Don't wanna be here? Send us removal request.
Photo

Personalizing AI speech - US Patent 9601104
In general, AI talks to everyone the same way. This lack of personalization limits AI’s ability to relate to and communicate with people. But patent 9601104 could make impersonal AI a thing of the past. IBM scientists created a way for AI systems to analyze, interpret and mirror users’ unique speech and linguistic traits––making it easier to talk to your technology.
This is just one of the record-breaking 9,000+ patents IBM received in 2017. Explore more patents->
10K notes
·
View notes
Photo

Epiphytes, often called air plants, can grow without soil, without parasitising another plant. They are often found in humid conditions, growing on larger organisms like trees.
Image: BBC Nature
#epiphytes
463 notes
·
View notes
Link
Prior research has shown that the drug ketamine, generally used as an anesthetic drug, can lead to reduced symptoms of depression in some people. In this new effort, the researchers have delved farther into the brain to find out why.
The efforts by the team actually resulted in two papers, both printed in Nature. In the first, they report finding that ketamine reduces depression symptoms by blocking LHb neural bursting (where groups of nerves fire as a barrage rather than as a slow pulse). They also noted that for the drug to work, both N-methyl-d-aspartate receptors and low-voltage-sensitive T-type calcium channels had to be active. In their second paper, they describe identifying a possible means for regulating the bursting behavior, reducing the need for blockers such as ketamine.
The results explain why ketamine works so quickly, in as little as 30 minutes, to reduce depression symptoms, while other drugs can take weeks or months. Instead of causing changes in brain chemical levels.
More information: Yan Yang et al. Ketamine blocks bursting in the lateral habenula to rapidly relieve depression, Nature (2018). DOI: 10.1038/nature25509
194 notes
·
View notes
Photo

When you think you can smell snow, you aren’t actually smelling anything. It’s a sensory experience caused by colder weather, humidity, and the feeling of cold air. The cold slows down air molecules, humidity boosts your olfactory nerves, freezing air hits the nerve that transmits sensations from your face to your brain, and this creates the crisp ‘scent’ of snow. Source Source 2
2K notes
·
View notes
Photo

Discovery Deepens Understanding of Brain’s Sensory Circuitry
“There is a good chance that these infrabarrels reveal a kind of circuit architecture that wasn’t appreciated before,” Connors said.
The research is in Cell Reports. (full open access)
26 notes
·
View notes
Photo

Stuttering: Stop Signals in the Brain Disturb Speech Flow
One per cent of adults and five per cent of children are unable to achieve what most of us take for granted–speaking fluently. Instead, they struggle with words, often repeating the beginning of a word, for example “G-g-g-g-g-ood morning” or get stuck with single sounds, such as “Ja”
The research is in Brain. (full open access)
28 notes
·
View notes
Photo

Hyperbaric Oxygen Therapy May Alleviate Alzheimer’s Symptoms
A new Tel Aviv University study reveals that hyperbaric oxygen treatments may ameliorate symptoms experienced by patients with Alzheimer’s disease.
The research is in Neurobiology of Aging. (full access paywall)
34 notes
·
View notes
Video
tumblr
Nicotine in cigarettes reaches your brain in just 10 seconds. Exposure to nicotine as a teen may lead to long lasting effects, like increased impulsivity and mood disorders.
13K notes
·
View notes
Photo

Injectable Gel Helps Heart Muscles Regenerate After Heart Attack
In mammals, including humans, the cells that contract the heart muscle and enable it to beat do not regenerate after injury. After a heart attack, there is a dramatic loss of these heart muscle cells and those that survive cannot effectively replicate. With fewer of these contractile cells, known as cardiomyocytes, the heart pumps less blood with each beat, leading to the increased mortality associated with heart disease.
The research is in Nature Biomedical Engineering. (full access paywall)
45 notes
·
View notes
Photo

How Insulin in the Brain May Suppress the Subjective Feeling of Hunger
Eating behavior and the subjective feeling of hunger are regulated by a variety of hormones. Here a key role is played by the hormone insulin because it is not only active in the body, but also in the brain. It was previously known that insulin acts on the homeostatic region (hypothalamus*). Now, however, scientists have found that the hormone is also active in other brain regions. Researchers at the Institute for Diabetes Research and Metabolic Diseases of Helmholtz Zentrum München at the University of Tübingen, a partner of the DZD, have further deciphered the function of insulin in the brain as well as its influence on the subjective feeling of hunger and have published their findings in Scientific Reports, a Nature research journal.
To better understand the mechanism of action of insulin, the researchers administered insulin intranasally to healthy young adults. Through the application of the hormone via a nasal spray, the blood-brain barrier is bypassed and the insulin reaches the brain directly. In the study, 25 lean, ten overweight and 12 obese participants “sniffed” insulin or the placebo. Brain activity was then visualized and recorded by means of a functional magnetic resonance imaging (fMRI) scan. The result in all study participants: Intranasal insulin improves functional connectivity in the prefrontal regions of the default-mode network (DMN), a group of brain regions that are activated when a person is at rest and is not performing any tasks. This region is central to cognitive processes. In addition, the functional connectivity between the DMN and the hippocampus as well as the hypothalamus is strengthened. These changes in the brain also influence eating behavior and alter the relationship between adiposity and the hunger sensation. Actually, people with a lot of visceral adipose tissue** have an increased sensation of hunger. “Insulin-enhanced connectivity between the DMN and the hippocampus suppresses the relationship between adipose tissue and the subjective hunger feeling,” said Stephanie Kullmann, author of the study. The study participants felt less hunger after being administered intranasal insulin.
In addition, the scientists observed that insulin in the brain also improves the effect of the hormone in the body. Study participants with insulin-induced increased functional connectivity in the DMN have higher insulin sensitivity in the body. This counteracts obesity and type 2 diabetes. The current results show that insulin in the brain – due to increased functional connectivity between cognitive and homeostatic regions – may help regulate eating behavior and facilitate weight loss. * The hypothalamus is the supreme regulatory center for all vegetative and endocrine processes. The hypothalamus coordinates water and saline balance as well as blood pressure. It ensures the maintenance of the inner milieu (homeostasis) and regulates food intake. ** The fatty tissue on and especially in the abdomen is called visceral fat. It is stored in the free abdominal cavity and envelops the internal organs – especially the organs of the digestive system. There is a relationship between visceral adipose tissue and the subjective feeling of hunger.
125 notes
·
View notes
Photo

The Brain’s Rejuvenating Cells
Alzheimer’s disease is a neurodegenerative disease manifested by various neuronal pathological processes and a significant decline in brain function. Aggregates of beta-amyloid protein (“plaques”) accumulate within and between brain cells. Due to both structural changes and the weakening of chemical communication pathways, the junctions of neuronal networks (synapses) are lost. In addition, the cytoskeletal proteins of the axons lose their normal structure, impairing their function and causing massive neuronal death.
The brain is a fragile and unique organ that has its own specially tailored immune system, separate from the rest of the body. The primary role of the brain’s immune cells, called microglia, is to recognize, disassemble, and dispose of various substances that do not function properly in the brain, from dying cells to various cell debris and protein aggregates. Yet microglia activity is under tight regulation to allow them to dispose of waste without harming adjacent healthy neurons that retain important information. The gamut of their activity – from essential immune function to the risk of damaging healthy neurons due to hyperactivity – is well balanced in young healthy individuals, but might become a disadvantage in aging and under neuropathological conditions. A key question is, why are the brain’s resident immune cells not effective in repairing the damage associated with Alzheimer’s disease?
Alzheimer’s is often associated with local inflammation. In the absence of a clear understanding of the contribution of the systemic and brain immune cells to disease pathology, many scientists have interpreted the local brain inflammation that accompanies Alzheimer’s disease as a negative outcome of excessively aggressive microglia and the uncontrolled entry of immune cells from the periphery into the brain. Anti-inflammatory treatments were therefore attempted, without success, leaving researchers in the field puzzled as to the function of immune cells in neurodegenerative diseases.
Prof. Michal Schwartz of the Weizmann Institute of Science’s Department of Neurobiology has shown over the years that mobilizing cells from the systemic immune system does not always cause harm – and in fact, if well controlled, can even help in coping with various brain pathologies. But the question regarding the role of the brain’s own immune cells, the microglia, remains open: are they, themselves, useful? Useless? Or, perhaps, harmful?
Prof. Schwartz, together with Prof. Ido Amit of the Department of Immunology and members of their research groups – postdoctoral researchers Drs. Hadas Keren-Shaul and Assaf Weiner, and research students Amit Spinrad, Orit Matcovitch-Natan, and Raz Dvir-Szternfeld – now provide an answer to this question, along with a new research approach toward finding ways of treating Alzheimer’s.
The scientists studied a genetically engineered mouse model of the disease, whose genetic makeup includes five mutant human genes that cause an aggressive form of Alzheimer’s. The brains of these mice exhibit similar features to those that take place in the brains of humans suffering from Alzheimer’s. A significant obstacle to understanding the roles of immune cells in Alzheimer’s and other neurodegenerative diseases is the ability to accurately distinguish between similar cells with different functions, and thus understand who is a friend and who is a foe. The scientists employed advanced single-cell genomic sequencing technology – a “genetic microscope” developed in Prof. Amit’s lab in recent years – which enables scientists to fully sequence the genetic material of individual cells, allowing them to identify the unique function of these immune cells, even when they are extremely rare – in other words, separating the wheat from the chaff.
In this study, the scientists sequenced the RNA content of all the immune cells in the brains of the mice with Alzheimer’s – an endeavor that, until very recently, could not have been undertaken. Since Alzheimer’s is a progressive disease, the team repeated this experiment at different points in time during the disease’s progression, and compared the results with those from healthy mice. This led them to a fascinating finding: a subset of unique microglial cells not found in healthy mice, and which gradually change as the disease progresses. They called these cells disease-associated microglia (DAM).
The scientists found that the development of this unique type of cell depends on the reduction in the expression of regulatory proteins (checkpoints) that restrain microglia activity in the brain, and an increase in the expression of a protein complex that recognizes the accumulation of foreign lipids (fat-like molecules) and dead cells, including a protein called TREM2. A mutation in this protein is accompanied by an early – and dramatic – onset of the disease.
When the researchers, in collaboration with Prof. Marco Colonna of the Washington University School of Medicine in St. Louis, used an Alzheimer’s mouse model that does not express TREM2, the microglia failed to acquire the repair pathways of the DAM cells to remove the beta-amyloid plaques. An examination of the brains of the Alzheimer’s mouse model and a postmortem of Alzheimer’s disease patients revealed that these unique cells are located in close proximity with aggregates of amyloid plaques, suggesting a connection between the mechanism that leads to the activation of these unique microglia and their mode of activity. In fact, the newly discovered microglia express many proteins that have been previously classified as disease “risk markers” in Alzheimer’s patients, which highlight their important beneficial role in these patients. In other words, mutations in proteins expressed by these cells cause dysfunction of plaque disposal and are therefore accompanied by an earlier onset and more severe disease.
“This broad set of findings,” says Prof. Amit, “leads us to the current understanding that a certain [genetic or environmental] failure in the process of downregulating the expression of the regulatory proteins [checkpoints] does not allow for sufficient upregulation of repair pathways, leading to the inability of the DAM cells we identified to appropriately perform their plaque-disposal tasks.
“This is a completely new concept in comprehending Alzheimer’s disease, based on data-driven models that allow for a mechanistic understanding of the central role of microglial cells in the disease, and on the insight that microglial checkpoints, which are imperative for normal function, become an obstacle in the diseased brain.”
These discoveries signify new potential targets in the search for an Alzheimer’s therapy, according to Prof. Schwartz: “By identifying key proteins that restrain microglia transition to become DAM, we will search for molecular ways to selectively reduce their expression/activity, thereby enhancing the repair pathways. In turn, this would lead to the acceleration of DAM cell development, an increase in their number and efficiency in removing ‘plaque’ in the brain, and, possibly, to curbing various disease symptoms. These, as well as targets that activate their phagocytic pathways, might serve as potential new targets for drug development.”
“Further,” says Dr. Keren-Shaul, one of the study’s lead authors, “our current studies are focusing on identifying the optimal molecules to target.”
“This challenge is central to the current investigations of our research groups,” say the two team leaders.
120 notes
·
View notes
Link
2 notes
·
View notes
Photo

Prepare to be amazed by artifacts released from the archives of the British Library, unseen sketches and manuscript pages from J.K. Rowling, and incredible illustrations from artist Jim Kay.
4K notes
·
View notes
Photo

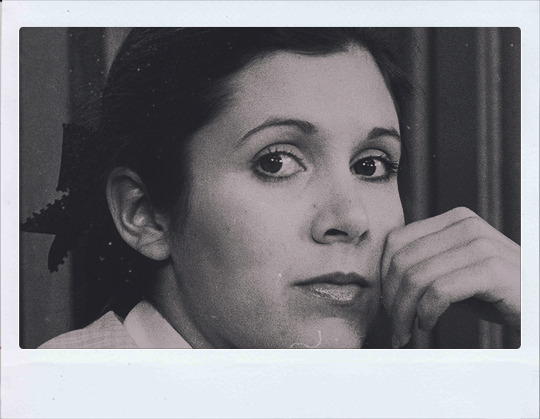





Stay afraid, but do it anyway. What’s important is the action. You don’t have to wait to be confident. Just do it and eventually the confidence will follow.
Happy Birthday, Carrie Fisher! (october 21, 1956)
29K notes
·
View notes
Text
What’s Up November 2017
What’s Up For November?
Dawn pairing of Jupiter and Venus, Moon shines near star clusters, meteor activity all month long!

This month binoculars will come in handy–to view the moon, star clusters, and a close pairing of Venus and Jupiter.

You can’t miss bright Venus in the predawn sky. This month Venus pairs up with Jupiter on the morning of November 13th.

The Leonids peak on a moonless November 17th. Expect no more than 10 meteors an hour around 3:00 a.m., the height of the shower.

The Northern and Southern sub-branches of the Taurid meteor shower offer sparse counts of about 5 meteors per hour, but slow, bright meteors are common.

The nearby November Orionids peak on the 28th. In contrast to the Taurids, the Orionids are swift. But don’t expect more than 3 meteors per hour.

The moon glides by three beautiful star clusters in the morning sky this month, and a pair of binoculars will allow you to see the individual stars in the clusters. Aim your binoculars at the Pleiades and the moon on the 5th.

Then aim at the Messier or M-35 cluster and the moon on the 7th and the Beehive cluster and the moon on the 10th.

Meanwhile, at dusk, catch Saturn as it dips closer to the western horizon and pairs up with Mercury on the 24th through the 28th.

Also, Comet C/2017 O1 should still be a binocular-friendly magnitude 7 or 8 greenish object in November. Use Polaris, the North Star as a guide. Look in the East to Northeast sky in the late evening.
Watch the full What’s Up for November Video:
youtube
Make sure to follow us on Tumblr for your regular dose of space: http://nasa.tumblr.com.
2K notes
·
View notes
Photo

Sloths risk their lives every time they poop. It’s basically the only reason they descend to the ground, even though over half of them die whenever they leave the safety of their trees. They can get pretty backed up because it only happens once a week - so every time a sloth poops, it has to stand up, hug the base of a tree, and do a little poo dance to get it all out. Source Source 2 Source 3

That was the fast-motion version… (obvi)
2K notes
·
View notes
Photo

Where microseconds matter
In the mammalian auditory system, sound waves impinging on the tympanic membrane of the ear are transduced into electrical signals by sensory hair cells and transmitted via the auditory nerve to the brainstem. The spatial localization of sound sources, especially low-frequency sounds, presents the neuronal processing system with a daunting challenge, for it depends on resolving the difference between the arrival times of the acoustic stimulus at the two ears. The ear that is closer to the source receives the signal before the contralateral ear. But since this interval – referred to as the interaural timing difference (ITD) – is on the order of a few microseconds, its neuronal processing requires exceptional temporal precision. Members of the research group led by LMU neurobiologists Professor Benedikt Grothe and Dr. Michael Pecka have now uncovered a specific combination of mechanisms, which plays a crucial role in ensuring that auditory neurons can measure ITDs with the required accuracy. Their findings appear in the journal PNAS.
Before cells in the auditory brainstem can determine the ITD, the signals from both ears must first be transmitted to them via chemical synapses that connect them with the sensory neurons. Depending on the signal intensity, synapses themselves can introduce varying degrees of delay in signal transmission. The LMU team, however, has identified a pathway in which the synapses involved respond with a minimal and constant delay.“ Indeed, the duration of the delay remains constant even when rates of activation are altered, and that is vital for the precise processing of interaural timing differences,” Benedikt Grothe explains.
In addition, Grothe and his colleagues demonstrate that a particular structural feature of the wrapping of the signal-transmitting fibers (“axons”) by discontinuous membrane sheaths, which they first described in the journal Nature Communications in 2015, correlates with the constancy of synaptic delay in the pathway. In that study, they had found that these axons are particularly thick and that their wrapping exhibits a highly unusual pattern to enable rapid signal transmission – which is an important prerequisite for accurate measurement of minimal timing differences. Both of these features are found in mammals such as gerbils, which use ITDs for the localization of low-frequency sounds, but not in mice, which only hear high frequencies and don’t use ITDs. “Our work underlines the fact that nerve cells and neuronal circuits are anatomically and physiologically adapted for the specific nature of their biological function,” says Dr. Michael Pecka. “We assume that all mammals that are capable of perceiving low-frequency sounds make use of these structural adaptations.” (PNAS 2017)
84 notes
·
View notes