Don't wanna be here? Send us removal request.
Text

Stomach Cancer: How To Diagnose?
If you have symptoms that may suggest stomach cancer, your doctor will determine if they are caused by cancer or another condition. If a stomach tumour is suspected, various diagnostic tools will be used to confirm the diagnosis, locate the cancer, and assess its spread. These tests include:
Upper Endoscopy (Gastroscopy): This common method for detecting stomach cancer uses a thin tube with a camera (endoscope) inserted through the mouth to view the stomach lining and collect tissue samples if needed.
Endoscopic Ultrasound (EUS): This specialised form of endoscopy features an ultrasound probe at the tip of the endoscope. It helps assess the depth of tumour invasion and whether cancer has spread from the stomach lining into the stomach wall or nearby lymph nodes. It’s instrumental in staging the cancer.
CT Scan (Computed Tomography): Provides detailed cross-sectional images of the abdomen and pelvis to detect tumours or enlarged lymph nodes.
0 notes
Text
The Global Initiative of Asthma (GINA) celebrated the first World Asthma Day in 1988 during a meeting in Barcelona, Spain. Subsequently, every year, World Asthma Day is observed on the first Tuesday of May to raise awareness about asthma, improve the quality of care, and highlight its impact on millions of lives.
0 notes
Text

What is Black Coffee?
Black coffee is a simple coffee made without milk, sugar, or cream. Known for its strong and bold taste, it’s a very popular drink for people seeking a quick energy boost due to its high caffeine content. Black coffee also allows the pure, natural flavours of the coffee beans to come through, providing a rich coffee experience without any added sweetness or creaminess.
The advantages of black coffee go beyond taste. It’s low in calories, packed with antioxidants, and can boost metabolism, which helps in weight management. Black coffee may also support heart health, enhance mood, and improve focus, making it a healthy choice for coffee lovers.
0 notes
Text

Loss of Consciousness
Sudden and unexplained loss of consciousness is a hallmark symptom of SCA. The individual may collapse without any apparent reason, often catching bystanders off guard.
No Normal Pulse or Breathing
Check for signs of life by assessing the pulse and breathing. In the case of SCA, there will be an absence of both. It is crucial to act swiftly, as the lack of pulse indicates the heart's failure to pump blood effectively.
Chest Pain or Discomfort
While not always present, some individuals may experience chest pain or discomfort before the onset of SCA. This can be mistaken for a heart attack, emphasizing the importance of recognising the subtle differences between the two.
Abnormal Heart Rhythms
SCA is often triggered by irregular heart rhythms, known as arrhythmias. Ventricular fibrillation (VF) and ventricular tachycardia (VT) are common arrhythmias associated with SCA. If someone experiences palpitations or a rapid, irregular heartbeat, it could be a precursor to SCA.
Shortness of Breath
A sudden, severe shortness of breath may precede or accompany SCA. The heart's inability to pump blood effectively results in inadequate oxygen supply to the body, leading to respiratory distress.
Fatigue and Weakness
Individuals at risk of SCA may experience extreme fatigue and weakness, even during routine activities. This could be a manifestation of the compromised blood flow and oxygen delivery to the body's tissues.
Dizziness or Light-headedness
SCA may cause a sudden and profound drop in blood pressure, leading to dizziness or light-headedness. This can be a warning sign that the cardiovascular system is under duress.
Nausea and Vomiting
Some individuals may experience nausea or vomiting before or during SCA. This can be attributed to the overall stress on the body as a result of inadequate blood circulation.
0 notes
Text
When do you need a Total Hip Replacement?
Total hip replacement is often called the “operation of the century” due to its profound impact on patients’ lives. This surgical procedure can significantly improve the quality of life for individuals suffering from severe hip pain, arthritis, or injury. This blog aims to educate potential patients on when to consider this surgery, the conditions it treats, and what to expect from the procedure. We’ll also touch on the importance of consulting with an orthopaedic specialist to ensure the best care.
Synopsis
Understanding Total Hip Replacement
When to Get Hip Replacement?
Severe Hip Arthritis Management
Non-Surgical Options
Total hip replacement
The Hip Replacement Procedure- what to expect
Benefits of Hip Replacement
Conclusion
Understanding Total Hip Replacement
Total hip replacement involves removing the damaged hip joint and replacing it with an artificial one. This procedure is typically recommended for patients who experience severe hip pain that interferes with daily activities, such as walking, bending, or even resting. The goal is to relieve pain, improve joint function, and enhance the patient’s overall quality of life.
When to Get Hip Replacement?
Deciding when to get a hip replacement is a critical decision that should be made in consultation with an orthopaedic surgeon. Here are some key indicators that you might need a hip replacement:
Severe Hip Pain: Persistent pain that does not respond to conservative treatments like medications, physical therapy, or lifestyle changes.
Limited Mobility: Difficulty in performing everyday activities such as walking, climbing stairs, or getting in and out of car, difficulty in putting on socks and shoes.
Hip Stiffness: Stiffness in the hip joint that limits your range of motion and affects your ability to move freely.
Arthritis: Severe hip arthritis, including osteoarthritis, rheumatoid arthritis, or post-traumatic arthritis, which causes significant joint damage and pain.
Hip Injury: Fractures, dislocation or other injuries that damage the hip joint and lead to chronic pain and disability.
Severe Hip Arthritis Management
Arthritis is one of the most common reasons for hip replacement surgery. Severe hip arthritis treatment often begins with non-surgical options, but when these fail to provide relief, hip replacement becomes a viable option.
Non-Surgical Options
Analgesics: These are pain-relieving medications that help manage the discomfort associated with hip arthritis. Common analgesics include acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and naproxen. These medications can reduce pain and inflammation, making daily activities more manageable.
Physiotherapy: Physical therapy plays a crucial role in managing hip arthritis. A physiotherapist can design a personalized exercise program to strengthen the muscles around the hip, improve flexibility, and enhance joint function. Regular physiotherapy sessions can help reduce pain and improve mobility.
Intra-Articular Injections: These injections involve delivering medication directly into the hip joint. Corticosteroid injections are commonly used to reduce inflammation and provide pain relief. In some cases, hyaluronic acid injections may be used to lubricate the joint and improve movement.
When non-surgical treatments are no longer effective, hip replacement surgery may be considered. This procedure involves replacing the damaged hip joint with an artificial one, which can significantly improve quality of life by reducing pain and restoring mobility.
Total hip replacement
If you’re having symptoms related to your hip joint then you may require a hip replacement, it’s crucial to consult with an orthopaedic surgeon trained in joint replacement surgery. Orthopaedic hip surgery is known for its high standards, with surgeons who are experienced in the latest techniques and technologies.
The Hip Replacement Procedure- what to expect
Understanding what to expect from the hip replacement procedure can help alleviate some of the anxiety associated with surgery. Here is a brief overview of the process:
Pre-Surgery Evaluation: Your surgeon will conduct a thorough evaluation, including medical history, physical examination, and imaging tests like X-rays or MRIs.
Surgery: The procedure typically takes a couple of hours. The damaged hip joint is removed and replaced with a prosthetic implant made of metal, ceramic, or plastic.
Recovery: Post-surgery, you’ll spend a few days in the hospital. Physical therapy will begin almost immediately to help you regain mobility and strength.
Rehabilitation: Full recovery can take a few months. Adhering to your rehabilitation plan is crucial for a successful outcome.
Benefits of Hip Replacement
The benefits of hip replacement surgery are numerous and significantly improve your quality of life. These include:
Pain Relief: One of the most immediate benefits is the reduction or elimination of hip pain.
Improved Mobility: Enhanced ability to perform daily activities without discomfort.
Better Quality of Life: Increased independence and ability to engage in activities you enjoy.
Long-Lasting Results: Modern hip implants are designed to last many years, providing long-term relief.
Conclusion
Total hip replacement is a highly effective treatment for severe hip pain, arthritis, and injuries that affect daily activities. If you’re experiencing significant hip pain and other treatments haven’t worked, it may be time to consider hip replacement surgery. Consulting with an orthopaedic specialist can help you make an informed decision and ensure you receive the best possible care.
Contact Manipal Hospitals Ghaziabad for immediate support and care.
0 notes
Text
Hernia Repair Surgery: Fixing a Common Problem
Hernias are a common medical condition that can affect people of all ages. They occur when an organ or tissue pushes through a weak spot in the muscle or surrounding tissue wall, leading to discomfort and potential complications. Hernia repair surgery is a crucial procedure that helps alleviate symptoms and prevent serious health issues. This blog aims to provide a comprehensive overview of hernia repair surgery, including its types, procedures, and recovery process.
Synopsis
What is a Hernia?
Types of Hernia Repair Surgery
The Surgical Procedure
Recovery and Aftercare - Hernia Surgery
Success Rates and Long-term Outcomes
Conclusion
What is a Hernia?
A hernia is a condition where an internal body part, such as an organ or fatty tissue, protrudes through a weak spot in the muscle or surrounding tissue wall. This can happen in various parts of the body, leading to different types of hernias:
Inguinal Hernia: Occurs in the groin area and is more common in men.
Femoral Hernia: Appears in the upper thigh, just below the groin, and is more common in women.
Umbilical Hernia: Occurs near the belly button and is common in infants and pregnant women.
Hiatal Hernia: Happens when part of the stomach pushes up into the chest through the diaphragm.
Symptoms of hernias can include a visible lump and pain or discomfort, especially when bending, coughing, or lifting heavy things. If not treated, hernias can cause serious problems like strangulation, where the blood flow to the affected area is blocked, leading to severe pain and needing emergency surgery.
Here's a table summarizing why hernia repair surgery is necessary
Reason Description
Strangulation
When the blood supply to the herniated tissue is cut off, leading to tissue death and severe complications.
Obstruction
When the hernia blocks the passage of contents through the intestines, causing pain and digestive issues.
Chronic Pain
Persistent discomfort can interfere with daily activities and reduce quality of life.
Symptom Relief
Surgery can alleviate symptoms, providing relief from pain and discomfort.
Prevention of Complications
Surgery helps prevent serious complications like strangulation and obstruction.
Improved Quality of Life
Patients can enjoy a better quality of life post-surgery, free from the limitations caused by hernias.
Types of Hernia Repair Surgery
There are several types of hernia surgeries, each with its advantages and considerations:
1. Open Hernia Repair
Description: This traditional method involves making a larger incision over the hernia site.
Procedure: The surgeon pushes the protruding tissue back into place and repairs the muscle wall with stitches or a synthetic mesh to strengthen the area.
Pros and Cons: Open hernia repair is effective for large or complex hernias but involves a longer recovery time and more noticeable scarring compared to minimally invasive techniques.
2. Laparoscopic Hernia Repair
Description: A minimally invasive technique that uses small incisions and a laparoscope (a thin tube with a camera).
Procedure: The surgeon performs the repair using specialized instruments inserted through the small incisions, guided by the laparoscope's images.
Pros and Cons: This method offers a shorter recovery time, less postoperative pain, and smaller scars. However, it may not be suitable for all types of hernias, especially very large ones.
3. Robotic Hernia Repair
Description: An advanced form of laparoscopic hernia repair surgery that uses robotic arms controlled by the surgeon.
Procedure: The robotic system provides greater precision and flexibility, allowing for more complex repairs.
Pros and Cons: Robotic hernia repair shares the benefits of laparoscopic surgery, such as reduced pain and quicker recovery, with the added advantage of enhanced precision. However, it is more expensive and may not be available in all medical facilities
The Surgical Procedure
Before the surgery, patients undergo a thorough medical evaluation to ensure they are fit for the procedure. They are usually advised to fast for several hours before the operation. The surgery itself involves several steps:
Anesthesia: Patients are given general anaesthesia to ensure they are asleep and pain-free during the procedure.
Incision: Depending on the type of surgery, the surgeon makes either a large incision (open repair) or several small incisions (laparoscopic or robotic repair).
Repair: The protruding tissue is pushed back into place, and the muscle wall is repaired with stitches or mesh.
Closure: The incisions are closed with sutures, staples, or surgical glue.
The duration of the surgery varies but typically lasts between one to two hours. After the surgery, patients are monitored in the recovery room until the effects of anaesthesia wear off.
Recovery and Aftercare - Hernia Surgery
Recovery from hernia repair surgery depends on the type of surgery performed and the patient's overall health. Here is a typical recovery timeline:
Immediate Postoperative Period: Patients may experience some pain and discomfort, which can be managed with pain medication. They are usually encouraged to start walking soon after the surgery to promote circulation and prevent blood clots.
First Week: Most patients can return home the same day or the day after surgery. They should avoid strenuous activities and heavy lifting but can engage in light activities.
First Month: Gradual return to normal activities is encouraged, but patients should follow their surgeon's advice regarding activity restrictions.
Full Recovery: Complete recovery can take several weeks to a few months, depending on the type of surgery and individual healing rates.
Postoperative care tips include keeping the surgical site clean and dry, following a healthy diet to promote healing, and attending follow-up appointments to monitor recovery. Potential complications, such as infection, recurrence of the hernia, or chronic pain, should be promptly addressed with medical attention.
Success Rates and Long-term Outcomes
Hernia repair surgeries generally have high success rates, with most patients experiencing significant relief from symptoms and a low risk of recurrence. The success rates can vary depending on the type of surgery and the patient's overall health. Long-term benefits of hernia repair surgery include:
Reduced Risk of Recurrence: Proper repair techniques and the use of mesh can significantly lower the chances of the hernia returning.
Improved Functionality: Patients can return to their normal activities without the limitations caused by hernia symptoms.
Enhanced Quality of Life: Relief from pain and discomfort leads to better overall well-being.
Including patient testimonials or case studies can provide real-life examples of successful outcomes and inspire confidence in those considering the surgery.
Preventive Measure
Description
Maintain a Healthy Weight
Keeping a healthy weight reduces the strain on abdominal muscles, lowering the risk of hernias.
Proper Lifting Techniques
Use your legs, not your back, to lift heavy objects to avoid putting excessive pressure on the abdomen.
Strengthen Core Muscles
Engage in exercises that strengthen the core muscles, providing better support to the abdominal area.
Smoking Cessation
Quitting smoking improves overall health and reduces coughing, which can contribute to hernias.
Diet Improvements
Eat a balanced diet rich in fibre to prevent constipation, which can strain abdominal muscles.
Conclusion
Hernia repair surgery is a crucial procedure for addressing the discomfort and potential complications associated with hernias. Whether you need inguinal hernia repair surgery, umbilical hernia repair, or laparoscopic hernia surgery, Manipal Hospitals offers the expertise and advanced technology to ensure a successful outcome. Trust us to provide the best care and make your health our top priority.
If you are looking for hernia repair surgery, Manipal Hospital Ghaziabad is your best choice. Our hospital is conveniently located and easily accessible for residents of Noida and the surrounding areas, including Ghaziabad. We are committed to providing the highest quality care and ensuring the best possible outcomes for our patients.
For more information or to schedule a consultation, contact Manipal Hospital Ghaziabad today. We are proud to have one of the Best Hernia Surgeons in Ghaziabad waiting to cater the best to their patients.
0 notes
Text
Prostate Surgery: Treating Prostate Conditions
Prostate surgery is a critical medical procedure aimed at addressing various conditions affecting the prostate gland, a small walnut-shaped gland in men that produces seminal fluid. This blog will explore the different types of prostate surgeries, their purposes, prostate removal surgery, and prostate surgery recovery time, providing a comprehensive understanding of how these surgeries help treat prostate conditions.
Synopsis
Understanding Prostate Conditions
Types of Prostate Surgeries
Preparing for Prostate Surgery
The Surgical Experience
Robotic-Assisted Surgery
Minimally Invasive Procedures
Non-Surgical Treatments
Recovery and Aftercare
Potential Risks and Complications
Conclusion
Understanding Prostate Conditions
The prostate gland can be affected by several conditions, including:
Benign Prostatic Hyperplasia (BPH): This is a non-cancerous enlargement of the prostate gland, common in older men. It can cause urinary problems such as difficulty starting urination, a weak urine stream, and frequent urination, especially at night.

Prostate Cancer: One of the most common cancers in men, prostate cancer can range from slow-growing tumors that may not require immediate treatment to aggressive forms that need prompt intervention.
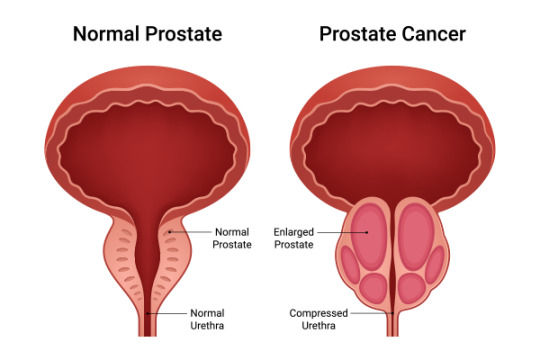
Prostatitis: This is an inflammation of the prostate gland, which can be either bacterial or non-bacterial. It can cause pain, urinary issues, and sexual dysfunction.
Types of Prostate Surgeries
Several surgical options are available to treat prostate conditions, each tailored to the specific condition and its severity.
Transurethral Resection of the Prostate (TURP):
Purpose: TURP is primarily used to treat BPH.
Procedure: During TURP, a resectoscope is inserted through the urethra to remove parts of the enlarged prostate that are obstructing urine flow.
Recovery: Patients typically stay in the hospital for one to two days. Full recovery can take a few weeks, during which patients may experience some urinary discomfort.
Prostatectomy:
Purpose: This surgery is often performed to treat prostate cancer.
Types:
Radical Prostatectomy: Removal of the entire prostate gland and some surrounding tissue.
Laparoscopic Prostatectomy: A minimally invasive procedure using small incisions and a camera to guide the surgery.
Robotic-Assisted Laparoscopic Prostatectomy: A more advanced form of laparoscopic surgery using robotic arms for greater precision.
Recovery: Hospital stays can range from one to three days. Recovery involves managing pain, catheter care, and gradually resuming normal activities over several weeks.
Transurethral Incision of the Prostate (TUIP):
Purpose: TUIP is used to treat mild to moderate BPH.
Procedure: Small cuts are made in the prostate to relieve pressure on the urethra and improve urine flow.
Recovery: This procedure often requires a shorter hospital stay and recovery period compared to TURP.
Laser Surgery:
Purpose: Laser surgeries, such as Holmium Laser Enucleation of the Prostate (HoLEP) and Photoselective Vaporization of the Prostate (PVP), are used to treat BPH.
Procedure: A laser is used to remove or vaporize excess prostate tissue.
Recovery: These minimally invasive procedures typically result in less bleeding and quicker recovery times.
Here's a comparative analysis of different types of prostate surgeries, highlighting their pros and cons: Type of SurgeryProsConsRobotic-Assisted Surgery
Greater precision
Shorter recovery times
Reduced side effects (less bleeding, fewer complications)
High cost
Requires specialized training
Risk of bleeding and infection
Transurethral Resection of the Prostate (TURP)
Effective for relieving symptoms of BPH
Widely available and well-studied
Risk of bleeding and infection
Potential for urinary incontinence and erectile dysfunction
Holmium Laser Enucleation of the Prostate (HoLEP)
Minimally invasive with faster recovery
Less bleeding and fewer side effects
Requires specialized equipment
May not be available in all medical centers
Optilume BPH Catheter System
Minimally invasive
Improves urinary flow with minimal side effects
Newer procedure with limited long-term data
High-Intensity Focused Ultrasound (HIFU)
Non-invasive
Can be used for both BPH and prostate cancer
Limited availability
May require multiple treatments
Immunotherapy
Less invasive
Utilizes the body's immune system
Not suitable for all patients
Potential for immune-related side effects
Proton Therapy
Precise targeting of cancer cells
Reduces damage to surrounding healthy tissue
High cost and limited availability
Preparing for Prostate Surgery
Preparation for prostate surgery involves several steps to ensure the patient's safety and the procedure's success:
Medical Evaluation: A thorough medical evaluation, including blood tests, imaging studies, and sometimes a biopsy, is conducted to assess the patient's overall health and the extent of the prostate condition.
Preoperative Instructions: Patients are given specific instructions regarding diet, medications, and activities to follow before surgery. This may include fasting and stopping certain medications.
Informed Consent: The surgeon will explain the procedure, potential risks, and benefits, and obtain the patient's informed consent.
The Surgical Experience
On the day of surgery, patients can expect the following:
Anesthesia: Depending on the type of surgery, general or spinal anaesthesia will be administered to ensure the patient is comfortable and pain-free during the procedure.
Surgery Duration: The length of the surgery varies based on the type of procedure but generally ranges from one to four hours.
Postoperative Care: After surgery, patients are monitored in a recovery room before being transferred to a hospital room. Pain management, catheter care, and monitoring for complications are essential aspects of postoperative care.
Robotic-Assisted Surgery
Robotic systems like the da Vinci robot enhance precision in prostate surgeries, leading to:
Shorter recovery times
Greater precision
Reduced side effects such as less bleeding and fewer complications.
Minimally Invasive Procedures
These techniques reduce risks and improve outcomes:
TURP: Refined to minimize complications.
Laser therapies: Like HoLEP, offering faster recovery and fewer side effects.
Optilume BPH catheter system: Improves urinary flow with minimal invasiveness.
Non-Surgical Treatments
Innovative non-surgical options include:
HIFU: Uses ultrasound waves to destroy prostate tissue.
Immunotherapy: Utilizes the immune system to fight prostate cancer.
Proton Therapy: Targets cancer cells precisely, sparing healthy tissue.
These advancements make prostate treatments more effective and less burdensome. If you have any specific questions, feel free to ask!
Recovery and Aftercare
Recovery from prostate surgery involves several stages:
Immediate Postoperative Period: Patients may experience some pain and discomfort, which can be managed with medications. A catheter is usually placed to help with urination.
Hospital Stay: The length of the hospital stay depends on the type of surgery and the patient's overall health. Most patients are discharged within a few days.
Home Recovery: At home, patients should follow their surgeon's instructions regarding activity levels, diet, and wound care. Gradual resumption of normal activities is encouraged, but heavy lifting and strenuous activities should be avoided for several weeks.
Follow-Up Appointments: Regular follow-up appointments are crucial to monitor the patient's recovery, manage any complications, and assess the effectiveness of the surgery.
Potential Risks and Complications
As with any surgery, prostate surgery carries potential risks and complications, including:
Infection: Postoperative infections can occur, requiring antibiotics and sometimes additional treatment.
Bleeding: Some bleeding is expected, but excessive bleeding may require intervention.
Urinary Incontinence: Temporary or, in rare cases, permanent urinary incontinence can occur.
Erectile Dysfunction: Depending on the type of surgery and the patient's condition, there may be a risk of erectile dysfunction.
Bladder Neck Contracture: Scar tissue can form at the bladder neck, causing obstruction and requiring further treatment.
Conclusion
Prostate surgery is a vital option for treating various prostate conditions, offering relief from symptoms and, in the case of cancer, potentially life-saving intervention. Understanding the different types of prostate surgeries, their purposes, procedures, and recovery processes can help patients make informed decisions about their treatment options. With advancements in surgical techniques and postoperative care, the outcomes of prostate surgeries continue to improve, enhancing the quality of life for many men.
For those seeking expert care and advanced treatment options, Manipal Hospital Ghaziabad stands out as a premier healthcare facility. With a team of highly skilled surgeons, state-of-the-art technology, and a patient-centric approach, Manipal Hospital Ghaziabad ensures the best possible outcomes for prostate surgeries and other medical treatments. Trust your health to the experts at Manipal Hospital Ghaziabad, where your well-being is our top priority.
0 notes
Text
Dengue Fever: Awareness and Prevention

Dengue fever poses a major public health threat, particularly in tropical and subtropical areas. As a mosquito-borne disease, it poses a serious threat to millions of people worldwide. In India, the incidence of dengue fever spikes during the monsoon season, making awareness and prevention crucial. This blog aims to provide comprehensive information on dengue fever, its prevention, and health tips for November, a critical month for dengue awareness in India.
Synopsis
Understanding Dengue Fever
Symptoms of Dengue Fever
Dengue Prevention
Health Tips for Dengue Prevention
India Health Awareness
Government Initiatives
Role of Non-Governmental Organizations (NGOs)
Dengue Fever vs. Other Mosquito-Borne Diseases
Conclusion
Understanding Dengue Fever
Dengue fever is caused by the dengue virus and is transmitted to humans through the bites of infected Aedes mosquitoes, especially Aedes aegypti. These mosquitoes are particularly active in the early morning and late afternoon. Dengue fever can range from mild to severe, with symptoms appearing 4-10 days after the mosquito bite.
Symptoms of Dengue Fever
The symptoms of dengue fever can vary but commonly include:
High fever
Severe headache
Pain behind the eyes
Joint and muscle pain
Nausea and vomiting
Skin rash
Mild bleeding (such as nose or gum bleeding, or easy bruising)
In severe cases, dengue can escalate to dengue hemorrhagic fever or dengue shock syndrome, both of which can be life-threatening. Symptoms of severe dengue include intense abdominal pain, persistent vomiting, rapid breathing, bleeding gums, fatigue, restlessness, and blood in vomit.
Consult our internal medicine specialists in Ghaziabad if you are experiencing dengue symptoms.
Dengue Prevention
Preventing dengue fever requires reducing mosquito populations and minimizing exposure to mosquito bites. Here are some effective strategies for dengue prevention:
Remove Breeding Sites: Aedes mosquitoes thrive in stagnant water. To prevent their breeding, regularly empty, clean, or cover containers that can hold water, such as buckets, flower pots, and discarded tyres. Make sure water storage containers are properly covered.
Use mosquito repellents: Apply repellents on exposed skin and clothing. For effective protection, choose products containing DEET, picaridin, or oil of lemon eucalyptus.
Wear Protective Clothing: Wear long-sleeved shirts, long pants, socks, and shoes to reduce skin exposure to mosquito bites, especially during peak mosquito activity times.
Install Screens and Nets: Fit window and door screens to prevent mosquitoes from entering your home. Sleeping under mosquito nets, especially for infants and young children, provides additional protection
Use Mosquito Traps and Insecticides: Employ mosquito traps and use insecticides to reduce mosquito populations. Follow the manufacturer's instructions for safe and effective use.
Community Efforts: Participate in community clean-up campaigns to eliminate mosquito breeding sites. Public health authorities often conduct fogging operations to kill adult mosquitoes.
Health Tips for Dengue Prevention
November is a critical month for dengue awareness in India due to the post-monsoon period, which creates ideal conditions for mosquito breeding. Here are some health tips to follow in November to prevent dengue fever:
Stay Informed: Keep yourself updated on dengue outbreaks in your area. Follow local health advisories and take necessary precautions.
Maintain Cleanliness: Ensure that your surroundings are clean and free of stagnant water. Regularly check and clean water storage containers, flower pots, and other potential breeding sites.
Promote Awareness: Educate your family, friends, and community about dengue prevention. Share information on social media and participate in awareness campaigns.
Seek Medical Attention: If you or someone you know exhibits symptoms of dengue fever seek medical attention promptly. Early diagnosis and treatment can prevent severe complications.
Support Public Health Initiatives: Support and cooperate with public health initiatives to control mosquito populations. Participate in community clean-up drives and follow guidelines issued by health authorities.
Consult our internal medicine hospital in Ghaziabad if you need dengue treatment.
India Health Awareness
In India, health awareness campaigns play a vital role in preventing and controlling dengue fever. The government and various health organizations conduct extensive awareness programs, especially during the monsoon and post-monsoon seasons. These campaigns focus on educating the public about dengue prevention, symptoms, and the importance of early medical intervention.
Government Initiatives
The Indian government has implemented several initiatives to combat dengue fever, including:
National Vector Borne Disease Control Programme (NVBDCP): This program focuses on preventing and controlling vector-borne diseases, including dengue. It involves surveillance, case management, and community participation.
Swachh Bharat Abhiyan (Clean India Mission): This nationwide campaign aims to promote cleanliness and hygiene, which are crucial in preventing mosquito breeding.
Public Awareness Campaigns: The government conducts regular public awareness campaigns through various media channels, including television, radio, and social media, to educate people about dengue prevention.
Role of Non-Governmental Organizations (NGOs)
NGOs also play a significant role in raising awareness about dengue fever. They organize community outreach programs, distribute informational materials, and conduct workshops to educate the public about dengue prevention and control.
Dengue Fever vs. Other Mosquito-Borne Diseases
Disease
Causative Agent
Mosquito Vector
Unique Symptoms
Prevention Methods
Dengue Fever
Dengue Virus
Aedes aegypti
High fever, severe muscle and joint pain ("break-bone fever"), pain behind the eyes, rash
Use mosquito repellents, wear long-sleeved clothing, use mosquito nets, eliminate standing water
Malaria
Plasmodium parasite
Anopheles
Cyclic fever, chills, sweating, anemia, jaundice
Use insecticide-treated bed nets, indoor residual spraying, antimalarial medications
Chikungunya
Chikungunya Virus
Aedes aegypti
Severe joint pain, fever, rash, headache
Use mosquito repellents, wear long-sleeved clothing, use mosquito nets, eliminate standing water
Zika Virus
Zika Virus
Aedes aegypti
Mild fever, rash, conjunctivitis, muscle and joint pain, headache
Use mosquito repellents, wear long-sleeved clothing, use mosquito nets, eliminate standing water
Conclusion
Dengue fever remains a major health challenge in India, particularly during the monsoon and post-monsoon seasons. Awareness and prevention are key to reducing the incidence of this mosquito-borne disease.
By following the prevention strategies outlined in this blog and staying informed about local health advisories, individuals and communities can protect themselves from dengue fever. Stay safe, stay informed, and take proactive steps to prevent dengue fever. Your health and the health of your community depend on it.
For comprehensive healthcare services and expert medical advice, visit Manipal Hospital, Ghaziabad. Their dedicated team of professionals is committed to providing top-notch care and support for all your health needs. Stay healthy and take preventive measures to protect yourself and your loved ones from dengue fever.
0 notes
Text
Diet For Chicken Pox: Foods to Eat and Avoid
Chickenpox, while commonly a childhood illness, can occur at any age. The symptoms can range from mild to severe, and proper nutrition plays a vital role in speeding up the recovery process. In this guide, we will discuss the importance of diet during chickenpox, foods to eat and avoid, and how to create a diet plan that supports your body’s healing process.
Synopsis
Nutritional Needs During Chickenpox
Foods for Symptom-Specific Relief
Recovery Tips Post-Chickenpox
Nutritional Benefits by Food Type
Sample Chickenpox Diet Chart
Impact of Age and Severity on Diet
Lifestyle Tips Beyond Diet
Cultural or Regional Diets
When to Seek Medical Help
Nutritional Needs During Chickenpox
Why Nutrition Matters:
Nutrition plays a crucial role in supporting the immune system, skin healing, and energy levels during chickenpox.
Certain nutrients help reduce inflammation, improve skin recovery, and enhance overall immunity.
Key Nutrients for Recovery:
Zinc: Crucial for wound healing and immune function.
Vitamin C: Boosts the immune system, reduces inflammation, and supports skin healing.
Vitamin A: Promotes skin regeneration and supports immune function.
Vitamin D: Helps in immune modulation and inflammation reduction.
Vitamin E: Speeds up skin recovery and reduces scarring.
Foods for Symptom-Specific Relief
Foods to Soothe Itching:
Oatmeal: Can be used both internally and externally (oatmeal baths) to calm itching.
Chamomile Tea: Known for its anti-inflammatory properties and ability to reduce skin irritation.
Anti-Inflammatory Fruits: Blueberries, strawberries, and cherries, which are rich in antioxidants.
Soft Foods for Mouth Sores:
If chickenpox blisters appear inside the mouth, consuming soft foods will reduce irritation.
Mashed Bananas
Applesauce
Soups (avoid spicy or acidic varieties)
Consult our infectious disease expert in Jaipur if you need a personalised Diet For Chicken Pox.
Recovery Tips Post-Chickenpox
Energy-Boosting Foods:
Bone Broth: Collagen-rich, helps with skin repair and provides energy.
Healthy Fats: Include nuts, seeds, and avocados to promote skin healing and immune function.
Skin Health:
Vitamin E: Foods like nuts, seeds, and leafy greens promote skin regeneration.
Hydration: Drink plenty of water and hydrating beverages like coconut water to keep the skin moist and prevent scarring.
Nutritional Benefits by Food Type
Food Type
Nutritional Benefits
Fruits
Rich in Vitamin C (immune support, skin healing)
Vegetables
High in fibre, antioxidants, and Vitamins A & E
Proteins
Supports immune function, and tissue repair (chicken, beans, tofu)
Healthy Fats
Boosts immunity, helps skin recovery (avocados, nuts)
Sample Chickenpox Diet Chart
Time of Day
Meal
Nutritional Benefits
Breakfast
Oatmeal with honey
Soothes itching and provides hydration
Mid-Morning
Fresh fruit smoothie
Vitamin C boost, antioxidants
Lunch
Lentil soup
High in zinc and protein, supports immune function
Snack
Apple slices with peanut butter
Protein for energy, fibre for digestion
Dinner
Bone broth and rice
Collagen-boosting aids skin repair
Tips:
Consistency in Diet: Maintaining a diet rich in vitamins, minerals, and protein helps speed up recovery and supports overall health.
Hydration: Drink plenty of water and herbal teas, and avoid sugary drinks to help with hydration and healing.
Impact of Age and Severity on Diet
Age-Specific Nutritional Needs:
Children: Require soft, easily digestible foods, like porridge or mashed potatoes.
Adults: Should focus on nutrient-dense foods to support the immune system and overall health.
Elderly: Special consideration may be needed for people with chronic conditions like diabetes, requiring blood sugar management along with immune-boosting foods.
Lifestyle Tips Beyond Diet
Rest: Rest is essential for recovery. Foods that promote relaxation, such as chamomile tea or warm milk, can also improve sleep quality.
Hygiene: Maintain strict hygiene while preparing food to prevent secondary infections during the recovery phase.
Stress Management: Herbal teas like peppermint and chamomile help in reducing stress and promoting healing.
Consult our infectious disease hospital in Jaipur if you need more information on the chicken pox diet chart.
Cultural or Regional Diets
Various cultures have their own approaches to diet during chickenpox:
India: Khichdi, a rice and lentil dish, is a comforting and easily digestible food.
Western Diets: Chicken broth is often recommended for its hydrating properties and easy-to-digest nature.
Asian Diets: Congee, a rice porridge, is consumed for its soothing qualities and easy digestion.
When to Seek Medical Help
While a balanced diet can aid recovery, it’s important to seek medical help if:
Symptoms worsen, such as a fever that doesn’t subside.
Dehydration sets in (dry mouth, dark-coloured urine).
If nutritional needs are not being met due to lack of appetite or inability to eat.
In severe cases, supplements or intravenous nutrition may be required, particularly for vulnerable groups such as the elderly or those with underlying health conditions.
By incorporating these dietary recommendations and lifestyle tips, you can enhance the healing process during chickenpox and make the recovery journey smoother. Remember to always consult your doctor or healthcare provider if symptoms worsen or if you have specific dietary concerns.
0 notes
Text
Thrombocytopenia: Understanding Symptoms, Causes, and Treatment

Thrombocytopenia is a medical condition characterised by an abnormally low number of platelets in the blood. Platelets, also known as thrombocytes, are crucial for blood clotting and wound healing. When platelet levels drop below the normal range (150,000 to 450,000 platelets per microliter of blood), it can lead to excessive bleeding and bruising. This blog will delve into the symptoms, causes, and treatment options for thrombocytopenia, providing a comprehensive understanding of this condition.
Synopsis
Symptoms of Thrombocytopenia
Diagnosis of Thrombocytopenia
Treatment of Thrombocytopenia
Prevention Strategies
Common Risk Factors
Emotional and Mental Health Support
Complications of Thrombocytopenia
Pediatric Thrombocytopenia
Advanced Diagnostic Techniques
Alternative and Complementary Therapies
When to See a Doctor
Symptoms of Thrombocytopenia
The symptoms of thrombocytopenia can vary depending on the severity of the condition. In mild cases, individuals may not experience any noticeable symptoms. However, as platelet levels decrease, symptoms can become more apparent and severe. Common symptoms include:
Easy or Excessive Bruising (Purpura): Individuals with thrombocytopenia may notice that they bruise easily or develop large bruises from minor injuries.
Prolonged Bleeding from Cuts: Even small cuts can result in prolonged bleeding that is difficult to stop.
Petechiae: These are tiny red or purple spots on the skin, often appearing on the lower legs, caused by bleeding under the skin.
Bleeding Gums and Nosebleeds: Frequent or severe bleeding from the gums or nose can be a sign of low platelet levels.
Blood in Urine or Stools: The presence of blood in urine (hematuria) or stools (melena) can indicate internal bleeding.
Heavy Menstrual Periods: Women with thrombocytopenia may experience unusually heavy menstrual bleeding (menorrhagia).
Fatigue: Chronic blood loss and the body's effort to compensate for low platelet levels can lead to fatigue and weakness.
Category
Cause
Description
Decreased Platelet Production
Leukemia and Other Cancers
Infiltrate the bone marrow and disrupt normal platelet production.
Aplastic Anemia
Bone marrow fails to produce sufficient blood cells, including platelets.
Viral Infections
Infections such as hepatitis C or HIV can impair bone marrow function.
Chemotherapy and Radiation Therapy
Treatments for cancer that can damage the bone marrow and reduce platelet production.
Heavy Alcohol Consumption
Excessive alcohol intake can suppress bone marrow activity.
Increased Platelet Destruction
Immune Thrombocytopenia (ITP)
Autoimmune disorder where the immune system mistakenly attacks and destroys platelets.
Thrombotic Thrombocytopenic Purpura (TTP)
Rare condition causing blood clots in small blood vessels, using up large numbers of platelets.
Disseminated Intravascular Coagulation (DIC)
Serious condition causing widespread clotting and bleeding throughout the body.
Medications
Certain medications, such as heparin, can trigger an immune response that destroys platelets.
Sequestration of Platelets in the Spleen
Liver Disease
Can cause the spleen to become enlarged and trap more platelets than usual.
Certain Cancers
Can lead to splenic sequestration, reducing the number of platelets in circulation.
Diagnosis of Thrombocytopenia
Diagnosing thrombocytopenia involves a combination of medical history, physical examination, and laboratory tests. Key diagnostic steps include:
Complete Blood Count (CBC): This test measures the number of platelets, red blood cells, and white blood cells in the blood. A low platelet count confirms thrombocytopenia.
Peripheral Blood Smear: A sample of blood is examined under a microscope to assess the appearance of platelets and other blood cells.
Bone Marrow Biopsy: If the cause of thrombocytopenia is unclear, a bone marrow biopsy may be performed to evaluate the production of blood cells.
Blood Clotting Tests: Tests such as prothrombin time (PT) and partial thromboplastin time (PTT) measure how long it takes for blood to clot and can help identify clotting disorders.
Consult our internal medicine specialist in Jaipur if you need treatment for Thrombocytopenia.
Treatment of Thrombocytopenia
The treatment of thrombocytopenia depends on the underlying cause and the severity of the condition. Treatment options include:
Medications:
Corticosteroids: These drugs can suppress the immune system and reduce platelet destruction in cases of immune thrombocytopenia.
Immunoglobulins: Intravenous immunoglobulins (IVIG) can temporarily increase platelet counts by interfering with the immune system's attack on platelets.
Thrombopoietin Receptor Agonists: These medications stimulate the bone marrow to produce more platelets.
Blood Transfusions: In severe cases, platelet transfusions may be necessary to quickly increase platelet levels and control bleeding.
Splenectomy: Surgical removal of the spleen may be considered if the spleen is trapping and destroying platelets. This procedure is typically reserved for cases where other treatments have failed.
Treating Underlying Conditions: Addressing the root cause of thrombocytopenia, such as treating infections, discontinuing causative medications, or managing liver disease, can help restore normal platelet levels.
Lifestyle Modifications: Patients with thrombocytopenia should avoid activities that increase the risk of bleeding and injury. This includes avoiding contact sports, using a soft-bristled toothbrush, and being cautious with sharp objects.
Consult our internal medicine hospital in Jaipur if you need the above treatment to manage thrombocytopenia.
Prevention Strategies
While some causes of thrombocytopenia cannot be prevented, certain strategies can help minimize the risk or manage symptoms:
Balanced Diet: Maintain a diet rich in nutrients like folate and vitamin B12 to support healthy blood cell production.
Limit Alcohol: Avoid excessive alcohol consumption, which can impair bone marrow function.
Medication Management: Use blood-thinning medications only when necessary and under medical supervision.
Regular Check-ups: Regular health check-ups can help detect early signs of thrombocytopenia and other health issues.
Common Risk Factors
Understanding who is at risk can help in early detection and management:
Age: Older adults are more susceptible to conditions that can cause thrombocytopenia.
Pre-existing Conditions: Autoimmune diseases, liver disease, and certain cancers increase the risk.
Medications and Chemicals: Exposure to certain medications and chemicals can lead to thrombocytopenia.
Genetic Predisposition: Family history of blood disorders can be a risk factor.
Table summarizing lifestyle management tips for living with thrombocytopenia:
Aspect
Tips
Injury Prevention
- Avoid contact sports and activities with a high risk of injury.
- Use protective gear (e.g., helmets, knee pads) when necessary.
- Be cautious with sharp objects and avoid activities that could cause cuts or bruises.
Dietary Recommendations
- Maintain a balanced diet rich in nutrients like folate and vitamin B12.
- Include foods that support platelet health, such as leafy greens, citrus fruits, and lean proteins.
- Stay hydrated and avoid excessive alcohol consumption.
Stress Management
- Practice relaxation techniques such as meditation, deep breathing, or yoga.
- Ensure adequate sleep to help the body recover and maintain immunity.
- Engage in regular, moderate exercise to boost overall health and reduce stress.
Emotional and Mental Health Support
The emotional impact of living with a chronic condition like thrombocytopenia should not be overlooked:
Coping Strategies: Develop coping strategies for dealing with the emotional stress of the condition.
Support Groups: Joining support groups or seeking counselling can provide emotional support and practical advice.
Complications of Thrombocytopenia
Awareness of potential complications underscores the importance of early intervention:
Internal Bleeding: Low platelet levels can lead to internal bleeding, which can be life-threatening.
Hemorrhagic Stroke: Severe thrombocytopenia can increase the risk of hemorrhagic stroke.
Surgical Risks: Patients with thrombocytopenia are at higher risk of severe blood loss during surgery or injury.
Pediatric Thrombocytopenia
Thrombocytopenia can also affect children, with some unique considerations:
Common Causes: Viral infections and immune thrombocytopenic purpura (ITP) are common causes in children.
Symptoms and Treatments: Symptoms and treatments may differ from those in adults, requiring specialised care.
Advanced Diagnostic Techniques
Cutting-edge diagnostic methods can provide more accurate assessments:
Imaging Techniques: Ultrasound can evaluate spleen size and function.
Genetic Testing: Identifying hereditary causes of thrombocytopenia through genetic testing.
Alternative and Complementary Therapies
Supportive therapies can help manage symptoms:
Natural Remedies: Some natural remedies, like papaya leaf extract, may support platelet health.
Complementary Therapies: Acupuncture and herbal medicine may provide symptom relief, but always consult healthcare professionals before starting any new treatment.
At Manipal Hospitals, Jaipur, we provide a comprehensive range of treatment options, from advanced medications to minimally invasive procedures, ensuring the best outcomes for our patients.
When to See a Doctor
Seek immediate medical care if you experience:
Uncontrolled bleeding.
Blood in your stool, urine, or vomit.
Large, unexplained bruises or red spots on your skin.
Manipal Hospitals Jaipur is committed to providing timely and compassionate care for thrombocytopenia and related conditions.
0 notes
Text
Endocarditis Symptoms, Causes, and Treatment: A Comprehensive Guide
Endocarditis is a serious condition that affects the heart's inner lining, including the heart valves. Bacterial infections most often cause it, and if not treated promptly, it can result in severe complications, including heart failure, stroke, or even death. Manipal Hospital Jaipur offers expert care for patients diagnosed with endocarditis, ensuring effective management and recovery. Here’s an in-depth guide on endocarditis symptoms, causes, treatment, and prevention.
Synopsis
What Are the Symptoms of Endocarditis?
Causes for Endocarditis
How Is Endocarditis Diagnosed?
Diet Recommendations
Managing Co-Morbidities
Infection Prevention
What Are the Risks and Complications of Endocarditis?
How to Prevent Endocarditis?
Endocarditis Outlook and Prognosis
Living With Endocarditis
Conclusion
What Are the Symptoms of Endocarditis?
Endocarditis symptoms can vary depending on the severity of the infection and how far it has spread. Some of the most common symptoms include:
Fever and chills: Often the first sign of infection.
Night sweats: Particularly common in cases of bacterial endocarditis.
Unexplained fatigue: Feeling excessively tired despite adequate rest.
Muscle and joint pain: General discomfort and aches throughout the body.
Skin changes: Red or purple spots on the skin, particularly on the feet or hands.
Heart murmur: A new or changed heart murmur can indicate damage to the valves.
Shortness of breath: Due to heart failure or complications from the infection.
Persistent cough: A dry or moist cough that doesn't go away.
Swelling in legs or abdomen: Caused by heart failure.
Red, painful bumps on fingers or toes: Known as Osler’s nodes.
Petechiae: Small, red, or purple spots under the skin caused by broken blood vessels.
If you are experiencing these symptoms, especially if you have a history of heart disease, it is important to consult a cardiologist for early diagnosis.
Causes for Endocarditis
Endocarditis is primarily caused by bacteria entering the bloodstream and infecting the heart valves. These bacteria often come from different parts of the body, particularly from:
Dental procedures: Tooth extractions, cleanings, or other oral surgeries can introduce bacteria into the bloodstream.
Infections in other parts of the body: Bacteria can spread from infections in the skin, urinary tract, respiratory system, or intestines.
Existing heart conditions: Those with damaged or artificial heart valves, congenital heart defects, or previous heart surgeries are more vulnerable to developing endocarditis.
Intravenous drug use: Use of non-sterile needles can introduce bacteria into the bloodstream.
Poor oral hygiene: Can lead to gum disease, which increases the risk of bacteria entering the bloodstream.
If you have risk factors for endocarditis, it is essential to be vigilant and get regular check-ups at Manipal Hospital Jaipur.
How Is Endocarditis Diagnosed?
Diagnosing endocarditis involves a combination of tests to confirm the presence of infection and assess its severity. These tests include:
Blood cultures: To identify the specific bacteria causing the infection. Blood cultures are typically taken before antibiotics are started.
Echocardiogram: An ultrasound of the heart to check for vegetation (growths on the valves) or damage to the valves.
Complete blood count (CBC): A high white blood cell count may indicate infection.
C-reactive protein (CRP) test: This test measures inflammation in the body, which is common in infections like endocarditis.
Chest X-ray: To check for complications such as heart failure or embolism.
Positron Emission Tomography (PET): A scan that helps locate infection sites.
At Manipal Hospital Jaipur, we use advanced diagnostic tools to provide an accurate diagnosis and tailor treatment plans for our patients.
Diet Recommendations
Balanced Diet: Eat a variety of fruits, vegetables, whole grains, lean proteins, and healthy fats to support overall health and immune function.
Limit Sodium: Reduce salt intake to help manage blood pressure and reduce strain on the heart.
Stay Hydrated: Drink plenty of water to stay hydrated, especially during recovery.
Managing Co-Morbidities
Diabetes Management: Keep blood sugar levels under control through diet, exercise, and medication as prescribed.
Hypertension Control: Monitor and manage blood pressure with lifestyle changes and medications if necessary.
Regular Check-Ups: Schedule regular visits with your healthcare provider to monitor and manage any existing health conditions.
Consult our cardiology hospital in Jaipur if you need endocarditis treatment.
Infection Prevention
Good Hygiene: Practice good personal hygiene, including regular hand washing to prevent infections.
Avoid IV Drug Use: Intravenous drug use increases the risk of endocarditis; seek help if needed to stop.
Vaccinations: Stay up-to-date with vaccinations, including the flu and pneumococcal vaccines, to reduce the risk of infections that could lead to endocarditis.
Skin Care: Take care of any cuts or wounds promptly to prevent infections from entering the bloodstream.
What Are the Risks and Complications of Endocarditis?
If not treated in time, endocarditis can cause severe complications, including:
Heart failure: due to damaged heart valves.
Stroke: Embolism from infected valve material can block blood flow to the brain.
Organ damage: Emboli can also affect other organs, including the kidneys, spleen, or lungs.
Sepsis: A widespread infection that can be life-threatening.
Permanent valve damage: requires surgical repair or replacement.
How to Prevent Endocarditis?
Preventing endocarditis is possible, especially for individuals at higher risk. Some key prevention strategies include:
Good oral hygiene: Brushing and flossing regularly and seeking dental care at Manipal Hospital Jaipur.
Preventive antibiotics: For high-risk patients (such as those with prosthetic heart valves), antibiotics may be prescribed before dental or surgical procedures.
Regular check-ups: Regular medical and dental check-ups to monitor heart health and prevent infections.
Avoiding intravenous drug use: Reducing the risk of infection through drug use is critical for preventing endocarditis.
Endocarditis Outlook and Prognosis
With timely and aggressive treatment, many people recover from infective endocarditis. The prognosis depends on:
The severity of the infection: The earlier the treatment, the better the outcome.
Presence of underlying heart conditions: Those with artificial heart valves or pre-existing valve disease may face higher risks.
Response to antibiotics: Some people may improve within days of treatment, while others may take longer.
At Manipal Hospital Jaipur, our expert team works diligently to provide the best care possible for patients diagnosed with endocarditis, ensuring optimal recovery.
Living With Endocarditis
Even after treatment, follow-up care is essential to monitor heart health. This includes:
Regular heart check-ups: Ongoing monitoring through echocardiograms and blood tests.
Medication adherence: Continuation of prescribed antibiotics or other medications as per the doctor's advice.
Lifestyle adjustments: Proper diet, exercise, and avoiding factors that could exacerbate the condition.
Ensure you stay on top of follow-up appointments at Manipal Hospital Jaipur to ensure your heart is healing properly.
Conclusion
Endocarditis is a serious but treatable condition. Early detection and prompt treatment are essential for preventing complications and promoting recovery. If you are experiencing symptoms, or if you are at risk due to a heart condition, make an appointment with Manipal Hospital Jaipur today for a thorough consultation and expert care.
If you suspect you may have endocarditis, don’t delay seeking medical help. Visit Manipal Hospital Jaipur for an accurate diagnosis and comprehensive treatment plan tailored to your specific needs.
0 notes
Text
What is Medical Termination of Pregnancy (MTP)?

Medical Termination of Pregnancy (MTP), often referred to as abortion, is a procedure to end a pregnancy. It's a decision that often carries significant emotional and personal weight. In India, the Medical Termination of Pregnancy Act provides a legal framework for safe and accessible abortion services.
Synopsis
Types of Abortion Procedures
Safety and Effectiveness
Legal Framework in India
Emotional and Psychological Considerations
Post-Abortion Care
Making Informed Decisions
Additional Considerations
Types of Abortion Procedures
There are primarily two methods for terminating a pregnancy:
1. Medical Abortion:
How it works: Involves taking medication, typically mifepristone and misoprostol, to induce a miscarriage.
When it's used: Most effective for early pregnancies, usually up to 10 weeks.
Advantages: Non-surgical, can be done at home and offers more privacy.
Disadvantages: It may take longer than surgical abortion, and there's a slight risk of incomplete abortion.
2. Surgical Abortion
How it works: A minor surgical procedure performed in a clinic or hospital.
When it's used: For later-stage pregnancies or when medical abortion is not suitable.
Common methods
Dilation and Curettage (D&C): The cervix is dilated, and the uterine lining is gently scraped to remove the pregnancy tissue.
Dilation and Evacuation (D&E): A more complex procedure used for later-stage pregnancies, involving the removal of fetal tissue using specialized instruments.
Advantages: Quicker and more predictable than medical abortion.
Disadvantages: Requires anaesthesia and carries a slightly higher risk of complications.
Safety and Effectiveness
Both medical and surgical abortions are generally safe when performed by qualified healthcare providers. It's crucial to choose a reputable clinic or hospital to minimise risks.
Legal Framework in India
The MTP Act outlines specific guidelines for abortion:
Up to 20 Weeks: Abortion is legal if it poses a risk to the woman's physical or mental health, or if the fetus has severe abnormalities.
20-24 Weeks: Abortion is permitted in limited circumstances, such as cases of rape or incest, or if the fetus has fatal abnormalities.
Emotional and Psychological Considerations
Abortion can evoke a range of emotions, including sadness, relief, or guilt. Seeking emotional support from friends, family, or a therapist can be beneficial. Many clinics offer counselling services to help individuals cope with the emotional aftermath.
Post-Abortion Care
After an abortion, it's essential to follow post-abortion care instructions provided by your healthcare provider. This typically includes:
Rest: Avoid strenuous activity for a few days.
Hygiene: Maintain good hygiene to prevent infection.
Pain Management: Use over-the-counter pain relievers as needed.
Contraception: Discuss contraception options with your healthcare provider to prevent future unintended pregnancies.
Aspect
Medical Abortion
Surgical Abortion
Method
Use of medications (Mifepristone and Misoprostol)
Surgical procedures (Dilation and Curettage, Dilation and Evacuation)
Gestational Age
Typically up to 9 weeks
Can be performed beyond the first trimester
Procedure Duration
Several hours to a few days
Usually completed within a few hours
Effectiveness
Approximately 98%
Over 99%
Recovery Time
A few days to two weeks
A few days to a week
Privacy
Can be done at home
Requires a clinical setting
Side Effects
Cramping, bleeding, nausea, mild fever
Cramping, light bleeding, risk of infectionRisks
Incomplete abortion, heavy bleeding, infection
Infection, uterine injury, retained tissue
Follow-up Care
Necessary to ensure complete abortion
Necessary to monitor for complications
Cost
Generally lower
Generally higher
Consult our gynaecology hospital in Jaipur if you need to know more about Medical Termination of Pregnancy
Making Informed Decisions
When considering an abortion, it's crucial to:
Consult a Healthcare Provider: Discuss your options, medical history, and any concerns.
Choose a Reputable Clinic: Ensure the facility is licensed and follows safety protocols.
Prioritize Your Well-being: Take care of your physical and emotional health.
Consult our gynaecologists in Jaipur if you need to know more about How Safe is Medical Abortion.
Additional Considerations
Minors and Survivors of Assault: The MTP Act provides special provisions for minors and survivors of sexual assault.
Alternative Abortion Methods: Manual Vacuum Aspiration (MVA) is a less invasive surgical option for early-stage pregnancies.
Long-Term Reproductive Health: Discuss future family planning goals with your healthcare provider.
Remember, you're not alone. If you're considering an abortion, seek support from trusted individuals and healthcare professionals.
0 notes
Text
The Importance of HPV Vaccination and Regular Pap Smears
The HPV vaccine is effective, and safe, and should be administered to girls starting from 9 to 14 years. School-going girls should be vaccinated, and if not vaccinated by 14 years, it can still be administered until 26 years, with the vaccine being licensed for use up to 45 years. In developed countries, even boys are getting vaccinated. Anyone who can afford vaccination for boys should get it done because boys can also be affected by the HPV virus, leading to other cancers like cancers of the oral tract or anus. That is why HPV vaccination is a must for both boys and girls before their sexual debut to achieve the best results.
Synopsis
The Importance of Regular Pap Smears and HPV Testing
Why Are These Tests Important?
Who Should Get Tested?
Overcoming Barriers to Testing
Conclusion
The Importance of Regular Pap Smears and HPV Testing
When it comes to women's health, regular Pap smears and HPV testing are like your personal health detectives. They play a crucial role in catching potential issues early, especially when it comes to cervical cancer. Let's dive into why these tests are so important and how they can make a difference in your life.
What is a Pap Smear?
Think of a Pap smear as a routine check-up for your cervix. During this quick and simple procedure, a healthcare provider collects cells from your cervix using a small brush or spatula. These cells are then examined under a microscope to spot any abnormalities. It's a bit like a detective looking for clues to ensure everything is in order. This is a new form of Pap smear. It is called liquid-based cytology.
What is HPV Testing?
HPV testing is another essential tool in your health toolkit. Human papillomavirus (HPV) is a common sexually transmitted infection, and certain high-risk strains can lead to cervical cancer. HPV testing involves collecting a sample of cells from your cervix, just like a Pap smear, and checking for the presence of these high-risk strains. It's like having an extra layer of security for your health.
Why Are These Tests Important?
Early Detection of Cervical Cancer: Imagine having a superpower that lets you catch problems before they become serious. Regular Pap smears and HPV testing do just that. They can detect abnormal cells early, making cervical cancer highly treatable if caught in time.
Prevention of Cervical Cancer: These tests can identify changes in cervical cells that might lead to cancer. By catching these changes early, your healthcare provider can recommend treatments to prevent cervical cancer from developing. It's like stopping a problem before it even starts.
Monitoring and Managing HPV: Since HPV is a leading cause of cervical cancer, regular testing helps keep an eye on any high-risk strains. If you test positive, your healthcare provider can monitor you closely and take action if needed. It's all about staying one step ahead.
Peace of Mind: Knowing you're taking proactive steps to monitor your health can bring a sense of relief. Regular screenings mean you're staying informed and in control of your health, reducing anxiety and stress.
Who Should Get Tested?
Guidelines for Pap smears and HPV testing can vary, but generally, women should start getting Pap smears at age 21 and continue every three years if results are normal. Women aged 30 and older might opt for co-testing (Pap smear and HPV test) every five years if the results are normal. Always consult with your Gynaecologist to determine the best schedule for you.
Overcoming Barriers to Testing
Despite their importance, some women face barriers to regular screenings. Let's tackle these challenges together:
Access to Healthcare: Finding affordable and convenient healthcare services is key. Look for low-cost or free screening programs and clinics in your area.
Education and Awareness: Understanding the importance of these tests can encourage more women to get screened. Share information with friends and family to spread the word.
Support and Counseling: If you feel anxious about the tests, seek support from healthcare providers or counselling services. Feeling comfortable and confident can make a big difference.
Note
The HPV (Human Papillomavirus) vaccine is crucial in preventing infections caused by HPV, a common sexually transmitted virus. It's important to note that HPV can infect anyone, even those with only one life partner, as it can be transmitted through intimate skin-to-skin contact. The virus often remains in the body for extended periods without causing any symptoms, making it difficult to detect. This asymptomatic nature means that individuals can unknowingly carry and transmit the virus. Over time, HPV can lead to serious health issues, including cervical cancer and other types of cancer. Therefore, vaccination is a key preventive measure to protect against the long-term risks associated with HPV.
Conclusion
If you're in Delhi and looking for a reliable healthcare provider, consider Manipal Hospitals Delhi. They offer comprehensive women's health services, including Pap smears and HPV testing. With a team of experienced healthcare professionals, Manipal Hospitals Delhi is dedicated to providing high-quality care and support for all your health needs. Don't wait—schedule your screening today and take charge of your health!
0 notes
Text
Understanding the Recent HMPV Virus Outbreak: Insights from Dr. Ankita Baidya
The recent outbreak of the Human Metapneumovirus (HMPV) has raised significant concerns, especially given its potential to affect vulnerable populations such as children and the elderly. Dr. Ankita Baidya, Consultant - Infectious Diseases at Manipal Hospitals Dwarka, New Delhi, provides valuable insights into the nature of this virus and the necessary precautions to mitigate its spread.
Synopsis
Symptoms and Vulnerable Populations
Preventive Measures
Potential for a Pandemic
Current Situation in India
Symptoms and Treatment
Conclusion
Symptoms and Vulnerable Populations
Flu-like symptoms: Fever, sore throat, runny nose, nasal congestion, cough, body ache, and malaise.
Severe complications: Pneumonia, particularly in children and the elderly.
Hospitalization: May be required in severe cases.
Preventive Measures
Hand hygiene: Regularly wash hands with soap and water.
Wearing masks: Especially in crowded places or when experiencing symptoms.
Social distancing: Maintain distance to reduce transmission.
Incubation period: 3-6 days; individuals with symptoms should wear masks to prevent transmission.
Travel precautions: Report to health authorities upon arrival from impacted regions.
Potential for a Pandemic
Global reports: HMPV has been reported worldwide, primarily affecting children and infants.
Current strain: Increased hospitalizations in affected countries like China.
Preventive measures: Understanding virus properties and implementing timely precautions are crucial.
Current Situation in India
As of now, there are three confirmed cases of HMPV in India, primarily affecting children under two years of age. With improved testing, more cases may be identified. However, Dr. Baidya advises against panic, emphasizing the importance of respiratory precautions and isolation for those showing symptoms or traveling from outbreak areas.
Symptoms and Treatment
Common symptoms: Fever, sore throat, cold, sneezing, blocked nose, headache, dry cough, and shortness of breath.
Severe disease: More common in children and the elderly.
Supportive care: Focus on alleviating symptoms.
Recovery: Typically within a week for patients with good immunity.
Conclusion
Dr. Baidya's insights underscore the importance of vigilance and timely precautions in managing the HMPV outbreak. By maintaining hand hygiene, wearing masks, practicing social distancing, and strengthening diagnostic facilities, we can mitigate the spread of this virus and protect vulnerable populations. Stay informed, stay safe, and take the necessary steps to protect yourself and your loved ones from HMPV.
0 notes
Text
Battling the Invisible Enemy: Human Metapneumovirus Insights
Human Metapneumovirus (HMPV) is a significant respiratory pathogen, particularly affecting young children, the elderly, and those with compromised immune systems. As the first human member of the Metapneumovirus genus in the Pneumovirinae subfamily within the Paramyxoviridae family, HMPV is an enveloped negative-sense single-stranded RNA virus.
Recently, HMPV has been making headlines due to a notable surge in cases, especially in China, raising global concerns about its spread and potential public health impact.
Synopsis
Surge in China
Symptoms of Human Metapneumovirus (HMPV)
Prevention and Treatment
Vaccine Development and WHO Response
Cases in India
Conclusion
Surge in China
Recent reports indicate a significant surge in HMPV cases in China, with an alarming increase in hospitalizations. The outbreak is raising fears that the virus, which causes symptoms similar to the flu or common cold, may overwhelm the healthcare system, especially during the winter season when respiratory viruses tend to spread more rapidly. This surge has prompted increased monitoring and responses from both national and international health bodies.
Symptoms of Human Metapneumovirus (HMPV)
Fever: A common initial symptom, often accompanied by chills.
Cough: Persistent and can be either dry or productive.
Nasal Congestion: Blocked or runny nose, often leading to difficulty breathing through the nose.
Sore Throat: Pain or irritation in the throat, especially when swallowing.
Wheezing: A high-pitched whistling sound during breathing, indicating respiratory distress.
Bronchiolitis: Inflammation of the small airways in the lungs, more common in infants.
Pneumonia: Infection that inflames the air sacs in one or both lungs, which can fill with fluid.
Respiratory Distress: Severe difficulty in breathing, requiring immediate medical attention.
HMPV is highly contagious and spreads through respiratory droplets, making it easily transmissible in close-contact environments like schools, hospitals, and crowded public spaces. Given its similarities with other respiratory viruses, it can sometimes be mistaken for the flu or a common cold, making timely diagnosis critical.
Consult our internal medicine specialist in Delhi if you are experiencing symptoms of HMPV and need treatment.
Prevention and Treatment
Currently, there is no specific antiviral treatment for HMPV infections. The focus remains on supportive care, such as fluid management, fever control, and ensuring adequate oxygen levels for patients who experience severe respiratory symptoms. In some cases, patients may require mechanical ventilation if respiratory distress occurs.
Prevention of HMPV is similar to measures taken for other respiratory viruses. These include regular hand washing, using tissues when coughing or sneezing, wearing masks in high-risk areas, and avoiding close contact with infected individuals. Maintaining good hygiene and disinfecting surfaces in high-traffic areas can help reduce transmission. Additionally, protecting vulnerable populations such as infants, the elderly, and immunocompromised individuals from exposure is key to controlling the spread of HMPV.
Consult our internal medicine specialist in Delhi if you need treatment of HMPV
Vaccine Development and WHO Response
As of now, no specific vaccine exists for human metapneumovirus. However, researchers are actively investigating the development of vaccines and antiviral treatments to reduce the burden of the disease. The World Health Organization (WHO) is closely monitoring the outbreak and continues to work with countries like China to understand the virus's behaviour and mitigate its spread[4]. WHO has recommended that national health authorities enhance surveillance and reporting of HMPV cases to better assess the situation and allocate resources for response.
According to WHO, “China’s reported levels of acute respiratory infections, including HMPV, are within the expected range for the winter season with no unusual outbreak patterns reported. Chinese authorities confirmed that the healthcare system is not overwhelmed, hospital utilization is currently lower than this time last year, and there have been no emergency declarations or responses triggered”[4]. However, the WHO has issued advisories emphasizing the importance of timely diagnosis, effective treatment protocols, and enhancing public health awareness campaigns. Additionally, WHO has urged governments to strengthen health systems to ensure they are prepared to handle potential surges in cases, especially during peak respiratory virus seasons.
Cases in India
India, too, has reported sporadic cases of HMPV, with a few localized outbreaks occurring in recent years. Given the country's dense population and high prevalence of respiratory diseases, HMPV poses a significant public health concern. As health authorities continue to monitor the situation, India has implemented measures similar to those in other countries, including enhanced surveillance and public health advisories.
While the immediate risk of a widespread outbreak in India remains low, the government and health experts emphasize the importance of preventive measures, particularly in areas with high levels of respiratory illnesses. Increased awareness and vigilance among healthcare providers are crucial for early detection and treatment.
Here's a table comparing Human Metapneumovirus (HMPV) with other common respiratory viruses:
Feature
HMPV
Influenza (Flu)
Respiratory Syncytial Virus
Common Cold (Rhinovirus)
Virus Family
Paramyxoviridae
OrthomyxoviridaeParamyxoviridae
Picornaviridae
Genus
Metapneumovirus
Influenzavirus
Orthopneumovirus
Enterovirus
Genome Type
RNA, negative-sense
RNA, negative-sense
RNA, negative-sense
RNA, positive-sense
Transmission
Respiratory droplets, direct contact
Respiratory droplets, direct contact
Respiratory droplets, direct contact
Respiratory droplets, direct contact
Common Symptoms
Fever, cough, nasal congestion, sore throat, wheezing
Fever, chills, muscle aches, cough, sore throat
Runny nose, decrease in appetite, coughing, sneezing, fever
Runny nose, sore throat, cough, sneezing
Severe Complications
Bronchiolitis, pneumonia, respiratory distress
Pneumonia, bronchitis, sinus infections, worsening of chronic conditions
Bronchiolitis, pneumonia, respiratory distress
Rare, but can lead to sinus infections or ear infections
Affected Populations
Young children, elderly, immunocompromised
All age groups, especially young children, the elderly, and those with chronic conditions
Infants, young children, elderly, immunocompromised
All age groups, particularly children
Seasonality
Winter and early spring
Fall and winter
Fall, winter, and early spring
Year-round, with peaks in fall and spring
Prevention
Hand washing, masks, avoiding close contact with infected individuals
Annual vaccination, hand washing, masksHand washing, masks, avoiding close contact with infected individual
Hand washing, masks, avoiding close contact with infected individuals
Treatment
Supportive care, no specific antiviral
Antiviral medications (e.g., oseltamivir), supportive care
Supportive care, no specific antiviral
Supportive care, no specific antiviral
Conclusion
In conclusion, while HMPV continues to pose a public health challenge, its management relies heavily on early detection, supportive treatment, and preventive strategies. The surge in China has heightened global attention, and the ongoing efforts of health organizations, such as the WHO, remain vital in controlling its spread
0 notes
Text
Sarcoidosis Disease: Causes, Symptoms, Treatment and Prevention

Sarcoidosis is a complex and often misunderstood disease that affects multiple organs in the body, primarily the lungs and lymph glands. It is characterized by the formation of tiny clumps of inflammatory cells called granulomas. These granulomas can disrupt the normal structure and function of affected organs. While the precise cause of sarcoidosis is unclear, it's thought to stem from an abnormal immune response.
Synopsis
What is Sarcoidosis?
Causes of Sarcoidosis
Symptoms of Sarcoidosis
Diagnosis of Sarcoidosis
Treatment of Sarcoidosis
Prevention of Sarcoidosis
Living with Sarcoidosis
Conclusion
What is Sarcoidosis?
Sarcoidosis is an inflammatory disease that can affect multiple organs in the body, but it most commonly impacts the lungs and lymph glands. It's marked by the formation of small clumps of inflammatory cells, called granulomas. These granulomas can alter the normal structure and function of the affected organ
Causes of Sarcoidosis
The precise cause of sarcoidosis is still a mystery, but it is thought to be related to an overactive immune system responding to an unknown trigger. This trigger could be an infection, environmental factors, or genetic predisposition. Here are some potential sarcoidosis causes:
Genetic Factors: Family history plays a role in the likelihood of developing sarcoidosis. Certain genetic markers have been associated with an increased risk of the disease.
Environmental Factors: Exposure to certain environmental agents, such as dust, chemicals, or infectious agents, may trigger the disease in genetically susceptible individuals.
Infections: Some researchers believe that bacteria, viruses, or fungi might trigger the immune response that leads to sarcoidosis.
Symptoms of Sarcoidosis
Sarcoidosis symptoms can vary widely depending on which organs are affected. Some people may have no symptoms at all, while others may experience severe symptoms. Common symptoms include:
1. General Symptoms
Fatigue
Fever
Swollen lymph nodes
Weight loss
Lung Symptoms:
Persistent dry cough
Shortness of breath
Chest pain
2. Skin Symptoms
Reddish-purple bumps or patches, often on the shins or ankles
Visible sores or lesions on the nose, cheeks, and ears
Patches of skin that are discoloured, either darker or lighter
3. Eye Symptoms
Blurred vision
Eye pain
Severe redness
Sensitivity to light
4. Heart Symptoms
Irregular heartbeats (arrhythmias)
Heart palpitations
Shortness of breath
Swelling caused by fluid buildup (oedema)
5. Nervous System Symptoms
Headaches
Weakness or numbness in an arm or leg
Facial paralysis
Consult our pulmonologist in Delhi if you are experiencing sarcoidosis symptoms.
Diagnosis of Sarcoidosis
Diagnosing sarcoidosis can be challenging due to its wide range of symptoms and similarity to other diseases. A thorough medical history, physical examination, and various tests are often required. These tests may include:
Chest X-ray: To look for granulomas or enlarged lymph nodes in the chest.
CT Scan: Provides a more detailed image of the lungs and other organs.
Pulmonary Function Tests: Pulmonary function tests measure lung capacity, airflow, and gas exchange.
Biopsy: A small sample of tissue is taken from an affected organ to look for granulomas.
Blood Tests: To check for signs of inflammation and other abnormalities.
Treatment of Sarcoidosis
There is no cure for Sarcoidosis Disease, but treatment can help manage symptoms and improve quality of life. Treatment options vary depending on the severity of the disease and the organs affected. Common treatments include:
1. Medications
Corticosteroids: These are the most commonly prescribed drugs for sarcoidosis. They help reduce inflammation and suppress the immune system.
Immunosuppressive Drugs: Medications such as methotrexate, azathioprine, and hydroxychloroquine may be used if corticosteroids are not effective or cause significant side effects.
TNF-alpha Inhibitors: These drugs, such as infliximab, can be used in severe cases to reduce inflammation.
2. Lifestyle Changes
Healthy Diet: A balanced diet, rich in fruits, vegetables, and whole grains, can boost your immune system.
Regular Exercise: Physical activity can help improve overall health and reduce fatigue.
Smoking Cessation: Quitting smoking is crucial, especially for those with lung involvement.
3. Supportive Therapies
Oxygen Therapy: For those with severe lung involvement, oxygen therapy can help improve breathing.
Physical Therapy: Helps maintain muscle strength and mobility.
Consult our pulmonology hospital in Delhi if you need sarcoidosis treatment.
Prevention of Sarcoidosis
There is no known way to prevent sarcoidosis, but certain measures can help reduce the risk of complications and manage the disease effectively:
Regular Medical Check-ups: Early detection and treatment of symptoms can prevent complications.
Avoiding Triggers: Identifying and avoiding environmental or occupational triggers that may worsen the condition.
Healthy Lifestyle: Maintaining a healthy lifestyle with a balanced diet, regular exercise, and avoiding smoking can support overall health and potentially reduce the severity of symptoms.
Living with Sarcoidosis
Living with sarcoidosis can be challenging, but many people lead full and active lives with proper management. Support from healthcare providers, family, and support groups can make a significant difference. Here are some tips for managing life with sarcoidosis:
Education: Learn as much as possible about the disease to make informed decisions about treatment and lifestyle changes.
Support Groups: Joining a support group can provide emotional support and practical advice from others who understand what you’re going through.
Stress Management: Techniques such as meditation, yoga, and deep breathing exercises can help manage stress and improve overall well-being.
Conclusion
Sarcoidosis is a complex disease with a wide range of symptoms and potential complications. While there is no cure, understanding the causes, symptoms, and treatment options can help manage the disease effectively. With proper medical care and lifestyle adjustments, many people with sarcoidosis can lead healthy and fulfilling lives.
0 notes
