Don't wanna be here? Send us removal request.
Text
Understanding Agonal Rhythm: A Critical Cardiac Emergency
Agonal rhythm is a severe and life-threatening cardiac arrhythmia often seen in the final moments of life. This abnormal heart rhythm is characterized by extremely slow and irregular electrical activity, typically resulting in inadequate blood circulation to vital organs. It frequently occurs when the heart is nearing complete failure, such as during cardiac arrest or severe hypoxia. Agonal rhythm is often considered a sign of impending death and can be recognized by its distinctive, slow, wide, and erratic QRS complexes on an electrocardiogram (ECG).
Immediate medical intervention is crucial when agonal rhythm is detected, as it signifies the heart's inability to sustain normal function. Cardiopulmonary resuscitation (CPR), defibrillation, and advanced cardiac life support (ACLS) protocols are often initiated to restore a more effective heart rhythm. However, the prognosis for patients with agonal rhythm is generally poor, as it usually occurs in conjunction with critical underlying conditions, such as severe heart disease, trauma, or terminal illness. Despite aggressive treatment efforts, survival rates are low, and the primary goal may shift toward comfort care in certain cases. Recognizing agonal rhythm early is key to making informed decisions about treatment and care.

0 notes
Text
Left Anterior Fascicular Block: Causes, Diagnosis & Treatment
Left Anterior Fascicular Block (LAFB) occurs when the electrical conduction in the heart's left anterior fascicle is delayed or blocked, leading to a distinctive pattern on an ECG. It is often associated with conditions like coronary artery disease, hypertension, left ventricular hypertrophy, and heart valve disorders. Age-related degeneration of the heart's conduction system, past heart attacks, or myocarditis can also cause LAFB. In some cases, it may arise without any obvious underlying condition. Diagnosis is usually made through an electrocardiogram (ECG), which reveals specific changes in the electrical activity of the heart. Treatment focuses on addressing the underlying causes, such as controlling hypertension or managing coronary artery disease. Often, LAFB itself may not need direct intervention unless it is linked to other cardiac complications, but regular monitoring and managing risk factors are key to its long-term management.

0 notes
Text
Gym Cardio: Unlocking the Benefits for Heart Health
Engaging in regular cardio exercises at the gym can significantly enhance heart health. Cardio, short for cardiovascular exercise, is any activity that raises your heart rate and keeps it elevated over a sustained period. This includes running on a treadmill, cycling, or using an elliptical machine. By incorporating these activities into your fitness routine, you strengthen the heart, improve circulation, and increase the efficiency of oxygen delivery to muscles.
One of the key benefits of cardio is its ability to lower blood pressure, reduce cholesterol levels, and decrease the risk of heart disease. Regular aerobic exercise also helps maintain a healthy weight, reducing strain on the heart. Additionally, cardio workouts can improve your endurance, making daily tasks easier to perform and boosting your overall energy levels.
For optimal results, it’s recommended to perform moderate-intensity cardio for at least 150 minutes a week. This can be broken down into sessions that fit your schedule, making it easy to stay consistent. Not only does cardio benefit your heart, but it also improves mental well-being by reducing stress and promoting better sleep. Ultimately, gym cardio is a powerful tool in promoting long-term heart health and overall well-being.

0 notes
Text
Fetal Tachycardia: symptoms, causes, treatment
Fetal tachycardia refers to an abnormally high heart rate in an unborn baby, typically above 160-180 beats per minute. This condition can be detected during routine prenatal check-ups using ultrasound or fetal heart monitoring. Symptoms may not be directly noticeable by the mother, but signs such as rapid or irregular fetal movements can raise concern.
The causes of fetal tachycardia are varied and can include maternal factors like infections, fever, or dehydration, as well as fetal issues like anemia or structural heart problems. Certain medications or substances consumed by the mother, such as caffeine or nicotine, may also contribute to an increased fetal heart rate.
Treatment for fetal tachycardia depends on its underlying cause. In some cases, addressing maternal health concerns, such as reducing a fever or treating an infection, can stabilize the baby's heart rate. If the tachycardia is linked to a fetal heart condition, more specialized interventions may be necessary, such as medication to regulate the baby's heartbeat. In severe cases, early delivery might be considered if the condition poses significant risks to the baby’s health. Regular monitoring is key in managing fetal tachycardia effectively.

0 notes
Text
Fruits Good for the Heart: A Tasty Guide to Heart Health
Incorporating fruits into your diet is a simple and delicious way to support heart health. Many fruits are packed with essential nutrients like fiber, antioxidants, and vitamins that promote a healthy cardiovascular system.
Berries, such as strawberries, blueberries, and raspberries, are especially beneficial due to their high levels of antioxidants and fiber, which help lower cholesterol and blood pressure. Citrus fruits, like oranges and grapefruits, are rich in vitamin C and flavonoids, known for improving blood vessel function and reducing inflammation. Apples and pears are loaded with soluble fiber, which aids in reducing bad cholesterol levels. Bananas, a great source of potassium, help maintain healthy blood pressure by balancing the effects of sodium.
Additionally, fruits like avocados, rich in heart-healthy fats, and grapes, packed with antioxidants, contribute to overall heart wellness. Pomegranates, with their polyphenols, are known to improve heart function and reduce arterial plaque buildup.
By regularly consuming a variety of fruits, you can nourish your heart, reduce the risk of heart disease, and enjoy a flavorful, nutritious diet. Your heart will thank you for making these tasty choices a part of your daily routine!

0 notes
Text
10 Benefits of intermittent fasting for heart health
Intermittent fasting has gained popularity for its potential heart health benefits. First, it can help reduce blood pressure by lowering insulin levels and allowing blood vessels to relax. Second, it aids in weight loss and helps reduce excess body fat, a key factor in maintaining cardiovascular health. Third, fasting promotes improved cholesterol levels by increasing HDL (good cholesterol) and reducing LDL (bad cholesterol) and triglycerides. Fourth, it can help control blood sugar, reducing the risk of diabetes—a major risk factor for heart disease.
Fifth, intermittent fasting reduces inflammation, a critical factor in heart disease development. Sixth, it improves heart function by enhancing mitochondrial efficiency and cellular repair processes, helping heart cells work more effectively. Seventh, fasting can reduce oxidative stress, a contributor to cardiovascular aging and damage. Eighth, it promotes better heart rhythm and reduces the risk of arrhythmias.
Ninth, fasting helps regulate appetite hormones, which can prevent overeating and promote weight control. Lastly, intermittent fasting may help improve overall longevity and reduce the risk of age-related cardiovascular issues by enhancing metabolic health and reducing harmful markers associated with heart disease. These benefits make it a promising approach to maintaining heart health.

0 notes
Text
The Importance of Oxygenated Blood: A Vital Life Force
Oxygenated blood plays a crucial role in sustaining life, acting as a vital force that fuels every cell in the body. When we inhale, oxygen enters our lungs and binds to hemoglobin in red blood cells. This oxygen-rich blood is then circulated throughout the body, delivering oxygen to tissues and organs, enabling them to function properly. Oxygen is essential for cellular respiration, the process by which cells produce energy to carry out various biological activities. Without adequate oxygen, cells would be unable to generate the energy required for survival, leading to dysfunction or even cell death.
The importance of oxygenated blood extends beyond just energy production. It also helps in maintaining healthy brain function, muscle activity, and overall well-being. Proper oxygenation supports immune system function, aiding in the body's defense against infections and diseases. Furthermore, it assists in wound healing and tissue repair by promoting cell regeneration.
In conditions like hypoxia, where oxygen levels are insufficient, the body's organs can suffer damage, leading to serious health complications. Therefore, maintaining optimal levels of oxygenated blood is essential for overall health, making it a critical component of life itself.

0 notes
Text
How to Keep Heart Healthy: A Comprehensive Guide for Every Age
Taking care of your heart is essential at every stage of life. Regardless of age, adopting heart-healthy habits can significantly reduce the risk of cardiovascular diseases. A balanced diet, rich in fruits, vegetables, whole grains, and lean proteins, is a cornerstone of heart health. Limiting processed foods, added sugars, and unhealthy fats is equally important.
Regular physical activity, such as walking, cycling, or swimming, strengthens the heart and improves circulation. Aiming for at least 30 minutes of moderate exercise daily can make a big difference. Managing stress is also key, as chronic stress can raise blood pressure and strain the heart. Mindfulness practices, like meditation and yoga, can help in relaxation.
Avoiding smoking and limiting alcohol intake are critical in reducing heart disease risk. Regular health check-ups, including monitoring blood pressure, cholesterol levels, and blood sugar, allow early detection of potential issues. Staying informed and proactive about your heart health ensures a long, active, and fulfilling life. By making these choices part of your routine, you can protect your heart and enjoy overall well-being at any age.

0 notes
Text
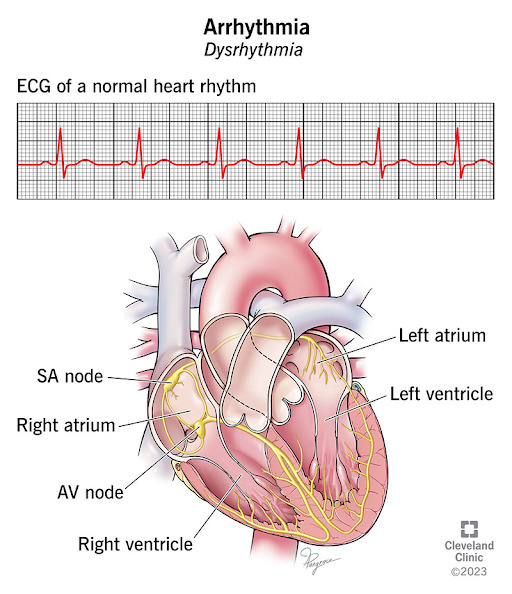
Understanding the Pathophysiology of Cardiac Arrhythmia
Cardiac arrhythmia refers to abnormal heart rhythms that arise from irregularities in the heart's electrical system. This disruption in the heart’s electrical impulses can lead to various arrhythmias, each with distinct causes and effects. The heart's rhythm is regulated by electrical signals that ensure a coordinated contraction of heart muscles. When these signals become erratic or are delayed, it results in arrhythmias such as atrial fibrillation, ventricular tachycardia, or bradycardia.
The pathophysiology of arrhythmias often involves changes in the heart’s electrical pathways or cells, which may be due to underlying heart disease, genetic factors, or external triggers like stress or certain medications. For instance, in atrial fibrillation, the electrical signals in the atria become chaotic, leading to irregular and often rapid heartbeats. Similarly, ventricular tachycardia involves rapid electrical signals in the ventricles, which can impair the heart’s ability to pump blood effectively.
Understanding the pathophysiology of cardiac arrhythmias is crucial for diagnosing and managing these conditions. Treatment strategies may include medications, lifestyle changes, or procedures like catheter ablation to restore normal heart rhythm and reduce the risk of complications such as stroke or heart failure.
0 notes
Text
What is the Difference between Tachycardia and Bradycardia?
Oxygenated blood is essential for sustaining life, acting as the primary carrier of oxygen throughout the body. It plays a crucial role in maintaining the health and function of every organ and tissue. The heart pumps oxygen-rich blood, absorbed through the lungs, to cells, ensuring that they receive the energy needed to perform vital processes. Without a steady supply of oxygenated blood, cells would be deprived of oxygen, leading to impaired function, and in severe cases, cell death.
The importance of oxygenated blood extends to every part of the body, including the brain, which requires a constant flow of oxygen to function properly. A lack of oxygen can lead to cognitive decline, dizziness, and even brain damage. Similarly, muscles rely on oxygen to produce energy, enabling movement and strength. Oxygenated blood also plays a role in healing, as it promotes tissue repair and helps fight infections by delivering essential nutrients and immune cells to affected areas.
In essence, oxygenated blood serves as a life force, fueling the body’s systems, promoting overall well-being, and ensuring survival. Its continuous flow is indispensable to maintaining health and preventing serious medical conditions.

0 notes
Text
Understanding the Significance of Ventricular Trigeminy in Heart Health
Ventricular trigeminy is a heart rhythm disorder where every third heartbeat is a premature ventricular contraction (PVC). These abnormal beats originate from the ventricles, the heart's lower chambers, and can disrupt the regular rhythm. While occasional PVCs are often harmless, frequent occurrences like ventricular trigeminy can signal underlying heart issues and should not be ignored.
The significance of ventricular trigeminy lies in its potential connection to heart disease. It may be linked to conditions such as cardiomyopathy, coronary artery disease, or electrolyte imbalances. If left untreated, it could lead to more severe arrhythmias or complications like heart failure. Individuals with ventricular trigeminy might experience symptoms like palpitations, dizziness, or shortness of breath, but in some cases, it can be asymptomatic and discovered only through an ECG or other heart monitoring tests.
Early detection and proper management are crucial. Treatment may involve lifestyle changes, medications, or more advanced procedures, depending on the severity and cause of the trigeminy. Understanding and addressing ventricular trigeminy can help prevent further heart complications and improve overall heart health, making regular check-ups essential for those at risk.

0 notes
Text
Understanding Bad Food for Heart Health: What to Avoid
To maintain a healthy heart, it's crucial to be mindful of foods that can negatively impact heart health. Certain foods can increase the risk of heart disease, and avoiding them is key to preserving cardiovascular health. High-fat and processed meats, such as bacon, sausages, and hot dogs, are loaded with saturated fats that can raise cholesterol levels. Similarly, fried foods like French fries, doughnuts, and fried chicken contain unhealthy trans fats, which can clog arteries and lead to heart complications.
Sugary drinks and snacks, including soda, candies, and pastries, contribute to obesity, high blood pressure, and diabetes, all of which are risk factors for heart disease. Additionally, foods high in sodium, such as canned soups, salty snacks, and processed meals, can elevate blood pressure, putting extra strain on the heart.
Limiting the intake of refined carbohydrates, like white bread and pasta, is also important, as they can cause blood sugar spikes and increase the likelihood of heart-related issues. Instead, opting for a diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats can help protect heart health and reduce the risk of cardiovascular diseases.

0 notes
Text
Difference Between Pulmonary and Systemic Circulation: Understanding the Body’s Vital Blood Circuits
The human circulatory system consists of two crucial circuits: pulmonary and systemic circulation. These pathways work together to ensure oxygenated blood reaches the body and deoxygenated blood returns to the lungs for reoxygenation.
Pulmonary circulation focuses on the exchange of gases. Deoxygenated blood from the body is transported to the right side of the heart, which then pumps it to the lungs via the pulmonary arteries. In the lungs, carbon dioxide is exchanged for oxygen, and the now oxygen-rich blood returns to the left side of the heart through the pulmonary veins.
Systemic circulation, on the other hand, distributes this oxygenated blood throughout the body. The left side of the heart pumps oxygen-laden blood into the aorta, which branches into various arteries delivering it to tissues and organs. As cells utilize oxygen and produce carbon dioxide, the deoxygenated blood is returned to the right side of the heart via veins, completing the circuit.
Together, pulmonary and systemic circulations create a continuous loop that ensures vital oxygen delivery and waste removal, maintaining homeostasis and supporting life’s essential processes.

0 notes
Text
Heart Palpitations are frequent? Know when to seek help
Heart palpitations, the feeling of your heart racing, pounding, or fluttering, are often harmless and usually triggered by everyday factors such as stress, caffeine, dehydration, or physical exertion. These sensations, although alarming, are typically not a cause for concern when they occur infrequently. Common triggers include emotional stress or anxiety, excessive intake of caffeine or alcohol, smoking, or engaging in intense exercise. Hormonal changes, particularly during pregnancy, menstruation, or menopause, can also lead to palpitations. Certain medications, such as asthma inhalers, decongestants, or drugs used to treat arrhythmias, may contribute to this condition. However, if heart palpitations become frequent or persistent, it could be a sign of an underlying medical issue that requires attention. Conditions like hyperthyroidism, low blood sugar (hypoglycemia), anemia, or electrolyte imbalances can all cause palpitations. It's essential to be aware of these triggers and know when to seek medical advice. If palpitations are accompanied by dizziness, shortness of breath, chest pain, or fainting, it’s crucial to consult a healthcare provider, as these symptoms could indicate a more serious heart condition, such as an arrhythmia or other cardiovascular issues.

0 notes
Text
Understanding the Difference Between Arteries and Veins
Arteries and veins are two types of blood vessels that play crucial roles in the circulatory system, but they function quite differently. Arteries are responsible for carrying oxygen-rich blood away from the heart to the body’s tissues. They have thick, elastic walls to withstand the high pressure exerted as blood is pumped out of the heart. Their elasticity helps maintain blood pressure during the intervals between heartbeats.
In contrast, veins carry deoxygenated blood back to the heart from the body. Since the blood pressure in veins is much lower than in arteries, their walls are thinner and less elastic. To assist blood flow against gravity, especially in the legs, veins are equipped with valves that prevent backflow and keep blood moving towards the heart.
Additionally, arteries are generally located deeper in the body to protect them from injury, while veins are often closer to the skin's surface. The color difference in the blood they carry is due to oxygen levels: arterial blood is bright red because it’s oxygenated, whereas venous blood is darker as it lacks oxygen. Together, arteries and veins form a complementary system that ensures proper circulation throughout the body.

0 notes
Text
Understanding Monophasic Defibrillators: A Comprehensive Guide
Monophasic defibrillators are life-saving medical devices used to treat cardiac arrhythmias, particularly ventricular fibrillation and pulseless ventricular tachycardia. These devices deliver a single, high-energy electrical shock through the heart, aiming to reset the heart's rhythm. In a monophasic defibrillator, the current travels in one direction, from one electrode pad to another, across the heart. This unidirectional current flow is different from biphasic defibrillators, which send the current in two phases, first in one direction and then in the opposite.
While monophasic defibrillators were the standard for decades, they have largely been replaced by biphasic devices in modern medical practice. Biphasic defibrillators are considered more efficient, as they require less energy to achieve the same effect, reducing potential heart muscle damage and increasing the success rate of resuscitation. However, monophasic defibrillators are still used in certain settings due to their simplicity and lower cost.
Understanding the function and role of monophasic defibrillators is important for healthcare professionals, particularly those working in emergency and critical care, as these devices remain a crucial tool in cardiac resuscitation, especially in resource-limited environments.

0 notes
Text
Defibrillator Pad Placement: A Comprehensive Guide
Defibrillator pad placement is critical to the effectiveness of defibrillation and ensuring the best chance of survival during cardiac arrest. Proper pad positioning allows the electrical current to pass through the heart, restoring normal rhythm. Typically, the two recommended positions are anterolateral and anteroposterior.
In the anterolateral position, one pad is placed on the right upper chest, just below the collarbone, while the other is placed on the left side of the chest, below the armpit. This configuration allows the current to pass through the heart in the shortest, most direct route.
The anteroposterior position involves placing one pad on the center of the chest, just below the left breast, and the other pad on the back, between the shoulder blades. This method is often used when front placement is challenging or when there are special considerations, such as pacemakers or implanted devices.
It's crucial to follow the defibrillator manufacturer's instructions for proper pad placement. Pads should always be applied to clean, dry skin and positioned as indicated on the pads themselves. Correct placement can significantly improve the chances of a successful shock and patient recovery.

0 notes