#Stress and Poor Diet Directly Linked to Thyroid Disease
Text
Understanding Fatigue and Brain Fog: Causes, Symptoms, and Solutions

Introduction
Fatigue and brain fog are more than just buzzwords. They’re real, debilitating conditions that affect countless people worldwide. Fatigue refers to a state of extreme tiredness and lack of energy, while brain fog encompasses a range of cognitive difficulties, including memory issues, lack of focus, and mental clarity. Understanding these conditions is crucial for managing them effectively and improving one’s quality of life.
What is Fatigue?
Physical Fatigue
Physical fatigue is the kind of tiredness that lingers even after a good night’s sleep. It’s a pervasive feeling of exhaustion that can make even the simplest tasks feel monumental.
Mental Fatigue
Mental fatigue, on the other hand, is characterized by a lack of mental energy. It can result in difficulty concentrating, forgetfulness, and a general feeling of being overwhelmed.
What is Brain Fog?
Cognitive Symptoms
Brain fog is often described as a cloudy or fuzzy feeling in the head. It can impair cognitive functions like memory, attention, and problem-solving skills.
Emotional Impact
The emotional toll of brain fog shouldn’t be underestimated. It can lead to frustration, irritability, and even depression, further exacerbating the symptoms.
Common Causes of Fatigue and Brain Fog
Lack of Sleep
One of the most obvious culprits is insufficient sleep. Quality sleep is essential for physical and mental rejuvenation.
Poor Diet
A diet high in processed foods and low in essential nutrients can sap your energy and cloud your mind.
Stress and Anxiety
Chronic stress and anxiety put your body in a constant state of fight-or-flight, which can be incredibly draining.
Medical Conditions
Certain medical conditions like chronic fatigue syndrome, depression, and thyroid disorders are directly linked to fatigue and brain fog.
Lifestyle Factors Contributing to Fatigue and Brain Fog
Sedentary Lifestyle
Not moving enough can lead to decreased energy levels and poor circulation, both of which contribute to fatigue.
Poor Work-Life Balance
Overworking without adequate rest and relaxation can leave you feeling burnt out and mentally drained.
Overuse of Technology
Excessive screen time, especially before bed, can interfere with your sleep and mental clarity.
Medical Conditions Linked to Fatigue and Brain Fog
Chronic Fatigue Syndrome
This condition is characterized by extreme, persistent tiredness that doesn’t improve with rest.
Depression and Anxiety Disorders
Mental health issues like depression and anxiety can drain your energy and cloud your thoughts.
Thyroid Problems
An underactive thyroid can slow down your metabolism, leading to fatigue and cognitive sluggishness.
Autoimmune Diseases
Conditions like lupus and multiple sclerosis can cause widespread inflammation and fatigue.
The Role of Nutrition in Combating Fatigue and Brain Fog
Importance of a Balanced Diet
Eating a diet rich in whole foods provides the necessary vitamins and minerals to support energy levels and brain function.
Foods to Avoid
Sugary snacks and processed foods can cause spikes and crashes in blood sugar, leading to fatigue.
Plant-Based Foods that Boost Energy and Clarity
Incorporate foods like leafy greens, nuts, seeds, and whole grains to enhance mental clarity and stamina.
The Impact of Sleep on Fatigue and Brain Fog
Importance of Good Sleep Hygiene
Good sleep hygiene includes practices like maintaining a consistent sleep schedule and creating a restful environment.
Tips for Better Sleep
Avoid caffeine and screens before bed, and try relaxation techniques like reading or taking a warm bath.
How Sleep Disorders Contribute
Sleep disorders like insomnia and sleep apnea can significantly impair your sleep quality, leading to fatigue and brain fog.
Stress Management Techniques
Mindfulness and Meditation
Practicing mindfulness and meditation can help calm your mind and reduce stress levels.
Exercise and Physical Activity
Regular physical activity boosts your mood and energy levels, making it easier to combat fatigue.
Time Management Skills
Effective time management can help reduce stress by ensuring you have time for work, rest, and leisure activities.
Natural Remedies and Alternatives
Herbal Teas
Herbal teas like chamomile and peppermint can help relax the mind and body.
Essential Oils
Aromatherapy with essential oils like lavender and eucalyptus can promote relaxation and mental clarity.
Breathing Exercises
Simple breathing exercises can reduce stress and increase oxygen flow to the brain, enhancing mental clarity.
Cognitive Exercises to Combat Brain Fog
Brain Training Games
Games that challenge your brain, like Sudoku or crossword puzzles, can improve cognitive function.
Puzzles and Challenges
Engage in activities that require problem-solving skills to keep your mind sharp.
Learning New Skills
Taking up a new hobby or learning a new skill can stimulate your brain and improve mental clarity.
Professional Help and When to Seek It
Consulting a Doctor
If your symptoms persist, it’s essential to consult a healthcare professional to rule out underlying conditions.
Therapy and Counseling
Talking to a therapist can help you manage stress and anxiety, which can alleviate fatigue and brain fog.
Medical Tests and Diagnostics
Tests like blood work and sleep studies can identify issues that contribute to your symptoms.
Building Healthy Habits for Long-Term Benefits
Routine Establishment
Establishing a daily routine can help you maintain consistent energy levels and mental clarity.
Setting Realistic Goals
Set achievable goals to prevent feeling overwhelmed and burnt out.
Maintaining a Positive Mindset
Cultivate a positive attitude to help you cope with challenges more effectively.
Personal Stories and Testimonials
Case Studies
Explore real-life case studies of individuals who have successfully managed their symptoms.
Success Stories
Read about people who have overcome fatigue and brain fog through lifestyle changes and treatment.
Real-Life Experiences
Hearing from others who share your experiences can provide motivation and hope.
Conclusion
Understanding fatigue and brain fog is the first step toward managing them effectively. By making lifestyle changes, seeking professional help, and adopting healthy habits, you can significantly improve your energy levels and mental clarity. Don’t let fatigue and brain fog control your life — take action today for a brighter, clearer tomorrow.
FAQs
What are the main differences between fatigue and brain fog?
Fatigue primarily refers to physical and mental exhaustion, while brain fog encompasses cognitive issues like memory problems and lack of focus.
How long does brain fog typically last?
The duration of brain fog varies. It can last from a few hours to several weeks, depending on the underlying cause and lifestyle factors.
Can diet alone cure fatigue and brain fog?
While a balanced diet can significantly improve symptoms, other factors like sleep, stress management, and medical conditions also play crucial roles.
Are there any quick fixes for brain fog?
Quick fixes like caffeine can provide temporary relief, but addressing the root causes through lifestyle changes and medical intervention is more effective for long-term improvement.
What are some red flags indicating a need for medical intervention?
Persistent fatigue and brain fog that don’t improve with lifestyle changes, severe memory issues, and significant impact on daily functioning are red flags that warrant medical attention.
0 notes
Text
How To Treat ADHD Naturally: 5 Most Important Steps
Is there a way to treat ADHD naturally? What one should do?More than 1 in 10 children, ages 4-17 have ADHD (attention deficit hyperactivity disorder) (1), defined as “limited attention and hyperactivity.”
Common characteristics of ADHD include:
Difficulty sustaining attention or focusing
Difficulty following through with tasks
Hyperactivity
Difficulty organizing self and tasks
Impulsive behavior
To officially be diagnosed with ADHD, symptoms must persist for at least 6 months, and behaviors and symptoms must be abnormal for children of the same age and negatively affect his or her school, home life or relationships in more than one setting (i.e. at home and at school).
Unfortunately, for many of these kids who are diagnosed, ADHD will continue into their adulthood, and conventional medicine believes that the disease is “manageable, but not curable.” In order to help kids “manage” their ADHD, treatment typically consists of medications and behavioral interventions, such as occupational therapy, behavioral therapy and sensory or movement “breaks.”
After those options are exhausted however, there is little, if anything else doctors say they can do.
The missing link most docs and conventional medicine is not talking about?
A little superpower known as the “brain gut connection.”
According to the latest in research about the brain-gut connection, ADHD is not only manageable, but it is reversible and remissible.
In this article we’ll cover the basics about the brain-gut connection, plus learn 5 essential steps to treat ADHD naturally (that your doctor probably won’t tell you about).
THE BRAIN GUT CONNECTION
The “brain-gut” connection is essentially what it sounds like: Your gut and brain are directly linked.
Your vagus nerve (the nerve responsible for directing how you think and your brain function) is connected from your frontal brain lobe to the top stomach. In addition, about 95% of your serotonin (“feel good” brain chemical) is produced in your gastrointestinal tract.
Couple this with the fact that your gastrointestinal tract is lined with more than a 100 million nerve cells, and it makes sense: the inner workings of your digestive system don’t just help you digest food, but also guide your emotions.
In short: When your gut is unhappy or stressed…your brain is unhappy or stressed.
Enter: The “brain-gut connection.”
Inflammation in your gut sends signals to your brain, causing a similar response (inflammation, stress and in many children’s cases, anxiety, sensory processing disorders, and ADHD).
The bottom line: If you have an unhealthy gut, your brain function gets thrown off. And, if you have an unhealthy brain (i.e. stressed), your gut function can also get thrown off.
THE MISSING LINKS IN ADHD TREATMENT: GUT HEALTH & STRESS
Unfortunately, for years, we’ve come to see the body and mind as two separate entities.
The mind is often treated separately from the body, other than using medications to suppress “neuro-chemical imbalances.” Patients with ADHD or other mood disorders and mental illnesses are then typically referred out to see a psychotherapist or occupational therapist to address “behavior” and emotional issues, in hopes of remediating the symptoms, with sub-par results or a lifetime spent in therapy, using coping strategies and taking medications.
From a functional medicine perspective, we want to address ADHD and other mental health conditions in the same way that we address any other health condition (i.e. autoimmune disease, diabetes, GERD, hypertension, etc.). We want to look at what the underlying causes are for these conditions. This is essential to treat ADHD naturally.
While mental illness, like ADHD, is a complex combination of various genetic and epigenetic factors, (including nutritional, physical, biochemical, environmental, social, emotional, and spiritual influences), many traditional methods of diagnosis and treatment fail to address two of the biggest drivers of disease: gut health and chronic inflammation (i.e. stress).
Our stress levels and gut health are the gateways to health.
In fact, the American Psychological Association estimates that 99% of ALL disease is attributed to stress alone (2). Stress is defined as any “outside force that exceeds the body’s ability to recover or maintain homeostasis.”
Just like the “stress” of a poor quality diet, lack of sleep and sedentary lifestyle leads to conditions like diabetes and high blood pressure, and just like poor gut health, such as “intestinal permeability” (leaky gut) is connected to conditions like autoimmune disease, skin breakouts and anxiety, stress levels and gut health play a key role in ADHD.
STRESS 101
Contrary to popular belief, “stress” goes far beyond mental stress. Physiological stress equally imbalances the optimal function of the body—brain balance included. Common sources of physical stress and inflammation for many ADHD sufferers include:
Inadequate sleep or poor quality sleep. More than half of kids do NOT get 8-9 hours of quality sleep. (3)
Sedentary lifestyles. Kids are moving less than ever before with 1 in 5 getting the recommended minimum of 60-minutes of physical activity 5 days per week. (4)
Overexposure to screens and blue lights. The average kid spends 6-9 hours/day in front of a screen. (5)
Lack of spontaneous play and time in nature. Only 10% of kids spend time outside every day (6) and a 2018 Gallup study found that children nationwide spend less time on creative play than ever before, spending 18.6 hours each week to screen-based play per week, versus 14.6 hours on indoor screen-free play (7).
Antibiotic drug exposure. 1 in 4 kids get antibiotics every year that are unnecessary and 5 in 6 kids take an antibiotic every year (8).
Poor quality nutrition and processed foods. Nearly 50% of kids’ diets, ages 2-18 consist of empty calories from added sugars and and processed foods including: soda, fruit drinks, dairy desserts, grain desserts, pizza, and conventional milk (9).
Poor gut health. Including about 2 in 5 kids with constipation (10), 1 in 4 with GERD or “reflux” (11) and millions of kids with allergies and asthma—the #1 “chronic disease” of kids nationwide (12) (linked to poor gut health) (13, 14).
GUT HEALTH 101
Much of the chronic diseases we face today can also be traced back to our gut health, including ADHD. If we could address the problems in our gut, we can find the right ways to treat ADHD naturally.
The human gut contains more than 100 trillion gut bacteria—up to 10 times more bacteria than human cells in our blood stream and body.
The healthier and more diverse your gut bacteria, the healthier your body is overall. However, the less healthy or less diverse your gut bacteria, the less healthy or “out of balance” you are.
Our gut bacteria influence the health of our:
Blood sugar and insulin levels
Hormone health
Thyroid
Detoxification
Mood
Immune system (allergies, skin health)
Digestion
Mental health
How do gut bacteria get unhealthy in the first place? Go back to the topic of stress! It’s a vicious cycle, but common sources of “unhealthy gut bacteria” include:
Poor sleep
Poor quality foods (packaged, processed, conventional meat, dairy, sweeteners, etc.)
Environmental toxins (additives, plastics, medicines, toxic cleaning and hygiene products)
C-section births and processed formula feedings as a baby
Infection & Illness
Sedentary lifestyles
Antibiotics
Underlying gut pathologies, often caused by stressors (parasites
The good news? If we address the gut health, then we could treat ADHD naturally—if not reversed.
Research backs this up.
SURVEY SAYS: ADHD & GUT RESEARCH
A 2017 peer-reviewed study found significant connections between increased gut inflammation and test subjects with ADHD, regardless of age and previous diagnosis (15). The volunteers with ADHD had more Bifidobacterium genus, often associated with SIBO or small intestinal bacterial overgrowth (16).
In another review in the European Child & Adolescent Psychiatry Journal, researchers state that while studies on ADHD and the gut microbiota in patients is budding, there is clear evidence about the link between obesity and ADHD and between obesity and alteration of the gut microbiota.
There is a way to treat ADHD naturally.
Obesity induces a low-grade inflammatory state which has been associated with behavioral and cognitive alterations, being gut micro-biota most likely an important mediator between inflammation and altered behaviors.
Overall, data from gluten-free mice studies, antibiotic treatment studies, and probiotic interventions suggest that alterations in gut microbiota that reduce the inflammatory state also reduce stress-related behaviors, supporting the role of the gut microbiota as a mediator between inflammation and behavioral alterations.
And, another clinical trial (18) is currently underway, as researchers have concluded from previous research that ADHD is in are linked to shifts in gut microbiota composition.
5 ESSENTIAL STEPS TO TREAT ADHD NATURALLY
The main strategy to heal and treat ADHD naturally involve balancing out stress levels, and NOT irritating the gut barrier and gut immune system. Here are 5 essential steps to start.
STEP 1: EAT REAL FOOD (ESPECIALLY FATS & PROTEINS)
When we eat, we not only feed ourselves, but we also feed our gut bugs. This is a crucial step to treat ADHD naturally. It’s not rocket science: Real, whole, nutrient-dense foods make an unhealthy gut a healthier gut. While most kids’ favorite foods include chicken nuggets, mac and cheese, French fries, Honey Nut Cheerios, possibly fruit and anything with ketchup, they are humans too.
And humans were wired to eat real foods. Real foods include: sustainable, organic meats and fish, colorful fruits and veggies and essential healthy fats (coconut oil, ghee, grass-fed butter, pastured egg yolks, avocado, raw nuts and seeds.
STEP 2: CUT OUT THE CULPRITS
This goes beyond just going a gluten-free (since many gluten free products contain just as many additives as the gluten version)s. Experiment with cutting out grains, conventional dairy, sugar and additives (dyes, sweeteners, chemicals) for 30 days and watch your kids’ brains come to life. Do it together with a non-diet mentality as a challenge for the family for stronger bodies and better brains. A great way to help treat ADHD naturally.
STEP 3: LOVE YOUR GUT BUGS
Give your kids a daily soil-based probiotic and prebiotic fiber to treat ADHD naturally. These include partially hydrolyzed guar gum, to help the healthy probiotics stick in their gut. Soil based probiotics are typically better tolerated by most people, and contain probiotic like cultures that were once found in the rich soils of our ancestors. Start with 1/2 capsule of a probiotic, 2 times per day, and 1 teaspoon of a prebiotic. Other “gut loving” additions include:
Colostrum (similar to the gut-healing natural colostrum found in the “perfect food:” a mother’s milk)
Digestive Enzymes (support natural enzymes that help break down food)
Betaine HCL (hydrochloric acid) found in capsules (naturally boosts stomach acid to enhance digestion)
Optional: Digestive “bitters” to support detoxification mixed into homemade dark chocolate syrup (5 drops of bitters + 1 tablespoon cacao powder + 1 tablespoon raw honey (use maple syrup for kids under 1 year of age) +fresh juice from half a small lemon)
STEP 4: DESTRESS
For kids, this includes encouraging them to get 60-minutes (at least) of active play and exercise each day, as well as outdoor time and sunshine, about 9 hours of sleep each night and creative, imaginative playaway from screens.
Magnesium Citrate at night is also a natural calming mineral, mixed into bedtime tea or water.
STEP 5: TEST, DON’T GUESS
Work with a functional medicine practitioner or healthcare practitioner knowledgeable in gut health analysis and treatment of any underlying conditions that may play a role in your child’s brain-gut-connection. Lab tests may include: Stool testing, Organic Acids Urine Testing, Comprehensive Bloodwork Analysis, Food Sensitivity Testing, and Small Intestinal Bacterial Overgrowth Breath Testing. This can help to treat ADHD naturally.
Not all tests are essential, but can give you and your child a clearer picture into their unique presentation if an underlying gut pathology is behind their condition. (Note: Many traditional GI doctors do not perform these tests on kids, beyond food allergy, not sensitivity, testing and potential scope and CT scan imaging).
The bottom line:
In the end, address the roots of cognitive imbalance first (gut and stress), not the symptoms. This is very important step to treat ADHD naturally.
Resources:
2018. ADHD. https://www.cdc.gov/ncbddd/adhd/data.html.
2018. How Stress Affects Your Health. https://www.apa.org/helpcenter/stress-facts.pdf; American Institute of Stress. https://www.stress.org/americas-1-health-problem/ (Cited: Perkins (1994) showed that 60% to 90% of doctor visits were stress-related)
Sleep Foundation. 2010. Sleep in America. http://sleepfoundation.org/sites/default/files/2014-NSF-Sleep-in-America-poll-summary-of-findings—FINAL-Updated-3-26-14-.pdf
2018. Physical Activity Facts. https://www.cdc.gov/healthyschools/physicalactivity/facts.htm
Kaiser Family Foundation. Generation M2: Media in the Lives of 8-18-year-olds. 2010 https://kaiserfamilyfoundation.files.wordpress.com/2013/04/8010.pdf
The Nature Conservancy. Connecting America’s Youth to Nature. 2011. https://www.nature.org/newsfeatures/kids-in-nature/youth-and-nature-poll-results.pdf
Doug & Melissa. 2018. Time to Play Study. http://ww2.melissaanddoug.com/MelissaAndDoug_Gallup_TimetoPlay_Study.pdf
2017. Antibiotic Use in the United States, 2017: Progress and Opportunities. https://www.cdc.gov/antibiotic-use/stewardship-report/outpatient.html
Facts & Statistics: Physical Activity. 2018. https://www.hhs.gov/fitness/resource-center/facts-and-statistics/index.html (Cited Source: Reedy J, Krebs-Smith SM. Dietary sources of energy, solid fats, and added sugars among children and adolescents in the United States. Journal of the American Dietetic Association, Volume 110, Issue 10, Pages 1477-1484, October 2010. Available at: http://www.ncbi.nlm.nih.gov/pubmed/20869486.)
Blackmer AB, Farrington EA. Constipation in the pediatric patient: an overview and pharmacologic considerations. Journal of Pediatric Health Care. 2010;24(6):385–399.
Nelson SP, Chen EH, Syniar GM, Christoffel KK. Pediatric Practice Research Group. Prevalence of symptoms of gastroesophageal reflux during childhood. Archives of Pediatric and Adolescents Medicine. 2000;154:150–154
Asthma & Allergy Foundation. 2018. Allergy Facts and Figures. http://www.aafa.org/page/allergy-facts.aspx
Volz, F. Wölbing, F. Regler, S. Kaesler, T. Biedermann. 232 NOD2 signaling critically influences sensitization to orally ingested allergens and severity of anaphylaxis. Journal of Investigative Dermatology, 2016; 136 (9): S201 DOI: 10.1016/j.jid.2016.06.252
Neonatal gut microbiota associates with childhood multisensitized atopy and T cell differentiation. Fujimura KE, Sitarik AR, Havstad S, Lin DL, Levan S, Fadrosh D, Panzer AR, LaMere B, Rackaityte E, Lukacs NW, Wegienka G, Boushey HA, Ownby DR, Zoratti EM, Levin AM, Johnson CC, Lynch SV. Nat Med. 2016 Sep 12. doi: 10.1038/nm.4176. [Epub ahead of print]. PMID: 27618652.
Aarts, E., Ederveen, T. H. A., Naaijen, J., Zwiers, M. P., Boekhorst, J., Timmerman, H. M., … Arias Vasquez, A. (2017). Gut microbiome in ADHD and its relation to neural reward anticipation. PLoS ONE, 12(9), e0183509. http://doi.org/10.1371/journal.pone.0183509
Quigley & Quera. 2006. Small Intestinal Bacterial Overgrowth: Roles of Antibiotics, Prebiotics, and Probiotics. http://www.deerlandenzymes.com/wp-content/uploads/2015/04/Small-Intestinal-Bacterial-Overgrowth-Roles-of-Antibiotics-Prebiotics-and-Probiotics.pdf
Carmen Cenit, María & Campillo Nuevo, Isabel & codoñer-franch, Pilar & G. Dinan, Timothy & Sanz, Yolanda. (2017). Gut microbiota and attention deficit hyperactivity disorder: new perspectives for a challenging condition. European Child & Adolescent Psychiatry. 26. 10.1007/s00787-017-0969-z. https://www.researchgate.net/profile/Pilar_Codoner-franch/publication/314967081_Gut_microbiota_and_attention_deficit_hyperactivity_disorder_new_perspectives_for_a_challenging_condition/links/5a2f81e50f7e9bfe81705387/Gut-microbiota-and-attention-deficit-hyperactivity-disorder-new-perspectives-for-a-challenging-condition.pdf?origin=publication_detail
Xijing Hospital. 2018. Gut Microbiome and Serum Metabolome Alterations in ADHD Patients (ADHD). https://clinicaltrials.gov/ct2/show/NCT03447223
The post How To Treat ADHD Naturally: 5 Most Important Steps appeared first on Meet Dr. Lauryn.
Source/Repost=>
https://drlauryn.com/family-kid-health/treat-adhd-naturally-5-essential-steps/ ** Dr. Lauryn Lax __Nutrition. Therapy. Functional Medicine ** https://drlauryn.com/
1 note
·
View note
Photo

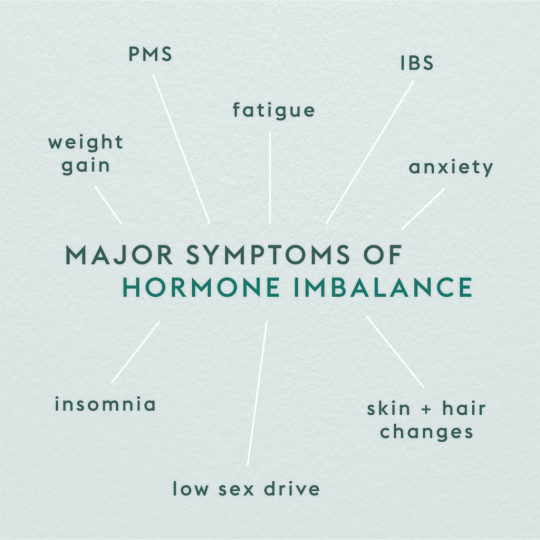
7 Signs You Have a Hormonal Imbalance
Hormones are the most potent chemical messengers in our bodies, telling your body what to do and when.
That’s why when your hormones are out of balance, you may be able to feel the effects, whether it be via insomnia, fatigue, weight gain, hair loss, or mood swings. But usually these imbalances are reversible—learn how to balance hormones naturally and turn your hormonal imbalance around.
Produced by our endocrine glands—adrenals, thyroid, pancreas, female or male reproductive system—hormones perform essential functions, relay important warnings and communicate messages throughout the body.
That means, they make sure everything is running smoothly and that your rhythms stay in sync.
Hormones can impact your:
Appetite
Metabolism
Heart rate
Sleep patterns
Reproduction
Mood
Many things can challenge your endocrine system, disrupting hormone balance and function. The longer a system is “out of order” the more difficult it can be to bring it back into harmony. Identifying and correcting the causes of hormonal imbalance early on will help maintain your health and prevent the onset of chronic disease.
Potential causes of a hormonal imbalance:
Underactive thyroid (hypothyroidism)
Overactive thyroid (hyperthyroidism)
Chronic stress
Diabetes
Birth control or hormonal replacement
Poor diet
Cushing syndrome
Exposure to endocrine disruptors
So how do you know if you have a hormone imbalance? Find out the signs of hormonal imbalance to look out for, and natural remedies for hormonal imbalance that can help.
Fatigue, weight gain, insomnia, PMS, or PCOS? We treat the root cause of hormonal imbalance so you can get back to feeling like yourself again. Check out www.nefariouss.com - Nutrition. All our listed products, help battle these issues.
7 signs and symptoms of hormonal imbalances
These seven major symptoms can help you determine if you have a hormonal imbalance.
1. Fatigue
Everyone is tired sometimes. But you should recover with adequate rest, hydration, and a healthy diet. If you feel you are taking care of yourself but are still exhausted or just can’t seem to get back to your best, consider having a comprehensive evaluation of your hormone levels. Adrenal fatigue and hypothyroidism are more prevalent in our high-paced society than you may think and a hormonal imbalance test can help diagnose this.
2. Anxiety
Nope, it’s not all in your head. Nearly 18 percent of Americans suffer from an anxiety-related disorder and 7 percent from a major depressive disorder each year. Women may be at a higher risk because changes in estrogen during menstrual cycles, pregnancy, or menopause are associated with worsening depression. A study on the effect of estrogen receptors in the brain found that estrogen calms the fear response and anxiety in both humans and rodents. Higher levels of estrogen were correlated less fearful responses when stimulated by fear-inducing scenarios. Men with low levels of testosterone are more prone to developing anxiety or major depressive discover when compared to those with normal levels.
3. Weight gain or difficulty losing weight
Why do so many people struggle with weight loss and maintenance? Usually, it’s because they are eating too little and working too hard. The body processes this hard work as stress and when the body is stressed, it goes into survival or “fight or flight” mode, producing cortisol. When you’re chronically stressed, your cortisol is always high and in an effort to protect itself from whatever danger it senses, your body holds onto fat as a form of energy.
4. Trouble sleeping
Insomnia can be linked to a dysregulated hypothalamic pituitary adrenal (HPA) axis, which is your central stress response system, where your endocrine system and central nervous system interact. It’s also responsible for regulating the sleep-wake cycle through the release of hormones, such as melatonin and cortisol. Melatonin works on the part of the brain that controls our circadian rhythm, allowing us to fall asleep faster and stay asleep longer. An inability to secrete melatonin may result in difficulty falling asleep or adjusting to a new sleep pattern. Similarly, when your cortisol levels are too high in the evening, you may have trouble falling asleep and feel wired but tired in the evening.
40 percent of women going through perimenopause, the phase in which your body is nearing menopause, also report sleep disturbances, such as waking up in the middle of the night with chills and drenched in sweat.
5. Digestive issues
There are more neurotransmitters in the gut than there are in the brain, so it should be no surprise that anxiety and depression are sometimes accompanied by digestive symptoms. Hormones influence gut function through the microbiome and bacterial system in our intestines, so a hormone imbalance can impact the population and function of the bacteria in your gut, leading to symptoms like bloating, diarrhea, or nausea.
6. Skin and hair changes
Acne. A sudden increase in acne is one easy way to identify a possible hormonal imbalance. One of the few hormones involved is androgens. Androgens, typically referred to as “male hormones,” but found in both males and females, regulate your skin’s sebum production., If your body produces androgens in excess, sebum can build up in your pores and cause a pimple to surface.
Hair loss. The quality and vitality of your hair is also directly related to your hormones. Thyroid abnormalities, for example, may cause dry hair or skin, thinning hair, or brittle nails. Hypothyroidism, hyperthyroidism, and parathyroid disorder can also cause hair loss.
7. PMS and low sex drive
Low testosterone, estrogen, and progesterone are all associated with a decreased sex drive in both men and women. This is especially common after age 50 when estrogen and testosterone production declines. Since estrogen is one of the main hormones regulating a woman’s menstrual cycle a decrease in production can also lead to irregular periods that are too long, too short, unpredictable, heavy, or painful, infertility, hot flashes, mood swings, or painful intercourse.
At Parsley Health, we work with our members who have hormone imbalances to naturally bring their hormones back into balance without the need for hormonal replacement medications. These are some of our tried and true strategies.
5 ways to balance your hormones naturally
1. Incorporate healthy fats into your diet.
Adding healthy polyunsaturated fats to your diet, such as omega-3 and omega-6 may help reduce your appetite and decrease your risk of obesity. Fatty acids signal the production of leptin, a hormone that reduces appetite by suppressing the area of the brain that controls our appetite and signals to us it’s time to eat. Without adequate healthy fats in your diet, you’re more likely to have low leptin levels, which can induce overeating and an inability to feel satiated. That may be one reason women have been experimenting with seed cycling for hormone balance.
2. Try adaptogenic herbs.
Next time you grab a coffee or matcha try adding in some adaptogenic herbs. Adaptogens have been shown to decrease levels of cortisol, a stress hormone secreted from our glands when we experience stress. Certain adaptogens can help regulate the hypothalamic-pituitary adrenal (HPA) axis which controls cortisol levels. Lowering your cortisol levels can help hormonal imbalance symptoms, such as fatigue or sleep issues. Consistently high levels of cortisol not only impact bodily functions associated with hormones, but can feed the beginnings of hyperglycemia and suppress immune and inflammatory responses. In a study looking at the impact of adaptogens on the central nervous system, Adapt 232/Chisan (a combination of Rhodiola rosea, Schisandra chinensis and Eleutherococcus senticosus extracts) was found to decrease cortisol levels and activate the body’s self defense mechanism in response to stress. Adaptogens that aid adrenal function include ashwagandha, ginseng, jiaogulan, Chinese licorice, reishi, and Rhodiola rosea.
3. Take a high-quality probiotic and incorporate fermented foods.
Taking a probiotic can help balance your gut microbiome and the amount of “good” versus “bad” bacteria that lives in your system. The greater the “good” bacteria, the easier it is on your digestive system to process food. Research has shown that estrogen-related imbalances might be able to be reversed with probiotic supplementation by restoring the set of bacteria known as estrobolome, which is responsible for metabolizing estrogen. Probiotics can also lessen the impact chronic stressors may have on the hypothalamic pituitary axis (our stress response system), which is why probiotics are starting to be considered a form of treatment for those dealing with depression and anxiety. Fermented foods, which also contain live bacteria, can also aid in the regulation of gut bacteria.
4. Supplement with Vitamin D.
A Vitamin D deficiency is more common than you may think, with over a billion people worldwide suffering from either a deficient or insufficient supply of this critical vitamin. Vitamin D plays an extremely important role in a number of bodily functions, such as immune function, cell differentiation, and inflammatory response. Low levels of Vitamin D have been associated with an increased risk in colon, prostate, and breast cancer, as well as tuberculosis, influenza, and heart disease. A relationship has also been found between hypothyroidism and a vitamin D deficiency.
Ideally, we would get our daily dose of Vitamin D from 10 to 30 minutes of uninterrupted sun exposure, but this is unrealistic for most, that’s why it’s important to take a Vitamin D3 supplement and eat foods rich in Vitamin D, such as eggs and salmon. It’s also important to note that as we age, our production of Vitamin D decreases, so make sure you’re monitoring your levels and getting them checked by your primary care provider.
5. Biohack your way to better sleep.
When life is busy, often the first thing we sacrifice is sleep. Sleep or rather inadequate sleep quickly throws our body off balance. This is why it’s one of the first things our doctors ask about when patients come in for their initial visit. In a small study testing the impact of prolonged sleep restriction, participants that slept only 4 hours versus 10 or 12 hours experienced an increase in ghrelin, a hormone responsible for appetite regulation, alongside a decrease in leptin, a hormone responsible for communicating satiation. For many of us, 10 or 12 hours might be hard to achieve. That’s why here at Parsley we recommend getting at least 8 hours of sleep per night. The benefits of adequate sleep will not only increase your glucose metabolism and leptin concentrations but increase your body’s secretion of growth hormones responsible for cell reproduction and regeneration, which all take place during periods of rest.
Final thoughts on hormonal imbalances.
Some of the most common symptoms of hormone imbalances include unexplained weight gain, fatigue, insomnia, and changes in hair, skin, and nails.
Root causes of hormonal imbalances include compromised gut health, high inflammation, and high stress levels.
Natural ways to balance your hormones include eating anti-inflammatory polyunsaturated fats, getting adequate sleep, and using supplements to fill in any nutritional gaps related to gut health and vitamin D levels.
0 notes
Text
Nutritional Causes of Cancer
It is still hard for many of us to believe disease and nutrition are intimately linked. One main reason is that our food supply has become contaminated with antibiotics, pesticides, herbicides, fungicides, many environmental poisons and heavy metals including neuro-toxic mercury. Foods like milk today carry radioactive iodine because when Fukushima blew up it cast out a huge amount of radioactive iodine, the kind that they do not like to talk about because it will be around for a million years. It got into the grass that cows eat so when we drink our milk it gets into our thyroid especially if we are iodine deficient, which most people are today.
Ultra-processed foods have been repeatedly tied to adverse health outcomes. Two new studies from France[1]and Spain[2], both published in the British Medical Journal, show that consuming convenient junk food has been linked to increased heart disease and early death. Junk food creates nutritional stress, which is a main cause of cancer.
Researchers found that those who consumed more than four servings a day of ultra-processed foods had a 62% increased risk of early mortality. Each additional serving of ultra-processed food, after four servings, increased mortality rates by 18%. So the more junk food you eat the greater the chance you will get cancer and die from it.
Poor diet is associated with 1 in 5 deaths worldwide, according to a new, large study. That’s equivalent to 11 million deaths a year, making unhealthy eating habits responsible for more deaths than tobacco and high blood pressure.
The strength of the cells adaptive capacity is directly related to nutritional sufficiency and proper cellular respiration that removes toxins and wastes through the cell wall. Dr. Joel D. Wallach says, “Our immune system requires all 90 nutrients (60 minerals, 16 vitamins, 12 essential amino acids and two essential fatty acids) to maintain and repair itself in order to protect us from infectious diseases.”
Sugar
Researchers at Huntsman Cancer Institute in Utah were one of the first to discover that sugar “feeds” tumors. According to the Credit Suisse Research Institute’s 2013 study, “Sugar: Consumption at a Crossroads,” as much as 40 percent of US healthcare expenditures are for diseases directly related to the over-consumption of sugar. The fact that sugar and obesity are linked to an increased risk of cancer is now well-recognized but oncologists still do not talk about diet to their patients.
Nearly two-thirds of obesity-related cancers, which include colon, rectum, ovary, and womb cancers — occur in North America and Europe. A more recent British report estimates obesity may result in an additional 670,000 cancer cases in the UK alone over the next 20 years.
According to a report on the global cancer burden, published in 2014, obesity is responsible for an estimated 500,000 cancer cases worldwide each year. Sugar causes inflammation and cancer is an inflammation. Sugar and inflammation lead to low oxygen conditions. Moderate carbohydrate restriction can reduce markers of chronic inflammation.
According to researchers at the University of California, San Francisco, sugar poses a health risk—contributing to around 35 million deaths globally each year. So high is its toxicity that it should now be considered a potentially toxic substance like alcohol and tobacco. Its link with the onset of diabetes is such that punitive regulations, such as a tax on all foods and drinks that contain “added’’ sugar, are now warranted researchers have concluded. They also recommend banning sales in or near schools, as well as placing age limits on the sale of such products.
Sugar turns the body into a suitable breeding ground for viruses, bacteria, fungi and cancer. Sugar plays a major role in the nation’s obesity crisis and everyone knows obesity increases the incidence of cancer. The more sugar we consume to greater our oxidative stress and inflammation.
We can prevent disease by eating well and help treat disease with concentrated nutritional substances, organic food, ketogenic diets for cancer patients, and even by fasting. Dr. Dominic D’Agostino, a researcher with the University of South Florida Morsani College of Medicine, said “cancer is starved” by eating a diet that is restricted in carbohydrates but high in certain fats. Cancer loves sugar so not eating any starves cancer.
Mineral Deficiencies
Minerals are the building blocks of our bodies. They are required for body structure, fluid balance, protein structures and to produce hormones. They are a key for the health of every body system and function. They act as co-factors, catalysts or inhibitors of all enzymes in the body.
Minerals help with everyday body processes, reduce risk of certain cancers, strengthen muscles and tissues, and help develop organs and tissues as well as keeping them from deteriorating. Without minerals we would not be able to survive.
Severe deficiencies in minerals are directly associated with higher incidence of cancer so it makes sense, no matter what cancer treatment you elect to go with, to use concentrated forms of minerals.
White sugar, as well as other white foods like white rice, bread, salt and pasta create magnesium deficiencies, which creates chronic inflammation in the body. Magnesium and other mineral deficiencies depress immune system strength, prevent cells from detoxifying—all helping the body slide slowly into cancer.
It is known by science that only a little selenium a day keeps death from cancer away and iodine is essential if one does not want to fall to thyroid, breast, ovarian and prostate cancer.
Selenium is Basic to Cancer Treatment
Science knows that people who live in areas of selenium-rich or magnesium-rich soils are many times less likely to get cancer. In the low-selenium classification, three times as many people died from cancer as in the high-selenium classification. One major study found cancer incidence and mortality 42% to 52% lower (respectively) when selenium was supplemented. People who had taken selenium had 63% fewer prostate cancers, 58% fewer colorectal cancers, 46% fewer lung cancers and overall 37% fewercancers. Selenium was found to reduce the risk of lung cancer to a greater degree than stopping smoking.
Magnesium is Basic to Cancer Treatment
Several studies have shown an increased cancer rate in regions with low magnesium levels in soil and drinking water as well. In Egypt the cancer rate was only about 10% of that in Europe and America. In the rural fellah it was practically nonexistent. The main difference was an extremely high magnesium intake of 2.5-3 g in these cancer-free populations, ten times more than in most western countries.
Coffee
A 2017 review of 201 coffee studies and 17 clinical trials, published in The BMJ, found coffee was “associated with a lower risk of several cancers, including prostate, endometrial, skin and liver cancer, as well as type 2 diabetes, gallstones, and gout.” Above that, the researchers discovered positive effects on brain health: Coffee consumption was linked to a lower risk of Parkinson’s disease, depression, and Alzheimer’s disease.
However, this is a good moment to say that whatever the studies say about this food or that lowering the risk of cancer, cancer rates have exploded in recent decades no matter how much coffee people drink. Humility is not found in numbers, medical science or medical practice. That is why we need to take everything and put it together to develop the best picture we can for our health and for our children.
Alcohol
According to data published in the British Journal of Cancer in 2002, 4% of all breast cancers in the United Kingdom—about 44,000 cases a year—are due to alcohol consumption.
Super-foods
Many centuries ago Hippocrates – Father of Western Medicine said: “Let your food be your medicine and let your medicine be your food.” Concentrated super-foods and concentrated minerals give us a way to practice what Hippocrates said. Spirulina, chlorella, wheat and barley grass juice, sprouts, hemp seed proteins, or one of many combination super-foods like Rejuvenate deliver enough nutrition to be considered a medicine. The secret is eating low on the food chain.
Eating the Sun
Dr. Joan Lappe and her colleagues looked prospectively at more than 400 postmenopausal women over a four-year period of time. Women in the study group were given 1100 IU of vitamin D and 1000 mg of calcium daily. The control group did not receive this. Results: Women who took the vitamin D and calcium reduced their rate of cancer by 60%. The authors found that for every 10 ng/ml increase in a woman’s vitamin D blood level, the relative risk of cancer dropped by 35%.
Whenever there are no clouds blocking the sunrise I literally eat the sun each morning with the ancient practice of solar gazing. For about five minutes I stare directly into the sun clearing my mind of all thoughts. One should not be afraid of the sun but fear dermatologists who teach one to cover oneself with toxic sunscreens. Recently medical science has shown that indeed the chemicals do enter the blood. When we get to the tenth cause of cancer, doctors, our first example is doctors telling us to stay out of the sun or when we are out in it to cover our skin thus lowering our vitamin D blood levels.
Conclusion
The secret to recovery from all diseases is found in healing through the fulfillment of nutritional law. There is no comparison between using drugs with devastating side effects, even at low dosage, and concentrated natural nutritional substances, which can be used at exceptionally high dosages. Nutrition is life serving whereas pharmaceuticals are mitochondrial poisons.
That said, note that though food is medicinal it is extremely hard to eat oneself out of cancer (Gerson Method) or totally prevent cancer with the foods one eats, though of course it is possible. The right foods will go a long way but in the face of environmental poisons and emotional stress and trauma we need a lot of extra help. Many times I have met perfect eaters who were not perfect in their consciousness and thus suffered all kinds of different disorders. Food only goes so far in helping us resolve or prevent cancer. However, when one considers oxygen as a food and hydrogen as a food we can see how these ‘medicines’ that are food in gas form can be very helpful in treating cancer. (See low oxygen as a cause of cancer.)
Dr. Mark Sircus AC., OMD, DM (P)
References (2)
Ultra-processed food intake and risk of cardiovascular disease: prospective cohort study (NutriNet-Santé) BMJ 2019; 365 doi: https://doi.org/10.1136/bmj.l1451(Published 29 May 2019)
Association between consumption of ultra-processed foods and all cause mortality: SUN prospective cohort study. BMJ 2019; 365 doi: https://doi.org/10.1136/bmj.l1949 (Published 29 May 2019)
Related Posts
Sugar and Cancer Growth Research
Orthodox Cancer Treatments Don’t Treat Cancer
Dr. von Ardenne on Cancer, Inflammation and Oxygen
Oxygen and Cancer
from WordPress https://ift.tt/2XR9ijU
via IFTTT
0 notes
Text
Can Gluten Affect Your Hormones?
How Gluten Affects Your Hormones
Hormones are chemicals produced by various glands throughout your body and released to regulate specific functions. For example, your thyroid hormone helps regulate your metabolism. Estrogen, a sex hormone, helps regulate menstruation in women. And cortisol, a stress hormone, helps regulate blood pressure. Thus, hormones play many vital roles, which means any imbalances can lead to dysfunction and disease.
Symptoms of Hormonal Imbalances
A hormone imbalance occurs when there’s too much or not enough of a specific hormone circulating in your bloodstream at a specific time. For example, estrogen rises and falls twice throughout your menstrual cycle. And insulin rises after you eat and falls hours later.
Sadly, hormonal imbalances are prevalent in today’s modern world. Common symptoms include (but are not limited to):
Painful and/or irregular periods
Infertility
Low libido
Headaches
Fatigue
Weight gain
Mood swings and irritability
Insomnia
Skin rashes, dry skin, and acne
Brain fog
Hair loss
Anxiety and depression
Hot flashes
Muscle aches and stiffness
Constipation or diarrhea
And while these symptoms are common, they’re not normal. These are signs that something isn’t quite right.
Causes of Hormonal Imbalances
There are many avenues to explore when it comes to hormonal imbalances. Stress, environmental toxins, disease, medications, and physical injuries to glands. But one that often gets overlooked is nutrition. And gluten alone can cause a wide range of hormonal problems.
Nutrition and Your Hormones
Your diet plays a significant role in hormone health. For example, your body needs certain nutrients to synthesize hormones. Steroid hormones, such as estrogen and testosterone, are made from cholesterol. And insulin is made from protein.
Vitamins and minerals also regulate the synthesis of hormones. For instance, in the absence of iodine, your thyroid hormone production decreases. Therefore, an iodine deficiency can lead to hypothyroidism (a.k.a. under active or low thyroid).
This is relevant because those with gluten sensitivity often experience nutrient deficiencies. Essentially, gluten irritates and damages the lining of the small intestine. And the small intestine is responsible for a significant portion of digestion and nutrient absorption.
Plus, grain-based foods, such as bread, pasta, crackers, and sweets, are heavily processed and void of essential nutrients.
Gluten is an Endocrine Disruptor
An endocrine disruptor is a substance that can mimic your hormones and lead to imbalances, dysfunction, and disease. For instance, they can bind to hormone receptors on your cells and trigger a response. Sometimes the response may be too strong, not strong enough, or different than desired.
Gluten itself can act as an endocrine disruptor. More specifically, gluten proteins may cross-react with antigens on your cells and trigger an inflammatory immune response. This helps explain why several common abnormalities among those with celiac disease are hormonal in nature, including delayed puberty, type 1 diabetes, low thyroid, and low cortisol.
Wheat is also sprayed with an herbicide known as glyphosate before harvesting to help speed up the drying process. And glyphosate is a known hormone disruptor in human cells. Plus, it’s toxic effects can also damage your DNA.
In addition, some pesticides used to grow grains can also have endocrine-disrupting effects. And studies have shown they can alter the synthesis or action of a wide range of hormones, including estrogen, testosterone, thyroid hormone, cortisol, progesterone, and prolactin.
Gluten and Cortisol Imbalances
As previously mentioned, cortisol is a stress hormone produced and secreted by your adrenal glands. Cortisol naturally rises and falls throughout the day. At normal levels, cortisol helps regulate your metabolism, blood pressure, and blood sugar. It also helps reduce inflammation.
However, when under stress, a cascade of events triggers your adrenal glands to release adrenaline and increase the output of cortisol to support your body’s “fight or flight” response.
This response is necessary to combat acute stress. For example, cortisol raises your blood sugar to ensure you have the energy you need to overcome the threat at hand. However, many people today are under constant stress, whether it be emotional, physical, or often a combination of both.
Chronic inflammation caused by gluten is a form of physical stress, which can raise your cortisol levels. If untreated, the consequences are far-reaching. For example, elevated cortisol hinders digestion, growth, and reproduction as well as immune function. There’s even a connection to a region in the brain that controls your mood.
Thus, symptoms associated with high cortisol include anxiety, depression, weight gain, digestive dysfunction, poor sleep, muscle weakness, and lack of focus among others. High cortisol is also associated with high blood pressure, heart disease, diabetes, hirsutism in women (excessive growth of dark, thick hair), and osteoporosis.
On the other hand, celiac disease is associated with Addison’s disease, an autoimmune condition that attacks your adrenal glands and causes low cortisol (a.k.a. adrenal insufficiency).
An animal study found that glyphosate directly influenced the adrenal glands, which led to abnormally low levels of cortisol. The symptoms mimicked adrenal insufficiency, which caused fatigue, anxiety, sweating, and weight loss. Other symptoms of adrenal insufficiency include low blood sugar, dehydration, and low blood pressure.
In addition, nutrient deficiencies caused by gluten can play a role in the development of Addison’s disease. For example, vitamin D appears to be involved in regulating genes responsible for the synthesis of cortisol.
Gluten and Sex Hormone Imbalances
The three sex hormones are estrogen, progesterone, and testosterone. They play a role in the development of sex distinguishing features as well as reproduction. Thus, common abnormalities and conditions associated with sex hormone imbalances include:
Infertility
Premenstrual syndrome (PMS)
Headaches
Irregular or missing periods
Polycystic ovary syndrome (PCOS)
Low libido
Your sex hormones may be affected by endocrine disruptors as I mentioned above. Gluten-induced inflammation, an overactive immune system, other hormonal imbalances (e.g., cortisol, thyroid hormone, prolactin), and nutrient deficiencies are also potential problems. This may help explain why those with celiac disease and gluten sensitivity are prone to the abnormalities listed above.
Science tells us that women with celiac disease are more likely to experience infertility and menstrual abnormalities than the general population. And these conditions are commonly linked to low progesterone, low thyroid hormone, and high prolactin.
If untreated, celiac disease also appears to increase a woman’s risk of abnormal fetal growth, unexplained miscarriage, and preterm birth.
A study comparing pregnancy outcomes of mothers with celiac disease on a gluten-free diet versus untreated mothers found the following:
The relative risk of miscarriage was 8.9 times higher in the untreated group
The relative risk of low birth weight was 5.84 times higher in the untreated group
The duration of breastfeeding was 2.54 times shorter in the untreated group
These are significant consequences. However, the same researchers also found that these outcomes were corrected with a gluten-free diet.
The exact mechanisms behind these correlations are not fully understood yet. But researchers believe an overactive immune system plays a role.
For example, one study found that celiac disease autoantibodies were binding to the placenta and causing dysfunction. And it’s worth noting that once established, the placenta is responsible for producing both progesterone and estrogen.
Another study analyzed the placentas from 32 full-term births of mothers with celiac disease. Of the mothers with untreated cases, researchers found large concentrations of gliadin, a gluten protein, in the cells of the placenta. And the birth weights of the babies in these cases were lower. This may suggest that gluten proteins interact unfavorably with the placenta in genetically susceptible women.
Gluten and Thyroid Hormone
Hypothyroidism is a condition in which your thyroid gland fails to produce enough thyroid hormone, which can cause most of the symptoms I listed in the introduction of this article. This is possible because your thyroid hormone helps regulate many functions, including your metabolism, brain development, protein synthesis, and bone growth to name a few.
There are four main causes of thyroid hormone dysfunction, which include:
Autoimmune disease (a.k.a. Hashimoto’s)
Nutrient deficiencies that affect the production, regulation, and/or activation of thyroid hormone
Chemical exposures/endocrine disruptors (e.g., glyphosate)
Physical damage to the thyroid gland
Autoimmune Thyroid Disease
Celiac disease is associated with many other autoimmune diseases, including Hashimoto’s. Essentially, damage to the lining of the gut leads to inflammation, over stimulation of the immune system, and cross-reactivity of gluten proteins with antigens on the thyroid gland. If unchecked, Hashimoto’s is likely to develop.
Science has shown that women with autoimmune thyroid disease that were put on a gluten-free diet experienced a reduction in antibodies that attack the thyroid as well as an increase in thyroid hormone and vitamin D. However, women in a control group that kept gluten in their diet didn’t experience any of these clinical changes.
Another study evaluated a diet without gluten and found that it significantly reduced markers associated with inflammation and immune system activation in women with Hashimoto’s. Plus, the women in the study experienced a reduction in related symptoms.
Nutrient Deficiencies and Thyroid Hormone
As previously mentioned, gluten can cause nutrient deficiencies. One nutrient specifically that greatly affects the thyroid is selenium. It’s necessary for the production and activity of thyroid hormone. Selenium also acts as an antioxidant and helps protect the thyroid gland from damage. Thus, gluten-induced selenium deficiency is believed to lead to thyroid dysfunction.
Other common nutrient deficiencies caused by gluten that are necessary for optimal thyroid function include magnesium, zinc, vitamin D, and vitamin B12.
Gluten and Insulin
When you eat a diet rich in heavily processed gluten-rich foods, it has a negative impact on your metabolic hormones. Because these foods contain high amounts of quickly digested starch and sugar, which spikes your insulin and can lead to chronically high insulin levels over time.
Insulin is a fat-storing hormone secreted by your pancreas. It pushes all sources of energy into your cells and excess energy gets stored as fat. It also prevents your body from burning stored fat.
If unchecked, insulin resistance, obesity, and type 2 diabetes are likely to develop. All of these conditions are inflammatory. Insulin resistance is also closely linked to polycystic ovarian syndrome (PCOS), which is characterized by elevated testosterone in women that causes infertility, hirsutism, and abnormal periods.
Gluten and Prolactin
The last hormone I want to discuss is prolactin–a hormone secreted by your pituitary gland that works with estrogen and progesterone to develop breast tissue and prepare for lactation.
There’s evidence that a compound in gluten acts as an opioid compound in the brain, which leads to an excess of prolactin. Researchers also suggest inflammation associated with gluten can contribute to elevated prolactin levels, which can cause low libido, irregular periods, infertility, bone loss, and erectile dysfunction.
Can Gluten Affect Your Hormones?
Hormonal balance is essential for optimal health. And gluten can affect many hormones throughout your body as well as trigger a cascade of hormone-related problems. Thus, if you’re experiencing any hormonal imbalance symptoms, don’t rule gluten out as a contributing factor. A gluten-free diet may be what your body needs most.
Have you recovered hormone function after going gluten free? Chime in below.
The post Can Gluten Affect Your Hormones? appeared first on Gluten-Free Society.
0 notes
Text
How To Treat ADHD Naturally: 5 Most Important Steps
Is there a way to treat ADHD naturally? What one should do?More than 1 in 10 children, ages 4-17 have ADHD (attention deficit hyperactivity disorder) (1), defined as “limited attention and hyperactivity.”
Common characteristics of ADHD include:
Difficulty sustaining attention or focusing
Difficulty following through with tasks
Hyperactivity
Difficulty organizing self and tasks
Impulsive behavior
To officially be diagnosed with ADHD, symptoms must persist for at least 6 months, and behaviors and symptoms must be abnormal for children of the same age and negatively affect his or her school, home life or relationships in more than one setting (i.e. at home and at school).
Unfortunately, for many of these kids who are diagnosed, ADHD will continue into their adulthood, and conventional medicine believes that the disease is “manageable, but not curable.” In order to help kids “manage” their ADHD, treatment typically consists of medications and behavioral interventions, such as occupational therapy, behavioral therapy and sensory or movement “breaks.”
After those options are exhausted however, there is little, if anything else doctors say they can do.
The missing link most docs and conventional medicine is not talking about?
A little superpower known as the “brain gut connection.”
According to the latest in research about the brain-gut connection, ADHD is not only manageable, but it is reversible and remissible.
In this article we’ll cover the basics about the brain-gut connection, plus learn 5 essential steps to treat ADHD naturally (that your doctor probably won’t tell you about).
THE BRAIN GUT CONNECTION
The “brain-gut” connection is essentially what it sounds like: Your gut and brain are directly linked.
Your vagus nerve (the nerve responsible for directing how you think and your brain function) is connected from your frontal brain lobe to the top stomach. In addition, about 95% of your serotonin (“feel good” brain chemical) is produced in your gastrointestinal tract.
Couple this with the fact that your gastrointestinal tract is lined with more than a 100 million nerve cells, and it makes sense: the inner workings of your digestive system don’t just help you digest food, but also guide your emotions.
In short: When your gut is unhappy or stressed…your brain is unhappy or stressed.
Enter: The “brain-gut connection.”
Inflammation in your gut sends signals to your brain, causing a similar response (inflammation, stress and in many children’s cases, anxiety, sensory processing disorders, and ADHD).
The bottom line: If you have an unhealthy gut, your brain function gets thrown off. And, if you have an unhealthy brain (i.e. stressed), your gut function can also get thrown off.
THE MISSING LINKS IN ADHD TREATMENT: GUT HEALTH & STRESS
Unfortunately, for years, we’ve come to see the body and mind as two separate entities.
The mind is often treated separately from the body, other than using medications to suppress “neuro-chemical imbalances.” Patients with ADHD or other mood disorders and mental illnesses are then typically referred out to see a psychotherapist or occupational therapist to address “behavior” and emotional issues, in hopes of remediating the symptoms, with sub-par results or a lifetime spent in therapy, using coping strategies and taking medications.
From a functional medicine perspective, we want to address ADHD and other mental health conditions in the same way that we address any other health condition (i.e. autoimmune disease, diabetes, GERD, hypertension, etc.). We want to look at what the underlying causes are for these conditions. This is essential to treat ADHD naturally.
While mental illness, like ADHD, is a complex combination of various genetic and epigenetic factors, (including nutritional, physical, biochemical, environmental, social, emotional, and spiritual influences), many traditional methods of diagnosis and treatment fail to address two of the biggest drivers of disease: gut health and chronic inflammation (i.e. stress).
Our stress levels and gut health are the gateways to health.
In fact, the American Psychological Association estimates that 99% of ALL disease is attributed to stress alone (2). Stress is defined as any “outside force that exceeds the body’s ability to recover or maintain homeostasis.”
Just like the “stress” of a poor quality diet, lack of sleep and sedentary lifestyle leads to conditions like diabetes and high blood pressure, and just like poor gut health, such as “intestinal permeability” (leaky gut) is connected to conditions like autoimmune disease, skin breakouts and anxiety, stress levels and gut health play a key role in ADHD.
STRESS 101
Contrary to popular belief, “stress” goes far beyond mental stress. Physiological stress equally imbalances the optimal function of the body—brain balance included. Common sources of physical stress and inflammation for many ADHD sufferers include:
Inadequate sleep or poor quality sleep. More than half of kids do NOT get 8-9 hours of quality sleep. (3)
Sedentary lifestyles. Kids are moving less than ever before with 1 in 5 getting the recommended minimum of 60-minutes of physical activity 5 days per week. (4)
Overexposure to screens and blue lights. The average kid spends 6-9 hours/day in front of a screen. (5)
Lack of spontaneous play and time in nature. Only 10% of kids spend time outside every day (6) and a 2018 Gallup study found that children nationwide spend less time on creative play than ever before, spending 18.6 hours each week to screen-based play per week, versus 14.6 hours on indoor screen-free play (7).
Antibiotic drug exposure. 1 in 4 kids get antibiotics every year that are unnecessary and 5 in 6 kids take an antibiotic every year (8).
Poor quality nutrition and processed foods. Nearly 50% of kids’ diets, ages 2-18 consist of empty calories from added sugars and and processed foods including: soda, fruit drinks, dairy desserts, grain desserts, pizza, and conventional milk (9).
Poor gut health. Including about 2 in 5 kids with constipation (10), 1 in 4 with GERD or “reflux” (11) and millions of kids with allergies and asthma—the #1 “chronic disease” of kids nationwide (12) (linked to poor gut health) (13, 14).
GUT HEALTH 101
Much of the chronic diseases we face today can also be traced back to our gut health, including ADHD. If we could address the problems in our gut, we can find the right ways to treat ADHD naturally.
The human gut contains more than 100 trillion gut bacteria—up to 10 times more bacteria than human cells in our blood stream and body.
The healthier and more diverse your gut bacteria, the healthier your body is overall. However, the less healthy or less diverse your gut bacteria, the less healthy or “out of balance” you are.
Our gut bacteria influence the health of our:
Blood sugar and insulin levels
Hormone health
Thyroid
Detoxification
Mood
Immune system (allergies, skin health)
Digestion
Mental health
How do gut bacteria get unhealthy in the first place? Go back to the topic of stress! It’s a vicious cycle, but common sources of “unhealthy gut bacteria” include:
Poor sleep
Poor quality foods (packaged, processed, conventional meat, dairy, sweeteners, etc.)
Environmental toxins (additives, plastics, medicines, toxic cleaning and hygiene products)
C-section births and processed formula feedings as a baby
Infection & Illness
Sedentary lifestyles
Antibiotics
Underlying gut pathologies, often caused by stressors (parasites
The good news? If we address the gut health, then we could treat ADHD naturally—if not reversed.
Research backs this up.
SURVEY SAYS: ADHD & GUT RESEARCH
A 2017 peer-reviewed study found significant connections between increased gut inflammation and test subjects with ADHD, regardless of age and previous diagnosis (15). The volunteers with ADHD had more Bifidobacterium genus, often associated with SIBO or small intestinal bacterial overgrowth (16).
In another review in the European Child & Adolescent Psychiatry Journal, researchers state that while studies on ADHD and the gut microbiota in patients is budding, there is clear evidence about the link between obesity and ADHD and between obesity and alteration of the gut microbiota.
There is a way to treat ADHD naturally.
Obesity induces a low-grade inflammatory state which has been associated with behavioral and cognitive alterations, being gut micro-biota most likely an important mediator between inflammation and altered behaviors.
Overall, data from gluten-free mice studies, antibiotic treatment studies, and probiotic interventions suggest that alterations in gut microbiota that reduce the inflammatory state also reduce stress-related behaviors, supporting the role of the gut microbiota as a mediator between inflammation and behavioral alterations.
And, another clinical trial (18) is currently underway, as researchers have concluded from previous research that ADHD is in are linked to shifts in gut microbiota composition.
5 ESSENTIAL STEPS TO TREAT ADHD NATURALLY
The main strategy to heal and treat ADHD naturally involve balancing out stress levels, and NOT irritating the gut barrier and gut immune system. Here are 5 essential steps to start.
STEP 1: EAT REAL FOOD (ESPECIALLY FATS & PROTEINS)
When we eat, we not only feed ourselves, but we also feed our gut bugs. This is a crucial step to treat ADHD naturally. It’s not rocket science: Real, whole, nutrient-dense foods make an unhealthy gut a healthier gut. While most kids’ favorite foods include chicken nuggets, mac and cheese, French fries, Honey Nut Cheerios, possibly fruit and anything with ketchup, they are humans too.
And humans were wired to eat real foods. Real foods include: sustainable, organic meats and fish, colorful fruits and veggies and essential healthy fats (coconut oil, ghee, grass-fed butter, pastured egg yolks, avocado, raw nuts and seeds.
STEP 2: CUT OUT THE CULPRITS
This goes beyond just going a gluten-free (since many gluten free products contain just as many additives as the gluten version)s. Experiment with cutting out grains, conventional dairy, sugar and additives (dyes, sweeteners, chemicals) for 30 days and watch your kids’ brains come to life. Do it together with a non-diet mentality as a challenge for the family for stronger bodies and better brains. A great way to help treat ADHD naturally.
STEP 3: LOVE YOUR GUT BUGS
Give your kids a daily soil-based probiotic and prebiotic fiber to treat ADHD naturally. These include partially hydrolyzed guar gum, to help the healthy probiotics stick in their gut. Soil based probiotics are typically better tolerated by most people, and contain probiotic like cultures that were once found in the rich soils of our ancestors. Start with 1/2 capsule of a probiotic, 2 times per day, and 1 teaspoon of a prebiotic. Other “gut loving” additions include:
Colostrum (similar to the gut-healing natural colostrum found in the “perfect food:” a mother’s milk)
Digestive Enzymes (support natural enzymes that help break down food)
Betaine HCL (hydrochloric acid) found in capsules (naturally boosts stomach acid to enhance digestion)
Optional: Digestive “bitters” to support detoxification mixed into homemade dark chocolate syrup (5 drops of bitters + 1 tablespoon cacao powder + 1 tablespoon raw honey (use maple syrup for kids under 1 year of age) +fresh juice from half a small lemon)
STEP 4: DESTRESS
For kids, this includes encouraging them to get 60-minutes (at least) of active play and exercise each day, as well as outdoor time and sunshine, about 9 hours of sleep each night and creative, imaginative playaway from screens.
Magnesium Citrate at night is also a natural calming mineral, mixed into bedtime tea or water.
STEP 5: TEST, DON’T GUESS
Work with a functional medicine practitioner or healthcare practitioner knowledgeable in gut health analysis and treatment of any underlying conditions that may play a role in your child’s brain-gut-connection. Lab tests may include: Stool testing, Organic Acids Urine Testing, Comprehensive Bloodwork Analysis, Food Sensitivity Testing, and Small Intestinal Bacterial Overgrowth Breath Testing. This can help to treat ADHD naturally.
Not all tests are essential, but can give you and your child a clearer picture into their unique presentation if an underlying gut pathology is behind their condition. (Note: Many traditional GI doctors do not perform these tests on kids, beyond food allergy, not sensitivity, testing and potential scope and CT scan imaging).
The bottom line:
In the end, address the roots of cognitive imbalance first (gut and stress), not the symptoms. This is very important step to treat ADHD naturally.
Resources:
2018. ADHD. https://www.cdc.gov/ncbddd/adhd/data.html.
2018. How Stress Affects Your Health. https://www.apa.org/helpcenter/stress-facts.pdf; American Institute of Stress. https://www.stress.org/americas-1-health-problem/ (Cited: Perkins (1994) showed that 60% to 90% of doctor visits were stress-related)
Sleep Foundation. 2010. Sleep in America. http://sleepfoundation.org/sites/default/files/2014-NSF-Sleep-in-America-poll-summary-of-findings—FINAL-Updated-3-26-14-.pdf
2018. Physical Activity Facts. https://www.cdc.gov/healthyschools/physicalactivity/facts.htm
Kaiser Family Foundation. Generation M2: Media in the Lives of 8-18-year-olds. 2010 https://kaiserfamilyfoundation.files.wordpress.com/2013/04/8010.pdf
The Nature Conservancy. Connecting America’s Youth to Nature. 2011. https://www.nature.org/newsfeatures/kids-in-nature/youth-and-nature-poll-results.pdf
Doug & Melissa. 2018. Time to Play Study. http://ww2.melissaanddoug.com/MelissaAndDoug_Gallup_TimetoPlay_Study.pdf
2017. Antibiotic Use in the United States, 2017: Progress and Opportunities. https://www.cdc.gov/antibiotic-use/stewardship-report/outpatient.html
Facts & Statistics: Physical Activity. 2018. https://www.hhs.gov/fitness/resource-center/facts-and-statistics/index.html (Cited Source: Reedy J, Krebs-Smith SM. Dietary sources of energy, solid fats, and added sugars among children and adolescents in the United States. Journal of the American Dietetic Association, Volume 110, Issue 10, Pages 1477-1484, October 2010. Available at: http://www.ncbi.nlm.nih.gov/pubmed/20869486.)
Blackmer AB, Farrington EA. Constipation in the pediatric patient: an overview and pharmacologic considerations. Journal of Pediatric Health Care. 2010;24(6):385–399.
Nelson SP, Chen EH, Syniar GM, Christoffel KK. Pediatric Practice Research Group. Prevalence of symptoms of gastroesophageal reflux during childhood. Archives of Pediatric and Adolescents Medicine. 2000;154:150–154
Asthma & Allergy Foundation. 2018. Allergy Facts and Figures. http://www.aafa.org/page/allergy-facts.aspx
Volz, F. Wölbing, F. Regler, S. Kaesler, T. Biedermann. 232 NOD2 signaling critically influences sensitization to orally ingested allergens and severity of anaphylaxis. Journal of Investigative Dermatology, 2016; 136 (9): S201 DOI: 10.1016/j.jid.2016.06.252
Neonatal gut microbiota associates with childhood multisensitized atopy and T cell differentiation. Fujimura KE, Sitarik AR, Havstad S, Lin DL, Levan S, Fadrosh D, Panzer AR, LaMere B, Rackaityte E, Lukacs NW, Wegienka G, Boushey HA, Ownby DR, Zoratti EM, Levin AM, Johnson CC, Lynch SV. Nat Med. 2016 Sep 12. doi: 10.1038/nm.4176. [Epub ahead of print]. PMID: 27618652.
Aarts, E., Ederveen, T. H. A., Naaijen, J., Zwiers, M. P., Boekhorst, J., Timmerman, H. M., … Arias Vasquez, A. (2017). Gut microbiome in ADHD and its relation to neural reward anticipation. PLoS ONE, 12(9), e0183509. http://doi.org/10.1371/journal.pone.0183509
Quigley & Quera. 2006. Small Intestinal Bacterial Overgrowth: Roles of Antibiotics, Prebiotics, and Probiotics. http://www.deerlandenzymes.com/wp-content/uploads/2015/04/Small-Intestinal-Bacterial-Overgrowth-Roles-of-Antibiotics-Prebiotics-and-Probiotics.pdf
Carmen Cenit, María & Campillo Nuevo, Isabel & codoñer-franch, Pilar & G. Dinan, Timothy & Sanz, Yolanda. (2017). Gut microbiota and attention deficit hyperactivity disorder: new perspectives for a challenging condition. European Child & Adolescent Psychiatry. 26. 10.1007/s00787-017-0969-z. https://www.researchgate.net/profile/Pilar_Codoner-franch/publication/314967081_Gut_microbiota_and_attention_deficit_hyperactivity_disorder_new_perspectives_for_a_challenging_condition/links/5a2f81e50f7e9bfe81705387/Gut-microbiota-and-attention-deficit-hyperactivity-disorder-new-perspectives-for-a-challenging-condition.pdf?origin=publication_detail
Xijing Hospital. 2018. Gut Microbiome and Serum Metabolome Alterations in ADHD Patients (ADHD). https://clinicaltrials.gov/ct2/show/NCT03447223
The post How To Treat ADHD Naturally: 5 Most Important Steps appeared first on Meet Dr. Lauryn.
Source/Repost=>
https://drlauryn.com/family-kid-health/treat-adhd-naturally-5-essential-steps/ ** Dr. Lauryn Lax __Nutrition. Therapy. Functional Medicine ** https://drlauryn.com/
How To Treat ADHD Naturally: 5 Most Important Steps via https://drlaurynlax.weebly.com/
0 notes
Text
How To Treat ADHD Naturally: 5 Most Important Steps
Is there a way to treat ADHD naturally? What one should do?More than 1 in 10 children, ages 4-17 have ADHD (attention deficit hyperactivity disorder) (1), defined as “limited attention and hyperactivity.”
Common characteristics of ADHD include:
Difficulty sustaining attention or focusing
Difficulty following through with tasks
Hyperactivity
Difficulty organizing self and tasks
Impulsive behavior
To officially be diagnosed with ADHD, symptoms must persist for at least 6 months, and behaviors and symptoms must be abnormal for children of the same age and negatively affect his or her school, home life or relationships in more than one setting (i.e. at home and at school).
Unfortunately, for many of these kids who are diagnosed, ADHD will continue into their adulthood, and conventional medicine believes that the disease is “manageable, but not curable.” In order to help kids “manage” their ADHD, treatment typically consists of medications and behavioral interventions, such as occupational therapy, behavioral therapy and sensory or movement “breaks.”
After those options are exhausted however, there is little, if anything else doctors say they can do.
The missing link most docs and conventional medicine is not talking about?
A little superpower known as the “brain gut connection.”
According to the latest in research about the brain-gut connection, ADHD is not only manageable, but it is reversible and remissible.
In this article we’ll cover the basics about the brain-gut connection, plus learn 5 essential steps to treat ADHD naturally (that your doctor probably won’t tell you about).
THE BRAIN GUT CONNECTION
The “brain-gut” connection is essentially what it sounds like: Your gut and brain are directly linked.
Your vagus nerve (the nerve responsible for directing how you think and your brain function) is connected from your frontal brain lobe to the top stomach. In addition, about 95% of your serotonin (“feel good” brain chemical) is produced in your gastrointestinal tract.
Couple this with the fact that your gastrointestinal tract is lined with more than a 100 million nerve cells, and it makes sense: the inner workings of your digestive system don’t just help you digest food, but also guide your emotions.
In short: When your gut is unhappy or stressed…your brain is unhappy or stressed.
Enter: The “brain-gut connection.”
Inflammation in your gut sends signals to your brain, causing a similar response (inflammation, stress and in many children’s cases, anxiety, sensory processing disorders, and ADHD).
The bottom line: If you have an unhealthy gut, your brain function gets thrown off. And, if you have an unhealthy brain (i.e. stressed), your gut function can also get thrown off.
THE MISSING LINKS IN ADHD TREATMENT: GUT HEALTH & STRESS
Unfortunately, for years, we’ve come to see the body and mind as two separate entities.
The mind is often treated separately from the body, other than using medications to suppress “neuro-chemical imbalances.” Patients with ADHD or other mood disorders and mental illnesses are then typically referred out to see a psychotherapist or occupational therapist to address “behavior” and emotional issues, in hopes of remediating the symptoms, with sub-par results or a lifetime spent in therapy, using coping strategies and taking medications.
From a functional medicine perspective, we want to address ADHD and other mental health conditions in the same way that we address any other health condition (i.e. autoimmune disease, diabetes, GERD, hypertension, etc.). We want to look at what the underlying causes are for these conditions. This is essential to treat ADHD naturally.
While mental illness, like ADHD, is a complex combination of various genetic and epigenetic factors, (including nutritional, physical, biochemical, environmental, social, emotional, and spiritual influences), many traditional methods of diagnosis and treatment fail to address two of the biggest drivers of disease: gut health and chronic inflammation (i.e. stress).
Our stress levels and gut health are the gateways to health.
In fact, the American Psychological Association estimates that 99% of ALL disease is attributed to stress alone (2). Stress is defined as any “outside force that exceeds the body’s ability to recover or maintain homeostasis.”
Just like the “stress” of a poor quality diet, lack of sleep and sedentary lifestyle leads to conditions like diabetes and high blood pressure, and just like poor gut health, such as “intestinal permeability” (leaky gut) is connected to conditions like autoimmune disease, skin breakouts and anxiety, stress levels and gut health play a key role in ADHD.
STRESS 101
Contrary to popular belief, “stress” goes far beyond mental stress. Physiological stress equally imbalances the optimal function of the body—brain balance included. Common sources of physical stress and inflammation for many ADHD sufferers include:
Inadequate sleep or poor quality sleep. More than half of kids do NOT get 8-9 hours of quality sleep. (3)
Sedentary lifestyles. Kids are moving less than ever before with 1 in 5 getting the recommended minimum of 60-minutes of physical activity 5 days per week. (4)
Overexposure to screens and blue lights. The average kid spends 6-9 hours/day in front of a screen. (5)
Lack of spontaneous play and time in nature. Only 10% of kids spend time outside every day (6) and a 2018 Gallup study found that children nationwide spend less time on creative play than ever before, spending 18.6 hours each week to screen-based play per week, versus 14.6 hours on indoor screen-free play (7).
Antibiotic drug exposure. 1 in 4 kids get antibiotics every year that are unnecessary and 5 in 6 kids take an antibiotic every year (8).
Poor quality nutrition and processed foods. Nearly 50% of kids’ diets, ages 2-18 consist of empty calories from added sugars and and processed foods including: soda, fruit drinks, dairy desserts, grain desserts, pizza, and conventional milk (9).
Poor gut health. Including about 2 in 5 kids with constipation (10), 1 in 4 with GERD or “reflux” (11) and millions of kids with allergies and asthma—the #1 “chronic disease” of kids nationwide (12) (linked to poor gut health) (13, 14).
GUT HEALTH 101
Much of the chronic diseases we face today can also be traced back to our gut health, including ADHD. If we could address the problems in our gut, we can find the right ways to treat ADHD naturally.
The human gut contains more than 100 trillion gut bacteria—up to 10 times more bacteria than human cells in our blood stream and body.
The healthier and more diverse your gut bacteria, the healthier your body is overall. However, the less healthy or less diverse your gut bacteria, the less healthy or “out of balance” you are.
Our gut bacteria influence the health of our:
Blood sugar and insulin levels
Hormone health
Thyroid
Detoxification
Mood
Immune system (allergies, skin health)
Digestion
Mental health
How do gut bacteria get unhealthy in the first place? Go back to the topic of stress! It’s a vicious cycle, but common sources of “unhealthy gut bacteria” include:
Poor sleep
Poor quality foods (packaged, processed, conventional meat, dairy, sweeteners, etc.)
Environmental toxins (additives, plastics, medicines, toxic cleaning and hygiene products)
C-section births and processed formula feedings as a baby
Infection & Illness
Sedentary lifestyles
Antibiotics
Underlying gut pathologies, often caused by stressors (parasites
The good news? If we address the gut health, then we could treat ADHD naturally—if not reversed.
Research backs this up.
SURVEY SAYS: ADHD & GUT RESEARCH
A 2017 peer-reviewed study found significant connections between increased gut inflammation and test subjects with ADHD, regardless of age and previous diagnosis (15). The volunteers with ADHD had more Bifidobacterium genus, often associated with SIBO or small intestinal bacterial overgrowth (16).
In another review in the European Child & Adolescent Psychiatry Journal, researchers state that while studies on ADHD and the gut microbiota in patients is budding, there is clear evidence about the link between obesity and ADHD and between obesity and alteration of the gut microbiota.
There is a way to treat ADHD naturally.
Obesity induces a low-grade inflammatory state which has been associated with behavioral and cognitive alterations, being gut micro-biota most likely an important mediator between inflammation and altered behaviors.
Overall, data from gluten-free mice studies, antibiotic treatment studies, and probiotic interventions suggest that alterations in gut microbiota that reduce the inflammatory state also reduce stress-related behaviors, supporting the role of the gut microbiota as a mediator between inflammation and behavioral alterations.
And, another clinical trial (18) is currently underway, as researchers have concluded from previous research that ADHD is in are linked to shifts in gut microbiota composition.
5 ESSENTIAL STEPS TO TREAT ADHD NATURALLY
The main strategy to heal and treat ADHD naturally involve balancing out stress levels, and NOT irritating the gut barrier and gut immune system. Here are 5 essential steps to start.
STEP 1: EAT REAL FOOD (ESPECIALLY FATS & PROTEINS)
When we eat, we not only feed ourselves, but we also feed our gut bugs. This is a crucial step to treat ADHD naturally. It’s not rocket science: Real, whole, nutrient-dense foods make an unhealthy gut a healthier gut. While most kids’ favorite foods include chicken nuggets, mac and cheese, French fries, Honey Nut Cheerios, possibly fruit and anything with ketchup, they are humans too.
And humans were wired to eat real foods. Real foods include: sustainable, organic meats and fish, colorful fruits and veggies and essential healthy fats (coconut oil, ghee, grass-fed butter, pastured egg yolks, avocado, raw nuts and seeds.
STEP 2: CUT OUT THE CULPRITS
This goes beyond just going a gluten-free (since many gluten free products contain just as many additives as the gluten version)s. Experiment with cutting out grains, conventional dairy, sugar and additives (dyes, sweeteners, chemicals) for 30 days and watch your kids’ brains come to life. Do it together with a non-diet mentality as a challenge for the family for stronger bodies and better brains. A great way to help treat ADHD naturally.
STEP 3: LOVE YOUR GUT BUGS
Give your kids a daily soil-based probiotic and prebiotic fiber to treat ADHD naturally. These include partially hydrolyzed guar gum, to help the healthy probiotics stick in their gut. Soil based probiotics are typically better tolerated by most people, and contain probiotic like cultures that were once found in the rich soils of our ancestors. Start with 1/2 capsule of a probiotic, 2 times per day, and 1 teaspoon of a prebiotic. Other “gut loving” additions include:
Colostrum (similar to the gut-healing natural colostrum found in the “perfect food:” a mother’s milk)
Digestive Enzymes (support natural enzymes that help break down food)
Betaine HCL (hydrochloric acid) found in capsules (naturally boosts stomach acid to enhance digestion)
Optional: Digestive “bitters” to support detoxification mixed into homemade dark chocolate syrup (5 drops of bitters + 1 tablespoon cacao powder + 1 tablespoon raw honey (use maple syrup for kids under 1 year of age) +fresh juice from half a small lemon)
STEP 4: DESTRESS
For kids, this includes encouraging them to get 60-minutes (at least) of active play and exercise each day, as well as outdoor time and sunshine, about 9 hours of sleep each night and creative, imaginative playaway from screens.
Magnesium Citrate at night is also a natural calming mineral, mixed into bedtime tea or water.
STEP 5: TEST, DON’T GUESS
Work with a functional medicine practitioner or healthcare practitioner knowledgeable in gut health analysis and treatment of any underlying conditions that may play a role in your child’s brain-gut-connection. Lab tests may include: Stool testing, Organic Acids Urine Testing, Comprehensive Bloodwork Analysis, Food Sensitivity Testing, and Small Intestinal Bacterial Overgrowth Breath Testing. This can help to treat ADHD naturally.
Not all tests are essential, but can give you and your child a clearer picture into their unique presentation if an underlying gut pathology is behind their condition. (Note: Many traditional GI doctors do not perform these tests on kids, beyond food allergy, not sensitivity, testing and potential scope and CT scan imaging).
The bottom line:
In the end, address the roots of cognitive imbalance first (gut and stress), not the symptoms. This is very important step to treat ADHD naturally.
Resources:
2018. ADHD. https://www.cdc.gov/ncbddd/adhd/data.html.
2018. How Stress Affects Your Health. https://www.apa.org/helpcenter/stress-facts.pdf; American Institute of Stress. https://www.stress.org/americas-1-health-problem/ (Cited: Perkins (1994) showed that 60% to 90% of doctor visits were stress-related)
Sleep Foundation. 2010. Sleep in America. http://sleepfoundation.org/sites/default/files/2014-NSF-Sleep-in-America-poll-summary-of-findings—FINAL-Updated-3-26-14-.pdf
2018. Physical Activity Facts. https://www.cdc.gov/healthyschools/physicalactivity/facts.htm
Kaiser Family Foundation. Generation M2: Media in the Lives of 8-18-year-olds. 2010 https://kaiserfamilyfoundation.files.wordpress.com/2013/04/8010.pdf
The Nature Conservancy. Connecting America’s Youth to Nature. 2011. https://www.nature.org/newsfeatures/kids-in-nature/youth-and-nature-poll-results.pdf
Doug & Melissa. 2018. Time to Play Study. http://ww2.melissaanddoug.com/MelissaAndDoug_Gallup_TimetoPlay_Study.pdf
2017. Antibiotic Use in the United States, 2017: Progress and Opportunities. https://www.cdc.gov/antibiotic-use/stewardship-report/outpatient.html
Facts & Statistics: Physical Activity. 2018. https://www.hhs.gov/fitness/resource-center/facts-and-statistics/index.html (Cited Source: Reedy J, Krebs-Smith SM. Dietary sources of energy, solid fats, and added sugars among children and adolescents in the United States. Journal of the American Dietetic Association, Volume 110, Issue 10, Pages 1477-1484, October 2010. Available at: http://www.ncbi.nlm.nih.gov/pubmed/20869486.)
Blackmer AB, Farrington EA. Constipation in the pediatric patient: an overview and pharmacologic considerations. Journal of Pediatric Health Care. 2010;24(6):385–399.
Nelson SP, Chen EH, Syniar GM, Christoffel KK. Pediatric Practice Research Group. Prevalence of symptoms of gastroesophageal reflux during childhood. Archives of Pediatric and Adolescents Medicine. 2000;154:150–154
Asthma & Allergy Foundation. 2018. Allergy Facts and Figures. http://www.aafa.org/page/allergy-facts.aspx
Volz, F. Wölbing, F. Regler, S. Kaesler, T. Biedermann. 232 NOD2 signaling critically influences sensitization to orally ingested allergens and severity of anaphylaxis. Journal of Investigative Dermatology, 2016; 136 (9): S201 DOI: 10.1016/j.jid.2016.06.252
Neonatal gut microbiota associates with childhood multisensitized atopy and T cell differentiation. Fujimura KE, Sitarik AR, Havstad S, Lin DL, Levan S, Fadrosh D, Panzer AR, LaMere B, Rackaityte E, Lukacs NW, Wegienka G, Boushey HA, Ownby DR, Zoratti EM, Levin AM, Johnson CC, Lynch SV. Nat Med. 2016 Sep 12. doi: 10.1038/nm.4176. [Epub ahead of print]. PMID: 27618652.
Aarts, E., Ederveen, T. H. A., Naaijen, J., Zwiers, M. P., Boekhorst, J., Timmerman, H. M., … Arias Vasquez, A. (2017). Gut microbiome in ADHD and its relation to neural reward anticipation. PLoS ONE, 12(9), e0183509. http://doi.org/10.1371/journal.pone.0183509
Quigley & Quera. 2006. Small Intestinal Bacterial Overgrowth: Roles of Antibiotics, Prebiotics, and Probiotics. http://www.deerlandenzymes.com/wp-content/uploads/2015/04/Small-Intestinal-Bacterial-Overgrowth-Roles-of-Antibiotics-Prebiotics-and-Probiotics.pdf
Carmen Cenit, María & Campillo Nuevo, Isabel & codoñer-franch, Pilar & G. Dinan, Timothy & Sanz, Yolanda. (2017). Gut microbiota and attention deficit hyperactivity disorder: new perspectives for a challenging condition. European Child & Adolescent Psychiatry. 26. 10.1007/s00787-017-0969-z. https://www.researchgate.net/profile/Pilar_Codoner-franch/publication/314967081_Gut_microbiota_and_attention_deficit_hyperactivity_disorder_new_perspectives_for_a_challenging_condition/links/5a2f81e50f7e9bfe81705387/Gut-microbiota-and-attention-deficit-hyperactivity-disorder-new-perspectives-for-a-challenging-condition.pdf?origin=publication_detail
Xijing Hospital. 2018. Gut Microbiome and Serum Metabolome Alterations in ADHD Patients (ADHD). https://clinicaltrials.gov/ct2/show/NCT03447223
The post How To Treat ADHD Naturally: 5 Most Important Steps appeared first on Meet Dr. Lauryn.
Source/Repost=>
https://drlauryn.com/family-kid-health/treat-adhd-naturally-5-essential-steps/ ** Dr. Lauryn Lax __Nutrition. Therapy. Functional Medicine ** https://drlauryn.com/
How To Treat ADHD Naturally: 5 Most Important Steps via https://drlaurynlax.blogspot.com/
0 notes
Text
How To Treat ADHD Naturally: 5 Most Important Steps
Is there a way to treat ADHD naturally? What one should do?More than 1 in 10 children, ages 4-17 have ADHD (attention deficit hyperactivity disorder) (1), defined as “limited attention and hyperactivity.”
Common characteristics of ADHD include:
Difficulty sustaining attention or focusing
Difficulty following through with tasks
Hyperactivity
Difficulty organizing self and tasks
Impulsive behavior
To officially be diagnosed with ADHD, symptoms must persist for at least 6 months, and behaviors and symptoms must be abnormal for children of the same age and negatively affect his or her school, home life or relationships in more than one setting (i.e. at home and at school).
Unfortunately, for many of these kids who are diagnosed, ADHD will continue into their adulthood, and conventional medicine believes that the disease is “manageable, but not curable.” In order to help kids “manage” their ADHD, treatment typically consists of medications and behavioral interventions, such as occupational therapy, behavioral therapy and sensory or movement “breaks.”
After those options are exhausted however, there is little, if anything else doctors say they can do.
The missing link most docs and conventional medicine is not talking about?
A little superpower known as the “brain gut connection.”
According to the latest in research about the brain-gut connection, ADHD is not only manageable, but it is reversible and remissible.
In this article we’ll cover the basics about the brain-gut connection, plus learn 5 essential steps to treat ADHD naturally (that your doctor probably won’t tell you about).
THE BRAIN GUT CONNECTION
The “brain-gut” connection is essentially what it sounds like: Your gut and brain are directly linked.
Your vagus nerve (the nerve responsible for directing how you think and your brain function) is connected from your frontal brain lobe to the top stomach. In addition, about 95% of your serotonin (“feel good” brain chemical) is produced in your gastrointestinal tract.
Couple this with the fact that your gastrointestinal tract is lined with more than a 100 million nerve cells, and it makes sense: the inner workings of your digestive system don’t just help you digest food, but also guide your emotions.
In short: When your gut is unhappy or stressed…your brain is unhappy or stressed.
Enter: The “brain-gut connection.”
Inflammation in your gut sends signals to your brain, causing a similar response (inflammation, stress and in many children’s cases, anxiety, sensory processing disorders, and ADHD).
The bottom line: If you have an unhealthy gut, your brain function gets thrown off. And, if you have an unhealthy brain (i.e. stressed), your gut function can also get thrown off.
THE MISSING LINKS IN ADHD TREATMENT: GUT HEALTH & STRESS
Unfortunately, for years, we’ve come to see the body and mind as two separate entities.
The mind is often treated separately from the body, other than using medications to suppress “neuro-chemical imbalances.” Patients with ADHD or other mood disorders and mental illnesses are then typically referred out to see a psychotherapist or occupational therapist to address “behavior” and emotional issues, in hopes of remediating the symptoms, with sub-par results or a lifetime spent in therapy, using coping strategies and taking medications.
From a functional medicine perspective, we want to address ADHD and other mental health conditions in the same way that we address any other health condition (i.e. autoimmune disease, diabetes, GERD, hypertension, etc.). We want to look at what the underlying causes are for these conditions. This is essential to treat ADHD naturally.
While mental illness, like ADHD, is a complex combination of various genetic and epigenetic factors, (including nutritional, physical, biochemical, environmental, social, emotional, and spiritual influences), many traditional methods of diagnosis and treatment fail to address two of the biggest drivers of disease: gut health and chronic inflammation (i.e. stress).
Our stress levels and gut health are the gateways to health.
In fact, the American Psychological Association estimates that 99% of ALL disease is attributed to stress alone (2). Stress is defined as any “outside force that exceeds the body’s ability to recover or maintain homeostasis.”
Just like the “stress” of a poor quality diet, lack of sleep and sedentary lifestyle leads to conditions like diabetes and high blood pressure, and just like poor gut health, such as “intestinal permeability” (leaky gut) is connected to conditions like autoimmune disease, skin breakouts and anxiety, stress levels and gut health play a key role in ADHD.
STRESS 101
Contrary to popular belief, “stress” goes far beyond mental stress. Physiological stress equally imbalances the optimal function of the body—brain balance included. Common sources of physical stress and inflammation for many ADHD sufferers include:
Inadequate sleep or poor quality sleep. More than half of kids do NOT get 8-9 hours of quality sleep. (3)
Sedentary lifestyles. Kids are moving less than ever before with 1 in 5 getting the recommended minimum of 60-minutes of physical activity 5 days per week. (4)
Overexposure to screens and blue lights. The average kid spends 6-9 hours/day in front of a screen. (5)
Lack of spontaneous play and time in nature. Only 10% of kids spend time outside every day (6) and a 2018 Gallup study found that children nationwide spend less time on creative play than ever before, spending 18.6 hours each week to screen-based play per week, versus 14.6 hours on indoor screen-free play (7).
Antibiotic drug exposure. 1 in 4 kids get antibiotics every year that are unnecessary and 5 in 6 kids take an antibiotic every year (8).
Poor quality nutrition and processed foods. Nearly 50% of kids’ diets, ages 2-18 consist of empty calories from added sugars and and processed foods including: soda, fruit drinks, dairy desserts, grain desserts, pizza, and conventional milk (9).
Poor gut health. Including about 2 in 5 kids with constipation (10), 1 in 4 with GERD or “reflux” (11) and millions of kids with allergies and asthma—the #1 “chronic disease” of kids nationwide (12) (linked to poor gut health) (13, 14).
GUT HEALTH 101
Much of the chronic diseases we face today can also be traced back to our gut health, including ADHD. If we could address the problems in our gut, we can find the right ways to treat ADHD naturally.
The human gut contains more than 100 trillion gut bacteria—up to 10 times more bacteria than human cells in our blood stream and body.
The healthier and more diverse your gut bacteria, the healthier your body is overall. However, the less healthy or less diverse your gut bacteria, the less healthy or “out of balance” you are.
Our gut bacteria influence the health of our:
Blood sugar and insulin levels
Hormone health
Thyroid
Detoxification
Mood
Immune system (allergies, skin health)
Digestion
Mental health
How do gut bacteria get unhealthy in the first place? Go back to the topic of stress! It’s a vicious cycle, but common sources of “unhealthy gut bacteria” include:
Poor sleep
Poor quality foods (packaged, processed, conventional meat, dairy, sweeteners, etc.)
Environmental toxins (additives, plastics, medicines, toxic cleaning and hygiene products)
C-section births and processed formula feedings as a baby
Infection & Illness
Sedentary lifestyles
Antibiotics
Underlying gut pathologies, often caused by stressors (parasites
The good news? If we address the gut health, then we could treat ADHD naturally—if not reversed.
Research backs this up.
SURVEY SAYS: ADHD & GUT RESEARCH
A 2017 peer-reviewed study found significant connections between increased gut inflammation and test subjects with ADHD, regardless of age and previous diagnosis (15). The volunteers with ADHD had more Bifidobacterium genus, often associated with SIBO or small intestinal bacterial overgrowth (16).
In another review in the European Child & Adolescent Psychiatry Journal, researchers state that while studies on ADHD and the gut microbiota in patients is budding, there is clear evidence about the link between obesity and ADHD and between obesity and alteration of the gut microbiota.
There is a way to treat ADHD naturally.
Obesity induces a low-grade inflammatory state which has been associated with behavioral and cognitive alterations, being gut micro-biota most likely an important mediator between inflammation and altered behaviors.
Overall, data from gluten-free mice studies, antibiotic treatment studies, and probiotic interventions suggest that alterations in gut microbiota that reduce the inflammatory state also reduce stress-related behaviors, supporting the role of the gut microbiota as a mediator between inflammation and behavioral alterations.
And, another clinical trial (18) is currently underway, as researchers have concluded from previous research that ADHD is in are linked to shifts in gut microbiota composition.
5 ESSENTIAL STEPS TO TREAT ADHD NATURALLY
The main strategy to heal and treat ADHD naturally involve balancing out stress levels, and NOT irritating the gut barrier and gut immune system. Here are 5 essential steps to start.
STEP 1: EAT REAL FOOD (ESPECIALLY FATS & PROTEINS)
When we eat, we not only feed ourselves, but we also feed our gut bugs. This is a crucial step to treat ADHD naturally. It’s not rocket science: Real, whole, nutrient-dense foods make an unhealthy gut a healthier gut. While most kids’ favorite foods include chicken nuggets, mac and cheese, French fries, Honey Nut Cheerios, possibly fruit and anything with ketchup, they are humans too.
And humans were wired to eat real foods. Real foods include: sustainable, organic meats and fish, colorful fruits and veggies and essential healthy fats (coconut oil, ghee, grass-fed butter, pastured egg yolks, avocado, raw nuts and seeds.
STEP 2: CUT OUT THE CULPRITS
This goes beyond just going a gluten-free (since many gluten free products contain just as many additives as the gluten version)s. Experiment with cutting out grains, conventional dairy, sugar and additives (dyes, sweeteners, chemicals) for 30 days and watch your kids’ brains come to life. Do it together with a non-diet mentality as a challenge for the family for stronger bodies and better brains. A great way to help treat ADHD naturally.
STEP 3: LOVE YOUR GUT BUGS
Give your kids a daily soil-based probiotic and prebiotic fiber to treat ADHD naturally. These include partially hydrolyzed guar gum, to help the healthy probiotics stick in their gut. Soil based probiotics are typically better tolerated by most people, and contain probiotic like cultures that were once found in the rich soils of our ancestors. Start with ½ capsule of a probiotic, 2 times per day, and 1 teaspoon of a prebiotic. Other “gut loving” additions include:
Colostrum (similar to the gut-healing natural colostrum found in the “perfect food:” a mother’s milk)
Digestive Enzymes (support natural enzymes that help break down food)
Betaine HCL (hydrochloric acid) found in capsules (naturally boosts stomach acid to enhance digestion)
Optional: Digestive “bitters” to support detoxification mixed into homemade dark chocolate syrup (5 drops of bitters + 1 tablespoon cacao powder + 1 tablespoon raw honey (use maple syrup for kids under 1 year of age) +fresh juice from half a small lemon)
STEP 4: DESTRESS
For kids, this includes encouraging them to get 60-minutes (at least) of active play and exercise each day, as well as outdoor time and sunshine, about 9 hours of sleep each night and creative, imaginative playaway from screens.
Magnesium Citrate at night is also a natural calming mineral, mixed into bedtime tea or water.
STEP 5: TEST, DON’T GUESS
Work with a functional medicine practitioner or healthcare practitioner knowledgeable in gut health analysis and treatment of any underlying conditions that may play a role in your child’s brain-gut-connection. Lab tests may include: Stool testing, Organic Acids Urine Testing, Comprehensive Bloodwork Analysis, Food Sensitivity Testing, and Small Intestinal Bacterial Overgrowth Breath Testing. This can help to treat ADHD naturally.
Not all tests are essential, but can give you and your child a clearer picture into their unique presentation if an underlying gut pathology is behind their condition. (Note: Many traditional GI doctors do not perform these tests on kids, beyond food allergy, not sensitivity, testing and potential scope and CT scan imaging).
The bottom line:
In the end, address the roots of cognitive imbalance first (gut and stress), not the symptoms. This is very important step to treat ADHD naturally.
Resources:
2018. ADHD. https://www.cdc.gov/ncbddd/adhd/data.html.
2018. How Stress Affects Your Health. https://www.apa.org/helpcenter/stress-facts.pdf; American Institute of Stress. https://www.stress.org/americas-1-health-problem/ (Cited: Perkins (1994) showed that 60% to 90% of doctor visits were stress-related)
Sleep Foundation. 2010. Sleep in America. http://sleepfoundation.org/sites/default/files/2014-NSF-Sleep-in-America-poll-summary-of-findings—FINAL-Updated-3-26-14-.pdf
2018. Physical Activity Facts. https://www.cdc.gov/healthyschools/physicalactivity/facts.htm
Kaiser Family Foundation. Generation M2: Media in the Lives of 8-18-year-olds. 2010 https://kaiserfamilyfoundation.files.wordpress.com/2013/04/8010.pdf
The Nature Conservancy. Connecting America’s Youth to Nature. 2011. https://www.nature.org/newsfeatures/kids-in-nature/youth-and-nature-poll-results.pdf
Doug & Melissa. 2018. Time to Play Study. http://ww2.melissaanddoug.com/MelissaAndDoug_Gallup_TimetoPlay_Study.pdf
2017. Antibiotic Use in the United States, 2017: Progress and Opportunities. https://www.cdc.gov/antibiotic-use/stewardship-report/outpatient.html
Facts & Statistics: Physical Activity. 2018. https://www.hhs.gov/fitness/resource-center/facts-and-statistics/index.html (Cited Source: Reedy J, Krebs-Smith SM. Dietary sources of energy, solid fats, and added sugars among children and adolescents in the United States. Journal of the American Dietetic Association, Volume 110, Issue 10, Pages 1477-1484, October 2010. Available at: http://www.ncbi.nlm.nih.gov/pubmed/20869486.)
Blackmer AB, Farrington EA. Constipation in the pediatric patient: an overview and pharmacologic considerations. Journal of Pediatric Health Care. 2010;24(6):385–399.
Nelson SP, Chen EH, Syniar GM, Christoffel KK. Pediatric Practice Research Group. Prevalence of symptoms of gastroesophageal reflux during childhood. Archives of Pediatric and Adolescents Medicine. 2000;154:150–154
Asthma & Allergy Foundation. 2018. Allergy Facts and Figures. http://www.aafa.org/page/allergy-facts.aspx
Volz, F. Wölbing, F. Regler, S. Kaesler, T. Biedermann. 232 NOD2 signaling critically influences sensitization to orally ingested allergens and severity of anaphylaxis. Journal of Investigative Dermatology, 2016; 136 (9): S201 DOI: 10.1016/j.jid.2016.06.252
Neonatal gut microbiota associates with childhood multisensitized atopy and T cell differentiation. Fujimura KE, Sitarik AR, Havstad S, Lin DL, Levan S, Fadrosh D, Panzer AR, LaMere B, Rackaityte E, Lukacs NW, Wegienka G, Boushey HA, Ownby DR, Zoratti EM, Levin AM, Johnson CC, Lynch SV. Nat Med. 2016 Sep 12. doi: 10.1038/nm.4176. [Epub ahead of print]. PMID: 27618652.
Aarts, E., Ederveen, T. H. A., Naaijen, J., Zwiers, M. P., Boekhorst, J., Timmerman, H. M., … Arias Vasquez, A. (2017). Gut microbiome in ADHD and its relation to neural reward anticipation. PLoS ONE, 12(9), e0183509. http://doi.org/10.1371/journal.pone.0183509
Quigley & Quera. 2006. Small Intestinal Bacterial Overgrowth: Roles of Antibiotics, Prebiotics, and Probiotics. http://www.deerlandenzymes.com/wp-content/uploads/2015/04/Small-Intestinal-Bacterial-Overgrowth-Roles-of-Antibiotics-Prebiotics-and-Probiotics.pdf
Carmen Cenit, María & Campillo Nuevo, Isabel & codoñer-franch, Pilar & G. Dinan, Timothy & Sanz, Yolanda. (2017). Gut microbiota and attention deficit hyperactivity disorder: new perspectives for a challenging condition. European Child & Adolescent Psychiatry. 26. 10.1007/s00787-017-0969-z. https://www.researchgate.net/profile/Pilar_Codoner-franch/publication/314967081_Gut_microbiota_and_attention_deficit_hyperactivity_disorder_new_perspectives_for_a_challenging_condition/links/5a2f81e50f7e9bfe81705387/Gut-microbiota-and-attention-deficit-hyperactivity-disorder-new-perspectives-for-a-challenging-condition.pdf?origin=publication_detail
Xijing Hospital. 2018. Gut Microbiome and Serum Metabolome Alterations in ADHD Patients (ADHD). https://clinicaltrials.gov/ct2/show/NCT03447223
The post How To Treat ADHD Naturally: 5 Most Important Steps appeared first on Meet Dr. Lauryn.
Source/Repost=>
https://drlauryn.com/family-kid-health/treat-adhd-naturally-5-essential-steps/ ** Dr. Lauryn Lax __Nutrition. Therapy. Functional Medicine ** https://drlauryn.com/
How To Treat ADHD Naturally: 5 Most Important Steps via http://drlaurynlax.tumblr.com/
0 notes
Text
Brain Fog: How to Naturally Get Rid of Brain Fatigue

If you struggle with poor focus, mental fatigue, or confusion, brain fog may be the culprit. Though not a medically recognized condition, brain fog is a common complaint. Brain fog often happens in older people but can affect people of any age. Generally speaking, brain fog is a dysfunction in your ability to focus, learn, and remember.
If you have brain fog, natural remedies can clear the mist, so to speak. When you engage in lifestyle changes — diet, exercise, sleep, and nutritional supplements — you can improve your mental clarity and energy.
What Is Brain Fog?
Brain fog is a general term for mild to moderate difficulty with focus, concentration, memory, and other cognitive functions. Brain fog can present in different ways, many of which are subjective and self-reported.[1] You may experience mental fatigue, have difficulty finding the right words to express yourself, or feel slow, spaced-out, or forgetful. You might get easily distracted from daily tasks, have difficulty following conversations, or have poor concentration, mental clarity, and memory. Because brain fog is not a medical disorder, you may recognize it when you realize that you have a "cluster" of these symptoms.
Brain Fog Symptoms
If you have brain fog, you may experience one or more of the following symptoms.
Mental fatigue
Forgetfulness
Being easily distracted
Poor memory
Difficulty concentrating
Feeling "spaced out"
Disorientation
Irritability
The Top 7 Causes of Brain Fog
Hormonal changes, side effects from medications, and normal aging all contribute to the symptoms of brain fog. Here are the top seven causes.
1. Stress
Mental stress causes your body to produce excessive levels of the hormone cortisol. Stress also suppresses your immune system and stimulates your adrenal system, which regulates your body's production of hormones. Together, these issues impair working memory, concentration, motivation, and other physiological changes that lead to brain fog.[2]
2. Poor Dietary Choices
What you put in your body affects how efficiently your brain works. A diet full of high-fat or sugary foods can impair memory and other brain activities.[3] Many low-fat processed foods advertised as "good for you" are not: they contain chemical preservatives, MSG, and excess sodium, and are generally bad for your brain.
For peak mental performance, your diet should contain a balance of proteins, carbohydrates, and healthy fats, as well as the vitamins, minerals, and nutrients you need. A deficiency of any essential nutrient may cause brain fog. Make sure you drink plenty of water and avoid dehydration, which causes headaches and reduces mental focus.
3. Allergies & Food Intolerances
Food allergies — particularly with wheat gluten or dairy — may worsen brain fog. As one scientist puts it, "gluten sensitivity can be primarily, and at times, exclusively, a neurological disease." Scientists have shown a clear link between the gut and the brain. Celiac disease, a condition caused when someone sensitive to gluten continues consuming it, causes inflammation in the digestive system that, in turn, influences balance, concentration, and memory.[4] Likewise, consuming dairy when you have lactose intolerance or an allergy impacts the central nervous system and can cause brain fog.
4. Medications
Many commonly prescribed and over-the-counter medications may reduce your mental clarity. Benzodiazepines (a class of drugs prescribed to treat anxiety), opiate pain medications, and prescription and non-prescription sleep aids may exacerbate brain fog. Some medications can interact with each other, or even with over-the-counter products and nutritional supplements, amplifying their effects and affecting mental clarity.
5. Health Conditions
Certain medical conditions may impair cognition. For example, Type 2 diabetes not only affects mental focus due to changes in blood glucose levels, but it also may come with emotional challenges like depression.[5] Similarly, low thyroid function and Hashimoto's disease cause brain fog symptoms including fatigue and memory lapse. Depression, anemia, high blood pressure, and autoimmune disorders like lupus or multiple sclerosis are other health conditions linked to brain fog. Although not a medical condition, addiction to nicotine caused by smoking or other tobacco products may also contribute to brain fog, especially during withdrawals.
6. Inadequate Sleep
In a 2013 study, the top two causes people attributed their brain fog to were physical fatigue and sleep deprivation.[6] A review of decades of research on the topic found that poor sleep quality is often associated with cognitive decline in middle-aged adults, so make sure to get your beauty rest.[7] According to the U.S. Centers for Disease Control and Prevention (CDC), adults need at least seven to nine hours of sleep per night.[8]Sleeping is extremely important; not only does it boost your energy levels and mental clarity, but also ensures the proper functioning of all your body systems.
7. Age-Related Hormonal Changes
Your body undergoes hormonal changes at certain points in life. Women going through menopause, the time of life when periods cease, might experience brain fog or related symptoms. The most common age-related brain fog symptoms include trouble focusing, fatigue, and difficulty falling asleep.[9] Besides the hormonal changes associated with menopause, both men and women experience an age-related mental decline that can manifest as brain fog.
How to Naturally Get Rid of Brain Fog
You can find relief from brain fog with healthy habits that support your body and brain.
Essential Oils
Inhaling even a molecule of an aromatic essential oil sends a message directly to your brain, which makes it an easy way to reduce brain fog symptoms. Frankincense, for example, helped improve memory and other cognitive functions in rats who have a disorder similar to Alzheimer's disease.[10]Lavender, peppermint, and chamomile essential oils can relax and calm the mind and body, helping you get restorative sleep. One study found that vetiver oil had properties that stimulated alert wakefulness, which "might be beneficial for learning and memory processes."[11]
Add a drop of lavender essential oil in your hands and rub them together, then cup your hands over your nose and take five deep breaths.
Sleep More
An estimated 35 percent of American adults get less than seven to nine hours of sleep per night, the recommended amount. This lack of sleep leaves people fatigued and less productive and focused.[12] According to the CDC, "Getting enough sleep is not a luxury — it is something people need for good health."[13] Practice healthy sleep hygiene habits like maintaining a consistent and relaxing bedtime routine, limiting daytime naps to 30 minutes, and holding off on eating rich, fatty foods or consuming caffeine close to bedtime.[14] For more ideas, check out our natural sleep remedies article.
Eat Healthy Fats
Choose "healthy fats" that come from nuts, seeds, and vegetables — olive oil, avocado oil, and walnut oil. These contain omega-3 fatty acids, which play a critical role in brain health. Dietary fats play a role in the blood-brain barrier (which selectively keeps chemicals from penetrating the brain) and in maintaining healthy blood cholesterol levels.[15] Avoid animal-based saturated fats from red meat and high-fat dairy; one study found that people eating the highest amounts of these bad fats experienced the worst memory and cognition problems over time.[16] The exception to this rule is coconut oil, a saturated fat that — in contrast to animal-based options — actually lowers bad cholesterol in your blood.[17]
Eat Antioxidant-Rich Fruits & Vegetables
Antioxidants positively impact memory and other cognitive functions.[18] An antioxidant counteracts the harmful effects of free radicals, which otherwise will go around cells causing damage. By counteracting those, antioxidants are the superheroes of your body. They're readily available in dark green leafy vegetables, brightly colored fruits and berries, and herbs and spices like turmeric and cayenne pepper. There's even good news for chocolate lovers — cocoa contains antioxidants called flavanols that improve circulation and may preserve cognitive abilities.[19] Balance out your diet with healthy carbohydrates and proteins for optimal brain health.
Exercise
In addition to protecting you from weight gain, exercise stimulates your body to release hormones that improve brain health, particularly in the areas of mood and energy. A beneficial exercise routine doesn't take long to establish. When people spent just four weeks on a fitness program that combined aerobic exercise, strength training, and stretching, they experienced improved memory, attention, and mental processing speed.[20] Move your body in healthy ways. Simply spending time outdoors boosts cognitive development in kids and helps adults as well.[21]
Brain Fog Supplements
While it's always best to get your nutrition from your food, sometimes you need an extra boost of one nutrient or another. Several nutritional supplements support brain health, including these six.
Omega-3 Fatty Acids
One study found that over a period of 18 months, omega-3 fatty acids slowed mental decline in healthy elderly adults, improving brain fog symptoms like working memory and information retrieval.[22] Because these fats occur naturally in fish and other seafood, fish oil supplements are popular; however, fish oil supplements may have high levels of mercury and other contaminants, and the harvesting methods for these fish are often environmentally unsustainable. We recommend getting your omega-3 fatty acids from plant-based foods or supplements, such as flaxseed oil or algae oil.
Magnesium
Scientists have connected magnesium deficiency with a number of brain disorders. Magnesium plays a role in general brain health for everyone, including helping your neurons (nerve cells) "fire" — transmitting messages to the body and creating thoughts. Taking magnesium may protect cognitive function and memory, reducing brain fog.[23]
Maca Root
The natural fatty acids found in maca root (Lepidium meyenii) can help preserve overall brain health. Mice fed a diet that including maca root experienced heightened memory and other cognitive abilities.[24] Specifically, the study found that maca root boosted the activity of cellular mitochondria, the organelle inside each cell that provides energy. Past studies had also found maca encouraged a balanced mood and even increased vigor and energy levels.[24]
Vitamin B-12
Muddled thinking and forgetfulness may indicate you have low B-12 levels, an essential vitamin. Some studies even show that vitamin B-12 supplements can slow age-related brain decline, especially in people who are deficient. Since vitamin B-12 occurs mainly in animal-based foods, those who follow a vegetarian or vegan diet, or those who do not eat very much meat, may require a B-12 supplement.[25]
Bacopa
An herb used in many Ayurvedic remedies and one of the top herbs for mental health, studies have found Bacopa monnieri counteracts brain fog symptoms like short attention span, poor focus, and short-term memory.[26] Also called water hyssop or Brahmi (not to be confused with gotu kola which is also sometimes called Brahmi), bacopa appears to normalize cortisol in the body, which reduces stress, and may help your brain fog.[27] Bacopa also reduces stress which makes it an adaptogen — a substance that helps the body adapt to stress.
Mucuna pruriens
Mucuna pruriens, also called velvet bean, contains a high concentration of antioxidants. These antioxidants work with L-dopa, a brain chemical, to produce the neurotransmitter dopamine. Among other things, dopamine regulates processes associated with brain fog, including mental flexibility, memory, and motivation.[28]
Points to Remember
Brain fog is not a recognized medical condition, but it is a common issue for many people and includes symptoms like mental fatigue, poor memory, and lack of focus. A variety of issues may cause brain fog, but the top six causes are stress, poor diet, medications, health conditions, inadequate sleep, and age-related hormonal changes.
There are several natural strategies for reducing brain fog. Start by eating a healthy diet including many antioxidant-rich organic fruits and vegetables, whole grains, legumes, nuts, and seeds and avoid fried, processed, and animal-based foods. Exercise more, get more sleep, and try essential oils like peppermint. Herbal supplements like bacopa and Mucuna pruriens may also help you clear the fog, lending greater clarity to your thoughts.
How do you clear brain fog from your mind? Share your tips in the comments!
The post Brain Fog: How to Naturally Get Rid of Brain Fatigue appeared first on Dr. Group's Healthy Living Articles.
from Robert Morgan Blog https://www.globalhealingcenter.com/natural-health/brain-fog/
0 notes
Text
What Causes Slow Post-Workout Recovery—and What Can You Do About It?
One of the biggest mistakes I see among people who exercise is they forget this core truth: we get fitter not from training, but from recovering from training. This doesn’t just occur in beginners either. Some of the most experienced, hardest-charging athletes I know fail to heed the importance of recovery. Hell, the reason my endurance training destroyed my life and inadvertently set the stage for creation of the Primal Blueprint was that I didn’t grasp the concept of recovery. I just piled on the miles, thinking the more the merrier.
It didn’t work.
What is recovery, anyway?
There’s short-term recovery. Your heart rate slows back down, your body temperature drops, your sweat dries, your muscles and lungs stop burning.
Long-term recovery is less conspicuous, more internal. You replace lost energy stores, repair damaged muscle, clear out waste products, and begin the process of adaptation to the training.
When both short- and long-term recovery happen together, you “feel ready” to go again.
Some portion of how quickly we recover from training is out of our direct control.
Genetics is one factor we can’t control. Researchers have found genetic variants of collagen-encoding genes that increase or decrease the rate at which we recover from exercise-induced muscle damage, muscle tissue genes that increase resistance to exercise-induced muscle soreness, immune genes that affect the speed of adaptation to training. But even many genetic variants purported to affect recovery act through decisions carriers make. A carrier of a genetic variant linked to muscle power experienced more muscle damage and required more recovery after a soccer match, but only because that carrier “performed more speed and power actions during the game.”
Age is another factor out of our direct control. Sure, living, eating, and training right can stave off many of the worst effects of aging. Sure, a sedentary 70-year-old will recover from a workout far more slowly (if he or she can be cajoled into training) than a 70-year-old master athlete. But time does tick on. Following training that fatigues but doesn’t damage the muscles, like easy cycling, light weight training, or a sub-aerobic threshold jog, older athletes recover muscle function and performance at similar rates to younger athletes. After intense exercises that damage the muscles, like sprints, heavy lifting, intervals, or longer race-pace runs, however, older athletes recover more slowly than younger athletes.
Other factors, while preventable and modifiable over the long haul, inexorably inhibit workout recovery once they’re in place:
If you’re sick, you won’t recover as quickly. Illness diverts some of the resources that would otherwise be used to recover from training.
If you have heart disease, you’ll recover more slowly. In one study, having heart disease was the greatest predictor of a slower rate of heart rate recovery after exercise.
If your hormones are out of whack, you’ll likely recover more slowly. Hormones are the messengers and managers that tell our cells what to do. That includes muscle repair, hypertrophy, fuel replenishment, inflammatory signaling, and every other cellular function related to recovery.
Now I’ve got bad news and good news. Everything else that slows down workout recovery is under your direct control.
Factors We Can Control Stress
Stress is stress. Traffic is a stressor. A job you hate is a stressor. Procrastinating until you absolutely must get working is a stressor. And yes, exercise is a stressor. Too much of the psychological, lifestyle, or mental stress we all face impairs our ability to recover from exercise-induced stress.
Recent research confirms that “mental stress” impairs workout recovery, and it doesn’t speak in generalities. Thirty-one undergrads were assessed for stress levels using a battery of psychological tests, then engaged in a heavy lower body strength workout. At an hour post-workout, students in the high stress group had regained 38 percent of their leg strength, while students in the low stress group had regained 60 percent of their strength.
I developed my anti-stress supplement Primal Calm (now, Adaptogenic Calm) back in the chronic cardio days as a way to improve my training recovery. That’s what gave the product so much momentum in the endurance community—it turns out that beating back stress of all kinds quickened recovery from a very specific type of training stress.
Some stress is unavoidable. But most of us create additional stress in our lives and fail to do enough to counter or manage it. Stop making unforced errors.
Poor Sleep
Sleep debt impairs exercise recovery primarily via two routes: by increasing cortisol, reducing testosterone production, and lowering muscle protein synthesis; and by disrupting slow wave sleep, the constructive stage of slumber in which growth hormone secretion peaks, tissues heal, and muscles rebuild. That’s probably why sleep deprivation has been linked to muscular atrophy and increased urinary excretion of nitrogen, and why the kind of cortisol excess caused by sleep deprivation reduces muscle strength.
Additionally, sleep loss can increase the risk of injuries by decreasing balance and postural control. If you trip and fall, or throw out your back due to poor technique, you won’t even have a workout to recover from.
Most people think bad sleep is unavoidable. It happens to the best of us from time to time, but a night of bad sleep here and there isn’t going to slow down recovery. The real recovery killer is chronically bad sleep, and that’s the kind most of us can avoid by sticking to a good sleep hygiene regimen.
Nutrient Deficiencies
Since every physiological function requires a micronutrient substrate—vitamin, mineral, hormone, neurotransmitter, etc.—and physiological functions increase with exercise and recovery, active people require more micronutrients in their diet. “More of everything” is a safe bet, but there are a few key nutrients that working out especially depletes:
Zinc: Exercise, especially weight training, works better with plenty of testosterone on hand to build muscle and develop strength. Zinc is a key substrate for the production of testosterone, and studies show that exercise probably increases the need for zinc. In fact, one study found that exhaustive exercise depleted testosterone (and thyroid) hormones in athletes, while supplementing with zinc restored it.
Magnesium and Other Electrolytes: Magnesium is required for a number of physiological processes related to workout recovery, including oxygen uptake by cells, energy production, and electrolyte balance. Unfortunately, as one of the main electrolytes, lots of magnesium is lost to sweat during exercise. The same could be said for other electrolytes like calcium, sodium, and potassium, but most people get plenty of those minerals from a basic Primal eating plan. Getting enough magnesium, however, is a bit tougher, making magnesium deficiency a real issue for people trying to recover from workouts.
Iron: Intense exercise depletes iron, which is instrumental in the formation of red blood cells and oxygen delivery to your tissues during training and the immune response after it. They even have a name for it—exercise-induced anemia.
Soreness
Post-workout delayed onset muscle soreness, or DOMS, is no joke. While many of you folks reading this probably enjoy DOMS and take it as feedback for a job well done, it’s a hurdle that many beginners never move past. They join a gym, d0 a workout, feel great, go to bed feeling awesome, sleep like a baby, then wake up and find they have the bipedal capacity of a three-month-old. They can barely walk. Lifting their arms to brush their teeth is agony. Walking downstairs is out of the question. Some will move past the DOMS and get back into the gym. Many will not.
Low Fuel Availability
Working out expends energy. That energy must be replenished before you’re fully recovered and prepared to do another workout. Unless you’re trying to increase efficiency by training in a state of low fuel availability, like the “train low-carb, race high-carb” method, you should recover what’s been lost. What you replenish is conditional on the type of exercise you did. If you went for a long hike or easy bike ride that burned primarily body fat, you don’t need to—and probably shouldn’t—”replenish what you lost.” If you’re coming off a 30-minute full body CrossFit session that left you gasping on the ground in a puddle of sweat, you probably have some glycogen stores to refill.
This is a common issue for folks trying to lose weight through diet and exercise. Inadequate calorie intake coupled with intense exercise sends a “starvation” signal to the body, causing a down-regulation of anabolic hormones. Instead of growing lean mass and burning body fat, starvation (whether real or simulated) promotes muscle atrophy and body fat retention. Either alone can be somewhat effective, but combining the two for too long will only impair recovery.
Alcohol
Drinking directly impairs muscle protein synthesis, the essential step in muscle recovery and adaptation to training. Moderate or “social” drinking is probably safe (just don’t use alcohol as a post-workout recovery drink), but even just a single day per week of binge drinking is linked to 4x the risk of sarcopenia, or muscle-wasting. It’s hard to recover from your workouts if your muscles are atrophying.
Oddly, drinking directly after a training session also increases testosterone levels. One theory is that testosterone levels rise after drinking because it becomes less bioavailable; your muscle cells’ resistance to testosterone goes up, so it just circulates and gives “false” readings.
Things You Can Try
The obvious thing to try is the opposite of all the modifiable and preventable recovery-inhibitors mentioned above. Get good sleep, don’t drink too much (especially post-workout), get a handle on your stress, eat enough food, eat enough protein, get your micronutrients. What else?
Watermelon
L-citrulline is an amino acid found in watermelon that shows a significantly ameliorative effect on post-workout muscle pain, or delayed onset muscle soreness (DOMS). You can also supplement directly with L-citrulline, which may work, but watermelon is so good right now with a little salt, lime juice, and cayenne pepper, and it’s actually lower in carbs than you probably think (about 10 grams per cup of watermelon). I recommend fresh watermelon over pasteurized juice, as heat treatment reduces the effect.
Beets
Beets (and beet juice) aren’t only good for exercise performance. They also reduce DOMS. Nitrates have been posited as the primary constituent responsible for the effect, but beet juice works better than pure sodium nitrate.
Tart Cherry Juice
Tart cherry juice is best used to recover during competition, when your primary concern is to get back out there and perform. Its extreme effectiveness at killing muscle pain, reducing local and systemic inflammation and exercise-induced muscle damage suggests it may hamper training adaptations, however. It does also improve sleep, which should translate into better adaptations.
Massage
Massage feels great, and the evidence shows that it’s great for recovery from exercise. It alleviates DOMS. It speeds up the recovery of muscle strength and enhances proprioception. It improves central nervous system parasympathetic/sympathetic balance, even if the masseuse is one of those weird back massage machines.
Compression Garments
These aren’t just for show. A recent meta-analysis of the available research concluded that compression garments enhance muscle recovery after strength training and improve next-day cycling performance.
Whey
Compared to other proteins, whey protein accelerates muscle adaptation to eccentric exercise.
Creatine
Although we get creatine from red meat and fish, supplementary creatine can boost our recovery from exercise via a couple mechanisms. First, it increases muscle content of phosphocreatine. That’s the stuff we use for quick bursts of maximal effort, so carrying a little extra can do wonders for our ability to perform. Second, it enhances muscle glycogen replenishment without increasing insulin.
Fish Oil (or Fatty Fish)
Adding fish oil to a recovery drink reduced post-workout muscle soreness without affecting performance. Fish oil may also enhance muscle recovery from and adaptation to strength training.
Cold Water
A cold water plunge after training enhances the recovery of muscle function. However—and this is a big “however”—post training cold water plunges also seem to impair long term muscular adaptations to resistance training. In other words, a cold plunge might help you get back in the game for the short term at the cost of long-term adaptations.
More Carbs
I always say “Eat the carbs you earn.” While that often means eating fewer carbs than before, it can also mean eating more if you’ve trained hard enough to warrant them. This even applies to keto folks; depleting glycogen through exercise creates a “glycogen debt” that you can repay without inhibiting ketosis or fat-adaptation too much. The carbs—which you don’t need much of—go into muscle glycogen stores for recovery and later use without disrupting ketosis.
Don’t take this final section as a blanket recommendation, however. Before taking ice baths, dropping $500 on massages every week, taking a long list of expensive supplements, and walking around in a full body compression suit, make sure you’re sleeping, eating enough food, and giving yourself enough time between workouts. Quite often, handling the basics will be enough.
What have you found to be the best way to recover from your training? What are the biggest roadblocks? Let me know down below, and thanks for reading!
0 notes
Text
What Causes Slow Post-Workout Recovery—and What Can You Do About It?
One of the biggest mistakes I see among people who exercise is they forget this core truth: we get fitter not from training, but from recovering from training. This doesn’t just occur in beginners either. Some of the most experienced, hardest-charging athletes I know fail to heed the importance of recovery. Hell, the reason my endurance training destroyed my life and inadvertently set the stage for creation of the Primal Blueprint was that I didn’t grasp the concept of recovery. I just piled on the miles, thinking the more the merrier.
It didn’t work.
What is recovery, anyway?
There’s short-term recovery. Your heart rate slows back down, your body temperature drops, your sweat dries, your muscles and lungs stop burning.
Long-term recovery is less conspicuous, more internal. You replace lost energy stores, repair damaged muscle, clear out waste products, and begin the process of adaptation to the training.
When both short- and long-term recovery happen together, you “feel ready” to go again.
Some portion of how quickly we recover from training is out of our direct control.
Genetics is one factor we can’t control. Researchers have found genetic variants of collagen-encoding genes that increase or decrease the rate at which we recover from exercise-induced muscle damage, muscle tissue genes that increase resistance to exercise-induced muscle soreness, immune genes that affect the speed of adaptation to training. But even many genetic variants purported to affect recovery act through decisions carriers make. A carrier of a genetic variant linked to muscle power experienced more muscle damage and required more recovery after a soccer match, but only because that carrier “performed more speed and power actions during the game.”
Age is another factor out of our direct control. Sure, living, eating, and training right can stave off many of the worst effects of aging. Sure, a sedentary 70-year-old will recover from a workout far more slowly (if he or she can be cajoled into training) than a 70-year-old master athlete. But time does tick on. Following training that fatigues but doesn’t damage the muscles, like easy cycling, light weight training, or a sub-aerobic threshold jog, older athletes recover muscle function and performance at similar rates to younger athletes. After intense exercises that damage the muscles, like sprints, heavy lifting, intervals, or longer race-pace runs, however, older athletes recover more slowly than younger athletes.
Other factors, while preventable and modifiable over the long haul, inexorably inhibit workout recovery once they’re in place:
If you’re sick, you won’t recover as quickly. Illness diverts some of the resources that would otherwise be used to recover from training.
If you have heart disease, you’ll recover more slowly. In one study, having heart disease was the greatest predictor of a slower rate of heart rate recovery after exercise.
If your hormones are out of whack, you’ll likely recover more slowly. Hormones are the messengers and managers that tell our cells what to do. That includes muscle repair, hypertrophy, fuel replenishment, inflammatory signaling, and every other cellular function related to recovery.
Now I’ve got bad news and good news. Everything else that slows down workout recovery is under your direct control.
Factors We Can Control
Stress
Stress is stress. Traffic is a stressor. A job you hate is a stressor. Procrastinating until you absolutely must get working is a stressor. And yes, exercise is a stressor. Too much of the psychological, lifestyle, or mental stress we all face impairs our ability to recover from exercise-induced stress.
Recent research confirms that “mental stress” impairs workout recovery, and it doesn’t speak in generalities. Thirty-one undergrads were assessed for stress levels using a battery of psychological tests, then engaged in a heavy lower body strength workout. At an hour post-workout, students in the high stress group had regained 38 percent of their leg strength, while students in the low stress group had regained 60 percent of their strength.
I developed my anti-stress supplement Primal Calm (now, Adaptogenic Calm) back in the chronic cardio days as a way to improve my training recovery. That’s what gave the product so much momentum in the endurance community—it turns out that beating back stress of all kinds quickened recovery from a very specific type of training stress.
Some stress is unavoidable. But most of us create additional stress in our lives and fail to do enough to counter or manage it. Stop making unforced errors.
Poor Sleep
Sleep debt impairs exercise recovery primarily via two routes: by increasing cortisol, reducing testosterone production, and lowering muscle protein synthesis; and by disrupting slow wave sleep, the constructive stage of slumber in which growth hormone secretion peaks, tissues heal, and muscles rebuild. That’s probably why sleep deprivation has been linked to muscular atrophy and increased urinary excretion of nitrogen, and why the kind of cortisol excess caused by sleep deprivation reduces muscle strength.
Additionally, sleep loss can increase the risk of injuries by decreasing balance and postural control. If you trip and fall, or throw out your back due to poor technique, you won’t even have a workout to recover from.
Most people think bad sleep is unavoidable. It happens to the best of us from time to time, but a night of bad sleep here and there isn’t going to slow down recovery. The real recovery killer is chronically bad sleep, and that’s the kind most of us can avoid by sticking to a good sleep hygiene regimen.
Nutrient Deficiencies
Since every physiological function requires a micronutrient substrate—vitamin, mineral, hormone, neurotransmitter, etc.—and physiological functions increase with exercise and recovery, active people require more micronutrients in their diet. “More of everything” is a safe bet, but there are a few key nutrients that working out especially depletes:
Zinc: Exercise, especially weight training, works better with plenty of testosterone on hand to build muscle and develop strength. Zinc is a key substrate for the production of testosterone, and studies show that exercise probably increases the need for zinc. In fact, one study found that exhaustive exercise depleted testosterone (and thyroid) hormones in athletes, while supplementing with zinc restored it.
Magnesium and Other Electrolytes: Magnesium is required for a number of physiological processes related to workout recovery, including oxygen uptake by cells, energy production, and electrolyte balance. Unfortunately, as one of the main electrolytes, lots of magnesium is lost to sweat during exercise. The same could be said for other electrolytes like calcium, sodium, and potassium, but most people get plenty of those minerals from a basic Primal eating plan. Getting enough magnesium, however, is a bit tougher, making magnesium deficiency a real issue for people trying to recover from workouts.
Iron: Intense exercise depletes iron, which is instrumental in the formation of red blood cells and oxygen delivery to your tissues during training and the immune response after it. They even have a name for it—exercise-induced anemia.
Soreness
Post-workout delayed onset muscle soreness, or DOMS, is no joke. While many of you folks reading this probably enjoy DOMS and take it as feedback for a job well done, it’s a hurdle that many beginners never move past. They join a gym, d0 a workout, feel great, go to bed feeling awesome, sleep like a baby, then wake up and find they have the bipedal capacity of a three-month-old. They can barely walk. Lifting their arms to brush their teeth is agony. Walking downstairs is out of the question. Some will move past the DOMS and get back into the gym. Many will not.
Low Fuel Availability
Working out expends energy. That energy must be replenished before you’re fully recovered and prepared to do another workout. Unless you’re trying to increase efficiency by training in a state of low fuel availability, like the “train low-carb, race high-carb” method, you should recover what’s been lost. What you replenish is conditional on the type of exercise you did. If you went for a long hike or easy bike ride that burned primarily body fat, you don’t need to—and probably shouldn’t—”replenish what you lost.” If you’re coming off a 30-minute full body CrossFit session that left you gasping on the ground in a puddle of sweat, you probably have some glycogen stores to refill.
This is a common issue for folks trying to lose weight through diet and exercise. Inadequate calorie intake coupled with intense exercise sends a “starvation” signal to the body, causing a down-regulation of anabolic hormones. Instead of growing lean mass and burning body fat, starvation (whether real or simulated) promotes muscle atrophy and body fat retention. Either alone can be somewhat effective, but combining the two for too long will only impair recovery.
Alcohol
Drinking directly impairs muscle protein synthesis, the essential step in muscle recovery and adaptation to training. Moderate or “social” drinking is probably safe (just don’t use alcohol as a post-workout recovery drink), but even just a single day per week of binge drinking is linked to 4x the risk of sarcopenia, or muscle-wasting. It’s hard to recover from your workouts if your muscles are atrophying.
Oddly, drinking directly after a training session also increases testosterone levels. One theory is that testosterone levels rise after drinking because it becomes less bioavailable; your muscle cells’ resistance to testosterone goes up, so it just circulates and gives “false” readings.
Things You Can Try
The obvious thing to try is the opposite of all the modifiable and preventable recovery-inhibitors mentioned above. Get good sleep, don’t drink too much (especially post-workout), get a handle on your stress, eat enough food, eat enough protein, get your micronutrients. What else?
Watermelon
L-citrulline is an amino acid found in watermelon that shows a significantly ameliorative effect on post-workout muscle pain, or delayed onset muscle soreness (DOMS). You can also supplement directly with L-citrulline, which may work, but watermelon is so good right now with a little salt, lime juice, and cayenne pepper, and it’s actually lower in carbs than you probably think (about 10 grams per cup of watermelon). I recommend fresh watermelon over pasteurized juice, as heat treatment reduces the effect.
Beets
Beets (and beet juice) aren’t only good for exercise performance. They also reduce DOMS. Nitrates have been posited as the primary constituent responsible for the effect, but beet juice works better than pure sodium nitrate.
Tart Cherry Juice
Tart cherry juice is best used to recover during competition, when your primary concern is to get back out there and perform. Its extreme effectiveness at killing muscle pain, reducing local and systemic inflammation and exercise-induced muscle damage suggests it may hamper training adaptations, however. It does also improve sleep, which should translate into better adaptations.
Massage
Massage feels great, and the evidence shows that it’s great for recovery from exercise. It alleviates DOMS. It speeds up the recovery of muscle strength and enhances proprioception. It improves central nervous system parasympathetic/sympathetic balance, even if the masseuse is one of those weird back massage machines.
Compression Garments
These aren’t just for show. A recent meta-analysis of the available research concluded that compression garments enhance muscle recovery after strength training and improve next-day cycling performance.
Whey
Compared to other proteins, whey protein accelerates muscle adaptation to eccentric exercise.
Creatine
Although we get creatine from red meat and fish, supplementary creatine can boost our recovery from exercise via a couple mechanisms. First, it increases muscle content of phosphocreatine. That’s the stuff we use for quick bursts of maximal effort, so carrying a little extra can do wonders for our ability to perform. Second, it enhances muscle glycogen replenishment without increasing insulin.
Fish Oil (or Fatty Fish)
Adding fish oil to a recovery drink reduced post-workout muscle soreness without affecting performance. Fish oil may also enhance muscle recovery from and adaptation to strength training.
Cold Water
A cold water plunge after training enhances the recovery of muscle function. However—and this is a big “however”—post training cold water plunges also seem to impair long term muscular adaptations to resistance training. In other words, a cold plunge might help you get back in the game for the short term at the cost of long-term adaptations.
More Carbs
I always say “Eat the carbs you earn.” While that often means eating fewer carbs than before, it can also mean eating more if you’ve trained hard enough to warrant them. This even applies to keto folks; depleting glycogen through exercise creates a “glycogen debt” that you can repay without inhibiting ketosis or fat-adaptation too much. The carbs—which you don’t need much of—go into muscle glycogen stores for recovery and later use without disrupting ketosis.
Don’t take this final section as a blanket recommendation, however. Before taking ice baths, dropping $500 on massages every week, taking a long list of expensive supplements, and walking around in a full body compression suit, make sure you’re sleeping, eating enough food, and giving yourself enough time between workouts. Quite often, handling the basics will be enough.
What have you found to be the best way to recover from your training? What are the biggest roadblocks? Let me know down below, and thanks for reading!
(function($) { $("#dfvjzj4").load("https://www.marksdailyapple.com/wp-admin/admin-ajax.php?action=dfads_ajax_load_ads&groups=674&limit=1&orderby=random&order=ASC&container_id=&container_html=none&container_class=&ad_html=div&ad_class=&callback_function=&return_javascript=0&_block_id=dfvjzj4" ); })( jQuery );
ga('send', { hitType: 'event', eventCategory: 'Ad Impression', eventAction: '66337' });
The post What Causes Slow Post-Workout Recovery—and What Can You Do About It? appeared first on Mark's Daily Apple.
Article source here:Marks’s Daily Apple
0 notes
Text
How to Talk to Your Clients About Hormones
If your goal in life is to be a weight-loss guru, a bestselling author, and/or a supplement mogul, you can do it in three easy steps:
1. Fixate on a single hormone or hormone category.
2. Give that hormone credit or blame for everything a potential customer wants to have more or less of.
3. Come up with a training program, diet, and and/or nutritional product to enhance or counteract that hormone’s actions.
Granted, the competition is fierce for anything related to sex, muscle mass, or body fat. But all it takes is one new study—or someone hyping up a really old one—to crank up interest all over again.
Dr. Karl Nadolsky has a simple explanation for why there’s so much interest in molecules that so many of us pretend to understand but so few actually do:
“Hormones are sexy,” he says. “They’ve always been sexy. That’s why I went into endocrinology.”
Nadolsky is a clinical endocrinologist in Grand Rapids, Michigan, who’s also board-certified in internal medicine and a diplomate of the American Board of Obesity Medicine. Before medical school, he was a Division I wrestler at Michigan State, where he qualified for the NCAA tournament all four years.
And before all that, he was a lifter and athlete with an unusual ability to pack on muscle—a trait that got him interested in the endocrine system long before he knew what it was. “I’ve been accused of taking steroids since I was a little kid, even when I was prepubertal,” he says.
That’s why I figured Nadolsky would be the perfect guy to talk to about the most common misconceptions related to hormones, and the ways in which trainers should or shouldn’t talk about them with clients.
He sees the most confusion and misinformation in these three areas:
Adrenal system
Thyroid
Sex hormones
But before we get into the specifics, let’s take a step back and talk about hormones in general, and why they’re so difficult to understand without specialized training.
Blame It on Insulin
Your body manufactures some 50 hormones. It makes them everywhere from your brain to your throat to your sex organs. Your skin, bones, fat cells, muscles, organs, and gut all crank out one or more chemical messengers, each of them telling some part of your body what to do, or stop doing.
Virtually every human activity—eating, sleeping, thinking, moving—triggers, and is triggered by, hormonal signals. “All parts of the endocrine system interact to keep each other in some kind of harmonic balance,” Nadolsky says. “Even doctors don’t understand all the interactive pathways.”
We never think about the endocrine system when it’s all working according to factory specs. But when we suspect something has gone wrong, it’s all we can think about. And that’s where trainers are often too quick to jump into the weeds.
Take diabetes, for example. Those with type 1 diabetes need to take insulin because their bodies are incapable of making enough of it to clear glucose from the bloodstream. “Those patients can tend to gain weight,” Nadolsky says, as a result of nutrient partitioning from intensive insulin therapy. “That’s what some low-carbers use to show that insulin causes weight gain.”
Then there’s the well-known link between obesity and type 2 diabetes, a disease of blood-sugar regulation. One of its hallmarks is a drop in insulin sensitivity. The pancreas has to pump out more insulin initially because the tissues are less responsive, but ultimately fails to keep up. Unless the disease is checked, those patients may also end up needing insulin.
Because insulin and obesity are related, a lot of people have jumped to the wrong conclusion: that carbs, which temporarily raise insulin levels, cause obesity.
“All these things come from some sort of truth that gets altered to fit someone’s narrative,” Nadolsky says.
READ ALSO: How to Help a Client with Type 2 Diabetes
But at least diabetes is a real disease. When fitness pros talk about the adrenal hormones, the conversation often jumps from science to fiction.
Fatigued by the Adrenals
Have you heard of adrenal fatigue? Of course you have. It’s the scourge of modern life:
You burn the candle at all three ends with a high-pressure job, chaotic family life, and all-or-nothing training program. You run on adrenaline and cortisol until, at some point, your adrenal glands give out. You end up chronically tired, stressed, unmotivated, and foggy-brained.
But while the idea of adrenal fatigue makes sense, the diagnosis doesn’t.
“Physicians, naturopaths, and chiropractors, along with trainers and other lay people, sometimes propagate this contention of a disease state called adrenal fatigue,” Nadolsky says. “There is no such pathophysiology.”
Because it’s not a disease, there’s no test for it. And because there isn’t a test for it, anyone can claim a person has it, based on whatever criteria they think that person will find most believable. From there it’s just a short step to an alternative practitioner—well-meaning or otherwise—convincing one of your clients not only that she has it, but that the cure is a special combination of supplements the practitioner just happens to sell.
Your move:
You’re in no position to argue with someone your client considers a medical expert. But you can do three things:
Share this position paper from the Endocrine Society.
Recommend that your client get a second opinion, preferably from an endocrinologist like Nadolsky. Because there is a real condition called adrenal insufficiency, she may need more than a good night’s sleep.
Provide a less taxing training program, one that allows maximum recovery. But no matter how tired she is, encourage her to keep moving.
The Thyroid Challenge
“Thyroid problems are pretty common,” Nadolsky says. An estimated 12 percent of Americans, mostly women, have hypothyroidism—they produce too little of the crucial hormones that affect virtually part of your body.
Most of them don’t know they have it, either because they don’t have symptoms, or because the symptoms they have—fatigue, lethargy, depression, perhaps weight gain—are often diagnosed as something else. “But because it’s so common, more people think it must be the problem, even when it’s not,” Nadolsky says.
That’s when things get dicey. If a client becomes convinced she has a thyroid deficiency, she may take supplements that contain thyroid hormones. That, he says, can be dangerous, because too much thyroid hormone can lead to bone and/or heart damage, among other problems.
Another issue:
“People think they need to get a lot of tests,” he says, often at the advice of someone who stands to profit from those tests. But tests themselves don’t always show what we think they do.
“A hormone lab evaluation is extremely finicky,” he says. “Even I don’t understand all the nuances. Different lab assays have different problems that make them imperfect. You have to know what factors will change those labs, and what data the ranges are validated from.”
Your move:
If you think your client may be among the 12 percent with thyroid deficiency, recommend a full evaluation from their primary-care physician or an endocrinologist.
Exercise and a lower-calorie diet may help someone with hypothyroidism. But if a client tells you she has the opposite, hyperthyroidism, Nadolsky says you definitely want medical guidance before you give her a program.
The Mighty T
Once upon a time in America, it was understood that as men get older, their energy, libido, strength, and muscle mass will decline. That’s how aging is supposed to work. “But now every guy who’s middle-aged and has a little fatigue must have low testosterone,” Nadolsky laments. You can blame any number of suspects:
Pharmaceutical companies, which market drugs like Androgel directly to consumers.
“Anti-aging” clinics, which profit from diagnosing hypogonadism—low T—and selling hormone replacements to middle-aged men.
Gym culture, which rarely sees a problem that a little more testosterone wouldn’t fix.
The fixation begins with a kernel of truth: Natural levels of testosterone really do drop with age. But that doesn’t mean every older guy with lower T needs to have it topped off. In fact, the process of diagnosing hypogonadism is rigorous, and relatively few guys qualify for hormone replacement.
But even more important, Nadolsky says, is to identify the underlying cause of low T, and treat it, if possible.
Unfortunately, that’s not the message a lot of men hear from trainers, especially online trainers. “I honestly don’t understand why anyone would be pushing a specific hormone as a treatment,” he says.
Which is ironic, since trainers can actually do a lot to help those clients raise their endogenous T levels, especially those who are overweight or have obesity. Many of the problems men associate with low testosterone might also be associated with obesity:
Low energy
Low libido
Crummy mood
Low muscle mass
The solution can be simple, if not easy, Nadolsky says: “Free testosterone goes up with weight loss, and down with weight gain.”
That’s especially true if the man has sleep apnea, a common comorbid condition with obesity. Treating it can help restore his testosterone even before he loses a significant amount of weight.
Your move:
No matter what your client has been led to believe by friends, trainers, or TV commercials, hypogonadism isn’t something that can be diagnosed by a hobbyist. Even legit lab tests are just numbers on a sheet of paper. “Lab assays for testosterone have traditionally been very poor,” Nadolsky says. “We don’t treat numbers. We treat people.”
Your training program is a powerful tool. Higher volume is better than lower volume, and heavier weights are better than lighter ones.
Final Thoughts
We’ve only scratched the surface of what these hormones do, or the many ways health problems might arise when one or more of them malfunction, or the limited options trainers have when trying to help clients resolve those problems.
The biggest ones, though, are very much in your toolbox. “All endocrine systems benefit from exercise,” Nadolsky says. Exercise can make a client’s body more sensitive to insulin. It can reduce the fatigue and mood disorders linked to thyroid and adrenal issues. And it can raise testosterone directly.
All those benefits are enhanced with calorie reduction and weight loss. Type 2 diabetes and hypogonadism can be resolved by losing weight and treating related problems like sleep apnea.
Nadolsky shares this advice from Dr. Lou Pangaro, an endocrinologist at Walter Reed National Military Medical Center and his mentor: “Embrace complexity, but act with simplicity.”
So while a trainer’s moves may be limited, the impact of your work isn’t. You can have a dramatic effect on your clients’ health while staying in your lane and letting doctors handle theirs.
The post How to Talk to Your Clients About Hormones appeared first on The PTDC.
How to Talk to Your Clients About Hormones published first on https://medium.com/@MyDietArea
0 notes
Text
The coconut tree is a member of the family Arecaceae and the only species of the genus Cocos. The term coconut can refer to the whole coconut palm or the seed, or the fruit, which, botanically, is a drupe, not a nut.
Quick Facts:
Its Incredible Benefits & Uses Include;
_Natural Skin Moisturizer For Whole Body.
–Coconut oil for skin health & use as a moisturizer for face.
_It absorbs quickly, and is non-greasy. At room temperature,coconut is a solid, but it quickly melts when it comes into contact with hands.
_The oil is used to make soap and margarine and in cooking; the remains are used in cattle feed.
Nutritional Facts:
Coconuts also scientifically known as (Cocos nucifera) are abundantly nutritious and rich in fibre, vitamins C, E, B1, B3, B5 and B6 and minerals including iron, selenium, sodium,calcium, magnesium and phosphorous. Unlike cow’s milk, coconut milk is lactose free so can be used as a milk substitute by those with lactose intolerance.
Using and eating Coconut meat, drinking the juice, milking it or consuming it as oil, coconuts are a delicious and nutritious source of fiber, vitamins, minerals, and amino acids. It has tons of calcium, potassium, and magnesium, as well as plenty of electrolytes.

This natural herb is one of the wonderful resourceful economical nutritious plant in the nature that you can ever find! So be patient as I am about to reveal its amazing miraculous benefits which is very effective in the lives of millions more.
There we have more than 10 well known benefits not to mention others but hope its practical out there from traditional remedial uses to most genetically synthesized and processed products. Listed here are only 7 basic ones.
Fact #1. Regulates Thyroid Function.

Does Coconut Oil/milk Really Help? _ Unlike the polyunsaturated oils in many foods, coconut oil is high in (healthy) saturated fat, lauric acid, and medium chain fatty acids. It’s unique structure makes it a highly usable source of energy for the body and its particular fat balance is nourishing to the thyroid. coconut milk also helps in proper thyroid function. Thus Coconut milk speeds up metabolism and assists in the regulation and balance of thyroid functions.Coconut Oil/Milk promotes healthy thyroid function and helps to relieve the symptoms of chronic fatigue.
Fact #2. Improves Brain Function – (vitamin B1).

This vitamin B1 present in coconuts are amazing truth with benefit! Remember brain is the controlling tower stored with kinetic energy where body absorbs. Hence in the aid of brain function Coconut water’s minerals are utilized for hemoglobin function, ensuring healthy blood to flow all over the body. Coconut water contains vitamins B1, B2, B3, B5, B6, B7 and B9 (folate). 27. B1 improves brain function, protects the nerves, improves cardiovascular functioning, ensures eye health and is needed for energy production. It is an Energy Booster that provides a super nutritious source of extra energy. Coconut is utilized by the body to actually produce energy, rather than to store it as body fat. It supports improved endurance during physical and athletic performance.
Fact #3. Maintains Body Mass (Weight ).
If you’re under weight management or dietary then, I recommend Eating Coconut Oil Can Build Muscle Mass Faster And Increase Endurance. Coconut oil contains short and medium-chain fatty acids that help in taking off excessive weight and increases the body metabolism by removing stress on pancreases, thereby burning out more energy and helping obese and overweight people reduce their weight.
IMPORTANT FACT YOU SHOULD KNOW BY NOW!!!
Don’t you know that your waist size is a matter of aesthetics and also a powerful

indicator of a build-up of visceral fat, a dangerous type of fat around your internal organs that is strongly linked with type 2 diabetes and heart disease?
And there fore it is virgin coconut oil that shrinks your waist size!
Ingredient Aspect:
The coconut oil group presented:
Increased levels of HDL (good cholesterol)
Decreased LDL/HDL ratio
Reduced waist circumference/abdominal obesity
Fact #4. Stimulates and Boosts Immunity.
This function is a crucial one that plays positive role in the body cells so make it a habit with coconut oil in the kitchen instead of other cooking oils.
Comparable Measure other cooking oils. _Unsaturated vegetable oils, especially polyunsaturated ones like corn oil and soybean oil are structurally weak, making them highly susceptible to oxidation. Simply said, corn and soybean oils easily rot.
* Recent researchers have argued that polyunsaturated oils encourage cancer by harming the DNA of your cells. Because it’s highly saturated at 92 percent, coconut oil is ultra resistant to oxidative damage. Simply put, coconut oil can stay fresh for a long time. Coconut contains two special ingredients that make it excellent for immunity. These are anti-viral properties, commonly referred to as lauric acid and caprylic acid. Both are well-known for fighting off yeast overgrowth (candida), along with bacterial infections. If you care about long living the it’s nothing better than adding coconut oil to your daily meals.
Fact #5. Keeps Heart Healthy.
Coconut oil is about 90% saturated fat, which is a higher percentage than butter (about 64% saturated fat), beef fat (40%), or even lard (also 40%). Too much saturated fat in the diet is unhealthy because it raises “bad” LDL cholesterol levels, which increases the risk of heart disease. Most of the saturated fats in coconut oil comes from lauric acid, which can increase bad cholesterol (LDL) but also good cholesterol (HDL). Because it increases both good and bad cholesterol, the risk of using coconut oil may not be as significant, or even significant at all.
Fact #6. Improves Digestion.
This is a wonderful fact, happily coconut does not cause digestive upset; instead, it in fact, help with IBS, slow motility, inflammation, poor nutrient absorption, regularity, and can help seal the lining of the digestive tract that may be inflamed from leaky gut syndrome, inflammation, or other gastrointestinal. For decades, researches have recognized the ease of digesting coconut oil, compared to other fats. They contribute this to the medium chain fatty acids (MCFA) found in coconut oil.
Those anti-inflammatory benefits help heal injury to the digestive tract in patients who suffer from diseases like Crohn’s. Coconut oil is high in natural saturated fats. Saturated fats not only increase the healthy cholesterol (known as HDL cholesterol) in your body, but also help convert the LDL “bad” cholesterol into good cholesterols. By Increasing the HDL in the body, it helps promote heart health and lower the risk of heart disease.
Fact #7. Anti-Aging (Glows Skin).
The fatty acids found in coconut oil help work as an anti-inflammatory and anti-bacterial natural product. The vitamin E can help to fight damage to the skin thanks to its powerful antioxidant properties. Coconut oil is a natural way to hydrate your skin. Saggy skin benefits form proper hydration because it works to tighten and firm. Apply a bit directly to the loose skin several times per week. Lemon is a great source of Vitamin C. Because of its incredible health benefits, experts claimed that Coconut oil is used in many natural beauty products, for good reason and that is very true. By the truth that coconut oil is naturally antibacterial and antifungal.
Therefore coconut oil for skin is an excellent moisturizer, it can penetrate hair better than other oils, and, well, it smells like cookies. Coconut oil works as a topical lotion with no added chemicals or preservatives. The second benefit comes from three specific fatty acids that have strong anti-fungal and antimicrobial properties. A third benefit is vitamin E, which has long been known to keep skin healthy and have anti-aging benefits
*The bonus is that it will leave the skin hydrated and soft and reduces Acne or pimples.
In conclusion coconut oil is served;
To soothe dry hands.
As a cheekbone highlighter.
To shave your legs.
As a deep-conditioner.
To remove eye makeup.
As a body moisturizer.
To clean your face.
To add shine and more and so forth…
Should you have queries,questions or want to add on our discussion please don not hesitate to hit a comment box below thanks.
Surprising Health Benefits of Coconut Oil. The coconut tree is a member of the family Arecaceae and the only species of the genus Cocos.
#Aging skin#Anti-Aging (Glows Skin).#Boost Brain Memory#Brain Health#coconut milk#Garlic orf Skin and Hair#Health Benefits of Coconut Oil#Improve Eye Health#Improve The Immune System#Improves Brain Function - (vitamin B1).#Improves Digestion.#Improves Memory#Improves Brain Health#Ingredient Aspect:#Keeps Heart Healthy.#maintaining healthy skin#Maintains Body Mass (Weight ).#nourishing to the thyroid.#Nutritional Facts#Reduces Weight#Regulates Thyroid Function.#skin#Skin lightening.#Weight Control#Weight loss
0 notes
Text
New Post has been published on Healthy Food and Remedies
New Post has been published on http://www.healthyfoodandremedies.com/2017/05/04/roots-mental-health-maybe-theyre-not-heads/
The Roots of Mental Health—Maybe They’re Not In Our Heads
The number of people—and women in particular—who are taking antidepressants worldwide has skyrocketed in recent years. Here in the States, the count is at 30 million. One out of every four women in their forties and fifties takes them. And antidepressants aren’t just being prescribed for depression; they’re being given to those of us struggling with PMS, stress, irritability, anxiety, lack of sleep, and so on. But what if antidepressants aren’t a cure for any of these conditions, or even a safe way to treat the symptoms?
In her book, A Mind of Your Own, Dr. Kelly Brogan (board certified in psychiatry, psychosomatic medicine, and integrative holistic medicine) argues that our common understanding of depression as a disease caused by chemical imbalances in the brain is…entirely wrong. Lifestyle imbalances, and inflammation, she explains, are actually at the root of depression and anxiety. Dr. Brogan’s case against conventional medicine—backed up by a veritable library of shocking research studies, along with personal stories we can all relate to—is very compelling. As are her suggested solutions (and 30-day action plan) for finally feeling well and like yourself, pill-free. Below, Dr. Brogan shares a new paradigm for mental health.
A Q&A with Kelly Brogan, M.D.
Q
One of your big arguments is that depression is not a disease, but a symptom—can you explain?
A
We have been told a story about depression: that it’s likely genetically driven and if it develops, it’s because of brain chemical imbalances that require management by chemical medications, often for the rest of our lives. This is a false tale that has been sold to us by an industry that has influenced the training of doctors and has spent billions on messaging patients through direct-to-consumer advertising. I invested my entire career in this narrative as a conventionally trained psychiatrist until I learned the truth.
In six decades, there has been no evidence of a discrete chemical imbalance that causes depression. This isn’t all that surprising, however, when you zoom out a bit to realize that depression is not one thing. It is an indication of imbalance. It’s as if your toe hurts—it can hurt because you have an infection in the toenail, you have a string tied around it too tight, or you dropped a hammer on it. The hurting is just an invitation to investigate further to identify the best way to resolve the problem.
It is time, even according to leaders in the field, to let go of the chemical imbalance theory and take a fresh look at what the science says. Depression is rooted in inflammation, not the brain. The human body interacts with its environment with deep intelligence. Your body creates symptoms for a reason. Depression is a meaningful symptom of a mismatch, biologically, with lifestyle—we eat a poor diet, harbor too much stress, lack sufficient physical movement, deprive ourselves of natural sunlight, expose ourselves to environmental toxins, and take too many drugs. Inflammation is the language that the body speaks, expressing imbalance, telling you that something is wrong somewhere that needs your attention. We usually suppress these symptoms with medication, but that is like turning off the smoke alarm when you have a fire.
What if your depression is actually a thyroid imbalance? Blood sugar instability? Food intolerance or a side effect of a medication? It makes little sense to treat any of these reversible conditions with a psychiatric medication, but it’s easy to fall into the trap of the quick fix, particularly if you are a woman. Women are twice as likely to be prescribed medication when they present to their doctors with complaints like flat mood, fogginess, poor concentration, poor motivation, and feelings of overwhelm.
Depression is an opportunity. It is a sign for us to stop and figure out what’s causing our imbalance rather than just masking, suppressing, or rerouting the symptoms. It’s a chance to choose a new story, to engage in radical transformation, to say yes to a different life experience.
Q
Modern antidepressants are based on the idea that serotonin improves mood. But you make the case that this is all a myth—how?
A
Despite being taught, in my training, that antidepressants were to the depressed (and to the anxious, OCD, IBS, PTSD, bulimic, anorexic, etc.) what glasses are to the near-sighted, I don’t buy this anymore. I don’t think patients are getting the whole truth.
Here’s the deal: There is not a single human study that supports the “monoamine hypothesis” of depression, which is the idea that depression is caused by a certain kind of chemical imbalance in the brain, such as under-activity of serotonin. The only studies in which tryptophan (an amino acid precursor to serotonin) depletion resulted in depression were in patients who had previously taken antidepressants.
Imaging studies, post-mortem suicide assessments, and animal models have never yielded consistent patterns of neurotransmitter levels, metabolites, or receptor profiles. Compelling discussions by Drs. Joanna Moncrieff and David Cohen suggest that antidepressants actually create abnormal states rather than repair them. They use the analogy of alcohol’s disinhibiting effects: The fact that booze can ease one’s social phobia does not imply that alcohol is an appropriate treatment or a correcting agent.
Direct-to-consumer advertising in America has allowed pharmaceutical companies to “teach” the public about brain chemical imbalances and serotonin deficiencies through cleverly worded taglines and absent FDA-policing.
But they do work! Say many patients and their prescribers. And they do work! Sometimes. Thanks to active placebo effect or expectations of relief that manifest as actual physiologic changes—as demonstrated by Harvard’s Dr. Irving Kirsch, a placebo effect expert. (He also collected unpublished data to show that more studies demonstrated lack of effect compared to marginal benefit largely attributed to placebo.)
Q
What’s the thread that connects our gut and brain to inflammation and depression?
A
I think that for most of us, the impact of the brain on the gut is intuitive. We’ve all had butterflies with excitement, lost our appetite when we’ve fallen in love, or had diarrhea before a big performance or event. What’s less intuitive, but now has been substantiated by two decades of medical research, is the impact of the gut on the brain. We now understand that the gut communicates information to the brain about the environment and that the microbial ecology of our gut—the microbiome—manages this communication. The language used by the body is inflammatory messengers.
In this way, depression joins the ranks of all of the diseases of modern civilization, including heart disease, autoimmunity, and cancer. The body is setting off alarm bells in the form of inflammation in an effort to adapt to perceived stressors. The most powerful way to send a signal of safety is to heal the gut through whole foods. Ancient medical practices from Ayurveda to Chinese medicine have known this for thousands of years. We are just learning about the complex interconnectedness between all of these systems we have come to believe are separate entities.
Q
How does food affect our mood, and what kind of diet do you recommend to your patients struggling with stress/anxiety/depression?
A
We don’t eat food anymore. We eat food-like products, and when we eat actual foods, they have often been grown in depleted soil, shipped across the globe, and saturated with chemicals. Food is not just fuel, though. Food is information, and it speaks to our genes. We no longer can get away with eating food that screams at our genes. We need food that whispers a love song. The wrong food can impact your mood by driving blood sugar imbalance (which can masquerade as anxiety attacks, chronic fatigue, ADHD, and depression), by impacting your brain through your immune system in the case of dairy and wheat, and by depriving you of nutrients essential to balance hormones, your gut, your immune system, and your nervous system.
I work with a dietary template that I used to put my own Hashimoto’s thyroiditis into remission and that has worked with hundreds of patients. It is a diet high in natural fat, and organic foods, including those from animals. As a former ethical vegetarian, it has taken a lot of research, learning, and mentorship from the now late Dr. Nicholas Gonzalez to appreciate the role of animal foods in healing certain conditions. In the end, the dietary template I recommend often just “feels right” to the women it is meant to heal. It’s almost like I’m giving them permission to eat what they already know, deep down, that they should be eating.
Q
What’s the latest research on the link between toxins and anxiety/depression?
A
We are swimming in a sea of 80,000+ unstudied chemicals that we never evolved, over 2.5 million years, to recognize. Our immune systems are ablaze because of it and our hormones are going haywire. I have grave concerns about endocrine-disrupting plastics, about fluoride in our tap water that directly affects the brain and thyroid, about pesticides that decimate healthy gut bacteria, and about neurotoxic metals like mercury and aluminum. Mostly, we are beginning to see that the dose doesn’t necessarily make the poison and that small amounts of these chemicals combine and interact with our systems in unique ways to cause significant problems, many of which manifest psychiatrically.
We have to also include medications, now the third leading cause of death in America, in this discussion. Medications from antibiotics to birth control pills to antacids to over-the-counter pain relievers to even antidepressants themselves are based on a one-size-fits-all model of human physiology. This can be Russian Roulette-causing, and perpetuate chronic mental illness.
Q
What are other important lifestyle changes that can make a significant difference?
A
I put food first and I work with my patients to take this “prescription” very seriously. I want them to experience an internal shift through prioritizing nutrition. When they do, they understand that the power to change their experience was always just under their nose. They don’t need a doctor or a guru. They just need to get back to basics and honor themselves.
I also ask them to start with 3-12 minutes a day of a Kundalini yoga medical meditation. We have to rewire the nervous system, our perceptions, and release fear. In my experience, this ancient technology can take you there and beyond, very quickly.
I ask them to move. This can be 20 minutes a week of high intensity, low volume interval training on an elliptical. It can be dance or yoga.
I ask them to honor their sleep and we begin detoxification of their home environment—products, air, water, and electromagnetics.
We also engage in a mindset shift. Through this process, we remember what we have forgotten—that the body is best at self-healing if we just get out of our own way. We realize that we can reclaim something we gave away. Something that’s not available through a model of care based on life-long pharmaceuticals. It’s that feeling that we are always missing something even if our symptoms are “managed.” It’s our personal power and fearlessness. With this, anything is possible, including becoming medication-free after decades of exposure. Remember, this is your journey for a reason and there are no regrets.
Q
Which medical tests can actually help pinpoint the root cause of what we commonly think of as mood disorders?
A
At the very start of treatment, as my patients begin my strict dietary protocol, I order the following tests:
Thyroid function tests: TSH, free T3, free T4, thyroid autoantibodies, and reverse T3
Underlying genetic variant: the MTHFR gene test (the MTHFR gene produces the MTHFR enzyme, methylenetetrahydrofolate reductase, which is essential for several bodily processes that directly tie into mental well-being)
Signs of vitamin B12 deficiency: serum vitamin B12 levels and homocysteine levels, which can detect B12 deficiency as well
Levels of inflammation: High-sensitivity C-reactive protein
Blood sugar balance: Hemoglobin A1C
Vitamin D deficiency: Levels of 25OH vitamin D in the blood
Q
For people who are on antidepressant meds and who want to get off them, what’s your recommendation?
A
This has become my unintended specialty. I have learned that these medications can be some of the most challenging of all chemicals to detox from and that their withdrawal syndromes are serious. I believe everyone deserves a chance at a new chapter and a shift in mindset to one that embraces their human experience as meaningful and rejects the illusion of the magic pill that promises to keep you punching the clock. When my patients decide they are ready to taper off of medication, first we begin with healing their body. If you imagine yourself to be a bucket that is almost full, the stress of a taper is likely to cause overflow. If we can drain the bucket with lifestyle changes like those outlined in my program first, then the taper can be a relative breeze.
A typical pace can be determined after a “test dose” decrease of approximately 25% of the total daily dose. After 2-4 weeks, if this has been tolerated, this increment can be attempted at a pace of every 2-4 weeks. Many patients will need to drop down to 10% of the total dose, particularly closer to the final 25% of the total dose. Because withdrawal effects can be delayed and fluctuate, it can be challenging to identify whether symptoms are related to a recent dose decrease or even a previous one. Remaining stable for several months may sometimes be necessary before proceeding.
In my practice, I never taper if fear is the dominant emotion. We have too much data that tells us about the power of what is called expectancy (belief around what is happening in treatment) to determine the outcome of an intervention. If you are afraid of life without meds, life without meds will come back to scare you. If, on the other hand, you feel empowered, energized, and excited about awakening to your true self and moving through this window, then you will succeed. I do not start patients on meds under any circumstances, so if they struggle after a completed medication taper, we never return to meds. This means that we ask why they are struggling, we investigate whether it is physiologic and/or psycho-spiritual, and we commit to sitting in it for a bit, making space for it, until it becomes clear. This is a different mindset. It’s one of tolerance, patience, and trust. Fear is something we name, acknowledge, and allow, but do not engage or react from.
0 notes
Text
The Best Probiotic to Buy: 8 Essentials
Are you having problems picking the best probiotic for you? Here’s the complete guide to get it right!
You’ve probably heard that “probiotics are good for you.” After all, it seems like everyone, from Dr. Axe and Dr. Oz, to yogurt commercials, Cosmo magazine and even your primary care doc is talking about them.
In fact, over the past 10 years alone, the probiotic trend has witnessed over a 300% growth in sales, and kombucha bottles that one were hidden alongside sweet tea and sparkling water, now take up entire drink case walls at Whole Foods Market.
But, pop question: What exactly are probiotics?
Answer: essential healthy strains of gut bacteria that mimic the healthy gut bacteria that should be in your gut…but often are not.
Why Your Gut is Important
A healthy gut equals a healthier you. And healthier gut bugs (bacteria)—and lots of different types of them—equal a healthier gut.
Think of your digestive tract as the foundation of a house, and your gut bacteria as nails, sturdy wood, windows, doors and everything else that makes your house livable, or “healthy.” Your digestive tract is responsible for absorbing EVERY single nutrient you eat, as well as filtering out every single toxin you come in contact with, throughout your life.
Your gut determines whether or not your body’s cells and organs get fed and nourished to function, as well as keeps all body processes working in tip top shape. Your gut bacteria as what drive your body’s digestive system, helping it do its job—stay free from infection, and digest and absorb your nutrients properly.
Probiotics 101
Probiotics are healthy gut bacteria, found in supplements and fermented foods that can be taken or eaten to give your gut and body an extra oomph of “gut love” support.
Although the word “bacteria” may sound like a bad or icky thing, gut bacteria are an essential component to all human life and health.
Every human body is comprised of more than 100 trillion gut bacteria—10 times the amount of cells in your body. These gut bacteria influence the health of every body system and function.
In an ideal (healthy) world, most of your gut bacteria are healthy, vibrant and strong. However, if you experience health imbalances, theres a good chance some of this gut bacteria is unhealthy, infected, decreased or overgrown.
Gut Bacteria’s Role in Weight Gain, Acne, Allergies & More
Countless research shows that unhealthy or imbalanced gut bacteria is directly linked to a variety of health conditions (1), including:
Diabetes
Anxiety
Allergies
Autoimmune Disease
Thyroid Disorders
Headaches
ADHD
Heart Disease
Unwanted Weight Gain
Hormone Imbalances (PMS, infertility, PCOS)
Osteoporosis
Depression
Anxiety
Diarrhea
Constipation
Leaky gut syndrome
Irritable bowel syndrome
Fatigue
Autism
Parkinson’s Disease
Cancer
Rheumatoid Arthritis
Mood Swings
Brain Fog
—And just about every other chronic condition or disease you can think of!
How Your Gut Bacteria Gets Unhealthy
A variety of stressors wreak havoc on the balance (yin-yang) of your gut health. Like a wasp nest, if your body undergoes too much stress to handle at once, or stressors linger over time (like eating processed foods for years), then that wasp nest gets unhappy—and the gut bacteria become imbalanced or unhealthy.
Common triggers that stir your gut’s “wasp nest” include:
Low veggie intake
Nutrient deficiencies (low protein, low carb and/or low fat diet)
Inflammatory foods (grains, nuts, dairy, sugar, sweeteners, processed foods)
Eating lots of bars, shakes and packaged foods
Lack of sleep
Not chewing your food well and eating in a hurry/on the go
Eating out ALOT (industrial seed oils)
Poor food hygiene (not washing your food or hands before meal prep, eating old food)
Sedentary lifestyles OR overtraining
Circadian rhythm dysfunction
Tap water
Toxin-laden skin care, beauty, hygiene and cleaning products
Plastics & BPA ingestion
Heavy metals exposure (in fish, teeth fillings, metal retainers/braces, etc.).
What to Do About It: 5 Daily Gut Habits
Love your gut by establishing a healthy gut routine for baseline gut maintenance…. the best probiotics included.
Just like you brush your teeth every day to maintain healthy teeth and shower most days to maintain a clean body, daily gut-health habits are essential for maintaining a healthy gut.
My top 5 Daily Gut Habits include:
Water. Drink half your bodyweight in ounces of water
Apple Cider Vinegar. Add 1 tbsp apple cider vinegar to 2-4 oz. of water with meals
Probiotic & Prebiotic. Take a daily soil-based probiotic and prebiotic fiber, along with eating fermented foods and prebiotic foods.
Variety. Eat variety and lots of color (even on a limited diet, don’t eat the same things every day)
Soothe. Sip a daily cup of herbal tea and/or bone broth. Bonus: Add in a gut-lining and repair support, such as L-Glutamine, colostrum or collagen.
Bonus:
In addition, beyond just managing daily gut health, it is highly beneficial to also complete some basic gut testing to address any other underlying gut issues that won’t just go away with probiotics alone (things like SIBO, IBS, leaky gut, etc.).
Like a regular health check up at your doctor’s office for your vital signs and bloodwork, comprehensive gut health testing can give you a clear picture into what is going on “under the hood” and the health of your gut bacteria in general.
How to Buy the Best Probiotic
Now that you know why probiotics are GOOD for you, which probiotic should you choose?!
Here are 6 essentials you should know to buy the best probiotic for you…
Buy the Best Probiotic for You: 6 Essentials to Know
#1: Buyer Beware: 95% of Probiotic Supplements Don’t Contain the Probiotics They Claim
It’s been speculated, that upwards of 95% of probiotics sold on shelves do NOT contain the probiotics they claim.
Why? Temperature plays a role in the stability of probiotics. Poor processing and manufacturing practices, hot shipping conditions on 18-wheelers and improper storage of probiotics in supplement form can wreak havoc on the cultures inside the capsules.
This is especially true for lactobacillus and bifidobacteria probiotic strains, that are particularly sensitive to heat, processing and even digestion. For instance, an investigative review of probiotics in mainstream yogurts (claiming to be “good sources of probiotics”) found that none of the yogurts actually contained probiotics at all (2)—due to the manufacturing process, followed by cooling process. And even if probiotics are found in the supplement or foods, many probiotic supplements do not survive the heat and acids produced during digestion (especially in the absence of prebiotic fiber—essential fiber to help probiotics “stick” in your gut and make it to your large intestine, where the majority of gut bacteria reside).
For MOST supplements (particularly lactobacilli and bifidobacteria), high heat can degrade the liveliness of these organisms. Even under ideal storage conditions, the number of probiotics will slowly decline as months go on. For example, a typical number is a drop of 5% per month when stored in a refrigerator after opening. The exception? Soil based organisms—shelf stable supplements containing bacteria that mimic the same bacteria found in nutrient-rich soil and foods that humans consumed and thrived upon for years (before the Agricultural and Industrial Revolutions of food processing).
The Bottom Line: Although a probiotic label may claim that there are certain amounts or types of bacteria in the supplement, many probiotics are rarely if ever tested after production by manufacturers—meaning what started out as 100 billion strains of lactobacillus bacteria, may only end up as 5 billion strains by the time it hits shelves—and many do not survive high heat.
Q. So Which Probiotic Supplements are Quality?!
To benefit from the best probiotics and promote longevity of your probiotics opt for supplements containing:
Soil-Based Organisms with strains within the 6-10 billion range (as most of these are well-tolerated by most people). Look for names and strains such as:
Bacillus clausi
Bacillus subtilis
Bacillus coagulans
Baciullus Bifidus
Bacillus IndicusBacillus licheniformis
Saccharomyces boulardii
E. coli Nissle 1917
Quality refrigerated lactobacilli and Bifidobacterium strains of probiotics (see list below)
#2. You Get What You Pay For
Are probiotics a waste of money?! Nope. But, as mentioned in point #1, investing in quality probiotics is essential. No, you don’t have to pay $100 for “quality,” but in today’s market good probiotic will typically run anywhere between $30-$80. Chances are that $10 generic probiotic from Whole Foods, or fat free yogurt labeled “good source of probiotics” is basically all hype.
See the rest of this article to shop smart for your probiotics, but a good general rule of thumb to:
Spend the majority of your probiotic supplement money on Soil Based Organisms in supplement form (the most stable probiotics on shelves)
Purchase select amounts of lactobacilli and bifidobacteria from reputable manufactures with high-quality standards (see list below)
Incorporate real food probiotics and prebiotics in the form of fermented foods (sauerkraut, pickled veggies, full fat grass fed yogurt and kefir, limited low-sugar kombucha, and prebiotic fibers) into your daily diet
#3. There are 4 Main Types of Probiotic Bacteria & You Need Them All
Just like there are different types of phones you can buy different types of makeup you can buy (blush, powder, eyeshadow), there are different types of probiotic bacteria that all operate as gut bacteria (just like makeup helps makeup your face), but these bacteria have some distinct characteristics, purposes and differences. The 4 main types of probiotics include:
Soil Based Organisms
Lactobacilli (Lactobacillus acidophilus and Lactobacillus GG)
Bifidobacteria
Some healthy yeasts (like Saccharomyces boulardii)
Each type serves a unique purpose and we need a mix of all of them for a healthy gut microbiome—both in foods and supplements.
#4. Mix it Up: Not All Probiotic Strains Are Equal
Within the 4 main classes of probiotics (lactobacilli, bifidobacteria, soil-based organisms and yeasts), there are also hundreds of different strains of probiotics (just like there are hundreds of different brands of makeup—Clinique blush, MAC blush, Bobbi Brown blush, etc.). In fact, the human body contains 500 different strains of probiotic bacteria (such as Lactobacillus acidophilus, Lactobacillus Rhamnosus, Lactobacillus Plantarum, Bifidobacterium Infantis, Bifidobacterium Bidifum, etc.).
Each type of probiotic strain has particular effectiveness and potency, especially depending on your personal gut profile overall.
For example, a specific kind of Lactobacillus, like Lactobacillus acidophilus, may help you prevent an illness, but that doesn’t necessarily mean that another kind of Lactobacillus, like Lactobacillus plantarum, would have the same effect, or that any of the Bifidobacterium probiotics would do the same thing. Another person may have an overgrowth of Lactobacillus acidophilus, and experiencing symptoms of SIBO (bloating, gas, constipation), whereas another person may have no Lactobacillus acidophilus at all, and suffering from autoimmunity and fatigue.
In short: not all probiotics are created equal and incorporating a variety of types AND strains of probiotics is essential.
#5. You Need Pre-biotics & Postbiotics to Make Your Probiotics Stick
Common Myth: For a long time, we’ve thought that taking probiotics is like putting gas into your car tank—you fill it up and there’s more gas. But it doesn’t work that way. Instead, probiotics only serve as “maintainers” or gatekeepers of the “good” gut bacteria that you have ALREADY in your body—but they don’t produce more. And once you take them, they can be GONE in a matter of hours, UNLESS your have pre-biotics and post-biotics support!
Pre-biotics are starches and fibers (found in supplements and some foods like green-tipped bananas, plantains, cooked and cooled sweet potatoes and squashes, onions, and leeks)—that serve as food for your probiotics. In fact, pre-biotics are arguably MORE important and necessary than probiotics because they HELP your probiotics STICK AROUND and increase probiotic counts in your gut. (i.e. Pre-biotics feed your probiotics).
In addition, post-biotics (also known as “short chain fatty acids”) are the extra 1-2 punch to help you get the biggest bang for your probiotic buck! Short chain fatty acids, like butyrate, are the “gifts that keep on giving” to your gut, long after your probiotic and prebiotic foods and supplements have been digested. Healthy gut bacteria produce “short chain fatty acids” that help maintain overall gut balance in your gut as a whole (not too many of any one strain of bacteria). Unfortunately, since many folks have unhealthy or imbalanced gut bacteria to begin with (approximately 3 in 4 people have “gut issues”), short chain fatty acids also are reduced. The result? Without short-chain fatty acids, you may continue to experience imbalances in your gut bacteria.
The Bottom Line: Pre-biotics and post-biotics (short-chain fatty acids) help multiply your probiotics so you CAN increase YOU beneficial bacteria over time. (See recommendations below).
#6. If You Feel Sick, You May Have Other Gut Problems…
Probiotics make you break out or feel nauseas? If these symptoms continue longer than 7-14 days after starting a new probiotic, it may indicate you have other gut issues going on (such as bacterial overgrowth, parasites, leaky gut, etc.), OR you ALREADY have enough of the strains of probiotics you are taking.
“Healing reactions” are normal for many folks when first starting a probiotic (such as skin breakouts, loose stools, rashes, etc.) and can be a sign that your gut bacteria are getting “stirred up” (especially if you’ve had imbalances for some time).
However, if these reactions linger longer than a week or two, it’s vital to consider what else is going on under the hood.
The Bottom Line: If your probiotics are making you sick, consider getting a gut test completed or working with a practitioner to help you problem solve root issues going on.
Best Probiotic Recommendations
1. Soil Based Organisms
Megaspore Probiotic
Seed Daily Synbiotic
Primal Probiotic
Garden of Life Primal Defense Ultra (not good for SIBO or bloating)
2. Lactic Acid Bacteria
Klaire Labs Therabiotic (best general overall probiotic)
Ideal Bowel Support (best for constipation)
VSL #3 (best for loose stools)
Elixa Probiotic
3. Prebiotics
Glucomannan
Partially Hydrolyzed Guar Gum
4. Short Chain Fatty Acids
Enterovite by Apex Energetics**
Sodium-Potassium Butyrate by Body Bio
5. Fermented Foods
Fermented Veggies (carrots, beets, cucumber relish, dill pickles, etc.)
Pickled Veggies (no added sugar or additives)
Fermented Salsa
Fermented Horseradish
Goat’s Milk Yogurt & Kefir
Coconut Kefir
Water Kefir
Coconut Yogurt (no additives)
Low-Sugar Kombucha (5-6 grams per serving)
Beet Kvass
Kimchi
6. Prebiotic Foods
Asparagus (al-dente)
Coconut Flour
Cooked & cooled potatoes/sweet potatoes and squashes
Cooked and cooled Jasmine white rice & lentils
Garlic
Green tipped plantains/bananas
Jerusalem Artichoke
Onions
Mushrooms (reishi, shiitake and maitake)
Nutritional Yeast
Potato Starch or Plantain Starch
Seaweed/Algae (Beta-glucan, or ?-glucan—a soluble fiber)
**Contact us to place an order for practitioner grade supplements, not found on the web.
Probiotic Protocol
For basic daily gut maintenance, a healthy daily protocol includes:
Pre-breakfast:
1 Soil Based Organism Probiotic
Breakfast
Short Chain Fatty Acids
Lunch
Short Chain Fatty Acids
Dinner
Prebiotic Supplement
Post-Dinner
1 Soil Based Organism Probiotic
Bonus: Eat 1-2 fermented foods and 1-2 prebiotic foods daily
*Health Disclaimer: By reading and/or using this information you acknowledge you are responsible for your own health and decisions. Consult your healthcare practitioner for your specific health needs.
Resources:
Markowiak, Paulina; Śliżewska, Katarzyna.(2017). Effects of Probiotics, Prebiotics, and Synbiotics on Human Health. Nutrients, 9(9), 1021. doi:10.3390/nu9091021;
Scourboutakos, M., Franco-Arellano, B., Murphy, S., Norsen, S., Comelli, E., & L’Abbé, M. (2017). Mismatch between Probiotic Benefits in Trials versus Food Products. Nutrients, 9(4), 400. MDPI AG. Retrieved from
The post The Best Probiotic to Buy: 8 Essentials appeared first on Meet Dr. Lauryn.
Source/Repost=>
https://drlauryn.com/gut-health/best-probiotic-to-buy-8-essentials/ ** Dr. Lauryn Lax __Nutrition. Therapy. Functional Medicine ** https://drlauryn.com/
The Best Probiotic to Buy: 8 Essentials via https://drlaurynlax.weebly.com/
0 notes
Text
The Best Probiotic to Buy: 8 Essentials
Are you having problems picking the best probiotic for you? Here’s the complete guide to get it right!
You’ve probably heard that “probiotics are good for you.” After all, it seems like everyone, from Dr. Axe and Dr. Oz, to yogurt commercials, Cosmo magazine and even your primary care doc is talking about them.
In fact, over the past 10 years alone, the probiotic trend has witnessed over a 300% growth in sales, and kombucha bottles that one were hidden alongside sweet tea and sparkling water, now take up entire drink case walls at Whole Foods Market.
But, pop question: What exactly are probiotics?
Answer: essential healthy strains of gut bacteria that mimic the healthy gut bacteria that should be in your gut…but often are not.
Why Your Gut is Important
A healthy gut equals a healthier you. And healthier gut bugs (bacteria)—and lots of different types of them—equal a healthier gut.
Think of your digestive tract as the foundation of a house, and your gut bacteria as nails, sturdy wood, windows, doors and everything else that makes your house livable, or “healthy.” Your digestive tract is responsible for absorbing EVERY single nutrient you eat, as well as filtering out every single toxin you come in contact with, throughout your life.
Your gut determines whether or not your body’s cells and organs get fed and nourished to function, as well as keeps all body processes working in tip top shape. Your gut bacteria as what drive your body’s digestive system, helping it do its job—stay free from infection, and digest and absorb your nutrients properly.
Probiotics 101
Probiotics are healthy gut bacteria, found in supplements and fermented foods that can be taken or eaten to give your gut and body an extra oomph of “gut love” support.
Although the word “bacteria” may sound like a bad or icky thing, gut bacteria are an essential component to all human life and health.
Every human body is comprised of more than 100 trillion gut bacteria—10 times the amount of cells in your body. These gut bacteria influence the health of every body system and function.
In an ideal (healthy) world, most of your gut bacteria are healthy, vibrant and strong. However, if you experience health imbalances, theres a good chance some of this gut bacteria is unhealthy, infected, decreased or overgrown.
Gut Bacteria’s Role in Weight Gain, Acne, Allergies & More
Countless research shows that unhealthy or imbalanced gut bacteria is directly linked to a variety of health conditions (1), including:
Diabetes
Anxiety
Allergies
Autoimmune Disease
Thyroid Disorders
Headaches
ADHD
Heart Disease
Unwanted Weight Gain
Hormone Imbalances (PMS, infertility, PCOS)
Osteoporosis
Depression
Anxiety
Diarrhea
Constipation
Leaky gut syndrome
Irritable bowel syndrome
Fatigue
Autism
Parkinson’s Disease
Cancer
Rheumatoid Arthritis
Mood Swings
Brain Fog
—And just about every other chronic condition or disease you can think of!
How Your Gut Bacteria Gets Unhealthy
A variety of stressors wreak havoc on the balance (yin-yang) of your gut health. Like a wasp nest, if your body undergoes too much stress to handle at once, or stressors linger over time (like eating processed foods for years), then that wasp nest gets unhappy—and the gut bacteria become imbalanced or unhealthy.
Common triggers that stir your gut’s “wasp nest” include:
Low veggie intake
Nutrient deficiencies (low protein, low carb and/or low fat diet)
Inflammatory foods (grains, nuts, dairy, sugar, sweeteners, processed foods)
Eating lots of bars, shakes and packaged foods
Lack of sleep
Not chewing your food well and eating in a hurry/on the go
Eating out ALOT (industrial seed oils)
Poor food hygiene (not washing your food or hands before meal prep, eating old food)
Sedentary lifestyles OR overtraining
Circadian rhythm dysfunction
Tap water
Toxin-laden skin care, beauty, hygiene and cleaning products
Plastics & BPA ingestion
Heavy metals exposure (in fish, teeth fillings, metal retainers/braces, etc.).
What to Do About It: 5 Daily Gut Habits
Love your gut by establishing a healthy gut routine for baseline gut maintenance…. the best probiotics included.
Just like you brush your teeth every day to maintain healthy teeth and shower most days to maintain a clean body, daily gut-health habits are essential for maintaining a healthy gut.
My top 5 Daily Gut Habits include:
Water. Drink half your bodyweight in ounces of water
Apple Cider Vinegar. Add 1 tbsp apple cider vinegar to 2-4 oz. of water with meals
Probiotic & Prebiotic. Take a daily soil-based probiotic and prebiotic fiber, along with eating fermented foods and prebiotic foods.
Variety. Eat variety and lots of color (even on a limited diet, don’t eat the same things every day)
Soothe. Sip a daily cup of herbal tea and/or bone broth. Bonus: Add in a gut-lining and repair support, such as L-Glutamine, colostrum or collagen.
Bonus:
In addition, beyond just managing daily gut health, it is highly beneficial to also complete some basic gut testing to address any other underlying gut issues that won’t just go away with probiotics alone (things like SIBO, IBS, leaky gut, etc.).
Like a regular health check up at your doctor’s office for your vital signs and bloodwork, comprehensive gut health testing can give you a clear picture into what is going on “under the hood” and the health of your gut bacteria in general.
How to Buy the Best Probiotic
Now that you know why probiotics are GOOD for you, which probiotic should you choose?!
Here are 6 essentials you should know to buy the best probiotic for you…
Buy the Best Probiotic for You: 6 Essentials to Know
#1: Buyer Beware: 95% of Probiotic Supplements Don’t Contain the Probiotics They Claim
It’s been speculated, that upwards of 95% of probiotics sold on shelves do NOT contain the probiotics they claim.
Why? Temperature plays a role in the stability of probiotics. Poor processing and manufacturing practices, hot shipping conditions on 18-wheelers and improper storage of probiotics in supplement form can wreak havoc on the cultures inside the capsules.
This is especially true for lactobacillus and bifidobacteria probiotic strains, that are particularly sensitive to heat, processing and even digestion. For instance, an investigative review of probiotics in mainstream yogurts (claiming to be “good sources of probiotics”) found that none of the yogurts actually contained probiotics at all (2)—due to the manufacturing process, followed by cooling process. And even if probiotics are found in the supplement or foods, many probiotic supplements do not survive the heat and acids produced during digestion (especially in the absence of prebiotic fiber—essential fiber to help probiotics “stick” in your gut and make it to your large intestine, where the majority of gut bacteria reside).
For MOST supplements (particularly lactobacilli and bifidobacteria), high heat can degrade the liveliness of these organisms. Even under ideal storage conditions, the number of probiotics will slowly decline as months go on. For example, a typical number is a drop of 5% per month when stored in a refrigerator after opening. The exception? Soil based organisms—shelf stable supplements containing bacteria that mimic the same bacteria found in nutrient-rich soil and foods that humans consumed and thrived upon for years (before the Agricultural and Industrial Revolutions of food processing).
The Bottom Line: Although a probiotic label may claim that there are certain amounts or types of bacteria in the supplement, many probiotics are rarely if ever tested after production by manufacturers—meaning what started out as 100 billion strains of lactobacillus bacteria, may only end up as 5 billion strains by the time it hits shelves—and many do not survive high heat.
Q. So Which Probiotic Supplements are Quality?!
To benefit from the best probiotics and promote longevity of your probiotics opt for supplements containing:
Soil-Based Organisms with strains within the 6-10 billion range (as most of these are well-tolerated by most people). Look for names and strains such as:
Bacillus clausi
Bacillus subtilis
Bacillus coagulans
Baciullus Bifidus
Bacillus IndicusBacillus licheniformis
Saccharomyces boulardii
E. coli Nissle 1917
Quality refrigerated lactobacilli and Bifidobacterium strains of probiotics (see list below)
#2. You Get What You Pay For
Are probiotics a waste of money?! Nope. But, as mentioned in point #1, investing in quality probiotics is essential. No, you don’t have to pay $100 for “quality,” but in today’s market good probiotic will typically run anywhere between $30-$80. Chances are that $10 generic probiotic from Whole Foods, or fat free yogurt labeled “good source of probiotics” is basically all hype.
See the rest of this article to shop smart for your probiotics, but a good general rule of thumb to:
Spend the majority of your probiotic supplement money on Soil Based Organisms in supplement form (the most stable probiotics on shelves)
Purchase select amounts of lactobacilli and bifidobacteria from reputable manufactures with high-quality standards (see list below)
Incorporate real food probiotics and prebiotics in the form of fermented foods (sauerkraut, pickled veggies, full fat grass fed yogurt and kefir, limited low-sugar kombucha, and prebiotic fibers) into your daily diet
#3. There are 4 Main Types of Probiotic Bacteria & You Need Them All
Just like there are different types of phones you can buy different types of makeup you can buy (blush, powder, eyeshadow), there are different types of probiotic bacteria that all operate as gut bacteria (just like makeup helps makeup your face), but these bacteria have some distinct characteristics, purposes and differences. The 4 main types of probiotics include:
Soil Based Organisms
Lactobacilli (Lactobacillus acidophilus and Lactobacillus GG)
Bifidobacteria
Some healthy yeasts (like Saccharomyces boulardii)
Each type serves a unique purpose and we need a mix of all of them for a healthy gut microbiome—both in foods and supplements.
#4. Mix it Up: Not All Probiotic Strains Are Equal
Within the 4 main classes of probiotics (lactobacilli, bifidobacteria, soil-based organisms and yeasts), there are also hundreds of different strains of probiotics (just like there are hundreds of different brands of makeup—Clinique blush, MAC blush, Bobbi Brown blush, etc.). In fact, the human body contains 500 different strains of probiotic bacteria (such as Lactobacillus acidophilus, Lactobacillus Rhamnosus, Lactobacillus Plantarum, Bifidobacterium Infantis, Bifidobacterium Bidifum, etc.).
Each type of probiotic strain has particular effectiveness and potency, especially depending on your personal gut profile overall.
For example, a specific kind of Lactobacillus, like Lactobacillus acidophilus, may help you prevent an illness, but that doesn’t necessarily mean that another kind of Lactobacillus, like Lactobacillus plantarum, would have the same effect, or that any of the Bifidobacterium probiotics would do the same thing. Another person may have an overgrowth of Lactobacillus acidophilus, and experiencing symptoms of SIBO (bloating, gas, constipation), whereas another person may have no Lactobacillus acidophilus at all, and suffering from autoimmunity and fatigue.
In short: not all probiotics are created equal and incorporating a variety of types AND strains of probiotics is essential.
#5. You Need Pre-biotics & Postbiotics to Make Your Probiotics Stick
Common Myth: For a long time, we’ve thought that taking probiotics is like putting gas into your car tank—you fill it up and there’s more gas. But it doesn’t work that way. Instead, probiotics only serve as “maintainers” or gatekeepers of the “good” gut bacteria that you have ALREADY in your body—but they don’t produce more. And once you take them, they can be GONE in a matter of hours, UNLESS your have pre-biotics and post-biotics support!
Pre-biotics are starches and fibers (found in supplements and some foods like green-tipped bananas, plantains, cooked and cooled sweet potatoes and squashes, onions, and leeks)—that serve as food for your probiotics. In fact, pre-biotics are arguably MORE important and necessary than probiotics because they HELP your probiotics STICK AROUND and increase probiotic counts in your gut. (i.e. Pre-biotics feed your probiotics).
In addition, post-biotics (also known as “short chain fatty acids”) are the extra 1-2 punch to help you get the biggest bang for your probiotic buck! Short chain fatty acids, like butyrate, are the “gifts that keep on giving” to your gut, long after your probiotic and prebiotic foods and supplements have been digested. Healthy gut bacteria produce “short chain fatty acids” that help maintain overall gut balance in your gut as a whole (not too many of any one strain of bacteria). Unfortunately, since many folks have unhealthy or imbalanced gut bacteria to begin with (approximately 3 in 4 people have “gut issues”), short chain fatty acids also are reduced. The result? Without short-chain fatty acids, you may continue to experience imbalances in your gut bacteria.
The Bottom Line: Pre-biotics and post-biotics (short-chain fatty acids) help multiply your probiotics so you CAN increase YOU beneficial bacteria over time. (See recommendations below).
#6. If You Feel Sick, You May Have Other Gut Problems…
Probiotics make you break out or feel nauseas? If these symptoms continue longer than 7-14 days after starting a new probiotic, it may indicate you have other gut issues going on (such as bacterial overgrowth, parasites, leaky gut, etc.), OR you ALREADY have enough of the strains of probiotics you are taking.
“Healing reactions” are normal for many folks when first starting a probiotic (such as skin breakouts, loose stools, rashes, etc.) and can be a sign that your gut bacteria are getting “stirred up” (especially if you’ve had imbalances for some time).
However, if these reactions linger longer than a week or two, it’s vital to consider what else is going on under the hood.
The Bottom Line: If your probiotics are making you sick, consider getting a gut test completed or working with a practitioner to help you problem solve root issues going on.
Best Probiotic Recommendations
1. Soil Based Organisms
Megaspore Probiotic
Seed Daily Synbiotic
Primal Probiotic
Garden of Life Primal Defense Ultra (not good for SIBO or bloating)
2. Lactic Acid Bacteria
Klaire Labs Therabiotic (best general overall probiotic)
Ideal Bowel Support (best for constipation)
VSL #3 (best for loose stools)
Elixa Probiotic
3. Prebiotics
Glucomannan
Partially Hydrolyzed Guar Gum
4. Short Chain Fatty Acids
Enterovite by Apex Energetics**
Sodium-Potassium Butyrate by Body Bio
5. Fermented Foods
Fermented Veggies (carrots, beets, cucumber relish, dill pickles, etc.)
Pickled Veggies (no added sugar or additives)
Fermented Salsa
Fermented Horseradish
Goat’s Milk Yogurt & Kefir
Coconut Kefir
Water Kefir
Coconut Yogurt (no additives)
Low-Sugar Kombucha (5-6 grams per serving)
Beet Kvass
Kimchi
6. Prebiotic Foods
Asparagus (al-dente)
Coconut Flour
Cooked & cooled potatoes/sweet potatoes and squashes
Cooked and cooled Jasmine white rice & lentils
Garlic
Green tipped plantains/bananas
Jerusalem Artichoke
Onions
Mushrooms (reishi, shiitake and maitake)
Nutritional Yeast
Potato Starch or Plantain Starch
Seaweed/Algae (Beta-glucan, or 𝛽-glucan—a soluble fiber)
**Contact us to place an order for practitioner grade supplements, not found on the web.
Probiotic Protocol
For basic daily gut maintenance, a healthy daily protocol includes:
Pre-breakfast:
1 Soil Based Organism Probiotic
Breakfast
Short Chain Fatty Acids
Lunch
Short Chain Fatty Acids
Dinner
Prebiotic Supplement
Post-Dinner
1 Soil Based Organism Probiotic
Bonus: Eat 1-2 fermented foods and 1-2 prebiotic foods daily
*Health Disclaimer: By reading and/or using this information you acknowledge you are responsible for your own health and decisions. Consult your healthcare practitioner for your specific health needs.
Resources:
Markowiak, Paulina; Śliżewska, Katarzyna.(2017). Effects of Probiotics, Prebiotics, and Synbiotics on Human Health. Nutrients, 9(9), 1021. doi:10.3390/nu9091021;
Scourboutakos, M., Franco-Arellano, B., Murphy, S., Norsen, S., Comelli, E., & L’Abbé, M. (2017). Mismatch between Probiotic Benefits in Trials versus Food Products. Nutrients, 9(4), 400. MDPI AG. Retrieved from
The post The Best Probiotic to Buy: 8 Essentials appeared first on Meet Dr. Lauryn.
Source/Repost=>
https://drlauryn.com/gut-health/best-probiotic-to-buy-8-essentials/ ** Dr. Lauryn Lax __Nutrition. Therapy. Functional Medicine ** https://drlauryn.com/
The Best Probiotic to Buy: 8 Essentials via http://drlaurynlax.tumblr.com/
0 notes