centers
Medical billing & RCM companies
Telehealth platforms
Home healthcare providers
Types of Medical Services Offered
Clinical Services
General consultation
Emergency care
Surgical procedures
Specialized treatments (cardiology, neurology, etc.)
Diagnostic Services
Blood tests
X-rays, MRIs, and CT scans
Pathology and genetic testing
Support Services
Medical billing and coding
Health information management
Revenue cycle management (RCM)
Insurance verification and claims handling
Digital Healthcare Services
Telemedicine consultations
Remote patient monitoring
e-Prescriptions and digital health records
Why Medical Service Providers Are Important
Medical service providers play a critical role in:
Ensuring Timely Care: Quick and reliable services help improve patient outcomes.
Improving Healthcare Access: Through telemedicine and mobile clinics, services reach remote areas.
Streamlining Operations: Backend services like billing and RCM allow doctors to focus on patient care.
Maintaining Compliance: Trained providers ensure adherence to healthcare laws and data privacy (e.g., HIPAA).
Qualities of a Good Medical Service Provider
A top-tier provider should offer:
Skilled professionals and specialists
Transparent and secure systems
Reliable service delivery with timely support
Scalable solutions for clinics or hospitals
Data security and HIPAA compliance
Virtual Oplossing – Your Trusted Medical Service Provider
At Virtual Oplossing, we specialize in offering advanced medical support services including medical billing, coding, revenue cycle management, and digital health solutions. With a focus on accuracy, efficiency, and compliance, we help healthcare providers deliver better care while improving their financial outcomes.
Our Key Services:
Medical Billing & Coding
RCM Solutions
Telehealth Support
Data Management & Reporting
Conclusion
A reliable medical service provider helps bridge the gap between patient care and healthcare operations. Whether clinical or administrative, choosing the right partner can enhance efficiency, compliance, and patient satisfaction. As the industry continues to evolve, providers like Virtual Oplossing are leading the way in modern, tech-enabled healthcare support.
0 notes
Text
Discover the impact of telehealth on neurology billing. Stay compliant and profitable with actionable tips for revenue cycle management.
Contact number:- 888-357-3226 Email ID:[email protected] https://shorturl.at/udjBK
#denial management#medical billers and coders#medical billing company#medical billing services#medical coding services#rcm#rcm services#revenue cycle management#healthcare billing service#neurology billing services
0 notes
Text
Enhancing Profit Cycle Operation in Anesthesiology & Neurology Medical Billing
In today's healthcare landscape, optimizing profit cycle operations (RCM) is pivotal for the financial health of medical practices. For specialties like anesthesiology and neurology, accurate medical billing plays a crucial role in ensuring providers are compensated for the services they provide. The complexity of billing for these specialties requires an in-depth understanding of medical coding, insurance claims processing, and compliance with regulatory standards.
1. What is Profit Cycle Operation (RCM)?
Profit Cycle Operation refers to the process of managing and overseeing the financial transactions in a healthcare facility, from the moment a patient schedules an appointment to the final payment for the services rendered. It involves several crucial factors, including:
Case Enrollment : Collecting patient details for billing purposes.
Rendering : Translating medical procedures and judgments into standardized codes.
Claims Submission : Transmitting claims to insurance companies for payment.
Payment Posting : Recording payments received from both patients and insurance providers.
Denial Management : Handling any claim denials and resolving issues for resubmission.
Collections : Following up on overdue bills and securing payments.
For anesthesiology and neurology practices, effective RCM ensures that these processes are handled efficiently to maximize profit, minimize errors, and maintain compliance with healthcare regulations such as the Health Insurance Portability and Accountability Act (HIPAA) and the Affordable Care Act (ACA).
2. The Importance of Medical Billing Services in Anesthesiology and Neurology
Anesthesiology and neurology are complex fields, each with its own set of challenges in terms of billing. Understanding these specialties' nuances can significantly improve RCM processes.
Anesthesiology Medical Billing Services
Anesthesiology is often viewed as a critical support service in surgery and other medical procedures. Medical billing for anesthesiology involves specific codes for different anesthesia types, duration, and levels of service provided during a procedure. The unique aspects of anesthesiology medical billing services include:
Complex Anesthesia Codes : Anesthesia billing includes distinct codes for various types of anesthesia (general, regional, monitored anesthesia care, etc.) and for different durations.
Time-Based Billing : Anesthesia billing often involves time-based billing, meaning the duration of the anesthesia service must be recorded accurately.
Modifiers : Anesthesia billing often requires the use of modifiers, which are essential for providing additional details about the procedure.
Multiple Providers : In many cases, multiple anesthesiologists or certified registered nurse anesthetists (CRNAs) may be involved in patient care, complicating the billing process.
Payer Requirements : Different insurance companies have varying guidelines for anesthesiology billing. Staying up to date with these requirements is essential to ensure claims are processed and paid promptly.
Neurology Medical Billing Services
Neurology, which focuses on the nervous system, involves various services, from diagnoses to complex surgeries and interventions. Neurology medical billing services includes the following factors:
Diagnostic Tests and Procedures : Neurologists often order tests like MRIs, CT scans, EEGs, and lumbar punctures, each with its own set of billing codes.
Chronic Condition Management : Many neurological conditions, such as epilepsy, Parkinson's disease, and multiple sclerosis, require long-term management. Billing for ongoing care and medication prescriptions must be accurate and transparent to avoid errors.
Surgical Procedures : Neurological surgeries, such as spinal surgeries or brain tumor removals, require detailed billing codes.
Complex Diagnoses : Neurological conditions often have multiple underlying causes, and these diagnoses must be correctly reflected in the medical codes to avoid errors in payment.
Insurance Variability : Different insurance companies have varying guidelines and payment rates for neurology services, making it essential for neurologists to be aware of each payer's specifics.
3. Challenges in Anesthesiology and Neurology Medical Billing
While medical billing is integral to the success of any practice, anesthesiology and neurology face unique challenges that can hinder profitable cycle operations. Some of these challenges include:
3.1 Rendering Errors and Inaccuracies
The most common challenge in medical billing for anesthesiology and neurology is the risk of coding errors. Anesthesia and neurology services involve highly specific codes for procedures, diagnoses, and patient conditions. Any mistake in code selection can lead to claim denials or delayed payments.
3.2 Claim Denials and Rejections
Claims for both anesthesiology and neurology services are prone to rejection or denial due to various reasons, such as incorrect or incomplete information, improper coding, or failure to meet payer guidelines.
3.3 Complex Billing for Multiple Providers
Billing for multiple providers involved in a single patient's care is a challenge in both anesthesiology and neurology. For example, in anesthesiology, both the attending anesthesiologist and the CRNA may need to be reimbursed for their services. Similarly, a neurologist may collaborate with other specialists, such as neurosurgeons, physical therapists, or psychologists, complicating the billing process.
3.4 Inconsistent Payer Conditions
Payer conditions can vary greatly between insurance companies, leading to discrepancies that result in delayed payments or errors. For example, some insurance companies may have different rules for timing and documentation of anesthesia services.
3.5 Compliance and Regulatory Changes
Healthcare regulations and compliance standards are constantly evolving. New coding systems, payer guidelines, and government regulations (such as the Affordable Care Act and HIPAA) can cause confusion for medical billers and providers.
4. How Anesthesiology and Neurology Medical Billing Services Improve RCM
Specialized billing services tailored to anesthesiology and neurology practices can significantly enhance RCM by addressing the unique challenges faced by providers. Here's how professional medical billing services can improve profit cycle operations:
4.1 Expertise in Specialty-Specific Billing Codes
Anesthesiology and neurology medical billing services are provided by professionals who are experts in the complexities of coding for these specialties. This expertise reduces errors and ensures that claims are accurately coded, leading to faster claim approval and fewer rejections.
4.2 Timely Claim Submission
By using automated billing systems and trained billers, medical billing services ensure that claims are submitted promptly. Timely submission is crucial for maintaining a healthy profit cycle, as delayed claims can lead to late payments and unnecessary administrative work.
4.3 Denial Management and Resolution
Denials are an inevitable part of medical billing, but how they are handled can significantly affect a practice's profit. Specialized billing services are skilled in denial management and can quickly identify and resolve issues, whether it's a coding error, missing documentation, or an insurance policy discrepancy.
4.4 Ongoing Compliance Monitoring
Medical billing services dedicated to anesthesiology and neurology practices stay up to date with the latest regulatory changes and payer conditions. This ongoing compliance monitoring ensures that billing practices are always in line with current laws, reducing the risk of audits, penalties, or incorrect reimbursements.
4.5 Custom Reporting and Analytics
Effective RCM requires detailed insights into financial performance. Specialized billing services provide customized reports and analytics that allow practice managers to monitor cash flow, track outstanding claims, and identify areas for improvement.
4.6 Reduced Administrative Burden
Outsourcing anesthesiology medical billing services allows anesthesiology and neurology practices to focus on patient care while experts handle the billing process. This reduces the administrative burden on healthcare providers, allowing them to streamline operations, cut costs, and improve productivity.
5. Conclusion
Anesthesiology and neurology medical billing services are essential for enhancing profit cycle operations in these specialized fields. By addressing the unique challenges of these specialties, medical billing services help improve cash flow, minimize errors, and ensure timely reimbursements. Practices can maximize their financial performance by working with billing professionals who are well-versed in the complexities of anesthesiology and neurology billing codes, payer conditions, and regulatory compliance.
To truly benefit from enhanced profit cycle operations, practices should invest in medical billing services that understand their needs and can tailor solutions to meet the complexities of anesthesiology and neurology. With the right approach, medical billing can transform the financial health of these practices, allowing them to thrive in an increasingly complex healthcare environment.
0 notes
Text
Understanding Neurology Billing and Coding Challenges

Neurology billing is filled with intricate codes, time-based services, and diagnostic nuances that make accurate billing a complex task. Learn how to overcome these challenges to minimize claim denials and improve revenue flow.
#Neurology billing#Neurology medical billing#medical billing services#dme billing services#medical billing
0 notes
Text
https://handyclassified.com/neurology-billing-made-easy-increase-your-earnings-today
#Neurology Billing Services#Neurology Billing Services in US#outsourced Neurology Billing Services#Neurology revenue cycle management#neurology billing company#neurology medical billing Services#Neurology Billing specialist#neurology billing codes#neurology coding and billing#neurology medical coding
0 notes
Text
Breaking Down the $100K Revenue Boost with Ankr: How Telehealth Billing Transforms Your Bottom Line
In today's fast-paced healthcare environment, patient care doesn’t stop at the clinic door. Between phone calls, portal messages, and after-hours requests, providers often deliver high-value care that generates zero revenue. That’s where Ankr steps in — transforming those unreimbursed interactions into billable virtual visits with just one click.
If you're a practice looking to improve profitability without adding more staff or clinic hours, this guide will help you understand how Ankr helps unlock $100,000+ in new revenue per provider annually, using smart telehealth workflows and AI-driven automation.
The $100K Problem in Plain Numbers
Every provider knows the feeling: You're reviewing labs, refilling meds, answering a worried parent, or discussing symptoms over the phone — all in the name of patient care — but none of that time is billable.
Now imagine:
3 reimbursable virtual visits per day
$100 average reimbursement per visit
5 working days per week × 48 weeks per year
That's $72,000 - $100,000+ in revenue sitting on the table — and Ankr helps you capture it all with minimal effort.
How Ankr Makes It Happen
Ankr isn’t just another telehealth app. It’s a Virtual Clinic Experience (VCX) that replicates your in-office workflow in the cloud — seamlessly and intelligently.
Here’s how Ankr helps you bill for work you’re already doing:
✅ 1. Convert Messages to Billable Visits
Ankr turns unscheduled phone calls, portal messages, and inbox communications into fully billable telehealth visits. Patients are guided through a structured intake, and you're looped in when ready.
✅ 2. AI-Powered Documentation
Ankr’s ambient AI scribe automatically generates documentation for each virtual visit — so you don’t have to. It captures patient interactions, SOAP notes, and billing codes for rapid chart completion.
✅ 3. Works with Your EHR
Ankr integrates directly with popular EHRs like Epic®, Athena®, eClinicalWorks®, and more. That means no extra logins, no manual data entry, and no disruption to your existing workflows.
✅ 4. One-Click Billing
After each virtual visit, Ankr makes it easy to push charges to your billing system — ensuring providers get reimbursed accurately and promptly.
Why It Works for All Specialties
Ankr is already being used by providers in:
Primary Care (Internal Medicine, Family Practice)
Cardiology, Oncology, Gastroenterology
Orthopedics, Rheumatology, Neurology
Ob/Gyn, Urology, Nephrology, and more
Because the workflow is specialty-agnostic, Ankr helps all clinicians get paid for the care they’re already delivering — virtually or otherwise.
Real Impact for Real Practices
Here’s what practices are reporting with Ankr:
$100,000+ in new annual revenue per provider
8% reduction in wait times for new patient visits
Over 90% patient satisfaction with the virtual care experience
No need to hire more front-desk staff or scribes
Ankr Fits Right Into Your Workflow
Whether you're a solo practitioner or part of a multi-specialty group, Ankr is designed to plug into your phone tree, answering service, and EHR. It automates what your staff already does, but faster and more accurately.
From verifying insurance to scheduling appointments and connecting patients with interpreters — Ankr handles it all, so you can focus on care.
Recurring Revenue, Low Cost of Entry
Unlike traditional telehealth platforms that charge per seat or come with complex tech stacks, Ankr is:
Easy to adopt
Low cost to get started
Built to scale with your clinic
The result? Recurring monthly revenue from care that would’ve otherwise gone uncompensated.
Why Ankr is Differentnt
There are dozens of telehealth tools out there, but none that combine:
AI documentation
Telehealth visit conversion
EHR integration
Scheduling + intake automation
Ankr is the only VCX platform that replicates the entire in-office workflow, virtually and intelligently.
Ready to Capture Your $100K?
Your practice is already delivering care that deserves to be reimbursed. With Ankr, you can finally get paid for the work you do — without adding extra burden on your staff.
Talk to our team to see how much revenue Ankr can help you unlock.
0 notes