#The Direct Anterior Approach to Hip Reconstruction
Explore tagged Tumblr posts
Text
Direct Anterior Approach for Total Hip Arthroplasty

Here get detailed info on: Direct Anterior Approach for Total Hip Arthroplasty. Know about, The Direct Anterior Approach to Hip Reconstruction. Direct Anterior Approach Hip Precautions… from Dr. Aashish Arbat… Top Orthopedic Doctor in Pune. Top hip replacement doctor in Pune. hip replacement surgeon in Pune
#Direct Anterior Approach Hip Surgical Technique#The Direct Anterior Approach to Hip Reconstruction#Direct Anterior Approach Hip Orthobullets#Direct Anterior Approach Hip Replacement#Direct Anterior Approach Hip Precautions#Anterior Approach To Hip AO#Why I No Longer Do Anterior Hip Replacement
0 notes
Text
Why Your Choice of Surgeon Matters in Orthopaedic Surgery
When it comes to orthopaedic procedures—especially joint replacements and complex reconstructions—the skill and experience of your surgeon play a crucial role in the outcome. While advanced technology and hospital infrastructure are important, the surgeon's expertise is the single most significant factor affecting your recovery, mobility, and long-term joint health.
1. Experience Directly Impacts Success Rates
Surgeons who perform high volumes of orthopaedic surgeries consistently tend to have better outcomes and fewer complications. Dr. Saurabh Giri, for instance, has performed over 6000 orthopaedic procedures, giving him vast hands-on experience in both routine and complex cases.
2. Training and Specialization Make a Difference
Not all orthopaedic surgeons are trained alike. Dr. Giri’s international fellowships in hip and knee arthroplasty from prestigious centers in Italy and Germany have equipped him with advanced skills in:
Direct anterior approach for hip replacements
Revision joint replacements
Robotic-assisted surgeries for enhanced precision
Such global exposure ensures that patients receive care that’s in line with the best international standards.
3. Precision Is Critical in Joint Replacement
The placement of an implant needs to be exact—a few millimeters off can lead to pain, instability, or early failure. A well-trained surgeon uses meticulous planning and precise execution, often incorporating robotics, navigation systems, or patient-specific implants to achieve ideal alignment.
4. Better Surgeons Mean Faster Recovery
An experienced orthopaedic surgeon doesn’t just operate efficiently—they also know how to minimize trauma to soft tissues, reduce blood loss, and optimize post-op care. This means shorter hospital stays, faster rehabilitation, and better functional outcomes.
5. Compassion and Communication Matter Too
Surgical skill is vital, but so is the ability to communicate with and support patients through their recovery. Dr. Saurabh Giri is known not only for his technical excellence but also for his empathetic and patient-first approach—something that can make your recovery journey smoother and less stressful.
Conclusion
Choosing the right orthopaedic surgeon isn’t just about credentials—it’s about experience, global training, precision, and personal care. Whether you're facing a joint replacement, a revision surgery, or a complex arthroscopy, the right surgeon can make all the difference between a routine recovery and a life transformed.
0 notes
Text
Restoring Mobility Through Modern Joint Surgeries
Joint health plays a crucial role in maintaining an active and independent lifestyle. As advancements in orthopedic surgery continue, individuals suffering from joint degeneration or injury now have access to highly effective treatment options.
Hip replacement
One of the most transformative surgeries in orthopedic medicine is hip replacement. This procedure is commonly recommended for patients suffering from severe osteoarthritis, rheumatoid arthritis, or traumatic injury that has significantly damaged the hip joint. The goal of the surgery is to remove the damaged components of the hip and replace them with artificial parts made of metal, ceramic, or high-grade plastic.
Typically, a candidate for this surgery has experienced chronic pain, reduced range of motion, and difficulty in daily activities such as walking, climbing stairs, or even sitting. The procedure involves the removal of the femoral head and the acetabulum, which are then replaced with prosthetic components that mimic the natural anatomy of the hip joint.
A successful hip replacement can significantly enhance a patient’s mobility and reduce or eliminate pain. The recovery process usually begins the day after surgery, with physical therapy playing a vital role in regaining strength and function. Patients are encouraged to walk short distances with the assistance of a walker or crutches and gradually increase their activity levels.
One of the main advantages of modern hip implants is their longevity. Many implants now last 15 to 20 years or more, making the surgery a long-term solution for those suffering from debilitating hip conditions. Advances in surgical techniques, including minimally invasive approaches, have also reduced recovery time and improved outcomes.
Knee replacement
Following the discussion on hip surgery, another life-changing orthopedic intervention is knee replacement. This surgery is often necessary for individuals suffering from advanced arthritis or significant joint trauma that impairs movement and causes ongoing discomfort. The knee is a complex joint that bears a substantial portion of body weight, making it vulnerable to wear and tear over time.
During a typical knee replacement procedure, the surgeon removes the damaged cartilage and bone from the surface of the knee joint and replaces it with artificial components. These prosthetics are engineered to replicate the natural movement and structure of the knee, allowing for smoother mobility and a reduction in pain.
Candidates for this surgery often report severe pain that limits daily activities, stiffness, swelling, and deformity of the joint. The decision to undergo surgery usually comes after conservative treatments such as medications, physical therapy, and lifestyle modifications have failed to provide relief.
Postoperative rehabilitation is a cornerstone of successful recovery. Physical therapy typically begins within 24 hours of surgery and focuses on strengthening the muscles around the knee, improving flexibility, and retraining the joint for daily movements. Most patients can resume normal activities within six weeks, although full recovery might take several months.
Anterior cruciate ligament
Among the most common sports-related injuries, a torn anterior cruciate ligament (ACL) can significantly disrupt an active lifestyle. The ACL is a key ligament that provides stability to the knee joint, especially during dynamic movements like jumping, pivoting, and sudden changes in direction. Injuries to this ligament are particularly prevalent among athletes involved in sports such as soccer, basketball, and skiing.
When the ACL is torn, individuals often experience a popping sensation, followed by swelling, instability, and an inability to bear weight. While some may manage with rehabilitation alone, many—especially younger, more active patients—require surgical reconstruction to restore knee function.
Anterior cruciate ligament reconstruction involves replacing the torn ligament with a graft, which is usually harvested from the patient's own hamstring or patellar tendon. The graft is secured in place using screws or other fixation devices and gradually integrates with the surrounding tissue to form a new ligament.
0 notes
Text
Hip Reconstruction Market Analysis and Forecast (2024-2032)
The global hip reconstruction market has experienced steady growth, driven by advancements in medical technology, increasing prevalence of hip-related disorders, and an aging population. As healthcare infrastructure strengthens and innovative surgical techniques develop, demand for hip reconstruction surgeries is expected to rise further, creating significant opportunities within this market. This article explores the current market landscape, emerging trends, and future projections, aiming to provide a comprehensive overview for stakeholders, investors, and healthcare professionals.
1. Market Overview
Hip reconstruction is a vital orthopedic surgical procedure aimed at restoring mobility, alleviating pain, and enhancing the quality of life for patients with severe hip conditions. Common procedures in this category include hip replacements (total, partial, or revision), as well as minimally invasive techniques and hip resurfacing. The market is primarily driven by the demand for improved patient outcomes, which has been facilitated by innovation in implant technology and surgical techniques.
Key Market Segments:
Procedure Type: Total Hip Arthroplasty (THA), Partial Hip Arthroplasty (PHA), Revision Hip Arthroplasty, Hip Resurfacing
Material Type: Metal-on-Metal, Metal-on-Polyethylene, Ceramic-on-Ceramic, Ceramic-on-Polyethylene
End-User: Hospitals, Specialty Orthopedic Clinics, Ambulatory Surgical Centers
2. Market Drivers
Several factors drive the global hip reconstruction market, including:
Rising Aging Population: As life expectancy increases globally, the elderly population prone to degenerative bone diseases is expanding, creating a surge in demand for hip reconstruction.
Increasing Incidence of Hip Disorders: Conditions such as osteoarthritis, osteoporosis, and rheumatoid arthritis are becoming more prevalent, resulting in higher rates of hip-related disorders and subsequent surgeries.
Technological Advancements: Innovations like robotic-assisted surgery, minimally invasive procedures, and custom-fit implants are improving surgical outcomes, reducing recovery time, and contributing to market growth.
Growing Awareness and Access to Healthcare: With increasing healthcare awareness and enhanced infrastructure in emerging economies, more patients are opting for reconstructive surgeries to improve mobility and life quality.
3. Market Challenges
Despite promising growth potential, the hip reconstruction market faces certain challenges:
High Procedure Costs: Hip reconstruction surgeries, particularly those involving advanced technology and materials, can be expensive. The cost barrier remains significant, particularly in low- and middle-income countries.
Post-Surgical Complications: While surgery success rates are high, complications such as infections, implant loosening, and joint stiffness can affect patient outcomes, impacting market perception and growth.
Stringent Regulatory Approvals: Hip implants and related devices require rigorous testing and regulatory approval. This process can be lengthy and costly, delaying the launch of new products.
4. Emerging Trends
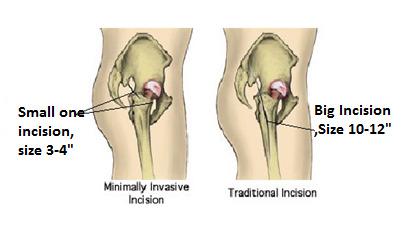
Minimally Invasive Surgery: Patients and surgeons are increasingly opting for minimally invasive procedures, which reduce incision size, decrease recovery time, and lower risk of complications. Techniques like direct anterior approach for hip replacement are gaining traction for their efficiency.
Robotic-Assisted Surgery: The adoption of robotic technology in hip reconstruction allows for high precision and customization. This technology, which includes systems like MAKO by Stryker, is popular in developed countries and is gradually penetrating emerging markets.
Biologic and 3D-Printed Implants: The use of biologic materials and custom-made implants through 3D printing technology is a trend that’s reshaping the market. Biologic materials improve integration with human tissue, reducing rejection rates, while 3D printing allows for personalized implants that fit patient anatomy perfectly.
5. Regional Analysis
The hip reconstruction market shows varying trends across regions:
North America: This region dominates the market due to its advanced healthcare infrastructure, high healthcare spending, and a well-established orthopedic industry. The presence of key players and a large elderly population make North America a prominent market.
Europe: Europe holds a substantial share of the market, driven by high incidence rates of hip-related disorders and robust healthcare facilities. Countries like Germany, France, and the UK have a high adoption rate for innovative hip reconstruction technologies.
Asia-Pacific: The APAC region is expected to see the fastest growth, thanks to increasing healthcare access, an aging population, and rising awareness. China and India are key contributors, with their large populations and government initiatives to improve healthcare access.
Latin America and Middle East & Africa (MEA): While these regions represent a smaller market share, they show significant potential for growth due to developing healthcare infrastructure and growing interest from global players to expand into these regions.
6. Competitive Landscape
The hip reconstruction market is highly competitive, with several key players investing in research and development to introduce innovative products. Major companies include:
Zimmer Biomet: Known for its comprehensive portfolio, including advanced materials and implant designs.
Stryker Corporation: A leader in robotic-assisted hip replacement surgeries, Stryker’s MAKO system is one of the most widely adopted globally.
Smith & Nephew: This company has a strong presence in minimally invasive and customized implant solutions.
Johnson & Johnson (DePuy Synthes): One of the largest orthopedic companies, DePuy Synthes offers a range of hip reconstruction solutions focusing on patient-specific outcomes.
7. Future Market Projections
Analysts project that the hip reconstruction market will experience substantial growth through 2032, driven by an increasing global population and demand for quality orthopedic care. The market is expected to grow at a compound annual growth rate (CAGR) of approximately 5.5% from 2024 to 2032.
Key Growth Drivers:
Expansion of robotic-assisted surgery and 3D-printed implants
Greater investment in emerging markets by global orthopedic companies
Focus on minimally invasive and patient-centric procedures
Buy the Full Report for More Insights into The Hip Reconstruction Market Forecast
Download A Free Report Sample
0 notes
Text
Elevate Your Quality of Life with Dr. Saurabh Giri's Expertise in Joint Replacement Surgery
Are you or your loved one struggling with hip or knee joint issues, hindering your daily activities and quality of life? Look no further. Dr. Saurabh Giri, a distinguished orthopedic surgeon specializing in joint replacement surgery, is here to offer you personalized care and advanced treatment options.
Introducing Dr. Saurabh Giri
With over 14 years of experience in orthopedic surgery, Dr. Saurabh Giri is renowned for his compassionate care and exceptional results. He holds an MS in Orthopedic Surgery, where he achieved the prestigious title of University Topper and was honored with a Gold Medal for his outstanding academic performance.
Dr. Giri's expertise extends globally, having trained and worked at esteemed international hospitals such as Santo Spirito Hospital in Italy and Helios Endo Klinik in Germany. He has also served as Head of Department for Robotic Joint Replacement at Deccan Hardikar Hospital and Accord Hospital, and as a visiting consultant at ONP Prime Hospital and Sahyadri Hospitals.
Advanced Techniques and Specializations
Dr. Giri's treatment philosophy is grounded in personalized care, recognizing that every patient and their condition is unique. He believes in exploring non-surgical options whenever possible and tailoring treatment plans to individual needs.
His areas of expertise include:
Robotic Joint Replacement Surgery
Knee Resurfacing (UKR) / Partial Knee Replacement Surgery
Total Hip and Total Knee Replacement Surgeries
Revision Knee Replacement Surgeries
Minimal Invasive Muscle Sparing Technique (MIS) Knee Replacement Surgery
High Flexion Knee Replacement with Highflex Knee Implants
Computer Assisted Navigation Surgeries (CAN)
Patient-Specific Instrumentation Surgeries (PSI)
Knee Arthroscopy
Regenerative Cell Therapy for Knee Arthritis
Anterior and Posterior Cruciate Ligament Reconstruction
Meniscus Repair
Arthroscopic Microfracture and Cartilage Repair Techniques
Multimodal Pain Management and Same-Day Mobilization in Knee and Hip Replacement Surgery
Daycare Knee Replacement Surgery
The Direct Anterior Approach (DAA)
Dr. Giri specializes in the Direct Anterior Approach (DAA) for total hip replacement surgery, a modern, minimally invasive technique that offers numerous advantages, including quicker recovery, fewer postoperative precautions, and a reduced risk of implant dislocation. His extensive training and experience in this advanced approach ensure optimal outcomes for his patients.
Personalized Care for Every Patient
Dr. Saurabh Giri's commitment to patient-centered care, coupled with his unparalleled expertise in joint replacement surgery, makes him a trusted choice for individuals seeking relief from hip and knee joint issues. With Dr. Giri, you can rest assured that you're in capable hands, receiving the highest standard of care tailored to your unique needs.
Don't let joint pain hold you back from living your best life. Schedule a consultation with Dr. Saurabh Giri today and take the first step towards reclaiming your mobility and independence.
Helios
(+91) 8971926236
0 notes
Text
Things To Be Aware Of The Orthopedics Department And Related Surgeries
In the present era, medical science has developed numerous treatment options that can bring ease to a person's life. A wide range of surgical methods has been designed that can put someone out of an uncomfortable situation. Like, if we talk about the sector of orthopedics, it focuses on treating issues of the musculoskeletal system. This system involves the presence of those essential components which are compulsory for healthy living and allows us to perform daily-life tasks. They are muscles, bones, ligaments, tendons, and soft tissues. Sometimes a problem can occur in the musculoskeletal system that may not settle with non-surgical approaches. At that time, an orthopedist takes help from orthopedic surgery treatment.
In the below section, we will try to bring your attention towards some of the widely known surgeries from the orthopedics department.
1. Pediatric Orthopedics
This department is dedicated to diagnose and treat various forms of musculoskeletal issues in children. There can be a presence of some problems in a child that needs to be treated on time. Otherwise, it may lead to futuristic worries. At that time, taking help from a pediatric orthopedic surgeon will be the best option to consider. They are highly professional and experienced candidates to handle the diseases and injuries of children better than others.
2. Joint Replacement Surgery
It is regarded as one of the vital kinds of orthopedic surgery in various parts of the world. It comes into use when non-surgical methods aren't useful in treating joint problems. Here, the damaged sections of the joint are replaced by artificial components. Some of the most common kinds of joint replacement surgeries include hip replacement, knee replacement, and shoulder replacement. With their assistance, a person finds relief from pain and restricted motion.
3. ACL Reconstruction Surgery
There is a ligament present in the center of the knee called the anterior cruciate ligament. It is one of the major ligaments that connect the tibia (shinbone) to the femur (thighbone). This ligament can tear due to physical activities that involve changes in directions, landing from a jump, or slowing down at the time of running. During this kind of surgery, the surgeon eliminates the torn ligament and replaces it with a tendon. He can take that graft tendon from another part of the body or it can be obtained through a deceased donor.
4. Spine Surgeries
One of the important body parts whose well-being is essential for us is the spine. It helps us to perform a wide range of activities and yes, it can suffer from some serious issues. Some cases of the spine can be critical and may demand a surgical procedure. A lot of orthopedic surgery treatment options are available to treat various issues of the spine. For example, vertebroplasty, kyphoplasty, laminectomy, laminoplasty, discectomy, spinal fusion, artificial disc replacement, etc.
5. Fracture Repair Surgery
A break or crack in the bone is a common occurrence and is usually treated with the help of casting, splinting, or bracing. But when a broken bone doesn't heal correctly with such measures, the surgeon will take help from a fracture repair surgery. During this kind of orthopedic surgery, the fractured bone will be set into its actual place. There can be a usage of screws, rods, plates, or pins for securing the bone in place.
6. Arthroscopy
To diagnose and treat joint problems, the surgeon can take help from this minimally invasive procedure. The procedure is done by making a small incision in the joint side. Thereafter, he inserts a thin telescope with an attachment of a fiber-optic camera. That camera displays the internal view to the surgeon and thus, he can identify the kind of problem. This minor surgery can also treat some issues with the help of smaller instruments. Some of its other advantages include lower infection rate, less post-operative pain, faster healing period, and minimum soft tissue trauma.
1 note
·
View note
Text
Experience Revolutionary Joint Replacement Surgery with Dr. Bakul Arora at Arora Clinic
Dr. Bakul Arora is a highly skilled Consultant Joint Replacement & Orthopaedic Surgeon with expertise on minimally invasive methods. The clinic he is working in currently Arora Clinic, a state-of-the-art orthopaedic clinic located at Hiranandani Meadows, Thane, within close proximity of Mumbai.
Dr. Bakul Arora is renowned for his experience in performing joint replacement surgeries using minimally invasive methods. He uses the subvastus approach for knee replacement surgery as well as the direct anterior approach for the hip joint replacement procedure. These techniques have numerous advantages for patients. These include smaller cuts, less pain quicker recovery time, as well as fewer issues.
Services
In the Arora Clinic at Arora Clinic, Arora Clinic, Dr. Bakul Arora offers a extensive array of orthopaedic services and surgeries that help patients recover from joint pain and increase their mobility. A closer look at the services provided at the Arora Clinic:
Knee Arthroscopy Surgery: A knee arthroscopy surgery is an minimally-invasive surgical procedure that is used to diagnose and treat knee issues including torn cartilage ACL injuries, or the damaged or loosened tissues surrounding the knee joint. Dr. Arora is an experienced surgeon who uses the latest techniques to perform knee arthroscopy procedure with little discomfort and a faster recovery time.

Knee Reconstruction Surgery: Knee replacement surgery is a standard procedure that is used to treat patients who suffer from severely painful knees and impairment. Dr. Arora uses minimally invasive techniques for knee replacement surgery. It requires replacing the damaged knee joint with a synthetic joint composed of metal and plastic parts.

Golden Knee Replacement Surgery: Golden Knee Replacement is a revolutionary and unique knee replacement procedure that utilizes modern techniques and technology in order to offer patients a more natural feeling knee joint. The surgery is carried out with the use of custom-made implants which are designed to fit each patient's specific anatomy.

Hip replacement surgery: Surgery for hip replacement is a surgery that will replace an injury or degenerative hip joint using an artificial joint made of metal and plastic components. Dr. Arora uses the direct anterior approach to do hip replacement surgery. It is a minimally invasive process that offers many benefits to patients.
Partial Knee Replacement Surgery: Partial knee replacement surgery is a procedure to treat patients with knee arthritis only in the two or one part of the knee joint. Dr. Arora performs partial knee replacement surgery by using minimally invasive techniques that result in reduced pain, faster healing and quicker return to normal activities.

Trauma Surgery: Trauma surgery is one of the surgical fields that deal dealing with injuries caused by accidents or physical force. Dr. Arora is experienced in the treatment of various traumatic injuries, including fractures, dislocations, and soft-tissue injuries.

Shoulder Replacement Surgery Surgery for shoulder replacement is a surgical procedure that can replace an injured or damaged shoulder joint with a new joint composed of both metal and plastic components. Dr. Arora uses the latest techniques to perform shoulder replacement surgery, which is performed with less discomfort and faster recovery time.

Robotic knee replacement surgery A knee replacement surgery a new and revolutionary surgical procedure that utilizes a robotic arm that assists the surgeon during the procedure. Dr. Arora is experienced in performing robotic knee replacement surgery and offers many benefits to patients, including greater accuracy, less pain, and a faster recovery time.
About Doctor
Dr. Bakul Arora is a highly competent Consultant Joint Replacement & Orthopaedic Surgeon who has extensive experience in treating patients with joint issues. The surgeon specializes in minimally-invasive procedures that bring multiple benefits for patients. These include smaller incisions, less pain faster recovery times, as well as fewer issues.
Dr. Bakul Arora is dedicated to providing his patients with the finest level of personal care. He is able to take note of his patients' needs to thoroughly analyze their situation and then create a customized treatment plan that meets their particular preferences.
Dr. Bakul Arora is renowned as an expert in the area of joint replacement procedures using minimally invasive methods. Dr. Bakul Arora uses subvastus approaches for knee replacement surgery, and the direct an anterior approach to hip replacement surgeries. The techniques offer numerous benefits for patients, including a speedier recovery time as well as less discomfort and less risk of complications.
Doctor. Bakul Arora's orthopaedic treatments extend beyond joint replacement surgery. He also provides treatments for common knee conditions such as ligament injuries, anterior knee pain, meniscal tear, patella instability, swollen knee, and tendonitis. His expertise is extensive in using minimally-invasive procedures that give patients multiple benefits.

About Clinic
Arora Clinic The Arora Clinic an orthopaedic facility that is state of the art which is situated within Hiranandani Meadows, Thane, near Mumbai. It is committed to providing patients with top-quality healthcare. It has been equipped with the latest and modern technology.
The clinic is run by Dr. Bakul Arora, a highly skilled Consultant Joint Replacement & Orthopedic surgeon with years of expertise in the treatment of patients suffering from joint problems. Dr. Bakul Arora specializes in minimally invasive methods that can provide many benefits to patients with fewer incisions, lower pain levels, shorter healing times and less complications.
Arora Clinic is well-known for its innovative procedures, including minimally-invasive knee replacement surgery. It is also called "PAIN-LESS SURGERY" for knee disease. Dr. Bakul Arora uses the latest techniques and technologies to ensure patients receive the best possible outcomes.
The facility offers a wide selection of orthopedic treatment and procedures, such as knee arthroscopy surgeries, knee replacement surgery golden knee replacement surgery and hip replacement surgery. partial knee replacement surgeries, shoulder replacement surgery and robotic knee replacement surgery. Dr. Bakul Arora and his team have a commitment to provide patients with the highest level of personalized care and pay attention to their concerns and create a custom treatment program that is tailored to the patient's unique requirements.
1 note
·
View note
Text
Christopher J. Nanson, MD, MPH, FAAOS, is a Leading Orthopedic Surgeon with Orthopedics Northwest in Tigard, OR
Christopher J. Nanson, MD, MPH, FAAOS, is a well-versed orthopedic surgeon who diagnoses and treats patients at Orthopedics Northwest in Tigard, Oregon. Furthermore, Dr. Nanson has staff memberships at several local hospitals, including Legacy Meridian Park Hospital, Providence Portland Medical Center, Providence Willamette Falls Medical Center, South Portland Surgical Center, and Oregon Outpatient Surgery Center. And, he is a team physician for the University of Portland Men & Women Athletic Teams and the U.S. Men & Women Soccer Teams. As an orthopedic surgeon, he specializes in the prevention, diagnosis, and treatment of disorders of the bones, joints, ligaments, tendons, and muscles. Dr. Nanson’s professional journey spans 11 years. He is an expert in direct anterior approach for hip replacement surgery and is trained and certified in robotic-assisted MAKO partial knee resurfacing and total knee and hip replacements. Dr. Nanson has a special interest in reconstructive joint surgery with emphasis on hip and knee reconstruction. For more information about Dr. Christopher J. Nanson, please visit https://www.christophernansonmd.com/christopher-nanson-orthopedics-northwest-tigard-oregon.html.
Christopher J. Nanson, MD, MPH, FAAOS, attended The Ohio State University College of Medicine in Columbus, OH, and received his medical degree in 2003. Then, he completed the surgical residency program at Phoenix Orthopedic Surgery in Phoenix, AZ (2003-2005), followed by the orthopedic surgery program at the University of Arizona in Tucson, AZ (2005-2008). Furthermore, he conducted his adult reconstructive surgery fellowship at OrthoCarolina Hip and Knee Center in Charlotte, NC (2008-2009). In addition, Dr. Nanson received board certification in orthopedic surgery from the American Board of Orthopedic Surgery. He is a member of the American Medical Association, the American Association of Hip and Knee Surgeons, the North Pacific Orthopedic Society, the Oregon Association of Orthopedic Surgeons, and the Western Orthopedic Society. Moreover, he attained fellowship of the American Academy of Orthopedic Surgeons. Prior to medical school, Dr. Nanson completed his undergraduate studies at the University of Arizona, where he received a Master of Public Health degree. For more information about Dr. Christopher J. Nanson, please visit https://www.findatopdoc.com/doctor/1689822-Christopher-Nanson-Orthopedist.
0 notes
Text
Iris Publishers-Open Access Journal of Rheumatology & Arthritis Research

Authored by Vianney Hope JM*
Introduction
Total hip arthroplasty (THA) has become one of the most successful interventions in reconstructive orthopedic surgery. However, dislocation remains the well-recognized challenging complication for the surgeon and the cause for pain and dissatisfaction for patients. According to the registers, dislocation occurs after 0.3% to 10% of primary total hip arthroplasties and after up to 28% of revision total hip arthroplasties [1- 4]. Component malpositioning and abductor insufficiency are two of the most important recognized causes of dislocation [5-7]. Dislocation after THA is easily recognized immediately after its occurrence and reduced immediately or few days later. Therefore, chronic dislocation is exceptionally unusual. Only less than ten cases of unilateral chronic dislocation following THA have been reported to date [1-8]. We report the first case of chronic THA dislocation with bilateral involvement caused by a malpositioned acetabular component in a 59-year-old patient. We aimed to present clinical and radiological features, treatment, and outcome of spontaneous chronic asymptomatic bilateral dislocation of 11-year duration after cemented total hip arthroplasty.
Case Report
A 59-year-old man presented to the surgical clinic eleven years after single stage bilateral cemented primary THA following bilateral hip osteoarthritis. He was operated at another institution (abroad) and had never returned for follow up due to financial constraints. He remained pain-free, had 2 cm of true right leg length shortening with a good range of movement. Since the operation, he was unable to walk without orthopedic aids. However, he was able to walk unlimited distances with a rolling walker. Due to the dissatisfaction caused by long-standing limping associated with a leg-length discrepancy after THA, he decided to consult to our clinic. The patient denied any fall injury or accident. On general physical examination, he was healthy appearing; walking with bilateral axillary crutches; alert and oriented; responds appropriately; in no acute distress. His general status was conserved. Blood pressure measurement revealed a pressure of 155/85 mmHg, his pulse rate was 78 beats/minute, his respiratory rate was 19 cycles/ minute and his body mass index (BMI) was 27.8. There was right lower limb length discrepancy of 2 cm compared to the left side. A posterolateral operative scar, indicative of Austin Moore approach, was seen bilaterally.
Musculoskeletal examination of the right hip showed that he could elevate the hell from the horizontal plane of the examination table; the muscle power of gluteal medius was at 3/5, adductor muscles at 4/5, hamstring muscles at 0/5 and quadriceps at 2/5. The hip flexion was at 110° and extension at -10°. On the left side, hell elevation from the horizontal plane of the bed was possible, muscle power of gluteus medius at 2/5, adductor muscles at 3 /5, hamstring muscles at 0/5 and quadriceps at 3/5. The hip flexion was at 110° and extension at 0°. Full range of motion (ROM) of both hips are presented in table 1. Postel Merle d’Aubigné (PMA) score was 10/18 and Harris Hip Score (HHS) 30/100 bilaterally. Neurovascular examination was unremarkable.
Conventional anteroposterior (AP) radiography of the pelvis showed bilateral postero-superior cemented total hip prostheses dislocation with excessive inclination of acetabular shell at 65° on the left hip and at 85° on the right side. The dislocated femoral components had formed a neoacetabulum within the ilium, in which they were freely articulating (Figure 1). Reconstructed axial and sagittal computed Tomography (CT) scans of both hips confirmed postero-superior total hip prostheses dislocation; muscle wastage with fat degeneration, aseptic loosening of both femoral and acetabular components with excessive inclination of acetabular components (Figure 2). The patient was put on bilateral trans-condylar skeletal traction using Boppe splint (Figure 3). Initial weight of 2 kilograms (Kg) was indicated with daily increase of 1 Kg and daily radiographic control to monitor the descent of the prosthetic heads. At day 5 post traction with traction-weight of 7 Kg, the heads were at the level of the tip of the acetabular shell. At day 9 post traction with traction-weight of 11 Kg, the heads were within the acetabular shell (Figure 4). The patient consented for a 2-month-interval bilateral total hip revision. Preoperative blood examination revealed WBC 8090/μl, Hb 11.4 g/dl, C-Reactive Protein 0.25 mg/dl, platelet 372000/μl, creatinine 10mg/l, uric acid 117mg/l and calcemia 87mg/l.
The right hip was first revised. In the left lateral decubitus position and under general anesthesia, the skin incision was made to the previous operative scar and hip was exposed through a standard posterolateral Austin Moore approach. Intraoperatively, a posterior and superior hip instability was identified as resulting from the combined movements of external rotation and adduction. We found that the prosthetic head has created a pseudoacetabulum and a neocapsule around it which was filled with citric fluids and rice body formations. The prosthetic head was found in the gluteus major muscle and both acetabular and femoral components were loosened with excessive inclination of acetabular component (Figure 5). We removed the implants along with the cement; and prepared for new implantation. Both acetabular and femoral components were revised using cemented modular shell and acetabular reconstruction with Kerboul reinforcement crossplate (acetabular lip). The femoral stem was cemented. The closure of the articular space and a good repair of the neocapsule and remaining short external rotators were performed. Intraoperatively satisfactory stability of the prosthesis movements in all directions was confirmed. The duration of the operation was 5 hours and the blood loss was 700 cc. The patient was transfused 2 units of whole blood. Postoperatively, the wound healed well by primary intention in 3 weeks. Two months later, the left hip was revised in the same way as the right one. Leg discrepancy was corrected. The second operation lasted 4 hours with blood loss of 600 cc. He was again transfused of two units of whole blood. The wound healed in 3 weeks.
He was thereafter scheduled for rehabilitation and monthly follow up. He made an uneventful recovery and returned to fulltime employment 8-month post left hip revision. At 7-year-follow up, he was satisfied and pain-free. The ROM of both hips were satisfactory (Table 1). The PMA score was 17/18 whereas the HHS was 99/100. Control AP pelvis radiography show well maintained total hip prostheses. Femoral and acetabular components are well positioned and fixed. No signs of loosening or impingement were detected (Figure 6).
Discussion
Dislocation following total hip arthroplasty (THA) is a complication which alarms both patient and surgeon. There have been numerous reports instancing the frequency of dislocation, with an overall incidence ranging from 0.3% to almost 10% after primary THA, with the highest risk believed to be within the first three months after surgery [1-5]. The incidence can be as high as 28% after revision surgery [9-15]. The definition of THA dislocation is complete loss of contact between the femoral head and acetabular component. This usually requires intervention to reduce the prosthetic head into the acetabular component. Dislocation may occur early or late and be single or recurrent. Early dislocation occurs in first 3 months postoperatively, and more than two dislocations are defined as recurrent [14]. The term chronicity refers to the time between the occurrence of dislocation and its reduction; thus, we have defined chronic dislocation as dislocation which is unreduced at least 3 weeks (21 days) after its occurrence. Very little has been written about chronic dislocation after THA, and less than ten cases of chronic dislocation following THA have been reported in the English literature. All these reported cases are unilateral [1-8]. We attribute the rarity of this lesion to the factor that hip dislocation is severely painful and patients with THA have a regular medical follow up. Thus, the dislocation is early diagnosed and immediately managed accordingly. At our center, the incidence of dislocation after THA is 0. 6%. For, this reported case of 11-year chronic asymptomatic bilateral dislocation, the primary THA was done in another institution and the patient failed to respect follow up program. Furthermore, the good range of movement and the absence of pain may explain the longstanding nature.
It may happen that an early postoperative total hip prosthesis dislocation is not diagnosed for few days in patients without weight-bearing, but this condition is extremely rare [16-17]. Often, THA dislocation is evident to both the patient and his neighborhood by the position of the dislocated limb and pain. The flexionadduction- external rotation and extension-abduction-internal motion positions are signs of posterior and anterior dislocation, respectively. Furthermore, in active patient’s total hip prosthesis dislocation may occur after a traumatic event (secondary or late dislocations). In our case, there is no possible link to traumatic events, and we think the dislocation is either spontaneous or positional.
Numerous factors influence the rate of dislocation after THA such as greater age, female gender, Musculo ligamentous laxity, previous surgery to the affected hip, revision surgery, infection, concomitant neurological deficiencies and other medical comorbidities, excessive alcohol intake, nonunion of the greater trochanter and cognitive impairment preventing adequate patient education. All cause soft-tissue imbalance and increase the risk of dislocation [9- 17]. Some authors have reported a higher rate of dislocation when using a posterior surgical approach and Kristiansen et al, noted less acetabular version with this approach [16-18]. Hedlundh U, et al. [19], registered twice the number of dislocations for inexperienced surgeons as compared with their more experienced colleagues, a correlation which was also reported by other authors [19]. Fackler CD and Poss R [20] observed a frequent association of dislocation with malposition of the component of which the surgeon was unaware at the time of surgery. This was seen more often among less experienced surgeons. The main reason for the higher rate of dislocation of inexperienced surgeons is malpositioning of the cup [20]. Soft-tissue imbalance and malposition are thought to be the two main causes of dislocation. Nonetheless, several authors have reported that excessive femoral anteversion may lead to dislocation [2]. Prosthetic design and selection can have an important effect on the incidence of dislocation. The most commonly considered implant factor is head diameter. In the author’s opinion, the perception that larger femoral heads would diminish the risk of dislocation [11]. In our case, there was excessive inclination of acetabular shell at 65° on the left hip and at 85° on the right side, and we have concluded that the cause of dislocation was malposition of acetabular components. There was soft tissue imbalance as a posterior dislocation injured the capsulo-muscular elements. Fortunately, the sciatic nerve was preserved. Intraoperatively, there were neocapsule around the prosthetic head which was filled with citric fluids and rice body formations which are the signs of chronicity. The prosthetic heads were found in the gluteus major muscle and both acetabular and femoral components were loosened.
Prevention of dislocation is much easier than treatment. This includes careful pre-operative templating and surgical planning. Proper patient positioning, care of the soft tissues, precise component position, intra-operative assessment of stability, and leg length are compulsory. Treatment of dislocation after THA begins with an assessment of the cause. Component position should be carefully evaluated, and hip offset and leg length should be assessed [2-4,7,11]. Surgical options include exchange of modular components to increase soft-tissue tension, or a switch to a larger head diameter, including bipolar or tripolar arthroplasty, and use of an acetabular lip. Malposition and impingement must be corrected. Soft-tissue or trochanteric advancement, and the use of constrained liners should be a last resort [15, 21-25]. In case of chronic dislocation, Butler et al, have used an Ilizarov apparatus to perform closed reduction of a chronic dislocation following THA (Figure 7). In our case, we started with a skeletal traction with progressive increment of traction-weight to preserve the sciatic nerve injury by elongation and to prevent muscle injuries as muscles were already weakened by fat degeneration. After the prosthetic heads were in the acetabular shells, bilateral total hip revision was carried out with a 2-month-interval. As there were loosening of both femoral and acetabular components, both components were revised. Treatment outcomes were uneventful. At 7-year-follow up, he was pain-free with excellent functional satisfaction.
Conclusion
Chronic dislocation after total hip arthroplasty (THA) refers to unreduced dislocation at least 3 weeks (21 days) after its occurrence. It is believed that several factors contribute to chronic dislocation such as surgical approach, inadequate restoration of soft-tissue tension, prosthetic design, and orientation of the prosthetic components. We have reported an unusual case of a longstanding (11-year duration), but asymptomatic, dislocated bilateral total hip replacement in a 59-year-old man. Our case illustrates that a dislocated total hip replacement may occasionally not cause symptoms that cause significant discomfort or reduction in range of movement. The prosthetic femoral head can form a neoacetabulum allowing a full range of pain-free movement.
Read more: Full Text To know more about Iris Publishers Research: https://unam.academia.edu/irispublishers
#iris publishers#iris publishers llc#iris publishers reviews#Rheumatology Scientific Journals#Arthritis Open access journals
0 notes
Text
Atlas of Operative Procedures in Surgical Oncology PDF Free Download
Atlas of Operative Procedures in Surgical Oncology PDF Free Download
We provide you Medical Books PDF Format Free Download and today, in this article, we are going to share with you Atlas of Operative Procedures in Surgical Oncology PDF for free using direct download links mentioned at the end of this article. We have uploaded these PDF and EPUB files to our online file repository so that you can enjoy a safe and blazing-fast downloading experience.
But before that, we proceed to the free PDF download of Atlas of Operative Procedures in Surgical Oncology PDF, let’s take a look into few of the important details regarding this book.
Overview
This volume is the product of the author’s long experience with melanomas and sarcomas and to a lesser but significant degree with upper gastrointestinal cancers, colorectal and breast cancers. As such, it offers a “hands-on” practical guide to approaching complex soft-tissue tumors and for performing more extensive tumor resections based on over 40 years of surgical experience. It provides important details about the positioning of patients, incision types, and exposure which can be of paramount importance in the resection of certain tumors. The book contains important general surgical principles for approaching tumors in a variety of locations but also offers the detail necessary for the safe and oncologically sound resection of these malignancies. Moreover, this operative atlas contains specific information for procedures which are not as commonly encountered in surgical training, but can be invaluable in the management of patients with locally aggressive tumors, such as hemipelvectomy and its variants, sacral resections, and forequarter amputation.
Through the use of multiple detailed illustrations, Atlas of Operative Procedures in Surgical Oncology serves as a valuable resource to the general surgeon or surgical oncologist in the operative management of patients with cancer in the abdomen, retroperitoneum, pelvis or extremities.
Features of Atlas of Operative Procedures in Surgical Oncology PDF
Here are the important features of this book:
Distal pancreatectomy
Epigastric vessel
Sextremity soft-tissue
Sarcomahepatic resection
Malignant melanoma
Node dissection
Pancreaticoduodenectomy
Retroperitoneal sarcomas
Scapulectomy
Sentinel node biopsy
Constantine P. Karakousis, MD, PhD (Author)
Constantine P. Karakousis, MD, PhD State University of New York at Buffalo, Department of Surgery, Buffalo General Hospital, Buffalo, NY, USA
Table of Contents
Below is the complete table of contents offered inside Atlas of Operative Procedures in Surgical Oncology PDF:
Chapter 1. Surgical Technique in Cancer Surgery Chapter 2. Intraoperative Lymphatic Mapping/Sentinel Lymphadenectomy Chapter 3. Tumor in the Hand Chapter 4. Tumor in the Wrist Chapter 5. Tumor in the Ventral Aspect of the Forearm Chapter 6. Tumor in the Dorsal Aspect of the Forearm Chapter 7. Tumor in the Anterior Compartment of the Arm Chapter 8. Tumor in the Dorsal Aspect of the Arm Chapter 9. Tumor in the Medial Arm Chapter 10. Axillary Node Dissection Chapter 11. In Continuity Axillary and Supraclavicular Node Dissection Chapter 12. Neck Dissection. Chapter 13. Tumor at the Shoulder Point Chapter 14. Tumor in the Neck Chapter 15. Scapulectomy Chapter 16. Shoulder Disarticulation Chapter 17. Forequarter Amputation Chapter 18. Tumor in the Back Chapter 19. Chest Wall Tumors Chapter 20. Tumor in the Lower Chest Wall and Upper Abdomen Chapter 21. Involvement of the Abdominal Wall by Tumor Chapter 22. One-Layer Closure of the Abdominal Wall Chapter 23. Midline Abdominal Wall Gaps and Incisional Hernia Chapter 24. Regional Chemotherapy Infusion Via the Hepatic Artery Chapter 25. Peritoneolysis in the Reconstruction of a Roux-en-Y Loop Chapter 26. Hilar Hepatojejunostomy Chapter 27. Hepatic Resection Chapter 28. Pancreaticoduodenectomy Chapter 29. Distal Pancreatectomy Chapter 30. Colonic Interposition for Esophageal Replacement Chapter 31. Ileal Loop Bladder-Interposition Conduit Chapter 32. Resection of Mesenteric Tumors Chapter 33. Dissection in the Bowel Mesentery and Its Clinical Applications Chapter 34. Retroperitoneal Node Dissection Chapter 35. Retroperitoneal Sarcomas Chapter 36. Tumor in the Lesser Sac Chapter 37. Tumor in the Right Abdomen Chapter 38. Tumor in the Left Abdomen Chapter 39. The T or L Incision in Resection of Tumors of the Pelvis Chapter 40. Groin Dissection Chapter 41. Abdominoinguinal Incision in the Resection of Pelvic Chapter 42. Resection of Pelvic Tumors with Visceral Involvement Chapter 43. Internal Hemipelvectomy 7 Chapter 44. The Surgical Importance of the Inferior Epigastric Vessels Chapter 45. Sacral Resection Chapter 46. Tumor in the Buttock Area Chapter 47. Tumor in the Anterior Thigh Chapter 48. Tumor in the Medial Thigh Chapter 49. Tumor in the Posterior Thigh Chapter 50. Popliteal Node Dissection Chapter 51. Tumor in the Leg Chapter 52. Tumor in the Foot Chapter 53. Hip Disarticulation Chapter 54. Hemipelvectomy (Hindquarter Amputation) Chapter 55. Variants of Hemipelvectomy Chapter 56. Central Venous Access Chapter 57. Resection of Tumors of the Ischiorectal Fossa
Product Details
Below are the technical specifications of Atlas of Operative Procedures in Surgical Oncology PDF:
Book Name: Constantine P. Karakousis, MD, PhD
Edition: 1st Edition | | ISBN: 978-1493916337
Author Name: Constantine P. Karakousis, MD, PhD
Category: Medical
Format / Pages: PDF – 338 Pages
Atlas of Operative Procedures in Surgical Oncology PDF Free Download
Here you will be able to download Atlas of Operative Procedures in Surgical Oncology PDF by using our direct download links that have been mentioned at the end of this article. This is a genuine PDF e-book file. We hope that you find this book interesting.
Below is a screenshot of the cover image of Atlas of Operative Procedures in Surgical Oncology PDF:
FILE SIZE: 42.1 MB
Please use the link below to download Atlas of Operative Procedures in Surgical Oncology PDF
:
$(function () { $("#condaianllkhir").click(function () { var seconds = 5; $("#CountDown").show(); $("#condaianllkhir").hide(); $("#DrRO").html(seconds); setInterval(function () { seconds--; $("#DrRO").html(seconds); if (seconds == 0) { $("#CountDown").hide(); window.location = "https://tinyurl.com/y4eneubg"; } }, 1000); }); });
Please Wait
seconds.
source https://www.medical-2019.cf/2020/08/atlas-of-operative-procedures-in.html
0 notes
Text
EUROPE PLATELET-RICH PLASMA MARKET ANALYSIS
Autologous platelet-rich plasma (PRP) is a blood plasma concentrate enriched with platelet count above the baseline of whole blood prepared from patient’s own blood. It is used to accelerate the healing of injured tendons, ligaments, muscles and joints.
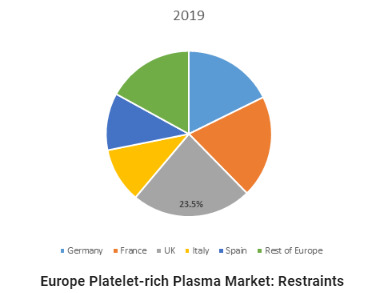
Europe platelet-rich plasma market is estimated to account for US$ 75.8 Mn in terms of value by the end of 2027.
Europe Platelet-rich Plasma Market: Drivers
Increasing prevalence of musculoskeletal injuries is expected to boost growth of Europe platelet-rich plasma market over the forecast period. For instance, according to the Study, ‘Prevalence of Musculoskeletal Injuries, Pain, and Illnesses in Elite Female Basketball Players, in Europe, in June 2019, the most frequently injured body parts were lower limbs: more than 60%, representing an injury rate of 0.14 per athletes and a 0.2 pain rate per athlete (during the study period).
Moreover, increasing geriatric population and high adoption of knee osteoarthritis treatment in by the age group is also expected to aid in growth of the market. Aging contributes to soft tissue degeneration and related-disorders, particularly of the knee. For instance, according to the study ‘Osteoarthritis in Europe: Impact on health status, work productivity and use of pharmacotherapies in five European countries’ that examined the impact of peripheral joint osteoarthritis across five European countries, UK (43.6%), France, (25.6%), Germany, (15.2%), Spain, (8.4%), and Italy (7.1%) recorded high prevalence of peripheral joint osteoarthritis, with majority of cases aging 55-74 years.
U.K. held dominant position Europe platelet-rich plasma market in 2019, accounting for 23.5% share in terms of valuee, followed by France.
Figure 1. Europe Platelet-rich Plasma Market Value (US$ Mn), by Country/Region, 2019
Europe Platelet-rich Plasma Market: Restraints
Lack of standardization in preparation and dosage of autologous blood concentrate and platelet-separation techniques is a major factor hindering growth of market. Lack of standardization in preparation and dosage of autologous blood concentrate and platelet-separation techniques lead in uncertainty about the evidence to support the increasing clinical use of platelet-rich plasma therapy as a treatment modality for musculoskeletal injuries, including orthopedic bone and soft-tissue injuries.
Moreover, uncertainty about therapeutic efficacy of platelet-rich plasma is also expected to hamper growth of the market. For instance, the study ‘Current Clinical Recommendations for Use of Platelet-Rich Plasma’ published in Current Reviews in Musculoskeletal Medicine in 2018, found moderate high-quality evidence that supported the use of leukocyte-rich (LR)-PRP injection for patellar tendinopathy and of PRP injection for plantar fasciitis and donor site pain in patellar tendon graft Bone-patellar tendon-bone anterior cruciate ligament reconstruction. Moreover, the review also noted insufficient evidence to routinely recommend PRP for rotator cuff tendinopathy, osteoarthritis of the hip, or high ankle sprains.
Europe Platelet-rich Plasma Market: Opportunities
Increasing adoption of PRP in skeletal muscle injuries is expected to offer lucrative growth opportunities for players in the market. PRP has promotes muscle recovery via anabolic growth factors released from activated platelets. This in turn reduces pain, swelling, and time for recovery in skeletal muscle injuries.
Moreover, technological advancements in PRP such as changes in production protocol (time and RPM/centrifugal force) and output level (volume and concentration above baseline) are also expected to aid in growth of the market.
Kits segment in Europe platelet-rich plasma market was valued at US$ 34.9 Mn in 2019 and is expected to reach US$ 60.4 by 2027 at a CAGR of 7.1% during the forecast period.
Market Trends/Key Takeaways
The demand for pure PRP fibrin therapy has increased significantly in the recent past, especially for the treatment of skin wound ulcers and in oral and maxillofacial surgeries. The platelet-rich fibrin therapy is classified as a second generation platelet concentrate, with rich platelet content and extensive growth factors in the form of fibrin membranes, which are free of any anti-coagulants or other artificial bio-chemical modifications and promote rapid and accelerated wound healing.
Increasing geriatric population in Europe has led to high demand for non-invasive or minimally invasive surgical treatments. PRP therapy is a simple, efficient, and minimally invasive procedure that represents an appropriate biological approach for ensuring tissue regeneration in a very short period of time. Such scenario has led to high adoption of PRP therapy for the treatment of orthopedic related injuries in geriatric patients.
Regulations
Europe
Directive 2002/98/EC of the European Parliament and Council of January 27, 2003, regulates the approval process for blood and blood-derived products
Harmonized regulatory framework for PRP therapies is not present
Devices must comply with Class II- medical device directive 93/42/EEC.
This committee is engaged in the establishment of quality, safety, and efficacy of blood products and in setting norms for collection, processing, and distribution of blood components across the European Union countries
Each country has its own approach to PRP regulation within the jurisdiction of national authorities
Device approval is overseen in each EU country by a governmental body called a ‘Competent Authority.’
The surgical use of PRP can be considered as an autologous graft within the surgical procedure as regulated by Directive 2004/23/EC
Europe Platelet-rich Plasma Market: Competitive Landscape
Major players operating in Europe include, Arthrex, Inc., Stryker Corporation, Johnson and Johnsons Ltd., Zimmer Biomet Holdings Inc., Terumo Corporation, Glofinn Oy, Medira Ltd., Regen Lab S.A., and Estar Technologies Ltd.
Europe Platelet-rich Plasma Market: Key Developments
In January 2020, SHVI PRP Therapy, announced a new website that is focused specifically at the use of PRP to mitigate hair loss.
In March 2019, CollPlant, a regenerative medicine company, renewed its exclusive distribution agreement with Arthrex for Vergenix STR, an injectable gel comprised of cross-linked bioengineered recombinant human type I collagen, rhCollagen, combined with autologous PRP, for the treatment of tendinopathy.
In January 2019, Generex Biotechnology Corporation entered into a letter of intent to acquire Medisource Partners, an FDA-registered distributor of medical and surgical products including supplies kits to process bone marrow aspirates and PRP biologics at the time of surgery.
In December 2018, Regenexx’s research published in the Journal of Translational Medicine, which involved use of patients' own bone marrow concentrate and PRP products demonstrated positive clinical outcomes for the treatment of osteoarthritis of the knee.
About Us- Coherent Market Insights is a global market intelligence and consulting organization focused on assisting our plethora of clients achieve transformational growth by helping them make critical business decisions. What we provide: Customized Market Research Services Industry Analysis Services Business Consulting Services Market Intelligence Services Long term Engagement Model Country Specific Analysis Mr. Shah
Coherent Market Insights Pvt.Ltd. Address: 1001 4th Ave, #3200 Seattle, WA 98154, U.S. Phone: +1–206–701–6702 Email: [email protected]
#EUROPE PLATELET-RICH PLASMA MARKET ANALYSIS#platelet-rich plasma#platelet-rich plasma market analysis#europe market analysis
0 notes
Text
How Dr. Saurabh Giri Approaches Complex Joint Cases with International Techniques
When it comes to complex joint conditions — such as revision surgeries, failed implants, or severely deformed joints — standard procedures often fall short. That’s where the expertise of a surgeon with international training becomes invaluable. Dr. Saurabh Giri, a leading joint replacement and arthroscopy surgeon in Pune and PCMC, brings global knowledge and advanced techniques to manage even the most challenging orthopaedic cases.
Global Training for Complex Cases
Dr. Giri has trained at world-renowned centers like:
Helios Endo Klinik, Germany — A high-volume revision joint replacement center
Santo Spirito Hospital, Italy — Specializing in minimally invasive hip surgery
Rome, Italy — SICOT Fellowship in Hip and Knee Arthroplasty with expertise in short stem and direct anterior approaches
These experiences exposed him to a wide spectrum of cases and cutting-edge solutions used in Europe’s top orthopaedic institutions.
Handling Revision Surgeries with Precision
Revision joint replacement is one of the most technically demanding orthopaedic surgeries. Dr. Giri’s approach includes:
Advanced pre-operative planning using 3D imaging
Use of modular and custom implants
Bone grafting and reconstruction of severe bone loss
Infection control strategies from international protocols
These techniques dramatically improve outcomes and reduce the risk of further revisions.
Direct Anterior Hip Replacement for Better Recovery
One of the advanced methods Dr. Giri uses is the direct anterior approach for hip replacement — learned during his training in Rome. This minimally invasive technique spares muscles and allows for:
Less post-operative pain
Faster recovery
Improved joint function
Earlier return to daily activity
Customized Care with Robotic Assistance
Dr. Giri integrates robotic technology into joint replacements to ensure precision, even in distorted anatomy or complex deformities. His dual leadership roles at Deccan Hardikar Hospital and Accord Hospital have helped him build surgical teams equipped to manage high-risk and unusual cases with confidence.
Conclusion
Complex joint cases require more than just experience — they require innovation, precision, and international perspective. With over 6000+ surgeries, global fellowships, and a patient-first mindset, Dr. Saurabh Giri is transforming joint care in Pune for even the most challenging orthopaedic conditions.
0 notes
Text
Technology in Orthopedic Surgery

Healthcare technology in orthopedic surgery is exciting and rapidly evolving. In my few short years as an orthopedic surgeon, I have seen the evolution of the Direct Anterior Approach for total hip replacements and the implementation of robotic assistance in total knee replacements. These technological advances promise faster recoveries and lower risk of complications. My personal history has prepared me to keep up with the latest trends in orthopedic surgery. As a millennial, I have always been good with computers. Growing up, I taught myself how to program computers and find tech to be interesting and exciting. As someone who has needed to wear hearing aids my whole life, I have seen how the evolution of hearing aids has allowed me to hear much better now than I did as a child. There are even hearing aids that exist now that can translate different languages, or play music from your phone! I understand how much of a difference technology can make in my life, and I know it can make a difference in my patient’s lives. As a young orthopedic surgeon, I have been blessed to have received the latest training in hip and knee reconstruction. I have presented new research at national meetings, keeping abreast of the latest technological updates. I think it is important to travel and see what other surgeons are doing across the nation and bring those new technologies back home to Hawaii. Read the full article
0 notes
Text
Best Orthopedic Surgeon in India
Welcare Hospital is one of the Best Orthopaedic hospital platforms in Gujarat and India. Dr. Bharat Mody is the Chief Orthopaedic surgeon and one of the Best Orthopaedic Surgeons of India. He has to his credit, an experience of having performed more than 40,000 Orthopaedic surgeries and procedures. He has a team of highly experienced and some of the best orthopedic doctors in India who are capable of handling all fields of Orthopaedics.

Tremendous advances have been made in orthopedic surgery since its inception over 250 years ago. Subspecialties such as Joint Replacement surgery, Arthroscopy, Spinal surgery, hand surgery and other such areas have made significant technological and biological advances in the past 40 years. These have developed into full fledged expertise areas in their own right, and deserve separate departments. Welcare hospital in Vadodara, Gujarat, has the most advanced Operation theatres in India. Dr. Bharat Mody has established the following departments in Orthopaedics: ARTHROSCOPY (Keyhole surgery of joints) Perhaps one of the most significant advances to occur in orthopedic surgery has been the addition of arthroscopic surgery, a minimally invasive technique. Prior to the introduction of endoscopic techniques, large incisions had to be made in order to obtain the surgical exposure needed to treat problems. With the introduction of endoscopic techniques came the ability to diagnose problems and even treat them without the subsequent morbidity that had accompanied many prior procedures. Recuperative time was greatly reduced. Because problems were frequently addressed at an earlier stage before the pathology had a chance to advance, results of operations were more likely to be successful. Arthroscopic surgery has revolutionized the approach to and treatment of joint disorders. Today, arthroscopy is performed on virtually all major joints of the body, and, because of its applications, the world has gained a greater understanding of joint mechanics, anatomy, and function. Its use continues to serve a vital role in the diagnosis and treatment of musculoskeletal ailments because of its high degree of clinical accuracy, low morbidity, infrequent complications, and quick recovery time. Additionally, the development and increased use of arthroscopic techniques have played major roles in the ability to perform surgical procedures on an outpatient basis, thereby saving money and resources. Dr. Bharat Mody is recognised as one of the best Arthroscopy surgeons of India. JOINT REPLACEMENT Before the advent of total joint arthroplasty, patients with significant arthritis of the hip or knee were often forced to endure their pain, with only minimal relief obtained by analgesic medications and other conservative treatments. Total joint arthroplasty (replacement) of the hip and the knee have been received with much enthusiasm by the orthopedic community because of their ability to relieve pain and restore function. The ideas and techniques initiated by the pioneers of joint replacement have given orthopedic surgeons the power to improve patients’ lives irrevocably and have forever changed the surgical treatment of arthritic joints. Today, total joint replacement of the hip and the knee are among the most successful surgical procedures performed by any specialty, with marked relief of pain and improved joint function in the majority of patients treated. Total joint replacement is a cost-effective procedure that significantly improves a patient’s quality of life and mobility. Dr. Bharat Mody is one of the best Knee and Hip Joint Replacement Surgeons of India. SPINE SURGERY Spinal surgery has also seen great improvements recently. Minimally invasive disc surgery and enhanced spinal fusions for degenerative disorders are significant advances. Spinal instrumentation, i.e., implantable devices used in the surgical treatment of spinal disorders, has been developed and can significantly correct spinal deformities that were previously untreatable. Likewise, rigid spinal fixation by the pedicle screw and other devices and advances in the techniques of vertebrectomy have improved the treatment of cancer patients with spinal metastases or patients with infection. Often, these treatments can result in significant pain relief and neurological recovery. FRACTURE SURGERY Improved fracture management: open reduction and internal fixation During the past few decades, there have been significant advances in the way orthopaedists treat fractures. Consequently, fractures are now healing more dependably and with less residual deformity than ever before. Patients treated for orthopedic trauma are more likely to subsequently lead normal lives without significant disability. One of the initial accomplishments of the AO/ASIF was the conception of 4 treatment principles that are still valid today. The first principle stresses the importance of obtaining an anatomical reduction of the fracture fragments, especially when the fracture extends into the joint. If closed methods of reduction prove inadequate, open reduction of the fragments by surgical means is carried out. Anatomic reduction is desired to prevent the development of posttraumatic arthrosis and to improve the chances of having a long-lasting and fully functional joint. The second principle is an extension of the first. After obtaining a good reduction of the fracture fragments, it is necessary to achieve stable fixation of the fragments to maintain the proper anatomic shape. This can be accomplished by a variety of methods ranging from external splints, such as plaster fixation, to internal fixation by plates, screws, wires, and intramedullary nails. Also included are transcutaneous splints—the so-called external fixators. Success of the modern fixation techniques over the past several decades has spawned substantial interest by equipment and instrument manufacturers to develop fracture stabilization equipment. The third principle is an important concept that has been increasingly recognized as a critical element for proper fracture healing. The preservation of the blood supply to the bone fragments and the soft tissue by means of atraumatic surgical techniques is vital in maintaining adequate nutrition to the fragments and preventing bone necrosis. Understanding of this simple concept is due in large part to the greater efforts of basic science researchers directed at the study of osteosynthesis. The fourth principle, early and pain-free mobilization, emphasizes the desire for early postoperative motion of the muscles and joints adjacent to the fracture. This concept was contrary to the opinion of the time—that prolonged immobilization was necessary for proper fracture healing to occur. The primary reason for advocating early, protected mobilization is that early motion prevents many of the undesirable sequelae that had, at that time, been accepted as unavoidable with the treatment of fractures. Problems, such as stiff joints, marked muscle atrophy, and osteoporosis, were common following immobilization, and more troublesome complications, such as pneumonia, decubitus ulceration, and deep vein thrombosis, were due in large part to prolonged recumbency. The move from an era in which prolonged immobilization was the mainstay of treatment to today’s emphasis on early motion and rehabilitation has improved, without compromise, fracture healing and posttraumatic musculoskeletal function. OTHER ADVANCES The major advances discussed above, i.e., arthroscopic surgery, joint replacement, and open reduction and internal fixation of fractures, have revolutionized the practice of orthopedic surgery as a whole, but by no means do we intend to imply that the list is comprehensive or that it represents the extent of improvement and development that has occurred in recent times. Indeed, great advances have been made within all the subspecialty areas of orthopedics. SPORTS MEDICINE Sports medicine has recently made great strides in the treatment of shoulder and knee pathology. An improved understanding of shoulder and knee mechanics has led to treatment strategies that are more likely to result in return of the athlete to sports.Procedures such as capsular shrinkage to stabilize the shoulder and arthroscopic reconstruction of the anterior cruciate ligament and partial meniscectomy in the knee are achieving this goal and hopefully resulting in long-term preservation of joint function. HAND SURGERY The subspecialty of hand surgery has acquired a valuable tool with the development of microsurgical techniques to perform technically challenging procedures such as nerve and small-vessel repair. Truly remarkable is the ability of surgeons, with the aid of an operating microscope, to re-implant a patient’s severed hand or arm with good recovery of limb function. PAEDIATRIC ORTHOPAEDIC SURGERY In paediatric orthopedics, one of the major areas of progress has been the greatly improved treatments now available for patients diagnosed with malignant bone tumours. These treatments have resulted in the increased survival of many patients whose diagnoses previously carried grave prognoses. Defects created by tumour resection are treated more effectively as well. Techniques such as distraction osteogenesis and bone transport now are used in the reconstruction of these bone defects and in cases in which significant trauma or infection has resulted in deformity. These relatively new technologies, originally used to correct limb length discrepancies in children, can dramatically correct limb deformity and restore function (10). Today, orthopedic researchers strive to improve orthopedic treatment modalities through better understanding of the composition, structure, and function of musculoskeletal tissues (2). Much knowledge has been gained in the past few decades regarding disease processes, such as rheumatoid and degenerative arthritis, and the body’s response to injury. Additionally, the areas of biomechanics and biomaterials have helped create the implants and prostheses that are now an integral part of orthopedic surgery. Research will continue at a never-before-seen pace and will certainly improve the understanding and treatment of musculoskeletal problems. Finally, it would be wrong for medical specialists today, especially orthopaedists, not to mention the contribution of diagnostic radiology in regard to diagnostic decision making. Computed tomography and magnetic resonance imaging have found a niche in orthopedics and are likely to remain as useful diagnostic tools. To know more, visit www.drbharatmody.com
0 notes
Link
Dr. Kaushal Malhan has expertise in techniques that changed the management of hip reconstructive surgery with a better outcome. He is the only surgeon offering the direct anterior approach for total hip replacement
0 notes
Text
Have Some Knowledge about Orthopedics and Some of Its Surgeries
In the current time, medical science has reached a different level. Things that were difficult in the last 30-40 years have now become easy and yes, people are taking benefits from various approaches. You may have heard about several departments of medical science that focus on providing treatment to different parts of the body. In this section, you will get to know about one of the chief branches that any of us may need at some point of life. We are talking about orthopedics that looks after the diagnosis, prevention, care, and treatment of the musculoskeletal system. Additionally, some information regarding various types of orthopedic surgery will be mentioned in the below section.
About Orthopedics
Our musculoskeletal system involves some of the major components of the body like:
* Muscles
* Bones
* Ligaments
* Soft Tissues
* Tendons
The specialist from this field is known as an orthopedist or an orthopedic doctor. Due to numerous events, a person may require visiting such professionals. For example, different kinds of pain like hip pain, knee pain, ankle pain, back pain, shoulder pain, foot pain, elbow pain, wrist or hand pain can bother a person. Some conditions like ligament tear, dislocated bone, muscle injury, compression fractures, or tendon injuries may also require immediate medical help.
Many conditions can settle down with the help of non-surgical approaches. Like, based on the problem, the orthopedic surgeon can recommend medicines, injections, or physical therapies. But, a lot of people have to go through orthopedic surgery as the last treatment option.
Let's know about some of the widely used surgeries.
1. Joint Replacement Surgery
You can find the presence of various joints in the body. Sometimes, their health can get upset due to some reasons. In cases when they become damaged or dysfunctional, the orthopedic surgeon recommends joint replacement surgery. It mainly comes into use when non-surgical methods don't prove valuable for the patient in reducing down his troubles. Here, the surgeon removes out the damaged joint and then replaces it with an artificial one called a prosthesis. People are taking benefits from a wide range of joint replacement surgeries like hip replacement, knee replacement, and shoulder replacement.
2. Arthroscopy
This minimally invasive surgery, also known as keyhole surgery, is used to find and treat the problems of the joint. If a person is suffering from damage, injury, or inflammation to the joint, the surgeon may guide him to have an arthroscopy. It can be used in almost every joint of the body but is mainly preferred for the knee, hip, shoulder, elbow, ankle wrist. The procedure of this orthopedic surgery involves making a small incision to the joint side and inserting a narrow telescope attached with a camera. The camera then delivers the inside view to the monitor outside by which the surgeon can identify what's happening to the joint.
3. Spinal Surgeries
A lot of issues are linked to the spine. That can be in the form of pain, movement problems, or injuries. Some conditions can be all right by non-surgical options. But in serious cases, implementing orthopedic surgery treatment becomes necessary. A wide range of spinal surgeries is there to observe in the orthopedic department. Some of them are spinal fusion, disc replacement, discectomy, laminectomy, vertebroplasty, kyphoplasty, and endoscopic spine surgery, etc.
4. ACL Reconstruction
ACL, full named as the anterior cruciate ligament is a vital ligament present in the knees. And yes, it is more at risk of suffering from an injury. This ligament can tear due to some activities that include sudden stops and changes in direction. ACL can't heal on its own. And especially when it is completely torn, there will be a need to go for orthopedic surgery treatment. During the procedure, the torn ligament is removed. The surgeon takes a piece of tendon from another part of the body or a deceased donor and then places it as a substitution.
5. Joint Fusion
Arthritis is a severe joint disease that can worsen the condition of our joints. If someone is suffering from the pain of arthritis, joint fusion can be an option. This orthopedic surgery apart from the joint replacement surgery proves to be effective in cases of damaged and painful joints. The procedure involves cutting off the ends of the bones along with damaged cartilage and then joining or fusing two ends of the bones. Consequently, it becomes stabilized and the motion remains absent in the joint. With the help of such procedures, a person finds relief from pain that has been done because of instability.
6. Soft Tissue Repair
There can be a presence of some soft tissue injuries in the life of a person. For example, tendinitis or bursitis. To fix such conditions, the surgeon may take help from orthopedic surgery.
7. Fracture Repair Surgery
If a fractured bone is placed in the wrong position, it will heal into an incorrect place. Thus, a person will have to face some problems. Some fractures call for a surgical treatment to hold the bone in its actual place. During this kind of orthopedic surgery treatment, the surgeon fixes the broken bone by using screws, pins, rods, and plates.
1 note
·
View note