#Best Nephrologist in California
Text
Reaching Your Work Goals While on Dialysis: 5 Tips to Help
You’ve been diagnosed with chronic kidney disease and told that you’ll need to start dialysis to keep your kidneys functioning. This may seem like a daunting task, but with a bit of organization and planning, you can reach your work goals while on dialysis. Here are five tips to help you get started.
Set Realistic Work Goals
The best way to start is by setting realistic work goals. When you’re on dialysis, your body is going through a lot. You need to be patient and give yourself time to adjust. You don’t want your work goals to add any extra stress to your life.
Start by thinking about the type of job you want. Do you want to continue working the same job you have now? Or are you looking for a new challenge? Maybe you would like to try working from home.
Think about the hours you would like to work each week and what type of work schedule would be best for you. Don’t forget to take into account your treatment schedule and how many hours you can realistically work each week.
Working With Your Medical Team
Your doctor and renal social worker are your best allies when it comes to working while on dialysis. They can help you understand your treatment and what to expect, as well as advocate for you with your employer.
Be sure to keep them in the loop about any changes in your health or work situation. They may need to adjust your treatment or work accommodations as needed. And remember, they’re there to help—so don’t be afraid to ask for their guidance.
Take Care of Yourself First
When it comes to working while on dialysis, it’s important to take care of yourself first and foremost. Here are five tips that can help:
Make sure you’re well-rested. Dialysis can be exhausting, so make sure you’re getting enough sleep.
Eat a healthy diet. This will help you feel your best and give you the energy you need to work.
Take breaks when needed. It’s important to listen to your body and take a break when you need it.
Drink plenty of fluids. This will help keep you hydrated and make dialysis easier on your body.
Pace yourself. Dialysis can be tiring, so try not to overdo it in the beginning.
Practical Strategies for Working on Dialysis
It’s important to have practical strategies in place to ensure that you’re able to stick to your dialysis routine and still have time for work.
Make sure you have flexible work hours/willingness at your workplace: Find out if there are flexible working arrangements that can cater to your dialysis schedule, and if need be, consider asking for accommodation if your workplace is compliant.
Learn about remote working options: Depending on the type of job you have, there may be opportunities where you can do some or all of your work remotely. Doing this will give you more control over your schedule and could help you better manage your time between dialysis and work.
Don’t forget breaks: Breaks are essential when it comes to taking care of yourself, so make sure you take the time to rest. It’s perfectly ok (and recommended) to take breaks during a busy day—all it requires is a little bit of planning ahead!
Speak up about situations where you feel overwhelmed: This includes speaking up if something at work is impacting your health negatively or draining too much energy away from doing regular dialysis treatments. It’s important that everyone understands how much effort just staying afloat takes with a chronic illness like peritoneal dialysis, and work colleagues need to be aware that they can be part of the solution.
Resources and Support
It’s important to remember that you’re not alone in this journey. There are resources and support groups available to help. It’s a good idea to talk to your healthcare team and dialysis center about how to balance work and treatments. They’re a valuable source of information when it comes to managing your schedule, as well as any potential health risks associated with working while on dialysis.
There are also programs specifically designed for individuals who are working while on dialysis, such as the National Kidney Foundation’s program called “Enhancing Life Through Employment” (ELTE). Through ELTE, you can find resources like job training and job search assistance, as well as support groups and counseling services.
These resources can make all the difference when it comes to managing work responsibilities and dialysis treatments, so don’t be afraid to reach out!
Conclusion
Reaching your work goals while on dialysis can seem daunting, but with these five tips, you can make it happen. First, be open with your boss and coworkers about your situation and what you need to maintain your treatment schedule. Second, make sure to take care of yourself and get the rest and nutrition you need. Third, set realistic goals and timelines for your work projects. Fourth, use your free time wisely to get ahead on your work. And finally, don’t be afraid to ask for help when you need it. With these tips, you can reach your work goals while on dialysis and maintain your treatment schedule.
#Nephrology Specialists in California#Best Nephrologist in California#covina#nearby nephrologist#pasadena#kidneytransplantation
0 notes
Text
Child Kidney Specialist in India
Child Kidney Specialist in India
Dr Sethi at Medanta, The Medicity is the leading Pediatric Nephrologist providing diagnostic and treatment services for children with conditions of the kidney, especially Nephrotic syndrome, Glomerular disorders, rare tubular disorders and Chronic Kidney disease. Our team is the leading dialysis and renal transplant service center for children.
Dr Sethi & team believes in personalized care that focuses on individual patient and family needs. Our team understands the challenges many of our families face when trying to access the care they need. Our caring goes beyond diagnostics and treatment. Our team is nationally recognized for their innovation, experience, dedication and expertise. We have the newest dialysis technology and provides comprehensive kidney transplant care to children of all ages.
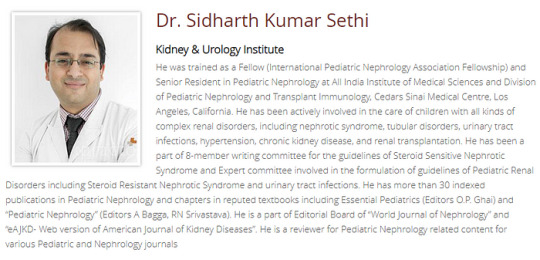
Dr. Sidharth Kumar Sethi
Kidney & Urology Institute
He was trained as a Fellow (International Pediatric Nephrology Association Fellowship) and Senior Resident in Pediatric Nephrology at All India Institute of Medical Sciences and Division of Pediatric Nephrology and Transplant Immunology, Cedars Sinai Medical Centre, Los Angeles, California. He has been actively involved in the care of children with all kinds of complex renal disorders, including nephrotic syndrome, tubular disorders, urinary tract infections, hypertension, chronic kidney disease, and renal transplantation. He has been a part of 8-member writing committee for the guidelines of Steroid Sensitive Nephrotic Syndrome and Expert committee involved in the formulation of guidelines of Pediatric Renal Disorders including Steroid Resistant Nephrotic Syndrome and urinary tract infections. He has more than 30 indexed publications in Pediatric Nephrology and chapters in reputed textbooks including Essential Pediatrics (Editors O.P. Ghai) and “Pediatric Nephrology” (Editors A Bagga, RN Srivastava). He is a part of Editorial Board of “World Journal of Nephrology” and “eAJKD- Web version of American Journal of Kidney Diseases”. He is a reviewer for Pediatric Nephrology related content for various Pediatric and Nephrology journals.
To schedule an appointment with Dr. Sidharth Sethi, please contact:
Name: Pediatric Nephrology India
Address: Division of Pediatric Nephrology, Kidney Institute, Medanta, The Medicity, Gurgaon, Haryana, India, 122001
Phone: 0124–4141414
Website: www.pediatricnephrologyindia.com
You can also search for these treatments
Pediatric Nephrology India, Best Pediatric Nephrologist In India, Best Pediatric Nephrologist In Gurgaon, Best Pediatric Nephrologist In Delhi, Child Kidney Specialist In Delhi, Child Kidney Specialist In Gurgaon, Child Kidney Specialist In India, Child Kidney Doctor In India, Child Kidney Doctor In Delhi, Child Kidney Doctor In Gurgaon, Pediatric Dialysis Specialist In India, Pediatric Dialysis Specialist In Delhi, Pediatric Kidney Transplant Specialist In Delhi, Nephrotic Syndrome Specialist In India, Nephrotic Syndrome Specialist In Delhi, Pediatric Nephrologist In Delhi, Best Pediatric Nephrology Doctor In India, Pediatric Kidney Doctor In India, Best Child Kidney Specialist In Delhi, Best Pediatric Nephrologist In Delhi, Best Paediatric Kidney Nephrologist In India, Best Child Kidney Doctor In India, Best Child Kidney Care In Delhi, Pediatric Nephrology,
#Pediatric Nephrology India#Best Pediatric Nephrologist In India#Best Pediatric Nephrologist In Gurgaon#Best Pediatric Nephrologist In Delhi#Child Kidney Specialist In Delhi#Child Kidney Specialist In Gurgaon#Child Kidney Specialist In India#Child Kidney Doctor In India#Child Kidney Doctor In Delhi#Child Kidney Doctor In Gurgaon#Pediatric Dialysis Specialist In India#Pediatric Dialysis Specialist In Delhi#Pediatric Kidney Transplant Specialist In Delhi#Nephrotic Syndrome Specialist In India#Nephrotic Syndrome Specialist In Delhi#Pediatric Nephrologist In Delhi#Best Pediatric Nephrology Doctor In India#Pediatric Kidney Doctor In India#Best Child Kidney Specialist In Delhi#Best Paediatric Kidney Nephrologist In India#Best Child Kidney Doctor In India#Best Child Kidney Care In Delhi#Pediatric Nephrology
1 note
·
View note
Text
Anti Factor H Antibodies in aHUS | Dr. Sidharth Kumar Sethi
Today our group has published a review on ‘Anti Factor H Antibodies in aHUS’ in ‘Frontiers in Immunology’ today. Antibodies to Factor H is the most common cause of aHUS in children in our country and we have published multiple research papers on this in last 2 decades.
Dr. Sidharth Kumar Sethi
Kidney & Urology Institute
He was trained as a Fellow (International Pediatric Nephrology Association Fellowship) and Senior Resident in Pediatric Nephrology at All India Institute of Medical Sciences and Division of Pediatric Nephrology and Transplant Immunology, Cedars Sinai Medical Centre, Los Angeles, California. He has been actively involved in the care of children with all kinds of complex renal disorders, including nephrotic syndrome, tubular disorders, urinary tract infections, hypertension, chronic kidney disease, and renal transplantation. He has been a part of 8-member writing committee for the guidelines of Steroid Sensitive Nephrotic Syndrome and Expert committee involved in the formulation of guidelines of Pediatric Renal Disorders including Steroid Resistant Nephrotic Syndrome and urinary tract infections. He has more than 30 indexed publications in Pediatric Nephrology and chapters in reputed textbooks including Essential Pediatrics (Editors O.P. Ghai) and “Pediatric Nephrology” (Editors A Bagga, RN Srivastava). He is a part of Editorial Board of “World Journal of Nephrology” and “eAJKD- Web version of American Journal of Kidney Diseases”. He is a reviewer for Pediatric Nephrology related content for various Pediatric and Nephrology journals.
TAG - Best Pediatric Nephrologist in India, Pediatric Dialysis Specialist in India, Nephrotic syndrome Specialist in India
0 notes
Text
How Doctors Are Using Artificial Intelligence to Battle Covid-19
https://sciencespies.com/nature/how-doctors-are-using-artificial-intelligence-to-battle-covid-19/
How Doctors Are Using Artificial Intelligence to Battle Covid-19
When the Covid-19 pandemic emerged last year, physician Lara Jehi and her colleagues at the Cleveland Clinic were running blind. Who was at risk? Who were the patients likely to get sicker? What kinds of care will they need?
“The questions were endless,” says Jehi, the clinic’s chief research information officer. “We didn’t have the luxury of time to wait and see what’s going to evolve over time.”
With answers urgently needed, the Cleveland Clinic turned to algorithms for help. The hospital assembled 17 of its specialists to define the data they needed to collect from electronic health records and used artificial intelligence to build a predictive treatment model. Within two weeks, the clinic created an algorithm based on data from 12,000 patients that used age, race, gender, socioeconomic status, vaccination history and current medications to predict whether someone would test positive for the novel coronavirus. Doctors used it early in the pandemic when tests were at a premium to advise patients whether they needed one.
Over the past year, the clinic published more than three dozen papers about using artificial intelligence. Jehi and her colleagues created models that identified those with the virus likely to need hospitalization which helped with capacity planning. They built another model that helped alert doctors to a patient’s risk for an intensive care unit and prioritized those at higher risk for aggressive treatment. And when patients were sent home and monitored there, the clinic’s software flagged which patients might need to return to the hospital.
Artificial intelligence had already been in use by hospitals, but the unknowns with Covid-19 and the volume cases created a frenzy of activity around the United States. Models sifted through data to help caregivers focus on patients most at-risk, sort threats to patient recovery and foresee spikes in facility needs for things like beds and ventilators. But with the speed also came questions about how to implement the new tools and whether the datasets used to build the models were sufficient and without bias.
At Mount Sinai Hospital in Manhattan, geneticist Ben Glicksberg and nephrologist Girish Nadkarni of the Hasso Plattner Institute for Digital Health and the Mount Sinai Clinical Intelligence Center, were asking the same questions as doctors at the Cleveland Clinic. “This was a completely new disease for which there was no playbook and there was no template,” Narkarni says. “We needed to aggregate data from different sources quickly to learn more about this.”
At Mount Sinai, with patients flooding the hospital during the spring epicenter of the outbreak in North America, researchers turned to data to assess patients’ risk for critical events at intervals of three, five and seven days after admission to anticipate their needs. Doctors decoded which patients were likely to return to the hospital and identified those who might be ready for discharge to free in-demand beds.
Nearly a year into looking to machine learning for help, Glicksberg and Narkani say it’s a tool, not an answer. Their work showed the models identified at-risk patients and uncovered underlying relationships in their health records that predicted outcomes. “We’re not saying we’ve cracked the code of using machine learning for Covid and can 100 percent reliably predict clinically-relevant events,” Glicksberg says.
“Machine learning is one part of the whole puzzle,” Nadkarni adds.
For Covid, artificial intelligence applications cover a broad range of issues from helping clinicians make treatment decisions to informing how resources are allocated. New York University’s Langone Health, for instance, created an artificial intelligence program to predict which patients can move to lower levels of care or recover at home to open up capacity.
Researchers at the University of Virginia Medical Center had been working on software to help doctors detect respiratory failure leading to intubation. When then pandemic hit, they adapted the software for Covid-19.
“It seemed to us when that all started happening, that this is what we had been working toward all these years. We didn’t anticipate a pandemic of this nature. But here it was,” says Randall Moorman, a professor of medicine with the university. “But it’s just the perfect application of the technology and an idea that we’ve been working on for a long time.”
The software, called CoMET, draws from a wide range of health measures including an EKG, laboratory test results and vital signs. It projects a comet shape onto a patient’s LCD screen that grows in size and changes color as their predicted risk increases, providing caregivers with a visual alarm, which stands out among the beeping alarms of a hospital unit. The software is in use at the University of Virginia hospital and is available to be licensed by other hospitals, Moorman says.
Jessica Keim-Malpass, Moorman’s research partner and a co-author of a paper about using predictive software in Covid treatment, says the focus was on making the model practical. “These algorithms have been proliferating, which is great, but there’s been far less attention placed on how to ethically use them,” she says. “Very few algorithms even make it to any kind of clinical setting.”
Translating what the software does into something easy for doctors, nurses and other caregivers to use is key. “Clinicians are bombarded with decisions every hour, sometimes every minute,” she says. “Sometimes they really are on the fence about what to do and oftentimes things might not be clinically apparent yet. So the point of the algorithm is to help the human make a better decision.”
While many models are in place in hospitals, there’s potential for more in the works. A number of applications have been developed, but have not yet rolled out. Researchers at the University of Minnesota have worked with Epic, the electronic health record vendor, to create an algorithm that assesses chest X-rays for Covid and takes seconds to find patterns associated with the virus. But it has not yet been approved by the Food and Drug Administration for use.
At Johns Hopkins University, biomedical engineers and heart specialists have developed an algorithm that warns doctors several hours before patients hospitalized with Covid-19 experience cardiac arrest or blood clots. In a preprint, researchers say it was trained and tested with data from more than 2,000 patients with the novel coronavirus. They are now developing the best way to set up the system in hospitals.
As hospitals look to integrate artificial intelligence into treatment protocols, some researchers worry the tools are being approved by the Food and Drug Administration before they have been deemed statistically valid. What requires FDA approval is fuzzy; models that require a health care worker to interpret the results don’t need to be cleared. Meanwhile, other researchers are also working to improve the software tools’ accuracy amid concerns they magnify racial and socioeconomic biases.
Researchers at the University of California in 2019 reported that an algorithm hospitals used to identify high-risk patients for medical attention showed that black patients with the same risk “score” were significantly sicker than white patients because of the data used to create the model. Because the pandemic disproportionately affects minorities, creating prediction models that do not account for their health disparities threatens to incorrectly assess their risk, for instance.
An August article in the Journal of the American Medical Informatics Association, researchers from Stanford University wrote that small data samples were not representative of overall patient populations and were biased against minorities. “There is hope that A.I. can help guide treatment decisions within this crisis; yet given the pervasiveness of biases, a failure to proactively develop comprehensive mitigation strategies during the COVID-19 pandemic risks exacerbating existing health disparities,” wrote the authors, including Tina Hernandez-Boussard, a professor at the Stanford University School of Medicine
The authors expressed concern that over-reliance on artificial intelligence—which appears objective, but is not—is being used for allocation of resources like ventilators and intensive care beds. ”These tools are built from biased data reflecting biased healthcare systems and are thus themselves also at high risk of bias—even if explicitly excluding sensitive attributes such as race or gender,” they added.
Glicksberg and Nadkarni, of Mount Sinai, acknowledge the importance of the bias issue. Their models drew from the Manhattan location with a diverse patient population from the Upper East Side and Harlem, but then were validated using information from other Mount Sinai hospitals in Queens and Brooklyn, hospitals with different patient populations that were used to make the models more robust. But the doctors acknowledge some underlying issues are not part of their data. “Social determinants of health, such as socioeconomic status, play an enormous role in almost everything health-related and these are not accurately captured or available in our data,” Glicksberg says. ”There is much more work to be done to determine how these models can be fairly and robustly embedded into practice without disrupting the system.”
Their most recent model predicts how Covid-19 patients will fare by examining electronic health records across multiple servers from five hospitals while protecting patient privacy. They found that model was more robust and a better predictor than those based on the individual hospitals. Since limited Covid-19 data is segregated across many institutions, the doctors called the new model “invaluable” in helping predict a patient’s outcome.
Jehi says the Cleveland Clinic database now has more than 160,000 patients with more than 400 data points per patient to validate its models. But the virus is mutating and the algorithms need to continue to chase the best possible treatment models.
“The issue isn’t that there isn’t enough data,” Jehi says. “The issue is that data has to be continuously reanalyzed and updated and revisited with these models for them to maintain their clinical value.”
#Nature
1 note
·
View note
Text
Results Of Kidney Transplantation In HIV-Infected Patients
Results Of Kidney Transplantation In HIV-Infected Patients.
A large, original think over provides more evidence that people infected with HIV, the virus that causes AIDS, do almost as well on the survival air as other patients when they undergo kidney transplants. Up until the mid-1990s, physicians tended to sidestep giving kidney transplants to HIV patients because of fear that AIDS would quickly kill them conceive. Since then, brand-new medications have greatly lengthened life spans for HIV patients, and surgeons routinely mount kidney transplants on them in some urban hospitals.
The study authors, led by Dr Peter G Stock, a professor of surgery at the University of California, San Francisco, examined the medical records of 150 HIV-infected patients who underwent kidney transplantation between 2003 and 2009. They dispatch their findings in the Nov malefine.icu. 18 stream of the New England Journal of Medicine.
The researchers found that about 95 percent of the displace patients lived for one year and about 88 percent lived for three years. Those survival rates be taken between those for kidney relocate patients in all-inclusive and those who are aged 65 and over. "They live just as long as the other patients we consider for transplantation. They're essentially the same as the balance of our patients," said transplant specialist Dr Silas P Norman, an helpmeet professor of internal medicine at the University of Michigan kya garvbati mahila ko jada oil khana chaiye. Norman was not part of the swatting team.
There was one troubling finding: the bodies of HIV patients were more likely to reject the kidneys than the bodies of other shift patients. It's likely that surgeons will need to better tailor their procedures to help foil organ rejection, said transplant surgeon Dr Dorry Segev. This should happen as surgeons income more experience with transplants in HIV patients an associate professor of surgery and epidemiology at Johns Hopkins Medical Institutions, who was social with the study findings.
Overall "treatment of HIV-infected patients undergoing kidney transplantation is audibly not straightforward, and this study has identified some challenges for the transplant community to address". On the promising side, transplant procedures didn't appear to have much of an impact on the HIV infections in the patients.
In years days beyond recall transplant surgeons worried about how the AIDS virus would interact with the medications given to remove patients that are designed to dampen the immune system. The concern was that "these patients are now doing well, and you're customary to give them medicine and undo all their benefits".
But it turns out that transplantation drugs have the opposite conclusion and often suppress the AIDS virus. This is because HIV revs up the immune system while the drugs revolve it down. Norman said he expects that the new findings will encourage more surgeons to perform kidney transplants on HIV patients, who are as often as not surviving long enough to develop diseases that typically butt older people. "There are still a lot of people in the community, including transplant professionals, nephrologists and contagious disease professionals, who still don't appreciate that many of these patients are good prospects for transplantation semenax best. They don't gain in value how many procedures have been done to date, and how we're getting overall very good outcomes".
2 notes
·
View notes
Text
Best Pediatric Nephrologist And Child Kidney Specialist in Delhi, Gurgaon, India - Dr. Sidharth Kumar Sethi
Dr. Sidharth Kumar Sethi
Kidney & Urology Institute
He was trained as a Fellow (International Pediatric Nephrology Association Fellowship) and Senior Resident in Pediatric Nephrology at All India Institute of Medical Sciences and Division of Pediatric Nephrology and Transplant Immunology, Cedars Sinai Medical Centre, Los Angeles, California. He has been actively involved in the care of children with all kinds of complex renal disorders, including nephrotic syndrome, tubular disorders, urinary tract infections, hypertension, chronic kidney disease, and renal transplantation. He has been a part of 8-member writing committee for the guidelines of Steroid Sensitive Nephrotic Syndrome and Expert committee involved in the formulation of guidelines of Pediatric Renal Disorders including Steroid Resistant Nephrotic Syndrome and urinary tract infections. He has more than 30 indexed publications in Pediatric Nephrology and chapters in reputed textbooks including Essential Pediatrics (Editors O.P. Ghai) and “Pediatric Nephrology” (Editors A Bagga, RN Srivastava). He is a part of Editorial Board of “World Journal of Nephrology” and “eAJKD- Web version of American Journal of Kidney Diseases”. He is a reviewer for Pediatric Nephrology related content for various Pediatric and Nephrology journals.
Tags - Best Pediatric Nephrologist in Delhi, Child Kidney Specialist in India,
Pediatric Dialysis Specialist in India
For more information link - www.pediatricnephrologyindia.com
#Best Pediatric Nephrologist in India#child kidney specialist in gurgaon#Pediatric Dialysis Specialist in India#Nephrotic syndrome Specialist in Delhi#Dr. Sidharth Kumar Sethi
1 note
·
View note
Text
Disparities in dialysis in children | Dr. Sidharth Kumar Sethi
Disparities In Dialysis In Children
HYPOTHESIS: Acute kidney injury (AKI) is a common cause of morbidity and mortality worldwide, with a pediatric incidence ranging from 19.3% to 24.1%. Treatment of pediatric AKI is a source of debate in varying geographical regions. Currently CRRT is the treatment for pediatric AKI, but limitations due to cost and accessibility force use of adult equipment and other therapeutic options such as peritoneal dialysis (PD) and hemodialysis (HD). It was hypothesized that more cost-effective measures would likely be used in developing countries due to lesser resource availability.
METHODS: A 26-question internet-based survey was distributed to 650 pediatric Nephrologists. There was a response rate of 34.3% (223 responses). The survey was distributed via pedneph and pcrrt email servers, inquiring about demographics, technology, resources, pediatric-specific supplies, and preference in renal replacement therapy (RRT) in pediatric AKI. The main method of analysis was to compare responses about treatments between nephrologists in developed countries and nephrologists in developing countries using difference-of-proportions tests.
RESULTS: PD was available in all centers surveyed, while HD was available in 85.1% and 54.1% (p = 0.00), CRRT was available in 60% and 33.3% (p = 0.001), and SLED was available in 20% and 25% (p = 0.45) centers of developed and developing world respectively. In developing countries, 68.5% (p = 0.000) of physicians preferred PD to costlier therapies, while in developed countries it was found that physicians favored HD (72%, p = 0.00) or CRRT (24%, p = 0.041) in infants.
CONCLUSIONS: Lack of availability of resources, trained physicians and funds often preclude standards of care in developing countries, and there is much development needed in terms of meeting higher global standards for treating pediatric AKI patients. PD remains the main modality of choice for treatment of AKI in infants in developing world.
About Dr.
Dr. Sidharth Kumar SethiKidney & Urology Institute
He was trained as a Fellow (International Pediatric Nephrology Association Fellowship) and Senior Resident in Pediatric Nephrology at All India Institute of Medical Sciences and Division of Pediatric Nephrology and Transplant Immunology, Cedars Sinai Medical Centre, Los Angeles, California. He has been actively involved in the care of children with all kinds of complex renal disorders, including nephrotic syndrome, tubular disorders, urinary tract infections, hypertension, chronic kidney disease, and renal transplantation. He has been a part of 8-member writing committee for the guidelines of Steroid Sensitive Nephrotic Syndrome and Expert committee involved in the formulation of guidelines of Pediatric Renal Disorders including Steroid Resistant Nephrotic Syndrome and urinary tract infections. He has more than 30 indexed publications in Pediatric Nephrology and chapters in reputed textbooks including Essential Pediatrics (Editors O.P. Ghai) and “Pediatric Nephrology” (Editors A Bagga, RN Srivastava). He is a part of Editorial Board of “World Journal of Nephrology” and “eAJKD- Web version of American Journal of Kidney Diseases”. He is a reviewer for Pediatric Nephrology related content for various Pediatric and Nephrology journals
Tags = Pediatric Dialysis Specialist in India, Pediatric Dialysis Specialist in delhi, Pediatric Nephrology India, Best Pediatric Nephrologist in Delhi
For more information = http://www.pediatricnephrologyindia.com/
See more blogs = https://child-kidney-specialist-in-delhi.blogspot.com/2022/06/what-is-nephrotic-syndrome-and-what.html
#Pediatric Dialysis Specialist in India#Pediatric Dialysis Specialist in delhi#Pediatric Nephrology India#Best Pediatric Nephrologist in Delhi
0 notes
Photo

LOS ANGELES, CA, UNITED STATES, August 26, 2019 /EINPresswire.com/ -- Zahra Tabassian, acclaimed doctor and author of “Dance to the Music of Your Soul,” wins Best of Los Angeles Award- “Best New Health Book- 2019”, according to Aurora DeRose, award coordinator for the Best of Los Angeles Award community.
The “Best of Los Angeles Award” community was formed four years ago and consists of over 5,400 professional members living and working in Southern California. It celebrates the best people, places and things in Los Angeles with a slogan “No Ads. No B.S. Only the Best.”
“The mission of the community is to celebrate the best of Los Angeles, and allow its community members to connect with other members who share the highest standards of quality and integrity,” expresses DeRose. "We're honored to include Zahra Tabassian into our BoLAA family."
A woman of many talents, Dr. Tabassian is a double-board certified internist and nephrologist (kidney and dialysis specialist). Her practice welcomes all aspects of medical diseases, but because kidney disease and dialysis dependency are strongly associated with diabetes and hypertension, a large number of her patients suffer from diabetes and hypertension as well. Her practice also serves patients who unfortunately suffer from multiple complications of diabetes and kidney failure, such as cardiovascular disease, i.e., heart failure and strokes.
Tabassian’s medical practice utilizes Dance Away CKD (chronic kidney disease) Therapy to prevent progression of kidney disease and to enhance promotion of its reversal. CKD has affected almost 50 million Americans and is found to be the fastest growing non-communicable disease in the United States between 20 to 56 years of age. Dr. Tabassian’s medical practice also utilizes Dance Away Diabetes Therapy to prevent and reverse diabetes. Implementing Dance Away Disease Therapy protocols and elevating the individual’s BEE (bioelectromagnetic energy), Dr. Tabassian takes care of the root cause of chronic diseases that have afflicted hundreds of millions of people in this country, called silent inflammation.
Her mission is to help her many patients lose weight, become motivated and make healthy choices. Dr. Tabassian believes, “with God in us and our patients all things become possible.”
Learn more by attending her monthly free health event every first Saturday at 1 pm. Please RSVP, phone: 310-671-2420.www.drtabassian.comAurora DeRose
Michael Levine Media
+1 310-396-6090
0 notes
Text
California Kidney Specialists: The Epitome of Nephrology Excellence in California

When it comes to the best nephrologists in California, one name stands out: California Kidney Specialists. Renowned for their exceptional care and expertise in kidney-related disorders, this esteemed group of physicians is dedicated to providing top-notch healthcare to their patients. Led by Dr. John Smith, a distinguished expert in chronic kidney disease, California Kidney Specialists boasts a team of exceptional professionals. Dr. Emily Johnson's unparalleled proficiency in kidney transplantation and Dr. Michael Davis's pioneering work in pediatric nephrology further solidify their position as leaders in the field. With California Kidney Specialists, you can trust that your kidney health is in the most capable hands.
0 notes
Text
Child Kidney Specialist in Delhi
Child Kidney Specialist in Delhi
Dr Sethi at Medanta, The Medicity is the leading Pediatric Nephrologist providing diagnostic and treatment services for children with conditions of the kidney, especially Nephrotic syndrome, Glomerular disorders, rare tubular disorders and Chronic Kidney disease. Our team is the leading dialysis and renal transplant service center for children.
Dr Sethi & team believes in personalized care that focuses on individual patient and family needs. Our team understands the challenges many of our families face when trying to access the care they need. Our caring goes beyond diagnostics and treatment. Our team is nationally recognized for their innovation, experience, dedication and expertise. We have the newest dialysis technology and provides comprehensive kidney transplant care to children of all ages.
He was trained as a Fellow (International Pediatric Nephrology Association Fellowship) and Senior Resident in Pediatric Nephrology at All India Institute of Medical Sciences and Division of Pediatric Nephrology and Transplant Immunology, Cedars Sinai Medical Centre, Los Angeles, California. He has been actively involved in the care of children with all kinds of complex renal disorders, including nephrotic syndrome, tubular disorders, urinary tract infections, hypertension, chronic kidney disease, and renal transplantation.
He has been a part of 8-member writing committee for the guidelines of Steroid Sensitive Nephrotic Syndrome and Expert committee involved in the formulation of guidelines of Pediatric Renal Disorders including Steroid Resistant Nephrotic Syndrome and urinary tract infections. He has more than 30 indexed publications in Pediatric Nephrology and chapters in reputed textbooks including Essential Pediatrics (Editors O.P. Ghai) and “Pediatric Nephrology” (Editors A Bagga, RN Srivastava). He is a part of Editorial Board of “World Journal of Nephrology” and “eAJKD- Web version of American Journal of Kidney Diseases”. He is a reviewer for Pediatric Nephrology related content for various Pediatric and Nephrology journals.
To schedule an appointment with Dr. Sidharth Sethi, please contact:
Name: Pediatric Nephrology India
Address: Division of Pediatric Nephrology, Kidney Institute, Medanta, The Medicity, Gurgaon, Haryana, India, 122001
Phone: 0124–4141414
Website: www.pediatricnephrologyindia.com
You can also search for these treatments
Pediatric Nephrology India, Best Pediatric Nephrologist In India, Best Pediatric Nephrologist In Gurgaon, Best Pediatric Nephrologist In Delhi, Child Kidney Specialist In Delhi, Child Kidney Specialist In Gurgaon, Child Kidney Specialist In India, Child Kidney Doctor In India, Child Kidney Doctor In Delhi, Child Kidney Doctor In Gurgaon, Pediatric Dialysis Specialist In India, Pediatric Dialysis Specialist In Delhi, Pediatric Kidney Transplant Specialist In Delhi, Nephrotic Syndrome Specialist In India, Nephrotic Syndrome Specialist In Delhi, Pediatric Nephrologist In Delhi, Best Pediatric Nephrology Doctor In India, Pediatric Kidney Doctor In India, Best Child Kidney Specialist In Delhi, Best Pediatric Nephrologist In Delhi, Best Paediatric Kidney Nephrologist In India, Best Child Kidney Doctor In India, Best Child Kidney Care In Delhi, Pediatric Nephrology,
#Pediatric Nephrology India#Best Pediatric Nephrologist In India#Best Pediatric Nephrologist In Gurgaon#Best Pediatric Nephrologist In Delhi#Child Kidney Specialist In Delhi#Child Kidney Specialist In Gurgaon#Child Kidney Specialist In India#Child Kidney Doctor In India#Child Kidney Doctor In Delhi#Child Kidney Doctor In Gurgaon#Pediatric Dialysis Specialist In India#Pediatric Dialysis Specialist In Delhi#Pediatric Kidney Transplant Specialist In Delhi#Nephrotic Syndrome Specialist In India#Nephrotic Syndrome Specialist In Delhi#Pediatric Nephrologist In Delhi#Best Pediatric Nephrology Doctor In India#Pediatric Kidney Doctor In India#Best Child Kidney Specialist In Delhi#Best Paediatric Kidney Nephrologist In India#Best Child Kidney Doctor In India#Best Child Kidney Care In Delhi#Pediatric Nephrology
1 note
·
View note
Text
Best Pediatric Nephrologist in India - Dr. Sidharth Kumar Sethi
He was trained as a Fellow (International Pediatric Nephrology Association Fellowship) and Senior Resident in Pediatric Nephrology at All India Institute of Medical Sciences and Division of Pediatric Nephrology and Transplant Immunology, Cedars Sinai Medical Centre, Los Angeles, California. He has been actively involved in the care of children with all kinds of complex renal disorders, including nephrotic syndrome, tubular disorders, urinary tract infections, hypertension, chronic kidney disease, and renal transplantation.
He has been a part of 8-member writing committee for the guidelines of Steroid Sensitive Nephrotic Syndrome and Expert committee involved in the formulation of guidelines of Pediatric Renal Disorders including Steroid Resistant Nephrotic Syndrome and urinary tract infections.
He has more than 30 indexed publications in Pediatric Nephrology and chapters in reputed textbooks including Essential Pediatrics (Editors O.P. Ghai) and “Pediatric Nephrology” (Editors A Bagga, RN Srivastava). He is a part of Editorial Board of “World Journal of Nephrology” and “eAJKD- Web version of American Journal of Kidney Diseases”. He is a reviewer for Pediatric Nephrology related content for various Pediatric and Nephrology journals.
TAG- Best Pediatric Nephrologist in India, Child Kidney Specialist in India, Nephrotic syndrome Specialist in Delhi, Pediatric Dialysis Specialist in India
#Best Pediatric Nephrologist in India#Child Kidney Specialist in India#Pediatric Dialysis specialist in India#Nephrotic Syndrome Specialist in Delhi
0 notes
Text
Kidney Experts Say It’s Time to Remove Race From Medical Algorithms. Doing So Is Complicated.
Alphonso Harried recently came across a newspaper clipping about his grandfather receiving his 1,000th dialysis treatment. His grandfather later died — at a dialysis center — as did his uncle, both from kidney disease.
“And that comes in my mind, on my weak days: ‘Are you going to pass away just like they did?’” said Harried, 46, who also has the disease.
He doesn’t like to dwell on that. He has gigs to play as a musician, a ministry to run with his wife and kids to protect as a school security guard.
Yet he must juggle all that around three trips each week to a dialysis center in Alton, Illinois, about 20 miles from his home in St. Louis, to clean his blood of the impurities his kidneys can no longer flush out. He’s waiting for a transplant, just as his uncle did before him.
“It’s just frustrating,” Harried said. “I’m stuck in the same pattern.”
Thousands of other Americans with failing kidneys are also stuck, going to dialysis as they await new kidneys that may never come. That’s especially true of Black patients, like Harried, who are about four times as likely to have kidney failure as white Americans, and who make up more than 35% of people on dialysis but just 13% of the U.S. population. They’re also less likely to get on the waitlist for a kidney transplant, and less likely to receive a transplant once on the list.
An algorithm doctors use may help perpetuate such disparities. It uses race as a factor in evaluating all stages of kidney disease care: diagnosis, dialysis and transplantation.
It’s a simple metric that uses a blood test, plus the patient’s age and sex and whether they’re Black. It makes Black patients appear to have healthier kidneys than non-Black patients, even when their blood measurements are identical.
“It is as close to stereotyping a particular group of people as it can be,” said Dr. Rajnish Mehrotra, a nephrologist with the University of Washington School of Medicine.

This race coefficient has recently come under fire for being imprecise, leading to potentially worse outcomes for Black patients and less chance of receiving a new kidney. A national task force of kidney experts and patients is studying how to replace it. Some institutions have already stopped using it.
But how best to assess a patient’s kidney function remains uncertain, and some medical experts say fixing this equation is only one step in creating more equitable care, a process complicated by factors far deeper than a math problem.
“There are so many inequities in kidney disease that stem from broader structural racism,” said Dr. Deidra Crews, a nephrologist and the associate director for research development at the Johns Hopkins Center for Health Equity. “It is just a sliver of what the broader set of issues are when it comes to both disparities and inequities in who gets kidney disease in the first place, and then in the care processes.”
Why Race Has Been Part of the Equation
Kidneys filter about 40 gallons of blood a day, like a Brita filter for the body. They keep in the good stuff and send out the bad through urine. But unlike other organs, kidneys don’t easily repair themselves.
“There’s a point of no return,” said Dr. Cynthia Delgado, a University of California-San Francisco nephrologist who is leading the task force working on the national recommendation to ditch the racial part of the equation.
Furthermore, it’s hard to gauge whether kidneys are working properly. Gold-standard tests involve a chemical infusion and hours of collecting blood and urine to see how quickly the kidneys flush the chemical out. An algorithm is much more efficient.
Buoyed by activism around structural racism, those seeking equity in health care have recently been calling out the algorithm as an example of the racism baked into American medicine. Researchers writing in the New England Journal of Medicine last year included kidney equations in a laundry list of race-adjusted algorithms used to evaluate parts of the body — from heart and lungs to bones and breasts. Such equations, they wrote, can “perpetuate or even amplify race-based health inequities.”
In March, ahead of the national task force’s upcoming formal recommendation, leaders in kidney care said race modifiers should be removed. And Fresenius Medical Care, one of the two largest U.S. dialysis companies, said the race component is “problematic.”
Until the late 1990s, doctors primarily used the Cockcroft-Gault equation. It didn’t ask for race, but used age, weight and the blood level of creatinine — a chemical that’s basically the trash left after muscles move. A high level of creatinine in the blood signals that kidneys are not doing their job of disposing of it. But the equation was based on a study of just 249 white men.
Then, researchers wrapping up a study on how to slow down kidney disease realized they were sitting on a mother lode of data that could rewrite that equation: gold-standard kidney function measurements from about 1,600 patients, 12% of whom were Black. They evaluated 16 variables, including age, sex, diabetes diagnosis and blood pressure.
They landed on something that accurately predicted the kidney function of patients better than the old equation. Except it made the kidneys of Black participants appear to be sicker than the gold-standard test showed they were.
The authors reasoned it might be caused by muscle mass. Participants with more muscle mass would likely have more creatinine in their blood, not because their kidneys were failing to remove it, but because they just had more muscles producing more waste. So they “corrected” Black patients’ results for that difference.
Dr. Andrew S. Levey, a professor at Tufts University School of Medicine who led the study, said it doesn’t make intuitive sense to include race — now widely considered a social construct — in an equation about biology.
Still, in 1999, he and others published the race equation, then updated it a decade later. Though other equations exist that don’t involve race, Levey’s latest version, often referred to as the “CKD-EPI” equation, is recommended for clinical use. It shows a Black patient’s kidneys functioning 16% better than those of a non-Black patient with the same blood work.
Removing the Race Number
Many patients don’t know about this equation and how their race has factored into their care.
“I really wish someone would have mentioned it,” Harried said.
He said it burned him up “knowing that this one little test that I didn’t know anything about could keep me from — or prolong me — getting a kidney.”

Glenda V. Roberts curbed her kidney disease with a vegan diet and by conducting meetings as an IT executive while walking. But after more than 40 years of slow decline, her kidney function finally reached the cutoff required to get on the transplant waitlist. When it did, the decline was swift — a pattern researchers have noted in Black patients. “It really makes you wonder what the benefit is of having an equation that will cause people who look like me — Black people — to get referrals later, to have to wait longer before you can get on the transplant list, but then have your disease progress more rapidly,” she said.
Roberts, who is now the director of external relations at the University of Washington’s Kidney Research Institute in Seattle and on the national task force, said a genetic test added to her feeling that a “Black/non-Black” option in an equation was a charade.
“In fact, I am not predominantly of African ancestry. I’m 25% Native American. I’m Swedish and English and French,” said Roberts. “But I am also 48% from countries that are on the continent of Africa.”
The Black/non-Black question also doesn’t make sense to Delgado, the University of California nephrologist. “I would probably for some people qualify as being non-Black,” said Delgado, who is Puerto Rican. “But for others, I would qualify as Black.”
So, theoretically, if Delgado were to visit two doctors on the same day, and they guessed her race instead of asking, she could come away with two different readings of how well her kidneys are working.
Researchers found that the race factor doesn’t work for Black Europeans or patients in West Africa. Australian researchers found using the race coefficient led them to overestimate the kidney function of Indigenous Australians.
But in the U.S., Levey and other researchers seeking to replace the race option with physical measurements, such as height and weight, hit a dead end.
To Crews, the Johns Hopkins nephrologist who is also on the national taskforce, the focus on one equation is myopic. The algorithm suggests that something about Black people’s bodies affects their kidneys. Crews thinks that’s the wrong approach to addressing disparities: The issue is not what’s unique about the inner workings of Black bodies, but instead what’s going on around them.
“I really wish we could measure that instead of using race as a variable in the estimating equations,” she said on the “Freely Filtered” podcast. “I don’t think it’s ancestry. I don’t think it’s muscle mass.”
It might not be that Black bodies are more likely to have more creatinine in the blood, but that Americans who experience housing insecurity and barriers to healthy food, quality medical care and timely referrals are more likely to have creatinine in their blood — and that many of them happen to be Black.
Systemic health disparities help explain why Black patients have unusually high rates of kidney failure, since communities of color have less access to regular primary care. One of the most serious consequences of poorly controlled diabetes and hypertension is failure of the organ.

Direct discrimination — intentional or not — from providers may also affect outcomes, said Roberts. She recalled a social worker categorizing her as unable to afford the post-transplant drugs required to keep a transplanted organ healthy, which could have delayed her getting a new organ. Roberts has held executive roles at several multimillion-dollar companies.
Delgado and Levey agree that removing race from the formula might feel better on the surface, but it isn’t clear the move would actually help people.
Studies recently published in the Journal of the American Medical Association and the Journal of the American Society of Nephrology noted that removing the race factor could lead to some Black patients being disqualified from using beneficial medications because their kidneys might appear unable to handle them. It could also disqualify some Black people from donating a kidney.
“Fiddling with the algorithms is an imperfect way to achieve equity,” Levey said.
As researchers debate the math problem and broader societal ones, patients such as Harried, the St. Louis minister and security guard, are still stuck navigating dialysis.
“One of things that keeps me going is knowing that soon they may call me for a kidney,” Harried said.
He doesn’t know how long his name will be on the transplant waitlist — or whether the race coefficient has prolonged the wait — but he keeps a hospital bag under his bed to be ready.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
USE OUR CONTENT
This story can be republished for free (details).
Kidney Experts Say It’s Time to Remove Race From Medical Algorithms. Doing So Is Complicated. published first on https://nootropicspowdersupplier.tumblr.com/
0 notes
Video
youtube
List of the top 10 Keto diet specialist you need to follow to get results. Ketogenic diet is a high-fat, adequate-protein, low-carbohydrate diet. Follow YouTubers like Thomas DeLauer on to get results. ➡️ SUBSCRIBE to BabbleTop! https://www.youtube.com/channel/UCX--mGSg0UwDjl7MDL8H5Jg?sub_confirmation=1 One of the big diets of the moment is the Ketogenic or Keto diet. Although not a new idea, the Keto diet is an ultra-low carb-high-fat diet that doctors have been using for decades to treat medical issues. Now everyone wants to try it... but if we really want it to work, then it's best to seek the advice of a specialist. Here are our Top 10 Keto Diet Specialists You Need To Follow To Get Results. The ketogenic diet (or keto diet, for short) is a low-carb, high-fat diet that offers many health benefits. The keto diet is a low-carb, high-fat diet. It lowers blood sugar and insulin levels, and shifts the body’s metabolism away from carbs and towards fat and ketones. If you enjoyed this video list of the top 10 ketogenic diet specialist you need to follow to get results. Comment: #keto #ketogenic #ketodiet TIMESTAMPS: 0:00 Keto Diet Specialist You Need To Follow To Get Results 0:32 Dr. Andreas Eenfeldt 1:41 Dr. Carol Loffelmann 3:09 Dr. Ken Berry 4:38 Dr. Eric Berg 5:59 Mike Mutzel - High-Intensity Health 7:17 Dr. Fit And Fabulous 8:34 Dr. Ryan Lowery 10:03 Dr. Don D'Agostino 11:25 Dr. Jason Fung 12:32 Thomas DeLauer (@Thomas DeLauer) SUMMARIES: - If you are a complete novice when it comes to this low carb - high-fat diet but want to give it a try, one of your first stops should be to check out the work of Dr. Andreas Eenfeldt. - After having her second child, Dr. Loffelmann struggled to lose the weight. First trying traditional diets and exercise, Dr. Loffelmann was still struggling. - If you're looking for the facts about the Keto diet and what it can do, then Dr. Ken Berry is the specialist for you. His Youtube channel, which also has many videos on a wide range of medical issues, diets, and the key to a healthy life, is hugely popular and easy to follow for everyone. - Dr. Berg is a chiropractor who specializes in 'Health Ketosis', which is the process of the body not having carbs to burn for energy, so it burns fats instead. - Don't think that Mike Mutzel is some kind of life coach or guru, because he is much more than that. - Dr. Jamie Seeman, the real name of Dr. Fit and Fabulous, is an obstetrician and gynecologist from Omaha, Nebraska. - One of the Ketogenic Bible's authors is the highly respected Dr. Ryan Lowery. - If you are one of those people that are looking towards the Keto diet as more than just a diet but also as a treatment, then Dr. Don D'Agostino's research could well be a lifeline. - Dr. Fung is a Canadian nephrologist and a world-leading expert in the field of intermittent fasting and low carb diets, especially in their relation to diabetes. - An elite performance coach from California, Thomas DeLauer may not exactly fit in on a list of Doctor's and scientists, but he is his own "guinea pig" and tests on himself to get real life results to share with you all. 📺 Thomas DeLauer https://www.youtube.com/channel/UC70SrI3VkT1MXALRtf0pcHg?sub_confirmation=1 ➡️ SUBSCRIBE to BabbleTop! https://www.youtube.com/channel/UCX--mGSg0UwDjl7MDL8H5Jg?sub_confirmation=1 🥳 JOIN and become a BabbleTop member! https://www.youtube.com/babbletop/join 👕 Check out our MERCH! https://ift.tt/2xcFumO 🔥 Our Most Popular VIDEOS! https://www.youtube.com/watch?v=uOvb3ZRIwh0&list=UUX--mGSg0UwDjl7MDL8H5Jg All clips used for fair use commentary, criticism, and educational purposes. See Hosseinzadeh v. Klein, 276 F.Supp.3d 34 (S.D.N.Y. 2017); Equals Three, LLC v. Jukin Media, Inc., 139 F. Supp. 3d 1094 (C.D. Cal. 2015).
0 notes
Text
Cerebral venous sinus thrombosis in pediatric nephrotic syndrome | Dr. Sidharth Kumar Sethi
Cerebral Venous Sinus Thrombosis In Pediatric Nephrotic Syndrome
A 2-year-old girl presented to the emergency room with recurrent seizures. The child had been diagnosed with nephrotic syndrome in the previous 2 weeks (serum albumin, 1.5 g/dl; serum creatinine, 0.4 mg/dl) and had been convulsing on and off since the week before presentation. Oral prednisolone (2 mg/kg per day) had been started for 2 weeks with no response. There was no metabolic cause of seizures with normal serum ammonia, blood gas, and serum electrolyte levels.
About Dr.
Dr. Sidharth Kumar SethiKidney & Urology Institute
He was trained as a Fellow (International Pediatric Nephrology Association Fellowship) and Senior Resident in Pediatric Nephrology at All India Institute of Medical Sciences and Division of Pediatric Nephrology and Transplant Immunology, Cedars Sinai Medical Centre, Los Angeles, California. He has been actively involved in the care of children with all kinds of complex renal disorders, including nephrotic syndrome, tubular disorders, urinary tract infections, hypertension, chronic kidney disease, and renal transplantation. He has been a part of 8-member writing committee for the guidelines of Steroid Sensitive Nephrotic Syndrome and Expert committee involved in the formulation of guidelines of Pediatric Renal Disorders including Steroid Resistant Nephrotic Syndrome and urinary tract infections. He has more than 30 indexed publications in Pediatric Nephrology and chapters in reputed textbooks including Essential Pediatrics (Editors O.P. Ghai) and “Pediatric Nephrology” (Editors A Bagga, RN Srivastava). He is a part of Editorial Board of “World Journal of Nephrology” and “eAJKD- Web version of American Journal of Kidney Diseases”. He is a reviewer for Pediatric Nephrology related content for various Pediatric and Nephrology journals.
Tag = Nephrotic syndrome Specialist in Delhi, Best Pediatric Nephrologist in Delhi, Pediatric Nephrology India
For more information = http://www.pediatricnephrologyindia.com/
#Nephrotic syndrome Specialist in Delhi#Best Pediatric Nephrologist in Delhi#Pediatric Nephrology India
0 notes
Text
Kaveh Sharif, MD, is an Outstanding Internist and Nephrologist with a Private Practice in Beverly Hills, California
Kaveh Sharif, MD, is a well-versed internist and nephrologist who sees patients at his own private practice located in Beverly Hills, California. In practice since 1996, he opened his private office in 2005 and specializes in the care of kidney disease, kidney transplant, hemodialysis and peritoneal dialysis, hypertension care, and diabetes mellitus. Dr. Sharif offers compassionate care of people with chronic kidney disease and people with end stage renal disease on dialysis. “I am advocate of home modalities for dialysis such as peritoneal dialysis and home hemodialysis and longer dialysis modalities such as nocturnal hemodialysis”, he adds. Featuring an impressive professional journey spanning two decades, Dr. Sharif can be found exercising his hospital privileges at Cedars-Sinai Medical Center in Los Angeles, California. Furthermore, he serves as Assistant Clinical Professor of Medicine at David Geffen School of Medicine, the school of medicine of The University of California, Los Angeles, in Los Angeles, California. He joined UCLA in 2015 and teaches in the nephrology fellowship program at Cedars-Sinai Medical Center. In addition to English, he speaks Farsi and French, which allows him to see a wider spectrum of patients. For more information about Kaveh Sharif, MD, please visit https://find-a-doctor.cedars-sinai.edu/provider/1366465825-kaveh-sharif.
Kaveh Sharif, MD, attended Université Catholique de Louvain in Belgium and was awarded his medical degree in 1988. Upon relocating to the United States, he went to The Ohio State University College of Medicine in Columbus, Ohio, and completed his internal medicine residency in 1993, followed by his nephrology fellowship at the University of Michigan Medical School in Ann Arbor, Michigan, in 1996. Dr. Sharif received board certification in internal medicine and nephrology from the American Board of Internal Medicine and maintains a professional membership with the American Society of Nephrology. He sees his success as an attribute of his hard work and perseverance and his hobbies include running, reading, jogging, and hiking. “My European medical school training and American specialty and subspecialty training as well as working in an underserved area in Wisconsin has given me a global view of medicine. I love diagnostic challenges and medical puzzles and I do my best to solve them”, states Dr. Sharif. For more information about Kaveh Sharif, MD, please visit https://www.findatopdoc.com/doctor/Kaveh-Sharif-Internist-Los-Angeles-California-90067.
0 notes
Text
Spurred By Convenience, Millennials Often Spurn The ‘Family Doctor’ Model
While this article focuses on Millennnials, the trend has been seen at all age groups. The emergence and availability of urgent care centers has made going to the doctor, especially the primary care doctor, almost an antiquated concept. There are a number of reasons that this is not a great trend - from urgent cares delivering primary care at a higher cost than a doctor to not having a quarterback overseeing your care - and is worth bucking if at all possible.
Spurred By Convenience, Millennials Often Spurn The ‘Family Doctor’ Model
by SandrG. Boodman
Calvin Brown doesn’t have a primary care doctor — and the peripatetic 23-year-old doesn’t want one.
Since his graduation last year from the University of San Diego, Brown has held a series of jobs that have taken him to several California cities. “As a young person in a nomadic state,” Brown said, he prefers finding a walk-in clinic on the rare occasions when he’s sick.
“The whole ‘going to the doctor’ phenomenon is something that’s fading away from our generation,” said Brown, who now lives in Daly City outside San Francisco. “It means getting in a car [and] going to a waiting room.” In his view, urgent care, which costs him about $40 per visit, is more convenient — “like speed dating. Services are rendered in a quick manner.”
Brown’s views appear to be shared by many millennials, the 83 million Americans born between 1981 and 1996 who constitute the nation’s biggest generation. Their preferences — for convenience, fast service, connectivity and price transparency — are upending the time-honored model of office-based primary care.
Many young adults are turning to a fast-growing constellation of alternatives: retail clinics carved out of drugstores or big-box retail outlets, free-standing urgent care centers that tout evening and weekend hours, and online telemedicine sites that offer virtual visits without having to leave home. Unlike doctors’ offices, where charges are often opaque and disclosed only after services are rendered, many clinics and telemedicine sites post their prices.
EMAIL SIGN-UP
Subscribe to KHN’s free Morning Briefing.
SIGN UP
A national poll of 1,200 randomly selected adults conducted in July by the Kaiser Family Foundation for this story found that 26 percent said they did not have a primary care provider. There was a pronounced difference among age groups: 45 percent of 18- to 29-year-olds had no primary care provider, compared with 28 percent of those 30 to 49, 18 percent of those 50 to 64 and 12 percent age 65 and older. (Kaiser Health News is an editorially independent program of the foundation.)
A 2017 survey by the Employee Benefit Research Institute, a Washington think tank, and Greenwald and Associates yielded similar results: 33 percent of millennials did not have a regular doctor, compared with 15 percent of those age 50 to 64.
“There is a generational shift,” said Dr. Ateev Mehrotra, an internist and associate professor in the Department of Health Care Policy at Harvard Medical School. “These trends are more evident among millennials, but not unique to them. I think people’s expectations have changed. Convenience [is prized] in almost every aspect of our lives,” from shopping to online banking.
So is speed. Younger patients, Mehrotra noted, are unwilling to wait a few days to see a doctor for an acute problem, a situation that used to be routine. “Now,” Mehrotra said, “people say, ‘That’s crazy, why would I wait that long?'”
Until recently, the after-hours alternative to a doctor’s office for treatment of a strep throat or other acute problem was a hospital emergency room, which usually meant a long wait and a big bill.
Luring Millennials
For decades, primary care physicians have been the doctors with whom patients had the closest relationship, a bond that can last years. An internist, family physician, geriatrician or general practitioner traditionally served as a trusted adviser who coordinated care, ordered tests, helped sort out treatment options and made referrals to specialists.
But some experts warn that moving away from a one-on-one relationship may be driving up costs and worsening the problem of fragmented or unnecessary care, including the misuse of antibiotics.
A recent report in JAMA Internal Medicine found that nearly half of patients who sought treatment at an urgent care clinic for a cold, the flu or a similar respiratory ailment left with an unnecessary and potentially harmful prescription for antibiotics, compared with 17 percent of those seen in a doctor’s office. Antibiotics are useless against viruses and may expose patients to severe side effects with just a single dose.
“I’ve seen many people who go to five different places to be treated for a UTI [urinary tract infection] who don’t have a UTI,” said Dr. Janis Orlowski, a nephrologist who is chief health care officer at the Association of American Medical Colleges, or AAMC. “That’s where I see the problem of not having some kind of continuous care.”
“We all need care that is coordinated and longitudinal,” said Dr. Michael Munger, president of the American Academy of Family Physicians, who practices in Overland Park, Kan. “Regardless of how healthy you are, you need someone who knows you.” The best time to find that person, Munger and others say, is before a health crisis, not during one.
And that may mean waiting weeks. A 2017 survey by physician search firm Merritt Hawkins found that the average wait time for a new-patient appointment with a primary care doctor in 15 large metropolitan areas is 24 days, up from 18.5 days in 2014.
While wait times for new patients may reflect a shortage of primary care physicians — in the view of the AAMC — or a maldistribution of doctors, as other experts argue, there is no dispute that primary care alternatives have exploded. There are now more than 2,700 retail clinics in the United States, most in the South and Midwest, according to Rand Corp. researchers.
Connecting With Care
To attract and retain patients, especially young adults, primary care practices are embracing new ways of doing business.
Many are hiring additional physicians and nurse practitioners to see patients more quickly. They have rolled out patient portals and other digital tools that enable people to communicate with their doctors and make appointments via their smartphones. Some are exploring the use of video visits.
Mott Blair, a family physician in Wallace, N.C., a rural community 35 miles north of Wilmington, said he and his partners have made changes to accommodate millennials, who make up a third of their practice.
“We do far more messaging and interaction through electronic interface,” he said. “I think millennials expect that kind of connectivity.” Blair said his practice has also added same-day appointments.
Although walk-in clinics may be fine as an option for some illnesses, few are equipped to provide holistic care, offer knowledgeable referrals to specialists or help patients decide whether they really need, say, knee surgery, he noted. Primary care doctors “treat the whole patient. We’re tracking things like: Did you get your mammogram? Flu shot? Pap smear? Eye exam?”
Dr. Nitin Damle, an internist and past president of the American College of Physicians, said that young people develop diabetes, hypertension and other problems “that require more than one visit.”
“We know who the best and most appropriate specialists in the area are,” said Damle, an associate clinical professor of medicine at Brown University in Providence, R.I. “We know who to go to for asthma, allergies, inflammatory bowel disease.”
Marquenttha Purvis, 38, said her primary care doctor was instrumental in helping arrange treatment for her stage 2 breast cancer last year. “It was important because I wouldn’t have been able to get the care I needed” without him, said Purvis, who lives in Richmond, Va.
Sometimes the fragmented care that can result from not having a doctor has serious consequences.
Orlowski cites the case of a relative, a 40-year-old corporate executive with excellent medical insurance. The man had always been healthy and didn’t think he needed a primary care physician.
“Between treating himself and then going to outpatient clinics,” he spent nearly a year battling a sore throat that turned out to be advanced throat cancer, she said.
For patients without symptoms or a chronic condition such as asthma or high blood pressure, a yearly visit to a primary care doctor may not be necessary. Experts no longer recommend the once-sacrosanct annual physical for people of all ages.
“Not all access has to be with you sitting on an exam table,” Munger said. “And I may not need to see you more than every three years. But I should be that first point of contact.”
Convenience Is Paramount
Caitlin Jozefcyk, 30, a high school history teacher in Sparta, N.J., uses urgent care when she’s sick. She dumped her primary care doctor seven years ago because “getting an appointment was so difficult” and he routinely ran 45 minutes behind schedule. During her recent pregnancy, she saw her obstetrician.
Jozefcyk knows she’s not building a relationship with a physician — she sees different doctors at the center — but “really likes the convenience” and extended hours.
Digital access is also important to her. “I can make appointments directly through an app, and prescriptions are sent directly to the pharmacy,” she said.
After years of going to an urgent care center or, when necessary, an emergency room, Jessica Luoma, a 29-year-old stay-at-home mother in San Francisco, recently decided to find a primary care doctor.
“I’m very healthy, very active,” said Luoma, who has been treated for a kidney infection and a miscarriage.
Luoma said her husband pushed her to find a doctor after the insurance offered by his new employer kicked in.
“He’s a little more ‘safety first’ than me,” she said. “I figured, ‘Why not?’ — just in case.”
0 notes