#Dr. Amod Manocha
Text

What is frozen shoulder?
Frozen shoulder is a shoulder pain condition where there is significant loss of motion of the shoulder joint accompanied by stiffness. The shoulder joint is surrounded by the strong capsule and the main problem in this condition is believed to be the tightening of this capsule. The resulting pain is generally deep seated and poorly localised. It may be constant or present only at night when lying on the affected side. All movements of the joint are affected, especially the ones involving reaching straight up and rotation of joint such as while reaching behind the back.
Frozen shoulder is seen more commonly in women, especially between the ages of 40–60 years. Non-dominant side is more commonly involved, although in 20% to 30% of individuals both sides may be affected. Diabetics have five times more chances of developing this condition and about 30% of people with frozen shoulder have diabetes. Patients with overactive or underactive thyroid or those with shoulder immobilisation (such as after a fracture or stroke) are also at higher risk for developing frozen shoulder.
What is capsular hydrodistention?
Hydrodistention or dilatation or hydrodilatation is a non-surgical procedure aimed at stretching of the tight shoulder joint capsule. This is achieved by injecting saline or a mixture of saline, steroids and local anaesthetics under ultrasound or x-ray guidance. Ultrasound guidance is preferred as it is quicker, can be performed in the OPD and does not involve any radiation exposure. This procedure is an alternative to a surgical procedure — manipulation under anaesthesia (MUA), with some studies indicating better results with hydrodistention.
How is capsular hydrodistention performed?
I perform this procedure under ultrasound guidance in a sitting or lying position. The injection area is cleaned with antiseptic solutions. Ultrasound scan is performed to identify the shoulder joint, its capsule and plan the best pathway into the joint. Local anaesthetic is used to numb the injection site. A fine needle is introduced onto the surface of the shoulder joint under ultrasound guidance. A solution containing saline, local anaesthetic and steroid is then injected below the capsule. As the injection mixture is given, the capsule can be seen lifting off the joint. Once the injection is complete the needle is removed and a small dressing is placed over the injection site. The procedure takes about 20- 30 minutes to complete.
How does capsular hydrodistention work?
Hydrodistension is thought to have a mechanical effect of opening up the joint and releasing sticky adhesions within the joint, although the exact mechanism of action is debated. With stretching, the pressure inside the joint is reduced and the shoulder volume is increased. These effects can help in reducing pain, stiffness and improving the range of motion.
There is research evidence supporting better outcomes with the combination of hydrodilatation with steroids and physiotherapy, compared to either of the modalities when used alone. Hydrodistension results are comparable or better to the surgical procedure manipulation-under-anaesthesia (MUA), although the risks are less. Diabetic patients with frozen shoulder have inferior outcomes and in these hydrodilatation is likely to be more beneficial. In case of incomplete recovery these patients can be considered for repeat injections.
The option of steroid injections directly into the joint is preferred over the oral steroid as they are associated with fewer side effects. Some studies have found that oral steroids are as much as 5 times more likely to give the typical steroid side effects one hears of, compared to the one-off joint injection. Also, the lack of long-term benefits makes oral steroids a less attractive option in this condition.
capsular hydrodistention, frozen shoulder, Frozen Shoulder Ultrasound Guided Capsular Hydrodistention, Pain Specialist in Delhi , Pain Management in Delhi
#capsular hydrodistention#frozen shoulder#Frozen Shoulder Ultrasound Guided Capsular Hydrodistention#Pain Specialist in Delhi#Pain Management in Delhi#Dr. Amod Manocha
0 notes
Text
Lower Back Pain Due To Spinal Arthritis Non-Surgical Pain Management in Delhi
Back pain treatment in Delhi
Lower Back Pain Due To Spinal Arthritis
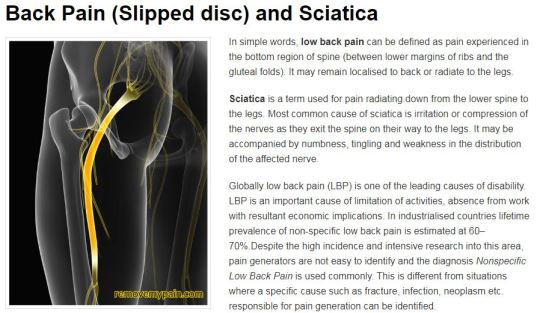
Low back pain (LBP), in simple words, is any pain in the bottom region of spine, between lower margins of ribs and the gluteal folds (end of buttocks). It is a leading cause of disability with lifetime prevalence estimated at 70–80%. In other words, 70- 80 % of us will be troubled by back pain at some point in our life. The pain may vary in severity from a mild discomfort or distraction to severe pain bringing life to a standstill. Common causes of LBP include muscle or ligament strain, arthritis of the spine, disc bulges/ rupture (slipped disc in common language) and pinched nerves. Other causes include degenerative discs, abnormal curvature or alignment of spine, narrowing of the spinal canal and referred pain from nearby areas. Fortunately, serious causes such as fracture, infection, cancer etc. are not so common. The pain may remain localised to the back or spread to the legs. Pain radiating to the legs accompanied by numbness, tingling and weakness is addressed as sciatica.
Back Pain Secondary Arthritis Of Spinal Joints
One of the causes of back pain is arthritis of the spinal joints. Spine is made up of a number of vertebrae stacked one above the other. The vertebrae join with each other at joints called the facet joints. These joints provide stability while allowing some degree of movement. As one ages, they can become painful and stiff as a result of wear and tear or inflammation. This condition is called facet joint arthritis or simply arthritis of the joints of the spine.
Prevention
This is a common question on everyone’s mind – What can one do to minimise the chances of developing this problem? Prevention involves combining healthy lifestyle with regular exercises to strengthen the core muscles. Healthy lifestyle includes eating healthy, maintaining a healthy weight, good posture, smart lifting using correct technique and not smoking.
Treatment
Injections for this pain issue are safe, effective, non-surgical interventions routinely performed as day cases under local anaesthesia. The options include
Facet Joint Injections
Radiofrequency Treatment
TAG :Back pain treatment in Delhi, Pain Management in South Delhi, Pain specialist doctor in Delhi
For more information :
https://www.removemypain.com/back-pain-and-sciatica.html
#Dr. Amod Manocha#back pain treatment in delhi#Best Back Pain Doctor in Delhi#best pain specialist in delhi#Pain Management in Gurgaon#Best Pain Specialist in South Delhi
0 notes
Link
0 notes
Link
#frozen shoulder ultrasound guided capsular hydrodistention#Shoulder pain treatment in delhi#best pain specialist in delhi#Body pain Treatment in delhi#Pain Management in South Delhi#Dr. Amod Manocha
0 notes
Text
Dr. Amod Manocha Provides Back Pain Solutions in Delhi with a Multidisciplinary Approach.
Connect To Disconnect From Your Pain
Dr. Amod Manocha and his team are dedicated spine specialists and industry experts committed to providing back pain treatment in India, the best knee pain treatment in Delhi, and affordable slipped disc treatment in Delhi.
In India, back pain is the leading cause of disability. Back pain is widespread, affecting everyone from construction workers to office…

View On WordPress
0 notes
Link
Dr. Amod Manocha is the Head of Pain Management Services at Max Super Speciality Hospital, Saket. He is trained as a Pain Management Specialist and an Anaesthetist in the UK. He has over 13 years of work experience in the UK including working as a Chronic Pain Consultant in many UK hospitals. Dr. Manocha believes in multidisciplinary approach and providing evidence-based treatments at par with international standards. He is committed to providing quality care and believes in building long-term relationship with patients based on honest communication and keeping their interests foremost.
#Dr. Amod Manocha#Best Back Pain Doctor in Delhi#Pain specialist doctor in Delhi#Neuropathic Pain treatment in Delhi#Pain Clinic in Gurgaon
0 notes
Text
Neck Pain Treatment in Delhi | Best Neck Pain Specialist in Delhi and Gurgaon - Removemypain
Neck Pain Treatment Gurgaon | Neck Pain Treatment in Delhi

Majority of us would experience neck pain at some point in our life. Neck Pain can disrupt daily routine activities. Muscle spasm, pain can make it difficult to turn head and activities such as driving become difficult. It is not uncommon for the neck pain to radiate to shoulders or lead to persistent headaches. Neck pain is more commonly observed in middle ages and may have a mechanical or postural basis. Most uncomplicated neck pain is associated with poor posture, anxiety and depression, neck strain, injuries. Fortunately majority of cases are not due to serious causes. If you are experiencing unresolving or severe pain, you should seek medical opinion from neck and shoulder pain treatment specialists in Delhi so that timely diagnosis can be done and corrective action can be taken.
Some common causes include –
Muscle sprain, spasm/ increased tension
Poor posture and work ergonomics
Incorrect positioning of the neck while sleeping
Aging: Degenerative disc disease and spinal osteoarthritis become more common as we age
Injuries/ Whiplash: Whiplash neck involves sudden jolting of neck forwards and backwards and is commonly observed in vehicular accidents. This can cause excessive stretching of neck muscles, ligaments or other injuries which can be associated with neck pain.
Neck pain can be a part of more widespread medical issues such as in fibromyalgia, arthritis, ankylosing spondylitis, infections, cancer etc. You can approach Pain Management Specialists in Delhi for diagnosing your problem and suggesting suitable solutions
It is advisable to seek early medical attention if you experience any of the following
Persisting symptoms or severe pain not responding to usual care or medications
Pain starting after fall, injury
New onset numbness, weakness or tingling in arms
Gait or balance problems
Loss or urine or stool control
Signs of infection/ meningitis
Pain worse at night time/interfering with your sleep
Some of the pain management techniques for neck pain include:
Lifestyle changes: Incorrect/ ignored posture while working on laptops mobiles etc can put excessive cervical spine strain leading to pain. Certain professions can be more prone to develop neck pain. Simple posture awareness and improvement, taking regular breaks can go a long way in reducing symptoms.
Medications: Anti-inflammatory drugs such as ibuprofen or naproxen and pain relievers like acetaminophen may initially be prescribed by your doctor. Sometimes medications like muscle relaxants or stronger painkillers may also be suggested by your doctor.
Physical Therapy: Regular exercise, good posture, stretching can help to reduce/ prevent to prevent unwanted stress and tension to your neck muscles. Heat or cold application may be used during the initial phases of injury to facilitate your recovery and physical exercise. Depending on the severity, time since injury and your recovery the specialist may recommend limiting normal physical activity or slow range-of-motion exercises or strengthening exercises.
There is research evidence supporting the use of specific strengthening exercises as part of a routine practice for chronic neck pain, cervicogenic headache and radiculopathy.
Ergonomics & Posture
Simple posture changes and better workplace ergonomics can help in preventing/reducing neck pain. Measures include adjustment of furniture height and computer position such that
Eyes point directly at the top third of the screen
Forearm is parallel to floor
Feet should be flat on the floor with thighs parallel with the floor
While sitting in office chair it’s a good practice to have back aligned against the back of the office chair and avoid slouching. Avoid sitting in one place for too long. Taking regular breaks to walk around and stretch is a good practice.
Relaxation techniques: relationship between stress and increase pain is well known and easily appreciated by most patients. Measures to deal with stress and anxiety help in more effective pain management.
Massage Therapy: The evidence supporting the use of massage therapy is limited although some people do find it useful in the short term. Massage can help in relaxing, loosening of muscles but it is important to remember that wrongly done massage can lead to harm.
Acupuncture: Certain people find Acupuncture helpful in neck pain management. When performed correctly it is a low risk procedure. The traditional acupuncture is based on the theory of restoring the energy balance in body and removing any blockages to the flow of energy.
Injections/ other interventions such as Radiofrequency ablation: These would depend on the cause of neck pain and actual pathology. They have been explained in more detail in the neck & arm pain section under treatments, on my website- removemypain.com
Ignoring persisting symptoms can aggravate the situation leading to chronic pain with reduced functionality. So, if your pain persists and does not respond to usual lifestyle changes and painkillers then seek medical opinion on time.
Tag = Pain Management in Delhi, Best pain specialist in Delhi
For More Information https://www.removemypain.com/neck-and-arm-pain.html
Follow us on https://www.instagram.com/removemypain/
#Best pain specialist in Delhi#Pain Management in Delhi#Removemypain#Dr. Amod Manocha#Neck Pain Treatment Gurgaon#Neck Pain Treatment in Delhi
0 notes
Text
GROIN OR INNER THIGH PAIN DUE TO ADDUCTOR SPRAIN - REMOVEMYPAIN
Adductor Strain
What is adductor strain?
Adductor muscles are a group of five muscles located in the inner thigh. These muscles help to bring the legs close to each other and stabilise the pelvis during standing and walking.
Strain, injury or imbalance of the adductor muscles is a common cause of inner thigh and groin pain, especially amongst individuals who are physically active or in competitive sports. Soccer players are commonly affected and as per one study adductor strains account for 10% of all injuries in soccer players. Other sports where associated with adductor injuries include hockey, basketball, tennis, figure skating, baseball, horse riding and karate. Tight adductor muscles can lead to hip, knee and back pain and affect our gait. Of all the adductor muscles, one called adductor longus is the one most frequently injured.
What are the symptoms of adductor sprain?
Common presenting features include:
Groin, inner thigh and lower abdominal pain. In some cases, the pain is intense at the beginning of athletic activity and is later replaced by a dull ache
Pain on sitting cross legged or when with coughing/ sneezing
Pain on activity such as
Lifting one leg as while stepping down from height or getting out of car
Turning or changing direction
Walking. In mild cases pain may be provoked by more strenuous activities such as running, kicking or performing lunges
Bruising or swelling in the painful area in severe cases
Localised tenderness in the upper inner thigh, close to where the adductor muscles attach to the pubic bone
Adductor strains are classified as
First degree: Pain without loss of strength or range
Second degree: Pain with loss of strength
Third degree: Complete disruption of muscle or tendon fibers with loss of strength
What causes adductor strain?
Adductor strains form a significant proportion of groin injuries. In a study among European soccer players, adductor muscle injuries were the second most common (23%) after hamstrings (37%). Risk factors contribution to injury include
Previous hip or groin injury
Overuse, fatigue and muscle imbalances
Weak adductors with poor flexibility
Poor hip/pelvic stability and strength
Running on hard surfaces, excessive running
Footwear
Training associated factors such as inadequate stretching, and lower levels of sport-specific training changes in training intensity, volume or type of training
Age- tendons become less able to absorb force as they age
Biomechanical abnormalities including excessive pronation or leg-length discrepancy
Genetic factors such as poor collagen
Adductor sprain can be of sudden or gradual onset. Acute injury is associated with sporting actions such as suddenly changing direction at speed, sudden acceleration in sprinting, sliding sideways or kicking. One study analysed the videos of acute adductor injuries in professional male football players and found that majority of injuries occurred in non-contact situations (71%). Common injury actions included change of direction (35%), kicking (29%), reaching (24%) and jumping (12%).
How is this condition diagnosed?
Diagnosis can be usually made clinically. MRI is used for confirming the diagnosis and assessing severity especially in chronic injuries unresponsive to conservative treatment modalities. Ultrasound scan is the alternative imaging option.
MRI Scans can give prognostic information as tears involving >50% of the cross-sectional area, tissue fluid collection, or deep muscle tears indicate more severe injury with prolonged recovery. The location of the tear is important as tears at the junction of the muscle with tendon (musculotendinous junction) can be more aggressively rehabilitated compares to one close to the joining of the tendon with bone, due to differences in the blood supply of the two areas. Tendons can be viewed as ropes tying the muscles to the bones. The musculotendinous junction is the most common site of injury in a muscle strain.
What are the treatment options for adductor strain?
Once the diagnosis has been established, treatment and prognosis are influenced by factors such as
Location of tear as those at the junction of the muscle with the bone can be dealt by aggressive rehabilitative treatment
Degree of strain/ tear
Duration of symptoms- acute or chronic
Presence of any biomechanical abnormalities such as muscular imbalances, leg length discrepancy
Acute injuries are initially treated with rest, ice, compression anti-inflammatory drugs and physical therapy with further management dependant of factors discussed earlier. Early treatment is recommended, and injections are used as required.
Education about load management and avoiding provoking factors is important. Activities like running can be replaced with swimming, walking, cycling as having baseline activities is preferred to absolute rest. Specific and individualised exercise programs have a role. A slowly progressive loading program can be used to improve strength and control of adductors, pelvis and lower limbs. The aim of the treatment initially is preventing further injury and inflammation and proving an optimal environment for healing to take place. As recovery occurs, this changes to restoration of range of motion and prevention of atrophy and then subsequently to regaining strength and flexibility.
Injections
This option is considered for individuals’ not responding to conservative measures. Injections are used in combination with physical therapy can help in confirming the diagnosis, providing early, lasting relief and possibly facilitation early return to usual activities. The options include
Steroid injections
PRP with or without needle tenotomy
Obturator Nerve block
Regardless of whichever option is used, ultrasound guidance is valuable in improving accuracy and reducing complications. Sometimes injections of the muscle in the lower abdomen (rectus abdominis muscle) are performed at the same time.
Steroid injections: There are quick to work, commonly performed injections. Steroids have anti-inflammatory effects and it may be all that is required to reduce the pain and help you actively engage with physical therapy. Some studies have shown better effects if the duration of symptoms is less that 6 weeks and hence the importance of early treatment. Post injection graded increase in activities can be commenced once the pain remains controlled for two weeks.
Platelet Rich Plasma (PRP): PRP injections are commonly used for treatment of tendinopathy and the evidence supporting their use is slowly accumulating. The procedure involves spinning one’s blood in a special machine which separates the platelets (containing the growth factors) from the other blood components. This concentrated platelet layer is then injected into the problem area to induce tissue healing. These injections take time to work with benefits becoming apparent 6 to 12 weeks after treatment. PRP injections are frequently used in combination with needle tenotomy which essentially implies repeated puncturing of the tendon to promote blood flow to the area and induce long-term healing.
Obturator Nerve Block: This injection can have added effect on top of the injections discussed previously. Obturator nerve supplies most of the adductor muscles and hence blocking this nerve can help in reducing the pain signals being transmitted. Injury or compression of the nerve leads to symptoms similar to adductor sprain and is addressed as obturator neuralgia. Obturator neuralgia can also be secondary to adductor strain and is a known cause of exercise induced groin, inner thigh pain. In this situation obturator nerve block can be especially useful.
Surgery: This option may be considered for acute complete tears with limb weakness or chronic tears with non-satisfactory response to other treatment modalities for a minimum of 6 -12 months. Surgery involves tendon release or dividing the tendon (tenotomy) and this may help to reduce the pain
Restarting activities: Return to play and activity is guided by symptom recovery as well as progress with treatment. Too soon a return is risk factor for repeat injury, which can cause chronic symptoms. Generally, after an acute strain return to sports is recommended on regaining 70% of strength and a painless range of motion. This can be usually achieved between 4 to 8 weeks, although can take up to 6 months chronic injuries. Maintaining adductor strength at a minimum of 80% of abductor strength has been shown to reduce adductor injuries.
Tags - Sport Injury Treatment in Delhi, Pain Treatment in Delhi, Best pain specialist in Delhi
For more information link - www.removemypain.com
See our documents - https://www.pearltrees.com/bestremovemypain/item437605870
#Sport Injury Treatment in Delhi#Pain Management in Delhi#Pain specialist doctor in Delhi#Dr. Amod Manocha#Removemypain
0 notes
Photo
#Back Pain Treatment in India#removemypain#dramodmanocha#dr amod manocha#Back pain treatment in delhi
0 notes
Link
Dr. Amod Manocha is the Head of Pain Management Services at Max Super Speciality Hospital, Saket. He is trained as a Pain Management Specialist and an Anaesthetist in the UK. He has over 13 years of work experience in the UK including working as a Chronic Pain Consultant in many UK hospitals. Dr. Manocha believes in multidisciplinary approach and providing evidence-based treatments at par with international standards. He is committed to providing quality care and believes in building long-term relationship with patients based on honest communication and keeping their interests foremost
#back pain treatment in gurgaon#Pain specialist in Gurgaon#slipped disc treatment in delhi#Pain management centre in Delhi
0 notes
Text

Introduction:
Sciatica is a term used for pain radiating down from the lower spine to the legs. Most common cause of sciatica is irritation or compression of the nerves as they exit the spine on their way to the legs. It may be accompanied by numbness, tingling and weakness in the distribution of the affected nerve.
1. What is sciatica?
The term sciatica originated from the sciatic nerve, which is the single largest nerve in our body. This nerve is responsible for a significant proportion of leg sensation and movement. Sciatica represents pain in the area supplied by the sciatic nerve.
Radicular pain/ radiculopathy are medical terms which doctors use when describing this condition. There are numerous reasons for having leg pain and every leg pain is not sciatica. Commonly people misinterpret sciatica as a disease and need to be explained that it is a symptom of the underlying problem.
2. What are symptoms of sciatica?
The severity and symptoms many vary considerably. In severe cases the affected individual may find it difficult to walk or even stand up straight.
Some of the commonly observed symptoms include
· Sharp, burning, stinging, shooting, electric shock or cramps like pain in one or both legs often as far down as the foot. Movement, coughing and sneezing can intensify the pain
· Tingling, pins and needles and/or numbness in leg or foot
· Muscle weakness with difficulty in weight bearing or walking.
· Buttock/low back pain and stiffness.
3. What causes sciatica?
· Disc herniation: Spine is formed of many bones called vertebrae arranged one above the other. In between these vertebrae are discs, which are like cushions or shock absorbers. The discs are made up of an outer tough substance and an inner soft jelly like substance. Herniation of the disc can occur if there is splitting or crack in the outer layers allowing the inner jelly like substance to protrude through the crack. This can cause inflammation and compression of the nerve roots in the vertebral column. Slipped disc is a commonly used term for this condition. There is an increased susceptibility to disc herniation as we age because the soft, jelly like substance dries out and shrinks with time, making the disc more fragile.
· Spinal stenosis: Stenosis means narrowing. The narrowing can be of the central canal of the spine or the passageways/ tunnels from which the nerves exit the spine. Besides disc problems, arthritis of the spinal joints or thickening of ligaments can also cause/ contribute to the narrowing.
· Spondylolisthesis: In this condition there is a problem with the alignment of vertebrae, where one vertebra is more forward or backwards, which can narrow the spaces for nerves and produce sciatica as a result.
· Piriformis syndrome: In this condition piriformis muscle in the pelvis is responsible for pressure on sciatic nerve.
· Trauma/ fractures
· Spinal tumors and infections are rare causes of sciatica
Back pain Treatment in Delhi is a common problem that must be consider that affects 8 out of 10 people at some point in their life. It can affect people of all ages and is a common reason for seeking medical assistance.
4. Can it resolve on its own?
Fortunately most cases of sciatica resolve within a period of weeks to months with conservative treatment. Specialist input and treatment can help. Painkillers, heat or cold pack, altered activity levels and physical therapy may be suggested depending on your condition. An injection of steroids into the epidural space within the spine can provide short-term pain relief in sciatica. Persistent pain can lead to changes in the nerves (referred to as plasticity). This can be a source of persistent pain even if the original inciting event is resolved … hence the importance of managing these sooner than later.
Having seen numerous cases over the years, I would say that it is not easy to predict the course. It can resolve but to what extend depends on numerous factors- some are modifiable and others are not. The recovery period varies from individual to individual.
5. What are the warning signs I need to be watch for?
Some symptoms point towards a serious problem and require urgent medical attention. Ignoring these could lead to permanent nerve damage. Some of these include
· Loss of urinary control/ inability to pass urine
· Loss of control over stools
· Numbness around the bottom
· Worsening leg weakness / loss of control
6. What can I do to reduce my risk of having sciatica?
Though it’s not possible to completely eliminate the risk of sciatica, however adopting a healthy life style can help in reducing the risk. This includes
· Giving up smoking
· Regular exercises
· Right posture and work ergonomics
· Healthy diet and maintaining weight in the normal range
· Using proper manual handling techniques while lifting to avoid back injury
· Stress Management
7. What investigations are generally considered for sciatica?
Your doctor may request for investigations such as magnetic resonance imaging (MRI) scan and blood tests. Sometimes computerized tomography (CT) scans may also be required. X-rays are not as helpful and they can provide only limited information.
Bulging discs on an MRI scan are not an uncommon finding. It is important not to get fixated on the MRI findings. A bulging disc is not permanent and can reverse. The investigation results should be interpreted in combination with patient history, examination findings to assess their significance. A number of patients with severe MRI findings may be asymptomatic and vice versa.
8. What are the other treatment options?
Sciatica is different from common ailments we all suffer and hence taking professional help is recommended. Your doctor can help to confirm that you have sciatica and help identify the cause. A range of different options- non surgical (such as injections- nerve root blocks, epidurals, piriformis injection etc) or surgical may be considered. There is no one solution for sciatica pain and the options are numerous — some with good evidence and others with not so robust evidence.
Generally a multimodal multidisciplinary approach is preferred as this helps in addressing not only the pain but also the impact of pain on one’s life. I ensure that the patient understands the nature or problem and the do’s and don’ts. Time spent in explaining the conditions and the expected course goes a long way in fostering realistic expectations. I generally use a combination of the modalities mentioned below to enhance the chances of quicker recovery.
Pain relief:
Pain reduction achieved by medicines help to maintain activity and improves physiotherapy compliance. The medications used depend on the type and severity of pain, duration of symptoms and individual factors such as co morbidities and allergies. Some of the commonly prescribed pain killers include
· Non steroidal anti-inflammatory drugs (NSAIDs)
This includes drugs such as DIclofenac, Naproxen, Aceclofenac, Ibuprofen etc. NSAIDs are prescribed to reduce the pain and inflammation during periods of acute sciatica although the evidence supporting their use is not very robust. The risk benefit ratio needs to be evaluated while prescribing any drugs.
· Neuropathic pain killers
This group includes antidepressants and anticonvulsants both of which are well known painkillers for nerve pain. It generally takes a few weeks for the full effects of these drugs to become apparent. Effects such as reduced anxiety and sedation can be used beneficially by tailored selection to suit individual patients. Their use is supported by the NICE guidelines, UK.
· Opioids
Weak opioids such as tramadol are often prescribed during pain flare up episodes. It is a good practice to be aware of the side effects of a medicine prior to using it.
· Muscle relaxants
These are used for short duration to relieve any muscle spasm contributing to the back pain.
Spinal Injections:
The use of epidural steroids/ Nerve root blocks has been shown to have beneficial improvements in leg pain and disability scores in short term. Steroids help by their anti-inflammatory and analgesic (pain relieving) effect. Epidural steroids are preferred to oral steroids as they are given close to site of actual problem and have less adverse effects.
Physiotherapy:
Physiotherapy is an essential component of sciatica treatment. Your physiotherapist can help with posture advice, do’s and don’ts relevant to your condition, understanding the concept of pacing of activities, setting practical goals, teaching strengthening exercises for core, leg muscles and manual handling techniques.
Surgery:
If a combination of above fails to provide adequate relief then surgical options such as discectomy (operation to remove bulging part of the disc or separated disc fragments) and microdiscectomy can be considered for sciatica resulting from disc bulge. Surgical options will vary depending on the cause of sciatica and sometimes may be the first choice, depending on the actual pathology and its severity.
Back Pain Treatment in Delhi, Causes Sciatica, Pain Specialist in Delhi, Risk of Sciatica, Symptoms of Sciatica
#Back Pain Treatment in Delhi#Causes Sciatica#Pain Specialist in Delhi#Risk of Sciatica#Symptoms of Sciatica#Dr. Amod Manocha
0 notes
Photo

Are You suffering from numbness, tingling or burning sensation after Chemotherapy?
Peripheral nerves carry sensations from the different parts of your body to the brain and control the movement of our arms and legs. The set of symptoms resulting from damage to these nerves is addressed as Peripheral neuropathy. Symptoms are usually symmetrical starting from toes and fingers, and progress towards the body.
#Dr. Amod Manocha#Pain management centre in Delhi#Pain Clinic in Gurgaon#Body pain Treatment in delhi#pain specialist in delhi
0 notes
Link
#Dr. Amod Manocha#best pain specialist in delhi#Pain Management Specialist In Delhi#back Pain Joint Pain#Diabetic Neuropathy Treatment
0 notes
Link
#pain specialist in delhi#best pain specialist in delhi#Back Pain Treatment in India#neck pain treatment in Delhi#Pain Specialist in Gurgaon#Pain Management in Gurgaon#Dr. Amod Manocha
0 notes
Text
0 notes